Contents
Atypical mycobacterial infections
Atypical mycobacterial infections also called non-tuberculous mycobacterial infections or non-tuberculous mycobacterium infections are infectious diseases that are caused non-tuberculous mycobacteria which are aerobic acid-fast bacilli that are resistant to acid and alcohol 1, 2, 3, 4, 5, 6. Atypical mycobacteria include all mycobacteria other than “typical” mycobacteria which are Mycobacterium tuberculosis that commonly cause tuberculosis (TB) in human, Mycobacterium bovis another mycobacterium that can cause tuberculosis (TB) disease in people, and Mycobacterium leprae that cause leprosy or Hansen disease 7.
Atypical mycobacterial infections may cause life-threatening disease in people with weakened immune systems (immunocompromised individuals). Atypical mycobacteria or nontuberculous mycobacteria can cause various diseases such as skin and soft tissue infection, lymphadenitis (infection or inflammation of lymph node), lung infection, disseminated infection, and a wide range of more rarely encountered infections 2. Infections with atypical mycobacteria (non-tuberculous mycobacteria) frequently occur after surgical procedures, penetrating accidental trauma, acupuncture, intravenous catheter use, intramuscular injections, subcutaneous injections, mesotherapy (alternative medicine therapy that uses micro-fine needles to inject vitamins into the middle layer of the skin or the mesoderm) and superficial skin abrasions 8, 9, 10. Several cases of atypical mycobacterial infections are caused by tattoos 11, 12, 13, 14, 15, cosmetic treatments 16, 17, 18, botulinum toxin injections 19, implant surgeries 20., have been described. Also, outbreaks of atypical mycobacterial infections related to contaminated instruments have been described in hospitals 21.
The non-tuberculous mycobacteria that most commonly cause atypical mycobacterial infection are most commonly found in the soil, indoor and outdoor water sources, and are recognized to colonize poorly sterilized medical equipment 2. Atypical mycobacteria (non-tuberculous mycobacteria) most commonly infect young children, immunocompromised individuals, individuals with indwelling medical equipment, and those who have recently undergone surgical or non-surgical procedures 2.
Atypical mycobacteria (non-tuberculous mycobacteria) bacteria can be further categorized into slow and rapidly growing organisms and grouped by the organ systems they commonly affect. Due to their size, shape and growth patterns, atypical mycobacteria are difficult to identify on diagnostic testing 2.
Atypical mycobacterium treatment often requires extended courses of combination antibiotic therapy, frequently with surgical intervention 22, 23. There are specific antibiotics for each family of atypical mycobacteria, because they are resistant to most antibiotic drugs and single therapy may be inadequate 24. This difficulty in treating atypical mycobacterial infections can lead to serious health complications, including death 25.
Figure 1. Atypical mycobacterial infection after skin tattoos
Footnote: Atypical mycobacterial infection after skin tattoos. Tattooed area of the right lower leg showing (A) thickened reddish bumps (indurated erythematous papules) and crust involving the tattoo on presentation (note the eruption appears to conform to the areas of soft shading through the rose design, sparing the distal lettering) and (B) clearing of skin bumps (papules) and reduced redness (erythema) after 4 months of combination antibiotic therapy, leaving some areas of residual post inflammatory hyperpigmentation and an area of hypopigmented scarring
