Contents
- What is red blood cell count
- When is red blood cell count ordered?
- What are red blood cells
- High red blood cell count
- Low red blood cell count
What is red blood cell count
Red blood cell count is the number of red blood cells in a microliter (μL or mcL or 1 mm3) of blood. Red blood cell count number varies from time to time even in healthy individuals. However, the typical red blood cell count range for adult males is 4,700,000 to 6,100,000 cells per microliter (μL), and that for adult females is 4,200,000 to 5,400,000 cells per microliter (μL).
Normal red blood cell count:
- Male – 4.7 to 6.1 million cells per microlitre (cells/mcL)
- Female – 4.2 to 5.4 million cells/mcL
The absolute numbers for red blood cell, white blood cell, and platelet counts can vary depending on how they are measured and the instruments used to measure them. For this reason, different sources may present different, but very similar, ranges of normal red blood cell count values.
An increase in the number of circulating red blood cells increases the blood’s oxygen-carrying capacity, much as a decrease in the number of circulating red blood cells decreases the blood’s oxygen-carrying capacity. Changes in this number may affect health. For this reason, red blood cell counts are routinely consulted to help diagnose and evaluate the courses of certain diseases.
A red blood cell count is typically ordered as part of a complete blood count (CBC) and may be used as part of a health checkup to screen for a variety of conditions. Red blood cell count test may also be used to help diagnose and/or monitor a number of diseases that affect the production or lifespan of red blood cells (RBCs).
Red blood cells (RBCs) circulate in the blood and carry oxygen throughout the body. They are produced in the bone marrow and then released into the bloodstream as they mature. Red blood cells (RBCs) have a typical lifespan of about 120 days and are continuously renewed and replaced as they age and degrade or are lost through bleeding. A relatively stable number of red blood cells is maintained in the circulation by increasing or decreasing the rate of production by the bone marrow.
Some conditions affect red blood cell production and may cause an increase or decrease in the number of mature red blood cells released into the blood circulation. Other conditions may affect the lifespan of red blood cells in circulation, especially if the red blood cells are deformed due to an inherited or acquired defect or abnormality. If red blood cells are lost or destroyed faster than they can be replaced, if bone marrow production is disrupted, or if the red blood cells produced do not function normally, then a person will become anemic, which affects the amount of oxygen reaching tissues.
If too many red blood cells are produced and released, then a person can develop polycythemia. This can cause decreased blood flow and related problems.
While a red blood cell count can be used to detect a problem with red blood cell production and/or lifespan, it cannot determine the underlying cause. In addition to the full complete blood count (CBC), some other tests may be performed at the same time or as follow up to help establish a diagnosis. Examples include:
- Blood smear
- Reticulocyte count
- Iron studies
- Vitamin B12 and folate levels
- In more severe conditions, a bone marrow examination
When is red blood cell count ordered?
A red blood cell count count is ordered as a part of the complete blood count (CBC), often as part of a routine physical or as part of a pre-surgical workup. When someone has signs and symptoms suggesting a disease that might affect red blood cell production, a complete blood count (CBC) that includes the red blood cell count may help make a diagnosis.
Some common signs and symptoms associated with low red blood cell count (anemia) that generally lead to a health practitioner ordering a CBC are:
- Weakness or fatigue
- Lack of energy
- Paleness
Some signs and symptoms that may appear with a high red blood cell count count (polycythemia) include:
- Disturbed vision
- Headache, dizziness
- Flushing
- Enlarged spleen
Red blood cell count test may also be performed on a regular basis to monitor people who have been diagnosed with conditions such as blood disorders, kidney disease, bleeding problems, chronic anemia, and polycythemia. Chemotherapy or radiation therapy often decreases bone marrow production of all the blood cells. Thus, a complete blood count (CBC) is typically ordered at regular intervals when monitoring people who are undergoing treatment for cancer.
What does abnormal red blood cell count test result mean?
Since a red blood cell count count is performed as part of a complete blood count (CBC), results from other components are taken into consideration. A rise or drop in the red blood cell count must be interpreted in conjunction with other parameters, such as hemoglobin (Hb), hematocrit (Hct), reticulocyte count, and/or red blood cell indices (e.g., MCV, MCHC, RDW).
Blood or red cell loss that occurs suddenly or over time and diseases and conditions that decrease red blood cell production in the bone marrow will result in a low red blood cell count.
A recent blood transfusion can affect results of an red blood cell count.
Alteration of the number of red blood cells is often temporary and can be easily corrected and/or returned to normal levels by treating and resolving the underlying condition.
During pregnancy, body fluids tend to accumulate, thus decreasing the red blood cell count in relation to fluid volume.
Living at high altitudes causes an increase in red blood cell count; this is the body’s response to the decreased oxygen available at these heights.
Women tend to have slightly lower red blood cell counts than men.
Some causes of a low red blood cell count (anemia) include:
- Trauma
- Red blood cell destruction, for example hemolytic anemia caused by autoimmunity or defects in the red cell itself; the defects could be a hemoglobinopathy (e.g., sickle cell anemia), thalassemia, an abnormality in the red blood cell membrane (e.g., hereditary spherocytosis), or enzyme defect (e.g., G6PD deficiency).
