Contents
What is canthaxanthin
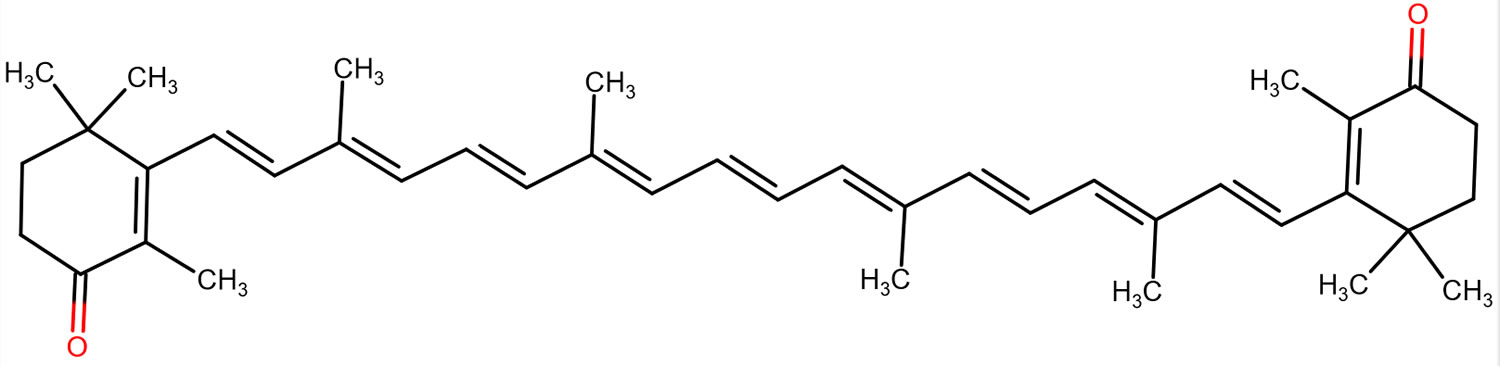
Canthaxanthin (β-β-carotene-4,4-dione) is a naturally occurring carotenoid pigment or keto-carotene which is synthesized by microorganisms and plants 1. Canthaxanthin is one of the carotenoids without provitamin activity 2. Canthaxanthin can be found in fruits, vegetables, and fish and primarily occurs in human tissue as a result of dietary ingestion. Like other carotenoids, it is fat-soluble and intensely colored. Canthaxanthin carries a red to orange hue and is used as an agent for coloring foods, dyes, and for skin bronzing. Experimental use has been successful for photoprotection for erythropoietic protoporphyria and cosmetic improvement in vitiligo 3. The bronzing effect is achieved through carotenoid deposition in the dermis and subcutaneous tissue. Past reports have concluded that this chemical canthaxanthin does not carry genotoxic, reproductive, or carcinogenic risks and does not have allergic potential as an oral medication and that acceptable daily intake is 0.03 mg/kg/day 4. However, there have been reports of adverse impacts on human health, mainly canthaxanthin retinopathy, which manifests as birefringent, yellow to red crystals in the macula 5. In addition, a case of aplastic anemia has been reported in association with canthaxanthin ingestion 6.
Both the Joint FAO/WHO Expert Committee on Food Additives (JECFA) and Scientific Committee on Food (SFC) committees have established an Acceptable Daily Intake (ADI) of 0.03 mg/kg body weight/day based on the formation of crystalline deposits in the retina (canthaxanthin retinopathy), which was observed in monkeys 7 and humans 8. The Acceptable Daily Intake (ADI) is defined as an estimate of the amount of a food additive, expressed on a body weight basis that can be ingested on a daily basis over a lifetime without appreciable risk to health. A no-observed-adverse-effect-level (NOAEL) of 0.25 mg/kg body weight/day for scotopic b-wave changes (without impairment of vision) was reported in a human study and a benchmark dose (BMD)05 of 12-20 mg/day, amounting to 0.20-0.33 mg/kg body weight/day for a 60 kg person, were derived in a worst case benchmark dose (BMD) analysis of the data from a meta-analysis on the crystal incidence in human eyes with increasing daily doses of canthaxanthin. Based on these two studies, the European Food Safety Authority (EFSA) Panel allocated an Acceptable Daily Intake (ADI) of 0.03 mg/kg body weight/day. This Acceptable Daily Intake (ADI) is in line with the ADI derived previously by JECFA and the SCF. The European Food Safety Authority (EFSA) Panel concluded that for both adults and children, total anticipated combined exposure to canthaxanthin from application as food and feed additive is unlikely to exceed the ADI.
