Contents
What is HbA1c
HbA1c is short for hemoglobin A1c, which is also called A1c or glycated hemoglobin. HbA1c is hemoglobin with glucose attached. HbA1c develops when hemoglobin, a protein within red blood cells that carries oxygen throughout your body, joins with glucose in the blood, becoming ‘glycated’. The HbA1c test evaluates the average amount of glucose in your blood over the last 2 to 3 months by measuring the percentage of glycated (glycosylated) hemoglobin. HbA1c is also a surrogate measure for a person’s risk of developing diabetes-related complications. However, despite the tremendous value of the HbA1c to clinical management, there are limitations to what the HbA1c can tell patients and physicians about their diabetes. The HbA1c measurement does not capture short-term variations in blood glucose, exposure to hypoglycemia and hyperglycemia, or the impact of blood glucose variations on individuals’ quality of life.
Hemoglobin is an oxygen-transporting protein found inside red blood cells. There are several types of normal hemoglobin, but the predominant form – about 95-98% – is hemoglobin A. As glucose circulates in the blood, some of it spontaneously binds to hemoglobin A.
The higher the level of glucose in the blood, the more glycated hemoglobin (HbA1c) is formed. Once the glucose binds to the hemoglobin, it remains there for the life of the red blood cell – normally about 120 days. The predominant form of glycated hemoglobin is referred to as HbA1c. HbA1c is produced on a daily basis and slowly cleared from the blood as older red blood cells die and younger red blood cells (with non-glycated hemoglobin) take their place.
By measuring glycated hemoglobin (HbA1c), clinicians are able to get an overall picture of what your average blood sugar levels have been over a period of weeks/months (2 to 3 months).
For people with diabetes this is important as the higher the HbA1c, the greater the risk of developing diabetes-related complications.
When your body processes sugar, glucose in the bloodstream naturally attaches to hemoglobin.
The amount of glucose that combines with this protein is directly proportional to the total amount of sugar that is in your system at that time.
Because red blood cells in the human body survive for 8-12 weeks (120 days) before renewal, measuring HbA1c (glycated hemoglobin) can be used to reflect average blood glucose levels over that duration, providing a useful longer-term gauge of blood glucose control.
HbA1c test for diabetes diagnosis
An HbA1c test does not directly measure the level of blood glucose, however, the result of the test is influenced by how high or low your blood glucose levels have tended to be over a period of 2 to 3 months.
Indications of diabetes or prediabetes are given under the following conditions:
- Normal: HbA1c 6.0% (below 42 mmol/mol )
- Prediabetes: HbA1c 6.0 to 6.4% (42 to 47 mmol/mol)
- Diabetes: HbA1c 6.5% or over (48 mmol/mol)
If your blood sugar levels have been high in recent weeks, your HbA1c will also be greater.
HbA1c can indicate people with prediabetes or diabetes as follows:
Table 1. HbA1c levels
| HbA1c | mmol/mol | % |
|---|---|---|
| Normal | Below 42 mmol/mol | Below 6.0% |
| Prediabetes | 42 to 47 mmol/mol | 6.0% to 6.4% |
| Diabetes | 48 mmol/mol or over | 6.5% or over |
In screening and diagnosis, some HbA1c results that may be seen include:
- A nondiabetic person will have an HbA1c result less than 5.7% (39 mmol/mol).
- Diabetes: HbA1c level is 6.5% (48 mmol/mol) or higher.
- Increased risk of developing diabetes in the future: HbA1c of 5.7% to 6.4% (39-46 mmol/mol).
The HbA1c test report also may include the result expressed in SI units (mmol/mol) and an estimated Average Glucose (eAG), which is a calculated result based on the hemoglobin HbA1c levels.
The purpose of reporting estimated Average Glucose (eAG) is to help a person relate HbA1c results to everyday glucose monitoring levels and to laboratory glucose tests. The formula for estimated Average Glucose (eAG) converts percentage HbA1c to units of mg/dL or mmol/L.
It should be noted that the estimated Average Glucose (eAG) is still an evaluation of a person’s glucose over the last couple of months. It will not match up exactly to any one daily glucose test result.
- The American Diabetes Association has adopted this calculation and provides a calculator and information on the estimated Average Glucose (eAG) on their DiabetesPro web site (https://professional.diabetes.org/diapro/glucose_calc).
