Contents
- What is pneumococcal vaccine
- Pneumococcal vaccine schedule for children
- Pneumococcal vaccine schedule for adults 65 years or older
- Pneumococcal conjugate vaccines
- Pneumococcal Polysaccharide Vaccine
- Where can I find pneumococcal vaccines?
- How well do these pneumococcal vaccines work?
- Which underlying medical conditions indicate that a child age 6 through 18 years should receive additional doses of pneumococcal vaccine beyond the routine schedule?
- What are the different serotypes of Streptococcus pneumoniae targeted by different pneumococcal vaccines?
- How effective are pneumococcal conjugate vaccines at preventing pneumococcal carriage or disease?
- How effective is pneumococcal polysaccharide vaccine at preventing pneumococcal carriage or disease?
- Pneumococcal vaccine composition
- Pneumococcal vaccine administration
- Pneumococcal vaccine contraindications and precautions
- Pneumococcal vaccine schedule
- Pneumococcal vaccine guidelines
- Pneumococcal vaccine Catch-Up Guidance
- Pneumococcal Vaccine Effectiveness
- Pneumococcal vaccine side effects
What is pneumococcal vaccine
Pneumococcal vaccines are very good at preventing severe pneumococcal disease, which is any type of infection caused by Streptococcus pneumoniae bacteria, needing treatment in the hospital and death 1. Pneumococcal vaccines help protect against some of the more than 100 serotypes of pneumococcal bacteria 2. However, pneumococcal vaccination is not guaranteed to prevent infection and symptoms in all people. Streptococcus pneumoniae or pneumococcus, is a type of bacterium that causes pneumococcal disease. Pneumococcal infections can range from ear and sinus infections to pneumonia and bloodstream infections. Each year in the United States, pneumococcal disease causes thousands of infections, such as meningitis, bloodstream infections, pneumonia, and ear infections. Children younger than 2 years old and adults 65 years or older are among those most at risk for disease, but older adults are at greatest risk of serious illness and death. The Centers for Disease Control and Prevention (CDC) recommends pneumococcal vaccination for children younger than 5 years and adults 65 years or older 3.
There are 2 types of pneumococcal vaccines used in the United States 4, 5:
- Pneumococcal conjugate vaccines (PCVs). A conjugate vaccine is a type of vaccine that joins a protein to an antigen (in the case of pneumococcal vaccines, the protein is connected to unique polysaccharides [long chains of sugar molecules] from the surface of each of the pneumococcal serotypes). The conjugate vaccines have the polysaccharides for different serotypes attached (or conjugated) to a carrier protein. The protein helps improve the quality of the immune system response to the vaccine compared to the response to an unconjugated polysaccharide (PPV). Immune response to pneumococcal conjugate vaccine (PCV) is a T-cell dependent response that produces memory B-cells and reduces carriage of the bacteria in the respiratory track. Pneumococcal conjugate vaccines (PCVs) are given to children younger than 5 years old and to older children who need it. Vaccine providers also give pneumococcal conjugate vaccines (PCVs) to adults 65 years or older and other adults who need it.
- Pneumococcal polysaccharide vaccine (PPSV). A polysaccharide vaccine is a type of vaccine that is composed of long chains of sugar molecules called polysaccharides, that resemble the surface of certain serotypes of pneumococcal bacteria in order to help the immune system mount a response. The immune response to the Pneumovax23 (PPSV23) vaccine is a T-cell independent immune response but does not reduce bacterial carriage. Vaccine providers may give Pneumovax23 (PPSV23) to children 2 through 18 years old with certain medical conditions. Vaccine providers give it to adults who receive PCV15 (Vaxneuvance). They also may give it to adults who have received an earlier vaccine called PCV13 (Prevnar 13). PCV13 (Prevnar 13) is FDA-licensed and may still be available in some clinics. PCV13 (Prevnar 13) is no longer routinely recommended; however, CDC guidance allows for its use as previously recommended in situations where PCV15, PCV20, or PCV21 is indicated but unavailable and the alternative is that the patient would not be vaccinated 9.
