Contents
What is epithelial cells in urine
Epithelial cells are a type of cell that lines the surfaces of your body. They are found on your skin, blood vessels, urinary tract, and organs. There are three types of epithelial cells that line the urinary tract. They are called transitional cells, renal tubular cells, and squamous cells. It’s normal to have a small amount of epithelial cells in your urine. A large amount of epithelial cells in your urine may indicate an infection, kidney disease, or other serious medical condition. If there are squamous epithelial cells in your urine, it may mean your urine sample was contaminated. This means that the urine sample contains cells from the urethra (in men) or the vaginal opening (in women). It can happen if you do not clean well enough when using the clean catch method.
To reduce the risk of contamination, urine samples should ideally be clean catch. Research data suggest that contamination is more likely in clean-catch urine if the patient is female, the urine sample was taken at home as opposed to the doctor’s surgery and if the patient is a child that had increased nappy use 24 hours prior to presenting at the surgery.
However, an epithelial cells in urine test is also part of a urinalysis called urine cytology, an examination of urine cells under a microscope to rule out bladder cancer 1. Urinary cytology identifies malignant cells that have been exfoliated from the urothelium into the urine. The specificity of urine cytology is greater than 90% 2, while the sensitivity for high-grade disease and carcinoma-in-situ (CIS) can be as high as 80 to 90% 3.
Your health care provider may have ordered an epithelial cells in urine test as part of your regular checkup or if your visual or chemical urine tests showed abnormal results. You may also need this test if you have symptoms of a urinary or kidney disorder. These symptoms may include:
- Frequent and/or painful urination
- Abdominal pain
- Back pain
Epithelial cells in urine test results are often reported as an approximate amount, such as “few,” moderate,” or “many” cells. “Few” cells are generally considered in the normal range. The normal range is less than 15-20 cells per high power field. “Moderate” or “many” cells may indicate a medical condition such as:
- Urinary tract infection (UTI)
- Yeast infection
- Kidney disease
- Liver disease
- Certain types of cancer
If your results are not in the normal range, it doesn’t necessarily mean that you have a medical condition that requires treatment. You may need more tests before you can get a diagnosis. To learn what your results mean, talk to your health care provider.
Type of urine samples
The most common type of urine specimen for cytologic analysis is voided urine. Again, keep in mind that although the submitted sample is marked as a “voided urine”, it is important to determine whether a cystoscopy has been performed, and if so, whether the sample is collected before or after the cystoscopy procedure. In collecting “true” voided urine, one should avoid a “first morning” specimen and collect the “second morning” voided sample, since the overnight urine often contains many degenerated urothelial cells complicating both morphologic and marker analysis. Although there are data to suggest that three specimens of “second morning” voided urine collected over three consecutive days may optimize the detection of urothelial malignancy 4, this is not a common practice, likely because of cost and convenience.
Another common urine sample is catheterized urine, which is usually more cellular than true voided urine but is otherwise identical. Genital contamination may be less of a problem compared to a true voided urine. The wash and brush samples from bladder, ureter, or renal pelves provide a complement to voided urine samples for the evaluation of urinary tract lesions where cystoscopy (or retrograde ureterocystoscopy) is performed at the same time. Depending on whether a suspicious lesion is seen, a washing or brushing may be performed at the same time as well. The advantages of washing and brushing samples include greater cellularity and a more targeted and homogeneous population of urothelial cells to be analyzed. For low grade lesions, cytomorphologic analysis alone for washing or brushing samples can be extremely challenging. In such a setting, correlating the cytology with the cystoscopy finding is essential. In contrast, for high grade lesions, especially carcinoma in situ, there may be many single or loosely cohesive, highly atypical cells on cytology while cystoscopy may or may not show a visible lesion. Biopsy may show only a few tumor cells on the surface (the “clinging” type of carcinoma in situ). A positive cytology coupled with what appears to be a negative cystoscopy or biopsy is another source of the so-called “false” false positive diagnosis. More discussion on this point will be provided in conjunction with the discussion on tumor markers below.
Other specimen types include ileal conduit or neobladder urine, which are often characterized by the presence of many degenerated columnar epithelial cells and inflammatory cells. On occasion, recurrent urothelial carcinoma may be seen, and diagnosis of such lesions can be extremely difficult since many biomarkers (as discussed below) may not be helpful in such a case.
What happens during an epithelial cells in urine test?
Your health care provider will need to collect a sample of your urine. During your office visit, you will receive a container to collect the urine and special instructions to make sure that the sample is sterile. These instructions are often called the “clean catch method.” The clean catch method includes the following steps:
- Wash your hands.
- Clean your genital area with a cleansing pad given to you by your provider. Men should wipe the tip of their penis. Women should open their labia and clean from front to back.
- Start to urinate into the toilet.
- Move the collection container under your urine stream.
- Collect at least an ounce or two of urine into the container. The container will have markings to indicate the amounts.
- Finish urinating into the toilet.
- Return the sample container as instructed by your health care provider.
