Contents
What are human blood types
Human blood types are based on the markers (specific carbohydrates or proteins) or antigens on the surface of red blood cells (RBCs). The 4 basic ABO blood types are O, A, B, and AB. Two major antigens or surface identifiers on human red blood cells are the A and B antigens. Another important surface antigen is called Rh (Rhesus or D antigen). People either have the D antigen on their red blood cells (Rh-positive) or do not (Rh-negative). Antibodies to the D antigen are not naturally-occurring; a person who is Rh-negative produces antibodies only after being exposed to red blood cells from another person that has the D antigen, for example, a mother exposed to her baby’s red blood cells during pregnancy or during a blood transfusion. Blood typing detects the presence or absence of these antigens to determine a person’s ABO blood group and Rh type.
After it was found that blood group A red blood cells reacted differently to a particular antibody (later called anti-A1), the blood group was divided into two phenotypes, A1 and A2. Red blood cells (RBCs) with the A1 phenotype react with anti-A1 and make up about 80% of blood type A 1. Red blood cells with the A2 phenotype do not react with anti-A1 and they make up about 20% of blood type A 1. A1 red cells express about 5 times more A antigen than A2 red cells, but both types of red cell react with anti-A, and as far as transfusion purposes are concerned, the A1 and A2 blood groups are interchangeable 1.
There are many other subgroups of blood group A in which red blood cells tend to weakly express the A antigen, whereas weak variants of the blood group B phenotype are rare 2.
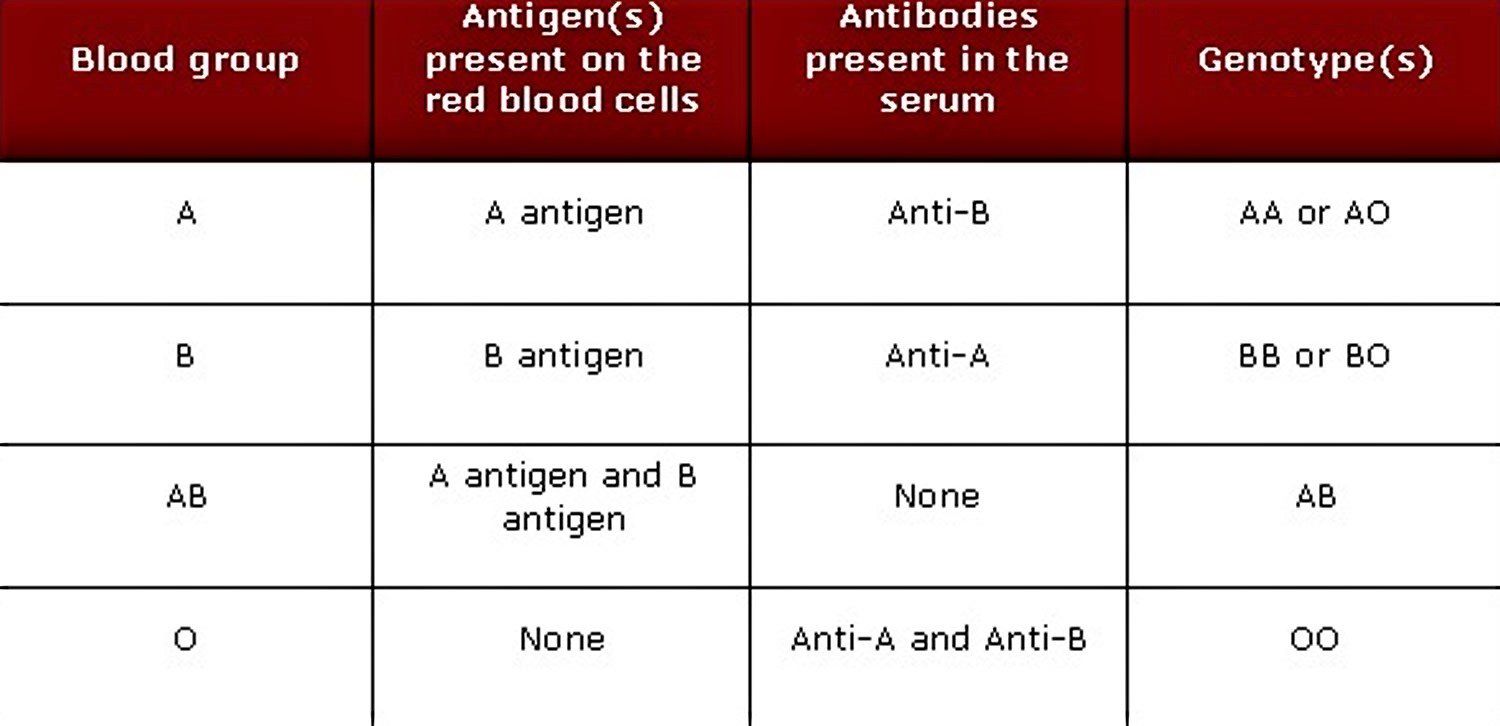
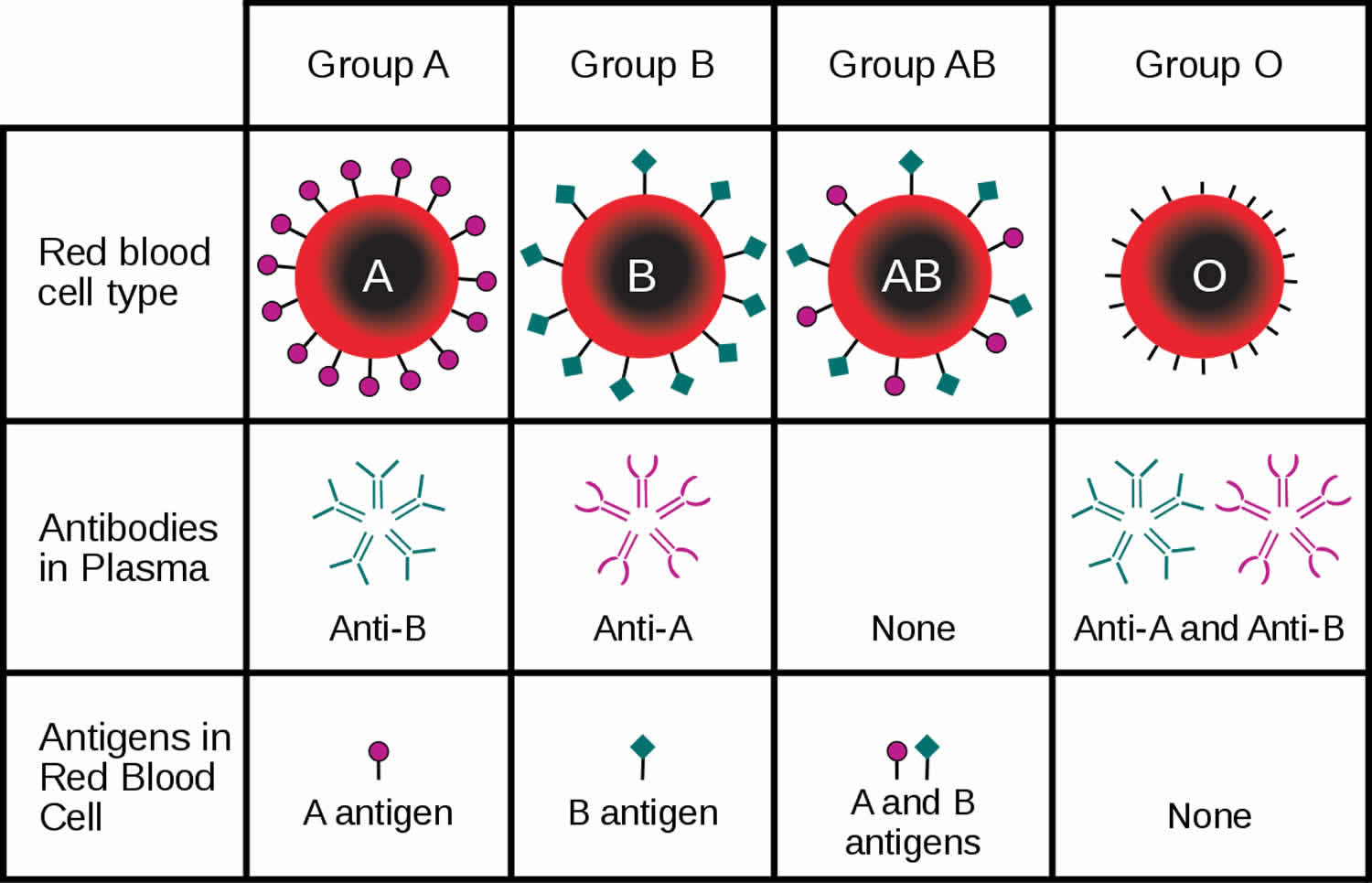
People whose red blood cells have A antigens (either A1 or A2) are in blood group A, those with B antigens are group B, those with both A and B antigens are in group AB, and those who do not have either of these markers are in blood group O, after the German word “Ohne”, which means “without” 1. The ABO blood group antigens are attached to oligosaccharide chains that project above the red blood cell surface. These chains are attached to proteins and lipids that lie in the red blood cell membrane.
