What is projectile vomiting
Projectile vomiting simply means forced vomiting often occurring suddenly and without warning, i.e. without nausea and retching. Consequently an individual may have an episode of projectile vomiting at any time, e.g. while standing in a queue, on public transport, or in a restaurant or hospital bed.
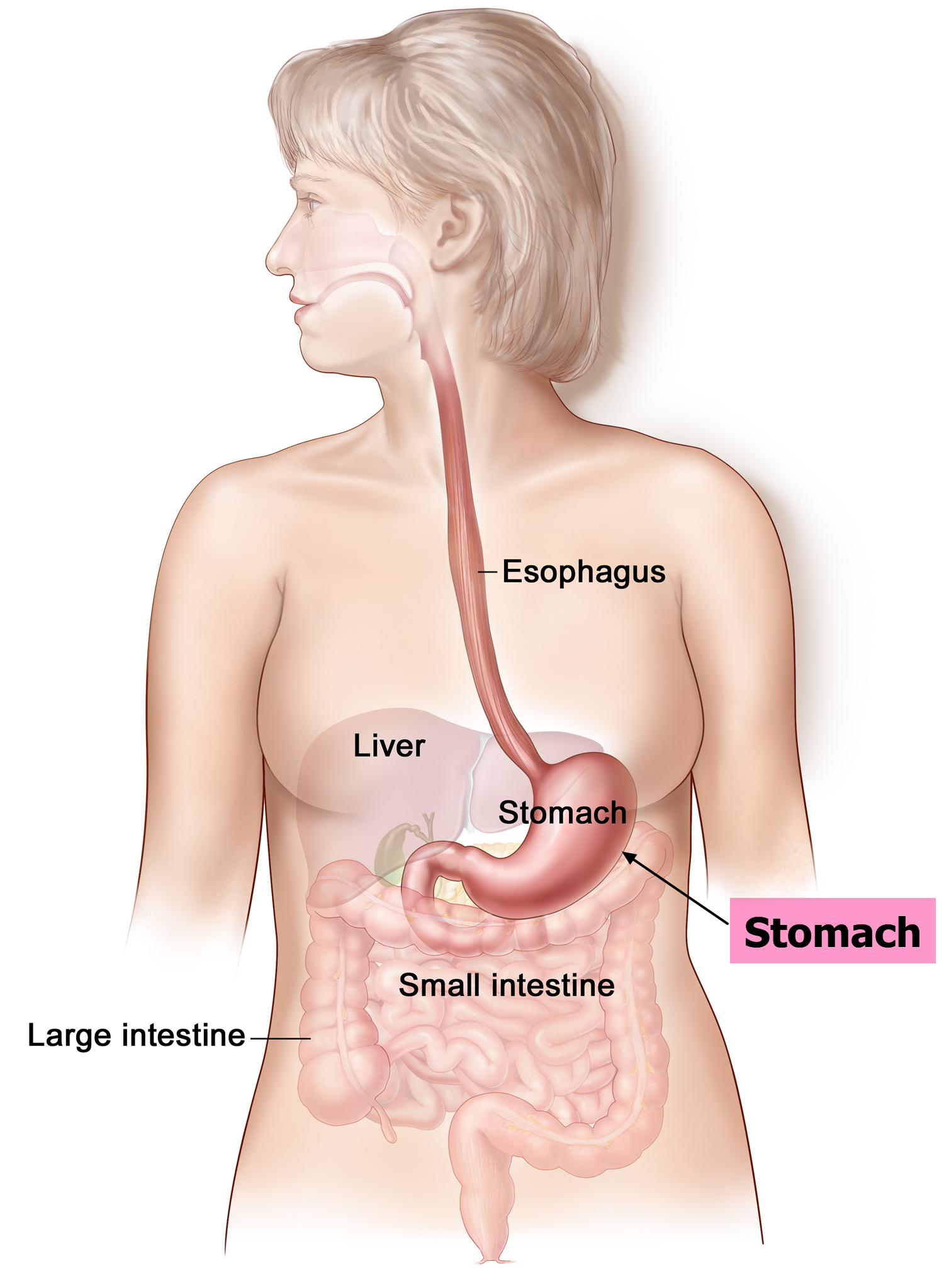
Figure 1. Stomach
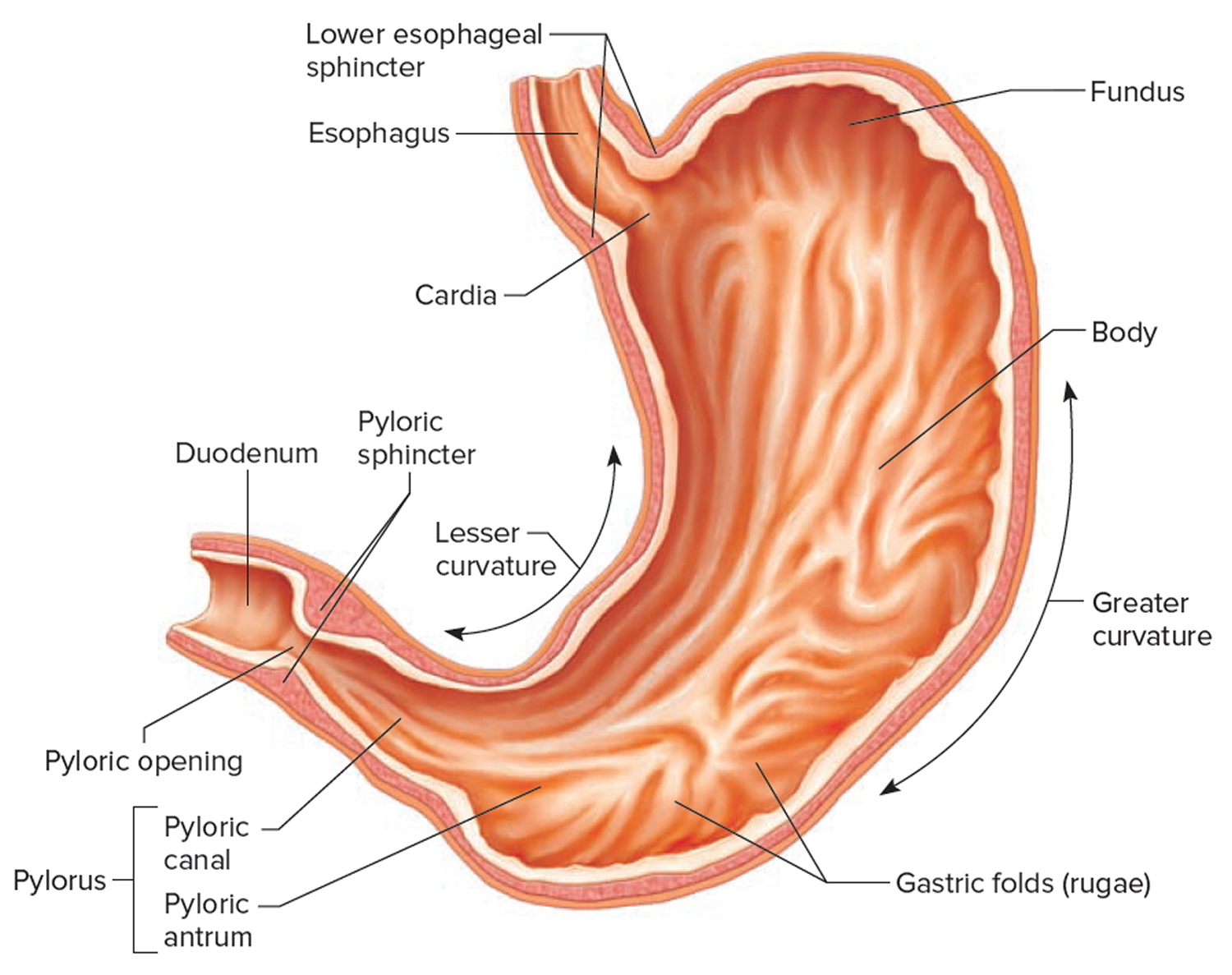
Figure 2. Parts of the stomach
Projectile vomiting in infants
Pyloric stenosis is an uncommon condition in infants that blocks food from entering the small intestine. Normally, food and other stomach contents pass through the pylorus, the lower part of the stomach, to enter the small intestine. A muscular valve (pyloric sphincter) between the stomach and small intestine holds food in the stomach until it is ready for the next stage in the digestive process. In pyloric stenosis, the pylorus muscles thicken and become abnormally large, blocking food from reaching the small intestine and prevents food from emptying out of the stomach.
