Contents
What is brain stem
The brain stem is the lowermost part of the brain that connects to the spinal cord. The brainstem is the part of the brain between the spinal cord and the
diencephalon. The brain stem contains bundles of very long nerve fibers that carry signals controlling muscles and sensation or feeling between the cerebrum and the rest the body. Special centers in the brain stem also help control breathing and the beating of the heart. Also, most cranial nerves (see Figures 2 and 3) start in the brain stem.
The brain stem consists of three structures:
- Medulla oblongata,
- Pons, and
- Midbrain.
Each region is roughly an inch long, and together they make up only 2.5% of total brain mass. The brain stem lies in the posterior cranial fossa of the skull, on the basilar part of the occipital bone. In a living person, the brain stem is oriented like a vertical stalk with the cerebrum perched on top like a mushroom cap. Postmortem changes give it a more oblique angle in the cadaver and consequently, in many medical illustrations. Towards the back end, the brain stem ends at the foramen magnum of the skull, and the central nervous system (CNS) continues below this as the spinal cord.
The brain stem has the same structural plan as the spinal cord, with outer white matter surrounding an inner region of gray matter. However, brain nuclei of gray
matter are also located in the white matter of the brain stem.
Extending through the brainstem is the reticular formation, a netlike region of interspersed gray and white matter.
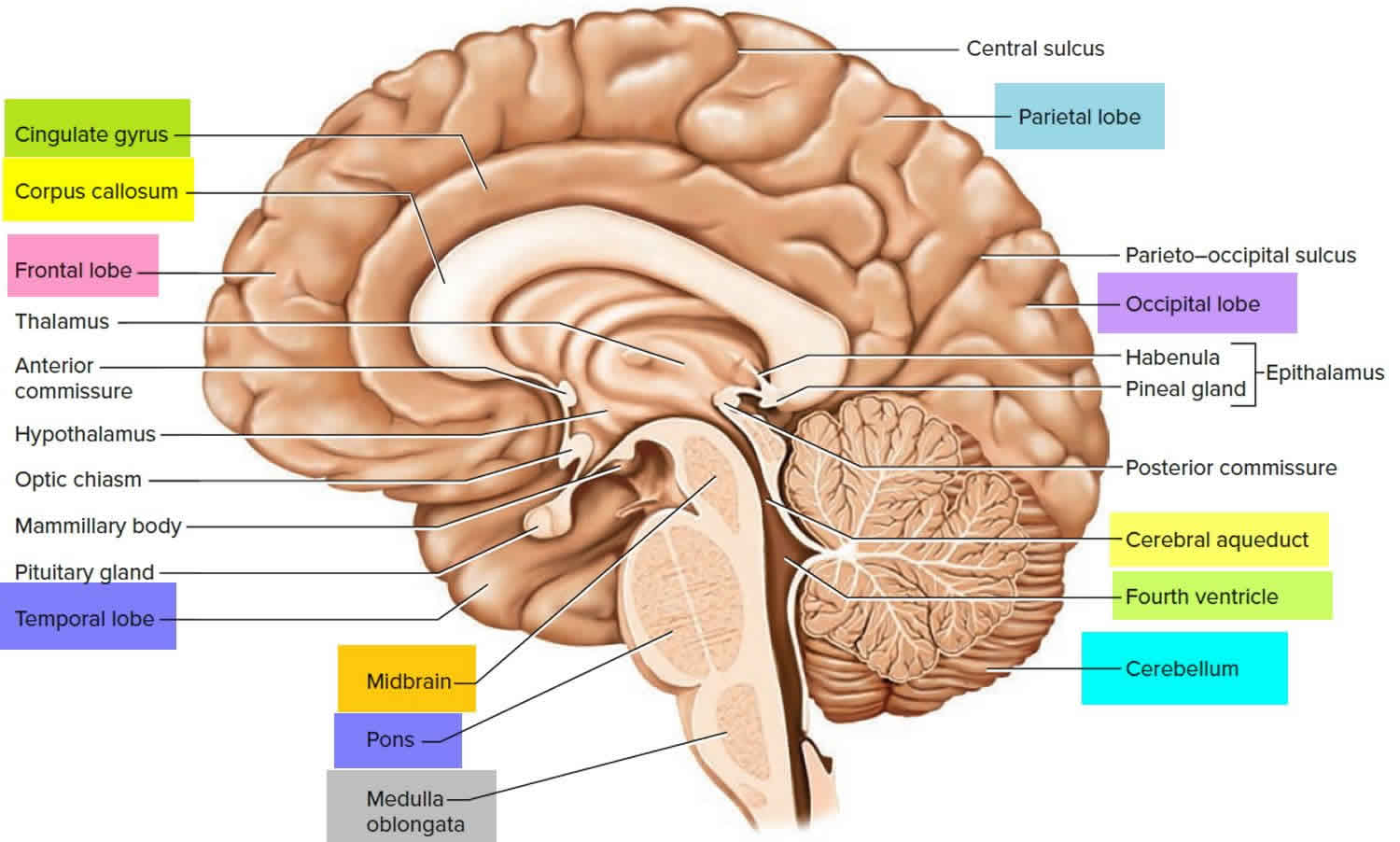
Figure 1. Human brain
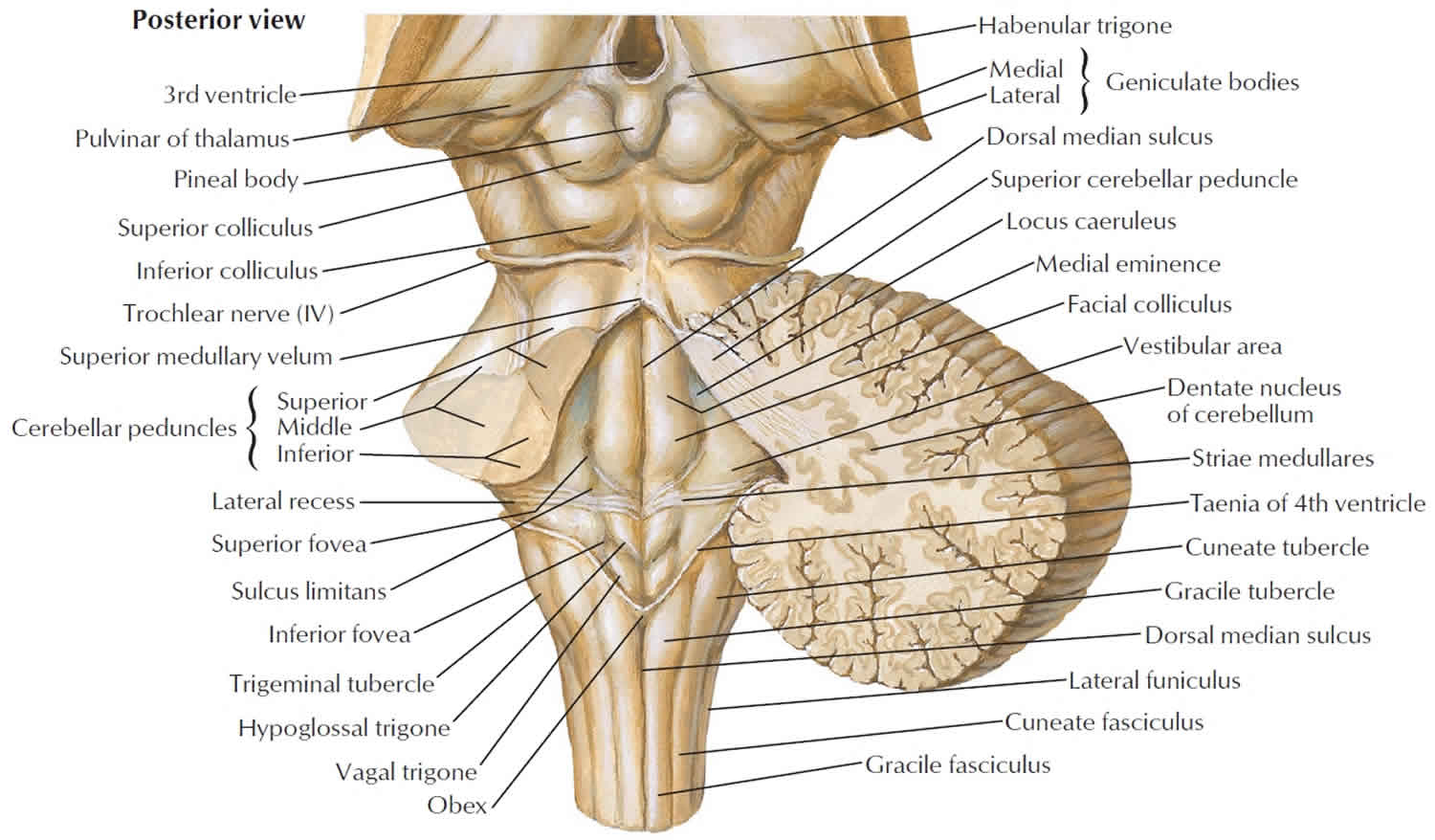
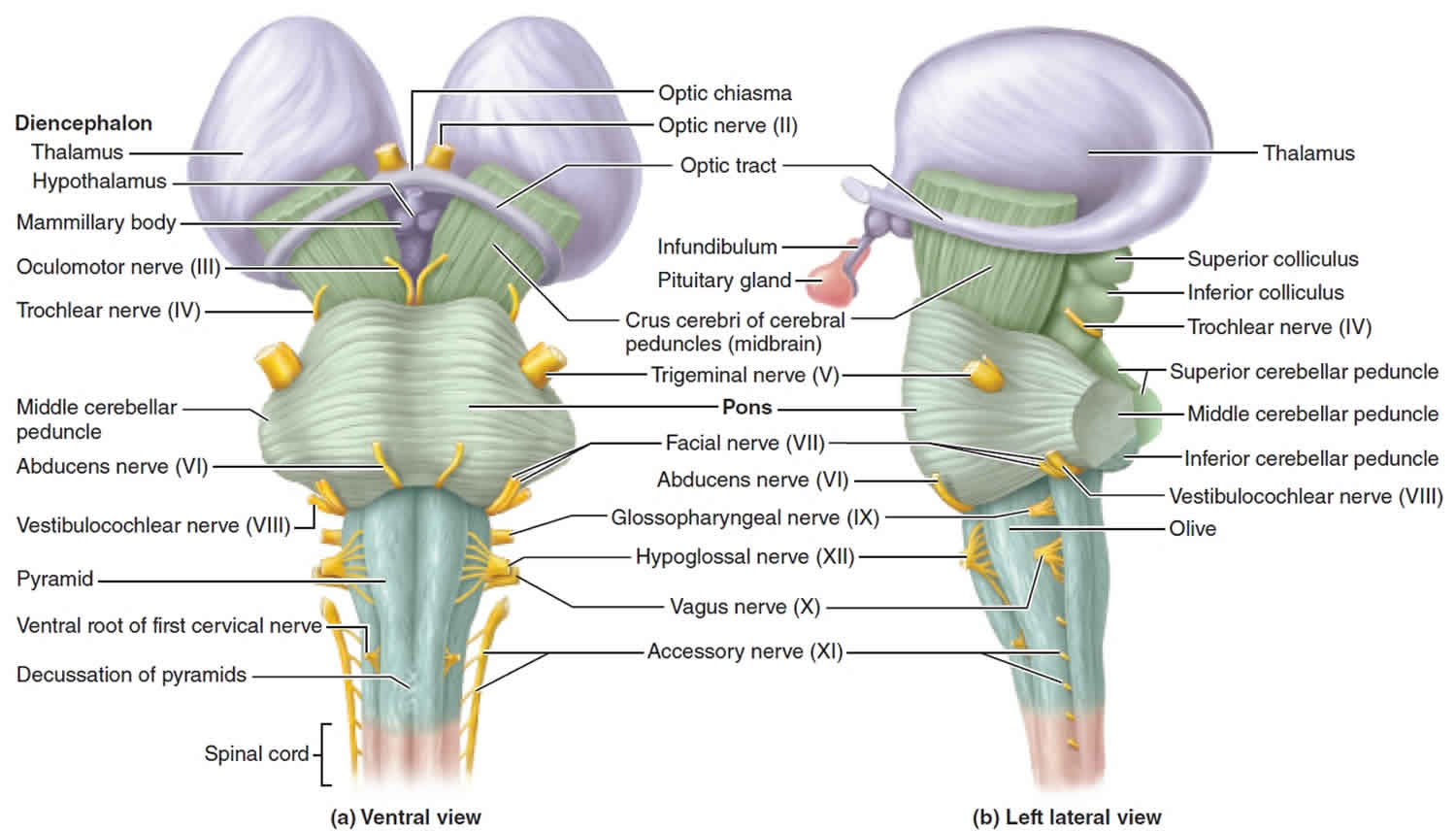
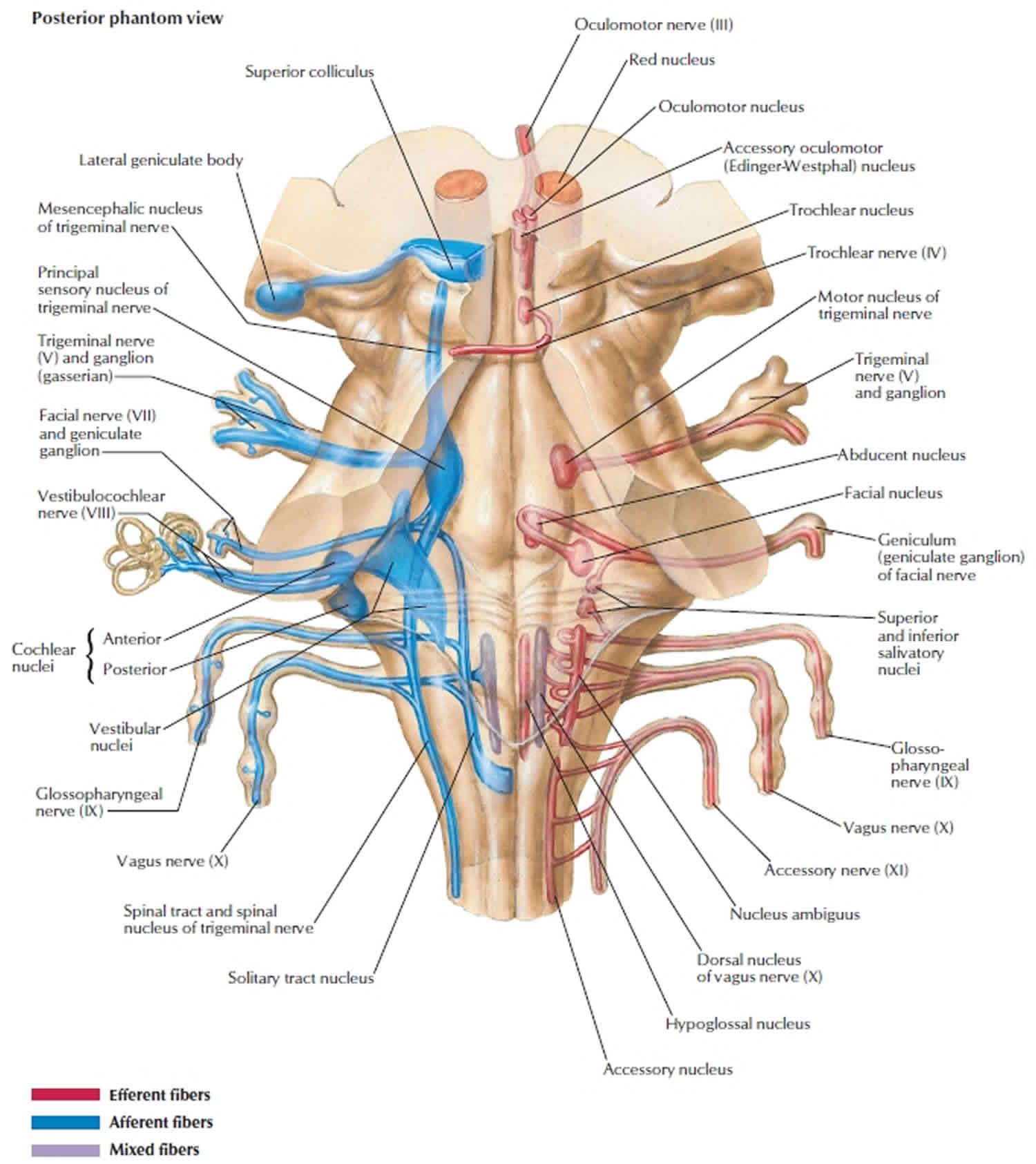
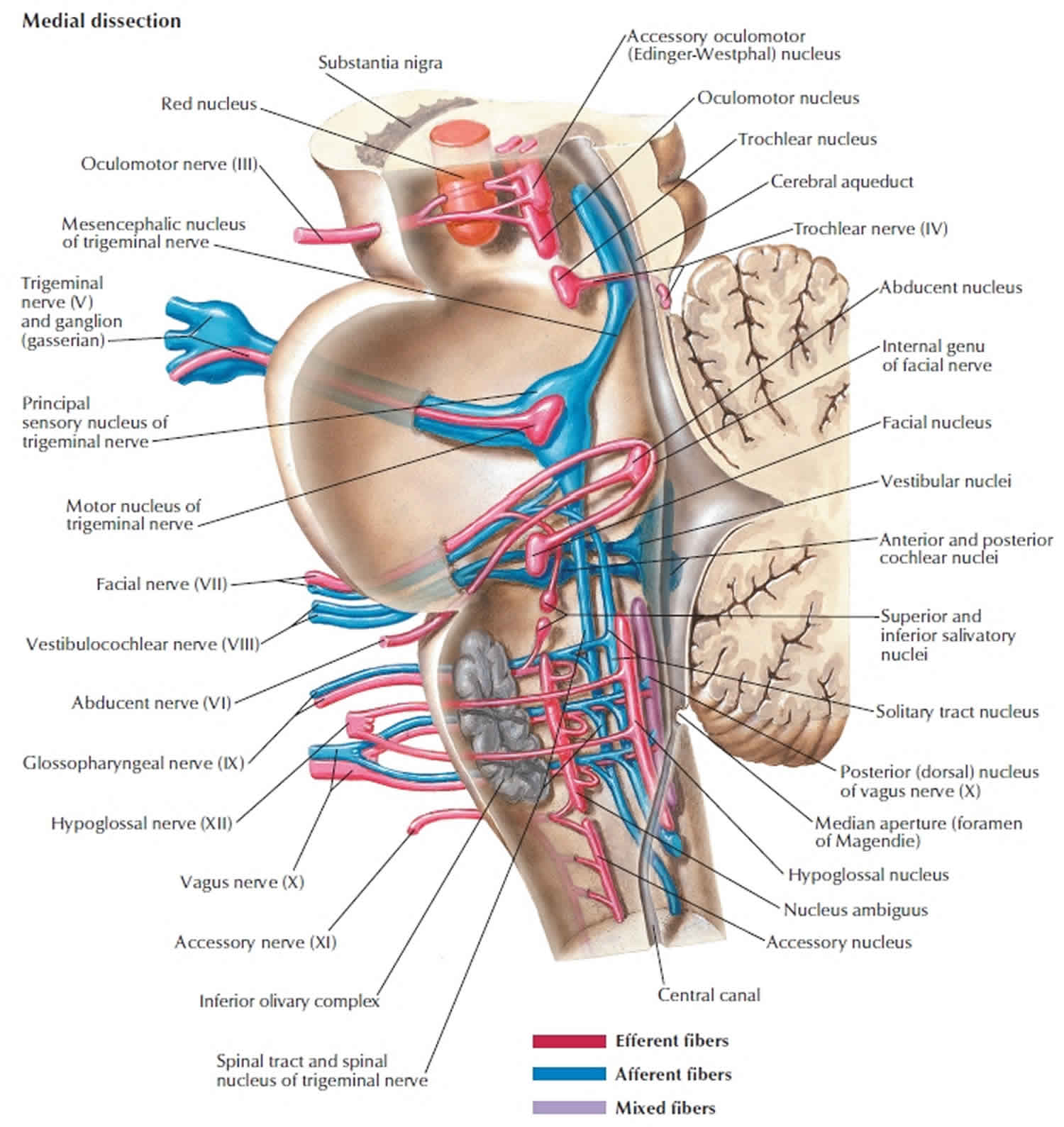
Figure 2. Brain stem
Brain stem parts
Medulla Oblongata
The medulla oblongata or more simply the medulla (“marrow”), is the most caudal part of the brain stem. The medulla oblongata is continuous with the superior part of the spinal cord at the level of the foramen magnum of the skull; it forms the inferior part of the brain stem. The medulla begins at the foramen magnum and extends to the inferior border of the pons, a distance of about 3 cm (1.2 in.).
