Contents
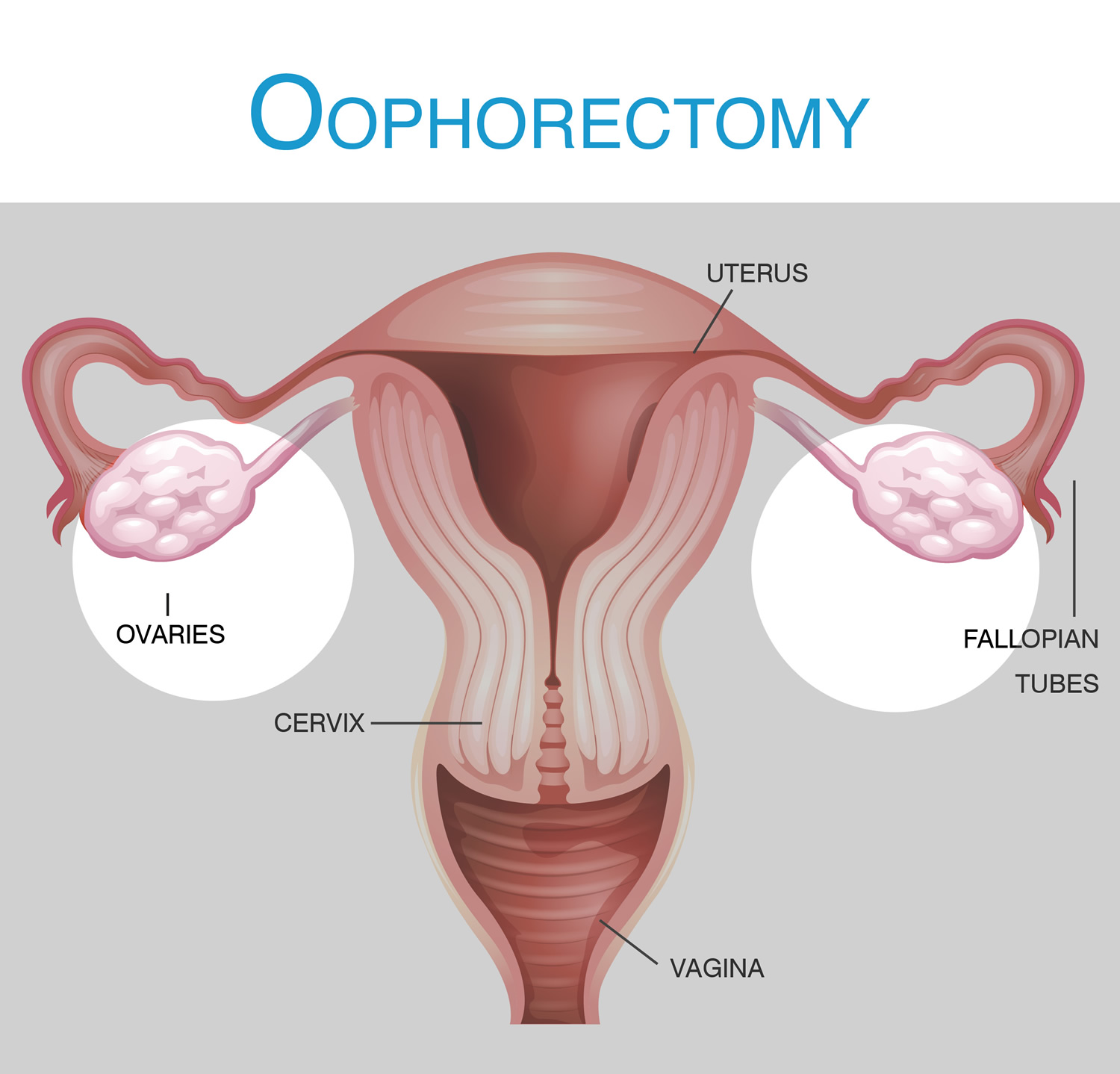
What is oophorectomy
Oophorectomy also called ovariectomy is a surgical procedure to remove one or both of your ovaries. Oophorectomy is usually performed to treat an ovarian cyst, ovarian cancer or some other problem related to the ovary. When the surgery involves removing only one ovary, it’s called unilateral oophorectomy. When an oophorectomy involves removing both ovaries, it’s called bilateral oophorectomy.
Why oophorectomy is done
Oophorectomy is usually performed to treat:
- an ovarian cyst
- ovarian torsion — the twisting of an ovary
- ovarian cancer
- endometriosis
- a tubo-ovarian abscess — a pus-filled pocket involving a fallopian tube and an ovary
- noncancerous (benign) ovarian tumors or cysts
- reducing the risk of ovarian cancer or breast cancer in those at increased risk
An ovarian cyst is a fluid-filled pocket in the ovary. There are different types of ovarian cysts. Most do not cause any problems, but some can turn out to be cancerous, meaning an oophorectomy may be necessary.
Large ovarian cysts can become twisted. This painful condition, known as ovarian torsion, is a surgical emergency. The cyst or entire ovary may need to be removed.
Women with ovarian torsion usually experience sudden, severe, sharp pains in the lower abdomen, often with nausea and vomiting. If you have these symptoms it is important to see a doctor immediately or call your local emergency services number and ask for an ambulance.
Ovarian cancer occurs when some cells in the ovary start to grow abnormally and develop into cancer. Ovarian cancer is usually treated with a type of surgery known as a laparotomy, which involves making a long cut in the abdomen. This allows for the ovaries, fallopian tubes and other organs, if they have been affected, to be removed.
Some women have a high family risk of developing ovarian cancer. If so, they may even choose to have their ovaries and fallopian tubes removed to reduce their risk.
Oophorectomy may also be used to treat endometriosis if other treatments have not worked. Endometriosis is a condition where the tissue lining of the uterus grows outside it. In severe cases, the uterus, ovaries and fallopian tubes may be removed.
Prophylactic oophorectomy
Preventive (prophylactic) surgery to remove the ovaries might be an option that people with a high risk of ovarian cancer and breast cancer to reduce their risk. Preventive bilateral oophorectomy (prophylactic oophorectomy) carries benefits and risks that must be carefully balanced when considering this procedure.
Prophylactic oophorectomy is usually reserved for those with:
Inherited gene mutations. People with a significantly increased risk of breast cancer and ovarian cancer due to an inherited mutation in the BRCA1 or BRCA2 gene — two genes linked to breast cancer, ovarian cancer and other cancers who have completed childbearing may consider this procedure.
- People with other inherited gene mutations that increase the risk of ovarian cancer, including those with Lynch syndrome, might also consider this procedure.
- Strong family history. Prophylactic oophorectomy may also be recommended if you have a strong family history of breast cancer and ovarian cancer but no known genetic alteration. It might also be recommended if you have a strong likelihood of carrying the gene mutation based on your family history but choose not to proceed with genetic testing.
Discuss your risk factors for breast cancer and ovarian cancer with your doctor. Your doctor may recommend that you see a genetic counselor to discuss your family history of cancer to help you decide whether you should consider genetic testing and which genes should be included in the testing.
How much can oophorectomy reduce the risk of cancer?
If you have a BRCA mutation, a prophylactic oophorectomy can reduce your:
- Breast cancer risk by up to 50 percent in premenopausal women. As an example, if a woman with a high risk of breast cancer had a 60 percent chance of being diagnosed with breast cancer at some point in her lifetime, bilateral oophorectomy could reduce her risk to 30 percent. Put another way, for every 100 women just like her, 60 could be expected to be diagnosed with breast cancer without oophorectomy. And 30 would be expected to be diagnosed with breast cancer after oophorectomy.
- Ovarian cancer risk by 80 to 90 percent. As an example, if a woman with a high risk of ovarian cancer had a 30 percent chance of being diagnosed with ovarian cancer at some point in her lifetime, oophorectomy could reduce her risk to 6 percent, assuming an 80 percent risk reduction. Put another way, for every 100 women just like her, 30 could be expected to be diagnosed with ovarian cancer without oophorectomy. And six would be expected to be diagnosed with ovarian cancer after oophorectomy.
In studies, the risk of breast cancer and ovarian cancer varies according to the particular gene mutations that you have. And your individual risk of breast cancer and ovarian cancer varies depending on many factors, including your age, your family history, your lifestyle choices and other strategies you’re using to reduce your risk of cancer.
For some, oophorectomy may offer great reduction in risk. For others, the risks of surgery and the potential side effects may not be worth the reduction in cancer risk.
Prophylactic oophorectomy might relieve much of your anxiety about developing cancer, but this type of surgery can also take an emotional toll on you. Even if you didn’t plan on having children, you might mourn the loss of your fertility.
