Contents
What is fibrinogen
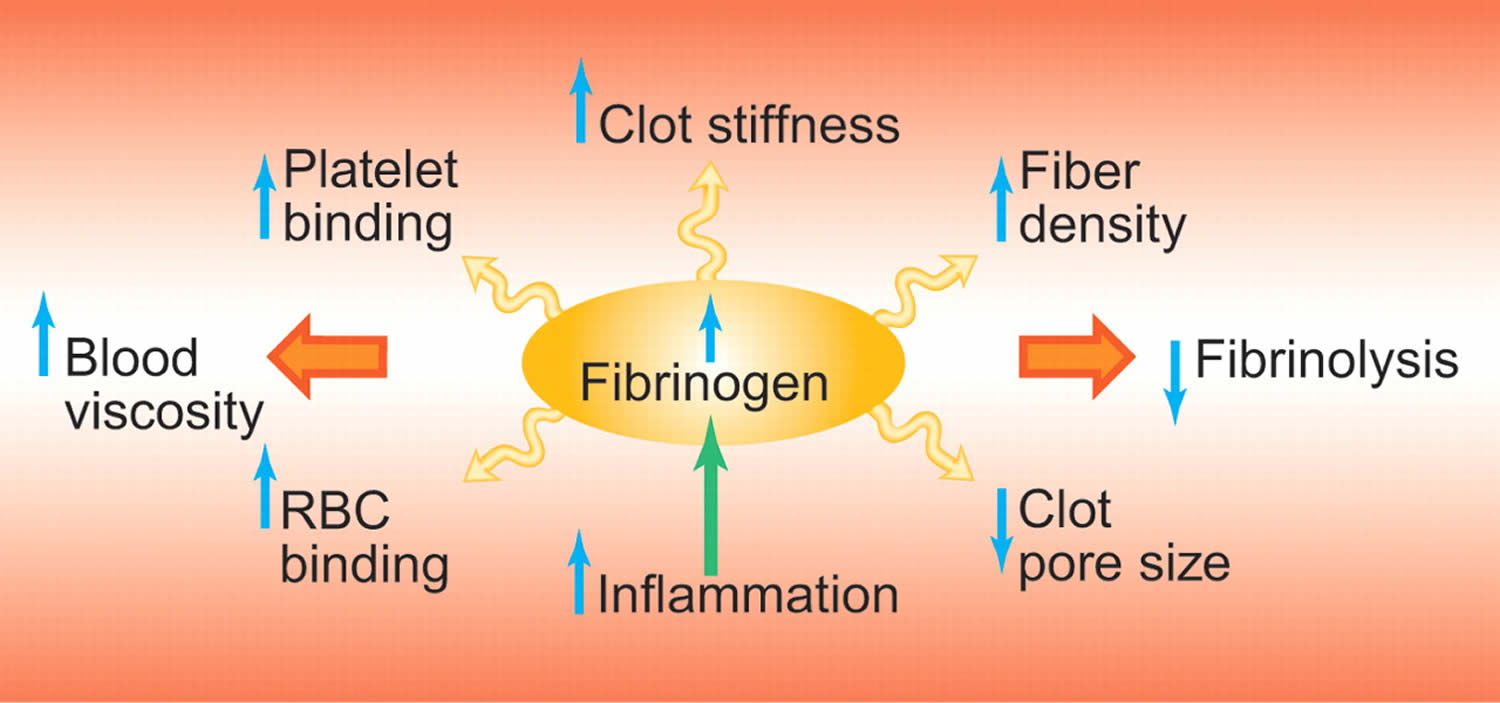
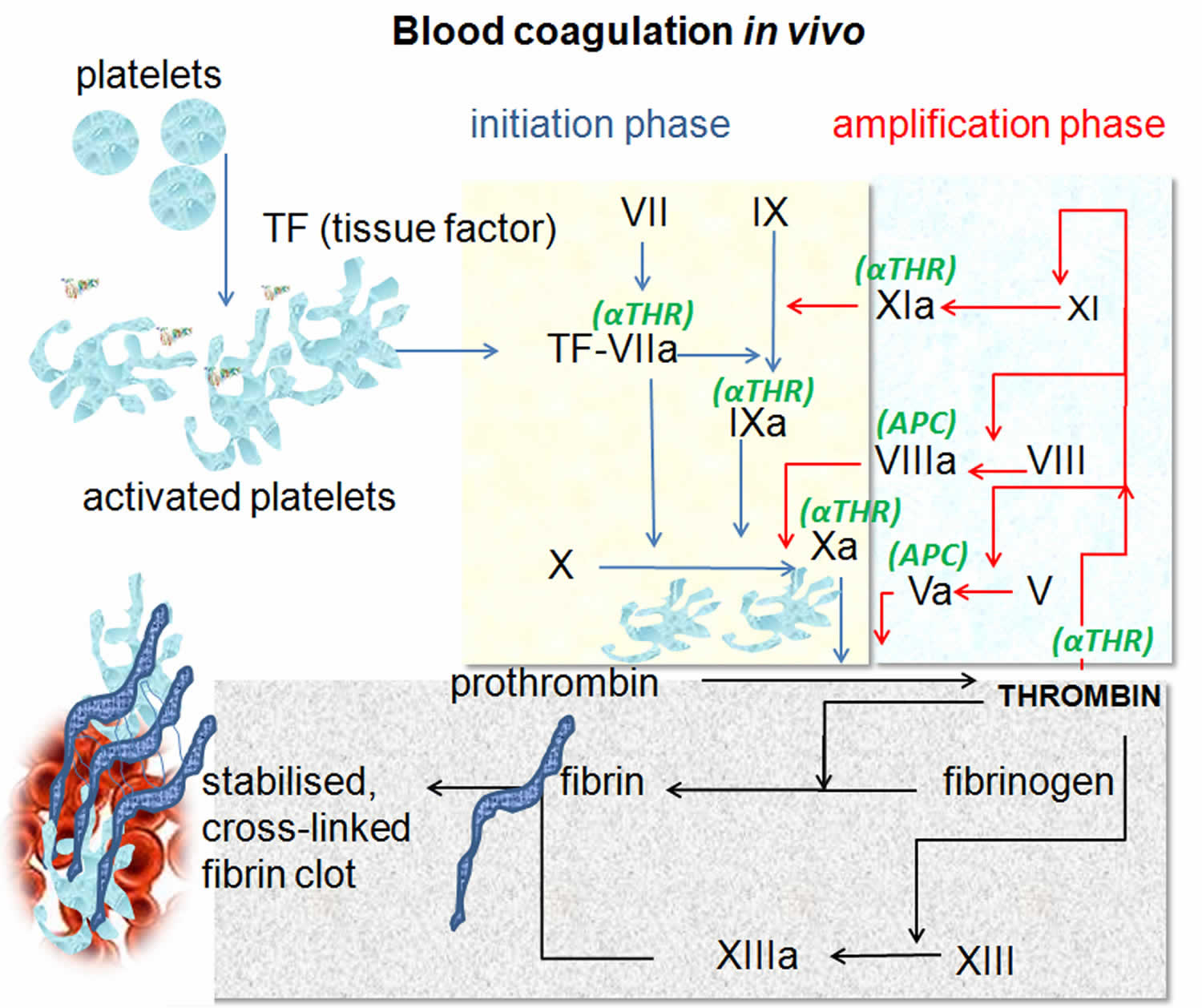
Fibrinogen is a protein, a coagulation factor (clotting factor 1) that occurs naturally in your body and is essential for blood clot formation. Fibrinogen is produced by your liver and released into circulation along with several other coagulation factor proteins. Fibrinogen has a biological half-life of 3 to 5 days in the circulating plasma. Normally, when a body tissue or blood vessel wall is injured, a process called hemostasis begins to help stop the bleeding by forming a plug at the injury site. Small cell fragments called platelets adhere to and aggregate at the site, a coagulation cascade begins, and clotting factors are activated one after the other.
