Contents
What is a CT scan
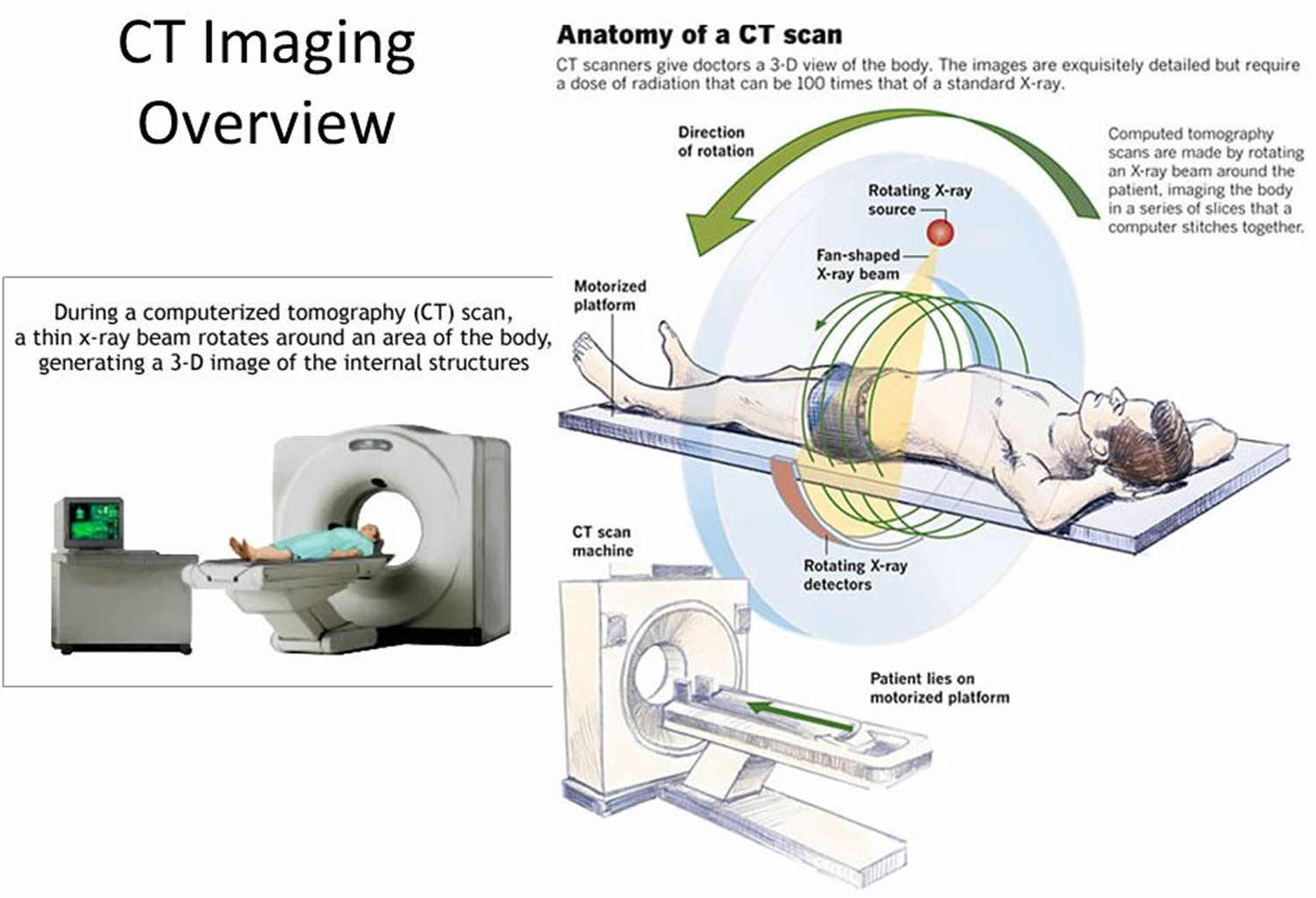
Computed tomography (CT) scan, also known as computerized axial tomography (CAT) scan, is a diagnostic imaging procedure that uses X-rays to build cross-sectional images (“slices”) of your body, like the slices in a loaf of bread. The entire series of pictures produced in CT is like a loaf of sliced bread—you can look at each slice individually (2-dimensional pictures) or you can look at the whole loaf (a 3-dimensional picture). Computer programs are used to create both types of pictures. The origin of the word “tomography” is from the Greek word “tomos” meaning “slice” or “section” and “graphe” meaning “drawing.” The cross-sectional images (see Figure 2) are used for a variety of diagnostic and therapeutic purposes. Compared to most other diagnostic X-ray procedures, CT scans result in relatively high radiation exposure. The risks associated with such exposure are greatly outweighed by the benefits of diagnostic and therapeutic CT scans. A CT scan has many uses, but it’s particularly well-suited to quickly examine people who may have internal injuries from car accidents or other types of trauma. A CT scan can be used to visualize nearly all parts of the body and is used to diagnose disease or injury as well as to plan medical, surgical or radiation treatment.
The use of CT scans in the US has reportedly tripled since 1993 to its present level of about 70 million scans per year 1. This sharp increase has been driven largely by advances in CT technology that make it extremely user-friendly, for both the patient and the physician.
During a CT scan, you lie still on a table. The table slowly passes through the center of a large X-ray machine – the emitter of x-rays rotates around the patient and the detector, placed in diametrically opposite side, picks up the image of a body section (beam and detector move in synchrony). The test is painless. During some tests you receive a contrast dye, which makes parts of your body show up better in the image.
CT scan is based on the fundamental principle that the density of the tissue passed by the X-ray beam can be measured from the calculation of the attenuation coefficient that is dependent on the amount of x rays absorbed in a particular tissue such as muscle or lung. Using this principle, CT scan allows the reconstruction of the density of your body, by two-dimensional section perpendicular to the axis of the acquisition system. In order to obtain tomographic images of the patient from the data in “raw” scan, the computer uses complex mathematical algorithms for 3-dimensional (3-D) image reconstruction of the bones, blood vessels and soft tissues inside your body. CT scan images provide more-detailed information than plain X-rays do. CT images are stored as electronic data files and are usually reviewed on a computer screen. A radiologist interprets these images and sends a report to your doctor.
Today most CT systems are capable of “spiral” (also called “helical”) scanning as well as scanning in the formerly more conventional “axial” mode. Helical CT has several advantages over older CT techniques: it is faster, produces better 3-D pictures of areas inside the body, and may detect small abnormalities better. The newest CT scanners, called multislice CT or multidetector CT scanners, allow more slices to be imaged in a shorter period of time. Such advances allow relatively larger volumes of anatomy to be imaged in relatively less time. Another advancement in the technology is electron beam CT, also known as EBCT. Although the principle of creating cross-sectional images is the same as for conventional CT, whether single- or multi-slice, the electron beam CT scanner does not require any moving parts to generate the individual “snapshots.” As a result, the electron beam CT scanner allows a quicker image acquisition than conventional CT scanners.
Concerns about CT scans include the risks from exposure to ionizing radiation (X-rays) and possible reactions to the intravenous contrast agent, or dye, which may be used to improve visualization. The exposure to ionizing radiation (X-rays) may cause a small increase in a person’s lifetime risk of developing cancer. Exposure to ionizing radiation (X-rays) is of particular concern in pediatric patients because the cancer risk per unit dose of ionizing radiation is higher for younger patients than adults, and younger patients have a longer lifetime for the effects of radiation exposure to manifest as cancer.
However, in children and adults, the risk from a medically necessary imaging exam is quite small when compared to the benefit of accurate diagnosis or intervention. It is especially important to make sure that CT scans in children are performed with appropriate exposure factors, as use of exposure settings designed for adults can result in a larger radiation dose than necessary to produce a useful image for a pediatric patient.
If a physician recommends a CT scan for you or your child, the U.S. Food and Drug Administration (FDA) encourages you to discuss the benefits and risks of the CT scan, as well as any past X-ray procedures you or your child have had, with your physician. A CT scan should always be performed if it is medically necessary and other exams using no or less radiation are unsuitable. At this time, the FDA does not see a benefit to whole-body scanning of individuals without symptoms.
Are CT scans safe?
Medical imaging exams — including computerized tomography (CT) scans — have been directly linked to greater life expectancy and declining cancer death rates. Medical imaging exams are also generally less expensive and safer than invasive procedures, such as exploratory surgery.
Like other X-ray imaging exams, CT scans expose you briefly to a small, targeted amount of ionizing radiation, which helps create an image of structures inside your body. CT scans provide more-detailed images of more types of tissue than traditional X-rays do, which allows your doctor to detect and locate many medical conditions.
