Contents
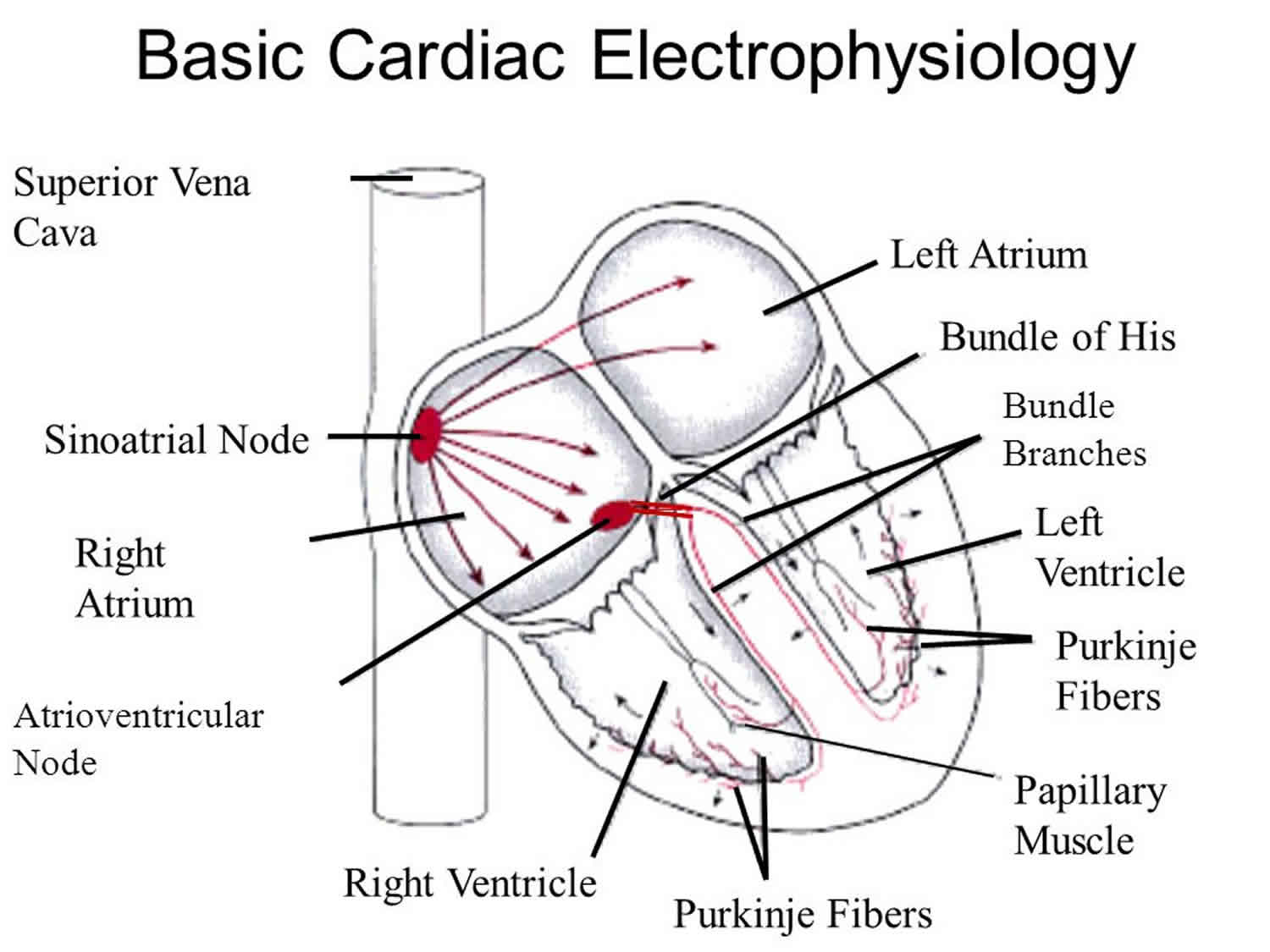
What is cardiac electrophysiology
Cardiac electrophysiology also called electrophysiology studies (EPS), use cardiac catheterization techniques to study patients who have irregular heartbeats (called arrhythmias). Cardiac electrophysiology shows how your heart reacts to controlled electrical signals. These signals can help doctors find out where in the heart the arrhythmia (irregular heartbeat) starts and what medicines will work to stop it. Cardiac electrophysiology can also help doctors know what other catheter techniques could be used to stop the arrhythmia.
