Contents
What is pulmonary fibrosis
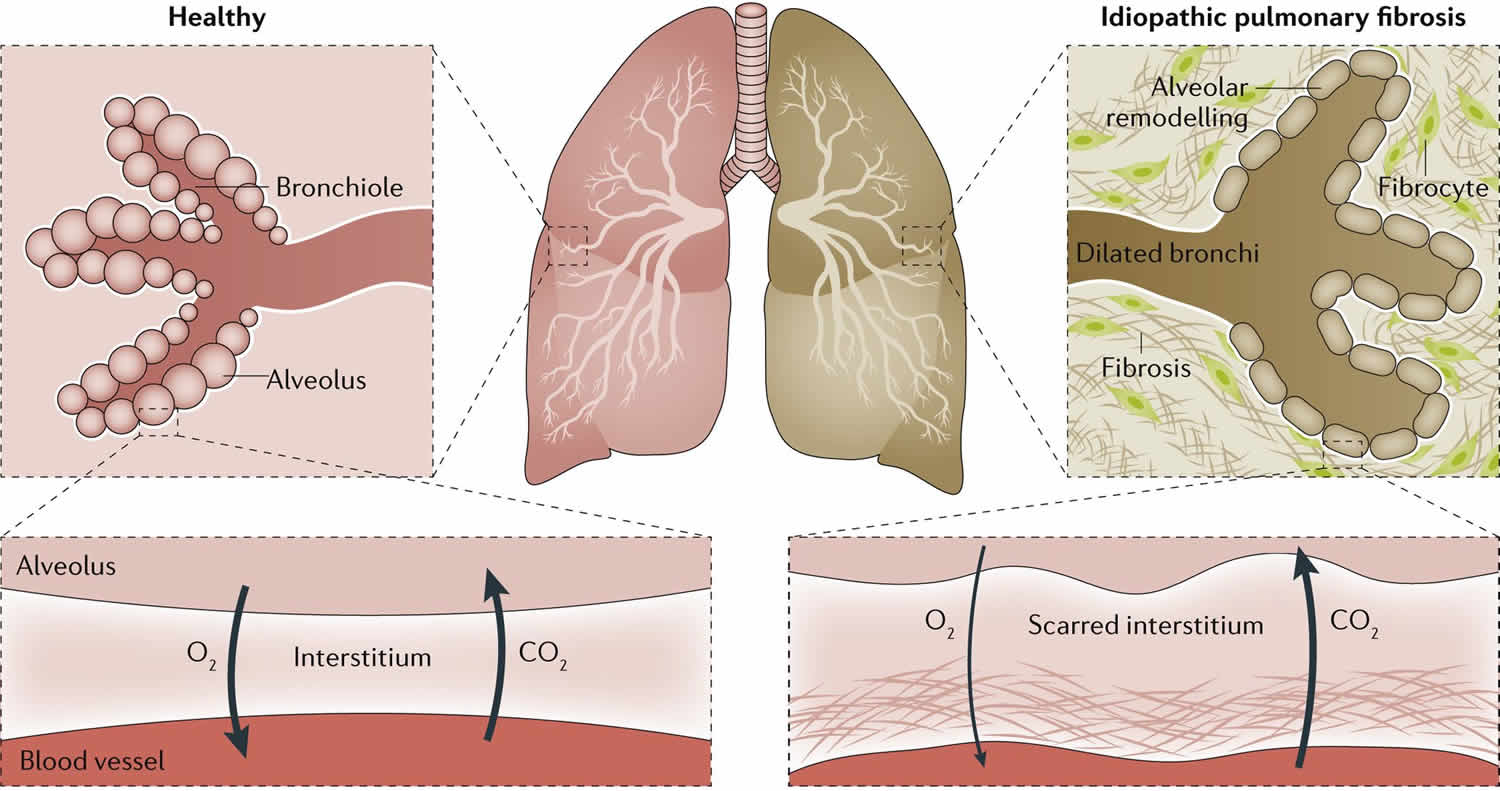
Pulmonary fibrosis is a lung disease in which the tissue deep in your lungs becomes scarred and damaged over time. This scarred lung tissue gets thick and stiff. This thickened, stiff tissue makes it more difficult for your lungs to work properly. That makes it hard for you to catch your breath, and your blood may not get enough oxygen. As pulmonary fibrosis worsens, you become progressively more short of breath.
Pulmonary fibrosis scars and thickens the tissue around and between the air sacs (alveoli) in your lungs. This makes it more difficult for oxygen to pass into your bloodstream. The scarring associated with pulmonary fibrosis can be caused by a multitude of factors, including environmental pollutants, long-term exposure to certain toxins, some medications, some connective tissue diseases, certain medical conditions, radiation therapy and interstitial lung disease. Interstitial lung disease is the name for a large group of diseases that inflame or scar the lungs. In most cases, the cause cannot be found. When a cause can’t be found, the condition is termed idiopathic pulmonary fibrosis (IPF).
The lung damage caused by pulmonary fibrosis can’t be repaired, but medications and therapies can sometimes help ease symptoms and improve quality of life. For some people, a lung transplant might be appropriate.
