Contents
What is nystagmus
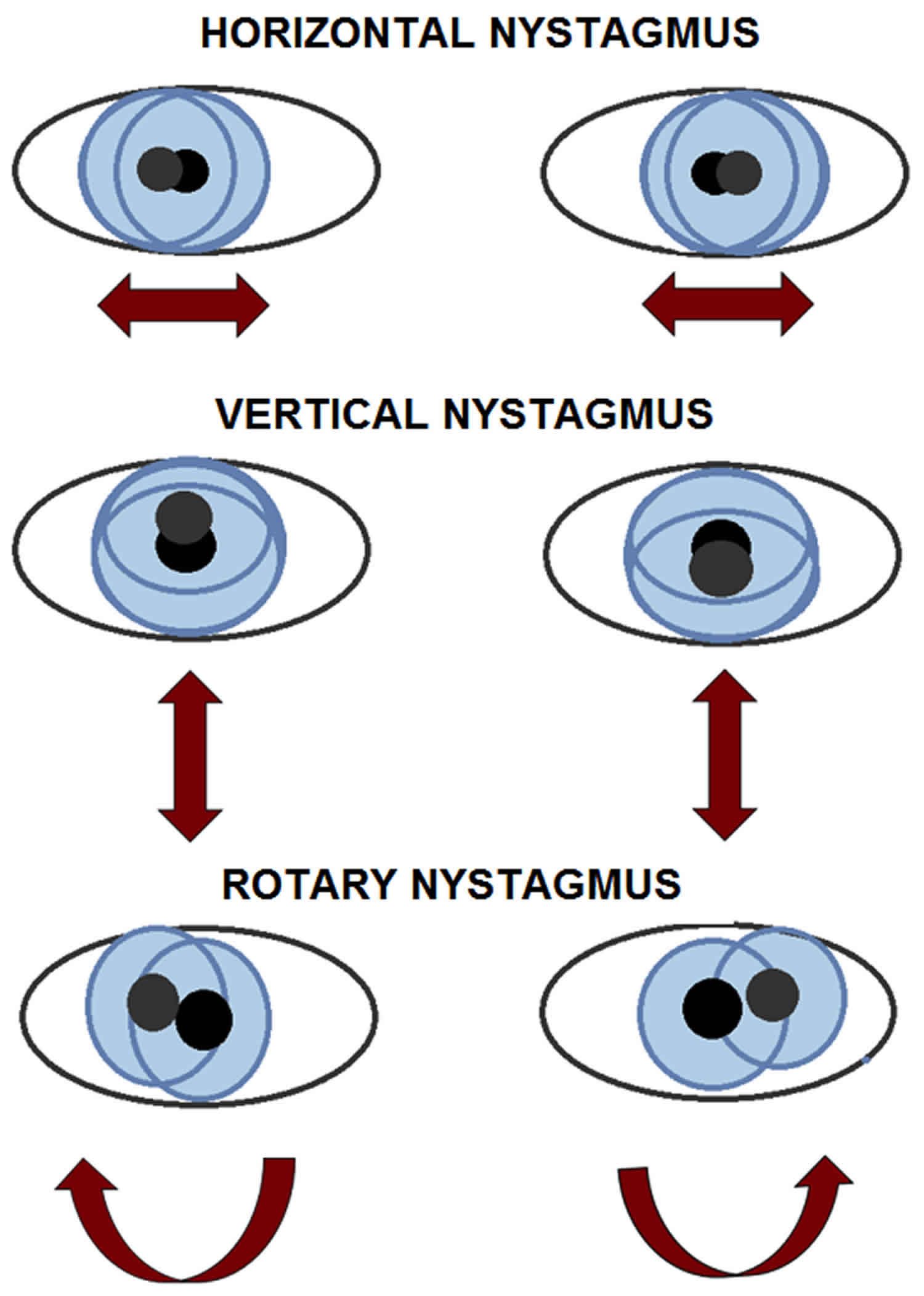
Nystagmus is defined by rhythmic, abnormal eye movements with a “slow” eye movement driving the eye off the target followed by a second movement that brings the eye back to the target. The movement can be horizontal (horizontal nystagmus), vertical (vertical nystagmus), rotary (rotary nystagmus) or a combination of these movements 1. Nystagmus can be jerk (named for fast phase) or pendular, variable amplitude and frequency, and can be worsened or improved by gaze position, fixation, or covering one eye (latent).
Nystagmus is a condition where the eyes move rapidly and uncontrollably. The eyes can move:
- side to side (horizontal nystagmus)
- up and down (vertical nystagmus)
- in a circle (rotary nystagmus)
The movement can vary between slow and fast and usually happens in both eyes. The eyes may shake more when looking in certain directions. People with nystagmus may tilt or turn their head to see more clearly. This helps to slow down the eye movements.
Nystagmus can be described as periodic, involuntary movements of one or both eyes in either a fast or slow oscillatory motion. By definition, nystagmus starts by a slow movement of the eye away from the visual target. The second movement brings the eye back to the visual target 1. If the second movement is slow, the nystagmus is said to be pendular. If this second movement is quick, the nystagmus is called jerk nystagmus. By convention, the direction of jerk nystagmus (e.g., right-beating nystagmus) is named after the fast phase of nystagmus. In a right-beating nystagmus, the fast phase is to the patient’s right.
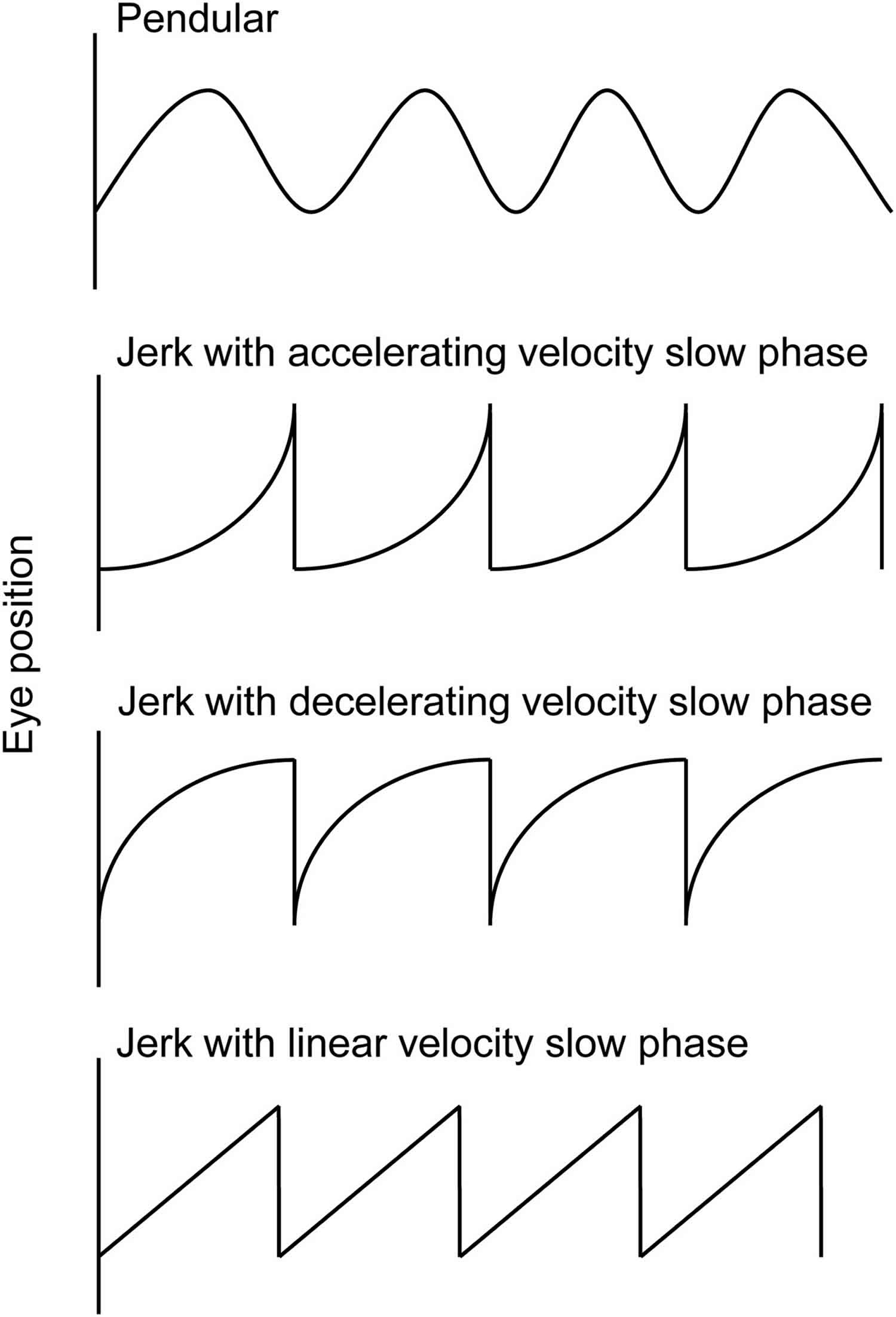
Nystagmus waveforms are named for their slow phase velocity profile (see Figure 2). The pendular form has no fast phase and is best depicted by the first wave of Figure 2. The exponential increasing velocity type is associated with congenital nystagmus. Decreasing velocity waveform is commonly seen in gaze-evoked nystagmus, which can be a physiologic finding. The linear waveform is typical of vestibular nystagmus. Dissociated nystagmus refers to the two eyes having nystagmus with the same direction but with differing amplitudes. Disconjugate nystagmus occurs when the two eyes have different direction of oscillation, one example of which is the sea-saw nystagmus. An interesting type of jerk nystagmus is the Periodic Alternating Nystagmus (PAN), which is characterized by a cycle of unidirectional jerk nystagmus followed by a dampening or cessation of the abnormal eye movement, then jerk nystagmus occurring in the opposite direction. In order to observe Periodic Alternating Nystagmus (PAN), the examiner should consider observing the patient for at least several minutes.
According to Sarvanathan et al. 2 who published the only epidemiological study of nystagmus in the general population, the prevalence of pathologic nystagmus is estimated to be 24 per 10,000 with a slight predilection toward European ancestry. The prevalence of infantile/pediatric nystagmus is said to be 17 per 10,000 by the same author. It has been reported to be as low as 6.7 per 100,000 3. The frequency of acquired nystagmus is estimated at 17% in children in contrast to 40% in adults. All forms of presumed acquired nystagmus need further diagnostic workup to determine the etiology. Nystagmus is considered to be acquired in patients presenting at or after the age of 6 months especially with asymmetric nystagmus (one eye with greater amplitude and/or frequency than the fellow eye), preservation of optokinetic nystagmus (in infantile idiopathic nystagmus, characteristic reversal of normal optokinetic nystagmus can be demonstrated), presence of a relative afferent pupillary defect, papilledema, or neurologic signs or symptoms 4.