- Sudden (acute) or chronic bleeding from the digestive tract (e.g., ulcers, polyps, colon cancer) or other sites, such as the bladder or uterus (in women, heavy menstrual bleeding, for example)
- Nutritional deficiency such as iron deficiency or vitamin B12 or folate deficiency
- Bone marrow damage (e.g., toxin, radiation or chemotherapy, infection, drugs)
- Bone marrow disorders such as leukemia, multiple myeloma, myelodysplasia, or lymphoma or other cancers that spread to the marrow
- Chronic inflammatory disease or condition
- Kidney failure—severe and chronic kidney diseases lead to decreased production of erythropoietin, a hormone produced by the kidneys that stimulates red blood cell production by the bone marrow.
Some causes of a high red blood cell count (polycythemia) include:
- Dehydration—as the volume of fluid in the blood drops, the count of red blood cells per volume of fluid artificially rises.
- Lung (pulmonary) disease—if someone is unable to breathe in and absorb sufficient oxygen, the body tries to compensate by producing more red blood cells.
- Pulmonary fibrosis – a lung condition that causes scarring of the lungs
- Congenital heart disease—with this condition, the heart is not able to pump blood efficiently, resulting in a decreased amount of oxygen getting to tissues.
- The body tries to compensate by producing more red blood cells.
- Kidney tumor that produces excess erythropoietin
- Smoking
- Genetic causes (altered oxygen sensing, abnormality in hemoglobin oxygen release)
- Polycythemia vera—a rare disease in which the body produces excess red blood cells inappropriately.
