Contents
Ingrown toenail
Toenails and fingernails are clear, hard derivatives of the stratum corneum. They are composed of very thin, dead, scaly cells, densely packed together and filled with parallel fibers of hard keratin. An ingrown toenail or onychocryptosis, occurs when the edge of the nail grows down and into the skin of the toe. There may be pain, redness, and swelling around the nail.
An ingrown toenail may occur at any age and is the mostly commonly encountered toenail problem likely to be seen in general practice 1.
The epidemiology of ingrown toenail (onychocryptosis) is difficult to determine as it is often considered to be a minor medical problem and as such has been some-what neglected in the literature. The few studies that have been conducted suggest a slightly higher male-to-female ratio, particularly in the 14–25 age group 2, but it can affect patients of any age. There are multiple reasons why an ingrown toenail will develop, including improper nail cutting technique, tight-fitting footwear, trauma, anatomical factors such as thickening of the nail plate, pincer-shaped toenail, pressure from abutting digits caused by hallux valgus or lesser toe deformities, the presence of a subungual exostosis and, occasionally, the use of isotretinoin in the treatment of severe acne 3, 4, 5.
Causes of ingrown toenail
An ingrown toenail can result from a number of things, but poorly fitting shoes and toenails that are not trimmed properly are the most common causes. The skin along the edge of a toenail may become red and infected. The great toe is usually affected, but any toenail can become ingrown.
Ingrown toenails may occur when extra pressure is placed on your toe. Most commonly, this pressure is caused by shoes that are too tight or too loose. If you walk often or participate in athletics, a shoe that is even a little tight can cause this problem. Some deformities of the foot or toes can also place extra pressure on the toe.
Nails that are not trimmed properly can also cause ingrown toenails.
- When your toenails are trimmed too short or the edges are rounded rather than cut straight across, the nail may curl downward and grow into the skin.
- Poor eyesight and physical inability to reach the toe easily, as well as having thick nails, can make improper trimming of the nails more likely.
- Picking or tearing at the corners of the nails can also cause an ingrown toenail.
Some people are born with nails that are curved and tend to grow downward. Others have toenails that are too large for their toes. Stubbing your toe or other injuries can also lead to an ingrown toenail.
Prevention of ingrown toenail
Wear shoes that fit properly. Shoes that you wear every day should have plenty of room around your toes. Shoes that you wear for walking briskly or for running should have plenty of room also, but not be too loose.
When trimming your toenails:
- Considering briefly soaking your foot in warm water to soften the nail.
- Use a clean, sharp nail trimmer.
- Trim toenails straight across the top. Do not taper or round the corners or trim too short.
- Do not pick or tear at the nails.
Keep the feet clean and dry. People with diabetes should have routine foot exams and nail care.