As the cascade nears completion, thrombin converts soluble fibrinogen into insoluble fibrin strands that crosslink and form a clot. These strands crosslink together to form a fibrin net that stabilizes at the injury site. The fibrin net adheres to the site of injury along with the platelets to form a stable blood clot. This barrier prevents additional blood loss and remains in place until the injured area has healed.
Figure 1. Blood coagulation process
For a stable clot to form there must be enough normally functioning platelets and coagulation factors. If there are dysfunctional coagulation factors or platelets, or too little or too much of them, it can lead to bleeding episodes and/or to formation of an in appropriate blood clot (thrombosis). Several laboratory tests, including fibrinogen tests, can be used to evaluate hemostasis.
- Normal fibrinogen level 196-441 mg/dL
Fibrinogen is an acute phase reactant. Blood levels of fibrinogen along with other acute phase reactants rise sharply with conditions causing acute tissue inflammation or damage, nephrotic syndrome, liver disease, pregnancy, estrogen therapy, and/or compensated intravascular coagulation. Tests for these acute phase reactants, including fibrinogen, may be performed to determine the extent of inflammation in the body.
Fibrinogen deficiencies can be congenital or acquired and lead to prolonged coagulation times. Isolated fibrinogen deficiency is an extremely rare inherited coagulation disorder. An isolated deficiency of fibrinogen may be inherited as an autosomal recessive trait (afibrinogenemia or hypofibrinogenemia) and is one of the rarest of the inherited coagulation factor deficiencies.
Acquired fibrinogen deficiency is most commonly caused by, acute or decompensated intravascular coagulation and fibrinolysis (disseminated intravascular coagulation or DIC). Other causes of fibrinogen deficiency include advanced liver disease, L-asparaginase therapy, or fibrinolytic agents (e.g, streptokinase, urokinase, tissue plasminogen activator).
Fibrinogen function abnormalities, dysfibrinogenemias, may be inherited (congenital) or acquired. Patients with dysfibrinogenemia are generally asymptomatic. However, the congenital dysfibrinogenemias are more likely than the acquired to be associated with bleeding or thrombotic disorders. While the dysfibrinogenemias are generally not associated with clinically significant hemostasis problems, they characteristically produce a prolonged thrombin time clotting test.
Acquired dysfibrinogenemias mainly occur in association with liver disease (eg, chronic hepatitis, hepatoma) or renal diseases (eg, chronic glomerulonephritis, hypernephroma) and usually are associated with elevated fibrinogen levels.
Fibrinogen is an acute phase reactant, so a number of acquired conditions can result in an increase in its plasma concentration:
- Acute or chronic inflammatory illnesses
- Nephrotic syndrome
- Liver disease and cirrhosis
- Pregnancy or estrogen therapy
- Compensated intravascular coagulation
- Diabetes
- Obesity
The finding of an increased level of fibrinogen in a patient with obscure symptoms suggests an organic rather than a functional condition. Chronically increased fibrinogen has been recognized as a risk factor for development of arterial thromboembolism.
Differentiation of congenital from acquired defects of fibrinogen requires clinical correlation and the results of standard clotting-based fibrinogen activity (Fibrinogen Plasma) testing.
Fibrinogen in pregnancy
Pregnancy is associated with a hypercoagulable state 1 and these changes occur in preparation for blood loss at the time of parturition. During pregnancy, there is an increase in procoagulant activity (characterized by increases in factors V, VII, VIII, IX, X, XII and XII, von Willebrand factor, fibrinogen), decreases in endogenous anticoagulant activity (characterized by increases in heparin cofactor II, a1 antitrypsin, protein S activity and activated protein C resistance), and depressed fibrinolytic activity 2. Of note, fibrinogen levels increase with advancing gestation and in the third-trimester are higher than those in non-pregnant women 3.
