Contents
What is CRP test
C-reactive protein test is also called CRP test, is a general blood test that checks for infection or inflammation in the body. C-reactive protein (CRP) test is used to determine the severity of inflammation and to monitor whether you are responding to treatment. C-reactive protein (CRP) is an acute phase reactant, a protein made by the liver and released into the blood within a few hours after tissue injury, the start of an infection, or other cause of inflammation as well as following a heart attack, surgery, or trauma. Markedly increased C-reactive protein levels are observed, for example, after trauma or a heart attack (myocardial infarction), with active or uncontrolled autoimmune disorders, and with serious bacterial infections like sepsis. The level of CRP can jump as much as a thousand-fold in response to inflammatory conditions, and its rise in the blood can precede pain, fever, or other clinical indicators. Thus, C-reactive protein (CRP) is one of several proteins that are often referred to as acute phase reactants. The C-reactive protein test measures the amount of CRP in the blood and can be valuable in detecting inflammation due to acute conditions or in monitoring disease activity in chronic conditions. However, CRP blood test does not show where the inflammation is in your body. A more sensitive form of the C-reactive protein test is called the high-sensitivity C-reactive protein (hs-CRP), that is used to assess your risk of heart disease.
Key points
- Normal CRP value ranges may vary slightly among different laboratories. In normal healthy individuals, C-reactive protein (CRP) is a trace protein (≤8 mg/L or ≤5 mg/L). Generally, there are low levels of CRP detectable in the blood. The levels often increase slightly with age, female gender and in African Americans. Talk to your health care provider about the meaning of your specific CRP test results.
- Elevated values are consistent with an acute inflammatory process. After onset of an acute phase response, the serum CRP concentration rises rapidly (within 6-12 hours and peaks at 24-48 hours) and extensively. Concentrations above 100 mg/L are associated with severe stimuli such as major trauma and severe infection (sepsis).
- Measuring changes in the concentration of CRP provides useful diagnostic information about the level of acuity and severity of a disease. It also allows judgments about the disease genesis. Persistence of a high serum CRP concentration is usually a grave prognostic sign that generally indicates the presence of an uncontrolled infection.
- The CRP test is a general test to check for inflammation in the body. It is not a specific test. That means it can reveal that you have inflammation somewhere in your body, but it cannot pinpoint the exact location. The CRP test is often done with the ESR or sedimentation rate test which also looks for inflammation.
- C-reactive protein (CRP) response may be less pronounced in patients suffering from liver disease.
- A low CRP level does not always mean that there is no inflammation present. Levels of CRP may not be increased in people with rheumatoid arthritis and lupus. The reason for this is unknown.
- Elevated CRP values are nonspecific and should not be interpreted without a complete clinical history.
The CRP test is not diagnostic, but it provides information to a health practitioner as to whether inflammation is present. This information can be used in conjunction with other factors such as signs and symptoms, physical exam, and other tests to determine if someone has an acute inflammatory condition or is experiencing a flare-up of a chronic inflammatory disease. The health practitioner may then follow up with further testing and treatment.
This standard CRP test is not to be confused with an high-sensitivity C-reactive protein (hs-CRP) test.
There are two different tests that measure C-reactive protein (CRP) and each test measures a different range of CRP level in the blood for different purposes:
- The standard C-reactive protein (CRP) test measures markedly high levels of the protein to detect diseases that cause significant inflammation. It measures CRP in the range from 10 to 1000 mg/L.
- The high-sensitivity C-reactive protein (hs-CRP) test accurately detects lower levels of the protein than the standard C-reactive protein (CRP) test and is used to evaluate individuals for risk of cardiovascular disease. It measures CRP in the range from 0.5 to 10 mg/L.
Since the high-sensitivity C-reactive protein (hs-CRP) and standard CRP tests measure the same protein, people with chronic inflammation, such as those with arthritis, should not have high-sensitivity C-reactive protein (hs-CRP) levels measured. Their CRP levels will already be very high due to the arthritis, so results of the high-sensitivity C-reactive protein (hs-CRP) test will not be meaningful.