If the Rh protein is present on the red blood cells, a person’s blood type is Rh+ (positive); if it is absent, the person’s blood is type Rh- (negative).
Human bodies naturally produce antibodies against the A and B antigens that they do not have on their red blood cells. For example, a person who is blood type A will have anti-B antibodies directed against the B antigens on red blood cells and someone who is type B will have anti-A antibodies directed against the A antigens. People with type AB blood (the least common blood group) have neither of these antibodies (neither anti-A nor anti-B in their serum), while those with type O blood have both (anti-B antibodies and anti-A antibodies) in their serum.
ABO antibodies in the serum are formed naturally 1. Their production is stimulated when the immune system encounters the “missing” ABO blood group antigens in foods or in micro-organisms 1. This happens at an early age because sugars that are identical to, or very similar to, the ABO blood group antigens are found throughout nature.
The ABO locus has three main alleleic forms: A, B, and O. The A allele encodes a glycosyltransferase that produces the A antigen (N-acetylgalactosamine is its immunodominant sugar), and the B allele encodes a glycosyltransferase that creates the B antigen (D-galactose is its immunodominant sugar) 1.
The O allele encodes an enzyme with no function, and therefore neither A or B antigen is produced, leaving the underlying precursor (the H antigen) unchanged. These antigens are incorporated into one of four types of oligosaccharide chain, type 2 being the most common in the antigen-carrying molecules in red blood cell membranes. Some of the other enzymes involved in the earlier stages of ABO antigen synthesis are also involved in producing antigens of the Hh blood group and the Lewis blood group.
Table 1 indicates the type of antibodies a person is expected to have based on their blood type
Table 2. Antibodies produced against ABO blood group antigens
| Antibody type | IgG and IgM Naturally occurring. Anti-A is found in the serum of people with blood groups O and B. Anti-B is found in the serum of people with blood groups O and A. |
| Antibody reactivity | Capable of hemolysis Anti-A and anti-B bind to RBCs and activate the complement cascade, which lyses the RBCs while they are still in the circulation (intravascular hemolysis). |
| Transfusion reaction | Yes — typically causes an acute hemolytic transfusion reaction Most deaths caused by blood transfusion are the result of transfusing ABO-incompatible blood. |
| Hemolytic disease of the newborn | No or mild disease Hemolytic disease of the newborn may occur if a group O mother has more than one pregnancy with a child with blood group A, B, or AB. Most cases are mild and do not require treatment. |
Table 3. Shows what types of blood patients can safely receive, based on their individual blood type
| Blood Group and Rh Type of Patient | Safe (Compatible) Blood Types for red blood cell Transfusion* |
| A positive | A positive, A negative, O positive, O negative |
| A negative | A negative, O negative |
| B positive | B positive, B negative, O positive, O negative |
| B negative | B negative, O negative |
| AB positive | AB positive, AB negative, A positive, A negative, B positive, B negative, O positive, O negative |
| AB negative | AB negative, A negative, B negative, O negative |
| O positive | O positive, O negative |
| O negative | O negative |
Footnote: *These apply for red blood cell transfusions only; when transfusing plasma products and platelets, the compatible choices are different.
