Contents
What is periorbital cellulitis
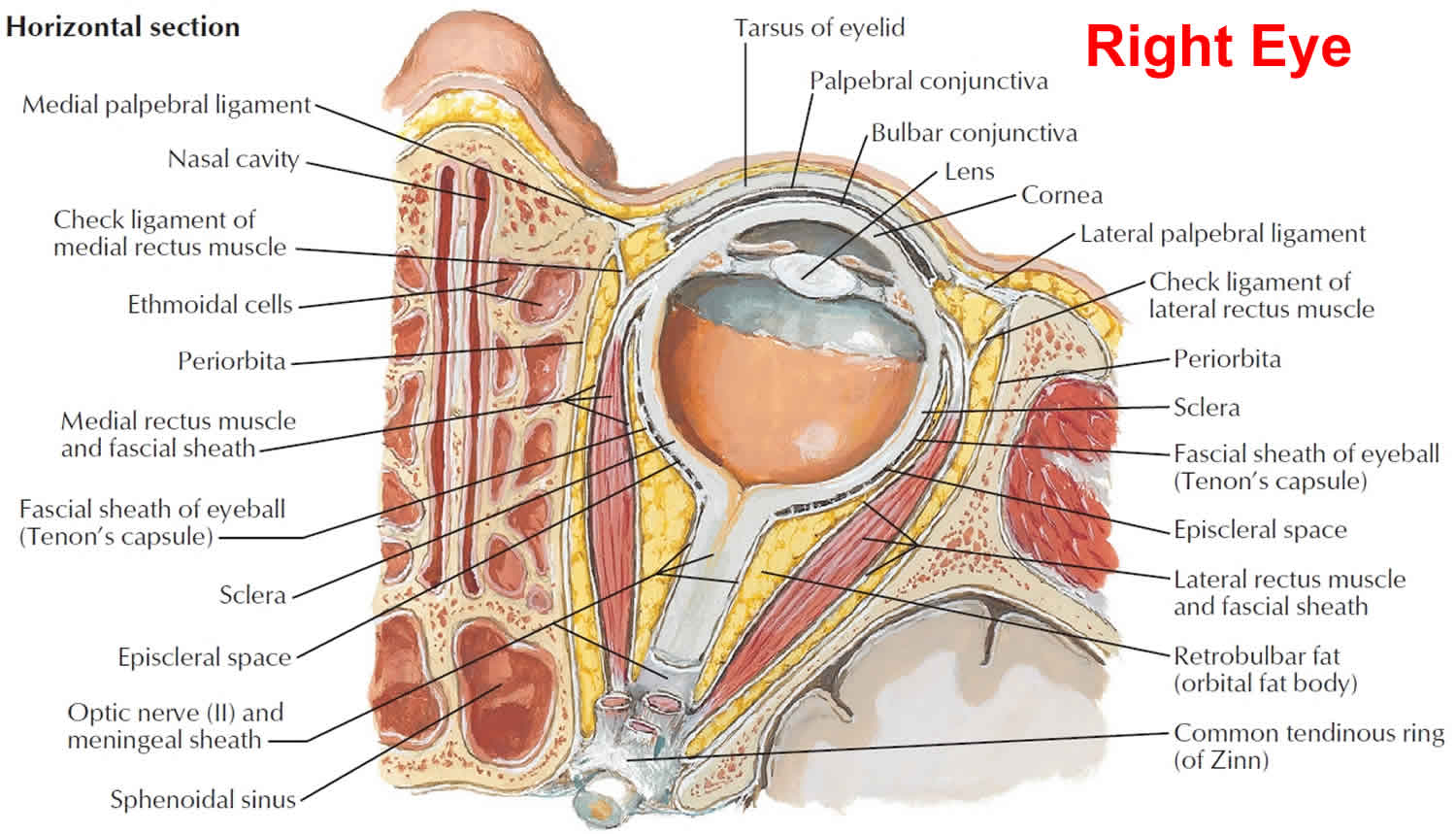
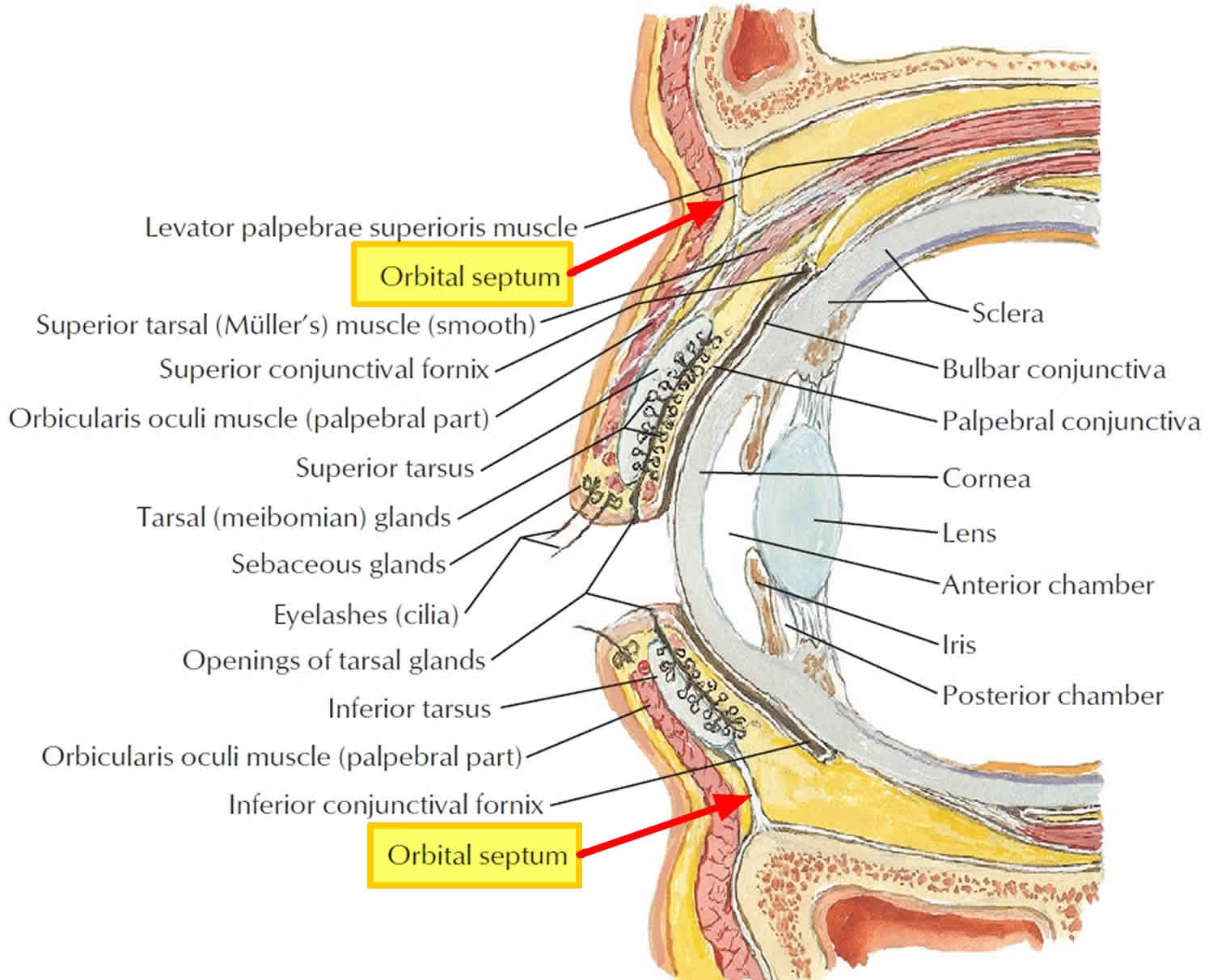
Periorbital cellulitis is also called preseptal cellulitis, is an eye infection that is limited to the soft tissues anterior to the orbital septum involving the eyelid or skin around the eye 1, often managed with oral antibiotics. The orbital septum is a fibrous tissue that divides the orbit contents in two compartments: preseptal (anterior to the septum) and postseptal (posterior to the septum). The infection that develops behind to orbital septum is known as “orbital cellulitis”. Both entities are caused by an infectious process.
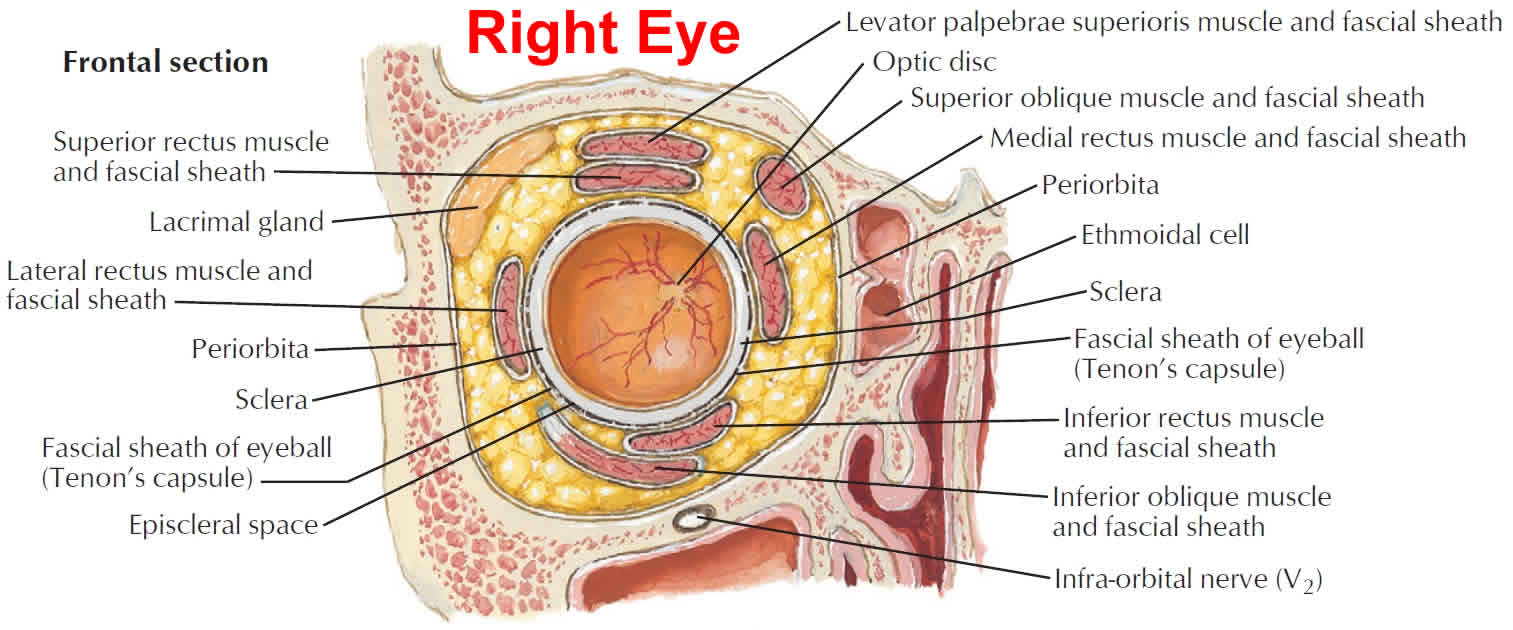
Differentiating orbital from periorbital cellulitis (preseptal cellulitis) is extraordinarily important given that orbital cellulitis has the potential to cause a compartment syndrome within the eye socket resulting in irreversible vision loss to the affected eye 2. The orbital septum is a membranous sheath extending from the periosteum of the orbit to the tarsal plate located in the eyelid, and is the key anatomical structure in differentiating preseptal from orbital cellulitis. The orbit (eye socket) is the bony structure in which the globe (eyeball) is housed, and it also contains extraocular muscles, fat, and the blood vessels and nerves that supply these structures. Orbital cellulitis (Figures 4 to 6 below), also called post-septal cellulitis, is inflammation of the soft tissues (muscles, fat, and connective tissue) of the orbit most commonly from infection. It is important to remember that in orbital cellulitis, the globe itself is not infected or inflamed. Because the orbit is surrounded by the frontal, ethmoid, and maxillary sinuses, infection often results from extension of a sinus infection.
