Contents
- What is benign paroxysmal positional vertigo
- Inner ear anatomy
- Benign paroxysmal positional vertigo symptoms
- Benign paroxysmal positional vertigo causes
- Benign paroxysmal positional vertigo diagnosis
- Benign paroxysmal positional vertigo treatment
- Benign paroxysmal positional vertigo maneuver
- Surgical treatment
What is benign paroxysmal positional vertigo
Benign paroxysmal positional vertigo (BPPV) is a problem with the inner ear. Benign paroxysmal positional vertigo occurs when small pieces of bone-like calcium carbonate crystals or otoconia (canaliths) break free and float inside small canals in your inner ear (see Figure 3). This sends confusing messages to your brain about your body’s position, which causes vertigo. Benign paroxysmal positional vertigo (BPPV) causes you to suddenly feel dizzy. Benign paroxysmal positional vertigo is the most common type of vertigo. Benign paroxysmal positional vertigo is also the easiest to treat.
Vertigo is a sensation of movement or spinning, tilting or swaying. Vertigo feels like you or everything around you is spinning – enough to affect your balance. It’s more than just feeling dizzy. With benign paroxysmal positional vertigo you might feel like the room is spinning around in circles or that your surroundings are moving. Benign paroxysmal positional vertigo is associated with feelings of vertigo when you move a certain way. This could be when you turn your head, stand up, roll over in bed, or lie down. You might also feel nauseated at the same time. The nausea and dizziness usually go away in a few seconds. Benign paroxysmal positional vertigo is bothersome, but it’s rarely serious.
The only thing you can do to prevent or avoid benign paroxysmal positional vertigo is to avoid head positions that trigger it.
BPPV is fairly common, with an estimated incidence of 107 per 100,000 per year2 and a lifetime prevalence of 2.4 percent 1. Benign paroxysmal positional vertigo (BPPV) most often affects older adults with a peak age of onset in the sixth decade 2. Benign paroxysmal positional vertigo (BPPV) may affect individuals of any age, but is quite uncommon in those under 20 years of age. Women are believed to be affected at least twice as often as men. The vast majority of cases occur for no apparent reason, with many people describing that they simply went to get out of bed one morning and the room started to spin. However associations have been made with trauma, migraine, inner ear infection or disease, diabetes, osteoporosis, intubation (presumably due to prolonged time lying in bed) and reduced blood flow. There may also be a correlation with one’s preferred sleep side 3.
Most of the time, treatment will cure benign paroxysmal positional vertigo. Sometimes, vertigo may return after a few weeks. About half the time, benign paroxysmal positional vertigo will come back. If this happens, you’ll need to be treated again. Your doctor may teach you how to perform the maneuver at home (see section “Benign paroxysmal positional vertigo maneuver” below).
Your doctor may prescribe medicines that can help relieve spinning sensations. However, these medicines often do not work well for treating vertigo.
Benign paroxysmal positional vertigo treatment at home
Benign paroxysmal positional vertigo can be bothersome and uncomfortable. But the simple head maneuvers usually help the symptoms go away (see section “Benign paroxysmal positional vertigo maneuver” below). It can come back at any time, but is easily treatable.
Your doctor can show you some easy head maneuvers that will help (see section “Benign paroxysmal positional vertigo maneuver” below). They move the particles out of the inner ear canals and into areas where they will not cause episodes of vertigo. Doing these movements can stop the symptoms. They may keep the dizziness from coming back.
How long does benign paroxysmal positional vertigo last?
Individuals with benign paroxysmal positional vertigo may be treated with canalith repositioning maneuvers (e.g., Epley maneuver, Deep Head Hanging maneuver, Lempert (BBQ) maneuver, Half Somersault maneuver and Semont maneuver), in which the head is put through a series of specific movements designed to shift the crystals (otoliths) out of the semicircular canals and back into the vestibule. Once the crystals are back in the vestibule, they are usually reabsorbed in a matter of days. The maneuvers may need to be repeated. Different maneuvers are required depending upon which of the three semicircular canals is involved.
Many studies have been done into the effectiveness of treatment maneuvers for benign paroxysmal positional vertigo, with results showing rates of resolution well into the 90% range by 1-3 treatments 4 (the more rare cupulolithiasis or ‘hung-up’ variant can be a little more stubborn, as can benign paroxysmal positional vertigo that is the result of trauma). It is possible to have more than one canal involved, especially after trauma, in which case your vestibular therapist would typically have to correct them one at a time. You may be advised to avoid certain head positions for a few days following treatment. However, current research suggests that post-maneuver restrictions do not significantly affect outcomes 5. Even after the crystals are back in the correct chamber and the spinning sensation has stopped, people can often feel some mild residual sensitivity to motion and unsteadiness, so it is important to follow up with your vestibular therapist so that they can evaluate this and provide home exercise techniques that typically correct this promptly.
Will benign paroxysmal positional vertigo come back?
Unfortunately, benign paroxysmal positional vertigo is a condition that can re-occur periodically with long-term recurrence rates as high as 50% within 5 years 6, especially in those whose benign paroxysmal positional vertigo is related to trauma. If it seems to always reoccur in the same canal and if deemed safe, your therapist may teach you to perform a specific treatment maneuver on yourself. However, it can be challenging to perform the maneuver on one’s self, so many people prefer to return to their vestibular therapist to confirm that they are experiencing the same problem, and if so, determine which maneuver is indicated and provide the appropriate treatment. There are other conditions that can mimic benign paroxysmal positional vertigo, and because there are so many different variants of benign paroxysmal positional vertigo, the maneuver that worked one time is not necessarily going to be the treatment that is indicated the next time.
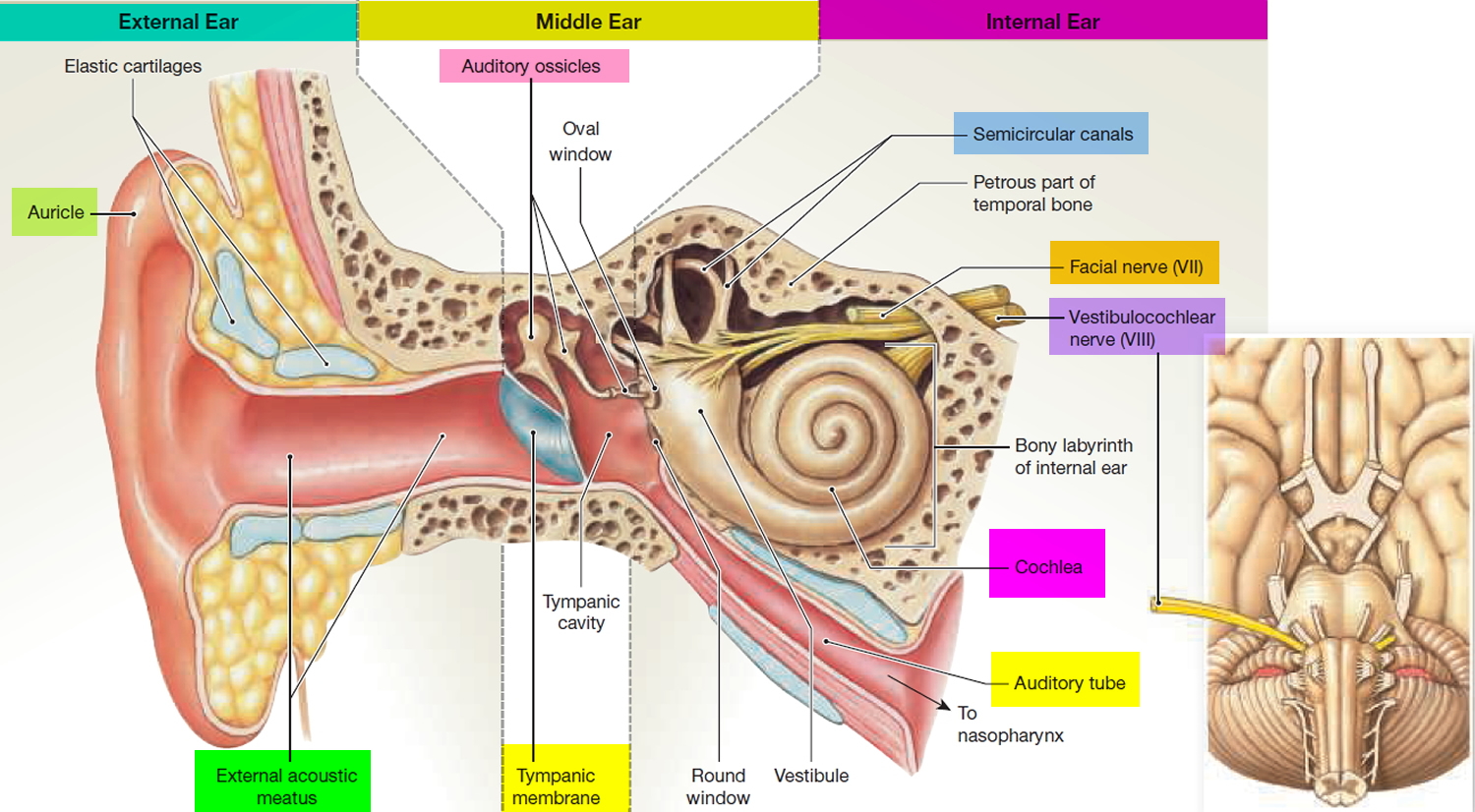
Inner ear anatomy
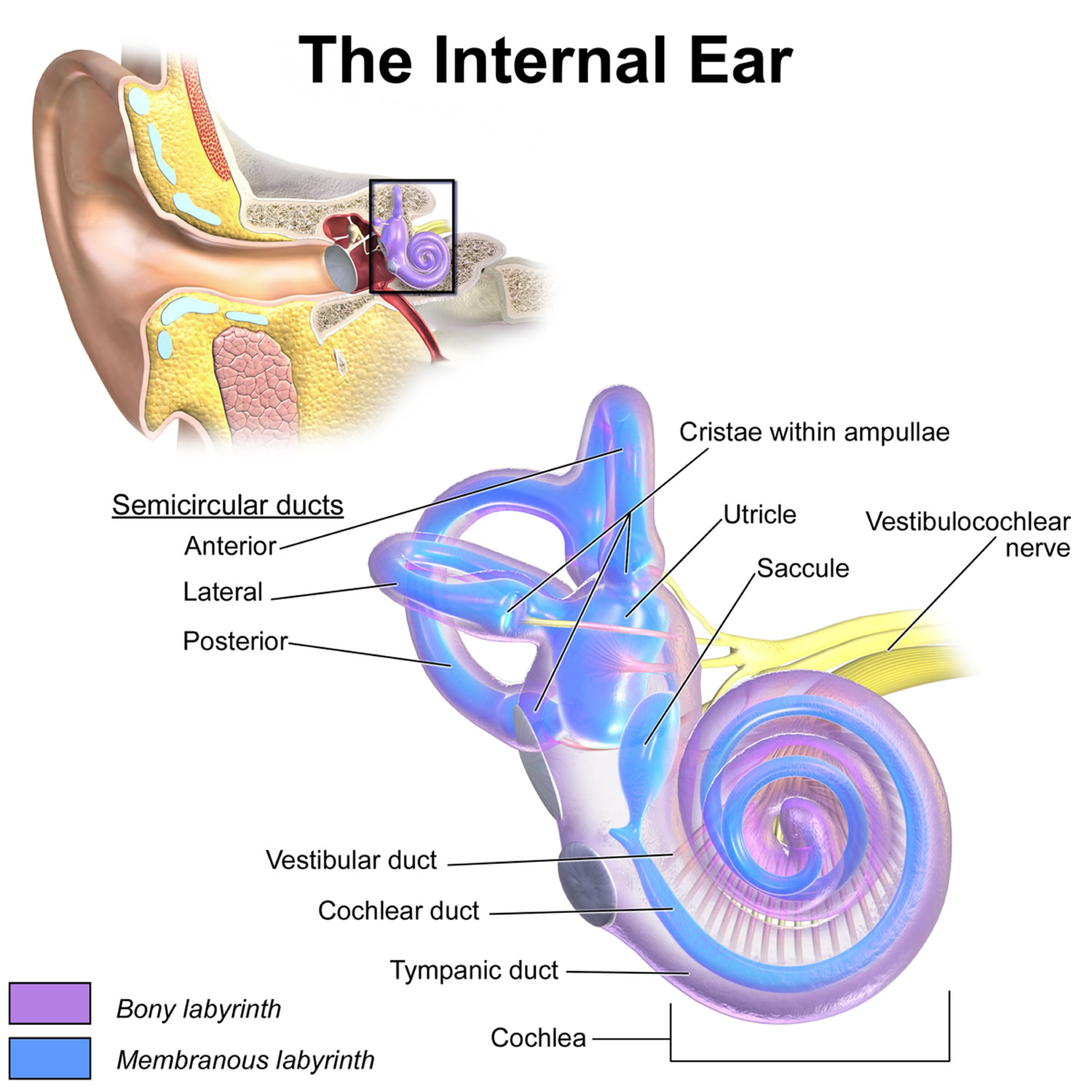
You rely on the inner ear, an intricate sensory organ, to hear and to maintain balance. The inner ear is a complex system of communicating chambers and tubes called a labyrinth. Each ear has two parts to the labyrinth—the bony (osseus) labyrinth and the membranous labyrinth (Figure 1). The bony labyrinth is a cavity within the temporal bone. The membranous labyrinth is a tube of similar shape that lies within the bony labyrinth. Between the bony and membranous labyrinths is a fluid called perilymph, which is secreted by cells in the wall of the bony labyrinth. The membranous labyrinth contains another fluid, called endolymph.