These antibodies are useful for determining a person’s blood type and help determine the types of blood that he or she can safely receive (compatibility). If a person who is group A with antibodies directed against the B antigen, for example, were to be transfused with blood that is type B, his or her own antibodies would target and destroy the transfused red blood cells, causing severe, potentially fatal complications. Thus, it is critical to match a person’s blood type with the blood that is to be transfused.
Unlike antibodies to A and B antigens, antibodies to Rh are not produced naturally. That is, Rh antibodies develop only after a person who does not have Rh factor on his or her red blood cells (Rh negative) is exposed to Rh positive red blood cells. This can happen during pregnancy or birth when an Rh-negative woman is pregnant with an Rh-positive baby, or sometimes when an Rh-negative person is transfused with Rh-positive blood. In either case, the first exposure to the Rh antigen may not result in a strong response against the Rh positive cells, but subsequent exposures may cause severe reactions.
The ABO blood group antigens remain of prime importance in transfusion medicine—they are the most immunogenic of all the blood group antigens. The most common cause of death from a blood transfusion is a clerical error in which an incompatible type of ABO blood is transfused 1. The ABO blood group antigens also appear to have been important throughout human evolution because the frequencies of different ABO blood types vary among different populations, suggesting that a particular blood type conferred a selection advantage (e.g., resistance against an infectious disease.)
Blood group O is the most common phenotype in most populations.
- Note: Blood group A is divided into two main phenotypes, A1 and A2 3.
- Caucasians:
- Blood group O, 44%;
- Blood group A1, 33%;
- Blood group A2, 10%;
- Blood group B, 9%;
- Blood group A1B, 3%;
- Blood group A2B, 1%
- Blacks:
- Blood group O, 49%;
- Blood group A1, 19%;
- Blood group A2, 8%;
- Blood group B, 20%;
- Blood group A1B, 3%;
- Blood group A2B, 1%
- Asians:
- Blood group O, 43%;
- Blood group A1, 27%;
- Blood group A2, rare;
- Blood group B, 25%;
- Blood group A1B, 5%;
- Blood group A2B, rare
Frequency of ABO blood group antigens:
- Blood group A: 43% Caucasians, 27% Blacks, 28% Asians
- Blood group B: 9% Caucasians, 20% Blacks, 27% Asians
- Blood group A1: 34% Caucasians, 19% Blacks, 27% Asians
- Note: Does not include AB blood groups 3.
Table 4. Approximate distribution of blood groups and types in the U.S. population
| Blood Type | Rh POSTIVE | Rh NEGATIVE | total |
|---|---|---|---|
| O | 39% | 9% | 48% |
| A | 30% | 6% | 36% |
| B | 9% | 2% | 11% |
| AB | 4% | 1% | 5% |
| TOTAL | 82% | 18% | 100% |
However, despite their obvious clinical importance, the physiological functions of ABO blood group antigens remain a mystery. People with the common blood type O express neither the A nor B antigen, and they are perfectly healthy. Numerous associations have been made between particular ABO phenotypes and an increased susceptibility to disease. For example, the ABO phenotype has been linked with stomach ulcers (more common in group O individuals) and gastric cancer (more common in group A individuals) 1. Another observation is that individuals with blood type O tend to have lower levels of the von Willebrand Factor (vWF), which is a protein involved in blood clotting 1.
In 1910, scientists proved that the red blood cells (RBCs) antigens were inherited, and that the A and B antigens were inherited codominantly over O. There was initially some confusion over how a person’s blood type was determined, but the puzzle was solved in 1924 by Bernstein’s “three allele model”.
