Contents
- What is hip replacement
- Hip Joint Anatomy
- Partial hip replacement
- Total hip replacement
- Hip replacement alternatives
- Is Hip Replacement Surgery for You?
- Possible complications of hip replacement surgery
- Preparing for hip replacement surgery
- Hip replacement surgery
- Hip replacement procedure
- Revision Total Hip Replacement
- Hip replacement surgery recovery
- Hip replacement recovery time
- Avoiding problems after hip replacement surgery
- Total Hip Replacement Exercise Guide
What is hip replacement
Hip replacement surgery is a procedure for people with severely damaged hip joint to replace it with an artificial one (known as a prosthesis). The most common reason for hip replacement is damaged hip caused by osteoarthritis. Osteoarthritis causes pain, swelling, and reduced motion in your joints. It can interfere with your daily activities. If your hip has been damaged by arthritis, a fracture, or other conditions, common activities such as walking or getting in and out of a chair may be painful and difficult. Your hip may be stiff, and it may be hard to put on your shoes and socks. You may even feel uncomfortable while resting.
If other treatments such as physical therapy, pain medicines, changes in your everyday activities, exercise and the use of walking supports do not adequately help your symptoms, you may consider hip replacement surgery.
Adults of any age can be considered for a hip replacement, although most are carried out on people between the ages of 60 and 80.
Hip replacement surgery is a safe and effective procedure that can relieve your pain, increase motion, and help you get back to enjoying normal, everyday activities.
Hip replacement surgery was first performed in 1960, hip replacement surgery is one of the most successful operations in all of medicine. Since 1960, improvements in joint replacement surgical techniques and technology have greatly increased the effectiveness of total hip replacement. According to the Agency for Healthcare Research and Quality, more than 300,000 total hip replacements are performed each year in the United States.
During a hip replacement operation, the surgeon removes damaged cartilage and bone from your hip joint and replaces them with new, man-made parts.
A modern artificial hip joint is designed to last for at least 15 years. Most people experience a significant reduction in pain and some improvement in their range of movement.
A hip replacement can:
- Relieve pain
- Help your hip joint work better
- Improve walking and other movements
The most common problem after a hip replacement surgery is hip dislocation. Because a man-made hip is smaller than the original joint, the ball can come out of its socket. The surgery can also cause blood clots and infections. With a hip replacement, you might need to avoid certain activities, such as jogging and high-impact sports.
Common causes of hip pain
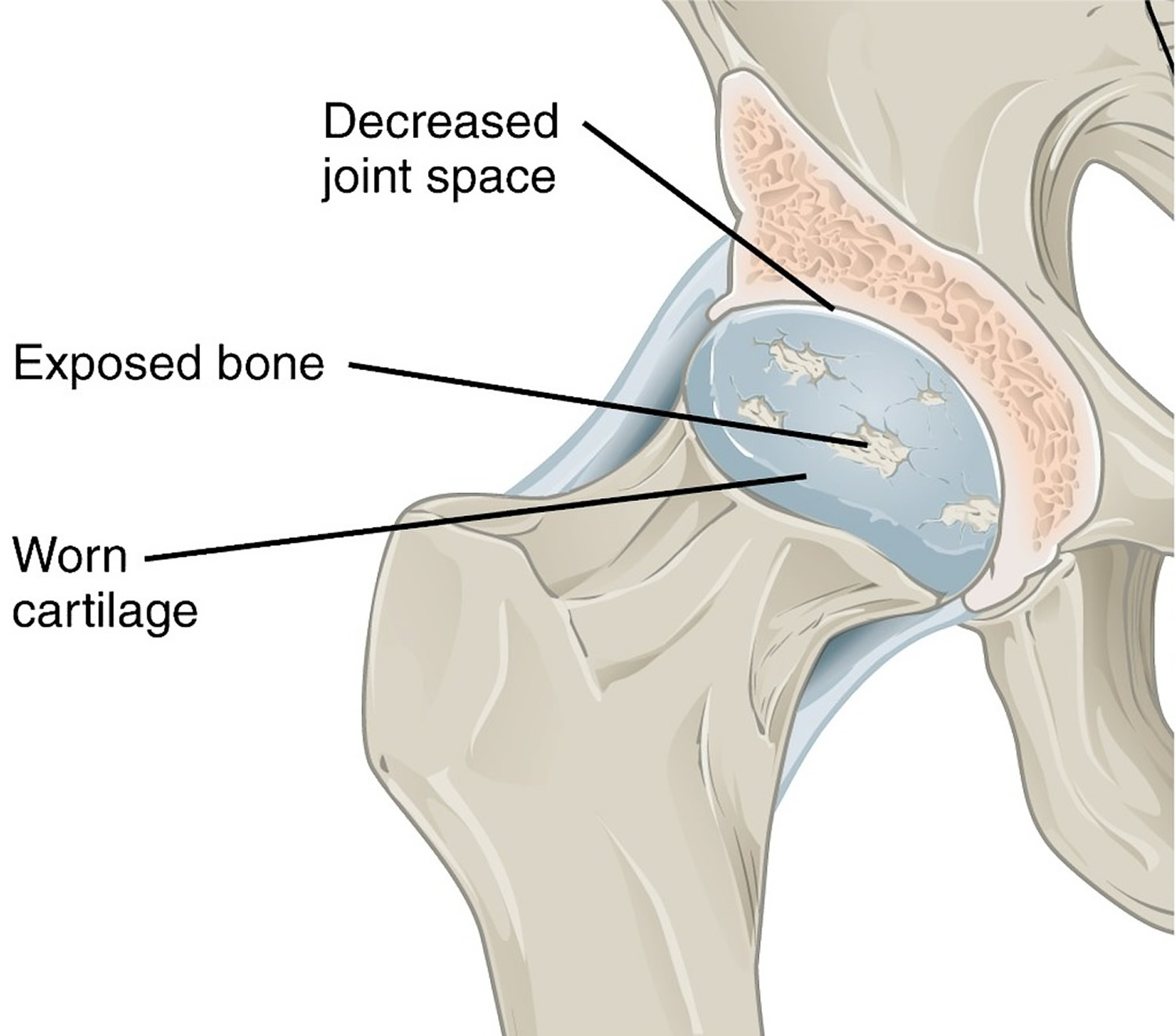
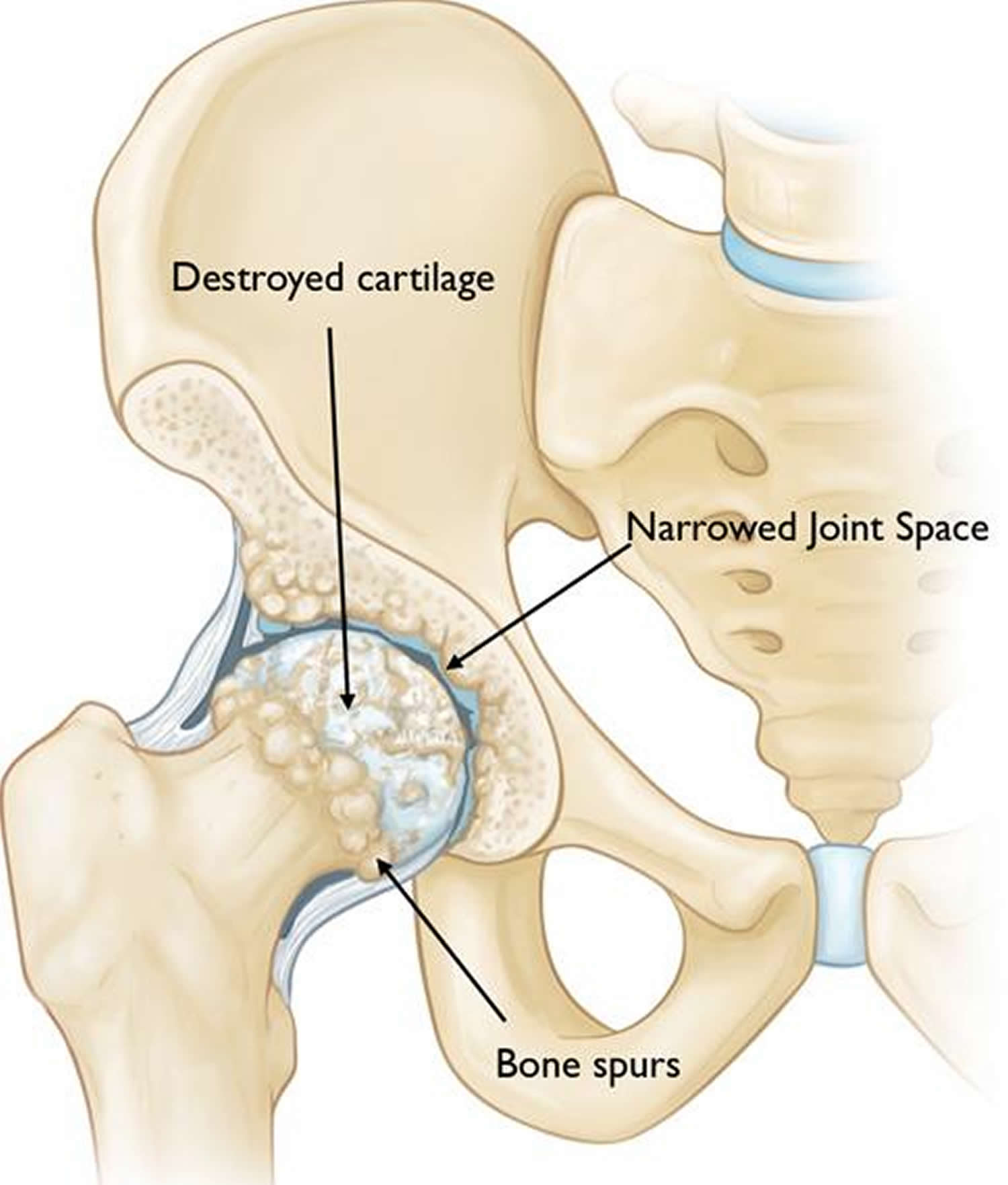
The most common cause of chronic hip pain and disability is arthritis. Osteoarthritis, rheumatoid arthritis, and traumatic arthritis are the most common forms of this disease.
- Osteoarthritis. This is an age-related “wear and tear” type of arthritis. It usually occurs in people 50 years of age and older and often in individuals with a family history of arthritis. The cartilage cushioning the bones of the hip wears away. The bones then rub against each other, causing hip pain and stiffness. Osteoarthritis may also be caused or accelerated by subtle irregularities in how the hip developed in childhood.
- Rheumatoid arthritis. This is an autoimmune disease in which the synovial membrane becomes inflamed and thickened. This chronic inflammation can damage the cartilage, leading to pain and stiffness. Rheumatoid arthritis is the most common type of a group of disorders termed “inflammatory arthritis.”
- Post-traumatic arthritis. This can follow a serious hip injury or fracture. The cartilage may become damaged and lead to hip pain and stiffness over time.
- Avascular necrosis. An injury to the hip, such as a dislocation or fracture, may limit the blood supply to the femoral head. This is called avascular necrosis (also commonly referred to as “osteonecrosis”). The lack of blood may cause the surface of the bone to collapse, and arthritis will result. Some diseases can also cause avascular necrosis.
- Childhood hip disease. Some infants and children have hip problems. Even though the problems are successfully treated during childhood, they may still cause arthritis later on in life. This happens because the hip may not grow normally, and the joint surfaces are affected.
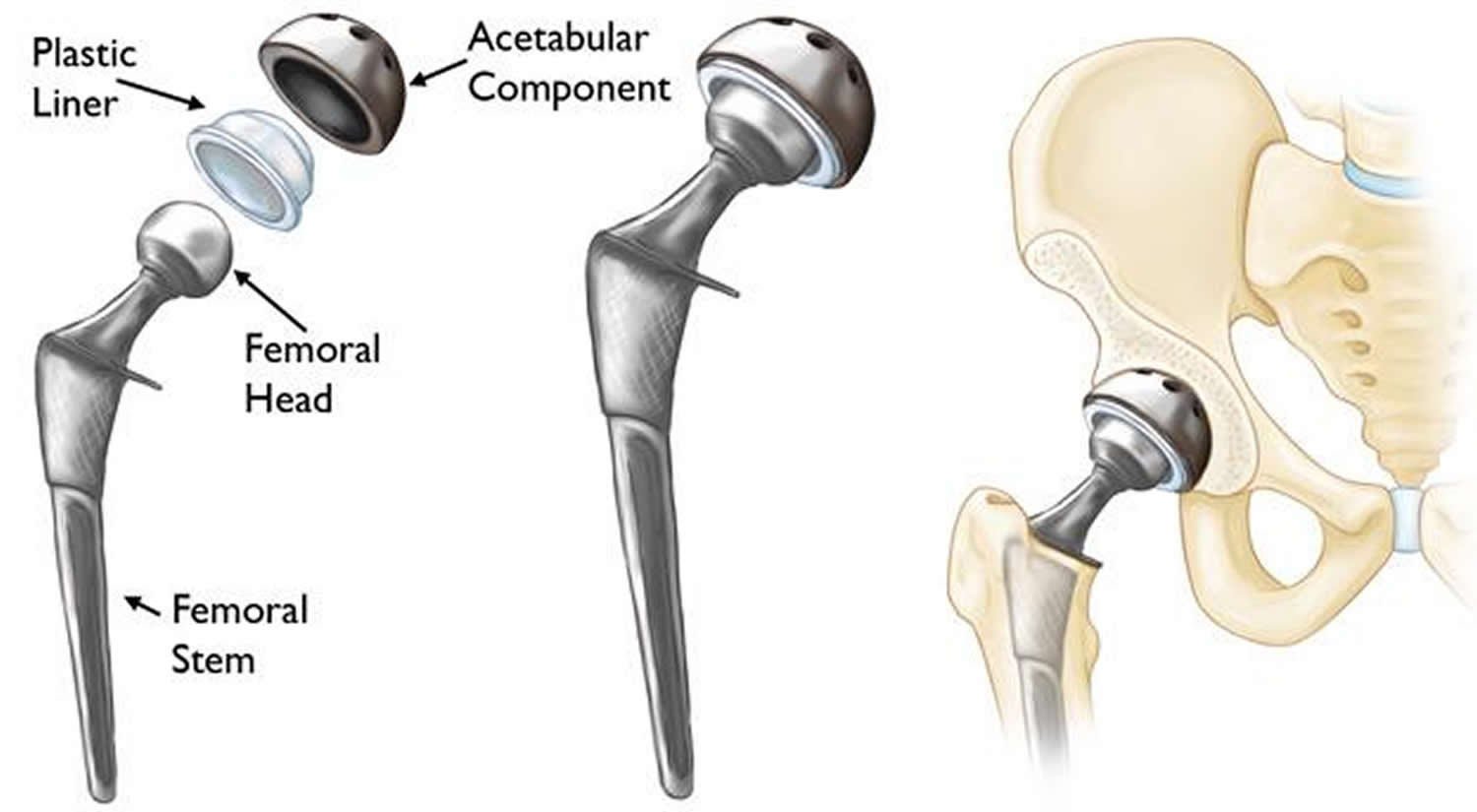
Figure 1. Hip replacement (total hip replacement) – Note: (Left) The individual components of a total hip replacement. (Center) The components merged into an implant. (Right) The implant as it fits into the hip.