Pyloric stenosis also called infantile hypertrophic pyloric stenosis, is a type of gastric outlet obstruction, which means a blockage from the stomach to the intestines, can lead to projectile vomiting, dehydration and weight loss. Babies with pyloric stenosis may seem to be hungry all the time.
Signs and symptoms of pyloric stenosis include:
- Vomiting after feeding. The baby may vomit forcefully, ejecting breast milk or formula up to several feet away (projectile vomiting). Vomiting might be mild at first and gradually become more severe as the pylorus opening narrows. The vomit may sometimes contain blood.
- Persistent hunger. Babies who have pyloric stenosis often want to eat soon after vomiting.
- Stomach contractions. You may notice wave-like contractions (peristalsis) that ripple across your baby’s upper abdomen soon after feeding, but before vomiting. This is caused by stomach muscles trying to force food through the narrowed pylorus.
- Dehydration. Your baby might cry without tears or become lethargic. You might find yourself changing fewer wet diapers or diapers that aren’t as wet as you expect.
- Changes in bowel movements. Since pyloric stenosis prevents food from reaching the intestines, babies with this condition might be constipated.
- Weight problems. Pyloric stenosis can keep a baby from gaining weight, and sometimes can cause weight loss.
Pyloric stenosis affects about 3 out of 1,000 babies in the United States. It’s more likely to affect firstborn male infants and also runs in families — if a parent had pyloric stenosis, then a baby has up to a 20% risk of developing it. Most infants who have pyloric stenosis develop symptoms 3 to 5 weeks after birth.
Pyloric stenosis needs immediate medical treatment and surgery cures pyloric stenosis.
Key points
- Correction of fluid deficit, electrolyte and acid base abnormalities is the priority
- Following fluid resuscitation (if required) 0.9% Sodium Chloride with 5% glucose and 20mmol/l Potassium Chloride should be used for replacement of deficit and ongoing fluid maintenance.
- Surgical correction may be safely delayed until correction of fluid deficit, electrolyte and acid base abnormalities.
Pyloric stenosis is an urgent condition that needs immediate treatment.
See your doctor if your baby:
- has lasting or projectile vomiting after feeding
- is losing weight or not gaining weight as expected
- is less active than usual or is very sleepy
- has few or no stools (poops) over a period of 1 or 2 days
- show signs of dehydration, such as more than 4 to 6 hours between wet diapers, a sunken “soft spot” on the head, or sunken eyes
Pyloric stenosis complications
Pyloric stenosis can lead to:
- Failure to grow and develop.
- Dehydration. Frequent vomiting can cause dehydration and a mineral (electrolyte) imbalance. Electrolytes help regulate many vital functions.
- Stomach irritation. Repeated vomiting can irritate your baby’s stomach and may cause mild bleeding.
- Jaundice. Rarely, a substance secreted by the liver (bilirubin) can build up, causing a yellowish discoloration of the skin and eyes.
What are the signs and symptoms of pyloric stenosis?
Symptoms of pyloric stenosis typically begin when a baby is around 3 weeks old. They include:
- Vomiting. The first symptom is usually vomiting. At first it may seem that the baby is just spitting up often, but then it tends to become projectile vomiting, in which the breast milk or formula is ejected forcefully from the mouth, in an arc, sometimes over a distance of several feet. Projectile vomiting usually takes place soon after the end of a feeding, although in some cases it can happen hours later. The vomited milk might smell curdled because it has mixed with stomach acid. The vomit will not contain bile, a greenish fluid from the liver that mixes with digested food after it leaves the stomach. Despite vomiting, a baby with pyloric stenosis is usually hungry again soon after vomiting and will want to eat. It’s important to know that even with the vomiting, the baby might not seem to be in great pain or at first look very ill.
