Contents
- What is kidney failure
- What causes kidney failure
- Kidney failure treatment
- How does Hemodialysis work ?
- How does Peritoneal Dialysis work ?
- How Kidney Transplantation Works
- Medical, Psychological, and Social Evaluation at a Transplant Center
- Who is on your transplant team ?
- Placement on the Waiting List
- Waiting Period
- Kidney Transplant Surgery
- Recovery from Kidney Transplant Surgery
- Pros and Cons of Kidney Transplantation
- What do you need to know about care after your kidney transplant ?
- What are signs that your body is rejecting your new kidney ?
- How do you know your new kidney is working properly ?
- What are the side effects of immunosuppressants ?
- What financial help is available to pay for a kidney transplant ?
- What help is available to pay for kidney transplant medicines ?
- Eating, Diet, and Nutrition for Kidney Transplant Patients
- What is conservative management for kidney failure ?
- Kidney failure diet
- What is acute kidney failure
- What are Signs and Symptoms of Acute Kidney Failure
- Causes of Acute kidney failure
- Risk factors for Acute kidney failure
- How to Prevent having an Acute Kidney Failure ?
- Complications of acute kidney failure
- Acute kidney failure diagnosis
- Treatment for acute kidney failure
- Home remedies for acute kidney failure
What is kidney failure
Kidney failure means your kidneys no longer work well enough to do their job 1. Healthy kidneys clean your blood by removing excess fluid, minerals, and wastes. They also make hormones that keep your bones strong and your blood healthy.
Glomerular filtration rate (GFR) is the best measure of overall kidney function in health and disease 2. The normal level of glomerular filtration rate (GFR) varies according to age, sex, and body size. Normal glomerular filtration rate (GFR) in young adults is approximately 120 to 130 mL/min per 1.73 m² and declines with age 3. A glomerular filtration rate (GFR) level less than 60 mL/min per 1.73 m² represents loss of half or more of the adult level of normal kidney function. Below this level, the prevalence of complications of chronic kidney disease increases. Although the age-related decline in GFR has been considered part of normal aging, decreased GFR in the elderly is an independent predictor of adverse outcomes, such as death and cardiovascular disease 4. In addition, decreased GFR in the elderly requires adjustment in drug dosages, as in other patients with chronic kidney disease 5. Therefore, the definition of chronic kidney disease is the same, regardless of age. Because GFR declines with age, the prevalence of chronic kidney disease increases with age; approximately 17% of persons older than 60 years of age have an estimated GFR less than 60 mL/min per 1.73 m² 6.
The National Kidney Foundation Practice Guidelines define kidney failure as either:
- GFR less than 15 mL/min per 1.73 m², which is accompanied in most cases by signs and symptoms of uremia, or
- A need to start kidney replacement therapy (dialysis or transplantation).
Having kidney failure means that:
- 85-90% of your kidney function is gone
- your kidneys don’t work well enough to keep you alive
There is no cure for kidney failure, but with treatment it is possible to live a long life.
- Approximately 98% of patients with kidney failure in the United States begin dialysis when their GFR is less than 15 mL/min per 1.73 m² 7. Kidney failure is not synonymous with end-stage renal disease (ESRD). End-stage renal disease is an administrative term in the United States. It indicates that a patient is treated with dialysis or transplantation, which is the condition for payment for health care by the Medicare end-stage renal disease Program. The classification of end-stage renal disease does not include patients with kidney failure who are not treated with dialysis and transplantation. Thus, although the term end-stage renal disease provides a simple operational classification of patients according to treatment, it does not precisely define a specific level of kidney function.
- The level of kidney function, regardless of diagnosis, determines the stage of chronic kidney disease according to the Kidney Disease Outcomes Quality Initiative chronic kidney disease classification.
Every day, your kidneys filter about 120 to 150 quarts of blood to produce about 1 to 2 quarts of urine, composed of wastes and extra fluid. Kidney failure means your kidneys are not filtering as well as they should. When your kidneys fail, harmful wastes and extra salt and fluid buildup in your body. You then need treatment to replace the work your damaged kidneys have stopped doing.
Your kidneys filter wastes and extra fluid from your blood to keep you healthy. The wastes and extra fluid become urine that is stored in your bladder until you urinate. When your kidneys fail, dialysis can take over a small part of the work your damaged kidneys can no longer do.
The treatments for kidney failure are:
- Hemodialysis
- Peritoneal dialysis
- Kidney transplant
These treatments can help you stay well.
Left untreated, kidney failure will lead to coma, seizures, and death.
You can make treatments work better by:
- sticking to your treatment schedule
- taking all medicines your doctor prescribes
- following a special diet that keeps wastes from building up in your blood
- being active most days of the week.
What causes kidney failure
Kidneys can become damaged from a physical injury or a disease like diabetes, high blood pressure, or other disorders.
Diabetes is the most common cause of kidney failure. High blood pressure is the second most common cause of kidney failure.
Other problems that can cause kidney failure include 8:
- Autoimmune diseases, such as lupus and IgA nephropathy
- Genetic diseases (diseases you are born with), such as polycystic kidney disease
- Nephrotic syndrome
- Urinary tract problems
Sometimes the kidneys can stop working very suddenly (within two days). This type of kidney failure is called acute kidney injury or acute renal failure. Common causes of acute renal failure include:
- Heart attack
- Illegal drug use and drug abuse
- Not enough blood flowing to the kidneys
- Urinary tract problems
This type of kidney failure is not always permanent. Your kidneys may go back to normal or almost normal with treatment and if you do not have other serious health problems.
Having one of the health problems that can lead to kidney failure does not mean that you will definitely have kidney failure.
Kidney failure does not happen overnight. It is the end result of a gradual loss of kidney function. In fact, some people do not even know they have kidney disease until their kidneys fail. Why not? Because people with early kidney disease may not have any symptoms. Symptoms usually show up late in the progression of the disease.
What are signs and symptoms of kidney failure
Healthy kidneys remove wastes and extra fluid from your blood. But when your kidneys fail, wastes and extra fluid can build up in your blood and make you feel sick. You may have some of the following symptoms:
- nausea
- little or no urination
- headaches
- drowsiness
- trouble sleeping
- loss of appetite
- weight loss
- weakness
- fatigue, or feeling tired
- generalized itching or numbness
- weight loss
- muscle cramps (especially in the legs)
- high blood pressure
- edema—swelling, usually in the legs, feet, or ankles and less often in the hands or face
- anemia (a low blood count)
- trouble sleeping
- darkened skin
- dry skin
- trouble concentrating
- vomiting
When these conditions occur, you need treatment to replace the work your damaged kidneys have stopped doing. Left untreated, kidney failure will lead to coma, seizures, and death.
Once you begin treatment for kidney failure, your symptoms will improve and you will begin to feel much better.