Figure 1. Eye nystagmus
Figure 2. Nystagmus waveforms
Types of nystagmus
Congenital nystagmus
Congenital nystagmus or infantile nystagmus syndrome, is nystagmus that is present at birth. Congenital nystagmus starts in infants, usually between 6 weeks and 3 months old. Children with congenital nystagmus tend to have it in both eyes, which move side to side. Usually doctors do not know what is causing the child’s condition. Sometimes it is inherited (passed down from parents to children).
Children with congenital nystagmus typically do not see things as “shaking.” Instead, they may have some blurry vision.
Congenital nystagmus is usually mild. It does not become more severe, and it is not related to any other disorder.
People with congenital nystagmus are usually not aware of the eye movements, but other people may see them. If the movements are large, sharpness of vision (visual acuity) may be less than 20/20. Surgery may improve vision.
Nystagmus may also be caused by congenital diseases of the eye. Although this is rare, an eye doctor (ophthalmologist) should evaluate any child with nystagmus to check for eye disease.
Acquired nystagmus
This condition happens later in life. It has many causes, including serious medical conditions or drug and alcohol use.
Unlike children with congenital nystagmus, adults with nystagmus often say that things around them look shaky.
The most common cause of acquired nystagmus is certain drugs or medicines. Phenytoin (Dilantin) – an antiseizure medicine, excessive alcohol, or any sedating medicine can impair the labyrinth’s function.
Other causes include:
- Head injury from motor vehicle accidents
- Inner ear disorders such as labyrinthitis or Meniere disease
- Stroke
- Thiamine or vitamin B12 deficiency
Any disease of the brain, such as multiple sclerosis or brain tumors, can cause nystagmus if the areas controlling eye movements are damaged.
Physiologic nystagmus
Physiologic nystagmus (nystagmus that is characteristic of normal oculomotor function) include optokinetic nystagmus (OKN), vestibular ocular reflex, caloric nystagmus, and post-rotatory nystagmus. As they do not represent pathologic states, they will only be briefly discussed here.
Vestibulo ocular reflex
Vestibulo-ocular reflex (VOR) is the reflexive movement of the eye that keeps the visual image stable on the retina during brief, high frequency rotation of the head. Vestibulo-ocular reflexes (VORs) are controlled by the vestibular system of the inner ears, namely the semicircular canals, utricle, and saccule.
Optokinetic Nystagmus
Optokinetic nystagmus (OKN) is a physiologic movement of the eyes in response to large, moving visual fields (e.g. when one is looking out the window of a moving train) 5. The initial movement is a smooth pursuit movement followed by contraversive saccade back to primary gaze or direction of visual interest. The optokinetic nystagmus system cannot be isolated from vestibulo-ocular reflex (VOR) for clinical demonstration, but the use of an optokinetic drum gives an approximation of optokinetic nystagmus in action. Asymmetry of the optokinetic nystagmus response to the rotating drum may suggest lesions of the cerebrum, typically a large lesion of the parietal or parieto-occipital cortex and associated with homonymous hemianopia. This is in contrast to the lesions of the occipital lobe which also produce homonymous hemianopia but without the optokinetic nystagmus asymmetry 6.
Caloric Nystagmus
Caloric nystagmus is a type of VOR (vestibulo-ocular reflex) that is elicited by stimulating the horizontal semicircle with either warm or cold water in the ear canal to create a convection current in the endolymph of the semicircle. In normal subjects, when cold water is placed in one ear, the eyes will slowly turn toward the ear with horizontal fast phase away from the ear. The absence of caloric nystagmus may indicate brain death 7.
Post-rotatory
Post-rotatory nystagmus is a reflexive, transient, conjugate, jerk nystagmus that occurs after the whole body of a subject is passively rotated about the z-axis then decelerated to rest. The nystagmus that occurs in this situation has the fast phase in the opposite direction of the previous rotation and is accompanied by somatogyral illusion(sensation of rotating in the opposite direction of the original rotation). This nystagmus is due to the movement of the cupulas in response to rotation and deceleration from rotation 8.
Early Onset (Childhood) Nystagmus
Congenital nystagmus
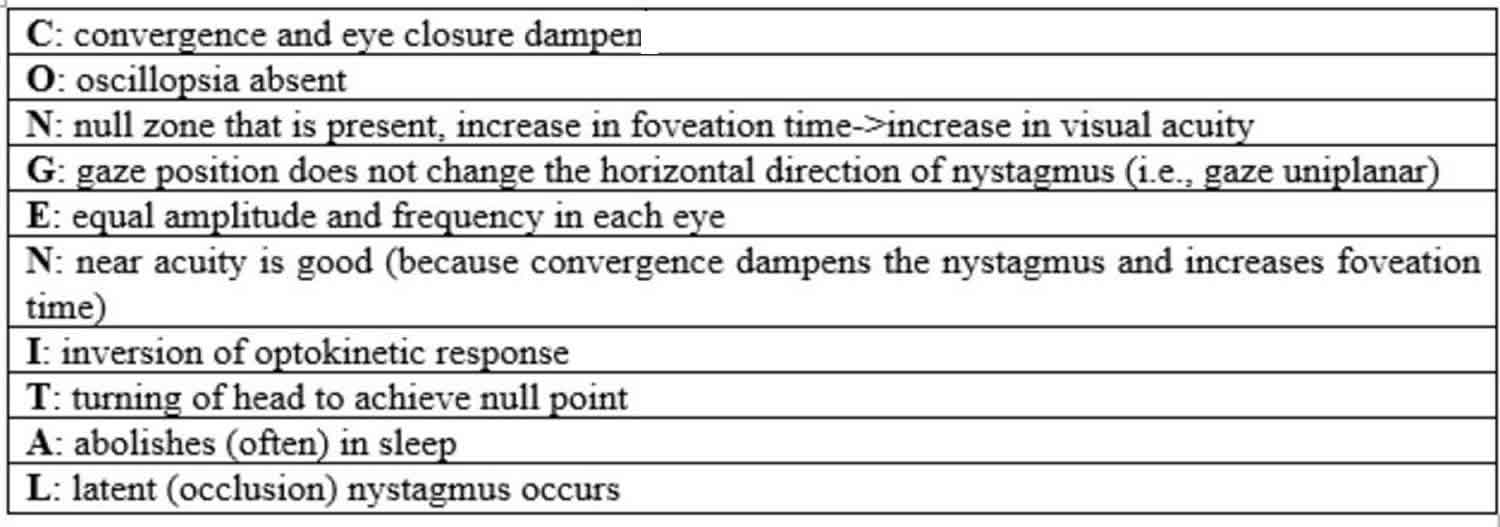
Congenital (motor) nystagmus also known as infantile idiopathic nystagmus, is the most common type of nystagmus seen in young patients followed by congenital sensory nystagmus 9. Congenital (motor) nystagmus (e.g. infantile idiopathic nystagmus) is by definition idiopathic (e.g. without a known cause or associated afferent pathway disease) and is therefore a diagnosis of exclusion. It is present from infancy but usually recognized a few months into life 10 and may even be evident only after the child has reached several years of age. Infantile idiopathic nystagmus is almost always bilateral, conjugate, and occurs in the horizontal plane, even in upgaze and downgaze, with little variability, which is in contrast to the highly variable presentation of spasmus nutans. Characteristics of congenital nystagmus can be concisely presented by the mnemonic “CONGENITAL” (table shown below):
Table 1. Congenital nystagmus mnemonic (infantile idiopathic nystagmus)
[Source 1 ]Both jerk and pendular types are seen in infantile idiopathic nystagmus, although pendular nystagmus can change to jerk waveform in right and left gaze. Note that congenital pendular nystagmus, a rare entity, is almost always horizontal, which is in contrast to acquired pendular nystagmus that can take horizontal, vertical and torsional planes with resultant elliptical waveforms[10]. Importantly, patients usually do not have oscillopsia 11 despite the presence of retinal slip exceeding 100 degrees/sec, which may be due to down-regulation of cortical activity in the area of MT/V5 bilaterally–an important part of the visual cortex for motion processing 12. The rarity of oscillopsia in infantile idiopathic nystagmus is a testament to the “efficacy of the mechanism by which the visual system compensates for nearly incessant retinal image motion” 13. There may be a family history of the disorder with X-linked mutations accounting for the most common mode of inheritance 14. In 2006, Tarpey et al. discovered the first gene causing infantile idiopathic nystagmus—the FRMD7 gene—so obtaining history and examining members may be of yield 2.
Two additional important signs of infantile idiopathic nystagmus are:
- Reversal of normal optokinetic nystagmus upon presentation of the rotating OKN drum 15
- Exponential increase of slow phase eye movement (see Figure 2, second waveform)
The visual acuity is proportional to the foveation time, and in most patients, the visual acuity is at or greater than 20/40 16. It is thought that infantile idiopathic nystagmus patients use “foveation strategy” such as “foveating saccades” to improve vision by maximizing the duration of the slow phase 17. Strabismus is present in about 15% of the patients with infantile idiopathic nystagmus. Good stereopsis is often present.
Visual attention and fixation amplifies (worsens) the nystagmus in infantile idiopathic nystagmus, but convergence on a near target dampens the amplitude and sleep abolishes it altogether 15. Infantile idiopathic nystagmus usually has a null point at which the abnormal eye movement has a lower intensity than in other directions of gaze. If the null point is not the primary gaze position, the patient may develop a head position/head turn in effort to reduce nystagmus. In these cases, extraocular muscle surgery can be performed to shift the null point to primary position and therefore minimize the amplitude of nystagmus at primary gaze position.
Sensory nystagmus
Sensory nystagmus, also known as nystagmus associated with afferent visual system abnormalities, is usually seen in the first 3-4 months and has the same oculomotor features as infantile nystagmus, but is due to anatomic disorders of the eye that, by limiting the proper visual sensory input to the eye, limit the visual development of the patient.
The causes of sensory nystagmus are many—but a few common etiologies can be remembered by the 5 A’s mnemonic:
- Aplasia (hypoplasia) of the optic nerve ( optic nerve hypoplasia),
- Leber congenital amaurosis,
- Aniridia,
- Achromatopsia, and
- Ocular albinism.
