Contents
What is pyogenic granuloma
Pyogenic granuloma is a common, benign (harmless) growth that often appears as a rapidly growing, bleeding bump on the skin or inside the mouth. Pyogenic granuloma is composed of blood vessels and may occur at the site of minor injury. Pyogenic granuloma carries no risk of cancer, is not contagious (cannot be spread to another person) and is not due to an infection.
When a pyogenic granuloma occurs in a pregnant woman, it is sometimes called a “pregnancy tumor” (granuloma gravidarum). Pyogenic granulomas develop in up to 5% of pregnant women.
Pyogenic granulomas occur in people of all races. Women are more frequently affected by pyogenic granulomas than men, though male and female children are equally affected.
Pyogenic granulomas are most often seen in:
- Children and young adults
- Pregnant women
- Women taking oral contraceptives
- People taking certain oral retinoid medications, including isotretinoin or acitretin (Soriatane®)
- People taking protease inhibitors such as indinavir (Crixivan®)
- People on chemotherapy
See your doctor if you notice any rapidly enlarging skin growth in order to establish a correct diagnosis. Because it is prone to easy bleeding, a pyogenic granuloma lesion should be covered with a bandage until you see your doctor.
Pyogenic granulomas that develop in pregnant women often resolve after delivery. Similarly, pyogenic granulomas associated with medications usually improve when the medicine is discontinued or the dosage is lowered. Depending on the size of the pyogenic granuloma and its location and symptoms, the doctor may decide that no treatment is necessary for pregnant women or for people who can safely stop or lower the dose of the medication that caused the lesion.
Although pyogenic granuloma is a benign condition, it is frequently removed due to its tendency to bleed, its tenderness, and its distressing appearance. However, untreated pyogenic granulomas may go away on their own.
- The main problem with pyogenic granulomas is the way that they ooze and bleed so easily after minor knocks. This can be of great nuisance, but they are usually not painful.
- People often worry that their rapid growth and bleeding mean that they are cancerous, even though they are not; however, you should always see your doctor if you have a rapidly growing skin lump.
In obvious cases of pyogenic granuloma, your physician may choose to treat it immediately after obtaining the biopsy. Such treatments include:
- Scraping and burning (curettage and cauterization). After numbing with local anesthetic, the area is scraped with a sharp instrument (a curette) and burned with an electric needle (cautery).
- Silver nitrate solution
- Topical imiquimod cream (Aldara®)
- Laser treatment
- Freezing with liquid nitrogen (cryotherapy)
- Surgical removal (excision)
Approximately 40% of pyogenic granulomas come back (recur) after treatment, especially those lesions located on the trunk of teenagers and young adults. Recurrent pyogenic granulomas are best treated by surgical excision.
Make an appointment with a dermatologist or another physician if any rapidly enlarging or bleeding growth develops on your skin or in the areas lining your nose or mouth (mucous membranes).
You should always go straight to your doctor if you have any marks on your skin that are growing or bleeding.
Are pyogenic granulomas inherited?
No. There doesn’t appear to be an increased risk in other family members.
Can a pyogenic granuloma be cured?
Yes, by removing it or treating it with a cream (see treatment below).
What do pyogenic granulomas look like?
As pyogenic granulomas are made up of small blood vessels, they are bright red; later they may turn a darker shade. Their surface is shiny and moist but may become crusty after they have bled.
Pyogenic granulomas stick out from the surface of the skin. Pyogenic granulomas are seldom more than 1 cm across. Some have a bumpy surface and look rather like a raspberry, while others are narrower where they come out from the skin and look as if they are on a stalk.