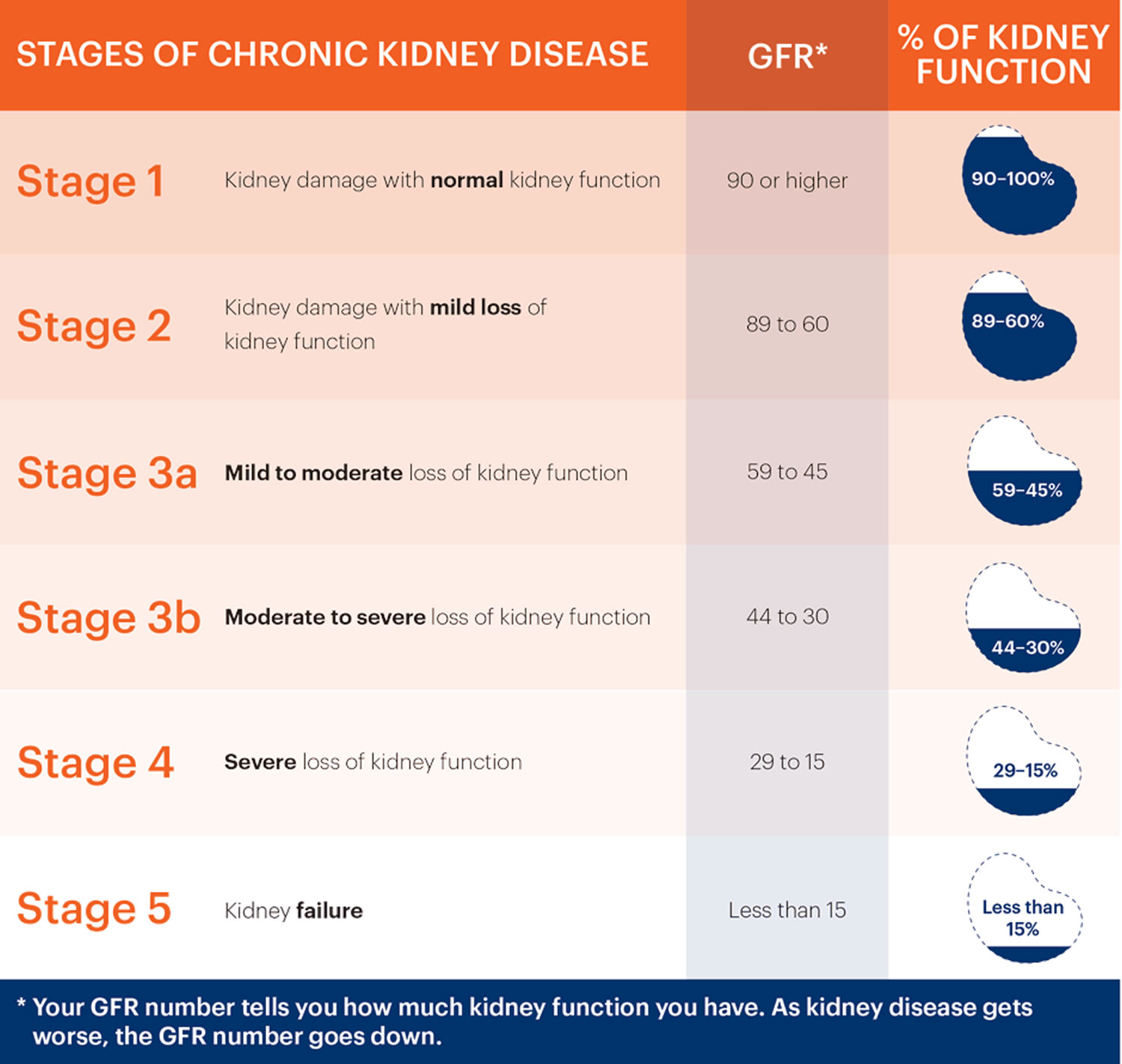
Stages of kidney failure
Chronic kidney disease progresses in stages.
The Glomerular filtration rate (GFR) provides an estimate of how much blood is filtered by the kidneys each minute. In normal kidneys are GFR > 60 ml/minute.
- The formula used to estimate GFR uses serum creatinine, age, gender, and race.
- eGFR (mL/min/1.73 m2) = 175 x (serum creatinine)–1.154 x (Age)–0.203 x (0.742 if female) x (1.212 if African American)
- End Stage Kidney failure (stage 5) is an eGFR < 15 ml/minute.
- eGFR is not reliable for patients with rapidly changing creatinine levels, extremes in muscle mass and body size, or altered diet patterns.
- For a free Glomerular Filtration Rate (GFR) Calculators please go here: https://www.niddk.nih.gov/health-information/communication-programs/nkdep/laboratory-evaluation/glomerular-filtration-rate-calculators
Table 1. Reference Table for Population Mean eGFR from NHANES III
Age (years) | Mean eGFR (mL/min/1.73 m²) |
20–29 | 116 |
30–39 | 107 |
40–49 | 99 |
50–59 | 93 |
60–69 | 85 |
70 | 75 |
Each stage of chronic kidney disease is related to the level of kidney function and kidney damage.
- Stage 1 – a normal eGFR greater than or equal to 90 ml per minute per 1.73 m2, and albuminuria, hematuria, a pathological abnormality or a structural abnormality.
- Stage 2 – a slightly decreased eGFR between 60 and 89 ml per minute per 1.73 m2, and albuminuria, haematuria, a pathological abnormality or a structural abnormality.
Note: If your kidney function is at stage 1 or 2, you only have chronic kidney disease if you have albuminuria, hematuria, a pathological abnormality or a structural abnormality.
- Stage 3a – a mild to moderate decrease in eGFR between 45 and 59 millilitres per minute per 1.73 m2.
- Stage 3b – a moderate to severe decrease in eGFR between 30 and 44 millilitres per minute per 1.73 m2.
- Stage 4 – a severe decrease in eGFR between 15 and 29 millilitres per minute per 1.73 m2.
- Stage 5 – end stage kidney disease, as eGFR decreases to less than 15 millilitres per minute per 1.73 m2 or dialysis is started.
How will kidney failure affect your life ?
Kidney failure will affect your life in many ways. You may find you cannot do all the things you used to do at home or at work. You may have less energy and may feel depressed. Physical problems may include:
- ankle or belly swelling
- stomach sickness
- throwing up
- loss of appetite
- feeling tired
- weakness
- confusion
- headaches
Having kidney failure does not have to take over your life. Having kidney failure does not have to mean giving up hobbies, work, social activities, or time with family.
Can you continue to work with kidney failure ?
Yes, many people with kidney failure continue to work. Your employer may give you lighter physical jobs or schedule your work hours around your hemodialysis sessions. If you are on peritoneal dialysis, you will need space and time to change the dialysis solution in the middle of the work day. Most employers are happy to make these changes.
As a result of the Americans with Disabilities Act, an employer cannot fire you because you are on dialysis or had a kidney transplant. The law requires an employer to make reasonable adjustments to the workplace for a person with a disability. If your employer is not willing to meet your needs, your dialysis clinic’s renal social worker may be able to help find a way to satisfy both you and your employer. As a last resort, you may need to file a complaint with the Equal Employment Opportunity Commission. Your renal social worker may be able to help you with this complaint, or you may need the help of a lawyer. Many times, just the mention of legal action is enough to cause an employer to make reasonable changes in the workplace.
Can you be active with kidney failure ?
Yes. Physical activity is an important part of staying healthy when you have kidney failure. Being active makes your muscles, bones, and heart stronger. Physical activity also makes your blood circulate faster so your body gets more oxygen. Your body needs oxygen to use the energy from food. If you are on dialysis, physical activity can help more wastes move into your blood for dialysis to remove them.
You will find that physical activity can also improve your mood and give you a sense of well-being.
Talk with your doctor before you start an exercise routine. Start slow, with easier activities such as walking at a normal pace or gardening. Work up to harder activities such as walking briskly or swimming. Aim for at least 30 minutes of exercise most days of the week.
Kidney failure treatment
You have three treatment options to choose from to filter your blood. A fourth option offers care without replacing the work of the kidneys. None of these treatments helps the kidneys get better. However, they all can help you feel better.
- Hemodialysis uses a machine to move your blood through a filter outside your body, removing wastes.
- Peritoneal dialysis uses the lining of your belly to filter your blood inside your body, removing wastes.
- Kidney transplantation is surgery to place a healthy kidney from a person who has just died or a living person, usually a family member, into your body to take over the job of filtering your blood.
- Conservative management is the choice not to treat kidney failure with dialysis or a transplant. Instead, the focus is on using medicines to keep you comfortable, preserving kidney function through diet, and treating the problems of kidney failure, such as anemia—a shortage of red blood cells that can make you tired—and weak bones.