In comparison, periorbital cellulitis (preseptal cellulitis) (Figure 1), is an infection of the eyelids and surrounding soft tissues that are anterior to the orbital septum. Both orbital cellulitis and preseptal cellulitis are more common in children, and preseptal cellulitis is much more common that orbital cellulitis.
Cellulitis is an infection that can affect the skin and/or the eyes. There are two types of cellulitis that affect the eyes:
- Periorbital cellulitis (preseptal cellulitis) — periorbital cellulitis (preseptal cellulitis) only affects eyelid tissue. Periorbital cellulitis (preseptal cellulitis) usually happens in children, especially young children.
- Orbital cellulitis — orbital cellulitis affects the eye socket (called the orbit). This form of cellulitis can cause the eye or eyelid to swell, keeping the eye from moving properly. Orbital cellulitis is a serious condition. It often needs to be treated more aggressively than periorbital cellulitis (preseptal cellulitis).
Periorbital cellulitis classification
A modification of Chandler’s classification of periorbital infections is still in use by many clinicians 3:
- Preseptal cellulitis.
- Orbital cellulitis.
- Subperiosteal abscess.
- Orbital abscess.
- Cavernous sinus thrombosis.
Table 1: Comparison of clinical, historical, and diagnostic characteristics of preseptal and orbital cellulitis
| Characteristic | Preseptal Cellulitis | Orbital Cellulitis |
| Eye pain | May be present | Yes |
| Eyelid erythema and/or tenderness | Yes | Yes |
| Pain with eye movements | No | May be present |
| Ophthalmoplegia ± diplopia | No | May be present* |
| Proptosis | No | May be present* |
| Vision loss | No | May be present* |
| Relative afferent pupillary defect | No | May be present* |
| Fever | Usually not present | Usually present |
| Intraocular Pressure (IOP) | Normal | May be elevated* |
| Resistance to Retropulsion | None | Present* |
| History of sinusitis | May be present, but often not | Present more often than not |
| CT or MRI imaging | Shows inflammation only anterior to the orbital septum | Show post-septal involvement of the inflammation. |
| Blood Cultures | Very rarely has bacteremia | Bacteremia may be present |
| *Emergency signs and symptoms that might warrant immediate lateral canthotomy/cantholysis | ||
There are three main routes for pathogen inoculation in the periorbital tissues:
- Direct inoculation: after eyelid trauma and infected insect bites.
- Spread from contiguous structures: paranasal sinuses are the most common (specially the ethmoids, since nerves and vessels traverse the lamina papyracea that divides the ethmoids sinuses from the orbit), chalazia/hordeolum, dacryocystitis, dacryoadenitis, canaliculitis, impetigo, erysipela, herpes simplex and herpes zoster skin lesions, endophthalmitis.
- Hematogenous: via blood vessels from an upper respiratory tract or a middle ear infection.
The venous drainage of the orbit, eyelids and sinuses goes primarily to the superior and inferior orbital veins, which drain to the cavernous sinus. Because these veins are devoid of valves, infection easily can spread to preseptal and postseptal space, and can also lead to cavernous sinus thrombosis.
Figure 1. Periorbital cellulitis
Figure 2. Orbital septum
 Is periorbital cellulitis contagious?
Is periorbital cellulitis contagious?
Yes. The majority of periorbital cellulitis are caused by bacteria. In the era before the establishment of the universal vaccination against Haemophilus influenza type b (Hib), periorbital cellulitis was a frequent cause especially in children under 5 years of age. Periorbital cellulitis is still common in unvaccinated patients.
Periorbital cellulitis causes
Periorbital cellulitis can occur at any age, but commonly affects children under 18 months old.
Periorbital cellulitis can occur after a scratch, injury, or bug bite around the eye, which allows germs to enter the wound. It can also extend from a nearby site that is infected, such as the sinuses.
The majority of periorbital cellulitis are caused by bacteria. Adenovirus, herpes simplex and varicella zoster are also associated to cellulitis. In the immunocompromised patient we must suspect fungi as a possible cause. Gram positive cocci are the most prevalent microorganisms identified in preseptal cellulitis – typically Staphylococcus and Streptococcus species (pyogenes and pneumonia). Staphylococcus aureus and epidermidis are commonly found after a penetrating eyelid trauma. Streptococcus pneumoniae is a common etiology in preseptal cellulitis secondary to sinusitis. In the era before the establishment of the universal vaccination against Haemophilus influenza type b (Hib), this was a frequent cause especially in children under 5 years of age. It is still common in unvaccinated patients. In preseptal cellulitis secondary to a human bite it is frequent to isolate anaerobic bacteria such as Clostridium.
