Contents
What is parathyroid hormone
Parathyroid hormone (PTH) is a hormone made by the parathyroid gland that helps your body maintain stable levels of calcium in your blood. Also called parathormone and parathyrin, the parathyroid hormone (PTH) helps your body store and use calcium. It is part of a feedback loop that includes calcium, parathyroid hormone, vitamin D, and to some extent, phosphorus (phosphate) and magnesium. Conditions and diseases that disrupt this feedback loop can cause inappropriate elevations or decreases in calcium and parathyroid hormone levels and lead to symptoms of hypercalcemia or hypocalcemia. A higher-than-normal amount of parathyroid hormone (hyperparathyroidism) causes high levels of calcium in the blood and may be a sign of disease. A condition characterized by underactivity of the parathyroid glands and reduced production of parathyroid hormone (hypoparathyroidism), symptoms may include tingling in the fingers and toes, muscle aches and spasms, fatigue, dry skin and brittle nails, headaches, anxiety, and depression.
- As calcium levels begin to increase in the blood, parathyroid hormone normally decreases.
- A decrease in the ionized calcium in the blood is the stimulus for the parathyroid hormone secretion.
- Magnesium also influences the parathyroid hormone level. Hypermagnesemia suppress the parathyroid hormone secretion, although not like calcium.
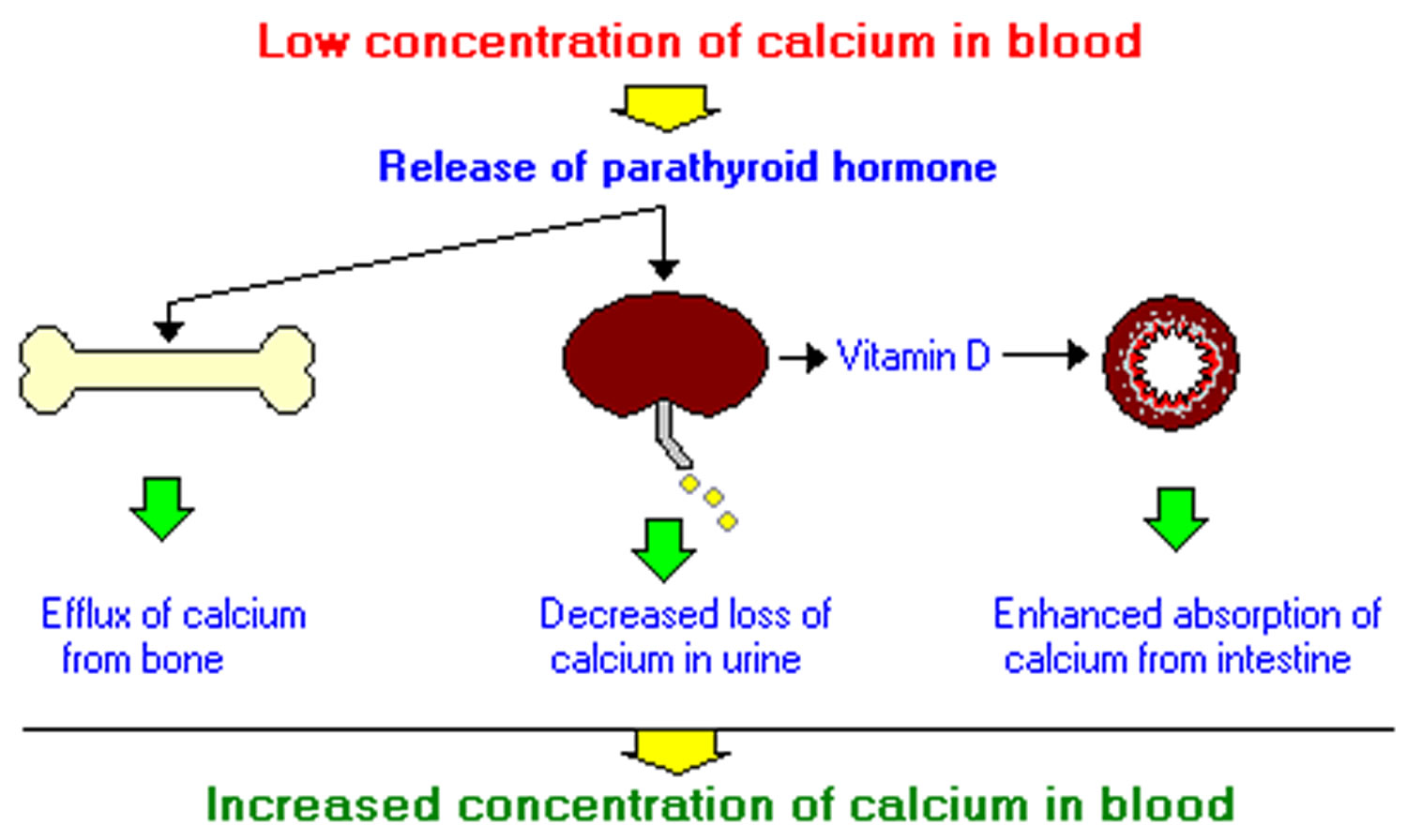
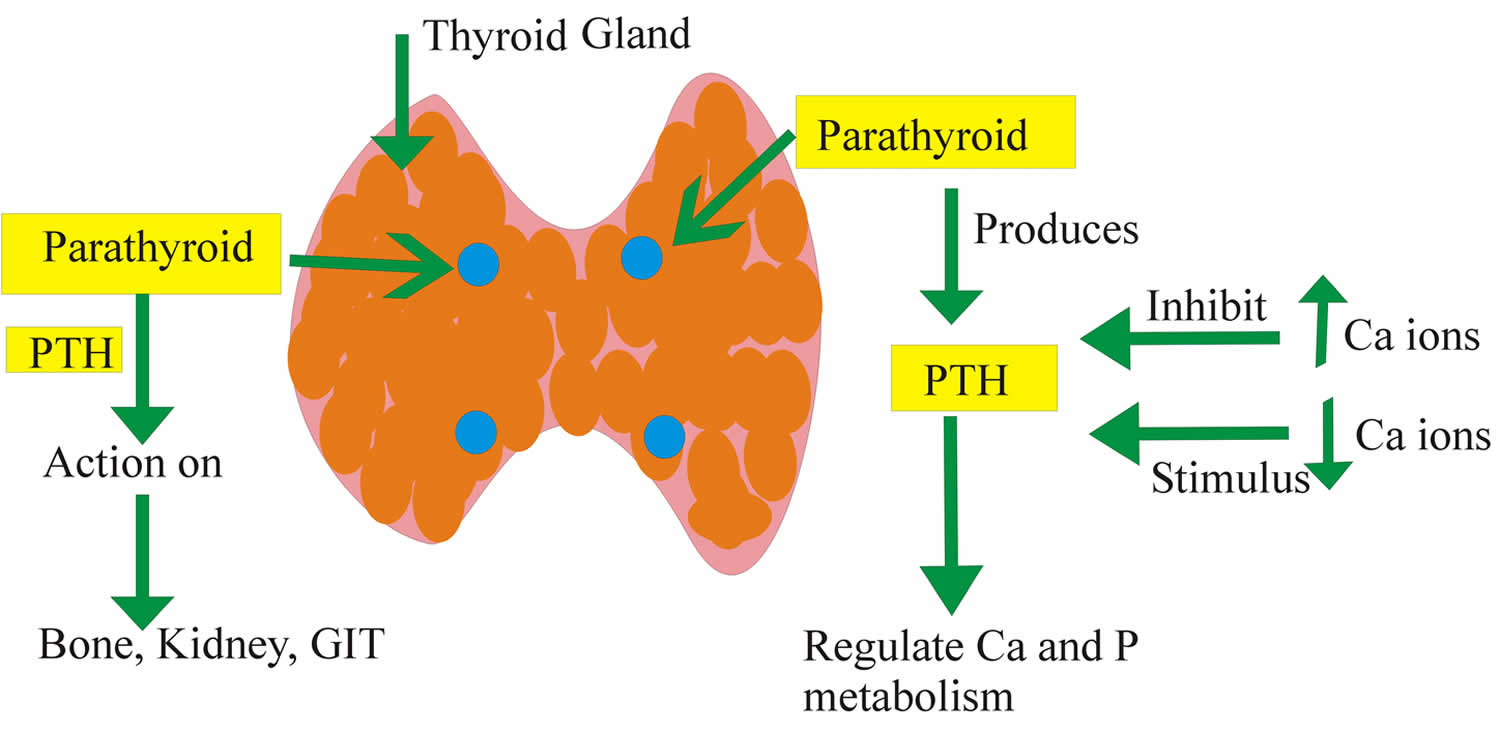
Parathyroid hormone is produced by four button-sized parathyroid glands that are located in the neck behind the thyroid gland. Normally, these glands secrete parathyroid hormone into the bloodstream in response to low blood calcium levels. The hormone works in three ways to help raise blood calcium levels back to normal:
- Parathyroid hormone promotes the release of calcium from bones into the bloodstream.
- Parathyroid hormone stimulates the kidneys to convert vitamin D from the inactive to the active form, which in turn increases the absorption of calcium from food in the intestines.
- Parathyroid hormone acts on the kidneys to suppress the excretion of calcium in the urine while encouraging excretion of phosphorus.
Parathyroid hormone itself is composed of 84 amino acids sometimes called parathyroid hormone 1-84. Intact and fragmented hormone is present in and secreted by the parathyroid gland. The intact hormone represents a smaller fraction, but its portion is increased when calcium levels are low and decreased when calcium levels are high. The “intact” and “whole or bioactive” parathyroid hormone assays have different reference ranges, but typically their results yield similar interpretations. The effects of fragmentation and disease are still being studied, and there are instances when the two assays may yield a different interpretation.
The so-called intact parathyroid hormone is the most frequently ordered parathyroid hormone test, which typically measures the whole molecule (PTH 1-84) and the larger fragments (predominantly PTH 1-74). Intact parathyroid hormone is used to help diagnose the cause of a low or high calcium level and to help distinguish between parathyroid-related and non-parathyroid-related causes. Intact parathyroid hormone may also be used to monitor the effectiveness of treatment when an individual has a parathyroid-related condition. Parathyroid hormone is routinely monitored for people with chronic kidney disease or who are on dialysis.