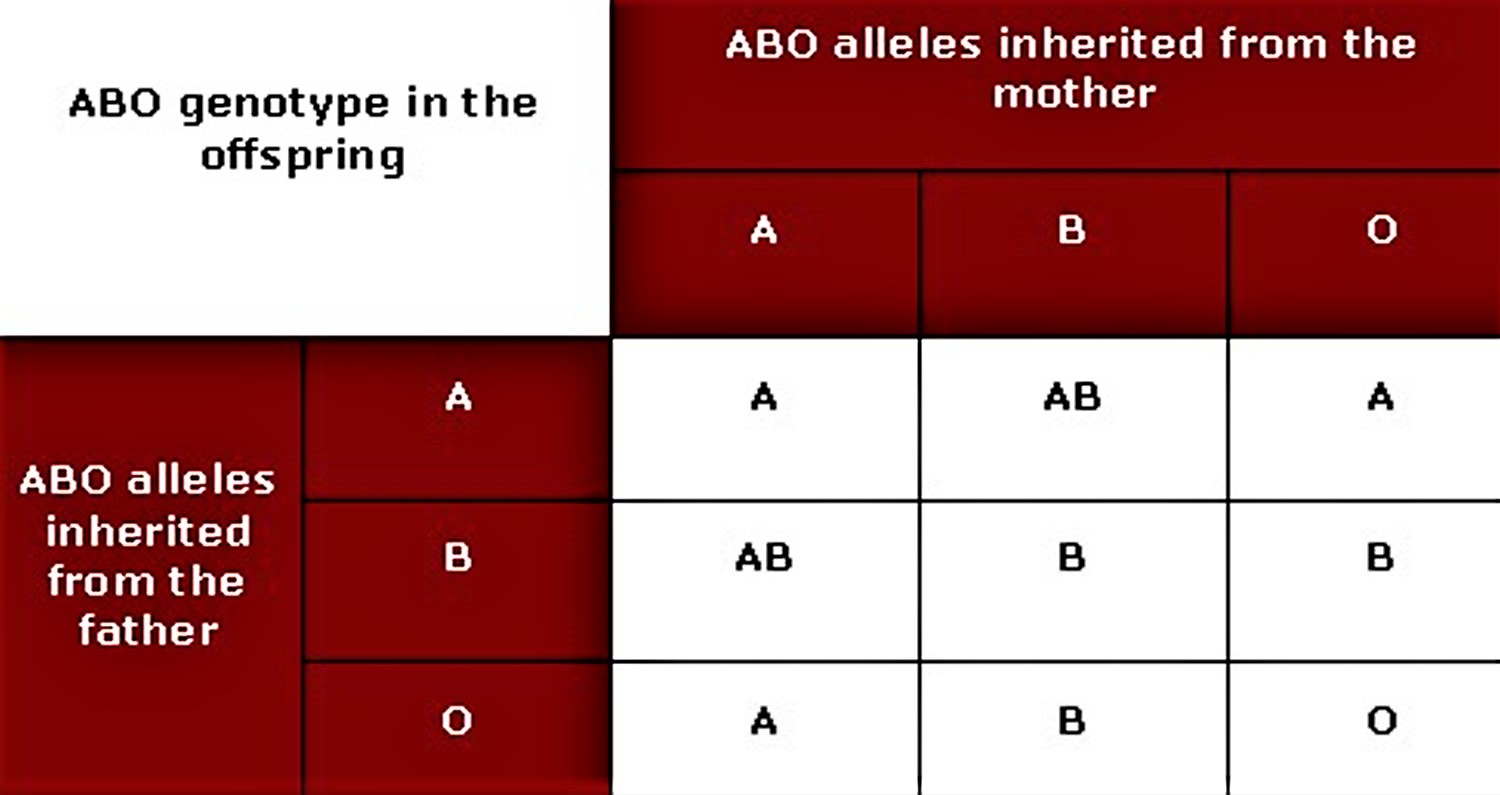
The ABO blood group antigens are encoded by one genetic locus, the ABO locus, which has three alternative (allelic) forms—A, B, and O. A child receives one of the three alleles from each parent, giving rise to six possible genotypes and four possible blood types (phenotypes).
Table 5. ABO blood group inheritance pattern
Do I need to know my blood type?
If you need a transfusion, healthcare practitioners at your healthcare facility will determine your blood type before they give you any blood. The only time you would not get a blood type test is in an extreme emergency and there is not enough time to type your blood. In this case, you would receive group O since this blood type does not have any A or B antigens that can potentially cause a hemolytic transfusion reaction. The use of Rh-negative blood depends upon the situation and the supply of O negative blood in the area.
Who are universal blood donors and recipients?
Universal blood donors have type O, Rh negative blood. This means they have no A or B antigens or Rh factor on their red blood cells to which the recipient’s antibodies can react. Recipients of their red blood cells have little risk of a hemolytic transfusion reaction due to ABO or Rh incompatibility.