Do diet and nutrition help keep red blood cells at healthy levels?
Yes, to the extent that if you eat a well-balanced diet, you can prevent anemia due to a lack of iron, vitamin B12, or folate in the foods you eat. Sometimes use of a supplement is recommended if you are at risk of a vitamin deficiency. However, the most common cause of vitamin B12 deficiency is malabsorption, and the most common cause of iron deficiency is bleeding. These conditions and other red blood cell problems that are caused by diseases other than nutritional deficiencies will not be corrected by diet.
Are there symptoms I should recognize if my red blood cells are dangerously low or high?
Fatigue and weakness may indicate a low or high red blood cell count. Fainting, pallor, shortness of breath, dizziness, and/or altered mental status can also indicate a low red blood cell count. Disturbed vision, headache, and flushing may be present with increased numbers of red blood cells.
What are red blood cells
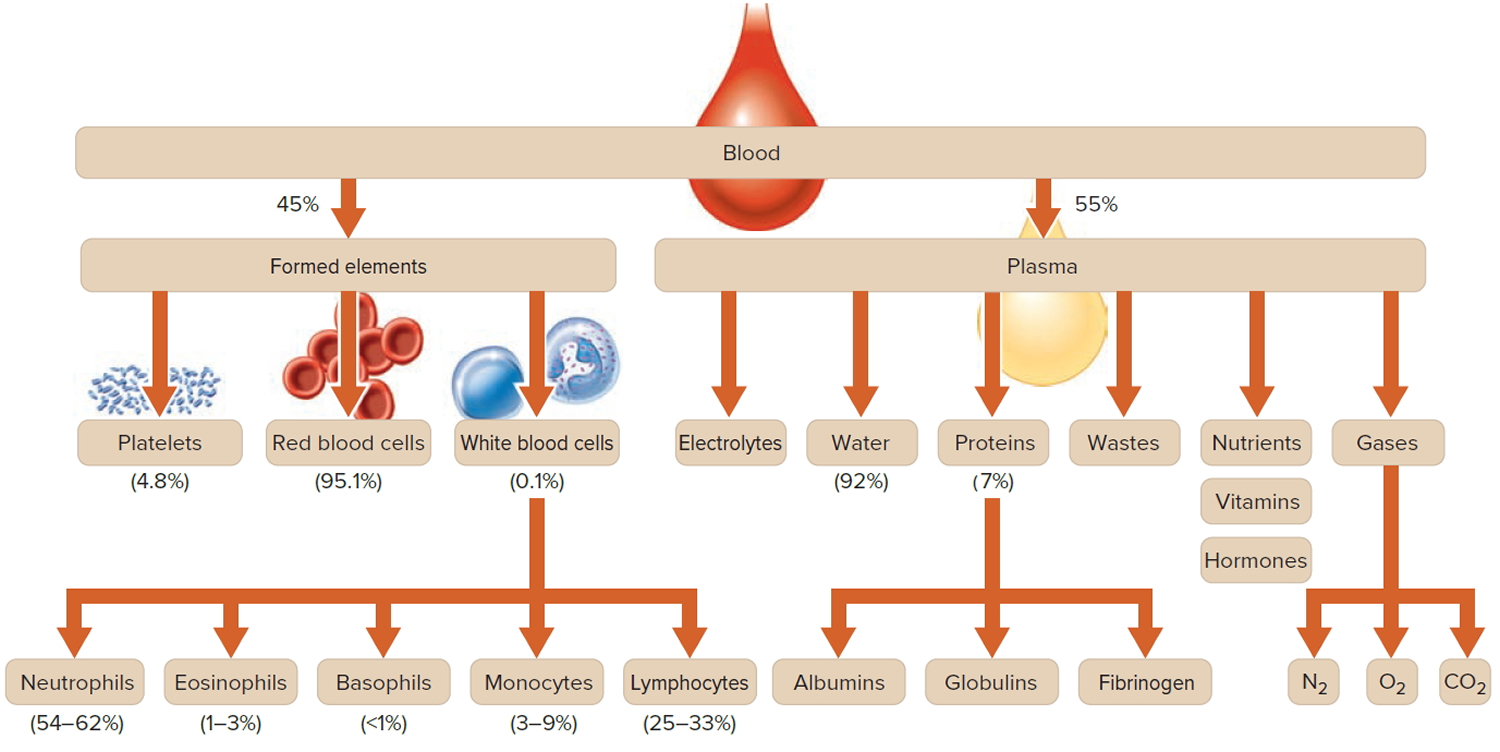
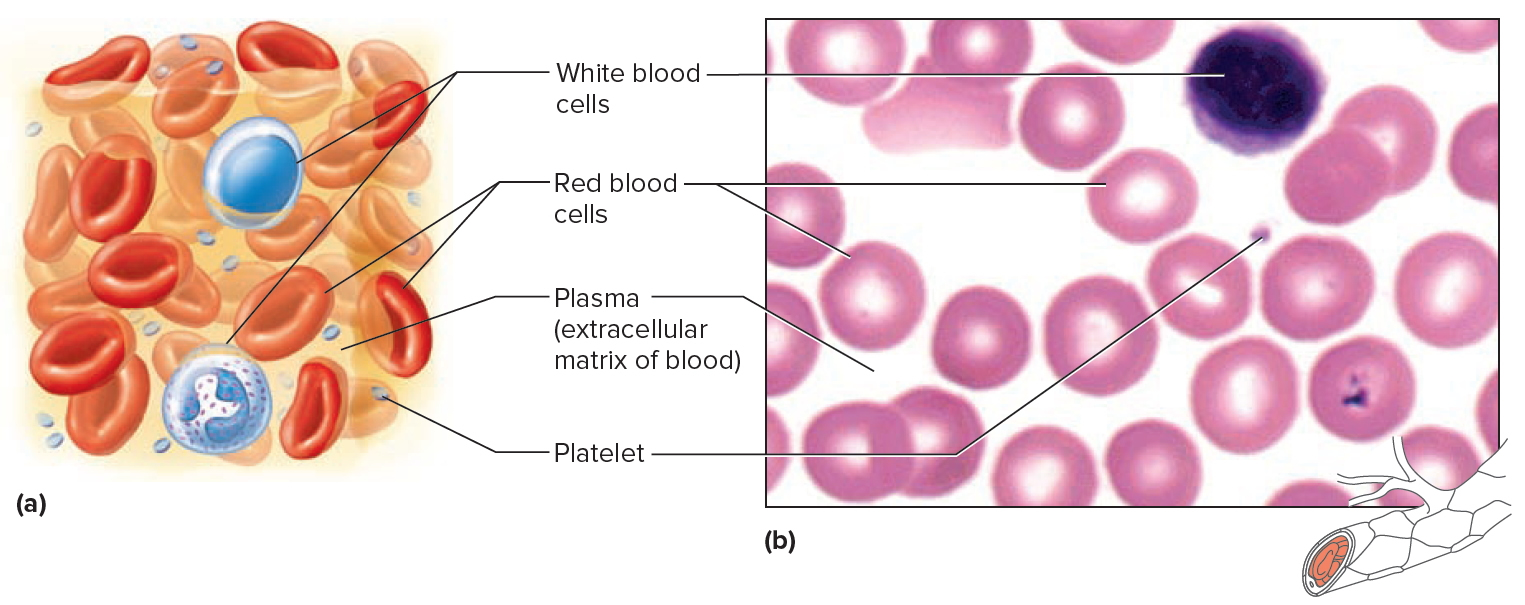
Blood transports a variety of materials between interior body cells and those that exchange substances with the external environment. In this way, blood helps maintain stable internal environmental conditions. Blood is composed of formed elements suspended in a fluid extracellular matrix called blood plasma. The “formed elements” include red blood cells, white blood cells, and cell fragments called platelets. Most blood cells form in red marrow within the hollow parts of certain long bones.
