Contents
What is a brain abscess
A brain abscess is a collection of pus, immune cells, and other material in the brain. A brain abscess usually occurs when bacteria or fungi enter the brain tissue after an infection or severe head injury. A brain abscess is regarded as a medical emergency. Swelling caused by the abscess can disrupt the blood and oxygen supply to the brain. There’s also a risk of the abscess bursting (rupturing). If left untreated, a brain abscess can cause permanent brain damage and could be fatal.
If untreated, a brain abscess is almost always deadly. With treatment, the death rate is about 10% to 30%. The earlier treatment is received, the better.
There are three main ways a brain abscess can develop. These are:
- an infection in another part of the skull – such as an ear infection, sinusitis or dental abscess, which can spread directly into the brain
- an infection in another part of the body – for example, the infection that causes pneumonia spreading into the brain via the blood
- trauma, such as a severe head injury – that cracks open the skull, allowing bacteria or fungi to enter the brain
However, in some cases, the source of the infection remains unknown.
According to studies, the incidence of brain abscess is approximately 8% of intracranial masses in developing countries and 1% to 2% in the Western countries with approximately four cases occurring per million 1. The prevalence of brain abscess in patients with AIDS is higher. Therefore, the prevalence rate has increased with the emanation of AIDS pandemic. Approximately 1500 to 2500 cases are diagnosed annually in the United States. The incidence of fungal brain abscess also has increased because of a higher usage of broad-spectrum antibiotics and immunosuppressive agents like steroids. Prevalence is highest in adult men younger than 30 years while pediatric disease occurs most frequently in children ages 4 to 7 years. Neonates are third in high-risk groups. Vaccination has reduced the prevalence in young children. Data suggests that brain abscesses are more predominant in males than in females with a male-to-female ratio varying between 2:1 and 3:1. Geographical and seasonal differences have no significant impact. In developing countries with poor living standards, brain abscess accounts for a disproportionate percentage of space-occupying intracranial lesions compared to developed nations 2.
Although the risk of developing a brain abscess is extremely low, it is a life-threatening condition and should be diagnosed and treated as soon as possible.
A brain abscess is usually treated using a combination of:
- medication – either antibiotics or antifungals
- surgery – either draining the pus through a hole in the skull (simple aspiration) or opening the skull and removing the abscess entirely (craniotomy). Some people may have long-term nervous system problems after surgery.
Treatment with antibiotics often begins before a diagnosis is confirmed, to reduce the risk of complications.
Brain abscess causes
Brain abscess commonly occurs when bacteria or fungi infect part of your brain. If the immune system is unable to kill an infection, it will try to limit its spread by using healthy tissue to form an abscess, to stop the pus infecting other tissue. As a result, swelling and irritation (inflammation) develop. Infected brain cells, white blood cells, live and dead bacteria, or fungi collect in an area of the brain. Tissue forms around this area and creates a mass, or abscess.
The germs that cause a brain abscess can reach the brain through the blood. Or, they enter the brain directly, such as during brain surgery. In rare cases, a brain abscess develops from an infection in the sinuses.
The source of the infection is often not found. However, the most common source is a lung infection. Less often, a heart infection is the cause.
Infections of the brain are rare because the body has evolved a number of defences to protect this vital organ. One of these is the blood-brain barrier, a thick membrane that filters out impurities from blood before allowing it into your brain.
However, in some cases, germs can get through these defences and infect the brain.
The following raise your chance of developing a brain abscess:
- A weakened immune system (such as in people with HIV/AIDS)
- Chronic disease, such as cancer
- Drugs that suppress the immune system (corticosteroids or chemotherapy)
- Congenital heart disease
Although the exact location of the original infection can’t always be identified, the most common sources are described below.