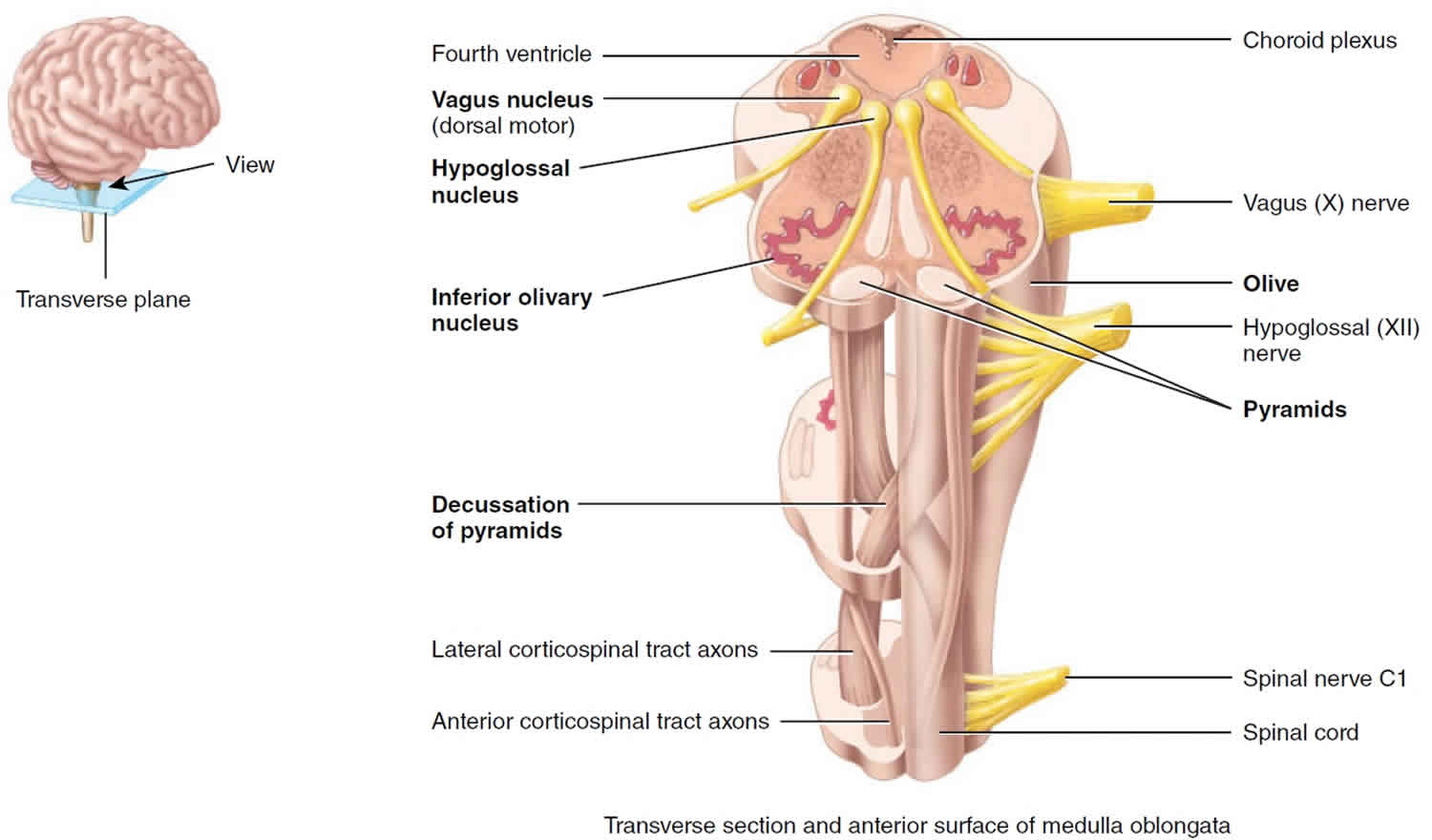
The medulla’s white matter contains all sensory (ascending) tracts and motor (descending) tracts that extend between the spinal cord and other parts of the brain. Some of the white matter forms bulges on the anterior aspect of the medulla. These protrusions, called the pyramids, are formed by the large corticospinal tracts that pass from the cerebrum to the spinal cord. The corticospinal tracts control voluntary movements of the limbs and trunk. These ridges are formed by the pyramidal tracts, large fiber tracts that originate from pyramid-shaped neurons in the cerebrum and descend through the brain stem and spinal cord carrying voluntary motor output to the spinal cord. Just superior to the junction of the medulla with the spinal cord, 90% of the axons in the left pyramid cross to the right side, and 90% of the axons in the right pyramid cross to the left side. This crossing is called the decussation of pyramids (“a crossing”) and explains why each side of the brain controls voluntary movements on the opposite side of the body.
The medulla also contains several nuclei (a collection of neuronal cell bodies within the CNS). Some of these nuclei control vital body functions. Examples of nuclei in the medulla that regulate vital activities include the cardiovascular center and the medullary rhythmicity center. The cardiovascular (CV) center regulates the rate and force of the heartbeat and the diameter of blood vessels. The medullary respiratory center adjusts the basic rhythm of breathing.
Besides regulating heartbeat, blood vessel diameter, and the normal breathing rhythm, nuclei in the medulla also control reflexes for vomiting, swallowing, sneezing, coughing, and hiccupping. The vomiting center of the medulla causes vomiting, the forcible expulsion of the contents of the upper gastrointestinal (GI) tract through the mouth. The deglutition center of the medulla promotes deglutition (swallowing) of a mass of food that has moved from the oral cavity of the mouth into the pharynx (throat). Sneezing involves spasmodic contraction of breathing muscles that forcefully expel air through the nose and mouth. Coughing involves a long-drawn and deep inhalation and then a strong exhalation that suddenly sends a blast of air through the upper respiratory passages. Hiccupping is caused by spasmodic contractions of the diaphragm (a muscle of breathing) that ultimately result in the production of a sharp sound on inhalation.
Just lateral to each pyramid is an oval-shaped swelling called an olive. Within the olive is the inferior olivary nucleus, a large wavy fold of gray matter viewable in cross section, which receives input from the cerebral cortex, red nucleus of the midbrain, and spinal cord. The inferior olivary nucleus is a relay station for sensory information traveling to the cerebellum, especially for proprioceptive information ascending from the spinal cord. Relay nuclei such as this process and edit information before sending it along. Neurons of the inferior olivary nucleus extend their axons into the cerebellum, where they regulate the activity of cerebellar neurons. By influencing cerebellar neuron activity, the inferior olivary nucleus provides instructions that the cerebellum uses to make adjustments to muscle activity as you learn new motor skills. The inferior cerebellar peduncles are fiber tracts that connect the medulla to the cerebellum dorsally.
Nuclei associated with sensations of touch, pressure, vibration and conscious proprioception are located in the posterior part of the medulla. These nuclei are the right and left gracile nucleus and cuneate nucleus. Ascending sensory axons of the gracile fasciculus and the cuneate fasciculus, which are two tracts in the posterior columns of the spinal cord, form synapses in these nuclei. Ascending fibers carrying general sensation from the discriminative senses (touch, pressure, limb/joint position) from the skin and proprioceptors synapse in these medullary nuclei along their pathway to the cerebrum. Postsynaptic neurons then relay the sensory information to the thalamus on the opposite side of the brain. The axons ascend to the thalamus in a band of white matter called the medial lemniscus (ribbon), which extends through the medulla, pons, and midbrain. The tracts of the posterior columns and the axons of the medial lemniscus are collectively known as the posterior column–medial lemniscus pathway.
The medulla also contains nuclei that are components of sensory pathways for gustation (taste), audition (hearing), and equilibrium (balance). The gustatory nucleus of the medulla is part of the gustatory pathway from the tongue to the brain; it receives gustatory input from the taste buds of the tongue. The cochlear nuclei of the medulla are part of the auditory pathway from the inner ear to the brain; they receive auditory input from the cochlea of the inner ear. The vestibular
nuclei of the medulla and pons are components of the equilibrium pathway from the inner ear to the brain; they receive sensory information associated with equilibrium from proprioceptors (receptors that provide information regarding body position and movements) in the vestibular apparatus of the inner ear.
Finally, the medulla contains nuclei associated with the following five pairs of cranial nerves.
- Vestibulocochlear (VIII) nerves. Several nuclei in the medulla receive sensory input from and provide motor output to the cochlea of the internal ear via the vestibulocochlear nerves. These nerves convey impulses related to hearing.