A calcium test is almost always ordered along with a parathyroid hormone test. It is not just the level in the blood that is important but the balance between calcium and parathyroid hormone and the response of the parathyroid glands to changing levels of calcium. Usually, health practitioners are concerned about either severe imbalances in calcium regulation that may require medical intervention or persistent imbalances that indicate an underlying problem.
Parathyroid hormone levels can be used to monitor people who have conditions or diseases that cause chronic calcium imbalances or to monitor those who have had surgery or another treatment for a parathyroid tumor.
Once released into the blood stream, parathyroid hormone has a very short life span; levels fall by half in less than 5 minutes due to uptake and cleavage in the liver and kidneys. The fragments are referred to as C-terminal fragments and are variably sized, missing anywhere from 6 amino acids to more than half the N-terminal portion of the molecule. C-terminal fragments have a longer half-life, exist in much higher concentrations, and are eventually cleared by the kidneys. Although it was originally thought that the C-terminal fragments were inactive, it now appears that certain fragments may have biologic activities that are able to oppose those of intact parathyroid hormone.
Figure 1. Parathyroid hormone function
Abbreviations: Ca = Calcium; P = Phosphate or Phosphorus; PTH = parathyroid hormone; GIT = gastrointestinal tract
Increased parathyroid hormone level is seen in:
- Primary hyperparathyroidism.
- Failure of the body to respond to parathyroid hormone (pseudohypoparathyroidism or secondary hyperparathyroidism).
