Contents
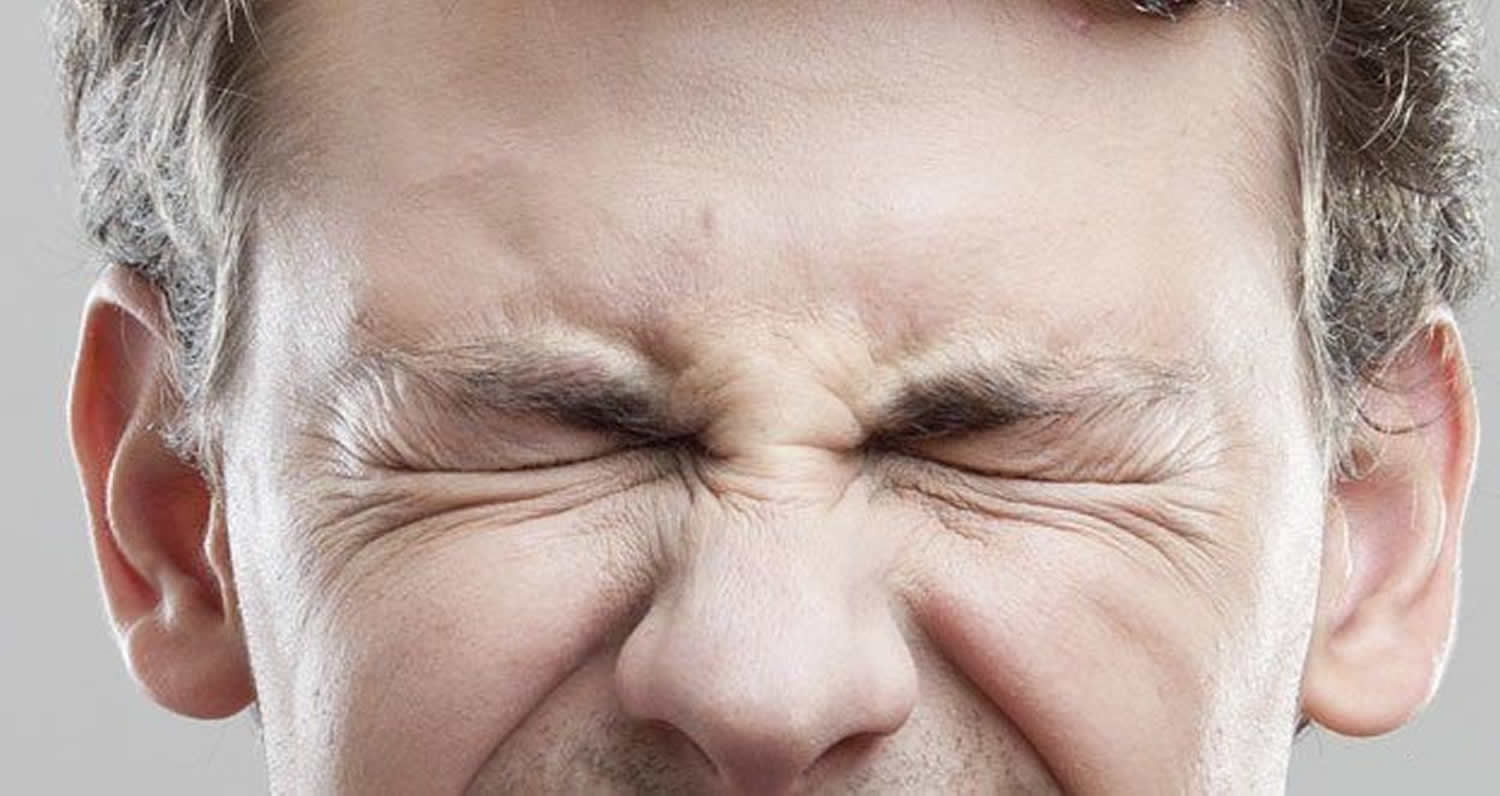
What is blepharospasm
Blepharospasm also called benign essential blepharospasm, is an abnormal, involuntary blinking or spasm of the eyelids. Blepharo means “eyelid”. Spasm means “uncontrolled muscle contraction”. “Benign” indicates the condition is not life threatening, and “essential” is a medical term meaning “of unknown cause”.