[Source 26 ]Figure 2. Atypical mycobacterial infection tattoo
Footnote: Atypical mycobacterial infection after skin tattoos. Pustules located in the black- and gray-shaded areas of a patient’s tattoo (culture positive for Mycobacterium abscessus).
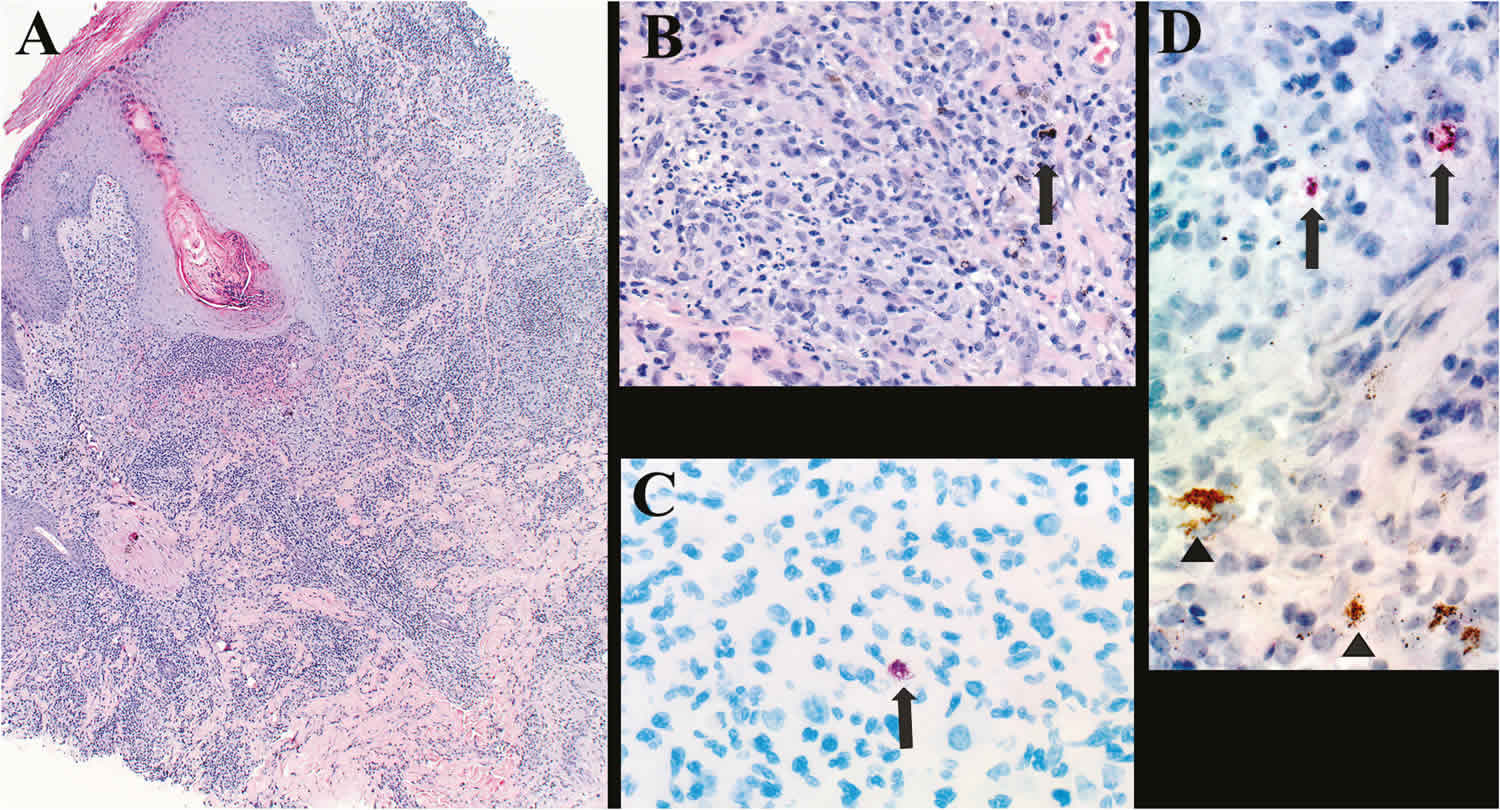
[Source 27 ]Figure 3. Atypical mycobacterial infection skin histopathology
Footnotes: Histopathology of tattoo-associated atypical mycobacterial infection. (A) Low-power photomicrograph of skin biopsy showing mixed acute and chronic inflammation with focal granulomatous areas as seen using hematoxylin and eosin (H&E) stain. (B) Higher-power magnification showing granulomatous inflammation with deposits of tattoo pigment (arrow) as seen by H&E stain. (C) Cluster of mycobacteria (arrow) as seen by Ziehl–Neelsen acid-fast stain. (D) Immunostaining (arrows) of mycobacteria as seen using Mycobacterium species immunohistochemical assay and brownish tattoo pigment (arrowheads). Original magnifications: 12.5× 100× 158× 158×.
[Source 27 ]Figure 4. Buruli ulcer caused by Mycobacterium ulcerans
[Source 28 ]Atypical mycobacterial infection cause
The most commonly encountered atypical mycobacteria that cause the majority of infection in humans are the Mycobacterium avium complex bacteria (MAC), Mycobacterium avium, and Mycobacterium intracellulare also known as Mycobacterium avium-intracellulare (MAI), Mycobacterium kansasii, Mycobacterium marinum, Mycobacterium ulcerans, Mycobacterium abscessus complex bacteria (abscessus, massiliense, and bolletii), Mycobacterium chelonae, and Mycobacterium fortuitum 2. These atypical mycobacteria (non-tuberculous mycobacteria) are most commonly found in the soil, indoor, and outdoor water sources and are recognized to colonize poorly sterilized medical equipment. Atypical mycobacteria most commonly infect young children, immunocompromised individuals, individuals with indwelling medical equipment, and those who have recently undergone surgical or non-surgical procedures. The type of disease caused by atypical mycobacteria is dependent on the mode of inoculation and the susceptibility of the host to infection. Lung infection occurs via inhalation of aerosolized material containing the bacteria, whereas lymphadenitis is often caused by ingestion or penetration through the soft tissues, and skin and soft tissue infection by access through skin breakdown or by indwelling medical equipment 22, 23.
Mycobacterium avium complex bacteria (MAC) or Mycobacterium avium-intracellulare (MAI) infection of lung is most commonly found in adults and those with impaired host defense of the lung, such as human immunodeficiency virus (HIV), patients on TNF-alpha inhibitors, and cystic fibrosis (CF) 2. Adult with atypical mycobacterial infection of the lung preferentially impacts White, middle-aged, or older men, who often have comorbid conditions such as chronic obstructive pulmonary disease (COPD), alcohol use, or tobacco use 2. A less common presentation referred to as “hot tub lung” can be seen as part of a hypersensitivity syndrome following mycobacterium avium complex bacteria (MAC) exposure related to bathing or recreational water exposure. Disseminated mycobacterium avium complex bacteria (MAC) or mycobacterium avium-intracellulare (MAI) is primarily observed in patients with significantly immunocompromised states such as acquired immunodeficiency syndrome (AIDS) 29, 30, 31, 32.