- Changes in stools. Babies with pyloric stenosis usually have fewer, smaller stools (poops) because little or no food is reaching the intestines. Constipation or poop with mucus also can happen.
- Failure to gain weight or weight loss. Most babies with pyloric stenosis will fail to gain weight or will lose weight. As the condition gets worse, they might become dehydrated.
- Dehydrated infants are less active than usual, and they may develop a sunken “soft spot” on their heads and sunken eyes, and their skin may look wrinkled. Because less pee is made, they can go more than 4 to 6 hours between wet diapers.
- Waves of peristalsis. After feeds, increased stomach contractions may make noticeable ripples, which move from left to right over the baby’s belly as the stomach tries to empty itself against the thickened pylorus.
It’s important to see your doctor if your baby has any of these symptoms.
Other conditions can cause similar problems. For instance:
- Gastroesophageal reflux (GER) usually begins before 8 weeks of age. Gastroesophageal reflux involves lots of spitting up (reflux) after feedings, which can look like vomiting. But most babies with gastroesophageal reflux don’t have projectile vomiting, and while they might have trouble gaining weight, they usually have normal poops.
- A milk protein allergy also can make a baby spit up or vomit, and have diarrhea. But these babies don’t have projectile vomiting.
- Gastroenteritis (inflammation in the digestive tract that can be caused by viral or bacterial infection) also can cause vomiting and dehydration. But babies with gastroenteritis usually also have diarrhea with loose, watery, or sometimes bloody stools. Diarrhea usually isn’t seen with pyloric stenosis.
What causes pyloric stenosis?
It’s thought that babies who develop pyloric stenosis are not born with it, but have progressive thickening of the pylorus after birth. A baby will start to show symptoms when the pylorus is so thick that the stomach can’t empty properly.
The cause of this thickening isn’t clear. It might be a combination of several things; for example, use of erythromycin (an antibiotic) in babies in the first 2 weeks of life or antibiotics given to moms at the end of pregnancy or during breastfeeding can be associated with pyloric stenosis.
Risk factors for pyloric stenosis
Risk factors for pyloric stenosis include:
- Sex. Pyloric stenosis is seen more often in boys — especially firstborn children — than in girls.
- Race. Pyloric stenosis is more common in Caucasians of northern European ancestry, less common in African-Americans and rare in Asians.
- Premature birth. Pyloric stenosis is more common in babies born prematurely than in full-term babies.
- Family history. Studies found higher rates of this disorder among certain families. Pyloric stenosis develops in about 20 percent of male descendants and 10 percent of female descendants of mothers who had the condition.
- Smoking during pregnancy. This behavior can nearly double the risk of pyloric stenosis.
- Early antibiotic use. Babies given certain antibiotics in the first weeks of life — erythromycin to treat whooping cough, for example — have an increased risk of pyloric stenosis. In addition, babies born to mothers who took certain antibiotics in late pregnancy also may have an increased risk of pyloric stenosis.
- Bottle-feeding. Some studies suggest that bottle-feeding rather than breast-feeding can increase the risk of pyloric stenosis. Most people in these studies used formula rather than breast milk, so it isn’t clear whether the increased risk is related to formula or the mechanism of bottle-feeding.
How is pyloric stenosis diagnosed?
The doctor will ask detailed questions about the baby’s feeding and vomiting patterns, including what the vomit looks like. The baby will be examined, and any weight loss or failure to maintain growth since birth will be noted.
The doctor will check for a lump in the abdomen, which usually is firm and movable and feels like an olive. If the doctor feels this lump, it’s a strong indication that a baby has pyloric stenosis.
Visible gastric peristalsis (may be more obvious following a feed).
Pyloric mass:
- Located at the lateral edge of the rectus abdominis muscle in the right upper quadrant
- Best felt from the left side with the infant settled and supine.
- May be difficult to palpate. May require repeated examinations or to wait for several minutes with hand on abdomen to feel.
When pyloric stenosis seems likely, an abdominal ultrasound usually is done. The enlarged, thickened pylorus can be seen on ultrasound images. The doctor may ask that the baby not be fed for several hours before an ultrasound.