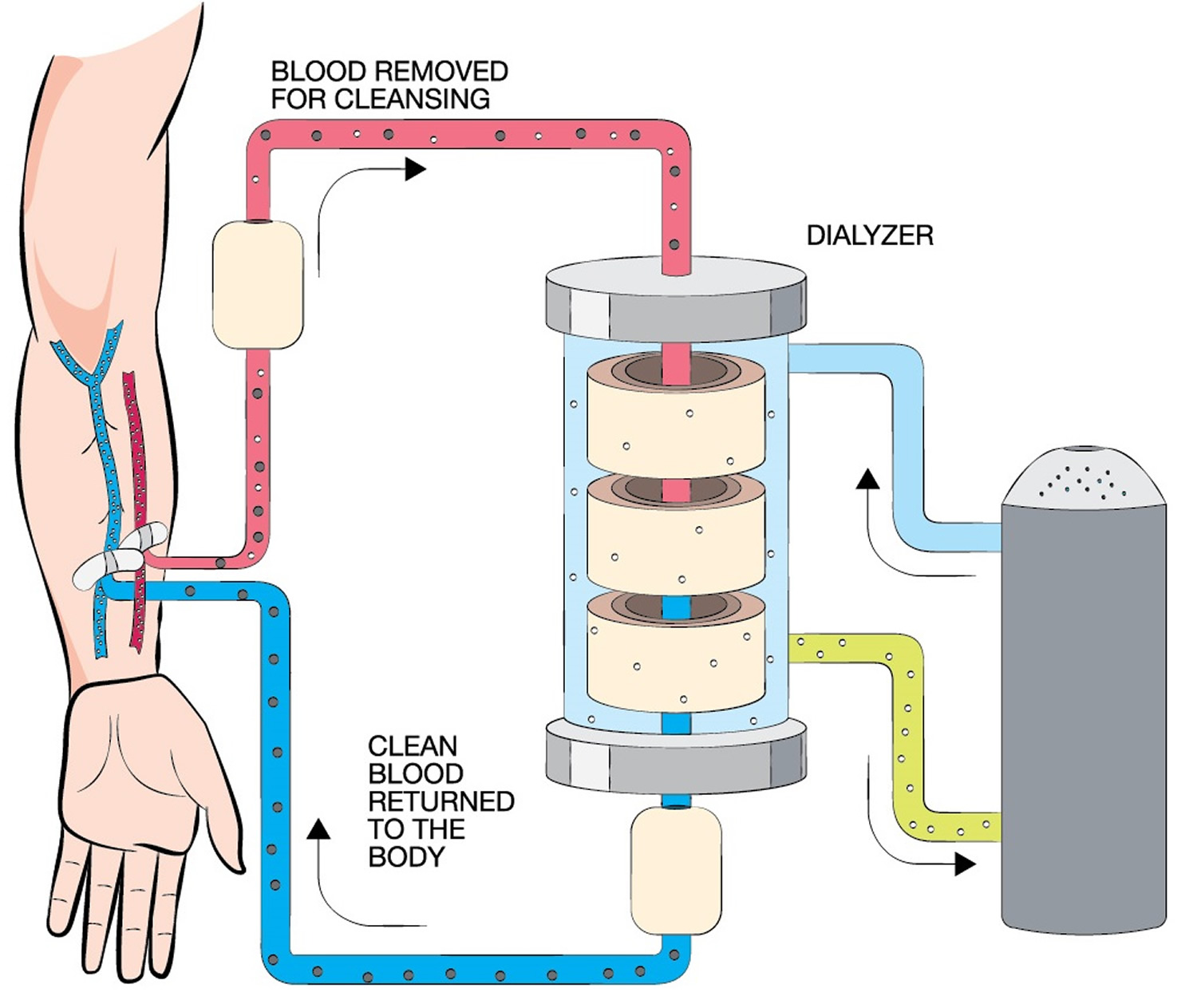
How does Hemodialysis work ?
Purpose of Hemodialysis
The purpose of hemodialysis is to filter your blood. This type of dialysis uses a machine to remove harmful wastes and extra fluid, as your kidneys did when they were healthy. Hemodialysis helps control blood pressure and balance important minerals, such as potassium, sodium, calcium, and bicarbonate, in your blood. Hemodialysis is not a cure for kidney failure; however, it can help you feel better and live longer.
How Hemodialysis Works
Before you can begin dialysis, a surgeon will create a vascular access, usually in your arm. A vascular access lets high volumes of blood flow continuously during hemodialysis treatments to filter the largest possible amounts of blood per treatment.
Hemodialysis uses a machine to move your blood through a filter, called a dialyzer, outside your body. A pump on the hemodialysis machine draws your blood through a needle into a tube, a few ounces at a time. Your blood then travels through the tube, which takes it to the dialyzer. Inside the dialyzer, your blood flows through thin fibers that filter out wastes and extra fluid. After the dialyzer filters your blood, another tube carries your blood back to your body. You can do hemodialysis at a dialysis center or in your home.
Hemodialysis can replace part of your kidney function. You will also need dietary changes, medicines, and limits on water and other liquids you drink and get from food. Your dietary changes, the number of medicines you need, and limits on liquid will depend on where you receive your treatments—at a dialysis center or at home—and how often you receive treatments—three or more times a week.
Pros and Cons of Hemodialysis
The pros and cons of hemodialysis differ for each person. What may be bad for one person may be good for another. Following is a list of the general pros and cons of dialysis center and home hemodialysis.
Dialysis Center Hemodialysis
Pros
- Dialysis centers are widely available.
- Trained health care providers are with you at all times and help administer the treatment.
- You can get to know other people with kidney failure who also need hemodialysis.
- You don’t have to have a trained partner or keep equipment in your home.
Cons
- The center arranges everyone’s treatments and allows few exceptions to the schedule.
- You need to travel to the center for treatment.
- This treatment has the strictest diet and limits on liquids because the longer time between treatments means wastes and extra fluid can build up in your body.
- You may have more frequent ups and downs in how you feel from day to day because of the longer time between sessions.
- Feeling better after a treatment may take a few hours.
Home Hemodialysis
Pros
- You can do the treatment at the times you choose; however, you should follow your doctor’s orders about how many times a week you need treatment.
- You don’t have to travel to a dialysis center.
- You gain a sense of control over your treatment.
- You will have fewer ups and downs in how you feel from day to day because of more frequent sessions.
- You can do your treatments at times that will let you work outside the home.
- You will have a more manageable diet and fewer limits on liquids because the shorter time between sessions prevents the buildup of wastes and extra fluid.
- You can take along a hemodialysis machine when traveling.
- You can spend more time with your loved ones because you don’t have to go to the dialysis center three times a week.
Cons
- Not all dialysis centers offer home hemodialysis training and support.
- You and a family member or friend will have to set aside a week or more at the beginning for training.
- Helping with treatments may be stressful for your family or friend.
- You need space for storing the hemodialysis machine and supplies at home.
- You will need to learn to put dialysis needles into your vascular access.
- Medicare and private insurance companies may limit the number of treatments they will pay for when you use home hemodialysis. Few people can afford the costs for additional treatments.