Increased serum CRP is related to traditional cardiovascular risk factors and may reflect the role of these risk factors in causing vascular inflammation.
According to the American Heart Association, results of the high-sensitivity C-reactive protein (hs-CRP) in determining the risk for heart disease can be interpreted as follows:
- You are at low risk of developing cardiovascular disease if your hs-CRP level is lower than 1.0 mg/L.
- You are at average risk of developing cardiovascular disease if your hs-CRP levels are between 1.0 mg/L and 3.0 mg/L.
- You are at high risk for cardiovascular disease if your hs-CRP level is higher than 3.0 mg/L.
What is the difference between regular CRP and hs-CRP tests?
Both tests measure the same protein in the blood. The high-sensitivity C-reactive protein (hs-CRP) test is for apparently healthy people to determine their risk of cardiovascular disease. It measures CRP in the range from 0.5 to 10 mg/L. The C-reactive protein (CRP) test is ordered to evaluate people who have signs and symptoms of a serious bacterial infection or of a serious chronic inflammatory disease such as rheumatoid arthritis. It measures CRP in the range from 10 to 1000 mg/L.
What is a normal C-reactive protein level?
Normal CRP values vary from lab to lab. Generally, there are low levels of CRP detectable in the blood. The levels often increase slightly with age, female gender and in African Americans. In normal healthy individuals, C-reactive protein (CRP) is a trace protein (≤8 mg/L or ≤5 mg/L)
When to get CRP blood test?
When your healthcare provider suspects that you have an acute condition causing inflammation, such as a serious bacterial or fungal infection or when you are suffering from an inflammatory disorder such as arthritis, an autoimmune disorder, or inflammatory bowel disease
C-reactive protein test application
- Assessment of acute phase reaction in inflammatory, infective and neoplastic disorders (cancers);
- Monitoring disease activity, particularly in inflammatory arthritis;
- Monitoring patients after premature rupture of the membranes, for developing infection; and
- Assessment of risk factors for myocardial infarction [heart attack] with high-sensitivity C-reactive protein (hs-CRP). Marginally raised high-sensitivity C-reactive protein (hs-CRP), and values within the normal range, have been demonstrated to be an independent risk factor for coronary artery disease. However, the applicability of measuring serum CRP for screening in asymptomatic populations for coronary artery disease risk remains unclear.
What does an elevated C-reactive protein mean?
Elevation of C-reactive protein (CRP) indicates acute phase response or active disease in chronic inflammatory disorders. CRP is a more sensitive early indicator of an acute phase response than the ESR (erythrocyte sedimentation rate or sedimentation rate). C-reactive protein (CRP) also returns towards normal more rapidly with improvement or resolution of the disease process.
C-reactive protein (CRP) elevations are nonspecific and may be useful for the detection of systemic inflammatory processes; to assess treatment of bacterial infections with antibiotics; to detect intrauterine infections with concomitant premature rupture of membranes (PROM); to differentiate between active and inactive forms of disease with concurrent infection, e.g., in patients suffering from systemic lupus erythematosus (SLE) or ulcerative colitis; to therapeutically monitor rheumatic disease and assess anti-inflammatory therapy; to determine the presence of postoperative complications at an early stage, such as infected wounds, thrombosis, and pneumonia; and to distinguish between infection and bone marrow rejection. Postoperative monitoring of CRP levels of patients can aid in the recognition of unexpected complications (persisting high or increasing levels).
However, the C-reactive protein (CRP) test is less sensitive than the ESR (erythrocyte sedimentation rate or sedimentation rate) for some disorders, for example, ulcerative colitis and SLE (systemic lupus erythematosus).
In patients at risk for myocardial infarction (heart attack) and without other causes of an acute phase response, the presence of slightly elevated or even high normal high-sensitivity C-reactive protein (hs-CRP) indicates a greater risk of myocardial infarction. The use of high sensitivity CRP in clinical practice remains undecided.