CT scans have various purposes. They include helping to diagnose a condition, guiding medical procedures, such as needle biopsies, and monitoring the effectiveness of certain treatments, such as cancer treatments.
At the low doses of radiation a CT scan uses, your risk of developing cancer from it is so small that it can’t be reliably measured. Because of the possibility of an increased risk, however, the American College of Radiology advises that no imaging exam be done unless there is a clear medical benefit.
Doctors are encouraged to use the minimal radiation necessary when performing imaging exams. If your doctor recommends a CT scan, ask about the potential benefits to your health, which generally greatly outweigh any small potential risk from radiation.
How a CT scan works
During a CT procedure, the person lies very still on a table, and the table passes slowly through the center of a large x-ray machine. With some types of CT scanners, the table stays still and the machine moves around the person. The person might hear whirring sounds during the procedure. At times during a CT procedure, the person may be asked to hold their breath to prevent blurring of the images.
Sometimes, CT involves the use of a contrast (imaging) agent, or “dye.” The dye may be given by mouth, injected into a vein, given by enema, or given in all three ways before the procedure. The contrast dye highlights specific areas inside the body, resulting in clearer pictures. Iodine and barium are two dyes commonly used in CT.
In very rare cases, the contrast agents used in CT can cause allergic reactions. Some people experience mild itching or hives (small bumps on the skin). Symptoms of a more serious allergic reaction include shortness of breath and swelling of the throat or other parts of the body. People should tell the technologist immediately if they experience any of these symptoms, so they can be treated promptly. Very rarely, the contrast agents used in CT can also cause kidney problems in certain patients. These kidney problems usually do not have any symptoms, but they can be detected by running a simple test on a blood sample.
CT does not cause any pain. However, lying in one position during the procedure may be slightly uncomfortable. The length of a CT procedure depends on the size of the area being scanned, but it usually lasts only a few minutes to half an hour. For most people, the CT is performed on an outpatient basis at a hospital or a radiology center, without an overnight hospital stay.
Some people are concerned about experiencing claustrophobia during a CT procedure. However, most CT scanners surround only portions of the body, not the whole body. Therefore, people are not enclosed in a machine and are unlikely to feel claustrophobic.
Women should let their health care provider and the technologist know if there is any possibility that they are pregnant, because radiation from CT can harm a growing fetus.
- A motorized table moves the patient (Figures 1 and 2) through a circular opening in the CT imaging system.
- As the patient passes through the CT imaging system, a source of x rays rotates around the inside of the circular opening. A single rotation takes about 1 second. The x-ray source produces a narrow, fan-shaped beam of x rays used to irradiate a section of the patient’s body (Figure 2). The thickness of the fan beam may be as small as 1 millimeter or as large as 10 millimeters. In typical examinations there are several phases; each made up of 10 to 50 rotations of the x-ray tube around the patient in coordination with the table moving through the circular opening. The patient may receive an injection of a “contrast material” to facilitate visualization of vascular structure.
- Detectors in rows opposite the X-ray source (the exit side of the patient) register the X-rays that pass through the patient’s body as a “snapshot” at one position (angle) of the source of x rays in the process of creating an image. Many different “snapshots” (at many angles through the patient) are collected during one complete rotation.
- The data are sent to a computer to reconstruct all of the individual “snapshots” into a cross-sectional image (slice) of the internal organs and tissues for each complete rotation of the source of x rays.
- CT images of internal organs, bones, soft tissue, and blood vessels provide greater clarity and more details than conventional X-ray images, such as a brain X-Ray.
What is combined PET/CT?
Combined PET/CT uses two imaging methods, CT and positron emission tomography (PET), in one procedure. CT scan is done first to create anatomic pictures of the organs and structures in the body, and then PET is done to create colored pictures that show chemical or other functional changes in tissues.
Different types of positron-emitting (radioactive) substances can be used in PET. Depending on the substance used, different kinds of chemical or functional changes can be imaged. The most common type of positron emission tomography (PET) procedure uses an imaging agent called FDG [2-deoxy-2-(18F)fluoro-D-glucose] (a radioactive form of the sugar glucose), which shows the metabolic activity of tissues. Because cancerous tumors are usually more metabolically active than normal tissues, they appear different from other tissues on a PET scan. Other PET imaging agents can provide information about the level of oxygen in a particular tissue, the formation of new blood vessels, the presence of bone growth, or whether tumor cells are actively dividing and growing.
Combining CT scan and PET scan may provide a more complete picture of a tumor’s location and growth or spread than either test alone. The combined procedure may improve the ability to diagnose cancer, to determine how far a tumor has spread, to plan treatment, and to monitor response to treatment. Combined PET/CT may also reduce the number of additional imaging tests and other procedures a patient needs.
Figure 1. CT scan machine
Common Types of CT Scans
CT scan use can be categorized according to the population of patients (adult or pediatric) and the purpose of imaging (diagnosis in symptomatic patients or screening of asymptomatic patients) 2. CT-based diagnosis in adults is the largest of these categories. About half of diagnostic CT examinations in adults are scans of the body, and about one third are scans of the head, with about 75% obtained in a hospital setting and 25% in a single-specialty practice setting 3. The largest increases in CT use, however, have been in the categories of pediatric diagnosis 4, 5 and adult screening 6 and these trends can be expected to continue for the next few years.
The growth of CT use in children has been driven primarily by the decrease in the time needed to perform a scan — now less than 1 second — largely eliminating the need for anesthesia to prevent the child from moving during image acquisition 4. The major growth area in CT use for children has been presurgical diagnosis of appendicitis, for which CT appears to be both accurate and cost-effective — though arguably no more so than ultrasonography in most cases 7. Estimates of the proportion of CT studies that are currently performed in children range between 6% and 11% 8.
A large part of the projected increase in CT scanning for adults will probably come from new CT-based screening programs for asymptomatic patients. The four areas attracting the most interest are CT colonography (virtual colonoscopy) 6, CT lung screening for current and former smokers 9, CT cardiac screening 10 and CT whole-body screening 11.
What is total, or whole-body, CT scan?
Total, or whole-body, CT scan creates pictures of nearly every area of the body—from the chin to below the hips. This procedure, which is used routinely in patients who already have cancer, can also be used in people who do not have any symptoms of disease. However, whole-body CT scan has not been shown to be an effective screening method for healthy people. Most abnormal findings from this procedure do not indicate a serious health problem, but the tests that must be done to follow up and rule out a problem can be expensive, inconvenient, and uncomfortable. In addition, whole-body CT scan can expose people to relatively large amounts of ionizing radiation—about 12 mSv, or four times the estimated average annual dose received from natural sources of radiation. Most doctors recommend against whole-body CT scan for people without any signs or symptoms of disease.
What is a CT scan used for?
In addition to its use in cancer, CT is widely used to help diagnose circulatory (blood) system diseases and conditions, such as coronary artery disease (atherosclerosis), blood vessel aneurysms, and blood clots; spinal conditions; kidney and bladder stones; abscesses; inflammatory diseases, such as ulcerative colitis and sinusitis; and injuries to the head, skeletal system, and internal organs. CT can be a life-saving tool for diagnosing illness and injury in both children and adults.
CT scans can be used to:
- Diagnose conditions – including damage to bones, injuries to internal organs, problems with blood flow, strokes and cancer
- Guide further tests or treatments – for example, CT scans can help to determine the location, size and shape of a tumour before having radiotherapy, or allow a doctor to take a needle biopsy (where a small tissue sample is removed using a needle) or drain an abscess
- Monitor conditions – including checking the size of tumours during and after cancer treatment.
CT scans wouldn’t normally be used to check for problems if you don’t have any symptoms (known as screening). This is because the benefits of screening may not outweigh the risks, particularly if it leads to unnecessary testing and anxiety.
Doctors use CT scans to look for:
- Diagnose muscle and bone disorders, such as bone tumors and fractures
- Pinpoint the location of a tumor, infection or blood clot
- Guide procedures such as surgery, biopsy and radiation therapy
- Detect and monitor diseases and conditions such as cancer, heart disease, lung nodules and liver masses
- Monitor the effectiveness of certain treatments, such as cancer treatment
- Detect internal injuries and internal bleeding
CT scan is used in cancer in many different ways:
- To detect abnormal growths
- To help diagnose the presence of a tumor
- To provide information about the stage of a cancer
- To determine exactly where to perform (i.e., guide) a biopsy procedure
- To guide certain local treatments, such as cryotherapy, radiofrequency ablation, and the implantation of radioactive seeds
- To help plan external-beam radiation therapy or surgery
- To determine whether a cancer is responding to treatment
- To detect recurrence of a tumor
Studies have shown that CT scan can be effective in both colorectal cancer screening (including screening for large polyps) and lung cancer screening.
