Contents
What is laparoscopy
Laparoscopy is another name for “keyhole” surgery or “minimally invasive” diagnostic medical procedure used to check or to operate on the internal organs or tissues inside your belly (abdomen) or pelvic cavities. Laparoscopy can also check a woman’s pelvic organs. A laparoscopy procedure (also known as peritoneoscopy) uses a thin lighted tube that has a video camera called a laparoscope, that is inserted through a tiny cut or incision in your abdominal wall, to examine the inside of the abdomen. Gas (carbon dioxide or CO2) is used to inflate your belly so the surgeon can see the organs properly. One or more other small incisions may be made for other small instruments if needed. The video camera images can be seen on a computer screen.
Laparoscopy is performed under general anesthesia, usually by a surgeon or gynecologist (women’s health specialist).
Laparoscopy may be recommended as a test to help with the diagnosis of a variety of symptoms and conditions, including:
- endometriosis (a condition affecting women, where uterus lining tissue grows outside the uterus);
- unexplained severe pelvic or abdominal pain;
- infertility in women;
- ovarian cysts;
- cancers in the abdomen or pelvis.
During the procedure, your doctor may take some small tissue samples – biopsies – to help make a diagnosis.
Sometimes treatment can be carried out at the same time as a laparoscopic investigation.
Using laparoscopy to treat disease:
Laparoscopy can be used not only to look at the pelvic organs, but also to undertake procedures. By using the laparoscope to view the pelvis, instruments can be passed through the keyholes in the abdomen, and the gynecologist can perform many operations, for example:
- hysterectomy
- removal of the tubes or ovaries
- removal of cysts or other tumors in the pelvis
- treatment of scar tissue
- treatment of endometriosis
- treatment of prolapse
- assessment of pain
- assessment of infertility
Laparoscopy can also be used to remove organs such as the appendix (appendectomy) or the gallbladder (cholecystectomy).
One benefit of laparoscopy is that it is minimally invasive. That means it uses a very small cut in the belly. Laparoscopy usually takes less time and has a faster recovery than open surgery. Laparoscopy has advantages over traditional surgery, such as more rapid recovery, reduced pain and much smaller scars. If you have a laparoscopy, it often means you don’t need to stay in hospital overnight. People who have laparoscopy surgery usually recover quite quickly.
If you had a laparoscopy as a diagnostic procedure (where no surgery was performed), you can usually return to your usual activities within about 5 days.
When you wake from the laparoscopy procedure, you may feel a little sore around the cuts. You may also have some pain in your shoulder – this is caused by pressure from the gas in your abdomen.
After a few hours in recovery, you are likely to be sent home with care instructions, including pain management, dressings and stitches you may have.
Laparoscopy recovery time
People who have had laparoscopic surgery need more recovery time, and the amount of time will depend on the procedure performed. However, the recovery time is much shorter than would be needed for an open operation.
If you had a laparoscopy as a diagnostic procedure (where no surgery was performed), you can usually return to your usual activities within about 5 days.
Because only tiny cuts are required with laparoscopic surgery, there is much less pain after the operation compared with open surgery (where a much larger incision is needed). This means that having a laparoscopy reduces the length of your hospital stay. Depending on the type of surgery you have, you may be able to leave hospital on the same day as your operation. It may take several weeks before you are able to participate in all of your usual activities – check with your doctor.
Because only small incisions are made, you will also have smaller, less noticeable scars. Your surgeon may wish to see you a week or so after the surgery to check that the wounds are healing well.
Minimally invasive surgery
Some common types of minimally invasive surgery are listed below:
- Laparoscopy involves placing a lighted telescope (called a laparoscope) with a camera into your belly through a very small incision in the belly button. This allows the surgeon to see inside your belly and pelvis.
- Robotic laparoscopy uses laparoscopic instruments controlled by a surgeon seated at a console.
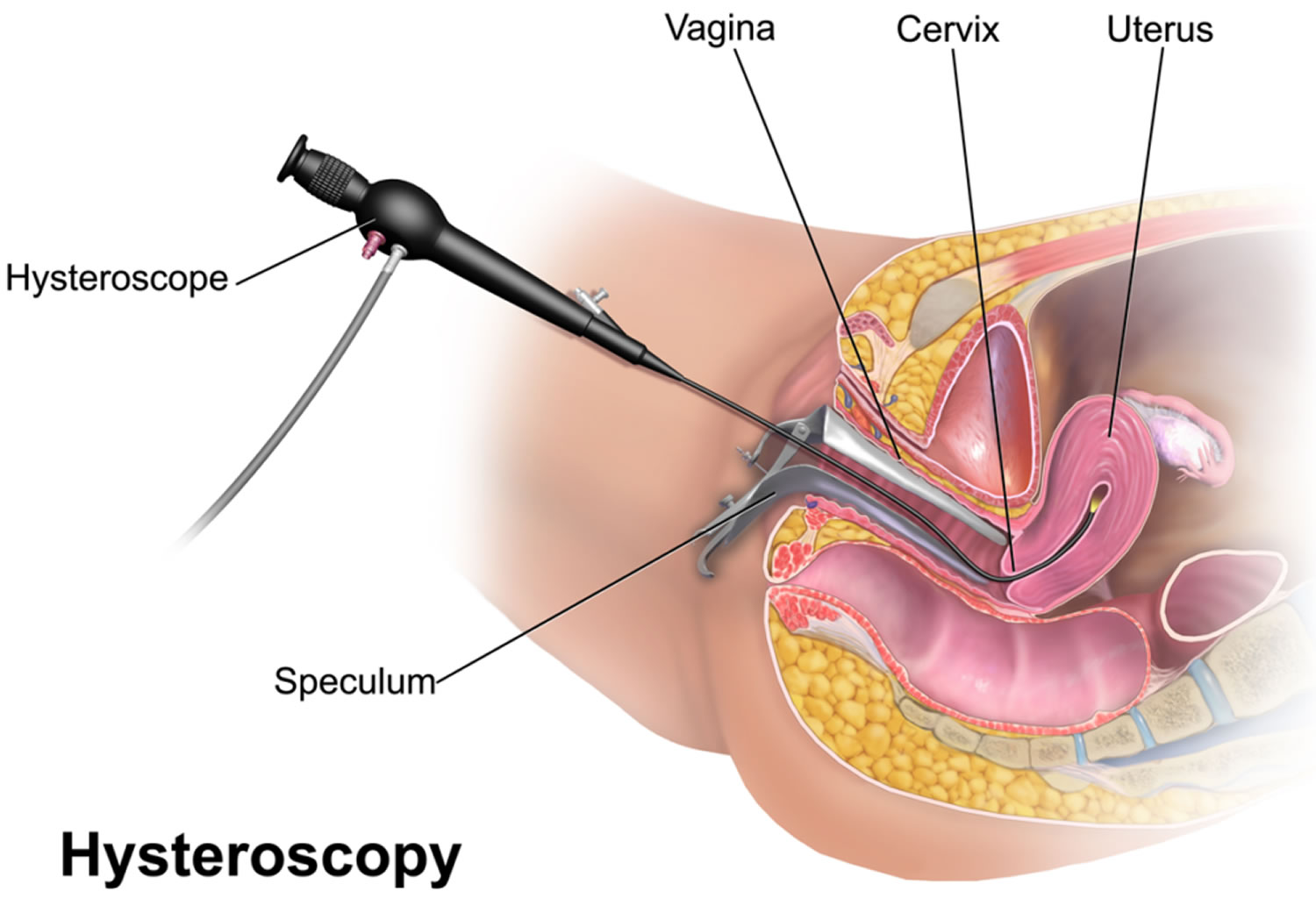
- Hysteroscopy uses a lighted telescope (called a hysteroscope) that is inserted through the vagina and cervix (neck of the womb) to see the inside of the uterus (womb). There are no incisions made.
Benefits of minimally invasive surgery
- Fewer scars on the outside
Scars from minimally invasive surgery are much smaller than in traditional open surgery. Laparoscopy involves 1 incision in the belly button and 1 to 3 others in the lower belly. These incisions are usually 1/4-1/2 inch long. Hysteroscopy leaves no scar because the instrument goes through the natural opening (neck of the womb) from the vagina into the uterus.
- Fewer scars on the inside
In general, all surgery can cause adhesions or scar tissue inside your lower belly abdomen). These scars can cause pain, problems with getting pregnant, or bowel blockage. Minimally invasive surgery may cause less scarring.
- Quicker recovery
Minimally invasive surgery doesn’t usually require a woman to stay overnight in the hospital, compared with 2 to 4 days after open surgery. This reduces the risk for problems such as blood clots in the legs or infection.
- Less pain, less medication
Because incisions are smaller, minimally invasive surgery is less painful than open surgery. This means that women need less pain medication and recover more quickly.