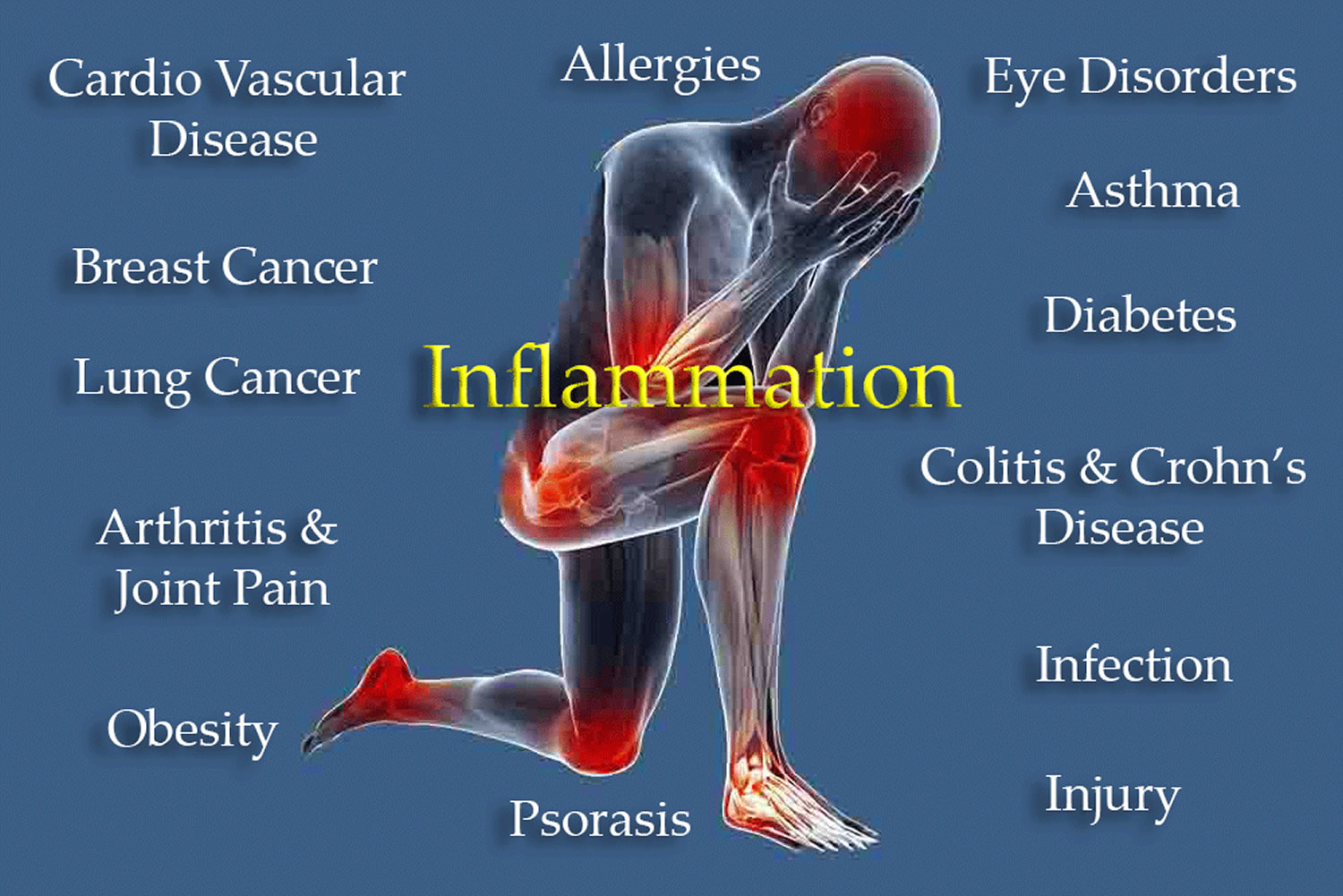
Elevated of C-reactive protein (CRP) test result means you have inflammation in the body. This may be due to a variety of conditions, including:
- Cancer
- Connective tissue disease
- Heart attack
- Infection
- Inflammatory bowel disease (IBD)
- Lupus or SLE (systemic lupus erythematosus)
- Pneumococcal pneumonia
- Rheumatoid arthritis
- Rheumatic fever
- Tuberculosis
Elevated of C-reactive protein (CRP) results also occur during the last half of pregnancy or with the use of birth control pills (oral contraceptives). Sometimes CRP is tested if a pregnant woman has ruptured her membranes (broken her waters) early (premature rupture of membrane or PROM). CRP can indicate if there are any problems with the baby.