- PPSV23 (Pneumovax23) helps protect against 23 types of Streptococcus pneumoniae bacteria 10. Following the 2022 changes to the pneumococcal vaccination schedule for adults, PPSV23 (Pneumovax23) is no longer recommended alone, however PPSV23 (Pneumovax23) is recommended for adults following PCV13 (Prevnar 13) or PCV15 (Vaxneuvance) vaccination. PPSV23 (Pneumovax23) is not recommended for people who have previously received a PCV20 (Prevnar 20) or PCV21 (Capvaxive) vaccination.
Each of these vaccines helps protect against specific serotypes, or strains of Streptococcus pneumoniae bacteria. The number at the end of the vaccine name tells how many serotypes the pneumococcal vaccine includes.
The Centers for Disease Control and Prevention (CDC) recommends pneumococcal vaccination for 11:
- Children
- All children younger than 5 years old
- Children 5 through 18 years old with certain risk conditions
- Adults
- All adults 65 years or older
- 19 through 64 years old with certain risk conditions
The latest Pneumococcal Vaccine Recommendation by the Centers for Disease Control and Prevention (CDC) is to use PCV15 (Vaxneuvance) or PCV20 (Prevnar 20) for routine pneumococcal vaccination for all children younger than 5 years of age 3, 12. And for all adults 65 years or older who have never received any pneumococcal conjugate vaccine (PCV) or whose previous vaccination history is unknown administer PCV15 (Vaxneuvance), PCV20 (Prevnar 20) or PCV21 (Capvaxive) 3, 12.
Pneumococcal vaccine schedule for children
Administer a 4-dose pneumococcal conjugate vaccine series (PCV15 [Vaxneuvance] or PCV20 [Prevnar 20]), 1 dose at each of the following ages 3:
- 2 months
- 4 months
- 6 months
- with a booster at age 12 through 15 months
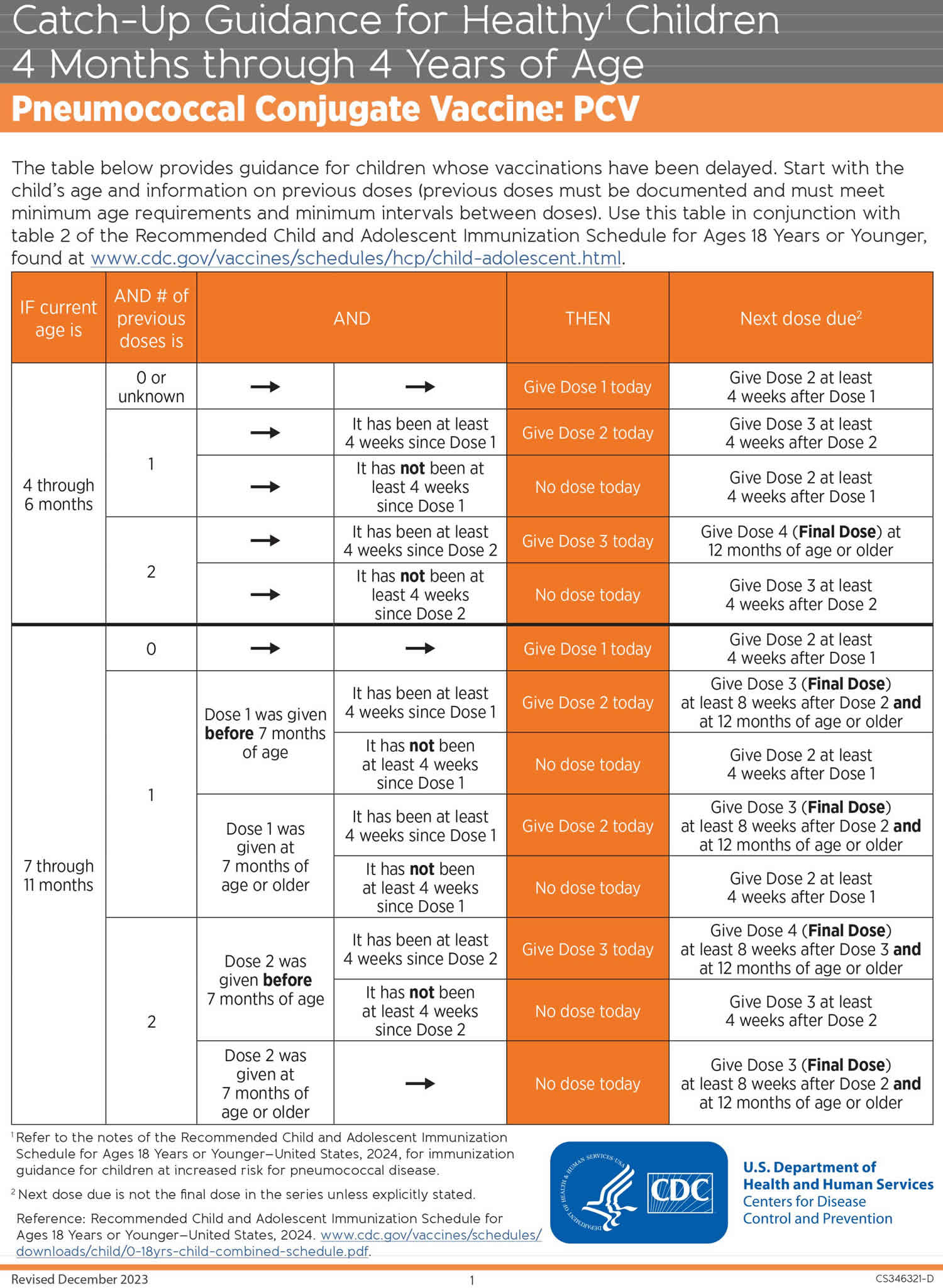
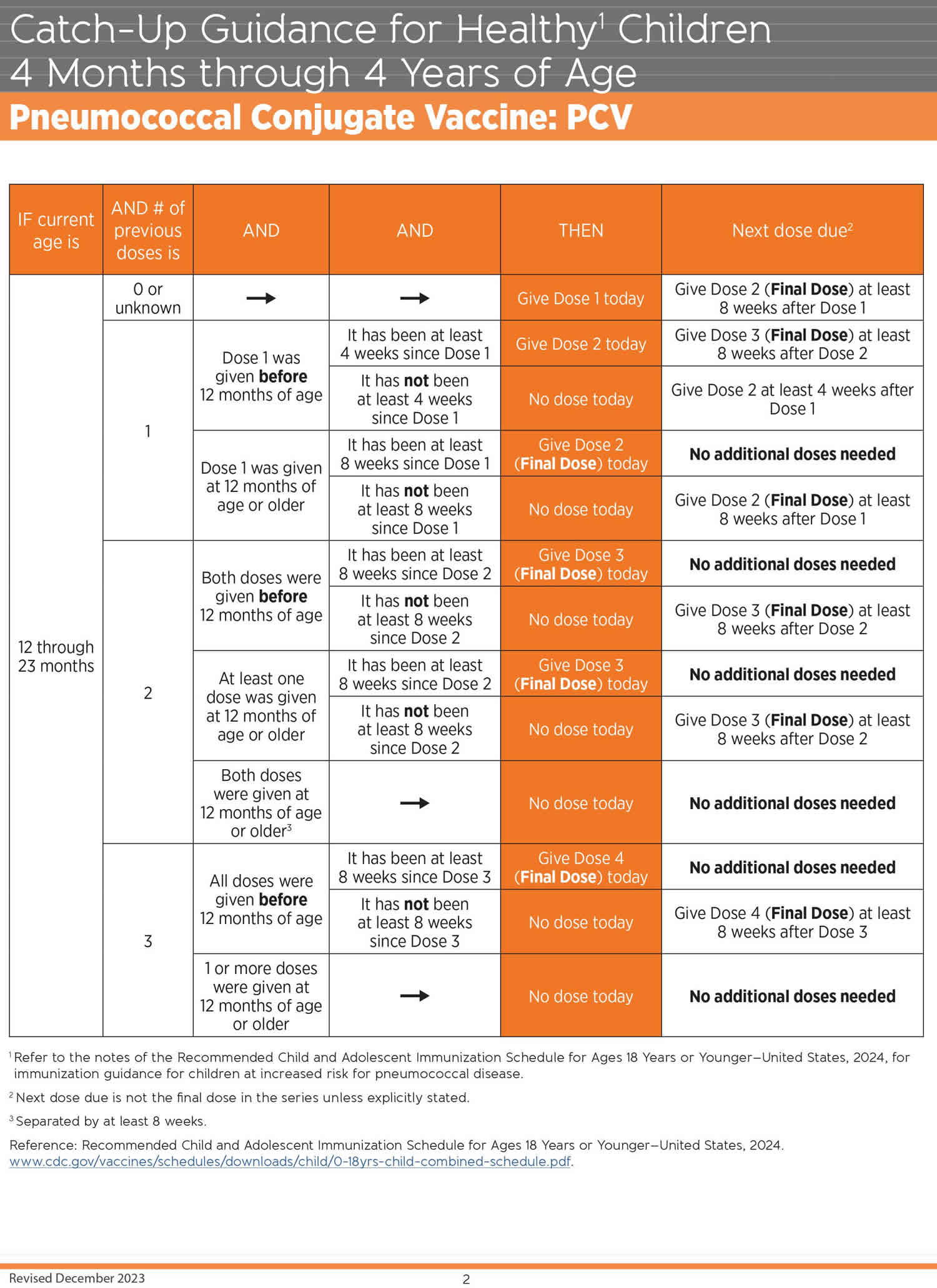
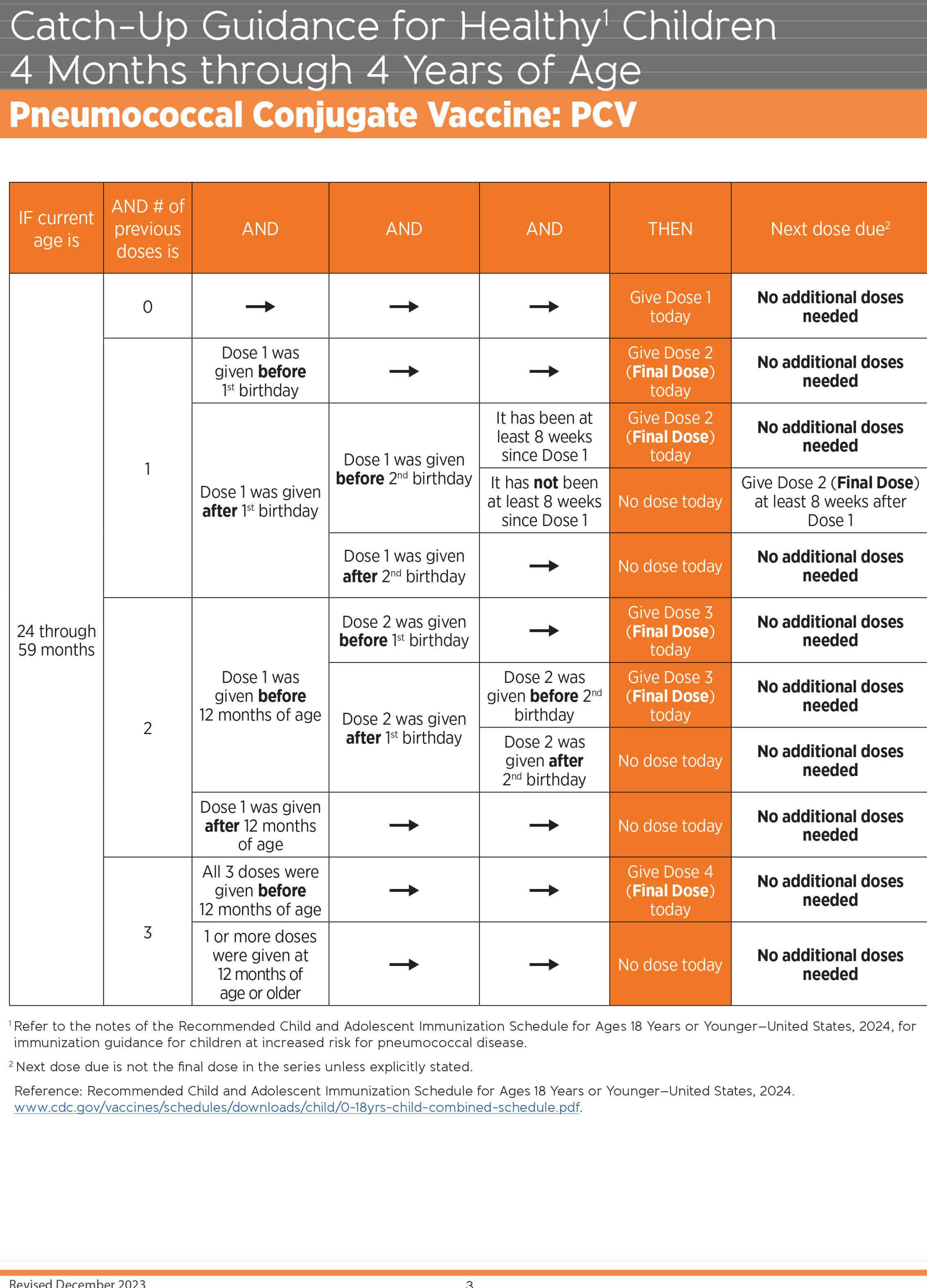
Catch-up guidance
Vaccinate children younger than 5 years of age who miss their shots or start the pneumococcal conjugate vaccine series later than recommended. The number of doses recommended and the intervals between doses will depend on the child’s age when vaccination begins. Otherwise healthy children who fall behind should be given catch-up vaccination through age 59 months; if they have certain underlying medical conditions they should be given catch-up vaccination through age 71 months.
Children may be at increased risk for febrile seizures if a pneumococcal conjugate vaccine is administered with inactivated influenza vaccine. However, clinicians may give either pneumococcal conjugate vaccine at the same time as an influenza vaccine.
Currently, no data from clinical trials are available for co-administration of Pneumovax23 (PPSV23) with other childhood vaccines during the same visit.
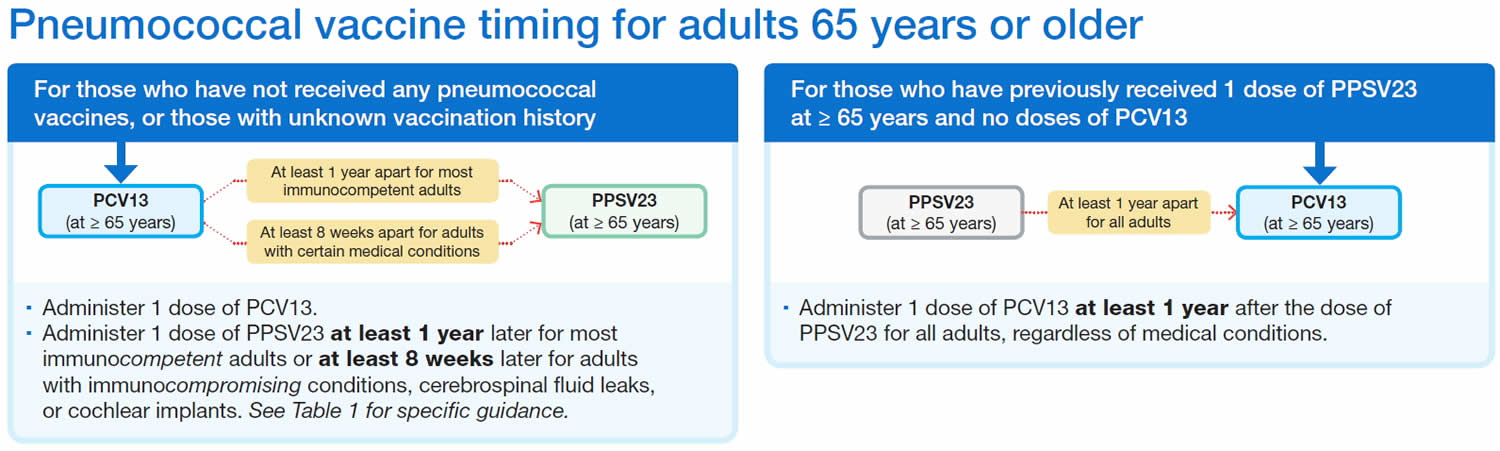
Pneumococcal vaccine schedule for adults 65 years or older
The CDC recommends PCV15 (Vaxneuvance), PCV20 (Prevnar 20) or PCV21 (Capvaxive) for all adults 65 years or older 3:
- Who have never received any pneumococcal conjugate vaccine (PCV)
- Whose previous vaccination history is unknown
If PCV15 (Vaxneuvance) is used, administer a dose of Pneumovax23 (PPSV23) one year later, if needed. Only one dose of Pneumovax23 (PPSV23) is indicated. If previously administered, another dose isn’t needed. If Pneumovax23 (PPSV23) is not available, one dose of PCV20 (Prevnar 20) or PCV21 (Capvaxive) may be given. Their pneumococcal vaccinations are complete 3.
The minimum interval is 8 weeks and can be considered in adults with 3:
- An immunocompromising condition
- A cochlear implant
- A cerebrospinal fluid leak
If PCV20 (Prevnar 20) or PCV21 (Capvaxive) is used, a dose of Pneumovax23 (PPSV23) isn’t indicated. Regardless of which vaccine is used (PCV20 or PCV21), their pneumococcal vaccinations are complete 3.