Other causes include impairment of the cortical system as seen in preterm infants with periventricular leukomalacia and those with traumatic brain injury or metabolic disorders. These entities must be ruled out in patients undergoing evaluation of their nystagmus by searching for impairment of visual tracking and optic atrophy. Neuroimaging may be recommended.
Latent Nystagmus (fusional maldevelopment nystagmus)
Latent nystagmus, also known as fusional maldevelopment nystagmus, is a benign, early onset conjugate horizontal jerk-nystagmus that only becomes manifest after occlusion of one eye. By definition, the nystagmus does not manifest under binocular conditions. The direction of the nystagmus is toward the uncovered eye, which means that the direction changes depending on which eye is occluded. Latent nystagmus is typically associated with congenital esotropia 18 and dissociated vertical deviation. Because of the induced nystagmus upon monocular occlusion, the visual acuity of these patients should be checked with partial optical blurring such as with a high-plus lens filter rather than with complete monocular occlusion.
Spasmus Nutans
Spasmus nutans is classically characterized by the triad of binocular small-amplitude pendular nystagmus, head nodding, and abnormal head posture or torticollis manifesting itself in the first year of life. Some authors suggest that the head nodding in spasmus nutans is a compensatory mechanism for oscillopsia rather than a separate pathological manifestation 19. Spasmus nutans in itself is a relatively benign condition that resolves by the end of the first decade of life though with often reduced visual acuity with or without significant refractive error 20. The pendular nystagmus of spasmus nutans is notable in that it is highly variable in amplitude and phase direction–at times becoming disconjugate, dissociated, purely monocular, then to conjugate over the course of minutes–which is in contrast to the stable nystagmus of congenital nystagmus. The markedly asymmetric and sometimes monocular involvement of spasmus nutans may be indistinguishable from the possibly life-threatening manifestations of optic pathway gliomas that cause monocular nystagmus of childhood. Neuroimaging should be considered.
Some authors reported the association between retinal dystrophies and suggested that electroretinographic studies be considered to assess for such disorders in patients presenting with suspected spasmus nutans 21.
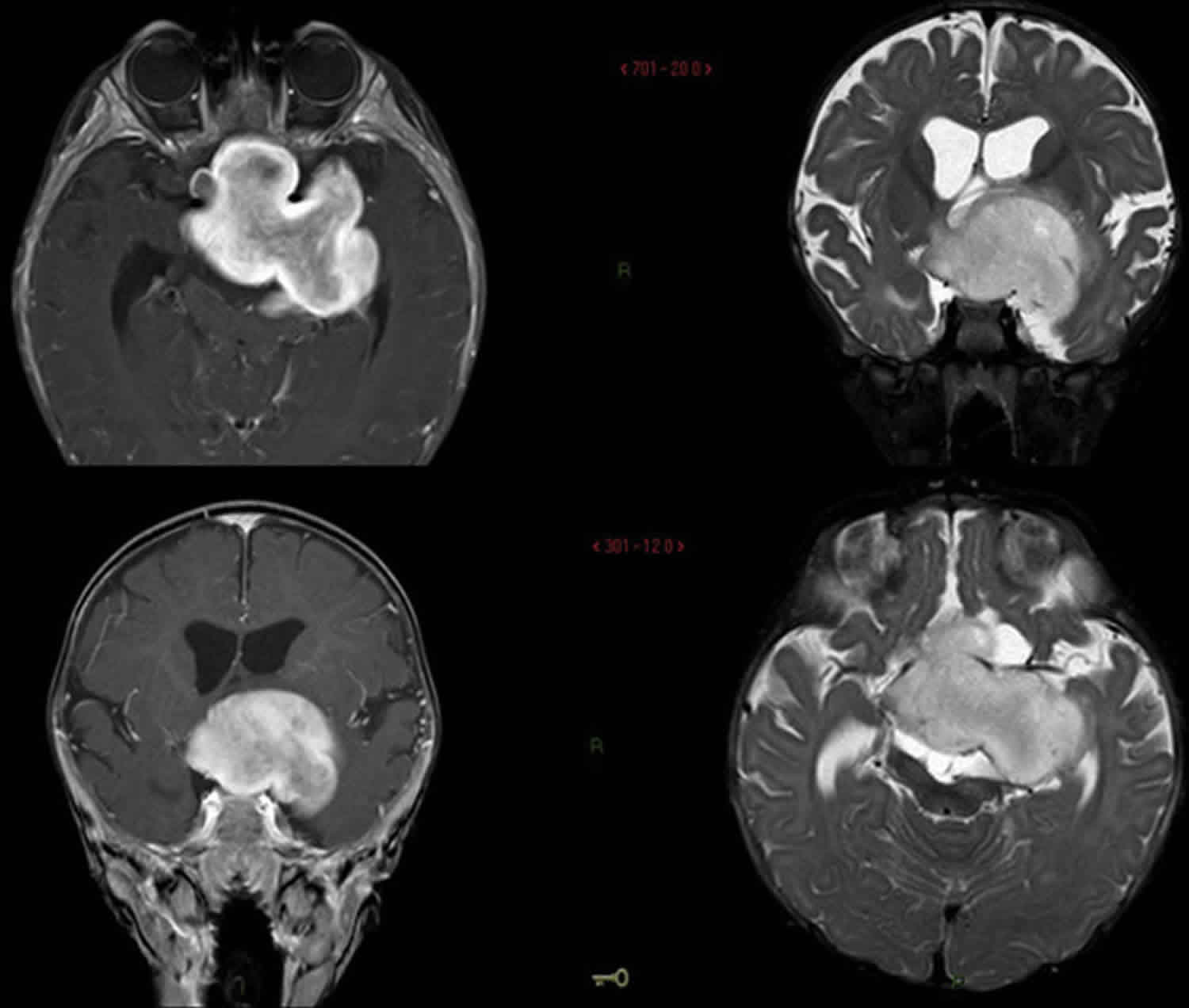
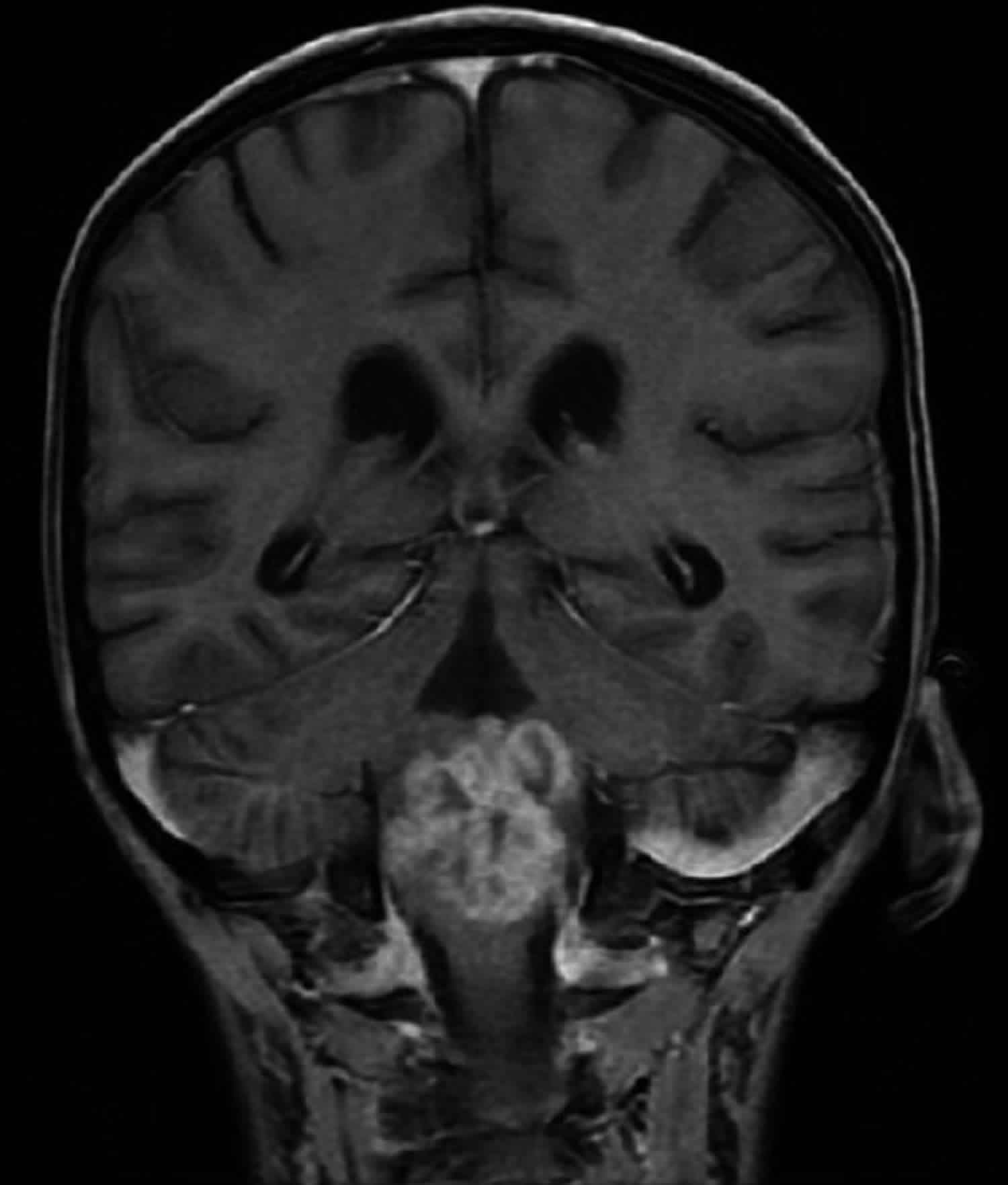
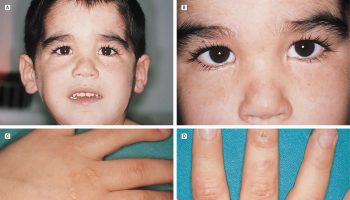
Monocular nystagmus of childhood
Monocular nystagmus of childhood is nystagmus that involves the same eye at all times in a child. The waveforms have small amplitude and can be vertical or elliptical. Heimann-Bielschowsky phenomenon is a type of monocular nystagmus that occurs due to longstanding poor vision in one eye with amblyopia, optic neuropathy, or dense cataract. It can often be inhibited by convergence or fixation. There are reports of improved monocular nystagmus after extraocular muscle surgery in the case of strabismic amblyopia causing the Heiman-Bielschowsky phenomenon 22. When an infant presents with signs of afferent pathway disease (e.g. optic disc atrophy, relative afferent pupillary defect, and the monocular nystagmus) however, neuroimaging should be considered 23. See Figure 3 for an example of a child who presented with monocular nystagmus and a chiasmic-hypothalamic glioma 24.
