Contents
- What is diaphragm contraceptive
- Types of diaphragm contraceptive
- How does a vaginal diaphragm work
- Who can safely use a diaphragm
- Diaphragm contraceptive risks
- Caya diaphragm
- How do I know that Caya diaphragm is inserted correctly and fits?
- Why does the Caya diaphragm have to remain in the vagina for 6 hours after intercourse?
- Why should Caya diaphragm not be worn for longer than 24 hours without interruption?
- What should I do if I forget to remove Caya diaphragm after 24 hours have passed?
- Can I have repeated consecutive intercourse with the Caya diaphragm?
- Can the Caya diaphragm also be used during menstruation?
- What do I have to observe in case of a vaginal infection?
- Can I use lubricants together with the Caya diaphragm?
- Could my partner feel the Caya diaphragm?
- Does the Caya diaphragm influence my sexual desire?
- What should I do if Caya diaphragm causes pain during intercourse?
- Can Caya diaphragm break or tear?
- How can I positively influence safety when using the Caya diaphragm?
- What should I do if Caya diaphragm accidentally comes out during intercourse?
- For how long can I use the Caya diaphragm?
- How to use a diaphragm
- Diaphragm effectiveness
- Cervical cap vs diaphragm
What is diaphragm contraceptive
The diaphragm is a birth control (contraceptive) device that prevents sperm from entering the uterus. The diaphragm is a small, reusable rubber or silicone cup with a flexible rim that covers the cervix. Before sex, the diaphragm is inserted deep into the vagina so that part of the rim fits snugly behind the pubic bone and the diaphragm dome covers the cervix, which is the entrance to the uterus (womb). Once you insert a diaphragm contraceptive it is held in place by your pelvic muscles. You don’t need a doctor to insert it, although it is a good idea to see a health professional to learn how to fit it properly first time. The diaphragm was developed in the 19th century, is one of the oldest methods of preventing pregnancy.
- The diaphragm contraceptive is effective at preventing pregnancy only when used with spermicide.
When used with spermicide, the diaphragm contraceptive helps prevent pregnancy. Among various benefits, the diaphragm:
- Diaphragm contraceptive doesn’t contain any hormones (and can be used if you are breastfeeding)
- Allows prompt return to fertility
- Can be used as a backup method of birth control because it’s effective immediately after insertion
- A diaphragm is effective even if it is inserted up to six hours before intercourse and thus can be inserted in advance to avoid disrupting sexual activity
- Can be used during breast-feeding beginning six weeks after childbirth
- Can be inserted up to six hours before sex and left in place for up to 24 hours
- Doesn’t require a partner’s cooperation
- Has few if any side effects
- Only needs to be used when having sex
- Can protect against pregnancy straight away
- Can be used more than once.
The diaphragm contraceptive isn’t appropriate for everyone, however. Your doctor may discourage use of the diaphragm if you:
- It is less effective than many other methods of contraception
- Some women find a diaphragm difficult to insert and risk placing it incorrectly
- Are allergic to silicone, latex or spermicide
- A diaphragm won’t protect you against sexually transmitted infections (STIs) – only condoms can do that, and even condoms won’t protect you against every STI.
- Are at high risk of or have HIV/AIDS
- Are at high risk of pregnancy — you’re younger than age 30; you have sex three or more times a week; you’ve had previous contraceptive failure with vaginal barrier methods; or you’re not likely to consistently use the diaphragm
- Have vaginal abnormalities that interfere with the fit, placement or retention of the diaphragm
- Have a vaginal or pelvic infection
- Inserting and removing it may be uncomfortable, and may increase the risk of urinary tract infection
- Have frequent urinary tract infections, between 1-10% of users experience this side effects
- Have a history of toxic shock syndrome
- Have significant pelvic organ prolapse, such as uterine prolapse — when the uterus descends into the vagina from its normal position in the pelvis
How much does a diaphragm cost?
Costs can range from $0 to about $250 for the diaphragm and the office visit. Many health insurance plans cover the costs, and family planning clinics (such as Planned Parenthood) may charge less. Also, the cost of spermicide is about $0.50 to $1.50 per use.
Where can I get the diaphragm?
A trained health care provider can determine the right size diaphragm for you and give you a prescription. You can purchase it at a pharmacy or clinic.
Types of diaphragm contraceptive
There are 4 types of diaphragms. They are made of either latex or silicone.
- The most common type is the arching spring diaphragm. It has a firm rim and is easiest to insert. It works best for women who have weak vaginal muscle tone.
- The coil spring diaphragm has a soft rim that is flexible. It works best for women who have average vaginal muscle tone.
- The flat spring diaphragm is similar, but has a thin rim. It works best for women who have strong vaginal muscle tone. You can use a diaphragm introducer tool to insert both the coil spring and flat spring types.
- The wide seal rim diaphragm is a silicone option. It is best for women who are allergic or sensitive to latex. It comes in arching spring or coil spring shapes.
See your primary doctor to get a diaphragm. They will help you decide which type of diaphragm is best and prescribe it for you. They will do an exam to measure you and find the correct size (60 to 90 mm in size). If it is too small, it may fall out or not block sperm. If it is too big, it will cause discomfort. The most common size is 75 millimeters (mm). It is important that your diaphragm fits right (see Figure 5 below). Your doctor will show you how to insert it properly and help you practice. It should rest right behind your pubic bone. A diaphragm that is too small will not sit snugly behind the pubic bone. Consequently, the diaphragm will fall out with a Valsalva’s maneuver or when you sits on the toilet or started walking. If the diaphragm does not sit snugly, a larger size should be tried. If a diaphragm that is 5 to 10 mm larger does not fit, another fitting examination should be performed.
A diaphragm that is too big will rest improperly in front of the pubic bone. You generally will have discomfort, and the diaphragm may interfere with urination.
With a properly fitted diaphragm, you should not be able to feel anything inside your vagina, even when you walk or strains during defecation. The diaphragm is removed by “hooking” the anterior rim with your index finger and pulling the device down and out of the vagina.
While proper size and fit of a diaphragm are important for effectiveness, correct use is even more important. The diaphragm can be inserted up to six hours to immediately before sexual intercourse. The diaphragm must remain in place for at least six hours after intercourse, but not for more than 24 hours (to reduce the risk of toxic shock syndrome). Douching should not be performed while the diaphragm is in place. If intercourse occurs more than once during the six hours that the diaphragm must remain in place, additional spermicidal jelly first should be inserted into the vagina. The diaphragm must be left in place while the spermicidal jelly is inserted.
When the diaphragm is removed, it should be washed with soap and water, rinsed and dried, and placed in its storage container. The diaphragm should be checked frequently for tears or holes. With good care and average use, diaphragms made of latex should last several years.