Disadvantages of minimally invasive surgery
- It’s not suitable for everyone
Some minimally invasive surgery is riskier for women who have had previous “open” surgery in the upper or lower part of their belly, or women with other medical problems. The surgeon may have other reasons to choose open, and not minimally invasive, surgery. Not all surgeries can be done with minimally invasive techniques.
- Special training and equipment
Surgeons need special training before they can perform minimally invasive surgery. Not all doctors are qualified to do these types of procedures and not all hospitals have the special equipment necessary to do some or all of these kinds of surgeries.
You should speak to your doctor to find out what type of surgery is best for you.
Laparoscopic surgery
An increasing number of problems that used to require major surgery can now be treated with laparoscopic surgery.
Laparoscopic surgery is commonly used by gynecologists (specialists in conditions affecting the female reproductive system) to perform procedures such as:
- female sterilization or tubal ligation (having your fallopian tubes ‘tied’ or clipped as a permanent form of contraception);
- hysterectomy (removal of the uterus);
- removal of ovarian cysts; and
- treatment of ectopic pregnancy (where a pregnancy implants outside the uterus – most often ectopic pregnancies occur in a fallopian tube).
Common non-gynecological laparoscopic operations include the following.
- Removal of the gallbladder (called laparoscopic cholecystectomy), which is a very common procedure and is usually done to treat people with gallstones that are causing problems.
- Removal of the appendix (appendectomy) to treat appendicitis.
