What is ear canal
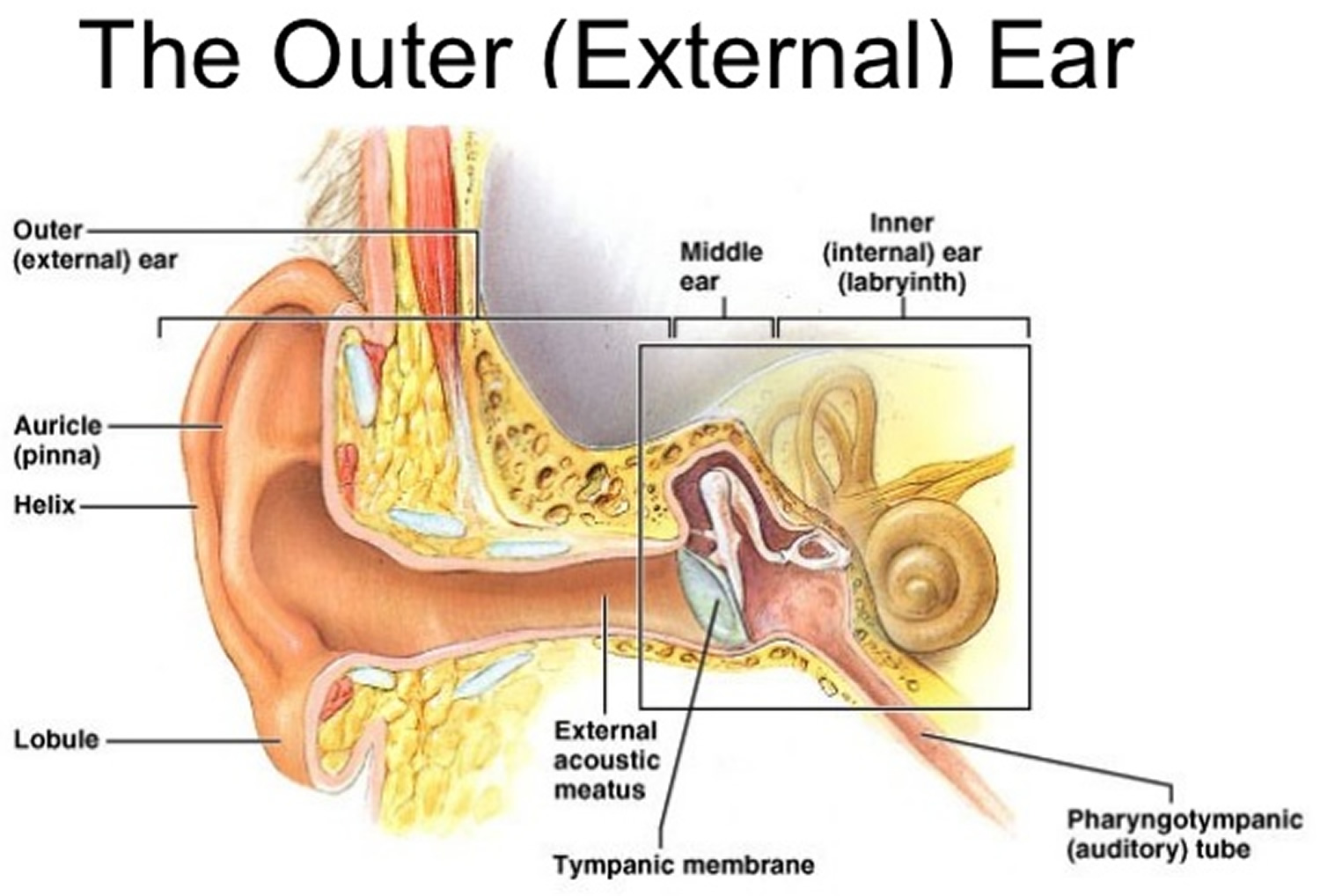
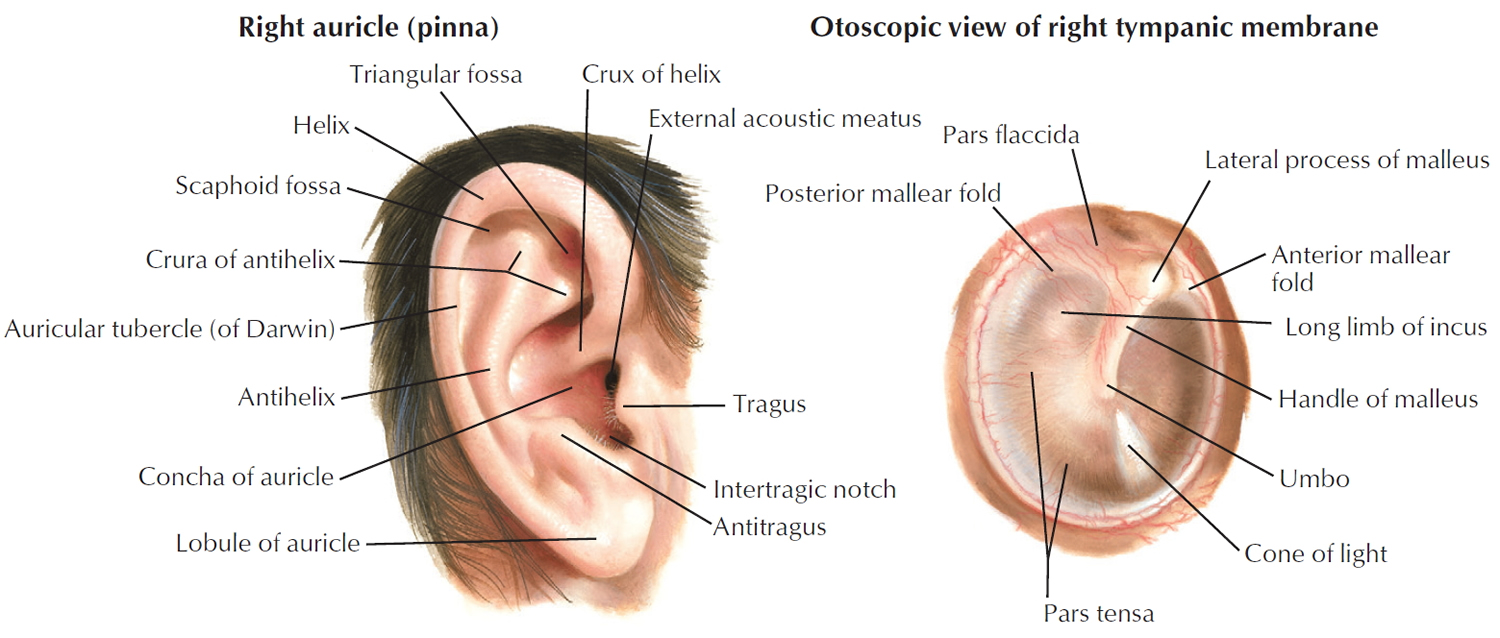
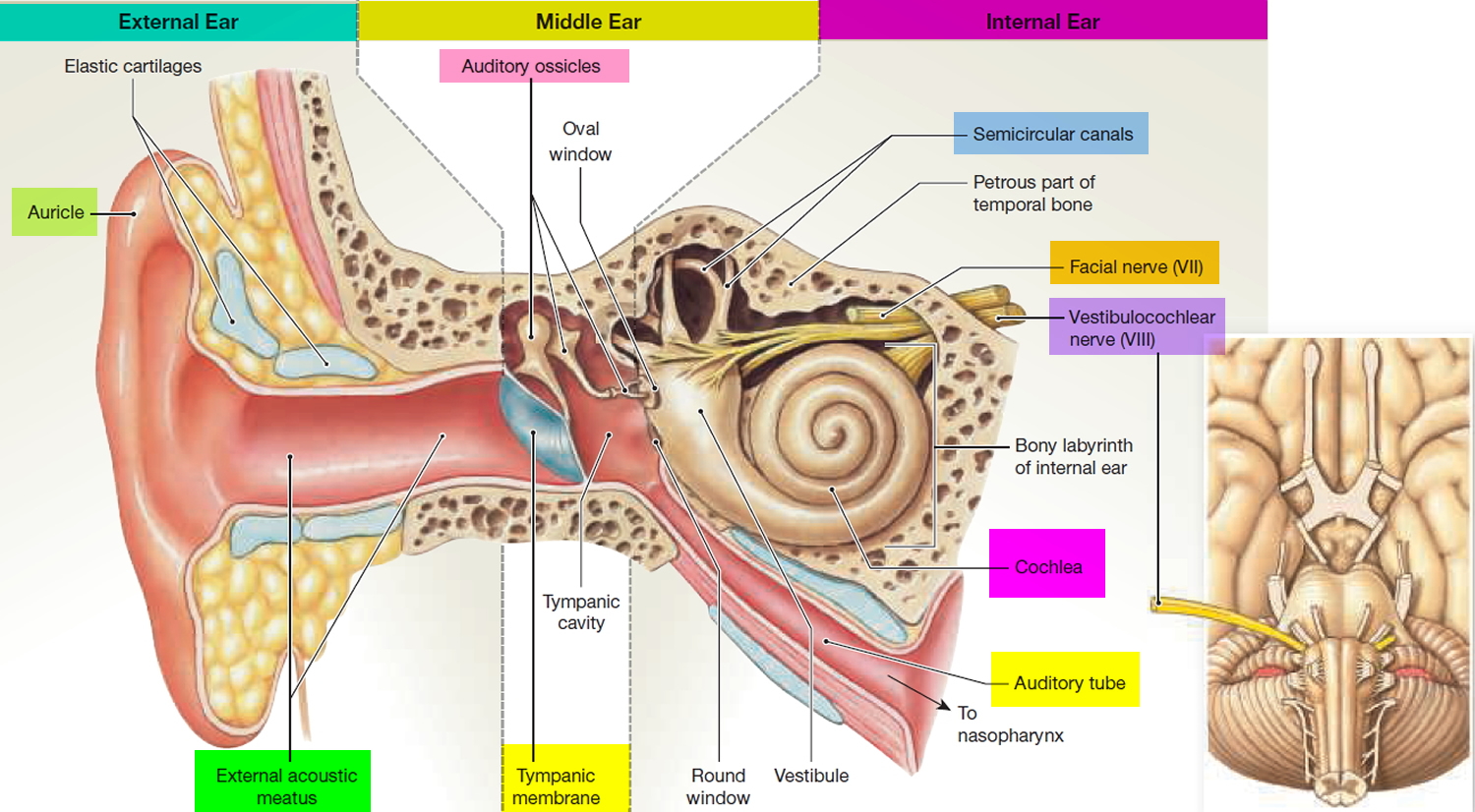
The external ear consists of the auricle and the external ear canal or external acoustic meatus. The auricle or pinna, is what most people call the ear—the shell-shaped projection that surrounds the opening of the external acoustic meatus. Most of the auricle, including the helix (rim), consists of elastic cartilage covered with skin. Its fleshy, dangling lobule (“earlobe”), however, lacks supporting cartilage. The function of the auricle is to gather and funnel (and thereby amplify) sound waves