Recommendation for shared clinical decision-making
Based on shared clinical decision-making, adults 65 years or older have the option to get no additional pneumococcal vaccines, PCV20 (Prevnar 20) or PCV21 (Capvaxive). They can get PCV20 (Prevnar 20) or PCV21 (Capvaxive) if they have received both 3:
- PCV13 (Prevnar 13) (but not PCV15, PCV20, or PCV21) at any age and
- Pneumovax23 (PPSV23) at or after the age of 65 years old
Pneumococcal conjugate vaccines
Pneumococcal conjugate vaccine is a type of vaccine that joins (conjugates) a protein to an antigen and in the case of pneumococcal vaccines, the protein is connected to unique polysaccharides (long chains of sugar molecules) from the surface of each of the pneumococcal serotypes. The conjugate vaccines have the polysaccharides for different serotypes attached (conjugated) to a carrier protein. The protein helps improve the quality of the immune system response to the vaccine compared to the response to an unconjugated polysaccharide (PPV). Immune response to pneumococcal conjugate vaccine (PCV) is a T-cell dependent response that produces memory B-cells and reduces carriage of the bacteria in the respiratory track. Pneumococcal conjugate vaccines (PCVs) are given to children younger than 5 years old and to older children who need it. Vaccine providers also give pneumococcal conjugate vaccines (PCVs) to adults 65 years or older and other adults who need it.
In United States there are 3 types of pneumococcal conjugate vaccines (PCVs) that are differentiated by the number of serotypes they provide protection against — PCV15 (Vaxneuvance), PCV20 (Prevnar 20) and PCV21 (Capvaxive) 4, 5. PCV13 (Prevnar 13) is no longer routinely recommended; however, CDC guidance allows for its use as previously recommended in situations where PCV15, PCV20, or PCV21 is indicated but unavailable and the alternative is that the patient would not be vaccinated 9.
Pneumococcal 13-valent conjugate vaccine (Prevnar 13)
Pneumococcal 13-valent conjugate vaccine (Prevnar 13) includes purified capsular polysaccharide of 13 serotypes of Streptococcus pneumoniae (1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 19A, 19F, 18C, and 23F) conjugated to a nontoxic variant of diphtheria toxin known as CRM197. A 0.5 milliliter (mL) pneumococcal 13-valent conjugate vaccine (Prevnar 13) dose contains approximately 2.2 micrograms (mcg) of polysaccharide from each of 12 serotypes and approximately 4.4 mcg of polysaccharide from serotype 6B; the total concentration of CRM197 is approximately 34 mcg. The vaccine contains 0.02% polysorbate 80, 0.125 milligrams of aluminum as aluminum phosphate adjuvant, and 5 mL of succinate buffer. Pneumococcal 13-valent conjugate vaccine (Prevnar 13) is administered by intramuscular injection.
Researchers conducted a randomized placebo-controlled trial (CAPiTA trial) in the Netherlands among approximately 85,000 adults 65 years or older from 2008 through 2013 13. This trial evaluated the clinical benefit of pneumococcal 13-valent conjugate vaccine (Prevnar 13) in the prevention of pneumococcal pneumonia. The results of the CAPiTA trial demonstrated:
- 46% efficacy against vaccine-type pneumococcal pneumonia
- 45% efficacy against vaccine-type non-bacteremic pneumococcal pneumonia
- 75% efficacy against vaccine-type invasive pneumococcal disease
Studies show that getting at least 1 shot of pneumococcal 13-valent conjugate vaccine (Prevnar 13) protects 14, 15, 13:
- At least 8 in 10 babies from serious infections called invasive pneumococcal disease
- 3 in 4 adults 65 years or older against invasive pneumococcal disease
- 9 in 20 adults 65 years or older against pneumococcal pneumonia
Substantial evidence demonstrates routine infant pneumococcal 7-valent conjugate vaccine (PCV7) and pneumococcal 13-valent conjugate vaccine (Prevnar 13) vaccination reduced carriage and transmission of Streptococcus pneumoniae vaccine serotypes. This resulted in lower invasive pneumococcal disease incidence among unvaccinated persons of all ages, including infants too young to receive the vaccine 4.
The Centers for Disease Control and Prevention (CDC) recommends routine administration of pneumococcal 13-valent conjugate vaccine (Prevnar 13) for all children younger than 2 years of age 16:
- Give pneumococcal 13-valent conjugate vaccine (Prevnar 13) to infants as a series of 4 doses, one dose at each of these ages: 2 months, 4 months, 6 months, and 12 through 15 months.
- Children who miss their shots or start the series later should still get their pneumococcal 13-valent conjugate vaccine (Prevnar 13). The number of doses recommended and the intervals between doses will depend on the child’s age when vaccination begins.
- 1 dose for healthy children age 24–59 months with any incomplete* pneumococcal 13-valent conjugate vaccine (Prevnar 13) series (* Not having received all doses in either the recommended series or an age-appropriate catch-up series in the pneumococcal vaccine recommendations)
The CDC also recommends pneumococcal vaccination for children 2 through 5 years old who have certain medical conditions.
- For a child with any of these conditions 17:
- Cerebrospinal fluid leak
- Chronic heart disease, particularly cyanotic congenital heart disease and cardiac failure
- Chronic lung disease, including asthma if treated with prolonged high-dose oral corticosteroid therapy
- Cochlear implant
- Diabetes mellitus
- The CDC recommends you:
- Give 2 doses of pneumococcal 13-valent conjugate vaccine (Prevnar 13) if they are unvaccinated or received an incomplete pneumococcal 13-valent conjugate vaccine (Prevnar 13) series with <3 doses. Give the second dose at least 8 weeks after the first.
- Give 1 dose of pneumococcal 13-valent conjugate vaccine (Prevnar 13) if they received 3 doses of pneumococcal 13-valent conjugate vaccine (Prevnar 13) but none were given after 12 months of age.
- Give 1 dose of pneumococcal polysaccharide vaccine (Pneumovax23 or PPSV23) at least 8 weeks after the pneumococcal 13-valent conjugate vaccine (Prevnar 13) series is complete.
- For a child with any of these conditions 17:
- Chronic renal failure or nephrotic syndrome
- Congenital immunodeficiency
- B- (humoral) or T-lymphocyte deficiency
- Complement deficiency, particularly C1, C2, C3, or C4 deficiency
- Phagocytic disorder, excluding chronic granulomatous disease
- Congenital or acquired asplenia, or splenic dysfunction
- Diseases associated with treatment of immunosuppressive drugs or radiation therapy
- Hodgkin disease
- Leukemia
- Lymphoma
- Malignant neoplasm
- Solid organ transplant
- HIV infection
- Sickle cell disease or other hemoglobinopathies
- The CDC recommends you:
- Give 2 doses of pneumococcal 13-valent conjugate vaccine (Prevnar 13) if they are unvaccinated or received an incomplete pneumococcal 13-valent conjugate vaccine (Prevnar 13) series with <3 doses. Give the second dose at least 8 weeks after the first.
- Give 1 dose of pneumococcal 13-valent conjugate vaccine (Prevnar 13) if they received 3 doses of pneumococcal 13-valent conjugate vaccine (Prevnar 13) but none were given after 12 months of age.
- Give 2 doses of pneumococcal polysaccharide vaccine (Pneumovax23 or PPSV23) after the pneumococcal 13-valent conjugate vaccine (Prevnar 13) series is complete. Give the first dose at least 8 weeks after any prior pneumococcal 13-valent conjugate vaccine (Prevnar 13) dose, then give the second dose of PPSV23 at least 5 years after the first PPSV23 dose.
The CDC recommends pneumococcal vaccination for children 6 through 18 years old who have certain medical conditions.
- For a child with any of these conditions 17:
- Cerebrospinal fluid leak
- Cochlear implant
- CDC recommends you:
- Give 1 dose of pneumococcal 13-valent conjugate vaccine (Prevnar 13) if they have not received any doses of pneumococcal 13-valent conjugate vaccine (Prevnar 13). Administer pneumococcal 13-valent conjugate vaccine (Prevnar 13) before giving any recommended doses of pneumococcal polysaccharide vaccine (Pneumovax23 or PPSV23).
- Give 1 dose of pneumococcal polysaccharide vaccine (Pneumovax23 or PPSV23) (if not already given earlier in childhood) at least 8 weeks after pneumococcal 13-valent conjugate vaccine (Prevnar 13).
- For a child with any of these conditions 17:
- Chronic renal failure or nephrotic syndrome
- Congenital immunodeficiency
- B- (humoral) or T-lymphocyte deficiency
- Complement deficiency, particularly C1, C2, C3, or C4 deficiency
- Phagocytic disorder, excluding chronic granulomatous disease
- Congenital or acquired asplenia
- Diseases associated with treatment of immunosuppressive drugs or radiation therapy
- Hodgkin disease
- Leukemia
- Lymphoma
- Malignant neoplasm
- Solid organ transplant
- HIV infection
- Sickle cell disease or other hemoglobinopathies
- CDC recommends you:
- Give 1 dose of pneumococcal 13-valent conjugate vaccine (Prevnar 13) if they have not received any doses of pneumococcal 13-valent conjugate vaccine (Prevnar 13). Administer pneumococcal 13-valent conjugate vaccine (Prevnar 13) before giving any recommended doses of pneumococcal polysaccharide vaccine (Pneumovax23 or PPSV23).
- Ensure the child receives 2 doses of pneumococcal polysaccharide vaccine (Pneumovax23 or PPSV23). The first dose of PPSV23 should be given at least 8 weeks after any prior pneumococcal 13-valent conjugate vaccine (Prevnar 13) dose, then the second dose of PPSV23 should be given at least 5 years after the first dose of PPSV23.
- For a child with any of these conditions 17:
- Chronic heart disease, particularly cyanotic congenital heart disease and cardiac failure
- Chronic lung disease, including asthma if treated with prolonged high-dose oral corticosteroid therapy
- Diabetes mellitus
- CDC recommends you:
- Give 1 dose of pneumococcal polysaccharide vaccine (Pneumovax23 or PPSV23) (if not already given earlier in childhood). * One dose of pneumococcal 20-valent conjugate vaccine (Prevnar 20) may be used if pneumococcal polysaccharide vaccine (Pneumovax23 or PPSV23) is not available
Pneumococcal 15-valent conjugate vaccine (Vaxneuvance)
Pneumococcal 15-valent conjugate vaccine (Vaxneuvance) is a sterile suspension of purified capsular polysaccharides from 15 serotypes of Streptococcus pneumoniae (1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F, 22F, 23F, and 33F) individually conjugated to a nontoxic variant of diphtheria toxin known as CRM197 4, 6, 18. A 0.5 mL PCV15 (Vaxneuvance) dose contains 2.0 mcg of polysaccharide from each of 14 serotypes and 4.0 µg of polysaccharide from serotype 6B, 30 mcg of CRM197 carrier protein, 1.55 mg L-histidine, 1 mg of polysorbate 20, 4.50 mg sodium chloride, and 125 mcg of aluminum as aluminum phosphate adjuvant. The vaccine does not contain any preservatives.
