What is arthropathy
Arthropathy is a disease of a joint.
What is facet arthropathy?
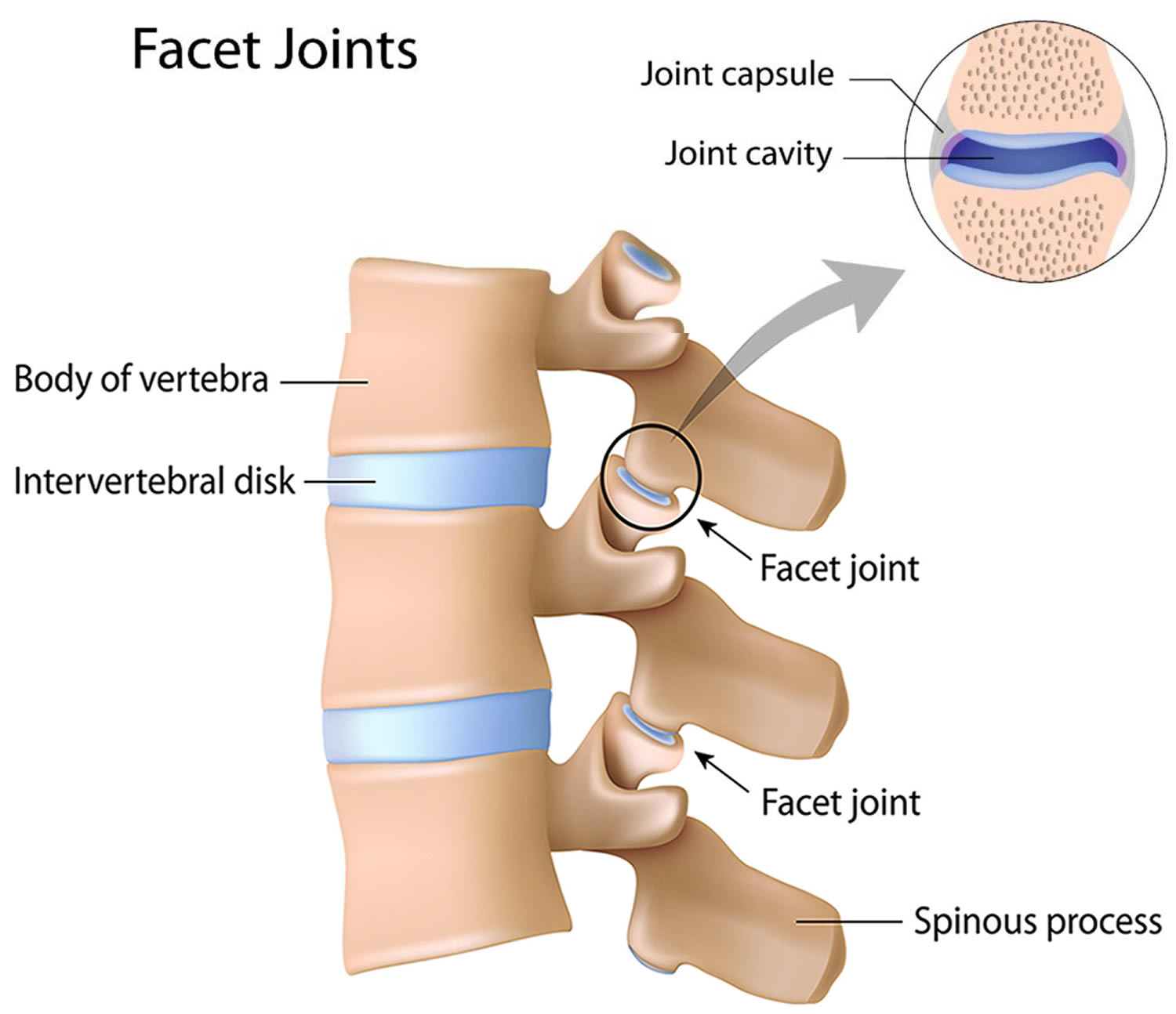
Facet arthropathy is a painful, arthritic condition of the facet joints also known as zygapophysial joints. The facet joints allow for bending, twisting, and alignment of the spine. The spinal nerves come off the spinal cord between the vertebra and the facet joints. At the front the vertebra rests on a spongy contained disc while at the back each of the two facet joints rest over the facet joint below it. In a healthy spine, the spinal disc and the facet joints support each other for healthy and safe movement.