coming into the external acoustic meatus. Moreover, the way that sound bounces off the ridges and cavities of the auricle provides the brain with clues about whether sounds come from above or below.
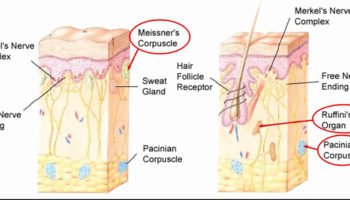
The external ear canal (external acoustic meatus) is a short tube (about 2.5 cm long) running medially, from the auricle to the eardrum. Near the auricle, its wall consists of elastic cartilage, but its medial two-thirds tunnels through the temporal bone. The entire canal is lined with skin that contains hairs, as well as sebaceous glands and modified apocrine sweat glands called ceruminous glands. The ceruminous and sebaceous glands secrete yellow-brown cerumen, or earwax. Earwax traps dust and repels insects, keeping them out of the auditory canal.
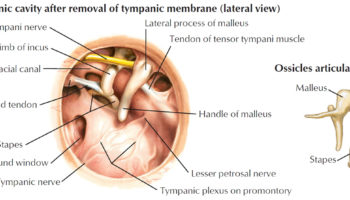
Sound waves entering the external acoustic meatus hit the thin, translucent tympanic membrane, or eardrum (tympanum = drum), which forms the boundary between the external and middle ears. The tympanic membrane is shaped like a flattened cone, the apex of which points medially into the middle ear cavity. Sound waves that travel through the air set the eardrum vibrating, and the eardrum in turn transfers the vibrations to tiny bones in the middle ear.