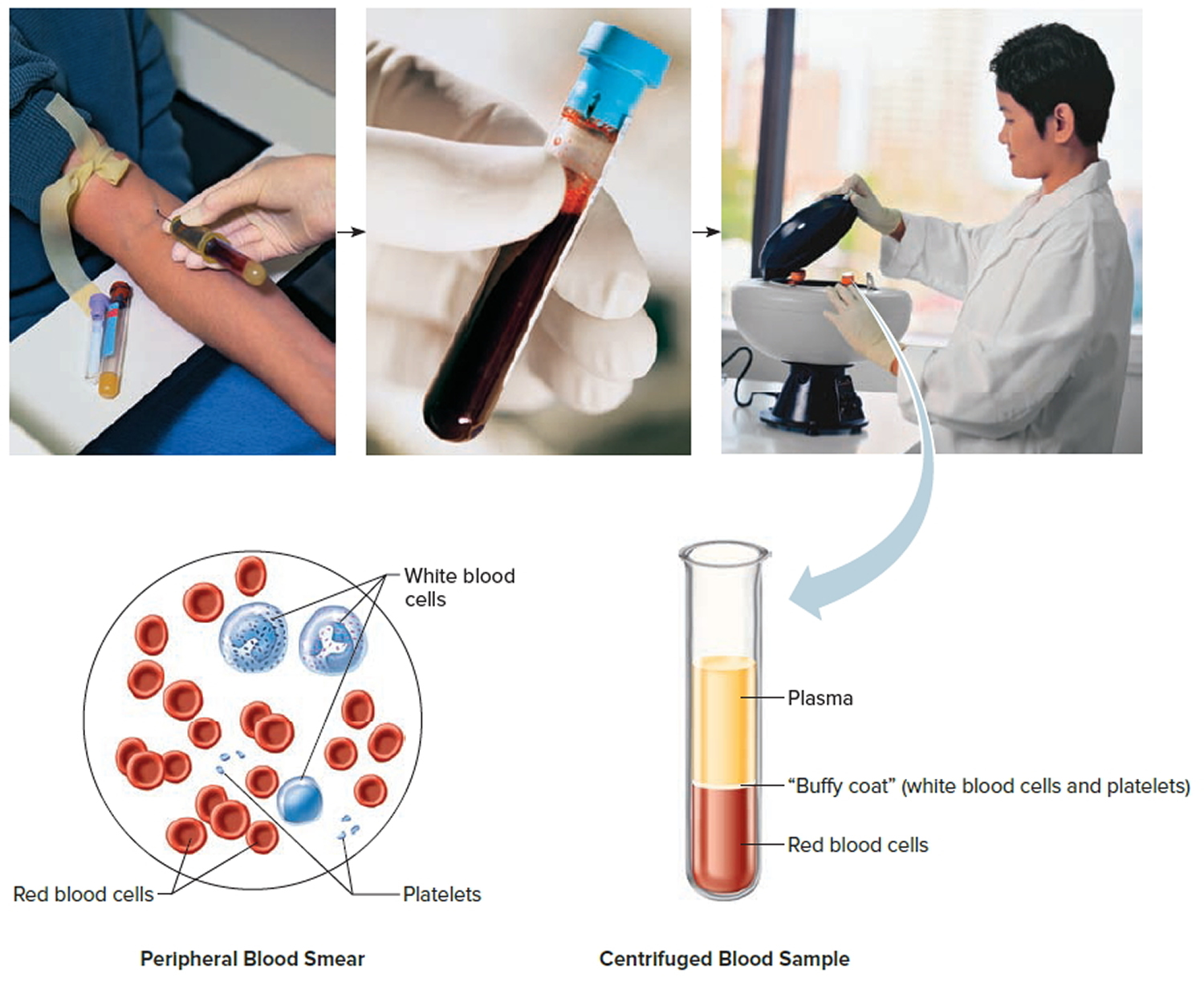
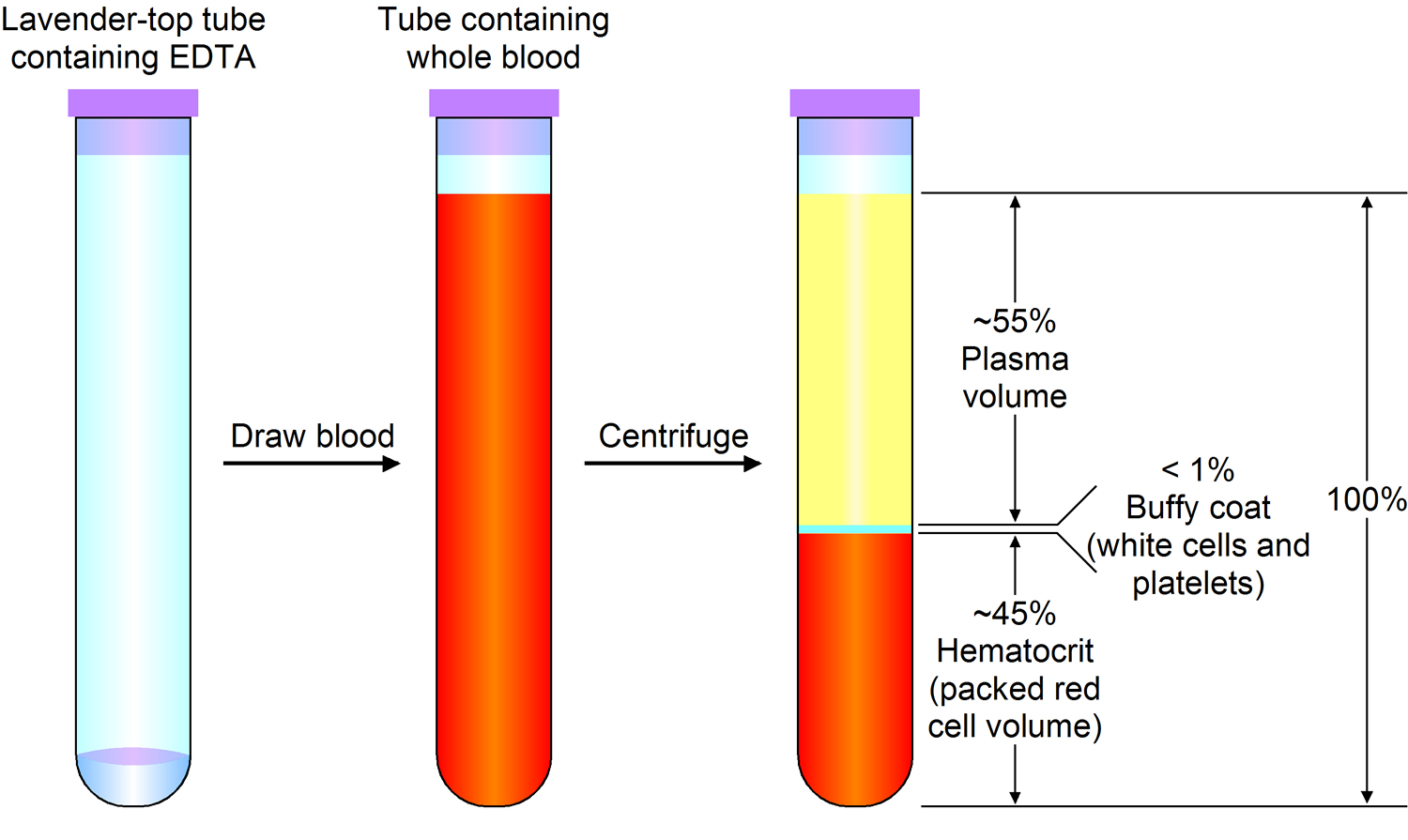
Most blood samples are roughly 37% to 49% red blood cells by volume – adult females is 38–46% (average = 42%) and for adult males, it is 40–54% (average = 47). This percentage is called the hematocrit. The white blood cells and platelets account for less than 1% of blood volume. The remaining blood sample, about 55%, is the plasma, a clear, straw-colored liquid. Blood plasma is a complex mixture of water, gases, amino acids, proteins, carbohydrates, lipids, vitamins, hormones, electrolytes, and cellular wastes (see Figure 1).