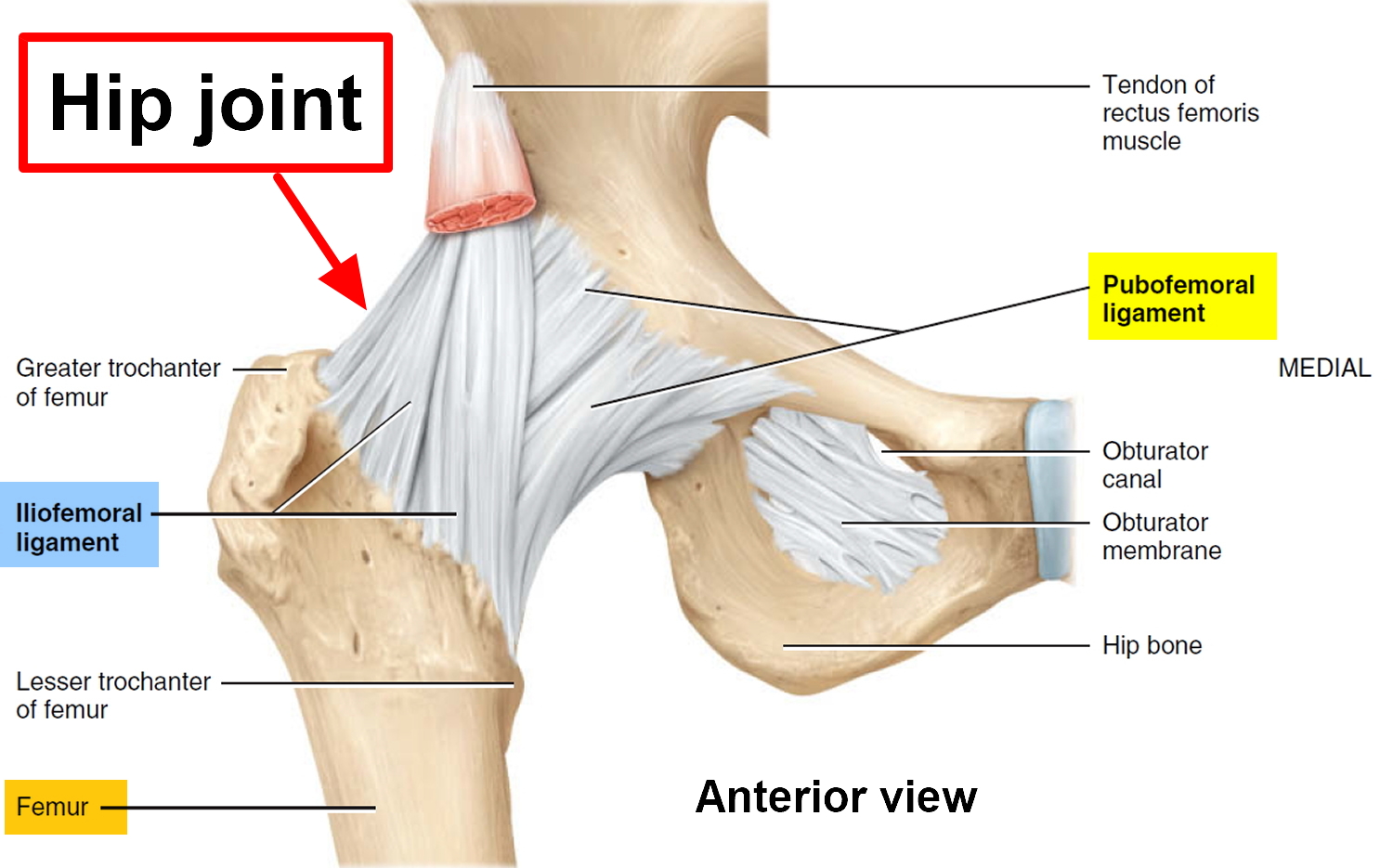
Hip Joint Anatomy
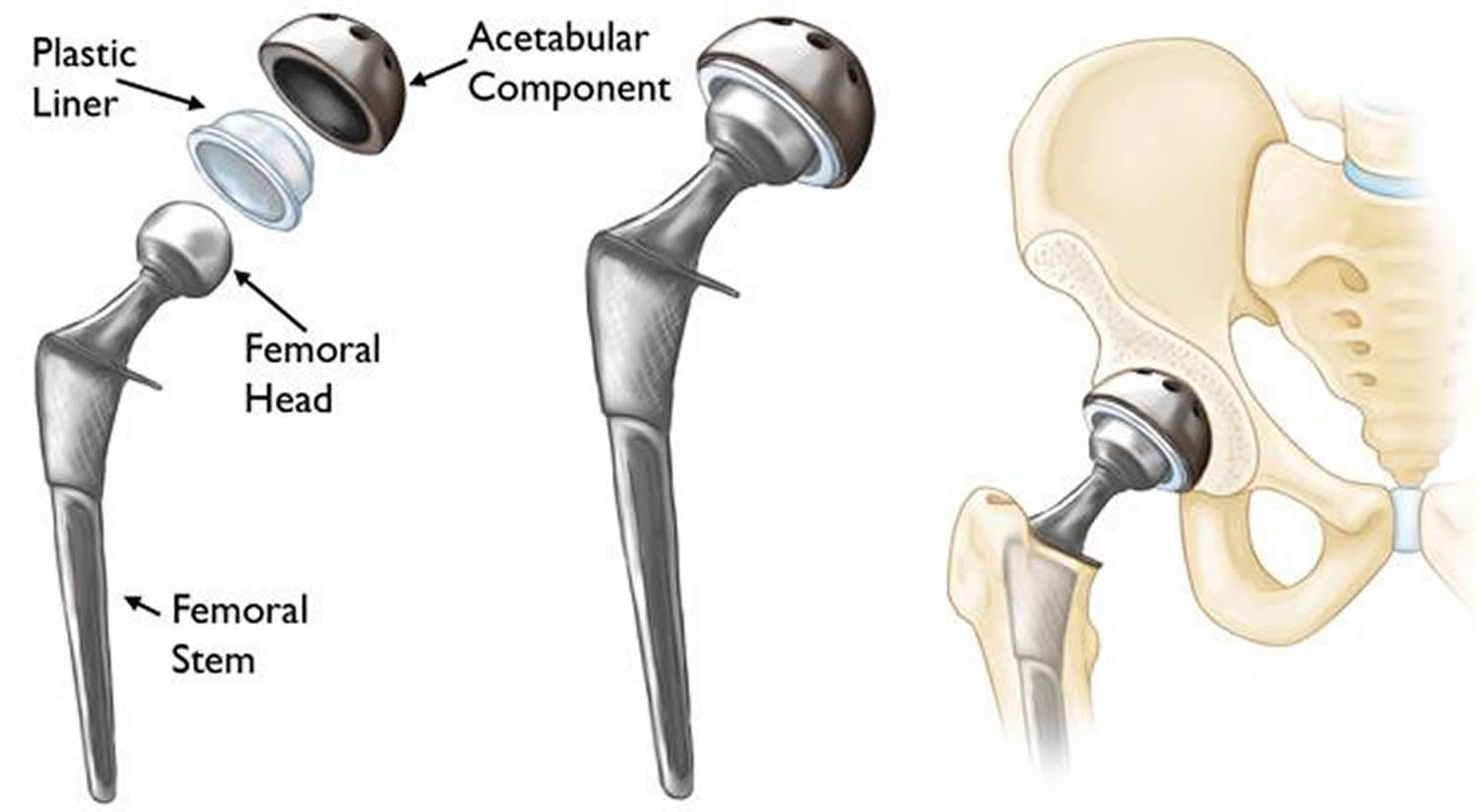
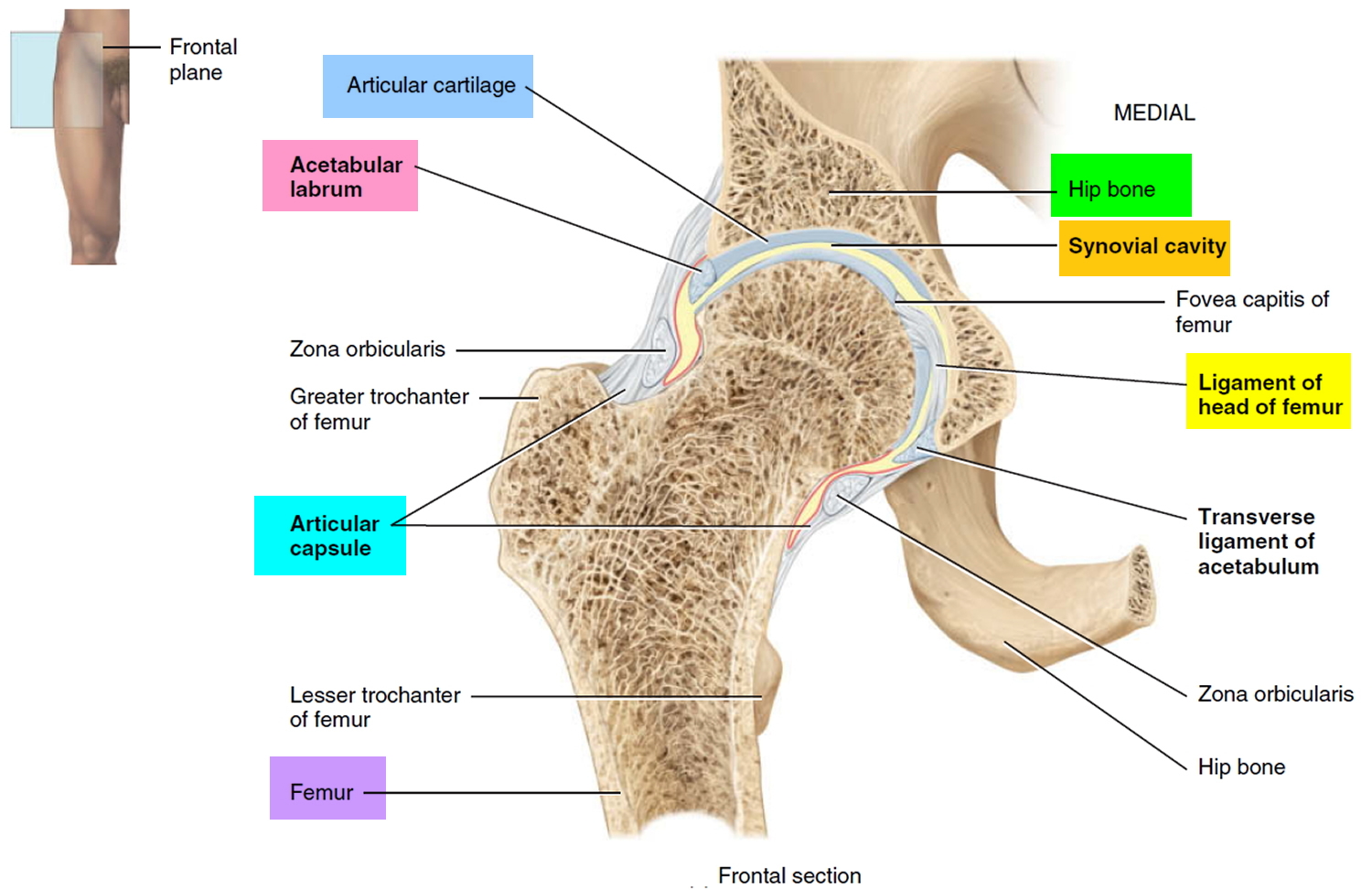
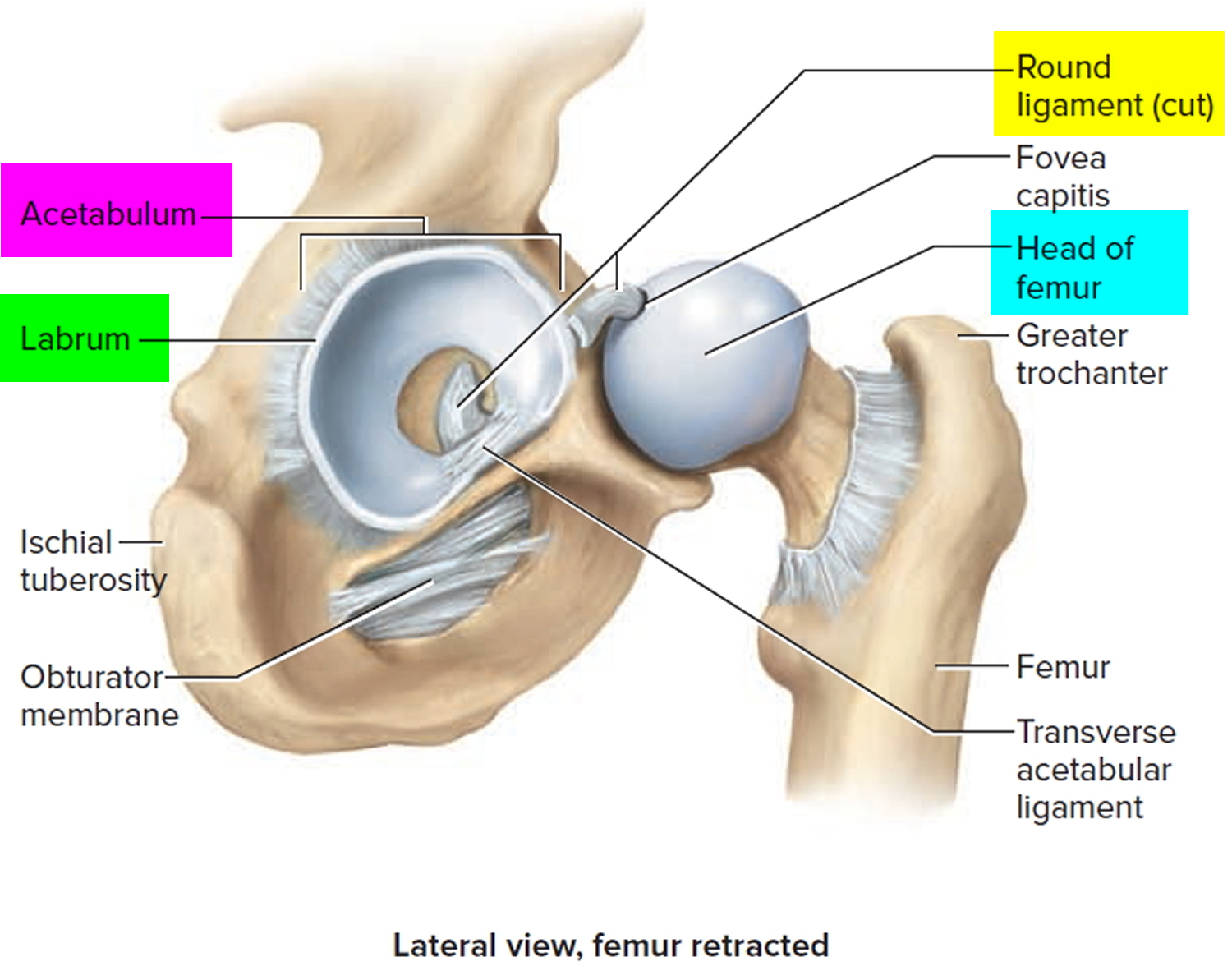
The hip is one of the body’s largest joints. The hip joint (coxal joint) is a ball-and-socket joint formed by the head of the femur and the acetabulum of the hip bone. The socket is formed by the acetabulum, which is part of the large pelvis bone. The ball is the femoral head, which is the upper end of the femur (thighbone). The bone surfaces of the ball and socket are covered with articular cartilage, a smooth tissue that cushions the ends of the bones and enables them to move easily.
A thin tissue called synovial membrane surrounds the hip joint. In a healthy hip, this membrane makes a small amount of fluid that lubricates the cartilage and eliminates almost all friction during hip movement.
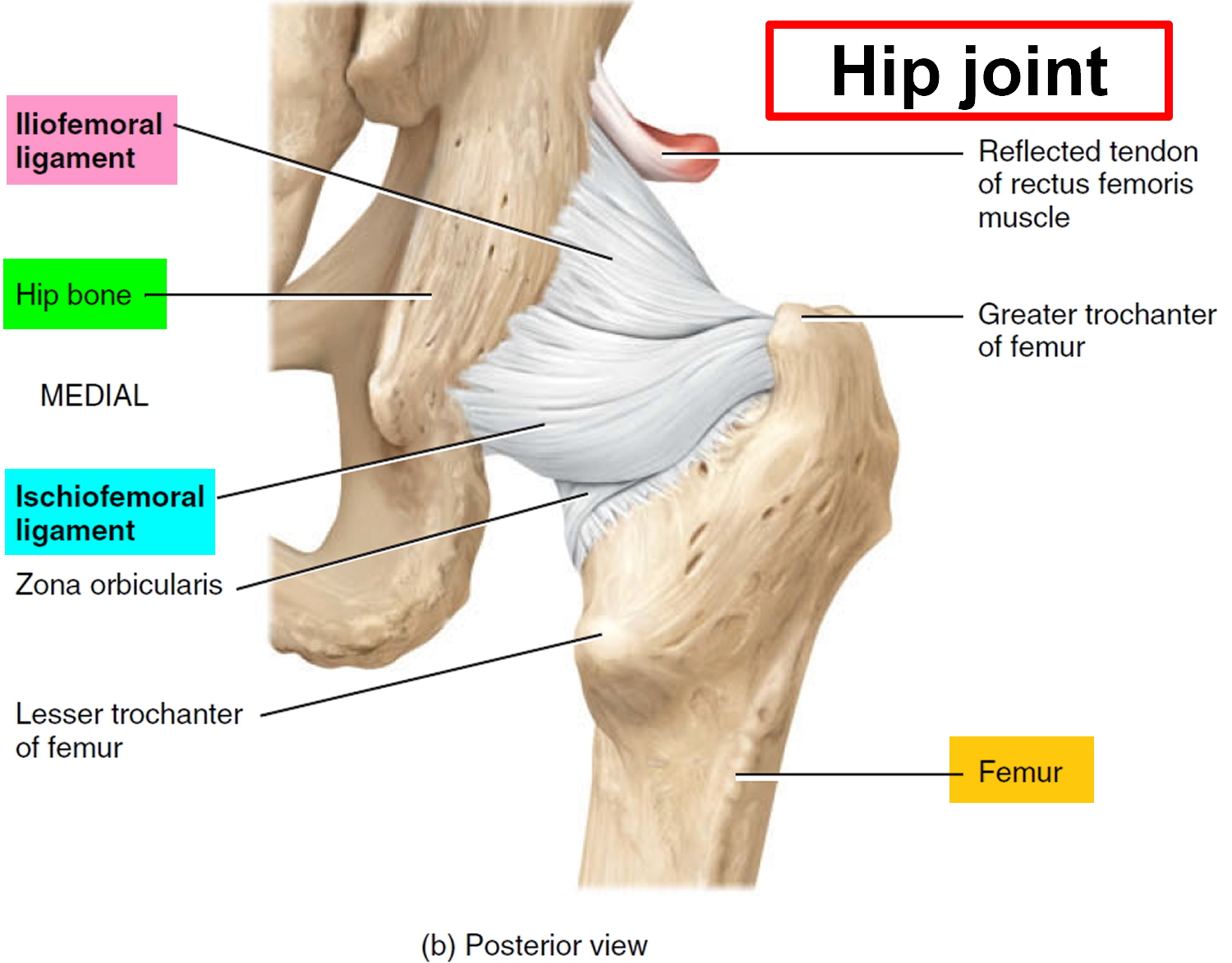
Bands of tissue called ligaments (the hip capsule) connect the ball to the socket and provide stability to the joint.
The hip joint allows flexion, extension, abduction, adduction, lateral rotation medial rotation, and circumduction of the thigh. The extreme stability of the hip joint is related to the very strong articular capsule and its accessory ligaments, the manner in which the femur fits into the acetabulum, and the muscles surrounding the joint.
Figure 2. Hip joint anatomy
 Hip joint anatomical components
Hip joint anatomical components
1. Articular capsule
Very dense and strong capsule that extends from the rim of the acetabulum to the neck of the femur (Figure 2). With its accessory ligaments, this is one of the strongest structures of the body. The articular capsule consists of circular and longitudinal fibers. The circular fibers, called the zona orbicularis, form a collar around the neck of the femur. Accessory ligaments known as the iliofemoral ligament, pubofemoral ligament, and ischiofemoral ligament reinforce the longitudinal fibers of the articular capsule.
2. Iliofemoral ligament
Thickened portion of the articular capsule that extends from the anterior inferior iliac spine of the hip bone to the intertrochanteric line of the femur (Figure 2). This ligament is said to be the body’s strongest and prevents hyperextension of the femur at the hip joint during standing.
3. Pubofemoral ligament
Thickened portion of the articular capsule that extends from the pubic part of the rim of the acetabulum to the neck of the femur. This ligament prevents overabduction of the femur at the hip joint and strengthens the articular capsule.
4. Ischiofemoral ligament
Thickened portion of the articular capsule that extends from the ischial wall bordering the acetabulum to the neck of the femur. This ligament slackens during adduction, tenses during abduction, and strengthens the articular capsule.
5. Ligament of the head of the femur
Flat, triangular band (primarily a synovial fold) that extends from the fossa of the acetabulum to the fovea capitis of the head of the femur. The ligament usually contains a small artery that supplies the head of the femur.
6. Acetabular labrum
Fibrocartilage rim attached to the margin of the acetabulum that enhances the depth of the acetabulum. As a result, dislocation of the femur is rare.
7. Transverse ligament of the acetabulum
Strong ligament that crosses over the acetabular notch. It supports part of the acetabular labrum and is connected with the ligament of the head of the femur and the articular capsule.
Partial hip replacement
Partial hip replacement also called hemiarthroplasty replaces only the ball part (the head of femur or femoral head) of your hip joint. Partial hip replacement is generally considered to be the treatment of choice in the most elderly patients with a displaced fracture of the femoral neck.
In elderly patients suffering from a displaced femoral neck fracture, a cemented hip arthroplasty, compared to internal fixation, partial hip replacement (hemiarthroplasty) has been shown to reduce the reoperation rate and give better hip function and health-related quality of life 1. In the healthy, active elderly with a long life expectancy, a total hip replacement is probably the best treatment 2 while a partial hip replacement (Hemiarthroplasty) is generally considered to be sufficient for the most elderly patients with lower functional demands and a shorter life expectancy.
There are two different types of partial hip replacement (hemiarthroplasty): unipolar and bipolar. The theoretical advantage of the bipolar partial hip replacement (Hemiarthroplasty) is a reduction of acetabular wear due to the dual-bearing system 3. On the other hand, a potential disadvantage is the risk of polyethylene wear that may contribute to mechanical loosening over time and there is also a risk of inter-prosthetic dissociation in certain bipolar partial hip replacements necessitating open reduction 4. However, dissociation appears to be rare in modern bipolar surgical systems.