Sometimes a barium swallow is done instead of an ultrasound. Babies swallow a small amount of a chalky liquid (barium), and then special X-rays are taken to view the pyloric area of the stomach to see if there is any narrowing or blockage.
The doctor also might order blood tests to check levels of electrolytes (minerals that help keep fluids balanced and vital organs working properly). An electrolyte imbalance often happens due to the ongoing vomiting of stomach acid and dehydration, and needs to be corrected.
Pyloric stenosis treatment
When an infant is diagnosed with pyloric stenosis, either by ultrasound or barium swallow, the baby will be admitted to the hospital and prepared for surgery. Any dehydration or electrolyte problems in the blood will be corrected with intravenous (IV) fluids, usually within 24 hours.
- Surgical correction of hypertrophic pyloric stenosis is usually delayed until correction of acid/base status, electrolyte disturbances and dehydration.
- It is particularly important to fully correct serum bicarbonate before surgery because of the risk of hypoventilation/apnoea post-operatively in the setting of a metabolic alkalosis.
A surgical procedure called pyloromyotomy, which involves cutting through the thickened muscles of the pylorus, will relieve the blockage. The pylorus is examined through a very small incision, and the muscles that are overgrown and thickened are spread and relaxed.
The surgery can also be done through laparoscopy. This is a technique that uses a tiny scope placed in an incision in the belly button, allowing the doctor to see the area of the pylorus. Using other small instruments placed in nearby incisions, the doctor can complete the surgery.
Potential complications from pyloric stenosis surgery include bleeding and infection. However, complications aren’t common, and the results of surgery are generally excellent.
Most babies return to normal feedings fairly quickly, usually 3 to 4 hours after the surgery. Because of swelling at the surgery site, a baby may still vomit small amounts for a day or so. If there are no complications, most babies who have had pyloromyotomy can return to a normal feeding schedule and go home within 24 to 48 hours of the surgery.
If you’re breastfeeding, you might worry about continuing while your baby is hospitalized. The hospital staff should be able to provide a breast pump and help you use it so that you can continue to express milk until your baby can feed regularly.
After a successful pyloromyotomy, your baby won’t need to follow any special feeding schedules. Your doctor will probably want to examine your child at a follow-up appointment to make sure the surgical site is healing properly and that your baby is feeding well and maintaining or gaining weight.
Pyloric stenosis should not happen again after a pyloromyotomy. If your baby still has symptoms weeks after the surgery, there might be another medical problem, such as gastritis or gastroesophageal reflux, so let your doctor know right away.
Projectile vomiting in adults
Vomiting may be due to a variety of diseases, particularly in the upper gastro-intestinal tract and these include gastric and duodenal ulcers and reflux oesaphagitis. Vomiting may also be a feature of gastro oesophageal reflux disease (GERD). If vomiting occurs soon after swallowing and consists of fresh food there may be obstruction in the esophagus. Vomiting may also occur in the older population when dysmotility is present. Vomiting can occur when there is obstruction in the small intestine or the colon, the vomitus usually is bile stained and contains mucus and altered food. When the obstruction is lower down in the bowel there may be a smell suggesting feces in the vomit. Medication is another cause of vomiting.