The acute oral toxicity of canthaxanthin is very low. The oral Lethal Dose 50% (LD50) of canthaxanthin in mice is reported to be 10 000 mg/kg body weight. Lethal Dose 50% (LD50) is the amount of the substance required (usually per body weight) to kill 50% of the test population. In subchronic (13-week) studies with canthaxanthin, doses of 500 mg/kg body weight/day and higher in mice and of 2000 mg/kg body weight/day in rats were associated with small decreases in body weight compared with controls and discoloration of some internal tissues, but no toxicologically relevant changes were seen. From the few available in vitro and in vivo studies, there are no indications that canthaxanthin is genotoxic.
Canthaxanthin was not carcinogenic in doses amounting to 1000 mg/kg body weight/day in laboratory rodents. In two carcinogenicity studies in rats increased plasma cholesterol (especially in females) and increases in other clinical-chemistry parameters along with increased relative liver weights (females only) and histological changes in the liver were indicative of liver injury, but some of the changes were reversible after a recovery period. There were no indications that canthaxanthin had adverse effects on reproduction and/or the developing fetus in doses up to 1000 mg/kg body weight/day in rats and in doses up to 400 mg/kg body weight/day in rabbits.
There are no indications that canthaxanthin has an allergenic potential upon oral intake.
In animals, only 3 to 8% of orally administered canthaxanthin is absorbed and faecal excretion is the major route of elimination (85 to 89% of the dose in monkeys). Canthaxanthin is further distributed to liver, spleen, adipose tissue and adrenals. It is suggested by studies in rats that the amount of lipids ingested with the diet can increase the absorption of canthaxanthin. In monkeys, the concentration of canthaxanthin in the retina is dose-related, but nonlinear, suggesting that saturation could occur. In animals as well as in humans, elimination from adipose tissue is very slow, while canthaxanthin is eliminated from other tissues soon after withdrawal. In humans, a part of the orally ingested canthaxanthin is absorbed (9 to 34% of the dose) and its elimination is characterized by a long half-life of about 5 days. No data on canthaxanthin metabolism were reported in humans.
Figure 1. Canthaxanthin chemical structure
Canthaxanthin is also not generally considered a dietary carotenoid, but it may be included in the human diet by its widespread application as a coloring factor in foods and animal feeds 9, 10. In addition, Canthaxanthin has an antioxidant action, are free radical quenchers, potent quenchers of reactive oxygen species and nitrogen oxygen species, and chain-breaking antioxidants 11. Canthaxanthin is a superior antioxidant and scavengers of free radicals when compared with the carotenoids such as β-carotene 12. Canthaxanthin is documented to be able to suppress the development of preneoplastic liver cell lesions caused by aflatoxin B1 in rats by the deviation of aflatoxin B1 metabolism towards detoxification pathways 13.
Anti-cancer activity
Canthaxanthin may prevent proliferation of human colon cancer cells protect mouse embryo fibroblasts from transformation 14 and kept mice from mammary and skin tumor development 15. Canthaxanthin has also proved effective at preventing both oral and colon carcinogenesis in rats 16. Although it is a potent antioxidant, the chemopreventive impacts of canthaxanthin may also be associated to its ability to up-regulate gene expression, resulting in increased gap junctional cell-cell communication 17. There are evidences showing that the canthaxanthin is pure antioxidants because it shows little or no prooxidative behavior even at high carotenoid content and high oxygen tension 18. The chemopreventive effects of canthaxanthin may also be correlated to its ability to induce xenobiotic metabolizing enzymes, as has been shown in the liver, lungs and kidneys of rats 19. Canthaxanthin overuse as a sunless tanning product has caused to the appearance of crystalline deposits in the human retina 20. There are some other studies showing induction of some enzymes by canthaxanthin. The group of researchers showed canthaxanthin induced P4501A1 and 1A2, and CYP1A1 and 1A2, which are involved in the metabolism of such potential carcinogens as polycyclic aromatic hydrocarbons, aromatic amines and aflatoxin 21. This xanthophyll also induced selected P450 enzymes in rat lung and kidney tissues, but not in the small intestine 22. On the basis of these studies, canthaxanthin shows inhibitory effects on cancer development in urinary bladder 23, tongue 24 and colorectum 25 by the prevention of cell proliferation. Canthaxanthin has also showed cancer chemopreventive actions in UV-B-induced mouse skin tumorigenesis 26 and chemically-induced gastric 27 and breast carcinogenesis 28. Canthaxanthin may inhibit the proliferation of human colon cancer cells and kept mouse embryo fibroblasts from transformation 14 and mice from mammary and skin tumor development 15. Canthaxanthin is efficient in preventing both oral and colon carcinogenesis in rats 29.
