Contents
What is plantar fasciitis
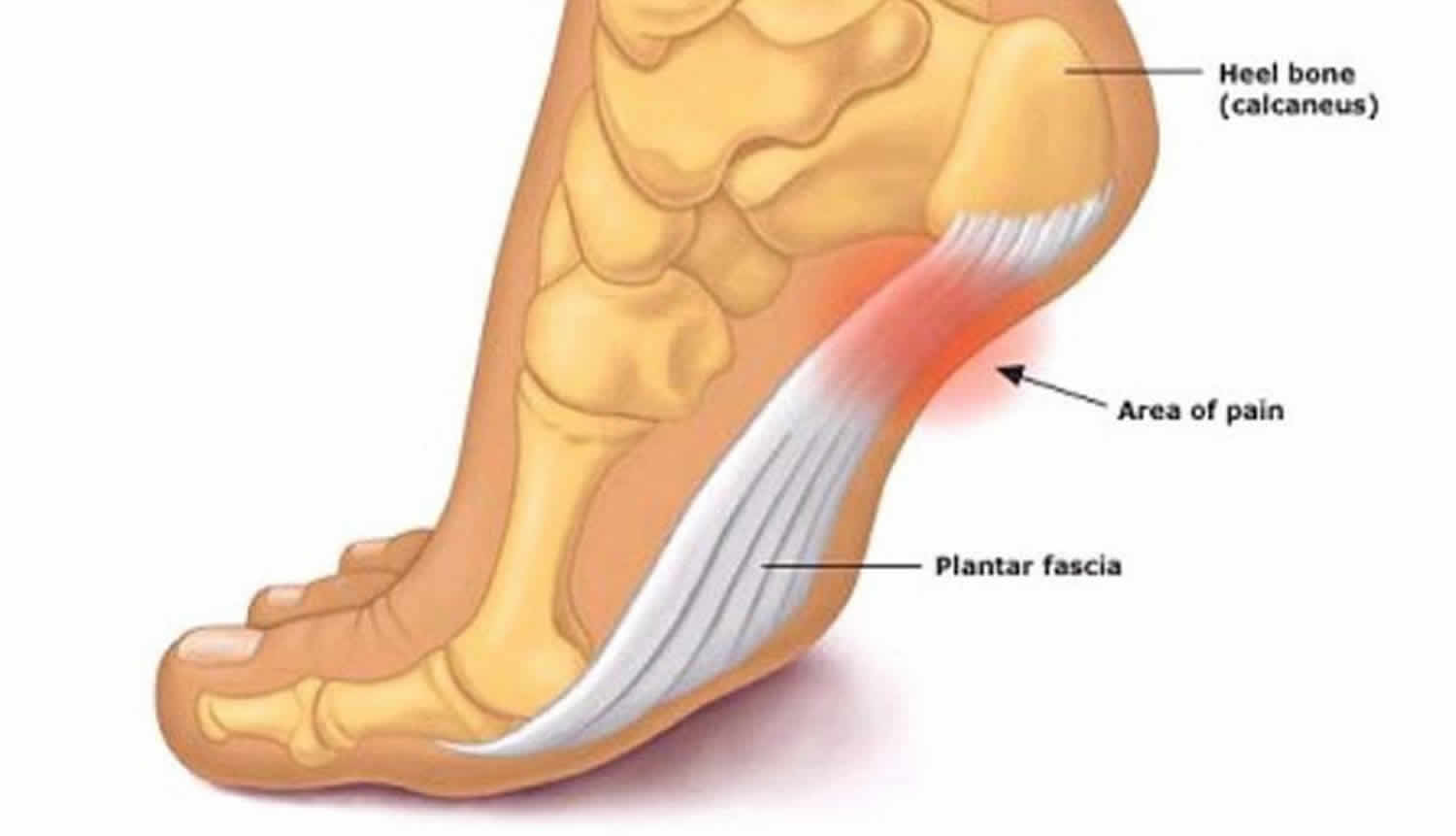
Plantar fasciitis is a localized, degeneration of the plantar fascia origin at the medial calcaneal tuberosity of the heel, the tough, fibrous band of tissue that connects your heel bone to the base of your toes. Plantar fasciitis occurs at the site where the plantar fascia is attached to the bottom of the heel bone. Plantar fasciitis is the most common cause of heel pain, affecting more than three million people every year according to statistics. Plantar fasciitis frequency is similar to those who suffer from lower back pain, which could mean many more people are suffering from the condition.