Signs and symptoms in benign essential blepharospasm are limited to the bilateral eyelids. They usually begin as mild and infrequent twitches that progress over time to forceful and frequent spasms of the eyelids, which abate during periods of sleep. In advanced cases, these episodes can cause functional blindness from periodic inability to open the eyes. This can severely limit the patient’s ability to preform activities of daily living and impart psychological stress. When blepharospasm is part of Meige’s syndrome, it is associated with facial grimacing. Reflex blepharospasm may be accompanied by photophobia and ocular signs of blepharitis and surface disease.
Benign essential blepharospasm is both a cranial and a focal dystonia. Cranial refers to the head and focal indicates confinement to one part. The word dystonia describes abnormal involuntary sustained muscle contractions and spasms. Patients with blepharospasm have normal eyes. The visual disturbance is due solely to the forced closure of the eyelids.
It is estimated that there are at least 50,000 cases of blepharospasm in the United States, with up to 2000 new cases diagnosed annually. The prevalence of blepharospasm in the general population is approximately 5 in 100,000 1. Epidemiologic reviews have revealed a family history ranging from 7 to 27.8% of cases, and an autosomal dominant, polygenic pattern of inheritance has been postulated. Factors contributing to the difficulty of studying the genetics of blepharospasm include the relatively rare occurrence of blepharospasm, geographical barriers for examination of symptomatic family members, and phenotypic heterogeneity.
The age at onset of blepharospasm symptoms ranged from 6 to 84 years, with an average of 53.4 years 2 and two thirds of patients are age 60 years or older 3. Blepharospasm has a female-to-male preponderance of Female:Male (2-4:1)
Blepharospasm should not be confused with:
- Ptosis – drooping of the eyelids caused by weakness or paralysis of a levator muscle of the upper eyelid
- Blepharitis – an inflammatory condition of the lids due to infection or allergies
- Hemifacial spasm – a non-dystonic condition involving various muscles on one side of the face, often including the eyelid, and caused by irritation of the facial nerve. The muscle contractions are more rapid and transient than those of blepharospasm, and the condition is always confined to one side
Benign essential blepharospasm is a progressive neurological disorder characterized by involuntary muscle contractions and spasms of the eyelid muscles. Benign essential blepharospasm is a form of dystonia, a movement disorder in which muscle contractions cause sustained eyelid closure, twitching or repetitive movements. Benign essential blepharospasm begins gradually with increased frequency of eye blinking often associated with eye irritation. Other symptoms may include increasing difficulty in keeping the eyes open, and light sensitivity. Generally, the spasms occur during the day, disappear in sleep, and reappear after waking. As the condition progresses, the spasms may intensify, forcing the eyelids to remain closed for long periods of time, and thereby causing substantial visual disturbance or functional blindness. It is important to note that the blindness is caused solely by the uncontrollable closing of the eyelids and not by a dysfunction of the eyes. Benign essential blepharospasm occurs in both men and women, although it is especially common in middle-aged and elderly women.
Botulinum toxin and myectomy (surgery of the eye muscles) help to control blepharospasm but may not cure it. In most cases of benign essential blepharospasm the treatment of choice is botulinum toxin injections which relax the muscles and stop the spasms. Other treatment options include medications (drug therapy) or deep brain stimulation surgery.
Botulinum toxin A is a safe, long-term treatment for patients with benign essential blepharospasm, but sustained treatment efficacy may require higher doses in later stages of the disease 4.
Botulinum toxin injections are sometimes still required following myectomy (surgery of the eye muscles) of the eyelid protractors.