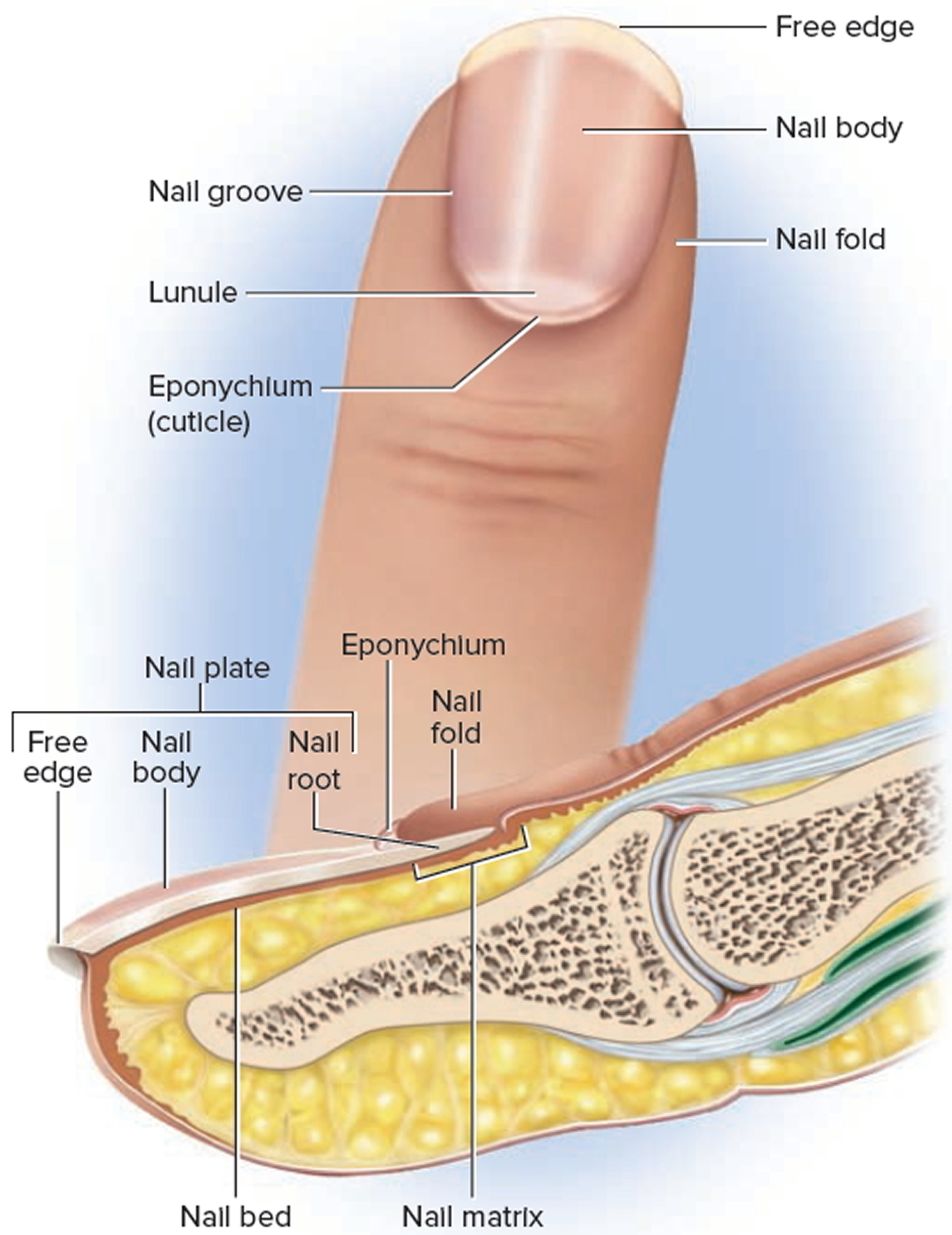
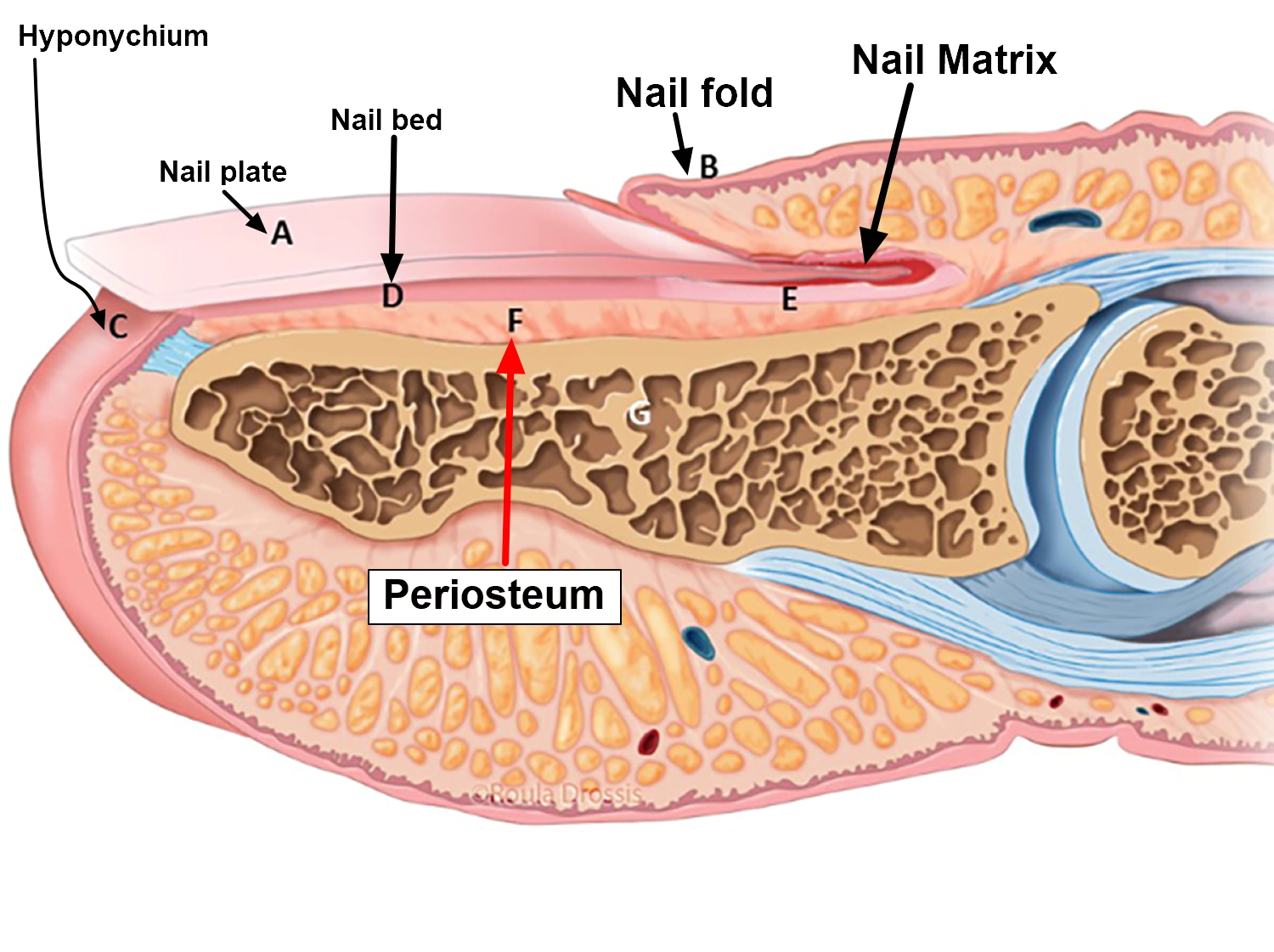
Figure 1. Ingrown toenail

Figure 2. Nail anatomy
How to treat an ingrown toenail
Often the medial or lateral nail edge of an incurved toenail may press into the nail sulcus without actual skin penetration, which leads to the formation of a painful hyperkeratotic lesion. Should the nail plate penetrate through the thin skin of the nail sulcus, infection and hypergranulation tissue will ensue and the toenail is then best described as ingrown (Figure 1) 6. Either condition may become symptomatic and require definitive surgical management. Some doctors suggest that, ideally, all presentations of ingrown toenail should be managed conservatively in the first instance 7.
Conservative treatment
Careful trimming of the affected distal nail corner is the preferred conservative management of an incurved toenail followed by application of a suitable antiseptic dressing. Referral to a podiatrist to carefully trim the nail edge and debride any hyperkeratotic lesion may be necessary. Traditional conservative treatments have included the use of astringent soaks such as hypertonic solution of Epsom salts or the application of 25% silver nitrate solution may be beneficial but are rarely used today. Encouraging patients to carefully trim their toenails to avoid creating sharp spicules and to place small inserts of cotton wool beneath the nail corners to protect the skin of the nail fold may also be helpful 8.
