Contents
What is meningococcemia
Meningococcemia also known as meningococcal septicemia or meningococcal bacteremia, is an acute (sudden onset) infection of the bloodstream and subsequent vasculitis (inflammation of the blood vessels) with the Neisseria meningitidis bacteria. Meningococcemia is a medical emergency. When someone has meningococcal septicemia, the Neisseria meningitidis bacteria enter the bloodstream and multiply, damaging the walls of the blood vessels. This causes bleeding into the skin and organs.
Neisseria meningitidis frequently lives in the upper respiratory tract with no evidence of illness. Some event is thought to trigger the onset of aggressive behavior of the organism and sporadic cases of meningococcemia and meningococcal meningitis appear.
Neisseria meningitidis is carried asmptomatically in 5-20% of the population. Neisseria meningitidis is found worldwide in 5 major serogroups. The most common disease causing groups are meningococcal A, B, C, W and Y. These are commonly referred to as MenA, MenB, MenC, MenW and MenY. Group A meningococcus causes epidemic disease in sub-Saharan Africa and parts of Asia. Groups Y and W also cause epidemic infection. Groups B and C tend to cause sporadic infection in Europe and North America.
The Neisseria meningitidis bacteria are spread through close contact with an infected person. Droplets in the air from a sneeze or close conversation can be inhaled and may cause infection. Many people who acquire and carry the bacteria in their nose and throat never develop symptoms. In rare cases, the bacteria multiply rapidly, causing serious illness in both children and adults.
Meningococcemia only occurs in a small percentage of those colonized. Meningococcemia depends on both host and bacterial factors and is more likely following viral upper respiratory infections.
Man is the only known reservoir of Neisseria meningitidis. Meningococcal infections are uncommon, but can be fatal. The meningococcal infection occurs when bacteria invade the nasal mucosa and enter the bloodstream. Meningococcal infections occur most often during the late winter and early spring months. Babies and children under the age of 5 are more commonly affected, but the infection also occurs in adolescents and adults. There is a secondary peak of disease amongst teenagers, with college freshman living in dorms are also at risk.
There may be few symptoms at first. Some may include:
- Fever
- Headache
- Irritability
- Fatigue
- Muscle pain
- Nausea and vomiting
- Cold hands and feet
- Cold chills
- Severe aches or pain in the muscles, joints, chest or abdomen (belly)
- Rapid breathing
- Diarrhea
- In the later stages, a dark purple rash with very small red or purple spots on the feet or legs
Later symptoms may include:
- A decline in your level of consciousness
- Large areas of bleeding under the skin
- Shock
People with meningococcemia are often admitted to the intensive care unit (ICU) of the hospital, where they are closely monitored. They may be placed in respiratory isolation for the first 24 hours to help prevent the spread of the infection to others.
Meningococcemia treatments may include:
- Antibiotics given through a vein immediately
- Breathing support
- Clotting factors or platelet replacement, if bleeding disorders develop
- Fluids through a vein
- Medicines to treat low blood pressure
- Wound care for areas of skin with blood clots
In developed countries there is a mortality rate of 10% from meningococcemia and 5% for meningococcal meningitis. Mild neurological complications such as vestibular nerve damage are common but serious brain damage is uncommon.
Figure 1. Meningococcemia rash
Meningococcemia causes
Meningococcemia is caused by bacteria called Neisseria meningitidis. The bacteria often live in a person’s upper respiratory tract without causing signs of illness. They can be spread from person to person through respiratory droplets. For example, you may become infected if you are around someone with the condition and they sneeze or cough.
Family members and those closely exposed to someone with the condition are at increased risk. The infection occurs more often in winter and early spring.
Risk groups for meningococcemia
Household or close contacts of case patients are at the highest risk for developing meningococcal disease. Infants less than one year old and adolescents 16 through 23 years old have higher rates of disease than other age groups. However, cases occur in all age groups including the elderly.
In addition, people with certain medical conditions are at increased risk for meningococcal disease. These medical conditions include
- Functional or anatomic asplenia
- Persistent complement component deficiencies (e.g., C3, C5-9, properdin, factor H, factor D)
- HIV infection
People who take eculizumab (Soliris®), typically for treatment of atypical hemolytic uremic syndrome (aHUS) or paroxysmal nocturnal hemoglobinuria (PNH), are also at increased risk for meningococcal disease. Recent data suggest that meningococcal vaccines likely provide incomplete protection against invasive meningococcal disease in eculizumab patients.
The following groups of people also have an increased risk for meningococcal disease:
- Microbiologists who are routinely exposed to isolates of Neisseria meningitidis
- People identified as being at increased risk because of an outbreak of meningococcal disease
- People traveling to a country where meningococcal disease is epidemic or highly endemic
- First-year college students who live in residence halls
- Military recruits
Meningococcal transmission
People spread meningococcal bacteria to others by exchanging respiratory and throat secretions during close or lengthy contact, especially if living in the same household. Humans are the only host. Asymptomatic nasopharyngeal carriers who are not a close contact of a patient with meningococcal disease do not require prophylaxis.
