Contents
What is norovirus
Norovirus (previously called Norwalk or Norwalk-like viruses) is a very contagious virus that causes sudden vomiting and diarrhea (acute gastroenteritis), but usually resolves itself within 1 to 3 days without treatment. Norovirus can be more serious for young children, the elderly, and people with other health conditions. Norovirus can lead to severe dehydration, hospitalization and even death.
Norovirus is highly contagious and norovirus is easily spread from person to person, so good hygiene practices are important to prevent others from becoming infected.
Anyone can get infected and sick with norovirus. You can get norovirus from:
- Having direct contact with an infected person
- Consuming contaminated food or water
- Touching contaminated surfaces then putting your unwashed hands in your mouth
Norovirus spreads from an infected person to others who have contact with:
- the infected person’s vomit or feces (poop)
- their unwashed hands
- surfaces or objects they have touched
- food or water they have contaminated.
If you are sick with norovirus, you can spread it to other people by having close contact, such as by caring for, preparing food, or sharing food or eating utensils, with them. You can also spread norovirus by contaminating surfaces. This can happen if you touch surfaces with your unwashed hands, then other people touch these surfaces and put their fingers in their mouths.
Norovirus is particularly likely to cause illness in places such as healthcare and aged care facilities, restaurants, schools and cruise ships. These are closed environments where lots of people eat food prepared by others. One infected person can easily pass the infection to other people.
About 20 million people get sick with norovirus each year in the United States 1. On average, a person will get norovirus about 5 times during their lifetime. People of all ages can get norovirus.
You can get norovirus any time of the year, but you are more likely to get it from November to April. Norovirus is also known as ‘winter vomiting’ because it tends to peak in winter when people stay together indoors. Some other common names for norovirus infection are gastric flu, stomach flu and viral gastro.
Norovirus infection is usually diagnosed based on the symptoms. A formal diagnosis will require laboratory testing of a stool (poop) sample. Public health authorities sometimes request this to help control norovirus outbreak.
Norovirus is highly contagious, so good hygiene is very important. There is no vaccine to prevent norovirus infection.
To help prevent norovirus infection:
- wash hands with soap and running water after using the toilet or changing nappies
- wash hands with soap and water before eating or handling food
- wash food before eating, especially oysters and shellfish, and fruits and vegetables
- wash bedding and clothing if they are stained by diarrhea or vomit
- clean contaminated household surfaces and disinfect with a diluted bleach-based cleaner
- clean contaminated soft furnishings or carpet with hot water and detergent followed by a steam clean.
If you have been infected, you will still be contagious for a couple of days after the diarrhea or vomiting has stopped. You should stay away from work, or keep an infected child home from childcare or school, until 48 hours after such symptoms have disappeared.
Norovirus infection should only last for a few days. Norovirus infection doesn’t usually require medication.
The most common problem with norovirus infection is dehydration. This happens if you do not drink enough fluids to replace what you lose through vomiting and diarrhea. Dehydration is most common in babies, young children, the elderly and people with weak immune systems. Older people, young children and those with a weakened immune system are at risk of developing more serious illnesses.
It is very important to drink plenty of fluids. See a doctor immediately if your child cannot keep down a sip of liquid or has dehydration (dry mouth, no urine for 6 hours or more, or lethargy). If you are unwell with diarrhea or vomiting, you could have norovirus gastroenteritis. A doctor can diagnose norovirus gastroenteritis after talking to and examining you. If you’re not getting better, the doctor may want to do stool (poop) tests to find out what’s making you ill.
You can get norovirus illness many times in your life because there are many different types of noroviruses. Infection with one type of norovirus may not protect you against other types. It is possible to develop immunity to (protection against) specific types. But, it is not known exactly how long immunity lasts. This may explain why so many people of all ages get infected during norovirus outbreaks. Also, whether you are susceptible to norovirus infection is also determined in part by your genes.