Figure 3. Monocular nystagmus of childhood
Footnote: Magnetic resonance neuroimaging (MRI) of an otherwise healthy, developmentally normal 4-month-old child with monocular nystagmus showing a large enhancing chiasmic-hypothalamic glioma.
Acquired Forms of Nystagmus
Nystagmus due to Defective Gaze-holding
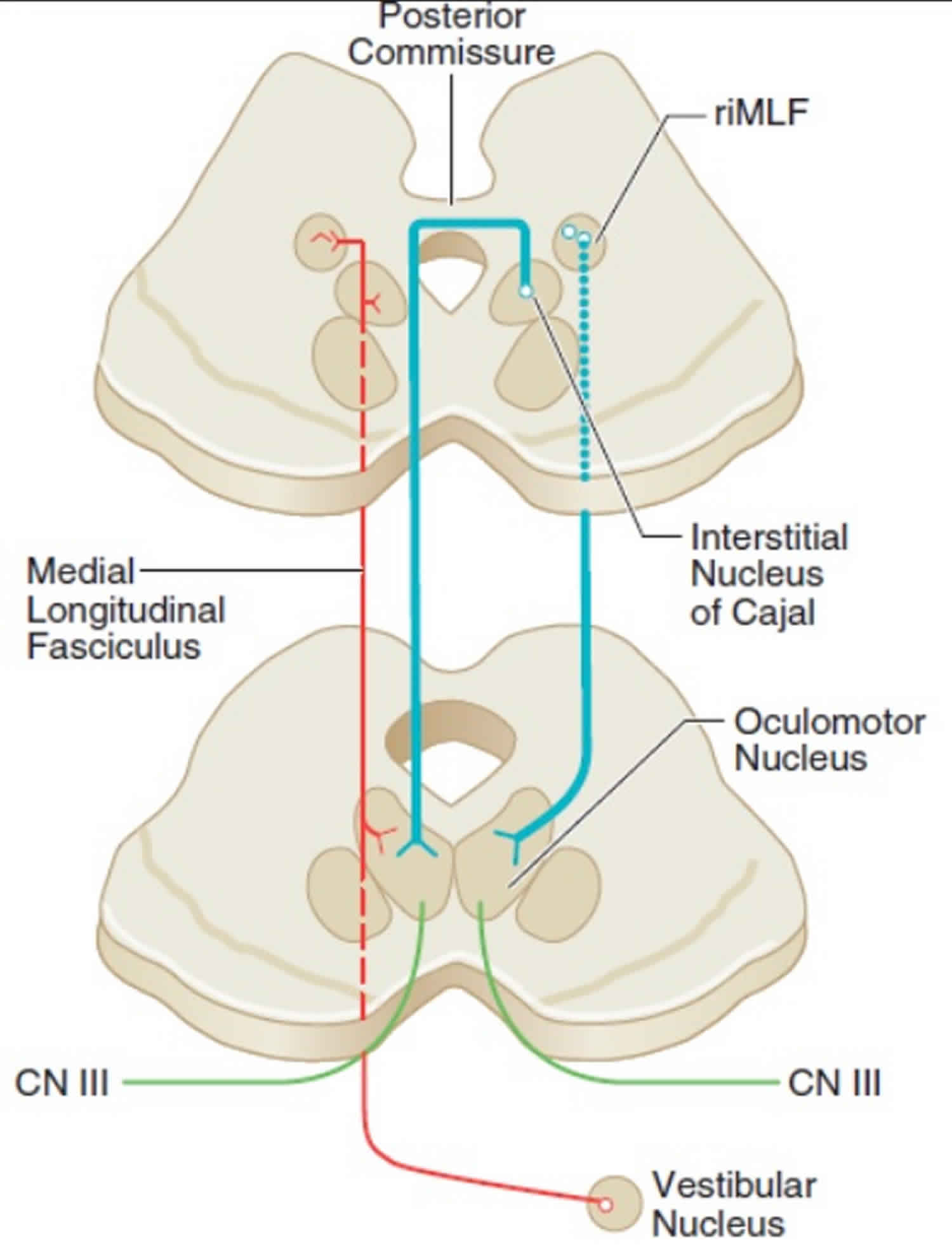
The neural mechanism for maintaining eccentric gaze involves a number of areas of the brainstem called the neural integrator. The horizontal gaze neural integrator consists of the nucleus prepositus hypoglossi and medial vestibular nuclei. Vertical and torsional gaze holding is maintained by the interstitial nucleus of Cajal. Other components of the neural integrator include the flocculus and nodulus of the cerebellum. All of these components are necessary to sustain eccentric gaze. When any part of the mechanism fails, defective gaze-holding manifests as nystagmus. See Figure 4 for illustration of the neural integrators.
Figure 4. Neural mechanism for maintaining eccentric gaze
Footnote: Elements of the neural integrator such as the vestibular nucleus and the interstitial nucleus of Cajal are intimately interconnected via the oculomotor nucleus.
[Source 25 ]Gaze-evoked Nystagmus and Rebound Nystagmus
Gaze-evoked nystagmus has jerk waveform movement that occurs in lateral gaze or upgaze. After each eccentric gaze, the eyes move toward the primary position followed by a saccade toward the eccentric direction, leading to right jerk nystagmus in right gaze and left jerk nystagmus in left gaze, etc. This format follows Alexander’s law, which states that nystagmus increases in amplitude and frequency as the patient looks in the direction of the fast phase. Unlike end-gaze nystagmus (conjugate, in both right and left directions of gaze, transient, low amplitude of under 4-degrees, more prominent with age, benign), gaze-evoked nystagmus is sustained, larger in amplitude, possibly asymmetric, and is often associated with down-beat nystagmus.
Gaze-evoked nystagmus is a sign of neural integrator dysfunction. Advanced age can cause degenerative impairment of the neural integrator, leading to an often symmetric, horizontal gaze-evoked nystagmus. Unsustained gaze evoked nystagmus of short duration, with a low amplitude and frequency, elicited at extreme horizontal fields of gaze, especially in an elderly patient, is usually physiologic and does not require further investigation. In contrast, primary position nystagmus, sustained (>20 seconds), or asymmetric gaze evoked nystagmus are usually pathologic however, and should prompt further investigation 3. Causes may include intoxication (e.g., sedatives, anticonvulsants, alcohol, illicit drug or hypnotic use), trauma, stroke, demyelination, Chiari malformation, or tumor. See Figure 5.
Figure 5. Gaze-evoked nystagmus
Footnote: An 11 year old boy who presented with gaze-evoked nystagmus, cachexia, and global weakness was found to have atypical teratoid rhabdoid tumor compressing the ventral medulla.
[Source 26 ]Rebound nystagmus is a variant of gaze-evoked nystagmus. When the subject resumes primary gaze after a period of eccentric gaze holding, the eyes drift back toward the prior eccentric direction of gaze with saccade back to primary gaze. The nystagmus is transient (usually less than 30 seconds). Rebound nystagmus is often associated with cerebellar disease such as those associated with gaze-evoked nystagmus.
Gaze-evoked and rebound nystagmus require attention and evaluation to find the underlying cause. The nystagmus themselves generally do not require treatment.
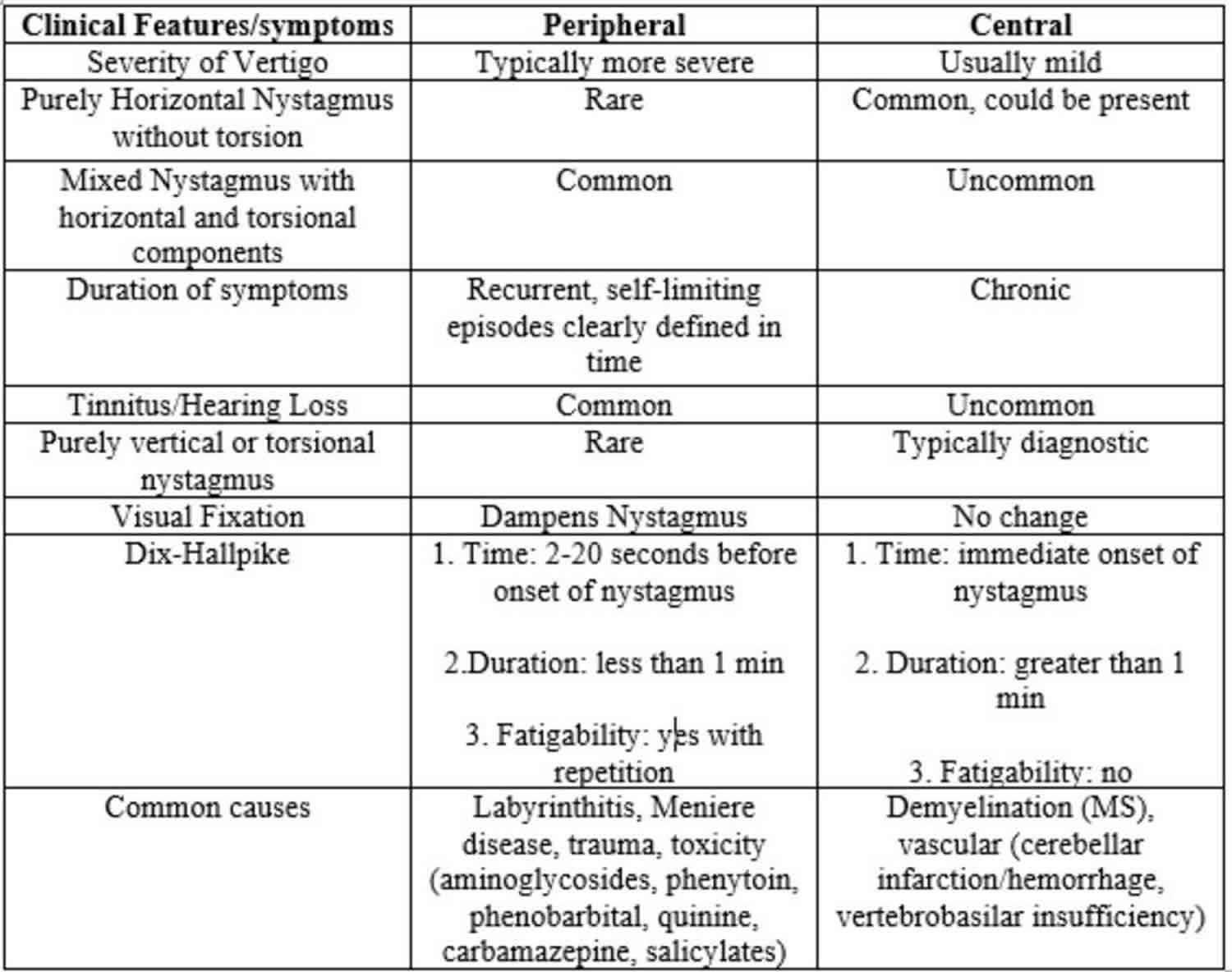
Peripheral Vestibular Nystagmus
Peripheral vestibular nystagmus arises from end-organ dysfunction. A table comparing the clinical characteristics and common causes of peripheral versus central vestibular nystagmus is shown below 6.
