Contents
- What is an echocardiogram
- What does echocardiogram show?
- Echocardiogram with abnormal results
- Who needs an echocardiogram?
- When an echocardiogram is used
- How an echocardiogram is carried out
- Echocardiogram risks or side effects
- Transthoracic echocardiogram
- Transesophageal echocardiogram
What is an echocardiogram
Echocardiogram also called heart ultrasound or “echo”, is a painless test that uses sound waves (ultrasound) to create moving pictures of your heart. An echocardiogram is a type of ultrasound scan, which means a small probe is used to send out high-frequency sound waves that create echoes when they bounce off different parts of the body. These echoes are picked up by the probe and turned into a moving image that’s displayed on a monitor while the scan is carried out. The pictures show the size and shape of your heart and how well the heart chambers and valves are working. They also show how well your heart’s chambers and valves are working. The picture and information an echocardiogram produces is more detailed than a standard x-ray image and an echocardiogram does not expose you to harmful x-ray radiation.
Echocardiogram is the cheapest and least invasive method available for screening cardiac anatomy.
Echocardiogram also can pinpoint areas of heart muscle that aren’t contracting well because of poor blood flow or injury from a previous heart attack. A type of echocardiogram called Doppler ultrasound shows how well blood flows through your heart’s chambers and valves.
Echocardiogram can detect possible blood clots inside the heart, fluid buildup in the pericardium (the sac around the heart), and problems with the aorta. The aorta is the main artery that carries oxygen-rich blood from your heart to your body.
Doctors also use echocardiogram to detect heart problems in infants and children.
An echocardiogram may be requested by a heart specialist (cardiologist) or any doctor who thinks you might have a problem with your heart, including your family physician.
Echocardiogram is usually be carried out at a hospital or clinic by a cardiologist or a trained specialist called a cardiac physiologist.
Although it has a similar name, an echocardiogram isn’t the same as an electrocardiogram (ECG or EKG), which is a test used to check your heart’s rhythm and electrical activity.
Abnormal echocardiogram results may indicate:
- Heart valve disease
- Cardiomyopathy
- Pericardial effusion
- Other heart abnormalities
Echocardiogram test is used to evaluate and monitor many different heart conditions.
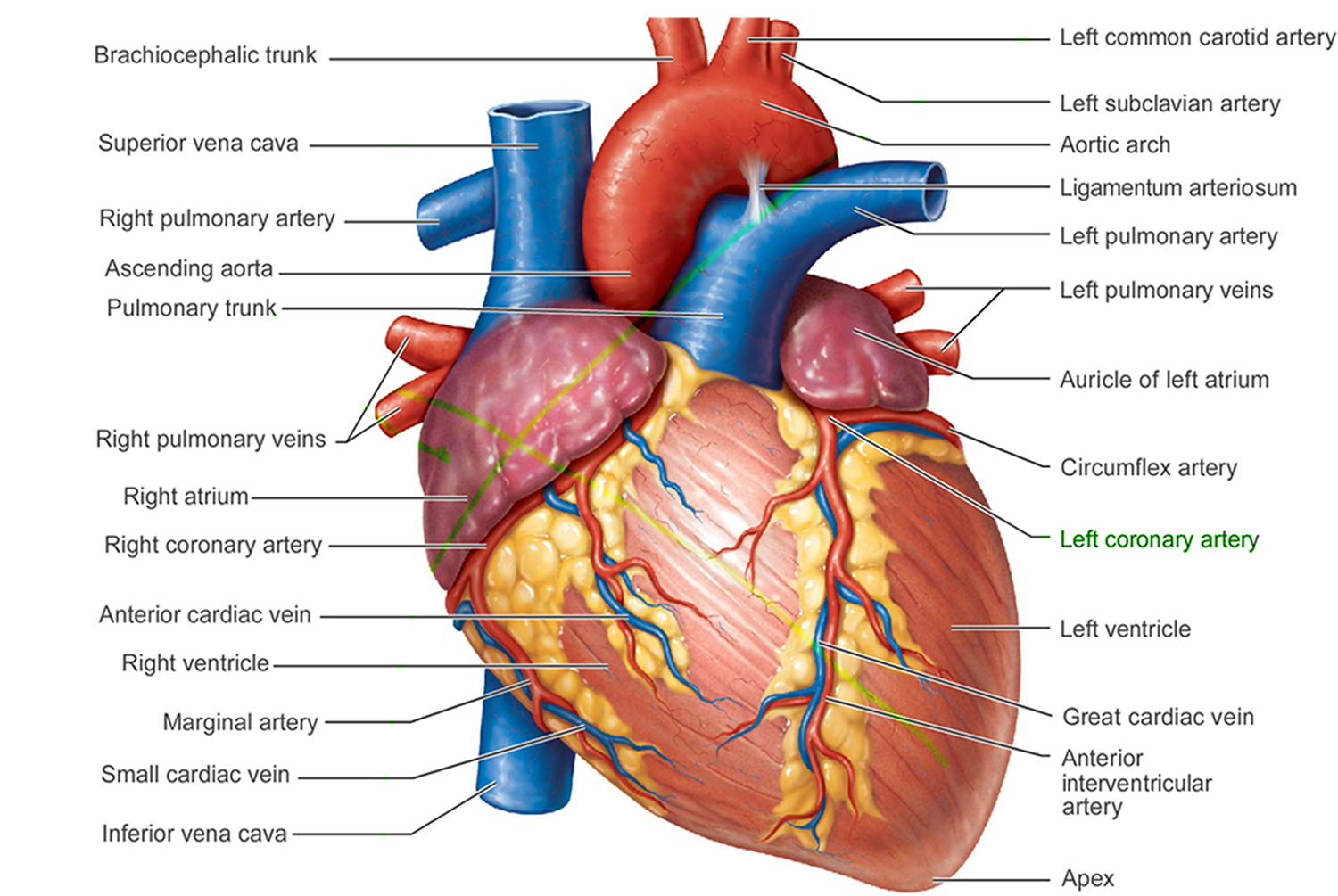
Figure 1. The anatomy of the heart
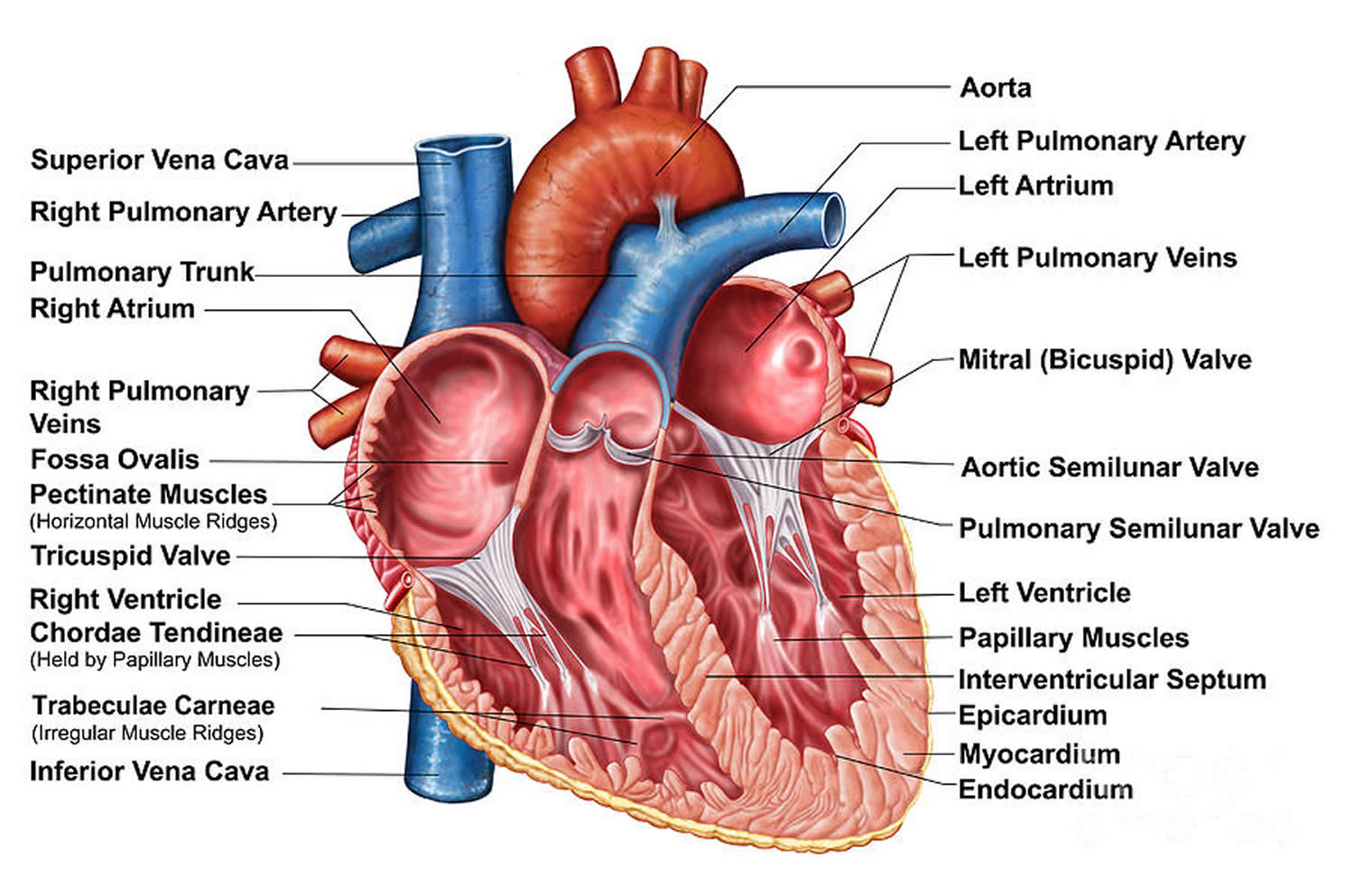
Figure 2. The anatomy of the heart chambers
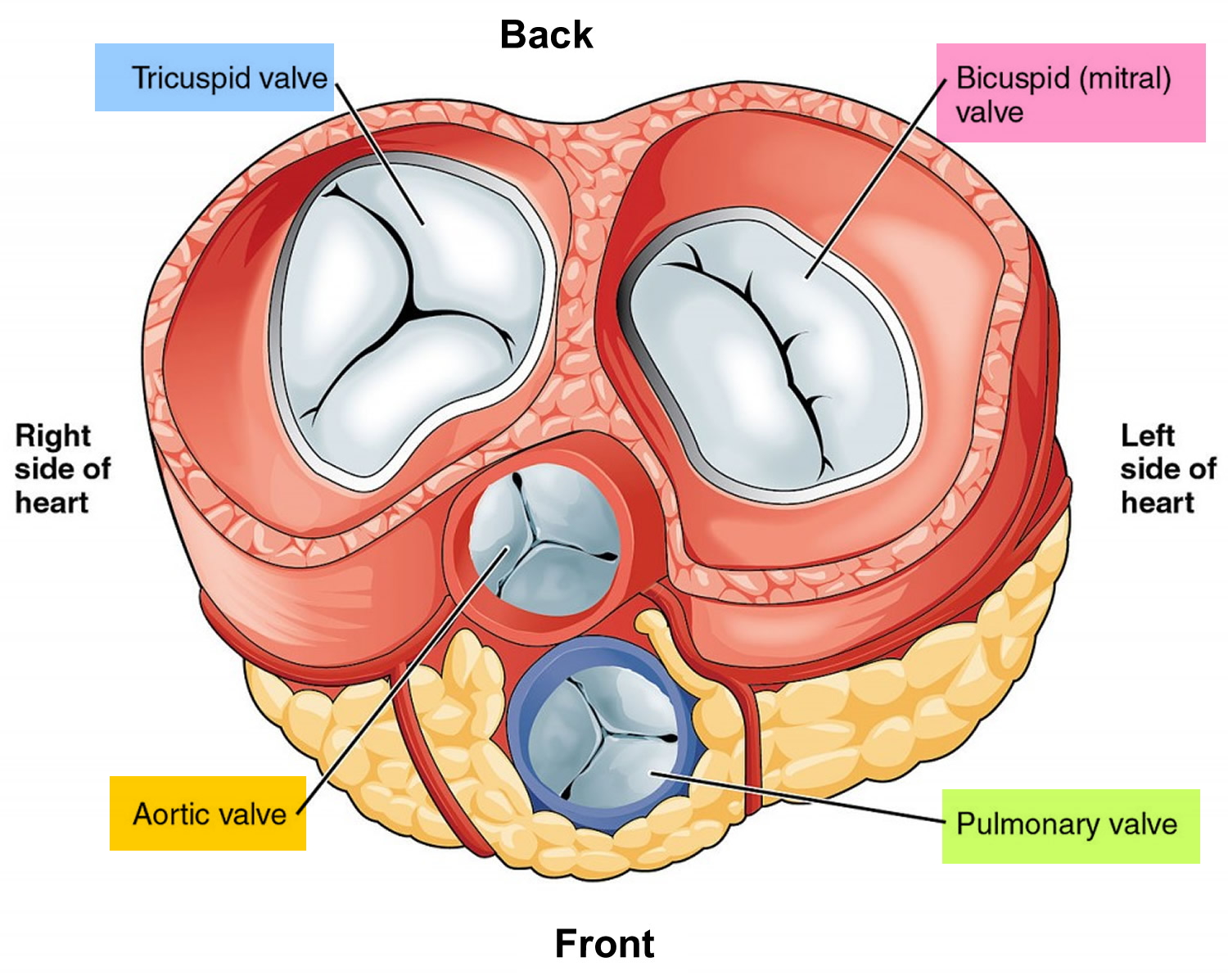
Figure 3. Top view of the 4 heart valves
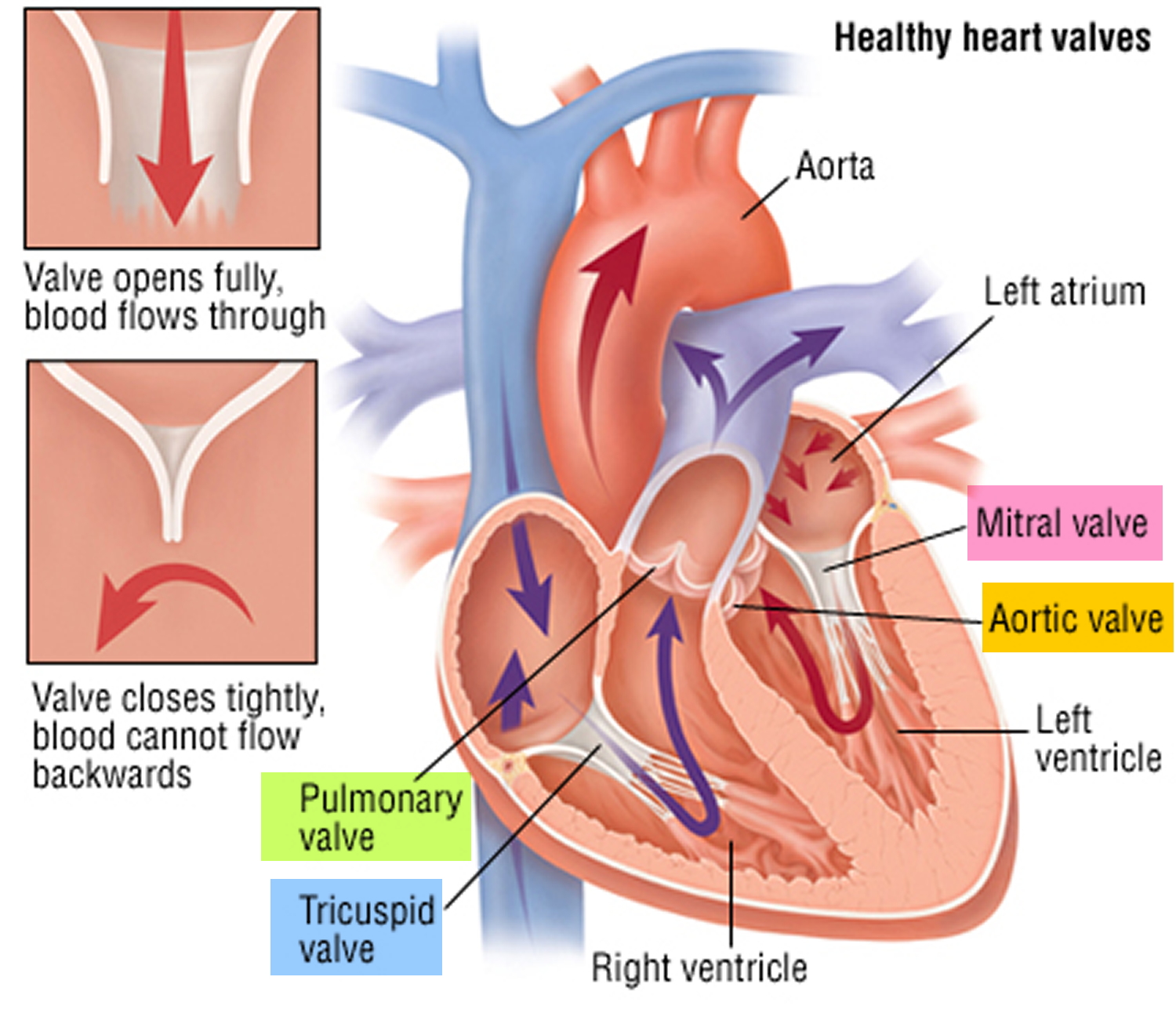
Figure 4. Heart valves function
What does echocardiogram show?
Echocardiogram shows the size, structure, and movement of various parts of your heart. These parts include the heart valves, the septum (the wall separating the right and left heart chambers), and the walls of the heart chambers. Doppler ultrasound shows the movement of blood through your heart.
Your doctor may use echocardiogram to:
- Diagnose heart problems
- Guide or determine next steps for treatment
- Monitor changes and improvement
- Determine the need for more tests
Echocardiogram can detect many heart problems. Some might be minor and pose no risk to you. Others can be signs of serious heart disease or other heart conditions. Your doctor may use echocardiogram to learn about:
- The size of your heart. An enlarged heart might be the result of high blood pressure, leaky heart valves, or heart failure. Echo also can detect increased thickness of the ventricles (the heart’s lower chambers). Increased thickness may be due to high blood pressure, heart valve disease, or congenital heart defects.
- Heart muscles that are weak and aren’t pumping well. Damage from a heart attack may cause weak areas of heart muscle. Weakening also might mean that the area isn’t getting enough blood supply, a sign of coronary heart disease.
- Heart valve problems. Echo can show whether any of your heart valves don’t open normally or close tightly.
- Problems with your heart’s structure. Echo can detect congenital heart defects, such as holes in the heart. Congenital heart defects are structural problems present at birth. Infants and children may have echo to detect these heart defects.
- Blood clots or tumors. If you’ve had a stroke, you may have echo to check for blood clots or tumors that could have caused the stroke.
Echocardiogram with abnormal results
Tetralogy of Fallot with pulmonary atresia: Fetal echocardiogram
3VT view demonstrates reverse filling of the duct, a key feature differentiating this subtype from the more common Tetralogy of Fallot with pulmonary stenosis.
Note that the duct is on the right side of the image, as the fetus is in breech position.
