Contents
- What is scabies
- Scabies is contagious and mode of transmission
- Did I get scabies from my pet ?
- Can scabies be spread by swimming in a public pool ?
- Who gets scabies ?
- If I come in contact with a person who has scabies, should I treat myself ?
- When can I return to work if I am diagnosed with scabies ?
- How can I remove scabies mites from my house or carpet ?
- How can I remove scabies mites from my clothes ?
- Can I get scabies from sharing an office chair or cubicle that is used by a person diagnosed with scabies ?
- If a co-worker is diagnosed with scabies, what precautions must be taken? Should the office be sprayed or fumigated ?
- What is Crusted (Norwegian) Scabies
- What causes scabies ?
- What does scabies look like and symptoms
- Possible Complications of Scabies
- How is scabies diagnosed ?
- What is the treatment for scabies ?
- What is the outlook for scabies ?
- Prevention & Control of Scabies
- Scabies is contagious and mode of transmission
What is scabies
Scabies is a very itchy rash caused by a parasitic mite that burrows in the skin surface. Human scabies is caused by an infestation of the skin by the human itch mite (Sarcoptes scabiei var. hominis). The microscopic scabies mite burrows into the upper layer of the skin where it lives and lays its eggs. The most common symptoms of scabies are intense itching and a pimple-like skin rash. The scabies mite usually is spread by direct, prolonged, skin-to-skin contact with a person who has scabies.
Scabies is contagious and mode of transmission
Scabies occurs worldwide and affects people of all races and social classes. The adult female scabies mites burrow into the upper layer of the skin (epidermis) where they live and deposit their eggs. The microscopic scabies mite almost always is passed by direct, prolonged, skin-to-skin contact with a person who already is infested. An infested person can spread scabies even if he or she has no symptoms. Humans are the source of infestation; animals do not spread human scabies.
- Scabies can be passed easily by an infested person to his or her household members and sexual partners. Scabies in adults frequently is sexually acquired.
Scabies can spread rapidly under crowded conditions where close body contact is frequent. Institutions such as nursing homes, extended-care facilities, and prisons are often sites of scabies outbreaks. Child care facilities also are a common site of scabies infestations.
Did I get scabies from my pet ?
No. Animals do not spread human scabies. Pets can become infested with a different kind of scabies mite that does not survive or reproduce on humans but causes “mange” in animals. If an animal with “mange” has close contact with a person, the animal mite can get under the person’s skin and cause temporary itching and skin irritation. However, the animal mite cannot reproduce on a person and will die on its own in a couple of days. Although the person does not need to be treated, the animal should be treated because its mites can continue to burrow into the person’s skin and cause symptoms until the animal has been treated successfully.
Can scabies be spread by swimming in a public pool ?
Scabies is spread by prolonged skin-to-skin contact with a person who has scabies. Scabies sometimes also can be spread by contact with items such as clothing, bedding, or towels that have been used by a person with scabies, but such spread is very uncommon unless the infested person has crusted scabies.
Scabies is very unlikely to be spread by water in a swimming pool. Except for a person with crusted scabies, only about 10-15 scabies mites are present on an infested person; it is extremely unlikely that any would emerge from under wet skin.
Although uncommon, scabies can be spread by sharing a towel or item of clothing that has been used by a person with scabies.
Who gets scabies ?
Scabies affects families and communities worldwide. It is most common in children, young adults and the elderly. Factors leading to spread of scabies include:
- Poverty and overcrowding
- Institutional care, such as rest homes, hospitals, prisons
- Refugee camps
- Individuals with immune deficiency or that are immune suppressed
- Low rates of identification and proper treatment of the disease.
If I come in contact with a person who has scabies, should I treat myself ?
No. If a person thinks he or she might have scabies, he/she should contact a doctor. The doctor can examine the person, confirm the diagnosis of scabies, and prescribe an appropriate treatment. Products used to treat scabies in humans are available only with a doctor’s prescription.
Sleeping with or having sex with any scabies infested person presents a high risk for transmission. The longer a person has skin-to-skin exposure, the greater is the likelihood for transmission to occur. Although briefly shaking hands with a person who has non-crusted scabies could be considered as presenting a relatively low risk, holding the hand of a person with scabies for 5-10 minutes could be considered to present a relatively high risk of transmission. However, transmission can occur even after brief skin-to-skin contact, such as a handshake, with a person who has crusted scabies. In general, a person who has skin-to-skin contact with a person who has crusted scabies would be considered a good candidate for treatment.