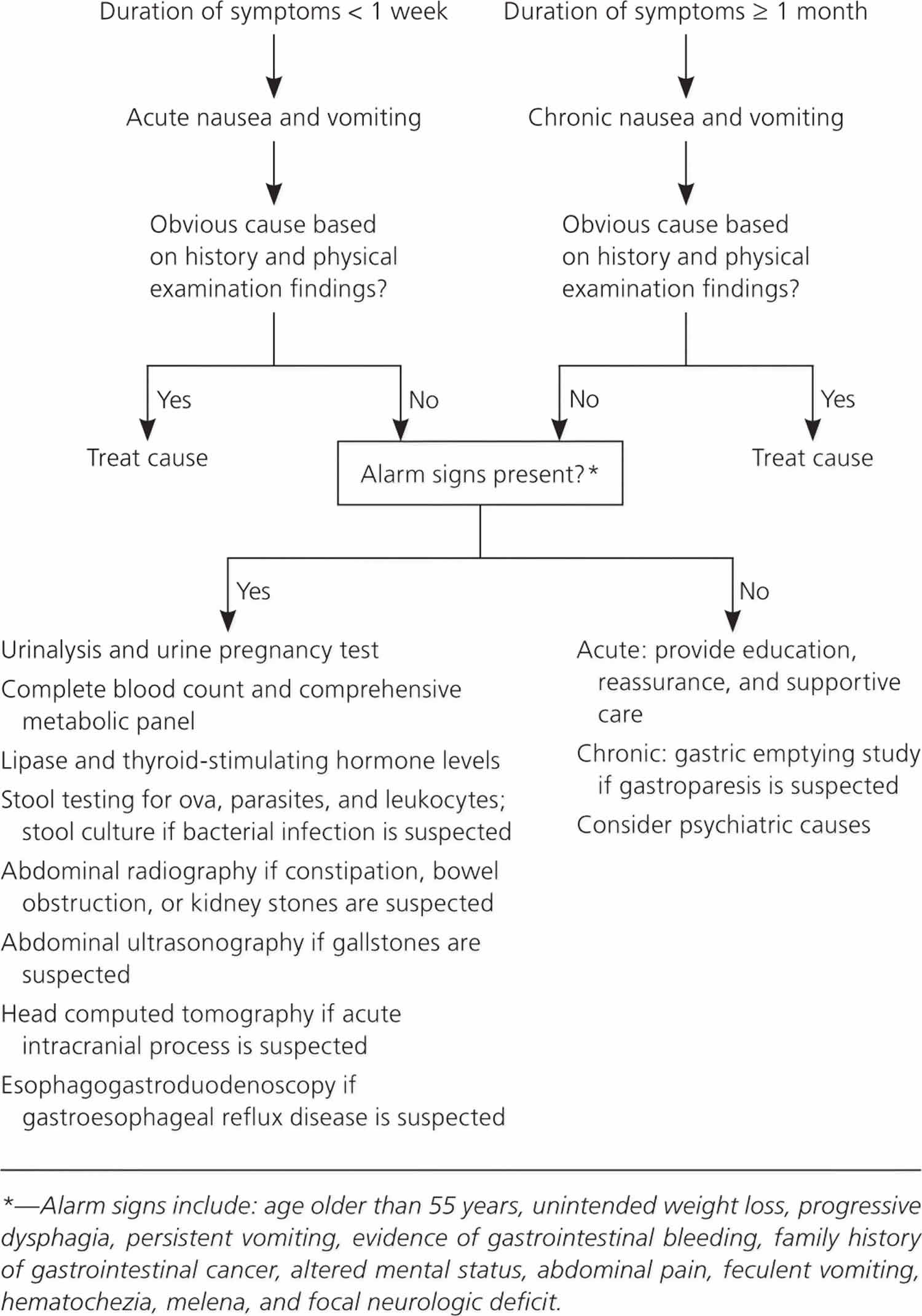
Other potential diagnoses include endocrine conditions (including pregnancy), central nervous system disorders, psychiatric causes, toxin exposure, metabolic abnormalities, and obstructive or functional gastrointestinal causes. The likely cause of a vomiting can usually be determined by history and physical examination. Alarm signs such as dehydration, acidosis caused by an underlying metabolic disorder, or an acute abdomen warrant additional evaluation. Based on the suspected diagnosis, basic laboratory testing may include urinalysis, urine pregnancy testing, complete blood count, comprehensive metabolic panel, amylase and lipase levels, thyroid-stimulating hormone level, and stool studies with cultures. Imaging studies include abdominal radiography, ultrasonography, and computed tomography. Computed tomography of the head should be performed if an acute intracranial process is suspected. Chronic nausea and vomiting is defined by symptoms that persist for at least one month. Patients with risk factors for gastric malignancies or alarm symptoms should be evaluated with esophagogastroduodenoscopy. If gastroparesis is suspected, a gastric emptying study is recommended. In addition to functional causes, it is also important to consider psychiatric causes when evaluating patients with chronic nausea and vomiting.