There are a number of different subtypes of tetralogy of Fallot: Tetralogy of Fallot with pulmonary stenosis (75%), Tetralogy of Fallot with pulmonary atresia (20%) and Dysplastic (absent/ring) pumonary valve syndrome (5%).
This case demonstrates the typical findings on the standard fetal echo views in a case of tetralogy of Fallot with pulmonary atresia. The key features that differentiate this from the more common pulmonary stenosis subtype are the absence of the pulmonary trunk on the RVOT view and reverse flow in the ductus appreciated on the 3VT view.
Tetralogy of Fallot with absent pulmonary valve syndrome: fetal echocardiogram. Age: Second trimester
Who needs an echocardiogram?
Your doctor may recommend echocardiogram (echo) if you have signs or symptoms of heart problems.
For example, shortness of breath and swelling in the legs are possible signs of heart failure. Heart failure is a condition in which your heart can’t pump enough oxygen-rich blood to meet your body’s needs. Echo can show how well your heart is pumping blood.
Echocardiogram also can help your doctor find the cause of abnormal heart sounds, such as heart murmurs. Heart murmurs are extra or unusual sounds heard during the heartbeat. Some heart murmurs are harmless, while others are signs of heart problems.
Your doctor also may use echocardiogram to learn about:
- The size of your heart. An enlarged heart might be the result of high blood pressure, leaky heart valves, or heart failure. Echo also can detect increased thickness of the ventricles (the heart’s lower chambers). Increased thickness may be due to high blood pressure, heart valve disease, or congenital heart defects.
- Heart muscles that are weak and aren’t pumping well. Damage from a heart attack may cause weak areas of heart muscle. Weakening also might mean that the area isn’t getting enough blood supply, a sign of coronary heart disease.
- Heart valve problems. Echo can show whether any of your heart valves don’t open normally or close tightly.
- Problems with your heart’s structure. Echo can detect congenital heart defects, such as holes in the heart. Congenital heart defects are structural problems present at birth. Infants and children may have echo to detect these heart defects.
- Blood clots or tumors. If you’ve had a stroke, you may have echo to check for blood clots or tumors that could have caused the stroke.
Your doctor also might recommend echo to see how well your heart responds to certain heart treatments, such as those used for heart failure.
When an echocardiogram is used
An echocardiogram can help diagnose and monitor certain heart conditions by checking the structure of the heart and surrounding blood vessels, analyzing how blood flows through them, and assessing the pumping chambers of the heart.
An echocardiogram can help detect:
- Damage from a heart attack – where the supply of blood to the heart was suddenly blocked
- Heart failure – where the heart fails to pump enough blood around the body at the right pressure
- Congenital heart disease – birth defects that affect the normal workings of the heart
- Problems with the heart valves – problems affecting the valves that control the flow of blood within the heart
- Cardiomyopathy – where the heart walls become thickened or enlarged
- Endocarditis – an infection of the heart valves
An echocardiogram can also help your doctors decide on the best treatment for these conditions.
How an echocardiogram is carried out
There are several different ways an echocardiogram can be carried out, but most people will have what’s known as a transthoracic echocardiogram (TTE). This procedure is outlined below.
You won’t usually need to do anything to prepare for the test, unless you’re having a transesophageal echocardiogram (TEE).
The type of echocardiogram you will have depends on the heart condition being assessed and how detailed the images need to be.
For example, a stress echocardiogram may be recommended if your heart problem is triggered by physical activity, while the more detailed images produced by a transesophageal echocardiogram (TEE) may be more useful in helping plan heart surgery.
Echocardiogram types
There are several types of echocardiography (echo)—all use sound waves to create moving pictures of your heart. This is the same technology that allows doctors to see an unborn baby inside a pregnant woman.
Unlike x rays and some other tests, echocardiogram doesn’t involve radiation.
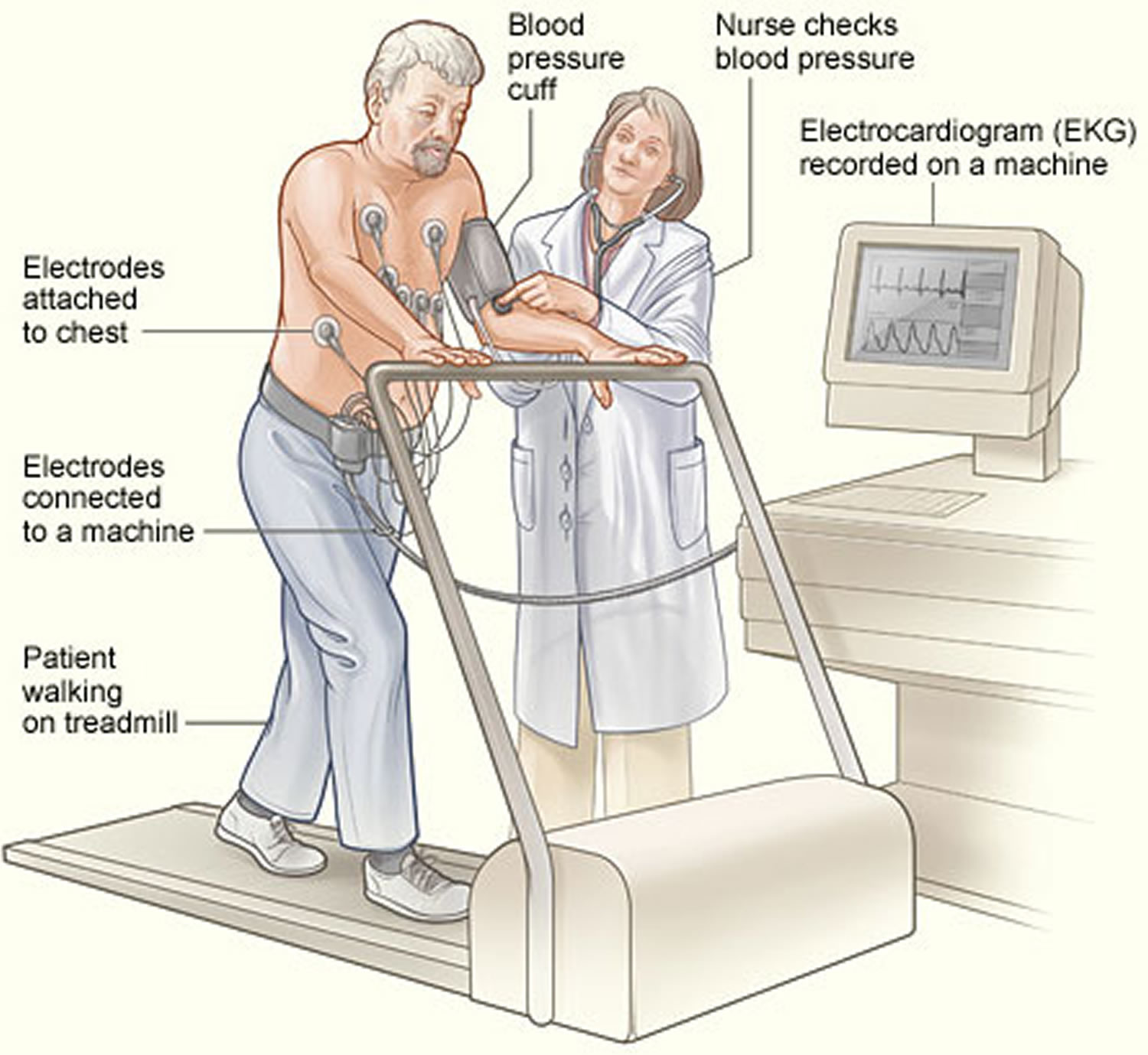
Stress echocardiogram
Stress echocardiogram uses an ultrasound to detect differences in your heart’s chambers and valves and how strongly your heart beats when exercised – during or just after a period of exercise on a treadmill or exercise bike or when stressed using a medicine (e.g. dobutamine) that is given via an injection to make your heart work harder. A radioactive substance (a tracer) is usually injected into your bloodstream as well. Stress echocardiogram will show how your heart works during exercise or stress.