Figure 1. Hemodialysis

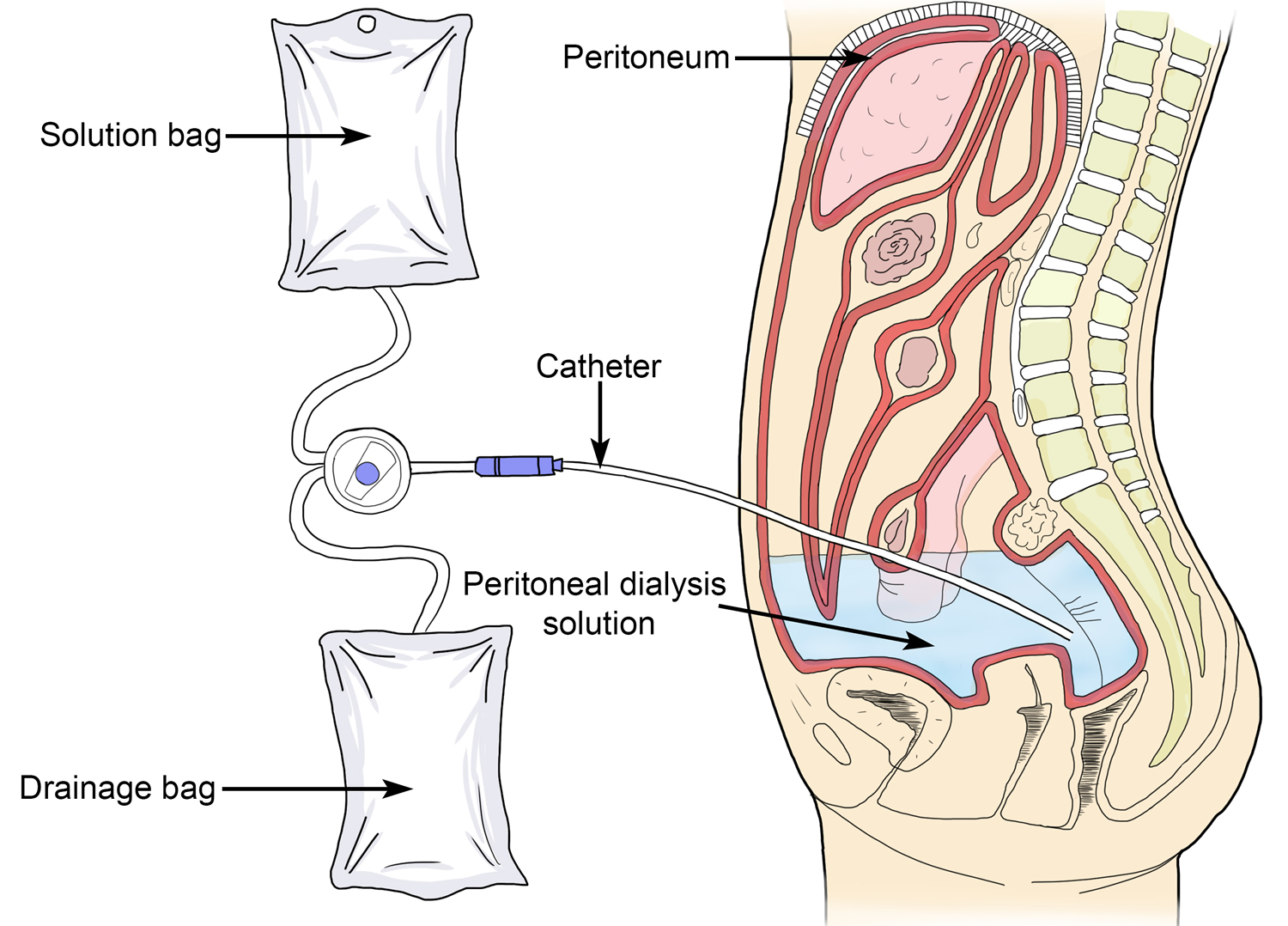
How does Peritoneal Dialysis work ?
Purpose of Peritoneal Dialysis
The purpose of peritoneal dialysis is to filter wastes and extra fluid from your body. This type of dialysis uses the lining of your belly—the space in your body that holds your stomach, bowels, and liver—to filter your blood. This lining, called the peritoneum, acts to do the work of your kidneys.
How Peritoneal Dialysis Works
A doctor will place a soft tube, called a catheter, in your belly a few weeks before you start treatment. The catheter stays in your belly permanently. When you start peritoneal dialysis, you will empty a kind of salty water, called dialysis solution, from a plastic bag through the catheter into your belly. When the bag is empty, you can disconnect your catheter from the bag so you can move around and do your normal activities. While the dialysis solution is inside your belly, it soaks up wastes and extra fluid from your body. After a few hours, you drain the used dialysis solution through another tube into a drain bag. You can throw away the used dialysis solution, now filled with wastes and extra fluid, in a toilet or tub. Then you start over with a fresh bag of dialysis solution. The process of emptying the used dialysis solution and refilling your belly with fresh solution is called an exchange. The process goes on continuously, so you always have dialysis solution in your belly soaking up wastes and extra fluid from your body.
Figure 2. Peritoneal dialysis
Types of Peritoneal Dialysis
Two types of peritoneal dialysis are available. After you have learned about the types of peritoneal dialysis, you can choose the type that best fits your life. If one schedule or type of peritoneal dialysis does not suit you, talk with your doctor about trying the other type.
Continuous ambulatory peritoneal dialysis does not require a machine and you can do it in any clean, well-lit place. The time period that the dialysis solution is in your belly is the dwell time. With continuous ambulatory peritoneal dialysis, the dialysis solution stays in your belly for a dwell time of 4 to 6 hours, or more. The process of draining the used dialysis solution and replacing it with fresh solution takes about 30 to 40 minutes. Most people change the dialysis solution at least four times a day and sleep with solution in their belly at night. With continuous ambulatory peritoneal dialysis, you do not have to wake up and perform dialysis tasks during the night.
Continuous cycler-assisted peritoneal dialysis uses a machine called a cycler to fill and empty your belly three to five times during the night while you sleep. In the morning, you begin one exchange with a dwell time that lasts the entire day. You may do an additional exchange in the middle of the afternoon without the cycler to increase the amount of waste removed and to reduce the amount of fluid left behind in your body.
You may need a combination of continuous ambulatory peritoneal dialysis and continuous cycler-assisted peritoneal dialysis if you weigh more than 175 pounds or if your peritoneum filters wastes slowly. For example, some people use a cycler at night and perform one exchange during the day. Others do four exchanges during the day and use a minicycler to perform one or more exchanges during the night. You’ll work with your health care team to find the best schedule for you.
Pros and Cons of Peritoneal Dialysis
Each type of peritoneal dialysis has pros and cons.
Continuous Ambulatory Peritoneal Dialysis
Pros
- You can do continuous ambulatory peritoneal dialysis alone.
- You can do continuous ambulatory peritoneal dialysis at the times you choose, as long as you perform the required number of exchanges each day.
- You can do continuous ambulatory peritoneal dialysis in many locations.
- You can travel as long as you bring dialysis bags with you or have them delivered to your destination.
- You don’t need a machine for continuous ambulatory peritoneal dialysis.
- You gain a sense of control over your treatment.
Cons
- Continuous ambulatory peritoneal dialysis can disrupt your daily schedule.
- Continuous ambulatory peritoneal dialysis is a continuous treatment, and you should do all exchanges 7 days a week.
- Boxes of dialysis solution will take up space in your home.
Continuous Cycler-assisted Peritoneal Dialysis
Pros
- You can do exchanges at night, while you sleep.
- You may not have to perform exchanges during the day.
Cons
- You need a machine.
- Your connection to the cycler limits your movement at night.
Is dialysis a cure for kidney failure ?
No. Hemodialysis and peritoneal dialysis help you feel better and live longer; however, they do not cure kidney failure. Although people with kidney failure are now living longer than ever, over the years kidney disease can cause other problems, such as heart disease, bone disease, arthritis, nerve damage, infertility, and malnutrition. These problems won’t go away with dialysis; however, doctors now have new and better ways to prevent or treat them. You should discuss these problems and their treatments with your doctor.
How Kidney Transplantation Works
The transplant process has many steps.
The first step is to talk with your health care provider about whether you are a candidate for a transplant. Transplantation is not for everyone. Your health care provider may tell you that you are not healthy enough for surgery or that you have a condition that would make transplantation unlikely to succeed. If you are a good candidate for a transplant, your health care provider will refer you to a transplant center.
Medical, Psychological, and Social Evaluation at a Transplant Center
The next step is a thorough physical, psychological, and social evaluation at the transplant center, where you will meet members of your transplant team. Your pretransplant evaluation may require several visits to the transplant center over the course of weeks or even months.
You will need to have blood tests as well as other tests to check your heart and other organs. Your blood type and other matching factors help determine whether your body will accept an available donor kidney.
Your transplant team will make sure you are healthy enough for surgery. Some medical conditions or illnesses could make transplantation less likely to succeed.
In addition, your team will make sure you can understand and follow the schedule for taking the medicines needed after surgery. Team members need to be sure that you are mentally prepared for the responsibilities of caring for a transplanted kidney.
If a family member or friend wants to donate a kidney, that person will need a health exam to test whether the kidney is a good match.
Who is on your transplant team ?
Your transplant team has many members, including your
- surgeon—the doctor who places the kidney in your body.
- nephrologist—a doctor who specializes in kidney health. The nephrologist may work in partnership with a nurse practitioner or a physician’s assistant.
- transplant coordinator—a specially trained nurse who will be your point of contact, arrange your appointments, and educate you before and after the transplant.
- social worker—a person who is trained to help people solve problems in their daily lives, such as finding employment, affordable housing, or daycare.
- dietitian—a person who is an expert in food and nutrition. Dietitians teach people about the foods they should eat and how to plan healthy meals.