Universal recipients have type AB, Rh positive blood. They recognize A, B and Rh antigens as “self” and can receive red blood cells of any ABO or Rh type with no risk of a serious hemolytic transfusion reaction due to ABO or Rh incompatibility.
Blood that is to be transfused must be compatible with the recipient’s ABO and Rh blood type because ABO and Rh antibodies present in the recipient’s blood have the potential to rapidly destroy (hemolyze) the transfused red blood cells and cause serious complications. Antibodies to the major blood types are routinely identified using blood typing tests, and blood for transfusion is matched with the ABO and Rh blood type of the recipient.
Besides ABO and Rh, are there other types of red blood cell antigens?
Yes, numerous other antigens can be present on the surface of red blood cells. These other red blood cell blood group antigens include, for example, Kell, Kidd, Duffy, and other Rh antigens. The body does not produce antibodies to these antigens unless it is exposed to these antigens through blood transfusion or during pregnancy, labor and delivery. These antibodies are not detected during routine blood typing but may be found with an red blood cell antibody screen.
Tests that classify antibodies directed against red blood cell antigens other than ABO are performed when the presence of an antibody is detected through a positive antibody screen (direct antiglobulin test (DAT) or red blood cell antibody screen). This screen may be done as part of a “type and screen,” which is ordered in situations such as:
- Part of a prenatal workup on a pregnant woman during each pregnancy to determine whether the mother has developed any red blood cell antibodies
- When a blood transfusion has been ordered
- In the investigation of a suspected transfusion reaction
- To confirm the presence and determine the cause of hemolytic disease of the newborn (HDN)
- Suspected autoimmune hemolytic anemia (in which the body inappropriately makes antibodies against antigens on its own red blood cells)
The red blood cell antibody identification test is used to name the specific antibody or antibodies that are present to determine if they are likely to be clinically significant, i.e., if they are likely to cause a transfusion reaction of hemolytic disease of the newborn (HDN). Some red blood cell antibodies are known to cause moderate to severe reactions while other less significant ones may cause a positive test but few to no symptoms or complications in the blood transfusion recipient or baby.
Examples of red blood cell antibodies and their clinical significance are shown in the table below.
| Clinically Significant | Sometimes Clinically Significant | Usually not Significant | Not Considered Significant |
| Rh (D, C, E, c, e) | MNS (U, Vw, Mur) | Lutheran (Lua, Lub) | Chido/Rodgers (Cha, Rga) |
| Kell (K, k, Ku) | Vel | Lewis (Lea, Leb) | JMH |
| Duffy (Fya, Fyb, Fy3) | Ge | MNS (M, N) | Bg |
| Kidd (Jka, Jkb, Jk3) | Hy | Csa | |
| Diego (Dia, Dib, Wra) | Yta | P1 | Xga |
| MNS (S, s) | |||
| A1 |
Complications can develop when a person with an red blood cell antibody is again exposed to red blood cells bearing the “foreign” antigen, whether by another transfusion or pregnancy. The red blood cell antibodies may attach to the specific antigens on the foreign red blood cells and target them for destruction. Depending on the antigen and antibody involved and the quantity of red blood cells affected, this can cause a reaction ranging from mild to severe and potentially life-threatening.
Antibody/antigen combinations capable of destroying red blood cells are called clinically significant. The reaction may happen immediately, such as during a blood transfusion, or take longer, from one to several days or longer following a transfusion. red blood cell destruction, called hemolysis, can occur within blood vessels or in the liver or spleen. Hemolysis can cause signs and symptoms such as fever, chills, nausea, flank pain, low blood pressure, bloody urine, and jaundice.
Should everyone have an red blood cell antibody screen performed?
It is not necessary unless someone is pregnant or may need a transfusion. Red blood cell antibodies do not otherwise affect the health of someone who has them. Sometimes a healthcare practitioner may test a woman after a pregnancy, especially if her baby had complications, to determine if there may be risks associated with a future pregnancy. Also, a healthcare practitioner may order a direct antiglobulin test (DAT) and red blood cell antibody screen if hemolysis or anemia due to autoantibodies is suspected.