PCV15 (Vaxneuvance) is for intramuscular injection only. Each dose of PCV15 (Vaxneuvance) is 0.5 mL.
- Children: Children need 4 doses of PCV15 (Vaxneuvance) vaccine 19:
- The first injection is given at 2 months old.
- The second injection is given at 4 months old.
- The third injection is given at 6 months old.
- The fourth injection is given at 12 through 15 months old.
- Adults: Administer VAXNEUVANCE as a single dose in adults 18 years of age and older.
Active ingredient(s): Bacterial sugars from 15 types of pneumococcus each linked to a protein (CRM 197 ). The sugars from these bacteria and the protein are not alive and do not cause disease.
Inactive ingredient(s): Sodium chloride, L-histidine, polysorbate 20 and aluminum (aluminum phosphate is included to help the vaccine work better).
PCV15 (Vaxneuvance) vaccine does not have any preservatives 18, 19. The tip cap and plunger stopper of the prefilled syringe are not made with natural rubber latex.
The most common side effects seen with PCV15 (Vaxneuvance) in children less than 2 years of age are 18, 19:
- Fever
- Pain, redness, swelling, or a lump where your child got the injection
- More fussy than usual
- More sleepy than usual
- Eating less than usual
The most common side effects seen with PCV15 (Vaxneuvance) in children and adolescents 2 through 17 years of age are 18, 19:
- Pain, swelling, redness or a lump where your child got the injection
- Muscle aches
- Feeling tired
- Headache
The most common side effects seen with PCV15 (Vaxneuvance) in adults 18 years of age and older are 18, 19:
- Pain, swelling or redness where you got the injection
- Feeling tired
- Muscle aches
- Headache
- Joint pain
In most people these side effects went away within three days. If you or your child have any side effects that become bothersome or any other unusual symptoms that develop after getting this injection, see your doctor. See your doctor right away if you or your child have symptoms of an allergic reaction which may include:
- Difficulty breathing
- Swelling of your face, lips, tongue or throat
- Hives
- Rash
There may be side effects that are not listed here. Ask your vaccine provider for more information.
Pneumococcal 20-valent conjugate vaccine (Prevnar20)
Pneumococcal 20-valent conjugate vaccine (Prevnar20) is a sterile suspension of saccharides from 20 serotypes of Streptococcus pneumoniae (1, 3, 4, 5, 6A, 6B, 7F, 8, 9V, 10A, 11A, 12F, 14, 15B, 18C, 19A, 19F, 22F, 23F, and 33F) individually linked to a nontoxic variant of diphtheria toxin known as CRM197 4, 6, 7, 20, 21. A 0.5 mL dose contains approximately 2.2 mcg of saccharides from each of 19 serotypes, approximately 4.4 mcg of saccharides from serotype 6B, 51 μg CRM197 carrier protein, 100 mcg polysorbate 80, 295 mcg succinate buffer, 4.4 mg sodium chloride, and 125 mcg aluminum as aluminum phosphate adjuvant.
PCV20 (Prevnar 20) is for intramuscular injection only. Each dose of PCV20 (Prevnar 20) is 0.5 mL.
- Children: 6 weeks through 15 months of age 20:
- The first injection is given at 2 months old.
- The second injection is given at 4 months old.
- The third injection is given at 6 months old.
- The fourth injection is given at 12 through 15 months old.
- Adults: Administer PCV20 (Prevnar 20) as a single dose in adults 18 years of age and older.
The most common side effects of PCV20 (Prevnar 20) are 20:
- In individuals 2, 4, 6, and 12 through 15 months of age vaccinated with a 4-dose schedule, the most commonly reported adverse reactions >10% were irritability (>60%), pain at the injection site (>30%), drowsiness (>30%), decreased appetite and injection site redness (>20%), injection site swelling (>10%), and fever (>10%). (6.1)
- In individuals 15 months through 17 years of age vaccinated with a single dose, the most commonly reported solicited adverse reactions >10% were irritability (>60% in individuals less than 2 years of age), pain at the injection site (>50%), drowsiness (>40% in individuals less than 2 years of age), fatigue and muscle pain (>20% in individuals 2 years of age and older), decreased appetite (>20% in individuals less than 2 years of age), injection site swelling and injection site redness (>10%) and headache (>10% in individuals 5 years of age and older), and fever (>10% in individuals less than 2 years of age).
- In individuals 18 through 59 years of age, the most commonly reported adverse reactions >10% were pain at the injection site (>70%), muscle pain (>50%), fatigue (>40%), headache (>30%), and arthralgia and injection site swelling (>10%).
- In individuals 60 years of age and older, the most commonly reported adverse reactions >10% were pain at the injection site (>50%), muscle pain and fatigue (>30%), headache (>20%), and arthralgia (>10%).
Pneumococcal 21-valent conjugate vaccine (CAPVAXIVE)
Pneumococcal 21-valent conjugate vaccine (CAPVAXIVE) was approved by the FDA on June 17, 2024 22, 8. Pneumococcal 21-valent conjugate vaccine (CAPVAXIVE) is indicated for the prevention of invasive pneumococcal disease caused by Streptococcus pneumoniae serotypes 3, 6A, 7F, 8, 9N, 10A, 11A, 12F, 15A,15B, 15C, 16F, 17F, 19A, 20A, 22F, 23A, 23B, 24F, 31, 33F, and 35B inindividuals 18 years of age and older 8.
Active ingredient(s): Bacterial sugars from 21 types of pneumococcus; each linked to a protein (CRM197). The sugars from these bacteria and the protein are not alive and do not cause disease 22.
Inactive ingredient(s): L-histidine, polysorbate 20, sodium chloride, water 22.
CAPVAXIVE does not have any preservatives 22. The tip cap and plunger stopper of the prefilled syringe are not made with natural rubber latex 22.
The most common side effects of CAPVAXIVE are 8:
- Pain, redness, or swelling where you got the injection
- Feeling tired
- Headache
- Muscle aches
- Fever
These side effects usually last less than 3 days. Tell your vaccine provider about these side effects or any unusual symptoms that develop after you get this vaccine. Get medical care right away if you have symptoms of an allergic reaction, which may include:
- Wheezing or trouble breathing
- Swelling of the face, lips, or tongue
- Hives
- Rash
There may be side effects not listed here. Ask your vaccine provider for more information.
Pneumococcal Polysaccharide Vaccine
Pneumococcal polysaccharide vaccine or Pneumovax23 (PPSV23) is a type of pneumococcal vaccine that is composed of long chains of sugar molecules called polysaccharides, that resemble the surface of certain serotypes of pneumococcal bacteria in order to help the immune system mount a response. Pneumovax23 (PPSV23) contains polysaccharide antigen from 23 types of pneumococcal bacteria 10, 23. It contains 25 µg of each antigen per dose and contains 0.25% phenol as a preservative. The immune response to the Pneumovax23 (PPSV23) vaccine is a T-cell independent immune response but does not reduce bacterial carriage.
PPSV23 (Pneumovax23) was first licensed in the US in 1983. Following the 2022 changes to the pneumococcal vaccination schedule for adults, PPSV23 (Pneumovax23) is no longer recommended alone, however PPSV23 (Pneumovax23) is recommended for adults following PCV13 (Prevnar 13) or PCV15 (Vaxneuvance) vaccination. PPSV23 (Pneumovax23) is not recommended for people who have previously received a PCV20 (Prevnar 20) or PCV21 (Capvaxive) vaccination.
Vaccine providers may give Pneumovax23 (PPSV23) to children 2 through 18 years old with certain medical conditions. Vaccine providers give it to adults who receive PCV15 (Vaxneuvance). They also may give it to adults who have received an earlier vaccine called PCV13 (Prevnar 13). PCV13 (Prevnar 13) is FDA-licensed and may still be available in some clinics. PCV13 (Prevnar 13) is no longer routinely recommended; however, CDC guidance allows for its use as previously recommended in situations where PCV15, PCV20, or PCV21 is indicated but unavailable and the alternative is that the patient would not be vaccinated 9.
Pneumococcal polysaccharide vaccine (Pneumovax 23)
Pneumococcal polysaccharide vaccine (Pneumovax23 or PPSV23) includes purified preparations of pneumococcal capsular polysaccharide. PPSV23 contains polysaccharide antigen from 23 types of pneumococcal bacteria (1, 2, 3, 4, 5, 6B, 7F, 8, 9N, 9V, 10A, 11A, 12F, 14, 15B, 17F, 18C, 19F, 19A, 20, 22F, 23F, and 33F) 10, 23. Pneumococcal polysaccharide vaccine (Pneumovax23) contains 25 mcg of each antigen per dose and contains 0.25% phenol as a preservative. The vial stoppers, syringe plunger stopper and syringe tip cap are not made with natural rubber latex 23, 24.
Pneumococcal polysaccharide vaccine (Pneumovax 23) is administered by either intramuscular or subcutaneous injection 23.
More than 80% of healthy adults who receive the pneumococcal polysaccharide vaccine (Pneumovax23) develop antibodies against the serotypes contained in the vaccine 4. This immune response usually occurs within 2 to 3 weeks after vaccination. Older adults and persons with some chronic illnesses or immunodeficiency may not respond as well. Elevated antibody levels persist for at least 5 years in healthy adults but decline more quickly in persons with certain underlying illnesses. Children younger than 2 years of age generally have a poor antibody response to pneumococcal polysaccharide vaccine (Pneumovax23).
Pneumococcal polysaccharide vaccine (Pneumovax23) vaccine efficacy studies have resulted in various estimates of clinical effectiveness 25, 26, 27, 28. Overall, the vaccine is 60% to 70% effective in preventing invasive disease caused by serotypes in the vaccine 4. Pneumococcal polysaccharide vaccine (Pneumovax23) shows reduced effectiveness among immunocompromised persons; however, because of their increased risk of invasive pneumococcal disease, the CDC recommends pneumococcal polysaccharide vaccine (Pneumovax23) for people in these groups who receive pneumococcal 15-valent conjugate vaccine (Vaxneuvance). There is no consensus regarding the ability of pneumococcal polysaccharide vaccine (Pneumovax23) to prevent non-bacteremic pneumococcal pneumonia.
Studies comparing patterns of asymptomatic pneumococcal carriage before and after pneumococcal polysaccharide vaccine (Pneumovax23) vaccination have not shown decreases in carrier rates among those vaccinated 4.