Based on the results of numerous studies 5, 6, 7, 8, 9, there does not appear to be any clinical disadvantage with the bipolar design. On the contrary, the results of this study 5 showed that the rate of acetabular erosion was significantly lower after the bipolar partial hip replacement, which in turn may indicate an advantage in the longer term. However, there is one frequently cited disadvantage associated with the bipolar partial hip replacement, i.e. the higher cost, the magnitude of which probably differs between countries. Since there were no differences in duration of surgery, need for blood transfusions, hospital stay and complications during the first year, this difference probably represents the total difference in primary costs for the two treatment modalities. This investment may well be justified in order to reduce the risk of future problems owing to acetabular erosion.
Figure 3. Partial hip replacement (Unipolar)
Figure 4. Partial hip replacement (Bipolar)
Total hip replacement
In a total hip replacement (also called total hip arthroplasty), the damaged bone and cartilage is removed and replaced with prosthetic components (see Figure 1 above).
- The damaged femoral head is removed and replaced with a metal stem that is placed into the hollow center of the femur. The femoral stem may be either cemented or “press fit” into the bone.
- A metal or ceramic ball is placed on the upper part of the stem. This ball replaces the damaged femoral head that was removed.
- The damaged cartilage surface of the socket (acetabulum) is removed and replaced with a metal socket. Screws or cement are sometimes used to hold the socket in place.
- A plastic, ceramic, or metal spacer is inserted between the new ball and the socket to allow for a smooth gliding surface.
Hip replacement alternatives
There is an alternative type of surgery to hip replacement, known as hip resurfacing. This involves removing the damaged surfaces of the bones inside the hip joint and replacing them with a metal surface.
An advantage to this approach is that it removes less bone. However, it may not be suitable for:
- adults over the age of 65 years – bones tend to weaken as a person becomes older
- women who have gone through the menopause – one of the side effects of the menopause is that the bones can become weakened and brittle (osteoporosis)
Resurfacing is much less popular now due to concerns about the metal surface causing damage to soft tissues around the hip.
Your surgeon should be able to tell you if you could be a suitable candidate for hip resurfacing.
Is Hip Replacement Surgery for You?
The decision to have hip replacement surgery should be a cooperative one made by you, your family, your primary care doctor, and your orthopaedic surgeon. The process of making this decision typically begins with a referral by your doctor to an orthopedic surgeon for an initial evaluation.
Hip replacement surgery is usually necessary when the hip joint is worn or damaged to the extent that your mobility is reduced and you experience pain even while resting.
The most common reason for hip replacement surgery is osteoarthritis. Other conditions that can cause hip joint damage include:
- rheumatoid arthritis
- a hip fracture
- septic arthritis
- ankylosing spondylitis
- disorders that cause unusual bone growth (bone dysplasias)
Candidates for hip replacement surgery
There are no absolute age or weight restrictions for total hip replacements. However, a hip replacement is major surgery, so is normally only recommended if other treatments, such as physiotherapy or steroid injections, haven’t helped reduce pain or improve mobility.
Recommendations for surgery are based on a patient’s pain and disability, not age. Most patients who undergo total hip replacement are age 50 to 80, but orthopedic surgeons evaluate patients individually. Total hip replacements have been performed successfully at all ages, from the young teenager with juvenile arthritis to the elderly patient with degenerative arthritis.
You may be offered hip replacement surgery if:
- you have severe pain, swelling and stiffness in your hip joint and your mobility is reduced
- your hip pain is so severe that it interferes with your quality of life and sleep
- everyday tasks, such as shopping or getting out of the bath, are difficult or impossible
- you’re feeling depressed because of the pain and lack of mobility
- you can’t work or have a normal social life
You’ll also need to be well enough to cope with both a major operation and the rehabilitation afterwards.
When hip replacement surgery is recommended
There are several reasons why your doctor may recommend hip replacement surgery. People who benefit from hip replacement surgery often have:
- Hip pain that limits everyday activities, such as walking or bending
- Hip pain that continues while resting, either day or night
- Stiffness in a hip that limits the ability to move or lift the leg
- Inadequate pain relief from anti-inflammatory drugs, physical therapy, or walking supports
The Orthopedic Evaluation
An evaluation with an orthopedic surgeon consists of several components.
- Medical history. Your orthopedic surgeon will gather information about your general health and ask questions about the extent of your hip pain and how it affects your ability to perform everyday activities.
- Physical examination. This will assess hip mobility, strength, and alignment.
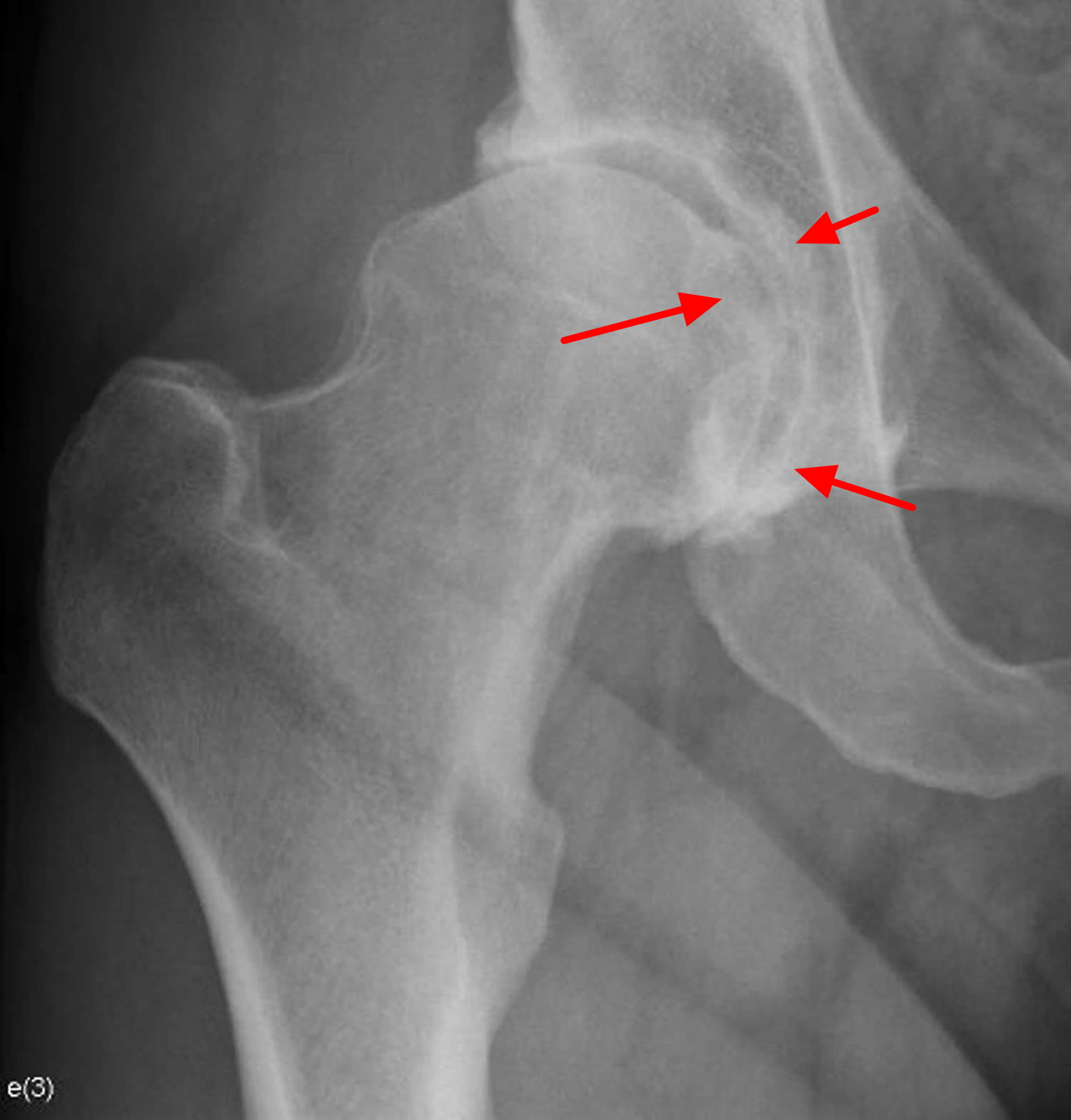
- X-rays. These images help to determine the extent of damage or deformity in your hip.
- Other tests. Occasionally other tests, such as a magnetic resonance imaging (MRI) scan, may be needed to determine the condition of the bone and soft tissues of your hip.
Figure 5. Hip osteoarthritis – note the smooth articular cartilage wears away and becomes frayed and rough
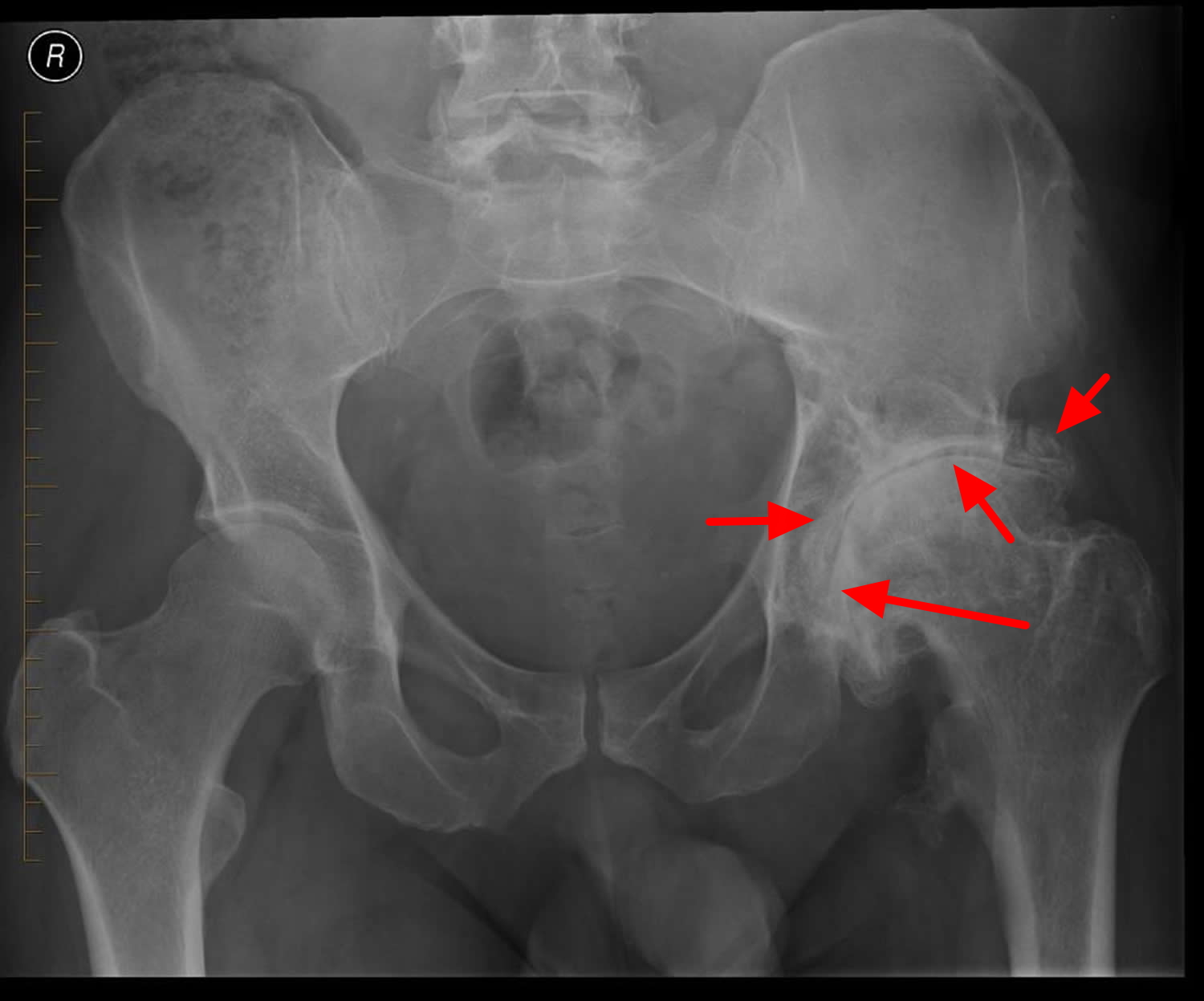
Figure 6. Hip osteoarthritis (X-ray)
Note: Dysplastic acetabulum with insufficient covering of the femoral head. Joint space narrowing, subchondral sclerosis and osteophytes at the femoroacetabular joint. Prominent bump at the antero-superior head-neck junction of the femur (cam deformity, also known as pistol grip deformity of the proximal femur).
Figure 7. Hip osteoarthritis (X-ray)
Note: Advanced left hip osteoarthritis with severe loss of joint space, subchondral sclerosis and marginal osteophytes.
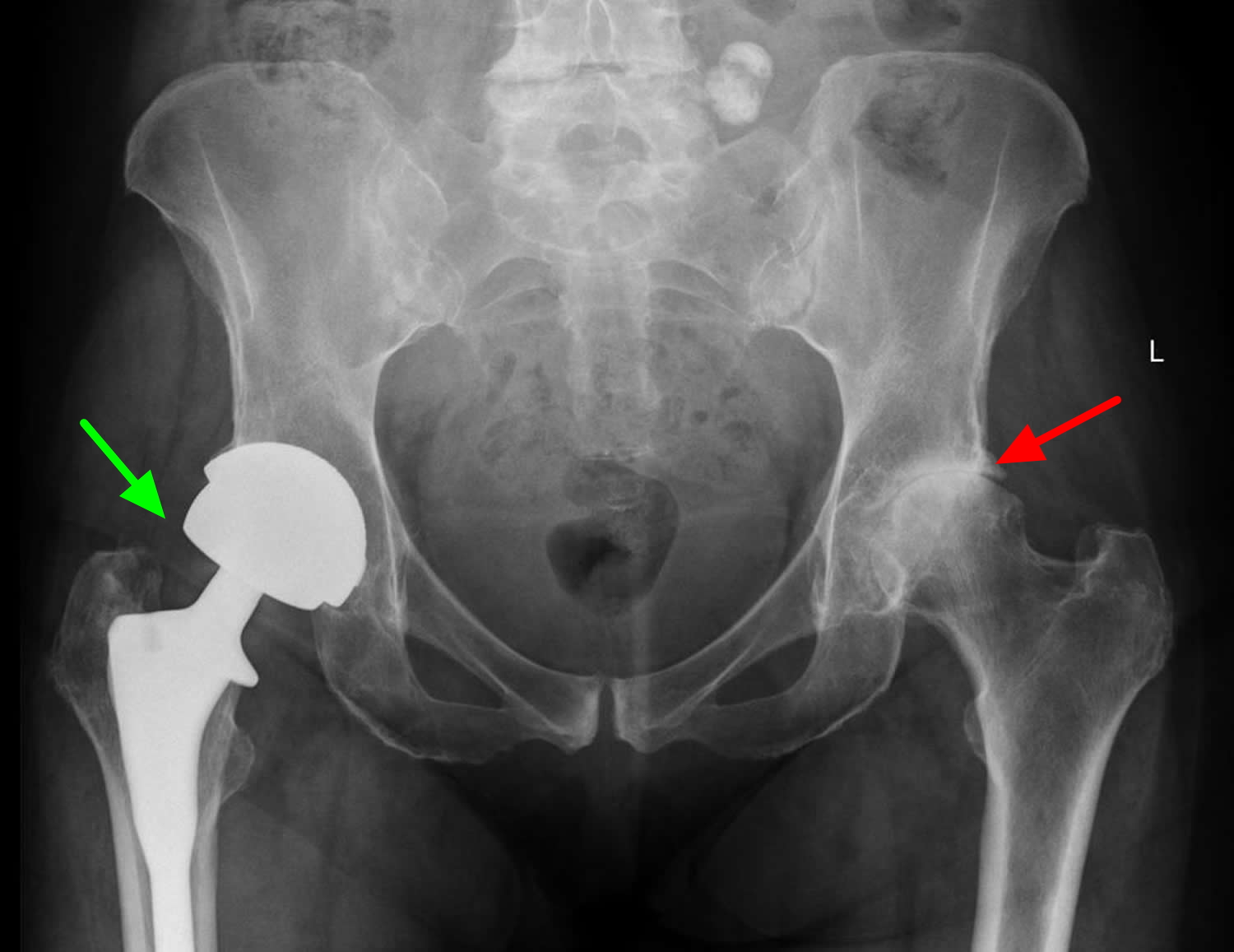
Figure 8. Total hip replacement (right hip – green arrow) and left hip osteoarthritis (red arrow) X-ray
Deciding to Have Hip Replacement Surgery
Talk with your doctor
Your orthopedic surgeon will review the results of your evaluation with you and discuss whether hip replacement surgery is the best method to relieve your pain and improve your mobility. Other treatment options — such as medications, physical therapy, or other types of surgery — also may be considered.
In addition, your orthopedic surgeon will explain the potential risks and complications of hip replacement surgery, including those related to the surgery itself and those that can occur over time after your surgery.
Never hesitate to ask your doctor questions when you do not understand. The more you know, the better you will be able to manage the changes that hip replacement surgery will make in your life.
Realistic expectations
An important factor in deciding whether to have hip replacement surgery is understanding what the procedure can and cannot do. Most people who undergo hip replacement surgery experience a dramatic reduction of hip pain and a significant improvement in their ability to perform the common activities of daily living.
With normal use and activity, the material between the head and the socket of every hip replacement implant begins to wear. Excessive activity or being overweight may speed up this normal wear and cause the hip replacement to loosen and become painful. Therefore, most surgeons advise against high-impact activities such as running, jogging, jumping, or other high-impact sports.
Realistic activities following total hip replacement include unlimited walking, swimming, golf, driving, hiking, biking, dancing, and other low-impact sports.
With appropriate activity modification, hip replacements can last for many years.
Possible complications of hip replacement surgery
The complication rate following hip replacement surgery is low. Serious complications, such as joint infection, occur in less than 2% of patients. Major medical complications, such as heart attack or stroke, occur even less frequently. However, chronic illnesses may increase the potential for complications. Although uncommon, when these complications occur they can prolong or limit full recovery.
Infection
A small percentage of patients undergoing hip replacement (roughly about 1 in 100) may develop an infection after the operation.
Infection may occur superficially in the wound or deep around the artificial implants. An infection may develop while in the hospital or after you go home. It may even occur years later.
Minor infections of the wound are generally treated with antibiotics. Major or deep infections may require more surgery and removal of the artificial implants. Any infection in your body can spread to your joint replacement.
Infections are caused by bacteria. Although bacteria are abundant in your gastrointestinal tract and on your skin, they are usually kept in check by your immune system. For example, if bacteria make it into your bloodstream, your immune system rapidly responds and kills the invading bacteria.