Do red blood cell antibodies go away?
No. They may drop to low levels in the blood but once you have developed them, the cells that make them remain in your body and the antibody level may increase significantly again with repeated exposure to the same red blood cell antigen. You should always get blood that is negative for the corresponding antigens to clinically significant antibodies.
Do red blood cell antibodies affect blood donation?
They do not affect the safety of the person donating and will not affect the processing of red blood cells for transfusion. If someone has potent red blood cell antibodies in their plasma, however, then that plasma may not be acceptable for all transfusions.
ABO blood group antigens expression
Although the ABO blood group antigens are regarded as red blood cell antigens, they are actually expressed on a wide variety of human tissues and are present on most epithelial and endothelial cells.
Each human red blood cell expresses about 2 million ABO blood group antigens. Other blood cells, such as T cells, B cells, and platelets, have ABO blood group antigens that have been adsorbed from the plasma. In individuals who are “secretors”, a soluble form of the ABO blood group antigens is found in saliva and in all bodily fluids except for the cerebrospinal fluid.
A number of illnesses may alter a person’s ABO phenotype. Patients can “acquire” the B antigen during a necrotizing infection during which bacteria release an enzyme into the circulation that converts the A1 antigen into a B-like antigen 4. During this time, patients should not receive blood products that contain the B antigen because their sera will still contain anti-B. Once the underlying infection is treated, the patients’ blood groups return to normal.
Illness can also cause patients to “lose” ABO blood group antigens. Any disease that increases the body’s demand for red blood cells may weaken the expression of ABO blood group antigens, e.g., thalassemia. In addition, ABO blood group antigens can be altered by hematological cancers that can modify the sugar chains that bear the ABO blood group antigens, lending to the use of the A and B antigens as tumor markers for acute leukemia, myeloproliferative disorders, and myelodysplasia.
Function of the A and B antigens
The functions of the ABO blood group antigens are not known. Individuals who lack the A and B antigens are healthy, suggesting that any function the antigens have is not important, at least not in modern times.
Diseases associated with ABO blood group antigens
No diseases are known to result from the lack of expression of ABO blood group antigens, but the susceptibility to a number of diseases has been linked with a person’s ABO phenotype. Such correlations remain controversial and include the observation that gastric cancer appears to be more common in group A individuals (4), whereas gastric and duodenal ulcers occur more often in group O individuals 5.
A clear correlation has been established between the ABO phenotype and the level of two proteins involved in blood clotting; factor VIII and von Willebrand factor (vWF) 6. Blood group O individuals have about 25% less factor VIII and von Willebrand factor in their plasma. It is well established that low levels of factor VIII and von Willebrand factor are a cause of excess bleeding, and therefore it may also be the case that increased levels make clotting more likely, increasing the risk of both arterial (ischemic heart disease) and venous (thromboembolic disease) problems. Indeed, non-group O individuals have been shown to be at an increased risk of both arterial and venous disease 6.
Clinical significance of ABO antibodies
ABO antibodies are of major clinical significance for two reasons: they are naturally occurring and are found universally, and, they are highly reactive.
Transfusion reactions
The routine practice of blood typing and cross matching blood products should prevent adverse transfusion reactions caused by ABO antibodies. However, clerical error can result in “the wrong blood” being transfused into a patient, an error which can result in the death of the patient 7.
If a recipient who has blood group O is transfused with non-group O red blood cells, the naturally occurring anti-A and anti-B in the recipient’s serum binds to their corresponding antigens on the transfused red blood cells. These antibodies fix complement and cause rapid intravascular hemolysis, triggering an acute hemolytic transfusion reaction that can cause disseminated intravascular coagulation (DIC), shock, acute renal failure, and death.
Anti-A1 is a less significant cause of transfusion reactions and does not appear to fix complement.
Besides A and B, many other antigens exist. Having a rare blood type is especially problematic if you need repeated transfusions, as sickle cell anemia and thalassemia patients do. If blood transfusions are not closely matched to blood types of patients, they may suffer transfusion reactions. Such reactions are less likely if donors and recipients are from the same racial or ethnic groups. Molecular testing techniques that analyze a person’s genes may be used to predict the presence of unusual or uncommon red cell antigens.