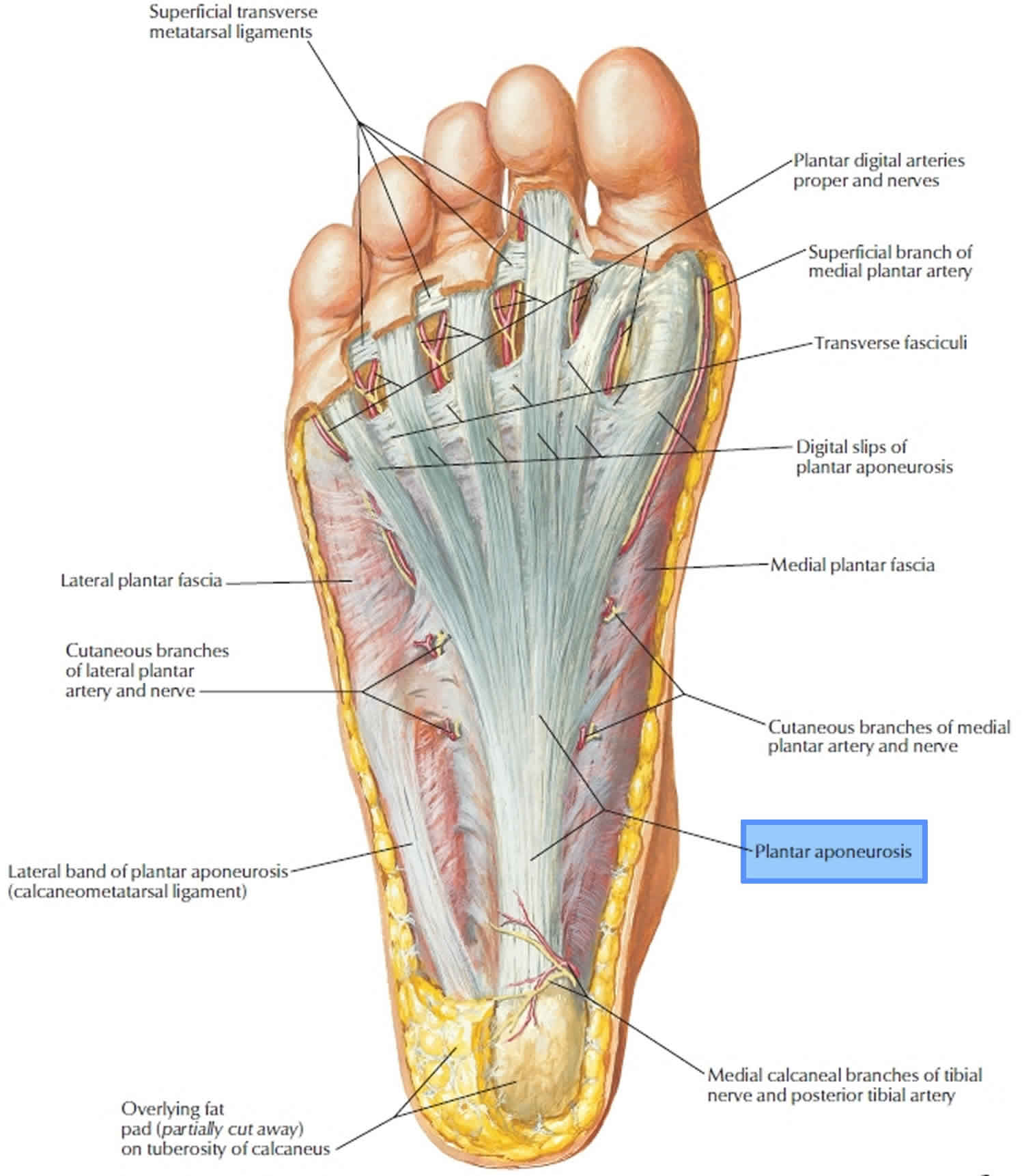
The plantar fascia is a piece of strong and thick tissue that runs along the bottom of the foot. The plantar fascia plays an important role in the normal biomechanics of the foot and is composed of three segments, all of which arise from the calcaneus. The plantar fascia connects the heel bone to the toes, creating the foot’s arch and providing shock absorption.