However, because joint replacements are made of metal and plastic, it is difficult for the immune system to attack bacteria that make it to these implants. If bacteria gain access to the implants, they may multiply and cause an infection.
Despite antibiotics and preventive treatments, patients with infected joint replacements often require surgery to cure the infection.
The most common ways bacteria enter the body include:
- Through breaks or cuts in the skin
- During major dental procedures (such as a tooth extraction or root canal)
- Through wounds from other surgical procedures
Some people are at a higher risk for developing infections after a joint replacement procedure. Factors that increase the risk for infection include:
- Immune deficiencies (such as HIV or lymphoma)
- Diabetes mellitus
- Peripheral vascular disease (poor circulation to the hands and feet)
- Immunosuppressive treatments (such as chemotherapy or corticosteroids)
- Obesity
Prevention
At the time of original joint replacement surgery, there are several measures taken to minimize the risk of infection. Some of the steps have been proven to lower the risk of infection, and some are thought to help but have not been scientifically proven. The most important known measures to lower the risk of infection after total joint replacement include:
- Antibiotics before and after surgery. Antibiotics are given within one hour of the start of surgery (usually once in the operating room) and continued at intervals for 24 hours following the procedure.
- Short operating time and minimal operating room traffic. Efficiency in the operation by your surgeon helps to lower the risk of infection by limiting the time the joint is exposed. Limiting the number of operating room personnel entering and leaving the room is thought to the decrease risk of infection.
- Use of strict sterile technique and sterilization instruments. Care is taken to ensure the operating site is sterile, the instruments have been autoclaved (sterilized) and not exposed to any contamination, and the implants are packaged to ensure their sterility.
- Preoperative nasal screening for bacterial colonization. There is some evidence that testing for the presence of bacteria (particularly the Staphylococcus species) in the nasal passages several weeks prior to surgery may help prevent joint infection. In institutions where this is performed, those patients that are found to have Staphylococcus in their nasal passages are given an intranasal antibacterial ointment prior to surgery. The type of bacteria that is found in the nasal passages may help your doctors determine which antibiotic you are given at the time of your surgery.
- Preoperative chlorhexidine wash. There is also evidence that home washing with a chlorhexidine solution (often in the form of soaked cloths) in the days leading up to surgery may help prevent infection. This may be particularly important if patients are known to have certain types of antibiotic-resistant bacteria on their skin or in their nasal passages (see above). Your surgeon will talk with you about this option.
- Long-term prophylaxis. Surgeons sometimes prescribe antibiotics for patients who have had joint replacements before they undergo dental work. This is done to protect the implants from bacteria that might enter the bloodstream during the dental procedure and cause infection. The American Academy of Orthopaedic Surgeons has developed recommendations for when antibiotics should be given before dental work and for which patients would benefit. In general, most people do not require antibiotics before dental procedures. There is little evidence that taking antibiotics before dental procedures is effective at preventing infection.
Antibiotics may also be considered before major surgical procedures; however, most patients do not require this.
Your orthopedic surgeon will talk with you about the risks and benefits of prophylactic antibiotics in your specific situation.
Symptoms of infection
Signs and symptoms of an infected joint replacement include:
- A high temperature (fever) of 38 °C (100.4 °F) or above
- Hip pain that can persist even when resting
- Increased pain or stiffness in a previously well-functioning joint
- Swelling
- Warmth and redness around the wound
- A discharge of liquid from the site of the surgery
- Wound drainage
- Fevers, chills and night sweats
- Fatigue
Blood Clots
There’s a small risk of developing a blood clot in the first few weeks after surgery – either deep vein thrombosis (DVT) in the leg or pulmonary embolism in the lung. Blood clots in the leg veins or pelvis are one of the most common complications of hip replacement surgery. These clots can be life-threatening if they break free and travel to your lungs. Your orthopedic surgeon will outline a prevention program which may include blood thinning medications, support hose, inflatable leg coverings, ankle pump exercises, and early mobilization.
Symptoms of DVT include:
- pain, swelling and tenderness in one of your legs (usually your calf)
- a heavy ache in the affected area
- warm skin in the area of the clot
Symptoms of pulmonary embolism include:
- breathlessness, which may come on suddenly or gradually
- chest pain, which may be worse when you breathe in
- coughing
If you suspect either of these types of blood clots you should seek immediate medical advice from your doctor or the doctor in charge of your care.
To reduce your risk of blood clots you may be given blood thinning medication such as warfarin, or asked to wear compression stockings.
Leg-length Inequality
Sometimes after a hip replacement, one leg may feel longer or shorter than the other. Your orthopedic surgeon will make every effort to make your leg lengths even, but may lengthen or shorten your leg slightly in order to maximize the stability and biomechanics of the hip. Some patients may feel more comfortable with a shoe lift after surgery.
Hip replacement dislocation
This occurs when the ball comes out of the socket. The risk for hip replacement dislocation is greatest in the first few months after surgery while the tissues are healing. Hip replacement dislocation is uncommon. If the ball does come out of the socket, a closed reduction usually can put it back into place without the need for more surgery. In situations in which the hip continues to dislocate, further surgery may be necessary.
Loosening and Implant Wear
Over years, the hip prosthesis may wear out or loosen. This is most often due to everyday activity. It can also result from a biologic thinning of the bone called osteolysis. If loosening is painful, a second surgery called a revision may be necessary.
Joint stiffening
The soft tissues can harden around the implant, causing reduced mobility.
This isn’t usually painful and can be prevented using medication or radiation therapy (a quick and painless procedure during which controlled doses of radiation are directed at your hip joint).
Other complications
Nerve and blood vessel injury, bleeding, fracture, and stiffness can occur. In a small number of patients, some pain can continue or new pain can occur after surgery.
Preparing for hip replacement surgery
Medical Evaluation
If you decide to have hip replacement surgery, your orthopedic surgeon may ask you to have a complete physical examination by your primary care doctor before your surgical procedure. This is needed to make sure you are healthy enough to have the surgery and complete the recovery process. Many patients with chronic medical conditions, like heart disease, may also be evaluated by a specialist, such a cardiologist, before the surgery.
Tests
Several tests, such as blood and urine samples, an electrocardiogram (EKG), and chest x-rays, may be needed to help plan your surgery.
Preparing your skin
Your skin should not have any infections or irritations before surgery. If either is present, contact your orthopedic surgeon for treatment to improve your skin before surgery.
Blood donations
You may be advised to donate your own blood prior to surgery. It will be stored in the event you need blood after surgery.
Medications
Tell your orthopedic surgeon about the medications you are taking. He or she or your primary care doctor will advise you which medications you should stop taking and which you can continue to take before surgery.
Weight Loss
If you are overweight, your doctor may ask you to lose some weight before surgery to minimize the stress on your new hip and possibly decrease the risks of surgery.
Dental evaluation
Although infections after hip replacement are not common, an infection can occur if bacteria enter your bloodstream. Because bacteria can enter the bloodstream during dental procedures, major dental procedures (such as tooth extractions and periodontal work) should be completed before your hip replacement surgery. Routine cleaning of your teeth should be delayed for several weeks after surgery.
Urinary evaluation
Individuals with a history of recent or frequent urinary infections should have a urological evaluation before surgery. Older men with prostate disease should consider completing required treatment before having surgery.
Social planning
Although you will be able to walk with crutches or a walker soon after surgery, you will need some help for several weeks with such tasks as cooking, shopping, bathing, and laundry.
If you live alone, your orthopedic surgeon’s office, a social worker, or a discharge planner at the hospital can help you make advance arrangements to have someone assist you at your home. A short stay in an extended care facility during your recovery after surgery also may be arranged.
Home planning
Several modifications can make your home easier to navigate during your recovery. The following items may help with daily activities:
- Securely fastened safety bars or handrails in your shower or bath
- Secure handrails along all stairways
- A stable chair for your early recovery with a firm seat cushion (that allows your knees to remain lower than your hips), a firm back, and two arms
- A raised toilet seat
- A stable shower bench or chair for bathing
- A long-handled sponge and shower hose
- A dressing stick, a sock aid, and a long-handled shoe horn for putting on and taking off shoes and socks without excessively bending your new hip
- A reacher that will allow you to grab objects without excessive bending of your hips
- Firm pillows for your chairs, sofas, and car that enable you to sit with your knees lower than your hips
- Removal of all loose carpets and electrical cords from the areas where you walk in your home
Hip replacement surgery
You will most likely be admitted to the hospital on the day of your surgery.
Anesthesia
After admission, you will be evaluated by a member of the anesthesia team. The most common types of anesthesia are general anesthesia (you are put to sleep) or spinal, epidural, or regional nerve block anesthesia (you are awake but your body is numb from the waist down). The anesthesia team, with your input, will determine which type of anesthesia will be best for you.
Implant Components
After you and your orthopedic surgeon have determined you are a candidate for hip replacement surgery, your surgeon will select a hip replacement device for you based on your body structure, medical history, and lifestyle.
There are more than 60 different types of implant or prosthesis. However, the options are usually limited to around four or five. Your surgeon can advise you on the type they think would suit you best.
Many different types of designs and materials are currently used in artificial hip joints. All of them consist of two basic components: the ball component (made of a highly polished strong metal or ceramic material) and the socket component (a durable cup of plastic/polyethylene, ceramic, or metal, which may have an outer metal shell). Sometimes, the socket is made of a different material than the ball, or is lined with a different material, and sometimes the ball and socket are made of the same material. Your orthopedic surgeon will recommend the best combination for you.
The prosthetic components may be “press fit” into the bone to allow your bone to grow onto the components or they may be cemented into place. The decision to press fit or to cement the components is based on a number of factors, such as the quality and strength of your bone. A combination of a cemented stem and a non-cemented socket may also be used.
Your orthopedic surgeon will choose the type of prosthesis that best meets your needs.
Figure 9. Femoral component of hip replacement – Note: (Left) A standard non-cemented femoral component. (Center) A close-up of this component showing the porous surface for bone ingrowth. (Right) The femoral component and the acetabular component working together.
Figure 10. Acetabular component of hip replacement – Note: (Left) The acetabular component shows the plastic (polyethylene) liner inside the metal shell. (Right) The porous surface of this acetabular component allows for bone ingrowth. The holes around the cup are used if screws are needed to hold the cup in place.
Metal-on-Metal Implants Precautions
In metal-on-metal devices both the ball and socket components are made of metal. These metal implants have been used in total hip replacement surgeries and hip resurfacing procedures.
Metal-on-metal implants feature a joint made of two metal surfaces:
- a metal “ball” that replaces the ball found at the top of the thigh bone (femur)
- a metal “cup” that acts like the socket found in the pelvis
Because of metal’s durability, metal-on-metal devices were expected to last longer than other hip implants. In addition, the ball in a metal-on-metal device is larger, making the hip joint more stable and less likely to dislocate.
Metal-on-metal implants have also been used because they avoid the complication of debris wear from implants made of plastic/polyethylene. However, recent information about the wear of certain metal-on-metal devices has raised concerns about their use. Like polyethylene, metal surfaces give off small particles of debris. In addition, metal surfaces can corrode, giving off metal ions. Metal debris (ions and particles) can enter the space around the implant, as well as enter the bloodstream. This can cause a reaction in some patients, such as pain or swelling around the hip, osteolysis, and very rarely symptoms in other parts of the body.
Although the vast majority of patients have not had any problems with metal-on-metal implants, orthopedic surgeons and the U.S. Food and Drug Administration 10 are concerned because cases have been reported in the peer-reviewed literature and through a British database in which patients have local hip symptoms (pain and swelling). In addition, there have been a very small number of cases that have had other medical concerns seemingly unrelated to the hip.
- Patients who have metal-on-metal implants should be monitored regularly for the life of the implant, and have tests to measure levels of metal particles (ions) in their blood.
Patients with these implants who have symptoms may be investigated with MRI or ultrasound scans, and patients without symptoms should have a scan if the level of metal ions in their blood is rising.
If after a joint replacement surgery you experience pain or have other, new medical concerns or issues, please talk to your doctor or orthopedic surgeon.
You should also be aware of the warning signs that could signal a problem.
What are the warning signs?
You should contact your doctor if you have:
- pain in the groin, hip or leg
- swelling at or near the hip joint
- a limp or problems walking
- grinding or clunking from the joint
These symptoms don’t necessarily mean your device is failing, but they do need investigating.
Any changes in general health should also be reported, including:
- chest pain or shortness of breath
- numbness or weakness
- changes in vision or hearing
- fatigue
- feeling cold
- weight gain
What exactly is the problem with metal-on-metal implants?
Wear and tear
All hip implants wear down over time as the ball and cup slide against each other during movements, including walking and running.
Although many people live the rest of their lives without needing a replacement implant, some people may eventually need surgery to remove or replace its components.
Data suggests that certain types of metal-on-metal implant wear down at a faster rate than other types.
As friction acts upon their surfaces, it can cause tiny metal particles to break off and enter the space around the implant.
People are thought to react differently to the presence of these metal particles, but they can trigger inflammation and discomfort in the area around the implant in some people.
If not caught early, this can cause damage and deterioration in the bone and tissue surrounding the implant and joint over time. This in turn may cause the implant to become loose and cause painful symptoms, meaning further surgery is required.
Metal ions in the bloodstream
Some news coverage has focused on the Medicines and Healthcare products Regulatory Agency’s recommendation to check for the presence of metal ions in the bloodstream.
Ions are electrically charged molecules. Levels of ions in the bloodstream, particularly of the cobalt and chromium used in the surface of the implants, may therefore indicate how much wear there is to the artificial hip.
These ions in the blood are not blood poisoning and don’t lead to sepsis, which is an entirely different type of illness. Talk of this in some of the news reports is very misleading and completely wrong.
There has been no definitive link between ions from metal-on-metal implants and illness, although there has been a small number of cases in which high levels of metal ions in the bloodstream have been associated with symptoms or illnesses elsewhere in the body, including effects on the heart, nervous system and thyroid gland.
Is there a way to determine ahead of time if I might have a reaction to the metal in the metal-on-metal hip implant system?
Currently there is no widely accepted test to predict if you will develop a reaction to the metal from a hip system, and there is insufficient evidence to support using a skin patch test to determine your sensitivity to a metal-on-metal hip implant. If, however, you have a known sensitivity to metal, it is important to share that information with your surgeon.
Are there any ways to prevent the metal from reaching the joint and bloodstream if I get a metal-on-metal hip implant?
No. All artificial hips require one component to slide against another component and it is inevitable that material at the surfaces will wear as they interact. In metal-on-metal hip implants, some tiny metal particles and metal ions are released into the joint space and metal ions can potentially enter the bloodstream. Certain characteristics may place patients at risk for increased wear and metal ion production, and these patients will need closer follow-up after implantation. However, how a patient reacts to the metal is variable.
Which patients should not have a metal-on-metal hip implant system implanted?
Each type of hip implant system has its own set of benefits and risks. Metal-on-metal hip implant systems are not for everyone. You should discuss your situation with your orthopedic surgeon to determine whether you are a candidate or not. In general, metal-on-metal hip systems are not meant to be implanted in patients:
- Who have kidney problems
- Who have a known allergy or sensitivity to metals
- Who have a suppressed immune system
- Who are currently receiving high doses of corticosteroids such as prednisone
- Who are women of childbearing age
In addition, people with smaller body frames may be at increased risk for adverse events and device failure.
Why are women of child-bearing age not good candidates for metal-on-metal hip implants?
As discussed above, recent information shows that metal ions can leave the artificial joint and enter the bloodstream. It is not known how long they remain in blood or other organs of the body.
Some metallic ions may cross the barrier from mother to fetus through the placenta. It is not known if the amount of ions is great enough to have any effect on the growing fetus or if the presence of metal ions in the mother’s bloodstream will have any effect on future pregnancies.
For this reason, it is recommended that younger women who need hip replacement surgery consider implant options other than metal-on-metal.
With the risk of adverse reactions to metal-on-metal hip implant systems, why are these devices still being offered to patients?
It is known that every different type of hip implant system has its own set of risks as well as its own set of benefits. FDA’s assessment of medical devices such as metal-on-metal hip implants is based on a risk-benefit ratio with the data available. Metal-on-metal hip implants overall have been shown to provide significant benefits (e.g., high survivorship) in certain patient populations. Although the exact prevalence of adverse reactions to metal debris is not known, current experience leads us to consider the adverse outcomes to be relatively low or equal (with some designs) to other types of hip implants. Thus, for many patients, currently available information supports a favorable risk-benefit ratio.
The orthopedic surgeon should assess the patient’s individual needs and should avoid using metal-on-metal hip implants in patients where the risks outweigh the benefits.
What symptoms might a metal-on-metal hip implant cause?
Symptoms may include hip/groin pain, local swelling, numbness or changes in your ability to walk. There are many reasons a patient with a metal-on-metal hip implant may experience such symptoms and it is important that you contact your surgeon to help determine why you are having them.
Are there other medical effects that can occur with my metal-on-metal hip implant system?
Metal-on-metal hip implants, like other types of hip implants, are known to have adverse events, including infection and joint dislocation. There are some case reports of the metal particles causing a reaction around the joint, leading to deterioration of the tissue around the joint, loosening of the implant, and failure of the device, as well as some of the symptoms described above. In addition, some metal ions from the implant may enter into the bloodstream. There have been a few recent case reports of patients with metal-on-metal hip implants developing a reaction to these ions and experiencing medical problems that might have been related to their implants, including effects on the nervous system, heart, and thyroid gland.
What are my chances of developing a reaction to my metal-on-metal hip implant and having these types of medical problems?
Although current data suggests that these events are rare, it is currently unknown how often they occur in patients with metal-on-metal hip implants.
Part of the difficulty in answering this question is that individuals vary in how they react to metal ions in their bodies. For example, a reaction may develop in Patient A in response to a very small amount of metal, whereas Patient B may be able to tolerate a much larger amount before a reaction develops.
What should I do if I am experiencing adverse events associated with my metal-on-metal hip implant?
If you are experiencing hip/groin pain, difficulty walking or a worsening of your previous symptoms, you should make an appointment to see your orthopedic surgeon for further evaluation of your implant. Your orthopedic surgeon may wish to perform a physical exam and an evaluation based on your symptoms.
If you experience any new symptoms or medical conditions in your body other than at your hip, you should report these to your primary physician and remind them that you have a metal-on-metal hip implant system during their evaluation.
What should I do if I am not experiencing adverse events associated with my metal-on-metal hip implant?
If you are not having any symptoms and your orthopedic surgeon believes the metal-on-metal hip implant is functioning appropriately, there are no data to support the need for additional tests. You should continue to follow-up with your orthopedic surgeon for periodic examinations.
What should I discuss with my other healthcare providers including my general internist or family practice doctor?
There are rare case reports of patients with metal-on-metal hip implants who experienced medical problems in areas of the body away from their hip implant. This may have resulted from the metal ions released by the metal-on-metal hip implant.
If you see a healthcare provider for the evaluation of any new or worsening symptoms outside the hip/groin area, including symptoms related to your heart, nervous system, or thyroid gland, it is important that you tell that clinician of your metal-on-metal hip implant. This information may affect the types of tests that are ordered to further evaluate the cause of your symptoms.