Facet Arthropathy is often associated with chronic low back pain. Low back pain potential causes include defects of the ligaments that attach the muscles to the spinal discs, compression or pinching of the spinal cord roots, the hard, protective covering of the spinal cord known as the dura, muscle disorders of the lower spine and facet joints.
Figure 1. Facet arthropathy
What causes facet arthropathy?
Facet arthropathy can be affected by widespread arthritis of other joints seen in ankylosing spondylitis, psoriatic arthritis, and rheumatoid arthritis. Trauma such as small undiagnosed fractures, disc tears, cartilage splitting or haemorrhage in the area can be some associated findings.
Doctors regularly observe patients with damaged and dysfunctional spinal discs presenting with facet joint damage at the same level in their spine. Loss of disc height and function places increased stress on the facet joints at that level, which can then cause wear and damage over time.
Osteoarthritis can cause lumbar facet pain. People with low back pain can also demonstrate X-Ray evidence of osteoarthritis. The severity of the symptoms also correlate with the degree of damage seen on the CT scan. Unusual orientation of the facet joints and enlarged ligaments can be associated with facet disease.
The synovial capsule may become distended and inflamed which puts pressure on the spinal nerves. When combined with degenerative arthritis and joint instability, pain in facet syndrome results in lower back pain. Rheumatoid arthritis is associated with damage to facets especially the mid-lumbar and lower lumbar areas.
Facet arthropathy symptoms
Initial studies showed that facet joint pain is worse with extension and rotation of the spinal column. Other studies found increased pain during hyper-extension and rotation were not associated with relief from facet joint injection of numbing medication (pain blocks).
Location of the pain tends to be lateral and tends to radiate towards the knee, and those with central pain did not respond to pain blocks. These findings were refuted when another study concluded that knee pain was not associated with facet pain and that there are no reliable diagnostic criteria. Pain from Facet Arthropathy does not usually radiate to other areas such as the buttocks in sciatica or pain and numbness noted in spinal stenosis.
Facet arthropathy diagnosis
No specific X-Ray or imaging test such as CT or MRI is diagnostic of facet arthropathy as many of the same findings are found in asymptomatic patients. One promising test for the diagnosing this condition is the injection of anaesthetic agents into the joint. If an 80% improvement in pain occurs after the injection, a presumptive diagnosis of facet arthropathy can be made.
Facet arthropathy treatment
There are several options for treating the pain and symptoms caused by facet arthropathy:
1. Medications: Such as NSAIDs, Aspirin, Ibuprofen, Naproxen, and Toradol are helpful to reduce pain as are cyclo-oxygenase-2 Inhibitors such as Celecoxib, and analgesics Acetomenophen, known as Paracetamol or Tylenol.
2. Non-surgical treatments: Physical therapy, strengthening exercises, avoiding movements that aggravate the symptoms, and medications such as NSAIDs like ibuprofen and naproxen can be used.
Intra-joint injections and medial branch blocks of steroids/numbing medication under radiographic guidance and radiofrequency (RF) ablation to block the sensation of pain are two standard therapies. It appears that medial branch blocks and RF ablation are the best options with the lowest complication rates.
Shockwave therapy is another therapy that appears to be better than steroid injections and as effective as RF ablation with better long-term outcomes. Shockwave therapy uses the same technology that breaks up kidney stones. The idea of this therapy
3. Stem Cell Regeneration: Stem cell regeneration is a non-invasive and experimental treatment for damaged and painful facet joints. For many years patients have achieved promising results from targeted stem cell treatments of the hip and knee joints, and in the facet joint this is also possible. During the treatment, stem cells are carefully injected into the facet joints under CT imaging guidance by an orthopaedic specialist. The cells respond to inflammatory signals from the arthritic joint and start working to repair and regenerate the joint. This can be assisted with shockwave therapy (mentioned above) and other supportive therapies.
4. Spine Surgery: For patients who have exhausted conservative therapies, surgery may be an option to relieve the pain of facet arthropathy – in cases of nerve compression, spinal stenosis, spinal instability and associated motor or sensory symptoms.