See your doctor if:
- the diarrhea lasts for more than 2 days in an adult, or for more than 24 hours in a baby
- you get dehydrated
- you also have a fever
- you have severe pain in your abdomen or rectum
- the diarrhea is bloody or black
- your child is very young or small (aged below 6 months or weighs less than 8 kg)
- your child is born preterm, or has other chronic conditions
- your child is passing less than 4 wet nappies/day
- you or your child is passing any blood in the stool
- you or your child is having dark green (bile) vomits
- you or your child vomits blood
- you or your child is having severe abdominal pain
- you or your child less than 3 years old and has a fever more than 101.3 °F (38.5° C)
- you or your child is showing signs of dehydration (very thirsty, cold hands and feet, dry lips and tongue, sunken eyes, sunken fontanelle, sleepy or drowsy)
- you or your child is unable to tolerate any oral intake because of severe vomiting
- you or your child becomes unusually drowsy
- vomiting persists more than two days
- diarrhea persists more than several days
- diarrhea turns bloody
- lightheadedness or fainting occurs with standing
- confusion develops
- worrisome abdominal pain develops
Norovirus Infection
Norovirus is the leading cause of vomiting and diarrhea from acute gastroenteritis (inflammation of the stomach and intestines) among people of all ages in the United States. Each year, on average in the United States, norovirus:
- causes 19 to 21 million cases of acute gastroenteritis
- leads to 1.7 to 1.9 million outpatient visits and 400,000 emergency department visits, primarily in young children
- contributes to about 56,000 to 71,000 hospitalizations and 570 to 800 deaths, mostly among young children and the elderly.
Norovirus is the leading cause of acute gastroenteritis among U.S. children less than 5 years of age who seek medical care. Norovirus is responsible for nearly 1 million pediatric medical care visits annually.
By 5 years of age:
- an estimated 1 in 278 children will be hospitalized,
- 1 in 14 will visit an emergency room, and
- 1 in 6 will receive outpatient care for norovirus illnesses.
- Norovirus is the leading cause of foodborne illness in the United States. It causes 58% of foodborne illnesses acquired in the United States. Each year, norovirus illness costs about $2 billion, mainly due to lost productivity and healthcare expenses in the United States.
You can get norovirus illness at any time during the year. Most norovirus outbreaks in the United States happen from November to April. Also, there can be 50% more norovirus illness in years when there is a new strain of the virus.
What is Norovirus incubation period?
There is no incubation period with norovirus. Just a very small amount – as few as 18 viral particles – of norovirus on your food or your hands can make you sick 2. In fact, the amount of virus particles that fit on the head of a pin would be enough to infect more than 1,000 people!
How long does norovirus last?
A person usually develops symptoms 12 to 48 hours after being exposed to norovirus. Most people with norovirus illness get better within 1 to 3 days.
How contagious is norovirus?
Norovirus is very contagious. When you are sick with norovirus, you can shed billions of virus particles in your vomit and poop. It only takes a few of these particles to make someone sick.
- Just a very small amount – as few as 18 viral particles – of norovirus on your food or your hands can make you sick 2.
- In fact, the amount of virus particles that fit on the head of a pin would be enough to infect more than 1,000 people!
You are most contagious:
- when you have symptoms of norovirus illness, especially vomiting
- during the first few days after you recover from norovirus illness
However, you may still be able to spread norovirus for two weeks or more after you feel better.
Take steps to keep norovirus from spreading:
- Wash your hands: Wash your hands thoroughly with soap and water, especially after using the toilet or changing diapers, and always before eating or preparing food.
- Handle and prepare food safely: Carefully wash fruits and vegetables, and cook oysters and other shellfish thoroughly before eating. If you are sick with norovirus, do not prepare food for others while you have symptoms and for at least 2 days after symptoms go away.
- Clean and disinfect surfaces: After you vomit or have diarrhea, always thoroughly clean and disinfect the entire area immediately. Put on rubber or disposable gloves, and wipe the entire area with paper towels, then disinfect the area using a bleach-based household cleaner as directed on the product label. Leave the bleach disinfectant on the affected area for at least five minutes then clean the entire area again with soap and hot water. Finish by cleaning soiled laundry, taking out the trash, and washing your hands.
- Wash laundry thoroughly: Immediately remove and wash clothing or linens that may have vomit or poop on it. Handle items carefully—try not to agitate them. If available, wear disposable gloves to handle soiled clothing or linens, and wash your hands after. Wash soiled items with detergent and hot water at the maximum available cycle length then machine dry them at the highest heat setting.
How long is norovirus contagious?
If you get norovirus illness, you can shed billions of norovirus particles that you can’t see without a microscope. Only a few norovirus particles can make other people sick. You are most contagious:
- when you have symptoms of norovirus illness, especially vomiting, and
- during the first few days after you recover from norovirus illness.