Patients presenting with an ingrown toenail that has penetrated the nail sulcus usually require a partial avulsion of the offending border of toenail to allow for drainage and the excision of any hypergranulation tissue 9. Local anesthesia should first be attained via a digital ring block injection of the hallux proximal to the area of erythema with plain local anaesthetic solution. Using small sterile nail nippers, the distal corner section of the involved nail edge is removed taking care not to leave any sharp projections. Care must be exercised not to extend the nail excision more proximal than necessary to avoid the nail matrix area. Hypergranulation tissue should be excised if present. Application of a haemostatic dressing such as Gelatamp may also be necessary. Oral antibiotics are sometimes required but are usually not necessary, providing the offending nail section and any hypergranulation tissue are removed. Home care then consists of soaking twice daily in Epsom salt or saline solution and using a topical antiseptic dressing until healed.
Home remedies for ingrown toenail
- If you have diabetes, nerve damage in the leg or foot, poor blood circulation to your foot, or an infection around the nail, go to the doctor right away. Do NOT try to treat this problem at home.
To treat an ingrown nail at home:
- Soak the foot in warm water 3 to 4 times a day if possible. Keep the toe dry, otherwise.
- Gently massage over the inflamed skin.
- Place a small piece of cotton or dental floss under the nail. Wet the cotton with water or antiseptic.
You may trim the toenail one time, if needed. When trimming your toenails:
- Consider briefly soaking your foot in warm water to soften the nail.
- Use a clean, sharp trimmer.
- Trim toenails straight across the top. Do not taper or round the corners or trim too short. Do not try to cut out the ingrown portion of the nail yourself. This will only make the problem worse.
Consider wearing sandals until the problem has gone away. Over-the-counter medications that are placed over the ingrown toenail may help some with the pain but do not treat the problem.
If this does not work and the ingrown nail gets worse, see your family doctor, a foot specialist (podiatrist) or a skin specialist (dermatologist).
If your ingrown nail does not heal or keeps coming back, your doctor may remove part of the nail.
- Numbing medicine is first injected into the toe.
- Using scissors, your doctor then cuts along the edge of the nail where the skin is growing over. This portion of the nail is then removed. This is called a partial nail avulsion.
- It will take 2 to 4 months for the nail to regrow.
Sometimes your doctor will use a chemical, electrical current, or another small surgical cut to destroy or remove the area from which a new nail may grow.
If the toe is infected, your doctor may prescribe antibiotics.
Ingrown Toenail Surgery – Winograd technique
If conservative care proves unsatisfactory or if the patient presents with a recurrent ingrown toenail then surgical treatment is indicated. Sharp nail resection and phenol-ablation techniques have been reported in the literature as safe and effective methods for treating ingrown toenails 10, 11, 12.
The Winograd technique is perhaps the most commonly performed sharp procedure 10 and is often used when a hypertrophied nailfold is in need of excision. Winograd, a US podiatrist first described the technique in 1929 13. A large case series analysis published by Güler et al 10 in 2014, which followed 239 patients who underwent a Winograd procedure for ingrown toenails, reported that 96.3% (n = 230) were satisfied with the procedure and 231 patients (96.6%) were satisfied with the cosmetic result 10. Another recent analysis performed by Kayalar et al 11 of 224 patients who underwent the Winograd procedure found a high success rate of 91.2% (n = 202), with revisional surgery only required in 7.1% (n = 16) at a minimum 10-month follow-up 11.