- The NGSP (National Glycohemoglobin Standardization Program) web site also provides a calculator to convert hemoglobin HbA1c in SI units mmol/mol into percentage (http://www.ngsp.org/convert1.asp).
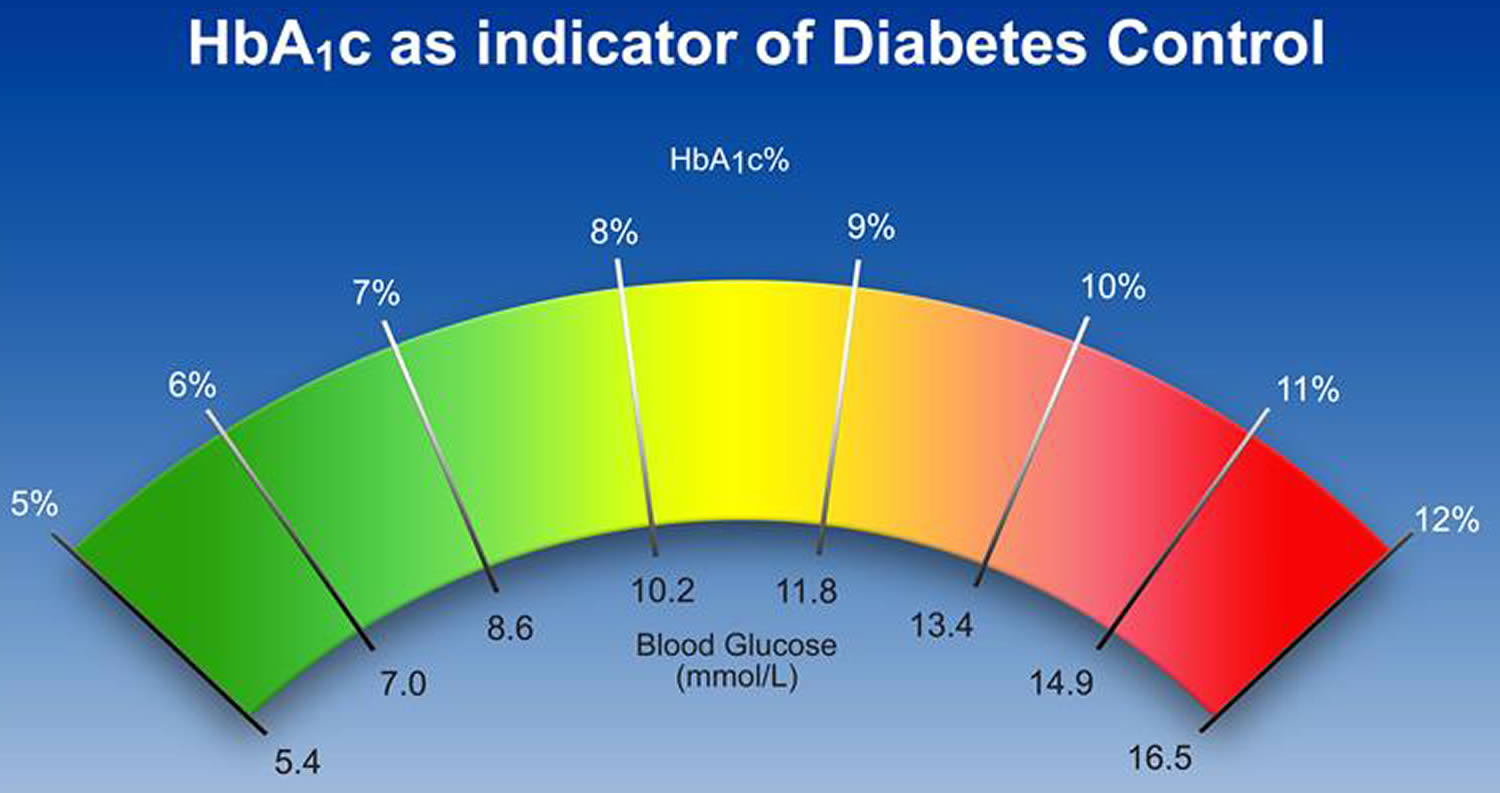
Figure 1. HbA1c chart
Table 2. Convert HbA1c between National Glycohemoglobin Standardization Program (NGSP), International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) and estimated Average Glucose (eAG)
NGSP HbA1c | IFCC HbA1c (mmol/mol) | eAG |
5.0 | 31 | 97 |
6.0 | 42 | 126 |
7.0 | 53 | 154 |
8.0 | 64 | 183 |
9.0 | 75 | 212 |
10.0 | 86 | 240 |
11.0 | 97 | 269 |
12.0 | 108 | 298 |
Table 3. Convert HbA1c and estimated Average Glucose (eAG) is described by the formula 28.7 x HbA1c – 46.7 = eAG (milligrams/deciliter, mg/dL)
| HbA1c | estimated Average Glucose (eAG) | |
| % | mg/dl | mmol/l |
| 6 | 126 | 7.0 |
| 6.5 | 140 | 7.8 |
| 7 | 154 | 8.6 |
| 7.5 | 169 | 9.4 |
| 8 | 183 | 10.1 |
| 8.5 | 197 | 10.9 |
| 9 | 212 | 11.8 |
| 9.5 | 226 | 12.6 |
| 10 | 240 | 13.4 |
Table 4. Recommended target Blood Glucose Level ranges
| Target Levels by Type | Upon waking | Before meals (pre prandial) | At least 90 minutes after meals (post prandial) |
|---|---|---|---|
| Non-diabetic* | 4.0 to 5.9 mmol/L | under 7.8 mmol/L | |
| Type 2 diabetes | 4 to 7 mmol/L | under 8.5 mmol/L | |
| Type 1 diabetes | 5 to 7 mmol/L | 4 to 7 mmol/L | 5 to 9 mmol/L |
| Children w/ type 1 diabetes | 4 to 7 mmol/L | 4 to 7 mmol/L | 5 to 9 mmol/L |
Normal and diabetic blood sugar ranges
For the majority of healthy individuals, normal blood sugar levels are as follows:
- Between 4.0 to 5.4 mmol/L (72 to 99 mg/dL) when fasting
- Up to 7.8 mmol/L (140 mg/dL) 2 hours after eating
For people with diabetes, blood sugar level targets are as follows:
- Before meals: 4 to 7 mmol/L for people with type 1 or type 2 diabetes
- After meals: under 9 mmol/L for people with type 1 diabetes and under 8.5mmol/L for people with type 2 diabetes