Lingering risk of cancer
Prophylactic oophorectomy doesn’t completely eliminate your risk of breast cancer or ovarian cancer. A type of cancer that looks and acts identical to ovarian cancer can develop after the ovaries and fallopian tubes are removed. The risk of this type of cancer, called primary peritoneal cancer, is low — much lower than the lifetime risk of ovarian cancer if the ovaries remain intact.
Are there alternatives to oophorectomy for preventing ovarian cancer?
Researchers are studying other ways to reduce the risk of ovarian cancer in people who have a high risk of the disease. But these other ways of preventing ovarian cancer haven’t been proved to reduce risk as much as oophorectomy has. For this reason, most doctors recommend oophorectomy.
But oophorectomy isn’t right for everyone with a high risk of breast cancer or ovarian cancer. So talk about the alternatives with your doctor to better understand how they may affect your risk. Options include:
- Increased screening for ovarian cancer. You may choose to have ovarian cancer screening once or twice each year to look for early signs of cancer. Screening usually includes a blood test for cancer antigen (CA) 125 and an ultrasound exam of your ovaries. In theory, increased screening should be able to help doctors catch ovarian cancer at its earliest stages, but whether that’s possible with current screening methods isn’t clear. Screening tests are noninvasive, but there’s no evidence that they save lives.
Birth control pills. Studies suggest that taking birth control pills reduces the risk of ovarian cancer in average-risk women. There is good evidence that birth control pills can also be beneficial in high-risk women, such as those with BRCA mutations. There is concern that newer birth control pill formulations are associated with a very small increase in the risk of breast cancer. However, the benefits of reducing ovarian cancer risk seem to outweigh the small risk of breast cancer.
Doesn’t mastectomy offer a greater reduction in breast cancer risk?
Yes. Surgery to remove your breasts (bilateral mastectomy) may reduce your risk of breast cancer by 90 percent. As an example, if your risk of developing breast cancer at some point in your lifetime is 50 percent, a preventive mastectomy may lower your risk to 5 percent.
Put another way, for every 100 women with that same level of risk who undergo preventive mastectomy, five could be diagnosed with breast cancer at some point in their lives.
Why might a person opt for oophorectomy over mastectomy?
Reasons you might choose oophorectomy over mastectomy include:
- Oophorectomy reduces your risk of two cancers. For those that haven’t yet experienced menopause, oophorectomy reduces the risk of breast cancer and ovarian cancer, while mastectomy reduces only the risk of breast cancer.
- There aren’t many options for preventing ovarian cancer. Ovarian cancer is sometimes seen as a greater threat than breast cancer because it isn’t easily detected, and it may be detected at a later stage when diagnosed. While there’s no proven method for finding ovarian cancer at an early stage, there are tests, such as mammograms and breast MRIs, to detect breast cancer at an early stage in very high-risk women.
- Removing your ovaries doesn’t affect your appearance. Some women are concerned about how they’ll look if they have their breasts removed. Oophorectomy won’t affect your appearance.
These benefits have to be balanced against the risks of oophorectomy and the early menopause that occurs as a result.
Oophorectomy surgery risks and side effects