Lumbar facet arthropathy
The lumbar zygapophysial joint, also known as facet joint, is a common generator of lower back pain. The facet joint is formed via the posterolateral articulation connecting the inferior articular process of a given vertebra with the superior articular process of the below adjacent vertebra. The facet joint is a true synovial joint, containing a synovial membrane, hyaline cartilage surfaces, and surrounded by a fibrous joint capsule 1. There is a meniscoid structure formed within the intra-articular folds. The facet joint is dually innervated by the medial branches arising from the posterior ramus at the same level and one level above the joint 2.
The facet joints play an important role in load transmission, assisting in posterior load-bearing, stabilizing the spine in flexion and extension, and restricting excessive axial rotation 2. Studies before and after facetectomy have shown that the facet joint may support up to 25% of axial compressive forces and 40% to 65% of rotational and shear forces on the lumbar spine 3.
Facet joint arthrosis is a pathological process involving the failure of the synovial facet joints 4. Degenerative changes begin with cartilage degradation, leading to the formation of erosions and joint space narrowing, and eventually sclerosis of subchondral bone. Risk factors include advanced age, a sagittal orientation of the facet joint, and concomitant intervertebral disk degeneration 5.
Estimates of the prevalence of lumbar facet-mediated pain have widely ranged in the literature, from under 5% to over 90% of patients reporting back pain. Many of these studies used a combination of history, physical exam, and radiologic findings, which have been shown to be unreliable in diagnosing facet pain. Studies following the criteria established by the International Association for the Study of Pain, involving controlled medial branch blocks, have implicated the lumbar facet joint as the source in 15% to 45% of the patients with chronic low back pain 6.
Age is strongly associated with the prevalence of lumbar facet arthropathy. According to one study, moderate to severe lumbar facet arthropathy was found in 36% of adults younger than age 45, 67% of adults age 45 to 64, and 89% of adults age 65 or older 7. Another study using lumbar CT and plain radiography found that women over the age of 50 are more likely to have facet joint osteoarthritis than men 8. The same study concluded that Caucasians are more likely to have facet joint osteoarthritis than African Americans. Body mass index (BMI) is another independent risk factor, with studies indicating increasing risk with higher BMI. BMI of 25 to 30 was found to increase the risk of facet joint osteoarthritis by 3 times normal, while a BMI of 30 to 35 was shown to have 5 times the risk of normal 9. Other independent risk factors noted are disk height narrowing, a sagittal orientation of the facet joint, and poor spinal extensors 4. Overall, lumbar facet osteoarthritis was found to be most prevalent at the L4-5 and L5-S1 levels. Less common are L3-L4 level, followed by the L1-2 and L2-3 levels 10.
Facet joint arthropathy causes
The cause of most lumbar facet pain is unknown. On occasion, the lumbar facet joints are affected by systemic inflammatory arthritides, such as rheumatoid arthritis and ankylosing spondylitis.
Facet joint arthrosis is a degenerative syndrome that typically occurs secondary to age, obesity, poor body mechanics, repetitive overuse and microtrauma 2. Numerous studies have linked facet joint degeneration to degeneration of intervertebral disks, showing that intervertebral disk degeneration likely occurs before facet joint arthrosis 11. One explanation for these findings is the increased mechanical changes in the loading of the facet joints following intervertebral disk degeneration. Other studies have demonstrated an increased propensity for facet joint degeneration with a more sagittal orientation of the facet joint 5.
Degenerative changes involving the facet joint begin with hyaline cartilage degradation, leading to the formation of erosions and joint space narrowing, and eventually sclerosis of subchondral bone. Studies have shown that over time the posterior capsule of the degenerative joint capsule becomes hypertrophied, with fibrocartilage proliferation and possibly synovial cyst formation. Osteophytes are likely to arise at the attachment sites (entheses) where the fibrocartilage extends beyond the original joint space 12. Facet mediated pain occurs secondary to these arthritic changes, as there is rich innervation of the entire joint complex. Other theories behind facet-mediated pain include, but are not limited to, facet intraarticular meniscoid entrapment and synovial impingement.