However, studies have shown that you can still spread norovirus for two weeks or more after you feel better.
Where do norovirus outbreaks from food contamination happen?
- Restaurant: 64% 3
- Catering or Banquet facility: 17%
- Private Residence: 4%
- Health Care Facilities: 1%
- Schools and Daycare: 1%
- Other/multiple: 13%
How is norovirus spread
Norovirus spreads very easily. You can get norovirus by accidentally getting tiny particles of poop or vomit from an infected person in your mouth. This can happen if you:
- eat food or drink liquids that are contaminated with norovirus,
- touch surfaces or objects contaminated with norovirus then put your fingers in your mouth, or
- have direct contact with someone who is infected with norovirus, such as by caring for them or sharing food or eating utensils with them.
If you get norovirus illness, you can shed billions of norovirus particles that you can’t see without a microscope. Only a few norovirus particles can make other people sick. You are most contagious:
- when you have symptoms of norovirus illness, especially vomiting, and
- during the first few days after you recover from norovirus illness.
However, studies have shown that you can still spread norovirus for two weeks or more after you feel better.
How food can get contaminated with norovirus
Norovirus can easily contaminate food and water because it only takes a very small amount of virus particles to make you sick. Food and water can get contaminated with norovirus in many ways, including when:
- An infected person touches food with their bare hands that have poop or vomit particles on them
- Food is placed on a counter or surface that has poop or vomit particles on it
- Tiny drops of vomit from an infected person spray through the air and land on the food
- The food is grown or harvested with contaminated water, such as oysters harvested from contaminated water, or fruit and vegetables irrigated with contaminated water in the field
How water can get contaminated with norovirus
Recreational or drinking water can get contaminated with norovirus and make you sick or contaminate your food. This can happen:
- At the source such as when a septic tank leaks into a well
- When an infected person vomits or poops in the water
- When water isn’t treated properly, such as not enough chlorine
How surfaces can get contaminated with norovirus
Surfaces can get contaminated with norovirus in many ways, including when:
- An infected person touches the surface with their bare hands that have poop or vomit particles on them
- An infected person vomits or has diarrhea that splatters onto surfaces
- Food, water, or objects that are contaminated with norovirus are placed on surfaces.
Norovirus symptoms
Norovirus causes inflammation of the stomach or intestines. This is called acute gastroenteritis.
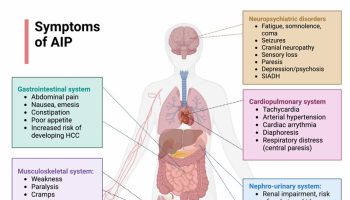
The most common symptoms of norovirus are:
- vomiting
- nausea
- diarrhea
- cramp-like stomach pain
- low-grade fever.
Other symptoms include:
- fever
- headache
- body aches
Symptoms usually appear 1 or 2 days after infection, but they can develop as soon as 12 hours after. They usually last for 1 to 3 days and rarely cause long-term harm in people who are otherwise healthy.
Symptoms can be more severe and long-lasting in elderly people, young children and people with a compromised immune system. If you or someone you care for has a severe infection, they may need hospital care.
If you have norovirus illness, you can feel extremely ill, and vomit or have diarrhea many times a day. This can lead to dehydration, especially in young children, older adults, and people with other illnesses.
Symptoms of dehydration include:
- decrease in urination
- dry mouth and throat
- feeling dizzy when standing up
Children who are dehydrated may cry with few or no tears and be unusually sleepy or fussy.
Norovirus outbreaks
Most outbreaks of norovirus illness happen when infected people spread the virus to others through direct contact, such as by caring for them or sharing food or eating utensils with them. Food, water, and surfaces contaminated with norovirus can also cause outbreaks.
Norovirus outbreaks have been reported in many settings, some of the most commonly reported outbreak settings are listed below.
Healthcare Facilities
The most commonly reported setting for norovirus outbreaks in the United States and other industrialized countries is healthcare facilities, including long-term care facilities and hospitals. Over half of all norovirus outbreaks reported in the United States occur in long-term care facilities 4.
The virus can be introduced into healthcare facilities by infected patients, staff, visitors, or contaminated foods. Outbreaks in these settings can sometimes last months. Norovirus illnesses can be more severe, occasionally even deadly, in patients in hospitals or long-term care facilities compared with healthy people.