An oophorectomy is a relatively safe procedure. However, with any surgical procedure, there are risks involved. The risk of complications depends on how the procedure is performed.
Complications that may occur during or after an oophorectomy include:
- bleeding
- infection
- damage to nearby organs such as your bowel, bladder or blood vessels
- developing a hernia near one of the cuts
- surgical emphysema
- damage to a ureter
- having a small part of the ovary left behind, which could cause problems and be painful, such as pelvic pain, in premenopausal women (ovarian remnant syndrome)
- rupture of a tumor, spreading potentially cancerous cells
- inability to get pregnant on your own, if both ovaries are removed
But more concerning is the impact of losing the hormones supplied by your ovaries. If you have yet to undergo menopause, oophorectomy causes early menopause. Early menopause carries many risks, including:
- Bone thinning (osteoporosis). Removing your ovaries reduces the amount of bone-building estrogen your body produces. This may increase your risk of a broken bone.
- Discomforts of menopause. Hot flashes, vaginal dryness, sexual problems, sleep disturbance and sometimes cognitive changes can occur during menopause. Removing your ovaries doesn’t mean you’ll immediately have these problems, but it does mean that any menopausal symptoms you develop will occur earlier and are more likely to reduce your quality of life than if they occurred during natural menopause.
- Increased risk of heart disease. Your risk of heart disease may increase if you have your ovaries removed.
Risks of premature menopause
If you haven’t undergone menopause, you will experience premature menopause if both ovaries are removed. This deprives the body of the hormones, such as estrogen and progesterone, produced in the ovaries, leading to complications such as:
- Menopause signs and symptoms, such as hot flashes and vaginal dryness
- Depression or anxiety
- Heart disease
- Memory problems
- Decreased sex drive
- Osteoporosis
- Premature death
Taking low doses of hormone replacement drugs after surgery and until about age 50 may reduce the risk of these complications. But hormone replacement therapy has risks of its own. Discuss your options with your doctor.
Do you need postmenopausal hormone therapy after oophorectomy?
Use of low-dose hormone therapy after oophorectomy is controversial. While studies have shown that use of hormone therapy after menopause may increase the risk of breast cancer, other studies suggest early menopause can cause its own serious risks.
Women who undergo prophylactic oophorectomy and don’t use hormone therapy up to age 45 have a higher rate of premature death, heart disease and neurological diseases. For this reason, doctors typically recommend that younger women who have surgically induced menopause should consider taking low-dose hormone therapy for a short time and stop around age 51.
It isn’t entirely clear what effect hormone therapy might have on your cancer risk. Several studies have found that short-term hormone therapy doesn’t increase the risk of breast cancer in those with BRCA mutations who have undergone prophylactic oophorectomy. Ask your doctor about your particular situation. If you decide to take low-dose estrogen, plan to discontinue this treatment around age 51.
You may opt to have your uterus removed during your oophorectomy surgery so that you can take a type of hormone therapy (estrogen-only hormone therapy) that may be safer for those with a high risk of breast cancer. Discuss the benefits and risks of hysterectomy with your surgeon.