Pneumococcal polysaccharide vaccine (Pneumovax 23) side effects
Problems following pneumococcal polysaccharide vaccine (Pneumovax23) can include 23, 24:
- Reactions where the shot was given
- Redness
- Pain
- Feeling tired
- Fever
- Muscle aches
The most common adverse reactions, reported in >10% of subjects vaccinated with Pneumovax23 for the first time in a clinical trial, were: injection-site pain/soreness/tenderness (60.0%), injection-site swelling/induration (20.3%), headache (17.6%), injection-site erythema (16.4%), asthenia/fatigue (13.2%), and myalgia (11.9%) 23.
If these problems occur, they usually go away within about 2 days.
Problems that could happen after getting any injected vaccine
- People sometimes faint after medical procedures, including vaccination. Sitting or lying down for about 15 minutes can help prevent fainting and injuries caused by a fall. Tell your doctor if you or your child:
- Feel dizzy
- Have vision changes
- Have ringing in the ears
- As with any medicine, there is a very remote chance of a vaccine causing a severe allergic reaction, other serious injury, or death.
Where can I find pneumococcal vaccines?
Your healthcare professional’s office is usually the best place to receive recommended vaccines for you or your child.
Pneumococcal conjugate vaccine is part of the routine childhood immunization schedule. Therefore, it is regularly available for children at:
- Pediatric offices
- Family practice offices
- Community health clinics
- Public health departments
If your healthcare professional does not have pneumococcal vaccines for adults, ask for a referral.
Pneumococcal vaccines may also be available for adults at:
- Pharmacies
- Workplaces
- Community health clinics
- Health departments
- Other community locations such as schools and religious centers
Federally funded health centers can also provide services if you don’t have a regular source of health care. Locate one near you here (https://www.vaccines.gov/getting/where/index.html). You can also contact your state health department here (https://www.cdc.gov/vaccines/imz-managers/awardee-imz-websites.html) to learn more about where to get pneumococcal vaccines in your community.
When receiving any vaccine, ask the provider to record the vaccine in the state or local registry, if available. This helps healthcare professionals know what vaccines you or your child has already received.
How do I pay for these pneumococcal vaccines?
There are several ways to cover the cost of pneumococcal vaccines:
Medicare
Medicare Part B covers 100% of the cost for both pneumococcal vaccines (when administered at least 12 months apart).
Private Health Insurance
Most private health insurance plans cover pneumococcal vaccines. Check with your insurance provider for details on whether there is any cost to you and for a list of in-network vaccine providers.
Vaccines for Children Program
The Vaccines for Children (VFC) Program provides vaccines to children whose parents or guardians may not be able to afford them. A child is eligible if they are younger than 19 years old and meets one of the following requirements:
- Medicaid-eligible
- Uninsured
- American Indian or Alaska Native
- Underinsured (have health insurance that does not cover vaccines or does not cover certain vaccines)
If your child is VFC-eligible, ask if your healthcare professional is a VFC provider. For help in finding a VFC provider near you, contact your state or local health department’s VFC Program Coordinator here: https://www.cdc.gov/vaccines/imz-managers/awardee-imz-websites.html
How well do these pneumococcal vaccines work?
Some pneumococcal infections are “invasive.” Invasive disease means that germs invade parts of the body that are normally free from germs. Invasive disease is usually very serious and can sometimes result in death.
Vaccines that help protect against pneumococcal disease work well, but cannot prevent all cases.
Studies show that at least 1 dose of pneumococcal conjugate vaccine protects 29, 30, 31:
- At least 8 in 10 babies from serious infections called invasive pneumococcal disease
- 75 in 100 adults 65 years or older against invasive pneumococcal disease
- 45 in 100 adults 65 years or older against pneumococcal pneumonia
Studies* show that 1 dose of pneumococcal polysaccharide vaccine protects
Between 50 to 85 in 100 healthy adults against invasive pneumococcal disease
* Studies looked at protection against infections caused by the serotypes covered by the specific vaccine used.
Which underlying medical conditions indicate that a child age 6 through 18 years should receive additional doses of pneumococcal vaccine beyond the routine schedule?
Medical conditions that increase the risk of pneumococcal disease and are indications for additional pneumococcal vaccine doses beyond the routine schedule are broken down into two categories: non-immunocompromising (non-IC) and immunocompromising (IC) 32. Recommendations differ slightly under certain circumstances by non-immunocompromising (non-IC) or immunocompromising (IC) category.
Non-immunocompromising (non-IC) conditions include 32:
- Cerebrospinal fluid (CSF) leak
- Chronic heart disease (especially cyanotic congenital heart disease and heart failure)
- Chronic kidney disease (except as specified in the immunocompromising (IC) list below)
- Chronic liver disease
- Chronic lung disease (including moderate persistent or severe persistent asthma)
- Diabetes mellitus
- Cochlear implant
Immunocompromising (IC) conditions include 32:
- Kidney disease and on maintenance dialysis
- Kidney disease with nephrotic syndrome
- Asplenia or splenic dysfunction
- Congenital or acquired immunodeficiency, including B-(humoral) or T-lymphocyte deficiency; complement deficiencies, particularly C1, C2, C3, and C4 deficiency; and phagocytic disorders (excluding chronic granulomatous disease)
- Treatment with immunosuppressive drugs or radiation therapy (including treatment for Hodgkin disease, leukemias, lymphomas, malignant neoplasm, and solid organ transplant)
- HIV infection
- Sickle cell disease or other hemoglobinopathies
An older child through age 18 years with any high-risk condition who completed a pneumococcal conjugate vaccine (PCV) series before age 6 years that included any dose of PCV20 (Prevnar 20), is not recommended to receive any additional pneumococcal conjugate vaccine (PCV) doses.
Children with non-immunocompromising (non-IC) or immunocompromising (IC) conditions who completed a pneumococcal conjugate vaccine (PCV) series before age 6 years with PCV13 (Prevnar 13) or PCV15 (Vaxneuvance) but who have not received PCV20 (Prevnar 20) or pneumococcal polysaccharide vaccine Pneumovax23 (PPSV23) should receive additional pneumococcal vaccination with a single dose of PCV20 at least 8 weeks after the most recent pneumococcal conjugate vaccine (PCV) dose. If PCV20 (Prevnar 20) is not available, a non-IC or IC child in this circumstance may, alternatively, receive a single dose of Pneumovax23 (PPSV23) at least 8 weeks after the most recent pneumococcal conjugate vaccine (PCV) dose. An immunocompromised (IC) child given Pneumovax23 (PPSV23) in this circumstance would also be due for a dose of either PCV20 (Prevnar 20) or a second dose of Pneumovax23 (PPSV23) at least 5 years after the first Pneumovax23 (PPSV23).
Doses of the PCV7 (Prevnar 7) do not count toward pneumococcal conjugate vaccine (PCV) vaccination when determining the current pneumococcal vaccination needs of a child or teen with a qualifying non-IC or IC condition.
When feasible, administer any needed pneumococcal vaccination at least two weeks before initiating planned interventions that place a child at high risk (such as a cochlear implant or spleen removal).
What are the different serotypes of Streptococcus pneumoniae targeted by different pneumococcal vaccines?
Streptococcus pneumoniae bacteria are serotyped based on the polysaccharides in the outer capsule of the bacteria. Serotypes vary in how common they are and in what percentage of pneumococcal disease they cause.
Among the pneumococcal conjugate vaccines (PCVs), PCV13 (Prevnar 13) includes serotypes: 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F and 23F. PCV15 (Vaxneuvance) includes all PCV13 serotypes plus 22F and 33F. PCV20 (Prevnar 20) includes all PCV15 serotypes plus 8, 10A, 11A, 12F, and 15B.
Pneumovax23 (PPSV23) vaccine does not contain serotype 6A, but contains 19 other serotypes present in PCV20, plus serotypes 2, 9N, 17F, and 20.
PCV21 (Capvaxive) is designed to target additional Streptococcus pneumoniae serotypes causing a significant proportion of disease in adults that are not prevented by the vaccines approved for children. PCV21 (Capvaxive)does not contain 10 serotypes found in other pneumococcal vaccines approved for children (1, 4, 5, 6B, 9V, 14, 18C, 19F, 23F, 15B, or 2). Instead, it contains an additional 11 serotypes not found in PCV20 (Prevnar 20): 9N, 17F, 20, 15A, 15C, 16F, 23A, 23B, 24F, 31, and 35B. Because of these differences, CDC estimates that PCV20 (Prevnar 20) targets serotypes that cause between 54% and 65% of invasive pneumococcal disease in adults, and PCV21 (Capvaxive) targets serotypes that cause between 77% and 85% of invasive pneumococcal disease in adults 32.
How effective are pneumococcal conjugate vaccines at preventing pneumococcal carriage or disease?
The United States Food and Drug Administration (FDA) licensed the first pneumococcal conjugate vaccine (PCV) against seven pneumococcus bacteria serotypes (PCV7, Prevnar 7) in 2000. A large clinical trial showed PCV7 (Prevnar7) reduced invasive disease caused by vaccine serotypes by 97%. Compared to unvaccinated children, children who received PCV7 (Prevnar 7) 32:
- Had 20% fewer episodes of chest X-ray confirmed pneumonia
- Had 7% fewer episodes of acute otitis media
- Underwent 20% fewer tympanostomy tube placements
FDA licensed PCV13 (Prevnar 13) based on studies comparing the serologic response of children who received PCV13 (Prevnar 13) to those who received PCV7 (Prevnar 7). Substantial evidence demonstrates that routine infant PCV7 and PCV13 vaccination reduces the carriage and transmission of vaccine serotypes.
Researchers conducted a randomized placebo-controlled trial (CAPiTA trial) in the Netherlands among approximately 85,000 adults 65 years or older from 2008 through 2013 33. The Community-Acquired Pneumonia Immunization Trial in Adults (CAPiTA trial) evaluated the clinical benefit of PCV13 (Prevnar 13) in the prevention of pneumococcal pneumonia. The results of the CAPiTA trial demonstrated 33:
- 46% efficacy against vaccine-type pneumococcal pneumonia
- 45% efficacy against vaccine-type non-bacteremic pneumococcal pneumonia
- 75% efficacy against vaccine-type invasive pneumococcal disease (IPD, i.e., bacteremia or meningitis)
FDA licensed PCV15 (Vaxneuvance) and PCV20 (Prevnar 20) in 2021 based on studies comparing the serologic response of adults who received either PCV15 or PCV20 to those who received PCV13 (Prevnar 13). These studies showed PCV15 (Vaxneuvance) and PCV20 (Prevnar 20) induced antibody levels comparable to those induced by PCV13 (Prevnar 13) and shown to be protective against invasive disease. FDA subsequently expanded the indication for use of PCV15 and PCV20 to include children starting at age 6 weeks in 2022 and 2023, respectively, based on serologic studies. PCV21 (Capvaxive) was licensed in 2024 based on a similar evaluation of serologic response to vaccination.