Figure 1. Outer ear
Figure 2. Ear anatomy
Swimmer’s ear
Swimmer’s ear is an infection in the outer ear canal, which runs from your eardrum to the outside of your head 1. It’s often brought on by water that remains in your ear after swimming, creating a moist environment that aids bacterial growth.
Putting fingers, cotton swabs or other objects in your ears also can lead to swimmer’s ear by damaging the thin layer of skin lining your ear canal 1.
Swimmer’s ear is also known as otitis externa. The most common cause of this infection is bacteria invading the skin inside your ear canal. Usually you can treat swimmer’s ear with eardrops. Prompt treatment can help prevent complications and more-serious infections.
Causes of Swimmer’s ear
Swimmer’s ear is an infection that’s usually caused by bacteria commonly found in water and soil. Infections caused by a fungus or a virus are less common. Swimmer’s ear is more common among children in their teens and young adults. It may occur with a middle ear infection or a respiratory infection such as a cold.
Swimming in unclean water can lead to swimmer’s ear. Bacteria commonly often found in water can cause ear infections. Rarely, the infection may be caused by a fungus.
Other causes of swimmer’s ear include:
- Scratching the ear or inside the ear
- Getting something stuck in the ear
Trying to clean (wax from the ear canal) with cotton swabs or small objects can damage the skin.
Long-term (chronic) swimmer’s ear may be due to:
- Allergic reaction to something placed in the ear
- Chronic skin conditions, such as eczema or psoriasis
Your ear’s natural defenses
Your outer ear canals have natural defenses that help keep them clean and prevent infection. Protective features include:
- Glands that secrete a waxy substance (cerumen). These secretions form a thin, water-repellent film on the skin inside your ear. Cerumen is also slightly acidic, which helps further discourage bacterial growth. In addition, cerumen collects dirt, dead skin cells and other debris and helps move these particles out of your ear. The waxy clump that results is the familiar earwax you find at the opening of your ear canal.
- Downward slope of your ear canal. Your ear canal slopes down slightly from your middle ear to your outer ear, helping water drain out.
How the swimmer’s ear occurs
If you have swimmer’s ear, your natural defenses have been overwhelmed. Conditions that can weaken your ear’s defenses and promote bacterial growth include:
- Excess moisture in your ear. Heavy perspiration, prolonged humid weather or water that remains in your ear after swimming can create a favorable environment for bacteria.
- Scratches or abrasions in your ear canal. Cleaning your ear with a cotton swab or hairpin, scratching inside your ear with a finger, or wearing headphones or hearing aids can cause small breaks in the skin that allow bacteria to grow.
- Sensitivity reactions. Hair products or jewelry can cause allergies and skin conditions that promote infection.
Risk factors for swimmer’s ear
Factors that may increase your risk of swimmer’s ear include:
- Swimming
- Swimming in water with elevated bacteria levels, such as a lake rather than a well-maintained pool
- A narrow ear canal — for example, in a child — that can more easily trap water
- Aggressive cleaning of the ear canal with cotton swabs or other objects
- Use of certain devices, such as headphones or a hearing aid
- Skin allergies or irritation from jewelry, hair spray or hair dyes.
Table 1. Predisposing factors for outer ear infection (swimmer’s ear)
Anatomic abnormalities |
|
|
|
Canal obstruction |
|
|
|
Cerumen/epithelial integrity |
|
|
|
|
Dermatologic conditions |
|
|
|
|
Water in ear canal |
|
|
|
Miscellaneous |
|
|
|
|
Symptoms of Swimmer’s ear
Swimmer’s ear symptoms are usually mild at first, but they may get worse if your infection isn’t treated or spreads. Doctors often classify swimmer’s ear according to mild, moderate and advanced stages of progression.