When would a hip revision surgery be needed?
There are multiple reasons why a surgeon may recommend a device revision (a surgical procedure where your implant is removed and another put in its place). Many of these reasons, including infection, dislocation, and device fracture, apply to any type of hip implant. Your surgeon might also consider revision if you develop evidence of local or systemic reactions to the metal from your hip implant. In that case, the surgeon will take several factors into account in considering if and when a revision surgery is advisable.
What are the risks of revision surgery?
Any surgical procedure, including revision surgery, has risks associated with it, including reaction to the anesthesia, infection, bleeding, and blood clots. The revision surgery may be more difficult if you had a local reaction to the implant that may have affected your soft tissue and/or bone quality.
What does it mean when I see that a hip implant system has been “recalled?”
A hip system may be recalled by the manufacturer for a number of reasons. If your device is recalled, this does not necessarily mean that the device needs to be removed and replaced. In some cases, the recall just calls for different or more frequent monitoring. It is important to discuss the reason for the recall with your surgeon to determine the most appropriate course of action. If you are unsure if your hip implant was recalled, consult with your orthopedic surgeon. Additional information on the recall can be obtained from the manufacturer.
Hip replacement procedure
The traditional surgical approach to total hip replacement uses a single, long incision to view and access the hip joint. A variation of this approach is a minimally invasive procedure in which one or two shorter incisions are used. In minimally invasive surgery, a smaller surgical incision is used and fewer muscles around the hip are cut or detached. The goal of using shorter incisions is to reduce pain and speed recovery. Unlike traditional total hip replacement, the minimally invasive technique is not suitable for all patients. Despite this difference, however, both traditional hip replacement surgery and minimally invasive surgery are technically demanding and have better outcomes if the surgeon and operating team have considerable experience.
Your orthopedic surgeon will discuss different surgical options with you.
The surgical procedure takes a few hours. During any hip replacement surgery, the damaged bone is cut and removed, along with some soft tissues.
Your orthopedic surgeon will remove the damaged cartilage and bone and then position new metal, plastic, or ceramic implants to restore the alignment and function of your hip.
After surgery, you will be moved to the recovery room where you will remain for several hours while your recovery from anesthesia is monitored. After you wake up, you will be taken to your hospital room.
How the operation is carried out
Once you’ve been anaesthetised, the surgeon removes the existing hip joint completely. The upper part of the thigh bone (femur) is removed and the natural socket for the head of the femur is hollowed out.
A socket is fitted into the hollow in the pelvis. A short, angled metal shaft (the stem) with a smooth ball on its upper end (to fit into the socket) is placed into the hollow of the thigh bone. The cup and the stem may be pressed into place or fixed with acrylic cement.
Metal-on-metal hip resurfacing is carried out in a similar way. The main difference is that less of the bone is removed from the femur as only the joint surfaces are replaced with metal inserts.
Materials
The prosthetic parts can be cemented or uncemented:
- cemented parts are secured to healthy bone using acrylic cement
- uncemented parts are made from material that has a rough surface; this allows the bone to grow on to it, holding it in place
Most prosthetic parts are produced using high-density polythene for the socket, titanium alloys for the shaft and sometimes a separate ball made of an alloy of cobalt, chromium and molybdenum.
Some surgeons use a metal ball and socket and in some cases ceramic parts are used, which don’t wear as quickly as plastic.
Traditional Hip Replacement
To perform a traditional hip replacement:
- A 10- to 12-inch incision is made on the side of the hip. The muscles are split or detached from the hip, allowing the hip to be dislocated and fully viewed by the surgical team.
- The damaged femoral head is removed and replaced with a metal stem that is placed into the hollow center of the femur, then a metal or ceramic ball is placed on the upper part of the stem. This ball replaces the damaged femoral head that was removed.
- The damaged cartilage surface of the socket (acetabulum) is removed and replaced with a metal socket. Screws or cement are sometimes used to hold the socket in place.
- A plastic, ceramic or metal spacer is inserted between the new ball and the socket to allow for a smooth gliding surface.
Figure 11. X-rays before and after total hip replacement – Note: In this case, non-cemented components were used.
Minimally Invasive Total Hip Replacement
In minimally invasive total hip replacement, the surgical procedure is similar, but there is less cutting of the tissue surrounding the hip. The artificial implants used are the same as those used for traditional hip replacement. However, specially designed surgical instruments are needed to prepare the socket and femur and to place the implants properly.
Minimally invasive total hip replacement can be performed with either one or two small incisions. Smaller incisions allow for less tissue disturbance.
- Single-incision surgery. In this type of minimally invasive hip replacement, the surgeon makes a single incision that usually measures from 3 to 6 inches. The length of the incision depends on the size of the patient and the difficulty of the procedure.
- The incision is usually placed over the outside of the hip. The muscles and tendons are split or detached from the hip, but to a lesser extent than in traditional hip replacement surgery. They are routinely repaired after the surgeon places the implants. This encourages healing and helps prevent dislocation of the hip.
- Two-incision surgery. In this type of minimally invasive hip replacement, the surgeon makes two small incisions:
- A 2- to 3-inch incision over the groin for placement of the socket, and
- A 1- to 2-inch incision over the buttock for placement of the femoral stem.
- To perform the two-incision procedure, the surgeon may need guidance from x-rays. It may take longer to perform the two-incision surgery than it does to perform traditional hip replacement surgery.
The hospital stay after minimally invasive surgery is similar in length to the stay after traditional hip replacement surgery–ranging from 1 to 4 days. Physical rehabilitation is a critical component of recovery. Your surgeon or a physical therapist will provide you with specific exercises to help increase your range of motion and restore your strength.
Candidates for Minimally Invasive Total Hip Replacement
Minimally invasive total hip replacement is not suitable for all patients. Your doctor will conduct a comprehensive evaluation and consider several factors before determining if the procedure is an option for you.
In general, candidates for minimal incision procedures are thinner, younger, healthier, and more motivated to participate in the rehabilitation process, compared with patients who undergo the traditional surgery.
Minimally invasive techniques are less suitable for patients who are overweight or who have already undergone other hip surgeries. In addition, patients who have a significant deformity of the hip joint, those who are very muscular, and those with health problems that may slow wound healing may be at a higher risk for problems from minimally invasive total hip replacement.
Summary of Minimally invasive total hip replacement
Minimally invasive and small incision total hip replacement surgery is an evolving area and more research is needed on the long-term function and durability of the implants.
The benefits of minimally invasive hip replacement have been reported to include less damage to soft tissues, leading to a quicker, less painful recovery and more rapid return to normal activities. Current evidence suggests that the long-term benefits of minimally invasive surgery do not differ from those of hip replacement performed with the traditional approach.
Like all surgery, minimally invasive surgery has a risk of complications. These complications include nerve and artery injuries, wound healing problems, infection, fracture of the femur, and errors in positioning the prosthetic hip implants.
Like traditional hip replacement surgery, minimally invasive surgery should be performed by a well-trained, highly experienced orthopedic surgeon. Your orthopaedic surgeon can talk to you about his or her experience with minimally invasive hip replacement surgery, and the possible risks and benefits of the techniques for your individual treatment.
How long does hip replacement surgery take?
The duration of a hip replacement varies a lot between patients and the orthopedic surgeon skills and experience. In general, the surgery usually takes around 60-90 minutes to complete.
It’s vitally important you choose a specialist who performs hip replacement regularly and can discuss their results with you.
This is even more important if you’re having a second or subsequent hip replacement (revision surgery), which is more difficult to perform.
Revision Total Hip Replacement
Total hip replacement is one of the most successful procedures in all of medicine. In the vast majority of cases, total hip replacement enables people to live more active lives without debilitating hip pain. Over time, however, a hip replacement can fail for a variety of reasons.
When this occurs, your doctor may recommend that you have a second operation to remove some or all of the parts of the original prosthesis and replace them with new ones. This procedure is called revision total hip replacement.
Although both procedures have the same goals—to relieve pain and improve function and quality of life—revision surgery is different than primary total hip replacement. Revision hip replacement is a longer, more complex procedure. It requires extensive planning, as well as the use of specialized implants and tools, in order to achieve a good result.
There are different types of revision surgery. In some cases, only some components of the prosthesis need to be revised. In other cases, the whole prosthesis needs to be removed or replaced and the bone around the hip needs to be rebuilt with augments (metal pieces that substitute for missing bone) or bone graft.
Damage to bone and soft tissue around the hip may make it difficult for the doctor to use standard primary hip implants for revision hip replacement. In most revisions, the doctor will use specialized implants that are designed to compensate for the damaged bone and soft tissue.
When revision total hip replacement is recommended
Hip replacement Loosening
The most common problem that can arise as a result of a hip replacement is loosening of the joint, which causes pain and feeling that the joint is unstable. This happens in around 10% of cases. Loosening of the joint can occur at any time, but it normally occurs 10-15 years after the original surgery was performed.
In order for a total hip replacement to function properly, an implant must remain firmly attached to the bone. During the initial surgery, the hip replacement components were either cemented into place or were “press fit” into the bone to allow bone to grow onto them. Sometimes, however, bone may fail to grow onto press-fit components. In addition, cemented or press-fit components that were once firmly fixed to the bone can eventually loosen, resulting in a painful hip.
The cause of loosening is not always clear, but repetitive high-impact activities, excessive body weight, and wear of the plastic liner between the ball and the metal cup are all factors that may contribute.
Implant Wear and Tear
Another common complication of hip replacement surgery is wear and tear of the artificial sockets. Particles that have worn off the artificial joint surfaces can be absorbed by surrounding tissue, causing loosening of the joint.
If wear or loosening is noticed on X-ray, your surgeon may request regular X-rays. Depending on the severity of the problem, you may be advised to have further surgery.
There have been reports about metal-on-metal implants wearing sooner than expected and causing complications. See Metal-on-Metal Implants Precautions above.
In addition, patients who are younger when they undergo the initial hip replacement may “outlive” the life expectancy of their artificial hip. For these patients, there is a higher long-term risk that revision surgery will be needed due to loosening or wear.
In some cases, tiny particles that wear off the cup’s plastic liner accumulate around the hip joint and are attacked by the body’s immune system. This immune response also attacks the healthy bone around the implant, leading to a condition called osteolysis. In osteolysis, the bone around the implant deteriorates, making the implant loose or unstable.
Fortunately, plastics have improved greatly over the years, so plastic wear and osteolysis occur less frequently today than they did with earlier generations of implants.
Infection
Infection is a potential complication of any surgical procedure, including total hip replacement. Infection occurs when bacteria attach in and around the surface of the prosthesis. Infection may occur while you are in the hospital or after you go home. It may even occur years later.
If a total hip replacement becomes infected, it can be painful and the implant may begin to lose its attachment to the bone. Even if the implant remains properly fixed to the bone, there may still be pain, instability, and drainage from the infection. Because bacteria cannot be easily eliminated from a joint replacement with antibiotics alone, revision surgery is usually necessary.
Revision surgery for infection can be done in different ways. To determine which procedure is best for you, your doctor will consider a number of factors, including:
- The type of bacteria
- The duration and severity of the infection
- Your preference for a specific treatment
Debridement. In this procedure, your doctor will open up your hip, wash out the bacteria, and exchange the ball and plastic liner. The metal implants that are firmly attached to the bone are left in place. After debridement, you will receive intravenous antibiotics for several weeks to help cure the infection.
Staged surgery. In some cases, the implants must be completely removed. If the implants are removed to treat the infection, your doctor will usually perform the revision in two separate surgeries.
In the first surgery, your doctor will remove the implants and place a temporary cement spacer in your hip. This spacer is treated with antibiotics to help fight the infection and will remain in your hip for several weeks. During this time, you will also receive intravenous antibiotics.
When the infection has been cleared, your doctor will perform a second surgery to remove the antibiotic spacer and insert a new prosthesis. In general, removing the implant leads to a higher chance of curing the infection, but is associated with a longer recovery.
In some cases, your doctor may be able to remove the implants, wash out the hip, and place a new prosthesis all in the same operation. This procedure, which is called a one-stage exchange, may be appropriate in limited situations.
Recurrent Dislocation
In around 3% of cases the hip joint can come out of its socket. This is most likely to occur in the first few months after surgery when the hip is still healing.
A hip replacement has a ball-and-socket structure like that of your natural hip. For a hip replacement to work well, the ball must remain inside the socket. Trauma or certain hip positions can sometimes cause the ball to become dislodged from the socket. This is called a “hip dislocation.” If you experience recurrent hip dislocations, you may need revision surgery to better align your hip joint or to insert a special implant designed to prevent dislocations.
Fracture
A periprosthetic fracture is a broken bone that occurs around the components of an implant. These fractures are most often the result of a fall, and often require revision surgery. To determine whether a revision is needed, your doctor will consider several factors, including the amount of remaining bone, whether your implant is loose, and the location of the fracture.
In rare circumstances, an implant itself can break. This also requires revision surgery.
Reaction to Metal Ions and Allergy to Metal
Over time, the metals used in implants can break down or wear, causing tiny particles to fall off the device into the space around the implant. This is more common with “metal-on-metal” devices, in which both the ball and socket components are made of metal. In some patients, sensitivity to the metal ions in these particles can result in damage to the bone and soft tissues around the hip and lead to the need for revision surgery.
In very rare cases, a patient allergy to the metal used in implants may cause pain around the site of the implant. There is no definitive agreement among doctors regarding metal allergy in this setting, however, and more studies are needed.
Other Factors
The likelihood of needing revision hip replacement is also impacted by individual differences among patients. For example, patients who are younger and more active are more likely to experience issues related to implant wear. Patients who have certain medical conditions, such as obesity or diabetes, and those who have had certain surgical procedures in the past, are more likely to experience infection or implant failure.
Long-Term Outcomes
The vast majority of patients who undergo revision surgery experience favorable long-term outcomes. This includes relief from pain, increased stability, and better function. Complete pain relief and restoration of function are not always achievable, however, and some patients may still experience some pain or dysfunction following revision surgery.
Hip replacement surgery recovery
The success of your hip replacement surgery will depend in large measure on how well you follow your orthopedic surgeon’s instructions regarding home care during the first few weeks after surgery.
Your hospital stay will typically last from 1 to 4 days, depending on the speed of your recovery. Before you are discharged from the hospital, you will need to accomplish several goals, such as:
- Getting in and out of bed by yourself.
- Having acceptable pain control.
- Being able to eat, drink, and use the bathroom.
- Walking with an assistive device (a cane, walker, or crutches) on a level surface and being able to climb up and down two or three stairs.
- Being able to perform the prescribed home exercises.
- Understanding any hip precautions you may have been given to prevent injury and ensure proper healing.
If you are not yet able to accomplish these goals, it may be unsafe for you to go directly home after discharge. If this is the case, you may be temporarily transferred to a rehabilitation or skilled nursing center.
When you are discharged, your healthcare team will provide you with information to support your recovery at home. Although the complication rate after total hip replacement is low, when complications occur they can prolong or limit full recovery. Hospital staff will discuss possible complications, and review with you the warning signs of an infection or a blood clot.
Wound Care
You may have stitches or staples running along your wound or a suture beneath your skin. The stitches or staples will be removed approximately 2 weeks after surgery.
Avoid getting the wound wet until it has thoroughly sealed and dried. You may continue to bandage the wound to prevent irritation from clothing or support stockings.
Diet
Some loss of appetite is common for several weeks after surgery. A balanced diet, often with an iron supplement, is important to promote proper tissue healing and restore muscle strength. Be sure to drink plenty of fluids.
Activity
Exercise is a critical component of home care, particularly during the first few weeks after surgery. You should be able to resume most normal light activities of daily living within 3 to 6 weeks following surgery. Some discomfort with activity and at night is common for several weeks.
Your activity program should include:
- A graduated walking program to slowly increase your mobility, initially in your home and later outside
- Resuming other normal household activities, such as sitting, standing, and climbing stairs
- Specific exercises several times a day to restore movement and strengthen your hip. You probably will be able to perform the exercises without help, but you may have a physical therapist help you at home or in a therapy center the first few weeks after surgery.
How your new hip is different
You may feel some numbness in the skin around your incision. You also may feel some stiffness, particularly with excessive bending. These differences often diminish with time, and most patients find these are minor compared with the pain and limited function they experienced prior to surgery.
Your new hip may activate metal detectors required for security in airports and some buildings. Tell the security agent about your hip replacement if the alarm is activated. You may ask your orthopedic surgeon for a card confirming that you have an artificial hip.
Protecting your hip replacement
There are many things you can do to protect your hip replacement and extend the life of your hip implant.
- Participate in a regular light exercise program to maintain proper strength and mobility of your new hip.
- Take special precautions to avoid falls and injuries. If you break a bone in your leg, you may require more surgery.
- Make sure your dentist knows that you have a hip replacement. Talk with your orthopedic surgeon about whether you need to take antibiotics prior to dental procedures.
- See your orthopedic surgeon periodically for routine follow-up examinations and x-rays, even if your hip replacement seems to be doing fine.
Hip replacement recovery time
Recovery times can vary depending on the individual and type of surgery carried out. It’s important to follow the advice your doctor gives you on looking after your hip. In general, your doctor will encourage you to use your “new” joint shortly after your operation. Although it may be challenging at times, following your doctor’s instructions will speed your recovery.
The rehabilitation process after surgery can be a demanding time and requires commitment. You may also be enrolled on an exercise programme that’s designed to help you regain and then improve the use of your new hip joint.
Most patients will experience some temporary pain in the replaced joint because the surrounding muscles are weak from inactivity, the body is adjusting to the new joint, and the tissues are healing. This pain should resolve in a few months.
Exercise is an important part of the recovery process. Your doctor or physical therapist will provide you with specific exercises to help restore movement and strengthen the joint.
The majority of patients are able to perform daily activities more easily after joint replacement surgery. Most people can expect their joint replacement to last for many years, providing them with an improved quality of life that includes less pain, along with improved motion and strength that would not have been possible otherwise.
For the first four to six weeks after the operation you’ll need a walking aid, such as crutches, to help support you.
Most people are able to resume normal activities within two to three months but it can take up to a year before you experience the full benefits of your new hip.
If you have any questions about limitations on your activities after total joint replacement, please consult your doctor.
After surgery
After the operation, you’ll be lying flat on your back and may have a pillow between your legs to keep your hip in the correct position. You may feel hazy or groggy as you come round from the general anaesthetic. A nurse may give you oxygen (through tubes in your nose or a mask) to help you feel better.
It’s common to feel sick or vomit after you’ve been given general anesthesia. Your nurse may offer you medicine to help with sickness. You may also have a sore throat and dry mouth.
The nursing staff will monitor your condition and you’ll have a large dressing on your leg to protect the wound.
You may be allowed to have a drink about an hour after you return to the ward and, depending on your condition, you may be allowed to have something to eat.
How soon will I be up and about?
The staff will help you to get up and walk about as quickly as possible after surgery. If you’ve had minimally invasive surgery or are on an enhanced recovery programme, you may be able to walk on the same day as your operation.