Cells normally occurring in urine
Normal cell components present in urine are:
- Urothelial cells – basal, intermediate, superficial (umbrella) cells
- Squamous cells – trigone, distal urethra, vagina, squamous metaplasia
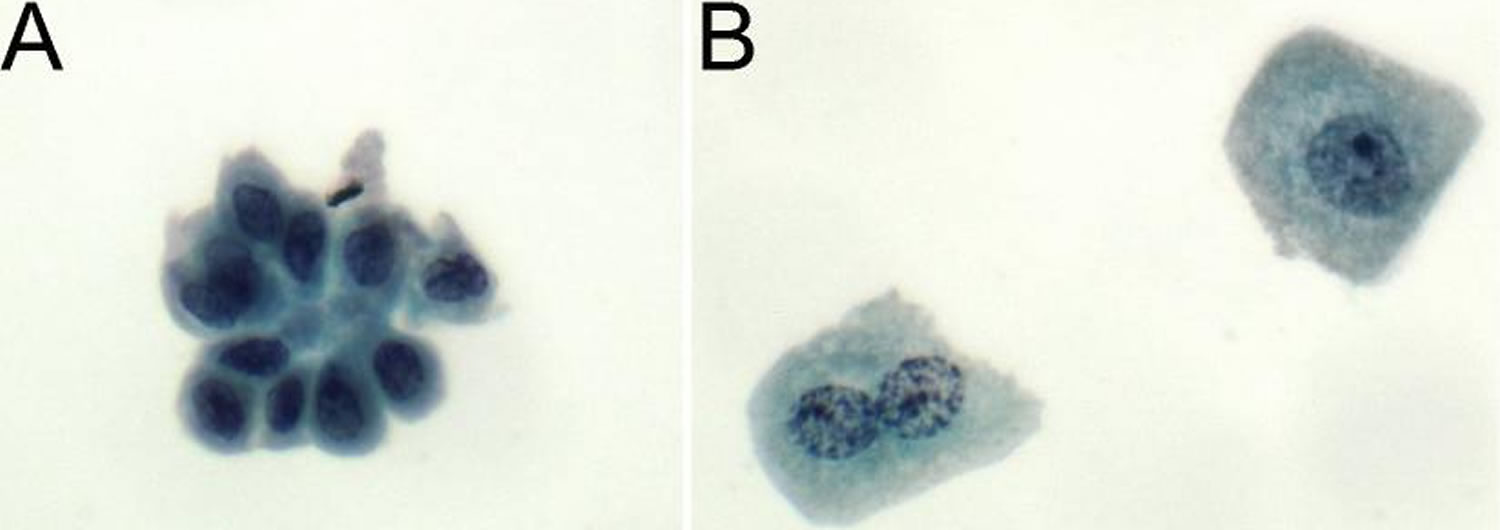
Figure 1. Normal epithelial cells in urine
Footnote: (A) Basal urothelial cells have moderate dense cytoplasm with well-defined borders. Nuclei are centrally-placed with small nucleoli and smooth nuclear contours. (B) Superficial urothelial cells (umbrella cells) have abundant granular cytoplasm with rounded and scalloped borders. Nuclei are large, round, frequently multiple, and centrally placed with prominent nucleoli and smooth nuclear borders.
[Source 1 ]Other cells in urine:
- Glandular cells – prostate, endometrium, cystitis glandularis, paraurethra
- Renal tubular cells (Figure 2)
- Lymphocytes, leukocytes, red blood cells