- Glossopharyngeal (IX) nerves. Nuclei in the medulla relay sensory and motor impulses related to taste, swallowing, and salivation via the glossopharyngeal nerves.
- Vagus (X) nerves. Nuclei in the medulla receive sensory impulses from and provide motor impulses to the pharynx and larynx and many thoracic and abdominal viscera via the vagus nerves.
- Accessory (XI) nerves (cranial portion). These fibers are actually part of the vagus (X) nerves. Nuclei in the medulla are the origin for nerve impulses that control swallowing via the vagus nerves (cranial portion of the accessory nerves).
- Hypoglossal (XII) nerves. Nuclei in the medulla are the origin for nerve impulses that control tongue movements during speech and swallowing via the hypoglossal nerves.
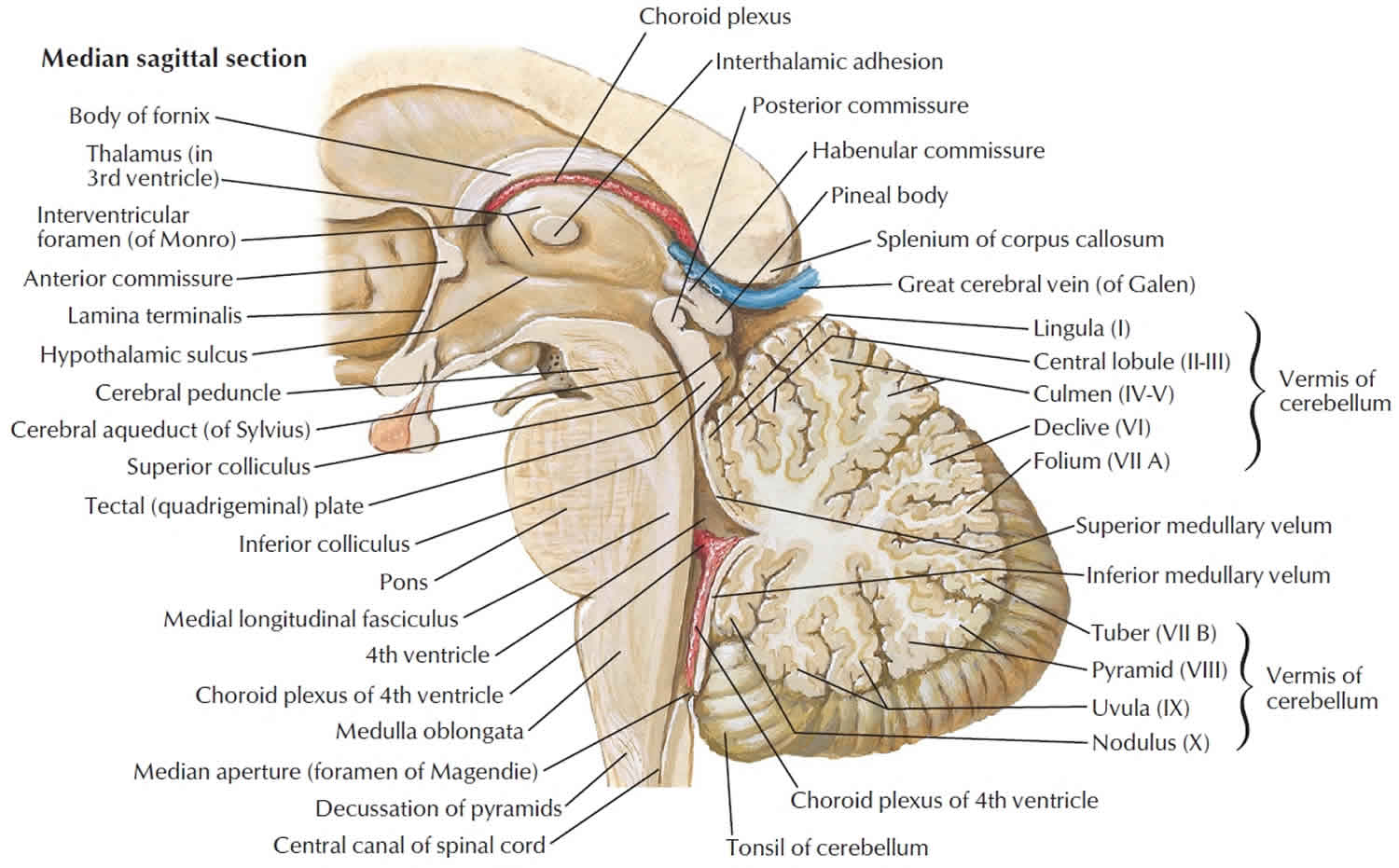
Figure 3. Brain stem parts
Figure 4. Medulla oblongata
Pons
The pons (= bridge) lies directly superior to the medulla and anterior to the cerebellum and is about 2.5 cm (1 in.) long. Like the medulla, the pons consists of both nuclei and tracts. As its name implies, the pons is a bridge that connects parts of the brain with one another. These connections are provided by bundles of axons. Some axons of the pons connect the right and left sides of the cerebellum. Others are part of ascending sensory tracts and descending motor tracts.
The pons has two major structural components: a ventral region and a dorsal region. The ventral region of the pons forms a large synaptic relay station consisting of scattered gray centers called the pontine nuclei. Entering and exiting these nuclei are numerous white matter tracts, each of which provides a connection between the cortex (outer layer) of a cerebral hemisphere and that of the opposite hemisphere of the cerebellum. This complex circuitry plays an essential role in coordinating and maximizing the efficiency of voluntary motor output throughout the body. The dorsal region of the pons is more like the other regions of the brainstem, the medulla and midbrain. It contains ascending and descending tracts along with the nuclei of cranial nerves.
Also within the pons is the pontine respiratory group. Together with the medullary respiratory center, the pontine respiratory group helps control breathing.
The pons also contains nuclei associated with the following four pairs of cranial nerves.
- Trigeminal (V) nerves. Nuclei in the pons receive sensory impulses for somatic sensations from the head and face and provide motor impulses that govern chewing via the trigeminal nerves.
- Abducens (VI) nerves. Nuclei in the pons provide motor impulses that control eyeball movement via the abducens nerves.
- Facial (VII) nerves. Nuclei in the pons receive sensory impulses for taste and provide motor impulses to regulate secretion of saliva and tears and contraction of muscles of facial expression via the facial nerves.
- Vestibulocochlear (VIII) nerves. Nuclei in the pons receive sensory impulses from and provide motor impulses to the vestibular apparatus via the vestibulocochlear nerves. These nerves convey impulses related to balance and equilibrium.