- Vitamin D deficiency (hereditary) and rickets.
- Vitamin D disorders, including not enough sunlight in older adults and problems absorbing, breaking down, and using vitamin D in the body
- Zollinger Ellison syndrome.
- Non-parathyroid hormone producing tumors give rise to paraneoplastic syndrome. They produce parathyroid hormone like protein which acts like parathyroid hormone.
- Chronic renal failure.
- Hypocalcemia. Lack of calcium, which may be due to not eating enough calcium, not absorbing calcium in the gut, or losing too much calcium in your urine
- Malabsorption.
- Drugs that may increase parathyroid hormone levels include phosphates, anticonvulsants, steroids, isoniazid, lithium, and rifampin.
- Disorders that increase phosphate or phosphorous levels in the blood, such as long-term (chronic) kidney disease
- Pregnancy or breastfeeding (uncommon)
- Tumors in the parathyroid gland, called adenomas
Decreased parathyroid hormone level is seen in:
- Parathyroid glands do not produce enough parathyroid hormone (hypoparathyroidism)
- Non-Parathyroid hypercalcemia.
- Secondary hypoparathyroidism. Accidental removal of parathyroid glands during thyroid surgery.
- Sarcoidosis and tuberculosis
- Metastatic bone tumors.
- Excess vitamin D intake.
- Milk-alkali syndrome.
- Excess calcium over a long period of time usually from excess calcium supplements or certain antacids, that contain calcium carbonate or sodium bicarbonate (baking soda)
- DiGeorge syndrome is a primary immunodeficiency disease where baby may also be born without parathyroid glands.
- Autoimmune destruction of the parathyroid gland
- Cancers that start in another part of the body (such as the breast, lungs, or colon) and spread to the bone.
- Low levels of magnesium in the blood.
- Radiation to the parathyroid glands.
What does parathyroid hormone do?
Parathyroid hormone helps control calcium, phosphorus, and vitamin D levels in the blood and bone.
- When calcium level is too low, the body responds by making more parathyroid hormone. This causes the calcium level in the blood to rise.
- As calcium levels begin to increase in the blood, parathyroid hormone normally decreases.
- Magnesium also influences the parathyroid hormone level. Hypermagnesemia suppress the parathyroid hormone secretion, although not like calcium.
What does vitamin D have to do with parathyroid hormone?
If you do not have enough vitamin D, your body will not be able to absorb calcium properly. Vitamin D regulates the intestinal absorption of calcium, while parathyroid hormone regulates the activation of vitamin D. Too much or too little vitamin D can cause an imbalance in calcium metabolism. During winter months with less sun exposure, especially further from the equator, vitamin D levels are typically lower and parathyroid hormone levels may therefore be higher. Diet and illness may affect the magnitude of these changes.
Parathyroid hormone normal range
Normal parathyroid hormone level:
- Intact parathyroid hormone molecule = 10 to 60 pg/mL.
- N-terminal = 8 to 24 pg/mL.
- C-terminal = 50 to 330 pg/mL.
- Mostly the intact parathyroid hormone molecule is recommended.
What does abnormal parathyroid hormone test result mean?
A health practitioner will evaluate both calcium and parathyroid hormone results together to determine whether the levels are appropriate and are in balance as they should be. If both parathyroid hormone and calcium levels are normal, then it is likely that the body’s calcium regulation system is functioning properly.
Low levels of parathyroid hormone may be due to conditions causing hypercalcemia or to an abnormality in parathyroid hormone production causing hypoparathyroidism. Excess parathyroid hormone secretion may be due to hyperparathyroidism, which is most frequently caused by a benign parathyroid tumor. In rare cases, it may be caused by cancer.
Calcium – Parathyroid hormone Relationship
- If calcium levels are low and parathyroid hormone levels high, then the parathyroid glands are responding appropriately, producing appropriate amounts of parathyroid hormone. Depending on the degree of hypocalcemia, a health practitioner may investigate a low calcium level further by measuring vitamin D, phosphorus, and magnesium levels.
