Contents
- What is HIV
- Is there a cure for HIV ?
- Where did HIV come from ?
- How do people get HIV / how HIV is Transmitted
- Oral Sex and HIV Risk
- How well does HIV survive outside the body
- Can I get HIV from casual contact (“social kissing”, shaking hands, hugging, using a toilet, drinking from the same glass or sneezing and coughing from an infected person)
- Can I get HIV from a tattoo or a body piercing ?
- Can I get HIV from being spit on or scratched by an HIV-infected person ?
- Can I get HIV from mosquitoes ?
- Can I get HIV from food ?
- Can I get HIV from anal sex ?
- Can I get HIV from vaginal sex ?
- Can I get HIV from oral sex ?
- Are lesbians or other women who have sex with other women at risk for HIV ?
- Is there a connection between HIV and other sexually transmitted infections ?
- Does my HIV-positive partner’s viral load affect my risk of getting HIV ?
- Can I get HIV from injecting drugs ?
- Can I get HIV from using other kinds of drugs ?
- If I already have HIV, can I get another kind of HIV ?
- Can I get HIV from receiving medical care ?
- What are Stages of HIV
- How do you know if you have HIV ?
- Prevention of HIV
- Is abstinence the only 100 percent effective HIV prevention option ?
- How can I prevent passing HIV to my baby ?
- How can I prevent getting HIV from anal or vaginal sex ?
- How well do condoms prevent HIV ?
- Can using a lubricant help reduce my HIV risk ?
- Can I use microbiocides to prevent HIV ?
- Can male circumcision prevent HIV ?
- Can I take medicines to prevent getting HIV ?
- Can I take medicines to prevent HIV after exposure ?
- Can I get vaccinated to prevent HIV ?
- If I’m living with HIV, how can I prevent passing it to others ?
- How can I prevent getting HIV from drug use ?
- HIV Symptoms
- Causes of HIV and AIDS
- Complications of HIV and AIDS
- Tests and Diagnosis for HIV
- Home test
- Tests to tailor treatment
- Tests for complications
- What kinds of tests are available and how do they work ?
- How soon after an exposure to HIV can a HIV test detect if I am infected ?
- What does a positive HIV test mean ?
- If I test positive for HIV, does that mean I have AIDS ?
- Should I share my positive test result with others ?
- What does a negative test result mean ?
- If I have a negative result, does that mean my partner is HIV-negative also ?
- Treatments and drugs for HIV and AIDS
- What is AIDS
What is HIV
HIV stands for human immunodeficiency virus. It weakens and harms your immune system by destroying important cells that fight disease and infection 1. HIV is the virus that can lead to acquired immunodeficiency syndrome or AIDS if not treated. Unlike some other viruses, the human body can’t get rid of HIV completely, even with treatment. So once you get HIV, you have it for life.
HIV is a virus spread through certain body fluids that attacks your body’s immune system, specifically the CD4 cells, often called T cells (T lymphocytes). These special T cells help the immune system fight off infections. Untreated, HIV can destroy so many of these T cells (CD4 cells) that your body can’t fight off infections and disease. This damage to the immune system makes it harder and harder for your body to fight off infections and some other diseases. Opportunistic infections or cancers take advantage of a very weak immune system and signal that the person has AIDS (acquired immunodeficiency syndrome), the last stage of HIV infection.
No effective cure exists for HIV. But with proper medical care, HIV can be controlled. The medicine used to treat HIV is called antiretroviral therapy or ART. If taken the right way, every day, this medicine can dramatically prolong the lives of many people infected with HIV, keep them healthy, and greatly lower their chance of infecting others. Before the introduction of ART in the mid-1990s, people with HIV could progress to AIDS in just a few years. Today, someone diagnosed with HIV and treated before the disease is far advanced can live nearly as long as someone who does not have HIV.
Some groups of people in the United States are more likely to get HIV than others because of many factors, including their sex partners, their risk behaviors, and where they live.
Is there a cure for HIV ?
No effective cure currently exists for HIV. But with proper medical care, HIV can be controlled. Treatment for HIV is called Antiretroviral therapy or ART. If taken the right way, every day, antiretroviral therapy (ART) can dramatically prolong the lives of many people infected with HIV, keep them healthy, and greatly lower their chance of infecting others. Before the introduction of antiretroviral therapy (ART) in the mid-1990s, people with HIV could progress to AIDS (the last stage of HIV infection) in a few years. Today, someone diagnosed with HIV and treated before the disease is far advanced can live nearly as long as someone who does not have HIV.
Where did HIV come from ?
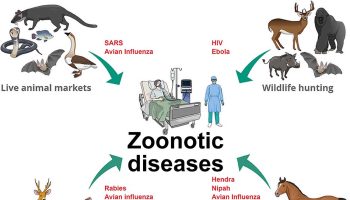
Scientists identified a type of chimpanzee in Central Africa as the source of HIV infection in humans. They believe that the chimpanzee version of the immunodeficiency virus (called simian immunodeficiency virus, or SIV) most likely was transmitted to humans and mutated into HIV when humans hunted these chimpanzees for meat and came into contact with their infected blood. Studies show that HIV may have jumped from apes to humans as far back as the late 1800s. Over decades, the virus slowly spread across Africa and later into other parts of the world. We know that the virus has existed in the United States since at least the mid to late 1970s.
The Centers for Disease Prevention and Control (CDC) announces that annual HIV diagnoses in the US fell by 19% from 2005-2014 2. There were steep declines among heterosexuals, people who inject drugs, and African Americans (especially black women), but trends for gay/bisexual men varied by race/ ethnicity. Diagnoses among white gay/bisexual men decreased by 18%, but they continued to rise among Latino gay/bisexual men and were up 24%. Diagnoses among black gay/bisexual men also increased (22%), but the increase has leveled off since 2010 2.
How do people get HIV / how HIV is Transmitted
You can get or transmit HIV only through specific activities.
- Most commonly, people get or transmit HIV through sexual behaviors and needle or syringe use.
Only certain body fluids—blood, semen (cum), pre-seminal fluid (pre-cum), rectal fluids, vaginal fluids, and breast milk—from a person who has HIV can transmit HIV. These fluids must come in contact with a mucous membrane or damaged tissue or be directly injected into the bloodstream (from a needle or syringe) for transmission to occur. Mucous membranes are found inside the rectum, vagina, penis, and mouth.
In the United States, HIV is spread mainly by:
- Having anal or vaginal sex with someone who has HIV without using a condom or taking medicines to prevent or treat HIV.
- For the HIV-negative partner, receptive anal sex (bottoming) is the highest-risk sexual behavior, but you can also get HIV from insertive anal sex (topping).
- Either partner can get HIV through vaginal sex, though it is less risky for getting HIV than receptive anal sex.
- Sharing needles or syringes, rinse water, or other equipment (works) used to prepare drugs for injection with someone who has HIV. HIV can live in a used needle up to 42 days depending on temperature and other factors.
Less commonly, HIV may be spread:
- From mother to child during pregnancy, birth, or breastfeeding. Although the risk can be high if a mother is living with HIV and not taking medicine, recommendations to test all pregnant women for HIV and start HIV treatment immediately have lowered the number of babies who are born with HIV.
- By being stuck with an HIV-contaminated needle or other sharp object. This is a risk mainly for health care workers.
In extremely rare cases, HIV has been transmitted by:
- Oral sex—putting the mouth on the penis (fellatio), vagina (cunnilingus), or anus (rimming). In general, there’s little to no risk of getting HIV from oral sex. But transmission of HIV, though extremely rare, is theoretically possible if an HIV-positive man ejaculates in his partner’s mouth during oral sex.
- Receiving blood transfusions, blood products, or organ/tissue transplants that are contaminated with HIV. This was more common in the early years of HIV, but now the risk is extremely small because of rigorous testing of the US blood supply and donated organs and tissues.
- Eating food that has been pre-chewed by an HIV-infected person. The contamination occurs when infected blood from a caregiver’s mouth mixes with food while chewing. The only known cases are among infants.
- Being bitten by a person with HIV. Each of the very small number of documented cases has involved severe trauma with extensive tissue damage and the presence of blood. There is no risk of transmission if the skin is not broken.
- Contact between broken skin, wounds, or mucous membranes and HIV-infected blood or blood-contaminated body fluids.
- Deep, open-mouth kissing if both partners have sores or bleeding gums and blood from the HIV-positive partner gets into the bloodstream of the HIV-negative partner. HIV is not spread through saliva.
Oral Sex and HIV Risk
Oral sex involves using the mouth to stimulate the penis (fellatio), vagina (cunnilingus), or anus (anilingus) 3.
- There is little to no risk of getting or transmitting HIV from oral sex.
- Other STDs (sexually transmitted diseases) and hepatitis can be transmitted during oral sex.
- Latex barriers and medicines to prevent and treat HIV can further reduce the very low risk of getting HIV from oral sex.
Risk of HIV
The chance an HIV-negative person will get HIV from oral sex with an HIV-positive partner is extremely low. However, it is hard to know the exact risk because a lot of people who have oral sex also have anal or vaginal sex. The type of oral sex that may be the riskiest is mouth-to-penis oral sex. But the risk is still very low, and much lower than with anal or vaginal sex.
Though the risk of HIV transmission through oral sex is low, several factors may increase that risk, including sores in the mouth or vagina or on the penis, bleeding gums, oral contact with menstrual blood, and the presence of other sexually transmitted diseases (STDs).
Risk of Other Infections
Other STDs, such as syphilis, herpes, gonorrhea and chlamydia, can be transmitted during oral sex. Anilingus can also transmit hepatitis A and B, intestinal parasites like Giardia, and bacteria like E. coli.
Reducing the Risk
Individuals can further reduce the already low risk of HIV transmission from oral sex by keeping their male partners from ejaculating in their mouth. This could be done by removing the mouth from the penis before ejaculation, or by using a condom.
Using a barrier like a condom or dental dam during oral sex can further reduce the risk of transmitting HIV, other STDs, and hepatitis. A dental dam is a thin, square piece of latex or silicone that is placed over the vagina or anus during oral sex. A latex condom can also be cut length-wise and used like a dental dam.