Meningococcemia prevention
Keeping up to date with recommended immunizations is the best defense against meningococcal disease. Maintaining healthy habits, like getting plenty of rest and not having close contact with people who are sick, also helps.
Cases of meningococcal disease should be reported to your local public health department. Staff will provide education to you and your family, as well as to the public.
Vaccination
Vaccines help protect against all three serogroups (B, C, and Y) of Neisseria meningitidis bacteria commonly seen in the United States. Like with any vaccine, meningococcal vaccines are not 100% effective. This means there is still a chance you can develop meningococcal disease after vaccination. People should know the symptoms of meningococcal disease since early recognition and quick medical attention are extremely important.
All 11 to 12 year olds should be vaccinated with a meningococcal conjugate vaccine. A booster dose is recommended at age 16 years. Teens and young adults (16 through 23 year olds) also may be vaccinated with a serogroup B meningococcal vaccine. In certain situations, other children and adults could be recommended to get meningococcal vaccines.
Talk with your or your child’s healthcare professional if you have questions about meningococcal vaccines.
There are two types of meningococcal vaccines available in the United States:
- Meningococcal conjugate vaccines (Menactra® and Menveo®)
- Serogroup B meningococcal vaccines (Bexsero® and Trumenba®)
In studies demonstrating the efficacy 1:
Menactra®
- Between 82% and 97% of adolescents vaccinated demonstrated a protective immune response one month after completing the series
- Between 74% and 89% of adults vaccinated demonstrated a protective immune response one month after completing the series
Menveo®
- Between 75% and 96% of adolescents vaccinated demonstrated a protective immune response one month after completing the series
- Between 69% and 94% of adults vaccinated demonstrated a protective immune response one month after completing the series
Bexsero®
- Between 63% and 94% of adolescents and young adults vaccinated demonstrated a protective immune response one month after completing the series
Trumenba®
- Between 81% and 84% of adolescents and young adults vaccinated had a protective immune response one month after completing the series
Available data suggest that protection from meningococcal conjugate vaccines decreases in many adolescents within 5 years, which emphasizes the importance of the 16-year-old booster dose so that adolescents maintain protection during the ages when they are most at risk for meningococcal disease. Early data on serogroup B meningococcal vaccines suggest that protective antibodies also decrease fairly quickly after vaccination.
The meningococcal vaccine, meningococcal conjugate vaccine (MCV4), is recommended by the Centers for Disease Control and Prevention (CDC) for all children 11 to 18 years old. Dosages of MCV4 are recommended for children between 11 and 12 years of age and again at 16 to18 years of age. If the vaccine was not given at age 11 to 12, it should be given when beginning high school, with a booster dose a few years later. High-risk infants and young children can receive meningococcal vaccines beginning at age 2 months. Other high-risk children and adolescents who require immunization with MCV4 include the following:
- People who have damaged spleens or who do not have spleens
- College students not already immunized in high school (immunization of college students is recommended by the American College Health Association)
- Military recruits
- People who are traveling to countries where the meningococcal infections are common
- Family members or those in close contact with people with meningitis
- People with a weak immune system
Antibiotics
Close contacts of a person with meningococcal disease should receive antibiotics to prevent them from getting sick. This is known as prophylaxis.
The CDC recommends the following contacts be treated if exposed to the bacteria:
- Household contacts or roommates, especially young children
- Child care or nursery school contacts, during previous seven days
- Direct exposure to the infected child’s body fluids through kissing or sharing toothbrushes or eating utensils
- People who frequently sleep in the same area as the infected child
- Anyone with direct contact with a patient’s oral secretions (saliva or spit), such as a boyfriend or girlfriend
Doctors or local health departments recommend who should get prophylaxis.
A hospitalized child will require isolation for 24 hours after antibiotics have been started. Family members or people who have been in close contact with a child with meningococcal disease may require antibiotics. If you have questions about exposure, please consult your child’s doctor.
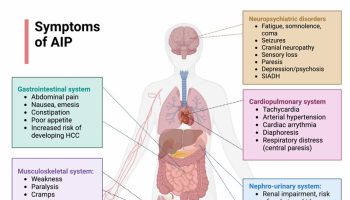
Meningococcemia symptoms
Meningococcemia symptoms may occur suddenly and get worse quickly. Immediate treatment is necessary.