Diagnostic and management strategies vary depending on the duration of symptoms.
What causes projectile vomiting in adults
Self-limited viral gastroenteritis is the most common cause 1. Approximately 179 million episodes of acute gastroenteritis occur each year in the United States and result in roughly 600,000 hospitalizations. Although this illness typically resolves in three to five days, it results in significant time lost from work and accounts for an estimated $1 billion per year in direct and indirect costs 2. Only 20% of acute gastroenteritis cases are attributed to a specific etiology 3. Viruses are the most common cause; norovirus is the most common in adults.
Common and uncommon causes of acute nausea and vomiting in adults 4:
Central nervous system
- Common
- Benign positional vertigo
- Migraine
- Motion sickness
- Uncommon
- Cerebrovascular event
- Closed head injury
- Hydrocephalus
- Mass lesion
- Meniere disease
- Meningitis
- Pseudotumor cerebri
- Seizure disorder
Gastrointestinal
- Common
- Appendicitis
- Cholecystitis
- Cholelithiasis
- Gastritis
- Gastroesophageal reflux disease (GERD)
- Gastroparesis
- Irritable bowel syndrome (IBS)
- Peptic ulcer disease
- Uncommon
- Adhesions
- Esophageal motility disorders
- Incarcerated hernia
- Intestinal obstruction
- Mesenteric ischemia
- Pancreatitis
- Peritonitis
Infections
- Common
- Bacterial gastroenteritis
- Foodborne illness
- Pyelonephritis
- Viral gastroenteritis
- Uncommon
- Brain abscess
- Encephalitis
- Meningitis
- Pneumonia
Metabolic
- Common
- Diabetic ketoacidosis
- Pregnancy
- Uremia
- Uncommon
- Adrenal disorders
- Parathyroid disorders
- Thyroid disorders
Medications and toxins
- Antiarrhythmics, antibiotics, anticonvulsants, arsenic, chemotherapeutics, digoxin, estrogens, ethanol overdose, nonsteroidal anti-inflammatory drugs, opiates, organophosphates and pesticides, overdoses and withdrawal, radiation therapy or exposure, ricin
Other
- Acute glaucoma, acute myocardial infarction, nephrolithiasis, pain, psychiatric disorder
Table 1. Nausea and Vomiting That Suggest Specific Diagnoses
| Clinical presentation | Suggested diagnoses | Suggested tests |
|---|---|---|
Acute onset | Cholecystitis, gastroenteritis, medication-related effect, pancreatitis | Cholecystitis: right upper-quadrant ultrasonography |
Pancreatitis: amylase and lipase levels, ultrasonography to assess for gallstones, contrast-enhanced abdominal computed tomography in patients with severe illness | ||
Associated with diarrhea, headache, and myalgias | Viral gastroenteritis | None |
Bilious vomiting | Small bowel obstruction | Abdominal radiography or computed tomography |
Continuous vomiting | Conversion disorders | Electrolyte levels |
Delayed vomiting (more than one hour after meals) | Gastric outlet obstruction, gastroparesis | Obstruction: abdominal radiography |
Gastroparesis: gastric emptying study | ||
Feculent or foul odor to vomitus | Intestinal obstruction | Abdominal radiography |
Habitual postprandial, irregular vomiting | Major depression | Patient Health Questionnaire-9, Beck Depression Inventory |
Insidious onset | Gastroesophageal reflux, gastroparesis, medication-related effect, metabolic disorders, pregnancy | Gastroesophageal reflux: esophagogastroduodenoscopy if patient has warning signs or does not improve with empiric therapy |
Gastroparesis: gastric emptying study | ||
Metabolic disorders: pulse oximetry, arterial blood gases, serum chemistries, chest radiography | ||
Pregnancy: pregnancy test in women of childbearing age, with pelvic ultrasonography if ectopic pregnancy is suspected | ||
Patient report of previous organic or functional gastrointestinal illness | Chronic psychogenic vomiting | Electrolyte levels, further evaluation if organic cause is suspected |
Projectile vomiting, may not be preceded by nausea | Intracranial disorders, increased intracranial pressure (also associated with normal emesis) | Brain computed tomography |