Canthaxanthin retinopathy
In the setting of canthaxanthin retinopathy, it is thought that damage occurs at the level of the macular vascular system around areas of canthaxanthin-lipoprotein complex deposits, which comprise the visible crystals 30. It is proposed that vascular dysfunction occurs due to aggregation of these complexes in vessel lipid layers, which modify and disrupt lipid membrane properties 30.
Incidence and prevalence of canthaxanthin-induced retinopathy are difficult to predict due to the generally asymptomatic course of canthaxanthin retinopathy. Some reports state an incidence between 12 and 14% 31. Harnois et al. 31 noted that crystal appearance follows a dose-dependent correlation, seen with 50% of patients ingesting a total dose of 37 g and with 100% ingesting greater than 60 g.
To reproduce and investigate in a primate animal model the phenomenon of the red carotenoid canthaxanthin (beta, beta-carotene-4’4′-dione) to induce crystal-like retinal deposits as they have been observed in the ocular fundus of humans after high canthaxanthin intake (i.e., more than 30 mg/day), this study involving cynomolgus monkeys 7. The researchers found a high intake of canthaxanthin 5.4, 16.2, or 48.6 mg canthaxanthin/kg body weight daily orally for 2.5 years led to the deposition of crystal-like birefringent inclusions in the inner layers of the peripheral retina and, to some extent, the central retina of cynomolgus monkeys 7.
Several animal studies investigated ocular toxicity related to canthaxanthin deposition in the eye. The crystalline deposits were not observed in animals receiving 0.2 mg canthaxanthin/kg body weight/day. The canthaxanthin-induced retinal inclusions were not accompanied by adverse effects on visual function measured by electroretinography (ERG). In humans, a meta-analysis of the published studies and the available unpublished reports on crystal formation by Köpcke et al. 32 indicated a significant dose-response relationship for both total and daily doses of canthaxanthin. The incidence rates were, for the following daily doses (per subject), <30mg = 0%, 30 mg = 9.6%, 45 mg = 20.3%, 75-105 mg = 43.1%, > 105 mg = 52%. Crystal formation was reversible as evidenced by their disappearance albeit slowly over time in patients that had ceased high-dose consumption of canthaxanthin.