Microtrauma
- Microtrauma of the facet joints can produce pain. Small fractures, capsular tears, splits in the articular cartilage, and hemorrhage have been documented on postmortem studies of trauma victims who had normal radiographic findings. Whether these abnormalities were painful was not recorded.
Osteoarthritis
Osteoarthritis is another cause of lumbar facet joint pain. However, not all cases of facet arthritis are painful; the radiographic changes of osteoarthritis are as common in patients with low back pain as in those without it. Some studies report that severely degenerated joints are more likely to cause symptoms. In a 2008 report, multidetector computed tomography (CT) scanning in 188 individuals revealed lumbar facet osteoarthritis in 59.6% of males and 66.7% of females 13. In this study population, however, the report found no association between osteoarthritis at any level of the lumbar spine and the development of low back pain.
Reports indicate that the orientation of the facet joints is associated with the development of spinal osteoarthritis. In a study of 150 patients, Linov et al found that a particularly sagittal orientation of the L4 and L5 facet joints appeared to be linked to the disease 14.
A study by Yoshiiwa et al. 15 indicated that ligamentum flavum hypertrophy is related to severe facet joint osteoarthritis, as well as to lumbar segmental instability and severe disk degeneration and a sagittalized facet joint orientation.
Synovial capsule distention and inflammation
Dory attributed low back pain from facet syndrome to distention and inflammation of the synovial capsule, with resultant stimulation of the nociceptive nerve endings 16. Expanded synovial recesses may also compress nerve roots in the spinal canal and neural foramina, which may explain the presence of radicular pain in patients with facet syndrome. Lippitt attributed pain in facet syndrome to a combination of synovitis, segmental instability, and degenerative arthritis 17.
Rheumatoid arthritis
Using magnetic resonance imaging (MRI) scans, a study by Yamada et al. 18 of 201 patients with rheumatoid arthritis found erosion of the lumbar facets and endplates in 76.6% and 70.6% of patients, respectively, with the erosion occurring at 38.7% and 33.8% of intervertebral levels, respectively. Facet and endplate erosion both occurred most commonly at the midlumbar and lower-lumbar areas. A correlation was seen between facet erosion and the presence of spondylolisthesis.
Other
Other theories regarding the causes of low back pain include meniscoid entrapment, synovial impingement, joint subluxation, chondromalacia facette, capsular and synovial inflammation, mechanical injury to the joint capsule, and the restriction of normal articular motion from soft or articular causes.
A study by Hawellek et al. 19 found a positive correlation between the amount of cartilage calcification in the lumbar facet joints and degeneration of the facet joints and intervertebral disks. The study did not find cartilage calcification in the lumbar facet joints to be associated with patient age, although a correlation was found between age and cartilage calcification in the lumbar intervertebral disks.
Differential diagnoses for lumbar facet arthropathy include, but are not limited to:
- Lumbar herniated disc
- Discogenic pain syndrome
- Lumbosacral radiculopathy
- Piriformis syndrome
- Paraspinal muscle/ligament sprain/strain
- Lumbar spondylosis/spondylolysis/spondylolisthesis
- Rheumatoid arthritis (more common in cervical)
- Seronegative spondyloarthritis (most commonly ankylosing spondylitis, psoriatic arthritis, reactive arthritis)
- Gout, pseudogout
- Diffuse idiopathic skeletal hyperostosis
- Sacroiliac joint dysfunction
- Thoracolumbar fascia dysfunction
- Infection
- Neoplasm
- Fibromyalgia
Lumbar facet arthropathy diagnosis
Lumbar facet joint pain will typically present as unprovoked chronic lower back pain. The pain can have varying features, and it is impossible to diagnose based on history and physical exam alone. Clues that may point to the facet as the pain generator include pain localized over the back with a non-dermatomal radiation pattern. In the lumbar spine, the referred pain is typically around the buttock and thigh and is rarely felt below the knee 20. Numbness and weakness of the lower extremities are unlikely. However, patients with osteophytes, large synovial cysts, or facet hypertrophy may have accompanied lumbar radiculopathy via nerve root irritation. Other neurological signs, such as bowel and bladder dysfunction, should point the practitioner away from the facet as a pain generator.