Coagulopathy can accompany a number of obstetric morbidities. Obstetrical disseminated intravascular coagulation (DIC) is an acute, severe complication linked to placental abruption, amniotic fluid embolism, and dead fetus syndrome 4. Although obstetrical disseminated intravascular coagulation (DIC) may secondarily result in obstetric hemorrhage, it has been less clear whether and to what degree the maternal coagulation profile is altered during the period of acute and ongoing blood loss, in the absence of pre-existing disseminated intravascular coagulation (DIC).
Recently, investigators have focused their attention on profiling changes in the maternal coagulation profile during the course of obstetric hemorrhage. Specifically, a low fibrinogen level has been identified an important predictor for severe postpartum hemorrhage 5. Charbit et al. 6 examined coagulation profiles among 128 patients with atonic postpartum hemorrhage (after administration of a second-line uterotonic) up to 24 hour after bleeding onset. The maternal fibrinogen level was independently associated with severe postpartum hemorrhage; for each 1g/L decrease in fibrinogen, there was a 2.6 fold increased odds of severe postpartum hemorrhage. A baseline fibrinogen level ≤2g/L taken at the time of bleeding onset had a positive predictive value of 100%. These findings signify that a low fibrinogen level during the early phase of postpartum bleeding can predict the later development of severe postpartum hemorrhage. Similar findings have been observed in other observational studies. In a secondary analysis of a population-wide study in France, Cortet et al. 7 observed that women who developed postpartum hemorrhage post-vaginal delivery who had fibrinogen levels <2g/L within 2 hour of postpartum hemorrhage diagnosis were independently associated with severe postpartum hemorrhage. In a retrospective study of 456 patients with severe postpartum hemorrhage, de Lloyd et al. 8 also found low fibrinogen levels were inversely correlated with post-delivery blood loss values. In another retrospective study examining 257 women with postpartum hemorrhage, low fibrinogen levels (<2 g/L) predicted the need for an advanced intervention (uterine artery embolization, intra-abdominal packing, vessel ligation or hysterectomy) 9. These data provide strong evidence of an association between low fibrinogen levels with severe postpartum hemorrhage. However, it is unclear whether this relationship is purely associative or causative. In a large, multicenter study of women with early postpartum hemorrhage, the effect of pre-emptive treatment with 2 g fibrinogen concentrate as a measure to reduce red blood cell transfusion compared with placebo 10. No between-group differences were observed in the rate of postpartum transfusion [fibrinogen group (20%) vs. placebo group (22%)], therefore fibrinogen concentrate given pre-emptively for patients with postpartum hemorrhage and normofibrinogenemia may not be advantageous. However, for women who develop severe postpartum hemorrhage, the use of purified virally inactivated fibrinogen concentrates may be as efficacious as cryoprecipitate in correcting hypofibrinongenemia and, if introduced into the treatment protocol for postpartum hemorrhage-related coagulopathy, may reduce the need for massive transfusion of red blood cells, plasma and platelets 11. Further studies of fibrinogen concentrate in the setting of postpartum hemorrhage are needed, and we await the results of another randomized trial using fibrinogen concentrate for the early treatment of postpartum hemorrhage 12.
How should I use fibrinogen?
Man-made fibrinogen is used to treat bleeding episodes in people with a congenital fibrinogen deficiency. Fibrinogen is made from human plasma (part of the blood) which may contain viruses and other infectious agents. Donated plasma is tested and treated to reduce the risk of it containing infectious agents, but there is still a small possibility it could transmit disease. Talk with your doctor about the risks and benefits of using fibrinogen.
You should not use fibrinogen if you are allergic to it, or if you have ever had a severe allergic reaction.
To make sure fibrinogen is safe for you, tell your doctor if you have:
- a history of stroke or blood clot.