- Weight loss surgery (also known as bariatric surgery) such as laparoscopic adjustable gastric banding (LAGB) or laparoscopic sleeve gastrectomy.
- Hernia repairs.
It is also possible to remove some cancers from the abdomen or pelvis laparoscopically. Sometimes this involves removal of the whole organ that is affected by cancer.
Why might you need a laparoscopy?
Laparoscopy is used to diagnosis conditions or perform surgery in the abdominal and pelvic area. It can be used to check the abdomen and the pelvic cavities and its organs for:
- Tumors and other growths
- Injuries
- Bleeding inside the belly
- Infections
- Belly pain that can’t be explained
- Blockages
- Other conditions
- Remove cysts or other tumors
- Remove the gall bladder
- Remove parts of the intestine
- Take a biopsy (a small tissue sample) for testing
- Search for the causes of ongoing abdominal or pelvic pain.
A laparoscopy is often done when the results of a physical exam, X-ray, or CT scan are not clear.
Laparoscopy may be used to determine a stage of cancer for an abdominal organ. Laparoscopy may also be used to check an abdominal injury. It can see where the injury is and how deep it is. Laparoscopy can also see how much internal bleeding you have.
For women, a gynecologic laparoscopy may be used to check:
- Diagnose or treat endometriosis
- Pelvic pain and problems
- Assess painful or heavy periods
- Ovarian cysts
- Uterine fibroids
- The fallopian tubes
- Remove the uterus, fallopian tubes or ovaries
- Diagnose or remove ovarian cysts
- Assess female infertility
- Treat ectopic pregnancy
Laparoscopy can also be used to treat endometriosis. This is when tissue that normally lines the uterus grows outside it. Laparoscopy may be done to treat an ectopic pregnancy or to do a tubal ligation (tie the fallopian tubes) to permanently prevent pregnancy.