Physical examination of the patient with facet pain may reveal tenderness to palpation over the lumbar paravertebral region over the transverse processes and paraspinal muscles. Pain may be exacerbated by spinal extension and rotation. Neurological findings, such as lower limb sensation, motor strength, and deep tendon reflexes will be normal. However, lower extremity strength may be diminished secondary to pain. The Kemp test (otherwise known as the quadrant test and extension-rotation test) is a provocative test that has been described as being potentially useful for diagnosing facet joint pain. In this maneuver, a patient performs combined extension and rotation of the spine, with a positive test defined as the reproduction of pain. However, studies have shown that the Kemp test has poor diagnostic accuracy, with a sensitivity under 50% and specificity under 67% 21.
The gold standard for diagnosis of facet-mediated pain is an anesthetic block of the facet joint 22. However, imaging remains a useful tool to rule out other causes of suspected lower back pain, including but not limited to disk herniation, spinal stenosis, spondylolisthesis, ankylosing spondylitis, diffuse idiopathic skeletal hyperostosis, infection, or neoplasm. Moreover, it is not uncommon to have concomitant facet joint degeneration along with the above alternative causes of lower back pain.
Classic radiographic findings in facet joint arthrosis include both degenerative and proliferative features. Imaging may reveal narrowing of the facet joint space, subarticular bone erosions, subchondral cysts, osteophyte formation, and hypertrophy of the articular process 4. Standard lumbar radiographs (x-ray) have limited value and should contain oblique views, as the facet joints are in an oblique position. However, oblique x-ray has only 55% sensitivity and 69% specificity in distinguishing the presence of facet joint disease 23. While some studies have reported MRI as more than 90% sensitive and specific in visualizing facet degeneration, others have shown that MRI is less sensitive than CT in depicting the bony cortex margin 23. Thus, CT remains the preferred evaluation method for imaging of facet arthropathy due to a more precise demonstration of bony details and relatively lower cost than MRI. However, MRI remains a superior diagnostic tool to rule out non-facet mediated pain. Other imaging techniques, such as bone scintigraphy with SPECT may be useful to depict bone areas with synovial changes and degenerative remodeling.
The diagnostic block of the facet joint is the most reliable means for diagnosing facet-mediated pain, with level I or level II evidence based on the United States Preventive Services Task Force criteria 24. Both intra-articular injections of the facet joint and medial branch blocks are equally effective; however, both have their drawbacks. Studies have also shown comparable accuracy between fluoroscopic guided and ultrasound-guided injection, although ultrasound is less accurate in obese patients. Intra-articular injection involves the injection of local anesthetic directly into the facet joint capsule. The joint capsule is so small that after injection of 1 to 2 mL of fluid the capsule is likely to rupture, spreading anesthetic to other surrounding possible pain-generating structures. In comparison, the medial branch block involves the injection of local anesthetic at the medial branch divisions of the dorsal rami at the level of and one above a given facet joint. A successful diagnostic block is considered if there is greater than or equal to 80% pain relief post-injection. Since the medial branch innervates many other possible local pain generating structures, including paraspinal muscle, fascia, ligaments, sacroiliac joint, there is a high false-positive rate (reported up to 25% to 40%) 6. It has therefore been suggested to perform a double diagnostic block. However, this is rarely practiced due to the risk of patient drop-out, cost-effectiveness, and an increased complication rate.
Lumbar facet arthropathy treatment
Treatment of chronic lower back pain begins with conservative management. This is true for facet mediated pain, even in the absence of confirmation via a diagnostic block. Physical therapy is a cornerstone of the treatment of chronic lower back pain and should include postural education, stretching, and exercises tailored to strengthen the core musculature. Pain medications, including nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen, are widely considered the first line for treatment of lower back pain. Adjuvant medications, such as antidepressants in chronic back pain and muscle relaxants in acute back pain have also demonstrated effectiveness.
No studies have compared the efficacy of one type of physical therapy over another in the treatment of lumbar facet arthropathy. Once the diagnosis of facet joint pain has been confirmed and pain has been brought under control with appropriate treatment, experienced clinicians generally recommend physical therapy for reconditioning, as well as lumbar stabilization exercises.