One important feature of most atypical mycobacteria is that they are acid-fast bacilli (AFB) 2. This staining property detected via the Kinyoun method is due to its hydrophobic mycolic acid outer layer. This mycolic acid layer allows them to form thick biofilms, enabling their survival in harsh environments that are not as well tolerated by other bacteria 2. These biofilms stunt the ability of antibiotics to penetrate the atypical mycobacteria effectively. The biofilms allow the atypical mycobacteria to survive in varying temperatures and protect the bacteria from being killed by water purifying chemicals such as chlorine, disinfectants, and cleaning products 2. The biofilms also allow these atypical mycobacteria to survive in oxygen-rich and anaerobic environments. Another defining characteristic of mycobacteria is their slow rate of growth.
Atypical mycobacteria are divided into rapid and slow-growing categories 2. The rapid-growing atypical mycobacteria take 7 to 30 days to grow on culture. The slow-growing atypical mycobacteria will take several weeks to months to demonstrate growth.
Atypical mycobacterial infection of lymph node (atypical mycobacterial lymphadenitis)
According to the American Thoracic Society and Infectious Disease Society of America, Mycobacterium avium complex (MAC) bacteria cause approximately 80% of atypical mycobacterial infections in children 2. Mycobacterial cervical lymphadenopathy is caused by tuberculous mycobacteria in 64% and by atypical mycobacteria in 36% of cases 33. The progression of atypical mycobacterial lymphadenitis has been described in four stages by Toretta et al. 2. The first stage describes a unilateral submandibular, preauricular, or cervical chain lymph node that slowly and painlessly enlarges over several days to months. Stage one was noted by the author to be unlikely to show systemic symptoms. Stage two describes the presence of tenderness indicative of necrosis within the lymph node. Stage three describes erythematous discoloration of the overlying skin. Stage four describes the progression of skin breakdown to the formation of sinus tracts.
Atypical mycobacterial infection of lung
The three species that make up the vast majority of atypical mycobacterial lung infections are the Mycobacterium avium complex bacteria (approximately 80%), Mycobacterium kansasii, and Mycobacterium abscessus 2. Mycobacterium avium complex infections can be further grouped into two different presentations. The first presentation is found more commonly in middle-aged males with the risk factors of long term alcohol and tobacco abuse. In these patients, the MAC bacteria tend to form large fibrocavitary lesions in the apex of the lung. These lesions can rapidly progress to encompass significant areas of the lung within 1 to 2 years and generally result in morbidity and mortality at a much faster rate. The second type of presentation of Mycobacterium avium complex lung disease more commonly affects postmenopausal caucasian women. In this presentation, the bacteria form small pulmonary nodules and cylindrical bronchiectasis with a concentration of nodules in the right middle lobe and ligula of the left upper lobe of the lungs. Similar presentations to Mycobacterium avium complex lung disease are seen with Mycobacterium kansasii and Mycobacterium abscessus. Mycobacterium kansasii tends to form large fibrocavities in the apex of the lung, similar to the first type of Mycobacterium avium complex disease presentation. A much smaller proportion of infections resemble the nodular and bronchiectatic type of presentation 2. Mycobacterium abscessus infection presents the majority of the time with a nodular and bronchiectatic presentation concentrated in the upper lung fields. Mycobacterium abscessus will form fibrocavities in approximately 15 percent of infections.
Atypical mycobacterial infection of skin and soft tissue
Atypical Mycobacteria enter the skin and soft tissue through trauma, surgical procedures, or via indwelling medical equipment 2. All species of atypical mycobacteria can cause skin and soft tissue infection 2. The most common species to cause skin and soft tissue infection are Mycobacterium chelonae, Mycobacterium abscessus, Mycobacterium fortuitum, Mycobacterium ulcerans, and Mycobacterium marinum.
Mycobacterium marinum infection is also known as the fish tank granuloma, after originally being discovered to cause soft tissue infection in fish tank workers or enthusiasts. It most commonly causes localized erythema and granuloma formation of the digits, which can progress to nodular lymphangitis of the hands and forearms similar in appearance to sporotrichosis. These bacteria more rarely can affect tendons, joint spaces and cause osteomyelitis. Immunocompromised patients have had recorded cases of disseminated infection.
Mycobacterium ulcerans is also known as the Buruli ulcer (Figure 4). Buruli ulcers are known for their large areas of destructive lesions of skin, deep ulceration, and soft tissue and even bone involvement. Buruli ulcers most commonly begin as a small, painless nodule, which slowly begins to ulcerate. Buruli ulcers are characterized by poorly defined and irregular borders and can cover extensive sections of the body. Other variations of these lesions may also begin as localized erythema, subcutaneous edema, or a violaceous skin rash. Of note, approximately 15% of Mycobacterium ulcerans infections cause osteomyelitis.
Mycobacterium fortuitum most commonly presents as a solitary subcutaneous nodule. The majority of cases of Mycobacterium fortuitum infection have low morbidity and limited infection. Immunocompromised patients, however, have been known to suffer from the more serious and disseminated infection.
Mycobacterium abscessus most commonly forms an abscess under the site of skin trauma/penetration. These abscesses are painful to the touch, may form draining sinus tracts, and may progress to ascending lymphadenitis. Disseminated disease can occur in immunocompromised individuals and produce diffuse subcutaneous nodules with lymphadenitis.