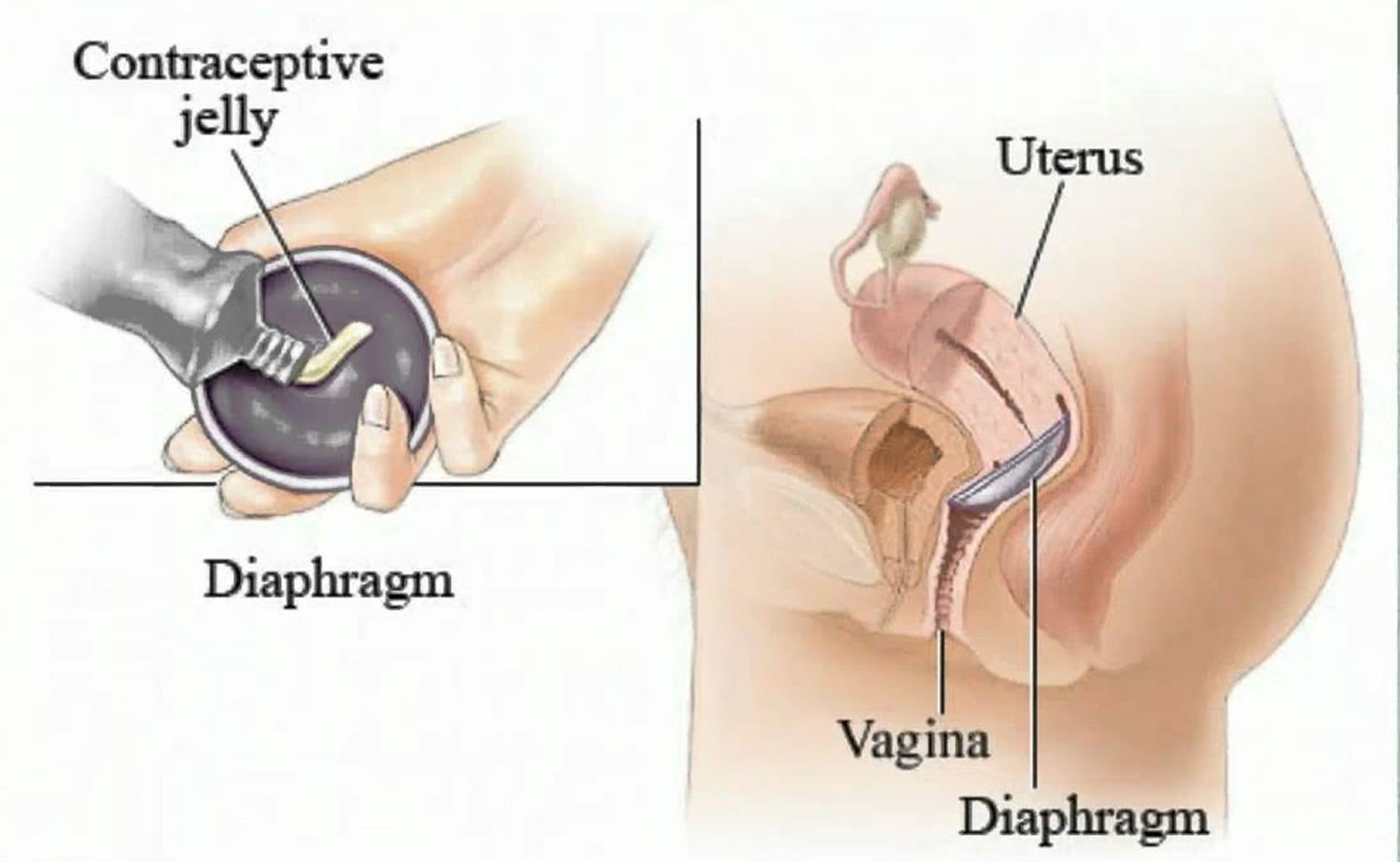
Figure 1. Female diaphragm contraceptive
Figure 2. Coil spring diaphragm
Figure 3. Arching spring diaphragm
Figure 4. Wide seal rim diaphragm
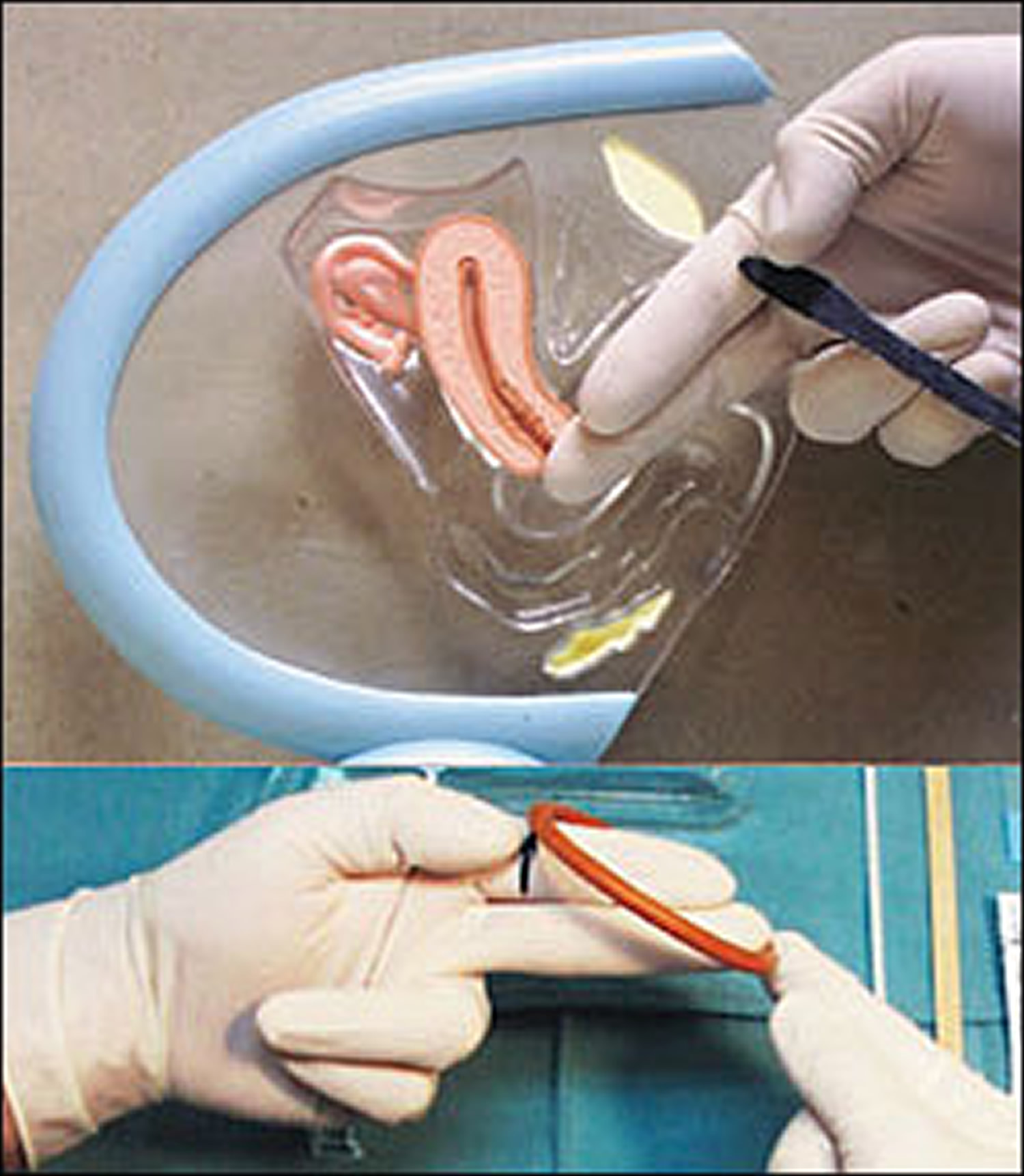
Figure 5. Diaphragm fitting using a fitting ring
Footnotes: (Top) The index and middle fingers are inserted into the vagina until the middle finger reaches the posterior fornix. The physician notes the spot where the bony inferior pubic arch touches the index finger. Before the fingers are removed from the vagina, this spot is marked with the thumb or an instrument. (Bottom) The diaphragm fitting ring is placed on the tip of the middle finger, and the opposite side of the rim is placed at the mark on the index finger. The diaphragm size is then determined (75 mm is a common size).