This list is not all inclusive.
A high CRP indicates that there is inflammation or an infection somewhere in your body. Other tests might be necessary to find out where or which specific illness is causing it.
If you are being treated for an infection or inflammation, CRP levels should decrease.
You should discuss the results with your doctor to understand what they mean specifically for you.
C-reactive protein cardiac
High-sensitivity C-reactive protein (hs-CRP) is used to help assess your risk of developing cardiovascular disease. The high-sensitivity CRP test measures low levels of CRP in the blood to identify low levels of inflammation that are associated with risk of developing cardiovascular disease (CVD). However, there is no current consensus exists on when to get tested; high-sensitivity C-reactive protein (hs-CRP) is often ordered in conjunction with other tests that are performed to assess your risk of heart disease, such as a lipid profile (cholesterol, triglycerides, HDL-C “good” cholesterol, LDL-C “bad” cholesterol) when your healthcare provider would like additional information on your risk.
It is now believed that a persistent low level of inflammation plays a major role in atherosclerosis, the narrowing of blood vessels due to build-up of cholesterol and other lipids, which is often associated with cardiovascular disease.
Cardiovascular disease causes more deaths in the U.S. each year than any other cause, according to the American Heart Association. A number of risk factors, such as family history, high cholesterol, high blood pressure, being overweight or diabetic, have been linked to the development of cardiovascular disease, but a significant number of people who have few or no identified risk factors will also develop cardiovascular disease. This fact has lead researchers to look for additional risk factors that might be either causing cardiovascular disease or that could be used to determine lifestyle changes and/or treatments that could reduce a person’s risk.
High-sensitivity C-reactive protein (hs-CRP) is one of a growing number of cardiac risk markers that are used to help determine a person’s risk. Some studies have shown that measuring CRP with a highly sensitive assay can help identify the risk level for cardiovascular disease in apparently healthy people. This more sensitive test can measure CRP levels that are within the higher end of the reference range. These normal but slightly high levels of CRP in otherwise healthy individuals can predict the future risk of a heart attack, stroke, sudden cardiac death, and peripheral arterial disease, even when cholesterol levels are within an acceptable range.
High-sensitivity C-reactive protein (hs-CRP) test
A high-sensitivity C-reactive protein (hs-CRP) test may be used to help evaluate an individual for risk of cardiovascular disease (CVD). It may be used in combination with a lipid profile or with other cardiac risk markers, such as a lipoprotein-associated phospholipase A2 (Lp-PLA2) test, to provide added information about heart disease risk.
CRP is a protein that increases in the blood with inflammation. Studies have suggested that a persistent low level of inflammation plays a major role in atherosclerosis, the narrowing of blood vessels due to build-up of cholesterol and other lipids, which is often associated with cardiovascular disease. The hs-CRP test accurately measures low levels of C-reactive protein to identify low but persistent levels of inflammation and thus helps predict a person’s risk of developing cardiovascular disease.
High-sensitivity C-reactive protein (hs-CRP) is thought by some experts to be a useful test for determining risk of cardiovascular disease, heart attacks, and strokes and that high-sensitivity C-reactive protein (hs-CRP) can play a role in the evaluation process before a person develops one of these health problems. Some say that the best way to predict risk is to combine a good marker for inflammation, like high-sensitivity C-reactive protein (hs-CRP), with the lipid profile. Several groups have recommended that this test be used for people who have a moderate risk of heart attack over the next 10 years.
However, not all health professionals agree on hs-CRP’s usefulness. Clinical trials that involve measuring high-sensitivity C-reactive protein (hs-CRP) levels are currently underway in an effort to better understand its role in cardiovascular events. These studies will help to form and refine guidelines on its use in screening and treatment decisions.