The risk of HIV transmission through oral sex is even lower if the HIV-negative partner is taking medicine to prevent HIV (pre-exposure prophylaxis or PrEP) or the HIV-positive partner is taking medicine to treat HIV (antiretroviral therapy or ART) and is virally suppressed.
How well does HIV survive outside the body
HIV does not survive long outside the human body (such as on surfaces), and it cannot reproduce outside a human host. It is not spread by:
- Mosquitoes, ticks, or other insects.
- Saliva, tears, or sweat that is not mixed with the blood of an HIV-positive person.
- Hugging, shaking hands, sharing toilets, sharing dishes, or closed-mouth or “social” kissing with someone who is HIV-positive.
- Other sexual activities that don’t involve the exchange of body fluids (for example, touching).
No. HIV isn’t transmitted
- By hugging, shaking hands, sharing toilets, sharing dishes, or closed-mouth or “social” kissing with someone who is HIV-positive.
- Through saliva, tears, or sweat that is not mixed with the blood of an HIV-positive person.
- By mosquitoes, ticks or other blood-sucking insects.
- Through the air.
Only certain body fluids—blood, semen (cum), pre-seminal fluid (pre-cum), rectal fluids, vaginal fluids, and breast milk—from an HIV-infected person can transmit HIV. Most commonly, people get or transmit HIV through sexual behaviors and needle or syringe use. Babies can also get HIV from an HIV-positive mother during pregnancy, birth, or breastfeeding.
Can I get HIV from a tattoo or a body piercing ?
There are no known cases in the United States of anyone getting HIV this way. However, it is possible to get HIV from a reused or not properly sterilized tattoo or piercing needle or other equipment, or from contaminated ink.
It’s possible to get HIV from tattooing or body piercing if the equipment used for these procedures has someone else’s blood in it or if the ink is shared. The risk of getting HIV this way is very low, but the risk increases when the person doing the procedure is unlicensed, because of the potential for unsanitary practices such as sharing needles or ink. If you get a tattoo or a body piercing, be sure that the person doing the procedure is properly licensed and that they use only new or sterilized needles, ink, and other supplies.
Can I get HIV from being spit on or scratched by an HIV-infected person ?
No. HIV isn’t spread through saliva, and there is no risk of transmission from scratching because no body fluids are transferred between people.
Can I get HIV from mosquitoes ?
No. HIV is not transmitted by mosquitoes, ticks, or any other insects.
Can I get HIV from food ?
You can’t get HIV from consuming food handled by an HIV-infected person. Even if the food contained small amounts of HIV-infected blood or semen, exposure to the air, heat from cooking, and stomach acid would destroy the virus.
Though it is very rare, HIV can be spread by eating food that has been pre-chewed by an HIV-infected person. The contamination occurs when infected blood from a caregiver’s mouth mixes with food while chewing. The only known cases are among infants.
Can I get HIV from anal sex ?
Yes. In fact, anal sex is the riskiest type of sex for getting or transmitting HIV.
HIV can be found in certain body fluids—blood, semen (cum), pre-seminal fluid (pre-cum), or rectal fluids—of a person who has HIV. Although receptive anal sex (bottoming) is much riskier for getting HIV than insertive anal sex (topping), it’s possible for either partner—the top or the bottom—to get HIV. The bottom’s risk is very high because the lining of the rectum is thin and may allow HIV to enter the body during anal sex. The top is also at risk because HIV can enter the body through the opening at the tip of the penis (or urethra); the foreskin if the penis isn’t circumcised; or small cuts, scratches, or open sores anywhere on the penis.
Can I get HIV from vaginal sex ?
Yes. Either partner can get HIV through vaginal sex, though it is less risky for getting HIV than receptive anal sex.
When a woman has vaginal sex with a partner who’s HIV-positive, HIV can enter her body through the mucous membranes that line the vagina and cervix. Most women who get HIV get it from vaginal sex.
Men can also get HIV from having vaginal sex with a woman who’s HIV-positive. This is because vaginal fluid and blood can carry HIV. Men get HIV through the opening at the tip of the penis (or urethra); the foreskin if they’re not circumcised; or small cuts, scratches, or open sores anywhere on the penis.
Can I get HIV from oral sex ?
The chance that an HIV-negative person will get HIV from oral sex with an HIV-positive partner is extremely low.
Oral sex involves putting the mouth on the penis (fellatio), vagina (cunnilingus), or anus (anilingus). In general, there’s little to no risk of getting or transmitting HIV through oral sex.
Factors that may increase the risk of transmitting HIV through oral sex are ejaculation in the mouth with oral ulcers, bleeding gums, genital sores, and the presence of other sexually transmitted diseases (STDs), which may or may not be visible.
You can get other STDs from oral sex. And, if you get feces in your mouth during anilingus, you can get hepatitis A and B, parasites like Giardia, and bacteria like Shigella, Salmonella, Campylobacter, and E. coli.
Are lesbians or other women who have sex with other women at risk for HIV ?
Case reports of female-to-female transmission of HIV are rare. The well-documented risk of female-to-male transmission shows that vaginal fluids and menstrual blood may contain the virus and that exposure to these fluids through mucous membranes (in the vagina or mouth) could potentially lead to HIV infection.
Is there a connection between HIV and other sexually transmitted infections ?
Yes. Having another sexually transmitted disease (STD) can increase the risk of getting or transmitting HIV.
If you have another STD, you’re more likely to get or transmit HIV to others. Some of the most common STDs include gonorrhea, chlamydia, syphilis, trichomoniasis, human papillomavirus (HPV), genital herpes, and hepatitis. The only way to know for sure if you have an STD is to get tested. If you’re sexually active, you and your partners should get tested for STDs (including HIV if you’re HIV-negative) regularly, even if you don’t have symptoms.
If you are HIV-negative but have an STD, you are about 3 times as likely to get HIV if you have unprotected sex with someone who has HIV. There are two ways that having an STD can increase the likelihood of getting HIV. If the STD causes irritation of the skin (for example, from syphilis, herpes, or human papillomavirus), breaks or sores may make it easier for HIV to enter the body during sexual contact. Even STDs that cause no breaks or open sores (for example, chlamydia, gonorrhea, trichomoniasis) can increase your risk by causing inflammation that increases the number of cells that can serve as targets for HIV.
If you are HIV-positive and also infected with another STD, you are about 3 times as likely as other HIV-infected people to spread HIV through sexual contact. This appears to happen because there is an increased concentration of HIV in the semen and genital fluids of HIV-positive people who also are infected with another STD.
Yes, as an HIV-positive person’s viral load goes down, the chance of transmitting HIV goes down.
Viral load is the amount of HIV in the blood of someone who is HIV-positive. When the viral load is very low, it is called viral suppression. Undetectable viral load is when the amount of HIV in the blood is so low that it can’t be measured.
In general, the higher someone’s viral load, the more likely that person is to transmit HIV. People who have HIV but are in care, taking HIV medicines, and have a very low or undetectable viral load are much less likely to transmit HIV than people who have HIV and do not have a low viral load.
However, a person with HIV can still potentially transmit HIV to a partner even if they have an undetectable viral load, because
HIV may still be found in genital fluids (semen, vaginal fluids). The viral load test only measures virus in blood.
A person’s viral load may go up between tests. When this happens, they may be more likely to transmit HIV to partners.
Sexually transmitted diseases increase viral load in genital fluids.
If you’re HIV-positive, getting into care and taking HIV medicines (called antiretroviral therapy or ART) the right way, every day will give you the greatest chance to get and stay virally suppressed, live a longer, healthier life, and reduce the chance of transmitting HIV to your partners.
If you’re HIV-negative and have an HIV-positive partner, encourage your partner to get into care and take HIV treatment medicines.
Taking other actions, like using a condom the right way every time you have sex or taking daily medicine to prevent HIV (called pre-exposure prophylaxis or PrEP) if you’re HIV-negative, can lower your chances of transmitting or getting HIV even more.
Can I get HIV from injecting drugs ?
Yes. Your risk for getting HIV is very high if you use needles or works (such as cookers, cotton, or water) after someone with HIV has used them.
People who inject drugs, hormones, steroids, or silicone can get HIV by sharing needles or syringes and other injection equipment. The needles and equipment may have someone else’s blood in them, and blood can transmit HIV. Likewise, you’re at risk for getting hepatitis B and C if you share needles and works because these infections are also transmitted through blood.
Another reason people who inject drugs can get HIV (and other sexually transmitted diseases) is that when people are high, they’re more likely to have risky sex.
Stopping injection and other drug use can lower your chances of getting HIV a lot. You may need help to stop or cut down using drugs, but many resources are available.
If you keep injecting drugs, you can lower your risk for getting HIV by using only new, sterile needles and works each time you inject. Never share needles or works.
Can I get HIV from using other kinds of drugs ?
When you’re drunk or high, you’re more likely to make decisions that put you at risk for HIV, such as having sex without a condom.
Drinking alcohol, particularly binge drinking, and using “club drugs” like Ecstasy, ketamine, GHB, and poppers can alter your judgment, lower your inhibitions, and impair your decisions about sex or other drug use. You may be more likely to have unplanned and unprotected sex, have a harder time using a condom the right way every time you have sex, have more sexual partners, or use other drugs, including injection drugs or meth. Those behaviors can increase your risk of exposure to HIV. If you have HIV, they can also increase your risk of spreading HIV to others. Being drunk or high affects your ability to make safe choices.
If you’re going to a party or another place where you know you’ll be drinking or using drugs, you can bring a condom so that you can reduce your risk if you have vaginal or anal sex.
Therapy, medicines, and other methods are available to help you stop or cut down on drinking or using drugs. Talk with a counselor, doctor, or other health care provider about options that might be right for you.
If I already have HIV, can I get another kind of HIV ?
Yes. This is called HIV superinfection.
HIV superinfection is when a person with HIV gets infected with another strain of the virus. The new strain of HIV can replace the original strain or remain along with the original strain.
The effects of superinfection differ from person to person. Superinfection may cause some people to get sicker faster because they become infected with a new strain of the virus that is resistant to the medicine (antiretroviral therapy or ART) they’re taking to treat their original infection.
Research suggests that a hard-to-treat superinfection is rare. Taking medicine to treat HIV (ART) may reduce someone’s chance of getting a superinfection.
Can I get HIV from receiving medical care ?