Infection in the skull
In up to half of cases, the brain abscess occurs as a complication of a nearby infection in the skull, such as:
- a persistent middle ear infection (otitis media)
- sinusitis – an infection of the sinuses, the air-filled cavities inside the cheekbones and forehead
- mastoiditis – infection of the bone behind the ear
This used to be a major cause of brain abscesses, but because of improved treatments for infections, a brain abscess is now a rare complication of these kinds of infection.
Infection through the bloodstream
Infections spread through the blood are thought to account for around one in four cases of brain abscesses.
People with a weakened immune system have a higher risk of developing a brain abscess from a blood-borne infection. This is because their immune system may not be capable of fighting off the initial infection.
You may have a weakened immune system if you:
- have a medical condition that weakens your immune system – such as HIV or AIDS
- receive medical treatment known to weaken the immune system – such as chemotherapy
- have an organ transplant and take immunosuppressant drugs to prevent your body rejecting the new organ
The most commonly reported infections and health conditions that may cause a brain abscess are:
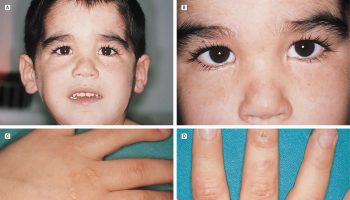
- cyanotic heart disease – a type of congenital heart disease (a heart defect present at birth) where the heart is unable to carry enough oxygen around the body; this lack of a regular oxygen supply makes the body more vulnerable to infection
- pulmonary arteriovenous fistula – a rare condition in which abnormal connections develop between blood vessels inside the lungs; this can allow bacteria to get into the blood and, eventually, the brain
- a dental abscess or treatment for tooth decay
- lung infections – such as pneumonia or bronchiectasis
- infections of the heart – such as endocarditis
- skin infections
- infections of the abdomen – such as peritonitis (an infection of the bowel lining)
- pelvic infections – such as infection of the bladder lining (cystitis)
Infection after a head injury
Direct trauma to the skull can also lead to a brain abscess and is thought to be responsible for 1 in 10 cases.
The most commonly reported causes include:
- a skull fracture caused by penetrating injury to the head
- a gunshot or shrapnel wound
In rare cases, a brain abscess can develop as a complication of neurosurgery.
Brain abscess signs and symptoms
In about two-thirds of cases, symptoms are present for 2 weeks or less. The diagnosis is made at a mean of 8 days after the onset of symptoms. The course ranges from indolent to fulminant. Most manifestations of brain abscess tend to be nonspecific, resulting in a delay in establishing the diagnosis. Most symptoms are a direct result of the size and location of the space-occupying lesion or lesions. The triad of fever, headache, and the focal neurologic deficit is observed in less than half of patients.
Symptoms of a brain abscess may develop slowly, over a period of several weeks, or they may develop suddenly. They may include:
- Headache – which is often severe, located in a single section of the head and can’t be relieved with painkillers. A headache (69% to 70%) the most common medical symptom.
- Changes in mental status (65% of cases), such as confusion, irritability, slow response or thinking, unable to focus, or sleepiness. Lethargy progressing to coma is indicative of severe cerebral edema and a poor prognostic sign.
- Problems with nerve function – such as muscle weakness, slurred speech or paralysis on one side of the body. Focal neurologic deficits (50% to 65%) occur days to weeks after the onset of a headache.
- Decreased ability to feel sensation.
- Third and sixth cranial nerve deficits.
- Pain is usually localized to the side of the abscess, and its onset can be gradual or sudden in nature. The pain is most severe in intensity and not relieved by over-the-counter pain medications.
- Fever of 100.4 °F (38 °C) or above and chills in 45% to 53% of cases.
- Seizures (fits) in 25% to 35% of cases. Grand mal seizures are particularly common in frontal abscesses.
- Stiff neck (15% of cases) are most commonly associated with occipital lobe abscess or an abscess that has leaked into a lateral ventricle.
- Language problems
- Vision changes – such as blurring, greying of vision or double vision (due to the abscess putting pressure on the optic nerve)
- Nausea and vomiting (40% of cases) are mostly seen with raised intracranial pressure
- Weakness
Rupture of abscess usually presented with suddenly worsening headache and followed by emerging signs of meningismus.