The parts of the labyrinths include three membranous semicircular ducts within three bony semicircular canals, and a cochlea. The semicircular canals and associated structures provide a sense of equilibrium (balance). The cochlea functions in hearing.
Figure 1. Inner ear anatomy
Figure 2. Parts of the inner ear
Sense of Equilibrium
The sense of equilibrium (balance) is really two senses:
- Static equilibrium and
- Dynamic equilibrium—that come from different sensory organs.
The organs of static equilibrium sense the position of the head, maintaining balance, stability and posture when the head and body are still. When the head and body suddenly move or rotate, the organs of dynamic equilibrium detect such motion and aid in maintaining balance.
Static Equilibrium
The organs of static equilibrium are in the vestibule, a bony chamber between the semicircular canals and the cochlea. The membranous labyrinth inside the vestibule consists of two expanded chambers—a utricle and a saccule (see Figure 2).
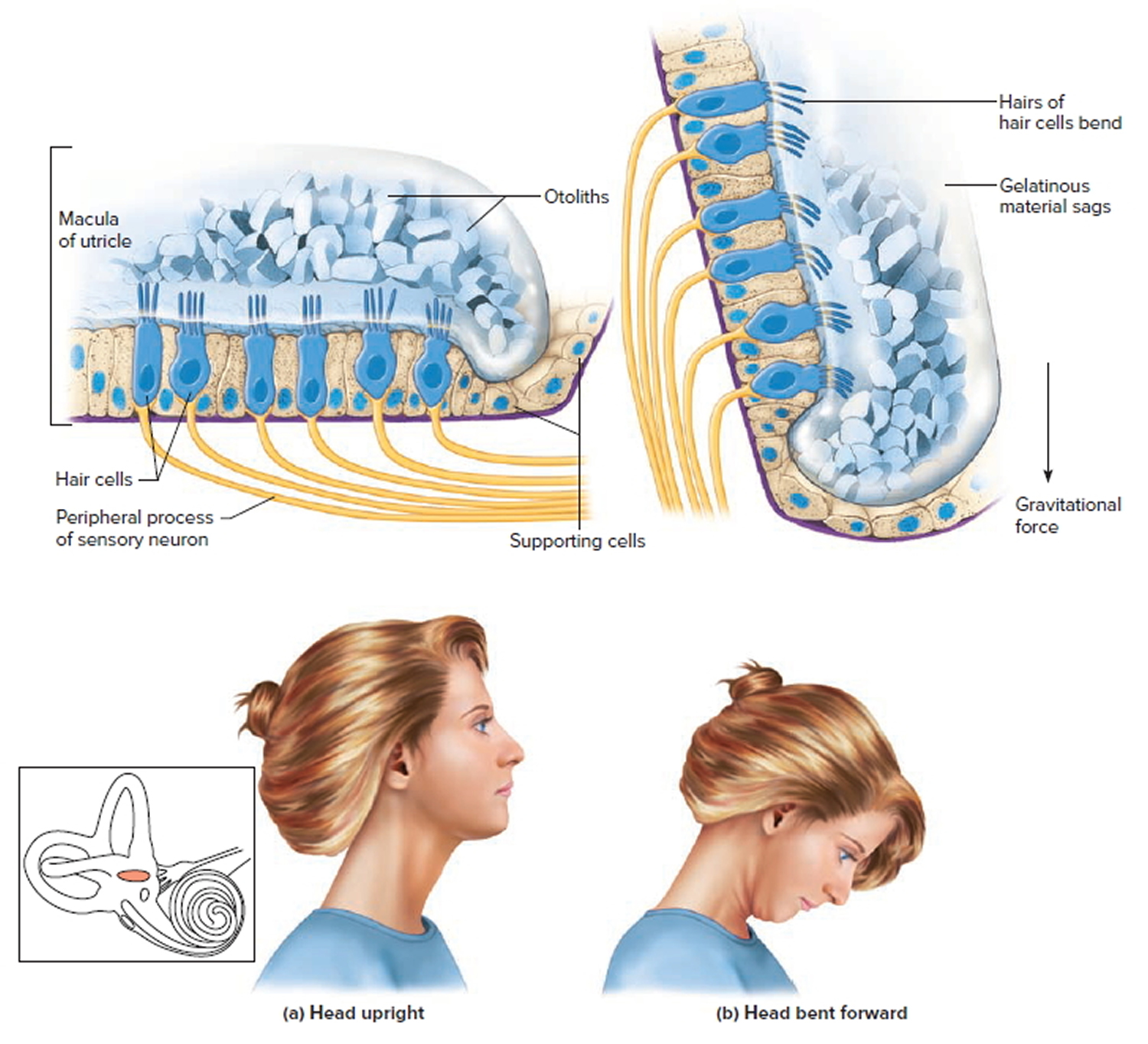
The saccule and utricle each have a tiny structure called a macula. Maculae have many hair cells, which serve as sensory receptors. The hairs of the hair cells project into a mass of gelatinous material, which has grains of calcium carbonate (otoliths) embedded in it. These particles add weight to the gelatinous structure.
Bending the head forward, backward, or to either side tilts the gelatinous masses of the maculae, and as they sag in response to gravity, the hairs projecting into them bend. This action causes the hair cells to signal the sensory neurons associated with them in a manner similar to that of hair cells associated with hearing. The resulting action potentials are conducted into the central nervous system on the vestibular branch of the vestibulocochlear nerve, informing the brain of the head’s new position. The brain responds by adjusting the pattern of motor impulses to skeletal muscles, which contract or relax to maintain balance (Figure 5).
Figure 3. Inner ear maculae respond to changes in head position
Note: (a) Macula of the utricle with the head in an upright position. (b) Macula of the utricle with the head bent forward.
Dynamic Equilibrium
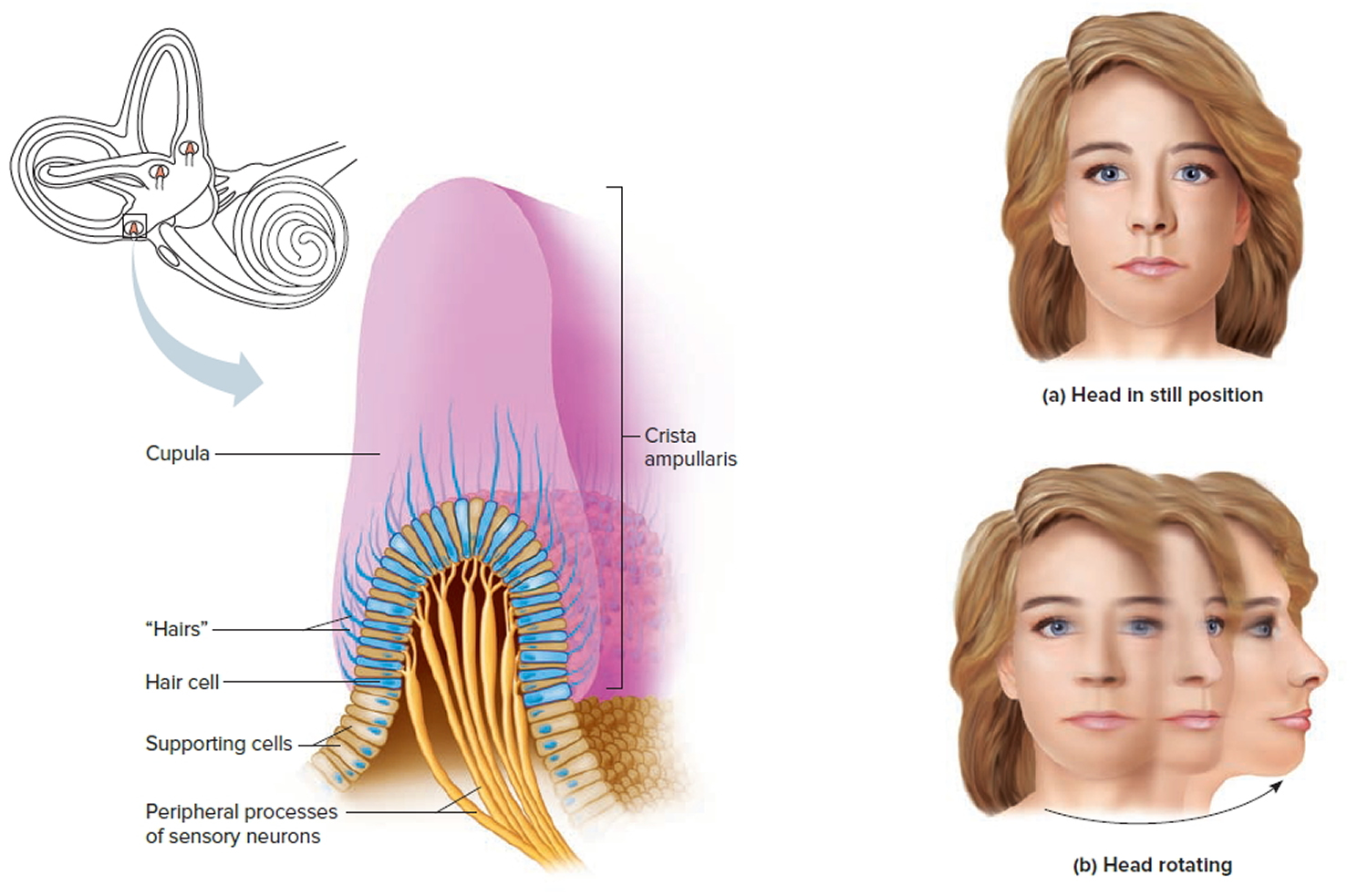
The organs of dynamic equilibrium are the three semicircular canals in the labyrinth. They detect motion of the head and aid in balancing the head and body during sudden movement. These canals lie at right angles to each other (see Figure 2).
Suspended in the perilymph of the bony portion of each semicircular canal is a membranous semicircular duct that ends in a swelling called an ampulla, which
houses the sensory organs of the semicircular canals. Each of these sensory organs, called a crista ampullaris, contains a number of sensory hair cells and supporting cells. Like the hairs of the maculae, the hair cells of the crista ampullaris extend upward into a dome-shaped, gelatinous mass called the cupula (Figure 4). When the head is stationary, the cupula of the crista ampullaris remains upright. When the head is moving rapidly, the cupula bends opposite the motion of the head, stimulating sensory receptors.