Blood volume varies with body size, percent adipose tissue, and changes in fluid and electrolyte concentrations. An average-size adult has a blood volume of about 5 liters (5.3 quarts), 4–5 liters in a female and 5–6 liters in a male.
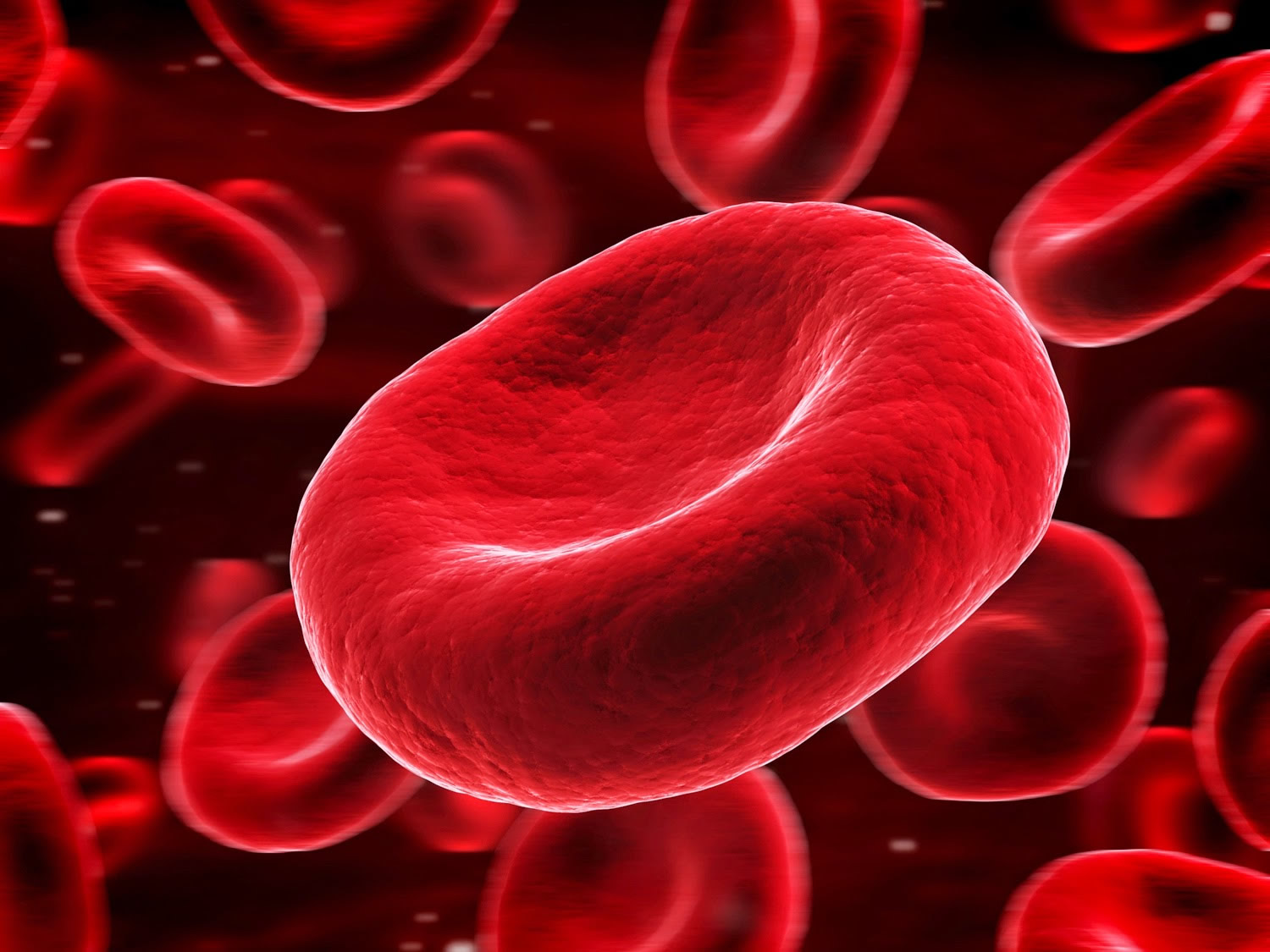
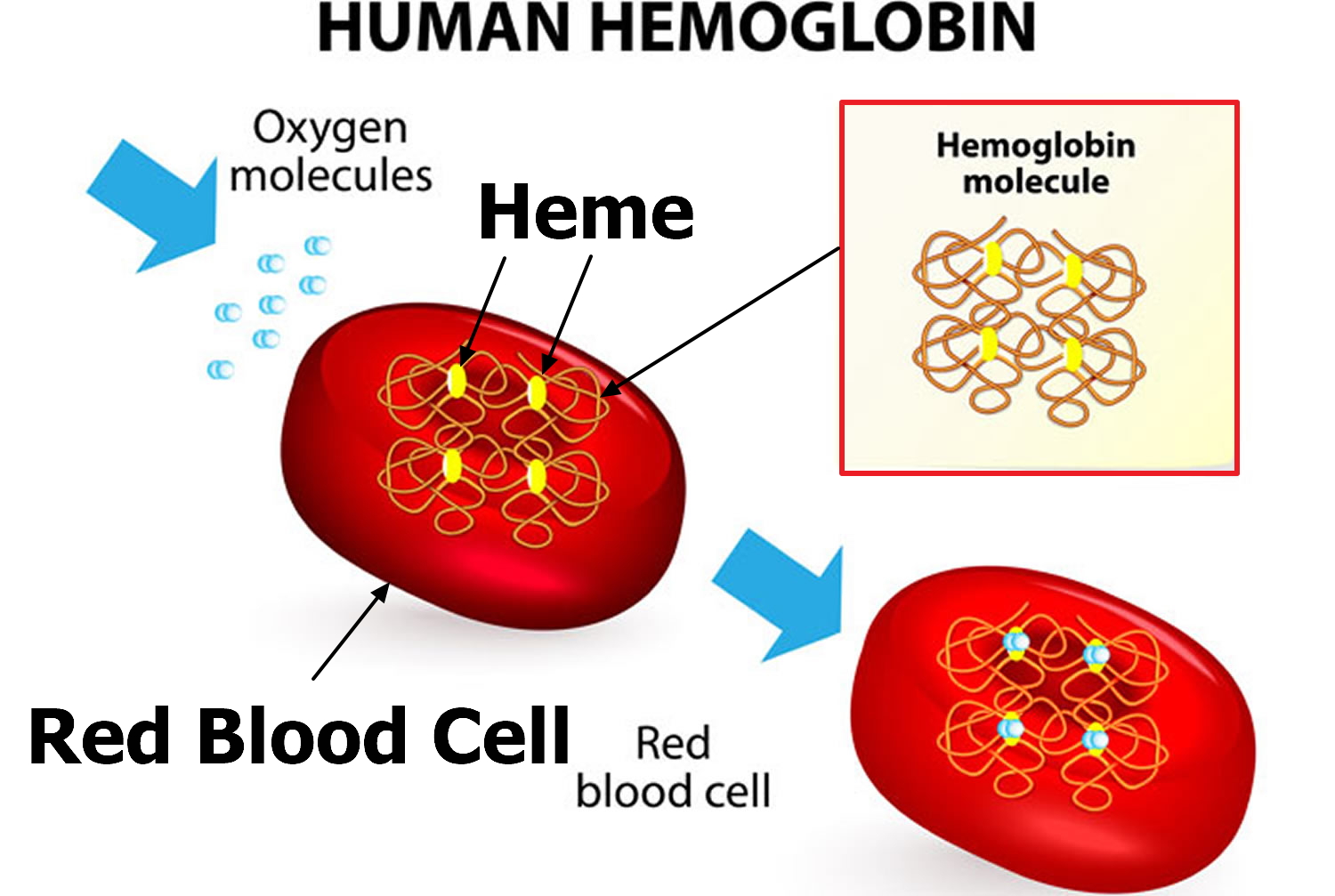
Red blood cell (also called erythrocyte) is biconcave disc without a nucleus. This biconcave shape is an adaptation for transporting the gases oxygen and carbon dioxide. It increases the surface area through which oxygen and carbon dioxide can diffuse into and out of the cell. The characteristic shape of a red blood cell also places the cell membrane closer to oxygen-carrying hemoglobin molecules in the cell reducing the distance for diffusion.
Each red blood cell is about one-third hemoglobin by volume. This protein imparts the color of blood. When hemoglobin binds oxygen, the resulting oxyhemoglobin is bright red, and when oxygen is released, the resulting deoxyhemoglobin is darker.