Pulmonary fibrosis isn’t just one disease. It is a family of more than 200 different lung diseases that all look very much alike. The pulmonary fibrosis family of lung diseases falls into an even larger group of diseases called the interstitial lung diseases, which includes all of the diseases that have inflammation and/or scarring in the lung. Some interstitial lung diseases don’t include scar tissue. When an interstitial lung disease does include scar tissue in the lung, doctors call it pulmonary fibrosis.
No one is certain how many people are affected by pulmonary fibrosis. One recent study estimated that idiopathic pulmonary fibrosis (which is just one of more than 200 types of pulmonary fibrosis) affects 1 out of 200 adults over the age of 60 and over in the United States—that translates to more than 200,000 people living with pulmonary fibrosis today. Approximately 50,000 new cases are diagnosed each year and as many as 40,000 Americans die from idiopathic pulmonary fibrosis each year.
Pulmonary fibrosis symptoms include:
- Shortness of breath
- A dry, hacking cough that doesn’t get better
- Fatigue
- Weight loss for no known reason
- Aching muscles and joints
- Clubbing, which is the widening and rounding of the tips of the fingers or toes
Your doctor may use your medical history, imaging tests, a biopsy, and lung function tests to diagnose pulmonary fibrosis. There is no cure. Treatments can help with symptoms and improve your quality of life. They include medicines, oxygen therapy, pulmonary rehabilitation, or a lung transplant.
Types of pulmonary fibrosis
Pulmonary fibrosis (pulmonary fibrosis) is a form of interstitial lung disease that causes scarring in the lungs. There are over 200 different types of pulmonary fibrosis and in most cases, there’s no known cause.
Idiopathic Pulmonary Fibrosis
The most common type of pulmonary fibrosis is idiopathic pulmonary fibrosis (IPF). This means this type of pulmonary fibrosis has no known cause. Approximately 50,000 new cases of idiopathic pulmonary fibrosis are diagnosed each year. Most idiopathic pulmonary fibrosis patients first start noticing symptoms between the ages of 50 and 70 years old. It is more common in men, but the number of cases of idiopathic pulmonary fibrosis in women is on the rise.
Pulmonary fibrosis from diseases
Some cases of pulmonary fibrosis are caused by autoimmune diseases like rheumatoid arthritis, scleroderma or Sjogren’s syndrome. Certain viral infections and gastroesophageal reflux disease (GERD) are also risk factors for pulmonary fibrosis. Gastroesophageal reflux disease (GERD) is a condition in which acid from your stomach backs up into your throat. Some people who have GERD may breathe in tiny drops of acid from their stomachs, which may injure the lungs.
Familial pulmonary fibrosis
Familial pulmonary fibrosis is very rare. pulmonary fibrosis is considered familial when two or more members within the same family have idiopathic pulmonary fibrosis (Ipulmonary fibrosis) or any other form of idiopathic interstitial pneumonia. There are genes that have been linked to pulmonary fibrosis but much is still unknown about this field. If someone in your family has had any type of interstitial lung disease, be sure to speak with your doctor and a genetic counselor about your risk.
Pulmonary fibrosis from exposures
Pulmonary fibrosis can be caused by exposure to hazardous materials. Examples include occupational exposures such as asbestos or silica. Some cases of pulmonary fibrosis are caused by breathing in bird or animal droppings. Radiation treatments and certain types of medications can cause pulmonary fibrosis. Cigarette smoking also increases a person’s risk of developing pulmonary fibrosis.
What is idiopathic pulmonary fibrosis
Idiopathic pulmonary fibrosis (IPF) is a type of lung disease that results in scarring (fibrosis) of the lungs for an unknown reason. Over time, the scarring gets worse and it becomes hard to take in a deep breath and the lungs cannot take in enough oxygen.
Idiopathic pulmonary fibrosis is a form of interstitial lung disease, primarily involving the interstitium (the tissue and space around the air sacs of the lungs), and not directly affecting the airways or blood vessels. There are many other kinds of interstitial lung disease that can also cause inflammation and/or fibrosis, and these are treated differently. It is important to work with your doctor to determine if you have idiopathic pulmonary fibrosis or another form of interstitial lung disease.
Figure 1. Idiopathic pulmonary fibrosis
What causes idiopathic pulmonary fibrosis
The cause of idiopathic pulmonary fibrosis is not completely understood. No one knows what causes idiopathic pulmonary fibrosis or why some people get it. “Idiopathic” means of unknown cause. Common risk factors for idiopathic pulmonary fibrosis include:
- Genetics (family history): Up to 20% of people with idiopathic pulmonary fibrosis have another family member with an interstitial lung disease. If more than one member of your family has idiopathic pulmonary fibrosis, the disease is called familial pulmonary fibrosis.
- Cigarette smoking: Approximately 75% of people with idiopathic pulmonary fibrosis are current or previous cigarette smokers.
- Acid reflux (gastroesophageal reflux disease [GERD]): Approximately 75% of people with idiopathic pulmonary fibrosis have symptoms of acid reflux or heartburn.
- Male sex: Approximately 75% of patients with idiopathic pulmonary fibrosis are male.
- Age: Almost all patients with idiopathic pulmonary fibrosis are over the age of 50 years
Idiopathic pulmonary symptoms
The two main symptoms of idiopathic pulmonary fibrosis are:
- Breathlessness (also known as shortness of breath or dyspnea): Usually the breathlessness of idiopathic pulmonary fibrosis first appears during exercise. Breathlessness can affect day-to-day activities such as showering, climbing stairs, getting dressed and eating. As scarring in the lungs gets worse, breathlessness may prevent all activities.