Placement on the Waiting List
If your medical evaluation shows you are a good candidate for a transplant, your transplant center will submit your name to be placed on the national waiting list for a kidney from a deceased donor. The Organ Procurement and Transplantation Network has a computer network that links all regional organ-gathering organizations—known as organ procurement organizations—and transplant centers. The United Network for Organ Sharing (UNOS), a private, nonprofit organization, runs the Organ Procurement and Transplantation Network under a contract with the Federal Government. When UNOS officially adds you to the waiting list, UNOS will notify you and your transplant team.
UNOS allows you to register with multiple transplant centers to increase your chances of receiving a kidney. Each transplant center usually requires a separate medical evaluation.
Waiting Period
UNOS gives preference to people who have been on the waiting list the longest. However, other factors—such as your age, where you live, and your blood type—may make your wait longer or shorter. Wait times can range from a few months to several years.
If you have a living donor, you do not need to be placed on the waiting list and can schedule the surgery when it is convenient for you and your donor.
While you are on the waiting list, notify the transplant center of changes in your health. Also, let the transplant center know if you move or change phone numbers. The center will need to find you immediately when a kidney becomes available.
While you wait for a kidney, you will have blood drawn once a month. The sample will be sent to the transplant center. The center must have a recent sample of your blood for comparison with any kidney that becomes available.
Organ procurement organizations identify potential organs for transplant and coordinate with the national network. When a deceased donor kidney becomes available, the organ procurement organization notifies UNOS and creates a computer-generated list of suitable recipients.
Whether you are receiving your kidney from a deceased donor or a living donor, the transplant team considers three factors in matching kidneys with potential recipients. These matching factors help predict whether your body’s immune system—which protects your body from infection by identifying and destroying bacteria, viruses, and other potentially harmful foreign substances—will accept or reject the new kidney.
- Blood type. Your blood type—A, B, AB, or O—must be compatible with the donor’s. Blood type is the most important matching factor. Some transplant centers have developed techniques for transplanting kidneys that are not matched by blood type.
- Human leukocyte antigens. These six antigens are proteins that help your immune system tell the difference between your own body’s tissues and foreign substances. You may still receive a kidney if the antigens do not completely match, as long as your blood type is compatible with the organ donor’s blood type and other tests show no problems with matching.
- Cross-matching antigens. The cross-match is the last test performed before a kidney transplant can take place. A lab technician mixes a small sample of your blood with a sample of the organ donor’s blood in a tube to see if the mixture causes a reaction. If no reaction occurs—called a negative cross-match—the transplant can proceed.
Kidney Transplant Surgery
If you are on a waiting list for a deceased donor kidney, you must go to the hospital as soon as you receive notification that a kidney is available. If a family member or friend is donating the kidney you will receive, you will schedule the operation in advance. Your transplant team will operate on you and your donor at the same time, usually in side-by-side rooms. One surgeon will perform the nephrectomy—the removal of the kidney from the donor—while another prepares you for placement of the donated kidney. In some centers, the same surgeon performs both operations. You will receive general anesthesia to make you sleep during the operation. The surgery usually takes 3 or 4 hours.
Surgeons—place most transplanted kidneys in the lower front part of your abdomen. The kidney is connected to an artery, which brings unfiltered blood into the kidney, and a vein, which takes filtered blood out of the kidney. The surgeon also transplants the ureter from the donor to let urine from the new kidney flow to your bladder. Unless your damaged kidneys cause problems such as infection, they can remain in their normal position. The transplanted kidney takes over the job of filtering your blood. Your body normally attacks anything it sees as foreign, so to keep your body from attacking the kidney you need to take medicines called immunosuppressants for as long as the transplanted kidney functions.
Recovery from Kidney Transplant Surgery
After surgery, you will probably feel sore and groggy when you wake up. However, many people who have a transplant report feeling much better immediately after surgery. Even if you wake up feeling great, you will typically need to stay in the hospital for several days to recover from surgery, and longer if you have any complications. You will have regular follow-up visits after leaving the hospital.
If you have a living donor, the donor will probably also stay in the hospital for several days. However, a new technique for removing a kidney for donation uses a smaller incision and may make it possible for the donor to leave the hospital in 2 to 3 days.
Pros and Cons of Kidney Transplantation
Following is a list of the pros and cons of kidney transplantation.
Kidney Transplantation
Pros
- A transplanted kidney works like a healthy kidney.
- If you have a living donor, you can choose the time of your operation.
- You may feel healthier and have an improved quality of life.
- You have fewer dietary restrictions.
- You won’t need dialysis.
- People who receive a donated kidney have a greater chance of living a longer life than those who stay on dialysis.
Cons
- Transplantation requires surgery.
- You will go through extensive medical testing at the transplant clinic.
- You may need to wait years for a deceased donor kidney.
- Your body may reject the new kidney, so one transplant may not last a lifetime.
- You’ll need to take immunosuppressants, which may cause other health problems, for as long as the transplanted kidney functions.
What do you need to know about care after your kidney transplant ?
You need to know how to keep your body from rejecting your new kidney. Your immune system will sense that your new kidney is foreign. To keep your body from rejecting it, you will have to take medicines, called immunosuppressants, that turn off, or suppress, your immune system response. You may have to take two or more immunosuppressants, as well as medicines such as antibiotics to protect against infections. Your transplant team will teach you what each medicine is for and when to take each one. Be sure you understand the instructions for taking your medicines before you leave the hospital.
What are signs that your body is rejecting your new kidney ?
Often, rejection begins before any signs appear. The signs of rejection include indications that your kidney is not working as well as it should—for example, high blood pressure or swelling because your kidney is not getting rid of extra salt and fluid in your body. Advances in immunosuppressants have made other signs of rejection—such as fever, soreness in the lower abdomen where the new kidney is, and a decrease in the amount of urine you make—rare. If you have any of these symptoms, tell your transplant team. You will receive stronger doses of your immunosuppressants and additional medicines to help keep your body from rejecting your new kidney.
Even if you do everything you should, your body may still reject the new kidney, and you may need to go on dialysis. Unless your transplant team determines that you are no longer a good candidate for transplantation, you can go back on the waiting list for another kidney.
How do you know your new kidney is working properly ?
Blood tests help you know your new kidney is working. Before you leave the hospital, you will schedule an appointment with your transplant team at the transplant center. At that appointment, a health care provider will draw blood to be tested. The tests show how well your kidneys are removing wastes from your blood. At first, you may return to the transplant center every 2 weeks, then every month. Eventually, you will need to return to the transplant center only once every 6 months or once every year, after your transplant team has determined that your kidney is doing its job.
Your blood tests may show that your kidney is not removing wastes from your blood as well as it should. You may have other signs that your body is rejecting your new kidney. If these problems occur, your transplant surgeon or nephrologist may order a kidney biopsy. Biopsy is a procedure that involves taking a small piece of tissue for examination under a microscope. Your transplant surgeon or nephrologist performs the biopsy in the transplant center or a hospital. The health care provider will give you light sedation and local anesthetic; however, in some cases, a patient may require general anesthesia. A pathologist—a doctor who specializes in diagnosing diseases—examines the tissue in a lab. The test can show whether your body is rejecting your new kidney.
What are the side effects of immunosuppressants ?
Some immunosuppressants may change your appearance. Your face may get fuller; you may gain weight or develop acne or facial hair. Not all people have these problems, and those who do can use diet, makeup, and hair removal to minimize changes in appearance.
Immunosuppressants weaken your immune system, which can lead to infections. In some people over long periods of time, a weakened immune system can increase their risk of developing cancer. Some immunosuppressants cause cataracts, diabetes, extra stomach acid, high blood pressure, and bone disease. When used over time, these medicines may also cause liver or kidney damage in some people. Your transplant team will order regular tests to monitor the levels of immunosuppressants in your blood and to measure your liver and kidney function.
What financial help is available to pay for a kidney transplant ?
United States citizens who have kidney failure are eligible to receive Medicare, the Federal Government insurance program. Treatment for kidney failure costs a lot; however, Medicare pays much of the cost, usually up to 80 percent. Often, private insurance pays the rest. For people who are not eligible for Medicare or who still need help with the portion Medicare does not cover, states have Medicaid programs that provide funds for health care based on financial need. Your social worker can help you locate resources for financial help.
What help is available to pay for kidney transplant medicines ?