To determine when prophylactic treatment should be given to reduce the risk of transmission, early consultation should be sought with a health care provider who understands:
- the type of scabies (i.e. non-crusted vs crusted) to which a person has been exposed;
- the degree and duration of skin exposure that a person has had to the infested patient;
- whether the exposure occurred before or after the patient was treated for scabies; and,
- whether the exposed person works in an environment where he/she would be likely to expose other people during the asymptomatic incubation period. For example, a nurse or caretaker who works in a nursing home or hospital often would be treated prophylactically to reduce the risk of further scabies transmission in the facility.
When can I return to work if I am diagnosed with scabies ?
Scabies usually is spread by prolonged skin-to-skin contact with a person who has scabies. Scabies sometimes also can be spread by contact with items such as clothing, bedding, or towels that have been used by a person with scabies, but such spread is very uncommon, with the exception of crusted scabies. Persons with crusted scabies should be considered highly contagious and appropriate isolation procedures should be used to protect other persons from becoming infested.
In general, a person diagnosed with scabies could return to work once treatment is begun.
How can I remove scabies mites from my house or carpet ?
Scabies mites do not survive more than 2-3 days away from human skin. Items such as bedding, clothing, and towels used by a person with scabies can be decontaminated by machine-washing in hot water and drying using the hot cycle or by dry-cleaning. Items that cannot be washed or dry-cleaned can be decontaminated by removing from any body contact for at least 72 hours.
Because persons with crusted scabies are considered very infectious, careful vacuuming of furniture and carpets in rooms used by these persons is recommended.
Fumigation of living areas is unnecessary.
How can I remove scabies mites from my clothes ?
Scabies mites do not survive more than 2-3 days away from human skin. Items such as bedding, clothing, and towels used by a person with scabies can be decontaminated by machine-washing in hot water and drying using the hot cycle or by dry-cleaning. Items that cannot be washed or dry-cleaned can be decontaminated by removing from any body contact for at least 72 hours.
Can I get scabies from sharing an office chair or cubicle that is used by a person diagnosed with scabies ?
Scabies usually is spread by prolonged skin-to-skin contact with a person who has scabies. Scabies sometimes also can be spread by contact with items such as clothing, bedding, or towels that have been used by a person with scabies, but such spread is very uncommon, with the exception of crusted scabies. Persons with crusted scabies should be considered highly contagious and appropriate isolation procedures should be used to protect other persons from becoming infested.
Getting scabies from an office chair or cubicle that is used by a person with scabies is very unlikely, unless the infested person has crusted scabies. If the person does not have crusted scabies, avoidance of prolonged skin-to-skin contact with the infested person and simple vacuuming of the infested person’s furniture, rugs, and carpeting should prevent any spread.
If the infested person has crusted scabies, he/she should be considered highly contagious for others and appropriate isolation measure should be used to prevent spread.
If a co-worker is diagnosed with scabies, what precautions must be taken? Should the office be sprayed or fumigated ?
Scabies usually is spread by prolonged skin-to-skin contact with a person who has scabies; persons who have had such contact should be evaluated by a physician and treated if necessary. Scabies mites do not survive more than 2-3 days away from human skin. Spraying or fumigating office or living areas is unnecessary.
However, transmission can occur even after brief skin-to-skin contact, such as a handshake, with a person who has crusted (Norwegian) scabies. In general, a person who has skin-to-skin contact with a person who has crusted scabies would be considered a good candidate for treatment.
To determine when prophylactic treatment should be given to reduce the risk of transmission, early consultation should be sought with a health care provider who understands: 1) the type of scabies (i.e. non-crusted vs crusted) to which a person has been exposed; 2) the degree and duration of skin exposure that a person has had to the infested patient; 3) whether the exposure occurred before or after the patient was treated for scabies; and, 4) whether the exposed person works in an environment where he/she would be likely to expose other people during the asymptomatic incubation period. For example, a nurse or caretaker who works in a nursing home or hospital often would be treated prophylactically to reduce the risk of further scabies transmission in the facility.