Although HIV transmission is possible in health care settings, it is extremely rare.
Careful practice of infection control, including universal precautions (using protective practices and personal protective equipment to prevent HIV and other blood-borne infections), protects patients as well as health care providers from possible HIV transmission in medical and dental offices and hospitals.
The risk of getting HIV from receiving blood transfusions, blood products, or organ/tissue transplants that are contaminated with HIV is extremely small because of rigorous testing of the US blood supply and donated organs and tissues.
It is important to know that you cannot get HIV from donating blood. Blood collection procedures are highly regulated and safe.
What are Stages of HIV
When people get HIV and don’t receive treatment, they will typically progress through three stages of disease. Medicine to treat HIV, known as antiretroviral therapy (ART), helps people at all stages of the disease if taken the right way, every day. Treatment can slow or prevent progression from one stage to the next. It can also dramatically reduce the chance of transmitting HIV to someone else.
Stage 1: Acute HIV infection
Within 2 to 4 weeks after infection with HIV, people may experience a flu-like illness, which may last for a few weeks. This is the body’s natural response to infection. When people have acute HIV infection, they have a large amount of virus in their blood and are very contagious. But people with acute infection are often unaware that they’re infected because they may not feel sick right away or at all. To know whether someone has acute infection, either a fourth-generation antibody/antigen test or a nucleic acid (NAT) test is necessary. If you think you have been exposed to HIV through sex or drug use and you have flu-like symptoms, seek medical care and ask for a test to diagnose acute infection.
Stage 2: Clinical latency (HIV inactivity or dormancy)
This period is sometimes called asymptomatic HIV infection or chronic HIV infection. During this phase, HIV is still active but reproduces at very low levels. People may not have any symptoms or get sick during this time. For people who aren’t taking medicine to treat HIV, this period can last a decade or longer, but some may progress through this phase faster. People who are taking medicine to treat HIV (ART) the right way, every day may be in this stage for several decades. It’s important to remember that people can still transmit HIV to others during this phase, although people who are on ART and stay virally suppressed (having a very low level of virus in their blood) are much less likely to transmit HIV than those who are not virally suppressed. At the end of this phase, a person’s viral load starts to go up and the CD4 cell count begins to go down. As this happens, the person may begin to have symptoms as the virus levels increase in the body, and the person moves into Stage 3.
Stage 3: Acquired immunodeficiency syndrome (AIDS)
AIDS is the most severe phase of HIV infection. People with AIDS have such badly damaged immune systems that they get an increasing number of severe illnesses, called opportunistic illnesses.
Without treatment, people with AIDS typically survive about 3 years. Common symptoms of AIDS include chills, fever, sweats, swollen lymph glands, weakness, and weight loss. People are diagnosed with AIDS when their CD4 cell count drops below 200 cells/mm or if they develop certain opportunistic illnesses. People with AIDS can have a high viral load and be very infectious.
How do you know if you have HIV ?
The only way to know for sure whether you have HIV is to get tested. Knowing your status is important because it helps you make healthy decisions to prevent getting or transmitting HIV.
Some people may experience a flu-like illness within 2 to 4 weeks after infection (Stage 1 HIV infection). But some people may not feel sick during this stage. Flu-like symptoms include fever, chills, rash, night sweats, muscle aches, sore throat, fatigue, swollen lymph nodes, or mouth ulcers. These symptoms can last anywhere from a few days to several weeks. During this time, HIV infection may not show up on an HIV test, but people who have it are highly infectious and can spread the infection to others.
If you have these symptoms, that doesn’t mean you have HIV. Each of these symptoms can be caused by other illnesses. But if you have these symptoms after a potential exposure to HIV, see a health care provider and tell them about your risk. The only way to determine whether you are infected is to be tested for HIV infection.
To find places near you that offer confidential HIV testing,
- Visit gettested.cdc.gov
- You can also use a home testing kit, available for purchase in most pharmacies and online.
After you get tested, it’s important to find out the result of your test so you can talk to your health care provider about treatment options if you’re HIV-positive or learn ways to prevent getting HIV if you’re HIV-negative.
Is the risk of HIV different for different people ?
Some groups of people in the United States are more likely to get HIV than others because of many factors, including the status of their sex partners, their risk behaviors, and where they live.
When you live in a community where many people have HIV infection, the chances of having sex or sharing needles or other injection equipment with someone who has HIV are higher. You can use CDC’s HIV, STD, hepatitis, and tuberculosis atlas 4 to see the percentage of people with HIV (“prevalence”) in different US communities. Within any community, the prevalence of HIV can vary among different populations.
Gay and bisexual men have the largest number of new diagnoses in the United States. Blacks/African Americans and Hispanics/Latinos are disproportionately affected by HIV compared to other racial and ethnic groups. Also, transgender women who have sex with men are among the groups at highest risk for HIV infection, and injection drug users remain at significant risk for getting HIV.
Risky behaviors, like having anal or vaginal sex without using a condom or taking medicines to prevent or treat HIV, and sharing needles or syringes play a big role in HIV transmission. Anal sex is the highest-risk sexual behavior. If you don’t have HIV, being a receptive partner (or bottom) for anal sex is the highest-risk sexual activity for getting HIV. If you do have HIV, being the insertive partner (or top) for anal sex is the highest-risk sexual activity for transmitting HIV.
But there are more tools available today to prevent HIV than ever before. Choosing less risky sexual behaviors, taking medicines to prevent and treat HIV, and using condoms with lubricants are all highly effective ways to reduce the risk of getting or transmitting HIV. Learn more about these and other strategies to prevent HIV.
Prevention of HIV
There’s no vaccine to prevent HIV infection and no cure for AIDS. But it’s possible to protect yourself and others from infection. That means educating yourself about HIV and avoiding any behavior that allows HIV-infected fluids — blood, semen, vaginal secretions and breast milk — into your body.
To help prevent the spread of HIV:
- Use a new condom every time you have sex. If you don’t know the HIV status of your partner, use a new condom every time you have anal or vaginal sex. Women can use a female condom.
- Use only water-based lubricants. Oil-based lubricants can weaken condoms and cause them to break. During oral sex use a nonlubricated, cut-open condom or a dental dam — a piece of medical-grade latex.
- Consider the drug Truvada. Use of the combination drug emtricitabine-tenofovir (Truvada) can reduce the risk of sexually transmitted HIV infection in those who are at high risk. Truvada is also used as an HIV treatment along with other medications.
When used to help prevent HIV infection, Truvada is only appropriate if your doctor is certain you don’t already have an HIV infection. Your doctor should also test for hepatitis B infection. If you have hepatitis B, your doctor should test your kidney function before prescribing Truvada.
Truvada must be taken daily, exactly as prescribed. Truvada should only be used along with other prevention strategies, such as condom use every time you have sex, as it doesn’t protect against other sexually transmitted infections, and it can’t provide complete protection against HIV transmission. If you’re interested in Truvada, talk with your doctor about the potential risks and benefits of the drug.
- Tell your sexual partners if you have HIV. It’s important to tell anyone with whom you’ve had sex that you’re HIV-positive. Your partners need to be tested and to receive medical care if they have the virus. They also need to know their HIV status so that they don’t infect others.
- Use a clean needle. If you use a needle to inject drugs, make sure it’s sterile and don’t share it. Take advantage of needle-exchange programs in your community and consider seeking help for your drug use.
- If you’re pregnant, get medical care right away. If you’re HIV-positive, you may pass the infection to your baby. But if you receive treatment during pregnancy, you can cut your baby’s risk significantly.
- Consider male circumcision. There’s evidence that male circumcision can help reduce a man’s risk of acquiring HIV.
Is abstinence the only 100 percent effective HIV prevention option ?
Yes. Abstinence means not having oral, vaginal, or anal sex. An abstinent person is someone who’s never had sex or someone who’s had sex but has decided not to continue having sex for some period of time. Abstinence is the only 100% effective way to prevent HIV, other sexually transmitted diseases (STDs), and pregnancy. The longer you wait to start having oral, vaginal, or anal sex, the fewer sexual partners you are likely to have in your lifetime. Having fewer partners lowers your chances of having sex with someone who has HIV or another STD.
How can I prevent passing HIV to my baby ?
If you have HIV, the most important thing you can do is to take medicines to treat HIV infection (called antiretroviral therapy or ART) the right way, every day.
If you’re pregnant, talk to your health care provider about getting tested for HIV and other ways to keep you and your child from getting HIV. Women in their third trimester should be tested again if they engage in behaviors that put them at risk for HIV.
If you are HIV-negative but you have an HIV-positive partner and are considering getting pregnant, talk to your doctor about taking pre-exposure prophylaxis (PrEP) to help keep you from getting HIV. Encourage your partner to take medicines to treat HIV (ART), which greatly reduces the chance that he will transmit HIV to you.
If you have HIV, take medicines to treat HIV (ART) the right way, every day. If you are treated for HIV early in your pregnancy, your risk of transmitting HIV to your baby can be 1% or less. After delivery, you can prevent transmitting HIV to your baby by avoiding breastfeeding, since breast milk contains HIV.
How can I prevent getting HIV from anal or vaginal sex ?
Use condoms the right way every time you have sex, take medicines to prevent or treat HIV if appropriate, choose less risky sexual behaviors, get tested for other sexually transmitted diseases (STDs), and limit your number of sex partners. The more of these actions you take, the safer you can be.
Specifically, you can:
- Use condoms the right way every time you have sex (see How well do condoms prevent HIV?). Learn the right way to use a male condom.
- Reduce your number of sexual partners. This can lower your chances of having a sex partner who will transmit HIV to you. The more partners you have, the more likely you are to have a partner with HIV whose viral load is not suppressed or to have a sex partner with a sexually transmitted disease. Both of these factors can increase the risk of HIV transmission.
- Talk to your doctor about pre-exposure prophylaxis (PrEP), taking HIV medicines daily to prevent HIV infection, if you are at very high risk for HIV. PrEP should be considered if you are HIV-negative and in an ongoing sexual relationship with an HIV-positive partner. PrEP also should be considered if you aren’t in a mutually monogamous relationship with a partner who recently tested HIV-negative, and you are a:
- gay or bisexual man who has had anal sex without a condom or been diagnosed with an STD in the past 6 months;
- man who has sex with both men and women; or
- heterosexual man or woman who does not regularly use condoms during sex with partners of unknown HIV status who are at very high risk of HIV
- infection (for example, people who inject drugs or women who have bisexual male partners).