- Chronic cough: About 85% of people with idiopathic pulmonary fibrosis have a chronic cough that has lasts longer than 8 weeks. This is often a dry cough, but some people may also cough up sputum or phlegm.
Other symptoms may include:
- chest pain or tightness
- unexplained weight loss
- loss of appetite
- tiredness and loss of energy
- change of finger shape called “clubbing”
Idiopathic pulmonary diagnosis
Idiopathic pulmonary fibrosis (IPF) can be difficult to diagnose since many lung diseases can cause breathlessness and cough, and some of these other diseases can have similar symptoms and X-ray results. You may have to see more than one specialist, including a respirologist, to help with the diagnosis.
- Your doctor will ask you questions about your home and work environments, your smoking history and your medical history. This will help them determine whether there were any environmental, occupational, genetic, or other factors that could be linked to the development of pulmonary fibrosis.
- Your doctor will do a physical examination of your lungs and will also examine other parts of your body including your heart, joints, fingernails, skin and muscles.
Although no single test can diagnose idiopathic pulmonary fibrosis, your doctor may recommend a number of different tests including:
- Pulmonary function test (PFT): A pulmonary function test, or breathing test, is a simple test to measure how much air you can blow in and out of your lungs and how well your lungs can absorb oxygen.
- Six-minute walk test: This test helps determine your physical fitness, as well as the amount of oxygen in your blood at rest and with physical activity.
- Chest x-ray: Chest X-rays are simple images that can screen for interstitial lung disease and can sometimes be useful to help monitor progression.
- Blood tests: A number of blood tests can be requested to help identify other causes of interstitial lung disease.
- Computed tomography (CT scan): These radiology images will determine whether there is scarring in your lungs and will help identify the subtype of interstitial lung disease.
- Bronchoscopy: Bronchoscopy is a procedure that involves inserting a small flexible tube, called bronchoscope, through your mouth or nose and into your lungs. This is not necessary for diagnosis but some patients with possible idiopathic pulmonary fibrosis undergo this procedure to help identify the presence of infection or to suggest other subtypes of interstitial lung disease.
- Surgical lung biopsy: Patients with an unclear diagnosis will sometimes undergo a surgical lung biopsy performed by a surgeon under general anesthetic. This test involves small incisions in the side of the chest, which allows removal of lung tissue and its examination under a microscope.
Idiopathic pulmonary fibrosis treatment
There is no cure for idiopathic pulmonary fibrosis and there are currently no procedures or medications that can remove the scarring from the lungs. Treatments are used to slow progression of the lung scarring, and may not necessarily lessen the symptoms of cough and breathlessness. Pirfenidone (Esbriet) and nintedanib have both been shown to slow the progression of idiopathic pulmonary fibrosis; however, some patients cannot take these medications due to their side effects. These medications are not approved for use in other interstitial lung diseases.
Some additional medications can be used to improve the symptoms of idiopathic pulmonary fibrosis, such as shortness of breath and cough. This includes treatment of gastroesophageal reflux with anti-acid therapy and treatment of shortness of breath with opioids (a class of medications that includes morphine). Other treatments include supplemental oxygen, pulmonary rehabilitation (exercise training, education and support for people with chronic lung disease), and lung transplant.
It is important to work with your family doctor or respirologist (lung specialist) to find the best treatment for you. Not all medications will work for everyone. Your doctor knows your medical history and will be able to determine the best treatment for you.
Lifestyle changes
Idiopathic pulmonary fibrosis is an irreversible, progressive disease. So it is important to learn good coping skills and educate yourself about the disease as much as possible.
- Quitting smoking is the most important thing you can do to help slow down the progression of any lung disease.
- Get a flu shot each year.
- Ask your doctor about getting a pneumonia shot.
- Keep away from people with chest infections and colds.
- Wash your hands properly and often.
- Stay as fit as you can.
Oxygen
The scarring in the lungs can prevent oxygen from being absorbed into your body. Low oxygen levels can make you feel short of breath and tired. If your blood oxygen levels are too low, your doctor may prescribe supplemental oxygen (home oxygen). This helps to reduce breathlessness and can help you be more active. Some people with idiopathic pulmonary fibrosis may need oxygen therapy all the time, while others may only need it during exercise or sleep.
If your doctor has prescribed supplemental oxygen, it is important to use it as prescribed. Many patients fear that they will become “addicted” to supplemental oxygen. Supplemental oxygen is not addictive and your body needs a proper amount to maintain normal body functions. People who take supplemental oxygen must continue taking their other medications.
Not everyone who has idiopathic pulmonary fibrosis needs to be on oxygen. Generally, oxygen therapy can help only people with very low blood-oxygen levels (hypoxemia). To find out if you need supplemental oxygen, speak to your doctor or certified respiratory educator.
Medications
There are no medications that cure idiopathic pulmonary fibrosis or decrease the amount of scarring in the lungs. Some medications help slow the progression of pulmonary fibrosis. It is very difficult to find medications that will work for everyone with idiopathic pulmonary fibrosis. Medications for idiopathic pulmonary fibrosis have side effects in some patients, so it is important to talk to your doctor about the possible risks.
As with any medication for any condition, you should talk to your doctor about different treatment options and ask about medication side effects.
