Contents
- What is emergency contraception
- How do I get emergency contraception?
- How can I get free or low-cost emergency contraception?
- When should I think about using emergency contraception?
- How quickly should I use emergency contraception after unprotected sex?
- Can I get emergency contraception pills before I need them?
- Does emergency contraception have side effects?
- Will emergency contraception pills affect my next period?
- Does body weight affect how well emergency contraception works for women?
- Can I use emergency contraception as my regular form of birth control?
- Will emergency contraception protect me from sexually transmitted infections (STIs)?
- What does it mean for birth control to “fail” or not work correctly?
- Copper-T Intrauterine Device (IUD) as Emergency Contraception
- Morning After Pill
- Plan B pill
- Emergency Contraception Pills – Options
What is emergency contraception
Emergency contraception is a form of birth control by preventing pregnancy from occurring. You must use emergency contraception as soon as possible after unprotected sex to be effective. Emergency contraception does not work if pregnancy has already occurred. Emergency contraception can help prevent pregnancy if used within 5 days of having sex. Emergency contraception pills are different from the abortion pill. If you are already pregnant, emergency contraception pills do not stop or harm your pregnancy. According to research, nearly half (45 percent) of all pregnancies in the United States are unplanned, 2.8 million occurred in 2011 alone, the last year for which data are available 1. Emergency contraception offers women a last chance to prevent pregnancy after unprotected intercourse.
You might use emergency contraception if:
- You had unprotected sex.
- You had unprotected sex and forgot to take your birth control pills.
- Your partner’s condom broke or slipped off during sex.
- Your diaphragm or sponge came out of place during sex.
- You were raped.
Emergency contraception must be used soon after unprotected sexual intercourse to be effective.
There are 2 types of emergency contraception available:
- One option is emergency contraception pill, which is often known as “the morning-after pill”, but you do not need to wait until the morning after unprotected sex to take it. In the United States, there are two types of FDA-approved emergency contraception pills available for emergency contraception:
- ella® (ulipristal acetate). Pills that contain ulipristal acetate requires a prescription. ella® (ulipristal acetate) is more effective than progestin-only (levonorgestrel-only) pills (like Plan B One-Step), particularly if you are close to ovulation. In clinical studies, the effectiveness of ella did not decline over a 5-day period after unprotected sex, while progestin-only emergency contraception may be ineffective on the fifth day. However, because each individual woman may not know exactly how close she is to ovulating, it is important to take emergency contraception as soon as possible after unprotected sex. Both ella® (ulipristal acetate) and progestin-only pills are more effective and have fewer side effects than combined emergency contraceptive pills.
- Plan B One-Step® (levonorgestrel-only) — Plan B One-Step® has several generic versions. Some common generic versions include AfterPill™, My Way®, Next Choice One Dose™, and Take Action™.
- In the United States, emergency contraception pills that contain levonorgestrel do not require a prescription from your doctor. You can purchase them over the counter at a pharmacy. Most medicine brands require a single dose of 1 pill. Some brands have 2 doses (1 pill followed by a second pill 12 hours later). Sometimes, you can take both pills together. However, follow the instructions for each specific brand. Some women feel nauseous after they take emergency contraceptive pills. This feeling should go away in about 2 days. Your doctor can give you medicine to reduce nausea. Other possible side effects include headache, cramping, and tender breasts.
- Research shows that emergency contraception pills work mostly by preventing or delaying ovulation (the release of an egg from the ovary). Less commonly, emergency contraception may prevent fertilization of the egg by the sperm if ovulation has already happened 2. If a fertilized egg has already implanted in your uterus (you are pregnant), emergency contraception pills will not stop or harm your pregnancy 3.
- The second option is to use an intrauterine device (IUD) that contains copper (ParaGard). You must go to a doctor to have a Copper-T intrauterine device (IUD) inserted.
Emergency contraceptive pills can be very effective if they are used in time. The sooner you take them after sex, the more effective they are. Ulipristal acetate pills reduce your risk of pregnancy more than levonorgestrel pills (morning after pills e.g. Plan B). They cannot prevent pregnancy if you have unprotected sex after taking them.
Emergency contraception can prevent pregnancy by:
- stopping ovulation (the release of an egg from your ovaries)
- stopping sperm from fertilizing an egg
- stopping a fertilized egg from implantation (attaching itself to the wall of your uterus).
Emergency contraception cannot prevent or end pregnancy if a fertilized egg already is implanted. Because of this, emergency contraception is not a means of abortion. Using emergency contraception does not cause an abortion. An abortion ends an existing pregnancy.
Keep in mind, emergency contraception does not protect against sexually transmitted diseases (STDs). You should not use any emergency contraception if you know you are pregnant or are trying to get pregnant.
Women who are breastfeeding should not use emergency contraception pills that contain ulipristal acetate. Emergency contraception pills also are less effective for women who are overweight or obese 4. Instead, these women should use the ParaGard intrauterine device (IUD).
Do not get an intrauterine device (IUD) if you:
- have abnormal bleeding
- have cancer of the cervix or uterus
- have the AIDS infection
- are allergic to copper.
Emergency contraceptive pills can affect your menstrual cycle. Talk to your doctor if you do not get your period within 1 month after taking them. Your doctor also can tell you when to start taking your regular form of birth control again. It will vary if you use a hormonal form, such as pills, shots, the patch, or a vaginal ring. If you use a barrier method, such as a diaphragm or condoms, you can start using it right away. If you do not use birth control, talk to your doctor about which method will work best for you.
Research over the past 30 years has shown that these methods are safe and effective. emergency contraception is endorsed by the World Health Organization and many other international and national organizations. Depending on the method used, emergency contraception can reduce a woman’s risk of becoming pregnant from a single act of intercourse by between 75 and 99 percent.
In 2006–2010, one in nine sexually experienced women aged 15–44 had used emergency contraception at least once. The ever-use of emergency contraception was most common among women aged 20–24, those who never married, Hispanic or non-Hispanic white women, and those who attended college. Most women who had used emergency contraception had done so once or twice.
Among women who had ever used emergency contraception, nearly equal percentages of women, around 50%, reported having used it because of fear of method failure and because of unprotected sex. Non-Hispanic black and Hispanic women and those with less education were more likely to have used emergency contraception because of unprotected sex, compared with women of other characteristics. Older women, non-Hispanic white women, and women with more education more often used emergency contraception because of fear of method failure, compared with women of other characteristics.
Key Facts about emergency contraception:
- You need to take the emergency contraceptive pill within 3 days (Plan B) or 5 days (ella) of unprotected sex for it to be effective – the sooner you take it, the more effective it’ll be.
- The intrauterine device (IUD) can be fitted up to 5 days after unprotected sex, or up to 5 days after the earliest time you could have ovulated, for it to be effective.
- The intrauterine device (IUD) is more effective than the contraceptive pill at preventing pregnancy – less than 1% of women who use the intrauterine device (IUD) get pregnant.
- Taking the emergency contraceptive pills Plan B or ella can give you a headache or tummy pain and make you feel or be sick.
- The emergency contraceptive pill can make your next period earlier, later or more painful than usual.
- If you’re sick (vomit) within 2 hours of taking Plan B or 3 hours of taking ella, go to your doctor, pharmacist or genitourinary medicine clinic, as you’ll need to take another dose or have an intrauterine device (IUD) fitted.
- If you use the intrauterine device (IUD) as emergency contraception, it can be left in and used as your regular contraceptive method.
- If you use the intrauterine device (IUD) as a regular method of contraception, it can make your periods longer, heavier or more painful.
- You may feel some discomfort when the intrauterine device (IUD) is put in, but painkillers can help.
- There are no serious side effects of using emergency contraception.
- Emergency contraception doesn’t cause an abortion.
Places to get emergency contraception include:
- your primary care doctor’s office
- college/university and women’s health centers
- public health departments
- hospital emergency departments
- Planned Parenthood centers (https://www.plannedparenthood.org/).
How do I get emergency contraception?
It depends on the type of emergency contraception you need.
- Plan B One-Step® and similar generic versions are available in stores without a prescription to anyone, of any age. If you do not see it on the shelf, ask the pharmacist for help.