With botulinum toxin treatment most individuals with benign essential blepharospasm have substantial relief of symptoms. Although some may experience side effects such as drooping eyelids, blurred or double vision, and eye dryness, these side effects are usually only temporary. The condition may worsen or expand to surrounding muscles; remain the same for many years; and, in rare cases, improve spontaneously.
Symptoms of benign essential blepharospasm can progress to render a person incapable of activities of daily living, such as reading and driving, and cause an unwanted cosmetic effect. The psychological distress is a real part of the disease and patient education, counseling, and support is as valuable as medical treatment.
Blepharospasm complications
Complications of benign essential blepharospasm may include the following:
- Ptosis following botulinum toxin injection
- Palsy after seventh denervation
- Scarring and edema after myectomy
Blepharospasm prognosis
- 90% improve symptomatically with botulinum (botox) injections, although continued injections are necessary.
- Patients with apraxia of eyelid opening often do not respond as well to injections.
Blepharospasm symptoms
Most people develop blepharospasm without any warning symptoms. Blepharospasm usually begins gradually with excessive blinking and/or eye irritation. In the early stages it may only occur with specific precipitating stressors, such as bright lights, fatigue, and emotional tension. As the condition progresses, the symptoms become more frequent during the day and facial spasms may develop. Blepharospasm may decrease or cease while a person is sleeping or concentrating on a specific task, and some people find that after a good night’s sleep, the spasms don’t appear for several hours after waking. Concentrating on a specific task may reduce the frequency of the spasms. As the condition progresses, the spasms may intensify so that when they occur, the patient is functionally blind; and the eyelids may remain forcefully closed for several hours at a time.
Blepharospasm may vary from only a slightly annoying condition to a disabling disorder that interferes with daily activities such as reading, watching television, driving and/or walking. Patients may develop anxiety, avoid social contact, become depressed, become occupationally disabled, and become suicidal 5.
The majority of patients, 62.2%, reported increased blinking as the initial symptom of blepharospasm, this was followed in frequency by involuntary eyelid closure, twitching of eyelids, and finally powerful or sustained closure of eyelids. Other symptoms were reported in 25% of cases, and included photophobia, dry eyes, and squinting. Twenty two percent of patients reported tremor, with the majority of patients reporting head tremor as location of tremor. Thirty-one percent of patients reported an eye condition prior to the onset of their blepharospasm; the majority described conjunctivitis. Eleven percent of patients reported a difficult or premature birth. Other diagnoses which preceded symptom onset included head trauma (14.1%), depression (6.5%), and anxiety (2.3%)
Blepharospasm causes
The cause of blepharospasm is probably multifactorial, but exact cause of benign essential blepharospasm is unknown. The mechanism underlying benign essential blepharospasm is not yet clearly understood. Basal ganglia dysfunction, overactivity of the seventh nerve leading to simultaneous forceful contractions of the eyelid protractors and retractors, ion channelopathy, and sensitization of the trigeminal system by photophobia are some of the proposed mechanisms.
In some patients, blepharospasm may result from genetics alone, whereas other patients might be genetically susceptible to blepharospasm and a specific risk factor may be necessary to trigger the onset of symptoms. Blepharospasm is associated with an abnormal function of the basal ganglion from an unknown cause. The basal ganglion is the part of the brain responsible for controlling the muscles. Scientists still do not know what goes wrong in the basal ganglia. It may be there is a disturbance of various “messenger” chemicals involved in transmitting information from one nerve cell to another. In most people blepharospasm develops spontaneously with no known precipitating factor. However, it has been observed that the signs and symptoms of dry eye frequently precede and/or occur concomitantly with blepharospasm. It has been suggested that dry eye may trigger the onset of blepharospasm in susceptible persons.
Variable risk factors for blepharospasm have been reported:
- Head or facial trauma.
- Family history of dystonia or tremor.
- Reflex blepharospasm is reportedly triggered by severely dry eyes and blepharitis, intraocular inflammation, meningeal irritation, light sensitivity.
- Stress may exacerbate benign essential blepharospasm.
- Medications, such as those used to treat Parkinson’s disease, have been associated with blepharospasm.