- Seminal vesicle cells (Figure 3)
What are renal epithelial cells in urine
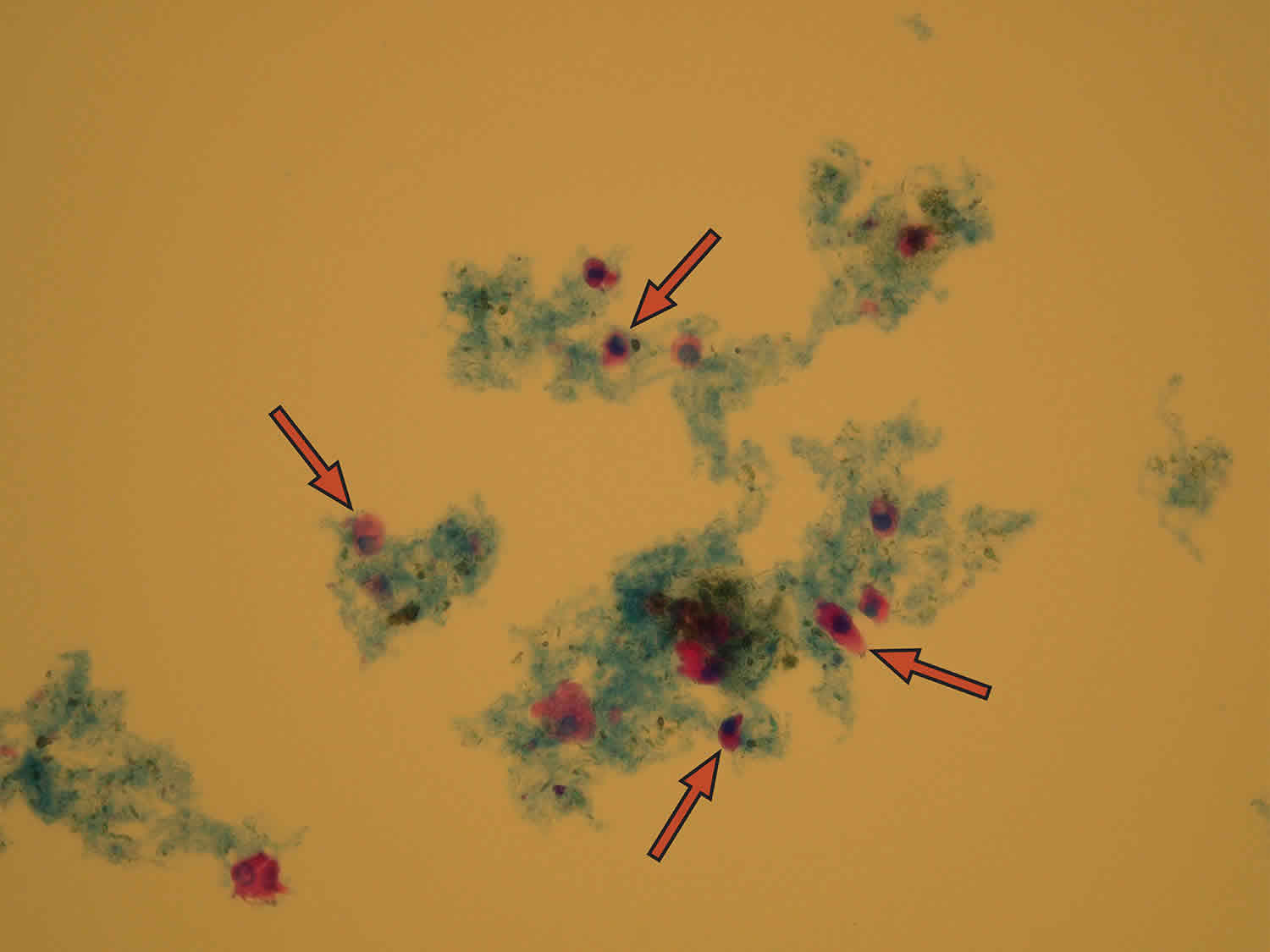
Renal tubular epithelial cells line the renal tubules. Observation of renal tubular epithelial cells in the urine sediment is more significant than observation of other types of epithelial cells. An renal tubular epithelial cell is distinguished by its polyedric shape with non-segmented eccentrically placed nucleus. Renal tubular epithelial cells can be round, oval, columnar, or cuboidal. Renal tubular epithelial cells are the smallest epithelial cells, approximately twice the size of a leukocyte. Renal tubular epithelial cells don’t absorb water and swell, but keep their polyedric shape. Proximal tubular cells have granulated cytoplasm and sometimes may appear as small or fragmented granular casts. They are clinically significant elements in urine in cases of acute tubular necrosis or viral infection and drug or heavy metal toxicity.