Periorbital cellulitis symptoms
Patients complain of eyelid swelling and redness. But also general malaise and low grade fever are commonly reported. Among the classic signs of periorbital cellulitis (preseptal cellulitis) are eyelid swelling/redness/warmth and fever. There are clinical keys that help distinguish between preseptal and orbital cellulitis.
- Periorbital cellulitis (preseptal cellulitis): eyelid edema and erythema, normal visual acuity, absence of proptosis, pupil with normal reaction to light, normal color saturarion, normal conjunctiva and normal ocular movements.
- Orbital cellulitis: eyelid edema and erythema, diminished visual acuity, proptosis is present, relative afferent pupillary defect may be present, reduced color saturation, chemotic conjunctiva and reduced extraocular movements with pain elicited by these movements.
Periorbital cellulitis (preseptal cellulitis) symptoms include:
- Redness around the eye or in the white part of the eye
- Swelling of the eyelid, whites of eyes, and surrounding area
- This condition does not often affect vision or cause eye pain.
Cellulitis may extend to the cheek and forehead. Also, it is common to see an eyelid abscess associated with preseptal cellulitis, which may require incision and drainage.
Periorbital cellulitis diagnosis
As previously discussed, the first step is to determine whether a patient has orbital cellulitis, which requires orbital imaging, admission, blood cultures and IV antibiotics. Begin with a thorough ophthalmologic exam, with particular attention to visual acuity, pupillary testing for a relative afferent pupillary defect, intraocular pressure, and assessment of proptosis and eye motility.
In cases of question, computed tomography (CT) with and without contrast of the orbits and sinuses should be ordered to look for evidence of post-septal involvement. If a diagnosis of orbital cellulitis is made, the patient needs to be immediately assessed monitored for signs of compartment syndrome and optic neuropathy which would warrant an emergent lateral canthotomy/cantholysis. This procedure allows for anterior expansion of orbital contents which relieves pressure within the orbit in restores blood flow to those structures. Even after initiating antibiotics the swelling may increase for the first 24-48 hours, so frequent re-evaluation is warranted. Immediate surgery may be indicated if there is evidence of a subperiosteal abscess, orbital abscess, or extension of the infection into the cranium. Consider consulting an otolaryngologist (ENT specialist) for management of sinus disease.
Patients whose history and examination are consistent with periorbital cellulitis (preseptal cellulitis) without symptoms of orbital cellulitis may be treated as an outpatient with oral antibiotics. Patients with periorbital cellulitis (preseptal cellulitis) who are appropriately treated typically recover completely without any permanent sequelae. If treated appropriately, patients with orbital cellulitis also often have good outcomes. However, failure to diagnose and treat orbital cellulitis in a timely manner may result in permanent vision loss. An ophthalmologist should be consulted in all cases of orbital or periorbital cellulitis (preseptal cellulitis). However, assessing for vision threatening orbital cellulitis should not be postponed until an ophthalmologist is available as an irreversible ischemic optic neuropathy can occur in less than 90 minutes.
It is useful to delineate the area of the face affected with cellulitis using a skin marker, in order to monitor progression along time. Photographs are also an invaluable tool.
Diagnostic Tests
- Complete blood count to document leukocytosis.
- CT scan: Sometimes the eyelid edema is so severe that precludes eye examination, thus making the distinction between preseptal and orbital cellulitis impossible. In these cases, it is useful to order a CT scan of the orbit and sinuses (to diagnose an associated sinusitis).
- Cultures of the eyelid wound (if evident), conjunctiva, blood (if febrile), abscess contents (if present and drained) or paranasal sinus secretion. These are important in order to prescribe the most appropriate antibiotic according to bacteria sensitivity.
- Lymph nodes of the head and neck to asses for lymphadenomegaly.
- Check for signs of meningeal irritation to evaluate the presence of intracranial complications.
Periorbital cellulitis treatment
Once diagnosed, periorbital cellulitis (preseptal cellulitis) can be treated in an outpatient or inpatient basis depending on the characteristics of the patient.
- If the patient is afebrile with a mild periorbital cellulitis (preseptal cellulitis) he can be followed as an outpatient with oral antibiotics and daily visits to monitor the progress of the disease. However, if the patient does not respond to oral antibiotics in 48 hours or if extension of the infectious process into the orbit is suspected, he or she should be admitted to the hospital: a CT scan must be performed and intravenous antibiotics must be indicated.
- Usually children under 2 years of age or febrile patients with a severe cellulitis are managed with intravenous antibiotics during hospitalization, with close followup. Hospitalization is also recommended in patients who cannot be followed up as outpatients. Intravenous antibiotics are usually indicated for two or three days, depending on improvement. If the condition improves, treatment can be switched to the appropriate oral antibiotics based on cultures.
These patients should be treated by a multidisciplinary team: ophthalmologist, pediatrician/primary care physician and ENT (in case of an associated sinusitis).
Empiric antibiotic therapy:
Broad spectrum antibiotics must be prescribed to cover gram positive and gram negative bacteria.
- Oral
- Against gram positive and negative bacteria: Ampicillin, Amoxicillin/clavulanate, Fluoroquinolones (levofloxacin), Azithromicin (also covers some anaerobic bacteria).