Through patient-assistance programs, prescription drug companies give discounts to people who can show they cannot afford the cost of their prescribed medicines. Social workers can help patients complete applications to these programs.
The Partnership for Prescription Assistance has a website that directs patients, caregivers, and doctors to more than 275 public and private patient-assistance programs, including more than 150 programs offered by pharmaceutical companies. The website www.pparx.org features tools to help a person determine which programs might be available.
NeedyMeds is a nonprofit organization that helps people find appropriate patient-assistance programs. The NeedyMeds website—www.needymeds.org —provides a directory of patient-assistance programs that can be searched by a medicine’s brand or generic name or by a program or company name. Applications for these programs are usually available online.
Eating, Diet, and Nutrition for Kidney Transplant Patients
The diet for transplant patients has more choices than the diet for dialysis patients, although you may still have to cut back on some foods. Your diet will probably change as your medicines, test results, weight, and blood pressure change.
- You may need to count calories. Your medicines may give you a bigger appetite and cause you to gain weight.
- You may have to eat less sodium. Your medicines may cause your body to retain sodium, leading to high blood pressure.
Your transplant center’s dietitian can help you understand the reasons for dietary limits, recognize foods you should avoid, and plan healthy and tasty meals.
What is conservative management for kidney failure ?
Conservative management for kidney failure is the choice to say no to or stop dialysis treatments. For many people, dialysis not only extends life, it also improves the quality of life. For others who have serious conditions in addition to kidney failure, dialysis may seem like a burden that only prolongs suffering. If you have serious conditions in addition to kidney failure, dialysis may not prolong your life or improve the quality of your life.
You have the right to say no to or stop dialysis. You may want to speak with your doctor, spouse, family, counselor, or renal social worker, who helps people with kidney disease, to help you make this decision.
If you stop dialysis treatments or say you do not want to begin them, you may live for a few weeks or for several months, depending on your health and your remaining kidney function. You may choose to receive care from a hospice—a facility or home program designed to meet the physical and emotional needs of the terminally ill—during this time. Hospice care focuses on relief of pain and other symptoms. Whether or not you choose to use a hospice, your doctor can give you medicines to make you more comfortable. Your doctor can also give you medicines to treat the problems of kidney failure, such as anemia or weak bones. You may restart dialysis treatment if you change your mind.
Advance Directives
An advance directive is a statement or document in which you give instructions either to withhold certain treatments, such as dialysis, or to provide them, depending on your wishes and the specific circumstances. Even if you are happy with your quality of life on dialysis, you should think about circumstances that might make you want to stop dialysis treatments. At some point in a medical crisis, you might lose the ability to tell your health care team and loved ones what you want. Advance directives may include
- a living will
- a durable power of attorney for health care decisions
- a do not resuscitate (DNR) order—a legal form that tells your health care team you do not want cardiopulmonary resuscitation (CPR) or other life-sustaining treatment if your heart were to stop or if you were to stop breathing.
A living will is a document that details the conditions under which you would want to refuse treatment. You may state that you want your health care team to use all available means to sustain your life, or you may direct that you be withdrawn from dialysis if you fall into a coma from which you most likely won’t wake up. In addition to dialysis, you may choose or refuse the following life-sustaining treatments:
- CPR
- feedings through a tube in your stomach
- mechanical or artificial means to help you breathe
- medicines to treat infections
- surgery
- receiving blood
Refusing to have CPR is the same as a do not resuscitate (DNR) order. If you choose to have a do not resuscitate (DNR) order, your doctor will place the order in your medical chart.
A durable power of attorney for health care decisions or a health care proxy is a document you use to assign a person to make health care decisions for you in the event you cannot make them for yourself. Make sure the person you name understands your values and will follow your instructions.
Each state has its own laws on advance directives. You can obtain a form for an advance medical directive that’s valid in your state from the National Hospice and Palliative Care Organization.
Kidney failure diet
Your dialysis center has a renal dietitian to help you plan your meals. A renal dietitian has special training in caring for the food and nutrition needs of people with kidney disease. Work with a registered dietitian to develop a meal plan that includes foods that you enjoy eating while maintaining your kidney health.
Use this information to help you learn how to eat right to feel right on hemodialysis. Read one section at a time. Then, review with your renal dietitian the sections marked “Talk with Your Renal Dietitian.”
Keep a copy of this information handy to remind yourself of foods you can eat and foods to avoid.
You will need to carefully plan your meals and keep track of the amount of liquids you eat and drink. It helps to limit or avoid foods and beverages that have lots of
- potassium
- phosphorus
- sodium—for example, vegetable juice and sports drinks
The first steps to eating right 10.
Step 1: Choose and prepare foods with less salt and sodium
Why? To help control your blood pressure. Your diet should contain less than 2,300 milligrams of sodium each day 10.
- Buy fresh food often. Sodium (a part of salt) is added to many prepared or packaged foods you buy at the supermarket or at restaurants.
- Cook foods from scratch instead of eating prepared foods, “fast” foods, frozen dinners, and canned foods that are higher in sodium. When you prepare your own food, you control what goes into it.
- Use spices, herbs, and sodium-free seasonings in place of salt.
- Check for sodium on the Nutrition Facts label of food packages. A Daily Value of 20 percent or more means the food is high in sodium.
- Try lower-sodium versions of frozen dinners and other convenience foods.
- Rinse canned vegetables, beans, meats, and fish with water before eating.
Look for food labels with words like sodium free or salt free; or low, reduced, or no salt or sodium; or unsalted or lightly salted.
Why is knowing about sodium important for someone with advanced chronic kidney disease ?
Too much sodium in a person’s diet can be harmful because it causes blood to hold fluid. People with chronic kidney disease need to be careful not to let too much fluid build up in their bodies. The extra fluid raises blood pressure and puts a strain on the heart and kidneys. A dietitian can help people find ways to reduce the amount of sodium in their diet. Nutrition labels provide information about the sodium content in food. The U.S. Food and Drug Administration advises that healthy people should limit their daily sodium intake to no more than 2,300 milligrams (mg), the amount found in 1 teaspoon of table salt. People who are at risk for a heart attack or stroke because of a condition such as high blood pressure or kidney disease should limit their daily sodium intake to no more than 1,500 mg. Choosing sodium-free or low-sodium food products will help them reach that goal.
Sodium is found in ordinary table salt and many salty seasonings such as soy sauce and teriyaki sauce. Canned foods, some frozen foods, and most processed meats have large amounts of salt. Snack foods such as chips and crackers are also high in salt.
Alternative seasonings such as lemon juice, salt-free seasoning mixes, and hot pepper sauce can help people reduce their salt intake. People with advanced chronic kidney disease should avoid salt substitutes that use potassium, such as AlsoSalt or Nu-Salt, because chronic kidney disease limits the body’s ability to eliminate potassium from the blood. The table below provides some high-sodium foods and suggestions for low-sodium alternatives that are healthier for people with any level of chronic kidney disease who have high blood pressure.
| High-sodium Foods | Low-sodium Alternatives |
|---|---|
|
|
Why is knowing about potassium important for someone with advanced chronic kidney disease ?
Keeping the proper level of potassium in the blood is essential. Potassium keeps the heart beating regularly and muscles working right. Problems can occur when blood potassium levels are either too low or too high. Damaged kidneys allow potassium to build up in the blood, causing serious heart problems. Potassium is found in many fruits and vegetables, such as bananas, potatoes, avocados, and melons. People with advanced chronic kidney disease may need to avoid some fruits and vegetables. Blood tests can indicate when potassium levels have climbed above normal range. A renal dietitian can help people with advanced chronic kidney disease find ways to limit the amount of potassium they eat. The potassium content of potatoes and other vegetables can be reduced by boiling them in water. The following table gives examples of some high-potassium foods and suggestions for low-potassium alternatives for people with advanced chronic kidney disease.
| High-potassium Foods | Low-potassium Alternatives |
|---|---|
|
|
Why is knowing about phosphorus important for someone with advanced chronic kidney disease ?
Damaged kidneys allow phosphorus, a mineral found in many foods, to build up in the blood. Too much phosphorus in the blood pulls calcium from the bones, making the bones weak and likely to break. Too much phosphorus may also make skin itch. Foods such as milk and cheese, dried beans, peas, colas, canned iced teas and lemonade, nuts, and peanut butter are high in phosphorus. A renal dietitian can help people with advanced chronic kidney disease learn how to limit phosphorus in their diet.