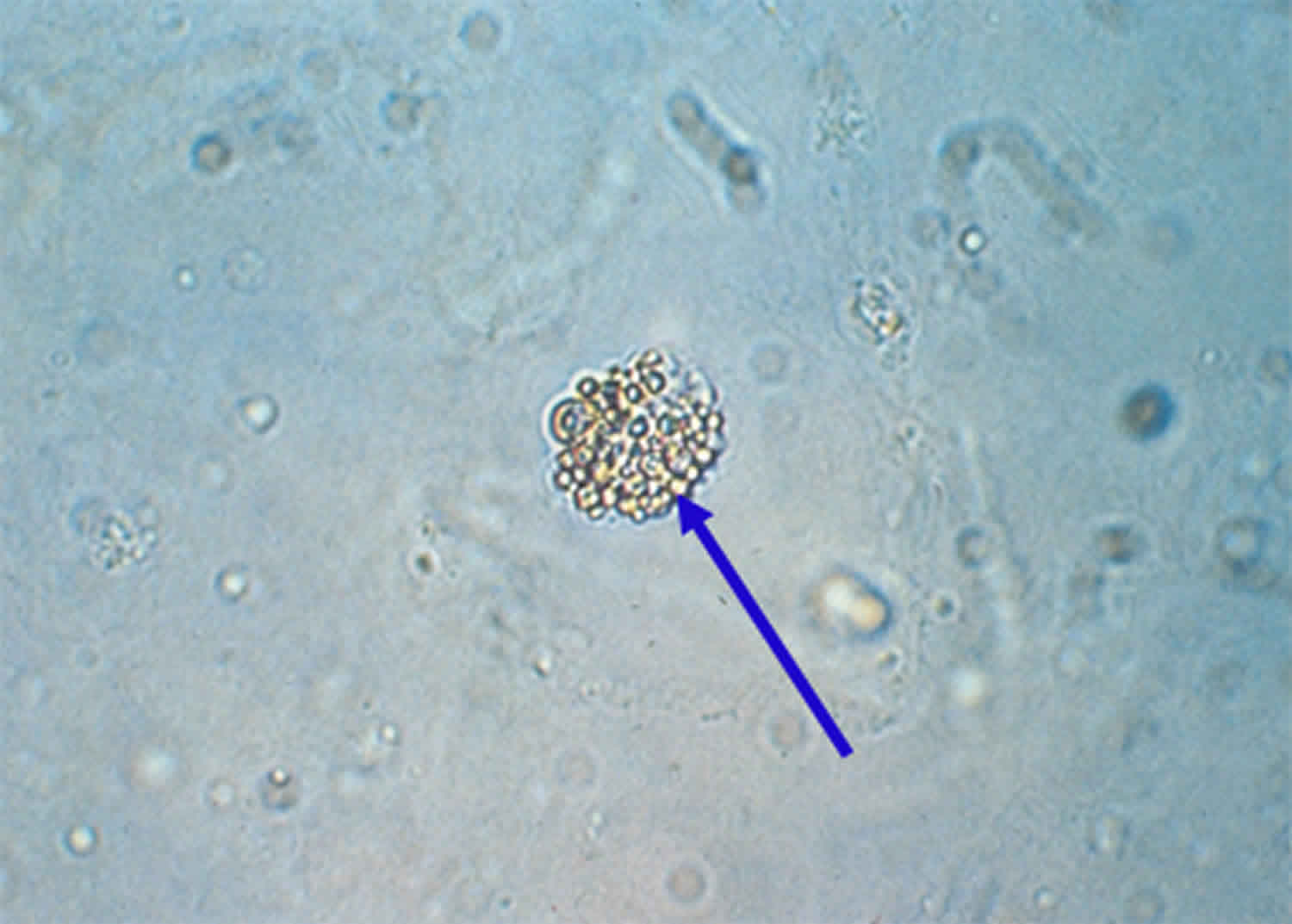
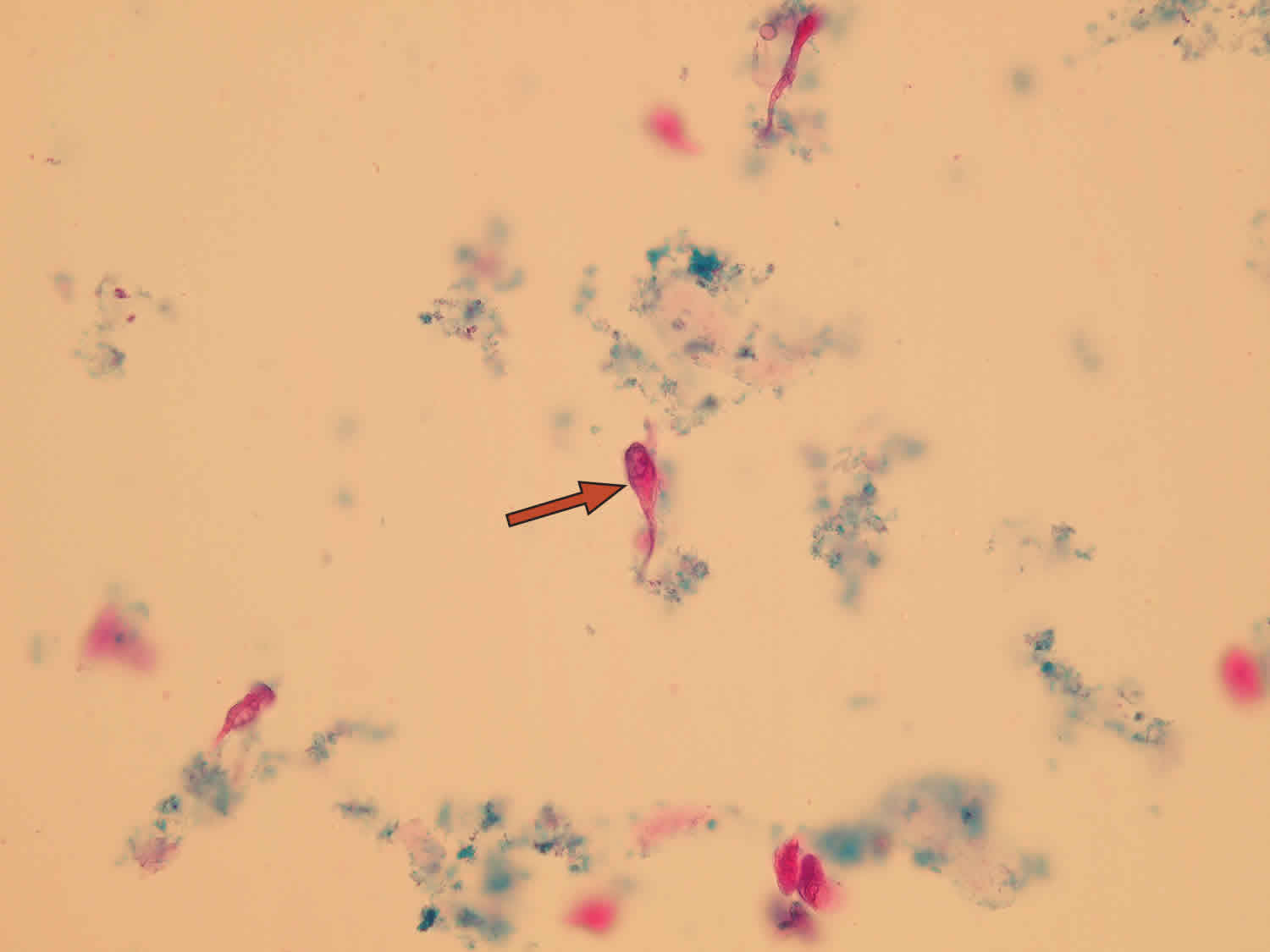
Papanicolaou stain is useful in distinguishing renal tubular epithelial cells from other mononuclear cells in urine. Increased numbers of proximal and distal convoluted renal tubular epithelial cells are seen in cases of acute tubular necrosis and certain drug or heavy metal intoxication. Oval fat bodies are renal tubular epithelial cells that have absorbed lipids in the urinary filtrate. Their identity can be confirmed using polarized microscopy and lipid stains. An oval fat body is indicated by the arrow in the lower image.
Renal epithelial fragments constitute of several renal cells of collecting duct origin. Their presence in urine is considered to be clinically severe and indicates heavy renal tubular damage.