- Levonorgestrel tablets (two-pill generic Next Choice® and LNG tablets 0.75 mg) are available to people aged 17 and older without a prescription. These brands are sold from behind the pharmacy counter.
- ella® (ulipristal acetate) is available only by prescription from your doctor, nurse, or family planning clinic.
To find a low-cost family planning clinic for emergency contraception, enter your ZIP code into the clinic finder on this page.
How can I get free or low-cost emergency contraception?
Under the Affordable Care Act (the health care law), most insurance plans cover FDA-approved prescriptions for emergency contraception and birth control at no cost to you. This includes Plan B One-Step® and ella®. Since you can buy Plan B One-Step® or the generic version in a store, without a prescription, call your insurance company to find out if your plan covers over-the-counter emergency contraception. You may need to get a prescription from your doctor if you want your insurance plan to pay for it.
- If you have insurance, check with your insurance provider to find out what’s included in your plan.
- If you have Medicaid, your insurance may cover emergency contraception. Coverage varies between states, so check with your state’s Medicaid program to learn about your benefits.
- If you don’t have insurance, find a family planning clinic in your area. They may provide emergency contraception for free or at low cost.
- To see if you are eligible for low-cost or no-cost health insurance, visit HealthCare.gov.
For information about other services covered by the Affordable Care Act, visit HealthCare.gov.
When should I think about using emergency contraception?
Consider using emergency contraception if you had sex and:
- You didn’t use birth control
- You think your birth control didn’t work
Consider asking your doctor for a prescription for emergency contraception pills, or having some type of emergency contraception pill already at home or with you in case you need it.
How quickly should I use emergency contraception after unprotected sex?
Emergency contraception works best when you use it as soon as possible after unprotected sex. If you are unable to take it right away, emergency contraception can still work to prevent pregnancy if taken up to three to five days after unprotected sex. How long after depends on which type of emergency contraception you use.
- Take Plan B One-Step® or a generic version as soon as possible within three days (or 72 hours) after unprotected sex.
- For the two-dose version (Next Choice®, LNG tablets 0.75 mg), take one pill as soon as possible within 3 days and the second pill 12 hours later.
- Take ella® (ulipristal acetate) as soon as possible within five days (or 120 hours) after unprotected sex.
Can I get emergency contraception pills before I need them?
Yes. Your doctor can give you a prescription to fill so you can have emergency contraception at home to use when you need it. Or, you can buy some types of emergency contraception pills from a store at any time.
Does emergency contraception have side effects?
Yes, but the side effects are rarely serious. Side effects differ for each woman and may include:
- Headache
- Abdominal pain
- Tiredness (fatigue)
- Dizziness
- Nausea
- Breast pain
The side effects are usually mild and do not last long. Your next period may come early or late, and you may have spotting (light bleeding that happens between menstrual periods).
Will emergency contraception pills affect my next period?
Maybe. After you take an emergency contraception pill, your next period may come sooner or later than normal. Most women will get their period within a week of the expected date. Your period also may be heavier, lighter, spotty, and more or less painful than is normal for you.
If you do not get your period more than one week after expected or if you think you might be pregnant after taking emergency contraception pills, take a pregnancy test to find out for sure.
Does body weight affect how well emergency contraception works for women?
Maybe. Research from the Centers for Disease Control and Prevention shows that emergency contraception pills may not prevent pregnancy as often for obese women (with a body mass index, or BMI, of 30 or greater) as for women who are not obese 4.
Find out your BMI here https://www.cdc.gov/healthyweight/assessing/bmi/adult_BMI/english_bmi_calculator/bmi_calculator.html.
If your BMI is greater than 30, talk to your doctor or nurse about your risk and your options for emergency contraception.
Can I use emergency contraception as my regular form of birth control?
No. Do not use Plan B One-Step® (or a generic version) or ella® as your regular birth control. Most other types of FDA-approved birth control, when used correctly, are much better at preventing pregnancy than emergency contraception pills and usually cost less. Also, while emergency contraception pills are safe for emergency use, they have not been tested as regular birth control and are not approved by the FDA for this purpose.
Women who are sexually active will need to use birth control to prevent pregnancy. What type of regular birth control you can use right away depends on the type of emergency contraception you take.
- If you take ella® (ulipristal acetate), do not use hormonal birth control (the pill, patch, vaginal ring, or intrauterine device) for at least five days after you take ella. Using them together may cause ella® not to work. Instead, use a condom, diaphragm, sponge, or cervical cap until you get your next period.10
- If you take Plan B One-Step® (or a generic version), you can start right away or continue using a regular form of birth control.
Read more about different types of birth control in our birth control methods fact sheet.
Will emergency contraception protect me from sexually transmitted infections (STIs)?
No. Emergency contraception does not protect you from sexually transmitted infections or diseases (STIs). To lower your risk of getting an STI, always use condoms when you have vaginal, oral, or anal sex.
See a doctor right away if you think you may have been exposed to an sexually transmitted infection (STI). Also, you can get medicine to help prevent HIV, the virus that causes AIDS.
If you were sexually assaulted, go to the nearest hospital emergency room as soon as possible. The National Sexual Assault Hotline at 800-656-4673 (https://www.rainn.org/about-national-sexual-assault-telephone-hotline) can help you find a hospital able to collect evidence of sexual assault. You can get medicine to prevent HIV and other STIs and get emergency contraception to prevent pregnancy.
What does it mean for birth control to “fail” or not work correctly?
Depending on the method of birth control you use, not working correctly means different things.
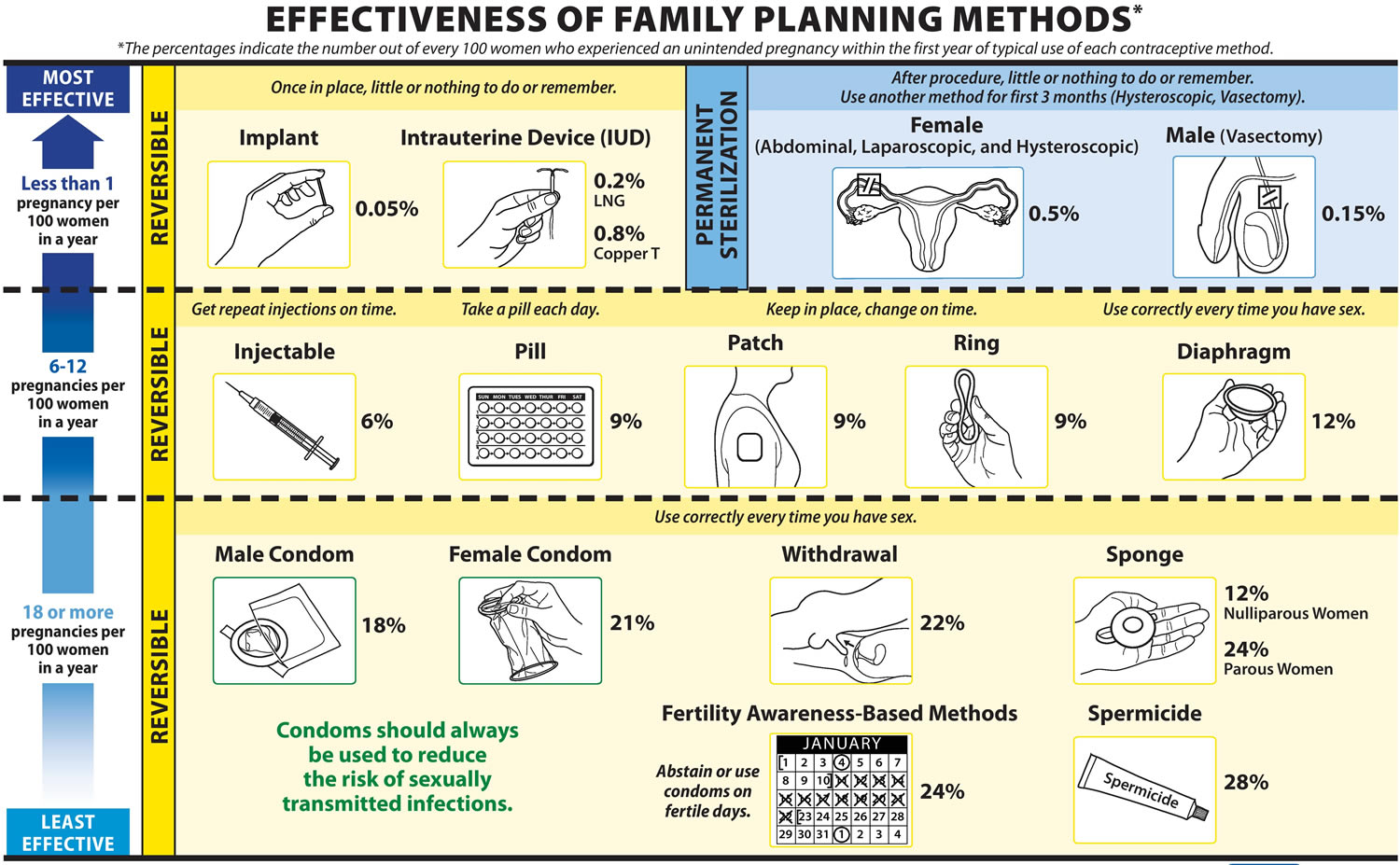
Table 1. Birth Control Chart
| Birth control method | Failure rate (number of pregnancies per 100 women in a year) | Examples of what can go wrong with your birth control |
|---|---|---|
| Natural planning method | 24 out of 100 women get pregnant | You have sex on the fertile days of your cycle and do not use another form of birth control (such as a condom or spermicide) |
| Cervical cap | 23 out of 100 women get pregnant (women who have given birth)13 out of 100 women get pregnant (women who have never given birth)5 | Slips off the cervix or has a tear/hole in the cap; is not used with spermicide |
| Male condom | 18 out of 100 women get pregnant | Breaks or comes off at any time during sex |
| Diaphragm with spermicide | 12 out of 100 women get pregnant | Slips out of place or has a tear or hole in it; is not used with a spermicide |