It is not known whether fibrinogen will harm an unborn baby. Tell your doctor if you are pregnant or plan to become pregnant.
It is not known whether fibrinogen passes into breast milk or if it could harm a nursing baby. Tell your doctor if you are breast-feeding a baby.
Your doctor will perform blood tests to make sure you do not have conditions that would prevent you from safely using fibrinogen.
Follow all directions on your prescription label. Do not use fibrinogen in larger or smaller amounts or for longer than recommended.
Fibrinogen is injected into a vein through an IV. You may be shown how to use an IV at home. Do not give yourself fibrinogen if you do not understand how to use the injection and properly dispose of needles, IV tubing, and other items used.
Fibrinogen is a powder medicine that must be mixed with a liquid (diluent) before using it. If you are using the injections at home, be sure you understand how to properly mix and store the medicine.
Do not mix fibrinogen with any other medicines, or give other medicines through the same IV line.
Fibrinogen contains no preservative. Once you have pierced the rubber top of a vial with a needle, you must use that vial right away or throw it away.
Do not shake the medication bottle or you may ruin the fibrinogen. Prepare your dose only when you are ready to give an injection. The fibrinogen mixture should be clear or slightly colored. Do not use if fibrinogen has changed colors or has particles in it. Call your pharmacist for new medicine.
Mixed fibrinogen must be used within 24 hours if you keep it at room temperature.
Each single-use vial (bottle) of fibrinogen is for one use only. Throw away after one use, even if there is still some fibrinogen left in it after injecting your dose.
Use a disposable needle only once. Follow any state or local laws about throwing away used needles and syringes. Use a puncture-proof “sharps” disposal container (ask your pharmacist where to get one and how to throw it away). Keep this container out of the reach of children and pets.
Tell your doctor if you have any changes in weight. Fibrinogen doses are based on weight, and any changes may affect the dose.
You may need frequent medical tests to help your doctor determine how long to treat you with fibrinogen.
Store the unmixed fibrinogen powder in a refrigerator or in a dark cool place. Protect from light and do not allow it to freeze. Throw away any unused vial after the expiration date on the label has passed.
What happens if I miss a dose?
Use the missed dose as soon as you remember. Skip the missed dose if it is almost time for your next scheduled dose. Do not use extra medicine to make up the missed dose.
What are the possible side effects of fibrinogen?
Get emergency medical help if you have signs of an allergic reaction: hives, rash; tightness in your chest; wheezing, difficult breathing; feeling like you might pass out; swelling of your face, lips, tongue, or throat.
Stop using fibrinogen and call your doctor at once if you have:
- signs of a stroke –sudden numbness or weakness (especially on one side of the body), sudden severe headache, slurred speech, problems with vision or balance;
- signs of a blood clot in the lung –chest pain, sudden cough, wheezing, rapid breathing, coughing up blood;
- signs of a blood clot in your leg –pain, swelling, warmth, or redness in one or both legs; or
- heart attack symptoms –chest pain or pressure, pain spreading to your jaw or shoulder, nausea, sweating.
Common side effects may include:
- fever; or
- headache.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects.
What other drugs will affect fibrinogen?
Other drugs may interact with fibrinogen, including prescription and over-the-counter medicines, vitamins, and herbal products. Tell each of your health care providers about all medicines you use now and any medicine you start or stop using.
Fibrinogen test
Fibrinogen is a protein, a coagulation factor (factor I) that helps your blood to clot. Two types of tests are available to evaluate fibrinogen:
- Fibrinogen activity test evaluates how well fibrinogen functions in helping to form a blood clot. A fibrinogen activity test measures the time that it takes for a fibrin clot to form following the addition of a standard amount of thrombin to plasma. This test evaluates the function of fibrinogen, its ability to be converted into fibrin. The time that is required for a clot to form directly correlates with the amount of active fibrinogen that is present. Prolonged clot-formation times may be due to decreased concentrations of normal fibrinogen or due to dysfunctional fibrinogen.