How does HbA1c differ from a blood glucose level?
HbA1c provides a longer-term trend, similar to an average, of how high your blood sugar levels have been over a period of 2 to 3 months.
An HbA1c reading can be taken from blood from a finger but is often taken from a blood sample that is taken from your arm.
Blood glucose level is the concentration of glucose in your blood at a single point in time, i.e. the very moment of the test.
This is measured using a fasting plasma glucose test, which can be carried out using blood taken from a finger or can be taken from a blood sample from the arm.
However, fasting glucose tests provide an indication of your current glucose levels only, whereas the HbA1c test serves as an overall marker of what your average levels are over a period of 2-3 months.
HbA1c can be expressed as a percentage (Diabetes Control and Complications Trial (DCCT) unit) or as a value in mmol/mol (International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) unit). Since 2009, mmol/mol has been the default unit to use in the US.
- Note that the HbA1c value, which is measured in mmol/mol, should not be confused with a blood glucose level which is measured in mmol/l.
- Use the Diabetes UK HbA1c conversion tool to help you with switching between the two measurement units (https://www.diabetes.co.uk/hba1c-units-converter.html).
How do blood glucose levels compare with HbA1c readings?
The table 5 below shows how average blood sugar levels in mmol/L would be translated into HbA1c readings, and vice versa.
- Use the Diabetes UK HbA1c conversion tool to help you with switching between the two measurement units (https://www.diabetes.co.uk/hba1c-units-converter.html).
It is important to note that because blood glucose levels fluctuate constantly, literally on a minute by minute basis, regular blood glucose testing is required to understand how your levels are changing through the day and learning how different meals affect your glucose levels.