Table 2. Peripheral vs. Central Nystagmus
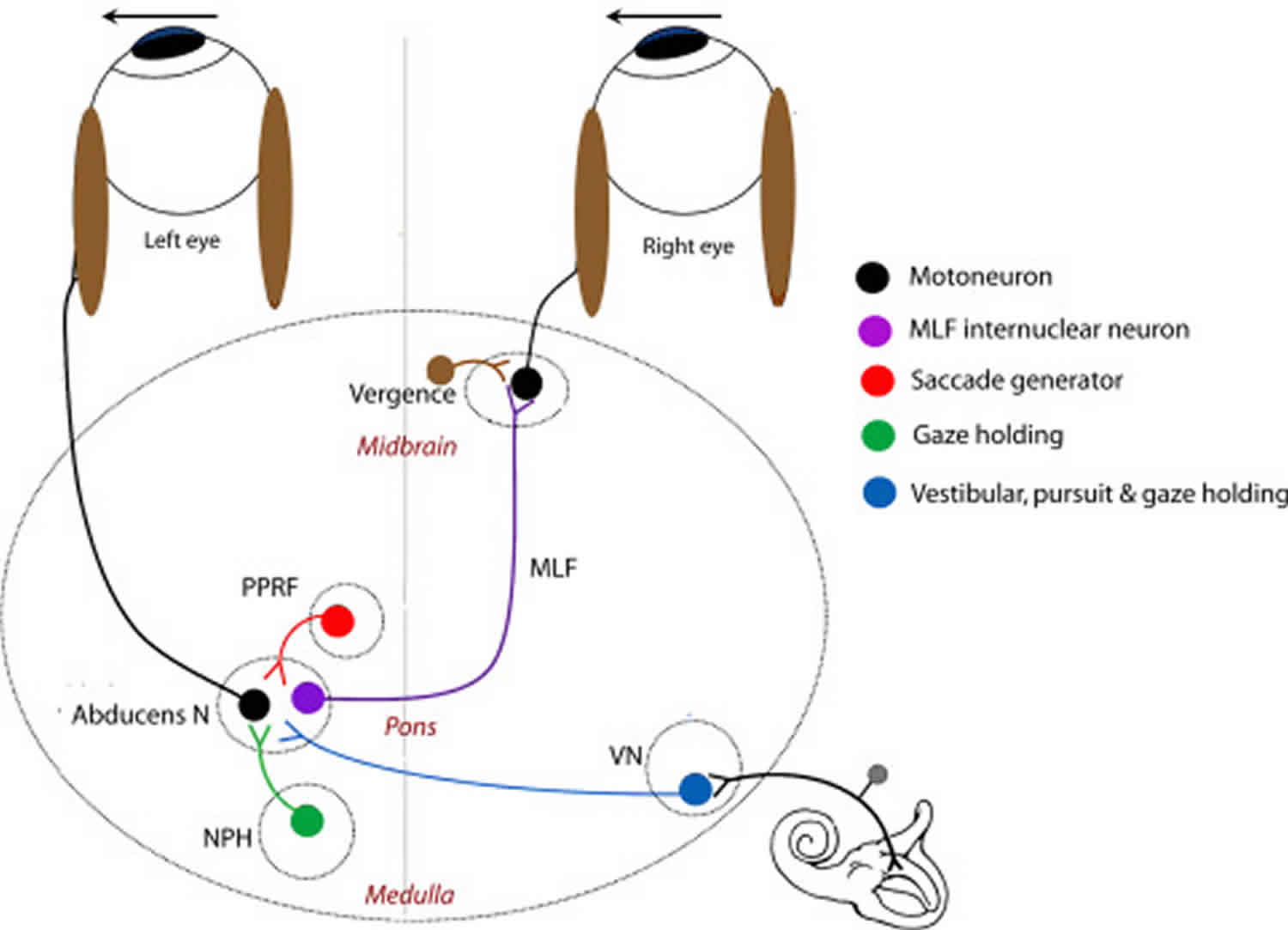
The vestibular system includes the inner ear elements such as the semicircular canals, otolithic structures, and the vestibular nerve. See Figure 6 for a diagram of the involved neural networks. Because of the disruption of the vestibular input into the neural integrator which routes the signal to the contralateral paramedian pontine reticular formation (PPRF), the resulting nystagmus has slow-phase toward the side of the problematic vestibular system. The nystagmus follows Alexander’s law. Generally, peripheral vestibular nystamus follows a horizontal-torsional pattern, which is in contrast to the purely vertical or torsional nystagmus seen in central vestibular nystagmus.
Because of the involvement of the vestibular system, patients often present with symptoms of inner ear disease such as vertigo, nausea, vomiting, oscillopsia, tinnitus, and sometimes even hearing loss. The symptoms usually improve over time though they may be recurrent. The type associated with tinnitus and hearing loss is called Méniere disease 27, while the type associated with vertigo in certain postures is known as benign paroxysmal positional vertigo (BPPV). The Dix-Hallpike maneuver is useful in the diagnosis of BPPV (benign paroxysmal positional vertigo), and the Epley maneuver is used to treat BPPV (benign paroxysmal positional vertigo) though with high disease recurrence rate.
A unique characteristic of peripheral vestibular nystagmus is the dampening effect on the nystagmus by visual fixation, which is in contrast to central vestibular nystagmus. Treatment of the different types of peripheral vestibular nystagmus may vary from observation to otolaryngologic surgery 27.
Figure 6. Major connections mediating eye movement associated with the vestibular system
Abbreviations: MLF = Medial longitudinal fasciculus; PPRF = Paramedian pontine reticular formation; NPH = nucleus prepositus hypoglossi; VN = Vestibular nucleus.
[Source 1 ]Central Vestibular Nystagmus
Central forms of vestibular nystagmus arise from dysfunction in one of the many interconnections between the central vestibular structures and the neural integrators. In contrast to peripheral vestibular nystagmus, centrally-derived nystagmus is not classically inhibited by visual fixation and is typically confined to one plane (e.g., purely vertical or torsional). Neuroimaging is crucial in determining the location of the etiologic structural lesions although metabolic and biochemical pathologies should also be considered. Generally, if patients present with small amplitude, eccentric nystagmus, the patient may be visually asymptomatic but may still have other associated brainstem or cerebellar signs 28.
Bruns Nystagmus
Bruns Nystagmus is a combination of peripheral and central vestibular nystagmus due to the involvement of 2 different neural pathways–(1) cerebellar flocculi (2) peripheral vestibular components of the cerebellum—and usually manifests as a symptom of cerebellar pontine angle tumors (e.g., acoustic neuromas or meningiomas) greater than 3.5 cm 9. Initially, with only peripheral involvement (e.g. vestibular nerve impairment), the first phase of oscillatory movement is toward the side of the lesion, initiating the second phase in the opposite direction, which is fast and corrective—rapid, small amplitude nystagmus away from the side of the lesion. As the lesion expands (e.g. enlargement of the tumor, compression of ipsilateral brainstem) involving the central nervous system, a second nystagmus may become manifest. With compression of the brain, specifically the cerebellar flocculus, the ability to hold ipsilateral eccentric gaze becomes impaired—the nystagmus is slower, with an increase in amplitude and change in direction towards the side of the lesion—slow, large amplitude nystagmus towards the side of the lesion. Thus, this specific type of nystagmus consists of two simultaneous nystagmus: (1) coarse, large amplitude, low frequency evoked on gaze ipsilateral to lesion (2) fine, low amplitude, high frequency evoked on gaze contralateral to lesion 9.
Downbeat Nystagmus
Downbeat nystagmus (downward fast phase) is the most common of the central vestibular nystagmus. Its jerk nystagmus waveform begins with upward drift of the eyes corrected with a downward saccade. This form of nystagmus follows Alexander’s Law and hence is accentuated by downgaze and also by lateral-down gaze, but is also amplified by convergence and lying prone 29. Concomitant gaze-evoked nystagmus and rebound nystagmus may be observed 28. Generally patients are symptomatic from vertical oscillopsia. The differential for down-beating nystagmus is broad, but structural lesions can be ruled out with neuroimaging. Cervico-medullary junction is the most probable location of a structural lesion most commonly Arnold-Chiari malformation or spinocerebellar degeneration (e.g. ataxia telangiectasia), which may be accompanied by a positive family history.
- Tumors at the foramen magnum
- Arnold-Chiari malformation Type 1
- Demyelination
- Stroke
- Cranial trauma
- Drug toxicity (lithium, anticonvulsants)
- Platybasia
- Spinocerebellar degeneration
- Brainstem encephalitis
- Paraneoplastic syndrome
- Impaired nutrition (e.g., Wernicke encephalopathy, parenteral feeding, magnesium deficiency)
- Antibody to glutamic acid decarboxylase (GAD)
- Idiopathic
There are several antibodies that have been associated with downbeat nystagmus in a growing number of cases, mainly antibodies to voltage gated calcium channels and to glutamic acid decarboxylase (GAD) 30. Glutamic acid is converted to GABA, a central player in neuronal signaling and transmission in the CNS, by glutamic acid decarboxylase (GAD). Downbeat nystagmus is caused by imbalance of the activities of the anterior and posterior canals due to lesions in the vestibulocerebellum (specifically the flocculi) and the medulla. The pathophysiology behind this association is the GABAergic neuronal regulation of communication between Purkinje cells and floccular neurons. Antibodies to glutamic acid decarboxylase (GAD) prevent the conversion of glutamic acid to GABA, reducing the innervation of floccular neurons to the anterior vestibular canals, thereby resulting in downbeat nystagmus 11. There were several case studies that reported that steroids and intravenous immunoglobulin (IVIG) may be beneficial for anti-GAD associated downbeat nystagmus or cerebellar ataxia 12.