Midbrain
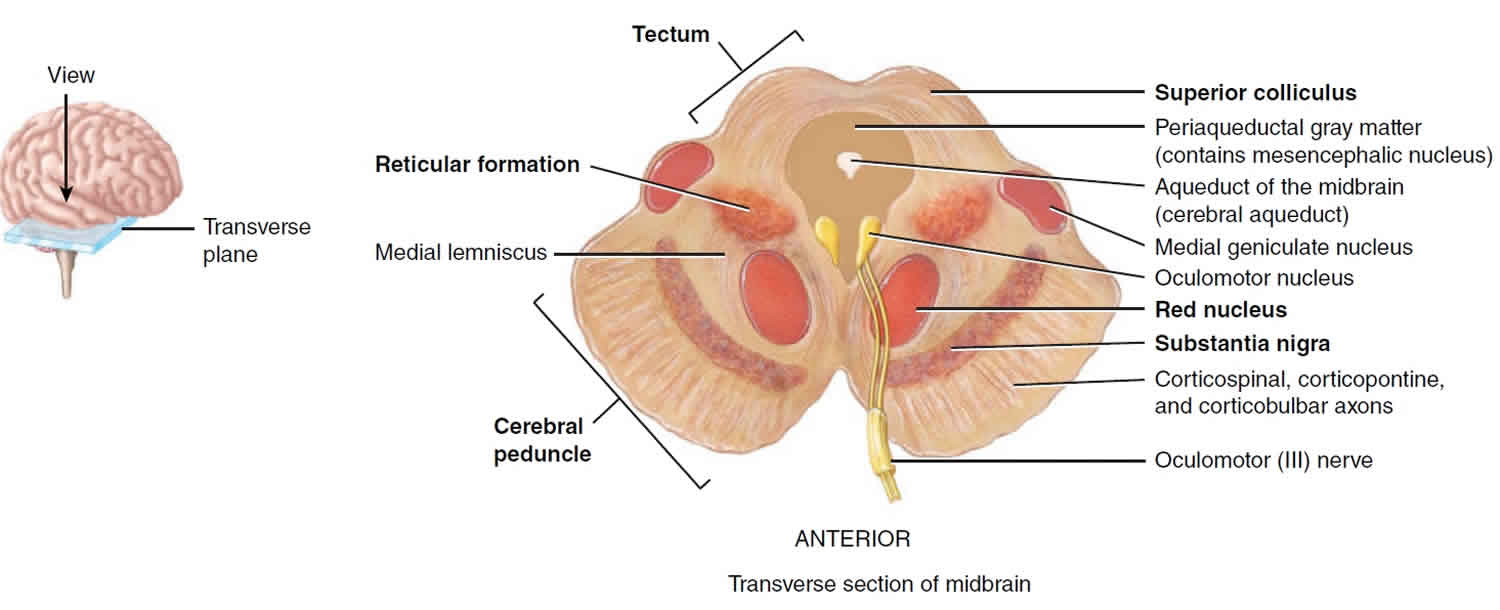
The midbrain or mesencephalon extends from the pons to the diencephalon and is about 2.5 cm (1 in.) long. The aqueduct of the midbrain (cerebral aqueduct) passes through the midbrain, connecting the third ventricle above with the fourth ventricle below. Like the medulla and the pons, the midbrain contains both nuclei and tracts.
The anterior part of the midbrain contains paired bundles of axons known as the cerebral peduncles (little feet). The cerebral peduncles consist of axons of the corticospinal, corticobulbar, and corticopontine tracts, which conduct nerve impulses from motor areas in the cerebral cortex to the spinal cord, medulla, and pons, respectively.
The posterior part of the midbrain, called the tectum (roof), contains four rounded elevations. The two superior elevations, nuclei known as the superior colliculi (singular is colliculus), serve as reflex centers for certain visual activities. Through neural circuits from the retina of the eye to the superior colliculi to the extrinsic eye muscles, visual stimuli elicit eye movements for tracking moving images (such as a moving car) and scanning stationary images (as you are doing to read this sentence). The superior colliculi are also responsible for reflexes that govern movements of the head, eyes, and trunk in response to visual stimuli. The two inferior elevations, the inferior colliculi, are part of the auditory pathway, relaying impulses from the receptors for hearing in the inner ear to the brain. These two nuclei are also reflex centers for the startle reflex, sudden movements of the head, eyes, and trunk that occur when you are surprised by a loud noise such as a gunshot.
The midbrain contains several other nuclei, including the left and right substantia nigra, which are large and darkly pigmented. Neurons that release dopamine, extending from the substantia nigra to the basal nuclei, help control subconscious muscle activities. Loss of these neurons is associated with Parkinson’s disease. Also present are the left and right red nuclei, which look reddish due to their rich blood supply and an iron-containing pigment in their neuronal cell bodies. Axons from the cerebellum and cerebral cortex form synapses in the red nuclei, which help control muscular movements.
Still other nuclei in the midbrain are associated with two pairs of cranial nerves:
- Oculomotor (III) nerves. Nuclei in the midbrain provide motor impulses that control movements of the eyeball, while accessory oculomotor nuclei provide motor control to the smooth muscles that regulate constriction of the pupil and changes in shape of the lens via the oculomotor nerves.
- Trochlear (IV) nerves. Nuclei in the midbrain provide motor impulses that control movements of the eyeball via the trochlear nerves.
Figure 5. Midbrain
Reticular Formation
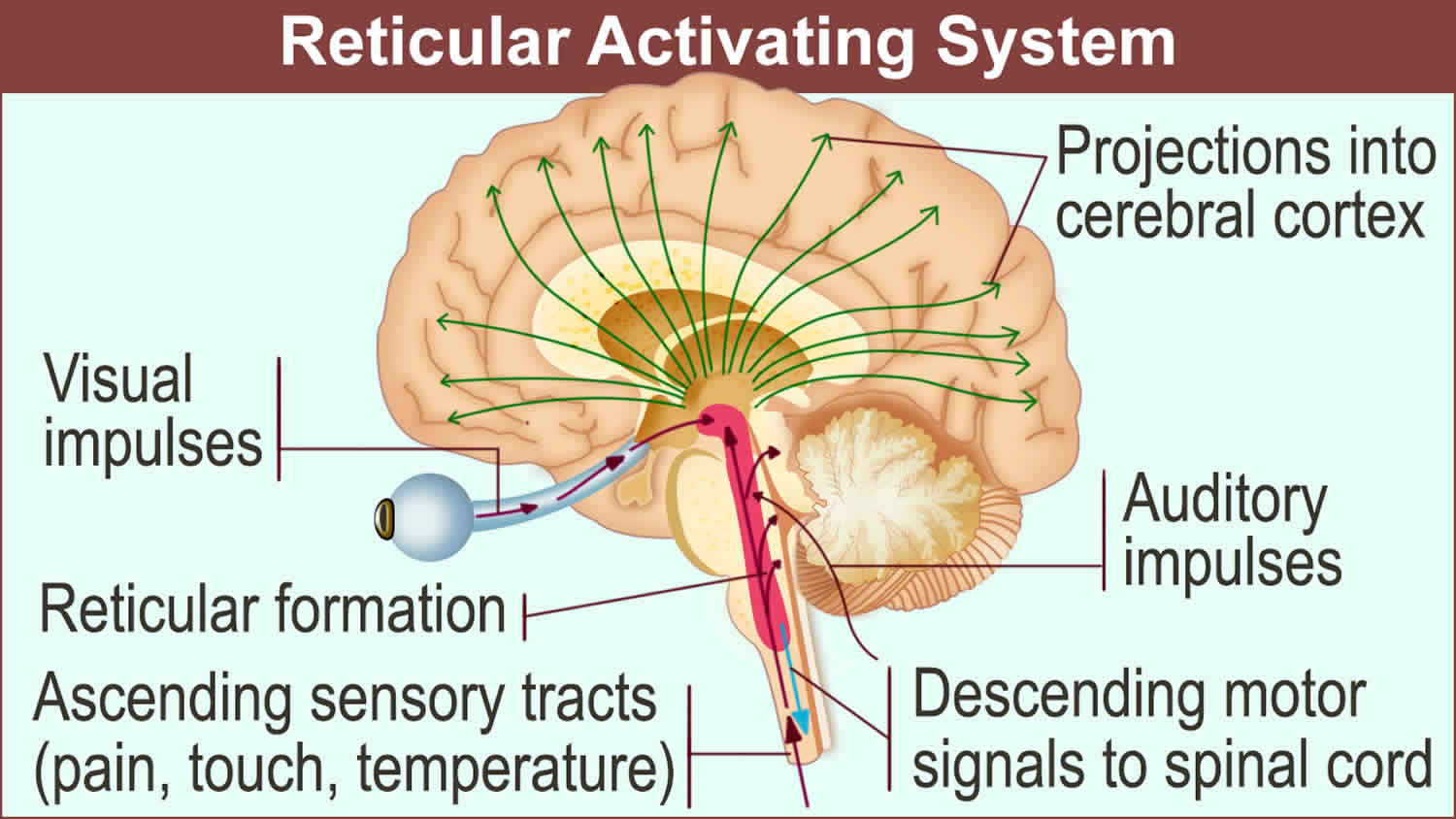
In addition to the well-defined nuclei already described, much of the brainstem consists of small clusters of neuronal cell bodies (gray matter) interspersed among small bundles of myelinated axons (white matter). The broad region where white matter and gray matter exhibit a netlike arrangement is known as the reticular formation. It extends from the superior part of the spinal cord, throughout the brainstem, and into the inferior part of the diencephalon. Neurons within the reticular formation have both ascending (sensory) and descending (motor) functions.