- Fibrinogen antigen test measures the amount of fibrinogen in the blood. A fibrinogen antigen test uses a fibrinogen antibody to bind to fibrinogen in a blood sample. This test allows the quantity, but not activity, of fibrinogen to be measured.
- Normal fibrinogen level 196-441 mg/dL
- Fibrinogen antigen levels <100 mg/dL are associated with an increased risk of bleeding.
- Adequate fibrinogen antigen levels in a context of low fibrinogen activity suggests a dysfibrinogenemia.
- Cautions:
- In patients with dysfibrinogenemias, fibrinogen concentration is often low and may be further differentiated from hypofibrinogenemia by measuring the fibrinogen antigen concentration.
- The presence of heparin (>2 U/mL) may cause falsely low fibrinogen results.
It is now understood that coagulation tests are based on what happens artificially in the test setting (in test tube) and thus do not necessarily reflect what actually happens in the body (in vivo). Nevertheless, the tests can be used to evaluate specific components of the hemostasis system. The fibrinogen activity test evaluates that part of the hemostatic process in which soluble fibrinogen is converted into fibrin threads. With the addition of thrombin to the test sample, the fibrinogen test bypasses the rest of the coagulation factors and focuses on the function of fibrinogen.
- Fibrinogen activity test measures the function of fibrinogen and its ability to be converted into fibrin. It is used:
- As part of an investigation of a possible bleeding disorder or inappropriate blood clot formation (thrombotic episode)
- As a follow-up to an abnormal bleeding disorder test (prothrombin time [PT] or partial thromboplastin time [PTT]) and/or an episode of prolonged or unexplained bleeding
- Along with tests such as prothrombin time, partial thromboplastin time, platelet function tests, fibrin degradation products and D-dimer to help diagnose disseminated intravascular coagulation (DIC) or abnormal fibrinolysis
- Occasionally to help monitor the status of a progressive disease (such as liver disease) over time or, rarely, to monitor treatment of an acquired condition (such as DIC)
- Sometimes along with other cardiac risk markers such as C-reactive protein (CRP) to help determine a person’s overall risk of developing cardiovascular disease. This use of the test has not gained widespread acceptance though because there are no direct treatments for elevated levels. However, many health practitioners feel that fibrinogen activity measurements give them additional information that may lead them to be more aggressive in treating those risk factors that they can treat (such as unhealthy levels of cholesterol).
- Fibrinogen antigen test is occasionally ordered as a follow-up test to determine whether decreased fibrinogen activity is due to insufficient fibrinogen or dysfunctional fibrinogen (caused by inherited or acquired dysfibrinogenemia).
Blood transfusions within the past month may affect fibrinogen test results.
Certain drugs may cause decreased levels, including anabolic steroids, phenobarbital, streptokinase, urokinase, L-asparaginase, tissue plasmogen activators, and valproic acid. Moderate elevations in fibrinogen are sometimes seen with pregnancy, cigarette smoking, and with oral contraceptives or estrogen use.
Dysfibrinogenemia is a rare coagulation disorder caused by mutations in the gene controlling the production of fibrinogen in the liver. It causes the liver to make an abnormal, dysfunctional fibrinogen, one that resists degradation when converted to fibrin or can not function normally in the coagulation cascade. Dysfibrinogenemia may increase a person’s risk of venous thrombosis or, rarely, cause a mild bleeding tendency. People with fibrinogen deficiency or dysfibrinogenemia may experience poor wound healing.
Genetic molecular testing is occasionally performed for those with inherited dysfibrinogenemia, hypofibrinogenemia, or afibrinogenemia to identify the genetic mutation responsible. Testing for this mutation may also be performed for other family members.
People with liver disease may develop acquired dysfibrinogenemia that could contribute to bleeding or thrombosis.