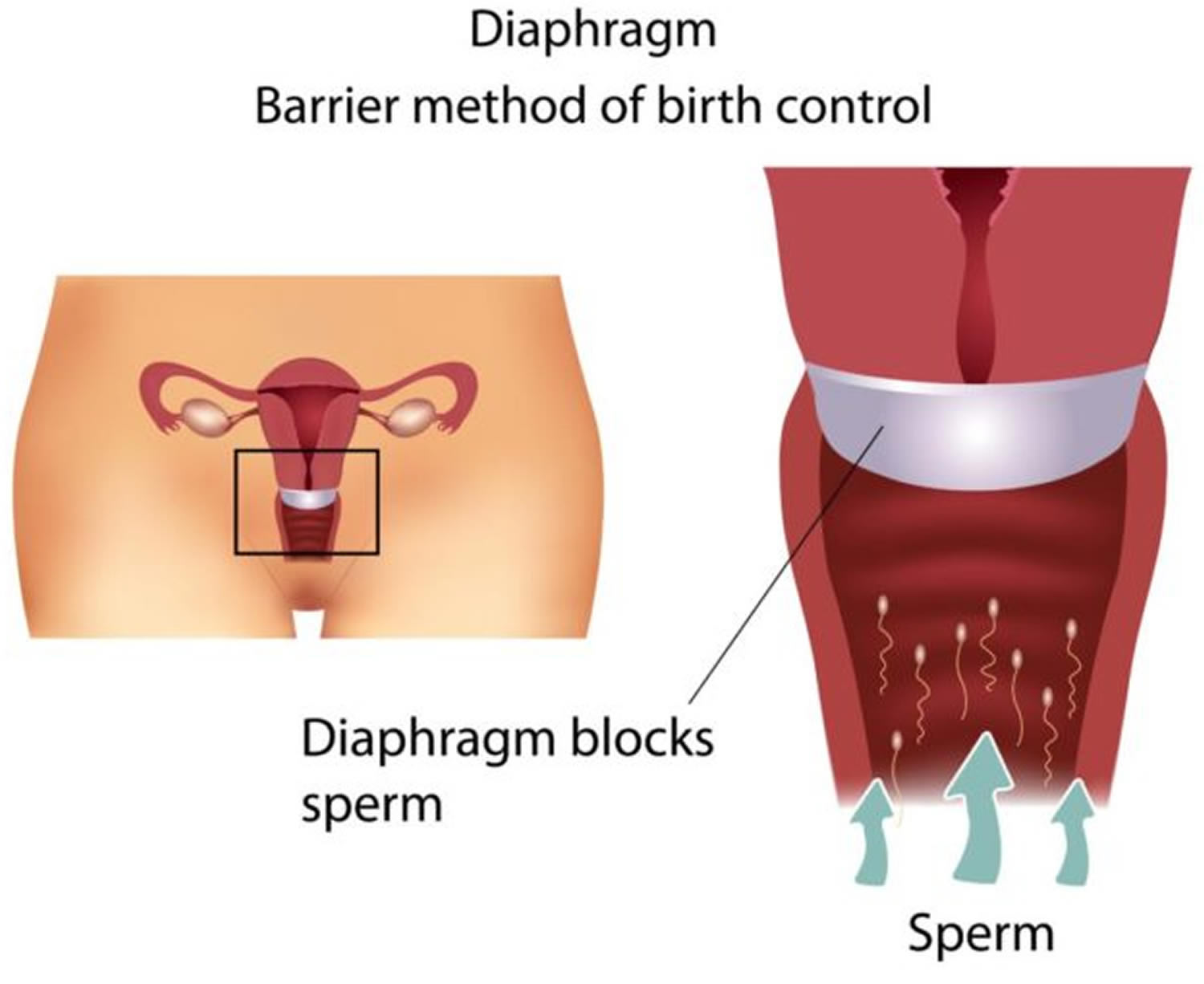
How does a vaginal diaphragm work
The diaphragm prevents pregnancy by blocking the cervical opening (the entrance to the uterus). During sex, the diaphragm stops sperm from entering the uterus. It forms a physical barrier between the man’s sperm and the woman’s egg, like a condom. So it is sometimes called a barrier method of contraception. If a woman is fertile, (if she has a viable egg in her uterus) sperm must enter the uterus to fertilize the egg. The egg cannot be fertilized once it has been expelled into the vagina. Thus, by preventing sperm from entering the uterus, the diaphragm also prevents sperm coming into contact with and fertilizing an egg.
The diaphragm needs to stay in place for at least 6 hours after sex. After 6 – but no longer than 24 hours after sex – it needs to be taken out and cleaned.
You can use the same diaphragm more than once, and it can last up to 2 years if you look after it.
Do not douche while you use a diaphragm. Do not leave a diaphragm in your vagina for more than 24 hours. This can cause irritation, infection, or a medical condition called toxic shock syndrome.
What could go wrong with diaphragm contraceptive?
The diaphragm can’t protect you from getting pregnant if it is not put in place properly, or moves out of place during sex. A health professional can show you how to fit a diaphragm before you use it for the first time.
If you take it out before 6 hours have passed after sex you risk becoming pregnant.
Your diaphragm could also break, tear, or develop tiny holes – which happens as it gets older – and this too could lead to an unintended pregnancy. You should examine your diaphragm for damage prior to using.
If you had a problem when using a diaphragm and are worried you could have become pregnant, you might want to consider taking emergency contraception, available from your doctor, chemist, health center or family planning clinic. This should be taken as soon as possible (within 5 days, but sooner is better).
Who can safely use a diaphragm
Most women can safely use a diaphragm contraceptive. However, some women may need to delay diaphragm use, and use a different method until they can safely use a diaphragm. These women include:
- Those who have experienced a second trimester miscarriage or abortion should wait for at least six weeks before having a diaphragm fitted;
- Those who have recently given birth should wait until at least six weeks after childbirth to have a diaphragm fitted;
- Those with uterine abnormalities, including uterine prolapse. These women should discuss other contraceptive methods which might be more suitable with their healthcare provider so that they can choose another method.
In addition, a diaphragm should NOT be used by the following women:
- Those with latex allergies should not use a latex diaphragm. A silicon diaphragm may be appropriate, or the woman’s healthcare provider will be able to give advice about other contraceptive methods.
- Those with sensitivity or an allergy to the chemicals in spermicide
- Women who have an unusually shaped or positioned cervix (entrance to the womb), or if you can’t reach your cervix
- Women with a history of toxic shock syndrome – as diaphragms increase the risk of this condition. Women who have previously experienced toxic shock syndrome should discuss other, more appropriate contraceptive methods with their healthcare provider. They should also not use a cervical cap);
- Women who have a getting an STI or high risk of HIV – for example, if you have multiple sexual partners; as a diaphragm is typically and most effectively used in conjunction with spermicide, and commonly available spermicides increase the risk of HIV infection, diaphragm use may increase a woman’s HIV risk. Women who are at risk of HIV infection, for example those who have sex with partners whose HIV status is unknown, should use condoms if possible, as these reduce the risk of HIV infection and other sexually transmitted infections. For some women find it is difficult to use condoms, for example if their partners refuse, there are pregnancy prevention methods which they can use without their partner’s knowledge including hormonal contraceptive injections or implants, or a diaphragm. However, these methods do not protect against STIs.
- Have repeated urinary tract infections
- Currently have a vaginal infection (wait until your infection clears before using a diaphragm or cap)
- Aren’t comfortable touching their vagina
Research shows spermicides that contain the chemical nonoxynol-9 don’t protect against STIs, and may even increase your risk of getting an infection.
Diaphragm contraceptive risks
The diaphragm doesn’t offer reliable protection from sexually transmitted infections (STIs).
An estimated 12 out of 100 women will get pregnant in the first year of typical use of the diaphragm. And an estimated six out of 100 women will get pregnant during the first year of use when following usage instructions exactly.
Consistent and correct use is essential to the effectiveness of the diaphragm birth control. For example, you may get pregnant when using a diaphragm if:
- You don’t use the diaphragm every time you have sex
- The diaphragm becomes dislodged from the cervix during sex
- You don’t use spermicide
- You remove the diaphragm within six hours after having sex
When to see your doctor
Call your doctor if you have any of the following problems:
- vaginal pain
- trouble urinating
- painful or frequent urination
- vaginal itching
- abnormal vaginal discharge
- fever. This can be a sign of toxic shock syndrome.
Side effects of diaphragm use:
Diaphragm use is commonly associated with urinary tract infections. This means that between 1-10% of users experience this side effects.
Candidiasis and bacterial vaginosis are uncommon side effects of diaphragm use, that is, they are side effects experienced by between 0.1%-1% of women who use the device. When the diaphragm is used in conjunction with a spermicide, these side effects are more likely.
Very rare cases of toxic shock syndrome have been reported in diaphragm users. Less that 0.01% of users experience this side effect.
Spermicide applied to the diaphragm may damage the cells lining the vagina, causing:
- Increased risk of contracting STIs
- Vaginal irritation
- Urinary tract or vaginal infection
Contact your health care provider if:
- The diaphragm slips out of place when you walk, sneeze, cough or strain
- You notice blood on the diaphragm after you remove it that isn’t related to your period
- You or your partner experiences pain during or following use of the diaphragm
- You have signs or symptoms of toxic shock syndrome, such as a sudden high fever, diarrhea, dizziness, vomiting, fainting or a rash that looks like sunburn
- You’re unable to remove the diaphragm
Limitations of the diaphragm include:
- The diaphragm must be inserted prior to every act of intercourse;
- The contraceptive protection of a diaphragm is much less effective than other methods (e.g. hormonal methods are typically >99% effective);
- To insert a diaphragm a woman must be comfortable with inserting her finger/s into her vagina. Women who have cultural or other objections to touching their genitals cannot use the method;
- Diaphragms do not provide adequate protection against sexually transmitted infections (STI). Women who have sexual partners of unknown STI status, should use male or female condoms if this is possible. Condoms offer high levels of protection against both pregnancy and STI.
Caya diaphragm
Caya diaphragm comes in only one size, and fits about 8 women out of 10. A health professional will be able to help you select another diaphragm contraceptive or other form of contraception if the Caya diaphragm is not suitable for you.
The shape of the Caya diaphragm is designed to fit the female anatomy. This shape and size fits a broad range of women.