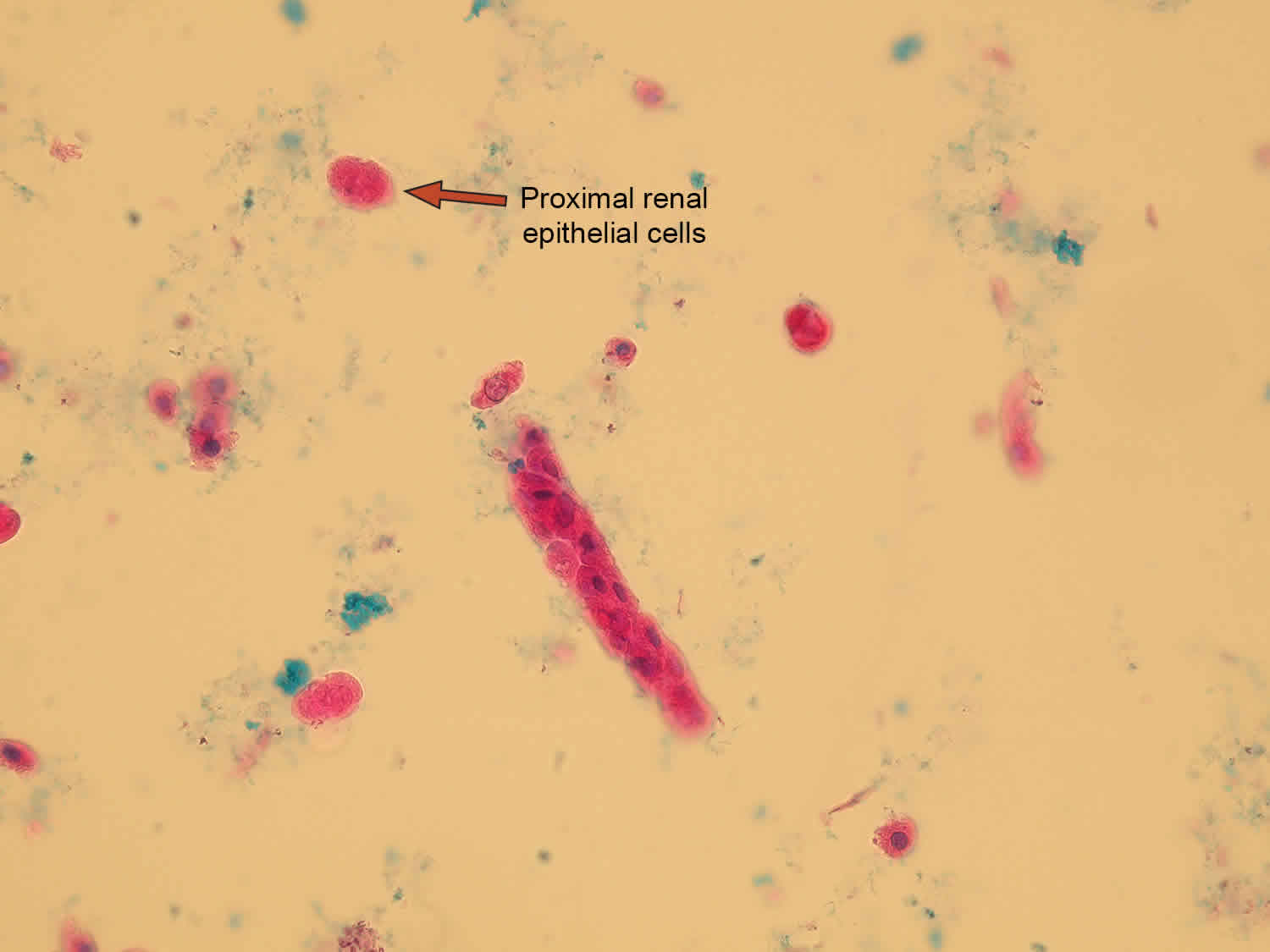
Figure 2. Renal tubular epithelial cells
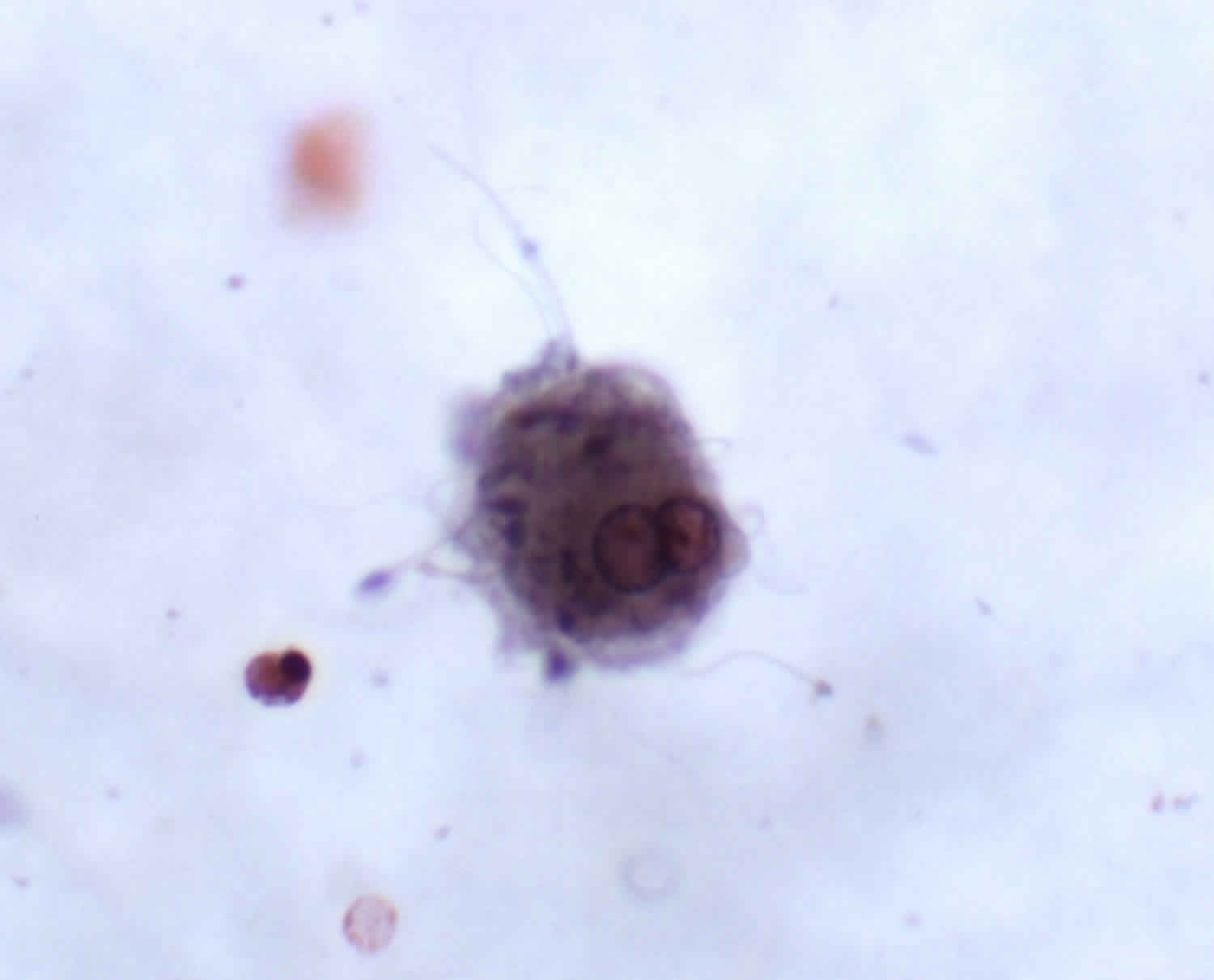
Seminal vesicle cells
Seminal vesicle cells may occasionally be seen in urine. The cytoplasm may have a golden-brown pigment. Nuclei tend to be hyperchromatic with degenerative chromatin.
- Seminal vesicle cells are sporadically seen in urine specimens of older patients
- Bizarre appearance with greatly enlarged nuclei and foamy fragmented cytoplasm
- Golden-brown lipofuscin pigment