Rapid movement of the head or body stimulates the hair cells of the crista ampullaris (Figure 4). At such times, the semicircular canals move with the head or body, but the fluid inside the membranous ducts remains stationary. Imagine turning rapidly while holding a full glass of water. This action bends the cupula in one or more of the canals in a direction opposite that of the head or body movement, and the hairs embedded in it also bend. The stimulated hair cells signal their associated neurons, which conduct impulses to the brain. The brain interprets these impulses as a movement in a particular direction.
Parts of the cerebellum are particularly important in interpreting impulses from the semicircular canals. Analysis of such information allows the brain to predict the consequences of rapid body movements. By modifying signals to appropriate skeletal muscles, the cerebellum can maintain balance.
Other sensory structures aid in maintaining equilibrium. For example, certain mechanoreceptors (proprioceptors), particularly those associated with the joints of the neck, inform the brain about the position of body parts. In addition, the eyes detect changes in position that result from body movements. Such visual information is so important that even if the organs of equilibrium are damaged, a person may be able to maintain normal balance by keeping the eyes open and moving slowly.
The nausea, vomiting, dizziness, and headache of motion sickness arise from sensations that don’t make sense. The eyes of a person reading in a moving car, for example, signal the brain that the person is stationary, because the print doesn’t move. However, receptors in the skin detect bouncing, swaying, starting, and stopping as the inner ear detects movement. The contradiction triggers the symptoms. Similarly, in a passenger of an airplane flying through heavy turbulence, receptors in the skin and inner ear register the chaos outside, but the eyes focus on the immobile seats and surroundings.
Figure 4. Dynamic inner ear balance organs (crista ampullaris) within the Semicricular ducts
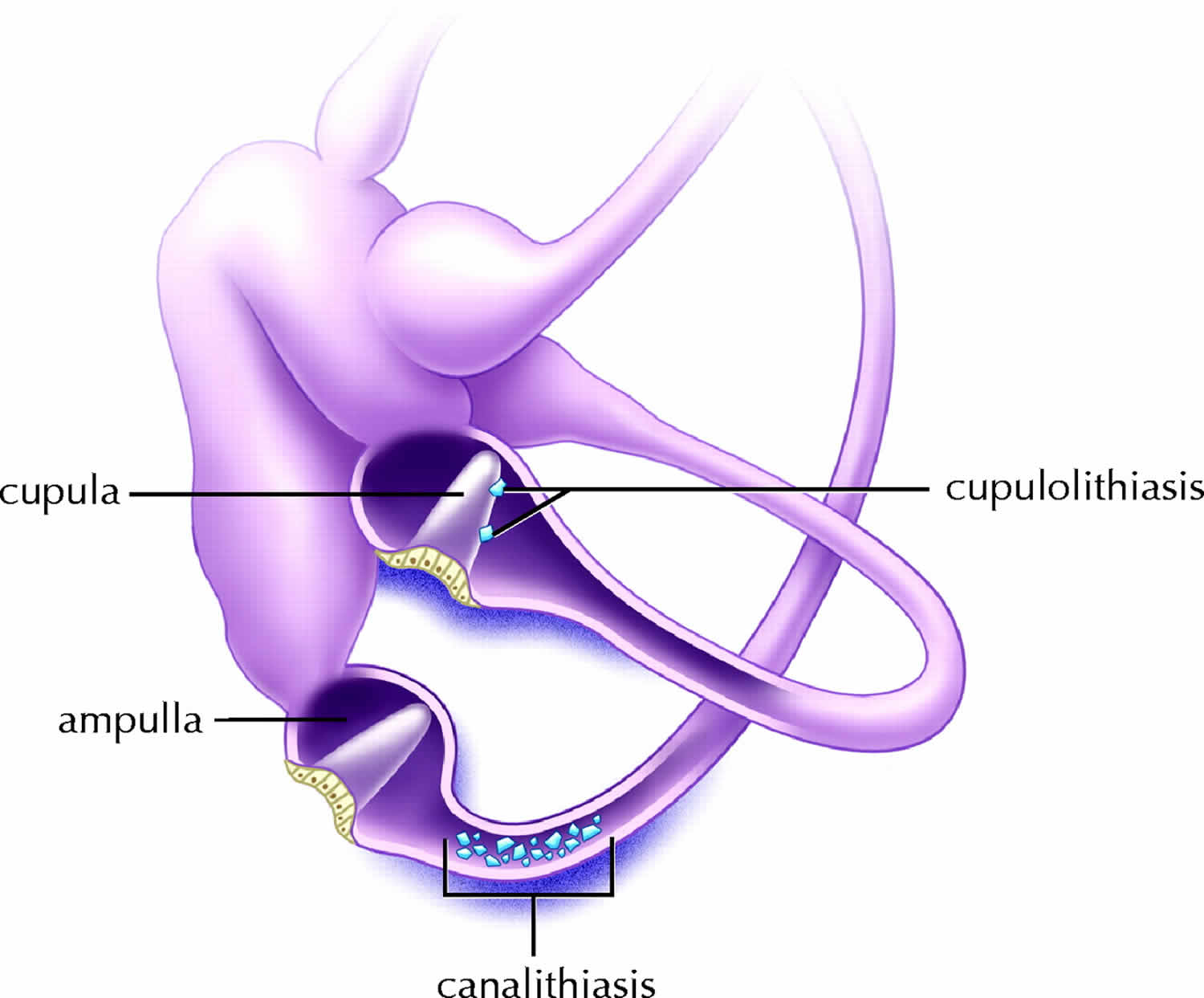
Figure 5. BPPV causes – Left inner ear. Depiction of canalithiasis of the posterior canal and cupulolithiasis of the lateral canal.
[Source 7 ]Benign paroxysmal positional vertigo symptoms
It is important to know that benign paroxysmal positional vertigo will NOT give you constant dizziness that is unaffected by movement or a change in position. It will NOT affect your hearing or produce fainting, headache or neurological symptoms such as numbness, “pins and needles,” trouble speaking or trouble coordinating your movements. If you have any of these additional symptoms, tell your healthcare provider immediately. Other disorders may be initially misdiagnosed as benign paroxysmal positional vertigo. By alerting your healthcare provider to symptoms you are experiencing in addition to vertigo they can re-evaluate your condition and consider whether you may have another type of disorder, either instead of or in addition to benign paroxysmal positional vertigo.
Benign paroxysmal positional vertigo symptoms include any of the following:
- Feeling like you are spinning or moving
- Feeling like the world is spinning around you
- Loss of balance
- Nausea and vomiting
- Hearing loss
- Vision problems, such as a feeling that things are jumping or moving
The spinning sensation:
- Is usually triggered by moving your head
- Often starts suddenly
- Lasts a few seconds to minutes
Certain positions can trigger the spinning feeling:
- Rolling over in bed
- Tilting your head up to look at something
Benign paroxysmal positional vertigo causes
The inner ear has fluid-filled tubes called semicircular canals. When you move, the fluid moves inside these tubes (semicircular canals). The canals are very sensitive to any movement of the fluid. The sensation of the fluid moving in the tube tells your brain the position of your body. This helps you keep your balance.
Your inner ear contains tiny calcium carbonate crystals (otoliths) that help you keep your balance. When you move your head, the calcium particles stimulate nerve cells. The nerve cells send your brain a signal telling it which direction your head is moving.
Normally, these tiny calcium carbonate crystals (otoliths) are distributed evenly in the inner ear’s 3 semicircular canals. Sometimes, the otoliths that are normally embedded in gel in the utricle, can break loose and clump together in one or more of the 3 fluid-filled semicircular canals, where they are not supposed to be. When enough of these particles accumulate in one of the canals they interfere with the normal fluid movement that these canals use to sense head motion, causing the inner ear to send false signals to the brain. When this happens, the nerve cells tell your brain that your head has moved more than it actually has. This incorrect signal results in vertigo.
Otoconia (tiny calcium carbonate crystals) migrate from the utricle, most commonly settling in the posterior semicircular canal or more rarely in the anterior or horizontal semicircular canals. The detached otoconia shift when the head moves, stimulating the cupula to send false signals to the brain that create a sensation of vertigo.
Benign paroxysmal positional vertigo has no major risk factors. But, your risk of developing benign paroxysmal positional vertigo may increase if you have:
- Family members with benign paroxysmal positional vertigo
- Had a prior head injury (even a slight bump to the head)
- Had an inner ear infection called labyrinthitis
Benign paroxysmal positional vertigo is most often associated with aging. It can also occur after you hit your head.
More than 90% of cases are idiopathic 8; the remaining, symptomatic cases are most commonly due to head trauma, vestibular neuritis, or Menière’s disease 9. Benign paroxysmal positioning vertigo is called “benign” because it usually resolves spontaneously within a few weeks or months; in some cases, however, it can last for years. If left untreated, it persists in about 30% of patients. Benign paroxysmal positioning vertigo also arises with greater than usual frequency after prolonged bed rest necessitated by other diseases, or after surgery. Benign paroxysmal positioning vertigo of the horizontal semicircular canal is rare and is precipitated by rotation of the head in the recumbent position.
The canalolithiasis hypothesis explains all of the manifestations of positioning vertigo and nystagmus 10. According to this hypothesis, the condition is due to the presence of agglomerates of many otoconia (small crystals of calcium carbonate in the saccule and utricle of the inner ear) that nearly fill the lumen of the semicircular canal and are freely mobile within it, instead of the small pieces of particulate matter that adhere firmly to the cupula (so-called cupulolithiasis).
Benign paroxysmal positional vertigo diagnosis
Your health care provider will do a physical exam and ask about your medical history.
Normal medical imaging (e.g. an MRI) is not effective in diagnosing benign paroxysmal positional vertigo, because it does not show the crystals that have moved into the semi-circular canals. However, when someone with benign paroxysmal positional vertigo has their head moved into a position that makes the dislodged crystals move within a canal, the error signals cause the eyes to move in a very specific pattern, called “nystagmus”.
The relationship between the inner ears and the eye muscles are what normally allow you to stay focused on our environment while your head is moving. Since the dislodged crystals make the brain think you’re moving when you’re not, it mistakenly causes the eyes to move, which makes it look like the room is spinning. The eye movement is the clue that something must be happening mechanically to move the fluid in the inner ear canals when it shouldn’t be.
The nystagmus will have different characteristics that allow a trained practitioner to identify which ear the displaced crystals are in, and which canal(s) they have moved into. Tests like the Dix-Hallpike involve moving the head into specific orientations, which allow gravity to move the dislodged crystals and trigger the vertigo while the practitioner watches for the tell-tale eye movements, or nystagmus.
There are two types of benign paroxysmal positional vertigo: one where the loose crystals can move freely in the fluid of the canal (canalithiasis), and, more rarely, one where the crystals are thought to be ‘hung up’ on the bundle of nerves that sense the fluid movement (cupulolithiasis). With canalithiasis, it takes less than a minute for the crystals to stop moving after a particular change in head position has triggered a spin. Once the crystals stop moving, the fluid movement settles and the nystagmus and vertigo stop. With cupulolithiasis, the crystals stuck on the bundle of sensory nerves will make the nystagmus and vertigo last longer, until the head is moved out of the offending position. It is important to make this distinction, as the treatment is different for each variant.
To diagnose benign paroxysmal positional vertigo, your doctor may perform a test called the Dix-Hallpike maneuver (see video below).
- Your provider holds your head in a certain position. Then you are asked to lie quickly backward over a table.
- As you do this, your provider will look for abnormal eye movements (called nystagmus) and ask if you feel like you are spinning.
If this test doesn’t show a clear result, you may be asked to do other tests.
Benign paroxysmal positional vertigo test
You may have brain and nervous system (neurological) tests to rule out other causes. These may include:
- Electroencephalogram (EEG)
- Electronystagmography (ENG)
- Head CT scan
- Head MRI scan.
- Hearing test
- Magnetic resonance angiography of the head
- Warming and cooling the inner ear with water or air to test eye movements (caloric stimulation)
Electronystagmography
The electronystagmography test is used to determine whether a balance or nerve disorder is the cause of dizziness or vertigo. Electronystagmography is very useful because it can record movements behind closed eyelids or with the head in many positions.