How effective is pneumococcal polysaccharide vaccine at preventing pneumococcal carriage or disease?
According to CDC, more than 80% of healthy adults who receive Pneumovax23 (PPSV23) develop antibodies against the serotypes contained in the vaccine that persist for at least 5 years 32. Older adults and people with some chronic illnesses or immunodeficiency may not respond as well and their antibody levels may decline more quickly.
Overall, the Pneumovax23 (PPSV23) vaccine is 60% to 70% effective in preventing invasive pneumococcal disease caused by serotypes in the vaccine 32. Pneumovax23 (PPSV23) shows less effectiveness among immunocompromised people; however, because of their increased risk of invasive pneumococcal disease, CDC recommends Pneumovax23 (PPSV23) for people in these groups who receive PCV15 (Vaxneuvance). There has not been consensus regarding the ability of Pneumovax23 (PPSV23) to prevent non-bacteremic pneumococcal pneumonia; however, recent observational studies reported 21%–46% effectiveness against Pneumovax23 (PPSV23)-type pneumococcal pneumonia when PPSV23 was given less than 5 years before illness onset.
Unlike pneumococcal conjugate vaccines (PCVs), Pneumovax23 (PPSV23) vaccination has not been shown to decrease nasal carriage of pneumococcal bacteria among those vaccinated 32.
Pneumococcal vaccine composition
Pneumococcal Conjugate Vaccine
Pneumococcal conjugate vaccine (PCV13 or Prevnar13®) includes purified capsular polysaccharide of 13 serotypes of Streptococcus pneumoniae (1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 19A, 19F, 18C, and 23F) conjugated to a nontoxic variant of diphtheria toxin known as CRM197. A 0.5-milliliter (mL) PCV13 dose contains approximately 2.2 micrograms (µg) of polysaccharide from each of 12 serotypes and approximately 4.4 µg of polysaccharide from serotype 6B; the total concentration of CRM197 is approximately 34 μg. The vaccine contains 0.02% polysorbate 80, 0.125 milligrams of aluminum as aluminum phosphate adjuvant, and 5 mL of succinate buffer. The vaccine does not contain thimerosal preservative.
Pneumococcal Polysaccharide Vaccine
Pneumococcal polysaccharide vaccine (PPSV23 or Pneumovax23®) includes purified preparations of pneumococcal capsular polysaccharide. PPSV23 contains polysaccharide antigen from 23 types of pneumococcal bacteria. It contains 25 µg of each antigen per dose and contains 0.25% phenol as a preservative.
Pneumococcal vaccine administration
Use a needle length appropriate for the age and size (22–25 Gauge) of the person receiving the pneumococcal vaccine. NEVER administer a pneumococcal conjugate vaccine (PCV15, PCV20, or PCV21) and Pneumovax23 (PPSV23) during the same visit 34. If someone is indicated to receive PCV15 (Vaxneuvance) and Pneumovax23 (PPSV23), administer PCV15 (Vaxneuvance) first followed by Pneumovax23 (PPSV23).
- Administer pneumococcal polysaccharide vaccine Pneumovax23 (PPSV23) intramuscularly or subcutaneously 34.
- Administer pneumococcal conjugate vaccines (PCV15 [Vaxneuvance] or PCV20 [Prevnar 20]) intramuscularly 34.
- For infants and young children, use the vastus lateralis muscle in the anterolateral thigh.
- For older children and adults, use the deltoid muscle.
- Administer pneumococcal conjugate vaccine (PCV21 [Capvaxive]) to adults intramuscularly using the deltoid muscle.
The primary series of PCV15 (Vaxneuvance) or PCV20 (Prevnar 20) consists of 3 doses routinely given at 2, 4, and 6 months of age. You can administer the first dose as early as 6 weeks of age. CDC recommends a fourth (booster) dose at 12 through 15 months of age. For children vaccinated when they are younger than 12 months of age, the minimum interval between doses is 4 weeks. Separate doses given at 12 months of age and older by at least 8 weeks.
The number and timing of doses for older children and adults depends on the medical indication, prior pneumococcal vaccination, and age.
For children (2 through 18 years old), the interval between PCV15 (Vaxneuvance) and Pneumovax23 (PPSV23) should be at least 8 weeks. If Pneumovax23 (PPSV23) is inadvertently administered first, wait at least 8 weeks to administer PCV15 (Vaxneuvance).
For adults, the recommended interval is at least 1 year. An 8-week minimum interval can be considered for adults with an immunocompromising condition, cochlear implant, or cerebrospinal fluid leak. If Pneumovax23 (PPSV23) is inadvertently administered first, wait at least 1 year to administer PCV15 (Vaxneuvance).
In adults, you can administer a pneumococcal vaccine (PCV15, PCV20, PCV21, or PPSV23) during the same visit with influenza vaccination or other recommended vaccines. Administer each vaccine with a separate syringe and, if feasible, at a different injection site. Annual influenza vaccination is important to help prevent the flu. Additionally, since having the flu increases the risk of getting pneumococcal disease, receiving a flu vaccine is important for preventing pneumococcal disease.
Pneumococcal vaccine contraindications and precautions
You should NOT get PCV13 [Prevnar 13]:
- If you ever had a severe allergic reaction (e.g., anaphylaxis) after a previous dose of PCV7 or PCV13 or to any vaccine containing diphtheria toxoid
- If you have a severe allergy to any component of this vaccine
- Anyone who has had a life-threatening allergic reaction to any of the following should not get PCV13:
- A dose of this vaccine
- An earlier pneumococcal conjugate vaccine called PCV7 (or Prevnar®)
- Any vaccine containing diphtheria toxoid (for example, DTaP)
- Anyone with a severe allergy to any component of PCV13 should not get the vaccine. Your or your child’s healthcare professional can tell you about the vaccine’s components.
You should NOT get PCV15 (Vaxneuvance), PCV20 (Prevnar 20) or PCV21 (Capvaxive) if you’ve:
- Had a life-threatening allergic reaction after any type of pneumococcal conjugate vaccination (PCV)
- Had a life-threatening allergic reaction to any vaccine containing diphtheria toxoid (DTaP)
- Have a severe allergy to any part of these vaccines
You should NOT get Pneumovax23 (PPSV23) if you:
- Are younger than 2 years old
- Had a life-threatening allergic reaction (e.g., anaphylaxis) after getting Pneumovax23 (PPSV23)
- Have a severe allergy to any part of Pneumovax23 (PPSV23)
You or your child are not feeling well.
- People who have a mild illness, such as a cold, can probably get the vaccine. People who have a more serious illness should probably wait until they recover. Your or your child’s doctor can advise you.
You are pregnant.
- There is no evidence that PPSV23 is harmful either to a pregnant woman or to her baby. However, as a precaution, women who need the vaccine should get it before becoming pregnant, if possible.
You may have pneumococcal vaccines, if your healthcare provider and parent or you deem the benefits of vaccination to outweigh the risks.
- People who have a mild illness, such as a cold, can probably get the vaccine. People who have a more serious illness should probably wait until they recover. Your or your child’s healthcare professional can advise you.
Pneumococcal vaccine schedule
The Centers for Disease Control and Prevention (CDC) recommends pneumococcal vaccination for 11:
- Children
- All children younger than 5 years old
- Children 5 through 18 years old with certain risk conditions
- Adults
- All adults 65 years or older
- 19 through 64 years old with certain risk conditions
The latest Pneumococcal Vaccine Recommendation by the Centers for Disease Control and Prevention (CDC) is to use PCV15 (Vaxneuvance) or PCV20 (Prevnar 20) for routine pneumococcal vaccination for all children younger than 5 years of age 3, 12. And for all adults 65 years or older who have never received any pneumococcal conjugate vaccine (PCV) or whose previous vaccination history is unknown administer PCV15 (Vaxneuvance), PCV20 (Prevnar 20) or PCV21 (Capvaxive) 3, 12.
CDC recommends pneumococcal vaccination for all children younger than 5 years old with 4-dose of either PCV15 (Vaxneuvance) or PCV20 (Prevnar 20), 1 dose at each of the following ages 3:
- 2 months
- 4 months
- 6 months
- a booster at 12 through 15 months.
Catch-up guidance
Vaccinate children younger than 5 years of age who miss their shots or start the series later than recommended. The number of doses recommended and the intervals between doses will depend on the child’s age when vaccination begins.
All adults 65 years or older who have never received any pneumococcal conjugate vaccine (PCV) or whose previous vaccination history is unknown administer PCV15 (Vaxneuvance), PCV20 (Prevnar 20) or PCV21 (Capvaxive) 3, 12.
If PCV15 (Vaxneuvance) is used, administer a dose of Pneumovax23 (PPSV23) one year later, if needed. Only one dose of Pneumovax23 (PPSV23) is indicated. If previously administered, another dose isn’t needed. If Pneumovax23 (PPSV23) is not available, one dose of PCV20 (Prevnar 20) or PCV21 (Capvaxive) may be given. Their pneumococcal vaccinations are complete 3.
The minimum interval is 8 weeks and can be considered in adults with 3:
- An immunocompromising condition
- A cochlear implant
- A cerebrospinal fluid leak
If PCV20 (Prevnar 20) or PCV21 (Capvaxive) is used, a dose of Pneumovax23 (PPSV23) isn’t indicated. Regardless of which vaccine is used (PCV20 or PCV21), their pneumococcal vaccinations are complete 3.
Recommendation for shared clinical decision-making
Based on shared clinical decision-making, adults 65 years or older have the option to get no additional pneumococcal vaccines, PCV20 (Prevnar 20) or PCV21 (Capvaxive). They can get PCV20 (Prevnar 20) or PCV21 (Capvaxive) if they have received both 3:
- PCV13 (Prevnar 13) (but not PCV15, PCV20, or PCV21) at any age and
- Pneumovax23 (PPSV23) at or after the age of 65 years old
Pneumococcal vaccine guidelines
The Centers for Disease Control and Prevention (CDC) recommends pneumococcal vaccination for 11:
- Children
- All children younger than 5 years old
- Children 5 through 18 years old with certain risk conditions
- Adults
- All adults 65 years or older
- 19 through 64 years old with certain risk conditions
The latest Pneumococcal Vaccine Recommendation by the Centers for Disease Control and Prevention (CDC) is to use PCV15 (Vaxneuvance) or PCV20 (Prevnar 20) for routine pneumococcal vaccination for all children younger than 5 years of age 3, 12. And for all adults 65 years or older who have never received any pneumococcal conjugate vaccine (PCV) or whose previous vaccination history is unknown administer PCV15 (Vaxneuvance), PCV20 (Prevnar 20) or PCV21 (Capvaxive) 3, 12.