Under normal circumstances, your plantar fascia acts like a shock-absorbing bowstring, supporting the arch in your foot. If tension and stress on that bowstring become too great, small tears can arise in the fascia. Repetitive stretching and tearing can cause the fascia to become irritated or inflamed, though in many cases of plantar fasciitis, the cause isn’t clear.
Plantar fasciitis is degenerative irritation of the plantar fascia, either through overstretching, overuse or a medical condition. Despite the name plantar fasciitis, this condition is notably characterized by an absence of inflammatory cells 1.
Common symptoms of plantar fasciitis include mild pain on the bottom of the heel, especially when taking your first steps of the day. Often, symptoms improve only to worsen later in the day. This happens due to over-stressing of the plantar fascia causing a chronic healing response at the attachment to the bone that may remain sore for months.
Plantar fasciitis can be caused by:
- Playing sports that put stress on the heel bone, like running, dance and aerobics.
- Flat-footed or high arches.
- Being middle-aged or older.
- Being overweight.
- Pregnancy.
- Spending a lot of time on your feet.
- Wearing shoes with poor arch support or stiff soles.
Plantar fasciitis is often associated with a heel spur which is a spike of bone poking out from the heel bone, but many people have heel spurs without any pain.
All foot types are prone to plantar fasciitis, including folks with high arches and those with what we call flat feet. The condition is common in middle-aged and older patients. It is also common in patients who walk or stand on hard surfaces a lot. It disproportionately affects those who are overweight.
Plantar fasciitis accounts for about 10% of runner-related injuries and 11% to 15% of all foot symptoms requiring professional medical care 2. Plantar fasciitis is thought to occur in about 10% of the general population as well, with 83% of these patients being active working adults between the ages of 25 and 65 years old. Plantar fasciitis may present bilaterally in a third of the cases. Some literature shows prevalence rates among a population of runners to be as high as 22% 3.
Most people who have plantar fasciitis recover with conservative treatments, including resting, icing the painful area and stretching, in several months (within 12 months of initial presentation and often sooner) 4.
If your heel pain was caused by a specific episode or injury, and doesn’t improve within a week of resting and icing the area, you should seek medical help. Since most cases are chronic, and the pain appears gradually and begins to worse over time, see an orthopedic foot and ankle specialist when your quality of life begins to suffer despite taking time to rest, stretch and ice the area. The orthopedic foot and ankle specialist will take a history of your symptoms and your past medical conditions, examine your foot and leg and take an x-ray to rule out any other possible causes for the pain.
Figure 1. Plantar fascia
Figure 2. Plantar fasciitis
Plantar fasciitis types
There are two types of plantar fasciitis — acute and chronic.
- Acute plantar fasciitis: The condition can be triggered by a specific injury, this is also called an acute type.
- Chronic plantar fasciitis: There is also a chronic type also known as the classic case of plantar fasciitis which becomes worse over time.
If you have plantar fasciitis, there are things you can do to help relieve the pain and heal your foot.