Electronystagmography is a test that looks at eye movements to see how well two nerves in the brain are working. These nerves are:
- Vestibular nerve (eighth cranial nerve), which runs from the brain to the ears
- Occulomotor nerve (third cranial nerve), which runs from the brain to the eyes
You may have electronystagmography test if you have:
- Dizziness or vertigo
- Hearing loss
- Possible damage to the inner ear from certain medicines
How the electronystagmography test is performed
Patches called electrodes are placed above, below, and on each side of your eyes. They may be sticky patches or attached to a headband. Another patch is attached to the forehead.
The health care provider will spray cold water or air into each ear canal at separate times. The patches record eye movements that occur when the inner ear and nearby nerves are stimulated by the water or air. When cold water enters the ear, you should have rapid, side-to-side eye movements called nystagmus.
Next, warm water or air is placed into the ear. The eyes should now move rapidly toward the warm water then slowly away.
You may also be asked to use your eyes to track objects, such as flashing lights or moving lines.
The test takes about 90 minutes.
How to prepare for the electronystagmography test
Most of the time, you do not need to take special steps before this test.
- Your doctor will tell you if you need to stop taking any medicines before you have this test.
- DO NOT stop or change your medicines without talking to your doctor first.
How the electronystagmography test will feel
You may find cold water in the ear slightly uncomfortable. Brief dizziness (vertigo) may occur during the test. You may have nausea or vomiting during the test.
Normal Results
- Certain eye movements should occur after the warm or cold water or air is placed into your ears.
Note: Normal value ranges may vary slightly among different laboratories. Talk to your doctor about the meaning of your specific test results.
What does abnormal results mean
Abnormal results may be a sign of damage to the nerve of the inner ear or other parts of the brain that control eye movements.
Any disease or injury that damages the acoustic nerve can cause vertigo. This may include:
- Blood vessel disorders with bleeding (hemorrhage), clots, or atherosclerosis of the blood supply of the ear
- Cholesteatoma and other ear tumors
- Congenital disorders
- Injury
- Medicines that are toxic to the ear nerves, including aminoglycoside antibiotics, some antimalarial drugs, loop diuretics, and salicylates
- Multiple sclerosis
- Movement disorders such as progressive supranuclear palsy
- Rubella
- Some poisons
Additional conditions under which the electronystagmography test may be performed:
- Acoustic neuroma
- Benign paroxysmal positional vertigo
- Labyrinthitis
- Meniere disease
Risks of electronystagmography test
Rarely, too much water pressure inside the ear can injure your ear drum if there has been previous damage. The water part of this test should not be done if your eardrum has been perforated recently.
Caloric stimulation test
Caloric stimulation is a test that uses differences in temperature to diagnose damage to the acoustic nerve. This is the nerve that is involved in hearing and balance. The test also checks for damage to the brain stem.
Caloric stimulation test may be used to find the cause of:
- Dizziness or vertigo
- Hearing loss that may be due to certain antibiotics or other drugs
It may also be done to look for brain damage in people who are in a coma.
How the caloric stimulation test is performed
This test stimulates your acoustic nerve by delivering cold or warm water or air into your ear canal. When cold water or air enters your ear and the inner ear changes temperature, it should cause fast, side-to-side eye movements called nystagmus. The test is done in the following way:
- Before the test, your ear, especially the eardrum, will be checked. This is to make sure it is normal.
- One ear is tested at a time.
- A small amount of cold water or air is gently delivered into one of your ears. Your eyes should show an involuntary movement called nystagmus. Then they should turn away from that ear and slowly back. If water is used, it is allowed to drain out of the ear canal.
- Next, a small amount of warm water or air is gently delivered into the same ear. Again, your eyes should show nystagmus. Then they should turn toward that ear and slowly back.
- Your other ear is tested in the same way.
During the test, the health care provider may observe your eyes directly. Most often, this test is done as part of another test called electronystagmography.
How to prepare for the caloric stimulation test
DO NOT eat a heavy meal before the test. Avoid the following at least 24 hours before the test, because they can affect the results:
- Alcohol
- Allergy medicines
- Caffeine
- Sedatives
DO NOT stop taking your regular medicines without first talking to your provider.
How the caloric stimulation test will feel
You may find the cold water or air in the ear uncomfortable. You may feel your eyes scanning back and forth during nystagmus. You may have vertigo, and sometimes, you can also have nausea. This lasts only a very short time. Vomiting is rare.
Normal Results
Rapid, side-to-side eye movements should occur when cold or warm water is placed into the ear. The eye movements should be similar on both sides.
What Abnormal Results Mean
If the rapid, side-to-side eye movements do not occur even after ice cold water is given, there may be damage to the:
- Nerve of the inner ear
- Balance sensors of the inner ear
- Brain
Abnormal results may be due to:
- Poor blood supply to the ear
- Bleeding (hemorrhage)
- Blood clot
- Brain or brain stem damage
- Cholesteatoma (a type of skin cyst in the middle ear and mastoid bone in the skull)
- Birth defects of the ear structure or brain
- Damage to the ear nerves
- Poisoning
- Rubella that damages the acoustic nerve
- Trauma
The caloric stimulation test may also be done to diagnose or rule out:
- Acoustic neuroma (tumor of the acoustic nerve)
- Benign paroxysmal positional vertigo
- Labyrinthitis (irritation and swelling of the inner ear)
- Meniere disease (inner ear disorder that affects balance and hearing)
Risks of electronystagmography test
Too much water pressure can injure an already damaged eardrum. This rarely occurs because the amount of water to be used is measured.
Water caloric stimulation should not be done if the eardrum is torn (perforated). This is because it can cause an ear infection. It also should not be done during an episode of vertigo because it can make symptoms worse.
Electroencephalogram (EEG)
Brain cells communicate with each other by producing tiny electrical signals, called impulses. An electroencephalogram (EEG) is a test to measure the electrical activity of the brain. An electroencephalogram (EEG) can be used to diagnose or monitor the following health conditions:
- Seizures and epilepsy
- Abnormal changes in body chemistry that affect the brain
- Brain diseases, such as Alzheimer disease
- Confusion
- Fainting spells or periods of memory loss that cannot be explained otherwise
- Head injuries
- Infections
- Tumors
An electroencephalogram (EEG) is also used to:
- Evaluate problems with sleep (sleep disorders)
- Monitor the brain during brain surgery
An EEG may be done to show that the brain has no activity, in the case of someone who is in a deep coma. It can be helpful when trying to decide if a person is brain dead.
An electroencephalogram (EEG) cannot be used to measure intelligence.
How the electroencephalogram (EEG) test is performed
The electroencephalogram (EEG) test is done by an electroencephalogram technologist in your doctor’s office or at a hospital or laboratory.
The electroencephalogram (EEG) test is done in the following way:
- You lie on your back on a bed or in a reclining chair.
- Flat metal disks called electrodes are placed all over your scalp. The disks are held in place with a sticky paste. The electrodes are connected by wires to a recording machine. The machine changes the electrical signals into patterns that can be seen on a monitor or drawn on paper. These patterns look like wavy lines.
- You need to lie still during the test with your eyes closed. This is because movement can change the results. You may be asked to do certain things during the test, such as breathe fast and deeply for several minutes or look at a bright flashing light.
- You may be asked to sleep during the test.
If your doctor needs to monitor your brain activity for a longer period, an ambulatory EEG will be ordered. In addition to the electrodes, you will wear or carry a special recorder for up to 3 days. You will be able to go about your normal routine as the EEG is being recorded. Or, your doctor may ask you to stay overnight in a special EEG monitoring unit where your brain activity will be monitored continuously.
How to prepare for the electroencephalogram (EEG) test
Wash your hair the night before the test. DO NOT use conditioner, oils, sprays, or gel on your hair. If you have a hair weave, ask your health care provider for special instructions.
Your provider may want you to stop taking certain medicines before the test. DO NOT change or stop taking any medicines without first talking to your provider. Bring a list of your medicines with you.
Avoid all food and drinks containing caffeine for 8 hours before the test.
You may need to sleep during the test. If so, you may be asked to reduce your sleep time the night before. If you are asked to sleep as little as possible before the test, DO NOT eat or drink any caffeine, energy drinks, or other products that help you stay awake.
Follow any other specific instructions you are given.
How the electroencephalogram (EEG) test will feel
The electrodes may feel sticky and strange on your scalp, but should not cause any other discomfort. You should not feel any discomfort during the test.
Normal Results
Brain electrical activity has a certain number of waves per second (frequencies) that are normal for different levels of alertness. For example, brain waves are faster when you are awake, and slower in certain stages of sleep.
There are also normal patterns to these waves.
Note: A normal EEG does not mean that a seizure did not occur.
What Abnormal Results Mean
Abnormal results on an EEG test may be due to:
- Abnormal bleeding (hemorrhage)
- An abnormal structure in the brain (such as a brain tumor)
- Tissue death due to a blockage in blood flow (cerebral infarction)
- Drug or alcohol abuse
- Head injury
- Migraines (in some cases)
- Seizure disorder (such as epilepsy)
- Sleep disorder (such as narcolepsy)
- Swelling of the brain (edema)
Risks of electroencephalogram (EEG) test
An EEG test is very safe. The flashing lights or fast breathing (hyperventilation) required during the test may trigger seizures in those with seizure disorders. The provider performing the EEG is trained to take care of you if this happens.
Benign paroxysmal positional vertigo treatment
Fortunately, in the vast majority of cases, benign paroxysmal positional vertigo can be corrected mechanically. Once your healthcare provider knows which canal(s) the crystals are in, and whether it is canalithiasis or cupulolithiasis, then they can take you through the appropriate treatment maneuver. The maneuvers make use of gravity to guide the crystals back to the chamber where they are supposed to be via a very specific series of head movements called Canalith Repositioning Maneuvers. In the case of cupulolithiasis, they would utilize rapid head movement in the plane of the affected canal to try to dislodge the ‘hung-up’ crystals first, called a Liberatory Maneuver, and then guide them out as described above.
One maneuver that is used for the most common location and type of benign paroxysmal positional vertigo is called the Epley maneuver. It is a series of head movements to reposition the canaliths in your inner ear. The procedure may need to be repeated if symptoms come back, but this treatment works best to cure benign paroxysmal positional vertigo. However, Epley maneuver will not work for all presentations of benign paroxysmal positional vertigo. Often people have tried the Epley maneuver themselves or had it performed on them without success. Later assessment reveals that it is actually a different maneuver that should have been used, or that it is not benign paroxysmal positional vertigo at all. This is why caution should be used with self-treatment or with being treated by someone who is not fully trained in identifying the many different variants of benign paroxysmal positional vertigo and respective treatment maneuvers. Additionally, before testing or treating for benign paroxysmal positional vertigo, the healthcare provider should perform a careful neurological scan, evaluation of the neck, and other safety-related investigations to determine if certain elements of the procedure need to be modified or avoided. This is another strong reason for caution with self-treatment or treatment by a minimally trained healthcare provider.
Your doctor may also teach you other repositioning exercises that you can do at home, but may take longer than the Epley maneuver to work. Other exercises, such as balance therapy, may help some people.
Some medicines can help relieve spinning sensations:
- Antihistamines
- Anticholinergics
- Sedative-hypnotics
But, these medicines often do not work well and and there is no evidence to support its use in treatment of benign paroxysmal positional vertigo 6.
In extremely rare circumstances, surgical options are considered. The frequency of surgery as a treatment for benign paroxysmal positional vertigo has dropped in recent years. Surgery for benign paroxysmal positional vertigo is reserved for individuals who fail to respond to less invasive treatment options and for whom symptoms are recurrent and problematic (intractable benign paroxysmal positional vertigo). The most common procedure used is plugging (occluding) the posterior semicircular canal in order to prevent crystals from causing deflection and stimulation of the cupula. Another procedure, called singular neurectomy, has also been discussed in the medical literature as a potential therapy for intractable benign paroxysmal positional vertigo. During a singular neurectomy, a surgeon cuts a specific nerve to the posterior semicircular canal, thereby eliminating the abnormal signals being transmitted from the inner ear. This causes symptoms to improve. However, single neurectomy is a difficult procedure and is rarely performed because it carries a risk of hearing loss. Canal plugging is used more often in the rare cases that require surgical intervention. Although it also has a risk of associated hearing loss, the hearing loss is usually temporary (transient). Surgical therapy is not considered for benign paroxysmal positional vertigo except as a last resort.