- Against gram positive (Staphylococcus) in case of an evident eyelid trauma: Dicloxacillin, Flucloxacillin, first generation cephalosporins (cefalexine, cefazolin).
- Intravenous
- These antibiotics provide coverage to gram positive and gram negative bacteria.
- Third-generation cephalosporins (these medications are less sensitive to β-lactamase producing bacteria such as S. aureus): Ceftriaxone, cefotaxime, ceftazidime.
- Ampicillin/sulbactam.
- These antibiotics provide coverage to gram positive and gram negative bacteria.
The results of antibiotic sensitivities should guide the treatment whenever possible. When the cultures reveal a methicillin-resistant Staphylococcus aureus (MRSA) the therapy choice must be reevaluated. Community associated MRSA is susceptible to these antibiotics administered in an oral route:
- Trimethoprim-Sulfamethoxazole.
- Rifampin.
- Clindamycin.
- Fluoroquinolones.
Hospital-associated MRSA is susceptible only to:
- Intravenous Vancomycin.
- Oral Linezolid.
If there was a penetrating eyelid injury with organic material or a human bite, antibiotics should also cover anaerobic organisms: Metronidazole, Clindamycin.
If an abscess localized in the preseptal space develops, it should be incised and drained. The surgeon must not open the orbital septum during the procedure, since this may spread the infection to the postseptal space and aggravate the infection. As mentioned in the work up section, the contents of the abscess should be cultured to determine appropriate antibiotic therapy.
Periorbital cellulitis prognosis and complications
Prognosis is usually good when this entity is promptly diagnosed and treated. However, complications can develop even with prompt treatment.
- Orbital extension and complications: orbital cellulitis, subperiosteal abscess, orbital abscess, cavernous sinus thrombosis.
- Central nervous system involvement (after orbital extension): meningitis, abscesses (brain, extradural or subdural).
- Necrotizing fasciitis: it is a rare complication caused by β-hemolytic Streptococcus. It presents as a rapidly progressive cellulitis with poorly demarcated borders and violaceous skin discoloration, which can lead to necrosis and toxic shock syndrome. The patient must be admitted to the hospital, intravenous fluids should be replenished, IV broad spectrum antibiotics must be prescribed and surgical debridement could be necessary.
Figure 3. Eye socket anatomy
Orbital vs periorbital cellulitis
Orbital cellulitis is an infection of the soft tissues of the eye socket behind the orbital septum, a thin tissue which divides the eyelid from the eye socket 4. This is in contrast to preseptal cellulitis which is a soft tissue infection of the eyelids anterior to the orbital septum. If a diagnosis of preseptal cellulitis is entertained, a well-defined event should be elicited from the patient (e.g. injury, stye, bug bite, etc). If a convincing event cannot be elicited, an orbital cause should always be investigated with orbital imaging.
Orbital cellulitis most commonly refers to an acute spread of infection into the eye socket from either the adjacent sinuses, skin or from spread through the blood. The most common bacterial organisms in orbital cellulitis include Streptococcus species, Staphylococcus aureus, Pseudomonas, Enterococcus, Klebsiella, and Haemophilus influenzae type B. Methocillin-resistant staph aureus is becoming more common in orbital cellulitis. If a fungal infection is suspected, consider Mucor and Aspergillus species.
90% of orbital cellulitis cases occur as a secondary extension of acute or chronic bacterial sinusitis, especially the ethmoid sinuses. Other extensions of periorbital structures include the face/eyelids, dacryocystitis and dental infections. Exogenous causes include trauma and orbital/periorbital surgery. An orbital foreign body (specifically organic) should always be entertained in the setting of an orbital cellulitis that is not responding to antibiotic therapy. Endogenous causes include septic embolization from bacteremia. There may also be intraorbital causes including endophthalmitis and dacryoadenitis.
Orbital cellulitis epidemiology:
- Increased incidence during the winter due to the increased incidence of sinusitis
- No ethnic preferences
- Blindness occurs in up to 11% of cases
- In children, twice as common in males
- More common in children than adults: mean age 7-12 years old.
Orbital clinical findings include proptosis (bulging of the eye anteriorly out of the orbit), ptosis (drooping of the upper eyelid), restriction of eye motility, eye pain, and chemosis (swelling of the conjunctiva). If there is decreased visual acuity, or a visual field or relative afferent pupillary defect, one must consider compressive optic neuropathy which warrants urgent aggressive management.
Systemic clinical findings are essential in the workup of possible orbital cellulitis. Pertinent findings include leukocytosis (elevated white blood cells) with elevated neutrophils, monocytes, ESR and CRP and fever, which also demonstrate an infectious etiology.
CT of the orbits and the paranasal sinuses is essential. Evidence of sinusitis mandates otolaryngology involvement. Lumbar puncture is necessary if meningeal signs and symptoms develop. Conjunctival cultures add very little information. Nasal cultures may be appropriate if there is significant nasal discharge in the setting of sinusitis. Blood cultures are appropriate in the setting of septicemia. If surgical drainage of the orbit and/or sinus is performed, cultures should be obtained.
Surgical intervention is less likely in orbital cellulitis in children (≤ 9 years old) because the infection is caused by a single gram positive organism. IV antibiotic therapy is the initial treatment of choice. Progression (worsening motility deficit, pain, optic nerve dysfunction) in a child after 24-48 hours of IV antibiotic therapy would lead one to drain the abscess. However, if this were an adult patient, with evidence of an abscess formation, early surgical intervention to drain the involved sinus and orbital abscess is usually indicated along with medical therapy given that the infection is more likely to be polymicrobial.