Plantar fasciitis cause
Plantar fasciitis is often an overuse injury that is primarily due to a repetitive strain causing micro tears of the plantar fascia but can occur as a result of trauma or other multifactorial causes 2. Some predisposing factors are flat feet (pes planus), high arch foot (pes cavus), limited ankle dorsiflexion, and excessive pronation or supination. Flat feet (pes planus) can cause increased strain at the origin of the plantar fascia. High arch foot (pes cavus) can cause excessive strain on the heel because the foot does not effectively evert or absorb shock. Tight gastrocnemius, soleus, and/or other posterior leg muscles have also been commonly found in patients with plantar fasciitis. It is thought that these tight muscles can alter the normal biomechanics of ambulation.
Approximately 50% of patients with plantar fasciitis will also have heel spurs, but the spurs themselves are not the cause. Plantar fasciitis is often associated with runners and older adults, but other risk factors include obesity, occupations requiring prolonged standing, and weight-bearing. Other causes include a pinched nerve in the heel region, thinning of the heel fat pad, or a stress fracture of the heel bone. Plantar fasciitis has also been found to be associated with various seronegative spondyloarthropathies, but in approximately 85% of cases, there are no known systemic factors 5.
Plantar fasciitis pathophysiology
Plantar fasciitis is primarily a degenerative process. Aside from degenerative changes, histological findings include granulation tissue, micro-tears, collagen disarray, and notably a lack of traditional inflammation. Ultrasound evaluation often reveals calcifications, intrasubstance tears, and thickening and heterogeneity of the plantar fascia. These changes, often seen on ultrasound, suggest a non-inflammatory condition and dysfunctional vasculature.
Risk factors for plantar fasciitis
Though plantar fasciitis can arise without an obvious cause, factors that can increase your risk of developing plantar fasciitis include:
- Age. Plantar fasciitis is most common between the ages of 40 and 60.
- Certain types of exercise. Activities that place a lot of stress on your heel and attached tissue — such as long-distance running, ballistic jumping activities, ballet dancing and aerobic dance — can contribute to an earlier onset of plantar fasciitis.
- Foot mechanics. Being flat-footed, having a high arch or even having an abnormal pattern of walking can affect the way weight is distributed when you’re standing and put added stress on the plantar fascia.
- Obesity. Excess pounds put extra stress on your plantar fascia.
- Occupations that keep you on your feet. Factory workers, teachers and others who spend most of their work hours walking or standing on hard surfaces can damage their plantar fascia.
Plantar fasciitis prevention
Take good care of your feet. Wear shoes with good arch support and heel cushioning. If you work on hard surfaces, stand on a thick rubber mat to reduce stress on your feet. Make sure that you stretch daily whether you are an athlete or not. Stay at a healthy weight to reduce the load on your feet.
Plantar fasciitis symptoms
The main symptom of plantar fasciitis is pain under the heel, which can be dull or sharp. The foot sole may ache or burn and your heel may be slightly swollen.
The pain is often worse:
- in the morning, as you take your first steps
- after prolonged standing or sitting
- after intense activity.
Plantar fasciitis complications
Ignoring plantar fasciitis may result in chronic heel pain that hinders your regular activities. Changing the way you walk to minimize plantar fasciitis pain might lead to foot, knee, hip or back problems.
Plantar fasciitis diagnosis
To check whether you have plantar fasciitis, your doctor will probably ask you some questions, for example, about your symptoms, the type of work you do and your lifestyle.
Also, it’s likely they’ll perform a physical exam to check the arches of your feet and to see whether there is any redness, swelling, tenderness, stiffness or tightness.
Patients will often present with a history of progressive pain at the inferior and medial heel, but can, however, radiate proximally in more severe cases. They will often describe the pain as sharp and worst with the first few steps out of bed in the morning. Long periods of standing, or in severe cases, sitting for prolonged periods, will also exacerbate symptoms. Pain often decreases with ambulation or beginning an athletic activity, but then increases throughout the day as activity increases. Pain can usually be reproduced by palpating the plantar medial calcaneal tubercle at the site of the plantar fascial insertion on the heel bone. Pain can also be reproduced with passive dorsiflexion of the foot and toes. Specifically, passive dorsiflexion of the first metatarsophalangeal joint is known as the windlass (or Jack’s) test and considered a positive test if pain is reproduced. Secondary findings may include a tight Achilles heel cord, pes planus, or pes cavus. It may also be beneficial to assess a patient’s gait to assess for biomechanical factors or predisposing factors mentioned previously. When considering the diagnosis of plantar fasciitis, one should consider fat pad contusion or atrophy, stress fractures, and nerve entrapments such as tarsal tunnel syndrome in the differential.