CT scan side effects
When used appropriately, the benefits of a CT scan far exceed the risks. CT scans can provide detailed information to diagnose, plan treatment for, and evaluate many conditions in adults and children. Additionally, the detailed images provided by CT scans may eliminate the need for exploratory surgery.
Radiation exposure
During a CT scan, you’re briefly exposed to ionizing radiation (X-rays). The amount of radiation is greater than you would get during a plain X-ray because the CT scan gathers more-detailed information. The low doses of radiation used in CT scans have not been shown to cause long-term harm, although at much higher doses, there may be a small increase in your potential risk of cancer.
CT scans have many benefits that outweigh any small potential risk. Doctors use the lowest dose of X-ray radiation possible to obtain the needed medical information. Also, newer, faster machines and techniques require less radiation than was previously used. Talk with your doctor about the benefits and risks of your CT scan.
Harm to unborn babies
Tell your doctor if you’re pregnant. Although the X-ray radiation from a CT scan is unlikely to injure your baby, your doctor may recommend another type of exam, such as ultrasound or MRI, to avoid exposing your baby to radiation. At the low doses of radiation used in CT imaging, no negative effects have been observed in humans.
Reactions to contrast material
In certain cases, your doctor may recommend that you receive a special dye called contrast material. This can be something that you are asked to drink before your CT scan, or something that is given through a vein in your arm or inserted into your rectum. Although rare, the contrast material can cause medical problems or allergic reactions.
Most reactions are mild and result in a rash or itchiness. In rare instances, an allergic reaction can be serious, even life-threatening. Tell your doctor if you’ve ever had a reaction to contrast material.
Is the radiation from CT scan harmful?
Some people may be concerned about the amount of radiation they receive during a CAT scan. CT imaging involves the use of x-rays, which are a form of ionizing radiation. Exposure to ionizing radiation is known to increase the risk of cancer. Standard x-ray procedures, such as routine chest x-rays and mammography, use relatively low levels of ionizing radiation. The radiation exposure from CT scan is higher than that from standard x-ray procedures, but the increase in cancer risk from one CT scan is still small. Not having the procedure can be much more risky than having it, especially if CT scan is being used to diagnose cancer or another serious condition in someone who has signs or symptoms of disease.
It is commonly thought that the extra risk of any one person developing a fatal cancer from a typical CT scan procedure is about 1 in 2,000 12. In contrast, the lifetime risk of dying from cancer in the U.S. population is about 1 in 5 13.
It is also important to note that everyone is exposed to some background level of naturally occurring ionizing radiation every day. The average person in the United States receives an estimated effective dose of about 3 millisieverts (mSv) per year from naturally occurring radioactive materials, such as radon and radiation from outer space (1). By comparison, the radiation exposure from one low-dose CT scan of the chest (1.5 mSv) is comparable to 6 months of natural background radiation, and a regular-dose CT scan of the chest (7 mSv) is comparable to 2 years of natural background radiation (1).
The widespread use of CT and other procedures that use ionizing radiation to create images of the body has raised concerns that even small increases in cancer risk could lead to large numbers of future cancers (4, 5). People who have CT procedures as children may be at higher risk because children are more sensitive to radiation and have a longer life expectancy than adults. Women are at a somewhat higher risk than men of developing cancer after receiving the same radiation exposures at the same ages (6).
People considering CT should talk with their doctors about whether the procedure is necessary for them and about its risks and benefits. Some organizations recommend that people keep a record of the imaging examinations they have received in case their doctors don’t have access to all of their health records.
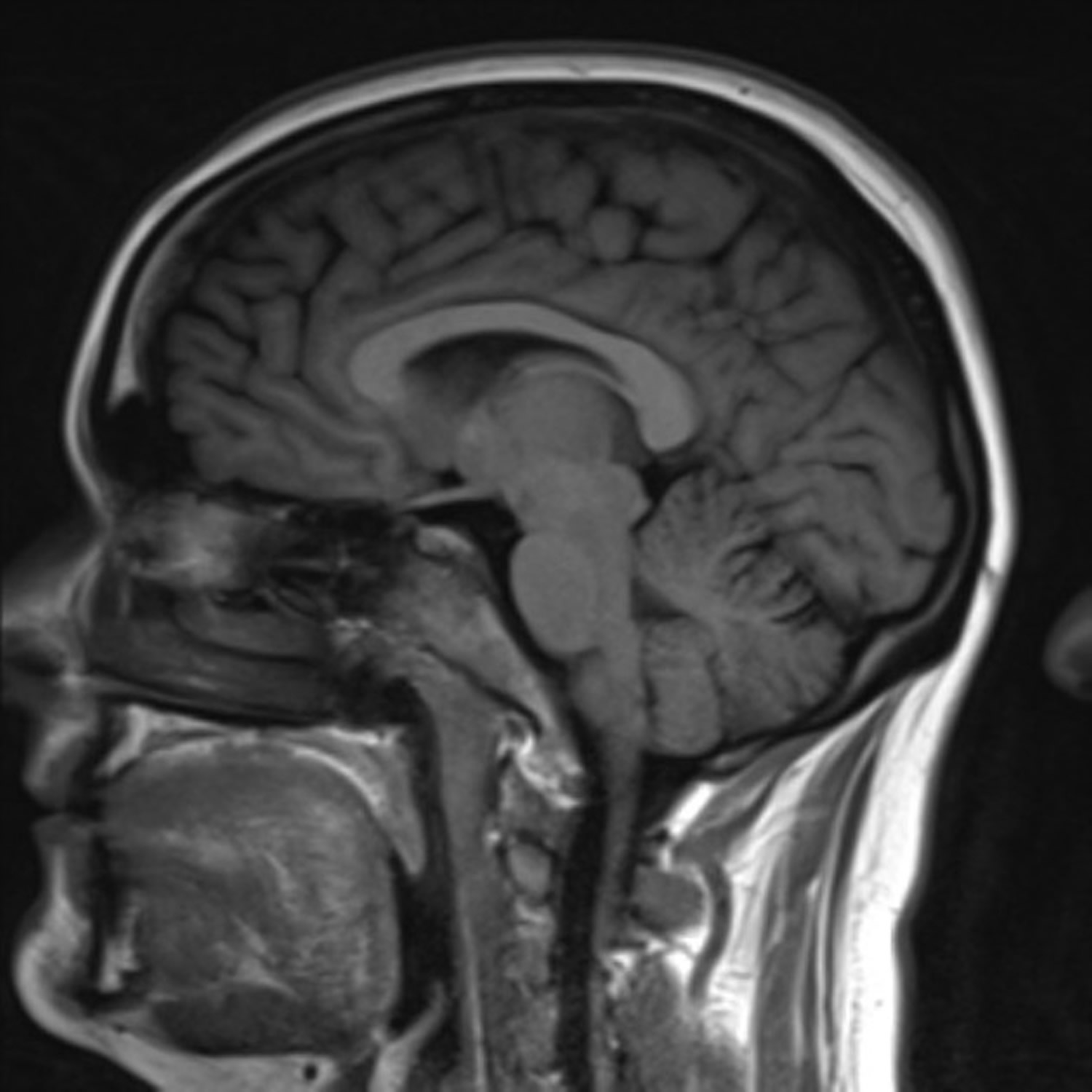
Figure 3. CT scan brain (normal)
Radiation Dose from CAT Scans
The quantity most relevant for assessing the risk of cancer detriment from a CAT scan procedure is the “effective dose”. The unit of measurement for effective dose is millisieverts (abbreviated mSv). Effective dose allows for comparison of the risk estimates associated with partial or whole-body radiation exposures. It also incorporates the different radiation sensitivities of the various organs in the body.
Radiation dose from CT scan procedures varies from patient to patient. The particular radiation dose will depend on the size of the body part examined, the type of procedure, and the type of CAT equipment and its operation. Typical values cited for radiation dose should be considered as estimates that cannot be precisely associated with any individual patient, examination, or type of CT system. The actual dose from a procedure could be two or three times larger or smaller than the estimates. Facilities performing “screening” procedures may adjust the radiation dose used to levels less (by factors such as 1/2 to 1/5 for so called “low dose CT scans”) than those typically used for diagnostic CT procedures. However, no comprehensive data is available to permit estimation of the extent of this practice and reducing the dose can have an adverse impact on the image quality produced. Such reduced image quality may be acceptable in certain imaging applications.
Estimates of the effective dose from a diagnostic CT procedure can vary by a factor of 10 or more depending on the type of CT procedure, patient size and the CT system and its operating technique. A list of representative diagnostic procedures and associated doses are given in Table 1.