Stress testing provides information about how your heart works during physical stress. Some heart problems are easier to diagnose when your heart is working hard and beating fast.
During stress testing, you exercise (walk or run on a treadmill or pedal a stationary bike) to make your heart work hard and beat fast. Tests are done on your heart while you exercise.
You might have arthritis or another medical problem that prevents you from exercising during a stress test. If so, your doctor may give you medicine to make your heart work hard, as it would during exercise. This is called a pharmacological stress test.
Doctors usually use stress testing to help diagnose coronary heart disease (coronary artery disease). They also use stress testing to find out the severity of coronary heart disease (coronary artery disease).
Coronary heart disease (coronary artery disease) is a disease in which a waxy substance called plaque builds up in the coronary arteries. These arteries supply oxygen-rich blood to your heart.
Plaque narrows the arteries and reduces blood flow to your heart muscle. The buildup of plaque also makes it more likely that blood clots will form in your arteries. Blood clots can mostly or completely block blood flow through an artery. This can lead to chest pain called angina (an-JI-nuh or AN-juh-nuh) or a heart attack.
You may not have any signs or symptoms of coronary heart disease (coronary artery disease) when your heart is at rest. But when your heart has to work harder during exercise, it needs more blood and oxygen. Narrow arteries can’t supply enough blood for your heart to work well. As a result, signs and symptoms of coronary heart disease (coronary artery disease) may occur only during exercise.
A stress test can detect the following problems, which may suggest that your heart isn’t getting enough blood during exercise:
- Abnormal changes in your heart rate or blood pressure
- Symptoms such as shortness of breath or chest pain, especially if they occur at low levels of exercise
- Abnormal changes in your heart’s rhythm or electrical activity
During a stress test, if you can’t exercise for as long as what is considered normal for someone your age, it may be a sign that not enough blood is flowing to your heart. However, other factors besides coronary heart disease (coronary artery disease) can prevent you from exercising long enough (for example, lung disease, anemia, or poor general fitness).
Doctors also may use stress testing to assess other problems, such as heart valve disease or heart failure.
A stress echocardiogram also can show areas of poor blood flow to your heart, dead heart muscle tissue, and areas of the heart muscle wall that aren’t contracting well. These areas may have been damaged during a heart attack, or they may not be getting enough blood.
Other imaging stress tests use radioactive dye to create pictures of blood flow to your heart. The dye is injected into your bloodstream before the pictures are taken. The pictures show how much of the dye has reached various parts of your heart during exercise and while you’re at rest.
Tests that use radioactive dye include a thallium or sestamibi stress test and a positron emission tomography (PET) stress test. The amount of radiation in the dye is considered safe for you and those around you. However, if you’re pregnant, you shouldn’t have this test because of risks it might pose to your unborn child.
Imaging stress tests tend to detect coronary artery disease better than standard (nonimaging) stress tests. Imaging stress tests also can predict the risk of a future heart attack or premature death.
An imaging stress echocardiogram might be done first (as opposed to a standard exercise stress test) if you:
- Can’t exercise for enough time to get your heart working at its hardest. (Medical problems, such as arthritis or leg arteries clogged by plaque, might prevent you from exercising long enough.)
- Have abnormal heartbeats or other problems that prevent a standard exercise stress test from giving correct results.
- Had a heart procedure in the past, such as coronary artery bypass grafting or percutaneous coronary intervention, also known as coronary angioplasty, and stent placement.
What does stress testing show?
Stress testing shows how your heart works during physical stress (exercise) and how healthy your heart is.
A standard exercise stress test uses an EKG (electrocardiogram) to monitor changes in your heart’s electrical activity. Imaging stress tests take pictures of blood flow throughout your heart. They also show your heart valves and the movement of your heart muscle.
Doctors use both types of stress tests to look for signs that your heart isn’t getting enough blood flow during exercise. Abnormal test results may be due to coronary heart disease (coronary artery disease) or other factors, such as poor physical fitness.
If you have a standard exercise stress test and the results are normal, you may not need further testing or treatment. But if your test results are abnormal, or if you’re physically unable to exercise, your doctor may want you to have an imaging stress test or other tests.
Even if your standard exercise stress test results are normal, your doctor may want you to have an imaging stress echocardiogram if you continue having symptoms (such as shortness of breath or chest pain).
Imaging stress echocardiogram is more accurate than standard exercise stress tests, but they’re much more expensive.
Imaging stress echocardiogram shows how well blood is flowing in the heart muscle and reveal parts of the heart that aren’t contracting strongly. They also can show the parts of the heart that aren’t getting enough blood, as well as dead tissue in the heart, where no blood flows. (A heart attack can cause heart tissue to die.)
If your imaging stress echocardiogram suggests significant coronary heart disease (coronary artery disease), your doctor may want you to have more testing and treatment.
Who Needs Stress Testing?
You may need stress testing if you’ve had chest pains, shortness of breath, or other symptoms of limited blood flow to your heart.
Imaging stress tests, especially, can show whether you have coronary heart disease or a heart valve problem. (Heart valves are like doors; they open and shut to let blood flow between the heart’s chambers and into the heart’s arteries. So, like coronary heart disease, faulty heart valves can limit the amount of blood reaching your heart.)
If you’ve been diagnosed with coronary heart disease or recently had a heart attack, a stress test can show whether you can handle an exercise program. If you’ve had percutaneous coronary intervention, also known as coronary angioplasty, (with or without stent placement) or coronary artery bypass grafting, a stress test can show how well the treatment relieves your coronary heart disease symptoms.
You also may need a stress test if, during exercise, you feel faint, have a rapid heartbeat or a fluttering feeling in your chest, or have other symptoms of an arrhythmia (an irregular heartbeat).
If you don’t have chest pain when you exercise but still get short of breath, your doctor may recommend a stress test. The test can help show whether a heart problem, rather than a lung problem or being out of shape, is causing your breathing problems.
For such testing, you breathe into a special tube. This allows a technician to measure the gases you breathe out. Breathing into the tube during stress testing also is done before a heart transplant to help assess whether you’re a candidate for the surgery.
Stress testing shouldn’t be used as a routine screening test for coronary heart disease. Usually, you have to have symptoms of coronary heart disease before a doctor will recommend stress testing.
However, your doctor may want to use a stress test to screen for coronary heart disease if you have diabetes. This disease increases your risk of coronary heart disease. Currently, though, no evidence shows that having a stress test will improve your outcome if you have diabetes.
Stress testing risks
Stress tests pose little risk of serious harm. The chance of these tests causing a heart attack or death is about 1 in 5,000. More common, but less serious side effects linked to stress testing include:
- An arrhythmia (irregular heartbeat). Often, an arrhythmia will go away quickly once you’re at rest. But if it persists, you may need monitoring or treatment in a hospital.
- Low blood pressure, which can cause you to feel dizzy or faint. This problem may go away once your heart stops working hard; it usually doesn’t require treatment.
- Jitteriness or discomfort while getting medicine to make your heart work hard and beat fast (you may be given medicine if you can’t exercise). These side effects usually go away shortly after you stop getting the medicine. Sometimes the symptoms may last a few hours.
Also, some of the medicines used for pharmacological stress tests can cause wheezing, shortness of breath, and other asthma-like symptoms. Sometimes these symptoms are severe and require treatment.
What to expect before stress testing
Stress testing is done in a doctor’s office or at a medical center or hospital. You should wear shoes and clothes in which you can exercise comfortably. Sometimes you’re given a gown to wear during the test.
Your doctor might ask you to fast (not eat or drink anything but water) for a short time before the test. If you’re diabetic, ask your doctor whether you need to adjust your medicines on the day of the test.
For some stress tests, you can’t drink coffee or other caffeinated drinks for a day before the test. Certain over-the-counter or prescription medicines also may interfere with some stress tests. Ask your doctor whether you need to avoid certain drinks or food or change how you take your medicine before the test.
If you use an inhaler for asthma or other breathing problems, bring it to the test. Make sure you let the doctor know that you use it.
What to expect during stress testing
During all types of stress testing, a doctor, nurse, or technician will always be with you to closely check your health status.
Before you start the “stress” part of a stress test, the nurse will put sticky patches called electrodes on the skin of your chest, arms, and legs. To help an electrode stick to the skin, the nurse may have to shave a patch of hair where the electrode will be attached.
The electrodes will be connected to an EKG (electrocardiogram) machine. This machine records your heart’s electrical activity. It shows how fast your heart is beating and the heart’s rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through your heart.
The nurse will put a blood pressure cuff on your arm to check your blood pressure during the stress test. (The cuff will feel tight on your arm when it expands every few minutes.) Also, you might have to breathe into a special tube so the gases you breathe out can be measured.
Next, you’ll exercise on a treadmill or stationary bike. If such exercise poses a problem for you, you might turn a crank with your arms instead. During the test, the exercise level will get harder. You can stop whenever you feel the exercise is too much for you.
If you can’t exercise, medicine might be injected into a vein in your arm or hand. The medicine will increase blood flow through your coronary arteries and make your heart beat fast, as it would during exercise. You can then have the stress test.
The medicine may make you flushed and anxious, but the effects go away as soon as the test is over. The medicine also may give you a headache.
While you’re exercising or getting medicine to make your heart work harder, the nurse will ask you how you’re feeling. You should tell him or her if you feel chest pain, short of breath, or dizzy.
Figure 5. Exercise stress test – the image shows a patient having a stress test. Electrodes are attached to the patient's chest and connected to an EKG (electrocardiogram) machine. The EKG records the heart’s electrical activity. A blood pressure cuff is used to record the patient’s blood pressure while he walks on a treadmill.
The exercise or medicine infusion will continue until you reach a target heart rate, or until you:
- Feel moderate to severe chest pain
- Get too out of breath to continue
- Develop abnormally high or low blood pressure or an arrhythmia (an irregular heartbeat)
- Become dizzy
The nurse will continue to check your heart functions and blood pressure after the test until they return to normal levels.
The “stress” part of a stress test (when your heart is working hard) usually lasts about 15 minutes or less.
However, there’s prep time before the test and monitoring time afterward. Both extend the total test time to about an hour for a standard stress test, and up to 3 hours or more for some imaging stress tests.
For an exercise stress echocardiogram test, the nurse will take pictures of your heart using echocardiography before you exercise and as soon as you finish.
A sonographer (a person who specializes in using ultrasound techniques) will apply gel to your chest. Then, he or she will briefly put a transducer (a wand-like device) against your chest and move it around.
The transducer sends and receives high-pitched sounds that you probably won’t hear. The echoes from the sound waves are converted into moving pictures of your heart on a screen.
You might be asked to lie on your side on an exam table for this test. Some stress echocardiogram tests also use dye to improve imaging. The dye is injected into your bloodstream while the test occurs.
Sestamibi or Other Imaging Stress Tests Involving Radioactive Dye
For a sestamibi stress test or other imaging stress test that uses radioactive dye, the nurse will inject a small amount of dye into your bloodstream. This is done through a needle placed in a vein in your arm or hand.