Restaurants and at Catered Events
Norovirus is the leading cause of outbreaks from contaminated food in the United States. About 50% of all outbreaks of food-related illness are caused by norovirus 4. Most of these outbreaks occur in food service settings like restaurants. Infected food workers are frequently the source of outbreaks in food-service settings, often by touching ready-to-eat foods, such as raw fruits and vegetables, with their bare hands before serving them. However, any food served raw or handled after being cooked can get contaminated with norovirus.
Norovirus outbreaks can also occur from food that is contaminated at the source or on the farm, such as oysters harvested from contaminated water, or fruit and vegetables sprayed with contaminated water in the field.
Foods that are commonly involved in norovirus outbreaks include:
- leafy greens (such as lettuce),
- fresh fruits, and
- shellfish (such as oysters).
Schools and Child Care Centers
Norovirus outbreaks also frequently occur in schools, child care centers, colleges, and universities. Norovirus outbreaks on school and university campuses have even led to campus closures. Close quarters, shared spaces, and shared surfaces make it easy for norovirus to spread in schools. Children are also less likely to practice proper hand washing habits.
Cruise Ships
Cruise ships account for a small percentage (1%) of reported norovirus outbreaks overall 4. However, norovirus is most often the cause of outbreaks of diarrheal disease on cruise ships (over 90%). Because norovirus is the cause of most diarrheal outbreaks on cruise ships, and these outbreaks frequently get media attention, some people call norovirus the “cruise ship virus.” Norovirus can be especially challenging to control on cruise ships because of the close living quarters, shared dining areas, and rapid turnover of passengers. When the ship docks, norovirus can be brought on board in contaminated food or water or by passengers who were infected while ashore. Repeated outbreaks on consecutive cruises may also result from infected crew or environmental contamination. This is because norovirus can persist on surfaces and is resistant to many common disinfectants.
Norovirus causes
Noroviruses are named after the original Norwalk strain, which caused an outbreak of gastroenteritis in a school in Norwalk, Ohio in 1968. They are a group of non-enveloped, single-stranded RNA viruses that cause acute gastroenteritis (inflammation of the stomach or intestines). Noroviruses belong to the family Caliciviridae, which cause acute gastroenteritis.
Currently, at least 33 different norovirus genotypes have been described. Noroviruses that infect humans are caused by genotypes belonging to three genogroups (GI, GII, and GIV). Variants of the GII.4 genotype have been the most common cause of norovirus illnesses worldwide. In recent years, previously rare genotypes (GII.17, GII.2) have emerged and caused the majority of norovirus illnesses is some parts of the world.
Since there are many different genotypes of noroviruses, you can get infected many times during your life. You can develop immunity to (protection against) norovirus, but only for a short period of time (6 months to 9 years). This may explain why so many people of all ages get infected during norovirus outbreaks. Also, whether you are susceptible to norovirus infection is determined in part by your genes.
Norovirus Laboratory Diagnosis
Diagnostic methods for norovirus focus on detecting viral antigen or viral RNA (genetic material). Diagnostic tests are available at all public health laboratories and many clinical laboratories, and most use real-time reverse transcription-polymerase chain reaction (RT-qPCR) assays to detect norovirus.
RT-qPCR Assays
TaqMan-based RT-qPCR assays detect the RNA of the virus. They can be used to test stool, vomitus, food, water, and environmental specimens. RT-qPCR assays are the preferred method to detect norovirus because they are very sensitive and specific. They can detect as few as 10 to 100 norovirus copies per gram of sample. They use different oligonucleotide primer sets to differentiate genogroup I and genogroup II norovirus. RT-qPCR assays can also be quantitative and can provide estimates of viral load.
Multiplex Gastrointestinal Platforms
Recently, several commercial platforms for detection of multiple gastrointestinal pathogens have become available. They include genogroup I and genogroup II norovirus. The sensitivity of these assays for norovirus is in the same range as RT-qPCR. These platforms include FilmArray Gastrointestinal Panel, xTAG Gastrointestinal Pathogen Panel, and Verigene Enteric Pathogens Test.
Enzyme Immunoassays
Rapid commercial enzyme immunoassays (EIAs) that detect norovirus antigen in stool samples are also available. However, these kits have poor sensitivity (50 to 75%), and are, in general, not recommended for testing single samples from sporadic cases of gastroenteritis. These assays can be used for preliminary identification of norovirus when testing multiple specimens during outbreaks. However, samples that test negative should be confirmed by a second technique, such as RT-qPCR. Thus, EIA kits should not replace RT-qPCR during outbreak investigations.