Any symptoms that suggest a problem with the brain and nervous system should be treated as a medical emergency. These include:
- slurred speech
- muscle weakness or paralysis
- seizures occurring in a person with no previous history of seizures
If you or someone you know experiences any of these symptoms, phone your local emergency services number immediately and ask for an ambulance.
Any symptoms that suggest a worsening infection, such as fever and vomiting, should be reported to your doctor immediately.
Brain abscess complications
Complications of a brain abscess can include:
- a reoccurring abscess – seek immediate medical advice if you think there’s even a small chance your abscess has reoccurred; this is more common in people with a weakened immune system or cyanotic heart disease
- brain damage – mild to moderate brain damage often improves with time but severe brain damage is likely to be permanent; brain damage is more of a risk if diagnosis and treatment are delayed
- epilepsy – where a person has repeated seizures (fits)
- meningitis – a life-threatening infection of the protective membranes around the brain, which requires urgent treatment; this is more common in children
Brain abscess diagnosis
If a brain abscess is suspected, an initial assessment will be made based on your symptoms, medical history and whether you’ve had a recent infection or a weakened immune system.
Blood tests can also be carried out to check for an infection.
If you’re referred to hospital for further tests, you may have either:
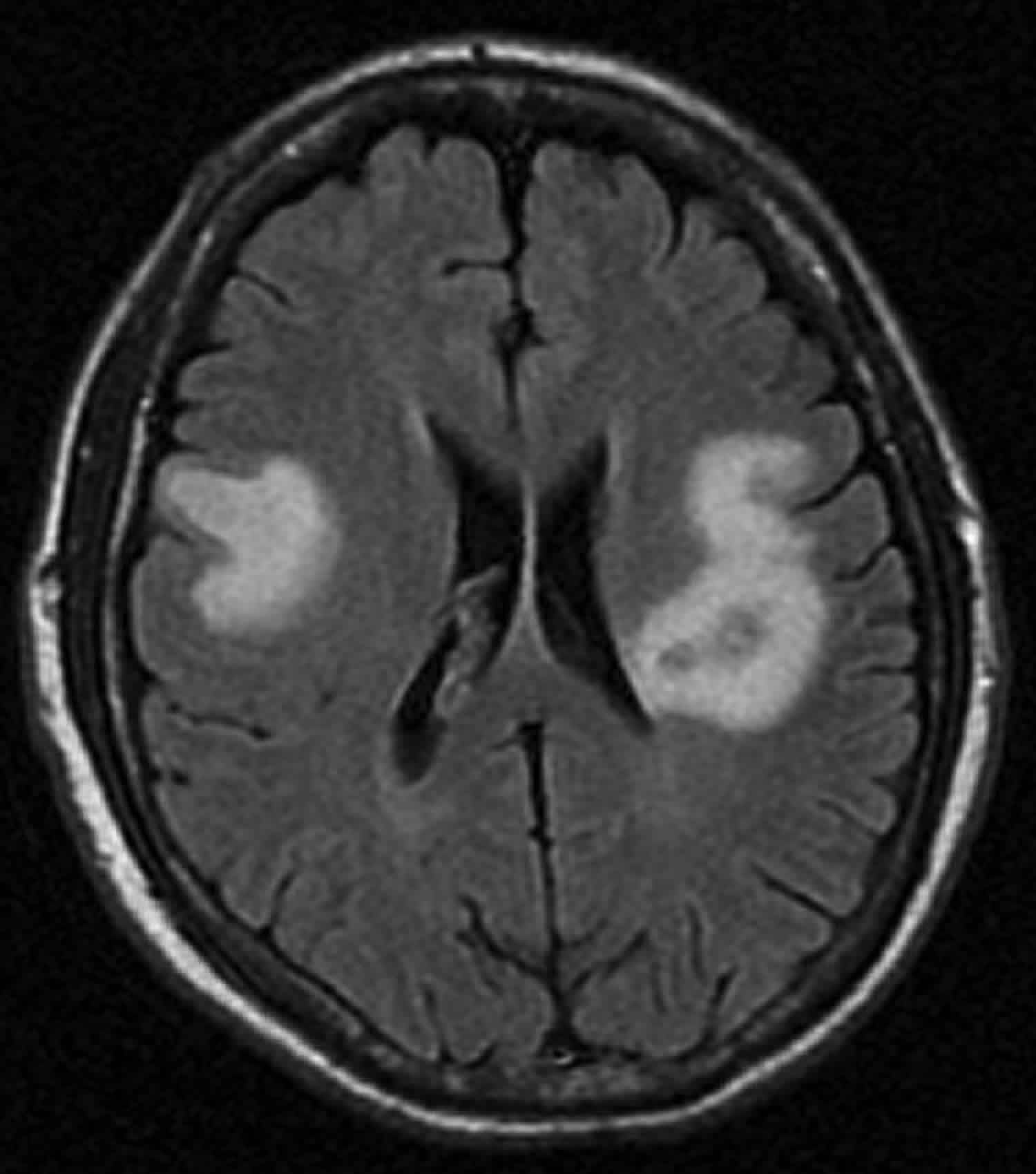
- a computerized tomography (CT) scan – a series of X-rays are used to produce a detailed image of the inside of your body
- a magnetic resonance imaging (MRI) scan – which uses strong magnetic fields and radio waves to produce a detailed image of the inside of your body.
If an abscess is found, a procedure known as CT-guided aspiration may be used to remove a sample of pus for testing. This involves using a CT scan to guide a needle to the site of the abscess.
Brain abscess treatment
A brain abscess is a medical emergency. Pressure inside the skull may become high enough to be life threatening. You will need to stay in the hospital until the condition is stable. Some people may need life support.