There may be other reasons for your provider to suggest a laparoscopy.
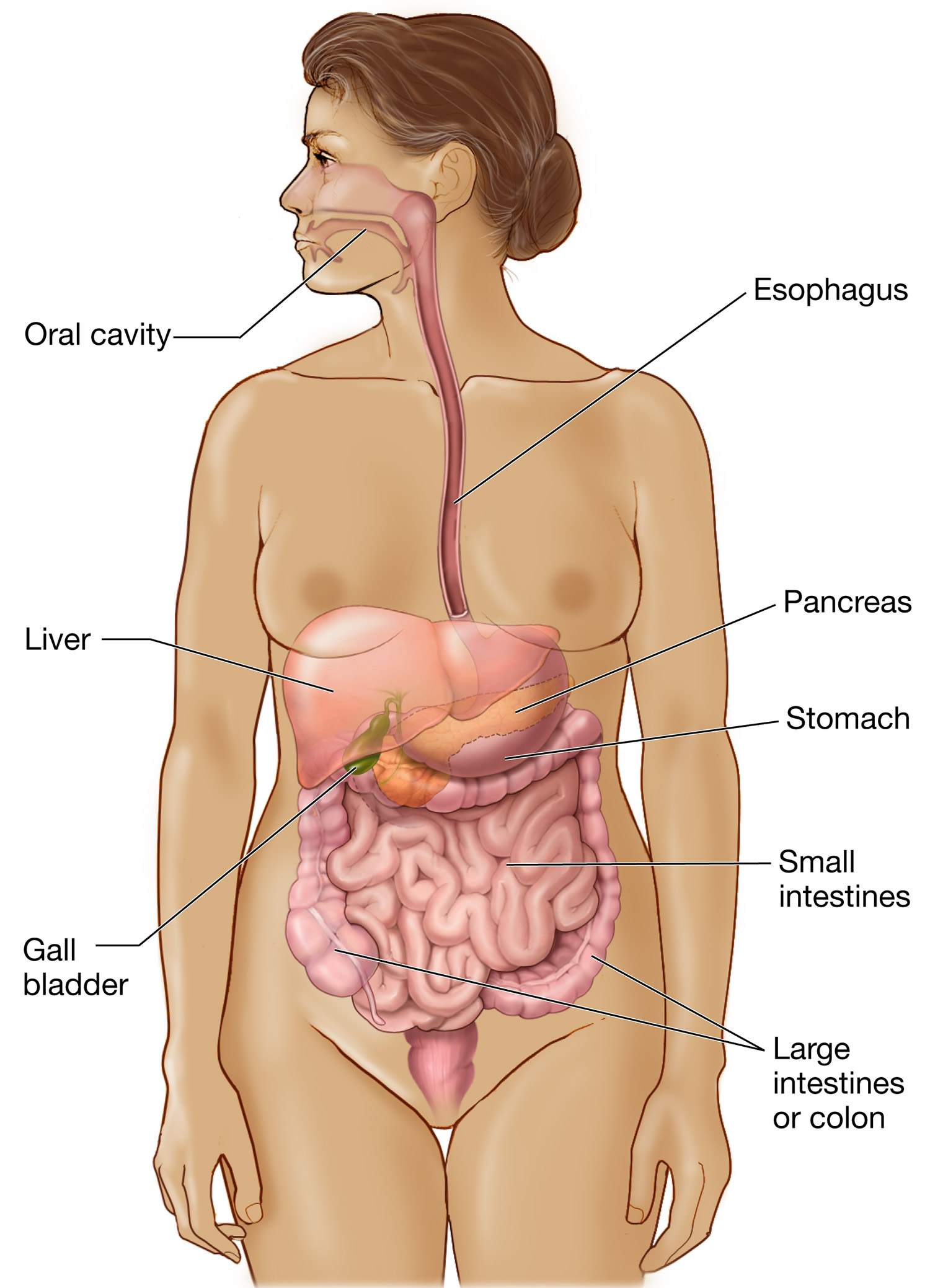
Figure 1. Gastrointestinal system (digestive system)
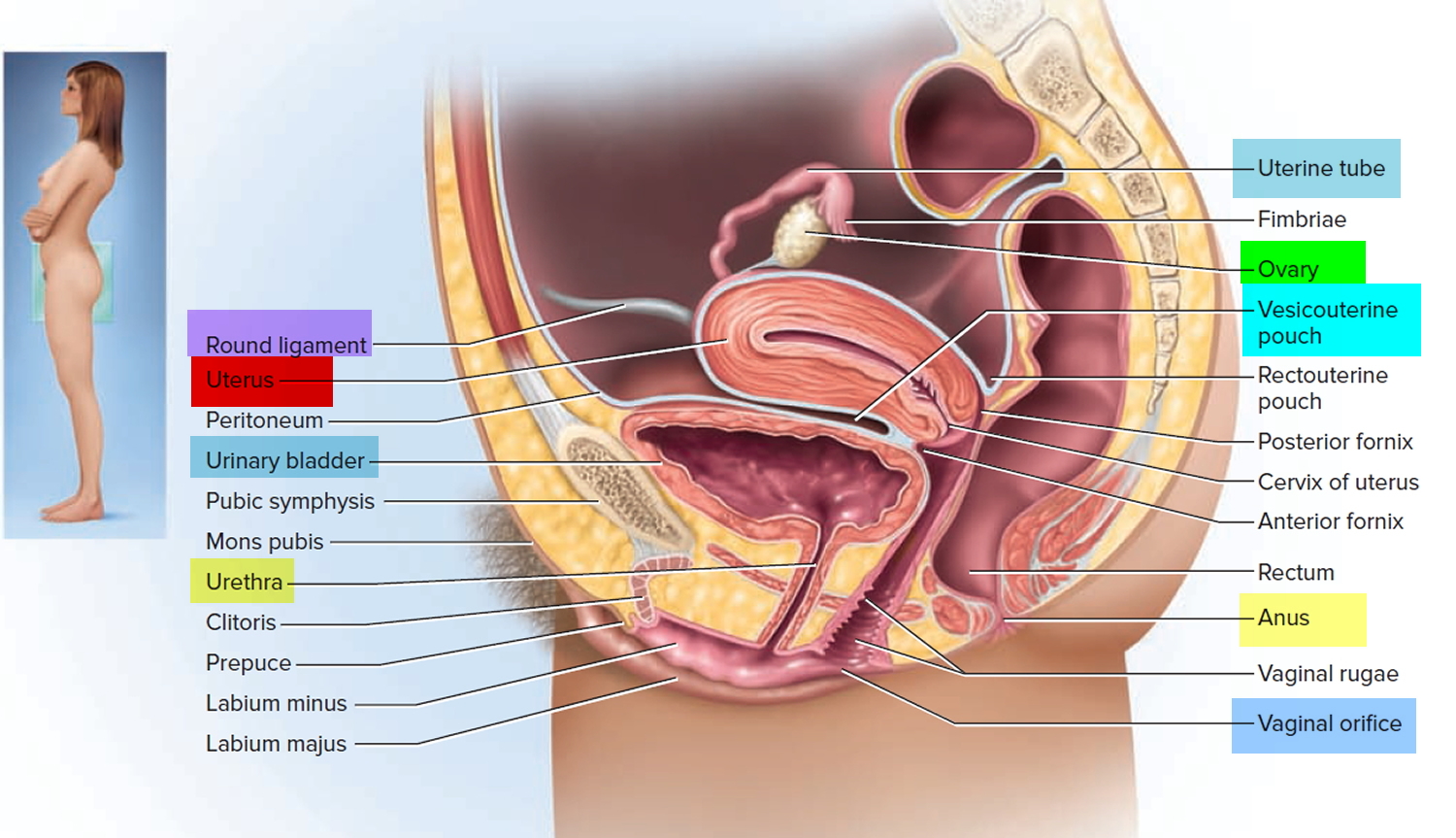
Figure 2. Uterus location
Diagnostic laparoscopy
Exploratory laparoscopy or diagnostic laparoscopy can help physicians diagnose many abdominal and gynecological problems including endometriosis, uterine fibroids and other structural abnormalities, ovarian cysts, adhesions (scar tissue), and ectopic pregnancy. If you have pain, history of past pelvic infection, or symptoms suggestive of pelvic disease, your physician may recommend this procedure as part of your evaluation. Laparoscopy is sometimes recommended after completing an initial infertility evaluation on both partners. Laparoscopy is usually performed soon after menstruation ends.
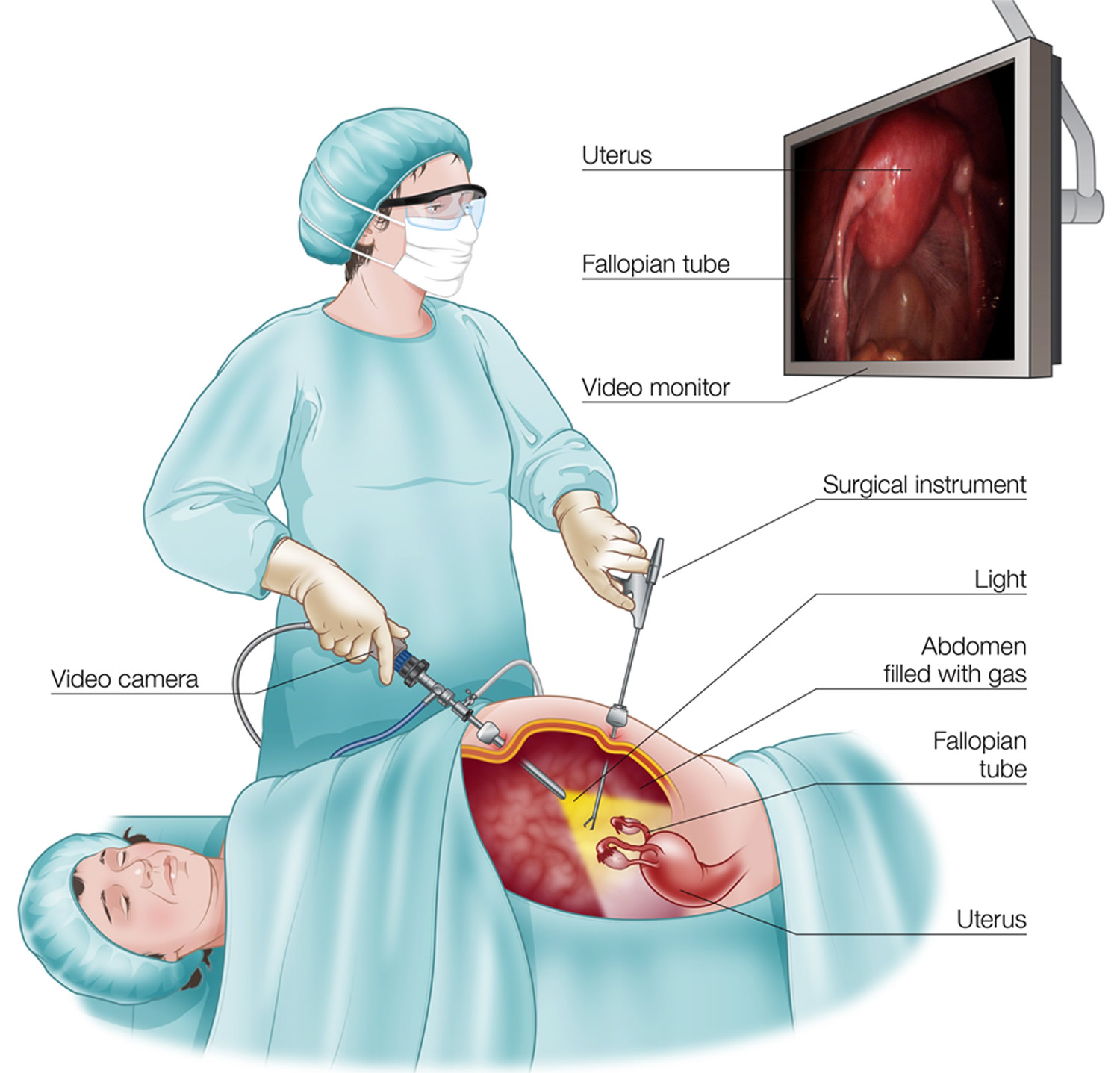
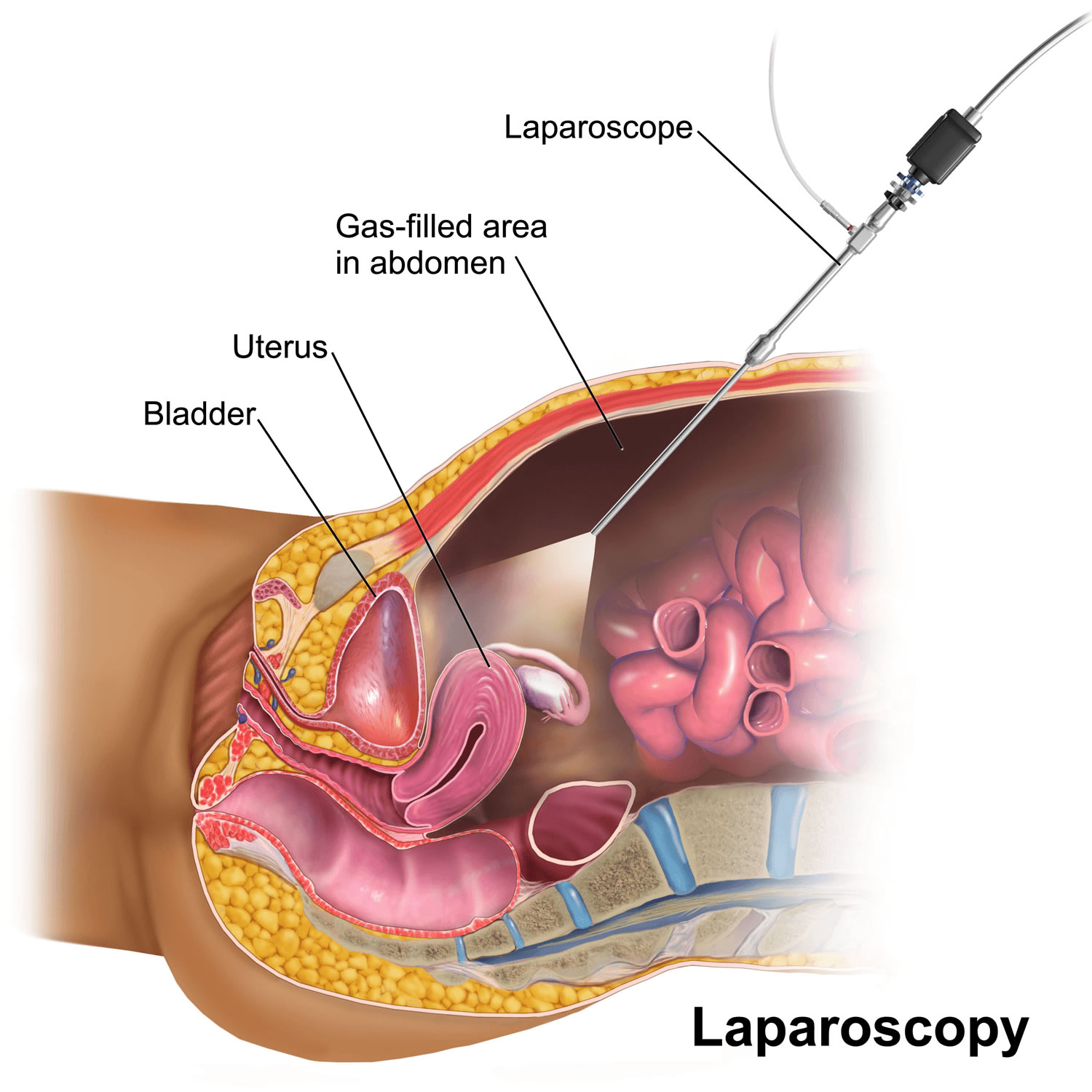
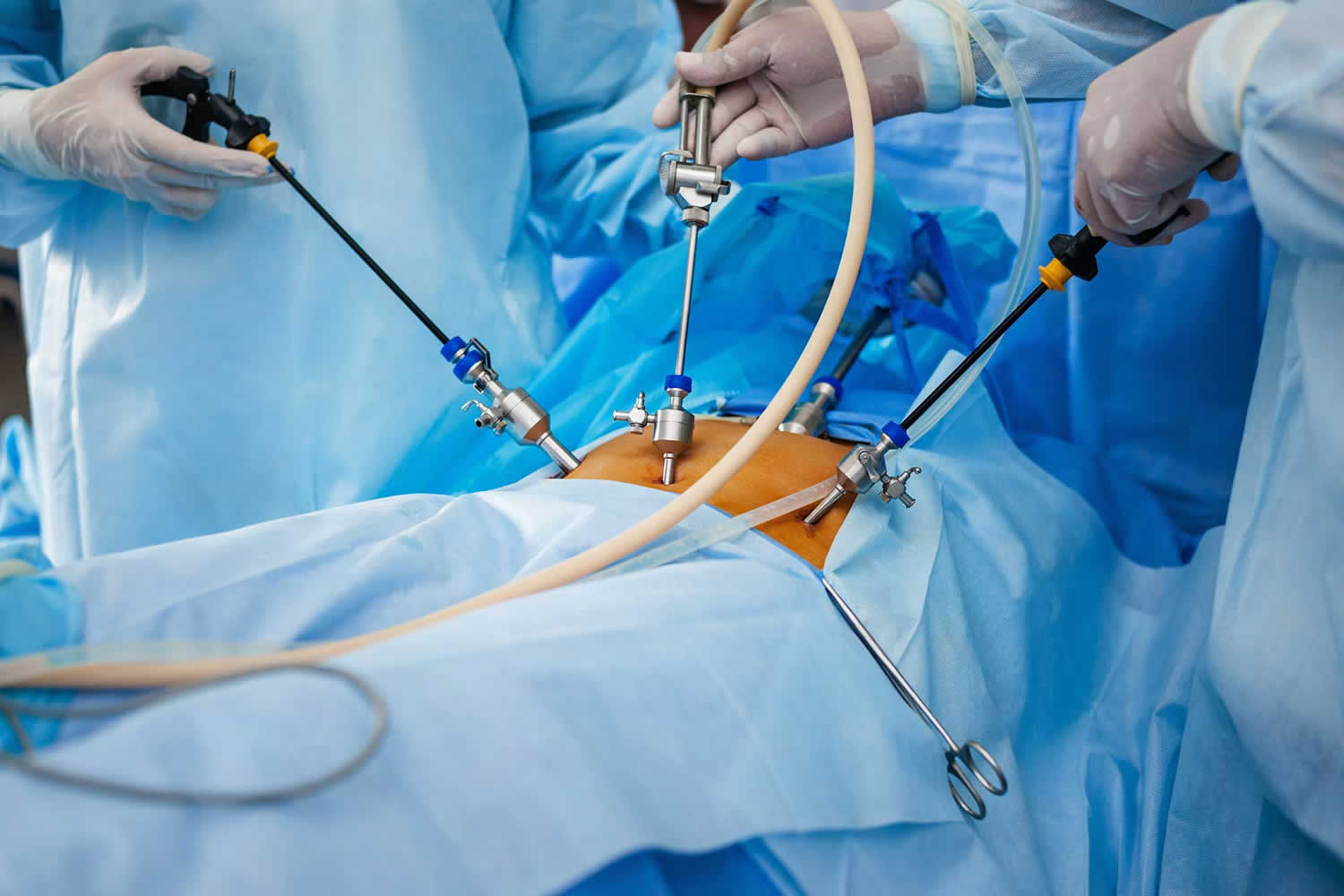
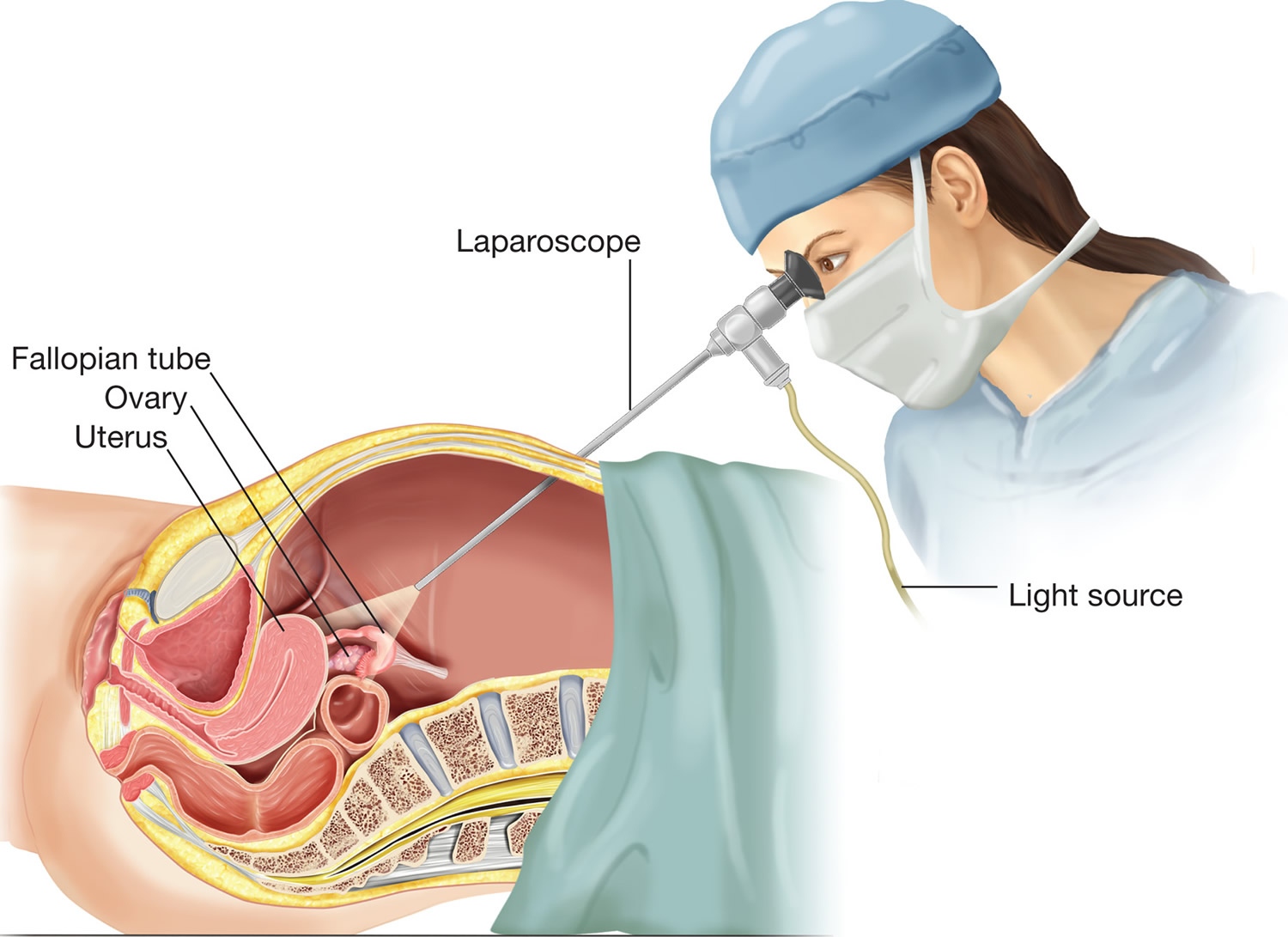
Laparoscopy is usually performed on an outpatient basis under general anesthesia. After the patient is under anesthesia, a telescope is placed through the navel. Carbon dioxide gas is used to fill the abdomen, which pushes the abdominal wall away from the internal organs and decreases the risk of injury to surrounding organs such as the bowel, bladder, and blood vessels. Occasionally, alternate sites may be used for the insertion of the laparoscope based upon physician experience or the patient’s prior surgical or medical history. These incisions are typically small (usually less than 1 inch in length). While looking through the laparoscope, the physician can see the reproductive organs including the uterus, fallopian tubes, and ovaries (Figure 3).