The ascending portion of the reticular formation is called the reticular activating system (RAS), which consists of sensory axons that project to the cerebral cortex, both directly and through the thalamus. Many sensory stimuli can activate the ascending portion of the reticular activating system (RAS). Among these are visual and auditory stimuli; mental activities; stimuli from pain, touch, and pressure receptors; and receptors in your limbs and head that keep you aware of the position of your body parts.
Perhaps the most important function of the reticular activating system (RAS) is consciousness, a state of wakefulness in which an individual is fully alert, aware, and oriented. Visual and auditory stimuli and mental activities can stimulate the reticular activating system (RAS) to help maintain consciousness. The reticular activating system (RAS) is also active during arousal, or awakening from sleep. Another function of the reticular activating system (RAS) is to help maintain attention (concentrating on a single object or thought) and alertness. The reticular activating system (RAS) also prevents sensory overload (excessive visual and/or auditory stimulation) by filtering out insignificant information so that it does not reach consciousness. For example, while waiting in the hallway for your anatomy class to begin, you may be unaware of all the noise around you while reviewing your notes for class. Inactivation of the reticular activating system (RAS) produces sleep, a state of partial consciousness from which an individual can be aroused. Damage to the reticular activating system (RAS), on the other hand, results in coma, a state of unconsciousness from which an individual cannot be aroused. In the lightest stages of coma, brainstem and spinal cord reflexes persist, but in the deepest states even those reflexes are lost, and if respiratory and cardiovascular controls are lost, the patient dies. Drugs such as melatonin affect the reticular activating system (RAS) by helping to induce sleep, and general anesthetics turn off consciousness via the reticular activating system (RAS). The descending portion of the reticular activating system (RAS) has connections to the cerebellum and spinal cord and helps regulate muscle tone, the slight degree of involuntary contraction in normal resting skeletal muscles. This portion of the reticular activating system (RAS) also assists in the regulation of heart rate, blood pressure, and respiratory rate.
Even though the reticular activating system (RAS) receives input from the eyes, ears, and other sensory receptors, there is no input from receptors for the sense of smell; even strong odors may fail to cause arousal. People who die in house fires usually succumb to smoke inhalation without awakening. For this reason, all sleeping areas should have a nearby smoke detector that emits a loud alarm. A vibrating pillow or flashing light can serve the same purpose for those who are hearing impaired.
Figure 6. Reticular activating system
Brain stem function
The brain stem has four general functions:
- It acts as a passageway for all the fiber tracts running between the cerebrum and the spinal cord.
- It is heavily involved with the innervation of the face and head; 10 of the 12 pairs of cranial nerves attach to it.
- It produces the rigidly programmed, automatic behaviors necessary for survival.
- It integrates auditory reflexes and visual reflexes.
The medulla also contains several nuclei (a collection of neuronal cell bodies within the CNS). Some of these nuclei control vital body functions. Examples of nuclei in the medulla that regulate vital activities include the cardiovascular center and the medullary rhythmicity center. The cardiovascular (CV) center regulates the rate and force of the heartbeat and the diameter of blood vessels. The medullary respiratory center adjusts the basic rhythm of breathing.
Besides regulating heartbeat, blood vessel diameter, and the normal breathing rhythm, nuclei in the medulla also control reflexes for vomiting, swallowing, sneezing, coughing, and hiccupping. The vomiting center of the medulla causes vomiting, the forcible expulsion of the contents of the upper gastrointestinal (GI) tract through the mouth. The deglutition center of the medulla promotes deglutition (swallowing) of a mass of food that has moved from the oral cavity of the mouth into the pharynx (throat). Sneezing involves spasmodic contraction of breathing muscles that forcefully expel air through the nose and mouth. Coughing involves a long-drawn and deep inhalation and then a strong exhalation that suddenly sends a blast of air through the upper respiratory passages. Hiccupping is caused by spasmodic contractions of the diaphragm (a muscle of breathing) that ultimately result in the production of a sharp sound on inhalation.
Medulla oblongata
The medulla oblongata contains sensory (ascending) and motor (descending) tracts. Cardiovascular center regulates heartbeat and blood vessel diameter. Medullary respiratory center (together with pons) regulates breathing. Contains gracile nucleus, cuneate nucleus, gustatory nucleus, cochlear nuclei, and vestibular nuclei (components of sensory pathways to brain). Inferior olivary nucleus provides instructions that cerebellum uses to adjust muscle activity when learning new motor skills. Other nuclei coordinate vomiting, swallowing, sneezing, coughing, and hiccupping. Contains nuclei of origin for vestibulocochlear (VIII), glossopharyngeal (IX), vagus (X), accessory (XI), and hypoglossal (XII) nerves. Reticular formation (also in pons, midbrain, and diencephalon) functions in consciousness and arousal.
Pons
The pons contains sensory and motor tracts. Pontine nuclei relay nerve impulses from motor areas of cerebral cortex to cerebellum. Contains vestibular nuclei (along with medulla) that are part of equilibrium pathway to brain. Pontine respiratory group (together with the medulla) helps control breathing. Contains nuclei of origin for trigeminal (V), abducens (VI), facial (VII), and vestibulocochlear (VIII) nerves.
Midbrain
The midbrain contains sensory and motor tracts. Superior colliculi coordinate movements of head, eyes, and trunk in response to visual stimuli. Inferior colliculi coordinate movements of head, eyes, and trunk in response to auditory stimuli. Substantia nigra and red nucleus contribute to control of movement. Contains nuclei of origin for oculomotor (III) and trochlear (IV) nerves.
Reticular activating system (RAS)
The reticular activating system (RAS) consists of sensory axons that project to the cerebral cortex, both directly and through the thalamus. Many sensory stimuli can activate the ascending portion of the reticular activating system (RAS). Among these are visual and auditory stimuli; mental activities; stimuli from pain, touch, and pressure receptors; and receptors in your limbs and head that keep you aware of the position of your body parts.