Usually no tests are necessary. Your doctor might suggest an X-ray, ultrasound scan or magnetic resonance imaging (MRI) to make sure your pain isn’t being caused by another problem, such as a stress fracture or a pinched nerve.
X-rays and/or ultrasound evaluation may show calcifications in the soft tissues or heel spurs on the inferior aspect of the heel. Additionally, ultrasound may show thickening and swelling of the plantar fascia which is a typical feature. If the patient is not responding to conservative therapy after longer periods of time, then the provider may consider ordering an MRI to evaluate for tears, stress fractures, or osteochondral defects 6.
Sometimes an X-ray shows a spur of bone projecting forward from the heel bone. In the past, these bone spurs were often blamed for heel pain and removed surgically. But many people who have bone spurs on their heels have no heel pain.
Plantar fasciitis treatment
More than 90% of patients with plantar fasciitis will improve within 10 months of starting simple treatment methods.
Initially, your doctor may recommend one or more of the following treatments:
- Pain-relief medicine, such as anti-inflammatory medication like ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve) or acetaminophen (paracetamol)
- Physiotherapy with specific stretching exercises
- Resting your foot as much as possible. Decreasing or even stopping the activities that make the pain worse is the first step in reducing the pain. You may need to stop athletic activities where your feet pound on hard surfaces (for example, running or step aerobics).
- Shoes with good support and cushioning
- Night splints to wear while sleeping. Most people sleep with their feet pointed down. This relaxes the plantar fascia and is one of the reasons for morning heel pain. A night splint stretches the plantar fascia while you sleep. Although it can be difficult to sleep with, a night splint is very effective and does not have to be used once the pain is gone.
- Cushioned soled shoes, heel cups or heel pads, and soft orthotics are useful in alleviating symptoms. Shoes with thick soles and extra cushioning can reduce pain with standing and walking. As you step and your heel strikes the ground, a significant amount of tension is placed on the fascia, which causes microtrauma (tiny tears in the tissue). A cushioned shoe or insert reduces this tension and the microtrauma that occurs with every step. Soft silicone heel pads are inexpensive and work by elevating and cushioning your heel. Pre-made or custom orthotics (shoe inserts) are also helpful.
- An icepack applied to your foot. Rolling your foot over a cold water bottle or ice for 20 minutes is effective. This can be done 3 to 4 times a day.
If these measures don’t work or your condition doesn’t improve after 12 weeks, your doctor may give you steroid injections in your heel. But, beware that having multiple injections may weaken the fibers of the fascia even more. Other interventions such as a night splint or shock wave therapy may also help.
Very occasionally, people have surgery to try to fix it. As a practice, doctors do not explore surgery for plantar fasciitis unless noninvasive treatments have failed, but statistics show that about 5 in 100 sufferers may be candidates.
Figure 3. Plantar fasciitis night splint
Plantar fasciitis stretches
Stretching is by far the best therapy to relieve the painful plantar fasciitis symptoms without damaging the integrity of the plantar fascia. Simple, corrective stretches to loosen up the calf muscle, the Achilles tendon and of course the plantar fascia itself.
A simple stretch that can be done at your desk involves folding one foot over the opposite knee with your toes flexed back towards you in a figure four formation. Another is the yoga pose called downward dog. The classic runner’s stretch also helps stretch the lower leg and bottom of the foot.
Plantar fasciitis exercises
Toe curls with towel
- Place a small towel on the floor. Using involved foot, curl towel toward you, using only your toes. Relax.
- Repeat 10 times, 1-2 times per day.