A small probe is usually inserted through another incision, in the lower abdomen, in order to move the pelvic organs into clear view (Figure 4). Additionally, a fluid is often injected through the cervix, uterus, and fallopian tubes to determine if the tubes are open. If no abnormalities are noted at this time, one or two stitches close the incisions. If abnormalities are discovered, diagnostic laparoscopy can become operative laparoscopy.
Figure 3. Exploratory laparoscopy
Figure 4. Laparoscopy procedure
Operative laparoscopy
During operative laparoscopy, many abdominal disorders can be treated safely through the laparoscope at the same time that the diagnosis is made. When performing operative laparoscopy, the physician inserts additional instruments such as probes, scissors, grasping instruments, biopsy forceps, electrosurgical or laser instruments, and suture materials through two or more additional incisions. Lasers, while a significant help in certain operations, are expensive and are not necessarily better or more effective than other surgical techniques or tools used during operative laparoscopy. The choice of technique and instruments depends on many factors, including the physician’s experience and preference and location of the problem. Some problems that can be attempted to be corrected with operative laparoscopy include treating adhesions (scar tissue) from around the fallopian tubes and ovaries, opening blocked tubes, removing ovarian cysts, and treating ectopic pregnancies. Endometriosis can also be removed or destroyed from the outside of the uterus, ovaries, or peritoneum. Under certain circumstances, fibroids on the uterus may also be removed. Operative laparoscopy can also be used to remove diseased ovaries and damaged fallopian tubes.
An increasing number of surgeons are performing hysterectomies with robotic assistance (robotic-assisted laparoscopy). However, robotic surgery is more expensive and generally more time-consuming than conventional surgery, and not all hospitals have this equipment available. It is also possible that evolving health-care changes will affect the availability of robotic and other “high-tech” procedures.
Figure 5. Operative laparoscopy
Treating endometriosis with laparoscopy
There are many options to manage and treat endometriosis including a healthy lifestyle, pain-relief medications, hormone therapy such as the oral contraceptive pill and progestins. Different types of surgery including laparoscopy, laparotomy and hysterectomy are available options.
If you suspect you have endometriosis, see your family doctor who can refer you to a specialist gynecologist. Many women with endometriosis are cared for by a team of health professionals including their doctor, a gynecologist who specializes in the area, a psychologist, medical sex therapist, pain specialist, colorectal surgeon and urologist.
The right treatment for you will depend on your symptoms, the severity of the condition and whether you are trying to become pregnant or maintain your ability to have children.
Laparoscopy surgery for endometriosis aims to remove as much visible endometriosis as possible and to repair any damage caused by the condition. Endometriosis is seen as implants (patches of endometriosis), cysts, nodules, endometriomas (chocolate cysts) and adhesions.
Laparoscopic surgery is an operation to reduce symptoms and improve fertility by removing endometriotic patches, implants, cysts, nodules and adhesions by cutting them out (excision) or burning them (diathermy). This is the usual method for excisional endometriosis surgery, to:
- remove large cysts and endometriomas
- remove an ovary/ovaries (fallopian) tubes
- surgically repair any damaged organs
Figure 6. Laparoscopy endometriosis
Laparoscopy and Hysteroscopy
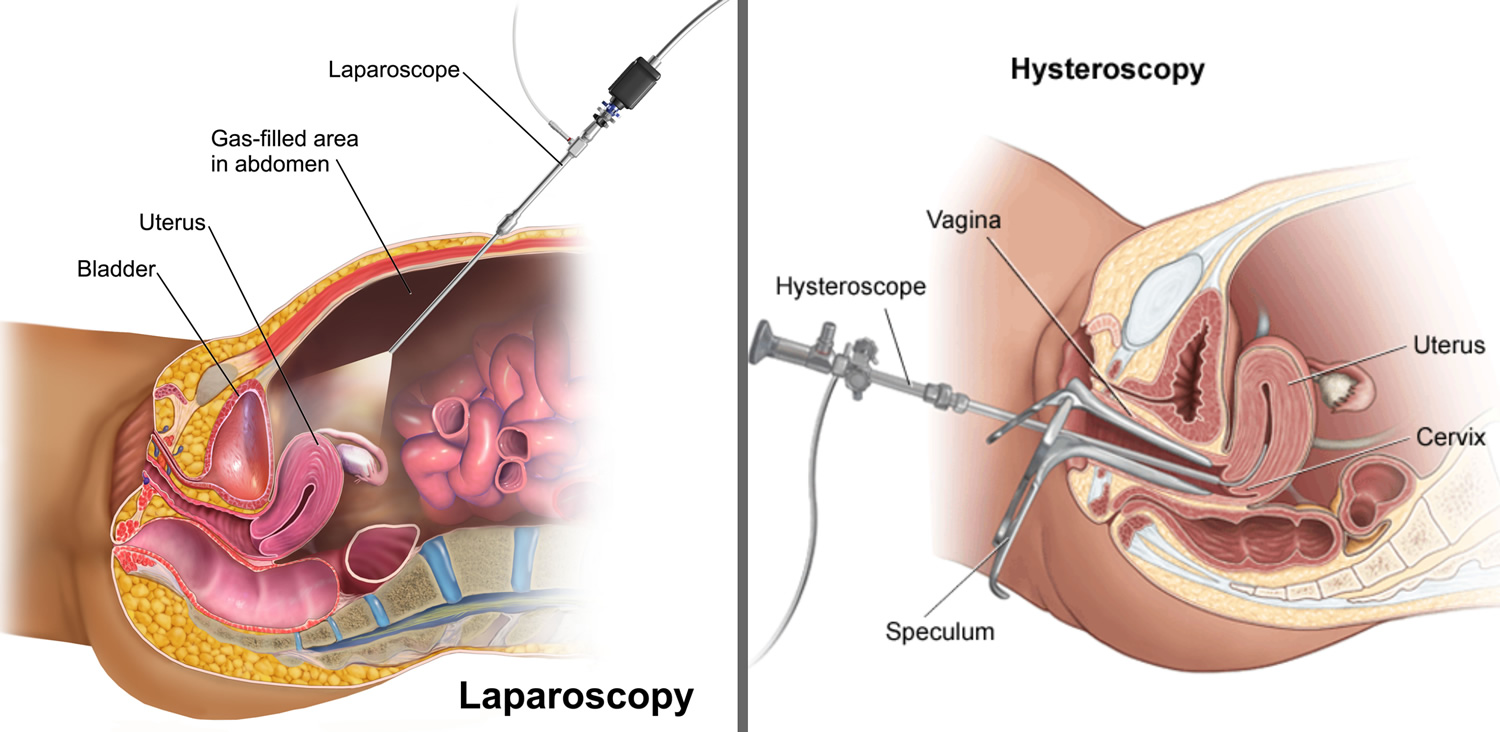
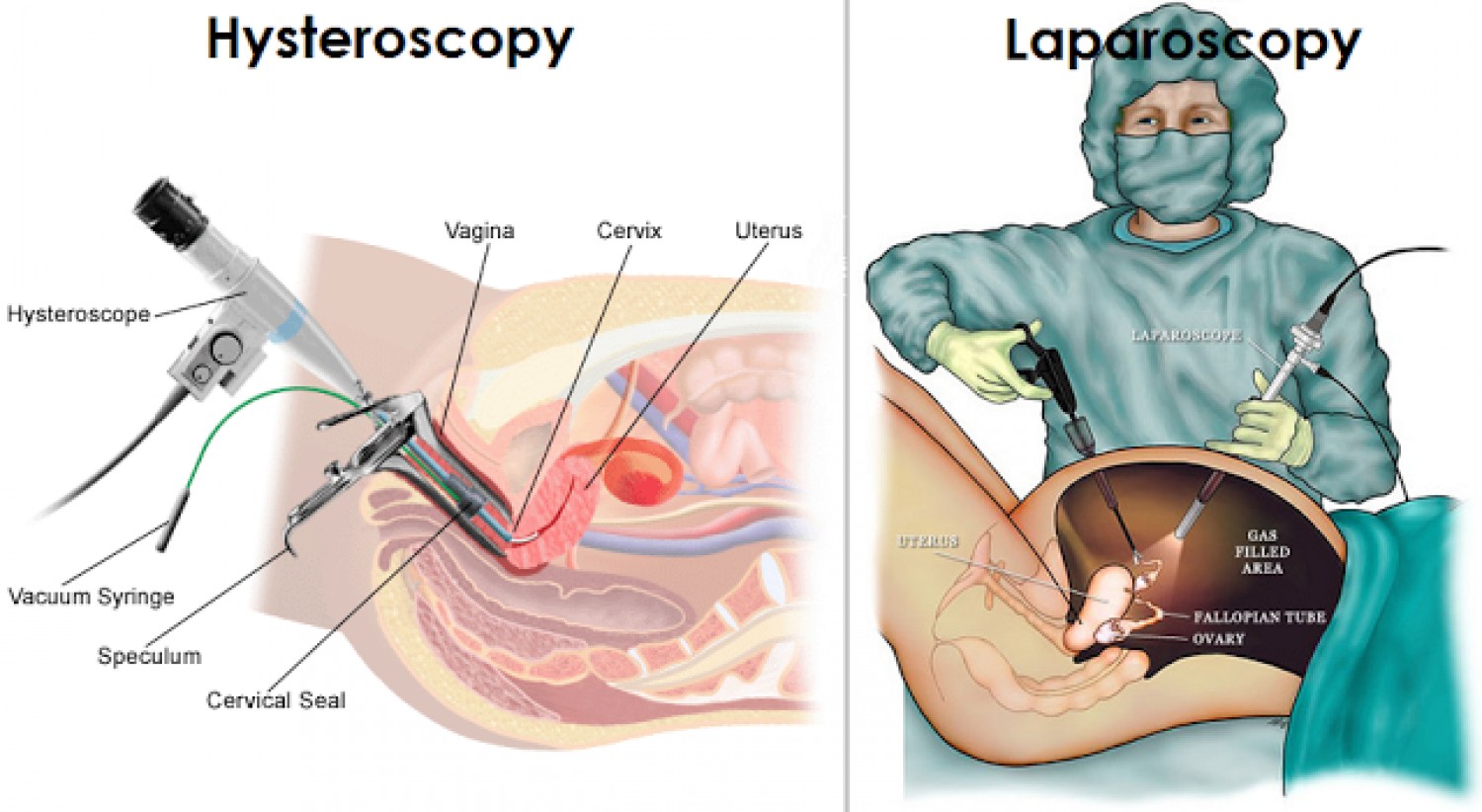
Laparoscopy and hysteroscopy can be used for both diagnostic (looking only) and operative (looking and treating) purposes (Figure 7).
Hysteroscopy is used to diagnose or treat problems of the uterus. A hysteroscope is a thin, lighted telescope-like device. It is inserted through your vagina into your uterus. The hysteroscope transmits the image of your uterus onto a screen. Other instruments are used along with the hysteroscope for treatment.
Why is hysteroscopy done?
One of the most common uses for hysteroscopy is to find the cause of abnormal uterine bleeding. Abnormal bleeding can mean that a woman’s menstrual periods are heavier or longer than usual or occur less often or more often than normal. Bleeding between menstrual periods also is abnormal.
Hysteroscopy also is used in the following situations:
- Remove adhesions that may occur because of infection or from past surgery
- Diagnose the cause of repeated miscarriage when a woman has more than two miscarriages in a row
- Locate an intrauterine device (IUD)
- Remove an intrauterine device (IUD)
- Perform sterilization, in which the hysteroscope is used to place small implants into a woman’s fallopian tubes as a permanent form of birth control
- Remove scar tissue from the womb
- Take a tissue sample (biopsy) from the cervix or womb
- Remove scar tissue from the womb
Hysteroscopy procedure may also have other uses not listed here.