Table 5. HbA1c and Blood Glucose Levels
| HbA1c (%) | HbA1c (mmol/mol) | Ave. Blood Glucose (mmol/L) |
|---|---|---|
| 13 | 119 | 18 mmol/L |
| 12 | 108 | 17 mmol/L |
| 11 | 97 | 15 mmol/L |
| 10 | 86 | 13 mmol/L |
| 9 | 75 | 12 mmol/L |
| 8 | 64 | 10 mmol/L |
| 7 | 53 | 8 mmol/L |
| 6 | 42 | 7 mmol/L |
| 5 | 31 | 5 mmol/L |
HbA1c diabetes
The American Diabetes Association recommends to begin HbA1c testing at age 45 for overweight or obese people; if the result is normal, the testing should be repeated at a minimum of 3-year intervals, with consideration of more frequent testing depending on initial results and risk status.
People who are not diagnosed with diabetes but are determined to be at increased risk for diabetes (prediabetes) should have HbA1c testing yearly.
- HbA1c targets or people with diabetes to aim for is 6.5% (48 mmol/mol)
Depending on the type of diabetes that a person has, how well that person’s diabetes is controlled, and on the healthcare provider’s recommendations, the HbA1c test may be measured 2 to 4 times each year. The American Diabetes Association recommends HbA1c testing for diabetics at least twice a year if they are meeting treatment goals and under stable glycemic control. When someone is first diagnosed with diabetes or if control is not good, HbA1c may be ordered quarterly.
Although HbA1c level alone does not predict diabetes complications, good control is known to lower the risk of complications.
How is estimated Average Glucose (eAG) calculated?
The ADAG (A1c-Derived Average Glucose) formula that is used to calculate the estimated Average Glucose (eAG) from your hemoglobin A1c (HbA1c) result is:
- eAG (milligrams/deciliter, mg/dL) = 28.7 x HbA1c (%) – 46.7
An example of this is an HbA1c of 6%. The calculation for this would be:
- 28.7 X 6 – 46.7 = 126 mg/dL estimated Average Glucose (eAG)
for an estimated average glucose of 126 mg/dL.
What this means is that for every one percent that your HbA1c goes up, it is equivalent to your average glucose going up by about 29 mg/dL.
Is HbA1c reported the same way around the world?
For monitoring purposes, the way that the HbA1c is reported is in the process of changing. Traditionally, in the United States, the HbA1c has been reported as a percentage, and the American Diabetes Association has recommended that people with diabetes strive to keep their HbA1c below 7%. While this is still generally true, more than a decade of national and international efforts to improve and standardize the HbA1c test and its reporting led to the release of a consensus statement in 2007 (and an update in 2010) by the American Diabetes Association, the European Association for the Study of Diabetes, the International Federation of Clinical Chemistry and Laboratory Medicine (IFCC), the International Society for Pediatric and Adolescent Diabetes, and the International Diabetes Federation. These joint statements and the completion of a study called ADAG (HbA1c-Derived Average Glucose) that further examined the relationship between blood glucose concentrations and HbA1c led to a recommendation that HbA1c be reported worldwide in two ways:
- As a percentage (based upon National Glycohemoglobin Standardization Program (NGSP) derived units) and
- In SI (Système International) units (mmol/mol)
An estimated Average Glucose (eAG) based upon a formula developed from the ADAG (HbA1c-Derived Average Glucose) study with either mg/dL or mmol/l as units that continue to be recognized by the American Diabetes Association and the American Association for Clinical Chemistry in the 2015 American Diabetes Association Diabetes Care Position Statement may also be reported.
What this means for diabetics and health practitioners in the U.S. is that HbA1c results will be reported as a percentage but may in addition to this be reported as mmol/mol and, in some cases, also as an estimated Average Glucose (eAG) with the same type of units (mg/dL) as are reported by home glucose monitors and laboratory results.
Why are my HbA1c and blood glucose different?
Beyond the difference in units used to report them, the HbA1c represents an average over time while your blood glucose reflects what is happening in your body now. Your blood glucose will capture the changes in your blood sugar that occur on a daily basis, the highs and the lows. Each blood glucose is a snapshot and each is different. The HbA1c is an indication that “in general” your glucose has been elevated over the last few months or “in general” it has been normal. It is inherently not as sensitive as a blood glucose. However, if your day-to-day glucose control is stable (good or bad), then both the HbA1c and blood glucose should reflect this. It is important to remember the time lag associated with the HbA1c. Good glucose control for the past 2-3 weeks will not significantly affect the HbA1c result for several more weeks.