- Earlier studies suggested that cigarette smoking was a negative risk factor, but more recent studies no longer support this.
In rare cases, heredity may play a role in the development of blepharospasm with more than one family member affected. In families with autosomal dominant familial dystonia, affected members may have a generalized or segmental dystonia, while other members have various focal dystonias, such as isolated blepharospasm. A study by DeFazio et al 6 examined the first-degree relatives of 122 patients with primary blepharospasm. The study investigated genetic and environmental connections regarding the disorder and found no major difference between familial and sporadic cases with regard to coffee drinking and existing eye diseases. These findings suggest that sporadic and familial blepharospasm most likely has a commonality in etiologic background and influences of environmental factors.
Wabbels has reported a single case of congenital blepharospasm 7.
Zhou et al 8 used functional MRI (fMRI) to identify abnormal neurological pathways in 9 patients with benign essential blepharospasm compared with controls.
Blepharospasm can occur with dystonia affecting the mouth and/or jaw (oromandibular dystonia, Meige syndrome). In such cases, spasms of the eyelids are accompanied by jaw clenching or mouth opening, grimacing, and tongue protrusion. Blepharospasm can be induced by drugs, such as those used to treat Parkinson’s disease. Tardive dystonia is probably the most common cause of secondary dystonia, including blepharospasm. Tardive dystonia consists of a persistent dystonic movement involving chiefly the face, jaws, neck, trunk, and arms. Blepharospasm may be the initial presentation of tardive dystonia. In addition to dopamine-receptor blocking drugs (neuroleptics), other drugs that can cause blepharospasm are lithium, lamotrigine, and others. When it is due to antiparkinsonian drugs, reducing the dose alleviates the problem.
Other causes of blepharospasm
Associated with neurodegenerative disorders
Primarily sporadic
- Parkinson disease
- progressive supranuclear palsy
- multiple system atrophy
- multiple sclerosis
- central pontine myelinolysis
- juvenile parkinsonism-dystonia
- progressive pallidal degeneration
- intraneuronal inclusion disease
- infantile bilateral striatal necrosis
- familial basal ganglia calcifications
Primarily inherited
- dystonia-plus syndromes
- atypical autosomal dominant dystonia (not DYT1 gene)
- myoclonic dystonia
- dopa-responsive dystonia (DRD) (DYT5-GTP cyclohydrolase I 14q22.1)
- rapid-onset dystonia-parkinsonism
- early-onset parkinsonism with dystonia
- X-linked dystonia parkinsonism or Lubag
- paroxysmal dystonia-choreoathetosis