Mild signs and symptoms
- Itching in your ear canal
- Slight redness inside your ear
- Mild discomfort that’s made worse by pulling on your outer ear (pinna, or auricle) or pushing on the little “bump” (tragus) in front of your ear
- Some drainage of clear, odorless fluid
Moderate progression
- More intense itching
- Increasing pain
- More extensive redness in your ear
- Excessive fluid drainage
- Discharge of pus
- Feeling of fullness inside your ear and partial blockage of your ear canal by swelling, fluid and debris
- Decreased or muffled hearing
Advanced progression
- Severe pain that may radiate to your face, neck or side of your head
- Complete blockage of your ear canal
- Redness or swelling of your outer ear
- Swelling in the lymph nodes in your neck
- Fever
When to see a doctor
See your doctor if you’re experiencing any signs or symptoms of swimmer’s ear, even if they’re mild.
Call your doctor immediately or visit the emergency room if you have:
- Severe pain
- Fever
Complications of Swimmer’s ear
Swimmer’s ear usually isn’t serious if treated promptly, but complications can occur.
- Temporary hearing loss. You may experience muffled hearing that usually gets better after the infection clears up.
- Long-term infection (chronic otitis externa). An outer ear infection is usually considered chronic if signs and symptoms persist for more than three months.
- Chronic infections are more common if there are conditions that make treatment difficult, such as a rare strain of bacteria, an allergic skin reaction, an allergic reaction to antibiotic eardrops, or a combination of a bacterial and fungal infection.
- Deep tissue infection (cellulitis). Rarely, swimmer’s ear may result in the spread of infection into deep layers and connective tissues of the skin.
- Bone and cartilage damage (necrotizing otitis externa). An outer ear infection that spreads can cause inflammation and damage to the skin and cartilage of the outer ear and bones of the lower part of the skull, causing increasingly severe pain. Older adults, people with diabetes or people with weakened immune systems are at increased risk of this complication. Necrotizing otitis externa is also known as malignant otitis externa, but it’s not a cancer.
- More widespread infection. If swimmer’s ear develops into necrotizing otitis externa, the infection may spread and affect other parts of your body, such as the brain or nearby nerves. This rare complication can be life-threatening.
Prevention of Swimmer’s ear
Follow these tips to avoid swimmer’s ear:
- Keep your ears dry. Dry your ears thoroughly after exposure to moisture from swimming or bathing. Dry only your outer ear, wiping it slowly and gently with a soft towel or cloth. Tip your head to the side to help water drain from your ear canal. You can dry your ears with a blow dryer if you put it on the lowest setting and hold it at least a foot (about 0.3 meters) away from the ear.
- At-home preventive treatment. If you know you don’t have a punctured eardrum, you can use homemade preventive eardrops before and after swimming. A mixture of 1 part white vinegar to 1 part rubbing alcohol may help promote drying and prevent the growth of bacteria and fungi that can cause swimmer’s ear. Pour 1 teaspoon (about 5 milliliters) of the solution into each ear and let it drain back out. Similar over-the-counter solutions may be available at your drugstore.
- Swim wisely. Watch for signs alerting swimmers to high bacterial counts and don’t swim on those days.
- DO NOT scratch the ears or insert cotton swabs or other objects in the ears.
- Avoid putting foreign objects in your ear. Never attempt to scratch an itch or dig out earwax with items such as a cotton swab, paper clip or hairpin. Using these items can pack material deeper into your ear canal, irritate the thin skin inside your ear or break the skin.
- Protect your ears from irritants. Put cotton balls in your ears while applying products such as hair sprays and hair dyes.
- Use caution after an ear infection or surgery. If you’ve recently had an ear infection or ear surgery, talk to your doctor before you go swimming.
Diagnosis of swimmer’s ear
Doctors can usually diagnose swimmer’s ear during an office visit. If your infection is at an advanced stage or persists, you may need further evaluation.
Initial testing
Your doctor will likely diagnose swimmer’s ear based on symptoms you report, questions he or she asks, and an office examination. You probably won’t need a lab test at your first visit. Your doctor’s initial evaluation will usually include:
- Examination of your ear canal with a lighted instrument (otoscope). Your ear canal may appear red, swollen and scaly. Flakes of skin and other debris may be present in the ear canal.
- Visualization of your eardrum (tympanic membrane) to be sure it isn’t torn or damaged. If the view of your eardrum is blocked, your doctor will clear your ear canal with a small suction device or an instrument with a tiny loop or scoop on the end (ear curette).
Further testing
Depending on the initial assessment, symptom severity or the stage of your swimmer’s ear, your doctor may recommend additional evaluation.