- Cervical cup: Accommodates a range of cervical sizes. Thin, covers the cervix, not felt during intercourse
- Rim: Flexible, provides stability and helps guide the Caya diaphragm deep into the vagina as the woman pushes on the anterior edge. Holds the diaphragm in place and ensures that it is positioned correctly
- Grip dimples: Orient the woman’s finger and provide a tactile cue for where to hold and squeeze the rim
- Removal dome: Allows for easy removal; a woman’s finger can fit under or over the dome to remove the device
- Center point: palpable center point for a better positioning of the diaphragm
Figure 6. Caya diaphragm contraceptive
How do I know that Caya diaphragm is inserted correctly and fits?
Use your longest finger (usually the middle finger) to verify the correct position of the Caya diaphragm, check whether the cup covers cervix and the removal dome located securely behind your pubic bone. If this is the case you are well protected.
Why does the Caya diaphragm have to remain in the vagina for 6 hours after intercourse?
Sperm cells are no longer active after this period. These 6 hours are for your own safety and to prevent an unwanted pregnancy.
Why should Caya diaphragm not be worn for longer than 24 hours without interruption?
Wearing the Caya diaphragm for longer than 24 hours without interruption can promote bacterial growth inside the vagina. These bacteria can lead to Toxic Shock Syndrome.
What should I do if I forget to remove Caya diaphragm after 24 hours have passed?
Remove Caya diaphragm and visit your doctor for an examination.
Can I have repeated consecutive intercourse with the Caya diaphragm?
Yes, your Caya diaphragm will remain in position, but you will have to apply additional spermicide gel with the aid of an applicator. Applicators for contraceptive gel can be purchased in the pharmacy.
Can the Caya diaphragm also be used during menstruation?
You should never use a diaphragm during your menstrual period. You will need to use another form of birth control at this time.
What do I have to observe in case of a vaginal infection?
Please visit your doctor for treatment in case of vaginal infection (e.g. fungus). Use condoms during treatment and NOT a diaphragm. Upon completion of treatment you should purchase and use a new Caya diaphragm for your own safety.
Can I use lubricants together with the Caya diaphragm?
The use of water-based lubricants (e.g. Sylk) has no influence on the use and safety of Caya diaphragm.
NOTICE: New research showed that all lubricants made of silicone oil are not compatible with Caya diaphragms. The manufacturer recommends women and users to only use water-based products when using additional lubricant.
Could my partner feel the Caya diaphragm?
This is highly unlikely. However, in rare cases, your partner may feel the rim of the diaphragm.
Does the Caya diaphragm influence my sexual desire?
No, the Caya diaphragm has no influence on your libido as it contains no hormones.
What should I do if Caya diaphragm causes pain during intercourse?
First verify the correct position of Caya diaphragm using a finger. If the Caya diaphragm continues to cause pain, please visit your doctor.
Are there restrictions for the use of the Caya diaphragm?
No, the only habit that requires changing is that one always uses the diaphragm when it is needed – during intercourse. The more often Caya diaphragm is used, the more confident one becomes in handling the diaphragm.
Can Caya diaphragm break or tear?
This is nearly ruled out. However, if you do notice that your Caya diaphragm is damaged in some way after intercourse, please visit your doctor immediately (within 5 days) to discus the possibility of emergency contraception (“morning-after-pill”).
How can I positively influence safety when using the Caya diaphragm?
The regular use of spermicide gel are important measures for ensuring safety. In addition, the diaphragm should always be inserted before and not during intercourse.
What should I do if Caya diaphragm accidentally comes out during intercourse?
Re-insert Caya diaphragm again after applying some more spermicide gel. If the diaphragm comes out after your partner has ejaculated or if you do not feel safe, visit your doctor to discuss whether you may need the “morning-after-pill”.
For how long can I use the Caya diaphragm?
After the first use, the Caya diaphragm should not be used for a period longer than 2 years.
How to use a diaphragm
The diaphragm contraceptive comes in different sizes. Your health care provider will find the correct size and fit you for the diaphragm contraceptive and demonstrate how to insert and remove the diaphragm. He or she may confirm that the diaphragm contraceptive is in the correct position by doing a pelvic exam.
Before you use the diaphragm contraceptive for the first time, practice inserting the diaphragm until you’re comfortable with it. You may want to use a backup method of contraception, such as a male condom, the first few times you use the diaphragm contraceptive.
- It is very important for a diaphragm user to know how to use the device correctly. The health practitioner who fits the diaphragm will explain to the woman how a diaphragm is used, when they do the fitting.
- Your health practitioner may recommend that new users begin by using their diaphragm in conjunction with another method. This is not because diaphragms do not work when they are first fitted, but rather to allow the woman to get used to inserting and removing the device correctly.
- Women using diaphragms should be aware that a new diaphragm must be fitted after childbirth or a second trimester abortion. A new diaphragm should also be fitted if the woman experiences weight gain of >5kg. Women who do not need to have a new diaphragm refitted should replace their device every two years.
Diaphragm users should also be aware that:
- For effective use, a diaphragm must be used prior to every act of intercourse;
- When a diaphragm is correctly inserted, the woman should not be able to feel it, even during intercourse;
- That diaphragms are most effective when used in conjunction with spermicides;
- That diaphragms have some side effects, the most common of which are urinary tract infections and vaginal discharges.
Always use the diaphragm contraceptive with spermicidal cream, foam or gel. Avoid use of body lotions near your vagina and vaginal medications when using the diaphragm. If you’re using a diaphragm and douche, wait until at least six hours after sex to avoid washing away spermicide.
Make sure you regularly check your diaphragm for puncture marks or cracks. To search for holes, hold your diaphragm up to the light and gently stretch the rubber between your fingers or fill the diaphragm with water. Replace your diaphragm contraceptive at least every two years. You may need to have your diaphragm checked and possibly refitted if:
- Your diaphragm no longer fits snugly or comfortably
- You’ve given birth or had an abortion
- You’ve had pelvic surgery
- You’ve gained or lost more than 10 pounds
- You have repeated urinary tract infections
- You or your partner feels pain or pressure during sex
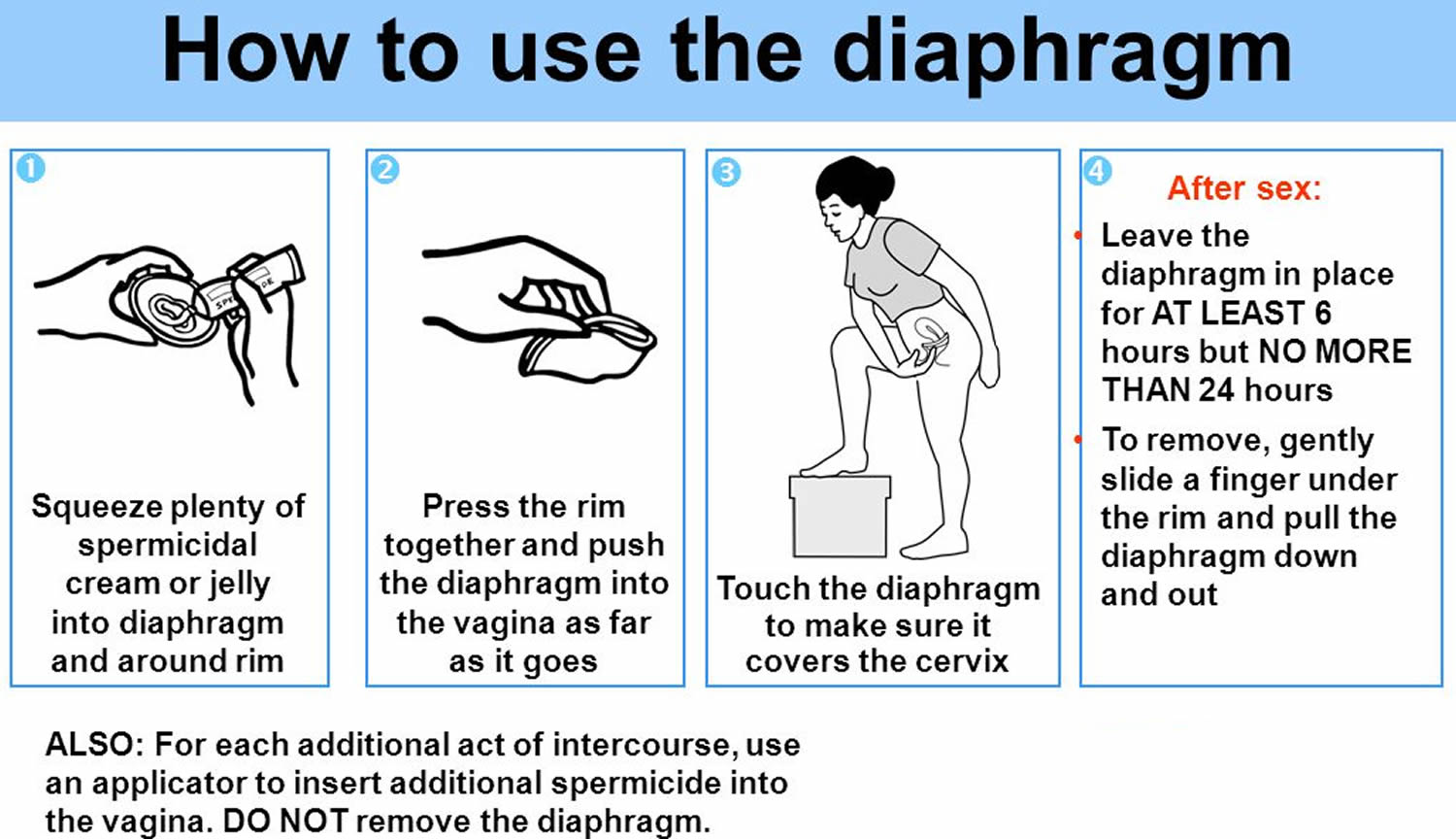
How use the diaphragm contraceptive:
- Begin by washing your hands.