You’ll get the dye about a half-hour before you start exercising or take medicine to make your heart work hard. The amount of radiation in the dye is considered safe for you and those around you. However, if you’re pregnant, you shouldn’t have this test because of risks it might pose to your unborn child.
Pictures will be taken of your heart at least two times: when it’s at rest and when it’s working its hardest. You’ll lie down on a table, and a special camera or scanner that can detect the dye in your bloodstream will take pictures of your heart.
Some pictures may not be taken until you lie quietly for a few hours after the stress test. Some patients may even be asked to return in a day or so for more pictures.
What to expect after stress testing
After stress testing, you’ll be able to return to your normal activities. If you had a test that involved radioactive dye, your doctor may ask you to drink plenty of fluids to flush it out of your body. You shouldn’t have certain other imaging tests until the dye is no longer in your body. Your doctor can advise you further.
Contrast echocardiogram
In contrast echocardiogram a harmless substance called a contrast agent is injected into your bloodstream before an echocardiogram is carried out; this substance shows up clearly on the scan and can help create a better image of your heart.
Fetal echocardiogram
Fetal echo is used to look at an unborn baby’s heart. A doctor may recommend this test to check a baby for heart problems. When recommended, the test is commonly done at about 18 to 22 weeks of pregnancy. For this test, the transducer is moved over the pregnant woman’s belly.
Three-Dimensional echocardiogram
A three-dimensional (3D) echocardiogram creates 3D images of your heart. These detailed images show how your heart looks and works.
During transthoracic echocardiogram or transesophageal echocardiogram, 3D images can be taken as part of the process used to do these types of echo.
Doctors may use 3D echocardiogram to diagnose heart problems in children. They also may use 3D echocardiogram for planning and overseeing heart valve surgery.
Researchers continue to study new ways to use 3D echocardiogram.
Echocardiogram risks or side effects
A standard echocardiogram is a simple, painless and safe procedure. There are no side effects from the scan, although the lubricating gel may feel cold and you may experience some minor discomfort when the electrodes are removed from your skin at the end of the test.
Unlike some other tests and scans, such as X-rays and computerised tomography (CT) scans, no radiation is used during an echocardiogram. However, there are some risks associated with the less common types of echocardiogram.
You may find the transesophageal echocardiogram (TEE) procedure uncomfortable and your throat may feel sore for a few hours afterwards. You won’t be able to drive for 24 hours after the test as you may still feel drowsy from the sedative. There’s also a small chance of the probe damaging your throat.
During a stress echocardiogram, you may feel sick and dizzy and you may experience some chest pain. There’s also a small chance of the procedure triggering an irregular heartbeat or heart attack, but you’ll be monitored carefully during the test and it will be stopped if there are signs of any problems.
Some people have a reaction to the contrast agent used during a contrast echocardiogram. This will often only cause mild symptoms such as itching, but in rare cases a serious allergic reaction can occur.
Transthoracic echocardiogram
When an echocardiogram is done with the transducer placed on the chestwall, outside of your body it’s called transthoracic echocardiogram (TTE) or “surface echocardiogram”. Transthoracic echocardiogram (TTE) is painless and noninvasive. “Noninvasive” means that no surgery is done and no instruments are inserted into your body.
Transthoracic echocardiogram (TTE) is the most commonly performed cardiac ultrasound examination. A high quality transthoracic echocardiogram (TTE) can be performed quickly at the bedside and has the potential to comprehensively evaluate left and right ventricular systolic and diastolic function, regional wall motion, valvular heart disease, and diseases of the pericardium.
Transthoracic echocardiogram is the type of echocardiogram that most people will have.
- A trained sonographer performs the test. A heart doctor (cardiologist) interprets the results.
- An instrument called a transducer is placed on various locations on your chest and upper abdomen and directed toward the heart. This device releases high-frequency sound waves.
- The transducer picks up the echoes of sound waves and transmits them as electrical impulses. The echocardiography machine converts these impulses into moving pictures of the heart. Still pictures are also taken.
- Pictures can be two-dimensional or three-dimensional. The type of picture will depend on the part of the heart being evaluated and the type of machine.
- A Doppler echocardiogram evaluates the motion of blood through the heart.
An echocardiogram shows the heart while it is beating. It also shows the heart valves and other structures.
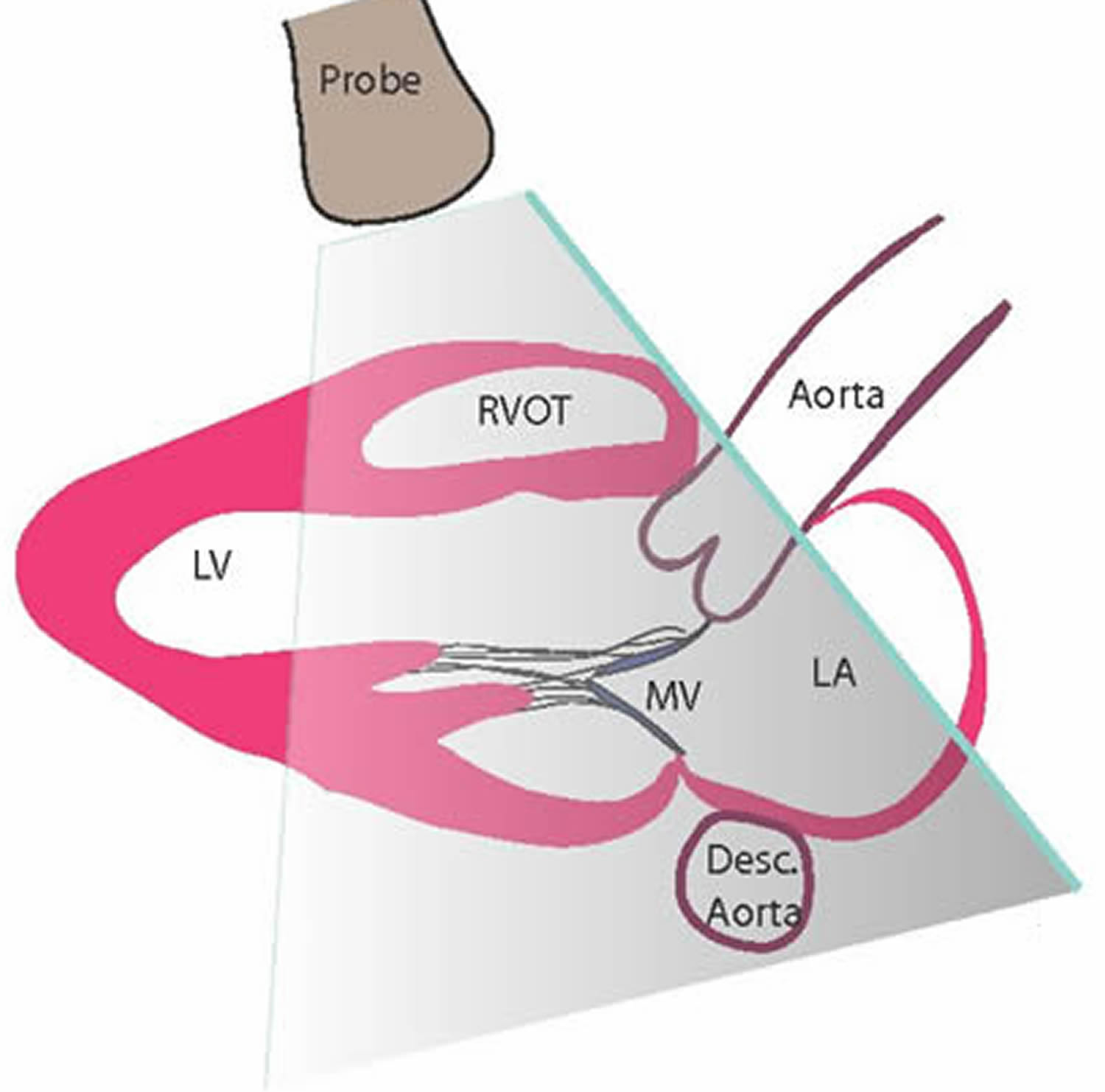
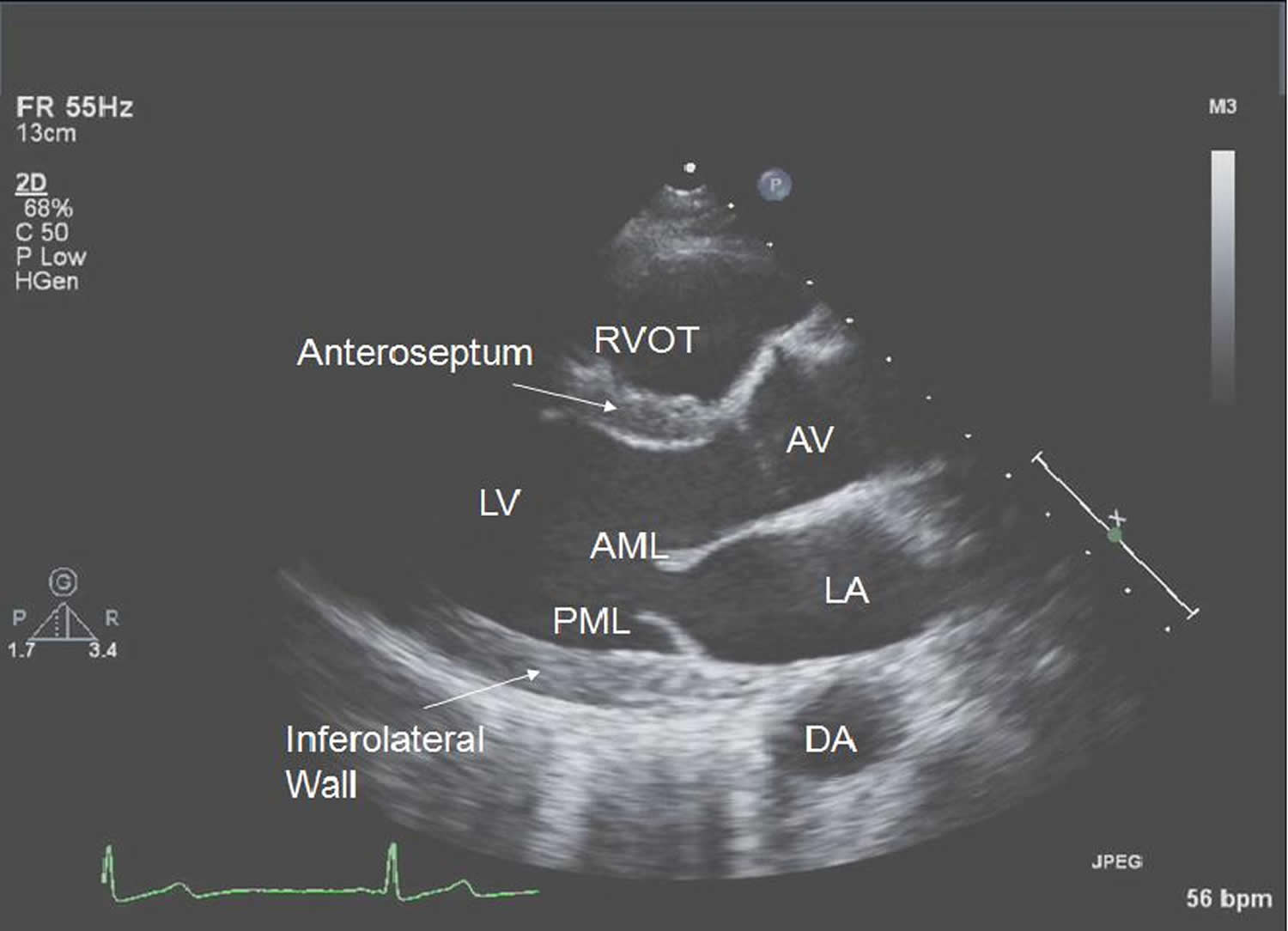
The transthoracic echocardiogram (TTE) has been largely standardized across institutions, such that images are generally obtained from at least 4 separate standard transducer positions which allow for different portions of the heart to be visualized in detail. These standard positions are the parasternal position (which has both long axis and short axis views), apical position , subcostal position and the suprasternal notch position.
In addition to appreciating the power of a transthoracic echocardiogram, after performing transthoracic echocardiograms you will also come to realize the limitations of this technique. Many patients will have suboptimal or in some cases minimal acoustic windows for ultrasound examination and this has been a source of much frustration for technologists and cardiology fellows. In some cases, your lungs, ribs, or body tissue may prevent the sound waves and echoes from providing a clear picture of heart function. For example, patients who are obese, those who have chronic lung disease, who are imaged supine or on a ventilator, or those who are recently post-op from cardiac or thoracic surgery will often have limited windows and possibly uninterpretable images no matter how skilled the sonographer. If this is a problem, the health care provider may inject a small amount of liquid (contrast) through an IV (intravenously) to better see the inside of the heart. Some of these limitations can be overcome with off axis imaging or with transesophageal echocardiogram (TEE) imaging if needed.