Pirfenidone
Pirfenidone is an anti-scarring (anti-fibrotic) medication that slows the progression of idiopathic pulmonary fibrosis. Some patients taking pirfenidone have side effects, most commonly stomach upset and skin rash, particularly with exposure to sun. Pirfenidone has been approved by Health Canada for the treatment of mild to moderate idiopathic pulmonary fibrosis.
Nintedanib
Nintedanib is an anti-scarring (anti-fibrotic) medication that slows progression of idiopathic pulmonary fibrosis. Some patients taking nintedanib have side effects, most commonly including diarrhea.
Corticosteroid pills
Corticosteroid pills (for example, Prednisone©) can reduce inflammation in your lungs by suppressing your immune system. Corticosteroids are only used in patients with idiopathic pulmonary fibrosis who have an acute exacerbation of their lung fibrosis, and can be harmful in patients with idiopathic pulmonary fibrosis that have scarring that is stable or slowly worsening.
N-Acetylcysteine (oral or aerosolized)
N-acetylcysteine (NAC, mucomyst) is an antioxidant that has frequently been used in patients with idiopathic pulmonary fibrosis. A large clinical trial published in May 2014 showed that NAC does not slow progression of idiopathic pulmonary fibrosis.
Other medications
Other medications have been studied and previously used in idiopathic pulmonary fibrosis, including azathioprine, cyclophosphamide, and others. These medications are not recommended in idiopathic pulmonary fibrosis as they have no proven benefit in idiopathic pulmonary fibrosis and are associated with significant side effects.
Gastrointestinal issues
Some medications for idiopathic pulmonary fibrosis (IPF) can cause nausea, lack of appetite and diarrhea. Always take your medication with a meal. Ask your doctor about lowering your dose if you are unable to tolerate the side effects.
- For loss of appetite:
- Eat several small meals throughout the day if you are not hungry for big meals.
- Add olive oil, milk or yogurt to increase calories and protein in a meal.
- Take a walk before you eat.
- Ask your doctor about medication to help increase your appetite.
- For nausea or vomiting:
- Ask your doctor about prescription medication to ease nausea.
- Eat bland foods such as toast or rice.
- Drink peppermint tea, ginger tea or ginger ale.
- For diarrhea:
- Avoid high fiber foods that are hard to digest (such as beans or raw vegetables).
- Eat bland foods such as toast or rice.
- Eat small meals and drink plenty of water between meals.
- Ask your doctor about medications to help reduce diarrhea.
Pulmonary rehabilitation
Pulmonary rehabilitation is an exercise and educational program designed just for patients with lung disease. Pulmonary rehabilitation can help in teaching patients with idiopathic pulmonary fibrosis how to breathe more efficiently and to perform their activities of daily living with less breathlessness.
Most pulmonary rehabilitation programs are designed for people with COPD (emphysema and chronic bronchitis), although the majority of pulmonary rehabilitation programs in Canada accept and welcome patients with idiopathic pulmonary fibrosis.
Lung transplant
Lung transplant is not right for everyone, but it may be a treatment option for some people. It is important to work with your doctor to see if lung transplant is an option for you.
If a person qualifies for a lung transplant, they are put on a waitlist for organ donation. The wait can be long and the surgery can be risky. People who get transplants must take several anti-rejection medications (immune-suppressants) for the rest of their lives.
Pulmonary fibrosis causes
It can be challenging for doctors to figure out what causes pulmonary fibrosis. Sometimes they are able to identify one or more causes of your disease. Pulmonary fibrosis of unknown cause is called “idiopathic pulmonary fibrosis”.
There are five main categories of identifiable causes of pulmonary fibrosis: Medications-induced, Radiation-induced, Environmental, Autoimmune, and Occupational. In the United States, Environmental and Autoimmune causes seem to be the most common types of pulmonary fibrosis of known cause.
Environmental causes
Environmental causes of pulmonary fibrosis are typically called hypersensitivity pneumonitis or chronic hypersensitivity pneumonitis. Hypersensitivity pneumonitis occurs when the lungs react with inflammation and scarring after breathing in mold spores, bacteria, animal proteins (especially from indoor or caged birds), or other known triggers. No one is certain why some people are so susceptible to developing hypersensitivity pneumonitis and others are not.
- Bird and animal droppings
- Exposure to mold
Occupational causes
Occupational causes of pulmonary fibrosis, also called pneumoconiosis, can develop after significant exposure to a wide variety of inorganic dusts, including asbestos, silica, coal dust, beryllium, and hard metal dusts.
Long-term exposure to a number of toxins and pollutants can damage your lungs. These include:
- Silica dust
- Asbestos fibers
- Hard metal dusts
- Coal dust
- Grain dust
Radiation treatments
Some people who receive radiation therapy for lung or breast cancer show signs of lung damage months or sometimes years after the initial treatment. The severity of the damage may depend on:
- How much of the lung was exposed to radiation
- The total amount of radiation administered
- Whether chemotherapy also was used
- The presence of underlying lung disease
Medications
Many drugs can damage your lungs, especially medications such as:
- Chemotherapy drugs. Drugs designed to kill cancer cells, such as methotrexate (Trexall, Otrexup, others) and cyclophosphamide, can also damage lung tissue.
- Heart medications. Some drugs used to treat irregular heartbeats, such as amiodarone (Cordarone, Nexterone, Pacerone), may harm lung tissue.