| Hormonal birth control pills | 9 out of 100 women get pregnant | You do not take a pill every day, as directed |
| Vaginal ring | 9 out of 100 women get pregnant | You put it in too late or take it out too soon during the month |
| Birth control patch | 9 out of 100 women get pregnant | You put it on too late or take it off too soon during the month, or it does not stick to your skin correctly |
| Hormonal birth control shot | 6 out of 100 women get pregnant | You are more than two weeks late getting the shot |
| Intrauterine device (IUD) | Less than 1 out of 100 women get pregnant* | Comes out before you are ready for it to be removed |
| Implantable rod | Less than 1 out of 100 women get pregnant | The rod is not removed or replaced in time (up to three years after it is placed in your arm) |
*This number may be higher, depending on when the IUD came out and how long before it was noticed.
[Sources 6, 7]Figure 1. Birth Control Methods Effectiveness Chart
[Sources 7]Copper-T Intrauterine Device (IUD) as Emergency Contraception
ParaGard, a copper intrauterine device (IUD), is a small, T-shaped device that is placed inside your uterus. Unlike pills, intrauterine devices (IUDs) don’t stop your ovaries from releasing an egg. Copper-T intrauterine devices (IUDs) can prevent an egg from being fertilized or implanted. An intrauterine device (IUD) is very effective for emergency contraception. It can reduce your risk of pregnancy by more than 99%. Copper intrauterine device (IUD) is more effective than the emergency contraception pill at preventing pregnancy after unprotected sex. This is if your doctor inserts it within 5 days of sex. This IUD can be left in your body for up to 10 years to prevent pregnancy. Some women use intrauterine devices (IUDs) as their regular form of birth control. Common side effects of a ParaGard IUD are heavier, longer periods and spotting or cramping between periods. Symptoms usually improve in the first 3 to 6 months.
As emergency contraception, the Copper-T IUD is much more effective than either type of emergency contraceptive pill (or “morning after pill”) because it reduces your risk of getting pregnant by more than 99%. Another advantage to the Copper-T IUD is that you can keep it in place to prevent pregnancy for up to ten years.
If you have been made to have sex against your will, or believe that you or your partner may be at risk for STIs (sexually transmitted diseases/infections), tell your doctor. If you have pelvic inflammatory disease (PID) or an active gonorrhea or Chlamydia infection, IUD insertion is not recommended. However, if you have an asymptomatic gonorrhea or Chlamydia infection, IUD insertion is considered safe. Your doctor can test you for STIs (sexually transmitted diseases/infections) and insert your IUD at the same time; if the test comes back positive for an STI, you can be treated with antibiotics right away.
Fertilized ovum implantation occurs 6-12 days following ovulation 8. Therefore, copper IUDs can be inserted up to 5 days after ovulation to prevent pregnancy. Thus, if a woman had unprotected intercourse three days before ovulation occurred in that cycle, the IUD could prevent pregnancy if inserted up to 8 days after intercourse. Because of the difficulty in determining the day of ovulation, however, many protocols recommend insertion up to only 5 days after unprotected intercourse. The latest World Health Organization guidelines allow IUDs to be inserted up to day 12 of the cycle with no restrictions and at any other time in the cycle if it is reasonably certain that she is not pregnant 9. A copper IUD can also be left in place to provide effective ongoing contraception for up to 12 years 10. But IUDs are not ideal for all women. Women with active sexually transmitted infections (STIs) are not good candidates for IUDs; insertion of the IUD in these women can lead to pelvic infection, which can cause infertility if untreated. Women not exposed to STIs have little risk of pelvic infection following IUD insertion 11 and use of a copper IUD is not associated with an increased risk of tubal infertility among nulligravid women (whereas infection with chlamydia is) 12.
New research about levonorgestrel IUDs as emergency contraception is emerging. One study compared copper IUDs and oral levonorgestrel emergency contraception pills with concomitant placement of a levonorgestrel IUD 13. More women in this study chose oral levonorgestrel emergency contraception plus levonorgestrel IUD (121 women) over the copper IUD (67 women) at the time of their visit. There were no pregnancies in the copper IUD group, and one pregnancy in the levonorgestrel group, which was determined to be an existing luteal phase pregnancy rather than a failure. This study may be too small to widely recommend this approach, but it is a promising area of future research.
Who can use the IUD?
Most women can use an IUD, including those who are HIV positive. A doctor or nurse will ask about your medical history to check if an IUD is suitable for you.
The IUD might not be suitable if you have:
- an untreated sexually transmitted infection (STI) or a pelvic infection
- problems with your womb or cervix
- unexplained bleeding between periods or after sex
The emergency IUD won’t react with any other medicines you’re taking.
Pregnancy and breastfeeding
The IUD shouldn’t be inserted if there’s a risk that you may already be pregnant.
It’s safe to use when you’re breastfeeding and it won’t affect your milk supply.
Side effects of the IUD
Complications after having an IUD fitted are rare, but can include:
- pain
- infection
- damage to the womb
- the IUD coming out of your womb
- heavier, longer or more painful periods if you continue to use it as a regular method of contraception
Morning After Pill
Morning After Pills are also called the “Day After Pills”, the name is misleading – the morning after pill can be used straight after sex and the morning after pill can be taken up to three or up to five days (120 hours) after sex to prevent pregnancy, depending on the type of pill. Emergency contraception pill should be taken as soon as possible after sex in order to be effective. In the U.S., progestin-only (levonorgestrel-only) emergency contraception pill is available on the shelf without age restrictions to women and men. Look for Plan B One-Step, Take Action, Next Choice One-Dose, My Way or other generics in the family planning aisle.
Emergency contraception pills are stocked by all major pharmacy chains, but be sure to call ahead to make sure that emergency contraception pill is available in your pharmacy. Regulations on the sale of emergency contraception pill have changed frequently, so it can be quite confusing. Below is some information about how the different brands of emergency contraception pill are sold. If you want to use ella (ulipristal acetate), you need a prescription from a doctor first before calling the pharmacy to be sure that it is in stock.
- Progestin-only (levonorgestrel-only) emergency contraception (like Plan B One-Step and its generic forms Take Action, Next Choice One Dose and My Way) are approved for unrestricted sale on store shelves. Anyone can buy it without needing to show ID.
- If you want to use insurance to purchase emergency contraception, go to the pharmacy counter and ask for help.
- You can order a generic form of Plan B One-Step at www.afterpill.com for $20 + $5 shipping. This site does not offer expedited shipping, so it’s not meant for emergency use, but you can stock up and keep it on hand for future use.