Organ doses from CT scanning are considerably larger than those from corresponding conventional radiography (Table 1). For example, a conventional anterior–posterior abdominal x-ray examination results in a dose to the stomach of approximately 0.25 mGy, which is at least 32 times smaller than the corresponding stomach dose from an abdominal CT scan.
Table 1 – Radiation Dose Comparisons
| Diagnostic Procedure | Typical Effective Dose (mSv) |
|---|---|
| Chest x-ray (PA film) | 0.02 |
| Lumbar spine | 1.5 |
| I.V. urogram | 3 |
| Upper G.I. exam | 6 |
| Barium enema | 8 |
| CT scan head | 2 |
| CT scan chest | 7 |
| CT scan abdomen | 8 |
| Coronary artery calcification CT scan | 3 |
| Coronary CT angiogram | 16 |
Note: The radiation dose, a measure of ionizing energy absorbed per unit mass, is expressed in grays (Gy) or milligrays (mGy); 1 Gray (1 Gy) = 1 joule per kilogram. The radiation dose is often expressed as an equivalent dose in sieverts (Sv) or millisieverts (mSv). For x-ray radiation, which is the type used in CT scanners, 1 mSV = 1 mGy
[Source 14]The radiation doses to particular organs from any given CT study depend on a number of factors. The most important are the number of scans, the tube current and scanning time in milliamp-seconds (mAs), the size of the patient, the axial scan range, the scan pitch (the degree of overlap between adjacent CT slices), the tube voltage in the kilovolt peaks (kVp), and the specific design of the scanner being used 15. Many of these factors are under the control of the radiologist or radiology technician. Ideally, they should be tailored to the type of study being performed and to the size of the particular patient, a practice that is increasing but is by no means universal 16. It is always the case that the relative noise in CT images will increase as the radiation dose decreases, which means that there will always be a tradeoff between the need for low-noise images and the desirability of using low doses of radiation 17.
Biologic Effects of Low Doses of Ionizing Radiation
Ionizing radiation, such as x-rays, is uniquely energetic enough to overcome the binding energy of the electrons orbiting atoms and molecules; thus, these radiations can knock electrons out of their orbits, thereby creating ions. In biologic material exposed to x-rays, the most common scenario is the creation of hydroxyl radicals from x-ray interactions with water molecules; these radicals in turn interact with nearby DNA to cause strand breaks or base damage. X-rays can also ionize DNA directly. Most radiation-induced damage is rapidly repaired by various systems within the cell, but DNA double-strand breaks are less easily repaired, and occasional misrepair can lead to induction of point mutations, chromosomal translocations, and gene fusions, all of which are linked to the induction of cancer 18.
Risks Associated with Low Doses of Radiation
Depending on the machine settings, the organ being studied typically receives a radiation dose in the range of 15 millisieverts (mSv) (in an adult) to 30 mSv (in a neonate) for a single CT scan, with an average of two to three CT scans per study. At these doses, the most likely (though small) risk is for radiation-induced carcinogenesis 19.
Most of the quantitative information that scientists have regarding the risks of radiation-induced cancer comes from studies of survivors of the atomic bombs dropped on Japan in 1945 20. Data from cohorts of these survivors are generally used as the basis for predicting radiation-related risks in a population because the cohorts are large and have been intensively studied over a period of many decades, they were not selected for disease, all age groups are covered, and a substantial subcohort of about 25,000 survivors 21 received radiation doses similar to those of concern — that is, less than 50 mSv. Of course, the survivors of the atomic bombs were exposed to a fairly uniform dose of radiation throughout the body, whereas CT scan involves highly nonuniform exposure, but there is little evidence that the risks for a specific organ are substantially influenced by exposure of other organs to radiation.
There was a significant increase in the overall risk of cancer in the subgroup of atomic-bomb survivors who received low doses of radiation, ranging from 5 to 150 mSv 22; the mean dose in this subgroup was about 40 mSv, which approximates the relevant organ dose from a typical CT scan study involving two or three scans in an adult.
Although most of the quantitative estimates of the radiation-induced cancer risk are derived from analyses of atomic-bomb survivors, there are other supporting studies, including a recent large-scale study of 400,000 radiation workers in the nuclear industry 23 who were exposed to an average dose of approximately 20 mSv (a typical organ dose from a single CT scan for an adult). A significant association was reported between the radiation dose and mortality from cancer in this cohort (with a significant increase in the risk of cancer among workers who received doses between 5 and 150 mSv); the risks were quantitatively consistent with those reported for atomic-bomb survivors.
The situation is even clearer for children, who are at greater risk than adults from a given dose of radiation, both because they are inherently more radiosensitive and because they have more remaining years of life during which a radiation-induced cancer could develop.
In summary, there is direct evidence from epidemiologic studies that the organ doses corresponding to a common CT study (two or three scans, resulting in a dose in the range of 30 to 90 mSv) result in an increased risk of cancer. The evidence is reasonably convincing for adults and very convincing for children.
Risk Estimates
The effective doses from diagnostic CT scan procedures are typically estimated to be in the range of 1 to 10 mSv. This range is not much less than the lowest doses of 5 to 20 mSv estimated to have been received by some of the Japanese survivors of the atomic bombs. These survivors, who are estimated to have experienced doses slightly larger than those encountered in CT, have demonstrated a small but increased radiation-related excess relative risk for cancer mortality.
The risk of developing cancer as a result of exposure to radiation depends on the part of the body exposed, the individual’s age at exposure, and the individual’s gender. For the purpose of radiation protection, a conservative approach that is generally used is to assume that the risk for adverse health effects from cancer is proportional to the amount of radiation dose absorbed and that there is no amount of radiation that is completely without risk. This conservative approach is called the “linear non-threshold” model. The amount of dose depends on the type of x-ray examination. A CT examination with an effective dose of 10 millisieverts (abbreviated mSv; 1 mSv = 1 mGy in the case of x-rays.) may be associated with an increase in the possibility of fatal cancer of approximately 1 chance in 2000. This increase in the possibility of a fatal cancer from radiation can be compared to the natural incidence of fatal cancer in the U.S. population, about 1 chance in 5 (equal to 400 chances in 2000). In other words, for any one person the risk of radiation-induced cancer is much smaller than the natural risk of cancer. If you combine the natural risk of a fatal cancer and the estimated risk from a 10 mSv CT scan, the total risk may increase from 400 chances in 2000 to 401 chances in 2000. Nevertheless, this small increase in radiation-associated cancer risk for an individual can become a public health concern if large numbers of people undergo increased numbers of CT screening procedures of uncertain benefit.
There is considerable uncertainty regarding the risk estimates for low levels of radiation exposure as commonly experienced in diagnostic radiology procedures. This is because the risk is quite low compared to the natural risk of cancer. At low doses, the radiation-related excess risk, which is thought to be proportional to dose, tends to be dwarfed by statistical and other variation in the background risk level. To obtain adequate evidence for a statistically valid estimate of cancer risk from exposure to low doses of radiation would require studying millions of people for many years. There are some who question whether there is adequate evidence for a risk of cancer induction at low doses. Some scientists believe that low doses of radiation do not increase the risk of developing cancer at all, but this is a minority view.
A modelling study 1 estimated that, on average, 29,000 future cancers in the US could be related to CT scans performed in 2007. The largest contributors were calculated to be scans of the abdomen and pelvis (14,000 cancers), chest (4,100) and head (4,000), as well as scans where high-dose radiation was used 1. A third of the expected cancers were attributed to scans performed between the ages of 35 and 54 years, while 15% were attributed to scans in those under 18 years 1. Two-thirds of the CT-related cancers were expected to be in women, due to the larger number of CT scans carried out in women 1.
In the cross-sectional study 24, the average age of patients when scanned by CT was 59 years, and 48% of the patients were women. The 11 most common types of CT scan made up about 80% of all CTs performed. Radiation doses varied significantly between the different types of CT scan, with average doses ranging from 2 millisieverts (mSv) for a routine head CT to 31mSv for a multiphase abdomen and pelvis CT scan. Doses also varied within and between hospitals, with an average 13-fold variation between the highest and lowest dose for each scan type. The estimated number of CT scans that would lead to the development of a cancer varied depending on the type of CT and the patient’s age and sex.
It was estimated that one in 270 women who had CT coronary angiography (a fairly high-radiation-dose scan of the heart blood vessels) at the age of 40 would develop additional cancers from that CT scan (one in 600 men) compared with an estimated one in 8,100 extra women who had a routine CT scan of the head (one in 11,080 men) 24. Risk for developing cancer in later life was higher for a person scanned at a young age, and lower for a person scanned at 60 years.