Consider surgical management if the patient has any of the following:
- > 9 years old
- Frontal sinusitis
- Non medial location of the subperiosteal abscess
- Large subperiosteal abscess
- Presence of gas in the abscess on CT suggesting an anaerobic etiology
- Recurrent episode of subperiosteal abscess
- Nasal polyps which suggest chronic sinusitis
- Evidence of acute optic neuropathy
- Dental infection (likely an anaerobic infection)
Clinical improvement does not correlate accurately with repeat CT scan analysis. It may take 48-72 hrs for the abscess to improve on imaging.
The majority of patients respond well to medical and/or surgical treatments. Rarely, orbital cellulitis may spread posteriorly to the cavernous sinus, meninges and the brain parenchyma.
Figure 4. Orbital cellulitis
Footnote: 8-month old with recent upper respiratory infection and orbital cellulitis. Infection resolved with intravenous antibiotics.
[Source 5 ]Figure 5. Orbital cellulitis
Footnote: Note the bullous, edematous conjunctiva (conjunctival chemosis), proptosis and the delineation of swelling around the orbital rim. This patient underwent an urgent lateral canthotomy/cantholysis.
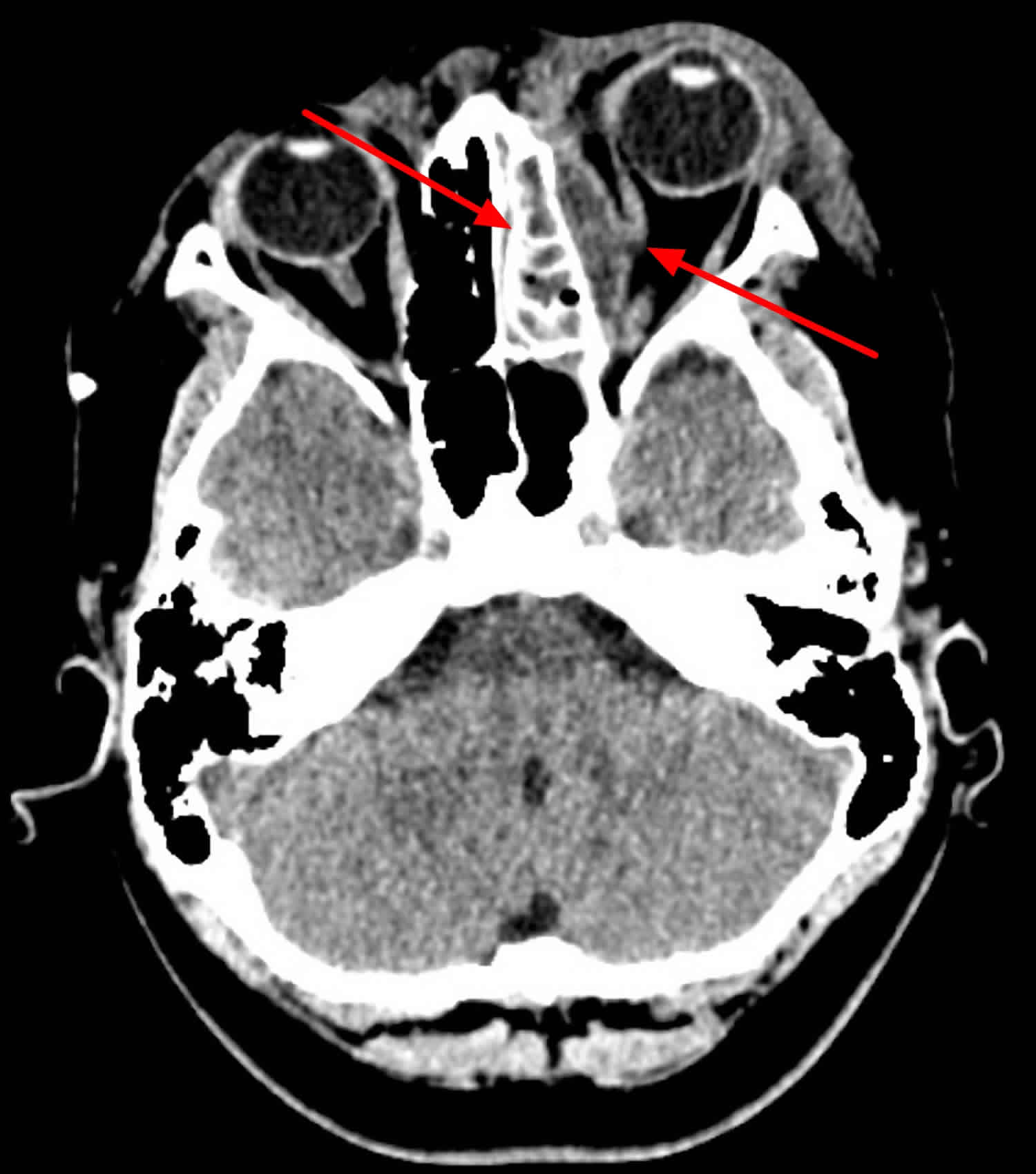
[Source 2 ]Figure 6. Orbital cellulitis CT-scan
Footnote: Subperiosteal abscess formation adjacent to the lamina papyracea of the left orbit with extensive sinusitis involving the left ethmoid sinus. Extensive opacification of all of the left ethmoid sinuses with obilteration of the left osteomeatal complex. Elliptical left subperisoteal collection adjacent to the ethmoid sinuses with displacement of the medial rectus muscle. No bony destruction at the collection site. No intracranial extension.