Mycobacterium chelonae presents in the majority of cases as small disseminated cutaneous nodules that are painful to the touch. The skin surrounding these lesions is often hyperpigmented. Lesions may also drain, form sinus tracts, appear as cellulitis or non-healing ulcers. Infection is most common in immunocompromised patients. Mycobacterium chelonae has also been known to cause osteomyelitis 22, 34, 35, 36.
Atypical mycobacterial infection signs and symptoms
Atypical mycobacterial lymph node infection (atypical mycobacterial lymphadenitis)
The majority of atypical mycobacterial lymphadenitis cases will present in children under the age of five whose parents have noticed one or more soft but firm, unilateral, subcutaneous masses, usually in the submandibular or cervical chain regions. The masses are usually non-tender at the beginning of the disease, followed by the later development of fluctuance and even purulent discharge from fistulizing tracts. A diagnosis of mycobacterial lymphadenitis is frequently suspected after enlarged cervical nodes in children fail to respond to empiric antibiotic therapy directed at Staphylococcus and Streptococcus or fail to resolve under watchful-waiting for a presumed viral process.
Atypical mycobacterial lung infections
Atypical mycobacterial lung infection typically presents in patients with impaired host defense of the lung. This includes patients with cystic fibrosis, chronic obstructive pulmonary disease (COPD), HIV, and other immunodeficiency syndromes 2. In patients without known immunodeficiency syndromes, patients are more often male, middle-aged or older, and have a history of comorbid alcohol and/or tobacco abuse. These patients present with cough and worsening lung function in all cases but can also present with pneumonia, hemoptysis, persistent fever, and weight loss 2. These patients tend to have a much more rapidly progressing disease. Another subset of patients with a more slowly progressing disease and similar symptoms has been identified as women who have undergone menopause, have a lower body mass index (BMI), scoliosis, or rib cage abnormalities 22, 23.
Atypical mycobacterial skin and soft tissue infections
Atypical mycobacterial skin and soft tissue infections can result from localized or disseminated infection and occur in patients of all ages 2. Patients with localized lesions may give a history in which they experienced trauma to their skin while swimming (freshwater, saltwater, swimming pool, hot tubs). Other risk factors for skin and soft tissue infections include patients who are currently immunosuppressed or have had recent surgical procedures. Skin lesions can range from erythematous papules/nodules that progressively ulcerate, to ecthyma, resembling cellulitis. A separate category of skin lesion, the Buruli ulcer, is characteristic of a painless area of soft tissue swelling that slowly begins to ulcerate with poorly defined and irregular borders. Untreated, they can grow from a few centimeters to span large areas of the body. Patients with these lesions are usually from West Africa, Central, and South America, Australia, and Japan 2.
Atypical mycobacterial infection complications
Atypical mycobacterial lymphadenitis can result in fistula formation and repeated need for surgical intervention 2. Excision of preauricular lymph nodes risks paralysis of the facial nerve as it courses through the underlying parotid gland 2. Repeated surgical procedures and scarring from the skin and soft tissue infection can result in cosmetic disfiguration 2. Since most lymphadenitis cases occur in the neck and facial region lymph nodes in young children, careful consideration of the psychosocial consequences of cosmetic disfiguration from repeated surgical procedures must be weighed against the chances of improved outcomes. The curative rate with antibiotics alone ranges from approximately 66% to 73%, which increases to around 95% with surgical intervention.
The ability of patients with advanced age and multiple comorbidities to tolerate the prolonged combination of antibiotic therapy or possible surgical intervention required to treat atypical mycobacterial lung infection necessitates the discussion of chronic suppressive therapy vs. curative therapy. Clarithromycin can cause gastrointestinal upset and may need to be divided into twice-daily dosing. Azithromycin can prolong the QT interval and might have to be avoided due to other medications previously prescribed to patients. Rifabutin can cause leukopenia and uveitis. Ethambutol can cause optic neuritis, and patients should be screened for decreases in visual acuity and color blindness. Severe atypical mycobacterial lung infection resulting in lobectomy can result in chronic respiratory complications even when the intervention is curative 22, 23, 37.
Atypical mycobacterial infection diagnosis
Atypical mycobacteria are difficult to identify detect by laboratory testing 2. Atypical mycobacteria contain a hydrophobic mycolic acid layer in their cell wall. Due to this property, they are not typically seen using Gram staining 2. The best method for detecting atypical mycobacteria is fluorochrome staining, a type of acid-fast staining where these bacteria will appear as yellow to orange bacilli 2. Rapidly growing mycobacteria are frequently not seen even with fluorochrome staining, and atypical mycobacteria overall are visualized in only 30% to 60% of cases 2. Rapidly growing atypical mycobacteria are noted to be more sensitive to the decolorization process in acid-fast staining. It is thought that using more delicate methods for decolorization can increase the chance of visualizing these bacteria. Other less sensitive staining methods that may also be used include the Ziehl-Neelsen method and the Kinyoun stain 22.
The initial workup for most infections begins with a complete blood count (CBC), which can show a normal to elevated white blood cell count. Inflammatory markers such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) can also be normal or elevated 2. Samples from fluid cultures obtained from soft tissue lesions or excised lymph nodes should undergo acid-fast or fluorochrome staining 2. Organisms are visualized in around 30% to 60% of cases 2. Culture of fluid and tissue samples should be obtained and yields an organism in approximately 65% of cases 2. 90% of patients diagnosed with a disseminated atypical mycobacterial infection will have positive blood cultures. Unlike the growth of common bacteria on culture, rapidly growing mycobacteria will take approximately 1 week or more to grow, and slow-growing mycobacteria will take several weeks to months to show growth 2.