- Spermatozoa accompany cells
- Abnormal DNA ploidy
- Eosinophilic inclusion bodies – giant lysosomes
- Hyaline inclusion bodies
Figure 3. Seminal vesicle cells seen in urine (note the associated spermatozoa)
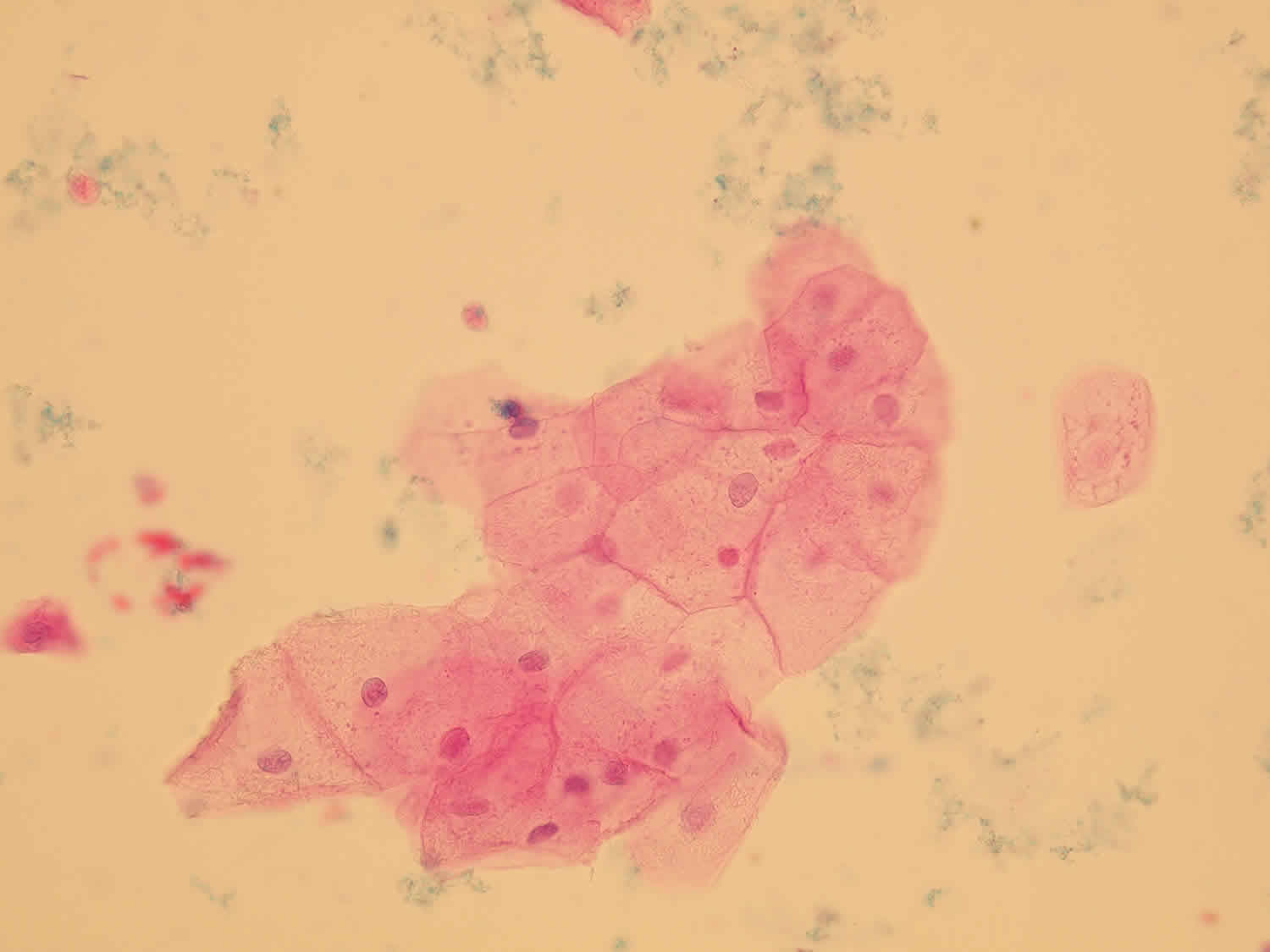
What is squamous epithelial cells in urine
Squamous epithelial cells are very large unevenly shaped cells with easily visible nucleus inside. Squamous epithelial cells originate from urethra or vagina. Squamous epithelial cells are very common elements with minimal clinical significance.