Regurgitation of undigested food | Achalasia, esophageal stricture, Zenker diverticulum | Esophagogastroduodenoscopy, upper gastrointestinal barium study |
Vomiting before breakfast | Alcohol ingestion, increased intracranial pressure, pregnancy, uremia | Increased intracranial pressure: brain computed tomography |
Pregnancy: pregnancy test in women of childbearing age, with pelvic ultrasonography if ectopic pregnancy is suspected | ||
Uremia: renal function testing, electrolyte levels | ||
Vomiting during or soon after meals | Anorexia, bulimia | Electrolyte levels |
Vomiting partly digested food or chyme several hours after meals | Gastric outlet obstruction (no bile), gastroparesis | Obstruction: abdominal radiography |
Projectile vomiting in adults diagnosis
Most conditions can be diagnosed by findings from the history and physical examination. Diagnostic testing may be warranted in patients with signs of significant dehydration (e.g., decreased urine output, skin tenting, dry mucous membranes), signs of acidosis caused by diabetic ketoacidosis or another underlying disorder (e.g., markedly increased respiratory rate, fruity odor to breath, altered mental status), severe abdominal pain or distension, hematochezia, jaundice, melena, severe headache, urinary tract infection symptoms, abdominal pain relieved by vomiting, hematemesis, or feculent vomiting 4.
Figure 3. Evaluation of Nausea and Vomiting in Adults
[Source 5]Imaging tests
Abdominal radiography is helpful in detecting bowel obstructions and kidney stones 6. Computed tomography of the abdomen is useful for detecting infections (e.g., appendicitis, cholecystitis) and for additional testing for bowel obstruction and kidney stones that are not detected on radiography.24 In adults, abdominal radiography combined with clinical examination and laboratory analysis (complete blood count and basic metabolic panel) is useful for predicting the need for urgent intervention in the first 24 hours of illness (sensitivity = 56%; specificity = 81%) 6.
Right upper-quadrant ultrasonography is used to evaluate for gallstones. Hepatobiliary iminodiacetic acid scans can determine whether delayed gallbladder emptying is the cause of nausea and abdominal pain when initial ultrasonography is negative.
Migraine should be diagnosed in patients who have headaches with at least four of the following characteristics: pulsatile quality, duration of four to 72 hours, unilateral location, nausea or vomiting, and disabling intensity 7. Cluster-type headaches, headaches with abnormal neurologic findings, undefined headaches, and headaches aggravated by exertion or the Valsalva maneuver are more likely to have associated intracranial pathology 7. Computed tomography or magnetic resonance imaging of the brain should be ordered for patients with these symptoms, and in those with other abnormal neurologic signs or symptoms.
- Scallan E, Hoekstra RM, Angulo FJ, et al. Foodborne illness acquired in the United States—major pathogens. Emerg Infect Dis. 2011;17(1):7–15.[↩]
- Skolnik NS, Albert RH. Essential Infectious Disease Topics for Primary Care. Totowa, N.J.: Humana Press; 2008.[↩]
- Scallan E, Griffin PM, Angulo FJ, Tauxe RV, Hoekstra RM. Foodborne illness acquired in the United States—unspecified agents. Emerg Infect Dis. 2011;17(1):16–22.[↩]
- Quigley EM, Hasler WL, Parkman HP. AGA technical review on nausea and vomiting. Gastroenterology. 2001;120(1):263–286.[↩][↩]
- Evaluation of Nausea and Vomiting in Adults: A Case-Based Approach. Am Fam Physician. 2013 Sep 15;88(6):371-379. https://www.aafp.org/afp/2013/0915/p371.html[↩][↩][↩]
- Smith JE, Hall EJ. The use of plain abdominal x rays in the emergency department. Emerg Med J. 2009;26(3):160–163.[↩][↩]
- Detsky ME, McDonald DR, Baerlocher MO, Tomlinson GA, McCrory DC, Booth CM. Does this patient with headache have a migraine or need neuroimaging? JAMA. 2006;296(10):1274–1283.[↩][↩]