The most important function of the reticular activating system (RAS) is consciousness, a state of wakefulness in which an individual is fully alert, aware, and oriented. Visual and auditory stimuli and mental activities can stimulate the reticular activating system (RAS) to help maintain consciousness. The reticular activating system (RAS) is also active during arousal, or awakening from sleep. Another function of the reticular activating system (RAS) is to help maintain attention (concentrating on a single object or thought) and alertness. The reticular activating system (RAS) also prevents sensory overload (excessive visual and/or auditory stimulation) by filtering out insignificant information so that it does not reach consciousness. For example, while waiting in the hallway for your anatomy class to begin, you may be unaware of all the noise around you while reviewing your notes for class. Inactivation of the reticular activating system (RAS) produces sleep, a state of partial consciousness from which an individual can be aroused. Damage to the reticular activating system (RAS), on the other hand, results in coma, a state of unconsciousness from which an individual cannot be aroused. In the lightest stages of coma, brainstem and spinal cord reflexes persist, but in the deepest states even those reflexes are lost, and if respiratory and cardiovascular controls are lost, the patient dies. Drugs such as melatonin affect the reticular activating system (RAS) by helping to induce sleep, and general anesthetics turn off consciousness via the reticular activating system (RAS). The descending portion of the reticular activating system (RAS) has connections to the cerebellum and spinal cord and helps regulate muscle tone, the slight degree of involuntary contraction in normal resting skeletal muscles. This portion of the reticular activating system (RAS) also assists in the regulation of heart rate, blood pressure, and respiratory rate.
Even though the reticular activating system (RAS) receives input from the eyes, ears, and other sensory receptors, there is no input from receptors for the sense of smell; even strong odors may fail to cause arousal. People who die in house fires usually succumb to smoke inhalation without awakening. For this reason, all sleeping areas should have a nearby smoke detector that emits a loud alarm. A vibrating pillow or flashing light can serve the same purpose for those who are hearing impaired.
Brain stem stroke
Brain stem strokes can have complex symptoms, and they can be difficult to diagnose. A person may have vertigo, dizziness and severe imbalance without the hallmark of most strokes — weakness on one side of the body. The symptoms of vertigo dizziness or imbalance usually occur together; dizziness alone is not a sign of stroke. A brain stem stroke can also cause double vision, slurred speech and decreased level of consciousness.
Only a half-inch in diameter, the brain stem controls all basic activities of the central nervous system: consciousness, blood pressure and breathing. All motor control for the body flows through it. Brain stem strokes can impair any or all of these functions. More severe brain stem strokes can cause locked-in syndrome, a condition in which survivors can move only their eyes.
If a stroke in the brain stem results from a clot, the faster blood flow can be restored, the better the chances for recovery. Patients should receive treatment as soon as possible for the best recovery.
Like all strokes, brain stem strokes produce a wide spectrum of deficits and recovery. Whether a survivor has minor or severe deficits depends on the location of the stroke within the brain stem, the extent of injury and how quickly treatment is provided.
Risk factors for brain stem stroke are the same as for strokes in other areas of the brain: high blood pressure, diabetes, heart disease, atrial fibrillation and smoking. Similarly, brain stem strokes can be caused by a clot or a hemorrhage. There are also rare causes, like injury to an artery due to sudden head or neck movements.
Recovery is possible. Because brain stem strokes do not usually affect language ability, the patient is often able to participate more fully in rehabilitation therapy. Double vision and vertigo usually resolve after several weeks of recovery in mild to moderate brain stem strokes.
Brain stem tumor
Tumors in this critical area of the brain can cause weakness, stiff muscles, or problems with sensation, facial or eye movement, hearing, or swallowing. Double vision is a common early symptom of brain stem tumors, as are problems with coordination in walking. Because the brain stem is a small area that is so essential for life, it might not be possible to surgically remove tumors in this area.
A brain stem glioma is any type of glioma that starts in the brain stem. This term refers to the location of the tumor, rather than the type of cell it starts in.
- A small number of brain stem gliomas occur as tumors with very distinct edges (called focal brain stem gliomas).
- More often, brain stem gliomas grow diffusely throughout the brain stem (where the tumor cells are spread throughout normal tissue), rather than growing as a focal tumor (where the tumor cells are clustered together). These are referred to as diffuse midline gliomas. These tumors most often start in the pons, where they are called diffuse intrinsic pontine gliomas (DIPGs). These tumors can be hard to treat.
About 10% to 20% of brain tumors in children are brain stem gliomas. Nearly all of these tumors are some type of astrocytoma.
Gliomas are not a specific type of brain tumor. Glioma is a general term for tumors that start in glial cells. A number of tumors can be considered gliomas, including:
- Astrocytomas (which include glioblastomas)
- Oligodendrogliomas
- Ependymomas
About 3 out of 10 of all brain tumors are gliomas. Most fast-growing brain tumors are gliomas.
Astrocytomas
Astrocytomas are tumors that start in glial cells called astrocytes. About 2 out of 10 brain tumors are astrocytomas.
Most astrocytomas can spread widely throughout the brain and blend with the normal brain tissue, which can make them very hard to remove with surgery. Sometimes they spread along the cerebrospinal fluid (CSF) pathways. It is very rare for them to spread outside of the brain or spinal cord.
Astrocytomas (like other brain tumors) are classified into 4 grades.
- Non-infiltrating (grade I) astrocytomas do not usually grow into nearby tissues and tend to have a good prognosis. These include pilocytic astrocytomas and subependymal giant cell astrocytomas (SEGAs). They are more common in children than in adults.
- Low-grade (grade II) astrocytomas, such as diffuse astrocytomas, tend to be slow growing, but they can grow into nearby areas and can become more aggressive and fast growing over time.
- Anaplastic (grade III) astrocytomas grow more quickly.
- Glioblastomas (grade IV) are the fastest growing. These tumors make up more than half of all gliomas and are the most common malignant brain tumors in adults.
Oligodendrogliomas
These tumors start in brain glial cells called oligodendrocytes. These are grade II tumors that tend to grow slowly. Most of these can grow into (infiltrate) nearby brain tissue and cannot be removed completely by surgery. Oligodendrogliomas sometimes spread along the CSF pathways but rarely spread outside the brain or spinal cord. As with astrocytomas, they can become more aggressive over time. Very aggressive (grade III) forms of these tumors are known as anaplastic oligodendrogliomas. Only about 2% of brain tumors are oligodendrogliomas.
Ependymomas
These tumors start in ependymal cells, which line the ventricles. They can range from fairly low-grade (grade II) tumors to higher grade (grade III) tumors, which are called anaplastic ependymomas. Only about 2% of brain tumors are ependymomas.
Ependymomas are more likely to spread along the cerebrospinal fluid (CSF) pathways than other gliomas but do not spread outside the brain or spinal cord. Ependymomas may block the exit of CSF from the ventricles, causing the ventricles to become very large – a condition called hydrocephalus.
Unlike astrocytomas and oligodendrogliomas, ependymomas usually do not grow into normal brain tissue. As a result, some (but not all) ependymomas can be removed completely and cured by surgery. But because they can spread along ependymal surfaces and CSF pathways, treating them can sometimes be difficult. Spinal cord ependymomas have the greatest chance of being cured with surgery, but treatment can cause side effects related to nerve damage.