When is high-sensitivity C-reactive protein (hs-CRP) ordered?
Currently, there is no consensus on when to get tested, though some guidelines include recommendations on hs-CRP testing. For example, a guideline from the American College of Cardiology Foundations and the American Heart Association says that hs-CRP testing may be useful when men 50 years old or younger and women 60 years old or younger have intermediate risk. It also may be useful for treatment decisions when men and women are older than these respective ages and have LDL-C less than 130 mg/L and meet several other criteria, such as no existing heart disease, diabetes, kidney disease, or inflammatory conditions.
When hs-CRP is evaluated, it may be repeated to confirm that a person has persistent low levels of inflammation.
Is high-sensitivity C-reactive protein (hs-CRP) specific for predicting heart disease?
No. C-reactive protein (CRP) is a marker of inflammation, a process that can affect a number of organ systems. Most studies to date have focused on heart disease, but new research shows that having C-reactive protein (CRP) in the high normal range may also be associated with other diseases such as colon cancer, complications of diabetes, and obesity. Furthermore, experts still don’t agree on when and how often the high-sensitivity C-reactive protein (hs-CRP) test should be ordered. As more clinical studies are completed that support its utility, high-sensitivity C-reactive protein (hs-CRP) test may be more frequently ordered.
High-sensitivity C-reactive protein (hs-CRP) test preparation requirement
No test preparation is needed; however, fasting for 9-12 hours before the blood sample is taken may be required if a lipid profile (including triglycerides) is to be done at the same time. In addition, the person being tested should be healthy at the time of the sample collection, without any recent illnesses, infections, inflammation, or injuries. A blood sample is drawn by needle from a vein in the arm.
Taking nonsteroidal anti-inflammatory drugs (NSAIDs, e.g., aspirin, ibuprofen, and naproxen) or statins may reduce C-reactive protein (CRP) levels in blood. Both anti-inflammatory drugs and statins may help to reduce inflammation, thus reducing CRP.
It is important that any person having this test be in a healthy state for the results to be of value in predicting the risk of coronary disease or heart attack. Any recent illness, tissue injury, infection, or other general inflammation will raise the amount of C-reactive protein (CRP) and give a falsely elevated estimate of risk.
Women on hormone replacement therapy have been shown to have elevated high-sensitivity C-reactive protein (hs-CRP) levels.
Since the high-sensitivity C-reactive protein (hs-CRP) and standard CRP tests measure the same protein, people with chronic inflammation, such as those with arthritis, should not have high-sensitivity C-reactive protein (hs-CRP) levels measured. Their CRP levels will already be very high due to the arthritis, so results of the high-sensitivity C-reactive protein (hs-CRP) test will not be meaningful.
What does the high-sensitivity C-reactive protein (hs-CRP) test result mean?
Relatively high levels of high-sensitivity C-reactive protein (hs-CRP) in otherwise healthy individuals have been found to be predictive of an increased risk of a future heart attack, stroke, sudden cardiac death, and/or peripheral arterial disease, even when cholesterol levels are within an acceptable range.
People with higher high-sensitivity C-reactive protein (hs-CRP) values have the highest risk of cardiovascular disease and those with lower values have less risk. Specifically, individuals who have high-sensitivity C-reactive protein (hs-CRP) results at the high end of the normal range have 1.5 to 4 times the risk of having a heart attack as those with high-sensitivity C-reactive protein (hs-CRP) values at the low end of the normal range.
The American Heart Association and U.S. Centers for Disease Control and Prevention have defined risk groups as follows:
- Low risk of developing cardiovascular disease: if your hs-CRP level is less than 1.0 mg/L
- Average risk of developing cardiovascular disease: if your hs-CRP level is between 1.0 to 3.0 mg/L
- High risk for cardiovascular disease: if your hs-CRP level is above 3.0 mg/L
These values are only a part of the total evaluation process for cardiovascular diseases. Additional risk factors to be considered are elevated levels of cholesterol, LDL-C “bad” cholesterol, triglycerides, and glucose. In addition, smoking, high blood pressure (hypertension), and diabetes also increase the risk level.