The local anesthetic preferred for the procedure is either bupivacaine 0.5% or ropivacaine 0.75% plain. Instruments and materials required are:
- nonstick antiseptic gauze (eg Bactigras paraffin-wax gauze)
- 4.0 non-absorbable suture
- suture forceps
- scalpel handle
- English anvil nail splitter
- small curette
- straight haemostat
- #15 blade
- sterile saline
- digit tourniquet (eg Tourni-cot ring)
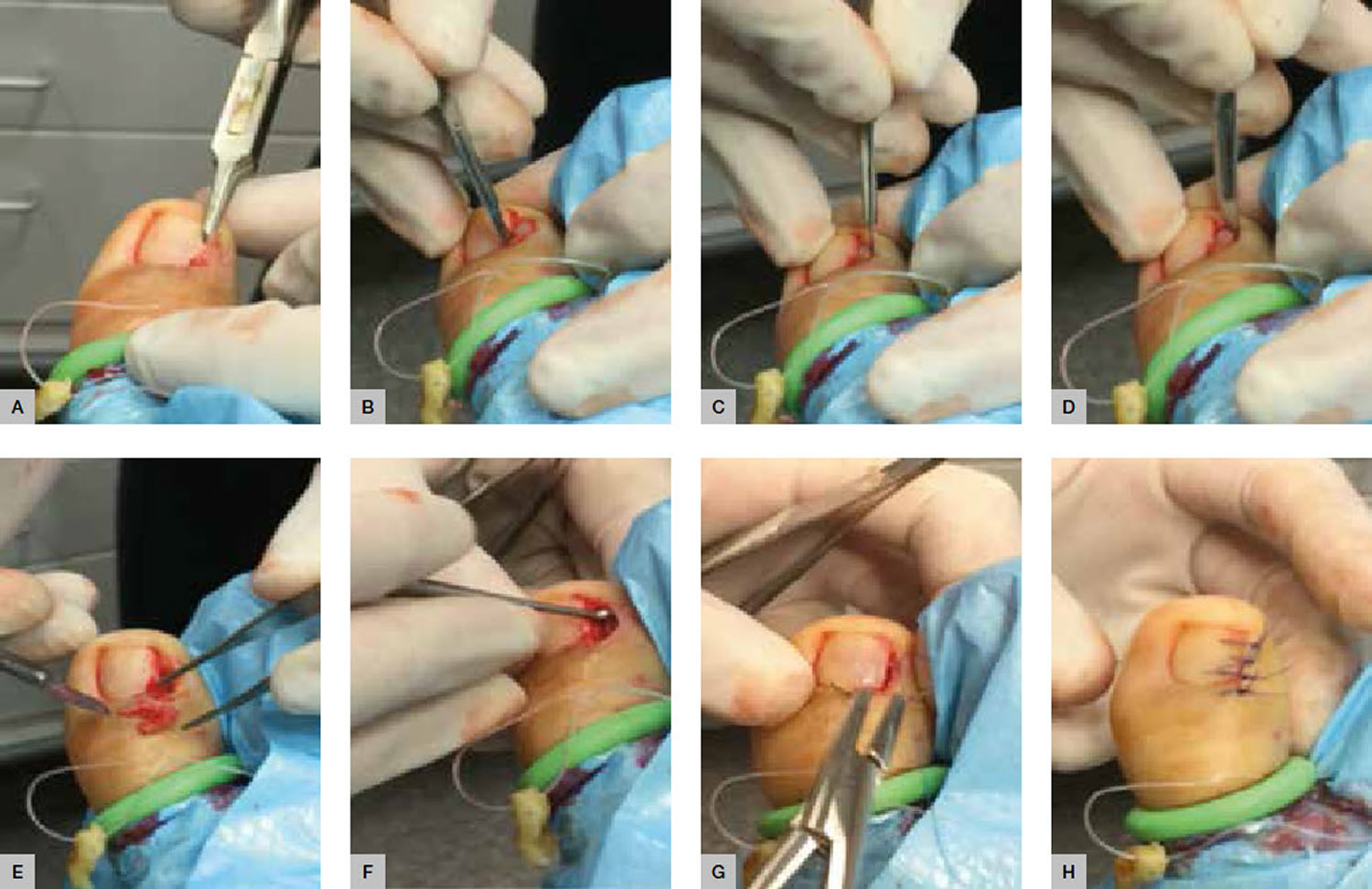