- Some antibiotics. Antibiotics such as nitrofurantoin (Macrobid, Macrodantin, others) or ethambutol can cause lung damage.
- Anti-inflammatory drugs. Certain anti-inflammatory drugs such as rituximab (Rituxan) or sulfasalazine (Azulfidine) can cause lung damage.
Medical conditions
Lung damage can also result from a number of conditions, including:
- Dermatomyositis
- Polymyositis
- Mixed connective tissue disease
- Systemic lupus erythematosus
- Rheumatoid arthritis
- Sarcoidosis
- Scleroderma
- Sjögren’s syndrome
- Pneumonia
Many substances and conditions can lead to pulmonary fibrosis. Even so, in most cases, the cause is never found. Pulmonary fibrosis with no known cause is called idiopathic pulmonary fibrosis.
Researchers have several theories about what might trigger idiopathic pulmonary fibrosis, including viruses and exposure to tobacco smoke. Also, some forms of idiopathic pulmonary fibrosis run in families, and heredity may play a role in idiopathic pulmonary fibrosis.
Many people with idiopathic pulmonary fibrosis may also have gastroesophageal reflux disease (GERD) — a condition that occurs when acid from your stomach flows back into your esophagus. Ongoing research is evaluating if gastroesophageal reflux disease (GERD) may be a risk factor for idiopathic pulmonary fibrosis, or if GERD may lead to a more rapid progression of the condition. However, more research is needed to determine the association between idiopathic pulmonary fibrosis and GERD.
Risk factors for pulmonary fibrosis
Factors that make you more susceptible to pulmonary fibrosis include:
- Age. Although pulmonary fibrosis has been diagnosed in children and infants, the disorder is much more likely to affect middle-aged and older adults.
- Sex. Idiopathic pulmonary fibrosis is more likely to affect men than women.
- Smoking. Far more smokers and former smokers develop pulmonary fibrosis than do people who have never smoked. Pulmonary fibrosis can occur in patients with emphysema.
- Certain occupations. You have an increased risk of developing pulmonary fibrosis if you work in mining, farming or construction or if you’re exposed to pollutants known to damage your lungs.
- Cancer treatments. Having radiation treatments to your chest or using certain chemotherapy drugs can increase your risk of pulmonary fibrosis.
- Genetic factors. Some types of pulmonary fibrosis run in families, and genetic factors may be a component.
Pulmonary fibrosis symptoms
Signs and symptoms of pulmonary fibrosis may include:
- Shortness of breath (dyspnea)
- A dry cough
- Fatigue
- Unexplained weight loss
- Aching muscles and joints
- Widening and rounding of the tips of the fingers or toes (clubbing)
The course of pulmonary fibrosis — and the severity of symptoms — can vary considerably from person to person. Some people become ill very quickly with severe disease. Others have moderate symptoms that worsen more slowly, over months or years.
Some people may experience a rapid worsening of their symptoms (acute exacerbation), such as severe shortness of breath, that may last for several days to weeks. People who have acute exacerbations may be placed on a mechanical ventilator. Doctors may also prescribe antibiotics, corticosteroid medications or other medications to treat an acute exacerbation.
Pulmonary fibrosis complications
Complications of pulmonary fibrosis may include:
- High blood pressure in your lungs (pulmonary hypertension). Unlike systemic high blood pressure, this condition affects only the arteries in your lungs. It begins when the smallest arteries and capillaries are compressed by scar tissue, causing increased resistance to blood flow in your lungs. This in turn raises pressure within the pulmonary arteries and the lower right heart chamber (right ventricle). Some forms of pulmonary hypertension are serious illnesses that become progressively worse and are sometimes fatal.
- Right-sided heart failure (cor pulmonale). This serious condition occurs when your heart’s lower right chamber (ventricle) has to pump harder than usual to move blood through partially blocked pulmonary arteries.
- Respiratory failure. This is often the last stage of chronic lung disease. It occurs when blood oxygen levels fall dangerously low.
- Lung cancer. Long-standing pulmonary fibrosis also increases your risk of developing lung cancer.
- Lung complications. As pulmonary fibrosis progresses, it may lead to complications such as blood clots in the lungs, a collapsed lung or lung infections.
Pulmonary fibrosis stages
Pulmonary fibrosis often gets worse over time. No one can predict how fast a patient’s pulmonary fibrosis will progress. In some people, pulmonary fibrosis progresses very quickly while others live with the disease for many years.
When someone is diagnosed with pulmonary fibrosis, it is normal to wonder: how advanced is the disease? There is no formal staging system for pulmonary fibrosis. Physicians use different factors, like the ones listed below, to describe the disease as mild, moderate, severe or very severe:
- Symptoms: Discussing symptoms with your doctor is key to determining the severity of your pulmonary fibrosis. You might be asked about how frequently you become breathless or how often you cough. Worsening breathlessness and cough don’t always mean the disease has progressed. But knowing your symptoms helps your doctor better understand your particular disease.
- Pulmonary Function Tests or Lung Function Tests give your doctor important information about the amount of air the lungs can hold and how forcefully you can empty air from the lungs. A pulmonary fibrosisT reveals your forced vital capacity (FVC) which is the amount of air that is exhaled starting from a maximal inhalation. This percentage can help your physician understand if you have mild, moderate, severe or very severe pulmonary fibrosis. The most basic test is spirometry.