When is fibrinogen test ordered?
A health practitioner may order a fibrinogen activity test when someone:
- Has unexplained or prolonged bleeding
- Has a thrombosis
- Has an abnormal prothrombin time [PT] and partial thromboplastin time [PTT] test result
- Has symptoms of or is undergoing treatment for DIC or abnormal fibrinolysis
- May have an inherited or acquired coagulation factor (clotting protein) deficiency or dysfunction
- Has an acquired bleeding disorder and the person’s health practitioner wants to evaluate and monitor their clotting ability (over time)
A fibrinogen antigen test may be performed when someone has a low result on a fibrinogen activity test to help determine whether it is due to insufficient or dysfunctional fibrinogen.
High fibrinogen levels have also been associated with coronary heart disease, myocardial infarction, and peripheral arterial disease. In some cases, fibrinogen activity testing is performed along with other tests when a health practitioner wants to evaluate an individual’s risk of developing cardiovascular disease.
How is fibrinogen test used?
Fibrinogen blood testing is used to evaluate fibrinogen, a protein that is essential for blood clot formation. When there is an injury and bleeding occurs, the body forms a blood clot through a series of steps. In one of the last steps, soluble fibrinogen is converted into insoluble fibrin threads that crosslink together to form a net that stabilizes and adheres at the injury site until the area has healed.
- Fibrinogen may be decreased in acquired conditions such as liver disease and acute intravascular coagulation and fibrinolysis and disseminated intravascular coagulation (DIC).
- Fibrinogen may be decreased in rare conditions including congenital afibrinogenemia or hypofibrinogenemia.
- Fibrinogen may be elevated with acute or chronic inflammatory conditions.
What is the difference between tests for fibrinogen, d-dimer, and fibrin degradation products?
Fibrinogen activity testing evaluates the conversion of fibrinogen into fibrin; fibrinogen antigen testing measures the amount of soluble Factor I (dissolved in the blood) before it has been turned into insoluble fibrin and been crosslinked into a fibrin net. D-dimer and fibrin degradation product testing both help evaluate the status of the fibrinolytic system, the body’s ability to break blood clots apart when they are no longer needed so that they can be removed. Fibrin degradation product is a measurement of all of the fragments of the dissolving clot, while D-dimer is a more specific measurement for one of the crosslinked, break-down fragments.
What does fibrinogen test result mean?
Fibrinogen test results are reported as the concentration of the protein in the blood. Fibrinogen activity tests are converted into concentrations for comparison with fibrinogen antigen results.
- Normal fibrinogen activity results usually reflect normal blood clotting ability.
- Significantly decreased fibrinogen activity may be due to decreased or dysfunctional fibrinogen. Reduced fibrinogen activity and antigen levels may impair the body’s ability to form a stable blood clot.
- Chronically low fibrinogen levels may be related to decreased production due to an inherited condition such as afibrinogenemia or hypofibrinogenemia or to an acquired condition such as end-stage liver disease or severe malnutrition.
- Acutely low fibrinogen levels are often related to consumption of fibrinogen such as may be seen with disseminated intravascular coagulation (DIC) and abnormal fibrinolysis, which occurs when the body is overactive in clearing blood clots. Reduced fibrinogen levels may also occur following rapid, large-volume blood transfusions and in people who are malnourished.
Sometimes a health practitioner will use a ratio of the antigen test and the activity test. This is to help to distinguish dysfibrinogenemia (high ratio) from hypofibrinogenemia (ratio close to 1).
Can I have decreased or abnormal fibrinogen and not know it?
Yes. Many people have relatively normal clotting even when fibrinogen concentrations and/or activity are low. Your condition may not be identified unless you bleed longer than expected after a surgical procedure or trauma or have coagulation-related testing performed for another reason, such as part of a pre-surgical screen.