Genotyping
Genetic characterization of noroviruses detected in stool and environmental samples can be very useful in epidemiologic investigations by linking cases, suggesting a common source, or identifying new emerging virus strains. Norovirus can be genotyped by sequence analysis of a RT-PCR product amplified from a partial region of both the polymerase gene and capsid gene (region B-C) in a single reaction for either genogroup I or genogroup II viruses.
All laboratories participating in CaliciNet (https://www.cdc.gov/norovirus/reporting/calicinet/index.html), a national laboratory surveillance network for norovirus outbreaks coordinated by CDC, use dual typing for norovirus. The sequences obtained are compared to CaliciNet reference sequences for typing. An example of dual typing nomenclature is the GII.P16-GII.4 Sydney norovirus strain that has caused about half of all norovirus outbreaks in the United States in recent years.
Norovirus prevention
Norovirus spreads very easily from infected people to others, and through contaminated foods and surfaces. There is currently no vaccine to prevent norovirus; although, this is an area of active research. You can help protect yourself and others from norovirus by following these prevention tips.
1. Practice proper hand hygiene
Wash your hands thoroughly with soap and water
- especially after using the toilet or changing diapers
- always before eating, preparing, or handling food, and
- before giving yourself or someone else medicine.
Norovirus can be found in your vomit or poop even before you start feeling sick. The virus can stay in your poop for 2 weeks or more after you feel better. It is important to continue washing your hands often during this time.
You can use alcohol-based hand sanitizers in addition to hand washing. But, you should not use hand sanitizer as a substitute for washing your hands with soap and water. Hand sanitizers aren’t as effective as washing hands with soap and water at removing norovirus particles.
2. Handle and prepare food safely
Carefully wash fruits and vegetables before preparing and eating them. Cook oysters and other shellfish thoroughly before eating them.
Be aware that noroviruses are relatively resistant to heat. They can survive temperatures as high as 145°F (63 °C) and quick steaming processes that are often used for cooking shellfish.
Food that might be contaminated with norovirus should be thrown out.
Keep sick infants and children out of areas where food is being handled and prepared.
3. When you are sick, do not prepare food or care for others who are sick
You should not prepare food for others or provide healthcare while you are sick and for at least 2 days after symptoms stop. This also applies to sick workers in restaurants, schools, daycares, long-term care facilities, and other places where they may expose people to norovirus.
4. Clean and disinfect surfaces
After someone vomits or has diarrhea, always thoroughly clean and disinfect the entire area immediately. Put on rubber or disposable gloves, and wipe the entire area with paper towels, then disinfect the area using a bleach-based household cleaner as directed on the product label. Leave the bleach disinfectant on the affected area for at least five minutes then clean the entire area again with soap and hot water. Finish by cleaning soiled laundry, taking out the trash, and washing your hands.
To help make sure that food is safe from norovirus, routinely clean and sanitize kitchen utensils, counters, and surfaces before preparing food.
You should use a chlorine bleach solution with a concentration of 1000 to 5000 ppm (5 to 25 tablespoons of household bleach [5% to 8%] per gallon of water) or other disinfectant registered as effective against norovirus by the Environmental Protection Agency (EPA). For more information, see EPA’s Registered Antimicrobial Products Effective Against Norovirus (https://www.epa.gov/sites/production/files/2016-06/documents/list_g_norovirus.pdf)
5. Wash laundry thoroughly
Immediately remove and wash clothes or linens that may be contaminated with vomit or poop.
You should:
- handle soiled items carefully without agitating them,
- wear rubber or disposable gloves while handling soiled items and wash your hands after, and
- wash the items with detergent and hot water at the maximum available cycle length then machine dry them at the highest heat setting.
Norovirus treatment
There is no specific medicine to treat people with norovirus illness.
The best treatment for a norovirus infection is rest and avoiding dehydration due to vomiting and diarrhea. This is particularly important for the elderly and babies.
Keep hydrated by drinking plenty of fluids such as an oral rehydration solution which you can buy at a pharmacy.
If you have a baby or young child with norovirus illness, it’s a good idea to have them checked by a doctor for dehydration. You can get rehydration fluids from a pharmacy. These are the best fluids to use in cases of gastroenteritis, especially for children.