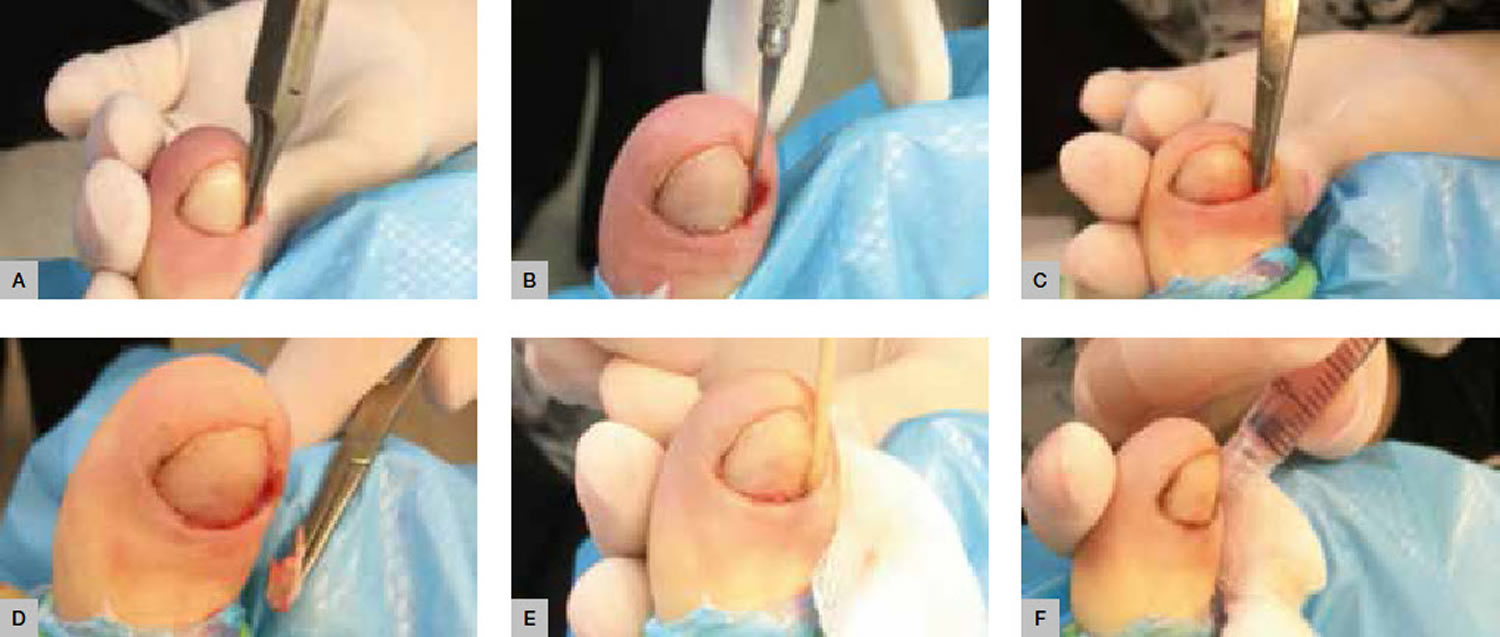
The procedure is illustrated in Figure 3 and outlined below:
- Prepare the toe using alcohol skin wipes and inject 3–4 ml of bupivcaine 0.5% or ropivacaine 0.75% plain as digital ring block.
- Use standard sterile technique after applying a suitable alcoholic chlorhexidine or povidone-iodine liquid solution to prepare the foot.
- Use a digit tourniquet to exsanguinate the toe.