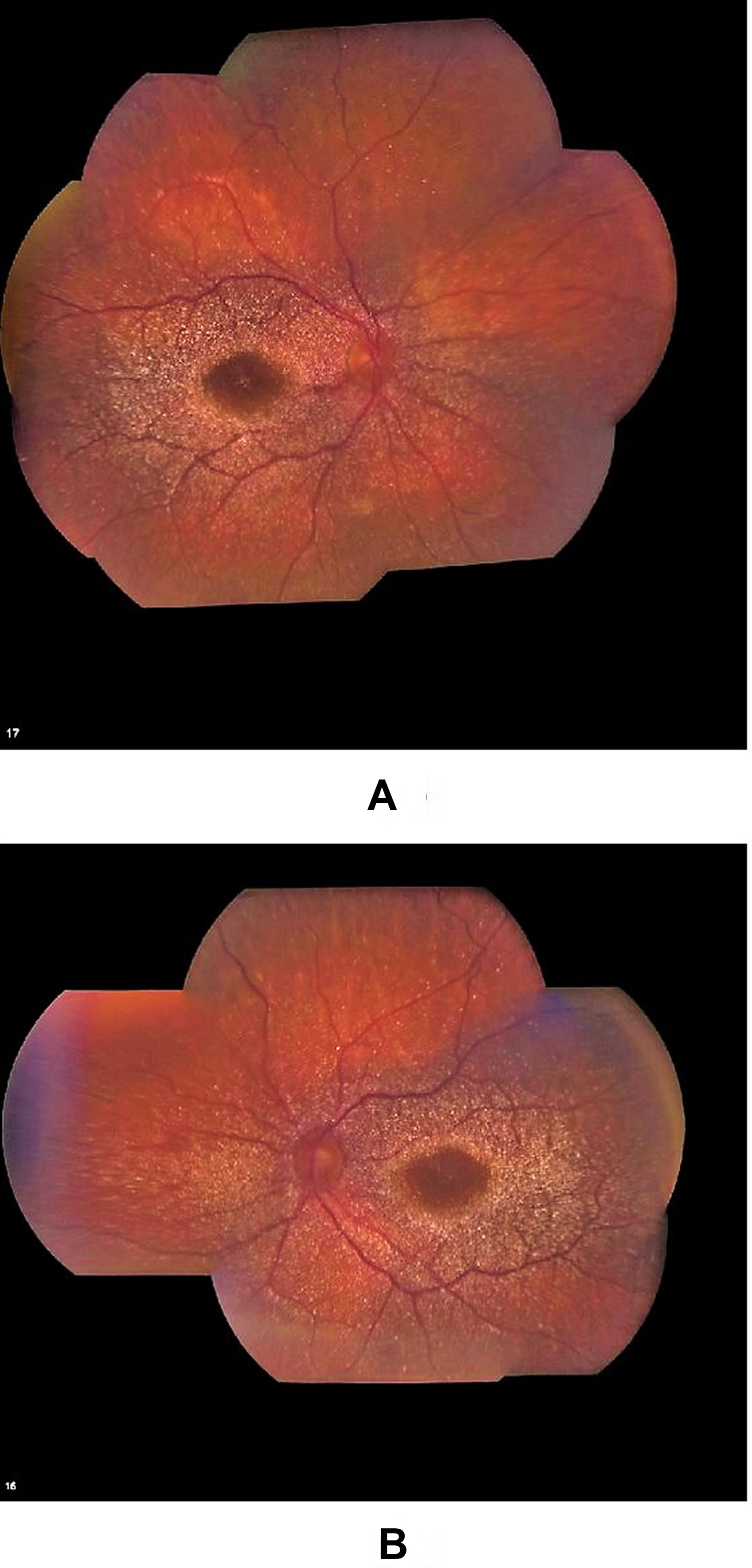
Funduscopic examination generally reveals highly reflective, tiny (30 μm) crystals accumulating in the perifoveal area. Daicker et al. 33 reported that, when examined posthumously, light microscopy revealed birefringent crystals in the inner layers of the entire retina, and analysis with ultrahigh resolution optical coherence tomography (OCT) has shown that canthaxanthin retinopathy crystals are found in the outer plexiform layer 34. While the vast majority of patients with canthaxanthin retinopathy remain asymptomatic, visual field defects, decreased visual acuity, abnormal electroretinogram testing, and low static luminance threshold may be present 35. Decreased static perimetry testing in patients with canthaxanthin retinopathy compared to control group was described by Harnois et al. 36, with a positive correlation with total drug dosage. On long-term followup, static perimetry testing returned to normal following discontinuation of the canthaxanthin. While often normal, fluorescein angiography may show a perifoveal ring of blocked fluorescence corresponding to areas of crystal deposition 8.
Treatment for canthaxanthin retinopathy is immediate discontinuation of the drug as soon as crystals are identified, even if the patient is asymptomatic 1. Prognosis is very good with complete recovery occurring in the vast majority of patients. Hueber et al. 8 followed five patients for 16–24 years and no long-term adverse effects were found, and fluorescein angiography results were normal, although complete resolution of golden particle appearance took up to 20 years.