- Check the diaphragm for cracks by holding it up to the light.
- Apply spermicide. Fill the diaphragm’s bowl with about 1 tablespoon (15 milliliters) of spermicide. Spread a thin layer of spermicide around the rim of the diaphragm with your finger. It is important to always check the expiry date of spermicides before using them. Use only water-based lubricants with the diaphragm.
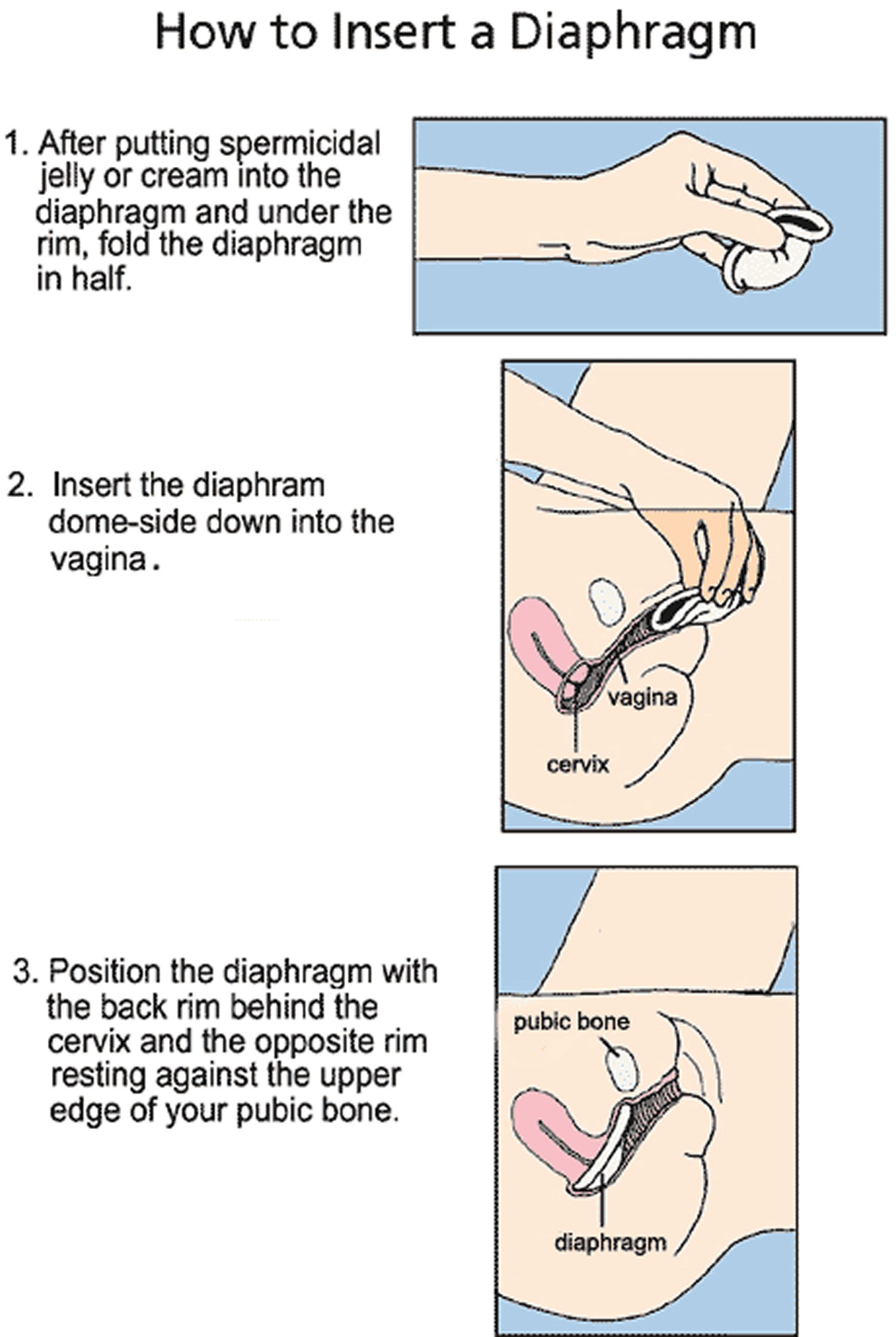
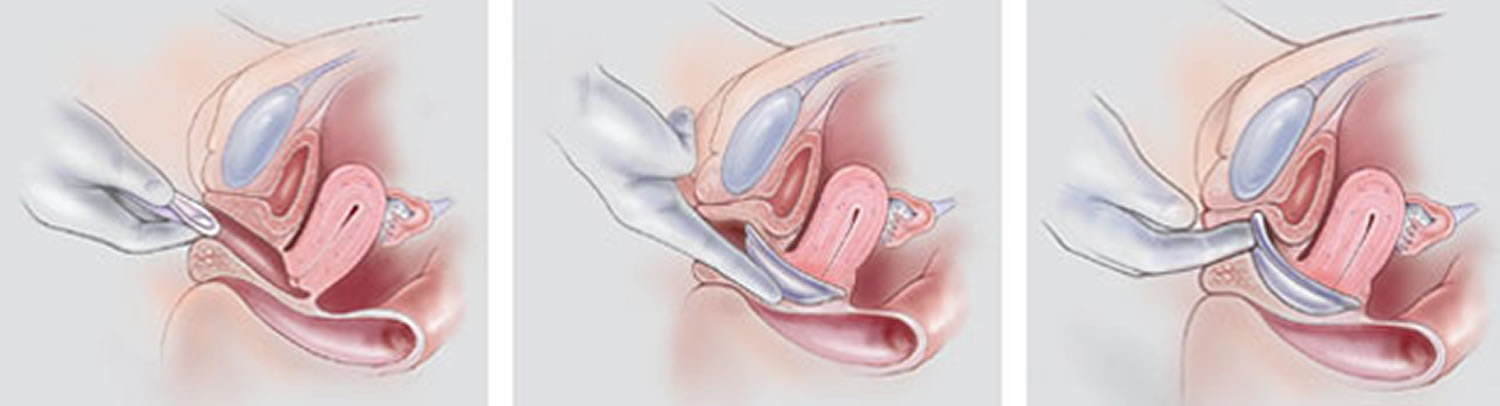
- Insert the diaphragm. Find a comfortable position, such as standing with one foot propped up, squatting or lying on your back. Separate your labia with one hand. With the other hand, hold the diaphragm with the bowl facing upward and squeeze the diaphragm between your thumb, index and middle fingers.
- Slide the diaphragm into your vagina and push it along the back wall of your vagina as far as it will go and move it up to cover the cervix, which is the entrance to the uterus (womb). Use your index finger to push the front rim of the diaphragm up behind your pubic bone.
- Check the diaphragm’s position before sex. Make sure you can feel your cervix through the soft dome of the diaphragm. The cervix feels similar to the tip of your nose, and can be felt through the diaphragm. After inserting the diaphragm, apply spermicide inside the vagina before each time you have sex. If the diaphragm is dislodged during sex, reapply spermicide.
- Remove and reinsert the diaphragm if you can feel it inside your vagina when you move.