Figure 6. Transthoracic echocardiogram – the illustration shows a patient having echocardiography. The patient lies on his left side. A sonographer moves the transducer on the patient’s chest, while viewing the echo pictures on a computer.
Figure 7. Transthoracic echocardiogram – As one can see, the most anterior structure is the right ventricular outflow tract (RVOT), just below the pulmonary artery and in the far field you have the left ventricle (LV), left atrium (LA) and descending aorta (desc. aorta).
Figure 8. Transthoracic echocardiogram standard parasternal long axis view
Notes: In the appropriate standard view shown above, the apex should not be visible. The left ventricle should be oriented almost horizontally. The right ventricular outflow tract [RVOT], left ventricular anteroseptum and inferolateral wall are visualized here as shown above with other key structures labeled. Note the RVOT is seen, and not the right ventricle. Posterior to the left atrium one can sometimes see the proximal descending thoracic aorta. RVOT – right ventricular outflow tract, AML – anterior mitral valve leaflet, PML – posterior mitral valve leaflet, LA – left atrium, LV – left ventricle, AV – aortic valve, and DA – descending aorta.
For a transthoracic echocardiogram, you’ll be asked to remove any clothing covering your upper half before lying down on a bed. You may be offered a hospital gown to cover yourself during the test.
When you’re lying down, several small sticky sensors called electrodes will be attached to your chest to allow an EKG (electrocardiogram) to be done. An EKG is a test that records the heart’s electrical activity. These will be connected to a machine that monitors your heart rhythm during the test.
A doctor or sonographer (a person specially trained to do ultrasounds) will apply lubricating gel to your chest or directly to the ultrasound probe. The gel helps the sound waves reach your heart. You’ll be asked to lie on your left side and the probe called a transducer will be moved across your chest. The transducer transmits ultrasound waves into your chest. A computer will convert echoes from the sound waves into pictures of your heart on a screen. During the test, the lights in the room will be dimmed so the computer screen is easier to see.
The transducer is attached by a cable to a nearby machine that will display and record the images produced.
You won’t hear the sound waves produced by the probe, but you may hear a swishing noise during the scan. This is normal and is just the sound of the blood flow through your heart being picked up by the probe.
The sonographer will record pictures of various parts of your heart. He or she will put the recordings on a computer disc for a cardiologist (heart specialist) to review.
During the test, you may be asked to change positions or hold your breath for a short time. This allows the sonographer to get better pictures of your heart.
At times, the sonographer may apply a bit of pressure to your chest with the transducer. You may find this pressure a little uncomfortable, but it helps get the best picture of your heart. You should let the sonographer know if you feel too uncomfortable.
The process described above is similar to the process for fetal echocardiogram. For that test, however, the transducer is placed over the pregnant woman’s belly at the location of the baby’s heart.
How long does an transthoracic echocardiogram take?
The whole procedure will usually take between 15 and 60 minutes, and you’ll normally be able to go home shortly afterwards.
Transthoracic echocardiogram results
In some cases, it may be possible for the person carrying out the scan to discuss the results with you soon after it’s finished.
However, the images from the scan will usually need to be analyzed before the results are sent to the doctor who requested the test. Your doctor will then discuss the results with you during your next appointment.
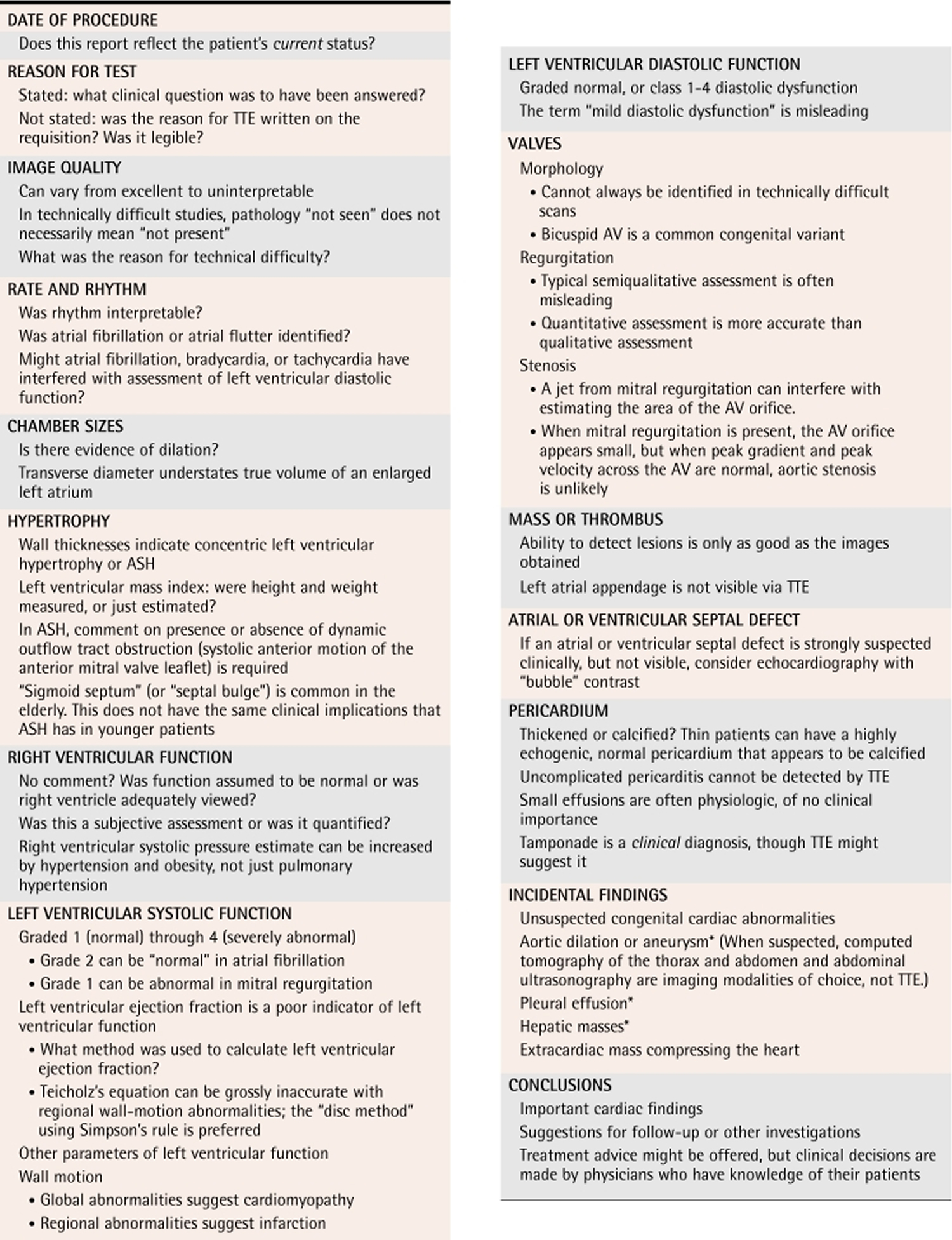
Content of transthoracic echocardiogram reports
- 1) Date of procedure
Before studying a transthoracic echocardiogram (TTE) report, check its date. Even recent studies can convey outdated impressions. Change is expected when a patient’s clinical status changes as a result of worsening disease or in response to treatment.
- 2) Reason for the test
Explaining why transthoracic echocardiogram (TTE) was ordered directs the laboratory to specific techniques that can best answer a referring physician’s question. Sometimes the referring physician must provide data before a conclusion can be reached. Knowing the type and diameter of a prosthetic valve is prerequisite to quantifying its function. If trends in improvement or deterioration are of interest, consultants need results of previous studies.
- 3) Image quality
With excellent, good, or satisfactory images, measurements in transthoracic echocardiogram are presumed accurate. Images characterized as technically difficult, fair, or poor can lead to erroneous conclusions. An error of only 1 mm in measuring wall thickness for the left ventricle (LV) translates into a 15-g difference in the estimate of left ventricle (LV) mass 1. A report stating honestly that accurate data could not be obtained is preferable to a seemingly more “complete” analysis based on inaccurate measurements.
Qualitative conclusions also depend on image quality. A statement that “no intracardiac mass or thrombus was seen” implies no more than it states. It cannot be inferred with certainty from technically difficult transthoracic echocardiogram reports that no such lesion exists.
When image quality is unsatisfactory, the reason should be indicated. Referring physicians can decide whether invasive and more costly transesophageal echocardiography would be justified to obtain betransthoracic echocardiogramr images.
- 4) Rate and rhythm
Correct identification of common dysrhythmias has important implications for transthoracic echocardiogram. Mild (grade II) left ventricle (LV) systolic dysfunction with global hypokinesis is often consistent with a normal myocardium in atrial fibrillation, when the observation has no other meaning unless specific segmental wall motion defects are also identified. In atrial fibrillation, marked bradycardia or tachycardia (data commonly used to assess diastolic function of the LV) are often abnormal—not necessarily because of LV diastolic dysfunction.
During transthoracic echocardiogram a rhythm strip is obtained. Sometimes cardiac rhythm is uninterpretable from a low-voltage rhythm strip, and a consultant might recommend a full electrocardiogram.
- 5) Chamber sizes
A table often lists the measured chamber sizes (diameters) and compares them with normal values. Increased values indicate chamber dilation.
- 6) Hypertrophy
The thicknesses of the interventricular septum and posterior left ventricle (LV) wall are used to determine the presence of concentric left ventricle (LV) hypertrophy or asymmetric septal hypertrophy. This practice can be misleading. Elderly patients often have a sigmoid-shaped septum that looks abnormally thick in most views 2. When asymmetric septal hypertrophy is identified, evaluation for dynamic left ventricle (LV) outflow tract obstruction is required; specific comment regarding presence or absence of systolic anterior motion of the anterior mitral valve leaflet is expected.
Because the mass of a normal heart correlates with the size of the patient, the left ventricle (LV) mass index in g/m2 is useful, because it relates LV mass to body surface area. Did laboratory staff measure the patient’s height and weight, or did they merely ask the patient to estimate them? Inaccurate self-reporting leads to inaccurate calculations.
- 7) Left ventricular systolic function
Left ventricular systolic performance has long been known to indicate severity of heart disease and to predict cardiovascular morbidity and mortality. Left ventricular systolic dysfunction is assessed using the ejection fraction (the percentage of the end diastolic volume ejected during systole). In most cases, this is estimated by eye from all the available echo views. A normal ejection fraction is 50%–80%, but values as low as 5% are compatible with life (end-stage heart failure) 3. A transthoracic echocardiogram report usually classifies LV ejection fraction (LVEF) from normal (grade 1) through severely decreased (grade 4). Most laboratories quantify LV ejection fraction (LVEF). For normal hearts, the Teicholz equation is reasonably accurate 4. When infarction has caused regional wall motion abnormalities, the “disc method” using Simpson’s rule is preferred 5. Reports should indicate which method was employed.
How LV ejection fraction (LVEF) should be interpreted depends on a patient’s clinical status and cardiac condition. While LV ejection fraction (LVEF) in the range of 40% to 55% is abnormal, it often has little clinical significance 6. In moderate or severe mitral regurgitation, however, even a nominally “normal” LVEF of 60% can indicate inadequate left ventricle (LV) performance.
Left ventricular ejection fraction is a misleading indicator of left ventricle (LV) function. It neither reflects myocardial contractility nor measures cardiac performance. Most importantly, LV ejection fraction (LVEF) depends on preload and afterload, both of which can change dramatically within hours.
Stroke volume, cardiac output, cardiac index, and the LV index of myocardial performance, also known as the “Tei Index,” are increasingly reported as more reliable quantifiers of LV systolic function 7. Higher values on the index of myocardial performance are associated with more severe LV disease and poorer prognosis 8.
When LV systolic function is impaired, the report will indicate whether the chamber was globally hypokinetic, typical of cardiomyopathy, or whether regional wall-motion abnormalities were seen, the result of myocardial infarction. To localize and classify LV regional wall motion, the American Society of Echocardiography divides the LV into 16 segments 9. The LV wall motion score index might be reported. Higher scores indicate more dysfunction.
In many US laboratories, intravenous “bubble” contrast is used routinely to outline the LV chamber when the endocardium is poorly outlined. In Canada, financial constraints often preclude this approach.
- 8) Left ventricular diastolic function
Diastolic dysfunction is an important factor in clinical heart failure 10. Left ventricular diastolic dysfunction usually precedes development of LV systolic dysfunction. Where LV systolic dysfunction exists, diastolic function is inevitably abnormal. The presence and severity of diastolic dysfunction are strong predictors of future nonvalvular atrial fibrillation in the elderly 11. Independent of systolic function, diastolic dysfunction of any degree is a strong predictor of all-cause mortality 12.