Pneumococcal vaccine by age
Pneumococcal vaccination schedules for children and adults are very complicated and as newer pneumococcal conjugate vaccines are licensed and added to the CDC recommendation, assessing what is needed for an individual patient of any age requires their age, pneumococcal vaccination history, and knowledge of any relevant high-risk conditions. There are several resources available from CDC: https://www2a.cdc.gov/vaccines/m/pneumo/pneumo.html
The PneumoRecs VaxAdvisor app for your mobile device allows you to answer basic questions about the age, health conditions, and pneumococcal vaccination history for an individual patient (https://www.cdc.gov/pneumococcal/hcp/vaccine-recommendations/app.html). The PneumoRecs VaxAdvisor app provides patient-specific guidance consistent with the immunization schedule recommended by the U.S. Advisory Committee on Immunization Practices (ACIP). CDC releases guideline changes and enhancements to the app itself through app updates. Use the app to eliminate the challenge of interpreting and synthesizing multiple pneumococcal vaccination recommendation statements.
Children Younger than 2 Years Old
CDC recommends routine administration of pneumococcal conjugate vaccine (PCV13 or Prevnar13®) for all children younger than 2 years of age:
- Give PCV13 [Prevnar 13] to infants as a series of 4 doses, one dose at each of these ages:
- 2 months,
- 4 months,
- 6 months, and
- 12 through 15 months.
- Children who miss their shots or start the series later should still get the vaccine. The number of doses recommended and the intervals between doses will depend on the child’s age when vaccination begins (see pneumococcal vaccine catch-up guidance below).
Children 2 through 4 Years Old without Certain Medical Conditions
CDC recommends PCV13 [Prevnar 13]vaccination for children 2 through 4 years old who are unvaccinated or received an incomplete PCV13 series.
- Have 1 dose of PCV13 [Prevnar 13].
Children 2 through 5 Years Old with Certain Medical Conditions
CDC recommends pneumococcal vaccination for children 2 through 5 years old who have certain medical conditions.
For a child with any of these conditions:
- Chronic heart disease
- Chronic lung disease
- Diabetes mellitus
- Cerebrospinal fluid leaks
- Cochlear implant(s)
CDC recommends you:
- Have 2 doses of PCV13 [Prevnar 13] if they are unvaccinated or received an incomplete PCV13 series with <3 doses. Have the second dose at least 8 weeks after the first.
- Have 1 dose of PCV13 [Prevnar 13] if they received 3 doses of PCV13 but none were given after 12 months of age.
- Have 1 dose of PPSV23 [Pneumovax 23] at least 8 weeks after the PCV13 series is complete.
For a child with any of these conditions:
- Sickle cell disease or other hemoglobinopathies
- Congenital or acquired asplenia, or splenic dysfunction
- HIV infection
- Chronic renal failure or nephrotic syndrome
- Diseases associated with treatment with immunosuppressive drugs or radiation therapy, including malignant neoplasm, leukemia, lymphomas, and
- Hodgkin’s disease, or solid organ transplantation
- Congenital immunodeficiency
CDC recommends you:
- Have 2 doses of PCV13 [Prevnar 13] if they are unvaccinated or received an incomplete PCV13 series with <3 doses. Have the second dose at least 8 weeks after the first.
- Have 1 dose of PCV13 if they received 3 doses of PCV13 but none were given after 12 months of age.
- Have 2 doses of PPSV23 [Pneumovax 23] after the PCV13 series is complete. Have the first dose at least 8 weeks after any prior PCV13 dose, then give the second dose of PPSV23 at least 5 years after the first.
Children 6 through 18 Years Old with Certain Medical Conditions
CDC recommends pneumococcal vaccination for children 6 through 18 years old who have certain medical conditions.
For a child with any of these conditions:
- Cerebrospinal fluid leaks
- Cochlear implant(s)
CDC recommends you:
- Have 1 dose of PCV13 [Prevnar 13] if they have not received any doses of PCV13. Administer PCV13 before giving any recommended doses of PPSV23.
- Have 1 dose of PPSV23 [Pneumovax 23] (if not already given earlier in childhood) at least 8 weeks after PCV13.
For a child with any of these conditions:
- Sickle cell disease or other hemoglobinopathies
- Congenital or acquired asplenia, or splenic dysfunction
- HIV infection
- Chronic renal failure or nephrotic syndrome
- Diseases associated with treatment with immunosuppressive drugs or radiation therapy, including malignant neoplasm, leukemia, lymphomas, and
- Hodgkin’s disease, or solid organ transplantation
- Congenital immunodeficiency
CDC recommends you:
- Have 1 dose of PCV13 [Prevnar 13] if they have not received any doses of PCV13. Administer PCV13 before giving any recommended doses of PPSV23.
- Ensure the child receives 2 doses of PPSV23 [Pneumovax 23]. The first dose of PPSV23 should be given at least 8 weeks after any prior PCV13 dose, then the second dose of PPSV23 should be given at least 5 years after the first.
For a child with any of these conditions:
- Chronic heart disease
- Chronic lung disease
- Diabetes mellitus
- Alcoholism
- Chronic liver disease
- Cigarette smoking
CDC recommends you:
- Have 1 dose of PPSV23 [Pneumovax 23] (if not already given earlier in childhood).
Adults 19 through 64 Years
CDC recommends pneumococcal vaccination for adults 19 through 64 years old who have certain medical conditions or who smoke.
For anyone with any of the conditions listed below who has not previously received the recommended pneumococcal vaccines:
- Cerebrospinal fluid leaks
- Cochlear implant(s)
CDC recommends you:
- Have 1 dose of PCV13 [Prevnar 13] and 1 dose of PPSV23 [Pneumovax 23]. Administer PCV13 first, then give the PPSV23 dose at least 8 weeks later.
For anyone with any of the conditions listed below who has not previously received the recommended pneumococcal vaccines:
- Sickle cell disease or other hemoglobinopathies
- Congenital or acquired asplenia
- Congenital or acquired immunodeficiency
- HIV infection
- Chronic renal failure or nephrotic syndrome
- Leukemia or lymphoma
- Hodgkin’s disease
- Generalized malignancy
- Iatrogenic immunosuppression (diseases requiring treatment with immunosuppressive drugs, including long-term systemic corticosteroids and radiation therapy)
- Solid organ transplantation
- Multiple myeloma
CDC recommends you:
- Have 1 dose of PCV13 [Prevnar 13] and 2 doses of PPSV23 [Pneumovax 23]. Administer PCV13 first, then give the first PPSV23 dose at least 8 weeks later. Have the second dose of PPSV23 at least 5 years after the first.
For anyone who smokes and has not previously received the recommended pneumococcal vaccine
CDC recommends you:
- Have 1 dose of PPSV23 [Pneumovax 23].
For anyone with any of the conditions listed below who has not previously received the recommended pneumococcal vaccine:
- Alcoholism
- Chronic heart disease
- Chronic liver disease
- Chronic lung disease
- Diabetes mellitus
CDC recommends you:
- Have 1 dose of PPSV23 [Pneumovax 23].
Adults 65 Years or Older
CDC recommends pneumococcal vaccination for all adults 65 years or older. Have a dose of PCV13 [Prevnar 13] to adults 65 years or older who have not previously received a dose. Then administer a dose of PPSV23 [Pneumovax 23] at least 1 year later.
- Have 1 dose of PCV13 [Prevnar 13] to all adults 65 years or older who have not previously received a dose.
- Have 1 dose of PPSV23 [Pneumovax 23] to all adults 65 years or older at least 1 year after any prior PCV13 dose and at least 5 years after any prior PPSV23 dose.
- Adults who received one or two doses of PPSV23 before age 65 should receive one final dose of the vaccine at age 65 or older.
Figure 1. Pneumococcal vaccine timing for adults 65 years or older
Pneumococcal vaccine Catch-Up Guidance
Pneumococcal vaccine Catch-Up Guidance for Healthy Children 4 Months to 4 Years of Age
Figure 3. Pneumococcal vaccine Catch-Up Guidance for Healthy Children 4 Months to 4 Years of Age
Pneumococcal Vaccine Effectiveness
Pneumococcal Conjugate Vaccine
FDA licensed the first pneumococcal conjugate vaccine (PCV7) in 2000. A large clinical trial showed PCV7 reduced invasive disease caused by vaccine serotypes by 97%. Compared to unvaccinated children, children who received PCV7 4:
- Had 20% fewer episodes of chest X-ray confirmed pneumonia
- Had 7% fewer episodes of acute otitis media
- Underwent 20% fewer tympanostomy tube placements
PCV7 also reduced nasopharyngeal carriage, among children, of pneumococcal serotypes in the vaccine.
FDA licensed PCV13 [Prevnar 13] in 2010 based on studies comparing the serologic response of children who received PCV13 to those who received PCV7. These studies showed PCV13 induced antibody levels comparable to those induced by PCV7 and shown to be protective against invasive disease.
In another study, children aged 7 through 71 months received up to 3 PCV13 doses according to age-appropriate immunization schedules. None of the children had previously received pneumococcal conjugate vaccine. The antibody responses were comparable to those achieved after the 3-dose infant PCV13 series in the U.S. immunogenicity trial with the exception of serotype 1. The IgG geometric mean concentration was lower for serotype 1 among children aged 24 through 71 months.
Researchers conducted a randomized placebo-controlled trial (CAPiTA trial) in the Netherlands among approximately 85,000 adults 65 years or older during 2008–2013. This trial evaluated the clinical benefit of PCV13 in the prevention of pneumococcal pneumonia. The results of the CAPiTA trial demonstrated 4:
- 45.6% efficacy of PCV13 against vaccine-type pneumococcal pneumonia
- 45.0% efficacy against vaccine-type non-bacteremic pneumococcal pneumonia
- 75.0% efficacy of PCV13 against vaccine-type invasive pneumococcal disease (IPD)
Substantial evidence demonstrates routine infant PCV7 and PCV13 vaccination reduced carriage and transmission of vaccine serotypes. This resulted in lower invasive pneumococcal disease incidence among unvaccinated persons of all ages, including infants too young to receive the vaccine.
Pneumococcal Polysaccharide Vaccine
More than 80% of healthy adults who receive PPSV23 develop antibodies against the serotypes contained in the vaccine 4. This immune response usually occurs within 2 to 3 weeks after vaccination. Older adults and persons with some chronic illnesses or immunodeficiency may not respond as well Elevated antibody levels persist for at least 5 years in healthy adults but decline more quickly in persons with certain underlying illnesses. Children younger than 2 years of age generally have a poor antibody response to PPSV23.