- ella is sold by prescription only, regardless of age. You can also order ella online at KwikMed or prjktruby, including next-day shipping.
Emergency contraception pills have no long-term or serious side effects, and it is safe for almost every woman to use them.
There are four different types of emergency contraception pills (“morning after pills”) available around the world, but the actual active ingredient (medicine) is the same in all of them. Most of the time, when someone mentions “emergency contraceptive pills,” “morning after pills,” or the “day after pill,” they are talking about using the same hormones found in regular daily oral contraceptive pills to reduce your chances of becoming pregnant if you had sex without using contraception, you think your birth control failed, or you were made to have sex against your will.
- The first type of emergency contraceptive pill contains a hormone called progestin or levonorgestrel. Progestin-only pills can reduce your risk of getting pregnant by 88%. You are also less likely to have side effects if you use these pills for emergency contraception, as compared with combined pills.
- The second type of emergency contraceptive pill contains ulipristal acetate, and is available by prescription only in the United States (sold as ella) and Europe (sold as ellaOne). It has been found to be highly effective and well-tolerated. It can be taken up to 5 days after unprotected sex, and is believed to be more effective than levonorgestrel emergency contraception pills.
- The third type of emergency contraceptive pill uses both the hormones progestin and estrogen (learn more about these “combined” emergency contraceptive pills). Many brands of the combined daily birth control pill can be used for emergency contraception in the United States (find out which ones here). These pills cut your chances of getting pregnant by 75%, and you are more likely to experience side effects like nausea and vomiting.
- The fourth type of emergency contraceptive pill contains small doses of mifepristone. This pill is also highly effective, with few side-effects. This type of emergency contraceptive pill is currently available only in China, Vietnam, Armenia and Russia.
Progestin-only emergency contraception pills
Progestin-only emergency contraceptive pills (“morning after pills”) are pills that contain levonorgestrel, a type of the hormone progestin researchers have found prevents pregnancy when taken in the few days after sex. In the United States, there are several dedicated progestin-only emergency contraceptive products that may be for sale, such as Plan B One-Step.
Progestin-only emergency contraception pills contain no estrogen. Only the progestin levonorgestrel has been studied for freestanding use as an emergency contraceptive. The original treatment schedule was one 0.75 mg dose within 72 hours after unprotected intercourse, and a second 0.75 mg dose 12 hours after the first dose. However, studies have shown that a single dose of 1.5 mg is as effective as two 0.75 mg doses 12 hours apart 14, 15. One of these studies showed no difference in side effects between the two regimens 14, while the other found greater levels of headache and breast tenderness (but not other side effects) among study participants taking 1.5 mg of levonorgestrel at once 15. Increasingly, levonorgestrel is marketed internationally in a one-dose formulation (one 1.5 mg pill) rather than the two-dose formulation (two 0.75 mg tablets, taken 12 hours apart). Another study found that two 0.75 mg doses 24 hours apart were just as effective as two 0.75 mg doses 12 hours apart 16. The progestin-only products available in the United States include are Plan B One-Step (1.5 mg), approved by the FDA in July 2009 and several generic forms of Plan B One-Step including Next Choice One Dose, My Way, Take Action and AfterPill; two-dose levonorgestrel emergency contraception pills are no longer sold in the US.
Plan B One-Step and its generic forms such as Take Action, Next Choice One Dose and My Way contain 1.5 mg of levonorgestrel in just one pill, which you take as soon as possible after sex. Research shows that you can use emergency contraception up to 120 hours after sex, although it is best to take it as soon as possible after sex. About one woman in four (23%) feels sick to her stomach and about one in 17 (6%) throws up after taking progestin-only emergency contraception.
Progestin-only emergency contraceptive pills reduce your risk of pregnancy by about 88%. Don’t worry, that doesn’t mean 12% of women get pregnant using these morning after pills. It just means that this type of emergency contraception prevents 88% of the pregnancies researchers would expect would happen when a woman doesn’t use birth control, her contraception fails (like the condom breaks or falls off), or she is made to have sex against her will. Usually, if 100 women have sex without using birth control one time during the second or third week of their menstrual cycle, about 8 of them will get pregnant. But if those same 100 women also use progestin-only emergency contraceptive pills, only one will get pregnant. These pills work better the sooner you take them after sex.
In addition to progestin-only emergency contraception, there is another emergency contraception pill available in the US, called ella® (ulipristal acetate). This is the most effective emergency contraception pill available here, and it is sold by prescription only. You can also use certain brands of birth control pills that contain two hormones (both progestin and estrogen) or the Copper-T IUD to prevent pregnancy after sex.
The second-generation antiprogestin ulipristal acetate (30 mg in a single dose) has been studied for use as emergency contraception and has been found to be highly effective and well-tolerated 17. It has been marketed for use as emergency contraception in Europe since October 2009; it was approved by the FDA in August 2010 and is available for sale by prescription only, marketed under the brand name ella. Ulipristal acetate EC (sold as ellaOne) is available without prescription in Europe.
The antiprogestin mifepristone has also been extensively studied for use as an emergency contraceptive pill. Mifepristone is a first-generation progesterone receptor modulator that is approved for use in many countries for early first-trimester medication abortion. Mifepristone has been shown to be highly effective for use as emergency contraception, with few side effects (delayed menstruation following the administration of mifepristone is one notable side effect.) 18. However, the use of mifepristone as an abortion pill may limit its widespread acceptability for use for emergency contraception, and it is currently available only in Armenia, Moldova, Ukraine, China, Russia, and Vietnam.
Meloxicam (a COX-2 inhibitor) 30 mg given for five consecutive days in the late follicular phase appears to be an effective emergency contraceptive option. This regimen does not alter the endocrine profile of the cycle and causes no menstrual disturbance 19. In contrast, the COX-2 inhibitor celecoxib appears to have no potential for emergency contraception 20.
In the United States, regulations on the sale of emergency contraception have changed frequently, so it can be quite confusing. Below is some information about how the different brands of emergency contraception are sold. If you want to use ella® (ulipristal acetate), call the pharmacy first to be sure that it is in stock.
- Progestin-only emergency contraception (like Plan B One-Step and its generic forms Take Action, Next Choice One Dose and My Way) are approved for unrestricted sale on store shelves. Anyone can buy it without needing to show ID.
- If you want to use insurance to purchase emergency contraception, go to the pharmacy counter and ask for help.
- You can order a generic form of Plan B One-Step at www.afterpill.com. This site does not offer expedited shipping, so it’s not meant for emergency use, but you can stock up and keep it on hand for future use.
- ella® (ulipristal acetate) is sold by prescription only, regardless of age. You can also order ella online at KwikMed or prjktruby, including next-day shipping.
Who can use the emergency contraception pill?
Most women can use the emergency contraceptive pill. This includes women who can’t use hormonal contraception, such as the combined pill and contraceptive patch. Girls under 16 years old can also use it.
But you may not be able to take the emergency contraceptive pill if you’re allergic to anything in it, have severe asthma or take any medicines that may interact with it, such as:
- the herbal medicine St John’s Wort
- some medicines used to treat epilepsy, HIV or tuberculosis (TB)
- medicine to make your stomach less acidic, such as omeprazole
- some less commonly used antibiotics (rifampicin and rifabutin)
ella® (ulipristal acetate) can’t be used if you’re already taking one of these medicines, as it may not work. Plan B may still be used, but the dose may need to be increased.
Tell a doctor, nurse or pharmacist what medicines you’re taking, and they can advise you if they’re safe to take with the emergency contraceptive pill.
You can also read the patient information leaflet that comes with your medicine for more information.
Breastfeeding
Plan B is safe to take while breastfeeding. Although small amounts of the hormones in the pill may pass into your breast milk, it’s not thought to be harmful to your baby.
The safety of ella® (ulipristal acetate) during breastfeeding isn’t yet known. The manufacturer recommends that you don’t breastfeed for one week after taking this pill.