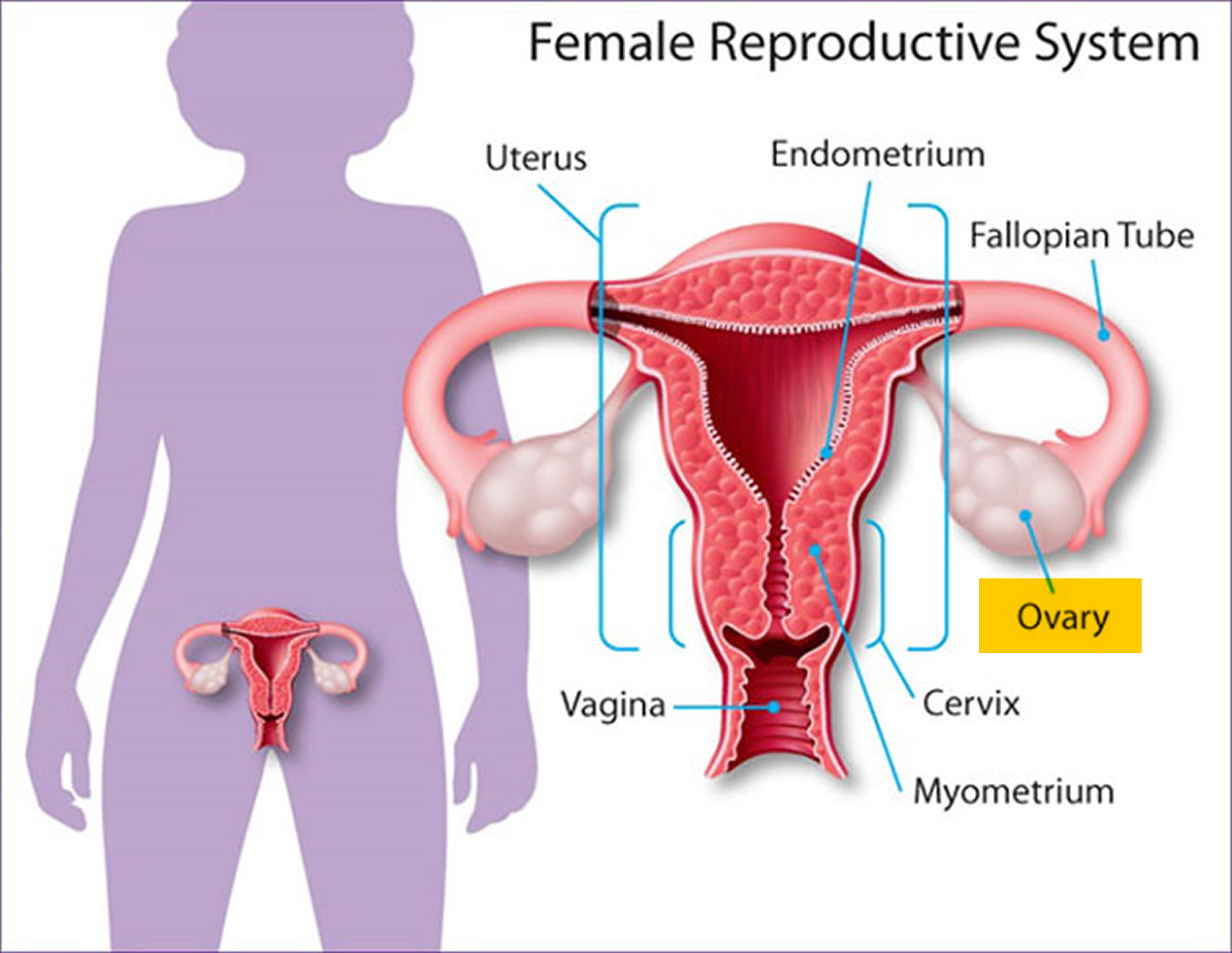
What are ovaries
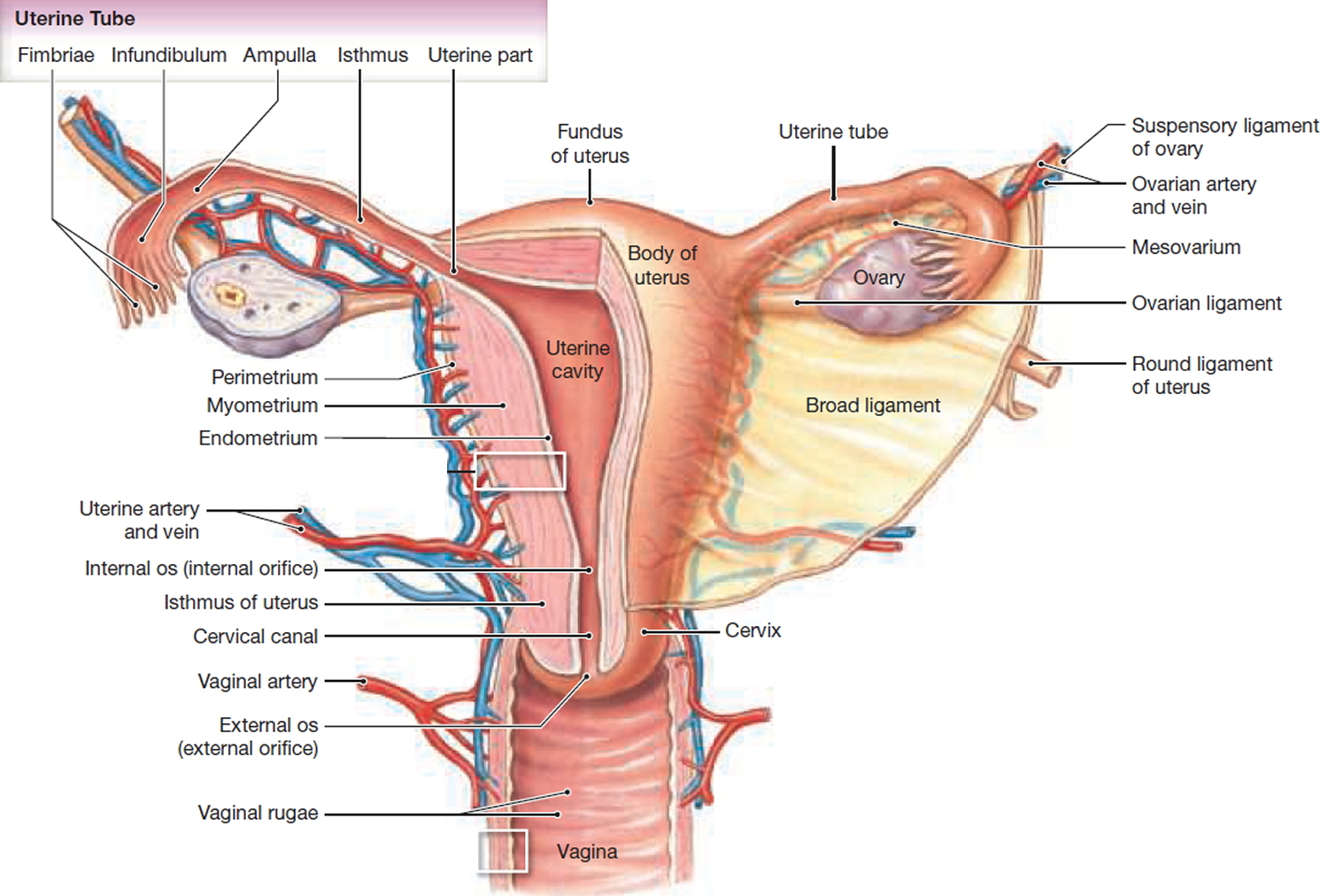
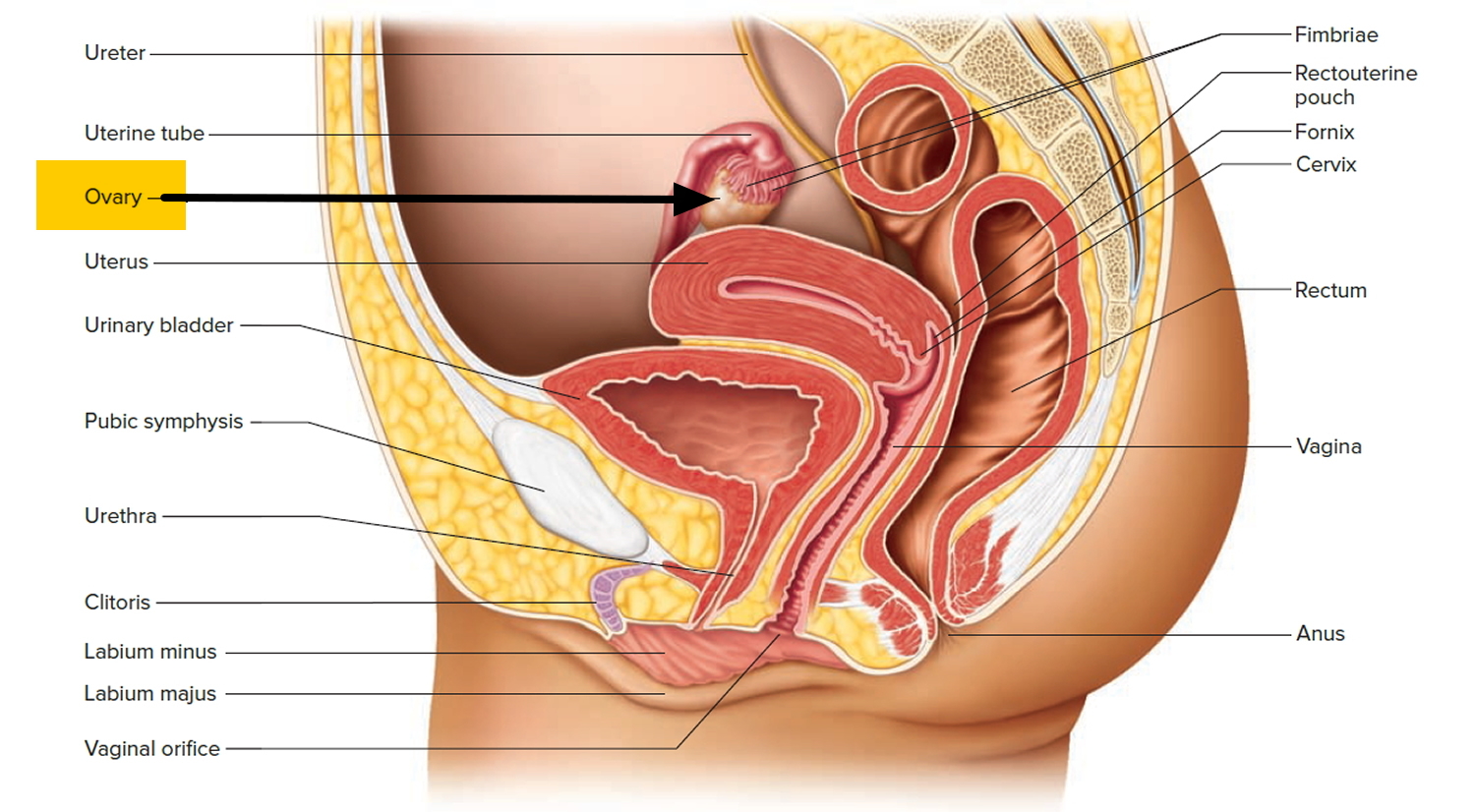
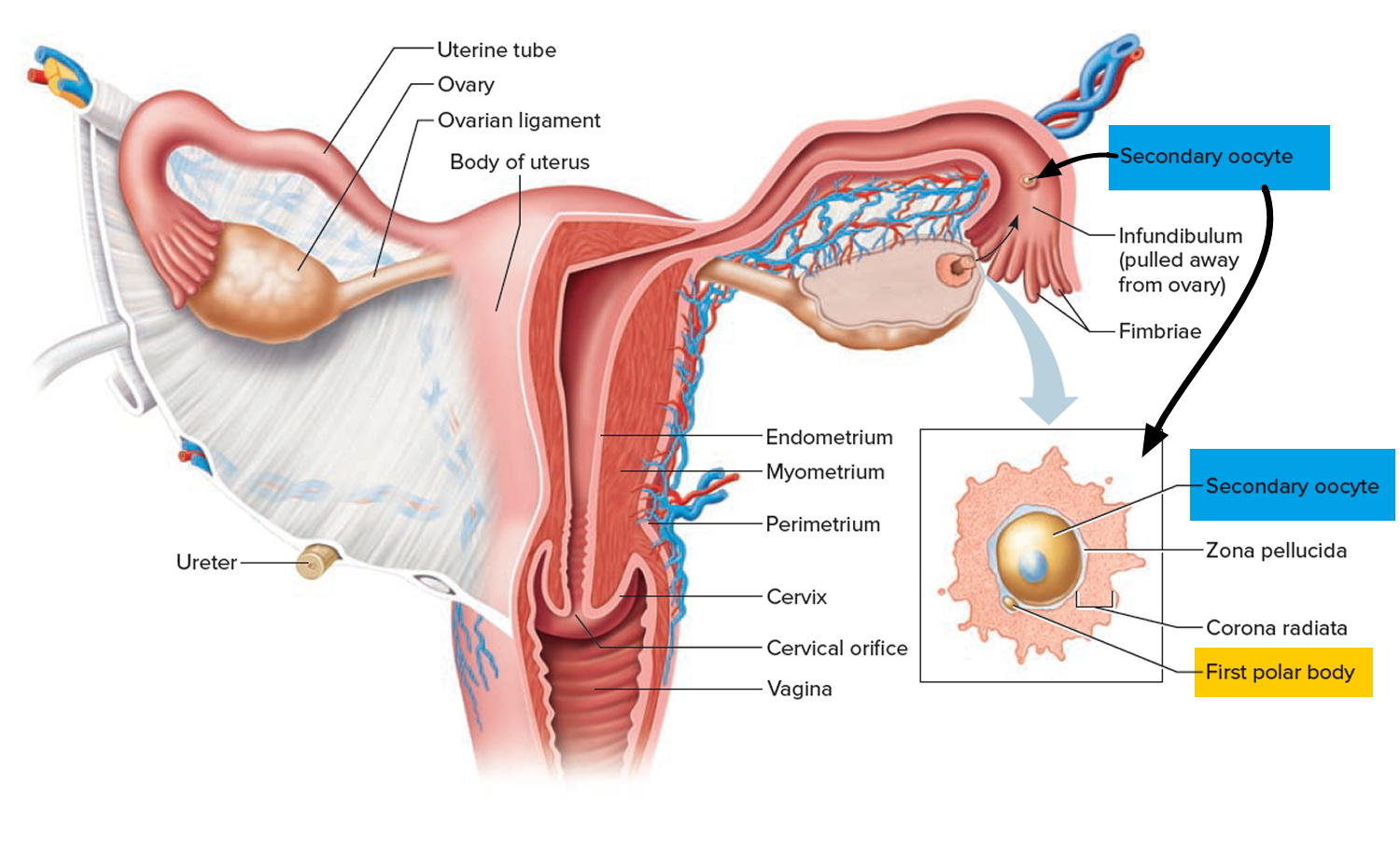
The ovaries are a pair of female reproductive glands in which the ova, or eggs, are formed. The two ovaries are solid, ovoid structures, each about 3.5 centimeters long, 2 centimeters wide, and 1 centimeter thick. The ovaries lie in shallow depressions in the lateral wall of the pelvic cavity one on each side of the uterus (see Figure 2).
Baby girls are born with all the egg cells in their ovaries that they will have in their lifetime 1. These egg cells lie in small pockets called follicles. Once puberty starts, different hormones ripen the first follicle so that it will release an egg cell (ovum). In addition to their role in producing ova, the ovaries also have the distinction of being an endocrine gland because they secrete hormones—primarily estrogen and progesterone—that are vital to normal reproductive development and fertility. Hormones are substances produced by the body that act as chemical transmitters. They regulate body functions like the menstrual cycle and body temperature. Hormones also trigger ovulation and promote the healthy development of female sex characteristics during puberty and to ensure fertility.
Progesterone and estrogen are necessary to prepare the uterus for menstruation, and their release is triggered by the hypothalamus.
Once you reach puberty, the ovaries release a single egg each month (the ovaries typically alternate releasing an egg)—this is called ovulation. The hypothalamus sends a signal to the pituitary gland to release gonadotrophic substances (follicle stimulating hormone [FSH] and luteinizing hormone [LH]). These hormones are essential to normal reproductive function—including regulation of the menstrual cycle.
As the egg migrates down the fallopian tube, progesterone is released. It is secreted by a temporary gland formed within the ovary after ovulation called the corpus luteum. Progesterone prepares the body for pregnancy by causing the uterine lining to thicken. If a woman is not pregnant, the corpus luteum disappears.
If a woman is pregnant, the pregnancy will trigger high levels of estrogen and progesterone, which prevent further eggs from maturing. Progesterone is secreted to prevent uterine contractions that may disturb the growing embryo. The hormone also prepares the breasts for lactation.
Increased estrogen levels near the end of pregnancy alert the pituitary gland to release oxytocin, which causes uterine contractions. Before delivery, the ovaries release relaxin, which as the name suggests, loosens the pelvic ligaments in preparation for labor.
More hormones are released during pregnancy than at any other time of a woman’s life, but during menopause—which marks the end of fertility—estrogen levels fall fast. This can lead to a range of complications.
Figure 1. Female reproductive system
Figure 2. The ovaries lie in shallow depressions in the lateral wall of the pelvic cavity
Function of the ovaries
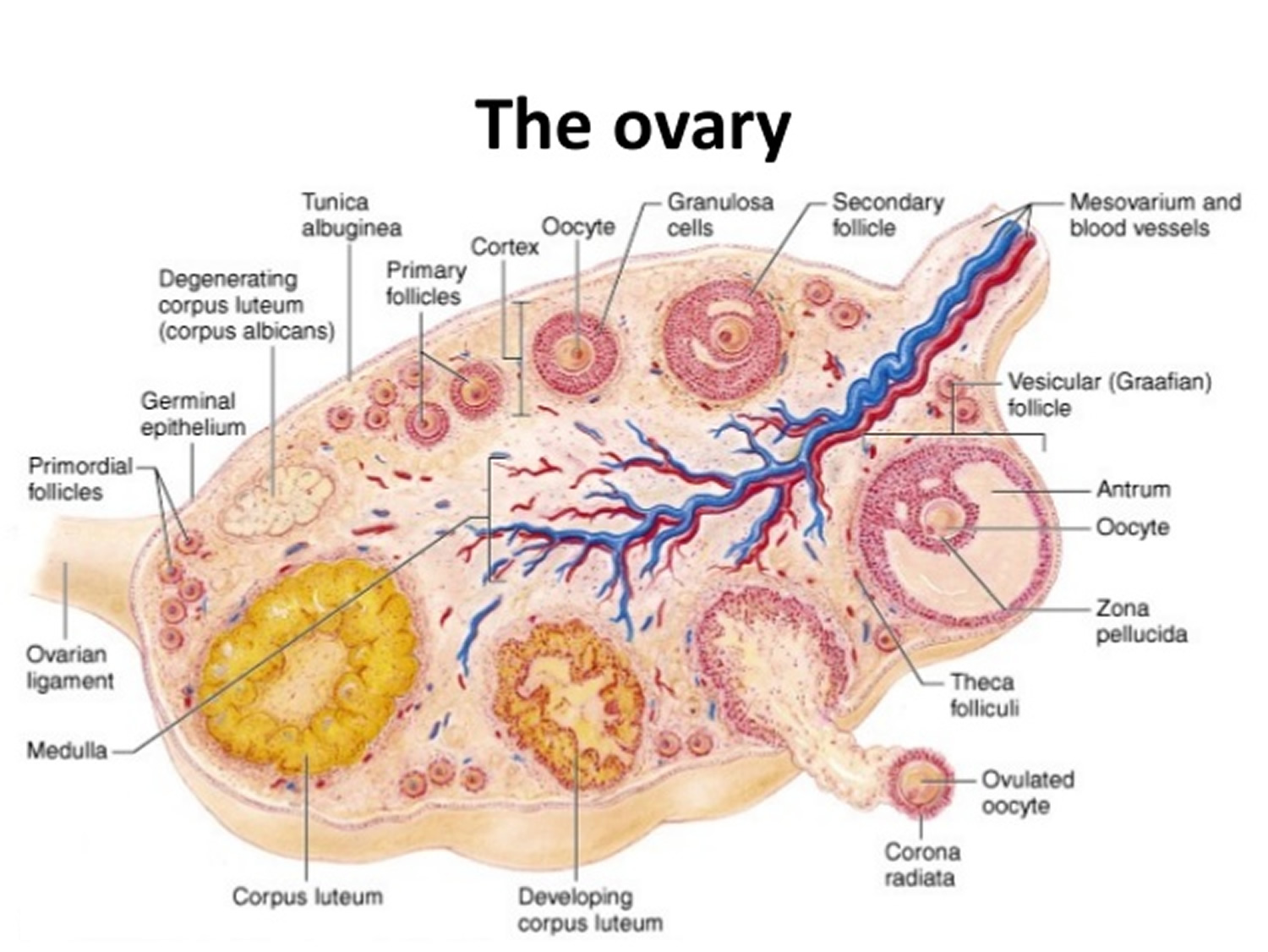
Ovarian tissues are divided into two indistinct regions—an inner medulla and an outer cortex. The ovarian medulla is mostly composed of loose connective tissue and contains many blood vessels, lymphatic vessels, and nerve fibers. The ovarian cortex consists of more compact tissue and has a granular appearance due to tiny masses of cells called ovarian follicles (see Figure 3). A layer of cuboidal epithelium covers the ovary’s free surface. Just beneath this epithelium is a layer of dense connective tissue.