Treatment for a brain abscess usually involves a combination of medication and surgery, depending on the size and number of brain abscesses.
Medication
In some cases, it may be possible to treat an abscess with medication alone, or surgery may be too risky.
Medicine, not surgery, is recommended if you have:
- A small abscess (less than 2 cm)
- An abscess deep inside the brain
- An abscess and meningitis
- Several abscesses (rare)
- Hydrocephalus (a build-up of fluid on the brain)
- Shunts in the brain for hydrocephalus (in some cases, the shunt may need to be removed temporarily or replaced)
- An infection called toxoplasmosis in a person with HIV/AIDS
- Meningitis (an infection of the protective membranes that surround the brain) as well as an abscess
Treatment with medication often begins before a diagnosis is confirmed to reduce the risk of complications. And you may be prescribed several different types of antibiotics to make sure treatment works.
You’ll normally be given antibiotics or antifungal (if the infection is likely caused by a fungus) medication through a drip, directly into a vein. Doctors will aim to treat the abscess and the original infection that caused it.
Specific antibiotic regimens according to microorganisms:
- Gram-positive bacteria including streptococci: third-generation cephalosporin (e.g., cefotaxime, ceftriaxone) or penicillin G are effective
- Staph aureus, staph epidermis is usually seen in association with penetrating brain trauma and or neurosurgical procedure. Should be covered with vancomycin. It is also effective for Clostridium species. In cases of vancomycin resistance, linezolid, trimethoprim-sulfamethoxazole or daptomycin can be considered.
- Fungal infections including Candida, Cryptococcus needs to be treated with Amphotericin B
- Aspergillus and Pseudallescheria boydii. Voriconazole can be considered
- Toxoplasma gondii infection is treated with pyrimethamine and sulfadiazine, can be combined with HAART in cases of HIV.
Steroids can be considered in select cases, especially to reduce the mass effect and improve antibiotic penetration and cerebral edema 3.
Surgery
If the abscess is larger than 2cm, it’s usually necessary to drain the pus out of the abscess. However, you’ll still need a course of antibiotics after surgery.