Hemolytic disease of the newborn
Although Rh incompatibility has more severe consequences, one of the most common causes of hemolytic disease of the newborn is actually an incompatibility between the mother’s and baby’s ABO blood groups, not the Rh factor. However, ABO grouping cannot be used to predict whether hemolytic disease of the newborn will occur because antibodies to the ABO blood groups are naturally occurring.
Most cases of hemolytic disease of the newborn that arise from an ABO incompatibility require no treatment. Cases of severe hemolysis that require exchange transfusions are less common, and fetal hydrops is rare 8.
Hemolytic disease of the newborn caused by ABO antibodies occurs almost exclusively in infants of blood group A or B who are born to group O mothers 9. This is because the anti-A and anti-B formed in group O individuals tend to be of the IgG type (and therefore can cross the placenta), whereas the anti-A and anti-B found in the serum of group B and A individuals, respectively, tends to be of the IgM type. Although uncommon, cases of hemolytic disease of the newborn have been reported in infants born to mothers with blood group A2 10 and blood group B 11.
Hemolytic disease of the newborn tends to be relatively mild in nature mainly because fetal red blood cells don’t express adult levels of A and B antigens. However, the strength of fetal ABO blood group antigens can vary, and therefore the degree of hemolysis and hence the severity of hemolytic disease of the newborn can be unpredictable 12. Early studies suggested that the race of a neonate was a risk factor for developing ABO hemolytic disease of the newborn 13. However, later studies showed that the prevalence of disease that required treatment did not differ significantly among Asian, Black, Hispanic, and Caucasian infants 14.
- Dean L. Blood Groups and Red Cell Antigens [Internet]. Bethesda (MD): National Center for Biotechnology Information (US); 2005. Chapter 5, The ABO blood group. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2267[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Daniels G. Human Blood Groups, Second ed. 2002, Blackwell Science.[↩]
- Reid ME and Lomas-Francis C. The Blood Group Antigen Facts Book. Second ed. 2004, New York: Elsevier Academic Press.[↩][↩]
- Stayboldt C , Rearden A , Lane TA . B antigen acquired by normal A1 red cells exposed to a patient’s serum. Transfusion. 1987;27:41–4.[↩]
- O’Donnell J , Laffan M A . The relationship between ABO histo-blood group, factor VIII and von Willebrand factor. Transfus Med. 2001;11(4):343–51.[↩]
- Fuchs CS , Mayer RJ . Gastric carcinoma. N Engl J Med. 1995;333:32–41.[↩][↩]
- Williamson LM , Lowe S , Love EM , Cohen H , Soldan K , McClelland DB , Skacel P , Barbara JA . Serious hazards of transfusion (SHOT) initiative: analysis of the first two annual reports. BMJ. 1999;319:16–9.[↩]
- Gilja BK , Shah VP . Hydrops fetalis due to ABO incompatibility. Clin Pediatr (Phila). 1988;27:210–2.[↩]
- Ozolek JA , Watchko JF , Mimouni F . Prevalence and lack of clinical significance of blood group incompatibility in mothers with blood type A or B. J Pediatr. 1994;125:87–91.[↩]
- Jeon H , Calhoun B , Pothiawala M , Herschel M , Baron BW . Significant ABO hemolytic disease of the newborn in a group B infant with a group A2 mother. Immunohematol. 2000;16:105–8.[↩]
- Haque KM , Rahman M . An unusual case of ABO-haemolytic disease of the newborn. Bangladesh Med Res Counc Bull. 2000;26:61–4.[↩]
- Grundbacher FJ . The etiology of ABO hemolytic disease of the newborn. Transfusion. 1980;20:563–8.[↩]
- Bucher KA , Patterson AM, Jr , Elston RC , Jones CA , Kirkman HN, Jr . Racial difference in incidence of ABO hemolytic disease. Am J Public Health. 1976;66:854–8.[↩]
- Toy PT , Reid ME , Papenfus L , Yeap HH , Black D . Prevalence of ABO maternal-infant incompatibility in Asians, Blacks, Hispanics and Caucasians. Vox Sang. 1988;54:181–3.[↩]