- Use the nail splitter to split 2–3 mm of the affected side of the nail longitudinally (Figure 3A)
- Make two skin incisions:
+ The first is made deeply through the split nail to include the nail bed extending proximally to include the dorsal skin over the nail matrix (Figure 3B)
+ The final incision is to excise the lateral nailfold, connecting the proximal and distal ends of the initial incision (Figure 3C, D). - Excise the nail section, bed and matrix tissue in total (Figure 3E) and the gently curette to remove any remaining matrix tissue (Figure 3F).
- Flush with normal saline.
- Close the wound with simple interrupted sutures (Figure 3F, H).
- Remove the tourniquet and allow the toe to bleed for a minute or two with local pressure to control the reactive hyperaemia often encountered after release of the tourniquet.
- Dress the toe with a suitable antiseptic dressing, sterile gauze and crepe bandage.
The patient should be advised of the following the post-operative protocol:
- Rest and elevate the foot.
- Use oral analgesics as needed.
- Keep the dressing dry until post-operative review.
- Advise of increasing pain/discomfort (infection).
- The suture will be removed in 5–7 days.
Figure 3. Ingrown Toenail Surgery – Winograd technique
Ingrown Toenail Surgery – Phenol Matrixectomy
Phenol matrixectomy is an alternative procedure often favoured by podiatrists and was first described by Boll, a US podiatrist, in 1945 14 and popularised by Bell, a UK podiatrist, in 1977 15. The procedure differs from the Winograd technique in that the nail matrix is destroyed via chemical ablation rather than being surgically excised. Phenol BP is caustic to tissues and, although the optimum application time has not been accurately determined, a histological study on fresh cadaveric specimens suggested at least 60 seconds is necessary for the phenol to penetrate matrix tissue 16. Phenol matrixectomy has been reported to offer certain advantages over the more traditional surgical approach, including lower levels of post-operative pain and infection, and has comparable success rates 17. A recently published randomised controlled trial of 123 patients with ingrown toenails concluded that the phenolic ablation technique produced less recurrence and spicule formation than the sharps nail resection (n =117 at 12 months follow-up) and no significant difference in post-operative infection rates 12. Another large retrospective case study of 197 phenolic ablations performed reported a 98.5% (n = 194) success rate at mean follow-up of 36 months with no severe complications observed 18.
The local anaesthetic preferred for this procedure is lignocaine 1–2% plain. Instruments and materials required are the same as those listed above for the Winograd technique plus:
- Betadine ointment
- Beaver handle with #62 Beaver blade
- sterile cotton-tipped applicators
- liquefied phenol BP.
No sutures are needed. The procedure is illustrated in Figure 4 and outlined below:
- Prepare the toe using alcohol skin wipes and inject 3–4 ml of lignocaine 1–2% plain as digital ring block.
- Use standard sterile technique after preparing the foot.
- Use a digit tourniquet to exsanguinate the toe.
- Use a nail splitter to split 2–3 mm of the affected side of nail longitudinally (Figure 4A) and complete to the proximal edge with the #62 Beaver blade (Figure 4B).
- Perform avulsion of the nail by grasping the sectioned nail with a haemostat and using a gentle distraction technique to rotate it towards the midline of the nail plate and ease the nail free of the nail bed (Figure 4C, D).
- Gently curette the surgical site to remove any remaining matrix tissue.
- Apply liquid phenol BP directly to the site of the germinal nail matrix using small cotton wool applicator tips or the corner of gauze soaked phenol in 3 x 20-second applications (Figure 4E). Application of phenol should be carefully confined to the immediate surgical area, avoiding excess phenol contact with surrounding skin as this may result in unnecessary tissue injury. It is important to ensure that the nail sulcus and matrix area are dried immediately before applying phenol as the chemical is quickly neutralised by body fluid.
- Flush the site using chlorhexidine solution (Figure 4F).
- Remove the tourniquet and use local pressure to control any bleeding, which is normally minimal if any.
- Dress the toe with Betadine ointment, sterile gauze and crepe bandage.