Polymerase chain reaction (PCR) is frequently used on samples to obtain faster results and is more sensitive in diagnosis, yielding an organism around 91% of the time 2. Tuberculin skin testing can also be used as a nonspecific method to confirm suspected atypical mycobacterial infection 2. It will result in a greater than 10 mm area of induration between 30% to 60% of the time 2. Diagnosis of lung infection is currently based on clinical suspicion of an active infection given active pulmonary symptoms, findings on chest X-ray or CT, and growth on 2 or more sputum cultures (also accepted is tissue biopsy or lavage cultures) 22, 23.
Atypical mycobacterial lung disease diagnostic criteria
The minimum evaluation of a patient suspected of atypical mycobacterial lung disease should include the following 22:
- Chest radiograph or, in the absence of cavitation, chest high-resolution computed tomography (HRCT) scan;
- Three or more sputum specimens for acid-fast bacilli (AFB) analysis; and
- Exclusion of other disorders, such as tuberculosis (TB).
Clinical, radiographic, and microbiologic criteria are equally important and all must be met to make a diagnosis of atypical mycobacterial lung disease. The following criteria apply to symptomatic patients with radiographic opacities, nodular or cavitary, or an high-resolution computed tomography (HRCT) scan that shows multifocal bronchiectasis with multiple small nodules. These criteria fit best with Mycobacterium avium complex (MAC), Mycobacterium kansasii, and Mycobacterium abscessus. There is not enough known about most other atypical mycobacteria to be certain that these diagnostic criteria are universally applicable for all atypical mycobacteria respiratory pathogens.
Pulmonary symptoms, nodular or cavitary opacities on chest radiograph, or an high-resolution computed tomography (HRCT) scan that shows multifocal bronchiectasis with multiple small nodules.
Positive culture results from at least two separate expectorated sputum samples. If the results from the initial sputum samples are nondiagnostic, consider repeat sputum AFB smears and cultures. Or positive culture results from at least one bronchial wash or lavage. Or transbronchial or other lung biopsy with mycobacterial histopathologic features (granulomatous inflammation or AFB) and positive culture for atypical mycobacteria or biopsy showing mycobacterial histopathologic features (granulomatous inflammation or AFB) and one or more sputum or bronchial washings that are culture positive for atypical mycobacteria.
Expert consultation should be obtained when atypical mycobacteria are recovered that are either infrequently encountered or that usually represent environmental contamination.
Patients who are suspected of having atypical mycobacteria lung disease but who do not meet the diagnostic criteria should be followed until the diagnosis is firmly established or excluded.
Making the diagnosis of atypical mycobacteria lung disease does not, per se, necessitate the institution of therapy, which is a decision based on potential risks and benefits of therapy for individual patients.
Atypical mycobacterial infection treatment
Atypical mycobacterium treatment often requires extended courses of combination antibiotic therapy, frequently with surgical intervention 22, 23. There are specific antibiotics for each family of atypical mycobacteria, because they are resistant to most antibiotic drugs and single therapy may be inadequate 24. This difficulty in treating atypical mycobacterial infections can lead to serious health complications, including death 25.
Atypical mycobacterial lung infection treatment
Recommended treatment for adults and children with Mycobacterium avium complex bacteria (MAC) infections includes azithromycin, rifampin, and ethambutol. Additional drug options are available for each drug class 2. Three times per week dosing is used in adult nodular or bronchiectatic disease with recommended regimens of azithromycin 500 to 600 mg, or clarithromycin 1000 mg, plus ethambutol 25 mg/kg, plus rifampin 600 mg 2. Daily dosing is required in cavitary disease with the additional option of three times weekly streptomycin or amikacin. Recommended daily dosages are: clarithromycin 500 to 1000 mg or azithromycin 250 to 300 mg, plus rifampin 450 to 600 mg, with either amikacin or streptomycin 2. The American Thoracic Society and Infectious Disease Society of America cite a study that suggests tolerated dosages of 25 mg/kg three times weekly for both drugs 22. They also state that certain experts recommend considering decreasing dosages to 8 to 10 mg/kg (maximum 500 mg) for patients older than 50 years or receiving treatment longer than 6 months 22. Antibiotics are continued until the patient has had 12 months of negative sputum cultures. The typical time to the first negative sputum culture is 3 to 6 months, with most patients obtaining negative sputum cultures within 12 months. Treatment failure is defined as the lack of sputum conversion after 12 months or the lack of sputum conversion within 6 months without any improvement clinically or on imaging. In cases of progressively worsening respiratory status where patients continue to fail sputum conversion, surgical resection of the lung parenchyma containing the cavitary disease may be required 22, 23.
Mycobacterium avium-intracellulare (MAI) has demonstrated rising minimum inhibitory concentrations and overall increased resistance to anti-mycobacterial agents compared to Mycobacterium avium, making it more complicated to treat at times.
Alternative agents utilized to treat Mycobacterium avium complex bacteria (MAC) or Mycobacterium avium-intracellulare (MAI) lung disease includes inhaled amikacin, clofazimine (as a substitute for rifampin), and moxifloxacin 2.