If you’re already using regular contraception
You may need to take the emergency pill if you:
- forgot to take some of your regular contraceptive pills
- didn’t use your contraceptive patch or vaginal ring correctly
- were late having your contraceptive implant or contraceptive injection
If you have taken Plan B, you should:
- take your next contraceptive pill, apply a new patch or insert a new ring within 12 hours of taking the emergency pill
- continue taking your regular contraceptive pill as normal
Use additional contraception, such as condoms, for:
- 7 days if you use the patch, ring, combined pill (except Qlaira), implant or injection
- 9 days for the combined pill Qlaira
- 2 days if you use the progestogen-only pill
If you have taken ella:
- wait at least 5 days before taking your next contraceptive pill, applying a new patch or inserting a new ring
Use additional contraception, such as condoms, until you restart your contraception and for an additional:
- 7 days if you use the patch, ring, combined pill (except Qlaira), implant or injection
- 9 days for the combined pill Qlaira
- 2 days if you use the progestogen-only pill
A doctor or nurse can advise further on when you can start taking regular contraception and how long you should use additional contraception.
How effective is the morning after pill
7 out of every 8 women who would have gotten pregnant will not become pregnant after taking the Morning-After-Pill. About 2 in every 100 women who use emergency contraception pills will become pregnant despite taking emergency contraception pills within the recommended amount of time. The effectiveness of emergency contraception methods is calculated differently from the effectiveness of other contraceptives because of how they are used. Because emergency contraception does not prevent all pregnancies, a woman should see her doctor if she doesn’t get her next expected period after taking it.
Morning after pill side effects
You should have a normal period within the next month after taking emergency contraceptive pills (also called “morning after pills” or “day after pills”). Sometimes, emergency contraception can change the length of your monthly menstrual cycle, making your next period come as much as a week earlier or a week later than usual. Some women also find that the hormones in the pills can cause unexpected bleeding, but this is not a common or serious side effect. If your next period is late, you might consider getting a pregnancy test.
Researchers 21 have conducted three studies designed specifically to find out how progestin-only emergency contraceptive pills (like Plan B One-Step or Next Choice) affect women’s bleeding patterns. Although the results were somewhat different, each found there were often changes in a woman’s monthly menstrual cycle.
In the first study, women who took the full dose (1.5 mg levonorgestrel) of this emergency contraceptive at one time in the first three weeks of their monthly menstrual cycles got their period much sooner than expected – and earlier than women who did not take the pills. The study also found that the earlier in their cycle women took the pills, the sooner they got their period. Women who took the full dose of emergency contraception in the fourth week of their cycle got their period at the usual time, but it lasted longer than normal. The emergency contraception pills had no effect on the duration of the post-treatment menstrual cycle, but the second period was prolonged. Intermenstrual bleeding was uncommon after emergency contraception pill use, although more common than among women who had not taken emergency contraception pills.
The second study found that women who took the full dose (1.5 mg levonorgestrel) of this emergency contraceptive at one time within two days before or after ovulation (when the egg is released) got their periods when they expected them. But, on average, women started their periods a day earlier when they used emergency contraception more than two days before ovulation, and their periods generally started two days later if they took the pills more than two days after ovulation. Menstrual period duration increased significantly when emergency contraception pills were taken after three days before ovulation in both the treatment and post-treatment cycles. The duration of the post-treatment menstrual cycle remained significantly longer when emergency contraception pills were taken more than two days after ovulation. During the treatment cycle, 15% of women experienced intermenstrual bleeding; this was significantly more common when emergency contraception pills were taken in the preovulatory phase.
A third study examined the effects of two 0.75 mg levonorgestrel pills taken 12 hours apart. When taken in the follicular phase, emergency contraception pills significantly shortened the cycle when compared with usual cycle length; no effect on cycle length was found when emergency contraception pills were taken in the periovulatory or luteal phase. The post-treatment cycle length was the same as the usual cycle length.
A study comparing levonorgestrel (like Plan B One-Step, Next Choice One Dose, Next Choice or Levonorgestrel Tablets) and ulipristal acetate (ella) found that women taking ulipristal acetate had their next period on average 2.1 days later than expected, while women taking levonorgestrel began their next period 1.2 days earlier than expected, but the duration of periods was not affected.
Plan B pill
Plan B (levonorgestrel) emergency contraception pill is used to prevent pregnancy after unprotected sex or failure of other forms of birth control (such as condom breakage, or missing 2 or more birth control pills). The active ingredient in Plan B pill is a medicine called levonorgestrel. Levonorgestrel is a female hormone that work by causing changes in your cervix, making it harder for sperm to reach the uterus and harder for a fertilized egg to attach to the uterus. Each Plan B One-Step tablet contains 1.5 mg of a single active steroid ingredient, levonorgestrel [18,19-Dinorpregn-4-en-20-yn-3-one-13-ethyl-17-hydroxy-, (17α)-(-)-], a totally synthetic progestogen. The inactive ingredients present are colloidal silicon dioxide, potato starch, gelatin, magnesium stearate, talc, corn starch, and lactose monohydrate. Levonorgestrel is a synthetic (man-made) hormone that has been used in birth control pills for over 35 years.
Plan B (levonorgestrel) is a female hormone that is believed to act as an emergency contraceptive principally by preventing ovulation or fertilization (by altering tubal transport of sperm and/or ova) by causing changes in your cervix, making it harder for sperm to reach the uterus and harder for a fertilized egg to attach to the uterus. In addition, Plan B (levonorgestrel) may inhibit implantation (by altering the endometrium). It is not effective once the process of implantation has begun.
Plan B One-Step (levonorgestrel) is in the form of one levonorgestrel pill (1.5 mg levonorgestrel ) that are taken by mouth after unprotected sex. To obtain optimal effectiveness, the first Plan B tablet should be taken as soon as possible within 72 hours of intercourse.
No specific investigation of the absolute bioavailability of Plan B in humans has been conducted. However, literature indicates that levonorgestrel is rapidly and completely absorbed after oral administration (bioavailability about 100%) and is not subject to first pass metabolism. The effect of food on the rate and the extent of levonorgestrel absorption following single oral administration of Plan B has not been evaluated.
Plan B can be used at any time during your menstrual cycle.
- DO NOT USE Plan B pill if you’re pregnant or suspect you’re pregnancy.
- Emergency contraception pill are not effective if a woman is already pregnant!
Plan B is not indicated for routine use as a contraceptive.
If vomiting occurs within two hours of taking either dose of Plan B emergency contraceptive pill, consideration should be given to repeating the dose. Do not take a second dose without first asking your doctor.
Key points
- Take Plan B as soon as possible and not more than 72 hours after unprotected intercourse or a known or suspected contraceptive failure.
- If you vomit within two hours of taking either tablet, immediately contact your healthcare provider to discuss whether to take another tablet.
- Seek medical attention if you experience severe lower abdominal pain 3 to 5 weeks after taking Plan B, in order to be evaluated for an ectopic pregnancy.
- After taking Plan B, consider the possibility of pregnancy if your period is delayed more than one week beyond the date you expected your period.
- Do not use Plan B as routine contraception.
- Plan B is not effective in terminating an existing pregnancy.
- Plan B does not protect against HIV-infection (AIDS) and other sexually transmitted diseases/infections.
Physical Examination and Follow-up
A physical examination is not required prior to prescribing Plan B. A follow-up physical or pelvic examination is recommended if there is any doubt concerning the general health or pregnancy status of any woman after taking Plan B pill.
Is Plan B over the counter?
Yes, progestin-only (levonorgestrel-only) emergency contraception (like Plan B One-Step and its generic forms Take Action, Next Choice One Dose and My Way) are approved for unrestricted sale on store shelves. Anyone can buy it without needing to show ID.
How does the Plan B pill work?
Plan B (levonorgestrel) is a female hormone that is believed to act as an emergency contraceptive principally by preventing ovulation or fertilization (by altering tubal transport of sperm and/or ova) by causing changes in your cervix, making it harder for sperm to reach the uterus and harder for a fertilized egg to attach to the uterus. In addition, Plan B (levonorgestrel) may inhibit implantation (by altering the endometrium). It is not effective once the process of implantation has begun.
- DO NOT USE Plan B pill if you’re pregnant or suspect you’re pregnancy.
- Emergency contraceptive pills are not effective if a woman is already pregnant!
Plan B Pill Important Information
Do not use Plan B (levonorgestrel) if you are already pregnant. Plan B (levonorgestrel) will not terminate a pregnancy that has already begun (the fertilized egg has attached to the uterus).