- If your eardrum is damaged or torn, your doctor will likely refer you to an ear, nose and throat specialist (ENT). The specialist will examine the condition of your middle ear to determine if that’s the primary site of infection. This examination is important because some treatments intended for an infection in the outer ear canal aren’t appropriate for treating the middle ear.
- If your infection doesn’t respond to treatment, your doctor may take a sample of discharge or debris from your ear at a later appointment and send it to a lab to identify the exact microorganism causing your infection.
Table 2. Conditions That May Be Confused with Swimmer’s Ear (Acute Outer Ear Infection)
| Condition | Distinguishing characteristics | Comment |
|---|---|---|
Acute middle ear infection (acute otitis media) | Presence of middle ear effusion, no tragal/pinnal tenderness | Use pneumatic otoscopy or tympanometry, treat with systemic antibiotics |
Chronic outer ear infection (chronic otitis externa) | Itching is often predominant symptom, erythematous canal, lasts more than three months | Treat underlying causes/conditions |
Chronic suppurative middle ear infection (suppurative otitis media) | Chronic otorrhea, nonintact tympanic membrane | Control otitis externa symptoms, then treat otitis media |
Contact dermatitis | Allergic reaction to materials (e.g., metals, soaps, plastics) in contact with the skin/epithelium; itching is predominant symptom | Check for piercings, hearing aids, or earplug use; discontinue exposure when possible |
Eczema | Itching is predominant symptom; often chronic; history of atopy, outbreaks in other locations | Consider treatment with topical corticosteroids |
Furunculosis (pimple or boil in ear canal) | Focal infection, may be pustule or nodule, often in distal canal | Consider treatment with heat, incision and drainage, or systemic antibiotics; can progress to diffuse otitis externa |
Malignant outer ear infection (malignant otitis externa) | High fever, granulation tissue or necrotic tissue in ear canal, may have cranial nerve involvement; patient with diabetes mellitus or immunocompromise, elevated erythrocyte sedimentation rate, findings on computed tomography | Medical emergency with high morbidity rate and possible mortality; warrants emergent consultation with otolaryngologist, hospitalization, intravenous antibiotics, debridement |
Myringitis | Tympanic membrane inflammation, may have vesicles; pain is often severe, no canal edema | Usually results from acute otitis media or viral infection |
Otomycosis (fungal ear infection of the outer ear canal) | Itching is predominant symptom, thick material in canal, less edema; may see fungal elements on otoscopy | Can coexist with bacterial infections; treat with acetic acid (Vosol), half acetic acid/half alcohol, or topical antifungals; meticulous cleaning of ear canal |
Ramsay Hunt syndrome | Herpetic ulcers in canal; may have facial numbness/paralysis, severe pain, loss of taste | Treatment includes antivirals, systemic corticosteroids |
Referred pain | Normal ear examination | Look for other causes based on patterns of referred pain |
Seborrhea | Itching and rash on hairline, face, scalp | Treatment includes lubricating or moisturizing the external auditory canal |
Sensitization to otics | Severe itching, maculopapular or erythematous rash in conchal bowl and canal; may have streak on pinna where preparation contacted skin; vesicles may be present | Type IV delayed hypersensitivity reaction to neomycin or other components of otic solutions; discontinue offending agent; treat with topical corticosteroids |
Treatment for swimmer’s ear
The goal of treatment is to stop the infection and allow your ear canal to heal.
Cleaning
Cleaning your outer ear canal is necessary to help eardrops flow to all infected areas. Your doctor will use a suction device or ear curette to clean away any discharge, clumps of earwax, flaky skin and other debris.
Medications for infection
For most cases of swimmer’s ear, your doctor will prescribe eardrops that have some combination of the following ingredients, depending on the type and seriousness of your infection:
- Acidic solution to help restore your ear’s normal antibacterial environment
- Steroid to reduce inflammation
- Antibiotic to fight bacteria
- Antifungal medication to fight an infection caused by a fungus
Ask your doctor about the best method for taking your eardrops. Some ideas that may help you use eardrops include the following:
- Reduce the discomfort of cool drops by holding the bottle in your hand for a few minutes to bring the temperature of the drops closer to body temperature.