Diagnostic laparoscopy may be recommended to look at the outside of the uterus, fallopian tubes, ovaries, and internal pelvic area. Diagnostic hysteroscopy is used to look inside the uterine cavity. If an abnormal condition is detected during the diagnostic procedure, operative laparoscopy or operative hysteroscopy can often be performed to correct it at the same time, avoiding the need for a second surgery. Both diagnostic and operative procedures should be performed by physicians with surgical expertise in these areas.
Hysteroscopy Risks
Hysteroscopy is a safe procedure. However, there is a small risk of problems. The uterus or cervix can be punctured by the hysteroscope, bleeding may occur, or excess fluid may build up in your system. In rare cases, hysteroscopy can cause life-threatening problems.
Risks of hysteroscopy may include:
- Hole (perforation) in the wall of the womb
- Scarring of the lining of the womb
- Damage to the cervix
- Need for surgery to repair damage
- Unusual fluid absorption during the procedure leading to low sodium levels
Risks of any pelvic surgery may include:
- Damage to nearby organs or tissues
- Blood clots, which could travel to the lungs and be deadly (rare)
Risks of anesthesia include:
- Nausea and vomiting
- Dizziness
- Headache
- Breathing problems
- Lung infection
Risks of any surgery include:
- Infection
- Bleeding
Biopsy results are usually available within 1 to 2 weeks.
Before the hysteroscopy procedure
Your provider may prescribe medicine to open your cervix. This makes it easier to insert the scope. You need to take this medicine about 8 to 12 hours before your procedure.
Before any surgery tell your provider:
- About all the medicines you take. This includes vitamins, herbs, and supplements.
- If you have diabetes, heart disease, kidney disease, or other health problems.
- If you are or could be pregnant.
- If you smoke, try to stop. Ask your provider for help. Smoking can slow wound healing.
In the 2 weeks before your procedure:
- You may need to stop taking drugs that make it hard for your blood to clot. These include aspirin, ibuprofen (Advil, Motrin), naproxen (Naprosyn, Aleve), clopidogrel (Plavix), and warfarin (Coumadin). Your provider will tell you what you should or should not take.
- Ask your provider which medicines you can take on the day of your procedure.
- Tell your provider if you have a cold, flu, fever, herpes outbreak, or other sickness.
- You will be told when to arrive at the hospital. Ask if you need to arrange for someone to drive you home.
On the day of the hysteroscopy procedure
- You may be asked not to drink or eat anything 6 to 12 hours before your procedure.
- Take any approved drugs with a small sip of water.
After the hysteroscopy procedure
You may go home the same day. Rarely, you may need to stay overnight. You may have:
- Menstrual-like cramps and light vaginal bleeding for 1 to 2 days. Ask if you can take over-the-counter pain medicine for the cramping.
- A watery discharge for up to several weeks.
You can return to normal daily activities within 1 to 2 days. DO NOT have sex until your provider says it is OK.
Diagnostic Hysteroscopy
Hysteroscopy is a useful procedure to evaluate women with infertility, recurrent miscarriage, or abnormal uterine bleeding. Diagnostic hysteroscopy is used to examine the uterine cavity (Figure 7), and is helpful in diagnosing abnormal uterine conditions such as fibroids protruding into the uterine cavity, scarring, polyps, and congenital malformations. A hysterosalpingogram (an x-ray using dye to outline the uterus and fallopian tubes), pelvic ultrasound or sonohysterogram (ultrasound with introduction of saline into the uterine cavity), or an endometrial biopsy may be performed to evaluate the uterus prior to hysteroscopy.
Diagnostic hysteroscopy is an outpatient procedure that is performed in a physician’s office or operating room. It is often performed soon after menstruation has ended because the uterine cavity is more easily evaluated. Hysteroscopy will be scheduled when you are not having your menstrual period.
Before the procedure, you may be given a medication to help you relax, or general anesthesia or local anesthesia may be used to block the pain. If you have general anesthesia, you will not be awake during the procedure.
The first step of diagnostic hysteroscopy often involves slightly stretching the canal of the cervix with a series of dilators to temporarily increase the size of the opening. You may be given medication that is inserted into the cervix, or special dilators may be used. A speculum is first inserted into the vagina. The hysteroscope (a long, thin, lighted, telescopelike instrument) is then inserted and gently moved through the cervix into your uterus. Skin incisions are not required for hysteroscopy. Carbon dioxide gas or a fluid, such as saline (salt water), will be put through the hysteroscope into your uterus to expand it. The gas or fluid helps your health care provider see the lining more clearly. The amount of fluid used is carefully checked throughout the procedure. Your health care provider can view the lining of your uterus and the openings of the fallopian tubes by looking through the hysteroscope. If a biopsy or other procedure is done, small instruments will be passed through the hysteroscope.