The researchers in the modelling study 1 said that the findings highlight several areas of CT scan use that can make large contributions to the total cancer risk. They also said that risk reduction efforts may be necessary for people in certain age groups who receive the largest numbers of scans, and where high radiation doses are used.
The cross-sectional study 24 concludes that radiation doses used in commonly performed CT examinations are higher and more variable than generally thought, which they say highlights the need for greater standardization across hospitals.
The modelling study 1 provides a detailed estimate of the potential future cancer risks based on current age- and sex-specific CT use in people in the US. The following points should be remembered:
- These figures must be considered as estimates only. They are based on data from a variety of different sources, which may result in inaccuracies, particularly as they use risk estimates from a variety of populations exposed to radiation in different ways (for example Japanese atomic bomb survivors in the Biological Effects of lonizing Radiation (BEIR) report). In addition, the calculated lifetime attributable risks used in the studies should not be viewed as exact patient risks. Despite these limitations, however, they show the trend and give broad estimates of the extent of the risk from this type of radiation.
- The study calculates the possible development of new cancers, but can say nothing about the expected stage and severity of these cancers or their likely mortality.
- In the cross-sectional study 24, radiation doses varied considerably between the type of scan and hospital where it was carried out and, as the researchers say, these may not be the standard doses used. The study did not investigate the specific indications for the choice of dose.
It should be emphasized that the risk to individuals who have had CT scans is likely to be very small. The issue these studies are calling attention to is that when more people are exposed to radiation from CT scans, their collective risk becomes higher. As a result, more cases of cancer can be expected to occur. This is an important area of further investigation, as reducing unnecessary CAT scans has the potential to reduce population risk and cancer numbers.
Doctors should always weigh the risk of radiation exposure from a scan against its benefits. That is, they should ensure that the scan is necessary and that radiological investigations are only performed when the findings have definite diagnostic and treatment implications.
Radiation Risks from CT scan in Children
Major national and international organizations responsible for evaluating radiation risks agree that there probably is no low-dose radiation “threshold” for inducing cancers. In other words, no amount of radiation should be considered absolutely safe.
The first study to assess directly the risk of cancer after CT scans in childhood found a clear dose-response relationship for both leukemia and brain tumors: risk increased with increasing cumulative radiation dose. For a cumulative dose of between 50 and 60 milligray or mGy (mGy is a unit of estimated absorbed dose of ionizing radiation) to the head, the investigators reported a threefold increase in the risk of brain tumors; the same dose to bone marrow (the part of the body responsible for generating blood cells) resulted in a threefold increase in the risk of leukemia. For both findings, the comparison group consisted of individuals who had cumulative doses of less than 5 mGy to the relevant regions of the body.
The number of CT scans required to give a cumulative dose of 50-60mGy depends on the type of CT scan, the age of the patient, and the scanner settings. If typical current scanner settings are used for head CT in children, then two to three head CT scans would result in a dose of 50-60mGy to the brain. The same dose to the bone marrow would be produced by five to 10 head CT scans, using current scanner settings for children under age 15.
Previously, the potential cancer risk from CT scan use has been estimated using risk projection models derived primarily from studies of survivors of the atomic bomb explosions in Japan. The risks observed in the study described above were consistent with those previous estimates.
It is important to stress that the absolute cancer risks associated with CT scans are small. The lifetime risks of cancer due to CT scans, which have been estimated in the literature using projection models based on atomic bomb survivors, are about 1 case of cancer for every 1,000 people who are scanned, with a maximum incidence of about 1 case of cancer for every 500 people who are scanned.
The benefits of properly performed and clinically justified CT examinations should always outweigh the risks for an individual child; unnecessary exposure is associated with unnecessary risk. Minimizing radiation exposure from pediatric CT scan, whenever possible, will reduce the projected number of CT-related cancers.
CT scan as a Diagnostic Tool
CAT scan can be a life saving tool for diagnosing illness and injury in children. For an individual child, the risks of CT scan are small and the individual risk-benefit balance favors the benefit when used appropriately.
Approximately 5 to 9 million CT examinations are performed annually on children in the United States. The use of CT scan in adults and children has increased about eightfold since 1980, with annual growth estimated at about 10 percent per year. Much of this increase is due to its utility in common diseases, as well as to technical improvements.
Despite the many benefits of CT scan, a disadvantage is the inevitable radiation exposure. Although CT scans comprise up to about 12 percent of diagnostic radiological procedures in large U.S. hospitals, it is estimated that they account for approximately 49 percent of the U.S. population’s collective radiation dose from all medical x-ray examinations. CT is the largest contributor to medical radiation exposure among the U.S. population.
Unique Considerations for Radiation Exposure in Children
Radiation exposure is a concern in both adults and children. However, there are three unique considerations in children.
- Children are considerably more sensitive to radiation than adults, as demonstrated in epidemiologic studies of exposed populations.
- Children have a longer life expectancy than adults, resulting in a larger window of opportunity for expressing radiation damage.
- Children may receive a higher radiation dose than necessary if CT settings are not adjusted for their smaller body size.
As a result, the risk for developing a radiation-related cancer can be several times higher for a young child compared with an adult exposed to an identical CT scan.
In the last decade improvements in CT scanning equipment have allowed for better images at lower doses. The use of appropriate settings has also become much more widespread, resulting in reductions in doses for children. There is no need for higher doses in children, and appropriate settings should always be used.
Regardless of the lower doses, multiple scans to an individual patient present a particular concern. In addition, the use of more than one scan (that is, more than one contrast “phase”) during a single examination will further increase the radiation dose. In the vast majority of cases, a single scan should be sufficient during pediatric CT scan.
Immediate Measures to Minimize CT Radiation Exposure in Children
Physicians, other pediatric health care providers, CT technologists, CT manufacturers, and various medical and governmental organizations share the responsibility to minimize CT radiation doses to children. Several immediate steps can be taken to reduce the amount of radiation that children receive from CT examinations:
- Perform only necessary CT examinations. Communication between pediatric health care providers and radiologists can determine the need for CT and the technique to be used. There are standard indications for CT in children, and radiologists should review reasons prior to every pediatric scan and be available for consultation when indications are uncertain. When appropriate, other modalities such as ultrasound or magnetic resonance imaging (MRI), which do not use ionizing radiation, should be considered.
- Adjust exposure parameters for pediatric CT based on:
- Child size: guidelines based on individual size / weight parameters should be used.
- Region scanned: the region of the body scanned should be limited to the smallest necessary area.
- Organ systems scanned: lower mA and/or kVp settings should be considered for skeletal, lung imaging, and some CT angiographic and follow up examinations.
- Scan resolution: the highest quality images (i.e., those that require the most radiation) are not always required to make diagnoses. In many cases, lower-resolution scans are diagnostic. Providers should be familiar with the dose descriptors available on CT scanners and minimize the use of CT examinations that use multiple scans obtained during different phases of contrast enhancement (multiphase examinations). These multiphase examinations result in a considerable increase in dose and are rarely necessary, especially in body (chest and abdomen) imaging.
Summary
Although CT scan remains a crucial tool for pediatric diagnosis, it is important for the health care community to work together to minimize the radiation dose to children. Radiologists should continually think about reducing exposure as low as reasonably achievable by using exposure settings customized for children. All physicians who prescribe pediatric CT should continually assess its use on a case-by-case basis. Used prudently and optimally, CT is one of the most valuable imaging modalities for both children and adults.
CT scan prep
Depending on which part of your body is being scanned, you may be asked to:
- Take off some or all of your clothing and wear a hospital gown
- Remove metal objects, such as a belt, jewelry, dentures and eyeglasses, which might interfere with image results
- Refrain from eating or drinking for a few hours before your scan, to help ensure that clear images are taken.
You should let the CT clinic know if you’re pregnant. CT scans aren’t usually recommended for pregnant women unless it’s an emergency, as there’s a small chance the X-rays could harm your baby.
Tell the radiographer if you feel anxious or claustrophobic about having the scan. They can give you advice to help you feel calm and can arrange for you to have a sedative (medication to help you relax) if necessary.
Contrast material
Before having the scan, you may be given a special dye called a contrast to help improve the quality of the images. This may be swallowed in the form of a drink, passed into your bottom (enema), or injected into a blood vessel. The contrast material is needed for some CT scans to help highlight the areas of your body being examined. The contrast material blocks X-rays and appears white on images, which can help emphasize blood vessels, intestines or other structures.
Contrast material might be given to you:
- By mouth. If your esophagus or stomach is being scanned, you may need to swallow a liquid that contains contrast material. This drink may taste unpleasant.
- By injection. Contrast agents can be injected through a vein in your arm to help your gallbladder, urinary tract, liver or blood vessels stand out on the images. You may experience a feeling of warmth during the injection or a metallic taste in your mouth.