Primordial Follicles
During prenatal development of a female, small groups of cells in the outer region of the ovarian cortex form several million primordial follicles. Each follicle consists of a single, large cell, called a primary oocyte, surrounded by epithelial cells called follicular cells.
Early in development, the primary oocytes begin to undergo meiosis, but the process soon halts and does not continue until the individual reaches puberty. Once the primordial follicles appear, no new ones form. Instead, the number of primary oocytes in the ovary steadily declines as many of the primary oocytes degenerate. Of the six to seven million primary oocytes that formed in the embryonic ovary, only a million or so remain at birth, and perhaps 300,000 are present at puberty. Of these, probably fewer than 300 to 400 oocytes will be released from the ovary during a female’s reproductive life.
Figure 3. Ovary anatomy
Figure 4. Ovulation
Female Sex Hormones
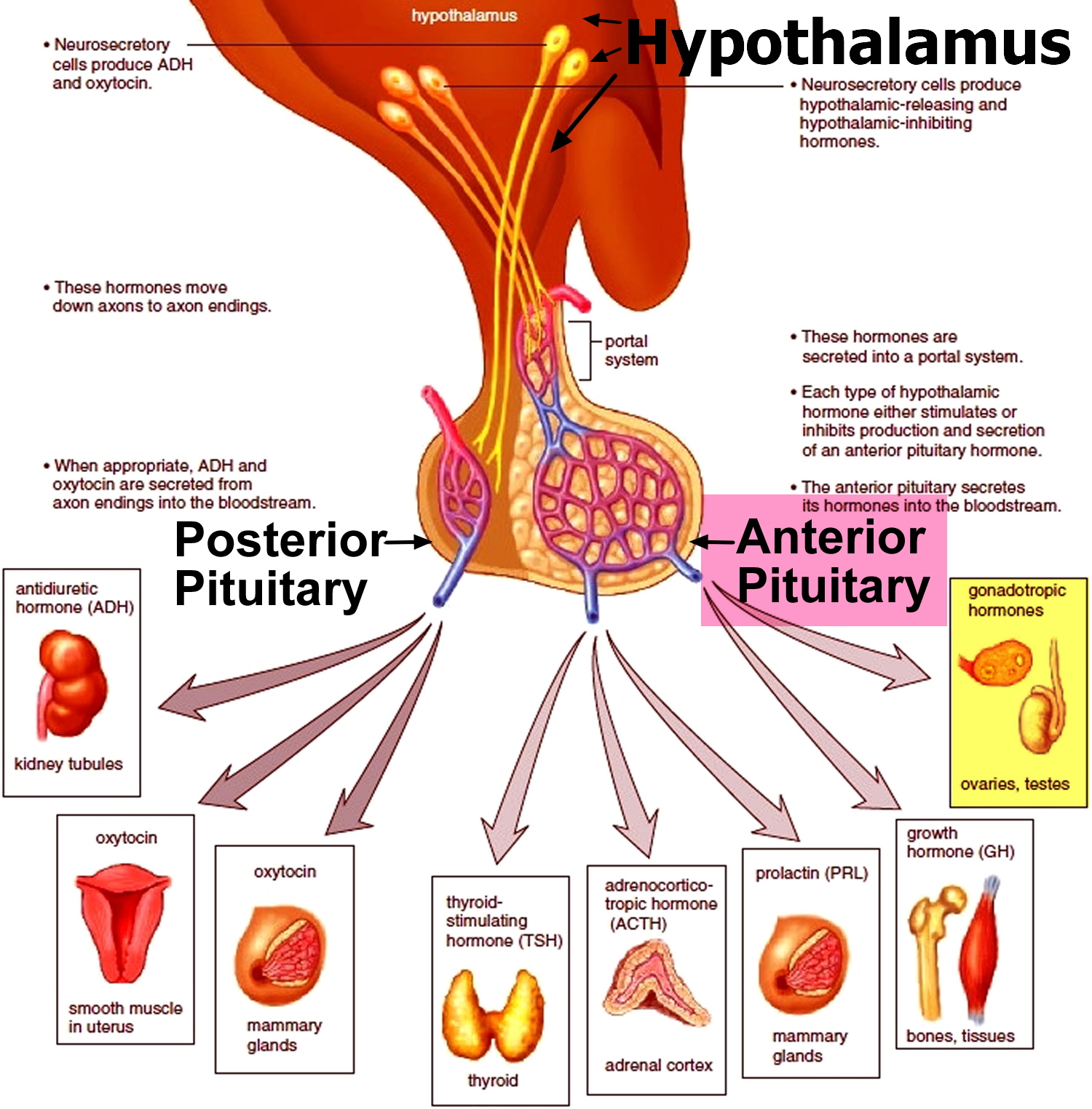
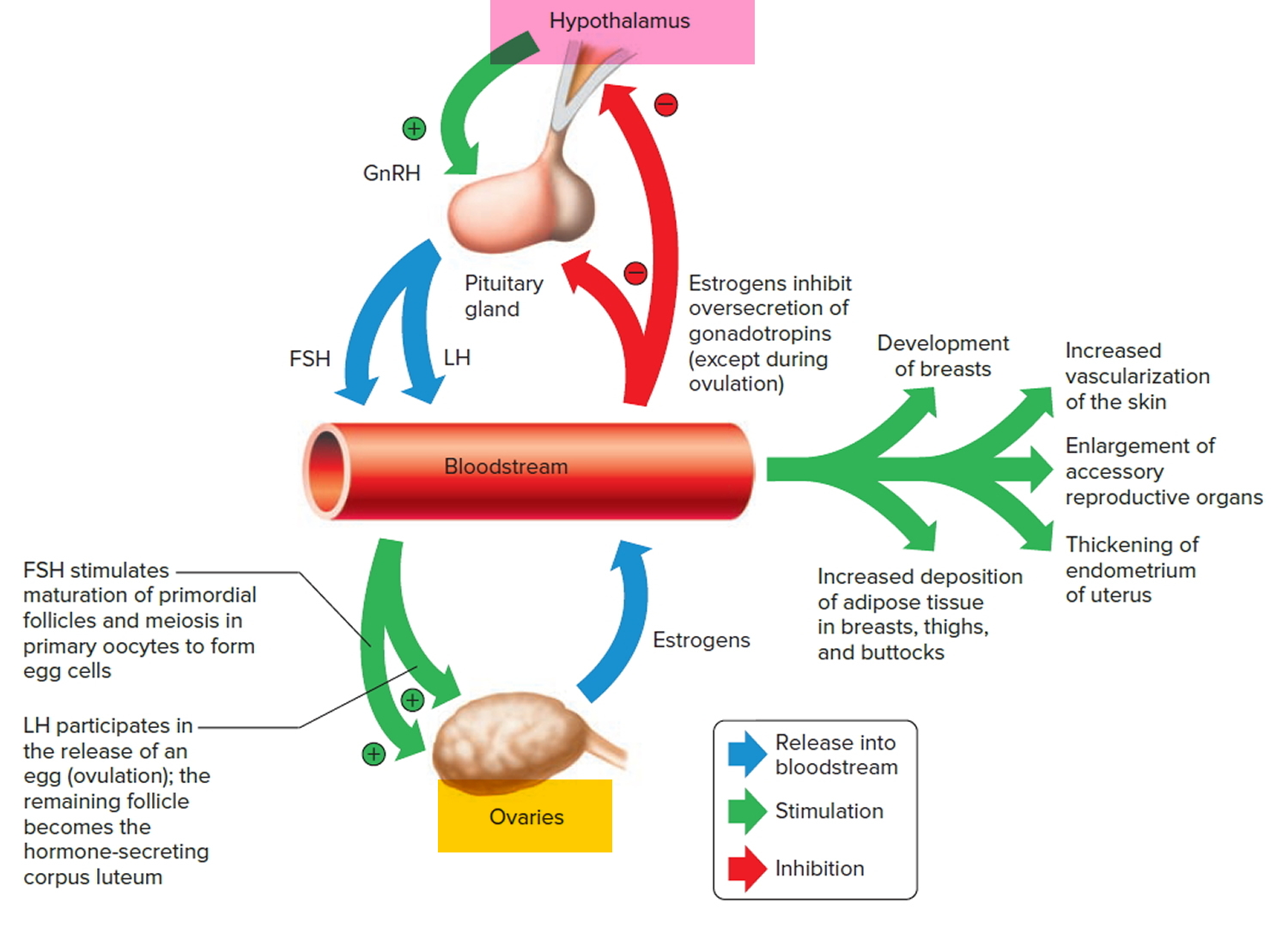
The female body is reproductively immature until about ten years of age. Then, the hypothalamus begins to secrete increasing amounts of Gonadotropin-releasing hormone (GnRH), which, in turn, stimulates the anterior pituitary to release the gonadotropins follicle-stimulating hormone (FSH) and luteinizing hormone (LH). These hormones play primary roles in controlling female sex cell maturation and in producing female sex hormones (Figure 5. Pituirary gland hormones).