- After sex, leave the diaphragm in place for at least six hours and up to 24 hours. To remove the diaphragm, hook your finger under the front rim of the diaphragm and gently pull it down and out of your vagina. If the diaphragm is difficult to remove, insert your finger between the rim of the diaphragm and your vaginal wall to break any suction. After removal, wash the diaphragm with mild soap and warm water and allow it to air-dry. Store the diaphragm in its provided container.
Note: If you are having sexual intercourse several times, you should not remove and reinsert the diaphragm between sex acts. Rather the diaphragm should be left in place and additional spermicide added each time.
Removing a diaphragm
- It is very important that the diaphragm is left in place for at least six hours following intercourse, but not for more than 24 hours.
Leaving the diaphragm in place for more than 24 hours may result in unpleasant odor or vaginal discharge, and in rare cases, toxic shock syndrome. Once at least six hours has elapsed since the last sexual intercourse, a woman should remove the diaphragm according to the following procedure:
- Before commencing, you should wash your hands;
- You then insert a finger into your vagina until you feel the rim of the diaphragm;
- You then gently slide your finger under the rim and pull the diaphragm down and out. Care should be taken to ensure the diaphragm does not tear or break;
- Finally, you should wash the diaphragm using mild soap and water. The diaphragm should then be dried and stored in a cool dry place.
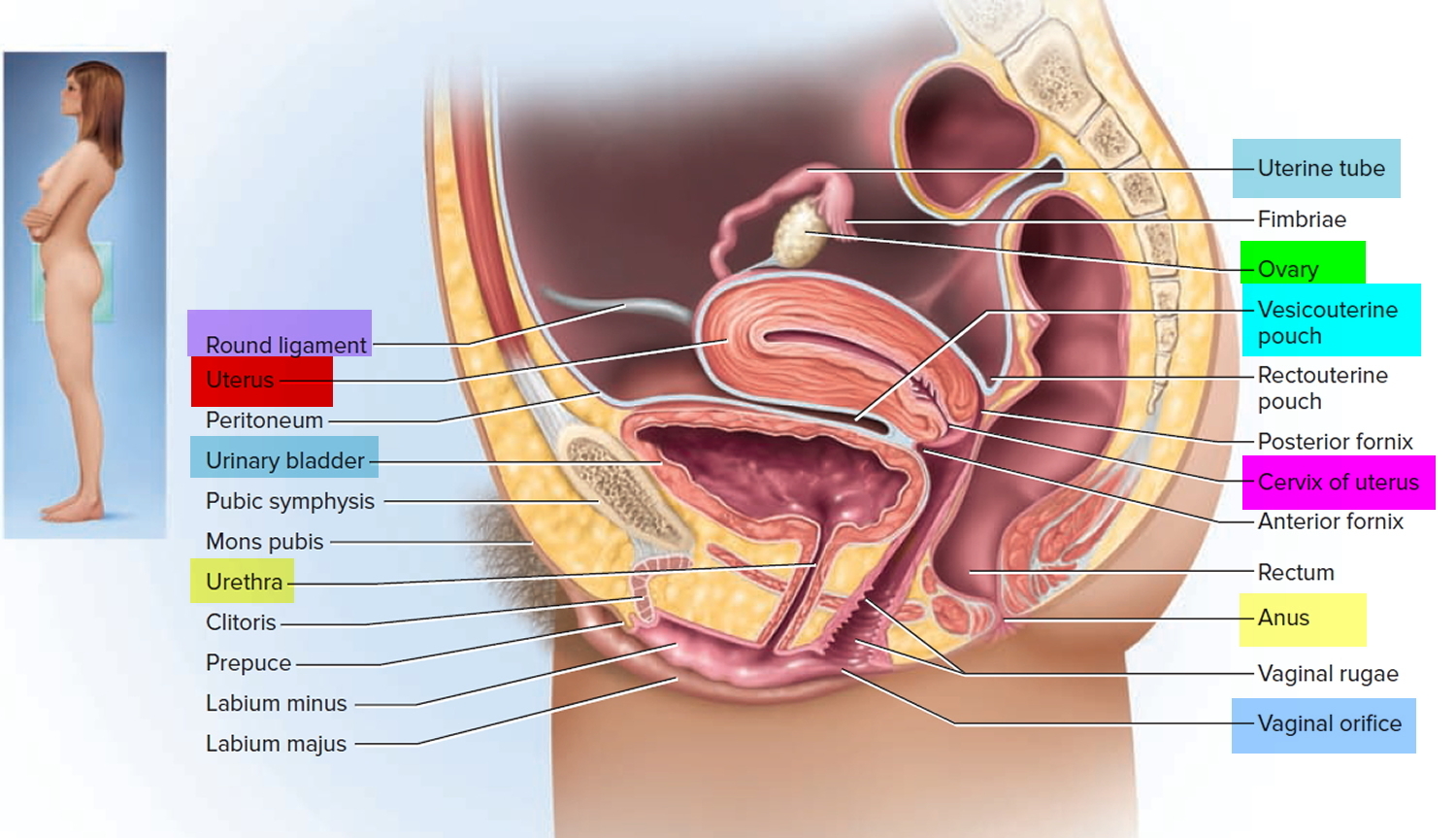
Figure 7. Cervix position
Figure 8. Cervix location
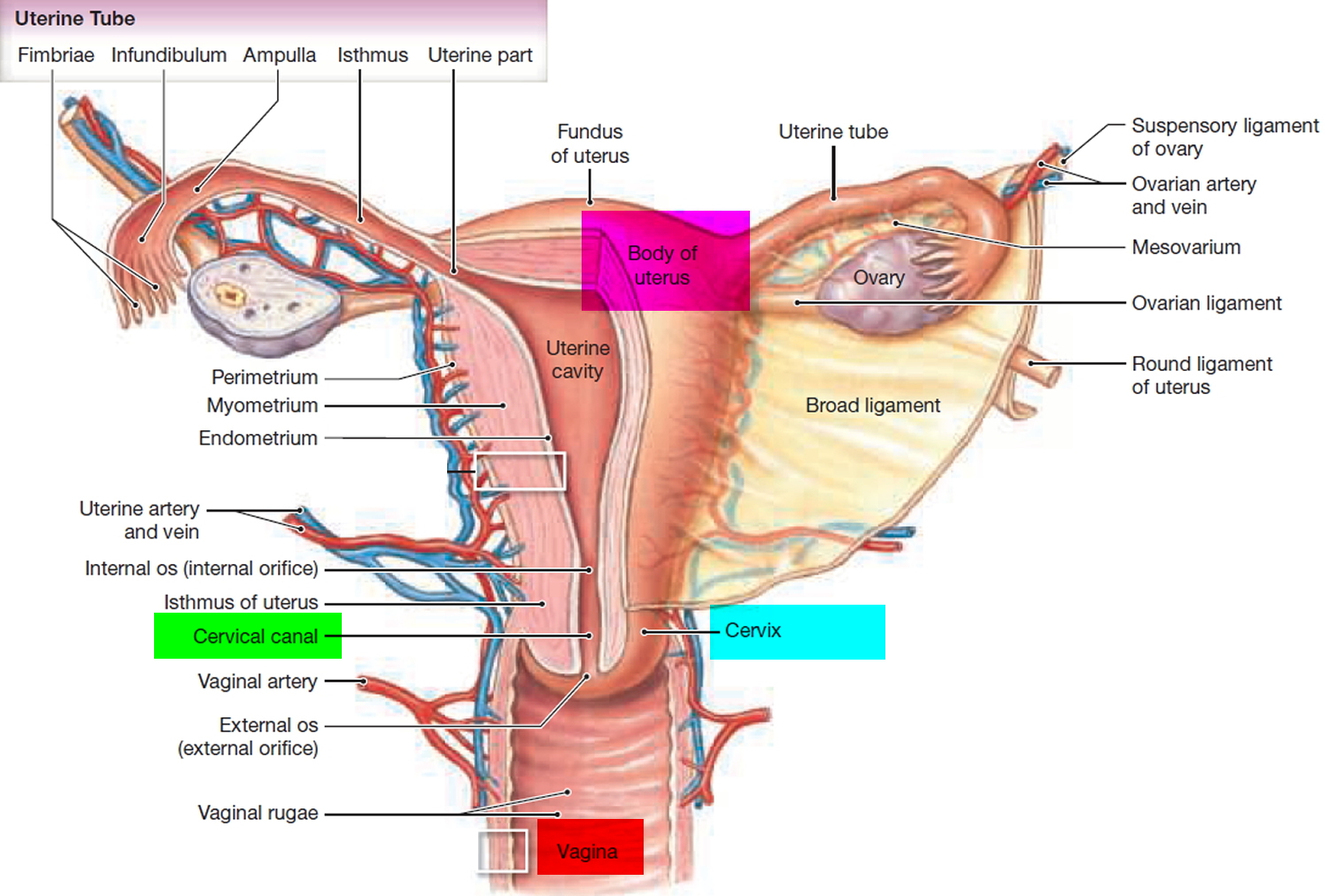
Figure 9. How to use the diaphragm birth control
Figure 10. How to insert the diaphragm contraceptive
Insertion of fitting diaphragm. (Left) The lubricated diaphragm is folded and inserted at the introitus. (Center) The cervix should be palpable through the dome of the diaphragm. (Right) The anterior rim of the diaphragm is nudged so that it fits directly behind the pubic bone.