Plan B (levonorgestrel) is not intended for use as a routine form of birth control and should not be used in this manner. Talk with your doctor about the many alternative types of birth control available.
Ask a doctor or pharmacist before taking Plan B (levonorgestrel) if you regularly use medication for seizures, tuberculosis, or HIV/AIDS. Certain other medicines can make Plan B (levonorgestrel) less effective.
Before taking Plan B pill
You should not use Plan B (levonorgestrel) if you are allergic to it.
- Do not use Plan B (levonorgestrel) pill if you are already pregnant.
- Plan B (levonorgestrel) emergency contraceptive pill will not terminate a pregnancy that has already begun (the fertilized egg has attached to the uterus).
Ask a doctor or pharmacist before taking Plan B (levonorgestrel) if you regularly use medication for seizures, tuberculosis, or HIV/AIDS. Certain medications can make levonorgestrel less effective as an emergency form of contraception.
Plan B (levonorgestrel) emergency contraception pill is not intended for use as a routine form of birth control and should not be used in this manner. Talk with your doctor about the many forms of birth control available.
Plan B (levonorgestrel) pill may slow breast milk production. Tell your doctor if you are breast-feeding.
What should I avoid while taking Plan B emergency contraceptive pill?
Plan B (levonorgestrel) emergency contraceptive pill will not protect you from sexually transmitted diseases–including HIV and AIDS. Using a condom is the only way to protect yourself from these diseases. Avoid having unprotected sex.
What other drugs will affect Plan B?
Certain other medications can make Plan B less effective, which may result in pregnancy.
Drugs or herbal products that induce enzymes, including CYP3A4, that metabolize progestins may decrease the plasma concentrations of progestins, and may decrease the effectiveness of progestin-only pills. Some drugs or herbal products that may decrease the effectiveness of progestin-only (levonorgestrel) pills include:
- barbiturates
- bosentan
- seizure medications–carbamazepine, felbamate, fosphenytoin, phenobarbital, phenytoin, primidone
- griseofulvin
- oxcarbazepine
- rifampin (Rifadin, Rifater, Rifamate, IsonaRif, Rimactane)
- efavirenz (Atripla, Sustiva)
- St. John’s wort
- topiramate
Significant changes (increase or decrease) in the plasma levels of the progestin have been noted in some cases of co-administration with HIV protease inhibitors or with non-nucleoside reverse transcriptase inhibitors.
Do not take this medicine without telling your doctor or pharmacist that you are using any of the following medications.
Consult the labeling of all concurrently used drugs to obtain further information about interactions with progestin-only pills or the potential for enzyme alterations.
This list is not complete. Other drugs may interact with levonorgestrel, including prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible interactions are listed here. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
How should I take Plan B emergency contraception pill?
Use exactly as directed on the label, or as prescribed by your doctor. Do NOT use in larger or smaller amounts or for longer than recommended.
Plan B (levonorgestrel) emergency contraception pill must be taken as soon as possible after unprotected sex (no later than 72 hours afterward).
Call your doctor right away if you vomit within 2 hours after taking Plan B (levonorgestrel) pill. Do not take a second dose without first asking your doctor.
Visit your doctor within 3 weeks after taking Plan B (levonorgestrel) emergency contraception pill. A doctor should confirm that you are not pregnant, and that Plan B (levonorgestrel) emergency contraception pill has not caused any harmful effects.
If your period is late by 1 week or longer after the expected date, you may be pregnant. Get a pregnancy test and contact your doctor if you are pregnant. Plan B (levonorgestrel) emergency contraception pill will not terminate pregnancy if the fertilized egg has attached to the uterus.
Store at room temperature away from moisture and heat.
Plan B Dosage
- Plan B One-Step tablet is supplied as an almost white, round tablet containing 1.5 mg of levonorgestrel and is marked G00 on one side.
- If taking Plan B One-Step (1.5 mg of levonorgestrel) only 1 (one) dose is required as soon as possible within 72 hours after unprotected intercourse or a known or suspected contraceptive failure. Efficacy is better if the tablet is taken as soon as possible after unprotected intercourse. Plan B One-Step can be used at any time during the menstrual cycle.
If vomiting occurs within two hours of taking either dose of medication, consideration should be given to repeating the dose. Call your doctor right away if you vomit within 2 hours after taking Plan B One-Step (1.5 mg levonorgestrel) pill. Do not take a second dose without first asking your doctor.
What happens if I miss a dose?
Since Plan B One-Step (1.5 mg levonorgestrel) emergency contraception pill is used as a single dose, it does not have a daily dosing schedule.
What happens if I overdose?
Because Plan B (levonorgestrel) emergency contraception pill is supplied as a single tablet in an exact strength, an overdose is unlikely to occur when the Plan B is used as directed. Do not take more than one tablet at the same time.
There are no data on overdosage of Plan B, although the common adverse event of nausea and associated vomiting may be anticipated.
How effective is Plan B?
7 out of every 8 women who would have gotten pregnant will not become pregnant after taking Plan B pill. About 2 in every 100 women who use emergency contraception pills will become pregnant despite taking emergency contraception pills within the recommended amount of time. The effectiveness of emergency contraception methods is calculated differently from the effectiveness of other contraceptives because of how they are used. Because emergency contraception does not prevent all pregnancies, a woman should see her doctor if she doesn’t get her next expected period after taking it.
Plan B (levonorgestrel) pill will not terminate pregnancy if the fertilized egg has already attached to the uterus.
Emergency contraceptives are not as effective as routine hormonal contraception since their failure rate, while low based on a single use, would accumulate over time with repeated use.
A double-blind, randomized, multinational controlled clinical trial in 1,955 evaluable women (mean age 27) compared the efficacy and safety of Plan B (one 0.75 mg tablet of levonorgestrel taken within 72 hours of unprotected intercourse, and one tablet taken 12 hours later) to the Yuzpe regimen (two tablets each containing 0.25 mg levonorgestrel and 0.05 mg ethinyl estradiol, taken within 72 hours of intercourse, and two additional tablets taken 12 hours later). After a single act of intercourse occurring anytime during the menstrual cycle, the expected pregnancy rate of 8% (with no contraceptive use) was reduced to approximately 1% with Plan B.
No formal studies have evaluated the effect of race. However, clinical trials demonstrated a higher pregnancy rate in Chinese women with both Plan B and the Yuzpe regimen (another form of emergency contraception). The reason for this apparent increase in the pregnancy rate with emergency contraceptives in Chinese women is unknown.
Plan B Pill Warnings and Precautions
Ectopic Pregnancy
Ectopic pregnancies account for approximately 2% of all reported pregnancies. Up to 10% of pregnancies reported in clinical studies of routine use of progestin-only (levonorgestrel) contraceptives are ectopic.
A history of ectopic pregnancy is not a contraindication to use of this emergency contraceptive method. Healthcare providers, however, should consider the possibility of an ectopic pregnancy in women who become pregnant or complain of lower abdominal pain after taking Plan B. A follow-up physical or pelvic examination is recommended if there is any doubt concerning the general health or pregnancy status of any woman after taking Plan B.
Existing Pregnancy
Plan B is not effective in terminating an existing pregnancy.
Effects on Menstrual Period
Some women may experience spotting a few days after taking Plan B (levonorgestrel). Menstrual bleeding patterns are often irregular among women using progestin-only (levonorgestrel) oral contraceptives and women using levonorgestrel for postcoital and emergency contraception.
If there is a delay in the onset of expected menses beyond 1 week, consider the possibility of pregnancy.
Sexually transmitted infections and HIV
Plan B does not protect against HIV infection (AIDS) or other sexually transmitted infections (STIs).
Fertility Following Discontinuation
A rapid return of fertility is likely following treatment with Plan B for emergency contraception; therefore, routine contraception should be continued or initiated as soon as possible following use of Plan B to ensure ongoing prevention of pregnancy.