Advise the patient of the following post-operative protocol:
- Postoperative analgesics are rarely required.
- Keep the toe dry overnight.
- Clean the site daily after showering using Epsom salts dissolved in water and to re-dress with Betadine ointment and a simple toe dressing until fully healed (2–3 weeks).
- Monitor for signs of increasing pain/discomfort (infection).
- The wound will be reviewed at 1 week post-operative to evaluate healing, at which time the wound should be debrided of any material inhibiting free drainage of the healing tissue.
Figure 4. Ingrown Toenail Surgery – Phenol-ablation technique
- Murtagh J. Patient education. Ingrowing toenails. Aust Fam Physician 1993;22:206.[↩]
- Langford DT, Burke C, Robertson K. Risk factors in onychocryptosis. Br J Surg 1989;76:45–48.[↩]
- Shaikh FM, Jafri M, Giri SK, Keane R. Efficacy of wedge resection with phenolization in the treatment of ingrowing toenails. J Am Podiatr Med Assoc 2008;98:118–22.[↩]
- Ikard RW. Onychocryptosis. J Am Coll Surg 1998;187:96–102.[↩]
- Baran R, Roujeau JC. New millennium, new nail problems. Dermatol Ther 2002;15:64–70.[↩]
- Heifetz CJ. Ingrown toenail: A clinical study. Am J Surg 1937;38:298–315.[↩]
- Ingrown toenails: the role of the GP. Australian Family Physician Volume 44, No.3, 2015 Pages 102-105. https://www.racgp.org.au/afp/2015/march/ingrown-toenails-the-role-of-the-gp/[↩]
- Ilfeld FW. Ingrown toenail treated with cotton collodion insert. Foot Ankle 1991;11:312–13.[↩]
- Crislip TW, Boberg JS. Nail Surgery. In: Southerland J, Alder D, Boberg J, et al, editors. McGlamry’s Comprehensive textbook of foot and ankle surgery. 4th edn. Vol 1. Philadelphia: Lippincott Williams & Wilkins, 2013;109–16.[↩]
- Güler O, Mahirogulları M, Mutlu S, Çerçi H, Seker A, Mutlu H. An evaluation of partial matrix excision with Winograd method for the surgical treatment of ingrown toenails. JAREM 2014;4:7–11.[↩][↩][↩][↩]
- Kayalar M, Bal E, Toros T, Özaksar K, Gürbüz Y, Ademoglu Y. Results of partial matrixectomy for chronic ingrown toenail. Foot Ankle Int 2011;32:888–95.[↩][↩][↩]
- Bos AM, van Tilburg MW, van Sorge AA, Klinkenbijl JH. Randomized clinical trial of surgical technique and local antibiotics for ingrowing toenail. J Br Surg 2007;94:292–96.[↩][↩]
- Winograd AM. A modification in the technique of operation for ingrown toenail. J Am Podiatr Med Assoc. 2007 Jul-Aug;97(4):274-7.[↩]
- Boll O. Surgical correction of ingrowing toenails. J Natl Assoc Chiropod 1945;35:8.[↩]
- Bell DRC. Advanced techniques. Chiropodist 1977;32:238–43.[↩]
- Boberg JS, Frederiksen MS, Harton FM. Scientific analysis of phenol nail surgery. J Am Podiatr Med Assoc 2002;92:575–79.[↩]
- Herold N, Houshian S, Riegels-Nielsen P. A prospective comparison of wedge matrix resection with nail matrix phenolization for the treatment of ingrown toenail. J Foot Ankle Surg 2001;40:390–95.[↩]
- Vaccari S, Dika E, Balestri R, Rech G, Piraccini BM, Fanti PA. Partial excision of matrix and phenolic ablation for the treatment of ingrowing toenail: A 36-month follow-up of 197 treated patients. Dermatol Surg 2010;36:1288–93.[↩]