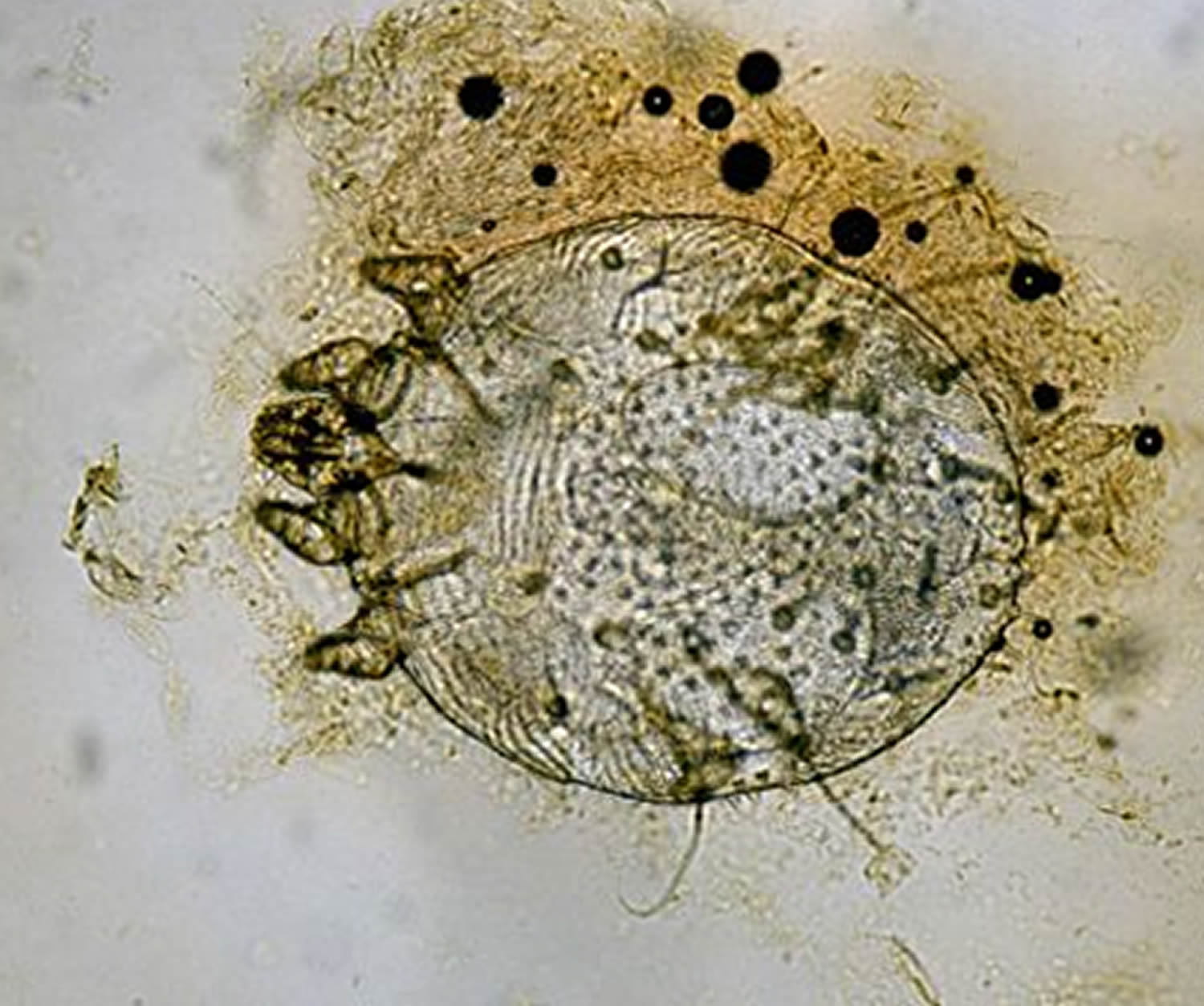
Figure 1. Scabies
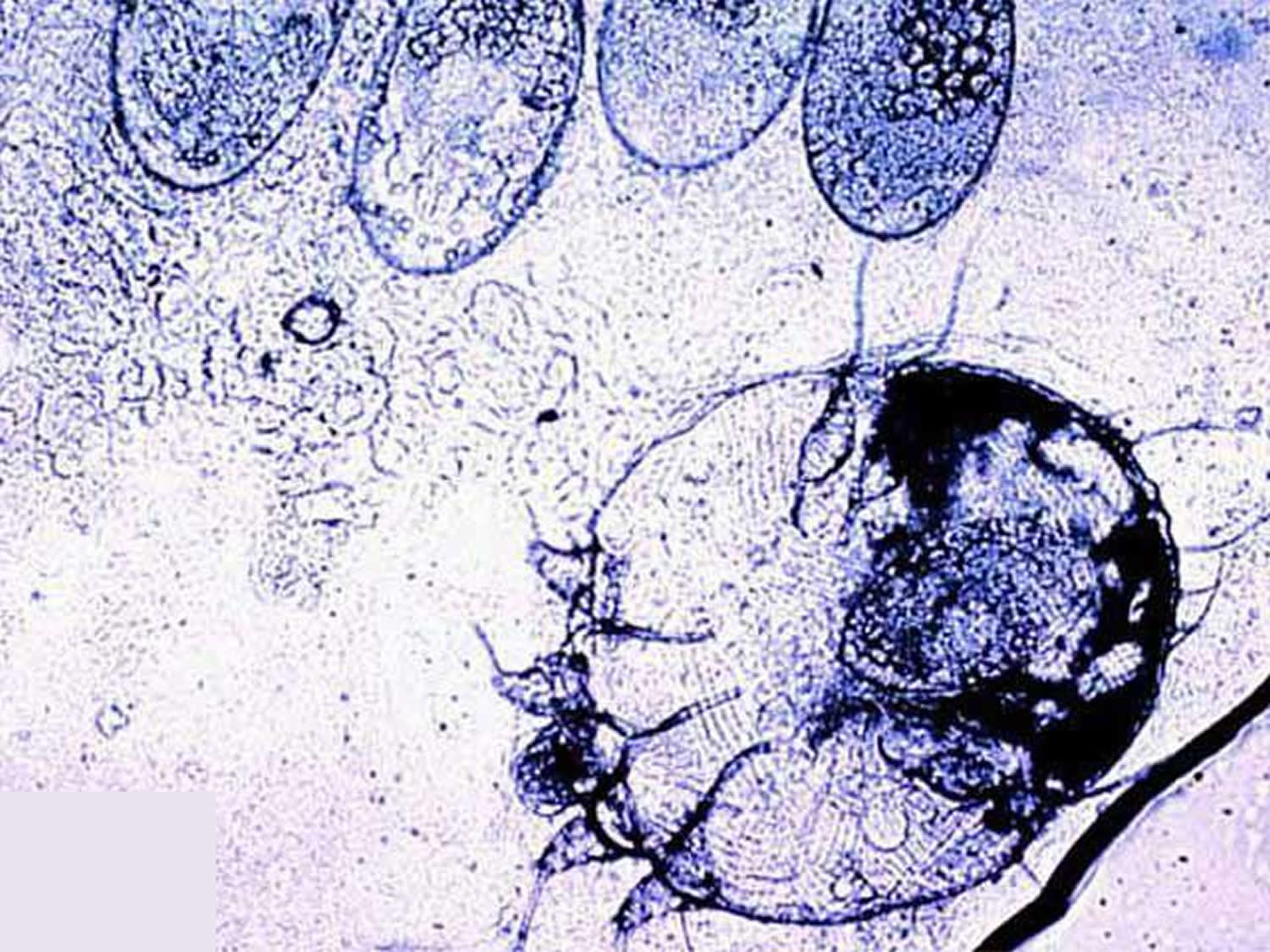
Figure 2. Scabies rash

What is Crusted (Norwegian) Scabies
Crusted scabies (previously called Norwegian scabies ) is a very contagious variant of scabies in which an individual is infested by thousands or millions of mites living in the surface of the skin.
- The patient presents with a generalized scaly rash. This is often misdiagnosed as psoriasis or seborrhoeic dermatitis.
- Scale is often prominent in the finger webs, on wrists, elbows, breasts and scrotum.
- Itch may be absent or minimal.
- Crusted scabies may affect the scalp.
Figure 3. Crusted (Norwegian) scabies

Risk factors for crusted scabies include:
- Very old age
- Malnutrition
- Immune deficiency
- Intellectual deficit
- Neurological disease
- Specific inherited immune defect in some otherwise healthy people
A case of crusted scabies is the usual reason for an outbreak of scabies in an institution. Patients and staff in the institution may present with:
- Usual scabies
- Crusted scabies
- Hypersensitivity rash but no burrows, i.e, not infested.
What causes scabies ?
Sarcoptes scabiei var. hominis, the human scabies mite, is in the arthropod class Arachnida, subclass Acari, family Sarcoptidae 1. The scabies mites burrow into the upper layer of the skin but never below the stratum corneum. The burrows appear as tiny raised serpentine lines that are grayish or skin-colored and can be a centimeter or more in length. Other races of scabies mites may cause infestations in other mammals, such as domestic cats, dogs, pigs, and horses. It should be noted that races of mites found on other animals may cause a self-limited infestation in humans with temporary itching due to dermatitis; however they do not multiply on the human host.
Scabies is nearly always acquired by skin-to-skin contact with someone else with scabies.
- The contact may be quite brief such as holding hands with an infested child.
- It is sometimes sexually transmitted.