Plan B pill side effects
Along with its needed effects, levonorgestrel (the active ingredient contained in Plan B) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking Plan B (levonorgestrel):
Common side effects of Plan B (levonorgestrel) may include:
- Changes in your menstrual periods
- Headache
- Nausea
- Dizziness
- Vomiting
- Breast pain
- Tiredness
- Lower stomach (abdominal) pain
- Heavy or light menstrual bleeding – incidence not known;
- Absent, missed or irregular menstrual periods;
- Cramps;
- Pain in the pelvis;
- Stopping of menstrual bleeding;
- Mild stomach pain;
- Breast pain or tenderness;
- Nausea, vomiting, diarrhea;
- Tenderness of the breasts
- Unusual tiredness or weakness
This is not a complete list of side effects and others may occur.
Some side effects of levonorgestrel may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Get emergency medical help if you have signs of an allergic reaction:
- hives;
- difficulty breathing;
- swelling of your face, lips, tongue, or throat.
Call your doctor or seek emergency medical help if you have severe pain in your lower stomach or side. This could be a sign of a tubal pregnancy (a pregnancy that implants in the fallopian tube instead of the uterus). A tubal pregnancy is a medical emergency.
Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
A double-blind, controlled clinical trial in 1,955 evaluable women compared the efficacy and safety of Plan B (one 0.75 mg tablet of levonorgestrel taken within 72 hours of unprotected intercourse, and one tablet taken 12 hours later) to the Yuzpe regimen (two tablets each containing 0.25 mg levonorgestrel and 0.05 mg ethinyl estradiol, taken within 72 hours of intercourse, and two tablets taken 12 hours later).
The most common adverse events (>10%) in the clinical trial for women receiving Plan B included menstrual changes (26%), nausea (23%), abdominal pain (18%), fatigue (17%), headache (17%), dizziness (11%), and breast tenderness (11%). Table 1 lists those adverse events that were reported in ≥ 5% of Plan B users.
Table 2: Plan B Adverse Events in ≥ 5 percent of Women, by percentages Frequency
Plan B (Levonorgestrel) N=977 (%) | |
| Nausea | 23.1 |
| Abdominal Pain | 17.6 |
| Fatigue | 16.9 |
| Headache | 16.8 |
| Heavier Menstrual Bleeding | 13.8 |
| Lighter Menstrual Bleeding | 12.5 |
| Dizziness | 11.2 |
| Breast Tenderness | 10.7 |
| Vomiting | 5.6 |
| Diarrhea | 5.0 |
Use in specific populations
Pregnancy
Many studies have found no harmful effects on fetal development associated with long-term use of contraceptive doses of oral progestins. The few studies of infant growth and development that have been conducted with progestin-only pills have not demonstrated significant adverse effects.
Breastfeeding
In general, no adverse effects of progestin-only pills have been found on breastfeeding performance or on the health, growth or development of the infant. However, isolated post-marketing cases of decreased milk production have been reported. Small amounts of progestins pass into the breast milk of nursing mothers taking progestin-only pills for long-term contraception, resulting in detectable steroid levels in infant plasma.
Pediatric Use
Safety and efficacy of progestin-only pills for long-term contraception have been established in women of reproductive age. Safety and efficacy are expected to be the same for postpubertal adolescents under the age of 16 and for users 16 years and older. Use of Plan B emergency contraception before menarche is not indicated.
Race
No formal studies have evaluated the effect of race. However, clinical trials demonstrated a higher pregnancy rate in Chinese women with both Plan B and the Yuzpe regimen (another form of emergency contraception). The reason for this apparent increase in the pregnancy rate with emergency contraceptives in Chinese women is unknown.
Hepatic Impairment
No formal studies were conducted to evaluate the effect of hepatic disease on the disposition of Plan B.
Renal Impairment
No formal studies were conducted to evaluate the effect of renal disease on the disposition of Plan B.
Emergency Contraception Pills – Options
You can also use a different dose of a number of brands of regular birth control pills. While these are not sold specifically as emergency contraceptive pills, they have been proven safe and effective for preventing pregnancy in the few days after sex. These daily birth control pills contain two hormones, progestin and estrogen, and are taken in two doses. You take the first dose as soon as possible (up to 120 hours after you have sex without using birth control, your birth control failed, or you were made to have sex against your will. You take the second dose 12 hours later (although being an hour or two early or late probably won’t make a difference in how effective the pills are).
Here are some other things to know about taking emergency contraceptive pills:
- Don’t take more than one kind of emergency contraception. The active ingredients in ella, Plan B One-Step (and its generic forms) may counteract each other and make your emergency contraception ineffective.
- Don’t take extra pills. They probably won’t reduce your risk of pregnancy any more than the recommended dose for emergency contraception. But they will make it more likely you’ll feel sick to your stomach (one of the more common side effects).
- If you feel sick to your stomach, it should be only mild nausea that goes away in a day or so.
- If you throw up within an hour after taking the pills, call your health care provider. You may need to repeat a dose, and it might make sense to take some anti-nausea medication.
- If you have any other symptoms you are worried about, contact your health care provider. Ask for an appointment right away if you have:
- Severe pain in your leg (calf or thigh)
- Several abdominal pain
- Chest pain or cough or shortness of breath
- Severe headaches, dizziness, weakness, or numbness
- Blurred or loss of vision or trouble speaking
- Jaundice (if you see a yellowish tint in the whites of your eyes, your skin, or your mucus membranes)
- Your next period should start within the next month, although it might come a few days early or late. If you don’t get your period by the time you expect it, you might consider getting a pregnancy test.
- Start using a regular birth control method you think you’ll be able to use every time you have sex because that will be more effective than relying only on emergency contraception. And, if there’s any chance you could be at risk of sexually transmitted infections, use a condom.
The table below lists all of the brands of oral contraception available in the U.S. which you can use to prevent pregnancy in the few days after sex. For information about how to use a specific pill as an emergency contraceptive, click on the brand name in the table.
Table 3. Oral contraceptives that can be used for emergency contraception in the United States
| Brand | Company | First Dose | Second Dose (12 hours later) | Ulipristal Acetate per Dose (mg) | Ethinyl Estradiol per Dose (µg) | Levonorgestrel per Dose (mg) |
| Ulipristal acetate (Dedicated EC pills) | ||||||
| ella | Afaxys | 1 white pill | None | 30 | – | – |
| Progestin-only (Dedicated EC pills) | ||||||
| Afterab | Teva | 1 white pill | None | – | – | 1.5 |
| AfterPillc | Syzygy | 1 white pill | None | – | – | 1.5 |
| Athentia Next | Aurobindo | 1 white pill | None | – | – | 1.5 |
| EContra Ezd | Afaxys | 1 white pill | None | – | – | 1.5 |
| Fallback Solo | Lupin | 1 white pill | None | – | – | 1.5 |
| My Way | Gavis | 1 white pill | None | – | – | 1.5 |
| Next Choice One Dose | Actavis | 1 peach pill | None | – | – | 1.5 |
| Opcicon One-Step | Sun Pharma | 1 white pill | None | – | – | 1.5 |
| Option 2 | Perrigo | 1 white pill | None | – | – | 1.5 |