Cardiac electrophysiology quick facts:
- Electrophysiology studies test the electrical activity of your heart to find where an arrhythmia (abnormal heartbeat) is coming from.
- These results can help you and your doctor decide whether you need medicine, a pacemaker, an implantable cardioverter defibrillator (ICD), cardiac ablation or surgery.
- Cardiac electrophysiology studies take place in a special room called an electrophysiology (EP) lab or catheterization (cath) lab while you are mildly sedated.
- Cardiac electrophysiology studies usually last 1 to 4 hours, but can sometimes take longer.
- The hospital will ask you not to eat or drink anything for a 6 to 8 hours beforehand.
- Thin flexible tubes, called catheters, are inserted into a blood vessel, usually in the groin. You will have a local anesthetic injection which numbs the area where the catheters are put in. You may also be given sedation to help you relax during the procedure.
- The catheters are moved into the position in the heart, where the special electrode tip stimulates the heart and records the electrical activity.
- This may make you feel as if you are having palpitations and can make some people feel dizzy. You should tell the staff if you experience any symptoms. You may also feel a sensation or discomfort in your chest, but this should not be painful.
- During the test you are continuously monitored by the nurses, doctors and technicians carrying out the procedure.
- The test is sometimes done as a day case. However, some people will need to stay in hospital overnight.
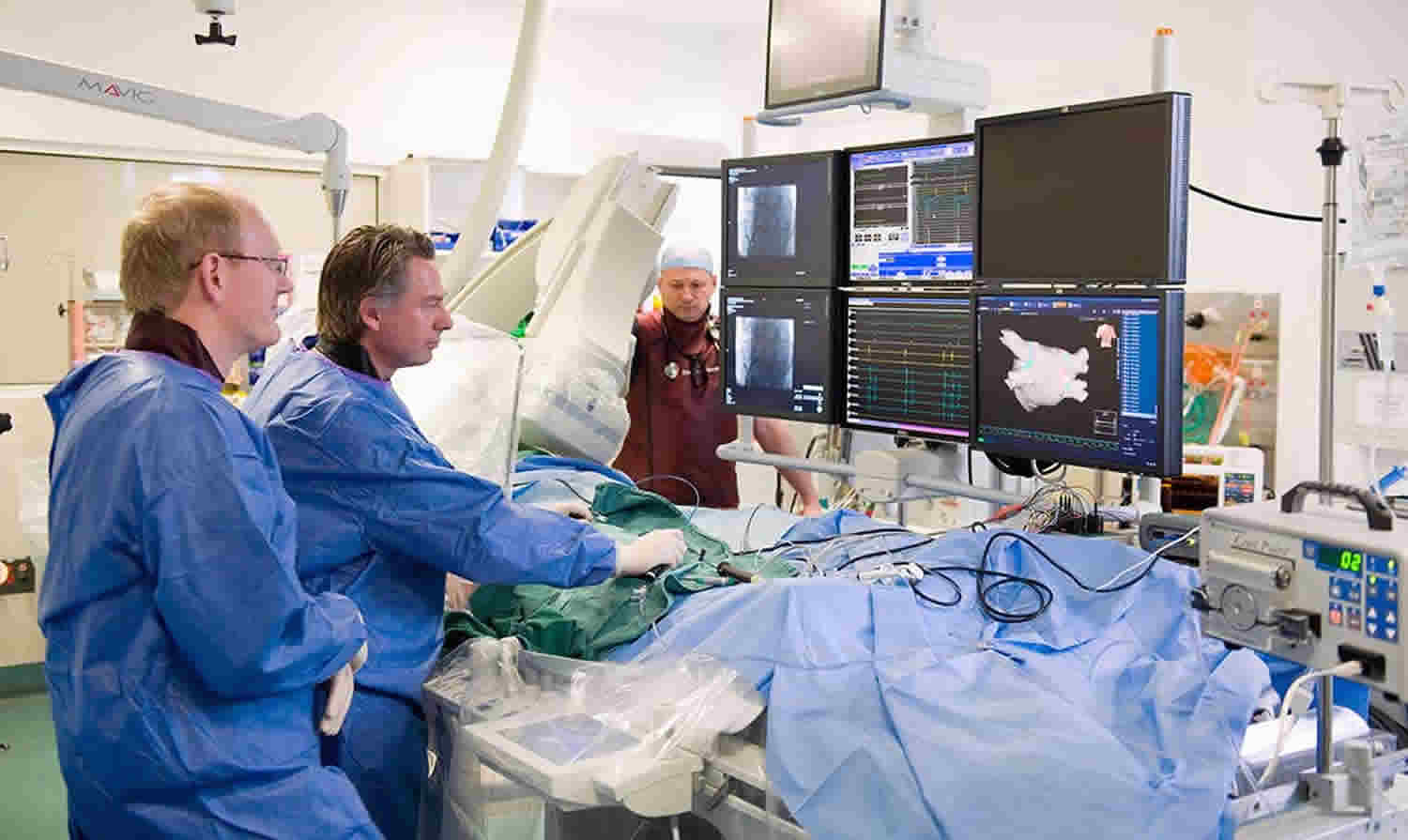
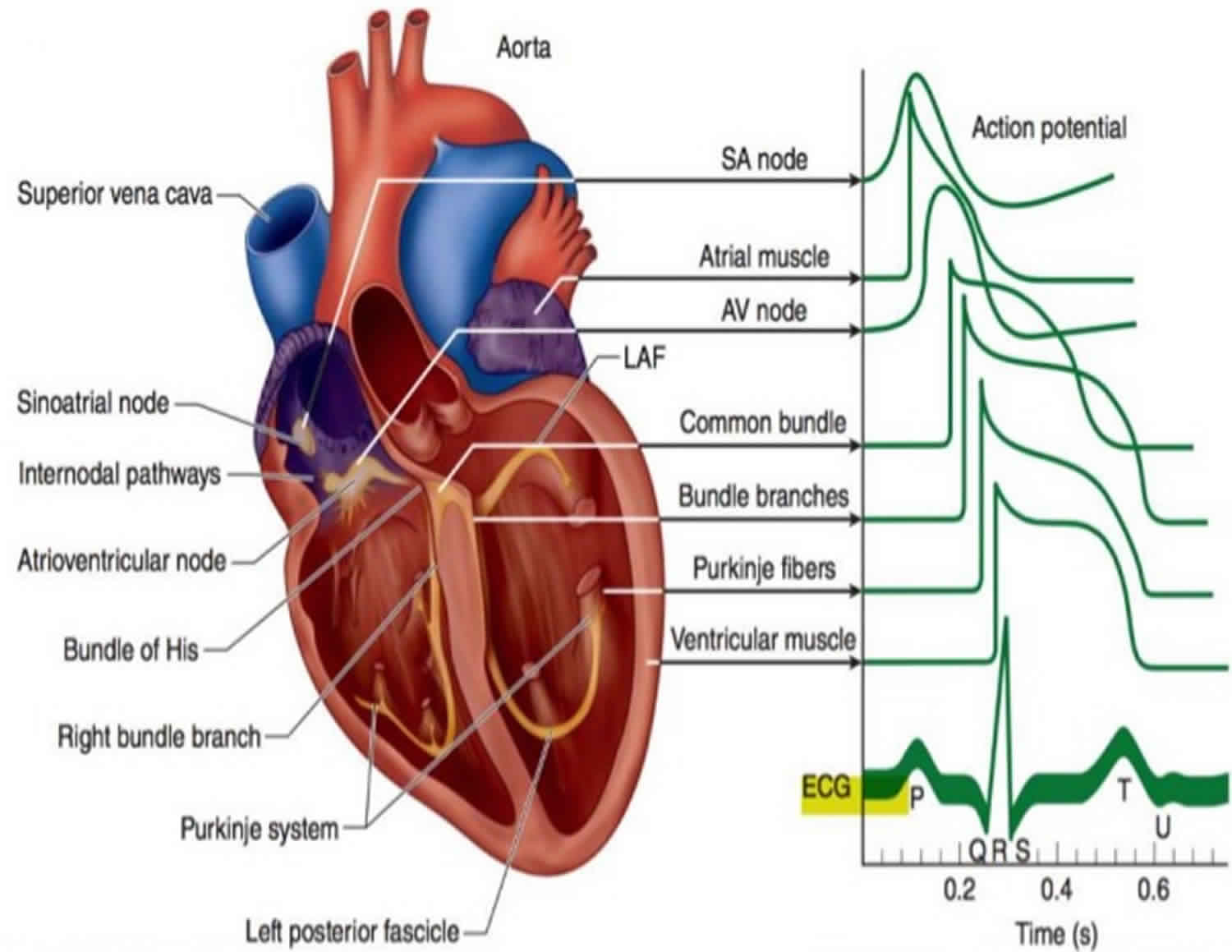
Figure 1. Electrophysiology of heart
Why do people have cardiac electrophysiology studies?