[Source 5 ]Orbital cellulitis causes
Orbital cellulitis most commonly occurs when bacterial infection spreads from the paranasal sinuses, most often from the ethmoid sinus through the thin lamina papyracea of the medial orbital wall. It can also occur when an eyelid skin infection or an infection in an adjacent area spreads to the orbit or from an infection in the blood system. The drainage of the eyelids, sinuses is largely throughout the orbital venous system, more specifically through the superior and inferior orbital veins that drain into the cavernous sinus. This venous system is devoid of valves and for this reason infection might spread, in preseptal and orbital cellulitis, into the cavernous sinus causing a sight threatening complication such as cavernous sinus thrombosis.
The organisms are best identified by microbiologic culture. The most common infectious pathogens include gram positive streptococcal and staphylococcal species. In children younger than 9, the infections are typically from one organism; in children older than 9 and in adults, the infections may be polymicrobial with both aerobic and anaerobic bacteria.
The most common pathogens in orbital cellulitis, strep and staph are both Gram positive. Streptococcal infections are identified on culture by their formation of pairs or chains. Streptococcal pyogenes (Group A Strep) requires blood agar to grow and exhibits clear (beta) hemolysis on blood agar. Streptococcus such as Streptococcus pneumonia produce Green (alpha) hemolysis, or partial reduction of red blood cell hemoglobin. Staphyloccal species show a cluster arrangement on gram stain. Staphylococcus aureus forms a large yellow colony on rich medium in distinction to Staphylococcus epidermidis which forms white colonies. Gram negative rods can be seen in both orbital cellulitis related to trauma and in some older children or adults. Anaerobic bacteria such as peptococcus, peptostreptococcus, bacteroides can be involved in infections extending from sinusitis in adults or older children. Fungal infections with either mucor or aspergillus need to be considered in immunocompromised or diabetic patients; immunocompetent patients may also have fungal infections in rare cases.
Orbital cellulitis most commonly occurs in the setting of an upper respiratory or sinus infection. The human upper respiratory tract is normally colonized with Strep pneumoniae and infection can occur through several mechanisms. Strep pyogenes infections also occur primarily in the respiratory tract. The complex cell surface of this gram positive organism determines its virulence and ability to invade the surrounding tissue and incite inflammation. Staph aureus infections occur commonly in the skin and spread to the orbit from the skin. Staphylococcal organisms also produce toxins which help to promote their virulence and leads to the inflammatory response seen in these infections. The inflammatory response elicited by all these pathogens plays a major role in tissue destruction in the orbit.
Risk factors for orbital cellulitis
Risk factors include recent upper respiratory illness, acute or chronic bacterial sinusitis, recent trauma, recent ocular or periocular infection, or systemic infection.
Orbital cellulitis prevention
Identifying patients and effectively treating upper respiratory or sinus infections before they evolve into orbital cellulitis is an important aspect of preventing preseptal cellulitis from progressing to orbital cellulitis. Equally important in preventing orbital cellulitis is prompt and appropriate treatment of preseptal skin infections or even odentogenic infections before they spread into the orbit.
Orbital cellulitis signs and symptoms
Orbital cellulitis signs
As a preseptal infection progresses into the orbit, the inflammatory signs typically increase with increasing redness and swelling of the eyelid with a secondary ptosis. As the infection worsens, proptosis develops and extraocular motility becomes compromised. When the optic nerve is involved, loss of visual acuity is noted and an afferent pupillary defect can be appreciated. The intraocular pressure often increases and the orbit becomes resistant to retropulsion. The skin can feel warm to the touch and pain can be elicited with either touch or eye movements. Examination of the nose and mouth is also warranted in order to look for any black eschar which would suggest a fungal infection.
Orbital cellulitis signs:
- Proptosis
- Ptosis
- Chemosis
- Lid erythema/edema
- Motility restriction
Orbital cellulitis symptoms
Systemic symptoms including fever and lethargy may or may not be present. Change in the appearance of the eyelids with redness and swelling is frequently a presenting symptom. Pain, particularly with eye movement, is commonly noted. Double vision may also occur.
Orbital cellulitis symptoms:
- Ocular/periorbital pain
- Decreased vision
- Diplopia
- Nasal discharge
- Worsening pain on eye movement
- Nasal tenderness
Orbital cellulitis complications
The complications of orbital cellulitis are ominous and include optic neuropathy, retinal vein occlusion, severe exposure keratopathy, cavernous sinus thrombosis, meningitis and death.
Orbital cellulitis prognosis
With prompt recognition and aggressive medical and surgical treatment the prognosis is excellent.
Orbital cellulitis diagnosis
The diagnosis of orbital cellulitis is based on clinical examination and CT-scan.The presence of orbital signs such as proptosis, pain with eye movements, ophthalmoplegia (paralysis or weakness of the eye muscles), optic nerve involvement as well as fever and leukocytosis confirm the diagnosis.
Medical history
The presence of a painful red eye, with lid edema in a child with a recent upper respiratory infection is the typical presentation of orbital cellulitis. Patient history should also include the presence of headache, orbital pain, double vision, progression of symptoms, recent upper respiratory symptoms (e.g. nasal discharge or stuffiness), pain over sinuses, fever, lethargy, recent periocular trauma or injury, family or health care contacts with methicillin-resistant Staphylococcus aureus (MRSA), history of sinus, ear, or facial infections or surgery, recent ocular surgery, pertinent medical conditions, medications currently used, as well as the presence of diabetes mellitus and the immune status of the patient.Specific questions regarding any change in mental status, pain with neck movement, or nausea or vomiting should be asked.