Prolonged oxygen deficiency (hypoxia) causes cyanosis, in which the skin and mucous membranes appear bluish due to an abnormally high blood concentration of deoxyhemoglobin in the superficial blood vessels. Exposure to low temperature may also result in cyanosis by constricting superficial blood vessels. This response to environmental change slows skin blood flow. As a result, more oxygen than usual is removed from the blood flowing through the vessels, increasing the concentration of deoxyhemoglobin.
Note: Blood is a complex mixture of formed elements in a liquid extracellular matrix, called blood plasma. Note that water and proteins account for 99% of the blood plasma.
Figure 1. Blood composition
Note: Blood consists of a liquid portion called plasma and a solid portion (the formed elements) that includes red blood cells, white blood cells, and platelets. When blood components are separated by centrifugation, the white blood cells and platelets form a thin layer, called the “buffy coat,” between the plasma and the red blood cells, which accounts for about 1% of the total blood volume. Blood cells and platelets can be seen under a light microscope when a blood sample is smeared onto a glass slide.
Blood Cell Formation
The process of blood cell formation, called hematopoiesis, begins in the yolk sac, which lies outside the human embryo. Later in the fetal development, red blood cells are manufactured (erythropoiesis) in the liver and spleen, and still later they form in bone marrow. After birth, these cells are produced in the red bone marrow.
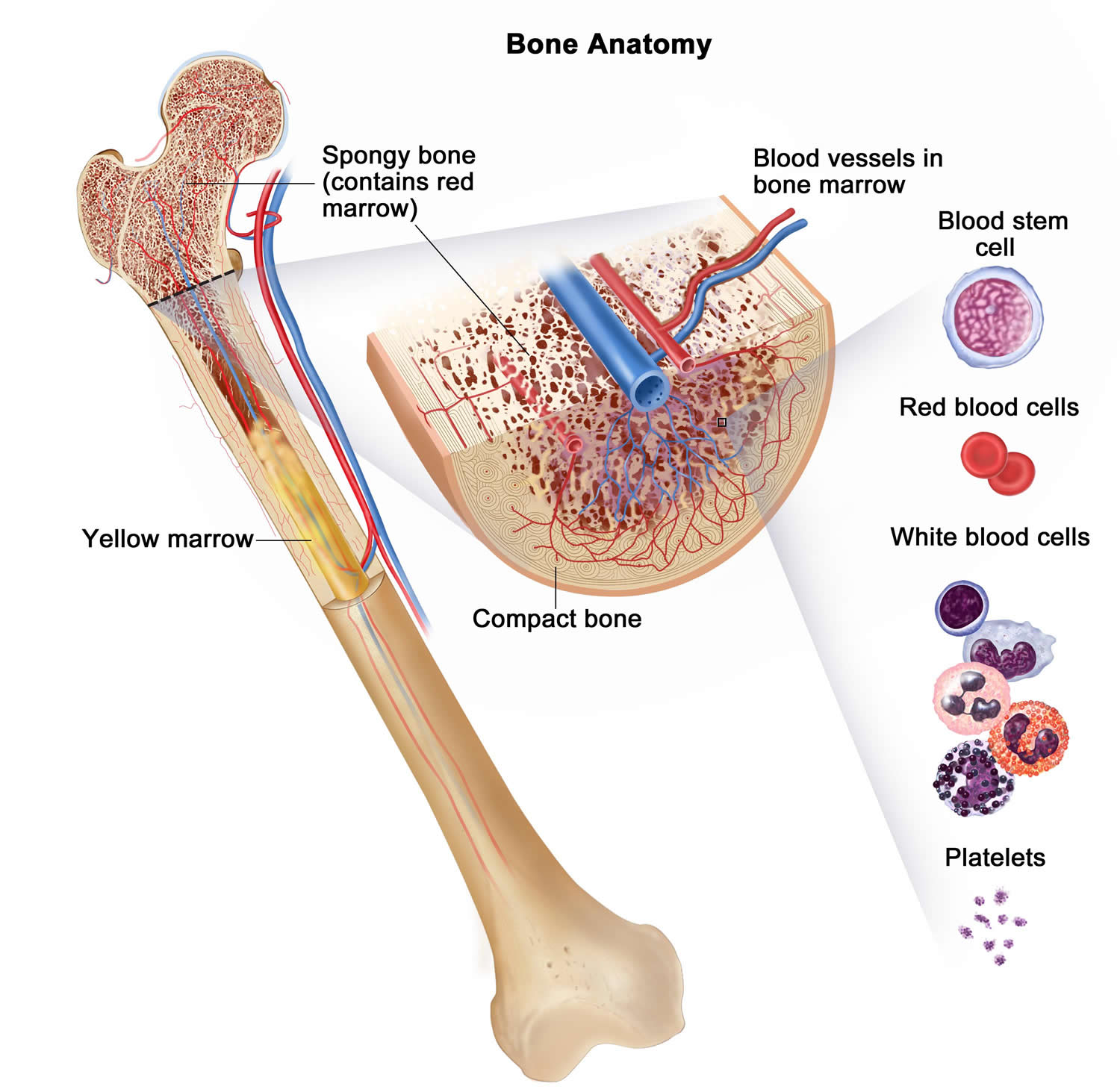
Bone marrow is a soft, netlike mass of connective tissue within the medullary cavities of long bones, in the irregular spaces of spongy bone, and in the larger central canals of compact bone tissue. It is of two kinds: red and yellow. Red bone marrow functions in the formation of red blood cells (erythrocytes), white blood cells (leukocytes), and blood platelets. The color comes from the oxygen-carrying pigment hemoglobin in the red blood cells.