As chronic kidney disease progresses, a person may need to take a phosphate binder such as sevelamer hydrochloride (Renagel), lanthanum carbonate (Fosrenol), calcium acetate (PhosLo), or calcium carbonate (Tums) to control the phosphorus in the blood. These medications act like sponges to soak up, or bind, phosphorus while it is in the stomach. Because it is bound, the phosphorus does not get into the blood. Instead, it is removed from the body in the stool.
The table below lists some high-phosphorus foods and suggestions for low-phosphorus alternatives that are healthier for people with advanced chronic kidney disease.
| High-phosphorus Foods | Low-phosphorus Alternatives |
|---|---|
|
|
Step 2: Eat the right amount and the right types of protein
Why? To help protect your kidneys. When your body uses protein, it produces waste. Your kidneys remove this waste. Eating more protein than you need may make your kidneys work harder.
- Eat small portions of protein foods.
- Protein is found in foods from plants and animals. Most people eat both types of protein. Talk to your dietitian about how to choose the right combination of protein foods for you.
When kidney function declines to the point where dialysis becomes necessary, patients should include more protein in their diet because dialysis removes large amounts of protein from the blood.
Animal-protein foods:
- Chicken
- Fish
- Meat
- Eggs
- Dairy
A cooked portion of chicken, fish, or meat is about 2 to 3 ounces or about the size of a deck of cards. A portion of dairy foods is ½ cup of milk or yogurt, or one slice of cheese.
Plant-protein foods:
- Beans
- Nuts
- Grains
A portion of cooked beans is about ½ cup, and a portion of nuts is ¼ cup. A portion of bread is a single slice, and a portion of cooked rice or cooked noodles is ½ cup.
Step 3: Choose foods that are healthy for your heart
Why? To help keep fat from building up in your blood vessels, heart, and kidneys. To help keep fat from building up in your blood vessels, heart, and kidneys.
- Grill, broil, bake, roast, or stir-fry foods, instead of deep frying.
- Cook with nonstick cooking spray or a small amount of olive oil instead of butter.
- Trim fat from meat and remove skin from poultry before eating.
- Try to limit saturated and trans fats. Read the food label.
Heart-healthy foods:
- Lean cuts of meat, such as loin or round
- Poultry without the skin
- Fish
- Beans
- Vegetables
- Fruits
- Low-fat or fat-free milk, yogurt, and cheese
Limit alcohol
Drink alcohol only in moderation: no more than one drink per day if you are a woman, and no more than two if you are a man. Drinking too much alcohol can damage the liver, heart, and brain and cause serious health problems. Ask your health care provider how much alcohol you can drink safely.
A renal dietitian can help people learn about the amount and sources of protein in their diet. Animal protein in egg whites, cheese, chicken, fish, and red meats contain more of the essential nutrients a body needs. With careful meal planning, a well-balanced vegetarian diet can also provide these nutrients. A renal dietitian can help people with advanced chronic kidney disease make small adjustments in their eating habits that can result in significant protein reduction. For example, people can lower their protein intake by making sandwiches using thinner slices of meat and adding lettuce, cucumber slices, apple slices, and other garnishes. The following table lists some higher-protein foods and suggestions for lower-protein alternatives that are better choices for people with chronic kidney disease trying to limit their protein intake.
Why is it important to keep track of how much liquid you eat or drink ?
You may feel better if you keep track of and limit how much liquid you eat and drink. Excess fluid can build up in your body and may cause
- swelling and weight gain between dialysis sessions
- changes in your blood pressure
- your heart to work harder, which can lead to serious heart trouble
- a buildup of fluid in your lungs, making it hard for you to breathe
Hemodialysis removes extra fluid from your body. However, hemodialysis can remove only so much fluid at a time safely. If you come to your hemodialysis with too much fluid in your body, your treatment may make you feel ill. You may get muscle cramps or have a sudden drop in blood pressure that causes you to feel dizzy or sick to your stomach.
Your health care provider can help you figure out how much liquid is right for you.
One way to limit how much liquid you have is to limit the salt in the foods you eat. Salt makes you thirsty, so you drink more. Avoid salty foods such as chips and pretzels.
Your renal dietitian will give you other tips to help you limit how much liquid you consume while making sure you don’t feel too thirsty.
What foods count as liquid and why ?
Foods that are liquid at room temperature, such as soup, contain water. Gelatin, pudding, ice cream, and other foods that include a lot of liquid in the recipe also count. Most fruits and vegetables contain water, such as melons, grapes, apples, oranges, tomatoes, lettuce, and celery. When you count up how much liquid you have in a day, be sure to count these foods.
What is your dry weight ?
Your dry weight is your weight after a hemodialysis session has removed all extra fluid from your body. Controlling your liquid intake helps you stay at your proper dry weight. If you let too much fluid build up between sessions, it is harder to achieve your dry weight. Your health care provider can help you figure out what dry weight is right for you.
My dry weight goal: _____________.
Should you take vitamin and mineral supplements ?
You may not get enough vitamins and minerals in your diet because you have to avoid so many foods. Hemodialysis also removes some vitamins from your body. Your health care provider may prescribe a vitamin and mineral supplement designed specifically for people with kidney failure.
Warning: Do not take nutritional supplements you can buy over the counter. These supplements may contain vitamins or minerals that are harmful to you. For safety reasons, talk with your health care provider before using probiotics, dietary supplements, or any other medicine together with or in place of the treatment your health care provider prescribes.
What is acute kidney failure
Acute kidney failure occurs when your kidneys suddenly become unable to filter waste products from your blood 11. When your kidneys lose their filtering ability, dangerous levels of wastes may accumulate, and your blood’s chemical makeup may get out of balance.
Acute kidney failure — also called acute renal failure or acute kidney injury — develops rapidly over a few hours or a few days 11. Acute kidney failure is most common in people who are already hospitalized, particularly in critically ill people who need intensive care.
Acute kidney failure can be fatal and requires intensive treatment 11. However, acute kidney failure may be reversible 11. If you’re otherwise in good health, you may recover normal or nearly normal kidney function 11.
What are Signs and Symptoms of Acute Kidney Failure
Signs and symptoms of acute kidney failure may include:
- Decreased urine output, although occasionally urine output remains normal
- Fluid retention, causing swelling in your legs, ankles or feet
- Drowsiness
- Shortness of breath
- Fatigue
- Confusion
- Nausea
- Seizures or coma in severe cases
- Chest pain or pressure
Sometimes acute kidney failure causes no signs or symptoms and is detected through lab tests done for another reason.
Causes of Acute kidney failure
Acute kidney failure can occur when:
- You have a condition that slows blood flow to your kidneys
- You experience direct damage to your kidneys
- Your kidneys’ urine drainage tubes (ureters) become blocked and wastes can’t leave your body through your urine
Impaired blood flow to the kidneys
Diseases and conditions that may slow blood flow to the kidneys and lead to kidney failure include:
- Blood or fluid loss
- Blood pressure medications
- Heart attack
- Heart disease
- Infection
- Liver failure
- Use of aspirin, ibuprofen (Advil, Motrin IB, others), naproxen (Aleve, others) or related drugs
- Severe allergic reaction (anaphylaxis)
- Severe burns
- Severe dehydration
Damage to the kidneys
These diseases, conditions and agents may damage the kidneys and lead to acute kidney failure:
- Blood clots in the veins and arteries in and around the kidneys
- Cholesterol deposits that block blood flow in the kidneys
- Glomerulonephritis, inflammation of the tiny filters in the kidneys (glomeruli)
- Hemolytic uremic syndrome, a condition that results from premature destruction of red blood cells
- Infection
- Lupus, an immune system disorder causing glomerulonephritis
- Medications, such as certain chemotherapy drugs, antibiotics, dyes used during imaging tests and zoledronic acid (Reclast, Zometa), used to treat osteoporosis and high blood calcium levels (hypercalcemia)
- Multiple myeloma, a cancer of the plasma cells
- Scleroderma, a group of rare diseases affecting the skin and connective tissues
- Thrombotic thrombocytopenic purpura, a rare blood disorder
- Toxins, such as alcohol, heavy metals and cocaine
- Vasculitis, an inflammation of blood vessels
Urine blockage in the kidneys
Diseases and conditions that block the passage of urine out of the body (urinary obstructions) and can lead to acute kidney failure include:
- Bladder cancer
- Blood clots in the urinary tract
- Cervical cancer
- Colon cancer
- Enlarged prostate
- Kidney stones
- Nerve damage involving the nerves that control the bladder
- Prostate cancer
Risk factors for Acute kidney failure
Acute kidney failure almost always occurs in connection with another medical condition or event. Conditions that can increase your risk of acute kidney failure include:
- Being hospitalized, especially for a serious condition that requires intensive care
- Advanced age
- Blockages in the blood vessels in your arms or legs (peripheral artery disease)
- Diabetes
- High blood pressure
- Heart failure
- Kidney diseases
- Liver diseases.