Initially, you’ll feel discomfort while walking and exercising, and your legs and feet may be swollen. You may be given an injection into your abdomen to help prevent blood clots forming in your legs, and possibly a short course of antibiotics to help prevent infection.
A physiotherapist may teach you exercises to help strengthen the hip and explain what should and shouldn’t be done after the operation. They’ll teach you how to bend and sit to avoid damaging your new hip.
Going home
You’ll usually be in hospital for around three to five days, depending on the progress you make and what type of surgery you have.
If you’re generally fit and well, the surgeon may suggest an enhanced recovery programme, where you start walking on the day of the operation and are discharged within one to three days.
Recovering at home
Don’t be surprised if you feel very tired at first. You’ve had a major operation and muscles and tissues surrounding your new hip will take time to heal. Follow the advice of the surgical team and call your doctor if you have any particular worries or queries.
You may be eligible for home help and there may be aids that can help you. You may want to arrange to have someone to help you for a week or so.
The exercises your physiotherapist gives you are an important part of your recovery. It’s essential you continue with them once you’re at home. Your rehabilitation will be monitored by a physiotherapist.
How soon will the pain go away?
The pain you may have experienced before the operation should go immediately. You can expect to feel some pain as a result of the operation itself, but this won’t last for long.
How long will it be before I feel back to normal?
Generally, you should be able to stop using your crutches within four to six weeks and feel more or less normal after three months, by which time you should be able to perform all your normal activities.
It’s best to avoid extreme movements or sports where there’s a risk of falling, such as skiing or riding. Your doctor or a physiotherapist can advise you about this.
When can I drive again?
You can usually drive a car after about six weeks, subject to advice from your surgeon. It can be tricky getting in and out of your car at first. It’s best to ease yourself in backwards and swing both legs round together.
When can I go back to work?
This depends on your job, but you can usually return to work 6-12 weeks after your operation.
How will it affect my sex life?
If you were finding sex difficult before because of pain, you may find that having the operation gives your sex life a boost. Your surgeon can advise when it’s OK to have sex again.
As long as you’re careful, you should be able to have sex after six to eight weeks. Avoid vigorous sex and more extreme positions.
Will I need another new hip?
Nowadays, most hip implants last for 15 years or more. If you’re older, your new hip may last your lifetime. If you’re younger, you may need another new hip at some point.
Revision surgery is more complicated and time-consuming for the surgeon to perform than a first hip replacement and complication rates are usually higher.
It can’t be performed in every patient, but most people who can have it report success for 10 years or more.
Avoiding problems after hip replacement surgery
Recognizing the Signs of a Blood Clot
Follow your orthopedic surgeon’s instructions carefully to reduce the risk of blood clots developing during the first several weeks of your recovery. He or she may recommend that you continue taking the blood thinning medication you started in the hospital. Notify your doctor immediately if you develop any of the following warning signs.
Warning signs of blood clots. The warning signs of possible blood clot in your leg include:
- Pain in your calf and leg that is unrelated to your incision
- Tenderness or redness of your calf
- New or increasing swelling of your thigh, calf, ankle, or foot
Warning signs of pulmonary embolism. The warning signs that a blood clot has traveled to your lung include:
- Sudden shortness of breath
- Sudden onset of chest pain
- Localized chest pain with coughing
Preventing Infection
A common cause of infection following hip replacement surgery is from bacteria that enter the bloodstream during dental procedures, urinary tract infections, or skin infections.
Following surgery, patients with certain risk factors may need to take antibiotics prior to dental work, including dental cleanings, or before any surgical procedure that could allow bacteria to enter your bloodstream. Your orthopedic surgeon will discuss with you whether taking preventive antibiotics before dental procedures is needed in your situation.
Warning signs of infection. Notify your doctor immediately if you develop any of the following signs of a possible hip replacement infection:
- Persistent fever (higher than 100°F or 37.8 °C orally)
- Shaking chills
- Increasing redness, tenderness, or swelling of the hip wound
- Drainage from the hip wound
- Increasing hip pain with both activity and rest
Looking after your new hip
With care, your new hip should last well. The following advice may be given by the hospital to help you care for your new hip. However, the advice may vary based on your doctors recommendations:
- avoid bending your hip more than 90° (a right angle) during any activity
- avoid twisting your hip
- don’t swivel on the ball of your foot
- when you turn around, take small steps
- don’t apply pressure to the wound in the early stages (so try to avoid lying on your side)
- don’t cross your legs over each other
- don’t force the hip or do anything that makes your hip feel uncomfortable
- avoid low chairs and toilet seats (raised toilet seats are available)
Avoiding Falls
A fall during the first few weeks after surgery can damage your new hip and may result in a need for more surgery. Stairs are a particular hazard until your hip is strong and mobile. You should use a cane, crutches, a walker, or handrails or have someone help you until you improve your balance, flexibility, and strength.