Several other atypical mycobacterial species have been shown to cause pulmonary disease and are generally susceptible to macrolides, rifampin/rifabutin, streptomycin, amikacin, doxycycline, and fluoroquinolones. Of note, the pulmonary disease caused by Mycobacterium abscessus is resistant to most antibiotics and can only be cured in a minority of patients by surgical resection. Those that are not cured are administered chronic intermittent antibiotic therapy to attempt to slow disease progression 22, 38.
Atypical mycobacterial lymphadenitis treatment
Treatment for atypical mycobacterial lymphadenitis is based on a two-drug regimen of one macrolide, azithromycin, or clarithromycin, combined with rifampin or ethambutol 2. Antibiotics are dosed daily and taken until the resolution of symptoms. Surgical resection of infected lymph nodes and tissue is typically used in combination with antibiotic therapy with significantly increased cure rates. The initial antibiotic regimen may be adjusted based on culture susceptibility results 23.
Atypical mycobacterial skin and soft tissue infection treatment
Skin and soft tissue atypical mycobacterium infections are treated with combination antibiotic therapy with a variety of options available, including macrolides, doxycycline, fluoroquinolones, trimethoprim/sulfamethoxazole, cephalosporins, or linezolid 2. Empiric therapies are adjusted once susceptibility testing yields results; however, combination antibiotic therapy is continued due to inducible antibiotic resistance 2. Surgical debridement is required for infections that are extensive and associated with necrosis 22.
Atypical mycobacterial infection prognosis
- Atypical mycobacterial lung infection: Treatment of Mycobacterium avium lung disease is successful in approximately 39% of patients with a 12% 5-year mortality rate 2. High levels of morbidity and mortality are seen in strains that exhibit macrolide resistance with a significantly higher 47% mortality rate at 5 years 2. Outcomes of pulmonary Mycobacterium abscessus infection are poor, with only around 41% of patients achieving sputum conversion with surgical and antibiotic intervention. Approximately 34% of patients achieve sputum conversion with antibiotics alone 39, 40.
- Atypical mycobacterial lymphadenitis: Children with lymphadenitis caused by Mycobacterium avium are cured in 95% of cases where both surgical excision and antibiotic therapy are used 41.
- Atypical mycobacterial skin and soft tissue infection: Resolution of infection is achieved in the vast majority of patients with Mycobacterium marinum, abscessus, ulcerans, fortuitum, and other skin and soft tissue infections when proper antibiotic and surgical treatments are utilized 22, 42, 43.
- Sajduda A, Martin A, Portaels F, Palomino JC. hsp65 PCR-restriction analysis (PRA) with capillary electrophoresis for species identification and differentiation of Mycobacterium kansasii and Mycobacterium chelonae–Mycobacterium abscessus group. Int J Infect Dis. 2012;16:193–197. doi: 10.1016/j.ijid.2011.11.011[↩]
- Winburn B, Sharman T. Atypical Mycobacterial Disease. [Updated 2023 Jan 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556117[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Sharma P, Vazquez Guillamet LJ, Miljkovic G. Atypical Mycobacterial Infection after Abdominoplasty Overseas: A Case Report and Literature Review. Case Rep Infect Dis. 2016;2016:3642567. doi: 10.1155/2016/3642567[↩]
- Diagnosis and treatment of disease caused by nontuberculous mycobacteria. Am Rev Respir Dis. 1990 Oct;142(4):940-53. doi: 10.1164/ajrccm/142.4.940. Erratum in: Am Rev Respir Dis 1991 Jan;143(1):204.[↩]
- Diagnosis and treatment of disease caused by nontuberculous mycobacteria. This official statement of the American Thoracic Society was approved by the Board of Directors, March 1997. Medical Section of the American Lung Association. Am J Respir Crit Care Med. 1997 Aug;156(2 Pt 2):S1-25. doi: 10.1164/ajrccm.156.2.atsstatement[↩]
- Gross PA, Barrett TL, Dellinger EP, Krause PJ, Martone WJ, McGowan JE Jr, Sweet RL, Wenzel RP. Purpose of quality standards for infectious diseases. Infectious Diseases Society of America. Clin Infect Dis. 1994 Mar;18(3):421. doi: 10.1093/clinids/18.3.421[↩]
- Jyotsna Bhattacharya, Sindhu Mohandas, David L. Goldman; Nontuberculous Mycobacterial Infections in Children. Pediatr Rev April 2019; 40 (4): 179–190. https://doi.org/10.1542/pir.2018-0131[↩]