- Occasionally scabies is acquired via bedding or furnishings.
Typically, several scabies mites infest an affected host. After mating, the male mite dies. The female scabies mite burrows into the outside layers of the skin, where she lays up to 3 eggs each day for her lifetime of one to two months. The development from egg to adult scabies mite takes 10–14 days.
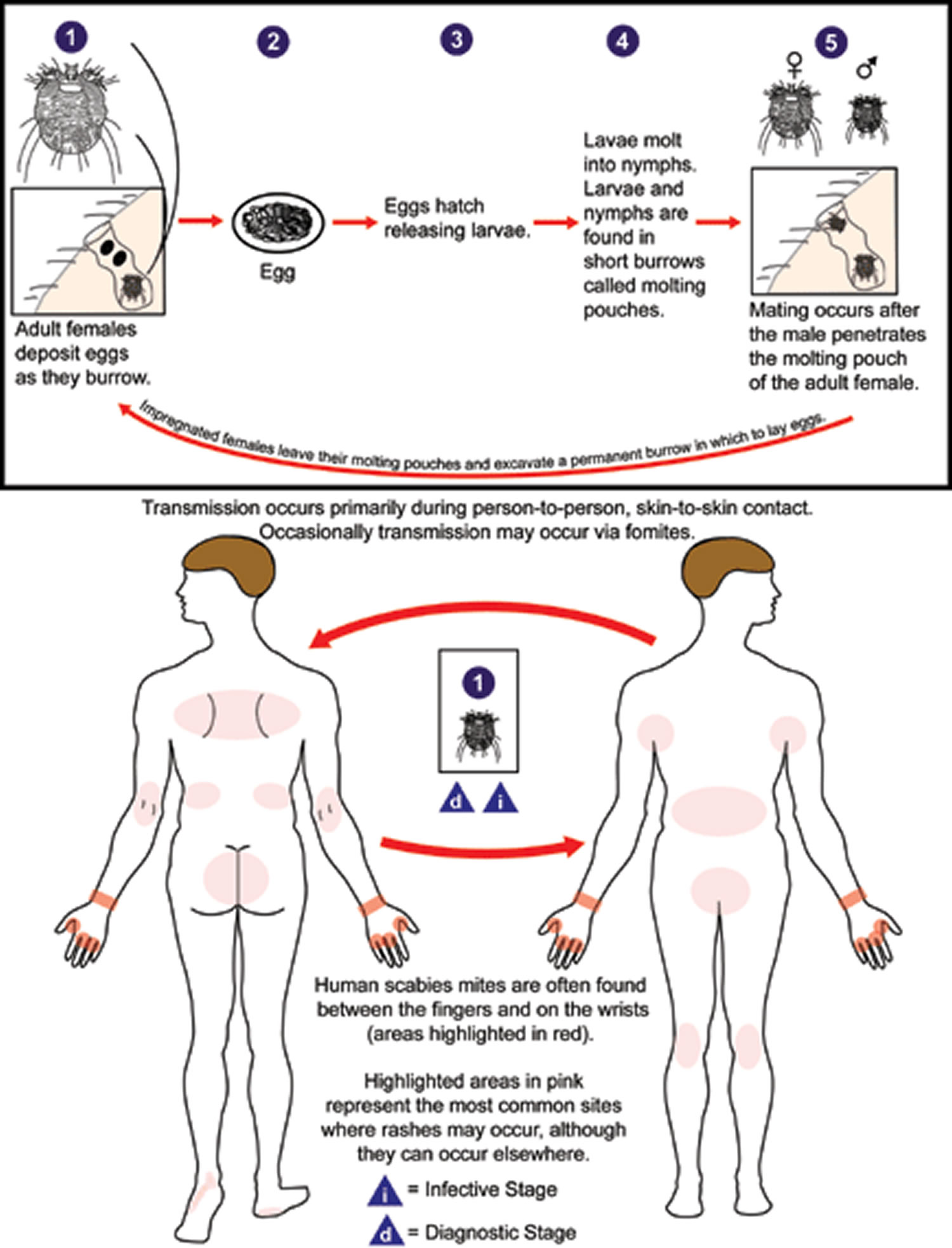
Scabies Life Cycle
Sarcoptes scabiei undergoes four stages in its life cycle: egg, larva, nymph and adult.
- Females deposit 2-3 eggs per day as they burrow under the skin.
- The Eggs are oval and 0.10 to 0.15 mm in length.