In summary, canthaxanthin retinal crystal deposition is a very common finding in patients with prolonged use of the canthaxanthin pills. Symptomatic visual loss is less common and correlates with total dosage and possibly patient age. Even with profound visual loss, prognosis for improvement is very good with recognition and discontinuation of the canthaxanthin drug 1.
Figure 2. Canthaxanthin retinopathy
Note: Fundus photographs of a woman showing diffuse canthaxanthin crystal deposition. (A) Right eye. (B) Left eye.
[Source 1]Canthaxanthin tanning pills
According to the U.S. Food and Drug Administration (FDA) there are no such tanning pills approved for this purpose 37. Nevertheless, pills bearing tanning claims continue to appear on the market. Consumers should be aware of risks associated with such products, as well as doubts about their efficacy.
Although canthaxanthin is approved by FDA for use as a color additive in foods, where it is used in small amounts, its use in so-called tanning pills is not approved 37. Imported tanning pills containing canthaxanthin are subject to automatic detention as products containing unsafe color additives 38.
The so-called tanning pills are promoted for tinting the skin by ingesting massive doses of color additives, usually canthaxanthin. When taken at these large doses – many times greater than the amount normally ingested in food – this substance is deposited in various parts of the body, including the skin, where it imparts a color. The color varies with each individual, ranging from orange to brownish. The bronzing effect is achieved through carotenoid deposition in the dermis and subcutaneous tissue. This coloration is not the result of an increase in the skin’s supply of melanin, melanin is the substance that is produced naturally in the skin to help protect it against UV radiation and gives skin its natural tan color.
Canthaxanthin side effects
Side effects of canthaxanthin pills include the deposition of crystals in the eye also known as “canthaxanthin-induced retinopathy” (see Figure 2 above). Hulisz and Boles 39 also referred to reports of “nausea, cramping, diarrhea, severe itching, and welts” associated with the use of canthaxanthin “tanning” pills.
- Beaulieu RA, Warwar RE, Buerk BM. Canthaxanthin Retinopathy with Visual Loss: A Case Report and Review. Case Reports in Ophthalmological Medicine. 2013;2013:140901. doi:10.1155/2013/140901. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3833018/[↩][↩][↩][↩]
- Tanaka T, Shnimizu M, Moriwaki H. Cancer chemoprevention by carotenoids. Molecules. 2012;17:3202–42 https://www.ncbi.nlm.nih.gov/pubmed/22418926[↩]
- Gupta AK, Haberman HF, Pawlowski D. Canthaxanthin. International Journal of Dermatology. 1985;24(8):528–532. https://www.ncbi.nlm.nih.gov/pubmed/3934089[↩]
- EFSA Panel on Food Additives Nutrient Sources added to Food ANS. Scientific Opinion on the reevaluation of canthaxanthin (E 161 g) as a food additive. EFSA Journal. 2010;8, 10[↩]
- Chang TS, Aylward GW, Clarkson JG, Gass JDM. Asymmetric canthaxanthin retinopathy. American Journal of Ophthalmology. 1995;119(6):801–802 https://www.ncbi.nlm.nih.gov/pubmed/7785700[↩]
- Bluhm R, Branch R, Johnston P, Stein R. Aplastic anemia associated with canthaxanthin ingested for “tanning” purposes. The Journal of the American Medical Association. 1990;264(9):1141–1142 https://www.ncbi.nlm.nih.gov/pubmed/2117075[↩]
- Occurrence of birefringent retinal inclusions in cynomolgus monkeys after high doses of canthaxanthin. Investigative Ophthalmology & Visual Science March 1997, Vol.38, 741-752. http://iovs.arvojournals.org/article.aspx?articleid=2161679[↩][↩][↩]