Follow instructions on how to take care for yourself at home. To keep your symptoms from getting worse, avoid the positions that trigger it.
Benign paroxysmal positional vertigo maneuver
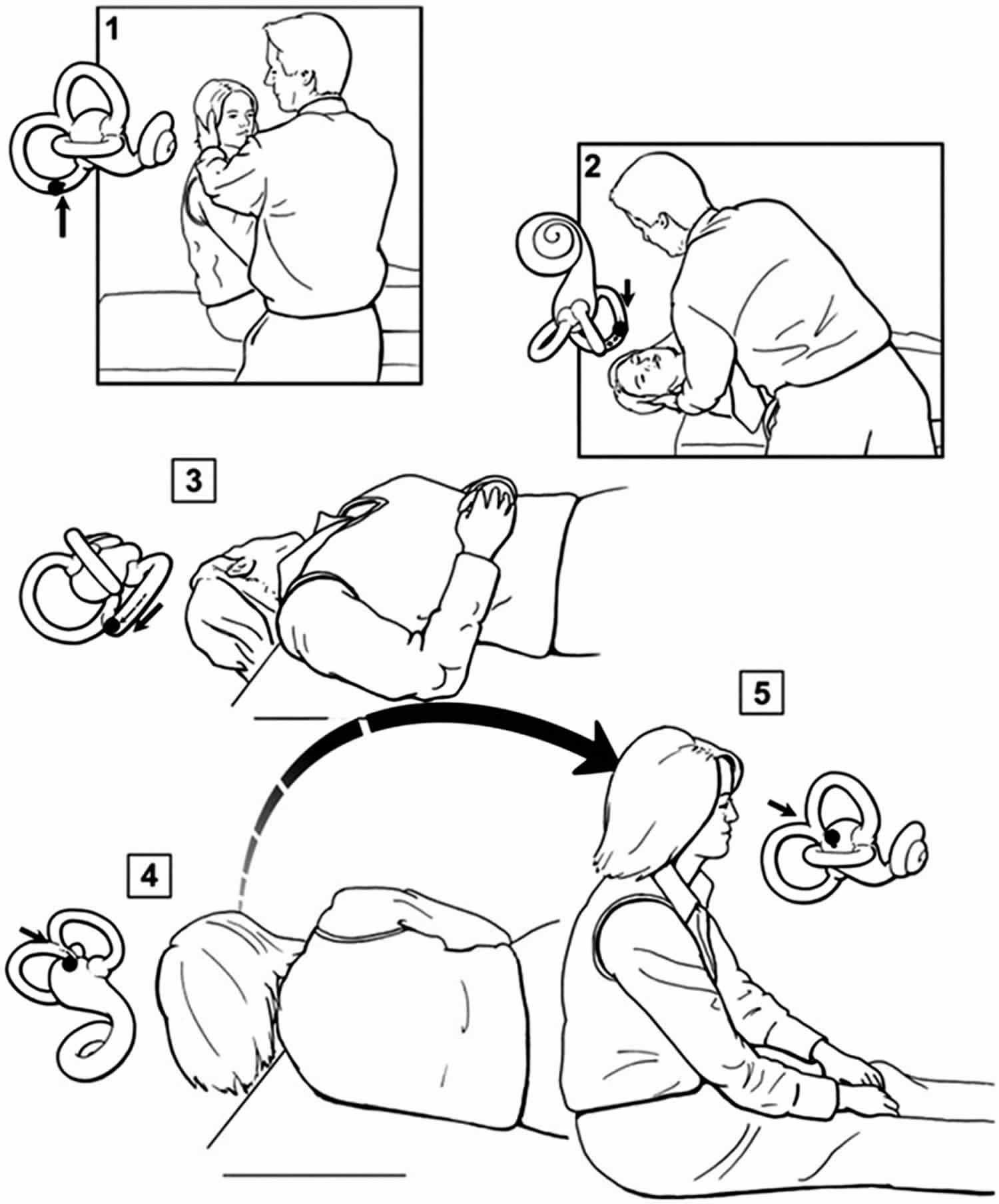
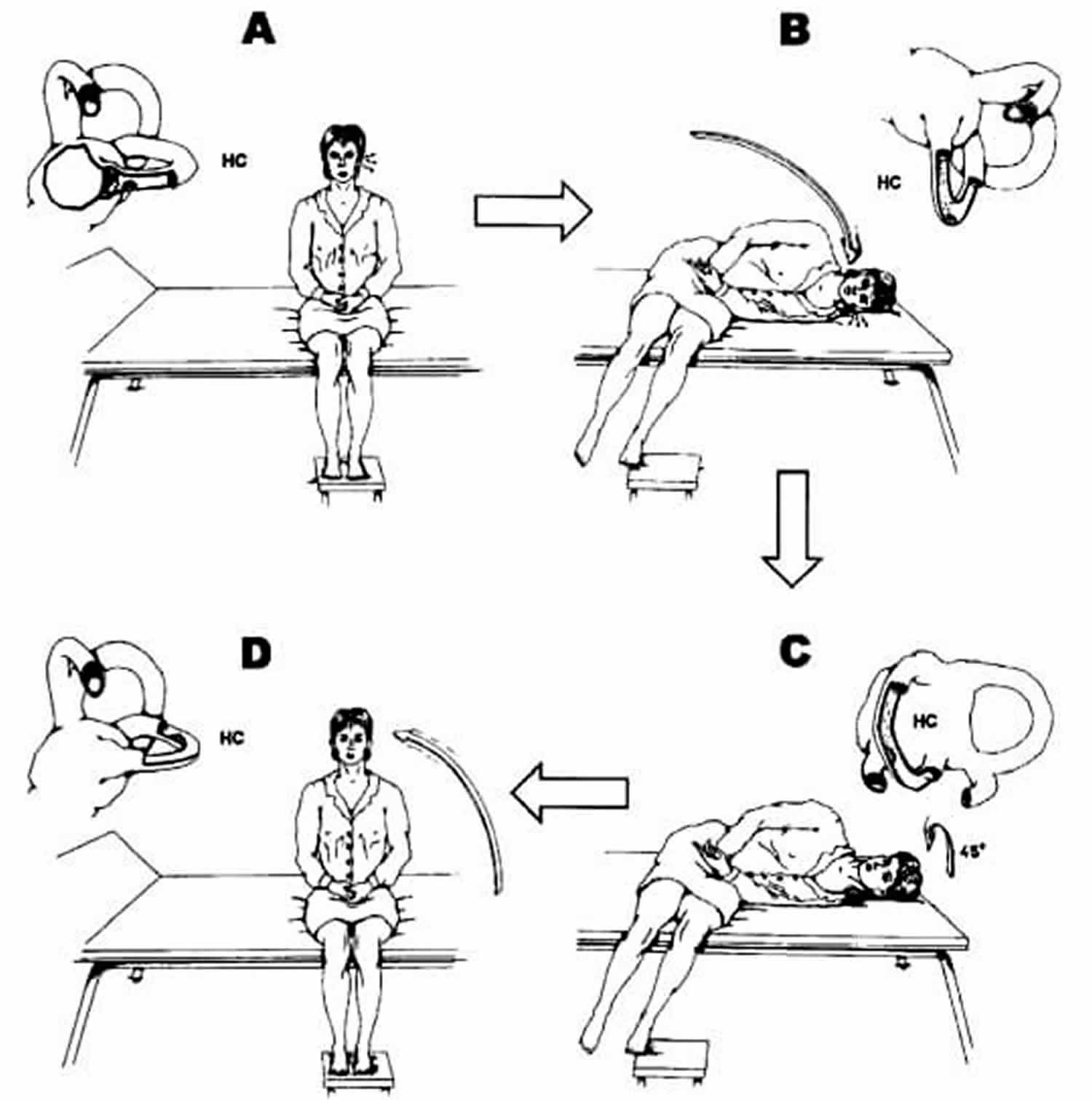
Benign paroxysmal positioning vertigo is treated with positioning maneuvers: rapid repositioning of the head can move the otoconial agglomerate out of the semicircular canal so that it can no longer cause positioning vertigo 8. The treatments of choice are the Semont 11 and Epley maneuvers. For the Semont maneuver, see Figure 6; the Epley maneuver involves rotation of the patient in the recumbent position with the head hanging down. Most patients can perform these maneuvers themselves after brief training. The two are equally effective, and the cure rate is more than 95% within a few days, as shown by multiple controlled studies and meta-analyses 12. The rate of recurrence of benign paroxysmal positioning vertigo is about 15% to 30% per year. The symptoms eventually recur at some time after effective treatment in about 50% of patients 13 but can then be treated effectively a second time in the same manner.
Epley maneuver – for BPPV
The Epley maneuver is a series of head movements to relieve symptoms of benign positional vertigo. Benign positional vertigo is also called benign paroxysmal positional vertigo (BPPV). Benign paroxysmal positional vertigo is caused by a problem in the inner ear. Vertigo is the feeling that you are spinning or that everything is spinning around you.
The patient is placed in the upright position, with eyes open and head turned 45 degrees toward the affected ear (right side) (step 1) and then laid back quickly to a position with the head extended below the shoulders, the head hanging 20 degrees off the end of the examination table (step 2). If benign paroxysmal positional vertigo (BPPV) is present, nystagmus ensues usually within seconds. The patient is held in the right head hanging 20 degrees off the end of the examination table (step 2) for 30 seconds, and then in step 3 the head is turned 90 degrees toward the unaffected side (left side). Step 3 the patient remains in this position for 30 seconds before the head is turned an additional 90 degrees to the left while the patient rotates his or her body 90 degrees in the same direction (step 4) so that the head is nearly in the face-down position. The patient remains in this position for 30 seconds (step 4). The patient sits up on the left side of the examination table. The movement of the particles within the labyrinth is depicted with each step, showing how particles are moved from the semicircular canal to the vestibule.
The procedure may be repeated on either side until the patient experiences relief of symptoms.
Figure 6. Epley maneuver for right-sided benign paroxysmal positional vertigo (BPPV)
[Source 14 ]Before the Epley maneuver procedure
Tell your provider about any medical conditions that you may have. The procedure may not be a good choice if you have had recent neck or spine problems or a detached retina.
For severe vertigo, your provider may give you medicines to reduce nausea or anxiety before starting the procedure.
After the Epley maneuver procedure
The Epley maneuver often works quickly. For the rest of the day, avoid bending over. For several days after treatment, avoid sleeping on the side that triggers symptoms.
After you go home:
- For the rest of the day, DO NOT bend over.
- For several days after treatment, DO NOT sleep on the side that triggers symptoms.
- Sleep semi-recumbent for the next two nights (head at a 45 degree angle). This is most easily done by using a recliner chair or by using pillows arranged on a couch. During the day, try to keep your head vertical and stilll.
- For at least one week, avoid provoking head positions that might bring BPPV on again. Use two pillows when you sleep. Avoid sleeping on the "bad" side. Don’t turn your head far up or far down. Be careful to avoid head-extended positions. This basically means to be cautious at the beauty parlor, dentist’s office, and while undergoing minor surgery where the head is often bent back. Try to stay as upright as possible.
- One week after treatment, no more restrictions are required and hopefully, the dizziness has completely resolved.
- Follow any other specific instructions your provider gave you.
Most of the time, treatment will cure benign paroxysmal positional vertigo. Sometimes, vertigo may return after a few weeks. About half the time, benign paroxysmal positional vertigo will come back later on. If this happens, you will need to be treated again. Your provider may prescribe medicines that can help relieve spinning sensations. But, these medicines often do not work well for treating the actual vertigo.
Risks of Epley maneuver
During the procedure, you may experience:
- Intense vertigo symptoms
- Nausea
- Vomiting (less common)
In a few people, the canaliths may move into another canal in the inner ear and continue to cause vertigo.