Figure 4. Toe curls with towel
Toe Extension
- Sit with involved leg crossed over uninvolved leg. Grasp toes with one hand and bend the toes and ankle upwards as far as possible to stretch the arch and calf muscle. With the other hand, perform deep massage along the arch of your foot.
- Hold 10 seconds. Repeat for 2-3 minutes. Repeat 2-4 sessions per day.
OR
- Stand with your foot directly in front of a wall. Make sure your shoe is off.
- Slowly position your foot so that your big toe is resting on the wall and the ball of your foot is a few centimeters from the floor. Your big toe should be bending gently backward.
- A gentle stretch should be felt on the bottom of your foot. Hold this position for 15 seconds, and then take your foot away from the wall.
- Repeat the stretch five times.
Figure 5. Toe extension
Standing calf stretch
- Stand placing hands on wall for support. Place your feet pointing straight ahead, with the involved foot in back of the other. The back leg should have a straight knee and front leg a bent knee. Shift forward, keeping back leg heel on the ground, so that you feel a stretch in the calf muscle of the back leg.
- Hold 45 seconds, 2-3 times. Repeat 4-6 times per day.
Figure 6. Standing calf stretch
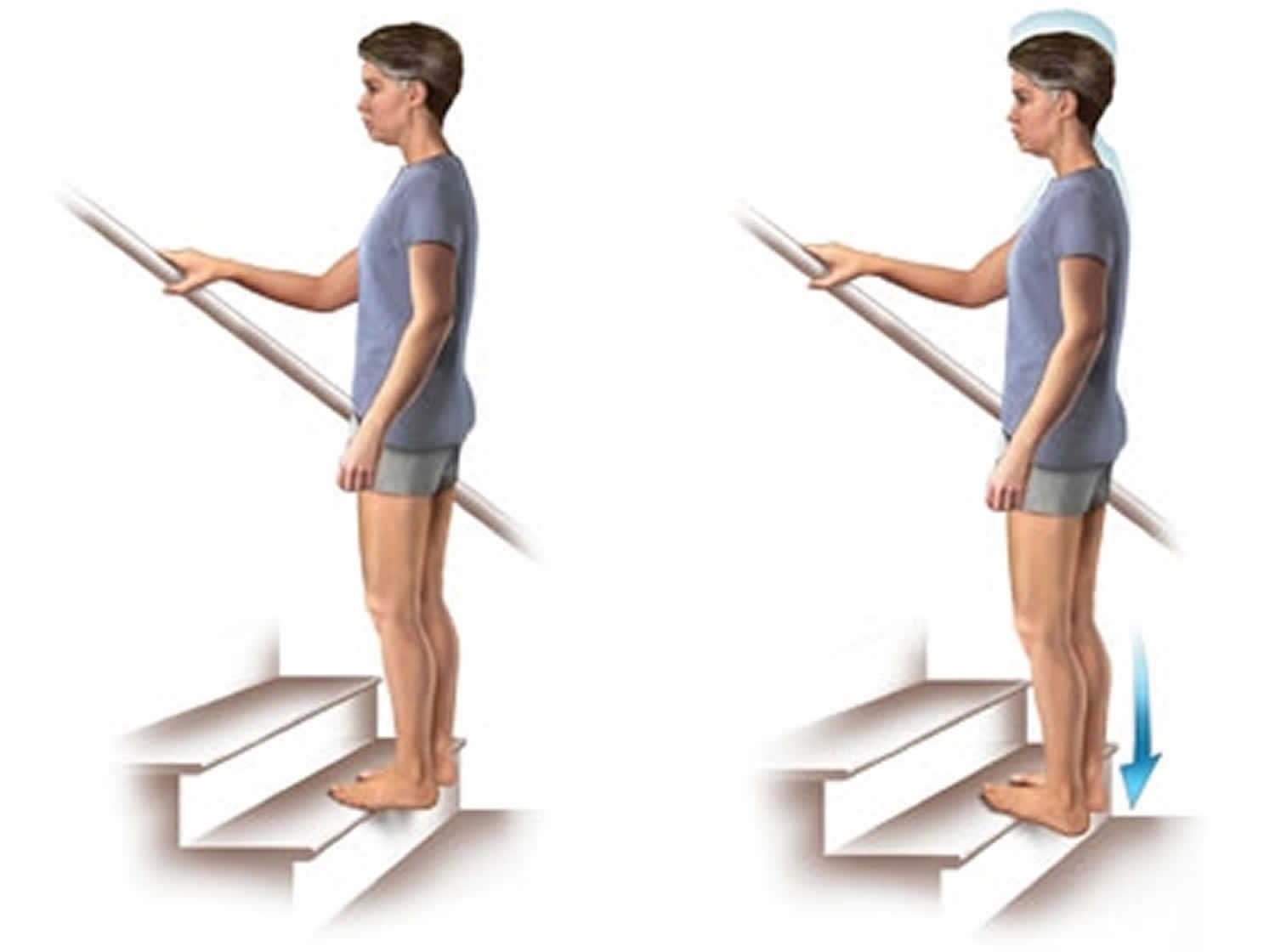
 Calf stretch on a step
Calf stretch on a step
- Stand with uninvolved foot flat on a step. Place involved ball of foot on the edge of the step. Gently let heel lower on involved leg to feel a stretch in your calf.
- Hold 45 seconds, 2-3 times. Repeat 4-6 times per day.
Figure 7. Calf stretch on a step
 Towel stretch
Towel stretch
The towel stretch is effective at reducing morning pain if done before getting out of bed.
- Sit with involved leg straight out in front of you. Place a towel around your foot and gently pull toward you, feeling a stretch in your calf muscle.
- Hold 45 seconds, 2-3 times. Repeat 4-6 times per day.
Figure 8. Towel stretch
Ice massage arch roll
- With involved foot resting on a frozen can or water bottle, golf ball, or tennis ball, roll your foot back and forth over the object.
- Repeat for 3-5 minutes, 2 times per day.
Figure 9. Ice massage arch roll
Plantar fasciitis home remedies