The ovaries produce and release two groups of sex hormones—progesterone and estrogen 2. There are actually three major estrogens, known as estradiol, estrone, and estriol. Estradiol is the most abundant of the estrogens. These substances work together to promote the healthy development of female sex characteristics during puberty and to ensure fertility.
Several other tissues, including the adrenal cortices, and the placenta (during pregnancy), secrete female sex hormones —estrogens and progesterone, also.
However, the ovaries are the primary source of estrogens (in a nonpregnant female). At puberty, under the influence of the anterior pituitary, the ovaries secrete increasing amounts of estrogens. Estrogens stimulate enlargement of reproductive organs, including the vagina, uterus, uterine tubes, ovaries, and external reproductive structures.
Estrogen (estradiol, specifically) is instrumental in breast development, fat distribution in the hips, legs, and breasts, and the development of reproductive organs 2.
To a lesser extent, the ovaries release the hormone relaxin prior to giving birth. Another minor hormone is inhibin, which is important for signaling to the pituitary to inhibit follicle-stimulating hormone (FSH) secretion.
Figure 5. The Hypothalamus controlling the anterior lobe of the pituitary and the ovaries
Note: Note: The hypothalamus controls the production of an egg cell, ovulation of the egg cell, and development of the female secondary sex characteristics. Negative feedback among the hypothalamus, the anterior lobe of the pituitary, and the ovaries helps control the concentration of estrogens in the female body.
Estrogens also develop and maintain the female secondary sex characteristics, which include (Figure 6. Pituirary gland hormones):
- Development of the breasts and the ductile system of the mammary glands in the breasts.
- Increased deposition of adipose tissue in thesubcutaneous layer generally and in the breasts, thighs and buttocks particularly.
- Increased vascularization of the skin.
The ovaries are also the primary source of progesterone (in a nonpregnant female). This hormone promotes changes in the uterus during the female menstrual cycle, affects the mammary glands, and helps regulate the secretion of gonadotropins from the anterior pituitary gland.
[Androgens (male sex hormone) secreted by the adrenal gland cortices produce certain other changes in females at puberty. For example, increased hair growth in the pubic and axillary regions. Conversely, development of the female skeletal configuration, which includes narrow shoulders and broad hips, is a response to a low androgen concentration.]Figure 6. Pituitary gland hormones under the influence of the hypothalamus controlling the ovaries production of egg cell, ovulation and development of the female secondary sex characteristics
Menstrual Cycle
The menstrual cycle is characterized by regular, recurring changes in the endometrium, which culminate in menstrual bleeding (menses). Such cycles usually begin around age thirteen and continue into the early fifties, then cease.
A female’s first menstrual cycle, called menarche, occurs after the ovaries and other organs of the reproductive control system mature and begin responding
to certain hormones. Then, the hypothalamic secretion of gonadotropin-releasing hormone (GnRH) stimulates the anterior pituitary to release threshold levels of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Follicle-stimulating hormone (FSH) stimulates the final maturation of an ovarian follicle. The follicular cells produce increasing amounts of estrogens and some progesterone. Luteinizing hormone (LH) stimulates certain ovarian cells to secrete precursor molecules (such as testosterone), also used to produce estrogens.
In a young female, estrogens stimulate the development of secondary sex characteristics. Estrogens secreted during subsequent menstrual cycles continue the development and maintenance of these characteristics.
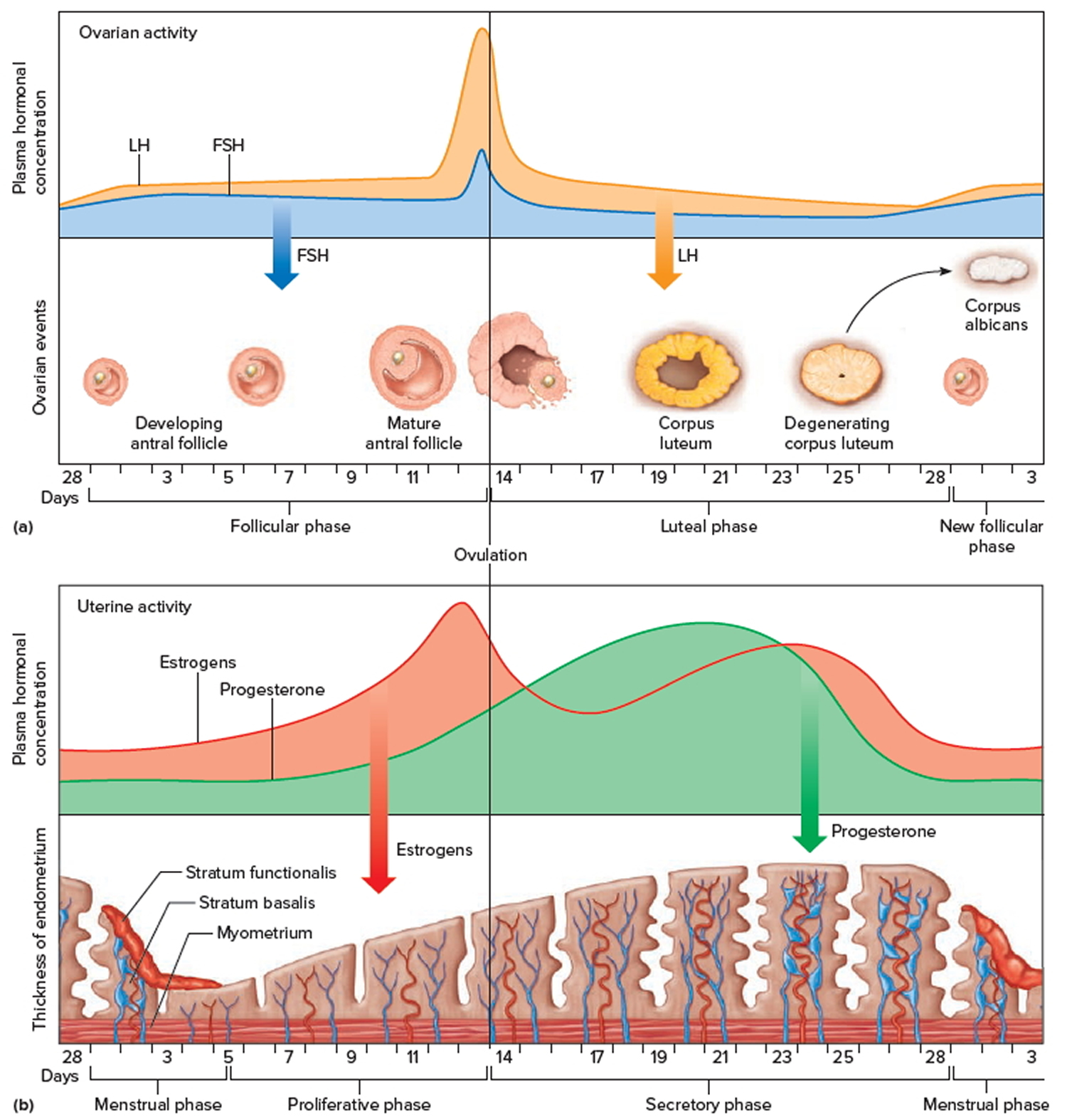
Figure 7. Ovarian activity during the Menstrual cycle
Note: Major events in the female menstrual cycle. (a) Plasma hormonal concentrations of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) affect follicle maturation in the ovaries. (b) Plasma hormonal concentrations of estrogen and progesterone influence changes in the uterine lining.