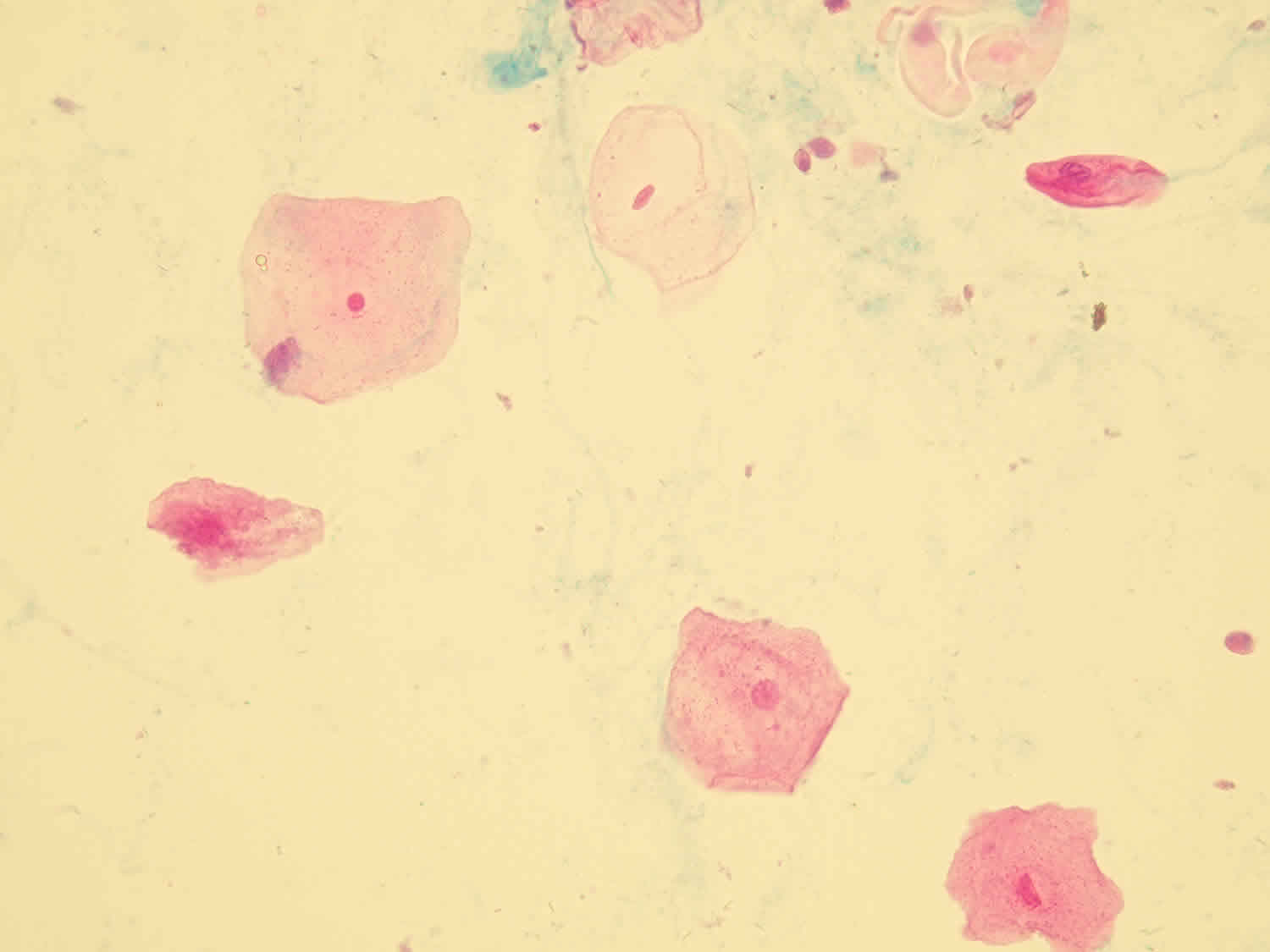
Figure 4. Squamous epithelial cells in urine (stained sediment)
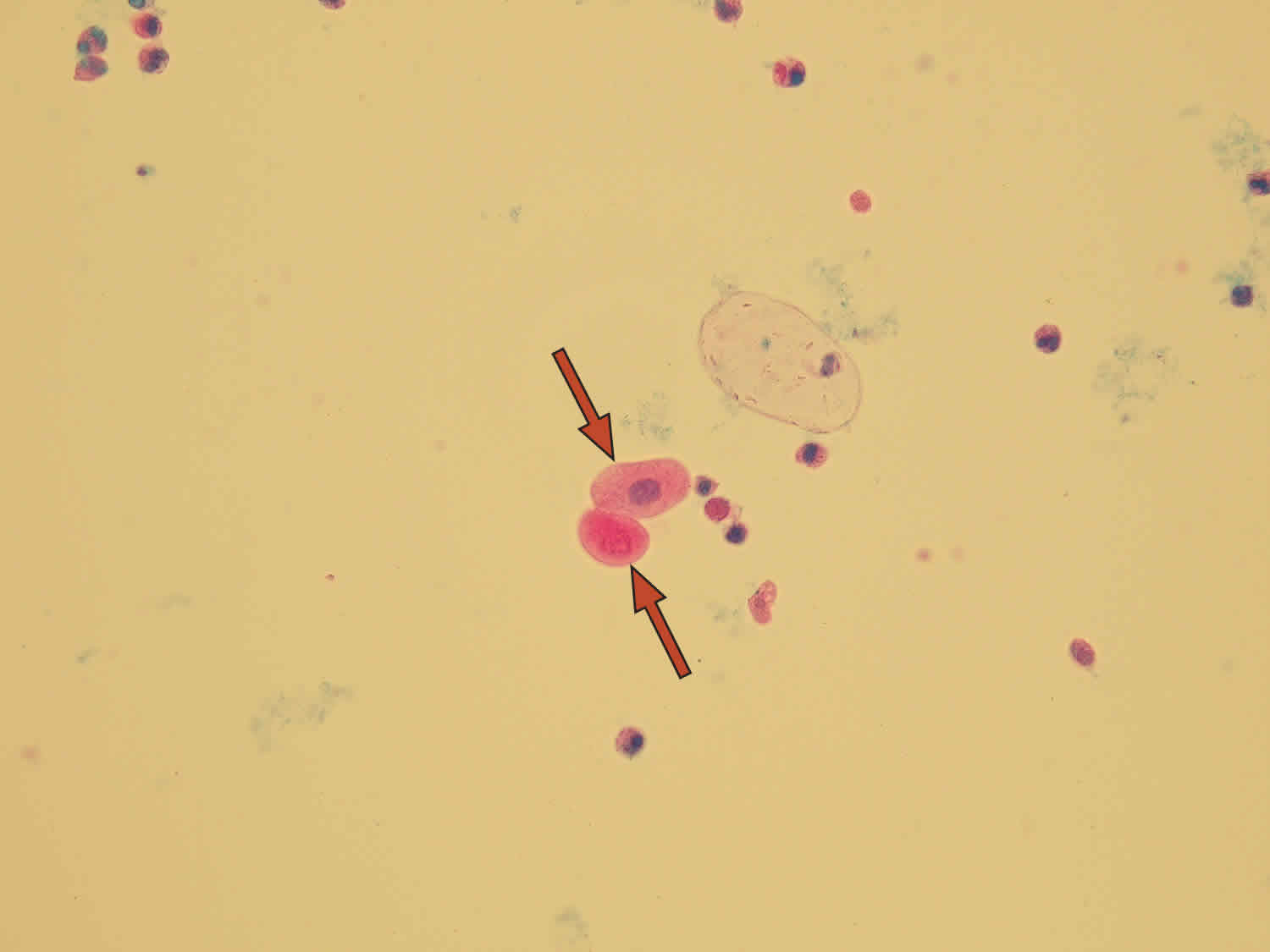
What are transitional epithelial cells in urine
Transitional epithelial cells have different shapes and sizes depending on their origin. Round transitional epithelial cells are most common. Their nucleus is in the middle of the cell, they are smaller than squamous epithelial cells and they come from the bladder or proximal segments of urethra in men. If they originate from deeper layers of epithelium or near the renal pelvis, they are smaller and more round.
Limited amount of round transitional epithelial cells may be normal, large amount accounts to urinary tract infection (UTI).
Another subcategory is called caudate cells. They come from deep layers of a bladder. The cells with two nuclei are also categorized as transitional epithelial cells. Large number of cells with two nuclei or asymmetric cells can be found in urine from patients with transitional cell (urothelial) carcinomas (bladder cancer).
Figure 5. Transitional epithelial cells in urine
Figure 6. Transitional epithelial caudate cells
- Sullivan PS, Chan JB, Levin MR, Rao J. Urine cytology and adjunct markers for detection and surveillance of bladder cancer. Am J Transl Res. 2010;2(4):412-40. Published 2010 Jul 25. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2923865/[↩][↩]
- Badalament RA, Kimmel M, Gay H, Cibas ES, Whitmore WF, Jr, Herr HW, Fair WR, Melamed MR. The sensitivity of flow cytometry compared with conventional cytology in the detection of superficial bladder carcinoma. Cancer. 1987;59:2078–2085[↩]
- Brown FM. Urine cytology. It is still the gold standard for screening? Urol Clin North Am. 2000;27:25–37[↩]
- Koss LG, Deitch D, Ramanathan R, Sherman AB. Diagnostic value of cytology of voided urine. Acta Cytol. 1985;29:810–816.[↩]