- The eggs hatch in 3 to 4 days. After the eggs hatch, the larvae migrate to the skin surface and burrow into the intact stratum corneum to construct almost invisible, short burrows called molting pouches.
- The larval stage, which emerges from the eggs, has only 3 pairs of legs and lasts about 3 to 4 days. After the larvae molt, the resulting nymphs have 4 pairs of legs. This form molts into slightly larger nymphs before molting into adults. Larvae and nymphs may often be found in molting pouches or in hair follicles and look similar to adults, only smaller. Adults are round, sac-like eyeless mites. Females are 0.30 to 0.45 mm long and 0.25 to 0.35 mm wide, and males are slightly more than half that size.
- Mating occurs after the active male penetrates the molting pouch of the adult female. Mating takes place only once and leaves the female fertile for the rest of her life. Impregnated females leave their molting pouches and wander on the surface of the skin until they find a suitable site for a permanent burrow. While on the skin’s surface, mites hold onto the skin using sucker-like pulvilli attached to the two most anterior pairs of legs. When the impregnated female mite finds a suitable location, it begins to make its characteristic serpentine burrow, laying eggs in the process. After the impregnated female burrows into the skin, she remains there and continues to lengthen her burrow and lay eggs for the rest of her life (1-2 months). Under the most favorable of conditions, about 10% of her eggs eventually give rise to adult mites. Males are rarely seen; they make temporary shallow pits in the skin to feed until they locate a female’s burrow and mate.
Transmission occurs primarily by the transfer of the impregnated females during person-to-person, skin-to-skin contact. Occasionally transmission may occur via fomites (e.g., bedding or clothing). Human scabies mites often are found between the fingers and on the wrists.
Figure 4. Scabies Life Cycle
What does scabies look like and symptoms
When a person is infested with scabies mites the first time, symptoms usually do not appear for up to two months (2-6 weeks) after being infested; however, an infested person still can spread scabies during this time even though he/she does not have symptoms.
If a person has had scabies before, symptoms appear much sooner (1-4 days) after exposure. An infested person can transmit scabies, even if they do not have symptoms, until they are successfully treated and the mites and eggs are destroyed.
Figure 5. Scabies rash (tracks or burrows)

Common Scabies Symptoms
Scabies causes a very itchy rash caused by sensitization (a type of “allergic” reaction) to the proteins and feces of the parasite. Severe itching (pruritus), especially at night, is the earliest and most common symptom of scabies. It’s important to search for burrows carefully in a patient with severe itch, especially if the rash is mild. Contacts should be examined for burrows, whether or not they are itchy.
A pimple-like (papular) itchy (pruritic) “scabies rash” is also common. Itching and rash may affect much of the body or be limited to common sites such as:
- Between the fingers
- Wrist
- Elbow
- Armpit
- Penis
- Nipple
- Waist
- Buttocks
- Shoulder blades
The head, face, neck, palms, and soles often are involved in infants and very young children, but usually not adults and older children.
Tiny burrows sometimes are seen on the skin; these are caused by the female scabies mite tunneling just beneath the surface of the skin. These burrows appear as tiny raised and crooked (serpiginous) grayish-white or skin-colored lines on the skin surface. Because mites are often few in number (only 10-15 mites per person), these burrows may be difficult to find. They are found most often in the webbing between the fingers, in the skin folds on the wrist, elbow, or knee, and on the penis, breast, or shoulder blades.
Itch
- If it is the first episode of scabies, itch arises 4–6 weeks after transmission of a mite
- It may occur within a few hours of subsequent infestation.
- Itch is characteristically more severe at night, disturbing sleep
- It affects the trunk and limbs, sparing the scalp.
- Itch is mild or absent in some patients with crusted scabies.
- Itch can persist for several weeks after successful treatment to kill the mites.
Burrows
Scabies burrows appear as 0.5–1.5 cm grey irregular tracks in the web spaces between the fingers, on the palms and wrists. They may also be found on or in elbows, nipples, armpits, buttocks, penis, insteps and heels. Dermatoscopic or microscopic examination of the contents of a burrow may reveal mites, eggs or mite faeces (scybala).
Generalised rash
Scabies rash is a hypersensitivity reaction that arises several weeks after initial infestation. It has a varied appearance.
- Erythematous papules on the trunk and limbs, often follicular
- Diffuse or nummular dermatitis
- Urticated erythema
- Vesicles on palms and soles
- Acropustulosis (sterile pustules on palms and soles) in infants
- Papules or nodules in the armpits, groins, buttocks, scrotum and along the shaft of the penis
- Rare involvement of face and scalp
Possible Complications of Scabies
The intense itching of scabies leads to scratching that can lead to skin sores. The sores sometimes become infected with bacteria on the skin, such as Staphylococcus aureus or beta-hemolytic streptococci.