- If calcium levels are low and parathyroid hormone levels are normal or low, then parathyroid hormone is not responding properly and the person tested probably has hypoparathyroidism. Hypoparathyroidism is a failure of the parathyroid glands to produce sufficient parathyroid hormone. It may be due to a variety of conditions and may be persistent, progressive, or transient. Causes include an autoimmune disorder, parathyroid damage or removal during surgery, a genetic condition, or a severe illness. Those affected will generally have low parathyroid hormone levels, low calcium levels, and high phosphorus levels.
- If calcium levels are high and parathyroid hormone levels are high, then the parathyroid glands are producing inappropriately high amounts of parathyroid hormone. A health practitioner may order X-rays or other imaging studies to help determine the cause and evaluate the severity of hyperparathyroidism. Hyperparathyroidism is a group of conditions characterized by an overproduction of parathyroid hormone by the parathyroid glands that is separated into primary, secondary, and tertiary hyperparathyroidism.
- If calcium levels are high and parathyroid hormone levels are low, then the parathyroid glands are responding properly, but a health practitioner is likely to perform further investigations to check for non-parathyroid-related reasons for the elevated calcium, such as rare mutations in calcium receptors or tumors that secrete a peptide that has parathyroid hormone-like activity and increases calcium concentration, which in turn decreases parathyroid hormone.
The table below summarizes results that may be seen:
| Calcium | Parathyroid hormone | Interpretation |
| Normal | Normal | Calcium regulation system functioning OK |
| Low | High | Parathyroid hormone is responding correctly; may run other tests to check for other causes of hypocalcemia |
| Low | Normal or Low | Parathyroid hormone not responding correctly; probably have hypoparathyroidism |
| High | High | Parathyroid gland producing too much parathyroid hormone; may do imaging studies to check for hyperparathyroidism |
| High | Low | Parathyroid hormone is responding correctly; may run other tests to check for non-parathyroid-related causes of elevated calcium |
| Normal | High | Mild hyperparathyroidism |
Can I have an abnormal parathyroid hormone level without having symptoms?
Yes, if your calcium level changes slowly, you may not have any noticeable symptoms. In this case, the imbalance will most likely be detected by finding an abnormal calcium level during a regular health check, then checking your parathyroid hormone level.
Parathyroid hormone and calcitonin
Calcitonin is a hormone produced by special cells in the thyroid gland called C-cells. The thyroid gland is a small butterfly-shaped gland that lies over and flat against the windpipe in the throat. The thyroid gland produces calcitonin and several hormones that help control the rate of metabolism, primarily thyroxine (T4) and triiodothyronine (T3).
Calcitonin is involved in the regulation of calcium levels in the blood through inhibiting bone breakdown (resorption) and decreasing kidney reabsorption of calcium. However, calcitonin’s role in calcium regulation is minor compared with parathyroid hormone (PTH) and 1,25-dihydroxyvitamin D (calcitriol). Thus, the measurement of calcitonin in blood is not useful for diagnosis of disorders of calcium regulation.
In two rare conditions, C-cell hyperplasia and medullary thyroid cancer, excessive amounts of calcitonin are produced. C-cell hyperplasia is a benign condition that may or may not progress to become medullary thyroid cancer. Medullary thyroid cancer is malignant – it can spread beyond the thyroid and can be difficult to treat if it is not discovered early.
Medullary cancer is a rare form of thyroid cancer that accounts for 1-2% of all thyroid cancers in the United States. About 75-80% of medullary thyroid cancer cases are sporadic, occurring in those who do not have a family history of the disease. About 20-25% of cases are related to an inherited mutation in the RET gene that leads to multiple endocrine neoplasia type 2 (MEN 2). Multiple endocrine neoplasia type 2 (MEN 2) is a syndrome associated with several related diseases, including medullary thyroid cancer and pheochromocytomas. The altered RET gene is inherited in an autosomal dominant fashion. Only one copy of the mutated gene – from either a father or mother – is required to have a greatly increased risk of developing medullary thyroid cancer. Most cases of sporadic medullary thyroid cancer develop when people are in their 40s or 50s, and the prevalence is higher in women. The inherited form affects both sexes equally and can occur at an earlier age.