High fibrinogen
Fibrinogen is an acute phase reactant, meaning that fibrinogen concentrations may rise sharply in any condition that causes inflammation or tissue damage. Elevated concentrations of fibrinogen are not specific; that is, they do not tell the health practitioner the cause or location of the disturbance. Usually these elevations in the fibrinogen level are temporary, returning to normal after the underlying condition has been resolved.
Elevated fibrinogen levels may be seen with:
- Acute infections
- Cancer
- Coronary heart disease, myocardial infarction
- Stroke
- Inflammatory disorders (like rheumatoid arthritis and glomerulonephritis, a form of kidney disease)
- Trauma
- Cigarette smoking
- Pregnancy
- Peripheral artery disease
While fibrinogen levels are elevated, a person’s risk of developing a blood clot may be increased and, over time, they could contribute to an increased risk for developing cardiovascular disease.
What can I do to reduce my fibrinogen level?
If your fibrinogen concentration is elevated due to pregnancy or to an acute inflammatory process, it will likely return to normal by itself once the underlying condition has resolved. If it is due to an acquired condition such as rheumatoid arthritis, there may be very little you can do to affect the level. If your health care provider has told you that elevated fibrinogen levels are increasing your risk of cardiovascular disease, you can make lifestyle changes that will affect other cardiac risk factors, such as reducing your cholesterol and raising your HDL (high density lipoproptein also known as “good” cholesterol). There is also some evidence that diets rich in omega-3 and omega-6 fatty acids (fish oils) may help reduce fibrinogen levels.
- Butwick AJ, Goodnough LT. Transfusion and coagulation management in major obstetric hemorrhage. Current opinion in anaesthesiology. 2015;28(3):275-284. doi:10.1097/ACO.0000000000000180. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4567035/[↩]
- Holmes VA, Wallace JM. Haemostasis in normal pregnancy: a balancing act? Biochem Soc Trans. 2005;33:428–432.[↩]
- Huissoud C, Carrabin N, Benchaib M, et al. Coagulation assessment by rotation thrombelastometry in normal pregnancy. Thromb Haemost. 2009;101:755–761.[↩]
- Kobayashi T, Terao T, Maki M, Ikenoue T. Diagnosis and management of acute obstetrical DIC. Semin Thromb Hemost. 2001;27:161–167.[↩]
- Butwick AJ. Postpartum hemorrhage and low fibrinogen levels: the past, present and future. Int J Obstet Anesth. 2013;22:87–91 https://www.obstetanesthesia.com/article/S0959-289X(13)00007-1/fulltext[↩]
- Charbit B, Mandelbrot L, Samain E, et al. The decrease of fibrinogen is an early predictor of the severity of postpartum hemorrhage. J Thromb Haemost. 2007;5:266–273.[↩]
- Cortet M, Deneux-Tharaux C, Dupont C, et al. Association between fibrinogen level and severity of postpartum haemorrhage: secondary analysis of a prospective trial. Br J Anaesth. 2012;108:984–989.[↩]
- de Lloyd L, Bovington R, Kaye A, et al. Standard haemostatic tests following major obstetric haemorrhage. Int J Obstet Anesth. 2011;20:135–141.[↩]
- Gayat E, Resche-Rigon M, Morel O, et al. Predictive factors of advanced interventional procedures in a multicentre severe postpartum haemorrhage study. Intensive Care Med. 2011;37:1816–1825.[↩]
- Wikkelso AJ, Edwards HM, Afshari A, et al. Pre-emptive treatment with fibrinogen concentrate for postpartum haemorrhage: randomized controlled trial. Br J Anaesth. 2015[↩]
- Mallaiah S, Barclay P, Harrod I, et al. Introduction of an algorithm for ROTEM-guided fibrinogen concentrate administration in major obstetric haemorrhage. Anaesthesia. 2015;70:166–175.[↩]
- Collins P. Fibrinogen concentrate versus placebo for treatment of postpartum haemorrhage: a multicentre, prospective, double blind randomised controlled trial.[↩]