- Hueber A, Rosentreter A, Severin M. Canthaxanthin retinopathy: long-term observations. Ophthalmic Research. 2011;46(2):103–106. https://www.ncbi.nlm.nih.gov/pubmed/21346389[↩][↩][↩]
- Astorg P. Food carotenoids and cancer prevention: an overview of current research. Trends Food Sci Technol. 1997;8:406–13.[↩]
- Baker RTM. Canthaxanthin in aqua feed applications: is there any risk? Trends Food Sci Technol. 2002;12:240–248.[↩]
- Aghajanpour M, Nazer MR, Obeidavi Z, Akbari M, Ezati P, Kor NM. Functional foods and their role in cancer prevention and health promotion: a comprehensive review. American Journal of Cancer Research. 2017;7(4):740-769. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5411786[↩]
- Pashkow FJ, Watumull DG, Campbell CL. Astaxanthin: a novel potential treatment for oxidative stress and inflammation in cardiovascular disease. Am J Cardiol. 2008;101:58D–68D https://www.ncbi.nlm.nih.gov/pubmed/18474276[↩]
- Gradelet S, Le Bon AM, Berges R, Suschetet M, Astorg P. Dietary carotenoids inhibit aflatoxin B1-induced liver preneoplastic foci and DNA damage in the rat: role of the modulation of aflatoxin B1 metabolism. Carcinogenesis. 1998;19:403–411 https://www.ncbi.nlm.nih.gov/pubmed/9525273[↩]
- Bertram JS, Pung A, Churley M, Kappock TJ, Wilkins LR, Cooney RV. Diverse carotenoids protect against chemically induced neoplastic transformation. Carcinogenesis. 1991;12:671–78 https://www.ncbi.nlm.nih.gov/pubmed/2013131[↩][↩]
- Mathews-Roth MM, Krinsky NI. Carotenoid dose level and protection against UV-B induced skin tumors. Photochem Photobiol. 1985;42:35–58 https://www.ncbi.nlm.nih.gov/pubmed/4059356[↩][↩]
- Tanaka T, Makita H, Ohnishi M, Mori H, Satoh K, Hara A. Chemoprevention of rat oral carcinogenesis by naturally occurring xanthophylls, astaxanthin and canthaxanthin. Cancer Res. 1995;55:4059–64 https://www.ncbi.nlm.nih.gov/pubmed/7664280[↩]
- Hanusch M, Gillette C, O’Neill C. Induction of gap junctional communication by 4-oxoretinoic acid generated from its precursor canthaxanthin. Arch Biochem Biophys. 1995;317:423–35 https://www.ncbi.nlm.nih.gov/pubmed/7893159[↩]
- Beutner S, Pung A, Churley M, Kappock TJ. Quantitative assessment of antioxidant properties of natural colorants and phytochemicals: carotenoids, flavonoids, phenols and indigoids. The role of β-carotene in antioxidant functions. J Sci Food Agric. 2001;81:559–65[↩]
- Jewell C, O’Brien NM. Effect of dietary supplementation with carotenoids on xenobiotic metabolizing enzymes in the liver, lung, kidney and small intestine of the rat. Br J Nutr. 1999;81:235–43 https://www.ncbi.nlm.nih.gov/pubmed/10434850[↩]
- Goralczyk R, Wu A, Goukassian D. Occurrence of birefringent retinal inclusions in cynomolgus monkeys after high doses of canthaxanthin. Invest Ophthalmol Vis Sci. 1997;38:741–52 https://www.ncbi.nlm.nih.gov/pubmed/9071228[↩]
- Gradelet S, Sewgobind K, Desai S, Dunn L. Modulation of aflatoxin B1 carcinogenicity, genotoxicity and metabolism in rat liver by dietary carotenoids: evidence for a protective effect of CYP1A inducers. Cancer Lett. 1997;114:221–29 https://www.ncbi.nlm.nih.gov/pubmed/9103297[↩]
- Jewell C, O’Brien NM. Effect of dietary supplementation with carotenoids on xenobiotic metabolizing enzymes in the liver, lung, kidney and small intestine of the rat. Br J Nutr. 1999;81:235–43[↩]