| Plan B One-Step | Teva | 1 white pill | None | – | – | 1.5 |
| Take Action | Teva | 1 white pill | None | – | – | 1.5 |
| Combined progestin and estrogen pills (Regular oral contraceptive pills) | ||||||
| Afirmelle | Aurobindo | 5 white pills | 5 white pills | – | 100 | 0.50 |
| Altavera | Sandoz | 4 peach pills | 4 peach pills | – | 120 | 0.60 |
| Amethia | Actavis | 4 white pills | 4 white pills | – | 120 | 0.60 |
| Amethia Lo | Actavis | 5 white pills | 5 white pills | – | 100 | 0.50 |
| Amethyst | Actavis | 6 white pills | 6 white pills | – | 120 | 0.54 |
| Aubra | Afaxys | 5 white pills | 5 white pills | – | 100 | 0.50 |
| Ayuna | Aurobindo | 4 orange pills | 4 orange pills | – | 100 | 0.50 |
| Aviane | Teva | 5 orange pills | 5 orange pills | – | 100 | 0.50 |
| Camrese | Teva | 4 light blue-green pills | 4 light blue-green pills | – | 120 | 0.60 |
| CamreseLo | Teva | 5 orange pills | 5 orange pills | – | 100 | 0.50 |
| Chateal | Afaxys | 4 white pills | 4 white pills | – | 120 | 0.60 |
| Crysellee | Teva | 4 white pills | 4 white pills | – | 120 | 0.60 |
| Elineste | Novast | 4 orange pills | 4 orange pills | – | 120 | 0.60 |
| Enpresse | Teva | 4 orange pills | 4 orange pills | – | 120 | 0.50 |
| Falmina | Novast | 5 orange pills | 5 orange pills | – | 100 | 0.50 |
| Introvale | Sandoz | 4 peach pills | 4 peach pills | – | 120 | 0.60 |
| Jolessa | Teva | 4 pink pills | 4 pink pills | – | 120 | 0.60 |
| Kurvelo | Lupin | 4 peach pills | 4 peach pills | – | 120 | 0.60 |
| Lessina | Teva | 5 pink pills | 5 pink pills | – | 100 | 0.50 |
| Levonest | Novast | 4 light brown pills | 4 light brown pills | – | 120 | 0.50 |
| Levora | Actavis | 4 white pills | 4 white pills | – | 120 | 0.60 |
| LoSeasonique | Teva | 5 orange pills | 5 orange pills | – | 100 | 0.50 |
| Low-Ogestrele | Actavis | 4 white pills | 4 white pills | – | 120 | 0.60 |
| Lutera | Actavis | 5 white pills | 5 white pills | – | 100 | 0.50 |
| Marlissa | Glenmark | 4 peach pills | 4 peach pills | – | 120 | 0.60 |
| Myzilra | Novast | 4 yellow pills | 4 yellow pills | – | 120 | 0.50 |
| Nordette | Teva | 4 light-orange pills | 4 light-orange pills | – | 120 | 0.60 |
| Orsythia | Vintage | 5 pink pills | 5 pink pills | – | 100 | 0.50 |
| Portia | Teva | 4 pink pills | 4 pink pills | – | 120 | 0.60 |
| Quasense | Actavis | 4 white pills | 4 white pills | – | 120 | 0.60 |
| Seasonale | Teva | 4 pink pills | 4 pink pills | – | 120 | 0.60 |
| Seasonique | Teva | 4 light-blue-green pills | 4 light-blue-green pills | – | 120 | 0.60 |
| Setlakin | Novast | 4 pink pills | 4 pink pills | – | 120 | 0.60 |
| Sronyx | Actavis | 5 white pills | 5 while pills | – | 100 | 0.50 |
| Triphasil | Wyeth | 4 yellow pills | 4 yellow pills | – | 120 | 0.50 |
| Trivora | Actavis | 4 pink pills | 4 pink pills | – | 120 | 0.50 |
| Vienva | Sandoz | 5 white pills | 5 white pills | – | 100 | 0.50 |
Notes:
a ella and the levonorgestrel EC products listed in the top section are dedicated products specifically marketed for emergency contraception. The regular oral contraceptives listed above have been declared safe and effective for use as ECPs by the United States Food and Drug Administration. In the U.S., levonorgestrel EC, like Plan B One-Step and Take Action, is available on the shelf with no restrictions. ella is available by prescription only.
b Aftera is sold exclusively at CVS stores
c Afterpill is sold online at www.afterpill.com
d EContra EZ is sold at family planning clinics and online at www.kwikmed.com
e The progestin in Cryselle, Elinest, and Low-Ogestrel is norgestrel, which contains two isomers, only one of which (levonorgestrel) is bioactive; the amount of norgestrel in each tablet is twice the amount of levonorgestrel.
- Finer LB, Zolna MR. Declines in Unintended Pregnancy in the United States, 2008–2011. New England Journal of Medicine. 2016;374:843-52.[↩]
- Gemzell-Danielsson K., Berger, C., Lalitkumar, P.G. (2014). Mechanisms of action of oral emergency contraception. Gynecological Endocrinology 30 (10): 685-687. https://www.ncbi.nlm.nih.gov/pubmed/25117156[↩]
- FDA’s Decision Regarding Plan B: Questions and Answers. https://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm109795.htm[↩]
- Curtis, K.M., Tepper, N.K., Jatlaoui, T.C., et al. (2016). U.S. Medical Eligibility Criteria for Contraceptive Use, 2016. MMWR Recomm Rep; 65(RR-3):1–104. Appendix A. https://www.cdc.gov/mmwr/volumes/65/rr/rr6503a1_appendix.htm[↩][↩]
- Birth Control. https://www.fda.gov/ForConsumers/ByAudience/ForWomen/FreePublications/ucm313215.htm[↩]
- Birth Control Chart. U.S. Food and Drug Administration. https://www.fda.gov/forconsumers/byaudience/forwomen/freepublications/ucm522453.htm[↩]
- Centers for Disease Control and Prevention. (2014). Effectiveness of Family Planning Methods. https://www.cdc.gov/reproductivehealth/UnintendedPregnancy/PDF/Family-Planning-Methods-2014.pdf[↩][↩]
- Wilcox AJ, Baird DD, Weinberg CR. Time of implantation of the conceptus and loss of pregnancy. N Engl J Med. 1999;340:1796-9.[↩]
- Selected practice recommendations for contraceptive use. Second Edition. Geneva: World Health Organization, 2004.[↩]
- United Nations Development Programme, United Nations Population Fund, World Health Organization, World Bank Special Programme of Research, Development and Research Training in Human Reproduction. Long-term reversible contraception. Twelve years of experience with the TCu380A and TCu220C. Contraception. 1997;6:341-52.[↩]
- Farley TMM, Rosenberg MJ, Rowe PJ, Chen J-H, Meirik O. Intrauterine devices and pelvic inflammatory disease: an international perspective. Lancet. 1992;339:785-8.[↩]
- Hubacher D, Lara-Ricalde R, Taylor DJ, Guerra-Infante F, Guzmán-Rodríguez R. Use of copper intrauterine devices and the risk of tubal infertility among nulligravid women. N Engl J Med. 2001;345:561-7.[↩]
- Turok DT, Sanders JN, Thompson IS, Royer PA, Eggebroten J, Gawron L. Preference for and efficacy of oral levonorgestrel for emergency contraception with concomitant placement of a levonorgestrel IUD: a prospective cohort study. Contraception. 2016;93:526-32.[↩]
- von Hertzen H, Piaggio G, Ding J, Chen J, Song S, Bártfai G, Ng E, Gemzell-Danielsson K, Oyunbileg A, Wu S, Cheng W, Lüdicke F, Pretnar-Darovec A, Kirkman R, Mittal S, Khomassuridze A, Apter D, Peregoudov A. Low dose mifepristone and two regimens of levonorgestrel for emergency contraception: a WHO multicentre randomised trial. Lancet. 2002;360:1803-10.[↩][↩]
- Arowojolu AO, Okewole IA, Adekunle AO. Comparative evaluation of the effectiveness and safety of two regimens of levonorgestrel for emergency contraception in Nigerians. Contraception. 2002;66:269-73.[↩][↩]
- Ngai SW, Fan S, Li S, Cheng L, Ding J, Jing X, Ng EHY, Ho PC. A randomized trial to compare 24h versus 12h double dose regimen of levonorgestrel for emergency contraception. Hum Reprod. 2004;20:307-11.[↩]
- Creinin MD, Schlaff W, Archer DF, Wan L, Frezieres R, Thomas M, Rosenberg M, Higgins J. Progesterone receptor modulator for emergency contraception: a randomized controlled trial. Obstet Gynecol. 2006;108:1089-97.[↩]
- Shen J, Che Y, Showell E, Chen K, Cheng L. Interventions for emergency contraception. Cochrane Database Syst Rev. 2017, Issue 7.[↩]
- Hester KE, Harper MJK, Duffy DM. Oral administration of the cyclooxygenase-2 (COX-2) inhibitor meloxicam blocks ovulation in non-human primates when administered to simulate emergency contraception. Hum Reprod. 2010;25:360-7.[↩]
- Edelman AB, Jensen JT, Doom C, Hennebold JD. Impact of the prostaglandin synthase-2 inhibitor celecoxib on ovulation and luteal events in women. Contraception. 2013;87:352-7.[↩]
- Emergency Contraception: A Last Chance to Prevent Unintended Pregnancy. http://ec.princeton.edu/questions/ec-review.pdf[↩]
- Types of Emergency Contraception. http://ec.princeton.edu/questions/dose.html[↩]