When someone’s heart doesn’t beat normally, doctors use cardiac electrophysiology studies to find out why. Electrical signals usually travel through the heart in a regular pattern. Heart attacks, aging and high blood pressure may cause scarring of the heart. This may cause the heart to beat in an irregular (uneven) pattern. Extra abnormal electrical pathways found in certain congenital heart defects can also cause arrhythmias.
During cardiac electrophysiology studies, doctors insert a thin tube called a catheter into a blood vessel that leads to your heart. A specialized electrode catheter designed for cardiac electrophysiology studies lets them send electrical signals to your heart and record its electrical activity.
Doctors use cardiac electrophysiology studies to see:
- Where an arrhythmia is coming from.
- How well certain medicines work to treat your arrhythmia.
- If they should treat a problem by destroying the place inside your heart that is causing the abnormal electrical signal. This procedure is called catheter ablation.
- If a pacemaker or implantable cardioverter defibrillator (ICD) might help you.
- If you are at risk for heart problems such as fainting or sudden cardiac death due to cardiac arrest (when your heart stops beating).
During an cardiac electrophysiology studies, about 3 to 5 electrically sensitive catheters are placed inside the heart to record electrical activity.
Electrophysiology procedure
Doctors will perform a cardiac catheterization procedure in which a long, thin tube (called a catheter) will be put into an artery in your leg and threaded into your heart. This catheter can be used to send the electrical signals into your heart.
Stimulating the heart will cause an arrhythmia, and doctors can record where in the heart it started. In some cases, you might be given a medicine to cause an arrhythmia. Certain medicines can also be given through the catheter to see which ones will stop the arrhythmia.
Once you are in the catheterization laboratory (also called the cath lab), you will see television monitors, heart monitors, and blood pressure machines. You will be asked to lie down on an examination table.
Electrodes will be placed on your chest. These electrodes have wires called leads, which hook up to an electrocardiogram machine. This machine will monitor your heart rhythm during the test.
To prevent infection, you will be shaved and cleansed around the area of your leg where the catheter will be inserted.
A needle with a tube connected to it will be put in your arm. This is called an intravenous line or IV. You will get a mild sedative through the IV to relax you throughout the test.
You will be given an anesthetic medicine with a needle to numb the area around where the catheter will be inserted. You may feel mild discomfort. Next, a small incision will be made in the skin. Once doctors see the artery into which the catheter will go, a special needle is used to poke into it. Doctors then put the catheter into the artery in your leg. You should not feel pain during this part of the test.
The catheter is gently threaded through the artery and into your heart. Once the catheter is in place, doctors will give your heart small electrical impulses to make it beat at different speeds. You will be able to feel your heartbeat changing speeds, and this may cause some mild discomfort. After the doctors have the information they need, the catheter and IV will be removed. Firm pressure will be applied to the site where the catheter was inserted to stop any bleeding. You will also be bandaged.
You will be moved to another room where you will need to rest for a few hours. You may feel a little sleepy until the sedative has worn off. You should try to lie still and not bend your knee too much. Nurses will watch you to see that your heart rate and blood pressure are normal. After this time of rest, you will be able to go home.
How do I prepare for cardiac electrophysiology studies?
- Don’t eat or drink anything for 6 to 8 hours before the test.
- Tell your doctor about any medicines you take, including over-the-counter medicines, herbs and vitamins. He or she may ask you not to take them before cardiac electrophysiology studies. Don’t stop taking your medicine until your doctor tells you to.
- Have someone drive you to your appointment and take you home.
- If you usually wear a hearing aid, wear it during your procedure. If you wear glasses, bring them to your appointment.
Do not eat or drink anything after midnight the night before your test. If you have diabetes, you should talk to your doctor about your food and insulin intake, because not eating can affect your blood sugar levels.
Talk to your doctor about any medicines (prescription, over-the-counter, or supplements) that you are taking, because he or she may want you to stop taking them before the test. Also, it may be helpful to make a list of your medicines and bring it with you to the procedure, so that doctors know exactly what you are taking and how much. You will most likely have blood tests, an electrocardiogram, and a chest x-ray taken before the procedure.
What happens during cardiac electrophysiology studies?
At a hospital or clinic, doctors and nurses do cardiac electrophysiology studies in a room that has special equipment for the tests. You may hear this room called the electrophysiology laboratory, or EP lab. Some call it the catheterization laboratory (cath lab). During the test:
- A nurse will put an IV (intravenous line) in your arm. You’ll get medicine (a sedative) that will help you relax. But you’ll be awake and able to follow instructions during the test.