Physical examination
The physical examination should include:
- Best-corrected visual acuity. Decreased vision might be indicative of optic nerve involvement or could be secondary to severe exposure keratopathy or retinal vein occlusion.
- Color vision assessment to assess the presence of optic nerve involvement.
- Proptosis measurements using Hertel exophthalmometry.
- Visual field assessment via confrontation.
- Assessment of pupillary function with particular attention paid to the presence of a relative afferent pupillary defect.
- Ocular motility and presence of pain with eye movements. Also, there might be involvement of the 3, 4, and 6 cranial nerve in cases of cavernous sinus involvement.
- Orbit exam should include documentation of direction of displacement of globe (a superior subperiosteal abscess will displace the globe inferiorly), resistance to retropulsion on palpation, unilateral or bilateral involvement
- Measurement of intraocular pressure (IOP).
- Slit-lamp biomicroscopy of the anterior segment if possible to look for signs of exposure keratopathy in cases of severe proptosis.
- Dilated fundus exam will exclude or confirm the presence of optic neuropathy or retinal vascular occlusion.
Laboratory test
Admission to the hospital is warranted in all cases of orbital cellulitis.A complete blood count with differential as well as blood cultures should be ordered.
Imaging test
Imaging of the orbits, paranasal sinuses and brain (ideally with contrast) is a very important radiological emergency in selected patients, typically children, with orbital cellulitis.
Computed tomography (CT) of the orbit is the imaging modality of choice for patients with orbital cellulitis. Most of the time, CT is readily available and will give the clinician information regarding the presence of sinusitis, subperiosteal abscess, stranding of orbital fat, or intracranial involvement. Nevertheless, in cases of mild to moderate orbital cellulitis with no optic nerve involvement, the initial management of the patient remains medical. Imaging is warranted only in cases of poor response to I.V. antibiotics, with progression of orbital signs in order to confirm the presence of complications such as subperiosteal abscess, or intracranial involvement. Although a magnetic resonance imaging(MRI) scan is safer in children since there is no risk of radiation exposure, the long acquisition time and the need for prolonged sedation make CT scan the imaging modality of choice.
The CT scan has three chief purposes 5:
- Is there a subperiosteal collection?
- It there any intracranial extension?
- Is there underlying severe sinusitis?
Orbital cellulitis treatment
The management of orbital cellulitis requires admission to the hospital and initiation of broad-spectrum i.v. antibiotics.Blood cultures, nasal, throat swabs, should be undertaken and the antibiotics should be modified based on the results.In infants with orbital cellulitis a 3rd generation cephalosporin is usually initiated such as cefotaxime, ceftriaxone or ceftazidime along with a penicillinase-resistane penicillin.In older children, since sinusitis is most commonly associated with aerobic and anaerobic organisms, clindamycin might be another option. Metronidazole is also being increasingly used in children. As mentioned before, the antibiotic regimen should be modified based on the results of cultures if needed. The child should be followed closely in the hospital setting for progression of orbital signs and development of complications.Once improvement has been documented with 48 hours of intravenous antibiotics, consideration for switching to oral antibiotics may be appropriate.
In children
- Inpatient – broad spectrum IV antibiotics which is narrowed or tailored to the most likely or documented organism. Consider covering for MRSA (methicillin-resistant Staphylococcus aureus). If the patient is afebrile and improving x 48hrs, may switch to oral antibiotics.
- Outpatient oral antibiotics for 2-3 weeks
- Consider surgical management if worsening on IV antibiotics or have the special conditions listed above in the Discussion section
In adults
- Inpatient – surgical debridement of orbital abscess and associated sinus along with IV antibiotics.
- Outpatient oral antibiotics for 2-3 weeks
Medical follow up
A multi-disciplinary approach is usually warranted for patients with orbital cellulitis under the care of pediatricians, ENT surgeons, ophthalmologists and infectious disease specialists.
Surgery
The prevalence of subperiosteal or orbital abscess complicating an orbital cellulitis approaches 10%. The clinician should suspect the presence of such an entity if there is progression of orbital signs, and /or systemic compromise despite the initiation of appropriate intravenous antibiotics for at least 24-48 hours. In these cases, a contrast-enhanced CT scan should be ordered to evaluate the orbit, the paranasal sinuses, and /or the brain. If an orbital abscess is present it should be drained. The management of subperiosteal abscess though remains more controversial since there are cases of resolution with the use of i.v. antibiotics only. As a general recommendation, observation with I.V. antibiotics only is indicated when:
- Child is under age of 9
- No intracranial involvement
- Medial wall abscess of moderate size
- No vision loss or afferent pupillary defect
- No frontal sinus involvement
- No dental abscess.
- Lebedis CA, Sakai O. Nontraumatic orbital conditions: diagnosis with CT and MR imaging in the emergent setting. Radiographics. 2008;28 (6): 1741-53. https://pubs.rsna.org/doi/10.1148/rg.286085515[↩]
- Preseptal vs Orbital Cellulitis. http://morancore.utah.edu/basic-ophthalmology-review/preseptal-vs-orbital-cellulitis/[↩][↩][↩]
- Preseptal cellulitis. http://eyewiki.org/Preseptal_cellulitis[↩]
- Orbital Cellulitis in a Child. https://webeye.ophth.uiowa.edu/eyeforum/cases/103-Pediatric-Orbital-Cellulitis.htm[↩]
- Orbital cellulitis with a subperiosteal abscess. https://radiopaedia.org/cases/orbital-cellulitis-with-a-subperiosteal-abscess[↩][↩][↩]