To reduce the pain of plantar fasciitis, try these self-care tips:
- Maintain a healthy weight. Lose weight if you’re overweight or obese to minimize stress on your plantar fascia.
- Choose supportive shoes. Avoid high heels. Buy shoes with a low to moderate heel, good arch support and shock absorbency. Don’t go barefoot, especially on hard surfaces.
- Don’t wear worn-out athletic shoes. Replace your old athletic shoes before they stop supporting and cushioning your feet. If you’re a runner, buy new shoes after about 400 to 500 miles of use.
- Change your sport. Try a low-impact sport, such as swimming or bicycling, instead of walking or jogging.
- Apply ice. Hold a cloth-covered ice pack over the area of pain for 15 to 20 minutes three or four times a day or after activity. Or try ice massage. Freeze a water-filled paper cup and roll it over the site of discomfort for about five to seven minutes. Regular ice massage can help reduce pain and inflammation.
- Stretch your arches. Simple home exercises can stretch your plantar fascia, Achilles tendon and calf muscles.
Other procedures
When more-conservative measures aren’t working after several months, your doctor might recommend:
Injections
Injecting a type of steroid medication into the tender area can provide temporary pain relief. Multiple injections aren’t recommended because they can weaken your plantar fascia and possibly cause it to rupture. More recently, platelet-rich plasma has been used, under ultrasound guidance, to provide pain relief with less risk of tissue rupture.
Corticosteroid injections have been shown to be beneficial in the short-term (less than four weeks) but ineffective in the long term 2.
Extracorporeal shock wave therapy
In this procedure, sound waves are directed at the area of heel pain to stimulate healing. It’s usually used for chronic plantar fasciitis that hasn’t responded to more-conservative treatments. This procedure might cause bruising, swelling, pain, numbness or tingling. Some studies show promising results, but it hasn’t been shown to be consistently effective.
Evidence of the efficacy of platelet rich plasma, dex prolotherapy, and extra-corporeal shockwave therapy is conflicting 2.