- Wilson disease
- Tourette syndrome
- Huntington disease
- Neurodegeneration with Brain Iron Accumulation (Hallervorden-Spatz disease)
- SCA3, SCA6, SCA16, SCA17, Friedreich’s ataxia
- Machado-Joseph disease
- ataxia telangiectasia
- neuroacanthocytosis
- dentato-rubral-pallidoluysian atrophy
- hereditary spastic paraplegia with dystonia
- Fragile-X syndrome
- Mohr-Tranebjaerg syndrome
Associated with metabolic disorders
Amino acid disorders
- glutaric academia
- methylmalonic academia
- homocystinuria
- Hartnup disease
- tyrosinosis
Lipid disorders
- metachromatic leukodystrophy
- ceroid lipofuscinosis
- dystonic lipidosis (“sea blue” histiocytosis) gangliosidoses
- hexosaminidase A and B deficiency
Miscellaneous metabolic disorders
- mitochondrial encephalopathies
- Leigh disease, Leber disease
- Lesch-Nyhan syndrome
- triosephosphate isomerase deficiency
- vitamin E deficiency
- biopterin deficiency
- pseudohypoparathyroidism
Due to a specific cause
Perinatal cerebral injury and kernicterus
- athetoid cerebral palsy
- delayed onset dystonia
Infection
- viral encephalitis
- encephalitis lethargica
- Reye syndrome
- subacute sclerosing panencephalitis
- Jakob-Creutzfeldt disease
- AIDS
- other: tuberculosis, syphilis, tetanus
Other disorders
- collagen vascular disorder
- paraneoplastic brainstem encephalitis
- cerebral vascular or ischemic injury (stroke)
- brain tumor
- arteriovenous malformation
- head trauma and brain surgery
- peripheral trauma
- toxins: MN, CO, CS2, methanol, disulfiram, wasp sting
- drugs: levodopa, bromocriptine, antipsychotics, metoclopramide, fenfluramine
- flecainide, ergot, anticonvulsants, certain calcium channel blockers
Due to an ophthalmologic cause
Reflex blepharospasm
- blepharitis, conjunctivitis, “dry eye syndrome,” keratitis, iritis, uveitis
- albinism, achromatopsia, maculopathies
- lesions in the nondominant temporoparietal lobe (Fisher sign)
Peripherally induced
- hemifacial spasm
- tic convulsif
- Bell palsy
- aberrant facial regeneration with facial synkinesis
- hemimasticatory spasm
- facial myokymia
- Schwartz-Jampel syndrome
- amyloidosis
- oculomasticatory myorhythmia (Whipple disease)
Benign essential blepharospasm diagnosis
Diagnosis of benign essential blepharospasm is made clinically and it is a diagnosis of exclusion, having ruled out the presence of associated conditions.