Figure 1. Pyogenic granuloma nose
Figure 2. Pyogenic granuloma mouth
Figure 3. Pyogenic granuloma gums
Figure 4. Pyogenic granuloma lip
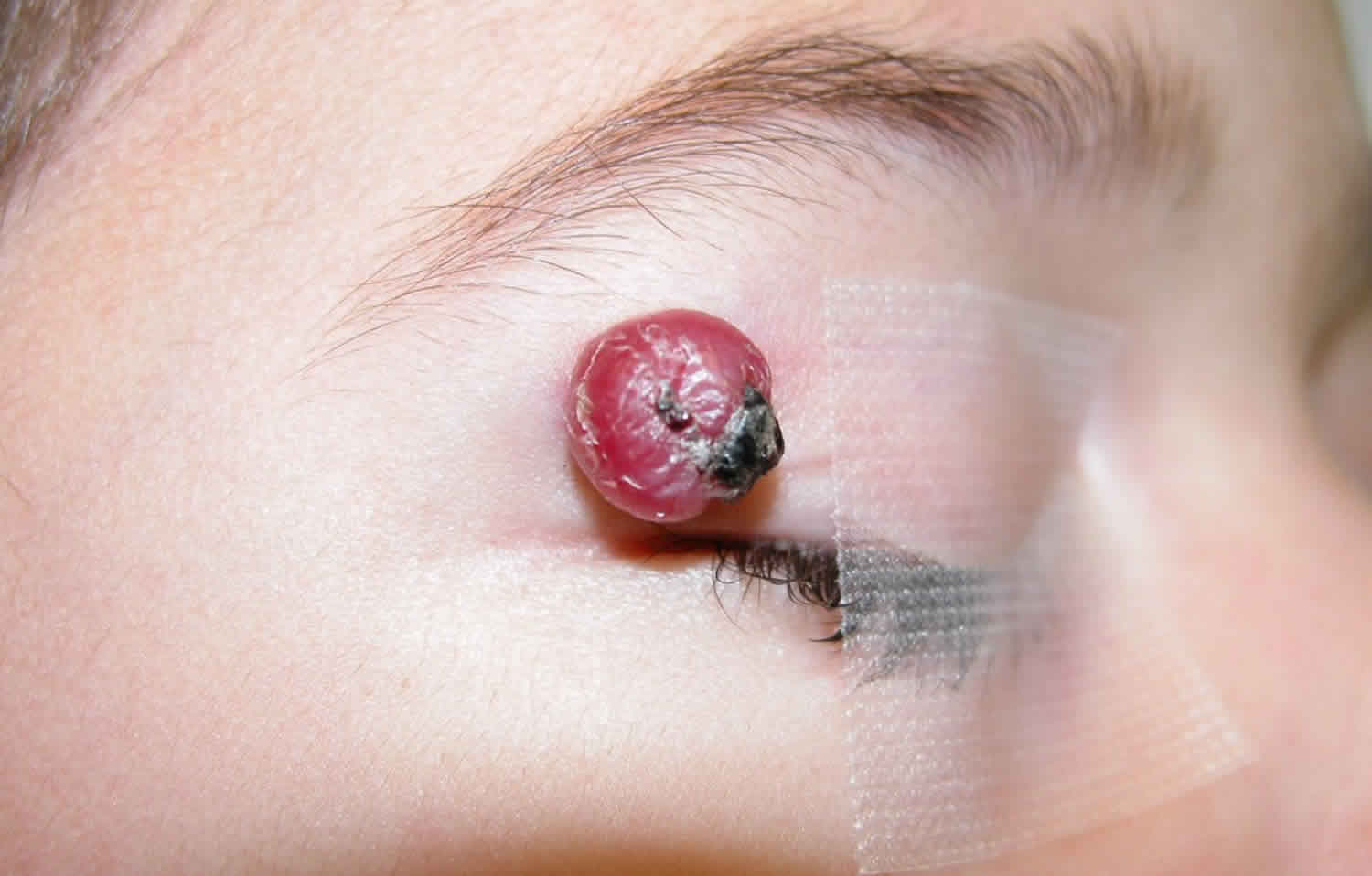
Figure 5. Pyogenic granuloma eye
Footnote: A 30-year-old man presented with a pedunculated lesion on his right lower eyelid that had grown over a period of 3 days. Two weeks before presentation, a cyst had ruptured on the same eyelid. The new lesion started as a small lump on the bulbar conjunctiva and progressively increased in size until it protruded from the eyelid. The patient’s clinical course and a physical examination were suggestive of a pyogenic granuloma, a benign vascular lesion characterized by inflammatory cells and lobular capillary proliferation. Conjunctival pyogenic granulomas grow rapidly in the days to weeks after a conjunctival injury from surgery or trauma and can develop on the conjunctiva or external surfaces of the eyelids. The differential diagnosis includes suture granulomas, squamous papillomas, and malignant tumors, such as squamous-cell carcinoma and amelanotic melanoma. Pyogenic granulomas are often friable and prone to bleeding and can be treated with topical glucocorticoids or surgical excision. In this case, an intralesional injection of triamcinolone was administered at the time of excision to reduce the risk of recurrence. A histopathological assessment confirmed the diagnosis. On review, 3 months after excision, there was minimal scarring of the conjunctival surface and no evidence of recurrence.