Modern echocardiography either reports diastolic function as normal or grades diastolic dysfunction by class (1 through 4) 13. Class 1 diastolic dysfunction (impaired myocardial relaxation) was formerly called “mild diastolic dysfunction,” an expression that is obsolete and misleading. In one series, class 1 diastolic dysfunction was associated with an 8-fold increase in all-cause mortality within 5 years 12. Mortality increases with the severity of diastolic dysfunction.
Increased left atrial (LA) volume is a morphologic expression of diastolic dysfunction, reflecting LV end diastolic pressure 14. It predicts development of atrial fibrillation 15. Size of the left atrium is usually represented by the transverse diameter of the chamber, although this measurement often underestimates the volume of an enlarged left atrium.
- 9) Right ventricle
When there is no comment on function of the right ventricle, it is presumed normal by visual assessment. A few laboratories report the right-sided index of myocardial performance. This ratio is analogous to the Tei Index for LV performance.
- 10) Valvular regurgitation
Most reports of valvular insufficiency are based on visual assessment. This common method of classifying regurgitation as trivial (or trace), mild, moderate, or severe is subjective, imprecise, and frequently misleading. Visualization by color Doppler depends on the velocity of the jet, not the volume of blood. A small, high-velocity jet through a small orifice could thus appear to be more severe than a much larger, but slower, blood volume regurgitating through a larger orifice 16.
An increasing number of laboratories quantify valvular regurgitation using the effective regurgitant orifice and the regurgitant volume of blood 17. Some reports refer to this as the “PISA” method (proximal isovelocity surface area) 18.
- 11) Valvular stenosis
Mitral and aortic stenoses are graded as mild, moderate, or severe, based on the maximum velocity, peak gradient across the valve, and estimated cross-sectional area of the orifice. These data are usually reported. Pulmonary stenosis can be indicated by an increased pressure gradient across the valve.
Intracardiac mass or thrombus.
Aortic stenosis
The etiology of aortic stenosis (AS) can be confirmed by the visualization of either a bicuspid valve or calcification. The severity of the stenosis can be estimated by measuring high-velocity flow across the valve by Doppler. This can be converted to an estimation of the pressure drop. In addition, the effective orifice area can be measured (see Table 1).
Table 1. Echo characteristics of aortic stenosis
| Mild or no aortic stenosis | Severe aortic stenosis | |
|---|---|---|
| Area of effective orifice (cm2) | >1 | <0.6 |
| Velocity across valve (m/s) | <3 | >4 |
| Gradient of pressure drop (mm Hg) | 0–60 | >60 |
Mitral stenosis
With mitral stenosis, as with aortic stenosis, calcified, immobile mitral valve leaflets can be demonstrated with 2D and M-mode echo. Anterior motion of the posterior mitral valve leaflet in diastole (caused by commissural fusion) is characteristic in mitral stenosis. Doppler demonstrates increased flow velocity and can be used to estimate the effective orifice area (see Table 2).
Table 3. Echo characteristics of mitral stenosis
| Mild mitral stenosis | Severe mitral stenosis | |
|---|---|---|
| Area of effective orifice (cm2) | >1.5 | <1 |
| Velocity across valve (m/s) | <2.5 | >3 |
Clots and masses in the LV are seen best by transthoracic echocardiogram 19. The left atrial appendage is poorly visualized. Transesophageal echocardiography has betransthoracic echocardiogramr sensitivity than transthoracic echocardiogram for detecting an intra-atrial embolic source in stroke 20.
Suspect echogenic features that could represent anatomic structures, unusual artifacts, primary or secondary cardiac tumours, thrombi, or vegetations will also be reported. Technically difficult transthoracic echocardiogram images often cannot differentiate between lesions and artifacts. Reporting physicians will point out any concerns, possibly recommending transesophageal echocardiography for clarification.
- 12) Septal defects
The location and size of atrial and ventricular septal defects will be reported. Unless the sonographer is specifically looking for a suspected atrial septal defect, images might not be obtained from the subcostal window, the best view for detecting it 21. Contrast echocardiography can be helpful when a septal defect is suspected on clinical grounds but is not visible via transthoracic echocardiogram.
- 13) Right ventricular systolic pressure
When failure on the right side of the heart is suspected, it is helpful to estimate the right ventricular systolic pressure or pulmonary systolic pressure. Measurements are often elevated by obesity and hypertension, not just by pulmonary hypertension.
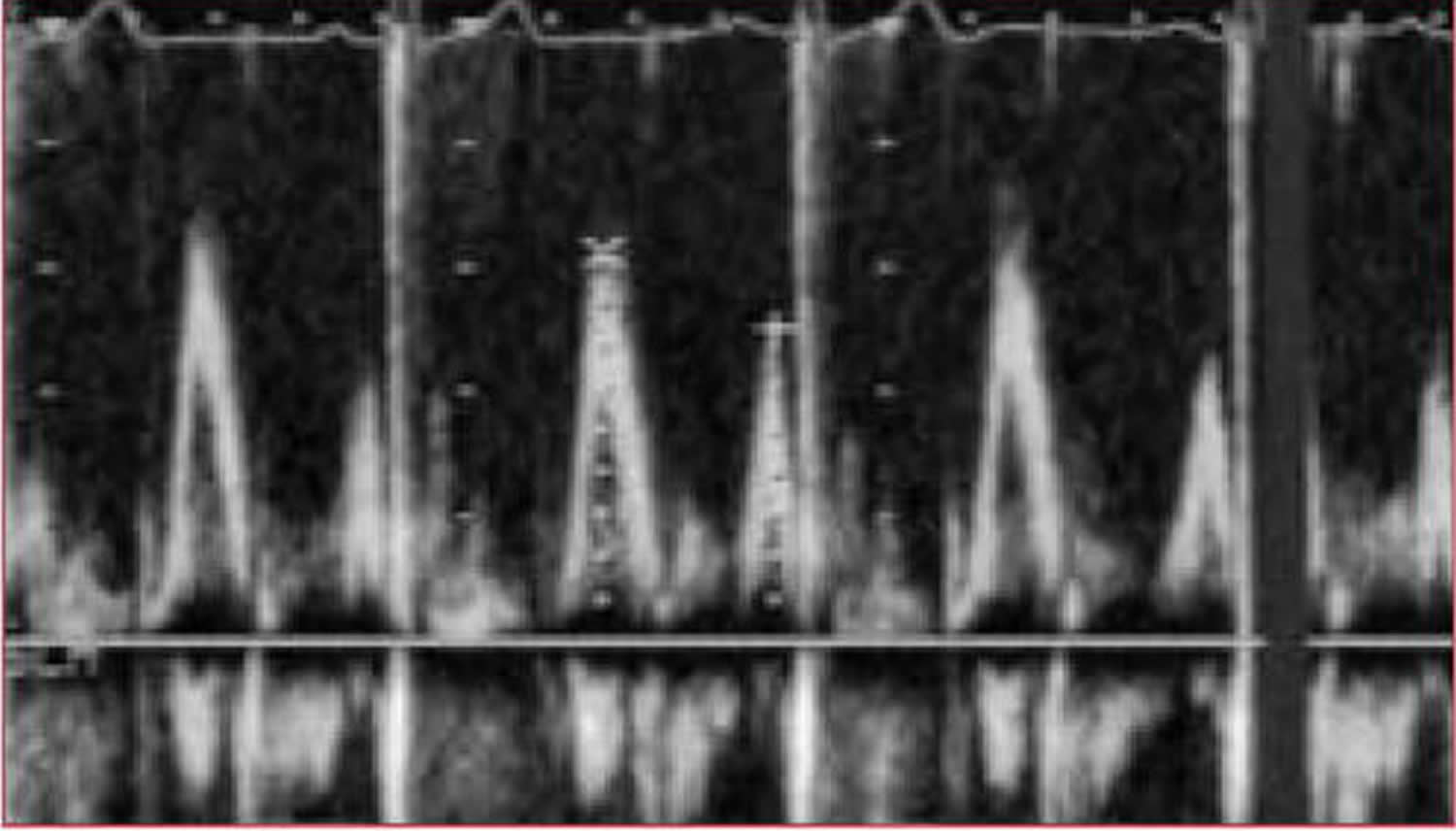
- 14) The E/A ratio
When flow across the mitral valve is assessed with pulsed-wave (PW) Doppler , two waves are characteristically seen. These represent passive filling of the ventricle (early [E] wave) and active filling with atrial systole (atrial [A] wave). Classically, the E-wave velocity is slightly greater than that of the A wave (see Figure 7). However, in conditions that limit the compliance of the LV, two abnormalities are possible:
- reversal – in which the A wave is greater than the E wave. This indicates slow filling caused by older age, hypertension, left ventricular hypertrophy (LVH), or diastolic dysfunction
- exaggeration of normal – a tall, thin E wave with a small or absent A wave. This indicates restrictive cardiomyopathy, constrictive pericarditis, or infiltrative cardiac disease (eg, amyloidosis)
Figure 9. Pulsed-wave Doppler – E and A waves representing mitral flow in a healthy heart (E>A)
[Source 3]- 15) Wall-motion abnormality
When ischemia occurs, contractile abnormalities of segments of the myocardium can be detected by echo prior to the appearance of electrocardiogram (ECG) changes or symptoms. Therefore, echo can be a valuable tool in the diagnosis of both stable coronary artery disease (via stress echo) and acute myocardial infarction. In the former situation, it offers localization of the ischemic region where the ECG cannot; in the latter, it offers some measure of the extent of the infarct and a screen for complications, such as ventricular septal defect (VSD).
- 16) Pericardium
The location of pericardial effusion and its size (trace, small, medium, or large) will be reported. Small pericardial effusions are often physiologic. If an effusion is reported, referring physicians want to know whether there is evidence of tamponade, although this is ultimately a clinical diagnosis, not an echocardiographic one. Patients with uncomplicated viral pericarditis have normal echocardiogram results 19.
- 17) Aorta
The diameter of the aortic root is measured routinely. Sometimes it is possible to identify dilation of the ascending aorta, the arch, or the descending aorta. Aortic dissection is an emergency requiring immediate contact between reporting and referring physicians.
- 18) Incidental findings
Unsuspected congenital cardiac abnormalities are discovered occasionally. Incidental findings might require investigation using other imaging modalities. Pleural effusions are often seen on the left. Intrahepatic lesions are sometimes identified and extrinsic masses compressing the heart are sometimes revealed.
- 19) Summary of findings
The limitations of transthoracic echocardiogram are implicit, but they might be stated in the conclusions if the questions asked by referring physicians are known. For example, if a laboratory is asked to rule out cardiac embolism in a patient with atrial fibrillation and a recent stroke, the report might remind the referring physician that the left atrial appendage is not visible on transthoracic echocardiogram and that transesophageal echocardiography is recommended. When myocardial ischemia is suspected in a patient scheduled for surgery, a technician might suggest a nuclear medicine study or stress echocardiography.
Follow-up echocardiography could be suggested. Advice concerning treatment exceeds the mandate of a laboratory report, but many referring physicians appreciate recommendations for prophylactic antibiotics, when indicated.
When transthoracic echocardiogram report conclusions fail to address the reason the procedure was ordered, chances are high that the reason was never stated on the requisition. Physician-to-physician discussion can answer many queries and concerns often raised about transthoracic echocardiogram procedure.