- Post-exposure prophylaxis (PEP) means taking HIV medicines after being potentially exposed to HIV to prevent becoming infected. If you’re HIV-negative or don’t know your HIV status and think you have recently been exposed to HIV during sex (for example, if the condom breaks), talk to your health care provider or an emergency room doctor about PEP right away (within 3 days). The sooner you start PEP, the better; every hour counts. If you’re prescribed PEP, you’ll need to take it once or twice daily for 28 days. Keep in mind that your chance of getting HIV is lower if your HIV-positive partner is taking medicine to treat HIV infection (called antiretroviral therapy, or ART) the right way, every day and his or her viral load remains suppressed.
- Get tested and treated for other STDs and encourage your partners to do the same. If you are sexually active, get tested at least once a year. Having other STDs increases your risk for getting or transmitting HIV. STDs can also have long-term health consequences. Find an STD testing site.
- If you’re HIV-negative and your partner is HIV-positive, encourage your partner to get and stay on treatment. If taken the right way, every day, the medicine to treat HIV (ART) reduces the amount of HIV (called “viral load”) in the blood and elsewhere in the body to very low levels. This is called “viral suppression.” Being virally suppressed is good for an HIV-positive person’s overall health and greatly reduces the chance of transmitting the virus to a partner.
- Choose less risky sexual behaviors. HIV is mainly spread by having anal or vaginal sex without a condom or without taking medicines to prevent or treat HIV.
Receptive anal sex is the riskiest type of sex for getting HIV. It’s possible for either partner—the partner inserting the penis in the anus (the top) or the partner receiving the penis (the bottom)—to get HIV, but it is much riskier for an HIV-negative partner to be the receptive partner. That’s because the lining of the rectum is thin and may allow HIV to enter the body during anal sex.
Vaginal sex also carries a risk for getting HIV, though it is less risky than receptive anal sex. Most women who get HIV get it from vaginal sex, but men can also get HIV from vaginal sex.
In general, there is little to no risk of getting or transmitting HIV from oral sex. Theoretically, transmission of HIV is possible if an HIV-positive man ejaculates in his partner’s mouth during oral sex. However, the risk is still very low, and much lower than with anal or vaginal sex. Factors that may increase the risk of transmitting HIV through oral sex are oral ulcers, bleeding gums, genital sores, and the presence of other STDs, which may or may not be visible.
Sexual activities that don’t involve contact with body fluids (semen, vaginal fluid, or blood) carry no risk of HIV transmission but may pose a risk for other STDs.
How well do condoms prevent HIV ?
If you use them the right way every time you have sex, condoms are highly effective in preventing HIV infection. But it’s important to educate yourself about how to use them the right way.
Condoms can also help prevent other sexually transmitted diseases (STDs) you can get through body fluids, like gonorrhea and chlamydia. However, they provide less protection against STDs spread through skin-to-skin contact, like human papillomavirus or HPV (genital warts), genital herpes, and syphilis.
There are two main types of condoms: male and female.
Male Condoms
- A male condom is a thin layer of latex, polyurethane, polyisoprene, or natural membrane worn over the penis during sex.
- Latex condoms provide the best protection against HIV. Polyurethane (plastic) or polyisoprene (synthetic rubber) condoms are good options for people with latex allergies, but plastic ones break more often than latex ones. Natural membrane (such as lambskin) condoms have small holes in them, so they don’t block HIV and other STDs.
- Use water- or silicone-based lubricants to lower the chances that a condom will break or slip during sex. Don’t use oil-based lubricants (for example, Vaseline, shortening, mineral oil, massage oils, body lotions, and cooking oil) with latex condoms because they can weaken the condom and cause it to break. Don’t use lubricants containing nonoxynol-9. It irritates the lining of the vagina and anus and increases the risk of getting HIV.
Female Condoms
- A female condom is a thin pouch made of a synthetic latex product called nitrile. It’s designed to be worn by a woman in her vagina during sex.
- When worn in the vagina, female condoms are comparable to male condoms at preventing HIV, other STDs, and pregnancy. Some people use female condoms for anal sex. We don’t currently know how well female condoms prevent HIV and other STDs when used by men or women for anal sex. But we do know that HIV can’t travel through the nitrile barrier.
- It is safe to use any kind of lubricant with nitrile female condoms.
Even if you use condoms the right way every time you have sex, there’s still a chance of getting HIV. For some individuals at high risk of getting or transmitting HIV, adding other prevention methods, like taking medicines to prevent and treat HIV, can further reduce their risk
Can using a lubricant help reduce my HIV risk ?
Yes, because lubricants can help prevent condoms from breaking or slipping.
Water-based and silicon-based lubricants are safe to use with all condoms. Oil-based lubricants and products containing oil, such as hand lotion, Vaseline, or Crisco, should not be used with latex condoms because they can weaken the condom and cause it to break. It is safe to use any kind of lubricant with nitrile female condoms. But lubricants containing nonoxynol-9 should not be used because nonoxynol-9 irritates the lining of the vagina and anus and increases the risk of getting HIV.
Can I use microbiocides to prevent HIV ?
No. Microbicides are gels, films, or suppositories that can kill or neutralize viruses and bacteria. Researchers are studying both vaginal and rectal microbicides to see if they can prevent sexual transmission of HIV, but none are currently available for use.
Can male circumcision prevent HIV ?
Circumcised men are less likely than uncircumcised men to get HIV from HIV-positive female partners, but circumcision doesn’t decrease their risk as much as other prevention options. There is no evidence that male circumcision decreases a woman’s risk of getting HIV, and the evidence about the benefits of circumcision among gay and bisexual men is inconclusive.
Circumcised men should take other actions, like using condoms the right way every time they have sex or taking medicine to prevent or treat HIV, to further reduce their risk of getting HIV or to protect their partners.
Can I take medicines to prevent getting HIV ?
If you are at very high risk for HIV from sex or injecting drugs, taking HIV medicines daily, called pre-exposure prophylaxis (or PrEP), can greatly reduce your risk of HIV infection. You can combine additional strategies with PrEP to reduce your risk even further.
Federal guidelines recommend that PrEP be considered for people who are HIV-negative and at very high risk for HIV. This includes anyone who is in an ongoing sexual relationship with an HIV-positive partner. It also includes anyone who:
- Is not in a mutually monogamous* relationship with a partner who recently tested HIV-negative, and
- Is a
- gay or bisexual man who has had anal sex without a condom or been diagnosed with an STD in the past 6 months;
- man who has sex with both men and women; or
- heterosexual man or woman who does not regularly use condoms during sex with partners of unknown HIV status who are at substantial risk of HIV infection (for example, people who inject drugs or women who have bisexual male partners).
PrEP is also recommended for people who’ve injected drugs in the past 6 months and have shared needles or works or been in drug treatment in the past 6 months.
If you have a partner who is HIV-positive and are considering getting pregnant, talk to your doctor about PrEP. It may be an option to help protect you and your baby.
PrEP involves daily medication and regular visits to a health care provider.
Can I take medicines to prevent HIV after exposure ?
Yes. Taking medicine after being potentially exposed to HIV, called post-exposure prophylaxis (or PEP), can keep you from becoming infected. But PEP must be started within 72 hours after a possible exposure.
If you think you’ve recently been exposed to HIV during sex (for example, if the condom breaks) or through sharing needles and works to prepare drugs (for example, cotton, cookers, water), talk to your health care provider or an emergency room doctor about PEP right away. The sooner you start PEP, the better; every hour counts. If you’re prescribed PEP, you’ll need to take it once or twice daily for 28 days.
Someone who is on PEP should continue to use condoms with sex partners and safe injection practices while taking PEP.
Can I get vaccinated to prevent HIV ?
No. There is currently no vaccine that will prevent HIV infection or treat those who have it.
If I’m living with HIV, how can I prevent passing it to others ?
There are many actions you can take to lower your risk of transmitting HIV to a partner. The more actions you take, the safer you can be.
- The most important thing you can do is to take medicines to treat HIV infection (called antiretroviral therapy, or ART) the right way, every day. These medicines reduce the amount of virus (viral load) in your blood and body fluids. They can keep you healthy for many years and greatly reduce your chance of transmitting HIV to your partners if you have a very low or undetectable viral load.
- If you’re taking medicines to treat HIV (ART), follow your health care provider’s advice. Visit your health care provider regularly and always take your medicines as directed.
- Use condoms the right way every time you have sex. Learn the right way to use a male condom.
- Choose less risky sexual behaviors. Anal sex is the highest-risk sexual activity for HIV transmission. If your partner is HIV-negative, it’s less risky if they’re the insertive partner (top) and you’re the receptive partner (bottom) during anal sex. Oral sex is much less risky than anal or vaginal sex. Sexual activities that don’t involve contact with body fluids (semen, vaginal fluid, or blood) carry no risk of HIV transmission.
- If you inject drugs, never share your needles or works with anyone.
- Talk to your partners about pre-exposure prophylaxis (PrEP), taking HIV medicines the right way, every day to prevent HIV infection. See Can I take medicines to prevent getting HIV?
- Talk to your partners about post-exposure prophylaxis (PEP) if you think they’ve recently had a possible exposure to HIV (for example, if they had anal or vaginal sex without a condom or if the condom broke during sex). Your partners should talk to a health care provider right away (within 72 hours) after a possible exposure. Starting PEP immediately and taking it daily for 28 days will reduce their chance of getting HIV.
- Get tested and treated for other STDs and encourage your partners to do the same. If you are sexually active, get tested at least once a year. STDs can have long-term health consequences. They can also increase the risk of getting or transmitting HIV. Find an STD testing site.
Also, encourage your partners who are HIV-negative to get tested for HIV so they are sure about their status and can take action to keep themselves healthy.
How can I prevent getting HIV from drug use ?
Stopping injection and other drug use can lower your chances of getting or transmitting HIV a lot. If you keep injecting drugs, use only sterile needles and works. Never share needles or works.
You are at very high risk for getting HIV if you use a needle or works after someone with HIV has used them. Also, when people are high, they’re more likely to have risky sex, which increases the chance of getting or transmitting HIV.