Low parathyroid hormone
Hypoparathyroidism is a rare condition where the parathyroid glands, which are in the neck near the thyroid gland, produce too little parathyroid hormone.
This makes blood calcium levels fall (hypocalcaemia) and blood phosphorus levels rise (hyperphosphataemia), which can cause a wide range of symptoms, including muscle cramps, pain and twitching.
Treatment for hypoparathyroidism involves taking supplements, usually for life, to restore calcium and phosphorus levels.
Causes of hypoparathyroidism
The most common cause of hypoparathyroidism is removal of or accidental injury to the parathyroid glands during surgery to the neck or thyroid.
Hypoparathyroidism may also be caused by any of the following:
- Autoimmune attack on the parathyroid glands, where the body mistakenly attacks its own tissues – such as Addison’s disease and pernicious anemia
- Being born without parathyroid glands or with glands that don’t work properly – for example, people with the inherited genetic disorder DiGeorge syndrome are born without parathyroid glands
- Radiotherapy to treat throat or neck cancer
- Low blood magnesium levels in the blood – for example, because of alcohol misuse
- DiGeorge syndrome is a childhood disease in which hypoparathyroidism occurs because all the parathyroid glands are missing at birth. DiGeorge syndrome is a primary immunodeficiency disease associated with susceptibility to infections due to decreased T cell production and function due to an absent or poorly developed thymus. The thymus is the “school house” where T-cells are educated to fight infection and prevent autoimmunity. DiGeorge syndrome is caused by abnormal cell and tissue development during fetal growth. In addition to possible immune system problems, this abnormal development can result in altered facial characteristics, abnormal gland development (parathyroid or thyroid) or heart defects. DiGeorge syndrome is a lifelong condition that is typically diagnosed in infancy or early childhood. Children with DiGeorge syndrome differ in the organs and tissues affected, as well as in the severity of the disease.
- Familial hypoparathyroidism occurs with other endocrine diseases such as adrenal insufficiency in a syndrome called type I polyglandular autoimmune syndrome (PGA I).
Symptoms of hypoparathyroidism
The symptoms of hypoparathyroidism can include:
- a tingling sensation (paresthesia) in your fingertips, toes and lips
- twitching facial muscles
- muscle pains or cramps, particularly in your legs, feet or tummy
- tiredness
- mood changes, such as feeling irritable, anxious or depressed
- dry, rough skin
- coarse hair that breaks easily and can fall out
- fingernails that break easily
- abdominal pain
- cataracts
- calcium deposits in some tissues
- decreased consciousness
- dry hair
- dry, scaly skin
- muscle cramps
- muscle spasms called tetany (can affect the larynx, causing breathing difficulties)
- pain in the face, legs, and feet
- painful menstruation
- seizures
- teeth that do not grow in on time, or at all
- weakened tooth enamel (in children)
Hypoparathyroidism possible complications
Hypoparathyroidism in children may lead to poor growth, abnormal teeth, and slow mental development.
Too much treatment with vitamin D and calcium can cause high blood calcium (hypercalcemia) or high urine calcium (hypercalciuria). Excess treatment may sometimes interfere with kidney function, or even cause kidney failure.
Hypoparathyroidism increases the risk of:
- Addison disease (only if the cause is autoimmune)
- Cataracts
- Parkinson’s disease
- Pernicious anemia (only if the cause is autoimmune)
Hypoparathyroidism diagnosis
Hypoparathyroidism is diagnosed after a blood test has shown:
- low parathyroid hormone levels
- low calcium levels
- high phosphorus levels
Hypoparathyroidism treatment
Treatment for hypoparathyroidism aims to relieve your symptoms and bring the levels of calcium and other minerals in your blood back to normal.