Patients who fail trial conservative management are considered candidates for a diagnostic block. If the diagnostic block is successful, more invasive treatment can be considered. Intra-articular steroid injections are a controversial treatment, with level III evidence to support their use 25. Radiofrequency neurotomy, via continuous, high-temperature medial branch radiofrequency ablation, carries level II evidence 26. Due to axonal regeneration, pain may return requiring repetition of the procedure, typically between 6 months to 1 year. Other reported interventions include pulsed radiofrequency ablation, cryo-denervation, and phenol neurolysis; however, these studies are uncontrolled and require further evaluation.
Facet mediated pain is rarely an indication for surgical intervention in itself. Studies have not demonstrated evidence for surgical intervention except in cases of traumatic dislocation. However, due to facet arthropathy, osteophytes or large synovial cysts may impinge upon other surrounding structures and lead to stenosis, nerve root impingement, and radiculopathy. In such cases, lumbar facetectomy may be performed. Medial facetectomy is the most commonly performed form of facetectomy and is often performed in conjunction with laminectomy. Complete facetectomy may be performed in the setting of lumbar fusion.
Lumbar facet arthropathy complications
Serious complications of facet intervention are rare. Intraarticular steroid injections carry the risk of metabolic and endocrine side effects related to elevated glucose levels and suppression of the hypothalamic-pituitary-adrenal access; however, there have been no studies reported to date. There have been case reports of infection following intraarticular steroid injection, including septic arthritis, epidural abscess, and meningitis. Other complications include dural puncture and spinal anesthesia.
The most common complication of radiofrequency neurotomy is neuritis, with a reported incidence of 5% 6. There have also been reports of transient numbness and/or dysesthesias. Other rare complications include burns, which may result from electrical faults.
Lumbar facet arthropathy prognosis
Facet arthropathy will increase with age. Conservative management, such as physical therapy is the first line in management. Patients who fail to respond to a trial of physical therapy may undergo diagnostic block of the facet joint. Successful radiofrequency neurotomy has been demonstrated to relieve pain for 6 months to up to 1 year, at which point repeat procedure may be indicated.
- Glover JR. Arthrography of the joints of the lumbar vertebral arches. Orthop. Clin. North Am. 1977 Jan;8(1):37-42[↩]
- Mann SJ, Singh P. Lumbar Facet Arthropathy. [Updated 2019 Mar 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538228[↩][↩][↩]
- Abumi K, Panjabi MM, Kramer KM, Duranceau J, Oxland T, Crisco JJ. Biomechanical evaluation of lumbar spinal stability after graded facetectomies. Spine. 1990 Nov;15(11):1142-7[↩]
- Gellhorn AC, Katz JN, Suri P. Osteoarthritis of the spine: the facet joints. Nat Rev Rheumatol. 2013 Apr;9(4):216-24[↩][↩][↩]
- Kalichman L, Hunter DJ. Lumbar facet joint osteoarthritis: a review. Semin. Arthritis Rheum. 2007 Oct;37(2):69-80[↩][↩]
- Cohen SP, Raja SN. Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet) joint pain. Anesthesiology. 2007 Mar;106(3):591-614[↩][↩][↩]
- Suri P, Miyakoshi A, Hunter DJ, Jarvik JG, Rainville J, Guermazi A, Li L, Katz JN. Does lumbar spinal degeneration begin with the anterior structures? A study of the observed epidemiology in a community-based population. BMC Musculoskelet Disord. 2011 Sep 13;12:202[↩]