If you can’t get any, or your child refuses to drink it, giving diluted fruit juice (one part juice to four parts of water) is reasonable. You could try a cube of ice or an iceblock if your child won’t drink. Avoid milk and other dairy products and do not give juice, sodas, sports drinks or other soft drinks as the sugar may make the diarrhea worse. It is fine to eat once you feel like it.
Babies can continue milk feeds throughout the illness, with rehydration fluid between feeds. Medication for nausea or diarrhea can be useful for adults, but may not be safe for kids. Antibiotics are rarely helpful.
If you are very sick with norovirus illness, you may need to go to hospital where you may be put on a drip.
Dehydration can lead to serious problems. Severe dehydration may require hospitalization for treatment with fluids given through your vein (intravenous or IV fluids).
Watch for signs of dehydration in children who have norovirus illness. Children who are dehydrated may cry with few or no tears and be unusually sleepy or fussy.
If you think you or someone you are caring for is severely dehydrated, see a doctor.
Juice, soft drink and cordial are all high in sugar, which can make diarrhea worse. If you don’t have a rehydration drink, you can have these drinks diluted:
- Juice or soft drink: mix 1 part drink to 4 parts water (for example, 40 ml of the drink with 160 ml water)
- Cordial: mix 1 part cordial to 20 parts water (for example, 5 ml cordial with 100 ml water)
There is no medication or antibiotic available to treat norovirus. You should only use anti-vomiting or anti-diarrheal medications if your doctor has recommended them.
Home remedies
To help keep yourself more comfortable and prevent dehydration while you recover, try the following:
- Let your stomach settle. Stop eating solid foods for a few hours.
- Try sucking on ice chips or taking small sips of water. You might also try drinking clear soda, clear broths or noncaffeinated sports drinks. Drink plenty of liquid every day, taking small, frequent sips.
- Ease back into eating. Gradually begin to eat bland, easy-to-digest foods, such as soda crackers, toast, gelatin, bananas, rice and chicken. Stop eating if your nausea returns.
- Avoid certain foods and substances until you feel better. These include dairy products, caffeine, alcohol, nicotine, and fatty or highly seasoned foods.
- Get plenty of rest. The illness and dehydration may have made you weak and tired.
- Be cautious with medications. Use many medications, such as ibuprofen (Advil, Motrin IB, others), sparingly if at all. They can make your stomach more upset. Use acetaminophen (Tylenol, others) cautiously; it sometimes can cause liver toxicity, especially in children. Don’t give aspirin to children or teens because of the risk of Reye’s syndrome, a rare, but potentially fatal disease. Before choosing a pain reliever or fever reducer discuss with your child’s pediatrician.
For infants and children
When your child has an intestinal infection, the most important goal is to replace lost fluids and salts. These suggestions may help:
- Help your child rehydrate. Give your child an oral rehydration solution, available at pharmacies without a prescription. Talk to your doctor if you have questions about how to use it. Don’t give your child plain water — in children with gastroenteritis, water isn’t absorbed well and won’t adequately replace lost electrolytes. Avoid giving your child apple juice for rehydration — it can make diarrhea worse.
- Get your child back to a normal diet slowly. Gradually introduce bland, easy-to-digest foods, such as toast, rice, bananas and potatoes.
- Avoid certain foods. Don’t give your child dairy products or sugary foods, such as ice cream, sodas and candy. These can make diarrhea worse.
- Make sure your child gets plenty of rest. The illness and dehydration may have made your child weak and tired.
- Avoid giving your child over-the-counter anti-diarrheal medications, unless advised by your doctor. They can make it harder for your child’s body to eliminate the virus.
If you have a sick infant, let your baby’s stomach rest for 15 to 20 minutes after vomiting or a bout of diarrhea, then offer small amounts of liquid. If you’re breast-feeding, let your baby nurse. If your baby is bottle-fed, offer a small amount of an oral rehydration solution or regular formula. Don’t dilute your baby’s already-prepared formula.
- Prevent the Spread of Norovirus. https://www.cdc.gov/Features/Norovirus/[↩]
- Journal of Medical Virology, August, 2008[↩][↩]
- Centers for Disease Control and Prevention. National Outbreak Reporting System, 2009-2012[↩]
- Common Settings of Norovirus Outbreaks. https://www.cdc.gov/norovirus/trends-outbreaks/outbreaks.html[↩][↩][↩]