- Lie on your side with your infected ear up for a few minutes to help medication travel through the full length of your ear canal.
- If possible, have someone help you put the drops in your ear.
If your ear canal is completely blocked by swelling, inflammation or excess discharge, your doctor may insert a wick made of cotton or gauze to promote drainage and help draw medication into your ear canal.
If your infection is more advanced or doesn’t respond to treatment with eardrops, your doctor may prescribe oral antibiotics.
Medications for pain
Your doctor may recommend easing the discomfort of swimmer’s ear with over-the-counter pain relievers, such as ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve, others) or acetaminophen (Tylenol, others).
If your pain is severe or your swimmer’s ear is at a more advanced stage, your doctor may prescribe a stronger medication for pain relief.
Helping your treatment work
During treatment, the following steps will help keep your ears dry and avoid further irritation:
- Don’t swim or scuba dive.
- Avoid flying.
- Don’t wear an earplug, hearing aid or headphones before pain or discharge has stopped.
- Avoid getting water in your ear canal when bathing. Use a cotton ball coated with petroleum jelly to protect your ear during a bath.
Prevention of Outer Ear Infection
A number of preventive measures have been recommended, including use of earplugs while swimming, use of hair dryers on the lowest settings and head tilting to remove water from the ear canal, and avoidance of self-cleaning or scratching the ear canal. Acetic acid 2% (Vosol) otic solutions are also used, either two drops twice daily or two to five drops after water exposure. However, no randomized trials have examined the effectiveness of any of these measures.
Chronic Outer Ear Infection
In chronic outer ear infection (chronic otitis externa), the symptoms and signs occur for more than three months. Classic symptoms include itching and mild discomfort; there may also be lichenification on otoscopy.
Treatment of outer ear infection
TOPICAL MEDICATIONS
Topical antimicrobials, with or without topical corticosteroids, are the mainstay of treatment for uncomplicated acute outer ear infection. Topical antimicrobials are highly effective compared with placebo, demonstrating an absolute increase in clinical cure rate of 46 percent or a number needed to treat of slightly more than two 3. Topical agents come in a variety of preparations and combinations; a recent systematic review included 26 different topical interventions 4. In some studies, ophthalmic preparations have been used off-label to treat outer ear infection 5, 4. Ophthalmic preparations may be better tolerated than otic preparations, possibly due to differences in pH between the preparations, and may help facilitate compliance with treatment recommendations. Commonly studied antimicrobial agents include aminoglycosides, polymyxin B, quinolones, and acetic acid. No consistent evidence has shown that any one agent or preparation is more effective than another 3, 6, 5, 4. There is limited evidence that use of acetic acid alone may require two additional days for resolution of symptoms compared with other agents, and that it is less effective if treatment is required for more than seven days 4.
Current guidelines recommend factoring in the risk of adverse effects, adherence issues, cost, patient preference, and physician experience. Some components found in otic preparations may cause contact dermatitis 7. Hypersensitivity to aminoglycosides, particularly neomycin, may develop in up to 15 percent of the population, and has been identified in approximately 30 percent of patients who also have chronic or eczematous outer ear infection 7, 8. Adherence to topical therapy increases with ease of administration, such as less frequent dosing 9. The addition of a topical corticosteroid yields more rapid improvement in symptoms such as pain, canal edema, and erythema. Cost varies considerably for the different preparations.
Outer Ear Infection Pain Relief
Pain is a common symptom of acute outer ear infection and can be debilitating 10. Oral analgesics are the preferred treatment. First-line analgesics include nonsteroidal anti-inflammatory drugs and acetaminophen. When ongoing frequent dosing is required to control pain, medications should be administered on a scheduled rather than as-needed basis. Opioid combination pills may be used when symptom severity warrants. Benzocaine otic preparations may compromise the effectiveness of otic antibiotic drops by limiting contact between the drop and the ear canal. The lack of published data supporting the effectiveness of topical benzocaine preparations in outer ear infection limits the role of such treatments 2.