Base-out prism and pharmacologic therapies with clonazepam, baclofen, gabapentin 31, memantine, aminopyridine have been suggested but usually with mixed success 32 and with side effects like conversion to upbeat nystagmus 33 or seizures 34. See section on pharmacologic therapy.
Upbeat Nystagmus
Upbeat nystagmus is purely-vertical conjugate nystagmus that manifests itself in primary gaze with slow downdrift of the eyes corrected by fast upward saccade. Patients may experience vertical oscillopsia. Structural lesions in the brainstem or in the anterior cerebellar vermis can cause this type of nystagmus. Causes include demyelinating disease 35, stroke, tumors, cerebellar degeneration, and tobacco smoking 36.
Rotary nystagmus
Eyes with rotary nystagmus have fast phase intorsion or extorsion that is usually conjugate and symmetric. Purely torsional nystagmus without horizontal or vertical components indicates a defect in the brainstem, while torsional with a vertical component indicates a lesion in the midbrain. See the table below for comparison of the two different types of rotary nystagmus. The differential includes stroke, demyelinating disease, and Chiari malformation. Neuroimaging is important for localization of structural lesions. See pharmacological therapy for treatment options.
Comparison of rotary nystagmus
| Purely torsional | Torsional with either downward or upward component | |
|---|---|---|
| Localization | Brainstem (pontomedullary junction) contralateral to fast phase | Midbrain |
| Ocular tilt reaction direction | Ipsi-lesional | Contra-lesional |
Seesaw Nystagmus and Hemi-Seesaw Nystagmus
Seesaw nystagmus, a subtype of torsional nystagmus, is descriptively named for the pendular, disconjugate movement of eyes in which one elevates/intorts while the fellow eye depresses/extorts. Hemi-seesaw nystagmus is similar but with jerk waveform rather than pendular. See the table below for common causes.
Comparison of seesaw and hemi-seesaw nystagmus
| Seesaw Nystagmus | Hemi-seesaw Nystagmus | |
|---|---|---|
| Common cause | Large parasellar tumor (craniopharyngioma, pituitary adenoma) | Midbrain hemorrhage, medullar infarcts, Chiari malformation |
Congenital achiasma has been rarely associated with seesaw nystagmus 37. Other ocular associations with seesaw nystagmus include retinitis pigmentosa 38 and albinism 39.
Periodic Alternating Nystagmus
This rare type of nystagmus is a strictly horizontal, conjugate, jerk nystagmus that periodically alternates its direction of fast phase. One half cycle of 30 to 90 seconds will involve right-beating nystagmus followed by the same duration of left-beating nystagmus. The two halves of each cycle is divided by a transition period of minimal to no nystagmus or small-amplitude vertical nystagmus. Because of the multi-minute duration of each cycle, the observer should consider watching the patient’s eye for at least several minutes to detect the change in direction. The patient may also alternate his/her head turn to the eye position to null point (right head turn during right-beating cycle) in accordance with Alexander’s law.
Periodic alternating nystagmus (PAN) can be congenital or acquired, although the congenital form is less predictably periodic compared to the acquired form 28. Associated central nervous system pathologies may involve Chiari malformation, multiple sclerosis, and stroke, but phenytoin use 40 and bilateral significant visual loss 41 should also be considered as the cause of PAN.
Acquired Pendular Nystagmus
Unlike congenital pendular nystagmus, acquired pendular nystagmus often entails slow-phase eye movements in horizontal, vertical, and torsional planes with resultant elliptical or circular nystagmus. The movements may be monocular, or if bilateral, conjugate or disconjugate, and may also be dissociated. The most common cause of acquired pendular nystagmus is multiple sclerosis. If the vision is asymmetric between the two eyes, the poorer-seeing eye has greater amplitude and frequency of nystagmus compared to the fellow eye 30.
Oculopalatal myoclonus or tremor
If acquired pendular nystagmus has concomitant palatal myoclonus (oscillation of the palate), it is called oculopalatal myoclonus or oculopalatal tremor. The eye movements are continuous with both torsional and vertical components with frequency of 1-3 Hz. Additional muscles (pharynx, face, vocal cords, respiratory muscles, and even trunk and extremities) may be involved in this involuntary rhythmic movement that persists during sleep.
MRI of the brain would show hypertrophic degeneration of the inferior olivary nucleus in the medulla (radiologic pimento sign) 42. This degeneration occurs as a result of brain infarct or hemorrhage, but the onset of the oculopalatal tremor is delayed for months or years after the initial insult due to neural deafferentation 28.
Oculo-masticatory myorhythmia
The combination of pendular vergence nystagmus and associated contractions of the masticatory/facial/pharyngeal muscles are pathognomonic for Whipple’s disease 43. The horizontal oscillation of each eye with oculomasticatory myorhythmia is out of phase and hence produces convergence-divergence nystagmus at about 1 cycle per second 28. Patients commonly have systemic manifestation of the disease including fever, abdominal pain, diarrhea, cognitive dysfunction, weight loss, and arthralgia. Definitive diagnosis can be made through biopsy of the duodenum that shows periodic acid-Schiff staining of foamy macrophages in the villae. Antibiotic therapy should be instituted for this lethal disease, which has a high rate of recurrence for CNS-involving manifestations 44. PCR of Tropheryma whippelii RNA can be a useful laboratory test.
Dissociated Nystagmus
Dissociated Nystagmus is characterized by a difference or dissimilarity of the direction, extent and/or periodicity of the ocular oscillations between the two eyes. The most common etiology of this type of nystagmus is lesion of the MLF (medial longitudinal fasciculus) and subsequent internuclear ophthalmoplegia (INO). This results in impaired horizontal movements with slowed or weakened adduction of the affected eye (ipsilateral to MLF lesion) and abduction nystagmus of the unaffected eye (contralateral to MLF lesion) 14. The pathogenesis of this condition is the development of an adaptive response and increased neural pulsing/signaling to compensate for weakened adduction on lateral gaze/medial rectus muscle. Hering’s Law of equal innervation follows that the increased neural pulsing/signaling should also be accompanied by equal pulsing/signaling to the contralateral yoke muscle, which in this case creates excessive saccadic movements on contralateral gaze/lateral rectus muscle 15.
Toxin/Illicit Drug-induced Nystagmus
Classically, phencyclidine (PCP) intoxication is associated with nystagmus, specifically rotatory or torsional nystagmus 45. Other common drugs/toxins that may be associated with vertical, horizontal, rotatory, or mixed nystagmus include anticonvulsants (phenytoin, carbamazepine, valproic acid, lamotrigine, topiramate), ethanol, amphetamines, barbiturates, benzodiazepines, 3,4-Methylenedioxymethamphetamine (MDMA), also known as “ecstasy”), salicylates, selective serotonin reuptake inhibitors (SSRI), lithium, dextromethorphan, ketamine and Lysergic acid diethylamide (LSD) 18.
What causes nystagmus
The brain controls eye movement. Your eyes move automatically to adjust when you move your head slightly. This stabilizes the image that you are looking at so you see a sharper image. In people with nystagmus, the areas of the brain that control eye movements do not work properly.
In some cases, it is not clear why someone has nystagmus. In other cases, nystagmus may be related to other eye problems.
Nystagmus can be related to the following:
- Having a family history of nystagmus
- Albinism (lack of color, or pigmentation, in the skin)
- A wide range of eye problems, including cataracts, strabismus and focusing problems
- Inner ear problems, such as Meniere’s disease
- Multiple sclerosis
- Stroke (a common cause of acquired nystagmus in older people)
- Head injury (a common cause of acquired nystagmus in younger people)
- Use of certain medications, such as lithium or anti-seizure medications
- Alcohol or drug use
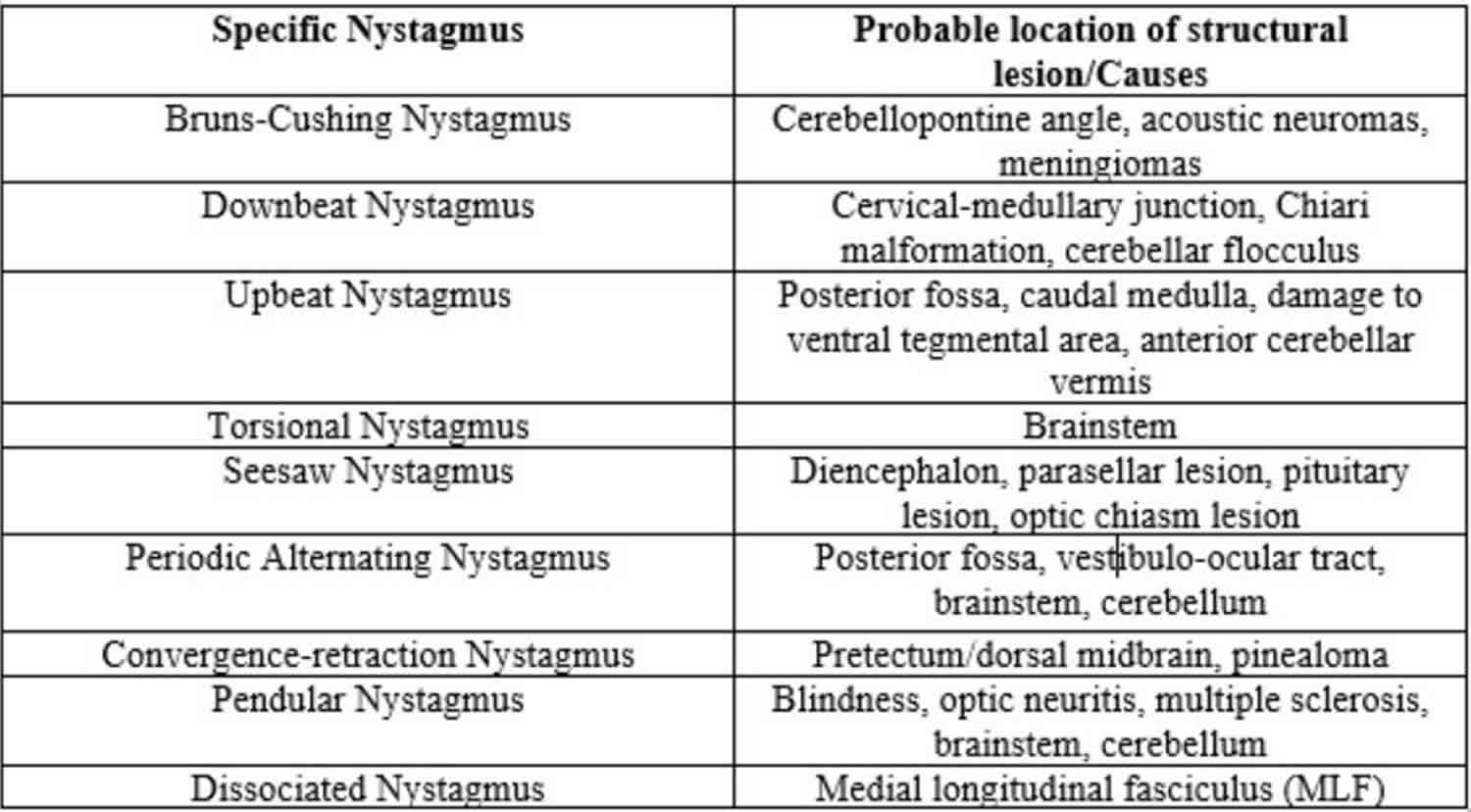
Selected nystagmus and their most common corresponding etiologic structural lesions are presented in Table 3 below 4.