Diaphragm effectiveness
Diaphragms work fairly well if they are put in place and used correctly, but not as well as the pill, a contraceptive implant or an IUD. If 100 women use a diaphragm for a year, around 14 to 18 will likely get pregnant.
Table 1. Birth control methods effectiveness and their risks and side effects
| Method | How it is Used | Failure Rate (average use) | Risks & Side Effects |
| Abstinence | No sexual intercourse and no type of contact between the male and female sexual organs where bodily fluids could be exchanged | 0% | No Side Effects |
| Cervical Cap | A soft rubber barrier that covers the cervix in order to prevent sperm from entering the uterus | 12% (higher after childbirth) | No Side Effects (unless allergic) |
| Condom – Female | A sheath, often made of latex rubber, inserted into the vaginal canal to block the passage of sperm | 21% | No Side Effects (unless allergic) |
| Condom – Male | A sheath, often made of latex rubber, covering the erect penis to block the passage of sperm | 18% | No Side Effects (unless allergic) |
| Depo-Provera Injection | Injection of Progestin that is given every 3 months to prevent ovulation, change cervical mucus to block sperm, and change the lining of the uterus to prevent implantation of a fertilized egg | 6% | Irregular, missed, or heavier than normal menstrual cycle, weight gain, breast tenderness, depression, bloating, abdominal pain, headaches, allergic reaction |
| Diaphragm | A soft rubber dome that covers the cervix to block the passage of sperm. | 12% | No Side Effects (unless allergic) |
| Fertility Awareness | Using the menstrual cycle and other tools to predict ovulation and abstaining from intercourse during these expected fertile times | 25% | No Side Effects |
| Implant – Hormonal | A small, matchstick-sized implant inserted in the upper arm and lasts for 3 years, releasing a hormone supply. Works in a similar way to Depo-Provera. | 0.05% | No period, spotting, light or heavy and prolonged bleeding; painful menstruation, acne, weight gain, depressed mood; blood clots, movement of implant, ectopic pregnancy, ovarian cysts |
| Intrauterine Device (IUD) – Copper | A device is inserted into a woman’s uterus (by a doctor) to block sperm and change the uterus lining to prevent implantation of a fertilized egg | 0.8% | Ectopic pregnancies, increased bleeding during menstrual cycle, severe menstruation cramps, perforation of the uterus, Pelvic Inflammatory Disease (PID) |
| Intrauterine Device (IUD) – Progestin | 0.2% | ||
| Nothing/Chance | No birth control method | 85% | No Side Effects; highest chance of unintended pregnancy |
| Oral Contraceptive (estrogen/progestin) | Taken daily by women to suppress ovulation, change cervical mucus, and change the lining of the uterus to prevent implantation of a fertilized egg | 9% | Nausea, headaches, weight gain, depression, irregular bleeding, acne, blood clots *Women who smoke are advised not to take oral contraceptives |
| Oral Contraceptive (progestin only) | Taken daily by women to change cervical mucus to block sperm and also changes the uterus lining to prevent implantation of a fertilized egg | 9% | Breast tenderness, weight gain, menstrual cycle changes *Women who smoke are advised not to take oral contraceptives |
| Ortho-Evra Patch | A patch containing synthetic hormones placed on your skin; works the same as oral contraceptives | 9% (greater if over 198 lbs) | Similar to oral contraceptives |
| Spermicide (only) | A jelly, foam, or cream containing chemicals that kill sperm | 28% | No Side Effects (unless allergic) |
| Sponge | A soft saucer-shaped polyurethane sponge that blocks the cervix and absorbs semen | 20% (40% after childbirth) | No Side Effects (unless allergic) |
| Sterilization – Female | Permanent surgical procedure to prevent pregnancy: fallopian tube is damaged (cut, tied, burnt) to prevent passage of eggs and sperm | 0.5% | If a woman conceives after a sterilization procedure there is a risk of ectopic pregnancies. The earlier the age of the woman at the time of the procedure, the greater risk of pregnancy after 10 years (up to ~5%). |
| Sterilization – Male | Permanent surgical procedure to prevent pregnancy: vas deferens tube is damaged (cut, tied, burnt) to prevent passage of sperm into ejaculate fluid | 0.15% | No Side Effects |
| Vaginal Ring – Hormonal | A flexible ring placed inside the vagina near the cervix. Active for 3 weeks. Has actions similar to oral contraceptives. | 9% | Blood clots, liver or gallbladder problems, TSS, depressed mood, acne, headache, weight gain, nausea/vomiting, movement of the ring |
| Withdrawal | Withdrawal of the penis before ejaculation | 22% | No Side Effects |
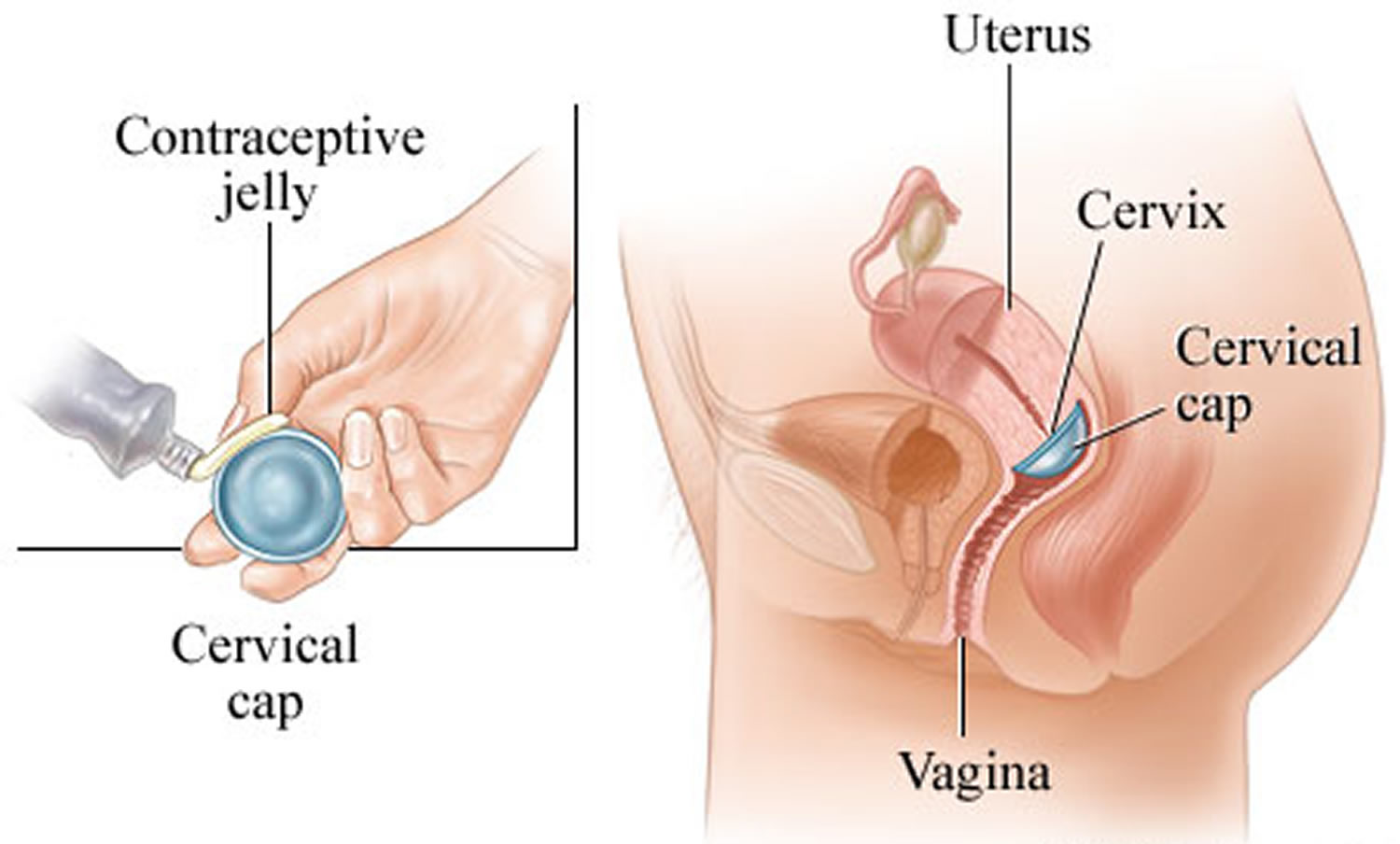
Cervical cap vs diaphragm
The cervical cap is a birth control (contraceptive) is a small plastic dome that fits tightly over the cervix and stays in place by suction, that prevents sperm from entering the uterus. The cervical cap is a reusable, deep silicone cup that is inserted into the vagina and fits tightly over the cervix. The cervical cap is held in place by suction and has a strap to help with removal. The cervical cap is effective at preventing pregnancy only when used with spermicide. The cervical cap does not protect against sexually transmitted infections (STIs), including HIV.