Deep Head Hanging Maneuver to treat benign paroxysmal positional vertigo
Particle repositioning maneuver
Although Epley had been teaching his technique for many years, it was not until 1992 that Epley 15 published his first report on the “canalith repositioning procedure” (Epley maneuver). This highly successful “Epley maneuver” is performed with the patient sedated. Mechanical skull vibration is routinely used and the patient’s head is moved sequentially through 5 separate positions. Epley postulated that the procedure enabled the otolithic debris to move under the influence of gravity from the posterior semicircular canal into the utricle. Most clinicians today are thought to use a modified version of the Epley maneuver.
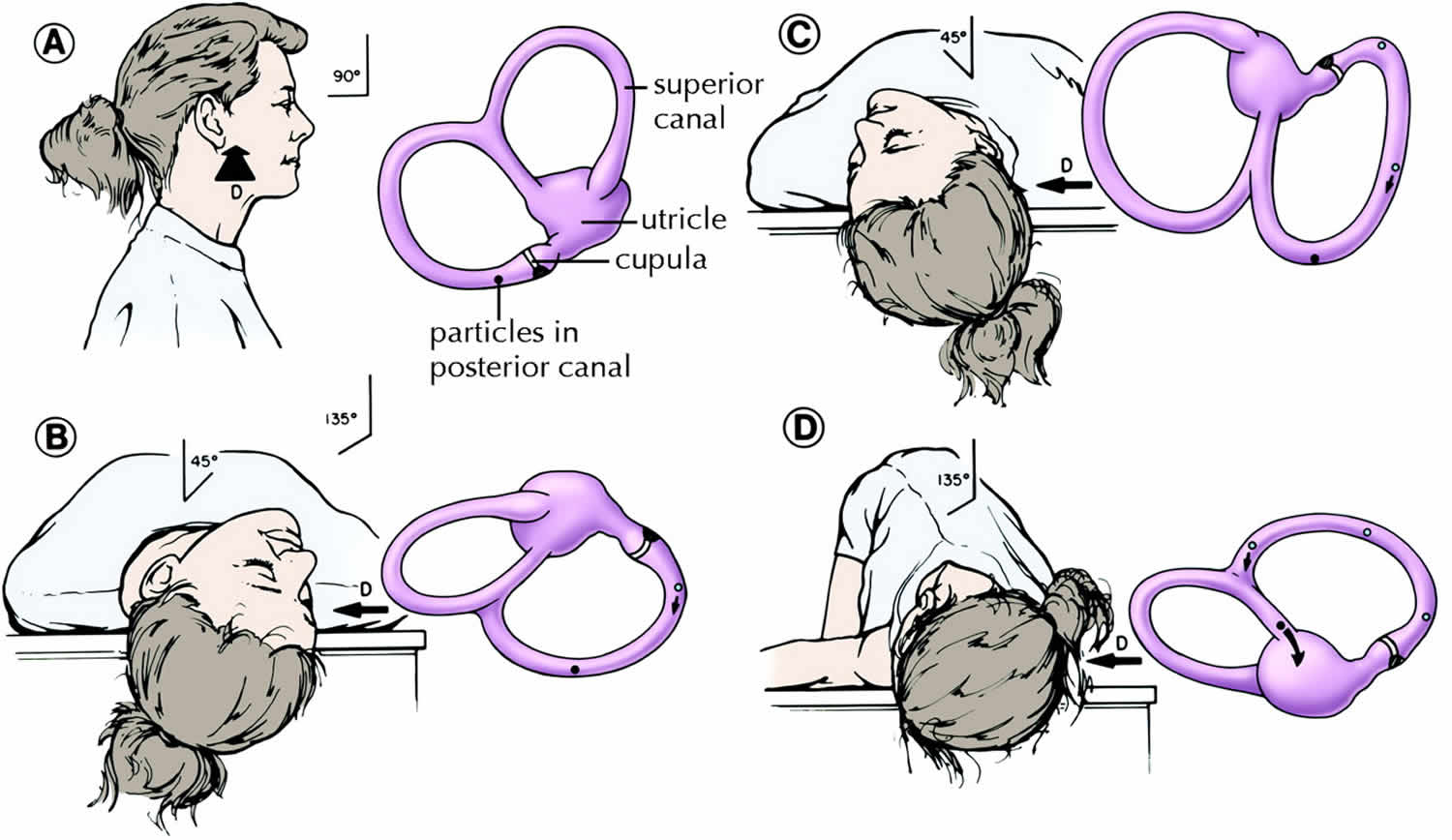
One modified Epley maneuver is the “particle repositioning maneuver” which is a 3-position maneuver that eliminates the need for sedation and mastoid vibration (Figure 6) 16. With proper understanding of inner ear anatomy and the pathophysiology of BPPV, various appropriately trained health professionals, including family doctors and physiotherapists, should be able to successfully carry out the modified Epley maneuver (canalith repositioning procedure) in most straightforward cases. Atypical cases or cases that do not respond to this maneuver should be referred to a tertiary care dizziness clinic.
In the modified Epley maneuver (particle repositioning maneuver) 7:
- Place the patient in a sitting position
- Move the patient to the head-hanging Dix–Hallpike position of the affected ear
- Observe the eyes for “primary stage” nystagmus
- Maintain this position for 1–2 minutes (position B)
- The head is turned 90° to the opposite Dix–Hallpike position while keeping the neck in full extension (position C)
- Continue to roll the patient another 90° until his or her head is diagonally opposite the first Dix–Hallpike position (position D). The change from position B, through C, into D, should take no longer than 3–5 seconds
- The eyes should be immediately observed for “secondary stage” nystagmus. If the particles continue moving in the same ampullofugal direction, that is, through the common crus into the utricle, this secondary stage nystagmus should beat in the same direction as the primary stage nystagmus.
- This position is maintained for 30–60 seconds and then the patient is asked to sit up. With a successful manoeuvre, there should be no nystagmus or vertigo when the patient returns to the sitting position because the particles will have already been repositioned into the utricle 17.
Overall, the modified Epley maneuver (particle repositioning maneuver) should take less than 5 minutes to complete. Patients are then typically asked to remain upright for the next 24–48 hours in order to allow the otoliths to settle, so as to prevent a recurrence of the BPPV.
Figure 7. Modified Epley maneuver
[Source 7 ]Semont Maneuver
An alternative maneuver which may help posterior BPPV is called the Semont or “liberatory maneuver” demonstrated in the image below when the right ear is affected.
- Patient is made to sit on the examination table with legs hanging over the edge and head turned 45 degrees horizontally towards the unaffected ear.
- While maintaining head rotation patient’s upper body is swiftly moved to side lying position on the affected side with head resting on examination table and nose pointed upwards. Position is maintained for 3-5 minutes or till vertigo and nystagmus subsides. This step moves the debris to the apex.
- Patient is rapidly moved through the sitting position (Position 1) to lying on the opposite or unaffected side (maintaining same head rotation) with nose pointed to the ground. Position is again maintained for 3-10 minutes or till the vertigo and nystagmus subsides, before slowly being brought back to the sitting position. This maneuver moves the debris towards exit of the canal.
In their series of 711 patients, Semont and colleagues 18 found an 84% response rate after 1 procedure and a 93% response rate after a second procedure 1 week later. Several other case series have had response rates of 52%–90% 5, with recurrence rates of up to 29% 19. There has been no difference in efficacy shown between the liberatory manoeuvre and particle repositioning manoeuvre, which is described in the following section, in randomized studies by Herdman and colleagues 20 and Cohen and Jerabek 21. The liberatory maneuver of Semont is effective, but is cumbersome with elderly and obese patients, and shows no increased efficacy compared with the simple particle repositioning maneuver (modified Epley maneuver).
Figure 8. The treatment of benign paroxysmal positioning vertigo with the Semont maneuver
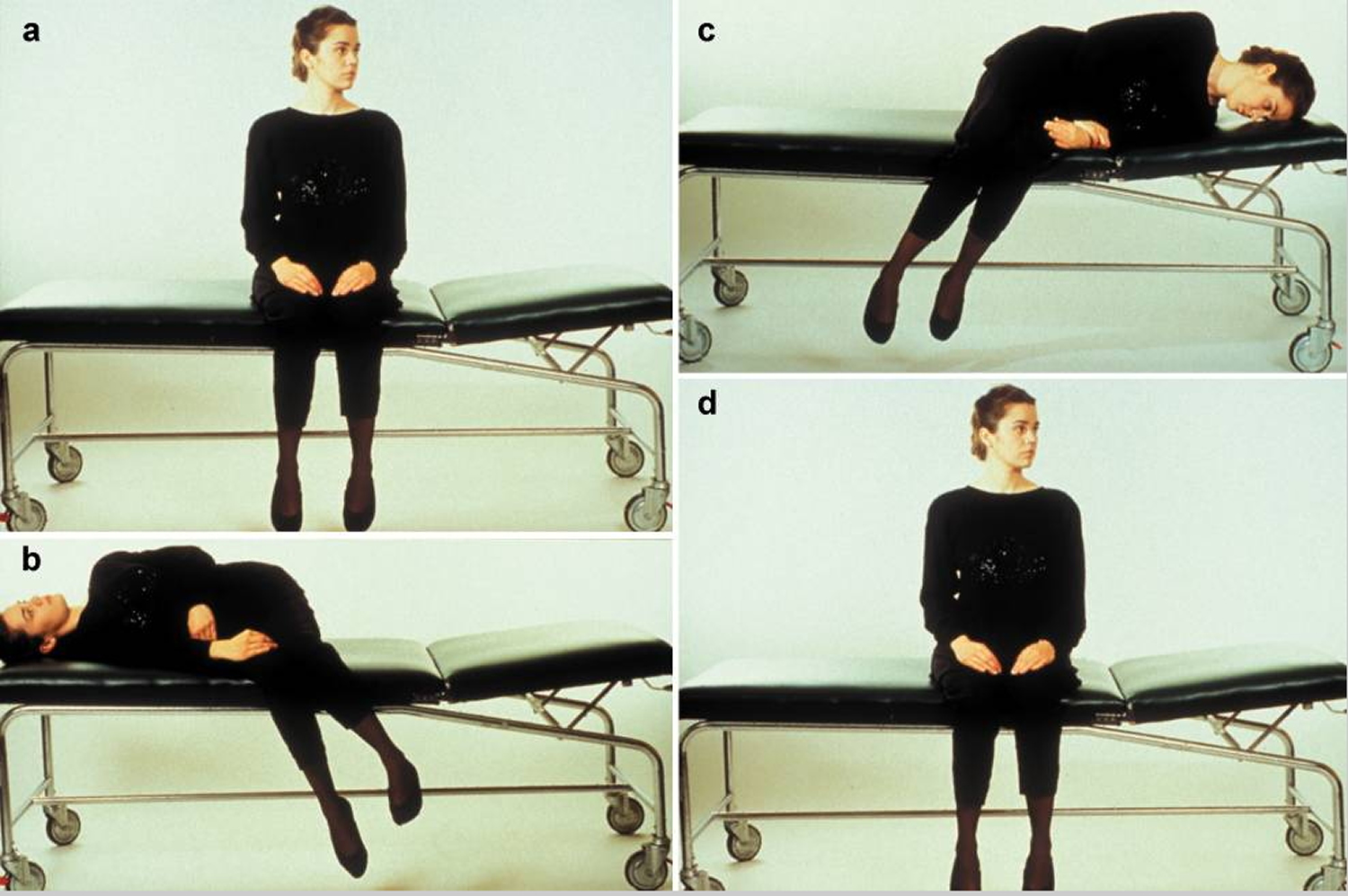
Footnote: The illustration shows the treatment of benign paroxysmal positioning vertigo (BPPV) due to canalolithiasis of the right posterior semicircular canal.
a) In the initial, sitting position, the head is turned 45° to the side of the unaffected (“healthy”) ear.
b) The patient is laid on the right side, i.e., on the side of the affected ear, while the head is kept in 45° of rotation to the other side. This induces movement of the particulate matter in the posterior semicircular canal by gravity, leading to rotatory nystagmus toward the lower ear that extinguishes after a brief interval. The patient should maintain this position for about one minute.
c) While the head is still kept in 45° of rotation toward the side of the healthy ear, the patient is rapidly swung over to the side of the unaffected ear, so that the nose now points downward. The particulate matter in the semicircular canal now moves toward the exit from the canal. This position, too, should be maintained for at least one minute.
d) The patient returns slowly to the initial, sitting position. The particulate matter settles in the utricular space, where it can no longer induce rotatory vertigo. This sequence (a-d) should be performed three times in a row three times per day, in the morning, at noon, and at night. Most patients are free of symptoms after doing this for three days.