Table 3. The approximate normal values for various cardiac structures. IV: interventricular; LV: left ventricular
| Normal ranges for measures of systolic and diastolic function | ||
|---|---|---|
| Echocardiography | ||
| Fractional shortening (%) | 28–44 | |
| Doppler | ||
| Systolic velocity integral (cm) | 15–35 | |
| Mitral valve E (cm/s) | 44–100 | |
| Mitral valve A (cm/s) | 20–60 | |
| E:A ratio | 0.7–3.1 | |
| Tricuspid valve E (cm/s) | 20–50 | |
| Tricuspid valve A (cm/s) | 12–36 | |
| E:A ratio | 0.8–2.9 | |
| Time intervals | ||
| Mitral E deceleration time (ms) | 139–219 | |
| Mitral A deceleration time (ms) | >70 | |
| Isovolumic relaxation time (ms) | 54–98 | |
| Normal intracardiac dimensions (cm) | ||
| Men | Women | |
| Left atrium | 3.0–4.5 | 2.7–4.0 |
| LV diastolic diameter | 4.3–5.9 | 4.0–5.2 |
| LV systolic diameter | 2.6–4.0 | 2.3–3.5 |
| IV septum (diastole) | 0.6–1.3 | 0.5–1.2 |
| Posterior wall (diastole) | 0.6–1.2 | 0.5–1.1 |
Table 4. Checklist and practice points for Transthoracic Echocardiogram Report
[Source 22]Transesophageal echocardiogram
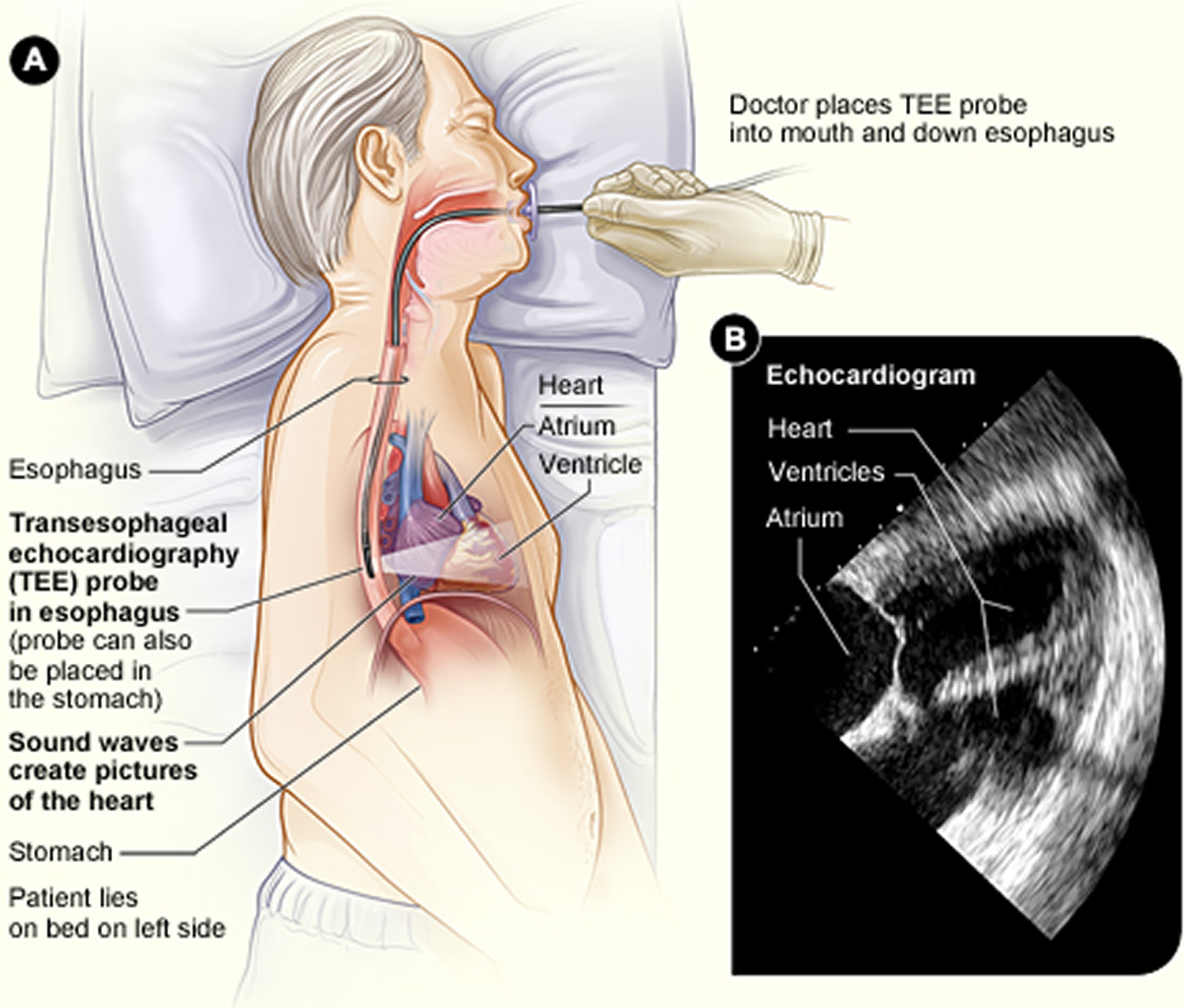
Transesophageal echocardiogram (TEE) is a test that uses sound waves to create high-quality moving pictures of the heart and its blood vessels. During an echocardiogram, a device called a transducer is used to send sound waves (called ultrasound) to the heart. As the ultrasound waves bounce off the structures of the heart, a computer in the echo machine converts them into pictures on a screen.
Transesophageal echocardiogram involves a flexible tube (probe) with a transducer at its tip. Your doctor will guide the probe down your throat and into your esophagus (the passage leading from your mouth to your stomach). This approach allows your doctor to get more detailed pictures of your heart because the esophagus is directly behind the heart.
Transesophageal echocardiogram can help doctors diagnose heart and blood vessel diseases and conditions in adults and children. Doctors also may use TEE to guide cardiac catheterization, help prepare for surgery, or assess a patient’s status during or after surgery.
Doctors may use transesophageal echocardiogram in addition to transthoracic echocardiogram (TTE), the most common type of echo. If transthoracic echocardiogram (TTE) pictures don’t give doctors enough information, they may recommend transesophageal echocardiogram to get more detailed pictures.
Outlook
Transesophageal echocardiogram has a low risk of complications in both adults and children. Even newborns can have transesophageal echocardiogram.
Types of Transesophageal Echocardiogram
Standard transesophageal echocardiography (TEE) pictures are two-dimensional (2D). It’s also possible to get three-dimensional (3D) pictures from transesophageal echocardiogram. These pictures provide even more details about the structure and function of the heart and its blood vessels.
Doctors can use 3D transesophageal echocardiogram to help diagnose heart problems, such as congenital heart disease and heart valve disease. Doctors also may use this technology to assist with heart surgery.
What does Transesophageal Echocardiogram show?
Transesophageal echocardiogram provides high-quality moving pictures of your heart and blood vessels. These pictures help doctors detect and treat heart and blood vessel diseases and conditions.
Transesophageal echocardiogram creates pictures from inside the esophagus (the passage leading from the mouth to the stomach) or, sometimes, from inside the stomach. Because the esophagus lies directly behind the heart, transesophageal echocardiogram provides closeup pictures of the heart.
Transesophageal echocardiogram also offers different views and may provide more detailed pictures than transthoracic echocardiography (TTE), the most common type of echo.
Your doctor may recommend transesophageal echocardiogram if he or she needs more information than transthoracic echocardiography (TTE) can provide. transesophageal echocardiogram can help diagnose and assess heart and blood vessel diseases and conditions in adults and children. Examples of these diseases and conditions include:
- Coronary heart disease
- Congenital heart disease
- Heart attack
- Aortic aneurysm
- Endocarditis
- Cardiomyopathy
- Heart valve disease
- Injury to the heart or aorta (the main artery that carries oxygen-rich blood from your heart to your body)
Transesophageal echocardiogram also can show blood clots that may have caused a stroke or that may affect treatment for atrial fibrillation, a type of arrhythmia.
Doctors also may use transesophageal echocardiogram during cardiac catheterization. Transesophageal echocardiogram can help doctors guide the catheter (thin, flexible tube) through the blood vessels. Transesophageal echocardiogram also can help doctors prepare for surgery or assess a patient’s status during or after surgery.
Who Needs Transesophageal Echocardiography
Doctors may recommend transesophageal echocardiography (TEE) to help diagnose a heart or blood vessel disease or condition. Transesophageal echocardiogram can be used for adults and children.
Doctors also may use transesophageal echocardiogram to guide cardiac catheterization, help prepare for surgery, or assess a patient’s status during or after surgery.
Transesophageal Echocardiography as a Diagnostic Tool
Transesophageal echocardiogram helps doctors detect problems with the structure and function of the heart and its blood vessels.
In general, transthoracic echocardiogram (TTE) is the first echocardiogram test used to diagnose heart and blood vessel problems. However, you might have transesophageal echocardiogram if your doctor needs more information or more detailed pictures than transthoracic echocardiogram (TTE) can provide.
For transthoracic echocardiogram (TTE), the transducer (the device that sends the sound waves) is placed on the chest, outside of the body. This means the sound waves may not always have a clear path to the heart and blood vessels. For example, obesity, scarring from previous heart surgery, or certain lung problems (such as a collapsed lung) may block the sound waves.
For transesophageal echocardiogram, the transducer is at the tip of a flexible tube (probe). Your doctor will guide the probe down your throat and into your esophagus (the passage leading from your mouth to your stomach).
Your healthcare provider may recommend a transesophageal echocardiogram (TEE) if:
- The regular (or transthoracic echocardiogram) is unclear. Unclear results may be due to the shape of your chest, lung disease, or excess body fat.
- An area of the heart needs to be looked at in more detail.
This approach allows your doctor to get more detailed pictures of your heart because the esophagus is directly behind the heart.
Doctors may use transesophageal echocardiogram to help diagnose:
- Coronary heart disease
- Congenital heart disease
- Heart attack
- Aortic aneurysm
- Endocarditis
- Cardiomyopathy
- Heart valve disease/abnormal heart valves
- Injury to the heart or aorta (the main artery that carries oxygen-rich blood from your heart to your body)
- Abnormal heart rhythms
- Damage to the heart muscle from a heart attack
- Heart murmurs
- Inflammation (pericarditis) or fluid in the sac around the heart (pericardial effusion)
- Infection on or around the heart valves (infectious endocarditis)
- Pulmonary hypertension
- Ability of the heart to pump (for people with heart failure)
- Source of a blood clot after a stroke or TIA (transient ichemic attack or mini stroke)
Transesophageal echocardiogram also can show blood clots that may have caused a stroke or that may affect treatment for atrial fibrillation, a type of arrhythmia.
Transesophageal Echocardiography and Cardiac Catheterization
Cardiac catheterization is a medical procedure used to diagnose and/or treat certain heart conditions. During this procedure, a long, thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck and threaded to your heart.
Doctors may use transesophageal echocardiogram to help guide the catheter while they’re doing the procedure.
Through the catheter, doctors can do tests and treatments on your heart. For example, cardiac catheterization might be used to repair holes in the heart, heart valve disease, and abnormal heart rhythms.
Transesophageal Echocardiography and Surgery
Doctors may use transesophageal echocardiogram to prepare for a patient’s surgery and identify possible risks. For example, they may use transesophageal echocardiogram to look for possible sources of blood clots in the heart or aorta. Blood clots can cause a stroke during surgery.
Transesophageal echocardiogram might be used in the operating room after a patient receives medicine to make him or her sleep during the surgery. The test can show the heart’s structure and function and help guide the surgery.
Transesophageal echocardiogram also helps doctors assess a patient’s status during surgery. For example, transesophageal echocardiogram can help check for blood flow and blood pressure problems.
At the end of surgery, transesophageal echocardiogram might be used again to check how well the surgery worked. For example, transesophageal echocardiogram can show whether heart valves are working well. Transesophageal echocardiogram also can show how well the heart is pumping.
People having surgery that isn’t related to the heart also may have transesophageal echocardiogram to check their heart function if they have known heart disease or a critical illness.
Transesophageal echocardiogram risks
Transesophageal echocardiogram (TEE) has a very low risk of serious complications in both adults and children. To reduce your risk, your medical team will carefully check your heart rate and other vital signs during and after the transesophageal echocardiogram procedure.
Some risks are associated with the medicine that might be used to help you relax during transesophageal echocardiogram. You may have a bad reaction to the medicine, problems breathing, or nausea (feeling sick to your stomach). Usually, these problems go away without treatment.
Your throat also might be sore for a few hours after the test. Although rare, the probe used during transesophageal echocardiogram can damage the esophagus (the passage leading from your mouth to your stomach).
Talk with your medical provider about the risks associated with this test.
Transesophageal echocardiogram prep
Transesophageal echocardiogram most often is done in a hospital. You usually will need to fast (not eat or drink) for 4 to 8 hours prior to the test, but your doctor will let you know exactly how long you should fast.
You should let your doctor know whether you’re taking any blood-thinning medicines, have trouble swallowing, or are allergic to any medicines. If you have dentures or oral prostheses, you’ll need to remove them before the test.
You may be given medicine to help you relax during transesophageal echocardiogram. If so, you’ll have to arrange for a ride home after the test because the medicine can make you sleepy.
Talk with your doctor about whether you need to take any special steps before having transesophageal echocardiogram. Your doctor can tell you whether you need to change how you take your regular medicines on the day of the test or whether you need to make other changes.
What to expect during transesophageal echocardiogram procedure
During transesophageal echocardiography, your doctor or your child’s doctor will use a probe with a transducer at its tip. The transducer sends sound waves (ultrasound) to the heart. Probes come in many sizes; smaller probes are used for children and newborns.
The back of your mouth will be numbed with gel or spray before the probe is put down your throat. You may feel some discomfort as the probe is guided into your esophagus (the passage leading from your mouth to your stomach).