In addition to this, it is also important to remember that glycated hemoglobin and blood glucose are two different but related things. For unknown reasons, some peoples’ HbA1c may not accurately reflect their average blood glucose.
Is there a home test for HbA1c?
Yes. If you have already been diagnosed with diabetes, a home test may be used to help monitor your glucose control over time. However, a home test (point-of-care test) is not recommended for screening or diagnosing the disease. There are FDA-approved tests that can be used at home.
What are the benefits of lowering HbA1c?
Two large-scale studies – the UK Prospective Diabetes Study (UKPDS) and the Diabetes Control and Complications Trial (DCCT) – demonstrated that improving HbA1c by 1% (or 11 mmol/mol) for people with type 1 diabetes or type 2 diabetes cuts the risk of microvascular complications by 25%.
Microvascular complications include:
- Retinopathy
- Neuropathy
- Diabetic nephropathy (kidney disease)
Research has also shown that people with type 2 diabetes who reduce their HbA1c level by 1% are 1:
- 19% less likely to suffer cataracts
- 16% less likely to suffer heart failure
- 43% less likely to suffer amputation or death due to peripheral vascular disease
What is HbA1c test
HbA1c test may be used to screen for and diagnose diabetes or risk of developing diabetes. Standards of medical care in diabetes from the American Diabetes Association state that diabetes may be diagnosed based on HbA1c criteria or plasma glucose criteria, either the fasting plasma glucose (FPG) or the 2-hour plasma glucose value after a 75-g oral glucose tolerance test (OGTT).
HbA1c test is also used to monitor treatment for someone who has been diagnosed with diabetes. HbA1c test helps to evaluate how well the person’s glucose levels have been controlled by treatment over time. For monitoring purposes, an A1c of less than 7% indicates good glucose control and a lower risk of diabetic complications for the majority of diabetics.
However, the American Diabetes Association and the European Association for the Study of Diabetes recommend that the management of glucose control in type 2 diabetes be more “patient-centered.” Data from recent studies have shown that low blood sugar (hypoglycemia) can cause complications and that people with risk of severe hypoglycemia, disease duration, underlying health conditions, established vascular complications, and a limited life expectancy do not necessarily benefit from having a stringent goal of less than 7% for their HbA1c. It is recommend that people work closely with their healthcare provider to select a goal that reflects each person’s individual health status and that balances risks and benefits.
- The HbA1c test will not reflect temporary, acute blood glucose increases or decreases, or good control that has been achieved in the last 3-4 weeks. The glucose swings of someone who has “brittle” diabetes will also not be reflected in the HbA1c.
- If an individual has a hemoglobin variant, such as sickle cell hemoglobin (hemoglobin S), that person will have a decreased amount of hemoglobin A. This may limit the usefulness of the HbA1c test in diagnosing and/or monitoring this person’s diabetes, depending on the method used.
- If a person has anemia, hemolysis, or heavy bleeding, HbA1c test results may be falsely low. If someone is iron-deficient, the HbA1c level may be increased.
- If a person receives erythropoietin (EPO) therapy or has had a recent blood transfusion, the HbA1c may be inaccurate and may not accurately reflect glucose control for 2-3 months.
How is HbA1c test used?
Screening and diagnosis
The hemoglobin A1c test may be used to screen for and diagnose diabetes and prediabetes in adults.
The HbA1c test, however, should not be used for screening for cystic fibrosis-related diabetes, for diagnosis of gestational diabetes in pregnant women, or for diagnosis of diabetes in children and adolescence, people who have had recent severe bleeding or blood transfusions, those with chronic kidney or liver disease, or people with blood disorders such as iron-deficiency anemia, vitamin B12 deficiency anemia, and some hemoglobin variants (e.g., patients with sickle cell disease or thalassemia). In these cases, a fasting plasma glucose or oral glucose tolerance test should be used for screening or diagnosing diabetes.
Only HbA1c tests that have been referenced to an accepted laboratory method (National Glycohemoglobin Standardization Program certified) should be used for diagnostic or screening purposes. Currently, point-of-care tests, such as those that may be used at a doctor’s office or a patient’s bedside, are not accurate enough for use in diagnosis but can be used to monitor treatment (lifestyle and drug therapies).