- Soilán B, Kawabata A, Salinas M, Paredes ME, Abente S, et al. Infección post quirúrgica por Micobacterias Atípicas de Crecimiento Rápido [Post-surgical infection by fast-growing atypical mycobacteria] (in Spanish) An Fac Cienc Méd. 2008;41[↩]
- Leto Barone AA, Grzelak MJ, Frost C, Ngaage LM, Ge S, Kolegraff K, Chopra K, Tornheim JA, Caffrey J, Lifchez SD, Rasko Y. Atypical Mycobacterial Infections After Plastic Surgery Procedures Abroad: A Multidisciplinary Algorithm for Diagnosis and Treatment. Ann Plast Surg. 2020 Mar;84(3):257-262. doi: 10.1097/SAP.0000000000002061[↩]
- Montague ML, Hussain SS, Blair RL. Three cases of atypical mycobacterial cervical adenitis. J R Soc Med. 2003 Mar;96(3):129-31. doi: 10.1177/014107680309600308[↩]
- Kerkemeyer KL, Darby JD, Jack Green F. Mycobacterium Abscessus infection of a new tattoo in an australian traveller returning from Bali. J Travel Med. 2020;27:taaa014. doi: 10.1093/jtm/taaa014[↩]
- Kluger N, Muller C, Gral N. Atypical Mycobacteria Infection Following Tattooing: Review of an Outbreak in 8 Patients in a French Tattoo Parlor. Arch Dermatol. 2008;144(7):941–942. doi:10.1001/archderm.144.7.941[↩]
- Kennedy BS, Bedard B, Younge M, Tuttle D, Ammerman E, Ricci J, Doniger AS, Escuyer VE, Mitchell K, Noble-Wang JA, O’Connell HA, Lanier WA, Katz LM, Betts RF, Mercurio MG, Scott GA, Lewis MA, Goldgeier MH. Outbreak of Mycobacterium chelonae infection associated with tattoo ink. N Engl J Med. 2012 Sep 13;367(11):1020-4. doi: 10.1056/NEJMoa1205114[↩]
- Isabel Griffin, Ann Schmitz, Christine Oliver, et al. Outbreak of Tattoo-associated Nontuberculous Mycobacterial Skin Infections, Clinical Infectious Diseases, Volume 69, Issue 6, 15 September 2019, Pages 949–955, https://doi.org/10.1093/cid/ciy979[↩]
- Centers for Disease Control and Prevention (CDC). Tattoo-associated nontuberculous mycobacterial skin infections–multiple states, 2011-2012. MMWR Morb Mortal Wkly Rep. 2012 Aug 24;61(33):653-6. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6133a3.htm[↩]
- Tung-Chen Y, Caballero-Cardona C. Infección por micobacterias no tuberculosas tras cirugía estética [Mycobacterium fortuitum infection in plastic surgery. Success with 12 weeks clarithromycin and levofloxacin treatment] (in Spanish) Med clínica. 2017;149:227–228. doi: 10.1016/j.medcli.2017.03.017[↩]
- Colás Orós CE, Lasso Olayo JM, Vallejo Germosen L. Infección cutánea por micobacteria atípica [Atypical mycobacterial skin infection]. Emergencias. 2015 Abr;27(2):135. Spanish. https://emergencias.portalsemes.org/descargar/infeccion-cutanea-por-micobacteria-atipica[↩]
- Schcolnik Cabrera A, Hernández Castro R, Vega Memije ME, Arenas Guzmán R, Fernández Martínez RF. Lipotransferencia complicada con micobacteriosis atípicas. Reporte de dos casos y revisión de la literatura [Atypical microbacteriosis: a report of two cases and review of the literature]. Gac Med Mex. 2014 Dec;150 Suppl 3:311-6. Spanish. https://www.anmm.org.mx/GMM/2014/s3/GMM_150_2014_S3_311-316.pdf[↩]
- Chen X, Jin Y, Torres KMT, Li B, Zhuo F, et al. Mycobacterium abscessus cutaneous infection secondary to botulinum toxin injection: A report of 2 cases. JAAD Case Rep. 2019;5:982–984. doi: 10.1016/j.jdcr.2019.09.017[↩]
- Rüegg E, Cheretakis A, Modarressi A, Harbarth S, Pittet-Cuénod B. Multisite Infection with Mycobacterium abscessus after Replacement of Breast Implants and Gluteal Lipofilling. Case Rep Infect Dis. 2015 doi: 10.1155/2015/361340[↩]
- Desai AN, Hurtado RM. Infections and outbreaks of nontuberculous mycobacteria in hospital settings. Curr Treat Options Infect Dis. 2018;10:169–181. doi: 10.1007/s40506-018-0165-9[↩]
- Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, Holland SM, Horsburgh R, Huitt G, Iademarco MF, Iseman M, Olivier K, Ruoss S, von Reyn CF, Wallace RJ Jr, Winthrop K; ATS Mycobacterial Diseases Subcommittee; American Thoracic Society; Infectious Disease Society of America. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007 Feb 15;175(4):367-416. doi: 10.1164/rccm.200604-571ST. Erratum in: Am J Respir Crit Care Med. 2007 Apr 1;175(7):744-5. Dosage error in article text.[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Bhattacharya J, Mohandas S, Goldman DL. Nontuberculous Mycobacterial Infections in Children. Pediatr Rev. 2019 Apr;40(4):179-190. doi: 10.1542/pir.2018-0131[↩][↩][↩][↩][↩][↩][↩][↩]