Adults having transesophageal echocardiogram may get medicine to help them relax during the test. The medicine will be injected into a vein.
Children always receive medicine to help them relax or sleep if they’re having transesophageal echocardiogram. This helps them remain still so the doctor can safely insert the probe and take good pictures of the heart and blood vessels.
Your doctor will insert the probe into your mouth or nose. He or she will then gently guide it down your throat into your esophagus. Your esophagus lies directly behind your heart. During this process, your doctor will take care to protect your transesophageal echocardiogramth and mouth from injury.
Your blood pressure, blood oxygen level, and other vital signs will be checked during the test. You may be given oxygen through a tube in your nose.
During the transesophageal echocardiogram:
- You will need to take off your clothes from the waist up and lie on an exam table on your back.
- Electrodes will be placed on your chest to monitor your heart beat.
- A gel is spread on your chest and the transducer will be moved over your skin. You will feel a slight pressure on your chest from the transducer.
- You may be asked to breathe in a certain way or to roll over onto your left side. Sometimes, a special bed is used to help you stay in the proper position.
- If you are having a transesophageal echocardiogram, you will receive some sedating (relaxing) medicines prior to having the probe inserted.
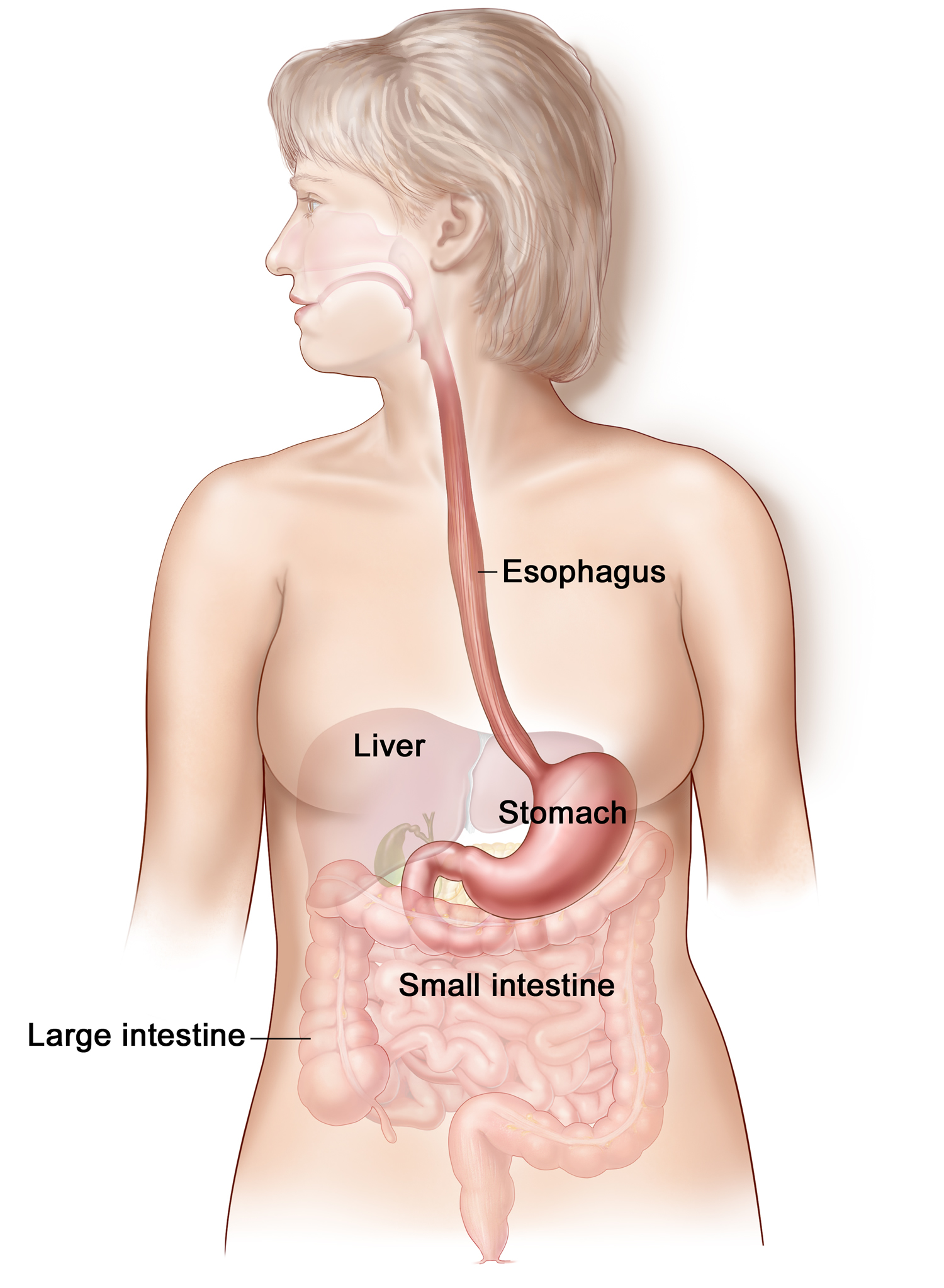
Figure 10. Esophagus
Figure 11. Transesophageal echocardiogram – Figure A shows a transesophageal echocardiography probe in the esophagus, which is located behind the heart. Sound waves from the probe create high-quality pictures of the heart. Figure B shows an echocardiogram of the heart’s lower and upper chambers (ventricles and atrium, respectively).
 How long does an transesophageal echocardiogram take?
How long does an transesophageal echocardiogram take?
Transesophageal echocardiogram takes less than an hour. However, if you received medicine to help you relax, you might be watched for a few hours after the test for side effects from the medicine.
After Transesophageal Echocardiogram – Recovery
After having transesophageal echocardiogram, your or your child’s blood pressure, blood oxygen level, and other vital signs will continue to be closely watched. You can likely go home a few hours after having the test.
After the transesophageal echocardiogram, you may have a sore throat for a few hours. You shouldn’t eat or drink for 30–60 minutes after having transesophageal echocardiogram. Most people can return to their normal activities within about 24 hours of the test.
Talk with your doctor or your child’s doctor to learn more about what to expect after having transesophageal echocardiogram.
- King DL. Three-dimensional echocardiography: use of additional spatial data for measuring left ventricular mass. Mayo Clin Proc. 1994;69:293–295 https://www.ncbi.nlm.nih.gov/pubmed/8133671[↩]
- Krasnow N. Subaortic septal bulge simulates hypertrophic cardiomyopathy by angulation of the septum with age, independent of focal hypertrophy: an echocardiographic study. J Am Soc Echocardiogr. 1997;10:545–555. https://www.ncbi.nlm.nih.gov/pubmed/9203495[↩]
- Ashley EA, Niebauer J. Cardiology Explained. London: Remedica; 2004. Chapter 4, Understanding the echocardiogram. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2215[↩][↩][↩][↩][↩]
- Kronik G, Slany J, Mosslacher H. Comparative value of eight M-mode echocardiographic formulas for determining left ventricular stroke volume. Circulation. 1979;60:1308–1316. https://www.ncbi.nlm.nih.gov/pubmed/498456[↩]
- Weyman AE. Principles and practice of echocardiography. 2nd ed. Philadelphia, Pa: Lea and Febiger; 1994.[↩]
- Edwards WD, Tajik AJ, Seward JB. Standardized nomenclature and anatomic basis for regional tomographic analysis of the heart. Mayo Clin Proc. 1981;56:479–497 https://www.ncbi.nlm.nih.gov/pubmed/7266059[↩]
- Tei C, Ling LH, Hodge DO, Bailey KR, Oh JK, Rodeheffer RJ, et al. New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function—a study in normals and dilated cardiomyopathy. J Cardiol. 1995;26(6):357–366. https://www.ncbi.nlm.nih.gov/pubmed/8558414[↩]
- Harjai KJ, Scott L, Vivekananthan K, Nunez E, Edupuganti R. The Tei Index: a new prognostic index for patients with symptomatic heart failure. J Am Soc Echocardiogr. 2002;15:864–868. https://www.ncbi.nlm.nih.gov/pubmed/12221401[↩]
- Schiller NB, Shah PM, Crawford M, DeMaria A, Devereaux R, Feigenbaum H, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-dimensional Echocardiograms. J Am Soc Echocardiogr. 1989;2:358–367. https://www.ncbi.nlm.nih.gov/pubmed/2698218[↩]
- Vasan RS, Benjamin EJ, Levy D. Prevalence, clinical features and prognosis of diastolic heart failure: an epidemiologic perspective. J Am Coll Cardiol. 1995;26:1565–1574. https://ac.els-cdn.com/0735109795003819/1-s2.0-0735109795003819-main.pdf?_tid=c6722420-5e9d-4b1c-81ed-7375141c6e7e&acdnat=1527864935_22907da6e34fb48f16341dfb35f87143[↩]
- Tsang TSM, Gersh BJ, Appleton CP, Tajik AJ, Barnes ME, Bailey KR, et al. Left ventricular diastolic dysfunction as a predictor of the first diagnosed nonvalvular atrial fibrillation in 840 elderly men and women. J Am Coll Cardiol. 2002;40:1636–1644. https://www.sciencedirect.com/science/article/pii/S0735109702023732[↩]
- Redfield MM, Jacobsen SJ, Burnett JC, Jr, Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community. JAMA. 2003;289(2):194–202. https://www.ncbi.nlm.nih.gov/pubmed/12517230[↩][↩]
- Rakowski H, Appelton CP, Chan KL, Dumesnil JG, Honos G, Jue J, et al. Recommendations for the measurement and reporting of diastolic function by echocardiography. J Am Soc Echocardiogr. 1996;9:736–760. https://www.ncbi.nlm.nih.gov/pubmed/8887883[↩]
- Tsang TSM, Barnes ME, Gersh BJ, Bailey KR, Seward JB. Left atrial volume as a morphophysiological expression of left ventricular diastolic dysfunction and relation to cardiovascular risk burden. Am J Cardiol. 2002;90:1284–1289. https://www.ncbi.nlm.nih.gov/pubmed/12480035[↩]
- Tsang TS, Barnes ME, Bailey KR, Leibson CL, Montgomery SC, Takemoto Y, et al. Left atrial volume: important risk marker of incident atrial fibrillation in 1655 older men and women. Mayo Clin Proc. 2001;76:467–475. https://www.ncbi.nlm.nih.gov/pubmed/11357793[↩]
- McCully RB, Enriquez-Sarano M, Tajik AJ, Seward JB. Overestimation of severity of ischemic/functional mitral regurgitation by color Doppler jet arm. Am J Cardiol. 1994;74:790–793. https://www.ncbi.nlm.nih.gov/pubmed/7942551[↩]
- Enriquez-Sarano M, Seward JB, Bailey KR, Tajik AJ. Effective regurgitant orifice area: a noninvasive Doppler development of an old hemodynamic concept. J Am Coll Cardiol. 1994;23:443–451. https://ac.els-cdn.com/0735109794904324/1-s2.0-0735109794904324-main.pdf?_tid=4351f52a-2170-4152-9e38-bf8202aa3548&acdnat=1527865439_0699d25dc55d0ffd31be8a075b1e613a[↩]
- Yamachika S, Reid CL, Savani D, Meckel C, Paynter J, Knoll M, et al. Usefulness of color Doppler proximal isovelocity surface area in quantitating valvular regurgitation. J Am Soc Echocardiogr. 1997;10:159–168. https://www.ncbi.nlm.nih.gov/pubmed/9083972[↩]
- Otto CM. The practice of clinical echocardiography. 2nd ed. Philadelphia, Pa: WB Saunders Co; 2002.[↩][↩]
- Lee RJ, Bartzokis T, Yeoh TK, Grogin HR, Choi D, Schnitther I. Enhanced detection of intracardiac sources of cerebral emboli by transthoracic echocardiography. Stroke. 1991;22:734–739 http://stroke.ahajournals.org/content/22/6/734.long[↩]
- Schub C, Dimopoulos IN, Seward JB, Callahan JA, Tancredi RG, Schattenberg TT, et al. Sensitivity of two-dimensional echocardiography in the direct visualization of atrial septal defect utilizing the subcostal approach: experience with 154 patients. J Am Coll Cardiol. 1983;2:127–135. https://ac.els-cdn.com/S0735109783803854/1-s2.0-S0735109783803854-main.pdf?_tid=c4b95043-e126-4c5d-9fa8-42a2697497f5&acdnat=1527865641_0b1a512457ba618a44014d536c83bf4e[↩]
- McAlister NH, McAlister NK, Buttoo K. Understanding cardiac “echo” reports: Practical guide for referring physicians. Canadian Family Physician. 2006;52(7):869-874. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1781094/[↩]