How to Prevent having an Acute Kidney Failure ?
Acute kidney failure is often difficult to predict or prevent. But you may reduce your risk by taking care of your kidneys. Try to:
- Pay attention to labels when taking over-the-counter (OTC) pain medications. Follow the instructions for OTC pain medications, such as aspirin, acetaminophen (Tylenol, others) and ibuprofen (Advil, Motrin IB, others). Taking too much of these medications may increase your risk of acute kidney failure. This is especially true if you have pre-existing kidney disease, diabetes or high blood pressure.
- Work with your doctor to manage kidney problems. If you have kidney disease or another condition that increases your risk of acute kidney failure, such as diabetes or high blood pressure, stay on track with treatment goals and follow your doctor’s recommendations to manage your condition.
- Make a healthy lifestyle a priority. Be active; eat a sensible, balanced diet; and drink alcohol only in moderation — if at all.
Complications of acute kidney failure
Potential complications of acute kidney failure include:
- Fluid buildup. Acute kidney failure may lead to a buildup of fluid in your lungs, which can cause shortness of breath.
- Chest pain. If the lining that covers your heart (pericardium) becomes inflamed, you may experience chest pain.
- Muscle weakness. When your body’s fluids and electrolytes — your body’s blood chemistry — are out of balance, muscle weakness can result. Elevated levels of potassium in your blood are particularly dangerous.
- Permanent kidney damage. Occasionally, acute kidney failure causes permanent loss of kidney function, or end-stage renal disease. People with end-stage renal disease require either permanent dialysis — a mechanical filtration process used to remove toxins and wastes from the body — or a kidney transplant to survive.
- Death. Acute kidney failure can lead to loss of kidney function and, ultimately, death. The risk of death is higher in people who had kidney problems before acute kidney failure.
Acute kidney failure diagnosis
If your signs and symptoms suggest that you have acute kidney failure, your doctor may recommend certain tests and procedures to verify your diagnosis. These may include:
- Urine output measurements. The amount of urine you excrete in a day may help your doctor determine the cause of your kidney failure.
- Urine tests. Analyzing a sample of your urine, a procedure called urinalysis, may reveal abnormalities that suggest kidney failure.
- Blood tests. A sample of your blood may reveal rapidly rising levels of urea and creatinine — two substances used to measure kidney function.
- Imaging tests. Imaging tests such as ultrasound and computerized tomography may be used to help your doctor see your kidneys.
- Removing a sample of kidney tissue for testing. In some situations, your doctor may recommend a kidney biopsy to remove a small sample of kidney tissue for lab testing. Your doctor inserts a needle through your skin and into your kidney to remove the sample.
Treatment for acute kidney failure
Treatment for acute kidney failure typically requires a hospital stay. Most people with acute kidney failure are already hospitalized. How long you’ll stay in the hospital depends on the reason for your acute kidney failure and how quickly your kidneys recover.
In some cases, you may be able to recover at home.
Treating the underlying cause of your kidney failure
Treatment for acute kidney failure involves identifying the illness or injury that originally damaged your kidneys. Your treatment options depend on what’s causing your kidney failure.
Treating complications until your kidneys recover
Your doctor will also work to prevent complications and allow your kidneys time to heal. Treatments that help prevent complications include:
- Treatments to balance the amount of fluids in your blood. If your acute kidney failure is caused by a lack of fluids in your blood, your doctor may recommend intravenous (IV) fluids. In other cases, acute kidney failure may cause you to have too much fluid, leading to swelling in your arms and legs. In these cases, your doctor may recommend medications (diuretics) to cause your body to expel extra fluids.
- Medications to control blood potassium. If your kidneys aren’t properly filtering potassium from your blood, your doctor may prescribe calcium, glucose or sodium polystyrene sulfonate (Kayexalate, Kionex) to prevent the accumulation of high levels of potassium in your blood. Too much potassium in the blood can cause dangerous irregular heartbeats (arrhythmias) and muscle weakness.
- Medications to restore blood calcium levels. If the levels of calcium in your blood drop too low, your doctor may recommend an infusion of calcium.
- Dialysis to remove toxins from your blood. If toxins build up in your blood, you may need temporary hemodialysis — often referred to simply as dialysis — to help remove toxins and excess fluids from your body while your kidneys heal. Dialysis may also help remove excess potassium from your body. During dialysis, a machine pumps blood out of your body through an artificial kidney (dialyzer) that filters out waste. The blood is then returned to your body.
Home remedies for acute kidney failure
During your recovery from acute kidney failure, your doctor may recommend a special diet to help support your kidneys and limit the work they must do. Your doctor may refer you to a dietitian who can analyze your current diet and suggest ways to make your diet easier on your kidneys.
Depending on your situation, your dietitian may recommend that you:
- Choose lower potassium foods. Your dietitian may recommend that you choose lower potassium foods. High-potassium foods include bananas, oranges, potatoes, spinach and tomatoes. Examples of low-potassium foods include apples, cabbage, green beans, grapes and strawberries.
- Avoid products with added salt. Lower the amount of sodium you eat each day by avoiding products with added salt, including many convenience foods, such as frozen dinners, canned soups and fast foods. Other foods with added salt include salty snack foods, canned vegetables, and processed meats and cheeses.
- Limit phosphorus. Phosphorus is a mineral found in foods, such as milk, cheese, dried beans, nuts and peanut butter. Too much phosphorus in your blood can weaken your bones and cause skin itchiness. Your dietitian can give you specific recommendations on phosphorus and how to limit it in your particular situation.
As your kidneys recover, you may no longer need to eat a special diet, although healthy eating remains important.
- Kidney Failure. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure[↩]
- Smith HW The Kidney: Structure and Function in Health and DiseaseNew YorkOxford Univ Pr, 1951, pg. 520-74[↩]
- Lindeman RD, TobinJ, ShockNW. Longitudinal studies on the rate of decline in renal function with age, J Am Geriatr Soc, 1985, vol. 33, pg. 278-85[↩]
- ManjunathG, TighiouartH, CoreshJ, MacleodB, SalemDN, GriffithJL. Level of kidney function as a risk factor for cardiovascular outcomes in the elderly, Kidney Int, 2003, vol. 63, pg. 1121-1129[↩]
- Aronoff GR, Berns JS, BrierME, GolperTA, MorrisonG, SingerI. Drug Prescribing in Renal Failure: Dosing Guidelines for AdultsPhiladelphiaAmerican College of Physicians, 2002[↩]
- CoreshJ, AstorBC, GreeneT, EknoyanG, LeveyAS. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey, Am J Kidney Dis, 2003, vol. 41, pg. 1-12[↩]
- ObradorGT, AroraPKauszAT, RuthazerR, PereiraBJ, LeveyAS. Level of renal function at the initiation of dialysis in the U.S. end-stage renal disease population, Kidney Int, 1999, vol. 56, pg. 2227-35[↩]
- Kidney failure. American Kidney Fund. http://www.kidneyfund.org/kidney-disease/kidney-failure/[↩]
- http://nkdep.nih.gov/professionals/gfr_calculators/gfr_faq.htm[↩]
- Eating Right for Chronic Kidney Disease. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/kidney-disease/chronic-kidney-disease-ckd/eating-nutrition[↩][↩]
- Acute kidney failure. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/kidney-failure/basics/definition/con-20024029[↩][↩][↩][↩][↩]