History is very important in making the diagnosis, and it also allows the clinician to distinguish between primary (essential) and secondary blepharospasm. In BEB, excessive blinking, which may start as unilateral and mild twitches, progresses to bilateral frequent and more forceful spasms. During severe episodes a patient may report the inability to pry the eyelids open. Episodes may interfere with the patient’s daily activities, such as reading and driving. The spasms disappear during sleep and may be reduced when concentrating on a specific task. In secondary etiologies, the patient may offer a history of drug use as with tardive dyskinesia, of ocular irritation from light or dry eye as in reflex blepharospasm, of associated facial grimacing as in Meige syndrome, or a history of other abnormal movements such as tics or cogwheeling of the neck and extremities in extrapyramidal disease states.
Physical examination
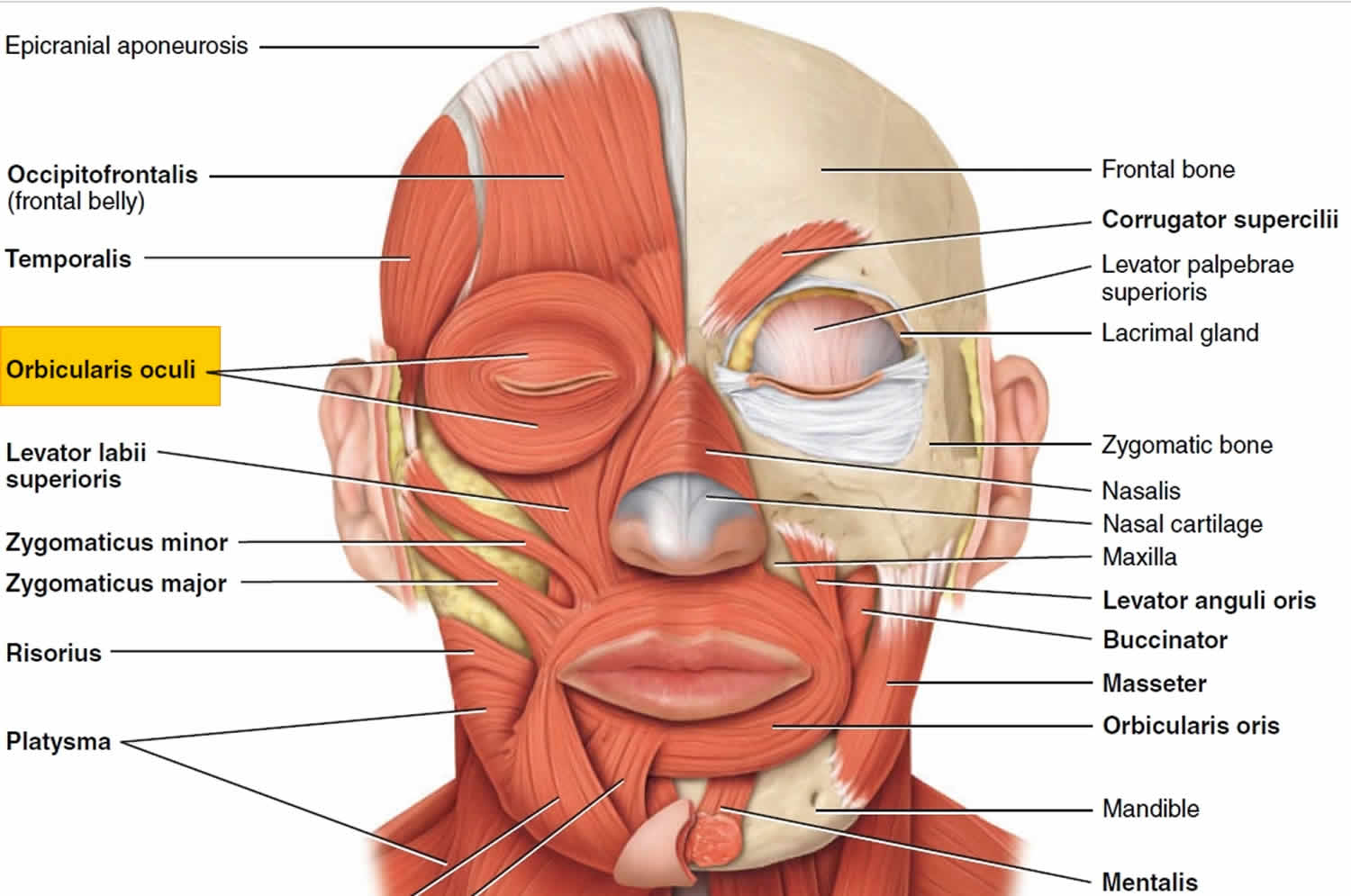
The physician may observe involuntary contraction of multiple eyelid muscles (both protractors and retractors) during a spasm episode. Careful slit lamp examination for ocular causes and inspection for other twitches in the face or extremities must be undertaken.
- No laboratory studies are required to diagnose, evaluate, or treat blepharospasm.
- No imaging study is necessary to diagnose, evaluate, or treat blepharospasm 9. Except for MRI of postcranial fossa for hemifacial spasm may need to be performed.
- No staging classification has been described for blepharospasm.
Blepharospasm treatment
To date, there is no successful cure for blepharospasm, although several treatment options can reduce its severity.
Blepharospasm is a chronic condition, which too often progressively worsens. Since the disease frequently progresses despite treatment, patients may become frustrated and resort to unconventional remedies, sometimes becoming the victims of charlatans 5.
The most effective of today’s conventional treatments include botulinum toxin injections, education, and support provided by the Benign Essential Blepharospasm Research Foundation (https://www.blepharospasm.org/), pharmacotherapy, and surgical intervention.
In the United States and Canada, the injection of Oculinum (botulinum toxin, or Botox) into the muscles of the eyelids is an approved treatment for blepharospasm. Botulinum toxin, produced by the bacterium Clostridium botulinum, paralyzes the muscles of the eyelids.
Medications taken by mouth for blepharospasm are available but usually produce unpredictable results. Any symptom relief is usually short term and tends to be helpful in only 15 percent of the cases.
Myectomy, a surgical procedure to remove some of the muscles and nerves of the eyelids, is also a possible treatment option. This surgery has improved symptoms in 75 to 85 percent of people with blepharospasm.
Alternative treatments may include biofeedback, acupuncture, hypnosis, chiropractic, and nutritional therapy. The benefits of these alternative therapies have not been proven.