Table 3. Localization of nystagmus
Nystagmus symptoms
The main symptom of nystagmus is rapid eye movement that cannot be controlled. Usually the movement is side to side (horizontal nystagmus). It can also be up and down (vertical nystagmus) or circular (rotary nystagmus). The movement can vary between slow and fast, and it usually happens in both eyes.
In addition to rapid eye movement, nystagmus symptoms include:
- sensitivity to light
- dizziness
- difficulty seeing in the dark
- vision problems
- holding the head in a turned or tilted position
- the feeling that the world is shaking
Nystagmus diagnosis
Nystagmus is diagnosed by an ophthalmologist. They will examine the inside of your eyes and test your vision. Your ophthalmologist will also look for other eye problems that may be related to nystagmus. These problems could include strabismus (misaligned eyes), cataracts (clouding of the eye’s lens), or a problem with the eyes’retina or optic nerve.
One way to see nystagmus is to spin a person around for about 30 seconds, stop and then have them try to stare at an object. If they have nystagmus, their eyes will first move slowly in one direction, then move rapidly in the opposite direction.
When assessing a patient with nystagmus, the examiner should consider assessing ocular stability/motility in primary gaze first followed by observation of the eye movement in cardinal gazes. A full description of the nystagmus should be gathered from examination, concisely presented in the form of the mnemonic DWARF—Direction, Waveform, Amplitude, Reducing direction, Frequency. In addition, the following characteristics should be identified:
- Monocular or binocular involvement
- Conjugacy (do both eyes move together?)
- Direction of movement (horizontal, vertical, torsional, or mixed)
Stability of direction of movement (is the phase gaze always to the right?) - Continuous or intermittent
- Amplitude (how big are the movements?)
- Frequency (how often are the movements happening?)
- Presence of null point (the direction of gaze or distance of fixation at which nystagmus is minimal to nil)
- Presence of slow phase (if there is no slow phase, the eye movement disorder is considered a saccadic intrusion)
- General condition of the patient (is the patient comatose?)
- Associated symptoms such as vertigo, nausea, and oscillopsia
Nystagmus test
Other tests that may be used to diagnose nystagmus are:
- Electro-oculography: An electrical method of measuring eye movements using tiny electrodes (to confirm the type of nystagmus and see details of the eye movements)
- An ear exam
- Vestibular testing by recording the movements of the eyes
- A neurological exam
- tests to get images of the brain, including computerized tomography (CT) and magnetic resonance imaging (MRI)
Nystagmus treatment
Treating nystagmus depends on the cause. Options for managing nystagmus can vary from observation to surgeries depending on the nature and cause of the nystagmus.
People born with nystagmus cannot be cured of this condition. However, they may benefit from glasses or contact lenses. These do not fix the nystagmus, but having clearer vision can help slow the eye movements.
Rarely, surgery may be done to reposition eye muscles that move the eyes. This keeps the head from needing to turn as far to keep the eyes from moving. However, surgery does not correct or cure nystagmus. It just allows someone to keep their head in a more comfortable position to limit eye movement.
Sometimes, acquired nystagmus can go away. This happens if the condition that causes the nystagmus is treated. That can include treating a medical problem or stopping drug or alcohol use.
Medications for nystagmus
For the treatment of congenital nystagmus (both in idiopathic and secondary forms), pharmacologic therapies with gabapentin and memantine have been studied in a randomized clinical trial of adult patients. Statistically significant improvement in visual acuity and nystagmus amplitude were measured in patients in the treatment arm compared to those in the placebo arm 46. Clonazepam and baclofen have also been tried with mixed results 47.
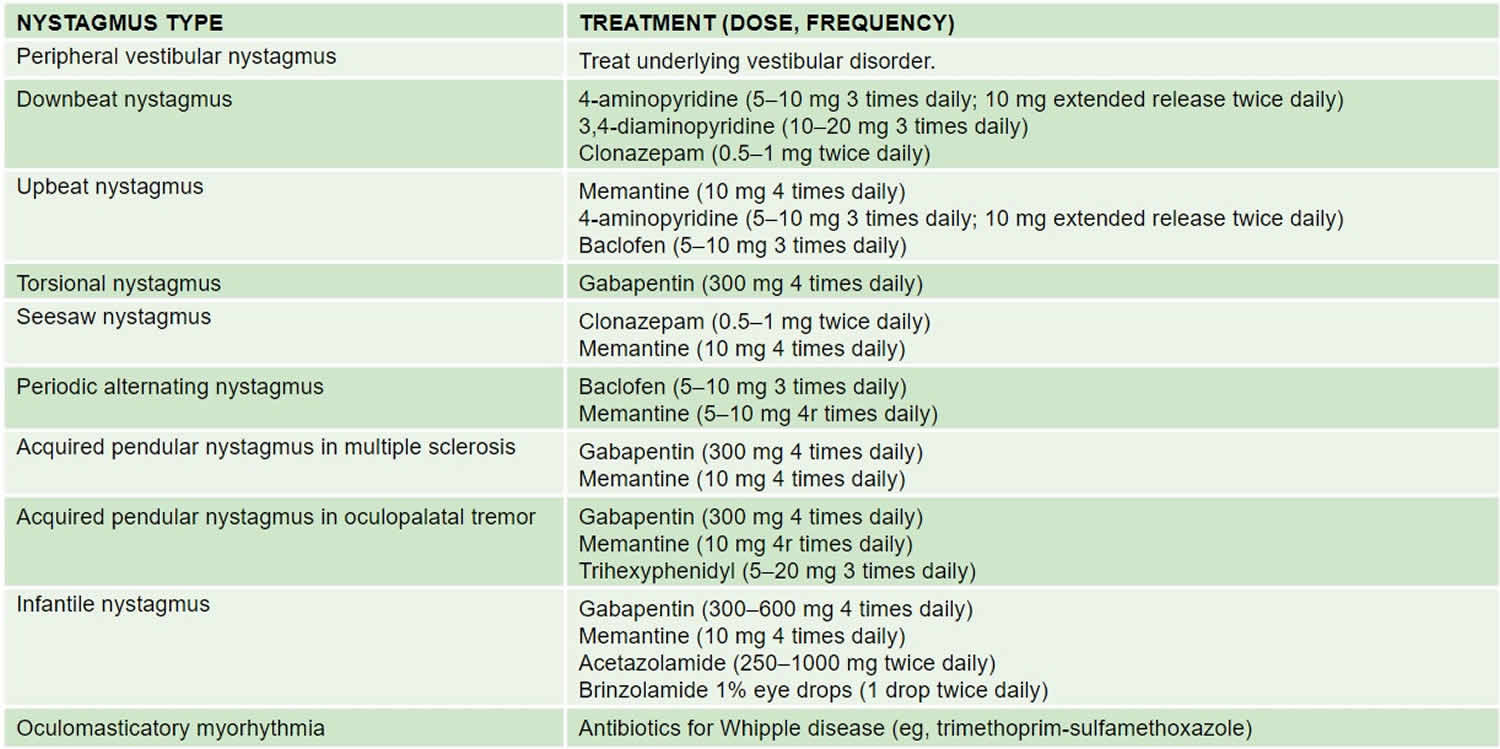
See the following summary of recommended pharmacologic treatment for the various clinical types of nystagmus 28. Note that none of these medications have been studied in children.
Table 4. Medications for nystagmus
Botulinum Toxin Injection
Trials of botulinum toxin injection into the retrobulbar space have been done to treat symptomatic nystagmus. While some patients reported improvement in oscillopsia 47, side effects including ptosis, diplopia, and paradoxical worsening of oscillopsia due to limitation of VOR 48 have limited the utility of botulinum toxin as a treatment option.
Optical Treatments
Correction of refractive error, which can be high in patients with nystagmus, is required 49. The use of contact lenses may be particularly useful in infantile nystagmus 50. Traditional amblyopia therapy may be employed in cases of latent nystagmus. If the nystagmus dampens with convergence (such as infantile idiopathic nystagmus and monocular nystagmus of childhood, base-out prism to induce convergence may help 51.
A prototype of an electro-optical, portable, image-shifting device has been developed to treat pendular nystagmus 52. The utility and efficacy of the device is unknown.
Surgery
Extraocular muscle surgery as a treatment for nystagmus is mostly for infantile nystagmus. The Anderson-Kestenbaum procedure mechanically shifts the null point from a horizontal cardinal position to primary position 53. An equivalent procedure may be performed for patients with vertical nystagmus 54. More recently, four-muscle tenotomy and reattachment without transposition has been found to be effective as well 55.
A case of a pilot, experimental intervention using magnetic oculomotor prosthesis has also been reported with objective improvement of visual acuity and reduction of acquired nystagmus 56.