- By enema. A contrast material may be inserted in your rectum to help visualize your intestines. This procedure can make you feel bloated and uncomfortable.
Preparing your child for a scan
If your infant or toddler is having a CT scan, the doctor may recommend a sedative to keep your child calm and still. Movement blurs the images and may lead to inaccurate results. Ask your doctor how to prepare your child.
CT scan procedure
You can have a CT scan done in a hospital or an outpatient facility. CT scans are painless and, with newer machines, take only a few minutes. The whole procedure typically takes about 30 minutes.
Before the scan starts, you may be asked to remove your clothing and put on a gown. You’ll also be asked to remove anything metal, such as jewellery, as metal interferes with the scanning equipment.
The radiographer will operate the scanner from the next room. While the scan is taking place, you’ll be able to hear and speak to them through an intercom.
While each scan is taken, you’ll need to lie very still and breathe normally. This ensures that the scan images aren’t blurred. You may be asked to breathe in, breathe out, or hold your breath at certain points.
The scan will usually take around 10-20 minutes.
During the procedure
CT scanners are shaped like a large doughnut standing on its side. You lie on a narrow, motorized table that slides through the opening into a tunnel. Straps and pillows may be used to help you stay in position. During a head scan, the table may be fitted with a special cradle that holds your head still.
While the table moves you into the scanner, detectors and the X-ray tube rotate around you. Each rotation yields several images of thin slices of your body. You may hear buzzing and whirring noises.
A technologist in a separate room can see and hear you. You will be able to communicate with the technologist via intercom. The technologist may ask you to hold your breath at certain points to avoid blurring the images.
After the procedure
After the exam you can return to your normal routine. If you were given contrast material, you may receive special instructions. In some cases, you may be asked to wait for a short time before leaving to ensure that you feel well after the exam. After the scan, you’ll likely be told to drink lots of fluids to help your kidneys remove the contrast material from your body.
Your scan results won’t usually be available immediately. A computer will need to process the information from your scan, which will then be analysed by a radiologist (a specialist in interpreting images of the body).
After analyzing the images, the radiologist will write a report and send it to the doctor who referred you for the CT scan, so they can discuss the results with you. This normally takes a few days or weeks.
CT scan vs MRI
MRI is an abbreviation for Magnetic Resonance Imaging. MRI is an imaging modality that uses powerful magnets (strong magnetic fields and radio waves) to capture detailed images of soft tissue in your body. An MRI scanner consists of a large, powerful magnet in which the patient lies. A radio wave antenna is used to send signals to the body and then receive signals back. These returning signals are converted into images by a computer attached to the scanner. Imaging of almost any part of your body can be obtained in any plane. A magnetic resonance imaging (MRI) scan is a painless procedure that lasts 15 to 90 minutes, depending on the size of the area being scanned and the number of images being taken.
MRIs do not use radiation so they are safer for pregnant women and young children, but because the imaging is created with magnets, anyone who had metal implants should not get an MRI.
An MRI scan can be used to examine almost any part of the body, including the:
- brain and spinal cord
- bones and joints
- breasts
- heart and blood vessels
- internal organs, such as the liver, womb or prostate gland
The results of an MRI scan can be used to help diagnose conditions, plan treatments and assess how effective previous treatment has been.
CT scans are quicker than MRIs, taking five to ten minutes depending on the area being scanned. Because the imaging is faster, the CT scanner is less sensitive to a patient’s movements. A CT scanner is also quiet and open, making it an easier option for heavier people and those with claustrophobia. While CT scans are less expensive, they use radiation and therefore are not recommended for young children or pregnant women.
MRI was initially called Nuclear Magnetic Resonance Imaging (NMR) after its early use for chemical analysis. The “Nuclear” was dropped off about 25 years ago because of fears that people would think there was something radioactive involved, which there is not.
MRI was discovered simultaneously by two physicists, Felix Bloch and Edward Mills Purcell, just after the end of World War II. Bloch trained in quantum mechanics and was involved with atomic energy and then radar counter-measures. At the end of the war, he returned to his earlier work in the magnetic moment of the neutron. Purcell was involved with the development of microwave radar during the war then pursued radio waves for the evaluation of molecular and nuclear properties. They received the Nobel Prize in Physics in 1952 for this discovery.
MRI, the use of Nuclear Magnetic Resonance Imaging (NMR) to produce 2D images was accomplished by Paul Lauterbur, imaging water, and Sir Peter Mansfield who imaged the fingers of a research student, Dr Andrew Maudsley in 1976. Maudsley continues to make a significant contribution to MRI R&D today. Raymond Damadian obtained human images a year later in 1977. Lauterbur and Mansfield received the Nobel Prize in Physiology or Medicine in 2003 for their development of MRI.
Who can have MRI
Magnetic resonance imaging (MRI) is very safe and most people can have the procedure, including pregnant women and babies.
However, there are some instances where an MRI scan may not be recommended, because the strong magnets used during the scan can affect any metal implants or fragments in your body.
Before having an MRI scan, you should tell medical staff if:
- you think you have any metal in your body
- you’re pregnant or breastfeeding
There’s no evidence to suggest MRI scans pose a risk during pregnancy. However, as a precaution, MRI scans aren’t usually recommended during pregnancy, particularly in the first three months.
Metal implants or fragments
Having something metallic in your body doesn’t necessarily mean you can’t have an MRI scan, but it’s important for medical staff carrying out the scan to be aware of it.
They can decide on a case-by-case basis if there are any risks, or if further measures need to be taken to ensure the scan is as safe as possible. For example, it may be possible to make a pacemaker or defibrillator MRI-safe, or to monitor your heart rhythm during the procedure.
If you’re unsure about any metal fragments in your body, you may need an X-ray.
Some examples of metal implants or fragments include:
- a pacemaker – an electrical device used to control an irregular heartbeat
- an implantable cardioverter-defibrillator (ICD) – a similar device to a pacemaker that uses electrical shocks to regulate heartbeats
- metal plates, wires, screws or rods – used during surgery for bone fractures
- a nerve stimulator – an electrical implant used to treat long-term nerve pain
- a cochlear implant – a device similar to a hearing aid that’s surgically implanted inside the ear
- a drug pump implant – used to treat long-term pain by delivering painkilling medication directly to an area of the body, such as the lower back
- brain aneurysm clips – small metal clips used to seal blood vessels in the brain that would otherwise be at risk of rupturing (bursting)
- metallic fragments in or near your eyes or blood vessels (common in people who do welding or metalwork for a living)
- prosthetic (artificial) metal heart valves
- penile implants – used to treat erectile dysfunction (impotence)
- eye implants – such as small metal clips used to hold the retina in place
- an intrauterine device (IUD) – a contraceptive device made of plastic and copper that fits inside the womb
- artificial joints – such as those used for a hip replacement or knee replacement
- dental fillings and bridges
- tubal ligation clips – used in female sterilisation
- surgical clips or staples – used to close wounds after an operation
Tattoos
Some tattoo ink contains traces of metal, but most tattoos are safe in an MRI scanner. Tell the radiographer immediately if you feel any discomfort or heat in your tattoo during the scan.
MRI scan prep
On the day of your MRI scan, you should be able to eat, drink and take any medication as usual, unless advised otherwise.
In some cases, you may be asked not to eat or drink anything for up to four hours before the MRI scan, and sometimes you may be asked to drink a fairly large amount of water beforehand. This depends on the area being scanned.
When you arrive at the MRI center, you’ll usually be asked to fill in a questionnaire about your health and medical history. This helps the medical staff to ensure you have the scan safely.
Once you’ve completed the questionnaire, you’ll usually be asked to give your signed consent for the scan to go ahead.
As the MRI scanner produces strong magnetic fields, it’s important to remove any metal objects from your body, including:
- watches
- jewellery, such as earrings and necklaces
- piercings, such as ear, nipple and nose rings
- dentures (false teeth)
- hearing aids
- wigs (some wigs contain traces of metal)
Any valuables can usually be stored in a secure locker.
Depending on which part of your body is being scanned, you may need to wear a hospital gown during the procedure. If you do not need to wear a gown, you should wear clothes without metal zips, fasteners, buttons, underwire (bras), belts or buckles.
Contrast dye
Some MRI scans involve having an injection of contrast dye. This makes certain tissues and blood vessels show up more clearly and in greater detail.
It’s possible for contrast dye to cause tissue and organ damage in people with severe kidney disease. If you have a history of kidney disease, you may be given a blood test to determine how well your kidneys are functioning and whether it’s safe to proceed with the scan.
You should also let the staff know if you have a history of allergic reactions or any blood clotting problems before having the injection.