What should I expect during recovery?
You should be able to go home shortly after the procedure. If you had general anesthesia, you may need to wait until its effects have worn off.
It is normal to have some mild cramping or a little bloody discharge for a few days after the procedure. You may be given medication to help ease the pain. If you have a fever, chills, or heavy bleeding, call your health care provider right away.
Figure 7. Laparoscopy hysteroscopy
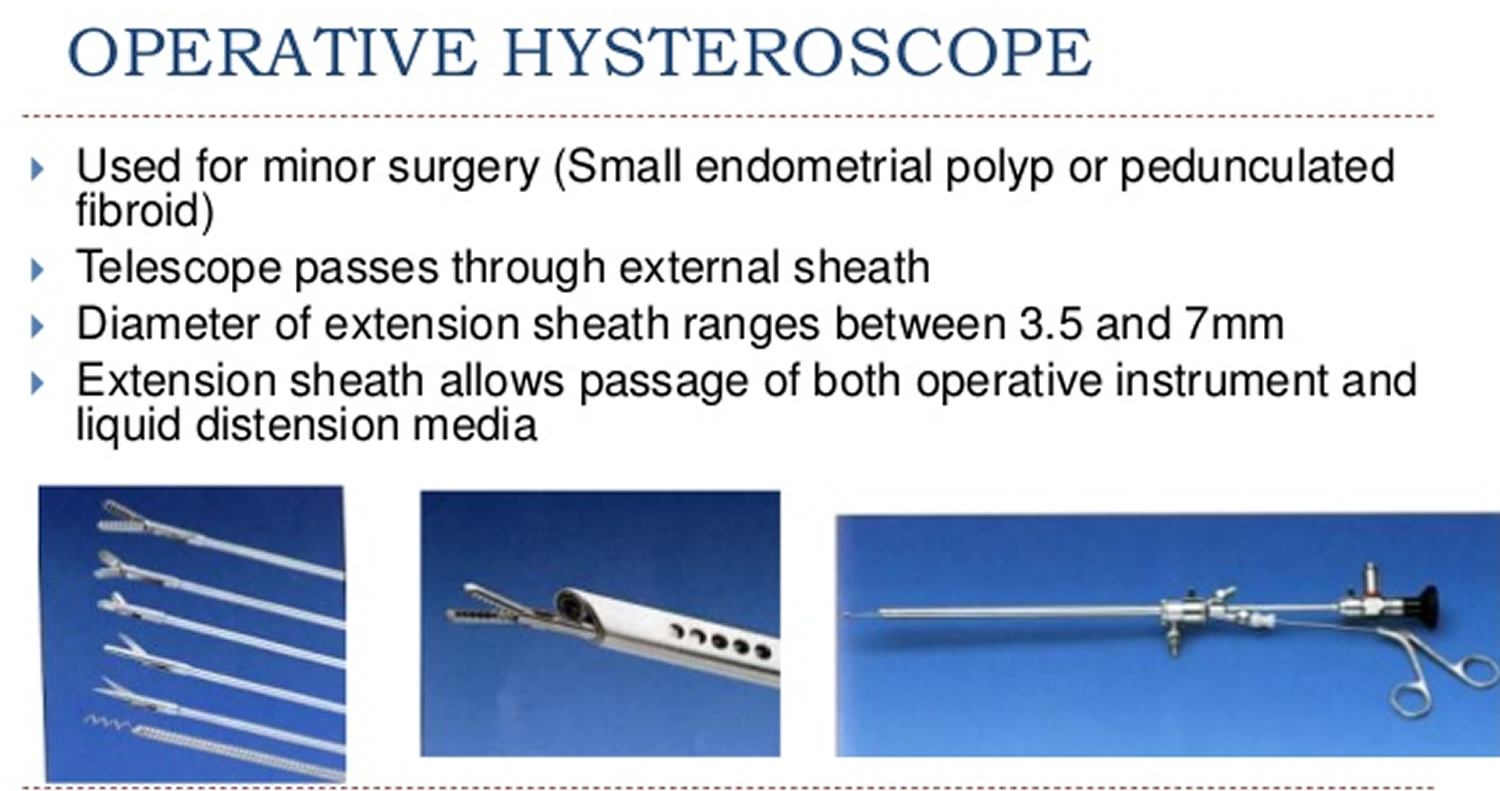
Operative Hysteroscopy
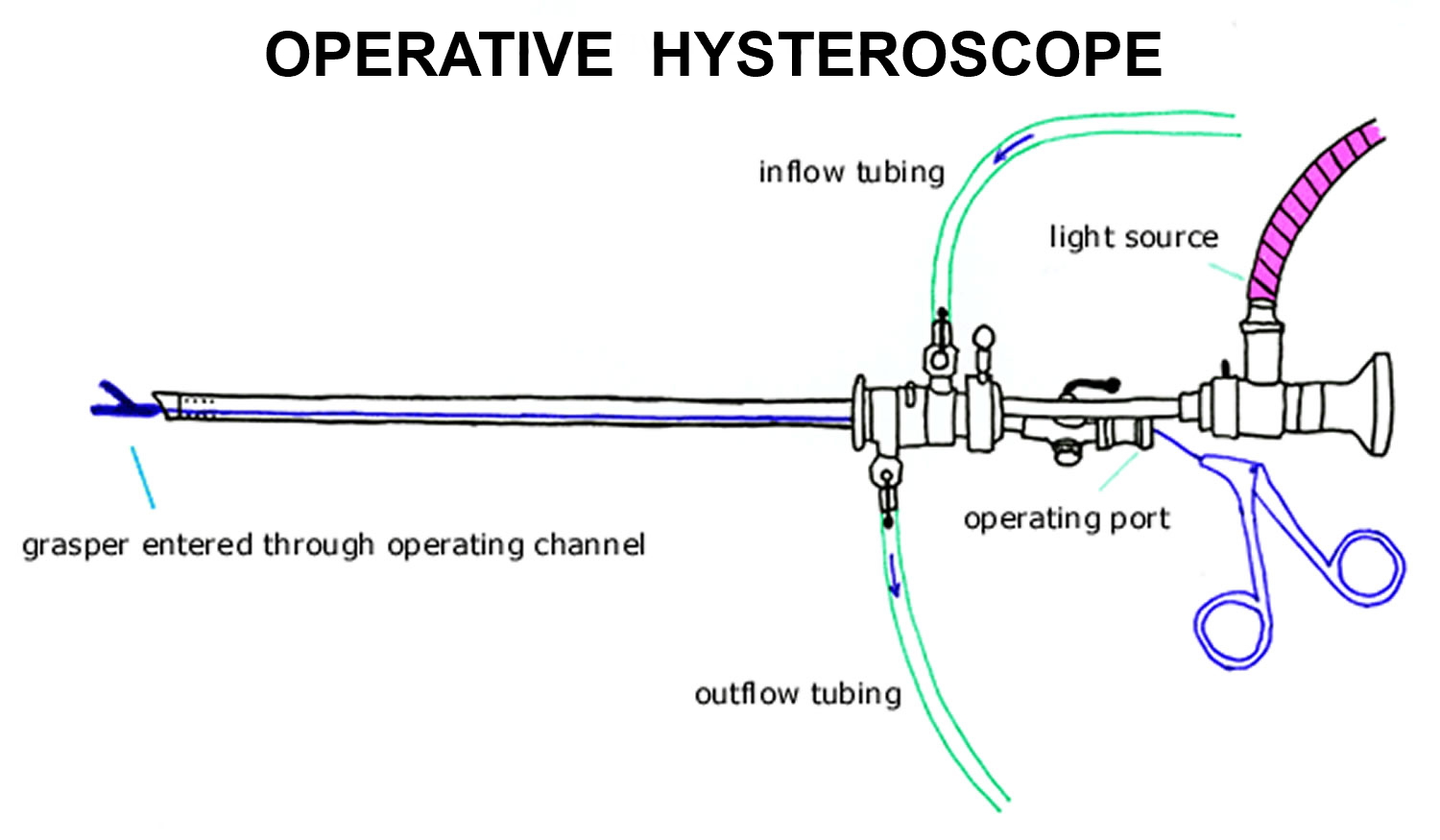
Operative hysteroscopy can treat many of the abnormalities found during diagnostic hysteroscopy or on other imaging studies. Operative hysteroscopy is similar to diagnostic hysteroscopy except that narrow instruments are placed into the uterine cavity through a channel in the operative hysteroscope (see Figures 9). Uterine fibroids, scar tissue, and polyps can be removed from inside the uterus. Some structural abnormalities, such as a uterine septum, may be corrected through the hysteroscope.