Only one cervical cap — FemCap — has Food and Drug Administration (FDA) approval in the U.S. It must be fitted and prescribed by a doctor, but can be purchased online if you have a current prescription. Your doctor may ask you to come back to make sure you know how to insert the cap and use it correctly.
Refitting may be needed after having a baby or after weight gain or loss. The cervical cap is less effective in women who have given birth. You should wait 6 weeks after giving birth to use the cervical cap, until the uterus and cervix return to normal size.
When used with spermicide, the cervical cap helps prevent pregnancy. Among various benefits, the cervical cap:
- Allows prompt return to fertility
- Can be used while breast-feeding beginning six weeks after delivery
- Can be inserted hours before sex and remain in place for up to 48 hours
- Doesn’t require a partner’s cooperation
- Poses few if any side effects
The cervical cap isn’t appropriate for everyone, however. Your health care provider may discourage use of the cervical cap if you:
- Are allergic to spermicide or silicone
- Are at high risk of or have HIV/AIDS
- Are at high risk of pregnancy — you’re younger than age 30; you have sex three or more times a week; you’ve had previous contraceptive failure with vaginal barrier methods; or you’re not likely to consistently use the cervical cap
- Have vaginal or cervical abnormalities that interfere with the fit, placement or retention of the cervical cap
- Have vaginal bleeding or have a vaginal, cervical or pelvic infection
- Have a history of pelvic inflammatory disease, toxic shock syndrome, cervical cancer, third-degree uterine prolapse, uterine tract infections, or vaginal or cervical tissue tears
- Recently gave birth or had a miscarriage or an abortion
- Recently had cervical surgery
What else do you need to know about cervical cap?
- Don’t use cervical cap during your period. Use another method, such as a condom, or don’t have intercourse.
- Check the cervical cap often. Get a new cervical cap if you see holes, tears, or discoloration.
- Wash the cervical cap with warm water and hand soap after removing it. Make sure it’s dry before you store it in its container. Do not use talcum or baby powder on the cap. These products may break down the silicone or irritate the vagina.
- You should be refitted for the cervical cap if you have a baby.
- The cervical cap doesn’t protect against sexually transmitted infections (STIs), such as herpes or HIV/AIDS. If you’re not sure whether your sex partner might have an STI, use a condom to protect against disease. Using a condom with the cap also protects better against pregnancy.
Figure 11. Cervical cap contraceptive
Figure 12. How to insert the cervical cap
Cervical cap risks
The cervical cap doesn’t offer protection from sexually transmitted infections (STIs).
An estimated 16 out of 100 women who’ve never been pregnant or given birth vaginally will become pregnant during the first year of typical use of the cervical cap. An estimated 32 out of 100 women who’ve given birth vaginally will become pregnant during the first year of typical use. This difference is due to the fact that the vagina and cervix are stretched by giving birth vaginally, which means the cervical cap may not fit as well.
Inconsistent or incorrect use of the cervical cap increases your risk of pregnancy. For example, you may get pregnant when using the cervical cap if:
- The cervical cap becomes dislodged from the cervix during sex
- You don’t use spermicide
- You remove the cervical cap within six hours after having sex
Spermicide applied to the cervical cap may damage the cells lining the vagina, causing:
- Increased risk of contracting STIs
- Urinary tract or vaginal infection
- Vaginal irritation
Contact your health care provider if:
- The cervical cap slips out of place when you walk, sneeze, cough or strain
- You have signs or symptoms of toxic shock syndrome, such as a sudden high fever, diarrhea, dizziness, vomiting, fainting or a rash that looks like sunburn
- You notice blood on the cervical cap after you remove it that isn’t related to your period
- You notice a foul odor when the cervical cap is in place or after you remove it
- You or your partner experiences pain during or following use of the cervical cap
- Your partner has abrasions on his penis following use of the cervical cap during sex
How to use the cervical cap
The cervical cap comes in different sizes. Your health care provider will fit you for the cervical cap and demonstrate how to insert and remove the cap. He or she may confirm that the cervical cap is in the correct position by doing a pelvic exam.
Make sure you regularly check your cervical cap for wear, holes or discoloration and replace your cervical cap each year. You may need to have your cervical cap refitted after childbirth. Always use the cervical cap with spermicide. Don’t wear the cervical cap during any kind of vaginal bleeding, including your period.
Before you use the cervical cap for the first time, practice inserting the cap and checking its placement. Use a backup method of contraception, such as a male condom, the first few times you use the cervical cap.
How to insert the cervical cap contraceptive
- Begin by washing your hands.
- Check the position of your cervix before inserting the cervical cap. To find your cervix, insert your finger deep into your vagina. The cervix feels like the tip of your nose. Its position will vary according to the time of the month and your body position.
- Apply spermicide. Fill the cervical cap’s bowl with about 1/4 teaspoon (1.25 milliliters) of spermicide. Spread a thin layer of spermicide on the brim of the cervical cap that faces the cervix. Place 1/2 teaspoon (2.5 milliliters) of spermicide in the groove between the rim and the dome of the cervical cap. Some experts suggest using an additional dose of spermicide if you have sex a second time with the cap still in. Don’t remove the cap for at least six hours after the last time you had sex.
- Insert the cervical cap. Insert the cervical cap into your vagina before sexual arousal to ensure proper placement. Find a comfortable position, such as squatting. Separate your labia with one hand. With the other hand, hold the cervical cap with the bowl facing upward and squeeze the rim of the cervical cap between your thumb and index finger. Slide the cervical cap into your vagina — making sure the taller brim of the cervical cap enters your vagina first. Push the cervical cap along the rear wall of your vagina as far as it will go. Use your finger to locate your cervix and press the rim of the cervical cap around the cervix until you’ve completely covered it.
- Always check the cervical cap’s position before sex. Squat, bear down, insert your finger into your vagina and press upward on the dome to make sure your cervix is covered. If the cervical cap is not covering your cervix completely, either push it onto the cervix or remove it and reinsert it.
- After sex, leave the cervical cap in place for at least six hours and up to two days. To remove the cervical cap, squat, bear down and rotate the cap. Relax your muscles and push up on the dome of the cervical cap to break the seal. Grasp the removal strap and gently pull. Be careful not to scratch your vagina. After removal, wash the cervical cap with mild soap and warm water and let it air-dry. Store the cervical cap in its provided container.
If you have sex more than one time when the cap is in place, put a small amount of spermicide on the tip of your finger. Insert your finger into your vagina and check the position of the cap. Don’t remove the cervical cap.
Avoid using any petroleum-based vaginal creams, oils, or ointments, which can damage the silicone. But water-based personal lubricants, such as Astroglide and K-Y Jelly, are safe to use.
What if you think the cap is not placed correctly or not protecting you from pregnancy?
- Always read the instructions.
- Call your doctor or nurse call line and use backup birth control, such as a condom, or don’t have intercourse until you know the cervical cap is working.
- If you had intercourse, you can use emergency contraception, such as the morning-after pill (Plan B). You can use emergency contraception for up to 5 days after having had sex, but it works best if you take it right away.
- Birth Control Failure. http://americanpregnancy.org/preventing-pregnancy/birth-control-failure[↩]