Anesthesia and sedatives
An MRI scan is a painless procedure, so anesthesia (painkilling medication) isn’t usually required. If you’re claustrophobic, you can ask for a mild sedative to help you relax – you should ask your doctor or consultant well in advance of having the scan.
If you decide to have a sedative during the MRI scan, you’ll need to arrange for a friend or family member to drive you home afterwards, as you won’t be able to drive for 24 hours.
General anaesthetic is often used when young children and babies have an MRI scan. This is because it’s very important to stay still during the scan, which young children and babies are often unable to do when they’re awake.
The MRI scanner will make loud tapping noises at certain times during the procedure. This is the electric current in the scanner coils being turned on and off. You’ll be given earplugs or headphones to wear.
You’re usually able to listen to music through headphones during the scan if you want to, and in some cases you can bring your own CD.
You’ll be moved out of the scanner when your scan is over.
How MRI scan is performed
An MRI scanner is a short cylinder that’s open at both ends. You’ll lie on a motorized bed that’s moved inside the scanner. You’ll enter the scanner either head first or feet first, depending on the part of your body being scanned.
In some cases, a frame may be placed over the body part being scanned, such as the head or chest. This frame contains receivers that pick up the signals sent out by your body during the scan and it can help to create a better-quality image.
While you’re having your scan, a friend or family member may be allowed to stay in the room with you. Children can usually have a parent with them. Anyone who stays with you will be asked whether they have a pacemaker or any other metal objects in their body. They’ll also have to follow the same guidelines regarding clothing and removing metallic objects.
During an MRI scan, you lie on a flat bed that’s moved into the scanner. Depending on the part of your body being scanned, you’ll be moved into the scanner either head first or feet first.
The MRI scanner is operated by a radiographer, who is trained in carrying out imaging investigations. They control the scanner using a computer, which is in a different room, to keep it away from the magnetic field generated by the scanner.
You’ll be able to talk to the radiographer through an intercom and they’ll be able to see you on a television monitor throughout the scan.
At certain times during the scan, the scanner will make loud tapping noises. This is the electric current in the scanner coils being turned on and off. You’ll be given earplugs or headphones to wear.
It’s very important to keep as still as possible during your MRI scan.
To avoid the images being blurred, it’s very important to keep the part of your body being scanned still throughout the whole of the scan until the radiographer tells you to relax.
A single scan may take from a few seconds to three or four minutes. You may be asked to hold your breath during short scans. Depending on the size of the area being scanned and how many images are taken, the whole procedure will take 15 to 90 minutes.
You’ll be moved out of the scanner when your scan is over.
After the MRI scan
An MRI scan is usually carried out as an outpatient procedure. This means you won’t need to stay in hospital overnight. After the scan, you can resume normal activities immediately.
However, if you’ve had a sedative, a friend or relative will need to take you home and stay with you for the first 24 hours. It’s not safe to drive, operate heavy machinery or drink alcohol for 24 hours after having a sedative.
Your MRI scan needs to be studied by a radiologist (a doctor trained in interpreting scans and X-rays) and possibly discussed with other specialists. This means it’s unlikely you’ll know the results of your scan immediately.
The radiologist will send a report to the doctor who arranged the scan, who will discuss the results with you. It usually takes a week or two for the results of an MRI scan to come through, unless they’re needed urgently.
MRI Advantages
The advantages of MRI include:
- The ability to image without the use of ionizing x-rays, in contradistinction to CT scanning
- Images may be acquired in multiple planes (axial, sagittal, coronal, or oblique) without repositioning the patient. CT images have only relatively recently been able to be reconstructed in multiple planes with the same spatial resolution
- MRI images demonstrate superior soft tissue contrast than CT scans and plain films making it the ideal examination of the brain, spine, joints and other soft tissue body parts
- Some angiographic (blood vessels) images can be obtained without the use of contrast material, unlike CT or conventional angiography
- Advanced techniques such as diffusion, spectroscopy and perfusion allow for precise tissue characterization rather than merely ‘macroscopic’ imaging
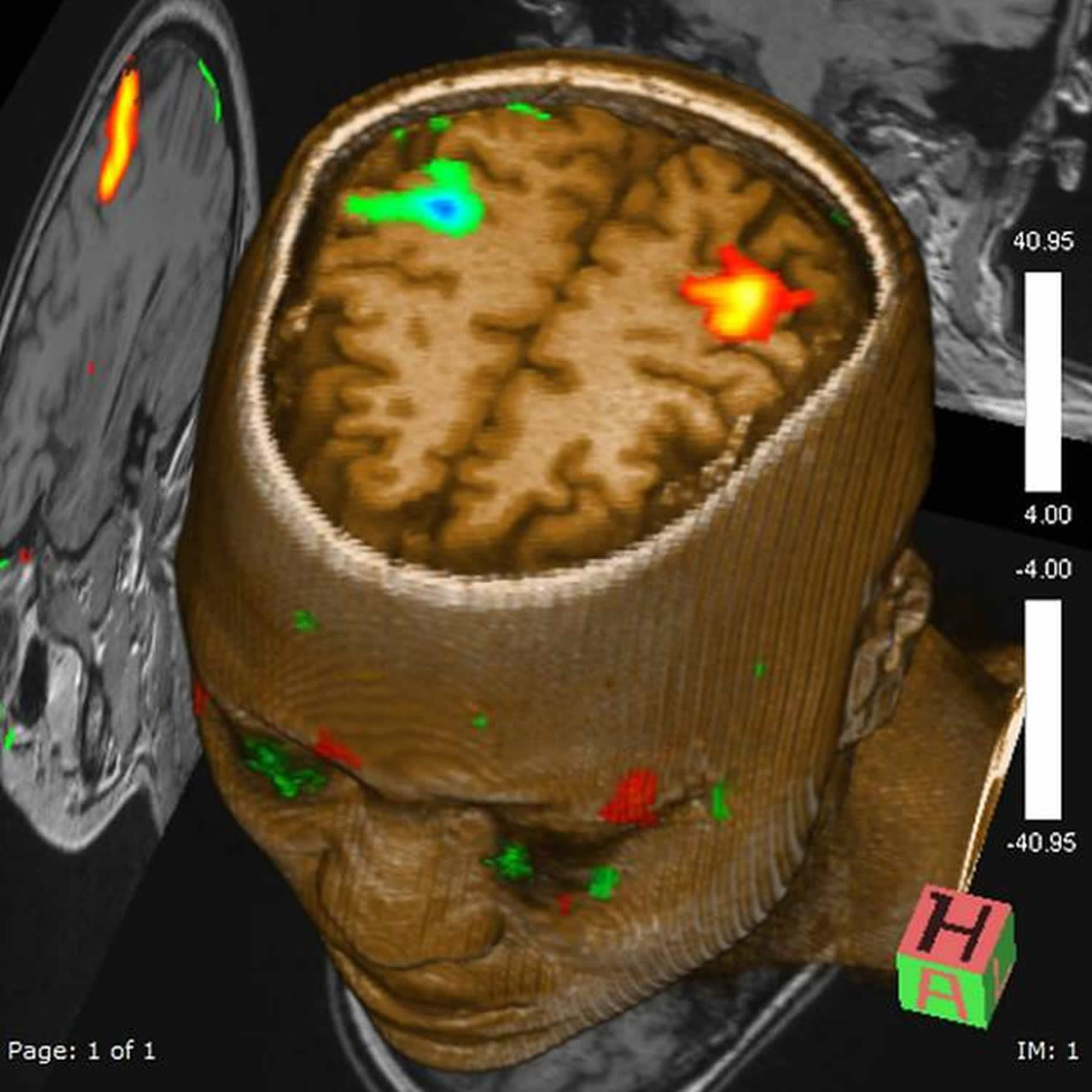
- Functional MRI (fMRI) allows visualization of both active parts of the brain during certain activities and understanding of the underlying networks. fMRI is technically challenging to perform as the techniques used to visualize cortical (brain) activity.
- Functional MRI (fMRI) detects subtle alteration in blood flow in response to stimuli or actions. It is used in two broad ways:
- Clinical practice
- typically in pre-surgical patients aimed at localizing eloquent areas (e.g. speech, motor function)
- Research
- often cohort of patients (often normals)
- aimed at elucidating novel neural networks
- Clinical practice
- Functional MRI (fMRI) detects subtle alteration in blood flow in response to stimuli or actions. It is used in two broad ways:
Disadvantages of MRI
There are many disadvantages and challenges to implementing MRI scanning.
MRI scans are more expensive than CT scans and take longer to acquire the images, so patient comfort is sometimes an issue. Additionally, images are subject to unique artefacts that must be recognized and abated.