- A six-minute walk test may be done to measure your exercise capacity.
- A high-resolution CT scan (HRCT) shows how much scarring is in the lungs.
A scoring system was recently developed called the GAP Model which uses Gender, Age and Physiology (and includes your forced vital capacity (FVC) score and diffusing capacity) to stage pulmonary fibrosis. Not all physicians use this staging system. Science is always advancing so ask your doctor to explain your stage and the tests you may need.
Pulmonary fibrosis diagnosis
To diagnose pulmonary fibrosis, your doctor may review your medical and family history, discuss your signs and symptoms, review any exposure you’ve had to dusts, gases and chemicals, and conduct a physical exam. During the physical exam, your doctor will use a stethoscope to listen carefully to your lungs while you breathe. He or she may also suggest one or more of the following tests.
Imaging tests
- Chest X-ray. A chest X-ray shows images of your chest. This may show the scar tissue typical of pulmonary fibrosis, and it may be useful for monitoring the course of the illness and treatment. However, sometimes the chest X-ray may be normal, and further tests may be required to explain your shortness of breath.
- Computerized tomography (CT) scan. CT scanners use a computer to combine X-ray images taken from many different angles to produce cross-sectional images of internal structures in the body. A high-resolution CT scan can be particularly helpful in determining the extent of lung damage caused by pulmonary fibrosis. Also, some kinds of fibrosis have characteristic patterns.
- Echocardiogram. An echocardiogram uses sound waves to visualize the heart. It can produce still images of your heart’s structures, as well as videos that show how your heart is functioning. This test can evaluate the amount of pressure occurring in the right side of your heart.
Lung function tests
- Pulmonary function testing. Several types of pulmonary function tests may be conducted. In a test called spirometry, you exhale quickly and forcefully through a tube connected to a machine. The machine measures how much air your lungs can hold and how quickly you can move air in and out of your lungs. Other tests may be conducted to measure your lung volumes and diffusing capacity.
- Pulse oximetry. This simple test uses a small device placed on one of your fingers to measure the oxygen saturation in your blood. Oximetry can serve as a way to monitor the course of the disease.
- Exercise stress test. An exercise test on a treadmill or stationary bike may be used to monitor your lung function when you’re active.
- Arterial blood gas test. In this test, your doctor tests a sample of your blood, usually taken from an artery in your wrist. The oxygen and carbon dioxide levels in the sample are then measured.
Tissue sample (biopsy)
If other tests haven’t diagnosed the condition, doctors may need to remove a small amount of lung tissue (biopsy). The biopsy is then examined in a laboratory to diagnose pulmonary fibrosis or rule out other conditions. The tissue sample may be obtained in one of these ways:
- Bronchoscopy. In this procedure, your doctor removes very small tissue samples — generally no larger than the head of a pin — using a small, flexible tube (bronchoscope) that’s passed through your mouth or nose into your lungs. The tissue samples are sometimes too small for an accurate diagnosis. The biopsy may also be used to rule out other conditions. The risks of bronchoscopy are generally minor and might include a temporary sore throat or discomfort in your nose from the passage of the bronchoscope. However, serious complications can include bleeding or a deflated lung. During bronchoscopy, your doctor may conduct an additional procedure called bronchoalveolar lavage. In this procedure, your doctor injects salt water through a bronchoscope into a section of your lung, and then immediately suctions it out. The solution that’s withdrawn contains cells from your air sacs. Although bronchoalveolar lavage samples a larger area of the lung than other procedures do, it may not provide enough information to diagnose pulmonary fibrosis. It might also be used to rule out other conditions.
- Surgical biopsy. Although a surgical biopsy is more invasive and has potential complications, it may be the only way to obtain a large enough tissue sample to make an accurate diagnosis. This procedure may be done as a minimally invasive surgery, called video-assisted thoracoscopic surgery (VATS), or as an open surgery (thoracotomy). During video-assisted thoracoscopic surgery (VATS), your surgeon inserts surgical instruments and a small camera through two or three small incisions between your ribs. The camera allows your surgeon to view your lungs on a video monitor while removing tissue samples from your lungs. This procedure is performed after you’ve been given a general anesthetic, so you’ll be asleep during the procedure. During open surgery (thoracotomy), a surgeon removes a lung sample through an incision in the chest between your ribs. The procedure takes place after you’ve been given a general anesthetic.
Blood tests
Doctors may also order blood tests to evaluate your liver and kidney function, and to test for and rule out other conditions.
Pulmonary fibrosis treatment
The lung scarring that occurs in pulmonary fibrosis can’t be reversed, and no current treatment has proved effective in stopping progression of the disease. Some treatments may improve symptoms temporarily or slow the disease’s progression. Others may help improve quality of life. Doctors will evaluate the severity of your condition to determine the most appropriate treatment for your condition.
Medications
Your doctor may recommend newer medications, including pirfenidone (Esbriet) and nintedanib (Ofev). These medications may help slow the progression of idiopathic pulmonary fibrosis. These medications are called anti-fibrotic agents, meaning that they have shown in clinical trials to slow down the rate of fibrosis or scarring in the lungs. Both medications have been approved by the Food and Drug Administration (FDA) for patients with mild, moderate and severe idiopathic pulmonary fibrosis (IPF). Your doctor will work with you to prescribe treatment tailored to your needs. While taking these medications, you will be monitored closely for any serious side effects. Monitoring will include routine blood work to make sure your liver remains healthy. Ask your doctor for a referral to a palliative care specialist who can help you manage any side effects from the drugs.