[Source 1 ]Figure 6. Pyogenic granuloma finger
Pyogenic granuloma clinical findings
Distribution
- Pyogenic granuloma can arise on any part of the body but the most common sites are the fingers / hands, head and upper trunk.Morphology
- Pyogenic granuloma starts as a small red spot but quickly enlarges into a nodule
- Initially smooth, but often becomes eroded and bleeds significantly on contact
Pyogenic granuloma causes
The exact cause of pyogenic granulomas is unknown. Most pyogenic granulomas come up for no obvious reason, but some appear to follow minor damage to the skin, such as a cut that does not heal properly or a prick from a thorn. Pyogenic granulomas can also occur after starting certain medications, such as retinoids (which are sometimes used for the treatment of acne). Pyogenic granulomas often appear following an injury on the hands, arms, or face.
Pyogenic granulomas are common in children, young adults and pregnancy, but can arise at any age. Pyogenic granuloma is sudden in onset, grows rapidly and bleeds after minimal trauma.
Pyogenic granuloma signs and symptoms
Typically, pyogenic granulomas appear as a beefy, red bump that enlarges rapidly over a few weeks. On average, pyogenic granulomas are about 5–10 mm in diameter. They may bleed easily and, in some cases, can be tender. Very rarely, more than one lesion of pyogenic granuloma may develop at the same time at the same site.
The most common locations for pyogenic granulomas include:
- Lips, gums, and inner mouth (particularly in pregnant women)
- Hands and fingers
- Head and neck
- Feet and toes
- Upper trunk
Pyogenic granuloma possible complications
These problems may occur:
- Bleeding from the granuloma
- Return of the condition after treatment
Pyogenic granuloma diagnosis
Your health care provider will do a physical exam to diagnose this condition.
You may also need a skin biopsy to confirm the diagnosis.
Although the diagnosis is often straightforward the main differential diagnosis is that of an amelanotic melanoma, which tend to bleed less than pyogenic granuloma. Other features that may increase the level of suspicion include no clear history of trauma and an atypical site or age group. To this end, lesions needing treatment are best removed surgically (deep curettage and cautery, or excision) and sent for histology.
Pyogenic granuloma treatment
If the diagnosis of pyogenic granuloma is suspected, your doctor will probably want to perform a skin biopsy. The procedure involves:
- Numbing the skin with an injectable anesthetic.
- Sampling a small piece of skin by using a flexible razor blade, a scalpel, or a tiny cookie cutter (called a “punch biopsy”). If a punch biopsy is taken, a stitch (suture) or two may be placed and will need to be removed 6–14 days later.
- Having the skin sample examined under the microscope by a specially trained physician (dermatopathologist).
Small pyogenic granulomas may go away suddenly. Larger bumps are treated with:
- Surgical shaving or excision
- Electrocautery (heat)
- Freezing
- A laser
- Creams applied to the skin (may not be as effective as surgery)
A few pyogenic granulomas lose their colour and shrivel with time, but most are such a nuisance that they need to be treated before then. Freezing a pyogenic granuloma with liquid nitrogen can get rid of it but does not provide a specimen that can be checked in the laboratory. The usual treatment is to scrape pyogenic granulomas off with a sharp spoon-like instrument (a curette) after the area has been made numb by an injection of a local anaesthetic. The bleeding area left behind is then sealed with a hot point (cauterized).
A gel containing timolol or topical steroids have also been used successfully to treat pyogenic granulomas. Although the evidence for this is still limited, it is growing. This maybe especially useful in children as it avoids more invasive procedures. Other non-surgical treatments that have been used with variable success on these lesions, mostly when they are multiple or recurrent, are steroid injections, imiquimod (medication cream used to treat warts and sun damage, works by stimulating the immune system), silver nitrate, and lasers.
Pyogenic granuloma prognosis
Most pyogenic granulomas can be removed. A scar may remain after treatment. There is a high chance that the problem will come back if the whole granuloma is not destroyed during treatment. There is a risk of up to 15% of the pyogenic granuloma coming back. In these cases, the area is sometimes cut out and the wound closed with stitches.
- Pyogenic Granuloma of the Conjunctiva. N Engl J Med 2017; 376:1667 DOI: 10.1056/NEJMicm1613657 https://www.nejm.org/doi/full/10.1056/NEJMicm1613657[↩]