Your physician may want you to take medications to prepare the uterus for surgery. At the conclusion of surgery, your physician may insert a balloon catheter or other device inside the uterus. Antibiotics and/or estrogen may be prescribed after some types of uterine surgery to prevent infection and stimulate healing of the endometrium. Endometrial ablation, a procedure in which the lining of the uterus is destroyed, can be used to treat some cases of excessive uterine bleeding. Ablation of the uterine lining is not performed in women who wish to become pregnant.
Risks of Hysteroscopy
Complications of hysteroscopy occur in about 2 out of every 100 procedures. Although still uncommon, perforation of the uterus (a small hole in the uterus) is the most common complication. Although perforations usually close spontaneously, they may cause bleeding or rarely result in damage to nearby organs, which may require further surgery. Uterine cavity adhesions or infections may develop after hysteroscopy. Serious complications related to the fluids used to distend the uterus include fluid in the lungs, blood clotting, fluid overload, electrolyte imbalance, and severe allergic reactions. Severe or life-threatening complications, however, are very uncommon. Some of the complications above may prevent completion of the surgery.
Hysteroscopy postoperative care
Following hysteroscopy, some vaginal discharge or bleeding and cramping may be experienced for several days. Most physical activities can usually be resumed within 1 or 2 days. You should ask your physician when to resume sexual intercourse. If a balloon catheter is left in the cavity, it is usually removed after several days. As noted above, antibiotics and/or estrogen may be prescribed after surgery.
Figure 8. Operative Hysteroscopy
Figure 9. Operative Hysteroscope
Laparoscopy preparation
Your healthcare provider will explain the laparoscopy procedure to you. Ask him or her any questions you have.
You may be asked to sign a consent form that gives permission for the laparoscopy procedure. Read the form carefully and ask questions if anything is not clear.
Your healthcare provider will ask questions about your past health. He or she may also give you a physical exam. This is to make sure you are in good health before the laparoscopy procedure. You may also need blood tests and other diagnostic tests.
- You must not eat or drink for 8 hours before the laparoscopy procedure. This often means no food or drink after midnight.
- Tell your provider if you are sensitive to or allergic to any medicines, latex, tape, and anesthesia medicines (local and general).
- Tell your provider about all the medicines you take. This includes both over-the-counter and prescription medicines. It also includes vitamins, herbs, and other supplements.
- Tell your provider if you have a history of bleeding disorders. Let your provider know if you are taking any blood-thinning medicines, aspirin, ibuprofen, or other medicines that affect blood clotting. You may need to stop taking these medicines before the procedure.
- Tell your provider if you are pregnant or think you may be pregnant.
- You will need to remove any piercing jewelry near your naval (belly button).
Depending on the laparoscopy surgery, you may be asked to take an oral laxative to cleanse your bowel before the laparoscopy surgery or you may have a solution put into your rectum and lower intestine (a cleansing enema) a few hours before the procedure. You may also be given an antibiotic.
You may be given a medicine to relax you (a sedative) before the procedure. This depends on the type of laparoscopy being done. If this is an outpatient procedure, someone must drive you home.
Your healthcare provider may have other instructions for you based on your medical condition.
What happens during a laparoscopy procedure
A laparoscopy may be done on an outpatient basis or as part of your stay in a hospital. The way laparoscopy is done may vary. It will depend on your condition and your healthcare provider’s practices.
A laparoscopy is generally done while you are asleep under general anesthesia. Your provider will choose the type of anesthesia based on the procedure and your overall health.
Generally, a laparoscopy follows this process:
- You will be asked to take off any jewelry or other objects that may interfere with the procedure.
- You will be asked to remove clothing and be given a gown to wear.
- An IV (intravenous) line will be inserted in your arm or hand.
- A small tube (urinary catheter) may be placed in your bladder to collect urine.
- You will be placed on your back on the operating table.
- The anesthesiologist will check your heart rate, blood pressure, breathing, and blood oxygen level during the surgery.
- If there is too much hair at the surgical site, it may be clipped off.
- The skin over the surgical site will be cleaned with a sterile (antiseptic) solution.
- If general anesthesia is not used, a local anesthetic may be shot (injected) into the incision site. This will numb the area. You will feel a needle stick and a brief sting.
- A small cut or incision will be made in your belly just below the belly button.
- More small cuts may be made so that other surgical tools can be used during the procedure.
- Carbon dioxide gas will be put into your belly so that it swells up. This makes it easier to see organs and other structures.
- If general anesthesia is not used, you may feel some mild pain in your belly and the top of your shoulder. This may happen as the carbon dioxide is injected and surgical tools are moved around.
- The laparoscope will be put in and the procedure will take place.
- Once the laparoscopy and any other procedures are done, the laparoscope, and other surgical tools will be taken out.
- The cuts will be closed with stitches, tape, or surgical staples.
- A sterile bandage or dressing or adhesive strips will be applied.
Laparoscopy recovery
After your laparoscopy surgery, you will be taken to the recovery room. Your recovery process will vary depending on the type of anesthesia you had. You will be watched closely. Once your blood pressure, pulse, and breathing are stable and you are alert, you will be taken to your hospital room. Or you may be sent home if this was an outpatient procedure.
When you are home, you must keep the cut clean and dry. Your doctor will give you instructions on how to bathe. Any stitches or surgical staples will be taken out at a follow-up office visit. If adhesive strips were used, they should be kept dry. They will often fall off in a few days.
The navel area (belly button) is usually tender and the abdomen may be bruised and tender.
You may feel pain from the carbon dioxide gas still in your belly. Gas used to distend the abdomen may cause discomfort in the shoulders, chest, and abdomen. It should feel a bit better each day. Don’t have any carbonated drinks for 1 or 2 days after the laparoscopy procedure. This will help reduce the mild pain from the carbon dioxide gas. Also, carbonated drinks may upset your stomach. Anesthesia can cause nausea and dizziness. The amount of discomfort depends on the type and extent of procedures performed. You may take a pain medicine as directed by your provider. Aspirin or other pain medicines may raise your risk of bleeding. Only take medicines that your provider has approved.
You may be allowed to drink clear fluids a few hours after the laparoscopy procedure. You may slowly move on to more solid foods as directed. Tell your healthcare provider if you have nausea or vomit.
You may be told to limit your physical activity for a few days.
Normal activities can usually be resumed within a few days. Significant abdominal pain, worsening nausea and vomiting, a temperature of 101 °F (38 °C) or higher, drainage of pus from an incision, or significant bleeding from an incision are potential serious complications requiring immediate medical attention.
Call your healthcare provider if you have any of the following:
- Fever or chills
- Redness, swelling, or bleeding or other drainage from the incision site
- More pain around the incision site
- Vomiting
- Trouble urinating
Your healthcare provider may give you other instructions, depending on your situation.
Laparoscopy risks
Postoperative bladder infection and skin irritation are most common. Similar to all surgeries, there are risks associated with laparoscopy. Serious complications of diagnostic and operative laparoscopy are rare. Possible complications of laparoscopy may include bleeding from the incision, injury to the organs in the abdomen, or the carbon dioxide gas entering places other than the abdomen. As with any operation, there is also a small risk of complications associated with general anesthesia.
Laparoscopy can have complications such as:
- Bleeding from the incisions
- Infection – pelvic or abdominal infections may occur
- The major risk is damage to the bowel, bladder, ureters, uterus, major blood vessels, or other organs, which may require additional surgery. Injuries can occur during the insertion of various instruments through the abdominal wall or during the operative treatment.
- Adhesions (scar tissue within the abdomen) may develop, although this is less likely than after an open procedure (laparotomy).
- Hematomas (bloodfilled bruising) of the abdominal wall can occur near the incisions.
Certain conditions may increase the risk of serious complications. These include previous abdominal surgery, especially bowel surgery, and a history or presence of bowel/pelvic adhesions, severe endometriosis, pelvic infections, obesity, or excessive thinness. Allergic reactions, nerve damage, and anesthesia complications rarely occur. Postoperative urinary retention is uncommon and venous thrombosis (blood clot) is rare. The risk of death as a result of laparoscopy is very small (around 3 in 100,000). When all possible complications are considered, 1 or 2 women out of every 100 may develop a complication, usually of minor consequence.
Sometimes a laparoscopy is not advised. This may be the case if you:
- Have advanced cancerous growths on your abdominal wall
- Have long-term (chronic) tuberculosis
- Have a bleeding problem such as low blood platelet count (thrombocytopenia)
- Have a lot of scar tissue (adhesions) from other surgeries
- Are taking blood-thinning medicine
There may be other risks depending on your medical condition. Be sure to talk about any concerns with your healthcare provider before the procedure.
Certain conditions may stop a laparoscopy from working well. These include being obese or having bleeding inside your abdomen.
Notify the hospital or your doctor immediately if you have:
- pain that is worsening or not improving
- increasing pain in your shoulders
- pain or other problems when urinating
- bleeding that is increasing or not settling
- a fever or temperature
- you feel that you are not recovering relatively quickly
- any other symptoms that you are concerned about.