The best way to reduce your risk of HIV is to stop using drugs. You may need help to stop or cut down using drugs, but many resources are available. Talk with a counselor, doctor, or other health care provider about substance abuse treatment.
If you keep injecting drugs, here are some things you can do to lower your risk for getting HIV and other infections:
- Use only new, sterile needles and works each time you inject. Many communities have needle exchange programs where you can get new needles and works, and some pharmacies may sell needles without a prescription.
- Never share needles or works.
- Clean used needles with bleach only when you can’t get new ones. Bleaching a needle may reduce the risk of HIV but doesn’t eliminate it.
- Use sterile water to fix drugs.
- Clean your skin with a new alcohol swab before you inject.
- Be careful not to get someone else’s blood on your hands or your needle or works.
- Dispose of needles safely after one use. Use a sharps container, or keep used needles away from other people.
- Get tested for HIV at least once a year.
- Ask your doctor about taking daily medicine to prevent HIV (called pre-exposure prophylaxis or PrEP).
- Don’t have sex if you’re high. If you do have sex, use a condom the right way every time. Learn the right way to use a male condom.
HIV Symptoms
You cannot rely on symptoms to tell whether you have HIV. The only way to know for sure if you have HIV is to get tested. Knowing your status is important because it helps you make healthy decisions to prevent getting or transmitting HIV.
The symptoms of HIV and AIDS vary, depending on the phase of infection 5.
Primary infection (Acute HIV Infection)
About 40% to 90% of people have flu-like symptoms within 2-4 weeks after HIV infection. Other people do not feel sick at all during this stage. This illness, known as primary or acute HIV infection, may last for a few days to several weeks. Possible signs and symptoms include:
- Fever
- Chills
- Night sweats
- Fatigue
- Headache
- Muscle aches and joint pain
- Rash
- Sore throat
- Swollen lymph glands, mainly on the neck
- Mouth ulcers
You should not assume you have HIV just because you have any of these symptoms. Each of these symptoms can be caused by other illnesses. And some people who have HIV do not show any symptoms at all for 10 years or more.
Although the symptoms of primary HIV infection may be mild enough to go unnoticed, the amount of virus in the bloodstream (viral load) is particularly high at this time.
During this time, HIV infection may not show up on some types of HIV tests, but people who have it are highly infectious and can spread the infection to others. As a result, HIV infection spreads more efficiently during primary infection than during the next stage of infection.
However, if you think you may have been exposed to HIV and could be in the early stage of HIV infection, get an HIV test. Most HIV tests detect antibodies (proteins your body makes as a reaction against the presence of HIV), not HIV itself. But it take can take a few weeks or longer for your body to produce these antibodies.
Some places use HIV tests that can detect acute and recent infections, but others do not. So be sure to let your testing site know if you think you may have been recently infected with HIV. Tests that can detect acute infection look for HIV RNA or p24 antigen. Most doctors and clinics that provide a full range of health care services can do this test, but some places that only do HIV testing may not have it. So you may want to contact the site before you go to ask if they can test you for acute HIV infection.
After you get tested, it’s important to find out the result of your test. If you’re HIV-positive, you should see a doctor and start HIV treatment as soon as possible. You are at high risk of transmitting HIV to others during the early stage of HIV infection, even if you have no symptoms. For this reason, it is very important to take steps to reduce your risk of transmission. If you’re HIV-negative, explore HIV-prevention options, like pre-exposure prophylaxis (PrEP), that can help you stay negative.
Clinical latent infection (Chronic HIV Infection)
After the early stage of HIV infection, the disease moves into a stage called the clinical latency stage (also called “chronic HIV infection”). During this stage, HIV is still active but reproduces at very low levels. People with chronic HIV infection may not have any HIV-related symptoms, or only mild ones.
In some people, persistent swelling of lymph nodes occurs during clinical latent HIV. Otherwise, there are no specific signs and symptoms. HIV remains in the body, however, and in infected white blood cells.
Clinical latent infection generally lasts around 10 years if you’re not receiving antiretroviral therapy. This phase can last for decades in people taking antiretroviral medications. But some people progress to more severe disease much sooner.
It’s important to remember that people can still transmit HIV to others during this phase even if they have no symptoms, although people who are on ART and stay virally suppressed (having a very low level of virus in their blood) are much less likely to transmit HIV than those who are not virally suppressed.
Early symptomatic HIV infection
As the virus continues to multiply and destroy immune cells, you may develop mild infections or chronic signs and symptoms such as:
- Fever
- Fatigue
- Swollen lymph nodes — often one of the first signs of HIV infection
- Diarrhea
- Weight loss
- Oral yeast infection (thrush)
- Shingles (herpes zoster)
Progression to AIDS
If you receive no treatment for your HIV infection, the disease typically progresses to AIDS in about 10 years. By the time AIDS develops, your immune system has been severely damaged, making you susceptible to opportunistic infections — diseases that wouldn’t usually trouble a person with a healthy immune system.
The signs and symptoms of some of these infections may include:
- Soaking night sweats
- Recurring fever
- Chronic diarrhea
- Persistent white spots or unusual lesions on your tongue or in your mouth
- Persistent, unexplained fatigue
- Weight loss
- Skin rashes or bumps
When to see a doctor
If you think you may have been infected with HIV or are at risk of contracting the virus, see a health care provider as soon as possible.
Causes of HIV and AIDS
HIV is a viral infection that can be transmitted through sexual contact, through blood or from mother to child during pregnancy, childbirth or breast-feeding.
How does HIV become AIDS ?
HIV destroys CD4 cells — a specific type of white blood cell that plays a large role in helping your body fight disease. Your immune system weakens as more CD4 cells are killed. You can have an HIV infection for years before it progresses to AIDS.
People infected with HIV progress to AIDS when their CD4 count falls below 200 or they experience an AIDS-defining complication.
How HIV is transmitted
To become infected with HIV, infected blood, semen or vaginal secretions must enter your body. You can’t become infected through ordinary contact — hugging, kissing, dancing or shaking hands — with someone who has HIV or AIDS. HIV can’t be transmitted through the air, water or insect bites.
You can become infected with HIV in several ways, including:
- By having sex. You may become infected if you have vaginal, anal or oral sex with an infected partner whose blood, semen or vaginal secretions enter your body. The virus can enter your body through mouth sores or small tears that sometimes develop in the rectum or vagina during sexual activity.
- From blood transfusions. In some cases, the virus may be transmitted through blood transfusions. American hospitals and blood banks now screen the blood supply for HIV antibodies, so this risk is very small.
- By sharing needles. HIV can be transmitted through needles and syringes contaminated with infected blood. Sharing intravenous drug paraphernalia puts you at high risk of HIV and other infectious diseases, such as hepatitis.
- During pregnancy or delivery or through breast-feeding. Infected mothers can infect their babies. But by receiving treatment for HIV infection during pregnancy, mothers significantly lower the risk to their babies.
Risk factors for HIV and AIDS
When HIV/AIDS first surfaced in the United States, it mainly affected men who had sex with men. However, now it’s clear that HIV is also spread through heterosexual sex.
Anyone of any age, race, sex or sexual orientation can be infected, but you’re at greatest risk of HIV/AIDS if you:
- Have unprotected sex. Unprotected sex means having sex without using a new latex or polyurethane condom every time. Anal sex is more risky than is vaginal sex. The risk increases if you have multiple sexual partners.
- Have another STI. Many sexually transmitted infections (STIs) produce open sores on your genitals. These sores act as doorways for HIV to enter your body.
- Use intravenous drugs. People who use intravenous drugs often share needles and syringes. This exposes them to droplets of other people’s blood.
- Are an uncircumcised man. Studies indicate that lack of circumcision increases the risk of heterosexual transmission of HIV.
Complications of HIV and AIDS
HIV infection weakens your immune system, making you highly susceptible to numerous infections and certain types of cancers.
Infections common to HIV/AIDS
- Tuberculosis (TB). In resource-poor nations, TB is the most common opportunistic infection associated with HIV and a leading cause of death among people with AIDS.
- Cytomegalovirus. This common herpes virus is transmitted in body fluids such as saliva, blood, urine, semen and breast milk. A healthy immune system inactivates the virus, and it remains dormant in your body. If your immune system weakens, the virus resurfaces — causing damage to your eyes, digestive tract, lungs or other organs.
- Candidiasis. Candidiasis is a common HIV-related infection. It causes inflammation and a thick, white coating on the mucous membranes of your mouth, tongue, esophagus or vagina.
- Cryptococcal meningitis. Meningitis is an inflammation of the membranes and fluid surrounding your brain and spinal cord (meninges). Cryptococcal meningitis is a common central nervous system infection associated with HIV, caused by a fungus found in soil.
- Toxoplasmosis. This potentially deadly infection is caused by Toxoplasma gondii, a parasite spread primarily by cats. Infected cats pass the parasites in their stools, and the parasites may then spread to other animals and humans.
- Cryptosporidiosis. This infection is caused by an intestinal parasite that’s commonly found in animals. You contract cryptosporidiosis when you ingest contaminated food or water. The parasite grows in your intestines and bile ducts, leading to severe, chronic diarrhea in people with AIDS.
Cancers common to HIV/AIDS
Kaposi’s sarcoma. A tumor of the blood vessel walls, this cancer is rare in people not infected with HIV, but common in HIV-positive people.
Kaposi’s sarcoma usually appears as pink, red or purple lesions on the skin and mouth. In people with darker skin, the lesions may look dark brown or black. Kaposi’s sarcoma can also affect the internal organs, including the digestive tract and lungs.
Lymphomas. This type of cancer originates in your white blood cells and usually first appears in your lymph nodes. The most common early sign is painless swelling of the lymph nodes in your neck, armpit or groin.
Other complications
Wasting syndrome. Aggressive treatment regimens have reduced the number of cases of wasting syndrome, but it still affects many people with AIDS. It’s defined as a loss of at least 10 percent of body weight, often accompanied by diarrhea, chronic weakness and fever.
Neurological complications. Although AIDS doesn’t appear to infect the nerve cells, it can cause neurological symptoms such as confusion, forgetfulness, depression, anxiety and difficulty walking. One of the most common neurological complications is AIDS dementia complex, which leads to behavioral changes and diminished mental functioning.