Increasing concentration of estrogens during the first week or so of a menstrual cycle changes the uterine lining, thickening the glandular endometrium (proliferative phase). Meanwhile, the follicle fully matures, and by around the fourteenth day of the cycle, the antral follicle appears on the ovary surface as a blisterlike bulge. Within the follicle, the follicular cells, which surround and connect the secondary oocyte to the inner wall, loosen. Follicular fluid accumulates.
While the follicle matures, it secretes estrogens that inhibit the release of luteinizing hormone (LH) from the anterior pituitary gland but allow luteinizing hormone (LH) to be stored in the gland. Estrogens also make anterior pituitary cells more sensitive to the action of gonadotropin-releasing hormone (GnRH), which is released from the hypothalamus in rhythmic pulses about ninety minutes apart.
Near the fourteenth day of follicular development, the anterior pituitary cells finally respond to the pulses of GnRH and release the stored LH. The resulting surge in LH concentration lasts about thirty-six hours. In response to the LH, the primary oocyte completes meiosis I. The LH also acts with FSH inducing complex interactions with prostaglandins, progesterone, plasmin, and proteolytic enzymes, leading to the weakening and rupturing of the bulging follicular wall. This event sends the secondary oocyte and follicular fluid out of the ovary (ovulation).
Following ovulation, the space containing the follicular fluid fills with blood, which soon clots. Under the influence of LH, the remnants of the follicle within the ovary form a temporary glandular structure in the ovary called a corpus luteum (“yellow body”).
Follicular cells secrete some progesterone during the first part of the menstrual cycle. During the second half of the cycle, cells of the corpus luteum secrete abundant progesterone and estrogens. Consequently, as a corpus luteum forms, the blood progesterone concentration sharply increases.
Progesterone causes the endometrium to become more vascular and glandular. It also stimulates the uterine glands to secrete more glycogen and lipids (secretory phase). The endometrial tissues fill with fluids containing nutrients and electrolytes, which provide a favorable environment for an embryo to develop.
High levels of estrogens and progesterone inhibit the anterior pituitary gland’s release of LH and FSH. Consequently, no other follicles are stimulated to complete development when the corpus luteum is active. However, if the secondary oocyte released at ovulation is not fertilized, the corpus luteum begins to degenerate (regress) on about the twenty-fourth day of the cycle. Eventually, connective tissue replaces it. The remnant of such a corpus luteum is called a corpus albicans, and is eventually absorbed.
When the corpus luteum ceases to function, concentrations of estrogens and progesterone rapidly decline, and in response, blood vessels in the endometrium constrict. This reduces the supply of oxygen and nutrients to the thickened endometrium (stratum functionalis and stratum basalis), and these lining tissues soon disintegrate and slough off. At the same time, blood leaves damaged capillaries, creating a flow of blood and cellular debris that passes through the vagina as the menstrual flow (menses). This flow usually begins about the twenty-eighth day of the cycle and continues for three to five days, while the concentrations of estrogens are relatively low. The beginning of the menstrual flow marks the end of a menstrual cycle and the beginning of the next cycle as a new developing antral follicle becomes available.
Low blood concentrations of estrogens and progesterone at the beginning of the menstrual cycle mean that the hypothalamus and anterior pituitary gland are no longer inhibited. Consequently, FSH and LH concentrations soon increase, stimulating a new antral follicle to mature. As this follicle secretes estrogens, the uterine lining undergoes repair, and the endometrium begins to thicken again.
Menopause
After puberty, menstrual cycles continue at regular intervals into the late forties or early fifties, when the ovaries start to produce less estrogen and progesterone. This results in the menstrual cycles becoming less predictable. Then, within a few months or years, the cycles cease. This period in life is called menopause or female climacteric.
Ovary removal surgery
How to prepare for the oophorectomy surgery
If you need to have an oophorectomy, you will probably meet with the surgeon and anesthetist before the operation to discuss the procedure. You will likely need to avoid drinking and eating for some hours before surgery. Your doctor will be able to advise you.
To prepare for an oophorectomy, your doctor may ask that you:
- Drink a solution to clear your intestines the day before surgery
- Stop eating the day before your surgery and limit liquids
- Stop taking certain medications
- Undergo imaging tests, such as ultrasound and computerized tomography (CT), to help surgeons plan for the procedure
Having both ovaries removed will result in menopause. If you were still having periods before surgery, they will stop immediately after. Knowing what will happen before an oophorectomy may help you feel more prepared to cope with the physical and emotional changes that will follow the surgery. You may also want to discuss with your doctor whether you will be able to become pregnant in the future.
Plan for a hospital stay
You may need to stay in the hospital for a few days after an oophorectomy. How long you stay depends on how the procedure is performed and the reason for your surgery. Ask your doctor what you can expect.
Plan ahead for time in the hospital by packing:
- A robe and slippers
- Personal items, such as your toothbrush
- Things to help you pass the time, such as books and magazines
Plan for infertility
If you want to have children, talk with your doctor about your options. For some conditions, you may need only one ovary removed (unilateral oophorectomy). With the remaining ovary, you’ll still have a menstrual cycle and conceive naturally.
If both of your ovaries are removed (bilateral oophorectomy), but your uterus remains, you may be able to become pregnant using assisted reproductive technology. Ask your doctor to refer you to a fertility specialist who can review your options with you.
What happens during the oophorectomy surgery?
Oophorectomy is usually performed under a general anesthetic so that you are asleep during the procedure. The surgeon will make a cut in your abdomen to remove your ovary.
An oophorectomy can be performed two ways:
- Laparotomy: In this surgical approach, the surgeon makes one long incision in your lower abdomen to access your ovaries. The surgeon separates each ovary from the blood supply and tissue that surrounds it and removes the ovary.