Surgery is needed if :
- Increased pressure in the brain continues or gets worse
- The brain abscess does not get smaller after medicine
- The brain abscess contains gas (produced by some types of bacteria)
- The brain abscess might break open (rupture)
- The brain abscess is large (more than 2 cm)
There are two surgical techniques for treating a brain abscess:
- simple aspiration
- craniotomy (opening the skull)
Surgery consists of opening the skull, exposing the brain, and draining the abscess. Laboratory tests are often done to examine the fluid. This helps identify the cause of the infection, so that the right antibiotics or antifungal medicine can be prescribed.
Needle aspiration guided by CT or MRI scan to locate the abscess, then drilling a small hole known as a “burr hole” into the skull, may be needed for a deep abscess. During this procedure, medicines may be injected directly into the mass. The pus is drained and the hole is sealed.
A simple aspiration takes around one hour to complete.
Certain diuretics (water pills) and steroids may also be used to reduce the swelling of the brain.
Craniotomy
Open aspiration and excisions are usually carried out using a surgical procedure known as a craniotomy.
A craniotomy may be recommended if an abscess doesn’t respond to aspiration or reoccurs at a later date.
During a craniotomy, the surgeon shaves a small section of your hair and removes a small piece of your skull bone (a bone flap) to gain access to your brain.
The abscess is then drained of pus or totally removed. CT-guidance may be used during the operation, to allow the surgeon to more accurately locate the exact position of the abscess.
Once the abscess has been treated, the bone is replaced. The operation usually takes around three hours, which includes recovery from general anaesthetic, where you’re put to sleep.
Complications of a craniotomy
As with all surgery, a craniotomy carries risks, but serious complications are uncommon.
Possible complications of a craniotomy may include:
- swelling and bruising around your face – which is common after a craniotomy and should lessen after the operation
- headaches – these are common after a craniotomy and may last several months, but should eventually settle down
- a blood clot in the brain – further surgery may be required to remove it
- stiff jaw – the surgeon may need to make a small cut to a muscle that helps with chewing, which will heal but can become stiff for a few months; exercising the muscle by regularly chewing sugar-free gum should help relieve the stiffness
- movement of the bone flap – the bone flap in your skull may feel like it moves and you may experience a clicking sensation; this can feel strange, but it’s not dangerous and will stop as the skull heals
The site of the cut (incision) in your skull can become infected, although this is uncommon. You’re usually given antibiotics around the time of your operation to prevent infection.
Brain abscess recovery time
Once your brain abscess has been treated, you’ll probably stay in hospital for several weeks so your body can be supported while you recover.
You’ll also receive a number of CT scans, to make sure the brain abscess has been completely removed.
Most people need a further six to 12 weeks rest at home before they’re fit enough to return to work or full-time education.
After treatment for a brain abscess, avoid any contact sport where there’s a risk of injury to the skull, such as boxing, rugby or football.
Brain abscess survival rate
The advent of antimicrobials and imaging studies as CT scanning and MRI, the mortality rate has reduced from 5% to 10% 1. Rupture of a brain abscess, however, is more fatal. The long-term neurological complications after the infection are dependent on the early diagnosis and administration of antibiotics.
- Bokhari MR, Mesfin FB. Brain Abscess. [Updated 2018 Nov 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441841[↩][↩]
- Gorji GRS, Rassouli M, Staji H. Prevalence of cerebral toxoplasmosis among slaughtered sheep in Semnan, Iran. Ann Parasitol. 2018;64(1):37-42[↩]
- Simjian T, Muskens IS, Lamba N, Yunusa I, Wong K, Veronneau R, Kronenburg A, Brouwers HB, Smith TR, Mekary RA, Broekman MLD. Dexamethasone Administration and Mortality in Patients with Brain Abscess: A Systematic Review and Meta-Analysis. World Neurosurg. 2018 Jul;115:257-263[↩]