Tenex procedure
This minimally invasive procedure removes the scar tissue of plantar fasciitis without surgery.
Plantar fasciitis surgery
Few people need surgery to detach the plantar fascia from the heel bone. It’s generally an option only when the pain is severe and all else fails 7. Surgery is considered only after 12 months of aggressive nonsurgical treatment.
Most patients have good results from surgery. However, because surgery can result in chronic pain and dissatisfaction, it is recommended only after all nonsurgical measures have been exhausted.
Complications of surgery include a weakening of the arch in your foot.
Gastrocnemius recession
This is a surgical lengthening of the calf (gastrocnemius) muscles. Because tight calf muscles place increased stress on the plantar fascia, this procedure is useful for patients who still have difficulty flexing their feet, despite a year of calf stretches.
In gastrocnemius recession, one of the two muscles that make up the calf is lengthened to increase the motion of the ankle. The procedure can be performed with a traditional, open incision or with a smaller incision and an endoscope, an instrument that contains a small camera. Your doctor will discuss the procedure that best meets your needs.
Complication rates for gastrocnemius recession are low, but can include nerve damage.
Plantar fascia release
If you have a normal range of ankle motion and continued heel pain, your doctor may recommend a partial release procedure. During surgery, the plantar fascia ligament is partially cut to relieve tension in the tissue. If you have a large bone spur, it will be removed, as well. Although the surgery can be performed endoscopically, it is more difficult than with an open incision. In addition, endoscopy has a higher risk of nerve damage.
The most common complications of release surgery include incomplete relief of pain and nerve damage.
Plantar fasciitis prognosis
Plantar fasciitis may be a benign disorder but if not adequately managed can be disabling and associated with moderate to severe pain. About 70-80% of patients with plantar fasciitis see symptom reduction in 9-12 months, but at least 5-10% require surgical release of the plantar fascia 8. Plantar fasciitis in athletes is associated with high morbidity and even when managed appropriately recurrences are not uncommon. The morbidity of plantar fasciitis is due to pain in the foot, difficulty with ambulation, limitation in exercise and inability to weight bear. Sometimes, the uneven ambulation can also leas to an injury of the knee and hip joints. Among people who have to stand for long hours, plantar fasciitis is one of the most common causes of worker’s compensation claims 9.
- Becker BA, Childress MA. Common Foot Problems: Over-the-Counter Treatments and Home Care. Am Fam Physician. 2018 Sep 01;98(5):298-303.[↩]
- Buchanan BK, Kushner D. Plantar Fasciitis. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431073[↩][↩][↩][↩]
- Cotchett M, Lennecke A, Medica VG, Whittaker GA, Bonanno DR. The association between pain catastrophising and kinesiophobia with pain and function in people with plantar heel pain. Foot (Edinb). 2017 Aug;32:8-14.[↩]
- Buchanan BK, Kushner D. Plantar Fasciitis. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431073.[↩]
- Finkenstaedt T, Siriwanarangsun P, Statum S, Biswas R, Anderson KE, Bae WC, Chung CB. The Calcaneal Crescent in Patients With and Without Plantar Fasciitis: An Ankle MRI Study. AJR Am J Roentgenol. 2018 Nov;211(5):1075-1082.[↩]
- Lai TW, Ma HL, Lee MS, Chen PM, Ku MC. Ultrasonography and clinical outcome comparison of extracorporeal shock wave therapy and corticosteroid injections for chronic plantar fasciitis: A randomized controlled trial. J Musculoskelet Neuronal Interact. 2018 Mar 01;18(1):47-54.[↩]
- McClinton S, Heiderscheit B, McPoil TG, Flynn TW. Physical therapist decision-making in managing plantar heel pain: cases from a pragmatic randomized clinical trial. Physiother Theory Pract. 2018 Jul 06;:1-25.[↩]
- [↩]
- Ling Y, Wang S. Effects of platelet-rich plasma in the treatment of plantar fasciitis: A meta-analysis of randomized controlled trials. Medicine (Baltimore). 2018 Sep;97(37):e12110.[↩]