- Esteban J, Navas E. Tratamiento de las Infecciones producidas Por Micobacterias no tuberculosas [Treatment of infections caused by nontuberculous mycobacteria] (in Spanish) Enf Infeccios y Microb Clín. 2018;36:586–592. doi: 10.1016/j.eimc.2017.10.008[↩][↩]
- Cardozo Lomaquiz CD, Frontanilla T, Scavone N, Fretes A, Torales N, Pereira ME, Mino de Kaspar H, Ortiz X, Henning R. Rapid growth atypical mycobacteria infection associated with growth hormone injections: a case report. Access Microbiol. 2021 Nov 8;3(11):000280. doi: 10.1099/acmi.0.000280[↩][↩]
- Karolina L Kerkemeyer, Jonathan D Darby, Jack Green, Mycobacterium abscessus infection of a new tattoo in an Australian traveller returning from Bali, Indonesia, Journal of Travel Medicine, Volume 27, Issue 6, August 2020, taaa014, https://doi.org/10.1093/jtm/taaa014[↩]
- Isabel Griffin, Ann Schmitz, Christine Oliver, et. al. Outbreak of Tattoo-associated Nontuberculous Mycobacterial Skin Infections, Clinical Infectious Diseases, Volume 69, Issue 6, 15 September 2019, Pages 949–955, https://doi.org/10.1093/cid/ciy979[↩][↩]
- What GPs need to know about the flesh-eating Buruli ulcer. https://www1.racgp.org.au/newsgp/clinical/what-gps-need-to-know-about-the-flesh-eating-burul[↩]
- Falkinham JO 3rd. Environmental sources of nontuberculous mycobacteria. Clin Chest Med. 2015 Mar;36(1):35-41. doi: 10.1016/j.ccm.2014.10.003[↩]
- Prevots DR, Marras TK. Epidemiology of human pulmonary infection with nontuberculous mycobacteria: a review. Clin Chest Med. 2015 Mar;36(1):13-34. doi: 10.1016/j.ccm.2014.10.002[↩]
- Zimmermann P, Curtis N, Tebruegge M. Nontuberculous mycobacterial disease in childhood – update on diagnostic approaches and treatment. J Infect. 2017 Jun;74 Suppl 1:S136-S142. doi: 10.1016/S0163-4453(17)30204-9[↩]
- Drummond WK, Kasperbauer SH. Nontuberculous Mycobacteria: Epidemiology and the Impact on Pulmonary and Cardiac Disease. Thorac Surg Clin. 2019 Feb;29(1):59-64. doi: 10.1016/j.thorsurg.2018.09.006[↩]
- Bayazit YA, Bayazit N, Namiduru M. Mycobacterial cervical lymphadenitis. ORL J Otorhinolaryngol Relat Spec. 2004;66(5):275-80. doi: 10.1159/000081125[↩]
- Appelberg R. Pathogenesis of Mycobacterium avium infection: typical responses to an atypical mycobacterium? Immunol Res. 2006;35(3):179-90. doi: 10.1385/IR:35:3:179[↩]
- Torretta S, Gaffuri M, Ibba T, Capaccio P, Marchisio P, Maruca A, Bosis S, Pignataro L. Surgical treatment of non-tuberculous mycobacterial lymphadenitis in children: Our experience and a narrative review. Int J Immunopathol Pharmacol. 2018 Jan-Dec;32:2058738418806413. doi: 10.1177/2058738418806413[↩]
- Gonzalez-Santiago TM, Drage LA. Nontuberculous Mycobacteria: Skin and Soft Tissue Infections. Dermatol Clin. 2015 Jul;33(3):563-77. doi: 10.1016/j.det.2015.03.017[↩]
- Haimi-Cohen Y, Markus-Eidlitz T, Amir J, Zeharia A. Long-term Follow-up of Observation-Only Management of Nontuberculous Mycobacterial Lymphadenitis. Clin Pediatr (Phila). 2016 Oct;55(12):1160-4. doi: 10.1177/0009922815617972[↩]
- Lee MR, Sheng WH, Hung CC, Yu CJ, Lee LN, Hsueh PR. Mycobacterium abscessus Complex Infections in Humans. Emerg Infect Dis. 2015 Sep;21(9):1638-46. doi: 10.3201/2109.141634[↩]
- Moon SM, Park HY, Kim SY, Jhun BW, Lee H, Jeon K, Kim DH, Huh HJ, Ki CS, Lee NY, Kim HK, Choi YS, Kim J, Lee SH, Kim CK, Shin SJ, Daley CL, Koh WJ. Clinical Characteristics, Treatment Outcomes, and Resistance Mutations Associated with Macrolide-Resistant Mycobacterium avium Complex Lung Disease. Antimicrob Agents Chemother. 2016 Oct 21;60(11):6758-6765. doi: 10.1128/AAC.01240-16[↩]
- Xu HB, Jiang RH, Li L. Treatment outcomes for Mycobacterium avium complex: a systematic review and meta-analysis. Eur J Clin Microbiol Infect Dis. 2014 Mar;33(3):347-58. doi: 10.1007/s10096-013-1962-1[↩]
- Wei JL, Bond J, Sykes KJ, Selvarangan R, Jackson MA. Treatment outcomes for nontuberculous mycobacterial cervicofacial lymphadenitis in children based on the type of surgical intervention. Otolaryngol Head Neck Surg. 2008 May;138(5):566-71. doi: 10.1016/j.otohns.2008.01.022[↩]
- Tanywe A, Fernandez RS. Effectiveness of rifampicin-streptomycin for treatment of Buruli ulcer: a systematic review. JBI Database System Rev Implement Rep. 2017 Jan;15(1):119-139. doi: 10.11124/JBISRIR-2016-003235[↩]
- Holden IK, Kehrer M, Andersen AB, Wejse C, Svensson E, Johansen IS. Mycobacterium marinum infections in Denmark from 2004 to 2017: A retrospective study of incidence, patient characteristics, treatment regimens and outcome. Sci Rep. 2018 Apr 30;8(1):6738. doi: 10.1038/s41598-018-24702-[↩]