PPSV23 vaccine efficacy studies have resulted in various estimates of clinical effectiveness. Overall, the vaccine is 60% to 70% effective in preventing invasive disease caused by serotypes in the vaccine. PPSV23 shows reduced effectiveness among immunocompromised persons; however, CDC recommends PPSV23 for these groups because of their increased risk of invasive pneumococcal disease. There is no consensus regarding the ability of PPSV23 to prevent non-bacteremic pneumococcal pneumonia.
Studies comparing patterns of asymptomatic pneumococcal carriage before and after PPSV23 vaccination have not shown decreases in carrier rates among those vaccinated.
Pneumococcal vaccine side effects
Most people who get a pneumococcal vaccine do not have any serious problems with it. With any medicine, including vaccines, there is a chance of side effects. These are usually mild and go away on their own within a few days, but serious reactions are possible.
Mild Problems
Pneumococcal Conjugate Vaccine PCV13 [Prevnar 13]
Mild problems following pneumococcal conjugate vaccination can include:
- Reactions where the shot was given
- Redness
- Swelling
- Pain or tenderness
- Fever
- Loss of appetite
- Fussiness (irritability)
- Feeling tired
- Headache
- Chills
Young children who get pneumococcal conjugate vaccine at the same time as inactivated flu vaccine may be at increased risk for seizures caused by fever. Ask your doctor for more information.
Pneumococcal Polysaccharide Vaccine PPSV23 [Pneumovax 23]
Mild problems following pneumococcal polysaccharide vaccination can include:
- Reactions where the shot was given
- Redness
- Pain
- Fever
- Muscle aches
If these problems occur, they usually go away within about two days.
Problems that Could Happen After Getting Any Injected Vaccine
People sometimes faint after a medical procedure, including vaccination. Sitting or lying down for about 15 minutes can help prevent fainting and injuries caused by a fall. Tell your healthcare professional if you or your child:
- Feels dizzy
- Has vision changes
- Has ringing in the ears
Some people get severe pain in the shoulder and have difficulty moving the arm where the doctor gave the shot. This happens very rarely.
Any medicine can cause a severe allergic reaction. Such reactions from a vaccine are very rare, estimated at about 1 in a million doses. These types of reactions would happen within a few minutes to a few hours after the vaccination.
As with any medicine, there is a very remote chance of a vaccine causing a serious injury or death.
- Pilishvili T., Bennett N.M. Pneumococcal disease prevention among adults: Strategies for the use of pneumococcal vaccines. Vaccine. 2015;33:D60–D65. doi: 10.1016/j.vaccine.2015.05.102[↩]
- Pneumococcal Vaccination: Information for Healthcare Professionals. https://www.cdc.gov/vaccines/vpd/pneumo/hcp/index.html[↩]
- Pneumococcal Vaccine Recommendations. https://www.cdc.gov/pneumococcal/hcp/vaccine-recommendations/index.html[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- About Pneumococcal Vaccines. https://www.cdc.gov/vaccines/vpd/pneumo/hcp/about-vaccine.html[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Types of Pneumococcal Vaccines. https://www.cdc.gov/pneumococcal/vaccines/types.html[↩][↩]
- VAXNEUVANCE. https://www.fda.gov/vaccines-blood-biologics/vaccines/vaxneuvance[↩][↩][↩]
- PREVNAR 20. https://www.fda.gov/vaccines-blood-biologics/vaccines/prevnar-20[↩][↩]
- CAPVAXIVE. https://www.fda.gov/vaccines-blood-biologics/capvaxive[↩][↩][↩][↩]
- Centers for Disease Control and Prevention (CDC). Licensure of 13-valent pneumococcal conjugate vaccine for adults aged 50 years and older. MMWR Morb Mortal Wkly Rep. 2012 Jun 1;61(21):394-5. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6121a3.htm[↩][↩][↩]
- PNEUMOVAX 23 – Pneumococcal Vaccine, Polyvalent. https://www.fda.gov/vaccines-blood-biologics/vaccines/pneumovax-23-pneumococcal-vaccine-polyvalent[↩][↩][↩]
- Pneumococcal Vaccination. https://www.cdc.gov/pneumococcal/vaccines/index.html[↩][↩][↩]
- ACIP Recommendations: Pneumococcal Vaccine. https://www.cdc.gov/acip-recs/hcp/vaccine-specific/pneumococcal.html[↩][↩][↩][↩][↩][↩][↩]
- Bonten MJ, Huijts SM, Bolkenbaas M, Webber C, Patterson S, Gault S, van Werkhoven CH, van Deursen AM, Sanders EA, Verheij TJ, Patton M, McDonough A, Moradoghli-Haftvani A, Smith H, Mellelieu T, Pride MW, Crowther G, Schmoele-Thoma B, Scott DA, Jansen KU, Lobatto R, Oosterman B, Visser N, Caspers E, Smorenburg A, Emini EA, Gruber WC, Grobbee DE. Polysaccharide conjugate vaccine against pneumococcal pneumonia in adults. N Engl J Med. 2015 Mar 19;372(12):1114-25. doi: 10.1056/NEJMoa1408544[↩][↩]
- Moore MR, Link-Gelles R, Schaffner W, Lynfield R, Holtzman C, Harrison LH, Zansky SM, Rosen JB, Reingold A, Scherzinger K, Thomas A, Guevara RE, Motala T, Eason J, Barnes M, Petit S, Farley MM, McGee L, Jorgensen JH, Whitney CG. Effectiveness of 13-valent pneumococcal conjugate vaccine for prevention of invasive pneumococcal disease in children in the USA: a matched case-control study. Lancet Respir Med. 2016 May;4(5):399-406. doi: 10.1016/S2213-2600(16)00052-7[↩]
- Pilishvili T, Bennett NM. Pneumococcal disease prevention among adults: Strategies for the use of pneumococcal vaccines. Vaccine. 2015 Nov 27;33 Suppl 4:D60-5. doi: 10.1016/j.vaccine.2015.05.102[↩]
- Pneumococcal Vaccine Recommendations. https://www.cdc.gov/vaccines/vpd/pneumo/hcp/recommendations.html[↩]
- Pneumococcal Vaccination: Summary of Who and When to Vaccinate. https://www.cdc.gov/vaccines/vpd/pneumo/hcp/who-when-to-vaccinate.html[↩][↩][↩][↩][↩]
- https://www.fda.gov/media/150819/download[↩][↩][↩][↩][↩]
- https://www.fda.gov/media/150818/download[↩][↩][↩][↩][↩]
- https://www.fda.gov/media/149987/download[↩][↩][↩]
- https://www.fda.gov/media/169126/download[↩]
- https://www.fda.gov/media/179428/download[↩][↩][↩][↩][↩]
- https://www.fda.gov/media/80547/download[↩][↩][↩][↩][↩][↩]
- https://www.fda.gov/media/81731/download[↩][↩]
- Gutierrez Rodriguez MA, Ordobas Gavin MA, Garcia-Comas L, Sanz Moreno JC, Cordoba Deorador E, Lasheras Carbajo MD, Taveira Jimenez JA, Martin Martinez F, Iniesta Fornies D, Arce Arnaez A. Effectiveness of 23-valent pneumococcal polysaccharide vaccine in adults aged 60 years and over in the Region of Madrid, Spain, 2008-2011. Euro Surveill. 2014 Oct 9;19(40):20922. doi: 10.2807/1560-7917.es2014.19.40.20922[↩]
- Kim JH, Chun BC, Song JY, Kim HY, Bae IG, Kim DM, Choi YH, Jun YH, Choi WS, Kang SH, Kwon HH, Jeong HW, Kee SY, Hur J, Chung JW, Yoon YK, Sohn JW, Yang KS, Kim MJ. Direct effectiveness of pneumococcal polysaccharide vaccine against invasive pneumococcal disease and non-bacteremic pneumococcal pneumonia in elderly population in the era of pneumococcal conjugate vaccine: A case-control study. Vaccine. 2019 May 9;37(21):2797-2804. doi: 10.1016/j.vaccine.2019.04.017[↩]
- Andrews NJ, Waight PA, George RC, Slack MP, Miller E. Impact and effectiveness of 23-valent pneumococcal polysaccharide vaccine against invasive pneumococcal disease in the elderly in England and Wales. Vaccine. 2012 Nov 6;30(48):6802-8. doi: 10.1016/j.vaccine.2012.09.019[↩]
- Shimbashi, R., Suzuki, M., Chang, B., Watanabe, H., Tanabe, Y., Kuronuma, K., Oshima, K., Maruyama, T., Takeda, H., Kasahara, K., Fujita, J., Nishi, J., Kubota, T., Tanaka-Taya, K., Matsui, T., Sunagawa, T., Oishi, K., & Adult IPD Study Group (2020). Effectiveness of 23-Valent Pneumococcal Polysaccharide Vaccine against Invasive Pneumococcal Disease in Adults, Japan, 2013-2017. Emerging infectious diseases, 26(10), 2378–2386. https://doi.org/10.3201/eid2610.191531[↩]
- Bonten MJ, Huijts SM, Bolkenbaas M, et al. Polysaccharide conjugate vaccine against pneumococcal pneumonia in adults. N Engl J Med. 2015;372(12):1114–25. https://www.nejm.org/doi/10.1056/NEJMoa1408544[↩]
- Moore MR, Link-Gelles R, Schaffner W, et al. Effectiveness of 13-valent pneumococcal conjugate vaccine for prevention of invasive pneumococcal disease in children in the USA: A matched case-control study. Lancet Respir Med. 2016;4(5):399–406. https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(16)00052-7/fulltext[↩]
- Pilishvili T, Bennett NM. Pneumococcal disease prevention among adults: Strategies for the use of pneumococcal vaccines. Vaccine. 2015;33(4):D60–5. https://www.ncbi.nlm.nih.gov/pubmed/26116257[↩]
- Ask the Experts: Pneumococcal. https://www.immunize.org/ask-experts/topic/pneumococcal[↩][↩][↩][↩][↩][↩][↩][↩]
- Theilacker C, Fletcher MA, Jodar L, Gessner BD. PCV13 Vaccination of Adults against Pneumococcal Disease: What We Have Learned from the Community-Acquired Pneumonia Immunization Trial in Adults (CAPiTA). Microorganisms. 2022 Jan 8;10(1):127. doi: 10.3390/microorganisms10010127. Erratum in: Microorganisms. 2022 May 12;10(5):1018. doi: 10.3390/microorganisms10051018[↩][↩]
- Administering Pneumococcal Vaccines. https://www.cdc.gov/vaccines/vpd/pneumo/hcp/administering-vaccine.html[↩][↩][↩]