Kidney disease. HIV-associated nephropathy (HIVAN) is an inflammation of the tiny filters in your kidneys that remove excess fluid and wastes from your bloodstream and pass them to your urine. Because of a genetic predisposition, the risk of developing HIVAN is much higher in blacks.
Regardless of CD4 count, antiretroviral therapy should be started in those diagnosed with HIV.
Tests and Diagnosis for HIV
HIV is most commonly diagnosed by testing your blood or saliva for antibodies to the virus. Unfortunately, it takes time for your body to develop these antibodies — usually up to 12 weeks.
A newer type of test that checks for HIV antigen, a protein produced by the virus immediately after infection, can quickly confirm a diagnosis soon after infection. An earlier diagnosis may prompt people to take extra precautions to prevent transmission of the virus to others.
Home test
A Food and Drug Administration-approved home test is available. To do the test, you swab fluid from your upper and lower gums. If the test is positive, you need to see your doctor to confirm the diagnosis and discuss your treatment options. If the test is negative, it needs to be repeated in three months to confirm the results.
Tests to tailor treatment
If you receive a diagnosis of HIV/AIDS, several types of tests can help your doctor determine what stage of the disease you have. These tests include:
- CD4 count. CD4 cells are a type of white blood cell that’s specifically targeted and destroyed by HIV. Even if you have no symptoms, HIV infection progresses to AIDS when your CD4 count dips below 200.
- Viral load. This test measures the amount of virus in your blood. Studies have shown that people with higher viral loads generally fare more poorly than do those with a lower viral load.
- Drug resistance. This blood test determines whether the strain of HIV you have will be resistant to certain anti-HIV medications.
Tests for complications
Your doctor might also order lab tests to check for other infections or complications, including:
- Tuberculosis
- Hepatitis
- Toxoplasmosis
- Sexually transmitted infections
- Liver or kidney damage
- Urinary tract infection.
What kinds of tests are available and how do they work ?
There are three types of tests available:
- Nucleic acid tests (NAT),
- Antigen/antibody tests, and
- Antibody tests.
HIV tests are typically performed on blood or oral fluid.
Nucleic acid tests (NAT)
A NAT looks for the actual virus in the blood. The test can give either a positive/negative result or an amount of virus present in the blood (known as an HIV viral load test). This test is very expensive and not routinely used for screening individuals unless they recently had a high-risk exposure or a possible exposure and they have early symptoms of HIV infection. Nucleic acid testing is usually considered accurate during the early stages of infection. However, it is best to get an antibody or antigen/antibody test at the same time to help the health care provider understand what a negative NAT means. Taking pre-exposure prophylaxis (PrEP) or post-exposure prophylaxis (PEP) may also reduce the accuracy of NAT if you have HIV.
Antigen/antibody tests
An antigen/antibody test looks for both HIV antibodies and antigens. Antibodies are produced by your immune system when you’re exposed to bacteria or viruses like HIV. Antigens are foreign substances that cause your immune system to activate. If you’re infected with HIV, an antigen called p24 is produced even before antibodies develop. Antigen/antibody tests are recommended for testing done in labs and are now common in the United States. There is also a rapid antigen/antibody test available.
Antibody tests
- Most rapid tests and home tests are antibody tests. HIV antibody tests look for antibodies to HIV in your blood or oral fluid. In general, antibody tests that use blood from a vein can detect HIV sooner after infection than tests done with blood from a finger prick or with oral fluid.
- While most laboratories are now using antigen/antibody tests, laboratory-based antibody screening tests are still available. These tests require blood to be drawn from your vein into a tube and then that blood is sent to a laboratory for testing. The results may take several days to be available.
- With a rapid antibody screening test, results are ready in 30 minutes or less. These tests are used in clinical and nonclinical settings, usually with blood from a finger prick or with oral fluid.
- The oral fluid antibody self-test provides fast results. You have to swab your own mouth to collect an oral fluid sample and use a kit to test it. Results are available in 20 minutes. The manufacturer provides confidential counseling and referral to follow-up testing sites. These tests are available for purchase in stores and online. They may be used at home, or they may be used for testing in some community and clinic testing programs.
- The home collection kit involves pricking your finger to collect a blood sample, sending the sample by mail to a licensed laboratory, and then calling in for results as early as the next business day. This antibody test is anonymous. The manufacturer provides confidential counseling and referral to treatment.
If you use any type of antibody test and have a positive result, you will need to take a follow-up test to confirm your results. If your first test is a rapid home test and it’s positive, you will be sent to a health care provider to get follow-up testing. If your first test is done in a testing lab and it’s positive, the lab will conduct the follow-up testing, usually on the same blood sample as the first test.
Talk to your health care provider to see what type of HIV test is right for you.
After you get tested, it’s important for you to find out the result of your test so that you can talk to your health care provider about treatment options if you’re HIV-positive. If you’re HIV-negative, continue to take actions to prevent HIV, like using condoms the right way every time you have sex and taking medicines to prevent HIV if you’re at high risk.
How soon after an exposure to HIV can a HIV test detect if I am infected ?
No HIV test can detect HIV immediately after infection.
- If you think you’ve been exposed to HIV in the last 72 hours, talk to your health care provider about post-exposure prophylaxis (PEP), right away.
The time between when a person may have been exposed to HIV and when a test can tell for sure whether they have HIV is called the window period. The window period varies from person to person and depends on the type of test used to detect HIV.
- A nucleic acid test (NAT) can usually tell you if you are infected with HIV 10 to 33 days after an exposure.
- An antigen/antibody test performed by a laboratory on blood from a vein can usually detect HIV infection 18 to 45 days after an exposure. Antigen/ antibody tests done with blood from a finger prick can take longer to detect HIV (18 to 90 days after an exposure). When the goal is to tell for sure that a person does not have HIV, an antigen/antibody test performed by a laboratory on blood from a vein is preferred.
- Antibody tests can usually take 23 to 90 days to reliably detect HIV infection. Most rapid tests and home tests are antibody tests. In general, antibody tests that use blood from a vein can detect HIV sooner after infection than tests done with blood from a finger prick or with oral fluid.
Ask your health care provider about the window period for the test you’re taking. If you’re using a home test, you can get that information from the materials included in the test’s package. If you get an HIV test after a potential HIV exposure and the result is negative, get tested again after the window period for the test you’re taking to be sure. If your health care provider uses an antigen/antibody test performed by a laboratory on blood from a vein you should get tested again 45 days after your most recent exposure. For other tests, you should test again at least 90 days after your most recent exposure to tell for sure if you have HIV.
If you learned you were HIV-negative the last time you were tested, you can only be sure you’re still negative if you haven’t had a potential HIV exposure since your last test. If you’re sexually active, continue to take actions to prevent HIV, like using condoms the right way every time you have sex and taking medicines to prevent HIV if you’re at high risk.
Learn the right way to use a male condom and female condom.
What does a positive HIV test mean ?
A follow-up test will be conducted. If the follow-up test is also positive, it means you are living with HIV (or HIV-positive).
If you had a rapid screening test, the testing site will arrange a follow-up test to make sure the screening test result was correct. If your blood was tested in a lab, the lab will conduct a follow-up test on the same sample.
It is important that you start medical care and begin HIV treatment as soon as you are diagnosed with HIV. Antiretroviral therapy or ART (taking medicines to treat HIV infection) is recommended for all people with HIV, regardless of how long they’ve had the virus or how healthy they are. ART works by lowering the amount of virus in your body to very low levels, called viral suppression. It slows the progression of HIV and helps protect your immune system. If you are on ART and virally suppressed, you can stay healthy for many years, and greatly reduce your chance of transmitting HIV to sex partners.
If you have health insurance, your insurer is required to cover some medicines used to treat HIV. If you don’t have health insurance, or you’re unable to afford your co-pay or co-insurance amount, you may be eligible for government programs that can help through Medicaid, Medicare, the Ryan White HIV/AIDS Program, and community health centers. Your health care provider or local public health department can tell you where to get HIV treatment.
To lower your risk of transmitting HIV:
- Take medicines to treat HIV (antiretroviral therapy or ART) the right way every day. Being on ART and getting and staying virally suppressed is the most effective thing you can do to reduce the chance of transmitting HIV.
- Use condoms the right way every time you have sex. Learn the right way to use a male condom and female condom.
- If your partner is HIV-negative, encourage them to talk to their health care provider to see if taking daily medicine to prevent HIV (called pre-exposure prophylaxis, or PrEP) is right for them.
- If you think your partner might have been recently exposed to HIV—for example, if the condom breaks during sex and you aren’t virally suppressed—they should talk to a health care provider as soon as possible within the next 3 days (72 hours) about taking medicines (called post-exposure prophylaxis, or PEP) to prevent getting HIV.
- Get tested and treated for STDs and encourage your partner to do the same.
Receiving a diagnosis of HIV can be a life-changing event. People can feel many emotions—sadness, hopelessness, or anger. Allied health care providers and social service providers, often available at your health care provider’s office, will have the tools to help you work through the early stages of your diagnosis and begin to manage your HIV.
Talking to others who have HIV may also be helpful. Find a local HIV support group. Learn about how other people living with HIV have handled their diagnosis.
If I test positive for HIV, does that mean I have AIDS ?
No. Being HIV-positive does not mean you have AIDS. AIDS is the most advanced stage of HIV disease. HIV can lead to AIDS if a person does not get treatment or take care of their health.
It’s important to share your status with your sex partners. Whether you disclose your status to others is your decision.
Partners
It’s important to disclose your HIV status to your sex partners even if you’re uncomfortable doing it. Communicating with each other about your HIV status means you can take steps to keep both of you healthy. The more practice you have disclosing your HIV status, the easier it will become.
Many resources can help you learn ways to disclose your status to your partners.
If you’re nervous about disclosing your test result, or you have been threatened or injured by your partner, you can ask your doctor or the local health department to tell them that they might have been exposed to HIV. This is called partner notification services. Health departments do not reveal your name to your partners. They will only tell your partners that they have been exposed to HIV and should get tested.
Many states have laws that require you to tell your sexual partners if you’re HIV-positive before you have sex (anal, vaginal, or oral) or tell your drug-using partners before you share drugs or needles to inject drugs. In some states, you can be charged with a crime if you don’t tell your partner your HIV status, even if your partner doesn’t become infected.