Nintedanib can cause side effects such as diarrhea and nausea. Side effects of pirfenidone include rash, nausea and diarrhea.
Additional medications and new formulations of these medications are being developed but have not yet been FDA approved.
There are certain types of pulmonary fibrosis (excluding idiopathic pulmonary fibrosis) that respond to treatment with steroids. Steroids, also known as glucocorticoids, are a class of medication that reduces inflammation (swelling). Corticosteroids can have harmful side effects, especially when used long term. You will need to be carefully monitored if you are on long-term steroids. Other groups of medications prescribed to reduce inflammation include azathioprine, cyclophosphamide and mycophenolate mofetil (Cellcept®, Myfortic®), which work by suppressing the immune system.
Researchers continue to study medications to treat pulmonary fibrosis.
Doctors may recommend anti-acid medications to treat gastroesophageal reflux disease (GERD), a digestive condition that commonly occurs in people with idiopathic pulmonary fibrosis. There are different types of anti-acid medications (e.g., Proton pump inhibitors including Prilosec OTC® and Nexium® as well as H2-Blockers including Zantac® and Pepcid®) that are prescribed to help block the formation of or minimize the amount of acid in the stomach. By doing so, it helps to reduce the amount of acid from the stomach that enters the lungs.
Medicines to treat cough
A dry, hacking cough is a common symptom of pulmonary fibrosis. Treating cough is mostly trial and error. What works for one patient may not work for another. Some treatment options for cough include:
- Over the counter cough medicine like Robitusson® and cough drops
- Prescription cough medicine like hydrocodone (Tussionex PennKenetic®) and benzonatate (Tessalon Perles®)
- Thalidomide (Thalomid® ) may be used for serious cases of cough in some patients.
- There are ongoing clinical trials for pulmonary fibrosis drugs, including ones to help relieve cough. Visit clinicaltrials.gov to see if any are available near you or ask your doctor.
Oxygen therapy
When you use oxygen as a medical treatment, it is called oxygen therapy or supplemental oxygen. Most pulmonary fibrosis patients need oxygen at some point during their treatment. You may need oxygen all day long, or only at night or when you exercise. Each pulmonary fibrosis patient’s oxygen needs are unique and depend on the severity of their disease and lifestyle. Your doctor will have you perform a simple walking test to see if you need supplemental oxygen.
You will monitor your oxygen levels at home using handheld pulse oximeters (available over the counter in many pharmacies). You will aim to maintain your oxygen saturation level above 90 percent throughout the day and night.
Using oxygen can’t stop lung damage, but it can:
- Make breathing and exercise easier
- Prevent or lessen complications from low blood oxygen levels
- Reduce blood pressure in the right side of your heart
- Improve your sleep and sense of well-being
You may receive oxygen when you sleep or exercise, although some people may use it all the time. Some people carry a canister of oxygen, making them more mobile.
Pulmonary rehabilitation
Pulmonary rehabilitation is a program of education and exercise classes that teach you about your disease, how to exercise and how to be more active with less shortness of breath.
Pulmonary rehab offers substantial benefits in improving lung function, reducing symptoms and improving quality of life for people with lung disease like PF. It also helps you learn how to conserve your energy and is a great way to start exercising in a safe environment. The nurses and respiratory therapists will be monitoring you, which can help relieve anxiety.
Pulmonary rehabilitation can help you manage your symptoms and improve your daily functioning. Pulmonary rehabilitation programs focus on:
- Physical exercise to improve your endurance
- Breathing techniques that may improve lung efficiency
- Nutritional counseling
- Counseling and support
- Education about your condition
Lung transplant
In pulmonary fibrosis, once the lung tissue becomes scarred, the damage cannot be reversed. Because of this, lung transplant (a surgical procedure that involves replacing one or both of your diseased lungs with healthy lungs) is a treatment option your doctor may suggest. Having a lung transplant can improve your quality of life and allow you to live a longer life. However, a lung transplant can involve complications such as rejection and infection. Your doctor may discuss with you if a lung transplant may be appropriate for your condition.
A lung transplant can improve your ability to breathe and be active, but it is a major operation. There are risks of complications that occur during and at any time after the operation.
Pulmonary fibrosis patients should be evaluated by a lung transplant physician soon after diagnosis. This specialist team will determine whether or not you are a candidate for this procedure. To be considered eligible for a lung transplant, you will need to meet certain requirements:
- Be in good physical condition aside from your lung function
- Have no other life-threatening illnesses
- Be willing to accept the risks of surgery
- Accept the post-transplant therapy
Lifestyle and home remedies
Being actively involved in your own treatment and staying as healthy as possible are essential to living with pulmonary fibrosis. For that reason, it’s important to:
- Stop smoking. If you have lung disease, it’s very important to stop smoking. Talk to your doctor about options for quitting, including smoking cessation programs, which use a variety of proven techniques to help people quit. And because secondhand smoke can be harmful to your lungs, avoid being around people who are smoking.