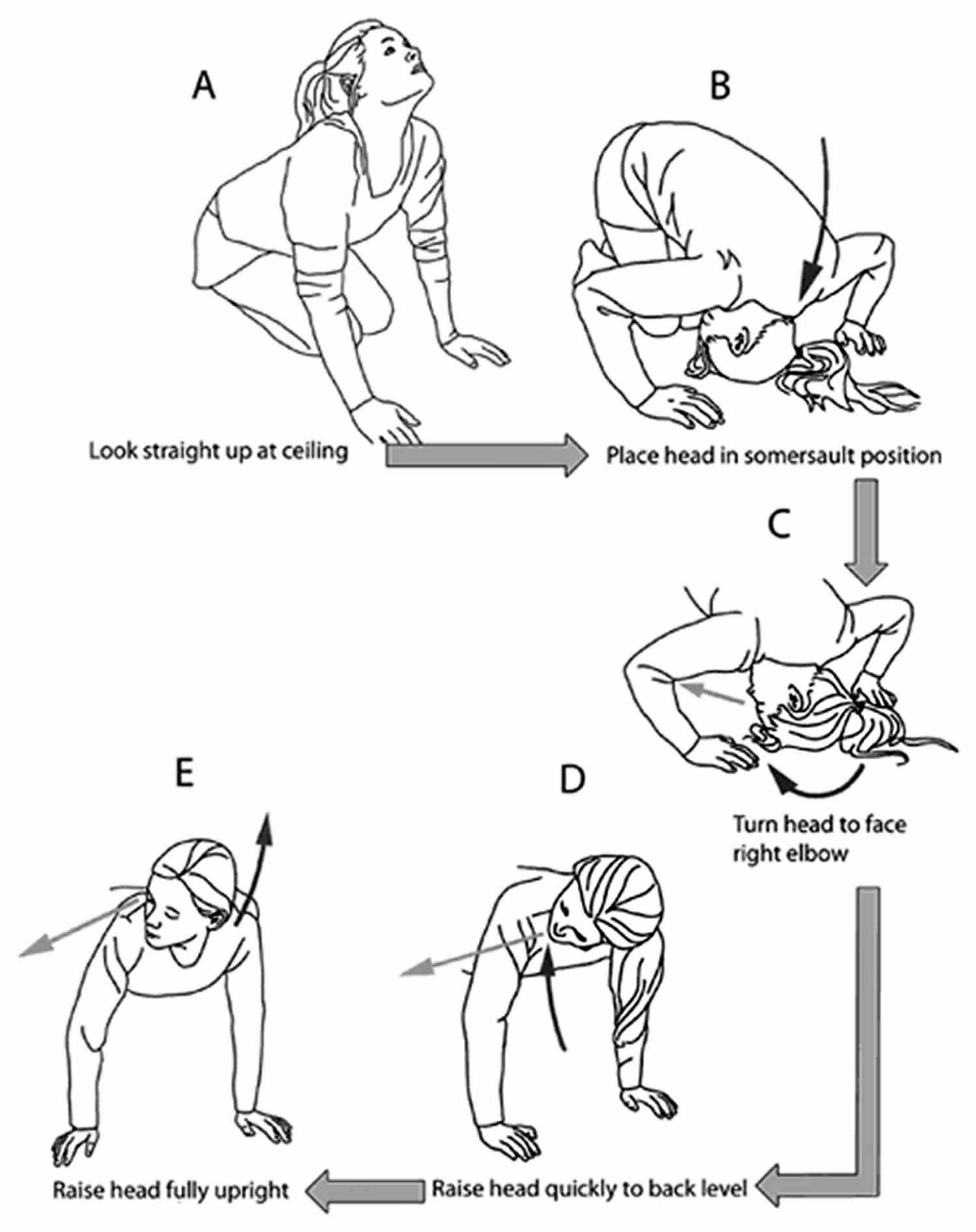
[Source 8]Foster Half-Somersault
The Foster Half-Somersault is probably the most feasible to perform in situations where laying down is not possible (i.e., at work or in a public place).
Half somersault for right-sided BPPV. After each position change, any dizziness is allowed to subside before moving into the next position; if there is no dizziness, the position should be held for 15 s. (A) While kneeling, the head is quickly tipped upward and back. (B) The somersault position is assumed, with the chin tucked as far as possible toward the knee. (C) The head is turned about 45° toward the right shoulder, to face the right elbow. (D) Maintaining the head at 45°, the head is raised to back/shoulder level. (E) Maintaining the head at 45°, the head is raised to the fully upright position. Dark curved arrows show head movements. Lighter arrows near eyes show the direction one should be facing.
- While kneeling, the head is quickly tipped upward and back.
- The somersault position is assumed, with the chin tucked as far as possible toward the knee.
- The head is turned about 45° toward the right shoulder, to face the right elbow (if the right ear is affected).
- Maintaining the head at 45°, the head is raised to back/shoulder level.
- Maintaining the head at 45°, the head is raised to the fully upright position. Dark curved arrows show head movements. Lighter arrows near eyes show the direction one should be facing.
Figure 9. Foster Half-Somersault maneuver
[Source 22 ]Half Somersault Maneuver to treat benign paroxysmal positional vertigo
Lateral (or Hoizontal) Canal BPPV
The lateral semi-circular canal is a less common location where BPPV occurs (5-20% of all BPPV). Dix-Hallpike is usually positive revealing a horizontal nystagmus that changes direction according to the ear that is down. But, the best test is the supine roll test which starts with the body laid flat on the back, head inclined forward 30 degrees, and then turning the head to either side.
The “barrel roll” was described by Epley 23 and involves rolling the patient 360°, from supine position to supine position, keeping the lateral semicircular canal perpendicular to the ground. The patient is rolled away from the affected ear in 90° increments until a full roll is completed. This is believed to move the particles out of the involved canal into the utricle. For less agile patients, Lempert and Tiel-Wilck 24 proposed the “log roll.” Here, the patient begins with his or her head turned completely toward the affected ear. The patient is then rapidly turned away from the affected ear in 90 degree increments for a total of 270 degree, with the head being held in each position for about 1 minute. Only 2 patients were in the study, but both were completely relieved of their vertigo.
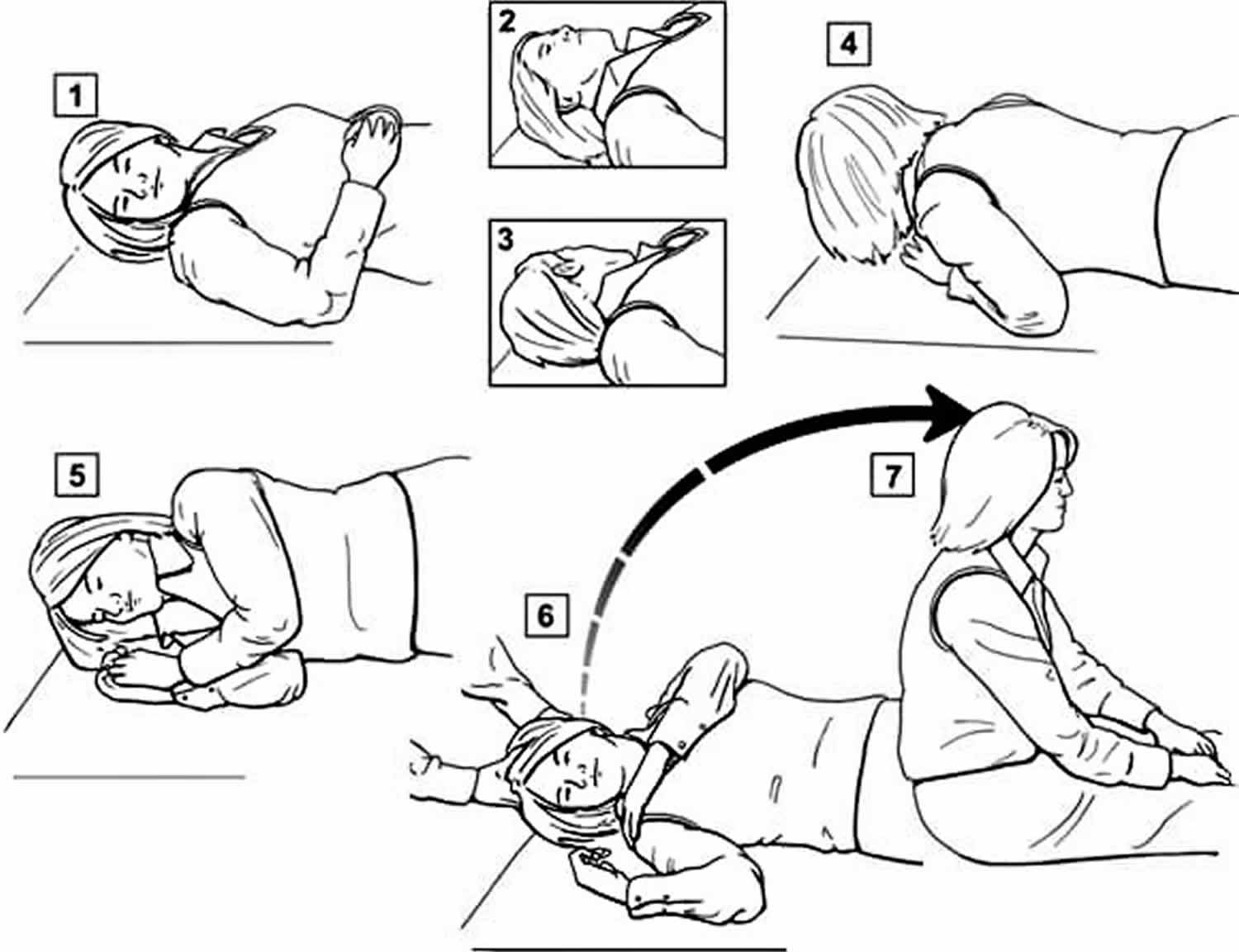
Lempert Maneuver
Log-roll (Lempert) exercises may also work and can be performed at home. This exercise essentially begins by laying down with head turned to side of the bad ear. From this side position, the patient than turns head in 90 degree steps rolling onto the back as the turns happen. Each turn is held for 30 seconds. The maneuver is completed when the patient has rolled 360 degrees before sitting up.
Lempert (BBQ) Maneuver to treat benign paroxysmal positional vertigo
Figure 10. Lempert maneuver
Gufoni Maneuver
This is a series of physical head maneuvers known as the Gufoni which is used to treat lateral BPPV.
There are two types of Gufoni Maneuver for lateral BPPV:
- For the geotrophic variant of lateral BPPV, one starts on the unaffected side (side of weaker nystagmus), and then proceeds to 45 deg nose down.
- For the ageotrophic variant, one starts on the affected side (again side of weaker nystagmus), and proceeds to 45 deg nose up (Step C) which is demonstrated in the image below.
Figure 11. Gufoni Maneuver
Benign paroxysmal positional vertigo treatment at home
Brandt-Daroff exercises
Home treatment with Brandt-Daroff exercises can also be successful (see video below). If there is no improvement with repeated repositioning Epley, Semont, or Foster maneuvers, or if atypical or ongoing nystagmus with nausea is present, another cause should be considered 25. Pharmacologic treatment has no role in the treatment of BPPV. Vestibular suppressant medications should be avoided because they interfere with central compensation and may increase the risk of falls 26.