Family and friends
In most cases, your family and friends will not know your test results or HIV status unless you tell them yourself. While telling your family that you have HIV may seem hard, you should know that disclosure has many benefits—studies have shown that people who disclose their HIV status respond better to treatment than those who don’t. And telling friends and family can provide an important source of support in managing your HIV.
If you are under 18, however, some states allow your health care provider to tell your parent(s) that you received services for HIV if they think doing so is in your best interest.
Employers
In most cases, your employer will not know your HIV status unless you tell them. But your employer does have a right to ask if you have any health conditions that would affect your ability to do your job or pose a serious risk to others. (An example might be a health care professional, like a surgeon, who does procedures where there is a risk of blood or other body fluids being exchanged.)
If you have health insurance through your employer, the insurance company cannot legally tell your employer that you have HIV. But it is possible that your employer could find out if the insurance company provides detailed information to your employer about the benefits it pays or the costs of insurance.
All people with HIV are covered under the Americans with Disabilities Act. This means that your employer cannot discriminate against you because of your HIV status as long as you can do your job.
What does a negative test result mean ?
A negative result doesn’t necessarily mean that you don’t have HIV. That’s because of the window period— the time between when a person may have been exposed to HIV and when a test can tell for sure whether they have HIV. The window period varies from person to person and is also different depending upon the type of HIV test.
Ask your health care provider about the window period for the test you’re taking. If you’re using a home test, you can get that information from the materials included in the test’s package. If you get an HIV test after a potential HIV exposure and the result is negative, get tested again after the window period for the test you’re taking to be sure. For example, if your health care provider uses an antigen/antibody test performed by a laboratory with blood from a vein you should get tested again 45 days after your most recent exposure. For other tests, you should test again at least 90 days after your most recent exposure to tell for sure if you have HIV.
If you learned you were HIV-negative the last time you were tested, you can only be sure you’re still negative if you haven’t had a potential HIV exposure since your last test. If you’re sexually active, continue to take actions to prevent HIV, like using condoms the right way every time you have sex and taking medicines to prevent HIV if you’re at high risk.
Learn the right way to use a male condom and female condom.
If I have a negative result, does that mean my partner is HIV-negative also ?
No. Your HIV test result reveals only your HIV status.
HIV is not necessarily transmitted every time you have sex. Therefore, taking an HIV test is not a way to find out if your partner is infected.
It’s important to be open with your partners and ask them to tell you their HIV status. But keep in mind that your partners may not know or may be wrong about their status, and some may not tell you if they have HIV even if they are aware of their status. Consider getting tested together so you can both know your HIV status and take steps to keep yourselves healthy.
Treatments and drugs for HIV and AIDS
There’s no cure for HIV/AIDS, but a variety of drugs can be used in combination to control the virus. Each class of anti-HIV drugs blocks the virus in different ways. It’s best to combine at least three drugs from two classes to avoid creating strains of HIV that are immune to single drugs.
The classes of anti-HIV drugs include:
- Non-nucleoside reverse transcriptase inhibitors (NNRTIs). NNRTIs disable a protein needed by HIV to make copies of itself. Examples include efavirenz (Sustiva), etravirine (Intelence) and nevirapine (Viramune).
- Nucleoside or nucleotide reverse transcriptase inhibitors (NRTIs). NRTIs are faulty versions of building blocks that HIV needs to make copies of itself. Examples include Abacavir (Ziagen), and the combination drugs emtricitabine-tenofovir (Truvada), and lamivudine-zidovudine (Combivir).
- Protease inhibitors (PIs). PIs disable protease, another protein that HIV needs to make copies of itself. Examples include atazanavir (Reyataz), darunavir (Prezista), fosamprenavir (Lexiva) and indinavir (Crixivan).
- Entry or fusion inhibitors. These drugs block HIV’s entry into CD4 cells. Examples include enfuvirtide (Fuzeon) and maraviroc (Selzentry).
- Integrase inhibitors. These drugs work by disabling integrase, a protein that HIV uses to insert its genetic material into CD4 cells. Examples include raltegravir (Isentress), elvitegravir (Vitekta) and dolutegravir (Tivicay).
When to start treatment
Everyone with HIV infection, regardless of CD4 count, should be offered antiviral medication.
HIV therapy is particularly important for the following situations:
- You have severe symptoms.
- You have an opportunistic infection.
- Your CD4 count is under 350.
- You’re pregnant.
- You have HIV-related kidney disease.
- You’re being treated for hepatitis B or C.
Treatment can be difficult
HIV treatment regimens may involve taking multiple pills at specific times every day for the rest of your life.
Side effects of treatment can include:
- Nausea, vomiting or diarrhea
- Heart disease
- Weakened bones or bone loss
- Breakdown of muscle tissue (rhabdomyolysis)
- Abnormal cholesterol levels
- Higher blood sugar levels
Other diseases and treatment
Some health issues that are a natural part of aging may be more difficult to manage if you have HIV. Some medications that are common for age-related cardiovascular, metabolic and bone conditions, for example, may not interact well with anti-HIV medications. Talk to your doctor about other conditions for which you’re taking medication.
Treatment response
Your doctor will monitor your viral load and CD4 counts to determine your response to treatment. Viral load should be tested at the start of treatment and then every three to four months during therapy. CD4 counts should be checked every three to six months.
HIV treatment should reduce your viral load to the point that it’s undetectable. That doesn’t mean your HIV is gone. It just means that the test isn’t sensitive enough to detect it. You can still transmit HIV to others when your viral load is undetectable.
Lifestyle and home remedies
Although it’s important to receive medical treatment for HIV/AIDS, it’s also essential to take an active role in your own care. The following suggestions may help you stay healthy longer:
- Eat healthy foods. Emphasize fresh fruits and vegetables, whole grains, and lean protein. Healthy foods help keep you strong, give you more energy and support your immune system.
- Avoid certain foods. Foodborne illnesses can be especially severe in people who are infected with HIV. Avoid unpasteurized dairy products, raw eggs and raw seafood such as oysters, sushi or sashimi. Cook meat until it’s well-done.
- Get immunizations. These may prevent infections such as pneumonia and the flu. Make sure the vaccines don’t contain live viruses, which can be dangerous for people with weakened immune systems.
- Take care with companion animals. Some animals may carry parasites that can cause infections in people who are HIV-positive. Cat feces can cause toxoplasmosis, reptiles can carry salmonella, and birds can carry the fungus cryptococcus or histoplasmosis. Wash hands thoroughly after handling pets or emptying the litter box.
Alternative medicine
People who are infected with HIV sometimes try dietary supplements that claim to boost the immune system or counteract side effects of anti-HIV drugs.
Supplements that may be helpful
- Acetyl-L-carnitine. Researchers have used acetyl-L-carnitine to treat nerve pain in people with diabetes. It’s possible that acetyl-L-carnitine might help nerve pain linked to HIV. But it may be helpful only if you’re already deficient in acetyl-L-carnitine.
- Whey protein. Preliminary evidence indicates that whey protein, a cheese byproduct, can help some people with HIV gain weight. Whey protein also appears to reduce diarrhea and increase CD4 counts.
Supplements that may be dangerous
- St. John’s wort. Commonly used to combat depression, St. John’s wort can reduce the effectiveness of several types of anti-HIV drugs by more than 50 percent.
- Garlic supplements. Although garlic may help strengthen the immune system, garlic supplements also interact with several anti-HIV drugs — reducing their effectiveness by 50 percent. Occasionally eating garlic in food appears to be safe.
Be sure to discuss the use of any dietary supplement with your doctor before trying it to ensure that it won’t adversely interact with any of your medications.
Coping and support
Receiving a diagnosis of any life-threatening illness is devastating. But the emotional, social and financial consequences of HIV/AIDS can make coping with this illness especially difficult — not only for you but also for those closest to you.
Fortunately, numerous services and resources are available to people with HIV. Most HIV/AIDS clinics have social workers, counselors or nurses who can help you with problems directly or put you in touch with people who can. They may be able to arrange transportation to and from doctor appointments, help with housing and child care, deal with employment and legal issues, and see you through financial emergencies.
Coming to terms with your illness may be the hardest thing you’ve ever done. For some people, having a strong faith or a sense of something greater than themselves makes this process easier. Others seek counseling from someone who understands HIV/AIDS. Still others make a conscious decision to experience their lives as fully and intensely as they can or to help other people who have the disease.
What is AIDS
AIDS (acquired immunodeficiency syndrome), the late stage of HIV infection.
AIDS Symptoms can include:
- Rapid weight loss
- Recurring fever or profuse night sweats
- Extreme and unexplained tiredness
- Prolonged swelling of the lymph glands in the armpits, groin, or neck
- Diarrhea that lasts for more than a week
- Sores of the mouth, anus, or genitals
- Pneumonia
- Red, brown, pink, or purplish blotches on or under the skin or inside the mouth, nose, or eyelids
- Memory loss, depression, and other neurologic disorders
Each of these symptoms can also be related to other illnesses. So the only way to know for sure if you have HIV is to get tested.
Many of the severe symptoms and illnesses of HIV disease come from the opportunistic infections that occur because your body’s immune system has been damaged.
What Are Opportunistic Infections ?
Opportunistic infections are infections that occur more frequently and are more severe in individuals with weakened immune systems, including people with HIV. People are at greatest risk for opportunistic infections when their CD4 count falls below 200, but you can get some opportunistic infections when your CD4 count is below 500.
Opportunistic infections are less common now than they were in the early days of HIV and AIDS because better treatments reduce the amount of HIV in a person’s body and keep a person’s immune system stronger. However, many people with HIV still develop opportunistic infections because they did not know they had HIV for many years after they were infected. Others people who know they have HIV can get opportunistic infections because they are not taking antiretroviral treatment (ART); they are on ART, but it is failing and the virus has weakened their immune system; or they have AIDS but are not taking medication to prevent opportunistic infections.
Staying in care and getting your lab tests done is one of the most important things you can do to prevent opportunistic infections. This will allow your provider to know when you might be at risk for opportunistic infections and work with you to prevent them. Some opportunistic infections can be prevented by taking additional medication that is used to prevent that opportunistic infection.