- Goode AP, Marshall SW, Renner JB, Carey TS, Kraus VB, Irwin DE, Stürmer T, Jordan JM. Lumbar spine radiographic features and demographic, clinical, and radiographic knee, hip, and hand osteoarthritis. Arthritis Care Res (Hoboken). 2012 Oct;64(10):1536-44[↩]
- Suri P, Katz JN, Rainville J, Kalichman L, Guermazi A, Hunter DJ. Vascular disease is associated with facet joint osteoarthritis. Osteoarthr. Cartil. 2010 Sep;18(9):1127-32.[↩]
- Kalichman L, Li L, Kim DH, Guermazi A, Berkin V, O’Donnell CJ, Hoffmann U, Cole R, Hunter DJ. Facet joint osteoarthritis and low back pain in the community-based population. Spine. 2008 Nov 01;33(23):2560-5[↩]
- Butler D, Trafimow JH, Andersson GB, McNeill TW, Huckman MS. Discs degenerate before facets. Spine. 1990 Feb;15(2):111-3[↩]
- Boszczyk BM, Boszczyk AA, Korge A, Grillhösl A, Boos WD, Putz R, Milz S, Benjamin M. Immunohistochemical analysis of the extracellular matrix in the posterior capsule of the zygapophysial joints in patients with degenerative L4-5 motion segment instability. J. Neurosurg. 2003 Jul;99(1 Suppl):27-33.[↩]
- Kalichman L, Li L, Kim DH, et al. Facet joint osteoarthritis and low back pain in the community-based population. Spine. 2008 Nov 1. 33(23):2560-5[↩]
- Linov L, Klindukhov A, Li L, et al. Lumbar facet joint orientation and osteoarthritis: a cross-sectional study. J Back Musculoskelet Rehabil. 2013. 26(4):421-6[↩]
- Yoshiiwa T, Miyazaki M, Notani N, Ishihara T, Kawano M, Tsumura H. Analysis of the Relationship between Ligamentum Flavum Thickening and Lumbar Segmental Instability, Disc Degeneration, and Facet Joint Osteoarthritis in Lumbar Spinal Stenosis. Asian Spine J. 2016 Dec. 10 (6):1132-1140.[↩]
- Dory MA. Arthrography of the lumbar facet joints. Radiology. 1981 Jul. 140(1):23-7.[↩]
- Lippitt AB. The facet joint and its role in spine pain. Management with facet joint injections. Spine. 1984 Oct. 9(7):746-50.[↩]
- Yamada K, Suzuki A, Takahashi S, et al. MRI evaluation of lumbar endplate and facet erosion in rheumatoid arthritis. J Spinal Disord Tech. 2014 Jun. 27(4):E128-35.[↩]
- Hawellek T, Hubert J, Hischke S, Rolvien T, Krause M, Püschel K, et al. Microcalcification of lumbar spine intervertebral discs and facet joints is associated with cartilage degeneration, but differs in prevalence and its relation to age. J Orthop Res. 2017 Dec. 35 (12):2692-9.[↩]
- Dreyfuss P, Halbrook B, Pauza K, Joshi A, McLarty J, Bogduk N. Efficacy and validity of radiofrequency neurotomy for chronic lumbar zygapophysial joint pain. Spine. 2000 May 15;25(10):1270-7[↩]
- Stuber K, Lerede C, Kristmanson K, Sajko S, Bruno P. The diagnostic accuracy of the Kemp’s test: a systematic review. J Can Chiropr Assoc. 2014 Sep;58(3):258-67[↩]
- Manchikanti L, Hirsch JA, Pampati V. Chronic low back pain of facet (zygapophysial) joint origin: is there a difference based on involvement of single or multiple spinal regions? Pain Physician. 2003 Oct;6(4):399-405[↩]
- Kalichman L, Hunter DJ. Lumbar facet joint osteoarthritis: a review. Semin. Arthritis Rheum. 2007 Oct;37(2):69-80.[↩][↩]
- Datta S, Lee M, Falco FJ, Bryce DA, Hayek SM. Systematic assessment of diagnostic accuracy and therapeutic utility of lumbar facet joint interventions. Pain Physician. 2009 Mar-Apr;12(2):437-60[↩]
- Manchikanti L, Kaye AD, Boswell MV, Bakshi S, Gharibo CG, Grami V, Grider JS, Gupta S, Jha SS, Mann DP, Nampiaparampil DE, Sharma ML, Shroyer LN, Singh V, Soin A, Vallejo R, Wargo BW, Hirsch JA. A Systematic Review and Best Evidence Synthesis of the Effectiveness of Therapeutic Facet Joint Interventions in Managing Chronic Spinal Pain. Pain Physician. 2015 Jul-Aug;18(4):E535-82[↩]
- Civelek E, Cansever T, Kabatas S, Kircelli A, Yilmaz C, Musluman M, Ofluoglu D, Caner H. Comparison of effectiveness of facet joint injection and radiofrequency denervation in chronic low back pain. Turk Neurosurg. 2012;22(2):200-6[↩]