- Your nurse will clean and shave the part of your body where the doctor will be working. This is usually in the groin but may be the arm or neck.
- You’ll be given a shot – a local anesthetic will be given — to make the area numb. Your doctor will make a needle puncture through your skin and into your blood vessel. A small straw-sized tube called a sheath will be inserted into your artery or vein. The doctor will gently guide several specialized EP catheters into your blood vessel through the sheath and advance them to your heart. A video screen will show the position of the catheters. You may feel some pressure in the area where the sheath was inserted, but you shouldn’t feel any pain.
- Your doctor will send small electric pulses through the catheters to make your heart beat at different speeds. You may feel your heart beat stronger or faster.
- Electrical signals produced by your heart will be picked up by the special catheters and recorded. This is called cardiac mapping and allows the doctor to locate where arrhythmias are coming from,
- Your doctor will remove the catheters and the IV line. Your nurse will put pressure on the puncture site to stop any bleeding.
If the type and location of the arrhythmia is identified and an appropriate therapy decided, cardiac ablation or insertion of a pacemaker or ICD may be performed during or immediately after the cardiac electrophysiology studies.
What happens after cardiac electrophysiology studies?
When the cardiac electrophysiology test is over, the catheters are removed. Sometimes there may be a small amount of bleeding when they are taken out. A nurse or doctor will press on the area for a short while to stop any bleeding.
You’ll be moved to a recovery room where you should rest quietly for 1 to 3 hours. During this time:
- Stay still as long as your nurse tells you to. Be sure to keep the arm or leg used for the test straight.
- Your nurse will check on you often to see if there is bleeding or swelling at the puncture site.
- After the sedative wears off, your doctor will talk to you about your test results.
- Before you leave, you’ll be told what to do at home.
You may feel tired afterwards, but you should feel back to normal within a few days.
What happens after I get home?
Follow the instructions your nurse or doctor gave you, including taking any new medicines that were prescribed. Most people can start eating food and taking their medicines within 4 to 6 hours after the test. Most can do their usual daily activities the day after the test. Don’t drive for at least 24 hours.
The puncture site may be sore for several days. A small bruise at the puncture site is normal. If the site starts to bleed, lie flat and press firmly on top of it. Have someone call the doctor or electrophysiology laboratory.
Call your local emergency services number if you notice:
- A sudden increase in swelling around the puncture site.
- Bleeding doesn’t slow down when you press hard on the site.
Call your doctor right away if you notice:
- Your arm or leg that was used for the sheath feels numb or tingles.
- Your hand or foot feels very cold or changes color.
- The puncture site looks more and more bruised.
- The puncture site begins to swell or fluids begin to come from it.
How do I learn the results of my cardiac electrophysiology studies?
Most of the time, doctors will ask you to make an appointment to discuss the results of your test. You’ll discuss your treatment at that appointment.
An cardiac electrophysiology study can diagnose abnormal heart rhythms and identify which areas are affected.
Abnormal heart rhythms often happen during the test. These can help with the results of the test but sometimes may need to be treated during the cardiac electrophysiology study.
If the cause of your abnormal heart rhythm is found, the doctor will sometimes want to treat the problem during the test by using catheter ablation. This treatment uses either heat (radio-frequency ablation) or freezing (cryogenic ablation) to destroy the areas inside the heart which are causing the abnormal rhythm.
If you have an abnormal heart rhythm, an cardiac electrophysiology study can also show how well your medication is controlling your condition.
Cardiac electrophysiology study risks
Cardiac electrophysiology study risks may include:
- Arrhythmia. During cardiac electrophysiology studies you may have abnormal heart rhythms that make you dizzy. If this happens, your doctor may give your heart an electric shock to bring back a regular heartbeat.
- Blood clots sometimes can form at the tip of the catheter, break off and block a blood vessel. Your doctor may give you medicine to prevent blood clots.
- Infection, bleeding and bruising at the site where the catheter went in (groin, arm or neck). Your doctor or nurse will help you avoid these problems.
An cardiac electrophysiology study does involve a very small amount of risk. Your doctor will explain this to you before you give your consent to have the test.
If there is bleeding from the area where the catheter was placed, you might develop a collection of blood under the skin, which is called a hematoma. It can be uncomfortable and cause bruising, but this should go down after a few days. However, contact your doctor if you have any concerns.
There is a small risk of damage to the heart’s normal electrical pathways. If this happens, you may need to be fitted with a pacemaker.
Your doctor will only recommend that you have an cardiac electrophysiology study if he or she thinks the benefits outweigh the risks.