- Nystagmus. http://eyewiki.org/Nystagmus[↩][↩][↩][↩]
- Sarvananthan N, Surendran M, Roberts EO, Jain S, Thomas S, Shah N, et al. The prevalence of nystagmus: the Leicestershire nystagmus survey. Invest Ophthalmol Vis Sci, 50 (2009), pp. 5201-5206[↩][↩]
- Nash DL, Diehl NN, Mohney BG. Incidence and Types of Pediatric Nystagmus. Am J Ophthalmol. 2017 Oct;182:31-34.[↩][↩]
- Ehrt O. Infantile and acquired nystagmus in childhood. Eur J Paediatr Neurol. 2012 Nov;16(6):567-72.[↩][↩]
- Büttner U, Kremmyda O. Smooth pursuit eye movements and optokinetic nystagmus. Dev Ophthalmol. 2007;40:76-89.[↩]
- Optokinetic Nystagmus Dysfunction. In: Basic and clinical science course (BCSC) Section 5: Neuro-Ophthalmology. Academy of Ophthalmology; 2015:192-193[↩][↩]
- Golia AG, Pawar M. The diagnosis of brain death. Indian J Crit Care Med. 2009 Jan-Mar; 13(1): 7–11.[↩]
- Howard IP, Zacher JE, Allison RS. Post-rotatory nystagmus and turning sensations after active and passive turning. J Vestib Res. 1998 Jul-Aug;8(4):299-312[↩]
- Papageorgiou E, McLean RJ, Gottlob I. Nystagmus in childhood. Pediatr Neonatol. 2014 Oct;55(5):341-51.[↩][↩][↩]
- Abadi RV, Dickinson CM. Waveform characteristics in congenital nystagmus. Doc Ophthalmol, 64 (1986), pp. 153-167[↩]
- LeeAG, BrazisPW. Localizing forms of nystagmus: symptoms, diagnosis, and treatment. Curr Neurol Neurosci Rep. 2006;6:414–420.[↩][↩]
- Schlindwein P, Schreckenberger M, Dieterich M. Visual-motion suppression in congenital pendular nystagmus. Ann New York Acad Sci, 1164 (2009), pp. 458-460. Basic and Clinical Aspects of Vertigo and Dizziness[↩][↩]
- Cham KM, Anderson AJ, Abel LA. Factors influencing the experience of oscillopsia in infantile nystagmus syndrome. Invest Ophthalmol Vis Sci. 2008 Aug;49(8):3424-31.[↩]
- Kerrison JB, Giorda R, Lenart TD, Drack AV, Maumenee IH. Clinical and genetic analysis of a family with X-linked congenital nystagmus (NYS1). Ophthalmic Genet, 22 (2001), pp. 241-248[↩][↩]
- Infantile Nystagmus Syndrome. In: Basic and clinical science course (BCSC) Section 5: Neuro-Ophthalmology. Academy of Ophthalmology; 2015:229.[↩][↩][↩]
- Thomas S, Proudlock FA, Sarvananthan N, Roberts EO, Awan M, McLean R, et al. Phenotypical characteristics of idiopathic infantile nystagmus with and without mutations in FRMD7. Brain, 131 (2008), pp. 1259-1267[↩]
- L.F. Dell’Osso, R.B. Daroff. Congenital nystagmus waveforms and foveation strategy. Doc Ophthalmol, 39 (1975), pp. 155-182[↩]
- Simonsz HJ, Kolling GH. Best age for surgery for infantile esotropia. Eur J Paediatr Neurol. 2011 May;15(3):205-8[↩][↩]
- Weissman BM, Dell’Osso LF, Abel LA, Leigh RJ. Spasmus nutans. A quantitative prospective study. Arch Ophthalmol. 1987;105:525–528.[↩]
- Kiblinger GD, Wallace BS, Hines M, Siatkowski RM. Spasmus nutans-like nystagmus is often associated with underlying ocular, intracranial, or systemic abnormalities. J Neuroophthalmol. 2007 Jun;27(2):118-22.[↩]
- Smith DE, Fitzgerald K, Stass-Isern M, Cibis GW. Electroretinography is necessary for spasmus nutans diagnosis. Pediatr Neurol. 2000 Jul;23(1):33-6.[↩]
- ElKamshoushy A, Sprunger DT. Recession of three muscles to reduce ocular oscillations in patients with Heimann-Bielschowsky phenomenon. J AAPOS. 2011 Feb;15(1):67-8[↩]
- Jacob FD, Ramaswamy V, Goez HR. Acquired monocular nystagmus as the initial presenting sign of a chiasmal glioma. Can J Neurol Sci. 2010 Jan;37(1):96-7.[↩]
- Toledano H, Muhsinoglu O, Luckman J, Goldenberg-Cohen N, Michowiz S. Acquired nystagmus as the initial presenting sign of chiasmal glioma in young children. Eur J Paediatr Neurol. 2015 Nov;19(6):694-700.[↩]
- Ropper AH, Samuels A, Kelin JP, Prasad S. Adams and Victor’s Principles of Neurology. 2015. Ch 13: Disorders of Ocular Movement and Pupillary Function.[↩]
- Udaka YT, Shayan K, Chuang NA, Crawford JR. Atypical presentation of atypical teratoid rhabdoid tumor in a child. Case Rep Oncol Med. 2013;815923.[↩]
- Espinosa-Sanchez JM, Lopez-Escamez JA. Menière’s disease. Handb Clin Neurol. 2016;137:257-77.[↩][↩]
- Fong AMF. A Practical Approach to Nystagmus and Saccadic Oscillations. Focal Points by American Academy of Ophthalmology. 2014.[↩][↩][↩][↩][↩][↩][↩][↩]
- Strupp M, Kremmyda O, Adamczyk C, Böttcher N, Muth C, Yip CW, Bremova T. Central ocular motor disorders, including gaze palsy and nystagmus. J Neurol. 2014 Sep;261 Suppl 2:S542-58.[↩]
- Acquired Pendular Nystagmus. In: Basic and clinical science course (BCSC) Section 5: Neuro-Ophthalmology. Academy of Ophthalmology; 2015:237[↩][↩]
- Averbuch-Heller L, Tusa RJ, Fuhry L, Rottach KG, Ganser GL, Heide W, Bu¨ttner U, Leigh RJ. A double-blind controlled study of gabapentin and baclofen as treatment for acquired nystagmus. Ann Neurol. 1997;41:818–825[↩]
- Claassen J, Spiegel R, Kalla R, Faldon M, Kennard C, Danchaivijitr C, Bardins S, Rettinger N, Schneider E, Brandt T, Jahn K, Teufel J, Strupp M, Bronstein A. A randomised double-blind, cross-over trial of 4-aminopyridine for downbeat nystagmus–effects on slow phase eye velocity, postural stability, locomotion and symptoms. J Neurol Neurosurg Psychiatry. 2013 Dec; 84(12):1392-9.[↩]
- Helmchen C, Sprenger A, Rambold H, Sander T, Kompf D, Straumann D. Effect of 3,4-diaminopyridine on the gravity dependence of ocular drift in downbeat nystagmus. Neurology. 2004;63:752–753[↩]
- Thurtell MJ, Leigh RJ. Therapy for nystagmus. J Neuroophthalmol. 2010 Dec;30(4):361-71.[↩]
- Tilikete C, Milea D, Pierrot-Deseilligny C. Upbeat nystagmus from a demyelinating lesion in the caudal pons. J Neuroophthalmol. 2008 Sep;28(3):202-6.[↩]
- Sibony PA, Evinger C, Manning KA. Tobacco-induced primary-position upbeat nystagmus. Ann Neurol. 1987 Jan;21(1):53-8.[↩]
- Davies-Thompson J, Scheel M, Jane Lanyon L, Sinclair Barton JJ. Neuropsychologia. 2013 Jun;51(7):1260-72. Functional organisation of visual pathways in a patient with no optic chiasm.[↩]
- Bergin DJ, Halpern J. Congenital see-saw nystagmus associated with retinitis pigmentosa.[↩]
- Hoyt CS, Gelbart SS. Vertical nystagmus in infants with congenital ocular abnormalities. Ophthalmic Paediatr Genet. 1984 Dec;4(3):155-61.[↩]
- Campbell WW Jr. Periodic alternating nystagmus in phenytoin intoxication. Arch Neurol. 1980 Mar;37(3):178-80.[↩]
- Jay WM, Williams BB, De Chicchis A. Periodic alternating nystagmus clearing after cataract surgery. J Clin Neuroophthalmol. 1985 Sep;5(3):149-52.[↩]
- Eggenberger E, Cornblath W, Stewart DH. Oculopalatal tremor with tardive ataxia. J Neuroophthalmol. 2001 Jun;21(2):83-6.[↩]
- Revilla FJ, de la Cruz R, Khardori N, Espay AJ. Teaching NeuroImage: Oculomasticatory myorhythmia: pathognomonic phenomenology of Whipple Disease. Neurology. 2008 Feb 5;70(6):e25.[↩]
- Ratnaike RN. Whipple’s disease. Postgrad Med J. 2000 Dec;76(902):760-6.[↩]
- Dell’Osso, R.B. Daroff. Congenital nystagmus waveforms and foveation strategy. Doc Ophthalmol, 39 (1975), pp. 155-182[↩]
- McLean R, Proudlock F, Thomas S, Degg C, Gottlob I. Congenital nystagmus: randomized, controlled, double-masked trial of memantine/gabapentin.Ann Neurol. 2007 Feb;61(2):130-8.[↩]
- Rucker JC. Current Treatment of Nystagmus. Curr Treat Options Neurol 2005;7:69-77[↩][↩]
- Acheson JF, Bentley CR, Shallo-Hoffmann J, Gresty MA. Dissociated effects of botulinum toxin chemodenervation on ocular deviation and saccade dynamics in chronic lateral rectus palsy. Br J Ophthalmol. 1998;82:67–71.[↩]
- Hertle RW. Examination and refractive management of patients with nystagmus. Surv Ophthalmol, 45 (2000), pp. 215-222[↩]
- Allen ED, Davies PD. Role of contact lenses in the management of congenital nystagmus. Br J Ophthalmol, 67 (1983), pp. 834-836[↩]
- Serra A, Dell’osso LF, Jacobs JB, Burnstine RA. Combined gaze-angle and vergence variation in infantile nystagmus: two therapies that improve the high-visual-acuity field and methods to measure it. Invest Ophthalmol Vis Sci. 2006; 47:2451–2460[↩]
- Smith RM, Oommen BS, Stahl JS. Image-shifting optics for a nystagmus treatment device. J Rehabil Res Dev. 2004 May;41(3A):325-36[↩]
- Kumar A, Shetty S, Vijayalakshmi P, Hertle RW. Improvement in visual acuity following surgery for correction of head posture in infantile nystagmus syndrome.J Pediatr Ophthalmol Strabismus. 2011 Nov-Dec;48(6):341-6.[↩]
- Taylor JN, Jesse K. Surgical management of congenital nystagmus. Aust N Z J Ophthalmol. 1987 Feb;15(1):25-34.[↩]
- Greven MA, Nelson LB. Four-muscle tenotomy surgery for nystagmus. Curr Opin Ophthalmol. 2014 Sep;25(5):400-5.[↩]
- Nachev P, Rose GE, Verity DH, Manohar SG, MacKenzie K, Adams G, Theodorou M, Pankhurst QA, Kennard C. Magnetic Oculomotor Prosthetics for Acquired Nystagmus. Ophthalmology. 2017 Oct;124(10):1556-1564.[↩]