The normal calcium range is around 2.2 to 2.6 millimoles per litre (mmol/L). You’ll be advised to keep your calcium levels in a slightly lower range – for example, 1.8 to 2.25mmol/L. Your recommended range will depend on your circumstances.
Calcium carbonate and vitamin D supplements – usually calcitriol (Rocaltrol) or alfacalcidol (One-Alpha) – can be taken to restore your blood calcium to these levels. They usually have to be taken for life.
You’ll also need to have regular blood tests to monitor your parathyroid hormone, calcium and phosphorus levels.
If your blood calcium levels fall to a dangerously low level or you keep having muscle spasms, you may need to be given calcium through a drip directly into your vein.
Dietary advice
It’s also recommended that you follow a high-calcium, low-phosphorus diet.
Good sources of calcium include:
- milk, cheese and other dairy foods
- leafy green vegetables, such as broccoli, cabbage and okra – but not spinach
- soya beans
- tofu
- soya drinks with added calcium
- nuts
- bread and anything made with fortified flour
- fish where you eat the bones, such as sardines and pilchards
Phosphorus is found in:
- red meat
- dairy
- fish
- poultry
- bread
- rice
- oats
Hypoparathyroidism prognosis
The outcome is likely to be good if the diagnosis is made early. But changes in the teeth, cataracts, and brain calcifications cannot be reversed in children who have undiagnosed hypoparathyroidism during development.
High parathyroid hormone
Hyperparathyroidism is where the parathyroid glands, which are in the neck near the thyroid gland, produce too much parathyroid hormone.
This causes blood calcium levels to rise (hypercalcaemia). Left untreated, high levels of calcium in the blood can lead to a range of problems.
Causes of hyperparathyroidism
There are 2 main types of hyperparathyroidism:
- Primary hyperparathyroidism – when there’s a problem within the parathyroid gland itself, usually a benign (non-cancerous) tumor of the gland
- Secondary hyperparathyroidism – when there’s nothing wrong with the gland, but a condition like kidney failure or vitamin D deficiency lowers calcium levels, causing the body to react by producing extra parathyroid hormone
Tertiary hyperparathyroidism is a term that describes long-standing secondary hyperparathyroidism that starts to behave like primary hyperparathyroidism.
It’s associated with very advanced kidney failure (usually requiring dialysis).
People with tertiary hyperparathyroidism are almost always under the care of kidney specialists.
Causes of primary hyperparathyroidism
- In 4 out of 5 cases, primary hyperparathyroidism is caused by a non-cancerous tumor called an adenoma on one of the parathyroid glands.
- Less commonly, it can occur if 2 or more parathyroid glands become enlarged (hyperplasia).
- Very rarely, primary hyperparathyroidism can be caused by cancer of a parathyroid gland.
- Women are twice as likely to develop primary hyperparathyroidism than men. Most women who develop it are 50 to 60 years of age.
Causes of secondary hyperparathyroidism
Medical conditions that cause low blood calcium or increased phosphate can also lead to hyperparathyroidism. Common conditions include:
- Conditions that make it hard for the body to remove phosphate
- Kidney failure
- Not enough calcium in the diet
- Too much calcium lost in the urine
- Vitamin D disorders (may occur in children who do not eat a variety of foods, and in older adults who do not get enough sunlight on their skin)
- Problems absorbing nutrients from food
Symptoms of hyperparathyroidism
Hyperparathyroidism usually causes few or no symptoms. The severity of symptoms doesn’t always relate to the level of calcium in your blood.
Hyperparathyroidism is often diagnosed before symptoms occur. For example, some people with a slightly raised calcium level may have symptoms, while others with high calcium levels may have few or no symptoms at all.