Figure 1. Muscles of the eyelids
Medical therapy
First line – blepharospasm botox
- Periodic injection of a botulinum toxin A (onabotulinumtoxinA – Botox, Allergan), incobotulinumtoxinA (Xeomin, Merz Pharmaceuticals), or abobotulinumtoxinA (Dysport, Tercica) is the treatment of choice for benign essential blepharospasm
- Botulinum toxin injection is directed into or adjacent to the orbicularis oculi muscle, every 3-4 months.
- The dosage varies from 2.5 to 5 units per injection site and 4 to 8 sites per eye.
- Average onset of action is in 2-3 days and average peak effect occurs at about 7-10 days, with duration of 3-4 months, at which time need for reinjection is anticipated.
Side effects associated with botulinum toxin injection include:
- Bruising, blepharoptosis, ectropion, epiphora, diplopia, lagophthalmos, and corneal exposure.
- These are all usually transient and related to spread of the toxin to adjacent muscles.
- The central portion of the pretarsal orbicularis is avoided to minimize the chance of inducing ptosis.
Second line
- Oral medications such as muscle relaxants and sedatives are rarely effective in the treatment of benign essential blepharospasm. They may dampen symptoms of mild benign essential blepharospasm or possibly prolong intervals between injections, but their side effects must be considered alongside their benefits.
- Use of FL-41 tinted glasses (rose-colored) may also be helpful in those patients who have significant photosensitivity.
- Some studies have suggested improvement of spasms with methylphenidate (ritalin), although additional controlled studies are needed.
- Reduce stress
- Some patients note benefits with acupuncture or herbal supplements
Medical follow up
1 month after botulinum injections, and if no complications observed, then every 3-4 months for reinjection.
Blepharospasm Surgery
Surgery is reserved for patients who are poorly responsive to botulinum therapy and are disabled by their symptoms. Patients with apraxia of eyelid opening may often proceed to surgery as chemodenervation with botulinum toxin is less effective. Surgical myectomy of the orbital and palpebral orbicularis muscle in the upper (and sometimes lower) eyelids as well as surgical ablation of the facial nerve are effective in treating benign essential blepharospasm. However, the latter procedure has been mostly abandoned owing to high recurrence rates incidence of hemifacial paralysis.
Surgery in patients with apraxia of eyelid opening may require a frontalis sling rather than a levator repair to help elevated the eyelids.
- Benign Essential Blepharospasm. https://emedicine.medscape.com/article/1212176-overview[↩]
- Risk Factors for Blepharospasm. http://www.blepharospasm.org/2002stacy.pdf[↩]
- Jankovic J, Orman J. Blepharospasm: demographic and clinical survey of 250 patients. Ann Ophthalmol. 1984 Apr. 16(4):371-6.[↩]
- Ababneh OH, Cetinkaya A, Kulwin DR. Long-term efficacy and safety of botulinum toxin A injections to treat blepharospasm and hemifacial spasm. Clin Experiment Ophthalmol. 2014 Apr. 42 (3):254-61.[↩]
- Hall TA, McGwin G, Searcey K. Health-related quality of life and psychosocial characteristics of patients with benign essential blepharospasm. Arch Ophthalmol. 2006 Jan. 124(1):116-9.[↩][↩]
- Defazio G, Abbruzzese G, Aniello MS, et al. Environmental risk factors and clinical phenotype in familial and sporadic primary blepharospasm. Neurology. 2011 Aug 16. 77(7):631-7.[↩]
- Wabbels B. Botulinum toxin therapy in congenital blepharospasm. Case Rep Ophthalmol. 2014 Sep-Dec. 5 (3):435-8.[↩]
- Zhou B, Wang J, Huang Y, Yang Y, Gong Q, Zhou D. A resting state functional magnetic resonance imaging study of patients with benign essential blepharospasm. J Neuroophthalmol. 2013 Sep. 33(3):235-40[↩]
- Dresel C, Haslinger B, Castrop F. Silent event-related fMRI reveals deficient motor and enhanced somatosensory activation in orofacial dystonia. Brain. 2006 Jan. 129(Pt 1):36-46.[↩]