Your orthopedic surgeon and physical therapist will help you decide which assistive aides will be required following surgery, and when those aides can safely be discontinued.
Other precautions
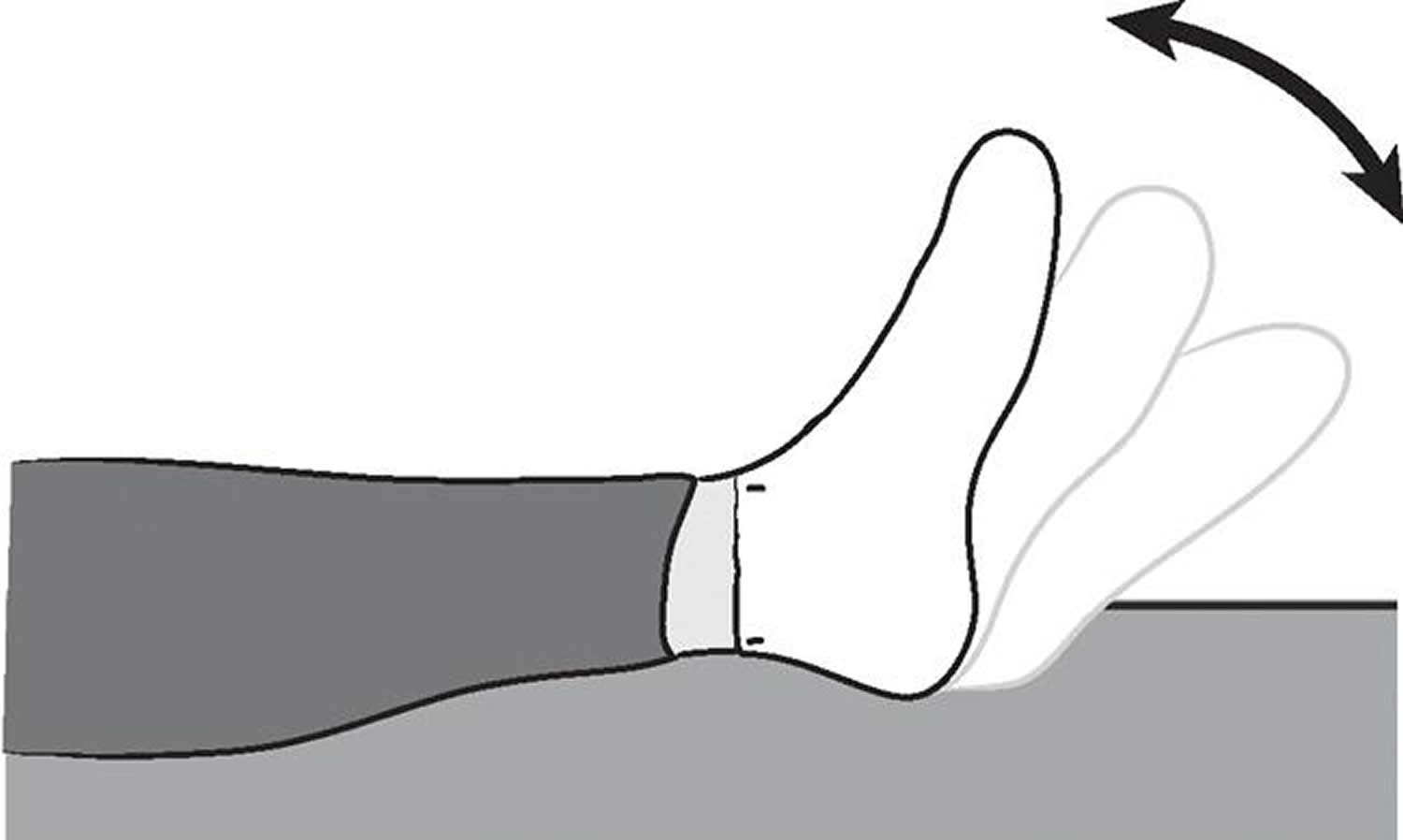
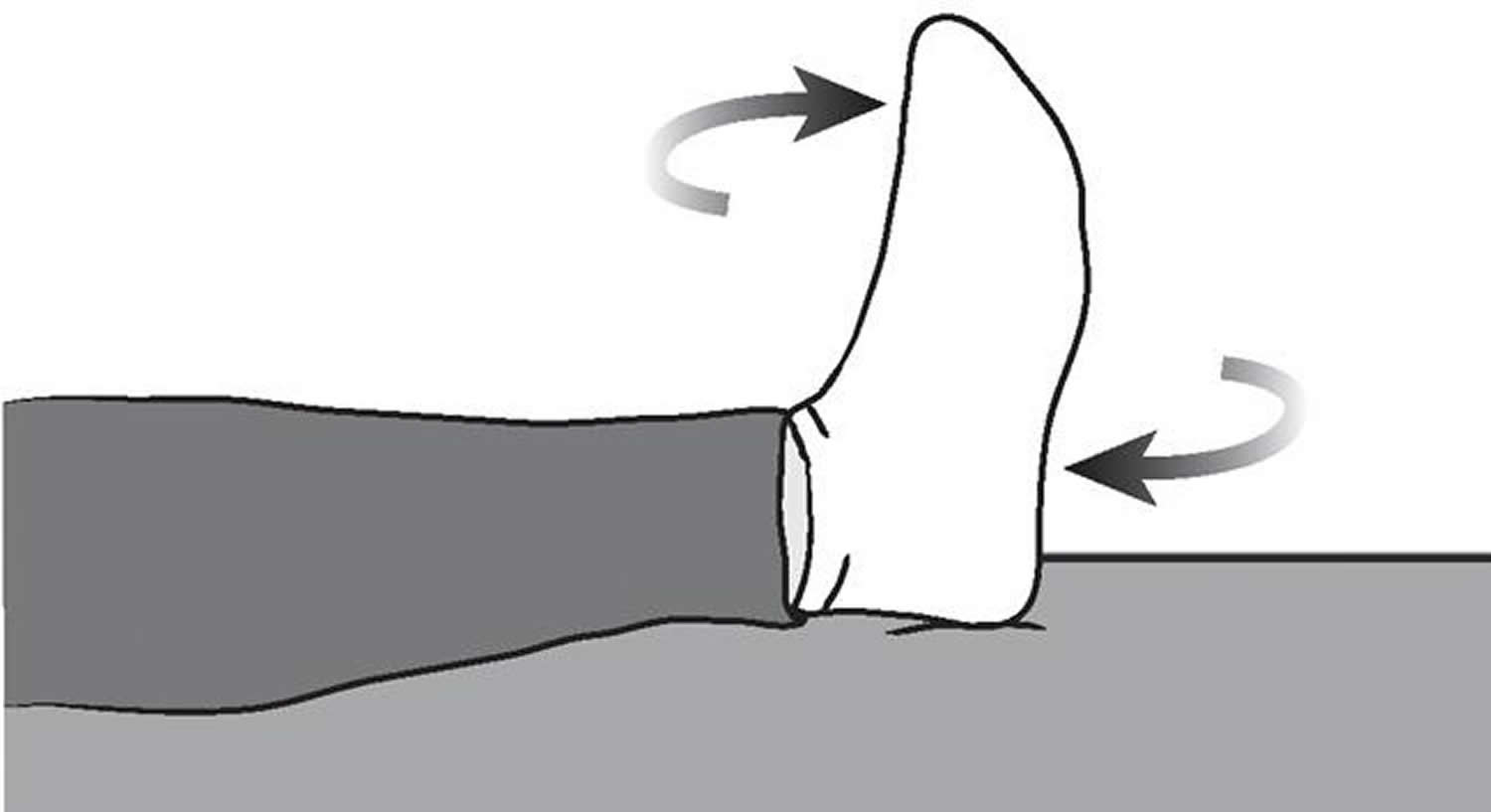
To assure proper recovery and prevent dislocation of the prosthesis, you may be asked to take special precautions when sitting, bending, or sleeping — usually for the first 6 weeks after surgery. These precautions will vary from patient to patient, depending on the surgical approach your surgeon used to perform your hip replacement.
Prior to discharge from the hospital, your surgeon and physical therapist will provide you with any specific precautions you should follow.
Total Hip Replacement Exercise Guide
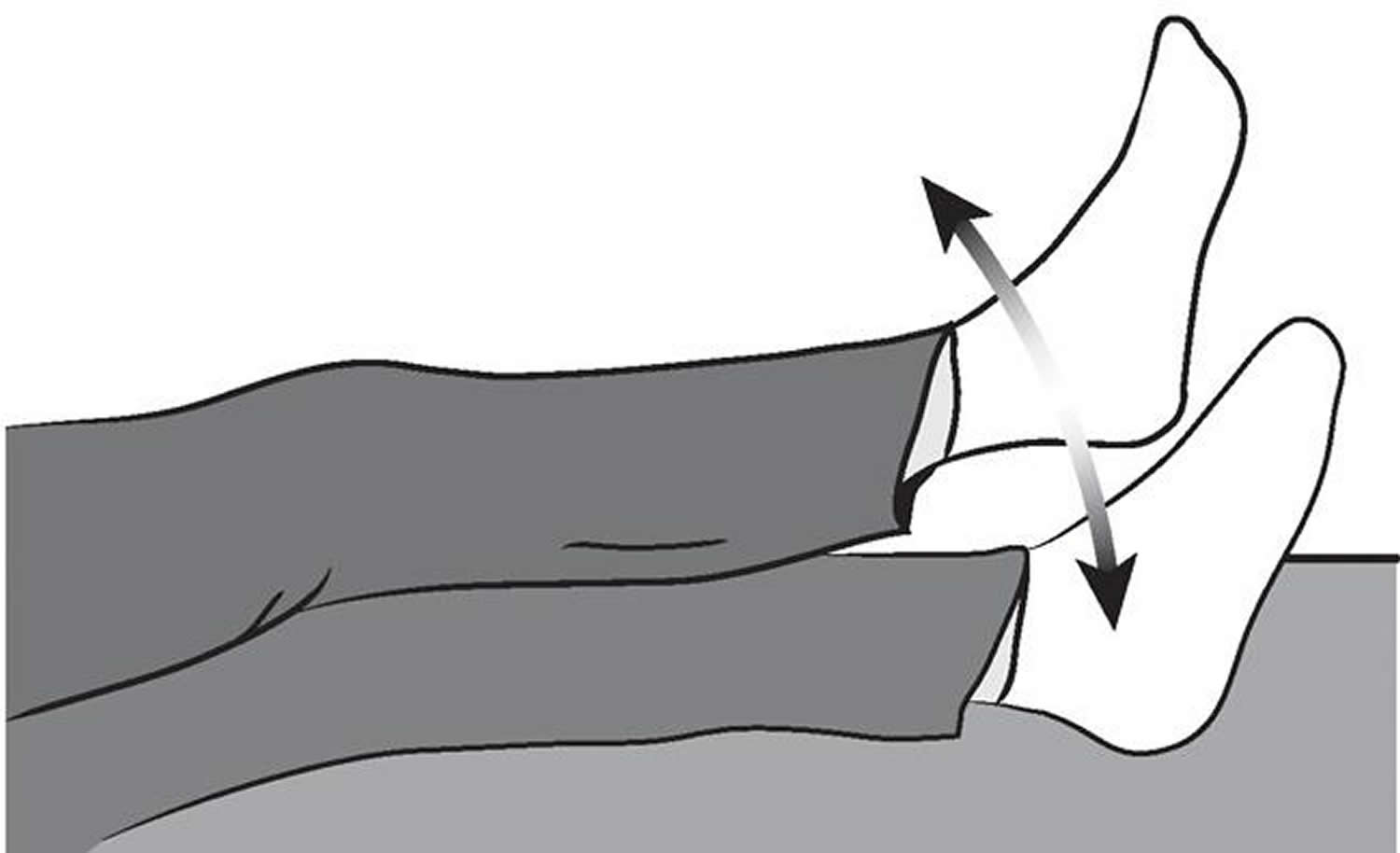
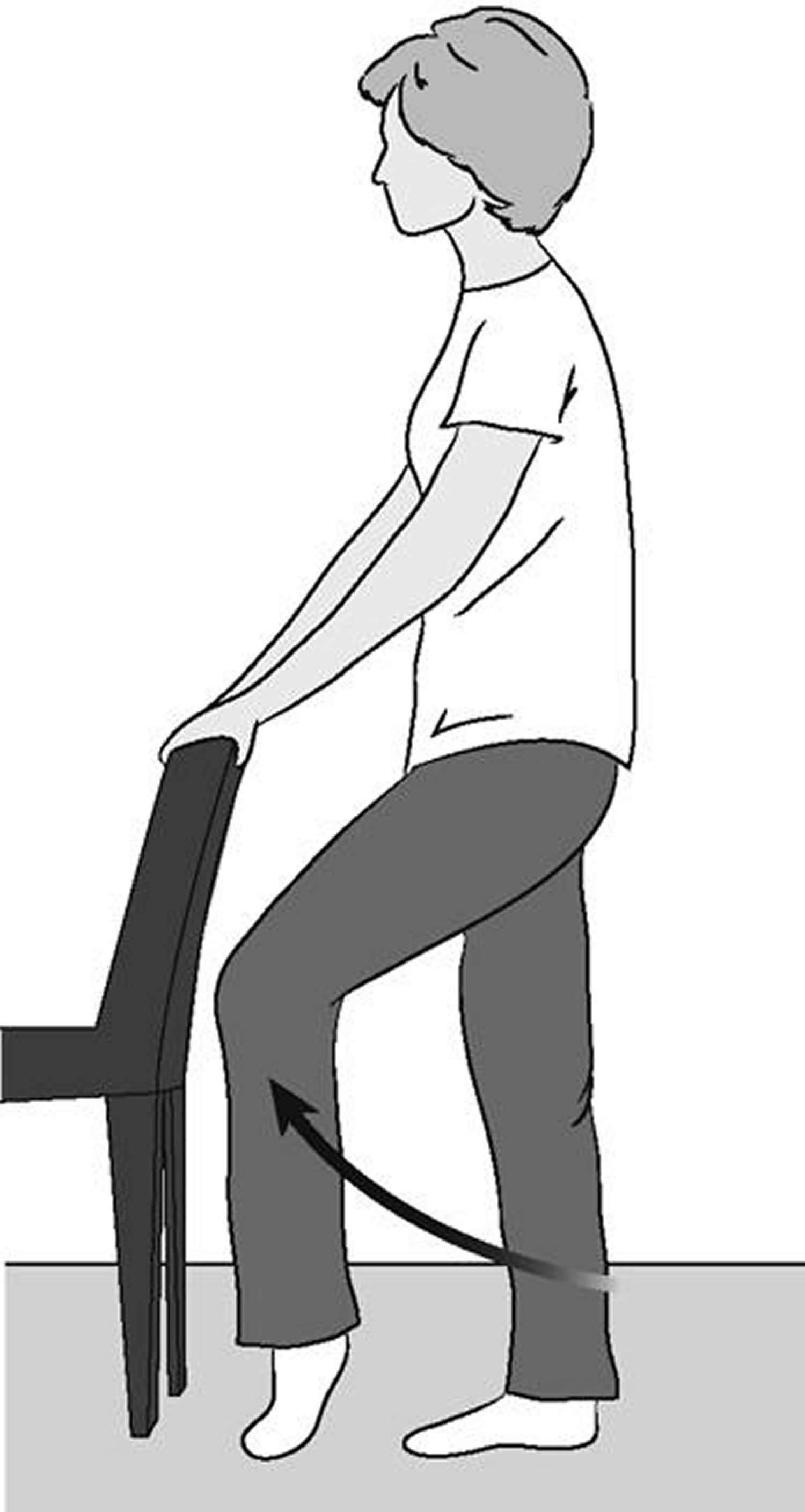
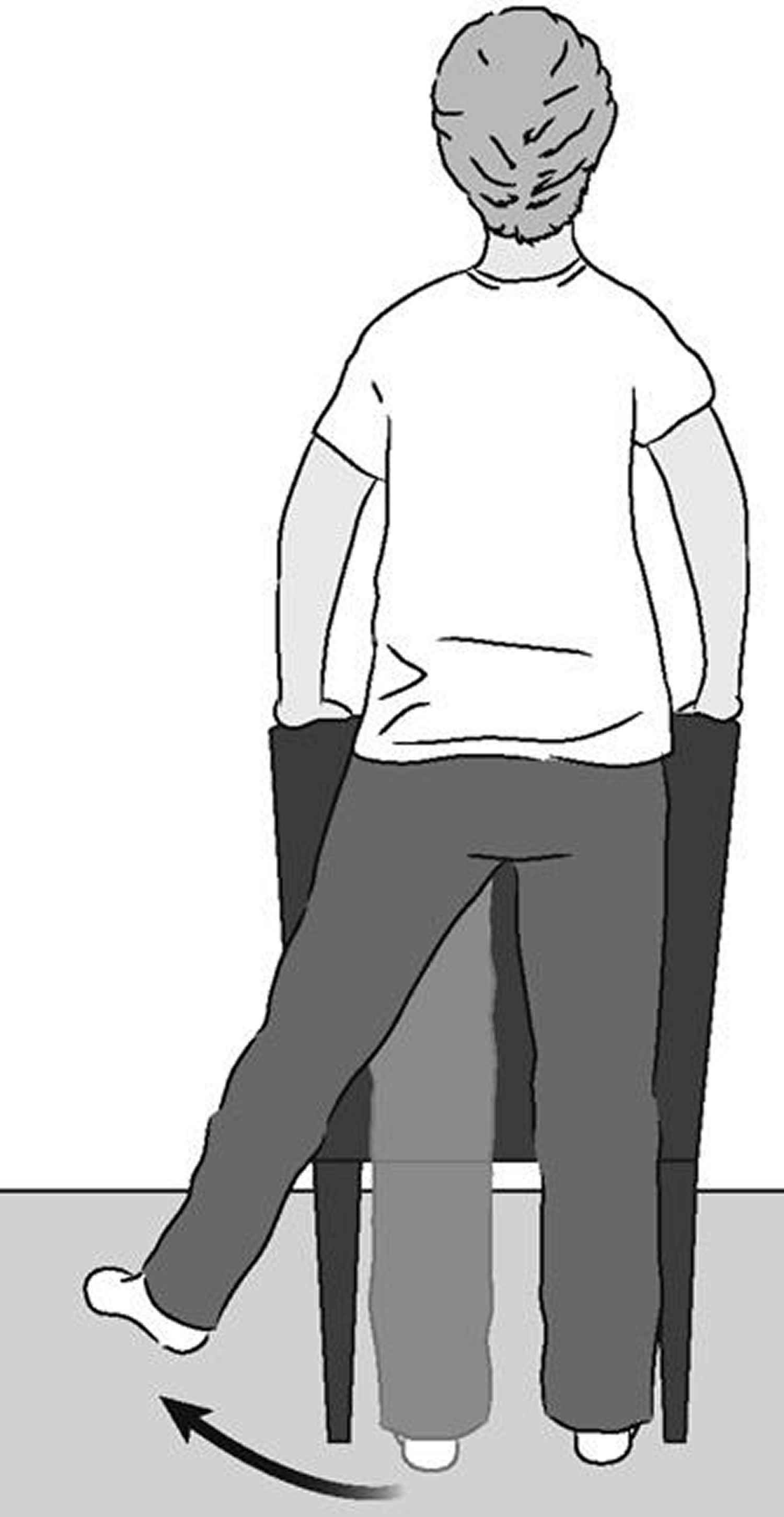
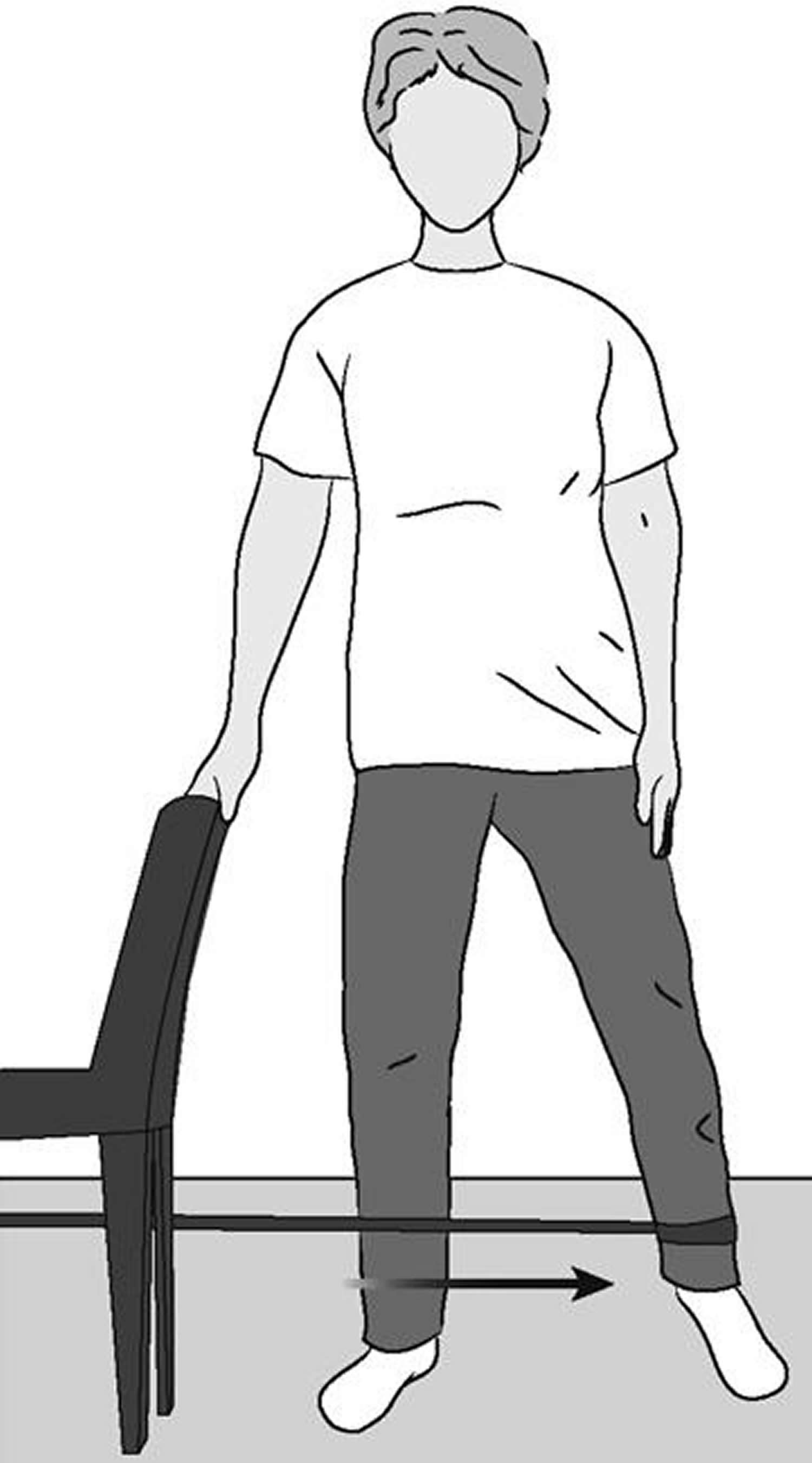
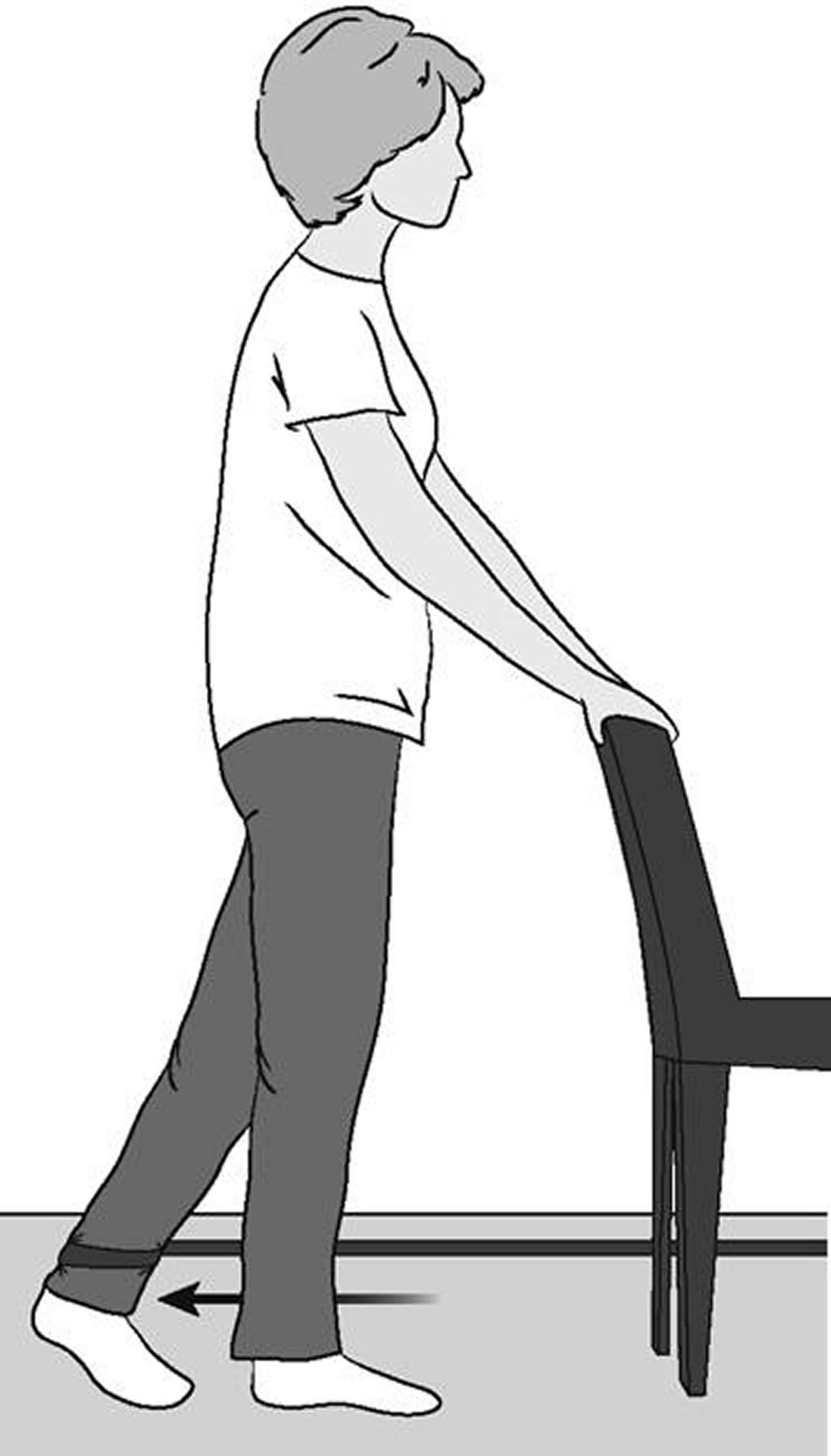
Regular exercise to restore strength and mobility to your hip and a gradual return to everyday activities are important for your full recovery after hip replacement. Your orthopedic surgeon and physical therapist may recommend that you exercise for 20 to 30 minutes, 2 or 3 times a day during your early recovery. They may suggest some of the exercises shown below.
This guide can help you better understand your exercise and activity program, supervised by your physical therapist and orthopedic surgeon. To ensure your safe recovery, be sure to check with your therapist or surgeon before performing any of the exercises shown.
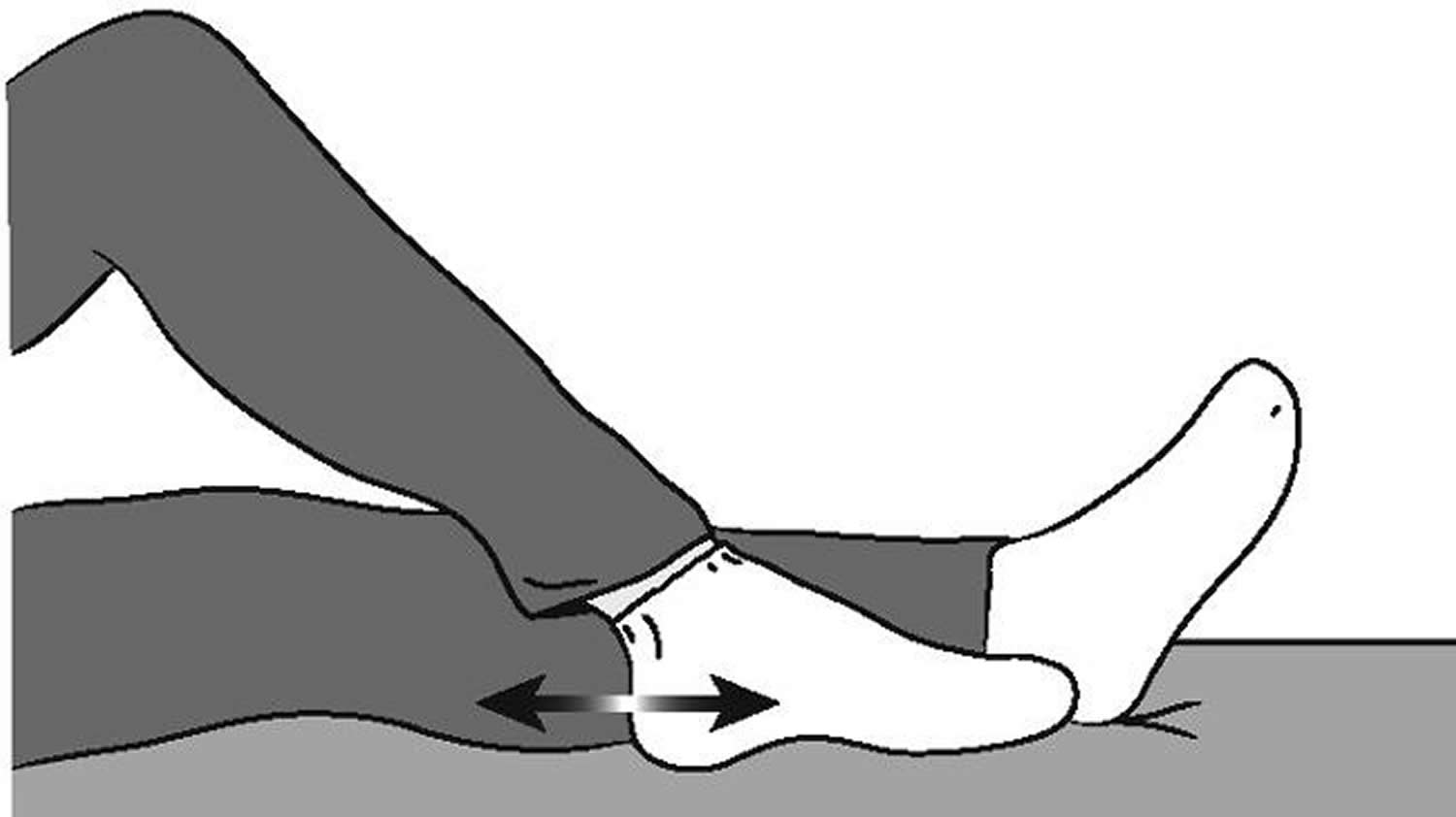
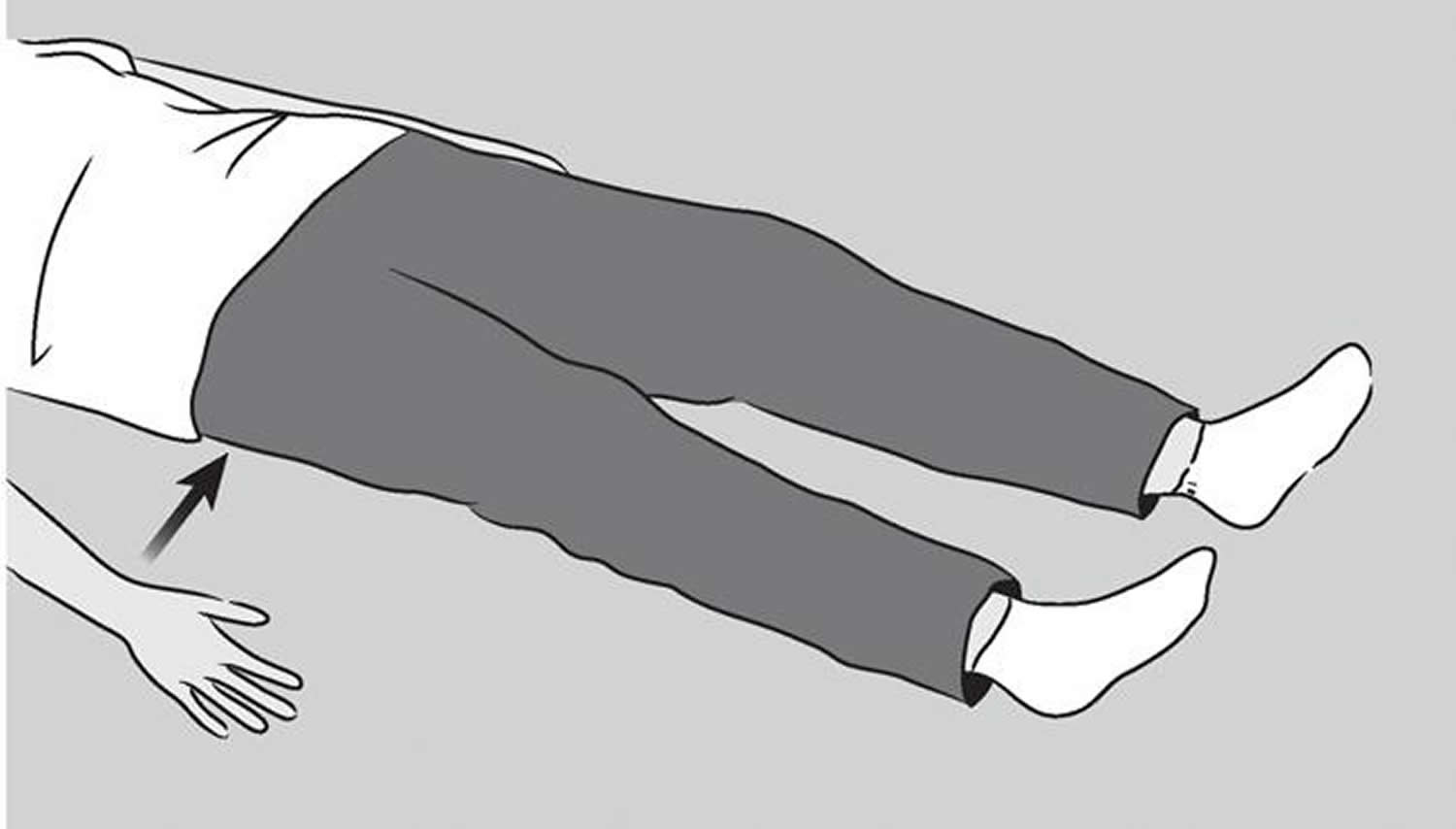
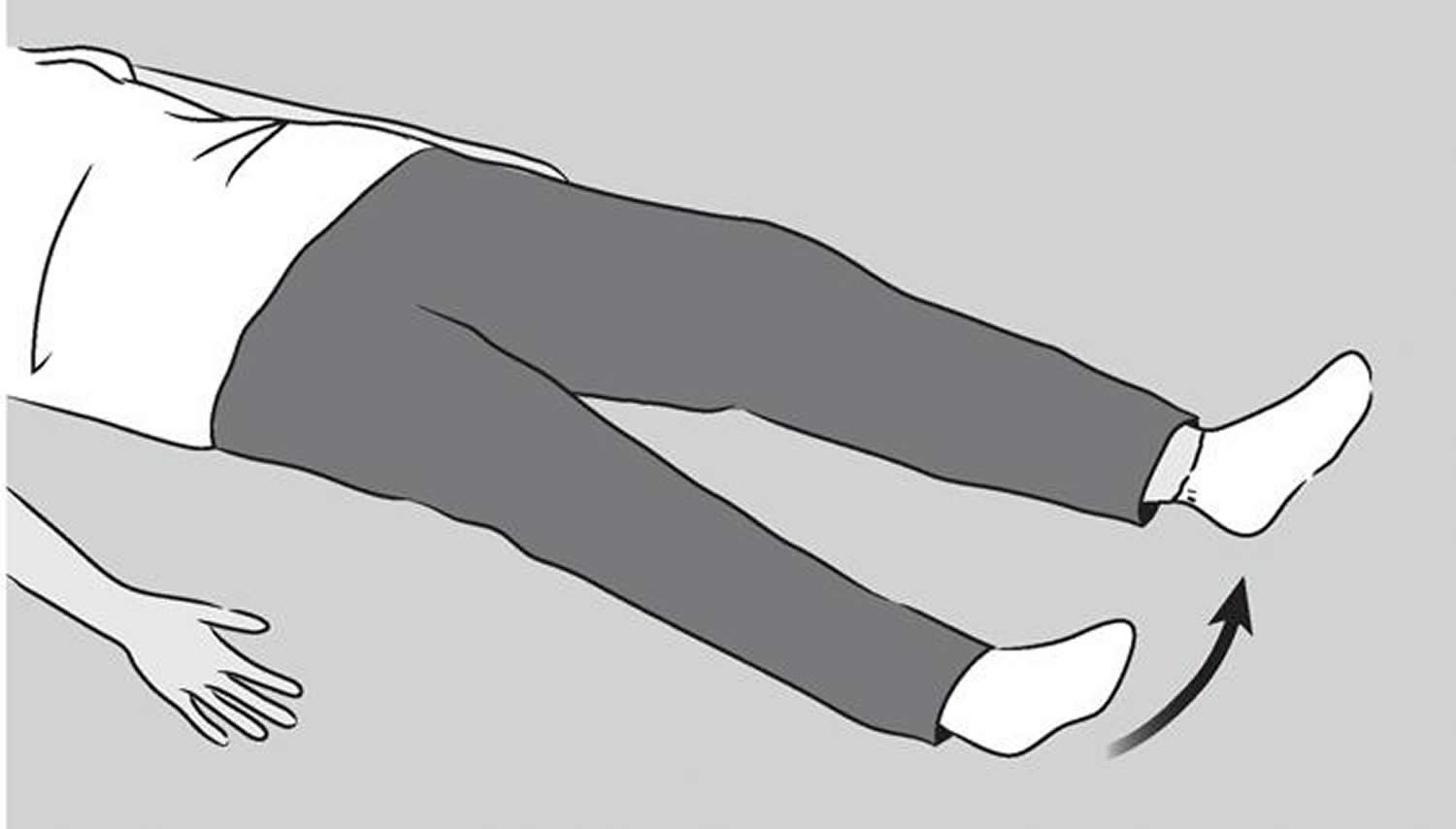
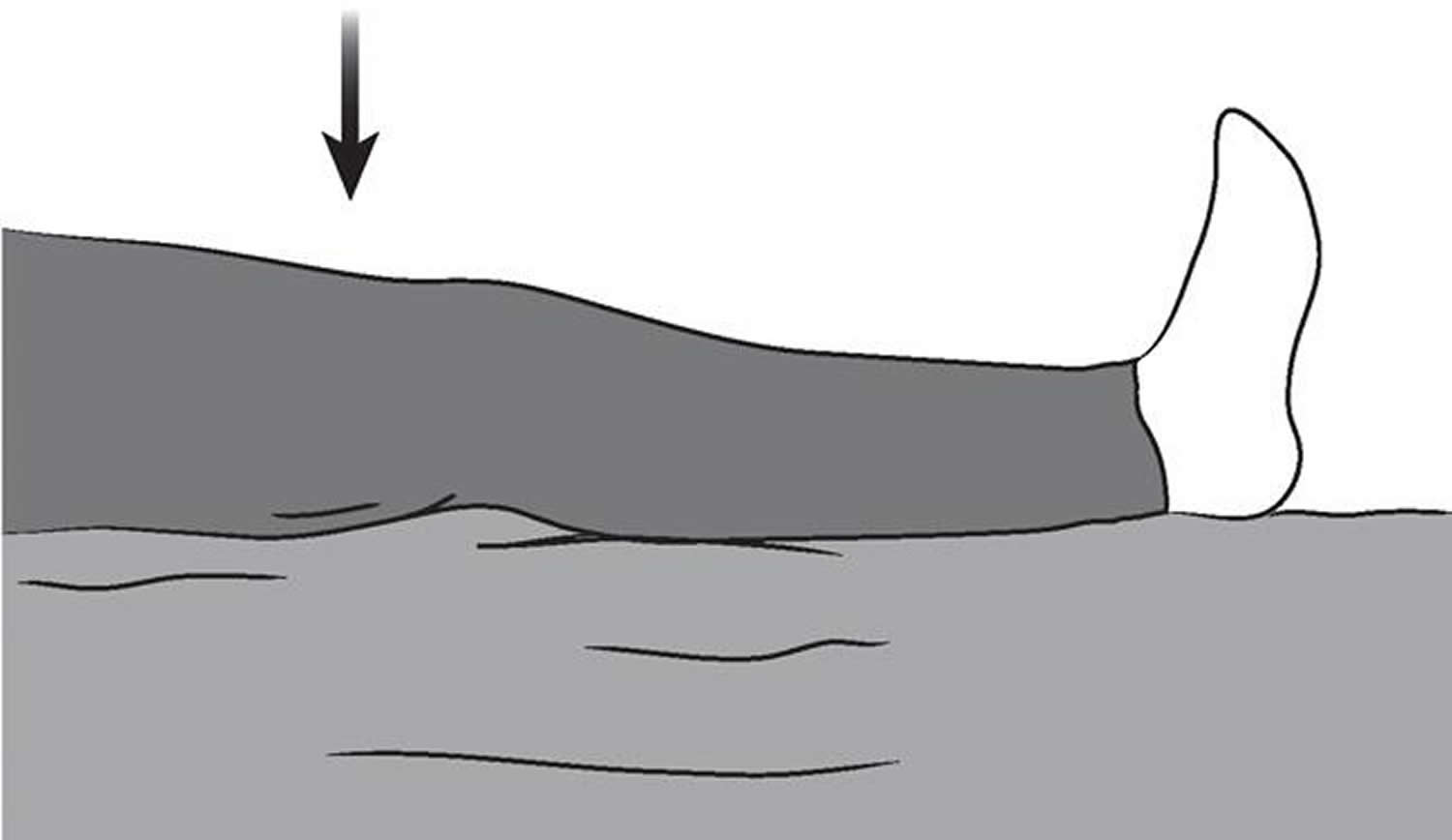
Early Hip Replacement Postoperative Exercises
The following exercises will help increase circulation to your legs and feet, which is important for preventing blood clots. They will also help strengthen your muscles and improve hip movement.
Start the exercises as soon as you are able. You can begin them in the recovery room shortly after surgery. You may feel uncomfortable at first, but these exercises will help speed your recovery and actually diminish your postoperative pain.
Ankle Pumps
Slowly push your foot up and down. Repeat this exercise several times, as often as every 5 or 10 minutes.
Begin this exercise immediately after surgery and continue it until you are fully recovered.
Figure 12. Ankle pumps exercise after a hip replacement
Ankle Rotations
Move your ankle inward toward your other foot and then outward away from your other foot.
Repeat 5 times in each direction.
Do 3 or 4 sessions a day.
Figure 13. Ankle Rotations after a hip replacement
Bed-Supported Knee Bends
Slide your foot toward your buttocks, bending your knee and keeping your heel on the bed. Do not let your knee roll inward. Hold your knee in a maximally bent position for 5 to 10 seconds and then straighten.
Repeat 10 times.
Do 3 or 4 sessions a day.
Figure 14. Bed-Supported Knee Bends exercise after a hip replacement
Buttock Contractions
Tighten your buttock muscles and hold to a count of 5.
Repeat 10 times.
Do 3 or 4 sessions a day.
Figure 15. Buttock contractions after a hip replacement
Abduction Exercise
Slide your leg out to the side as far as you can and then back.
Repeat 10 times.
Do 3 or 4 sessions a day.
Figure 16. Abduction exercise after a hip replacement
Quadriceps Set
Tighten your thigh muscle. Try to straighten your knee. Hold for 5 to 10 seconds.
Repeat this exercise 10 times during a 10-minute period, rest one minute and repeat.
Continue until your thigh feels fatigued.
Figure 17. Quadriceps exercise after a hip replacement
Straight Leg Raises
Tighten your thigh muscle with your knee fully straightened on the bed. Lift your leg several inches. Hold for 5 to 10 seconds. Slowly lower.
Repeat until your thigh feels fatigued.
Figure 18. Straight Leg Raises exercise after hip replacement
Standing Exercises
Soon after your hip replacement surgery, you will be out of bed and able to stand. You will require help at first but, as you regain your strength, you will be able to stand independently. While doing these standing exercises, make sure you are holding on to a firm surface such as a bar attached to your bed or a wall.
Standing Knee Raises
Lift your operated leg toward your chest. Do not lift your knee higher than your waist. Hold for 2 or 3 counts and put your leg down.
Repeat 10 times.
Do 3 or 4 sessions a day.
Figure 19. Standing Knee Raises exercise after hip replacement
Standing Hip Abduction
Be sure your hip, knee and foot are pointing straight forward. Keep your body straight. With your knee straight, lift your leg out to the side. Slowly lower your leg so your foot is back on the floor.
Repeat 10 times.
Do 3 or 4 sessions a day.
Figure 20. Standing Hip Abduction exercise after hip replacement
Standing Hip Extensions
Lift your operated leg backward slowly. Try to keep your back straight. Hold for 2 or 3 counts. Return your foot to the floor.
Repeat 10 times.
Do 3 or 4 sessions a day.
Figure 21. Standing Hip Extensions exercise after hip replacement
Early Activity
Soon after surgery, you will begin to walk short distances in your hospital room and perform light everyday activities. This early activity aids your recovery and helps your hip regain its strength and movement.
Walking
Early on, walking will help you regain movement in your hip.
Proper walking is the best way to help your hip recover. At first, you will walk with a walker or crutches. Your surgeon or therapist will tell you how much weight to put on your leg.
Stand comfortably and erect with your weight evenly balanced on your walker or crutches. Advance your walker or crutches a short distance; then reach forward with your operated leg with your knee straightened so the heel of your foot touches the floor first. As you move forward, your knee and ankle will bend and your entire foot will rest evenly on the floor. As you complete the step, your toe will lift off the floor and your and knee and hip will bend so that you can reach forward for your next step. Remember, touch your heel first, then flatten your foot, then lift your toes off the floor.