- Eat well. People with lung disease may lose weight both because it’s uncomfortable to eat and because of the extra energy it takes to breathe. Yet a nutritionally rich diet that contains adequate calories is essential. Try to eat smaller meals more often during the day. Aim to eat a variety of fruits and vegetables, whole grains, low-fat or fat-free dairy products, and lean meats. Avoid trans fat and saturated fat, too much salt, and added sugars. A dietitian can give you further guidelines for healthy eating.
- Get moving. Regular exercise can help you maintain your lung function and manage your stress. Aim to incorporate physical activity, such as walking or biking, into your daily routine. Talk to your doctor about which activities may be appropriate for you. If you require assistance with mobility over time, such as a wheelchair, look for activities or hobbies you can do that don’t require walking.
- Take time to rest. Make sure to get enough rest. Taking time to rest can help you have more energy and cope with the stress of your condition.
- Get vaccinated. Respiratory infections can worsen symptoms of pulmonary fibrosis. Make sure you receive the pneumonia vaccine and an annual flu shot. It’s important that your family members also be vaccinated. Aim to avoid crowds during flu season.
- Follow your treatment plan. You’ll need to have ongoing treatment from your doctor. Follow your doctor’s instructions, take your medications as prescribed, and adjust your diet and exercise as needed. Go to all of your doctor’s appointments.
Staying physically active is one of the most important things you can do to maintain a good quality of life. It not only helps you physically, it can relieve your stress and improve your self-esteem. It can be challenging for pulmonary fibrosis patients to work up the confidence to exercise. It seems counterintuitive to exercise if you have shortness of breath. However, physical activity can make your body stronger so you become less short of breath doing everyday activities.
Tips for staying active with pulmonary fibrosis:
- Enroll in a pulmonary rehabilitation program. Pulmonary rehab is a program of exercise, education and support to help you learn to breathe and get stronger. Some activities often done in pulmonary rehab include walking on a treadmill, riding a stationary bike, stretching and light weight training.
- Use your oxygen. Many patients find that using oxygen when they exercise is a game changer. They can be more active with less worry.
- Be active every day. This might be as simple as walking to get the mail. It can be tempting to spend most of your day sitting when you are feeling fatigued and breathless. Leave time for rest but also try and push yourself to move around as much as possible.
- Breathing exercises such as belly breathing and pursed lip breathing can help your lungs be more efficient.
Benefits of exercise for pulmonary fibrosis patients:
- Weight control
- Improved energy
- Reduced stress
- Better sleep
- Strengthens heart and muscles which helps you get more oxygen into your bloodstream
- Improved mood
- A sense of achievement
Pulmonary fibrosis prognosis
Pulmonary fibrosis is a progressive disease that naturally gets worse over time. This worsening is related to the amount of fibrosis (scarring) in the lungs. As this occurs, a person’s breathing becomes more difficult, eventually resulting in shortness of breath, even at rest.
Patients with pulmonary fibrosis experience disease progression at different rates. Some patients progress slowly and live with pulmonary fibrosis for many years, while others decline more quickly.
There is no cure for pulmonary fibrosis, but treatments can slow the progression of the disease in some people. Maintaining a healthy lifestyle and working closely with your care team can help you best manage your pulmonary fibrosis.
Pulmonary fibrosis exacerbation
Some patients will experience a sudden worsening of their pulmonary fibrosis, which is referred to as an acute exacerbation. This occurs when there is a triggering event that results in a sudden increase in the processes that lead to scarring. As the lung scarring gets worse, patients have a harder time breathing. The damage to the lungs during an acute exacerbation is permanent.
To determine if you are having an acute exacerbation, doctors take into consideration your symptoms, oxygen levels, CT scan results and often suggest other tests such as a bronchoscopy to assist with diagnosis.
Much is unknown about how to best treat and prevent exacerbations. If your doctor knows what is causing the exacerbation, the trigger will be treated. For example, if you have an infection, you will be prescribed antibiotics. Otherwise, doctors will provide supportive care—for example, extra oxygen.
During an acute exacerbation, many patients require hospitalization. If your exacerbation is severe, you may require ventilator support. This means that you are placed in a machine that acts as your lungs. Patients who are placed on a ventilator during an acute exacerbation are at an increased risk of dying. This is why it is important to talk with your doctor and family about your wishes and fill out an advance directive as soon as you are diagnosed with pulmonary fibrosis. When a serious health event occurs, the advance directive will help your family and care team honor your wishes if you are not able to speak for yourself.
Pulmonary fibrosis life expectancy
Pulmonary fibrosis is a serious disease, but research advancements are being made all the time that allow people to live longer and have a better quality of life.
No doctor can predict any one person’s lifespan with pulmonary fibrosis. Survival rates that you see for the disease are based on population averages taken over many years. They cannot predict your individual experience and your prognosis with pulmonary fibrosis can differ depending on factors such as age, health, lifestyle, and severity of the disease at diagnosis.
Patients with pulmonary fibrosis experience disease progression at different rates. Some patients progress slowly and live with pulmonary fibrosis for many years, while others decline more quickly.
If you are diagnosed with pulmonary fibrosis, the best thing you can do is talk with your doctor about how to take care of yourself. Eating right, exercising, and protecting your lungs are important in keeping you as healthy as possible. It is also important to discuss if any medications might be appropriate for treating your pulmonary fibrosis or symptoms.
That being said, it is always a good idea to plan ahead and make arrangements for the future. Consider asking your doctor for a referral to a counselor, therapist or social worker who can help you through this stressful time.