If you do develop an opportunistic infection, there are treatments available, such as antibiotics or antifungal drugs. Having an opportunistic infection may be a very serious medical situation and its treatment can be challenging. The best way to prevent opportunistic infections is to reduce your risk by staying in care, taking ART every day, and keeping your viral load undetectable or very low so that your immune system can stay strong.
Table 1. Most common opportunistic infections
| Candidiasis of bronchi, trachea, esophagus, or lungs | This illness is caused by infection with a common (and usually harmless) type of fungus called Candida. Candidiasis, or infection with Candida, can affect the skin, nails, and mucous membranes throughout the body. Persons with HIV infection often have trouble with Candida, especially in the mouth and vagina. However, candidiasis is only considered an OI when it infects the esophagus (swallowing tube) or lower respiratory tract, such as the trachea and bronchi (breathing tube), or deeper lung tissue. |
| Invasive cervical cancer | This is a cancer that starts within the cervix, which is the lower part of the uterus at the top of the vagina, and then spreads (becomes invasive) to other parts of the body. This cancer can be prevented by having your care provider perform regular examinations of the cervix |
| Coccidioidomycosis | This illness is caused by the fungus Coccidioides immitis. It most commonly acquired by inhaling fungal spores, which can lead to a pneumonia that is sometimes called desert fever, San Joaquin Valley fever, or valley fever. The disease is especially common in hot, dry regions of the southwestern United States, Central America, and South America. |
| Cryptococcosis | This illness is caused by infection with the fungus Cryptococcus neoformans. The fungus typically enters the body through the lungs and can cause pneumonia. It can also spread to the brain, causing swelling of the brain. It can infect any part of the body, but (after the brain and lungs) infections of skin, bones, or urinary tract are most common. |
| Cryptosporidiosis, chronic intestinal (greater than one month’s duration) | This diarrheal disease is caused by the protozoan parasite Cryptosporidium. Symptoms include abdominal cramps and severe, chronic, watery diarrhea. |
| Cytomegalovirus diseases (particularly retinitis) (CMV) | This virus can infect multiple parts of the body and cause pneumonia, gastroenteritis (especially abdominal pain caused by infection of the colon), encephalitis (infection) of the brain, and sight-threatening retinitis (infection of the retina at the back of eye). People with CMV retinitis have difficulty with vision that worsens ever time. CMV retinitis is a medical emergency because it can cause blindness if not treated promptly. |
| Encephalopathy, HIV-related | This brain disorder is a result of HIV infection. It can occur as part of acute HIV infection or can result from chronic HIV infection. Its exact cause is unknown but it is thought to be related to infection of the brain with HIV and the resulting inflammation. |
| Herpes simplex (HSV): chronic ulcer(s) (greater than one month’s duration); or bronchitis, pneumonitis, or esophagitis | Herpes simplex virus (HSV) is a very common virus that for most people never causes any major problems. HSV is usually acquired sexually or from an infected mother during birth. In most people with healthy immune systems, HSV is usually latent (inactive). However, stress, trauma, other infections, or suppression of the immune system, (such as by HIV), can reactivate the latent virus and symptoms can return. HSV can cause painful cold sores (sometime called fever blisters) in or around the mouth, or painful ulcers on or around the genitals or anus. In people with severely damaged immune systems, HSV can also cause infection of the bronchus (breathing tube), pneumonia (infection of the lungs) and esophagitis (infection of the esophagus, or swallowing tube). |
| Histoplasmosis | This illness is caused by the fungus Histoplasma capsulatum. Histoplasma most often infects the lungs and produces symptoms that are similar to those of influenza or pneumonia. People with severely damaged immune systems can get a very serious form of the disease called progressive disseminated histoplasmosis. This form of histoplasmosis can last a long time and involves organs other than the lungs. |
| Isosporiasis, chronic intestinal (greater than one month’s duration) | This infection is caused by the parasite Isospora belli, which can enter the body through contaminated food or water. Symptoms include diarrhea, fever, headache, abdominal pain, vomiting, and weight loss. |
| Kaposi’s sarcoma (KS) | This cancer, also known as KS, is caused by a virus called Kaposi’s sarcoma herpesvirus (KSHV) or human herpesvirus 8 (HHV-8). KS causes small blood vessels, called capillaries, to grow abnormally. Because capillaries are located throughout the body, KS can occur anywhere. KS appears as firm pink or purple spots on the skin that can be raised or flat. KS can be life-threatening when it affects organs inside the body, such the lung, lymph nodes or intestines. |
| Lymphoma, multiple forms | Lymphoma refers to cancer of the lymph nodes and other lymphoid tissues in the body. There are many different kinds of lymphomas. Some types, such as non-Hodgkin lymphoma and Hodgkin lymphoma, are associated with HIV infection. |
| Tuberculosis (TB) | Tuberculosis (TB) infection is caused by the bacteria Mycobacterium tuberculosis. TB can be spread through the air when a person with active TB coughs, sneezes, or speaks. Breathing in the bacteria can lead to infection in the lungs. Symptoms of TB in the lungs include cough, tiredness, weight loss, fever, and night sweats. Although the disease usually occurs in the lungs, it may also affect other parts of the body, most often the larynx, lymph nodes, brain, kidneys, or bones. |
| Mycobacterium avium complex (MAC) or Mycobacterium kansasii, disseminated or extrapulmonary. Other Mycobacterium, disseminated or extrapulmonary. | MAC is caused by infection with different types of mycobacterium: Mycobacterium avium, Mycobacterium intracellulare, or Mycobacterium kansasii. These mycobacteria live in our environment, including in soil and dust particles. They rarely cause problems for persons with healthy immune systems. In people with severely damaged immune systems, infections with these bacteria spread throughout the body and can be life-threatening. |
| Pneumocystis carinii pneumonia (PCP) | This lung infection, also called PCP, is caused by a fungus, which used to be called Pneumocystis carinii, but now is named Pneumocystis jirovecii. PCP occurs in people with weakened immune systems, including people with HIV. The first signs of infection are difficulty breathing, high fever, and dry cough. |
| Pneumonia, recurrent | Pneumonia is an infection in one or both of the lungs. Many germs, including bacteria, viruses, and fungi can cause pneumonia, with symptoms such as a cough (with mucous), fever, chills, and trouble breathing. In people with immune systems severely damaged by HIV, one of the most common and life-threatening causes of pneumonia is infection with the bacteria Streptococcus pneumoniae, also called Pneumococcus. There are now effective vaccines that can prevent infection with Streptococcus pneumoniae and all persons with HIV infection should be vaccinated. |
| Progressive multifocal leukoencephalopathy | This rare brain and spinal cord disease is caused by the JC virus. It is seen almost exclusively in persons whose immune systems have been severely damaged by HIV. Symptoms may include loss of muscle control, paralysis, blindness, speech problems, and an altered mental state. This disease often progresses rapidly and may be fatal. |
| Salmonella septicemia, recurrent | Salmonella are a kind of bacteria that typically enter the body through ingestion of contaminated food or water. Infection with salmonella (called salmonellosis) can affect anyone and usually causes a self-limited illness with nausea, vomiting, and diarrhea. Salmonella septicemia is a severe form of infection in which the bacteria circulate through the whole body and exceeds the immune system’s ability to control it. |
| Toxoplasmosis of brain | This infection, often called toxo, is caused by the parasite Toxoplasma gondii. The parasite is carried by warm-blooded animals including cats, rodents, and birds and is excreted by these animals in their feces. Humans can become infected with it by inhaling dust or eating food contaminated with the parasite. Toxoplasma can also occur in commercial meats, especially red meats and pork, but rarely poultry. Infection with toxo can occur in the lungs, retina of the eye, heart, pancreas, liver, colon, testes, and brain. Although cats can transmit toxoplasmosis, litter boxes can be changed safely by wearing gloves and washing hands thoroughly with soap and water afterwards. All raw red meats that have not been frozen for at least 24 hours should be cooked through to an internal temperature of at least 150oF. |
| Wasting syndrome due to HIV | Wasting is defined as the involuntary loss of more than 10% of one’s body weight while having experienced diarrhea or weakness and fever for more than 30 days. Wasting refers to the loss of muscle mass, although part of the weight loss may also be due to loss of fat. |
Preventing Opportunistic Infections
The best ways to prevent getting an opportunistic infection are to get into and stay on medical care and to take HIV medications as prescribed. Sometimes, your health care provider will also prescribe medications specifically to prevent certain opportunistic infections. By staying on HIV medications, you can keep the amount of HIV in your body as low as possible and keep your immune system healthy. It is especially important that you get regular check-ups and take all of your medications as prescribed by your care giver. Taking HIV medications is a life-long commitment.
In addition to taking HIV medications to keep your immune system strong, there are other steps you can take to prevent getting an opportunistic infection.
- Use condoms consistently and correctly to prevent exposure to sexually transmitted infections.
- Don’t share drug injection equipment. Blood with hepatitis C in it can remain in syringes and needles after use and the infection can be transmitted to the next user.
- Get vaccinated – your doctor can tell you what vaccines you need. If he or she doesn’t, you should ask.
- Understand what germs you are exposed to (such as tuberculosis or germs found in the stools, saliva, or on the skin of animals) and limit your exposure to them.
- Don’t consume certain foods, including undercooked eggs, unpasteurized (raw) milk and cheeses, unpasteurized fruit juices, or raw seed sprouts.
- Don’t drink untreated water such as water directly from lakes or rivers. Tap water in foreign countries is also often not safe. Use bottled water or water filters.
- Ask your doctor to review with you the other things you do at work, at home, and on vacation to make sure you aren’t exposed to an OI. For more information on international travel.
- HIV Basics. https://www.cdc.gov/hiv/basics/index.html[↩]
- Diagnoses of HIV Infection in the United States and Dependent Areas, 2014. https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-us.pdf[↩][↩]
- Oral Sex and HIV Risk. https://www.cdc.gov/hiv/risk/oralsex.html[↩]
- https://www.cdc.gov/NCHHSTP/Atlas/[↩]
- HIV/AIDS. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/hiv-aids/basics/symptoms/con-20013732[↩]
- Opportunistic Infections. https://www.cdc.gov/hiv/basics/livingwithhiv/opportunisticinfections.html[↩]