Secondary infection is due to scratching and effect of the scabies mite on the skin’s ability to fight bacteria.
- Staphylococcal or streptococcal infection results in crusted plaques and pustules (impetigo).
- Streptococcal cellulitis results in painful swelling and redness, and fever.
- Systemic sepsis with staphylococci and/or streptococci is potentially very serious.
- Scabies outbreaks lead to cases of post-streptococcal glomerulonephritis (inflammation of the kidneys) and rheumatic fever.
How is scabies diagnosed ?
Diagnosis of a scabies infestation usually is made based upon the customary appearance and distribution of the the rash and the presence of burrows.
The clinical suspicion of scabies in a patient with an itchy rash, especially when reporting itchy household members, can be confirmed by:
- Dermatoscopy: the mite at the end of a burrow has characteristic jet-plane or hang-glider appearance
- Microscopic examination of the contents of a burrow
- Skin biopsy: this may reveal characteristic scabies histopathology, but this is often negative or nonspecific, eg if taken from the inflammatory rash rather than the surface of a burrow.
What is the treatment for scabies ?
Management of a scabies outbreak involves identification and treatment of individual patients and household contacts with insecticides. Oral antibiotics are required for secondary infection.
Careful attention to instructions is essential if scabies is to be cured.
Medications commonly prescribed for scabies include:
- Permethrin cream, 5 percent (Elimite). Permethrin is a topical cream that contains chemicals that kill scabies mites (scabicide) and their eggs. It is generally considered safe for adults, pregnant women, and children ages 2 months and older. This medicine is not recommended for nursing mothers. The usual topical treatment is 5% permethrin cream, left on the entire skin for 8–10 hours. The permethrin cream is applied to the whole body from the scalp to soles. It should be applied under fingernails using a soft brush.
- Lindane lotion. This medication — also a chemical treatment — is recommended only for people who can’t tolerate other approved treatments, or for whom other treatments didn’t work. This medication isn’t safe for children younger than age 2 years, women who are pregnant or nursing, the elderly, or anyone who weighs less than 110 pounds (50 kilograms).
- Crotamiton (Eurax). This medication is available as a cream or a lotion. It’s applied once a day for two days. This medication isn’t recommended for children or for women who are pregnant or nursing. Frequent treatment failure has been reported with crotamiton.
- Ivermectin (Stromectol). Doctors may prescribe this oral medication for people with altered immune systems, for people who have crusted scabies, or for people who don’t respond to the prescription lotions and creams. Ivermectin isn’t recommended for women who are pregnant or nursing, or for children who weigh less than 33 pounds (15 kg). Oral ivermectin 200 mcg/kg is convenient, but more expensive than topical permethrin. It may be slightly less effective. It is mainly used for mass treatments in institutions, or in patients unable to use topical therapy.
Gamma benzene hexachloride cream is no longer recommended due to neurotoxicity. Other proven treatments include:
- 0.5% aqueous malathion lotion, left on for 24 hours
- 25% benzyl benzoate lotion, applied daily for 3 days. This is irritant, and should not be used in children.
- 2–10% precipitated sulphur ointment
Treatment should be repeated after 8–10 days after the first application to catch mites that have newly hatched. Crotamiton cream can be used to reduce itch; it is a weak scabicide.
Patients with crusted scabies may need repeated oral and topical treatments over several weeks or longer.
Additional management
Contacts must be identified and treated. In addition:
- Bed linen, towels and clothing should be laundered after treatment.
- Non-washable items should be sealed in a plastic bag and stored for one week.
- Rooms should be thoroughly cleaned with normal household products. Fumigation or specialised cleaning is not required.
- Carpeted floors and upholstered furniture should be vacuumed.
How soon after treatment will I feel better ?
If itching continues more than 2-4 weeks after initial treatment or if new burrows or rash continue to appear (if initial treatment includes more than one application or dose, then the 2-4 time period begins after the last application or dose), retreatment with scabicide may be necessary; seek the advice of a physician.
My spouse and I were diagnosed with scabies. After several treatments, he/she still has symptoms while I am cured. Why ?