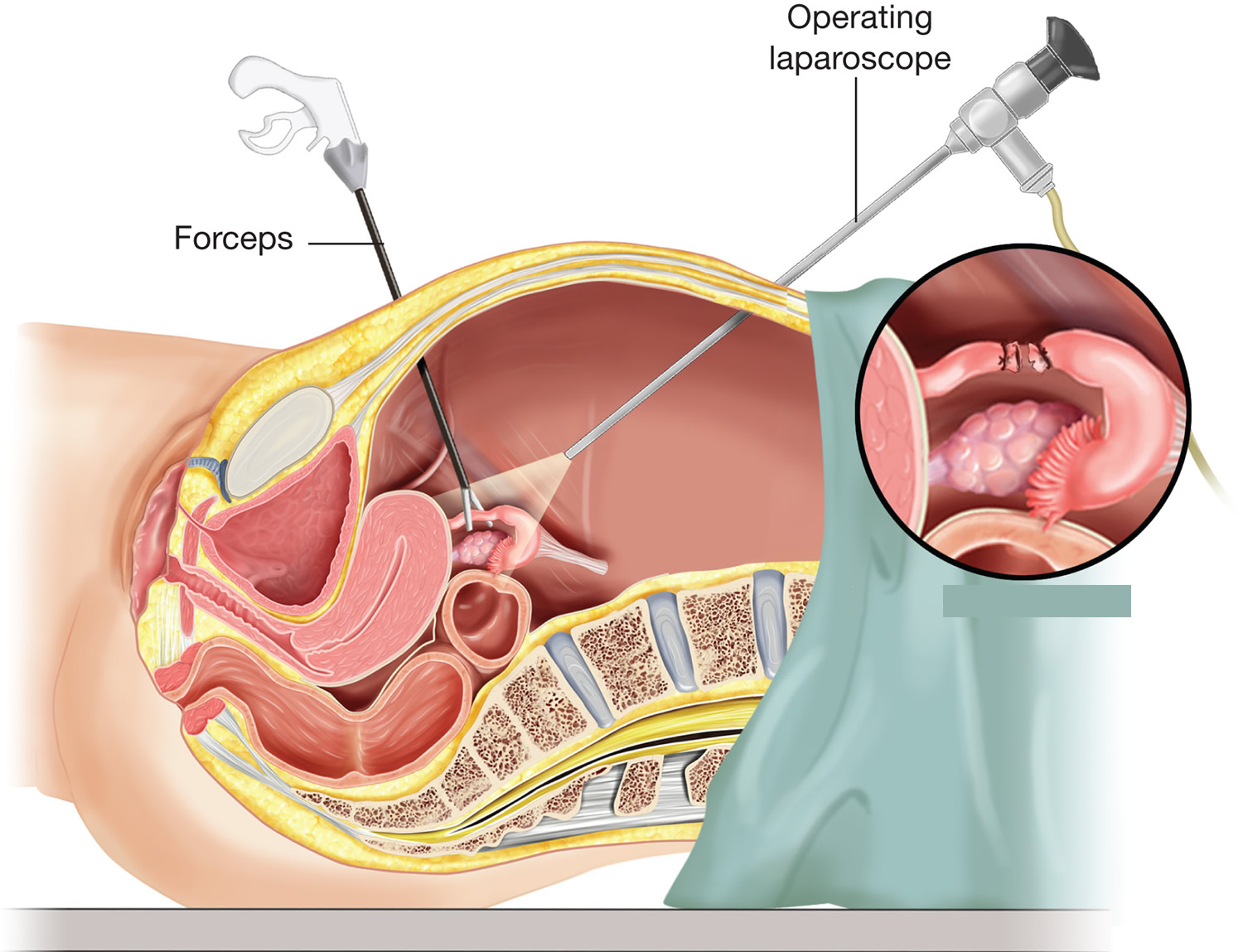
- Minimally invasive laparoscopic surgery: In this surgical approach, the surgeon makes three or four very small incisions in your abdomen. The surgeon inserts a tube with a tiny camera through one incision and special surgical tools through the others. The camera transmits video to a monitor in the operating room that the surgeon uses to guide the surgical tools. Each ovary is separated from the blood supply and surrounding tissue and placed in a pouch. The pouch is pulled out of your abdomen through one of the small incisions.
Laparoscopic oophorectomy may also be robotically assisted in certain cases. During robotic surgery, the surgeon watches a 3-D monitor and uses hand controls that allow finer movement of the surgical tools.
Whether your oophorectomy is an open, laparoscopic or robotic procedure depends on your situation. Laparoscopic or robotic oophorectomy usually offers quicker recovery, less pain and a shorter hospital stay. But these procedures aren’t appropriate for everyone, and in some cases, surgery that begins as laparoscopic may need to be converted to an open procedure during the operation.
Figure 5. Laparoscopic oophorectomy
Oophorectomy combined with other procedures
An oophorectomy can be done alone, but it is often done as part of a more-complete surgery to remove the uterus (hysterectomy) in women who have undergone menopause.
In those with an increased risk of ovarian cancer, an oophorectomy is commonly combined with surgery to remove the nearby fallopian tubes (salpingectomy) since they share a common blood supply with the ovaries. When combined, the procedure is called a salpingo-oophorectomy.
What to expect after the oophorectomy surgery
After an oophorectomy, you can expect to:
- Spend time in a recovery room as your anesthesia wears off
- Move to a hospital room where you may spend a few hours to a few days, depending on your procedure
- Get up and about as soon as you’re able in order to help your recovery
You might need to stay in hospital for a few days after an oophorectomy so you can recover. However, with laparoscopic oophorectomy you should be able to go home the same day. You may be given pain relief medication and advised on how to take care of your wound. You will probably be advised to avoid certain activities such as swimming or heavy lifting for a few weeks.
Ovary removal recovery time
How quickly you can go back to your normal activities after an oophorectomy depends on your situation, including the reason for your surgery and how it was performed.
Most people can return to full activity by six weeks after surgery. Those who undergo laparoscopic or robotic surgery may return to full activity sooner — as early as two weeks after surgery.
Discuss exercise, driving, sexual restrictions and overall activity level with your surgeon.
Call your doctor if you:
- Have a temperature of 101° F (38.3° C) or higher
- Have shortness of breath
- Have pain that doesn’t get better with pain medication
- Have increased redness around your incisions
- Have new or increased swelling around your incision
- Have discharge from your incision
- Have heavy vaginal bleeding
- Have swelling or tenderness in your calves or thighs
- Cough up blood
- Don’t have a bowel movement for 2 days or longer
- Have nausea or vomiting
- Have diarrhea (loose or watery bowel movements)
- Have any questions or concerns
How can I prevent constipation?
- Go to the bathroom at the same time every day. Your body will get used to going at that time. However, if you feel the urge to go, don’t put it off.
- Try to use the bathroom 5 to 15 minutes after meals. After breakfast is a good time to move your bowels. The reflexes in your colon are strongest at this time.
- Exercise, if you can. Walking is an excellent form of exercise.
- Drink 8 (8-ounce) glasses (2 liters) of liquids daily, if you can. Drink water, juices, soups, ice cream shakes, and other drinks that don’t have caffeine. Drinks with caffeine, such as coffee and soda, pull fluid out of the body.
- Slowly increase the fiber in your diet. Fruits, vegetables, whole grains, and cereals contain fiber. If you have an ostomy or have had recent bowel surgery, check with your doctor or nurse before making any changes in your diet.
- Both over-the-counter and prescription medications are available to treat constipation. Start with 1 of the following over-the-counter medications first:
- Docusate sodium (Colace) 100 mg. This is a stool softener that causes few side effects. Don’t take it with mineral oil.
- Polyethylene glycol (MiraLAX) 17 grams daily.
- Senna (Senokot) 2 tablets at bedtime. This is a stimulant laxative, which can cause cramping.
- If you haven’t had a bowel movement in 2 days, call your doctor or nurse.
When can I resume sexual activity?
Your doctor will tell you when you can resume sexual activity during your first follow-up visit after surgery. Don’t place anything in your vagina or have sex until your doctor says it’s okay.
When is it safe for me to drive?
You can start driving again 2 weeks after surgery, as long as you aren’t taking pain medication that may make you drowsy.
What exercises can I do?
Doing aerobic exercise, such as walking and stair climbing, will help you gain strength and feel better. Gradually increase the distance you walk. Climb stairs slowly, resting or stopping as needed.
Ask your doctor or nurse before starting more demanding exercises.
Will I be able to travel?
Yes, you can travel. If you’re traveling by plane within a few weeks after your surgery, make sure you get up and walk every hour. Be sure to stretch your legs, drink plenty of liquids, and keep your feet elevated when possible.
When can I return to work?
The time it takes to return to work depends on the type of work you do, the type of surgery you had, and how fast your body heals. Most people can return to work about 2 to 4 weeks after the surgery.
When can I lift heavy objects?
Ask your doctor when it’s safe for you to lift heavy objects after your surgery. Normally, you shouldn’t lift anything heavier than 5 to 10 pounds (2.27 to 4.5 kilograms) for at least 4 weeks after your surgery.
Bilateral salpingo oophorectomy
A bilateral salpingo-oophorectomy is a surgery to remove both your fallopian tubes and ovaries. You may be having a bilateral salpingo-oophorectomy for different reasons, such as you have an ovarian cyst or have a high chance of having ovarian cancer in the future. Your doctor will explain why you’re having the surgery.
After your surgery, you will stop menstruating (getting your period). You may experience normal symptoms of menopause, including night sweats, hot flashes, and vaginal dryness. If you’re in menopause or have already gone through it, you may still notice some of these symptoms. Talk with your doctor about ways to manage these symptoms.
You will also be infertile (unable to have biological children) after your surgery. If you would like to have biological children in the future, ask your doctor for a referral to a fertility nurse specialist.
You may have a dilation and curettage (D&C) after your salpingo-oophorectomy. This is a procedure that’s done so your surgeon can check for abnormal cells in your uterus.
During your dilation and curettage (D&C), your cervix will be dilated (opened) slightly. Your surgeon will put a tool called a curette through your cervix, into your uterus. They will use the curette to remove a small amount of tissue from the inside of your uterus.
Your surgeon may also want to look at the tissue lining the inside of your uterus to see if anything looks abnormal. This is called a hysteroscopy. During a hysteroscopy, your surgeon will insert a long, thin video camera through your cervix, into your uterus to examine the area.