If you do have symptoms, they can be wide ranging and include:
- depression
- tiredness
- feeling thirsty and peeing a lot
- feeling sick and losing your appetite
- muscle weakness
- constipation
- tummy pain
- loss of concentration
- mild confusion
Left untreated, high blood calcium levels may cause:
- vomiting
- drowsiness
- dehydration
- confusion
- muscle spasms
- bone pain or tenderness
- joint pain
- irregular heartbeat
- high blood pressure (hypertension)
It can also cause a number of other possible complications, including:
- osteoporosis and bone fractures
- kidney stones and blockage, and kidney damage or failure
- peptic ulcers
- pancreatitis (inflammation of the pancreas)
In very severe cases of hyperparathyroidism, high calcium levels can lead to rapid kidney failure, loss of consciousness, coma, or serious life-threatening heart rhythm abnormalities.
But hyperparathyroidism is usually diagnosed at an early stage in the US, and these complications are extremely rare.
Hyperparathyroidism possible complications
Long-term problems that can occur when hyperparathyroidism is not well controlled include:
- Bones become weak, deformed, or can break
- High blood pressure and heart disease
- Kidney stones
- Long-term kidney disease
Parathyroid gland surgery can result in hypoparathyroidism and damage to the nerves that control the vocal cords.
Hyperparathyroidism diagnosis
It’s important that hyperparathyroidism is diagnosed as soon as possible. Without treatment, it can gradually get worse and may lead to complications.
But in most cases, the condition is mild to moderate and remains stable for years.
Hyperparathyroidism is diagnosed after a blood test shows:
- high levels of parathyroid hormone
- high levels of blood calcium, often with low levels of phosphorus
A DEXA scan (a bone density X-ray) can help detect bone loss, fractures or bone softening, and X-rays, CT scans or ultrasound scans may show calcium deposits or kidney stones.
Hyperparathyroidism treatment
If you have a mildly increased calcium level and don’t have symptoms, you may choose to have regular checkups or get treated.
If you decide to have treatment, it may include:
- Drinking more fluids to prevent kidney stones from forming
- Exercising
- Not taking a type of water pill called thiazide diuretic
- Estrogen for women who have gone through menopause
- Having surgery to remove the overactive glands (usually for people under age 50)
If you have symptoms or your calcium level is very high, you may need surgery to remove the parathyroid gland that is overproducing the hormone.
If you have hyperparathyroidism from a medical condition, your provider may prescribe vitamin D, if you have a low vitamin D level.
If hyperparathyroidism is caused by kidney failure, treatment may include:
- Extra calcium and vitamin D
- Avoiding phosphate in the diet
- The medicine cinacalcet (Sensipar)
- Dialysis or a kidney transplant
- Parathyroid surgery, if the parathyroid level becomes uncontrollably high
Treating primary hyperparathyroidism
Surgery to remove the parathyroid gland is the only way of treating primary hyperparathyroidism. This cures about 97% of cases.
If your calcium levels are very high, you may need to be admitted to hospital urgently.
In this situation, dehydration needs to be corrected, usually with fluids given through an intravenous drip.
Medication called bisphosphonates may also be given to lower calcium. These are only used as a short-term treatment. Surgery will be needed once the calcium levels are stabilized.
For people who are unable to have surgery – for example, because of other medical conditions or they’re too frail – a tablet called cinacalcet (Sensipar) may be used to help control the condition.
Make sure you have a healthy, balanced diet.
You don’t need to avoid calcium altogether. A lack of dietary calcium is more likely to lead to a loss of calcium from your skeleton, resulting in brittle bones (osteoporosis).
But you should avoid a high-calcium diet and drink plenty of water to prevent dehydration.
Medications such as thiazide diuretics (water tablets commonly used to treat high blood pressure) should be avoided because they can cause dehydration and raise calcium levels.
Treating secondary hyperparathyroidism
Treatment for secondary hyperparathyroidism depends on the underlying cause.
Low vitamin D is the most common cause and can be corrected with oral vitamin D (cholecalciferol or vitamin D3).
Kidney disease is another common cause – read more about treating chronic kidney disease.
Treating tertiary hyperparathyroidism
Cinacalcet (Sensipar) may be used to treat tertiary hyperparathyroidism that occurs in very advanced kidney failure.
Hyperparathyroidism prognosis
Outlook depends on the cause of hyperparathyroidism.