The rash and itching of scabies can persist for several weeks to a month after treatment, even if the treatment was successful and all the mites and eggs have been killed. Your health care provider may prescribe additional medication to relieve itching if it is severe. Symptoms that persist for longer than 2 weeks after treatment can be due to a number of reasons, including:
- Incorrect diagnosis of scabies. Many drug reactions can mimic the symptoms of scabies and cause a skin rash and itching; the diagnosis of scabies should be confirmed by a skin scraping that includes observing the mite, eggs, or mite feces (scybala) under a microscope. If you are sleeping in the same bed with your spouse and have not become reinfested, and you have not retreated yourself for at least 30 days, then it is unlikely that your spouse has scabies.
- Reinfestation with scabies from a family member or other infested person if all patients and their contacts are not treated at the same time; infested persons and their contacts must be treated at the same time to prevent reinfestation.
- Treatment failure caused by resistance to medication, by faulty application of topical scabicides, or by failure to do a second application when necessary; no new burrows should appear 24-48 hours after effective treatment.
- Treatment failure of crusted scabies because of poor penetration of scabicide into thick scaly skin containing large numbers of scabies mites; repeated treatment with a combination of both topical and oral medication may be necessary to treat crusted scabies successfully.
- Reinfestation from items (fomites) such as clothing, bedding, or towels that were not appropriately washed or dry-cleaned (this is mainly of concern for items used by persons with crusted scabies); potentially contaminated items (fomites) should be machine washed in hot water and dried using the hot temperature cycle, dry-cleaned, or removed from skin contact for at least 72 hours.
- An allergic skin rash (dermatitis); or
- Exposure to household mites that cause symptoms to persist because of cross-reactivity between mite antigens.
If itching continues more than 2-4 weeks or if new burrows or rash continue to appear, seek the advice of a physician; retreatment with the same or a different scabicide may be necessary.
Home remedies for scabies
Itching may persist for some time after you apply medication to kill the mites. These steps may help you find relief from itching:
- Cool and soak your skin. Soaking in cool water or applying a cool, wet washcloth to irritated areas of your skin may minimize itching.
- Apply soothing lotion. Calamine lotion, available without a prescription, can effectively relieve the pain and itching of minor skin irritations.
- Take antihistamines. At your doctor’s suggestion, you may find that over-the-counter antihistamines relieve the allergic symptoms caused by scabies.
What is the outlook for scabies ?
Scabies itch and rash are expected to improve within a few days of successful treatment and to completely clear within a month.
A rash may persist after scabies treatment. Reasons for this include:
- Persistent infestation due to incorrectly applied treatment, treatment resistance, or re-infestation due to an untreated contact.
- The hypersensitivity reaction can be slow to settle, despite complete cure of parasitic infestation.
- On-going dermatitis can be due to the mite, the scratching, irritation of topical treatment, or other factors. Persistently itchy papules, nodules and eczematous plaques should be treated with frequent applications of emollients and mild topical corticosteroids once or twice daily.
- Incorrect diagnosis.
Prevention & Control of Scabies
When a person is infested with scabies mites the first time, symptoms may not appear for up to two months after being infested. However, an infested person can transmit scabies, even if they do not have symptoms. Scabies usually is passed by direct, prolonged skin-to-skin contact with an infested person. However, a person with crusted (Norwegian) scabies can spread the infestation by brief skin-to-skin contact or by exposure to bedding, clothing, or even furniture that he/she has used.
Scabies is prevented by avoiding direct skin-to-skin contact with an infested person or with items such as clothing or bedding used by an infested person. Scabies treatment usually is recommended for members of the same household, particularly for those who have had prolonged skin-to-skin contact. All household members and other potentially exposed persons should be treated at the same time as the infested person to prevent possible reexposure and reinfestation. Bedding and clothing worn or used next to the skin anytime during the 3 days before treatment should be machine washed and dried using the hot water and hot dryer cycles or be dry-cleaned. Items that cannot be dry-cleaned or laundered can be disinfested by storing in a closed plastic bag for several days to a week. Scabies mites generally do not survive more than 2 to 3 days away from human skin. Children and adults usually can return to child care, school, or work the day after treatment.
Persons with crusted scabies and their close contacts, including household members, should be treated rapidly and aggressively to avoid outbreaks. Institutional outbreaks can be difficult to control and require a rapid, aggressive, and sustained response.
Rooms used by a patient with crusted scabies should be thoroughly cleaned and vacuumed after use. Environmental disinfestation using pesticide sprays or fogs generally is unnecessary and is discouraged.
Starve the mites. Consider placing items you can’t wash in a sealed plastic bag and leaving it in an out-of-the-way place, such as in your garage, for a couple of weeks. Mites die after a few days without food.
- Scabies Biology. https://www.cdc.gov/parasites/scabies/biology.html[↩]