- Tanaka T, Morishita Y, Suzui M, Kojima T, Okumura A, Mori H. Chemoprevention of mouse urinary bladder carcinogenesis by the naturally occurring carotenoid astaxanthin. Carcinogenesis. 1994;15:15–19 https://www.ncbi.nlm.nih.gov/pubmed/8293542[↩]
- Tanaka T, Makita H, Ohnishi M, Mori H, Satoh K, Hara A. Chemoprevention of rat oral carcinogenesis by naturally occurring xanthophylls, astaxanthin and canthaxanthin. Cancer Res. 1995;55:4059–64. https://www.ncbi.nlm.nih.gov/pubmed/7664280[↩]
- Tanaka T, Kawamori T, Ohnishi M, Makita H, Mori H, Satoh K, Hara A. Suppression of azoxymethane-induced rat colon carcinogenesis by dietary administration of naturally occurring xanthophylls astaxanthin and canthaxanthin during the post initiation phase. Carcinogen. 1995;16:2957–63. https://www.ncbi.nlm.nih.gov/pubmed/8603470[↩]
- Black HS, Mathews-Roth MM. Protective role of butylated hydroxytoluene and certain carotenoids in photocarcinogenesis. Photochem Photobiol. 1991;53:707–16 https://www.ncbi.nlm.nih.gov/pubmed/1881965[↩]
- Santamaria L, Bianchi A, Arnaboldi A, Ravetto C, Bianchi L, Pizzala R, Andreoni L, Santagati G, Bermond P. Chemoprevention of indirect and direct chemical carcinogenesis by carotenoids as oxygen radical quenchers. Ann N Y Acad Sci. 1988;534:584–96 https://www.ncbi.nlm.nih.gov/pubmed/3133972[↩]
- Grubbs CJ, Eto I, Juliana MM, Whitaker LM. Effect of canthaxanthin on chemically induced mammary carcinogenesis. Oncology. 1991;48:239–45. https://www.ncbi.nlm.nih.gov/pubmed/1902560[↩]
- Tanaka T, Kawamori T, Ohnishi M, Makita H, Mori H, Satoh K, Hara A. Suppression of azoxymethane-induced rat colon carcinogenesis by dietary administration of naturally occurring xanthophylls astaxanthin and canthaxanthin during the post initiation phase. Carcinogen. 1995;16:2957–63 https://www.ncbi.nlm.nih.gov/pubmed/8603470[↩]
- Sujak A. Interactions between canthaxanthin and lipid membranes—possible mechanisms of canthaxanthin toxicity. Cellular and Molecular Biology Letters. 2009;14(3):395–410 https://www.ncbi.nlm.nih.gov/pubmed/19214394[↩][↩]
- Harnois C, Samson J, Malenfant M, Rousseau A. Canthaxanthin retinopathy: anatomic and functional reversibility. Archives of Ophthalmology. 1989;107(4):538–540. https://www.ncbi.nlm.nih.gov/pubmed/2495787[↩][↩]
- Köpcke W, Barker FM and Schalch W, 1995. Canthaxanthin-deposition in the retina. A biostatistical evaluation of 411 cases taking this carotenoid for medical or cosmetical purposes. Journal of Toxicology-Cutaneous and Ocular Toxicology 14, 89-104.[↩]
- Daicker B, Schiedt K, Adnet JJ, Bermond P. Canthaxanthin retinopathy. An investigation by light and electron microscopy and physicochemical analysis. Graefe’s Archive for Clinical and Experimental Ophthalmology. 1987;225(5):189–197 https://www.ncbi.nlm.nih.gov/pubmed/3111944[↩]
- Chan A, Ko TH, Duker JS. Ultrahigh-resolution optical coherence tomography of canthaxanthine retinal crystals. Ophthalmic Surgery Lasers and Imaging. 2006;37(2):138–139 https://www.ncbi.nlm.nih.gov/pubmed/16583635[↩]
- Fraunfelder FW. Ocular side effects from herbal medicines and nutritional supplements. American Journal of Ophthalmology. 2004;138(4):639–647 https://www.ncbi.nlm.nih.gov/pubmed/15488795[↩]
- Harnois C, Cortin P, Samson J, Boudreault G, Malenfant M, Rousseau A. Static perimetry in canthaxanthin maculopathy. Archives of Ophthalmology. 1988;106(1):58–60 https://www.ncbi.nlm.nih.gov/pubmed/3122712[↩]
- Tanning Pills. https://www.fda.gov/cosmetics/productsingredients/products/ucm134217.htm[↩][↩]
- https://www.accessdata.fda.gov/cms_ia/importalert_127.html[↩]
- Clinical review of canthaxanthin (‘tanning pills’). Am Pharm. 1993 Aug;NS33(8):44-6.[↩]