While each person may experience symptoms differently, the following are the most common meningococcemia symptoms:
- Fever
- Chills
- Sore throat
- Headache, especially when flexing the neck by moving the chin toward the chest
- Sensitivity to light
- Aching muscles and joints
- Malaise (not feeling well)
- Exhaustion and weariness
Meningococcemia rash, which may appear as follows:
- Small, red, flat or raised spots
- Progression of rash to larger red patches or purple lesions (similar in appearance to large bruises)
As the meningococcemia illness worsens quickly, symptoms may include:
- Low blood pressure
- Very low urine output
- Bleeding
- Shock, a serious state marked by decreased blood pressure and decreased blood flow to important organs such as the kidneys, liver, and brain
Meningococcal meningitis
In children older than 1 year, meningococcal meningitis symptoms may include:
- Fever
- Neck and/or back pain
- Headache
- Nausea and vomiting
- Neck stiffness
- A purple-red, splotchy rash or skin discoloration may appear as the disease progresses
In infants, meningococcal meningitis symptoms are difficult to pinpoint and may include:
- Irritability
- Listlessness and sleeping all the time
- Refusing a bottle
- Crying when picked up or being held
- Can’t be comforted while crying
- Bulging fontanel (soft spot on an infant’s head)
- Behavior changes
The symptoms of meningococcal meningitis and meningococcemia may look like other conditions or medical problems. Always consult your child’s doctor for a diagnosis.
Meningococcemia possible complications
Possible complications of this infection are:
- Arthritis
- Bleeding disorder (DIC or disseminated intravascular coagulation)
- Gangrene due to lack of blood supply
- Inflammation of blood vessels in the skin
- Inflammation of the heart muscle
- Inflammation of the heart lining
- Shock
- Severe damage to adrenal glands that can lead to low blood pressure (Waterhouse-Friderichsen syndrome)
Meningococcemia diagnosis
Meningococcal disease can be difficult to diagnose because the signs and symptoms are often similar to those of other illnesses.
In addition to a complete medical history and physical exam, other tests may include:
If a doctor suspects meningococcal disease, they will collect samples of blood or cerebrospinal fluid (CSF) (fluid near the spinal cord).
Lumbar puncture (spinal tap). A special needle is placed into the lower back, into the spinal canal. This is the area around the spinal cord. A small amount of cerebral spinal fluid (CSF) can be removed and sent for testing to determine if there is an infection. Cerebrospinal fluid (CSF) is the fluid that bathes your brain and spinal cord. Doctors then test the samples to see if there is an infection and, if so, what germ is causing it. A Gram stain of cerebrospinal fluid (CSF) may show Gram-negative diplococci. If Neisseria meningitidis bacteria are in the samples, laboratorians can grow (culture) the bacteria. Growing the bacteria in the laboratory allows doctors to know the specific type of bacteria that is causing the infection.
An aspirate (material drawn in negative pressure from a syringe) from petechiae and meningococci can also be cultured from CSF or blood and detected by PCR (polymerase chain reaction). Knowing this helps doctors decide which antibiotic will work best. Other tests can sometimes detect and identify the bacteria if the cultures do not.
- Blood culture
- Culture of skin lesions or rash (not common)
- Other blood tests
Meningococcemia treatment
Prompt treatment is needed for meningococcal infections. Antibiotics (for example, penicillin) are most commonly used. If a patient has severe allergies to penicillin, other antibiotics may be used to treat the infection. Five to seven days of antibiotic therapy is usually effective. A child with meningococcal meningitis or meningococcemia will usually require IV (intravenous) antibiotics and close observation in a hospital or intensive care unit (ICU).
Other treatment for meningococcal infections is supportive (aimed at treating the symptoms present). A child with severe infection may require supplemental oxygen or be put on a ventilator to assist with breathing.
Meningococcemia treatment
- Benzyl penicillin 2.4 g IV (intravenous) slowly should be given immediately for 7 days.
- Meningococcal vaccine against serogroup C is available. Meningococcal vaccine that covers some, but not all, strains of meningococcus is recommended for children age 11 or 12. A booster is given at age 16. Unvaccinated college students who live in dormitories should also consider receiving this vaccine. It should be given a few weeks before they first move into the dorm. Talk to your provider about this vaccine.
- Household, kissing or other close contacts of a case of meningococcal disease should be given oral rifampicin or ciproflaxin, (ciproflaxin should not be given to children), as prophylaxis.
- Immunization can be offered for a group C disease.
Re-Infection
Although rare, people can get meningococcal disease more than once. A previous infection will not offer lifelong protection from future infections. Therefore, CDC recommends meningococcal vaccines for all preteens and teens. In certain situations, children and adults should also get meningococcal vaccines.
Meningococcemia prognosis
Early treatment results in a good outcome. When shock develops, the outcome is less certain. Even with antibiotic treatment, 10 to 15 in 100 people infected with meningococcal disease will die 2. About 11 to 19 in 100 survivors will have long-term disabilities, such as loss of limb(s), deafness, nervous system problems, or brain damage 2.
The condition is most life threatening in those who have:
- A severe bleeding disorder called disseminated intravascular coagulopathy (DIC)
- Kidney failure
- Shock