Benign paroxysmal positional vertigo exercises
Some affected individuals may be referred for vestibular rehabilitation therapy (VRT). Vestibular rehabilitation therapy is the use of specific exercises that are designed to compensate for inner ear deficiencies. While this technique may coincidentally improve benign paroxysmal positional vertigo, it is really intended to promote adaptation by the brain to loss of balance function related to inner ear on one side. A physical or occupational therapist will develop a treatment plan tailored to an individual based upon a thorough examination. Basically, affected individuals will perform a series of exercises or postures that over time will lessen their symptoms. Initially, the exercises may temporarily worsen symptoms. However, if affected individuals persist with their instructions, vestibular rehabilitation therapy often leads to a decrease in symptom severity or complete disappearance of symptoms. In some cases, no other therapy is necessary.
Benign paroxysmal positional vertigo self-care
If vertigo returns, remember that you can easily lose your balance, fall, and hurt yourself. To help keep symptoms from getting worse and to help keep you safe:
- Sit down right away when you feel dizzy.
- To get up from a lying position, slowly sit up and stay seated for a few moments before standing.
- Make sure you hold on to something when standing.
- Avoid sudden movements or position changes.
- Ask your doctor about using a cane or other walking aid when you have a vertigo attack.
- Avoid bright lights, TV, and reading during a vertigo attack. They may make symptoms worse.
- Avoid activities such as driving, operating heavy machinery, and climbing while you are having symptoms.
To keep your symptoms from getting worse, avoid the positions that trigger it. Your doctor may show you how to treat yourself at home for benign paroxysmal positional vertigo. A physical therapist may be able to teach you other exercises to reduce your symptoms.
Having benign paroxysmal positional vertigo can be stressful. Make healthy lifestyle choices to help you cope:
- Eat a well-balanced, healthy diet. DO NOT overeat.
- Exercise regularly, if possible.
- Get enough sleep.
- Limit caffeine and alcohol.
- Learn to ease stress by using relaxation techniques, such as yoga, tai chi, or progressive muscle relaxation.
You should see your doctor if:
- Symptoms of vertigo return
- You have new symptoms
- Your symptoms are getting worse
- Home treatment does not work
Surgical treatment
BPPV is a benign disease and, therefore, surgery should only be reserved for the most intractable or multiply recurrent cases. Furthermore, before considering surgery, the posterior fossa should be imaged to rule out central lesions that might mimic BPPV 27.
Singular neurectomy
Singular neurectomy, or section of the posterior ampullary nerve, which sends impulses exclusively from the posterior semicircular canal to the balance part of the brain, was popularized by Gacek 28 in the 1970s. Although initial reports by Gacek 29 demonstrated high efficacy, there was a significant risk of sensorineural hearing loss 30 and the procedure has been found to be technically demanding. It has largely been replaced by the simpler posterior semicircular canal occlusion 31.
Posterior semicircular canal occlusion
Parnes and McClure 32 introduced the concept of posterior semicircular canal occlusion for BPPV. Obstruction of the semicircular canal lumen is thought to prevent endolymph flow. This effectively fixes the cupula and renders it unresponsive to normal angular acceleration forces and, more importantly, to stimulation from either free-floating particles within the endolymph or a fixed cupular deposit. Until the advent of this procedure, invasive inner ear surgery was felt to be too risky to otherwise normal- hearing ears. However, Parnes and McClure 33 laid the groundwork for this procedure in an animal model by demonstrating its negligible effect on hearing.
The procedure is performed under general anesthetic and should take no longer than 2–3 hours. Using a 5–6-cm postauricular incision, the posterior canal is accessed through a mastoidectomy. With the use of an operating microscope and drill, a 1-mm х3-mm fenestration is made in the bony posterior canal. A plug, fashioned from bone dust and fibrinogen glue, is used to occlude the canal. Most patients stay in hospital for 2–3 days after this procedure. Because the occlusion also impairs the normal inner ear physiology, all patients are expected to have postoperative imbalance and disequilibrium. For most people, the brain adapts to this after a few days to a few weeks, with vestibular physiotherapy hastening this process.
In 2001, Agrawal and Parnes 34 published a series of cases of 44 occluded posterior canals in 42 patients. All 44 ears were relieved of BPPV, with only 1 having a late atypical recurrence. Of the 40 ears with normal preoperative hearing, 1 had a delayed (3-month) sudden and permanent profound loss, whereas another had mild (20 dB) hearing loss.
Further studies by Pace-Balzan and Rutka 35, Dingle and colleagues 36, Hawthorne and el-Naggar 37, Anthony 38, and Walsh and colleagues 39 have supported the safety and efficacy of this procedure. In most otology clinics, posterior semicircular canal occlusion has become the surgical procedure of choice for intractable BPPV.
- von Brevern M, Radtke A, Lezius F, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry 2007;78:710–5.[↩]
- Benign Paroxysmal Positional Vertigo. https://rarediseases.org/rare-diseases/benign-paroxysmal-positional-vertigo/[↩]
- Shigeno K, et al. Benign paroxysmal positional vertigo and head position during sleep. J Vestib Res. 2012: Jan 1;22(4):197.[↩]
- Parnes LS, et al. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003 169(7):681-693.[↩]
- Nuti D, Nati C, Passali D. Treatment of benign paroxysmal positional vertigo: no need for postmaneuver restrictions. Otolaryngol Head Neck Surg 2000;122:440-4.[↩][↩]
- Fife TD, et al. Practice Parameter: Therapies for benign paroxysmal positional vertigo (an evidence-based review): Report on the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2008;70:2067-74.[↩][↩]
- Diagnosis and management of benign paroxysmal positional vertigo (BPPV). Lorne S. Parnes, Sumit K. Agrawal, Jason Atlas. CMAJ Sep 2003, 169 (7) 681-693; http://www.cmaj.ca/content/169/7/681.full[↩][↩][↩]
- Strupp M, Brandt T. Diagnosis and Treatment of Vertigo and Dizziness. Deutsches Ärzteblatt International. 2008;105(10):173-180. doi:10.3238/arztebl.2008.0173. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2696792/[↩][↩][↩]
- What inner ear diseases cause benign paroxysmal positional vertigo ? Karlberg M, Hall K, Quickert N, Hinson J, Halmagyi GM. Acta Otolaryngol. 2000 Mar; 120(3):380-5. https://www.ncbi.nlm.nih.gov/pubmed/10894413/[↩]
- Current view of the mechanism of benign paroxysmal positioning vertigo: cupulolithiasis or canalolithiasis ? Brandt T, Steddin S. J Vestib Res. 1993 Winter; 3(4):373-82. https://www.ncbi.nlm.nih.gov/pubmed/8275271/[↩]
- Curing the BPPV with a liberatory maneuver. Semont A, Freyss G, Vitte E. Adv Otorhinolaryngol. 1988; 42():290-3. https://www.ncbi.nlm.nih.gov/pubmed/3213745/[↩]
- Strupp M, Cnyrim C, Brandt T. Vertigo and dizziness: Treatment of benign paroxysmal positioning vertigo, vestibular neuritis and Menère’s disease. In: Candelise L, editor. Evidence-based Neurology – management of neurological disorders. Oxford: Blackwell Publishing; 2007. pp. 59–69.[↩]
- Benign paroxysmal positioning vertigo: a long-term follow-up (6-17 years) of 125 patients. Brandt T, Huppert D, Hecht J, Karch C, Strupp M. Acta Otolaryngol. 2006 Feb; 126(2):160-3. https://www.ncbi.nlm.nih.gov/pubmed/16428193/[↩]
- Kerber KA, Burke JF, Skolarus LE, et al. A prescription for the Epley maneuver: www.youtube.com?. Neurology. 2012;79(4):376-80. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3400093/[↩]
- Epley JM. The canalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg 1992;107:399-404.[↩]
- Parnes LS, Robichaud J. Further observations during the particle repositioning maneuver for benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg 1997;116: 238-43.[↩]
- Parnes LS, Price-Jones RG. Particle repositioning maneuver for benign paroxysmal positional vertigo. Ann Otol Rhinol Laryngol 1993;102:325-31.[↩]
- Semont A, Freyss G, Vitte E. Curing the BPPV with a liberatory maneuver. Adv Otorhinolaryngol 1988;42:290-3.[↩]
- Haynes DS, Resser JR, Labadie RF, Girasole CR, Kovach BT, Scheker LE, et al. Treatment of benign postional vertigo using the semont maneuver: efficacy in patients presenting without nystagmus. Laryngoscope 2002;112:796-801.[↩]
- Herdman SJ, Tusa RJ, Zee DS, Proctor LR, Mattox DE. Single treatment approaches to benign paroxysmal positional vertigo. Arch Otolaryngol Head Neck Surg 1993;119:450-4.[↩]
- Cohen HS, Jerabek J. Efficacy of treatments for posterior canal benign paroxysmal positional vertigo. Laryngoscope 1999;109:584-90.[↩]
- Foster C, A, Ponnapan A, Zaccaro K, Strong D: A Comparison of Two Home Exercises for Benign Positional Vertigo: Half Somersault versus Epley Maneuver. Audiol Neurotol Extra 2012;2:16-23. doi: 10.1159/000337947 https://www.karger.com/Article/Pdf/337947[↩]
- Epley JM. Human experience with canalith repositioning maneuvers. Ann N Y Acad Sci 2001;942:179-91.[↩]
- Lempert T, Tiel-Wilck K. A positional maneuver for treatment of horizontal-canal benign positional vertigo. Laryngoscope 1996;106:476-8.[↩]
- Hornibrook J. Benign paroxysmal positional vertigo (BPPV): history, pathophysiology, office treatment and future directions. Int J Otolaryngol. 2011;2011:835671.[↩]
- Wipperman J. Dizziness and vertigo. Prim Care. 2014;41(1):115–131.[↩]
- Dunniway HM, Welling DB. Intracranial tumors mimicking benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg 1998;118:429-36.[↩]
- Gacek RR. Further observations on posterior ampullary nerve transection for positional vertigo. Ann Otol Rhinol Laryngol 1978;87:300-5.[↩]
- Gacek RR. Singular neurectomy update. Ann Otol Rhinol Laryngol 1982;91:469-73.[↩]
- Gacek RR. Technique and results of singular neurectomy for the management of benign paroxysmal positional vertigo. Acta Otolaryngol 1995;115:154-7.[↩]
- Schessel DA, Minor LB, Nedzelski JM. Ménière’s disease and other peripheral vestibular disorders. In: Cummings, editor. Otolaryngology – head & neck surgery. Vol. 4. St. Louis: Mosby; 1998.[↩]
- Parnes LS, McClure JA. Posterior semicircular canal occlusion for intractable benign paroxysmal positional vertigo. Ann Otol Rhinol Laryngol 1990;99:330-4.[↩]
- Parnes LS, McClure JA. Effect on brainstem auditory evoked responses of posterior semicircular canal occlusion in guinea pigs. J Otolaryngol 1985; 14:145-50.[↩]
- Agrawal SK, Parnes LS. Human experience with canal plugging. Ann N Y Acad Sci 2001;942:300-5.[↩]
- Pace-Balzan A, Rutka JA. Non-ampullary plugging of the posterior semicircular canal for benign paroxysmal positional vertigo. J Laryngol Otol 1991;105:901-6.[↩]
- Dingle AF, Hawthorne MR, Kumar BU. Fenestration and occlusion of the posterior semicircular canal for benign positional vertigo. Clin Otolaryngol 1992; 17:300-2.[↩]
- Hawthorne M, el-Naggar M. Fenestration and occlusion of posterior semicircular canal for patients with intractable benign paroxysmal positional vertigo. J Laryngol Otol 1994;108:935-9.[↩]
- Anthony PF. Partitioning the labyrinth for benign paroxysmal positional vertigo: clinical and histologic findings. Am J Otol 1993;14:334-42.[↩]
- Walsh RM, Bath AP, Cullen JR, Rutka JA. Long-term results of posterior semicircular canal occlusion for intractable benign paroxysmal positional vertigo. Clin Otolaryngol 1999;24:316-23.[↩]