Monitoring
The HbA1c test is also used to monitor the glucose control of diabetics over time. The goal of those with diabetes is to keep their blood glucose levels as close to normal as possible. This helps to minimize the complications caused by chronically elevated glucose levels, such as progressive damage to body organs like the kidneys, eyes, cardiovascular system, and nerves. The HbA1c test result gives a picture of the average amount of glucose in the blood over the last 2-3 months. This can help diabetics and their healthcare providers know if the measures that are being taken to control their diabetes are successful or need to be adjusted.
HbA1c is frequently used to help newly diagnosed diabetics determine how elevated their uncontrolled blood glucose levels have been over the last 2-3 months. The test may be ordered several times while control is being achieved, and then at least twice a year to verify that good control is being maintained.
When is HbA1c test ordered?
Screening and diagnosis
HbA1c may be ordered as part of a health checkup or when someone is suspected of having diabetes because of classical signs or symptoms of increased blood glucose levels (hyperglycemia) such as:
- Increased thirst and drinking fluids
- Increased urination
- Increased appetite
- Fatigue
- Blurred vision
- Slow-healing infections
The HbA1c test may also be considered in adults who are overweight with the following additional risk factors:
- Physical inactivity
- First-degree relative (sibling or parent) with diabetes
- High-risk race/ethnicity (e.g., African American, Latino, Native American, Asian American, Pacific Islander)
- High blood pressure (hypertension)
- Abnormal lipid profile (low HDL cholesterol and/or high triglycerides)
- Women with polycystic ovary syndrome
- History of cardiovascular diseases
- Other clinical conditions associated with insulin resistance
The American Diabetes Association recommends to begin HbA1c testing at age 45 for overweight or obese people; if the result is normal, the testing should be repeated at a minimum of 3-year intervals, with consideration of more frequent testing depending on initial results and risk status.
People who are not diagnosed with diabetes but are determined to be at increased risk for diabetes (prediabetes) should have HbA1c testing yearly.
Monitoring
Depending on the type of diabetes that a person has, how well that person’s diabetes is controlled, and on the healthcare provider’s recommendations, the HbA1c test may be measured 2 to 4 times each year. The American Diabetes Association recommends HbA1c testing for diabetics at least twice a year if they are meeting treatment goals and under stable glycemic control. When someone is first diagnosed with diabetes or if control is not good, HbA1c may be ordered quarterly.
What does HbA1c test result mean?
In screening and diagnosis, some HbA1c results that may be seen include:
- A nondiabetic person will have an HbA1c result less than 5.7% (39 mmol/mol).
- Diabetes: HbA1c level is 6.5% (48 mmol/mol) or higher.
- Increased risk of developing diabetes in the future (Impaired glucose regulation (IGR) or Prediabetes): HbA1c of 5.7% to 6.4% (39-46 mmol/mol)
If your HbA1c test returns a reading of 6.0–6.4%, that indicates prediabetes. Your doctor should work with you to suggest appropriate lifestyle changes that could reduce your risk of developing type 2 diabetes.
- HbA1c is not used to diagnose gestational diabetes in the US. Instead, an oral glucose tolerance test (OGTT) is used.
A random blood glucose test will usually be used to diagnose type 1 diabetes. However, in some cases, an HbA1c test may be used to support a diagnosis of type 1 diabetes.
For monitoring glucose control, HbA1c is currently reported as a percentage and for most diabetics, it is recommended that they aim to keep their hemoglobin HbA1c below 7%. The closer diabetics can keep their HbA1c to the American Diabetes Association (ADA)’s therapeutic goal of less than 7% without experiencing excessive low blood glucose (hypoglycemia), the better their diabetes is in control. As the HbA1c increases, so does the risk of complications.
Why is HbA1c important?
- People with diabetes who reduced their HbA1c by less than 1% can cut their risk of dying within 5 years by 50%, according to Swedish research presented at the annual meeting of the European Association for the Study of Diabetes, Sept. 2012 2.
An individual with type 2 diabetes, however, may have an HbA1c goal selected by the person and his or her healthcare provider. The goal may depend on several factors, such as length of time since diagnosis, the presence of other diseases as well as diabetes complications (e.g., vision impairment or loss, kidney damage), risk of complications from hypoglycemia, limited life expectancy, and whether or not the person has a support system and healthcare resources readily available.