CLEANING THE EAR CANAL
Acute outer ear infection can be associated with copious material in the ear canal. Consensus guidelines published by the American Academy of Otolaryngology recommend that such material be removed to achieve optimal effectiveness of the topical antibiotics 3, 6. However, no randomized controlled trials have examined the effectiveness of aural toilet, and this is not typically done in most primary care settings 4. Topical medications rely on direct contact with the infected skin of the ear canal; hence, aural toilet takes on greater importance when the volume or thickness of the debris in the ear canal is great. Guidelines recommend aural toilet by gentle lavage suctioning or dry mopping under otoscopic or microscopic visualization to remove obstructing material and to verify tympanic membrane integrity 3. Lavage should be used only if the tympanic membrane is known to be intact, and should not be performed on patients with diabetes because of the potential risk of causing malignant outer ear infection 3. Pain medications may be required during the procedure.
Treatment of chronic outer ear infection
The treatment of chronic outer ear infection depends on the underlying causes. Because most cases are caused by allergies or inflammatory dermatologic conditions, treatment includes the removal of offending agents and the use of topical or systemic corticosteroids. Chronic or intermittent otorrhea over weeks to months, particularly with an open tympanic membrane, suggests the presence of chronic suppurative otitis media (suppurative middle ear infection). Initial treatment efforts are similar to those for acute otitis media. With control of the symptoms of outer ear infection, attention can shift to the management of chronic suppurative otitis media.
Follow-up and Referral
Most patients will experience considerable improvement in symptoms after one day of treatment. If there is no improvement within 48 to 72 hours, physicians should reevaluate for treatment adherence, misdiagnosis, sensitivity to ear drops, or continued canal patency. The physician should consider culturing material from the canal to identify fungal and antibiotic-resistant pathogens if the patient does not improve after initial treatment efforts or has one or more predisposing risk factors, or if there is suspicion that the infection has extended beyond the external auditory canal. There is a lack of data regarding optimal length of treatment; as a general rule, antimicrobial otics should be administered for seven to 10 days, although in some cases complete resolution of symptoms may take up to four weeks 3, 4.
Consultation with an otolaryngologist or infectious disease subspecialist may be warranted if malignant outer ear infection is suspected; in cases of severe disease, lack of improvement or worsening of symptoms despite treatment, and unsuccessful lavage; or if the primary care physician determines that aural toilet or ear wick insertion is warranted, but is unfamiliar with or concerned about performing the procedure.
- Swimmer’s ear. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/swimmers-ear/symptoms-causes/syc-20351682[↩][↩]
- Acute Otitis Externa: An Update. Am Fam Physician. 2012 Dec 1;86(11):1055-1061. http://www.aafp.org/afp/2012/1201/p1055.html[↩][↩][↩]
- Rosenfeld RM, Brown L, Cannon CR, et al.; American Academy of Otolaryngology–Head and Neck Surgery Foundation. Clinical practice guideline: acute otitis externa. Otolaryngol Head Neck Surg. 2006;134(4 suppl):S4–S23.[↩][↩][↩][↩][↩][↩]
- Kaushik V, Malik T, Saeed SR. Interventions for acute otitis externa. Cochrane Database Syst Rev. 2010(1):CD004740.[↩][↩][↩][↩][↩][↩]
- Rosenfeld RM, Singer M, Wasserman JM, Stinnett SS. Systematic review of topical antimicrobial therapy for acute otitis externa. Otolaryngol Head Neck Surg. 2006;134(4 suppl):S24–S48.[↩][↩]
- Hajioff D, Mackeith S. Otitis externa. Clin Evid (Online). 2010.[↩][↩]
- Smith IM, Keay DG, Buxton PK. Contact hypersensitivity in patients with chronic otitis externa. Clin Otolaryngol Allied Sci. 1990;15(2):155–158.[↩][↩]
- Yariktas M, Yildirim M, Doner F, Baysal V, Dogru H. Allergic contact dermatitis prevalence in patients with eczematous external otitis. Asian Pac J Allergy Immunol. 2004;22(1):7–10.[↩]
- Shikiar R, Halpern MT, McGann M, Palmer CS, Seidlin M. The relation of patient satisfaction with treatment of otitis externa to clinical outcomes: development of an instrument. Clin Ther. 1999;21(6):1091–1104.[↩]
- van Asperen IA, de Rover CM, Schijven JF, et al. Risk of otitis externa after swimming in recreational fresh water lakes containing Pseudomonas aeruginosa. BMJ. 1995;311(7017):1407–1410.[↩]