Walk as rhythmically and smoothly as you can. Don’t hurry. Adjust the length of your step and speed as necessary to walk with an even pattern. As your muscle strength and endurance improve, you may spend more time walking. You will gradually put more weight on your leg. You may use a cane in the hand opposite your surgery and, eventually, walk without an aid.
Walk with a cane until you have regained your balance skills. In the beginning, walk for 5 or 10 minutes, 3 or 4 times a day. As your strength and endurance improve, you can walk for 20 to 30 minutes, 2 or 3 times a day. Once you have fully recovered, regular walks of 20 to 30 minutes, 3 or 4 times a week, will help maintain your strength.
When you can walk and stand for more than 10 minutes and your leg is strong enough so that you are not carrying any weight on your walker or crutches, you can begin using a single crutch or cane. Hold the aid in the hand opposite the side of your surgery.
Stair Climbing and Descending
The ability to go up and down stairs requires both strength and flexibility. At first, you will need a handrail for support and will be able to go only one step at a time. Always lead up the stairs with your good leg and down the stairs with your operated leg. Remember, “up with the good” and “down with the bad.” You may want to have someone help you until you have regained most of your strength and mobility.
Stair climbing is an excellent strengthening and endurance activity. Do not try to climb steps higher than the standard height (7 inches) and always use a handrail for balance. As you become stronger and more mobile, you can begin to climb stairs foot over foot.
Advanced Exercises and Activities
The pain from your hip problems before your surgery and the pain and swelling after surgery have weakened your hip muscles. A full recovery will take many months. The following exercises and activities will help your hip muscles recover fully.
These exercises should be done in 10 repetitions, 4 times a day. Place one end of the tubing around the ankle of your operated leg and attach the opposite end of the tubing to a stationary object such as a locked door or heavy furniture. Hold on to a chair or bar for balance.
Elastic Tube Exercises
Resistive Hip Flexion
Stand with your feet slightly apart. Bring your operated leg forward keeping the knee straight. Allow your leg to return to its previous position.
Figure 22. Resistive Hip Flexion exercise after a hip replacement
Resistive Hip Abduction
Stand sideways from the door to which the tubing is attached and extend your operated leg out to the side. Allow your leg to return to its previous position.
Figure 23. Resistive Hip Abduction exercise after hip replacement
Resistive Hip Extensions
Face the door to which the tubing is attached and pull your leg straight back. Allow your leg to return to its previous position.
Figure 24. Resistive Hip Extensions exercise after hip replacement
Exercycling
Exercycling is an excellent activity to help you regain muscle strength and hip mobility.
At first, adjust the seat height so that the bottom of your foot just touches the pedal with your knee almost straight. Pedal backwards at first. Ride forward only after a comfortable cycling motion is possible backwards.
As you become stronger (at about 4 to 6 weeks) slowly increase the tension on the exercycle. Exercycle for 10 to 15 minutes twice a day, gradually building up to 20 to 30 minutes, 3 or 4 times a week.
- Keating JF, Grant A, Masson M, Scott NW, Forbes JF. Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty Treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Joint Surg Am. 2006;88:249–260. doi: 10.2106/JBJS.E.00215[↩]
- Baker RP, Squires B, Gargan MF, Bannister GC. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. A randomized, controlled trial. J Bone Joint Surg Am. 2006;88:2583–2589. doi: 10.2106/JBJS.E.01373[↩]
- Hedbeck CJ, Blomfeldt R, Lapidus G, Törnkvist H, Ponzer S, Tidermark J. Unipolar hemiarthroplasty versus bipolar hemiarthroplasty in the most elderly patients with displaced femoral neck fractures: a randomised, controlled trial. International Orthopaedics. 2011;35(11):1703-1711. doi:10.1007/s00264-011-1213-y. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3193971/[↩]
- Stability of hip hemiarthroplasties. Varley J, Parker MJ. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3456984/pdf/264_2004_Article_572.pdfInt Orthop. 2004 Oct; 28(5):274-7.[↩]
- Hedbeck CJ, Blomfeldt R, Lapidus G, Törnkvist H, Ponzer S, Tidermark J. Unipolar hemiarthroplasty versus bipolar hemiarthroplasty in the most elderly patients with displaced femoral neck fractures: a randomised, controlled trial. International Orthopaedics. 2011;35(11):1703-1711. doi:10.1007/s00264-011-1213-y https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3193971/[↩][↩]
- Cornell CN, Levine D, O’Doherty J, Lyden J (1998) Unipolar versus bipolar hemiarthroplasty for the treatment of femoral neck fractures in the elderly. Clin Orthop Relat Res 348:67–71[↩]
- Davison JN, Calder SJ, Anderson GH, Ward G, Jagger C, Harper WM, Gregg PJ. Treatment for displaced intracapsular fracture of the proximal femur. A prospective, randomised trial in patients aged 65 to 79 years. J Bone Joint Surg Br. 2001;83:206–212. doi: 10.1302/0301-620X.83B2.11128[↩]
- Raia FJ, Chapman CB, Herrera MF, Schweppe MW, Michelsen CB, Rosenwasser MP (2003) Unipolar or bipolar hemiarthroplasty for femoral neck fractures in the elderly? Clin Orthop Relat Res 259–265[↩]
- Calder SJ, Anderson GH, Jagger C, Harper WM, Gregg PJ. Unipolar or bipolar prosthesis for displaced intracapsular hip fracture in octogenarians: a randomised prospective study [see comments] J Bone Joint Surg Br. 1996;78:391–394[↩]
- Concerns about Metal-on-Metal Hip Implants. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/ImplantsandProsthetics/MetalonMetalHipImplants/ucm241604.htm[↩]