For example, a person with heart disease who has lived with type 2 diabetes for many years without diabetic complications may have a higher HbA1c target (e.g., 7.5%-8.0%) set by their healthcare provider, while someone who is otherwise healthy and just diagnosed may have a lower target (e.g., 6.0%-6.5%) as long as low blood sugar is not a significant risk.
Limitations of HbA1c tests
Whilst HbA1c tests are usually reliable, there are some limitations to the accuracy of the test. For example, people with forms of anaemia may not have sufficient hemoglobin for the test to be accurate and may need to have a fructosamine test instead.
Being pregnant or having an uncommon form of hemoglobin (known as a hemoglobin variant) can also return an inaccurate HbA1c, while readings can also be affected by short term issues such as illness as they can cause a temporary rise in blood glucose.
Because of the way the HbA1c test measures blood sugar, if you have higher blood sugar levels in the weeks leading up to your HbA1c test, this will have a greater impact on your test result than your glucose levels 2 to 3 months before the test.
HbA1c and Pregnancy
Keeping blood sugar levels under control is hugely important for women who either have diabetes going into pregnancy or who develop diabetes during their pregnancy.
Tight blood glucose control helps increase the chances of a successful pregnancy by cutting the risk of complications for your baby.
If you have diabetes, one of the ways your doctor or nurse will monitor your glycemic control is by carrying out a HbA1c test.
The HbA1c test measures glycated haemoglobin – a molecule within red blood cells that naturally bonds with glucose – to get a good indication of your average blood glucose over the past 8-12 weeks.
This guide outlines when your HbA1c readings will be taken and what HbA1c values should be before (planning stage), during and after your pregnancy.
Planning pregnancy
The National Institute for Health and Care Excellence (NICE) guidelines for Diabetes in Pregnancy 3 state that women with diabetes should aim to achieve an HbA1c result of 6.1% (43 mmol/mol) or lower.
If you are planning to become pregnant, you should be offered an HbA1c measurement on a monthly basis to help monitor your blood glucose control.
Meeting the target will help to minimize the risk of the baby developing risk of congenital malformations.
If you have an HbA1c above 10%, it is strongly advised to avoid becoming pregnant until good diabetes control is achieved and sustained.
During pregnancy
During the first trimester of pregnancy, the HbA1c target for women with diabetes is the same as for planning a pregnancy, that is 43 mmol/mol (6.1%) or lower.
During the second and third trimesters of pregnancy, from week 13 onwards, HbA1c should not be used for assessing blood glucose control.
Throughout pregnancy, women with diabetes should aim to meet the following blood glucose targets:
- Before meals: 3.5 to 5.9 mmol/l
- 1 hour after meals: 7.8 mmol/l or under
If pregnancy is not planned
If pregnancy has occurred unplanned, it is important to aim to reach the HbA1c target of 6.1% (43 mmol/mol) as soon as possible.
Some women may find this difficult. In this case, it is best to aim to get as close to the target as possible.
Try not to worry if you are failing to meet the target and work with your health team on ways you can get close to the target without becoming stressed or overly anxious.
Post pregnancy
Women with diabetes can return to their normal recommended HbA1c levels of 6.5% (48 mmol/mol) or under after the pregnancy.
Diagnosing gestational diabetes
HbA1c is not used for diagnosing gestational diabetes. Pregnant women without diabetes will be screened for possible gestational diabetes between weeks 8 and 12 of the pregnancy and an oral glucose tolerance test (OGTT) will be carried out between weeks 24 and 28.
If you have had gestational diabetes during a previous pregnancy, you will be given an OGTT between 16 and 18 weeks and then at 28 weeks.
- Association of glycaemia with macrovascular and microvascular complications of Type 2 diabetes: prospective observational study. British Medical Journal 2000; 321: 405-412.[↩]
- Abstracts of the 48th EASD (European Association for the Study of Diabetes) Annual Meeting of the European Association for the Study of Diabetes. October 1-5, 2012. Berlin, Germany. Diabetologia. 2012 Oct;55 Suppl 1:S7-537. doi: 10.1007/s00125-012-2688-9. https://link.springer.com/content/pdf/10.1007%2Fs00125-012-2688-9.pdf[↩]
- Diabetes in pregnancy: management from preconception to the postnatal period. https://www.nice.org.uk/guidance/ng3[↩]