MRI scans vary from ten minutes to an hour and even longer if an in-depth scan of a particular area is needed. Extremely sensitive, the MRI scanner produces high quality images of specific areas. However, this means that patients must lie completely still during the procedure. Often, patients are given a sedative to relax.
During an MRI, the patient lies still inside a tube-like scanner. The closed space can trigger claustrophobia in some patients. There are larger machines that accommodate more space.
MRI scanning is not safe for patients with some metal implants and foreign bodies. Careful attention to safety measures is necessary to avoid serious injury to patients and staff, and this requires special MRI compatible equipment and stringent adherence to safety protocols.
MRI safety
MRI scanners, although free from potentially cancer-inducing ionizing radiation (x-rays) found in plain radiography and CT scanners, have a host of safety issues which must be taken very seriously.
MRI safety can be divided into:
- main magnetic field
- varying magnetic (gradient) fields
- radiofrequency
Main magnetic field
The main magnetic field of a 1.5 Tesla magnet is about 30,000 times the strength of the earth’s magnetic field. It is strong enough to pull fork-lift tines off of machinery, pull heavy-duty floor buffers and mop buckets into the bore of the magnet, pull stretchers across the room and turn oxygen bottles into flying projectiles. Deaths have occurred from trauma as a result of these effects. Smaller objects such as pagers, bobby pins and pens have been known to be pulled off the person carrying them.
The strong field also affects common devices such as pacemakers and watches. The magnetic reed switch in modern pacemakers is disturbed by strong magnetic fields resulting in possible deleterious effects to the patient with one implanted. Mechanic watches will “freeze up” in a strong field, sometimes permanently.
Many intracranial aneurysm clips are ferromagnetic and as a result experience a torque or twisting in a magnetic field. Not everyone with an aneurysm clip experiences a fatal hemorrhage when placed in a magnet, but several cases have been reported.
Some types of heart valves (e.g. Starr-Edwards) are torqued in a magnetic field: however, this torque is less than the stresses that occur normally as a result of blood flow. Therefore heart valves are now considered not to be an absolute contraindication for MRI.
More of an annoyance than a safety problem is the ability of the magnetic field of a MRI machine to erase the information contained on the magnetic strip on ATM and credit cards. This may occur a short distance inside of the scanner room of a MRI machine.
Some metallic objects that are usually safe near an MRI machine are gold jewellery, shirt cuff-links and eyeglass frames.
Varying magnetic (gradient) fields
Varying magnetic fields are necessary in order to obtain images from MRI scanners. Changing magnetic field induce electrical currents in conductors (this is how an electrical generator works). In patients with metal in their body, the potential exists for electrical currents being induced in the metal with subsequent heating. This may occur with metal foreign bodies or some surgical implants. It does not universally occur and some patients with hip prostheses, for example, may be scanned without harm.
Very rapidly changing magnetic fields as may be achieved with echo planar imaging can cause nerve stimulation. This stimulation can affect motor nerves with resulting muscle contraction as well as the retina with resulting flickering lights called magnetophosphenes.
Radiofrequency
The radiofrequency (RF) power that is capable of being produced matches that of many small radio stations (15-20 kW). As a result there is the presence of heating effects from the radiofrequency (RF). In most pulse sequences, the heating is insignificant and does not exceed U.S. Food and Drug Administration (FDA) guidelines. New pulse sequences such as for echo planar imaging (EPI) and some spectroscopy localization techniques are capable of exceeding the FDA guidelines. Monitoring of the power deposition in patients is a requirement for FDA approval of clinical MRI scanners.
Potential for electrical shock exists with radiofrequency (RF) coils so proper grounding and insulation of coils is necessary. Any damage to coils or their cables needs prompt attention. Also looping of the cable to a coil can result in burns to patients that come into contact with them. It is best to avoid all contact with the radiofrequency (RF) coil cables.
Figure 4. MRI machine
Figure 5. MRI brain scan
Figure 6. Functional MRI (fMRI) – fMRI image of a person performing bilateral finger motor tasks. Note the increased blood flow in the motor and adjacent sensory strip.
- Projected Cancer Risks From Computed Tomographic Scans Performed in the United States in 2007. Arch Intern Med. 2009;169(22):2071-2077. doi:10.1001/archinternmed.2009.440 https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/415368[↩][↩][↩][↩][↩][↩][↩]
- Computed Tomography — An Increasing Source of Radiation Exposure. N Engl J Med 2007; 357:2277-2284 DOI: 10.1056/NEJMra072149 https://www.nejm.org/doi/full/10.1056/NEJMra072149[↩]
- What’s NEXT? Nationwide Evaluation of X-ray Trends: 2000 computed tomography. (CRCPD publication no. NEXT_2000CT-T.) Conference of Radiation Control Program Directors, Department of Health and Human Services https://www.crcpd.org/[↩]
- White KS. Helical/spiral CT scanning: a pediatric radiology perspective. Pediatr Radiol 1996;26:5-14[↩][↩]
- Linton OW, Mettler FA Jr. National conference on dose reduction in CT, with an emphasis on pediatric patients. AJR Am J Roentgenol 2003;181:321-329[↩]
- Heiken JP, Peterson CM, Menias CO. Virtual colonoscopy for colorectal cancer screening: current status. Cancer Imaging 2005;5:S133-S139[↩][↩]
- Stephen AE, Segev DL, Ryan DP, et al. The diagnosis of acute appendicitis in a pediatric population: to CT or not to CT. J Pediatr Surg 2003;38:367-371[↩]
- Mettler FA Jr, Wiest PW, Locken JA, Kelsey CA. CT scanning: patterns of use and dose. J Radiol Prot 2000;20:353-359[↩]
- Henschke CI, Yankelevitz DF, Libby DM, Pasmantier MW, Smith JP, Miettinen OS. Survival of patients with stage I lung cancer detected on CT screening. N Engl J Med 2006;355:1763-1771[↩]
- Brenner DJ. Radiation risks potentially associated with low-dose CT screening of adult smokers for lung cancer. Radiology 2004;231:440-445[↩]
- Beinfeld MT, Wittenberg E, Gazelle GS. Cost-effectiveness of whole-body CT screening. Radiology 2005;234:415-422[↩]
- U.S. Food and Drug Administration (August 2009). What are the Radiation Risks from CT? https://www.fda.gov/Radiation-EmittingProducts/RadiationEmittingProductsandProcedures/MedicalImaging/MedicalX-Rays/ucm115329.htm[↩]
- Howlader N, Noone AM, Krapcho M, et al. (eds). SEER Cancer Statistics Review, 1975-2010, National Cancer Institute. Bethesda, MD, 2013 https://seer.cancer.gov[↩]
- Average effective dose in millisieverts (mSv) from McCollough CH, Bushberg JT, Fletcher JG, Eckel LJ. Answers to common questions about the use and safety of CT scans. Mayo Clin Proc. 2015;90(10):1380-92.[↩]
- McNitt-Gray MF. AAPM/RSNA physics tutorial for residents — topics in CT: radiation dose in CT. Radiographics 2002;22:1541-1553[↩]
- Paterson A, Frush DP, Donnelly LF. Helical CT of the body: are settings adjusted for pediatric patients? AJR Am J Roentgenol 2001;176:297-301[↩]
- Martin CJ, Sutton DG, Sharp PF. Balancing patient dose and image quality. Appl Radiat Isot 1999;50:1-19[↩]
- Mitelman F, Johansson B, Mertens FE. Mitelman database of chromosome aberrations in cancer. Cancer Genome Anatomy Project, 2007. https://cgap.nci.nih.gov/Chromosomes/Mitelman[↩]
- Brenner DJ, Doll R, Goodhead DT, et al. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci U S A 2003;100:13761-13766[↩]
- Health risks from exposure to low levels of ionizing radiation — BEIR VII. Washington, DC: National Academies Press, 2005.[↩]
- Preston DL, Pierce DA, Shimizu Y, et al. Effect of recent changes in atomic bomb survivor dosimetry on cancer mortality risk estimates. Radiat Res 2004;162:377-389[↩]
- Preston DL, Shimizu Y, Pierce DA, Suyama A, Mabuchi K. Studies of mortality of atomic bomb survivors. Report 13: Solid cancer and noncancer disease mortality: 1950-1997. Radiat Res 2003;160:381-407[↩]
- Cardis E, Vrijheid M, Blettner M, et al. The 15-country collaborative study of cancer risk among radiation workers in the nuclear industry: estimates of radiation-related cancer risks. Radiat Res 2007;167:396-416[↩]
- Radiation Dose Associated With Common Computed Tomography Examinations and the Associated Lifetime Attributable Risk of Cancer. Arch Intern Med. 2009;169(22):2078-2086. doi:10.1001/archinternmed.2009.427 https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/415384[↩][↩][↩][↩]