In an infant, red marrow occupies the cavities of most bones. As a person ages, yellow bone marrow, which stores fat, replaces much of the red marrow. Yellow marrow is not active in blood cell production. In an adult, red marrow is primarily found in the spongy bone of the skull, ribs, breastbone (sternum), collarbones (clavicles), backbones (vertebrae), and hip bones. If the supply of blood cells is deficient, some yellow marrow may become red marrow, which then reverts to yellow marrow when the deficiency is corrected.
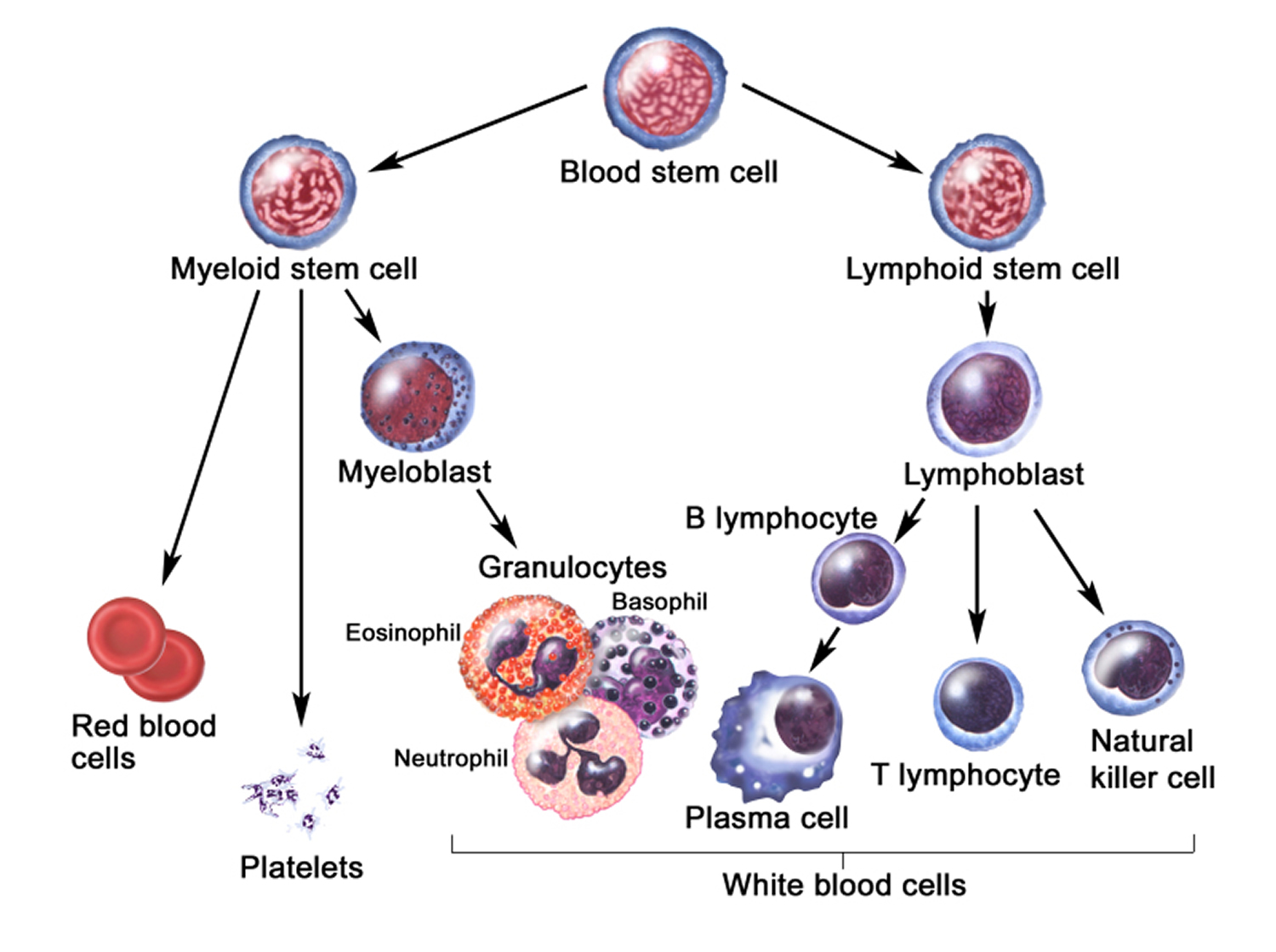
Figure 3 illustrates the stages in the formation of red blood cells from hematopoietic stem cells (blood-forming cells), which are also called hemocytoblasts.
Red blood cells have nuclei during their early stages of development but lose their nuclei as the cells mature. Losing the nuclei provides more space for hemoglobin. Because mature red blood cells do not have nuclei, they cannot divide. They use none of the oxygen they carry because they do not have mitochondria. Mature red blood cells produce ATP through glycolysis only.
The average life span of a red blood cell is 120 days. Many of these cells are removed from the circulation each day, and yet the number of cells in the circulating blood remains relatively stable. This observation suggests a homeostatic control of the rate of red blood cell production.
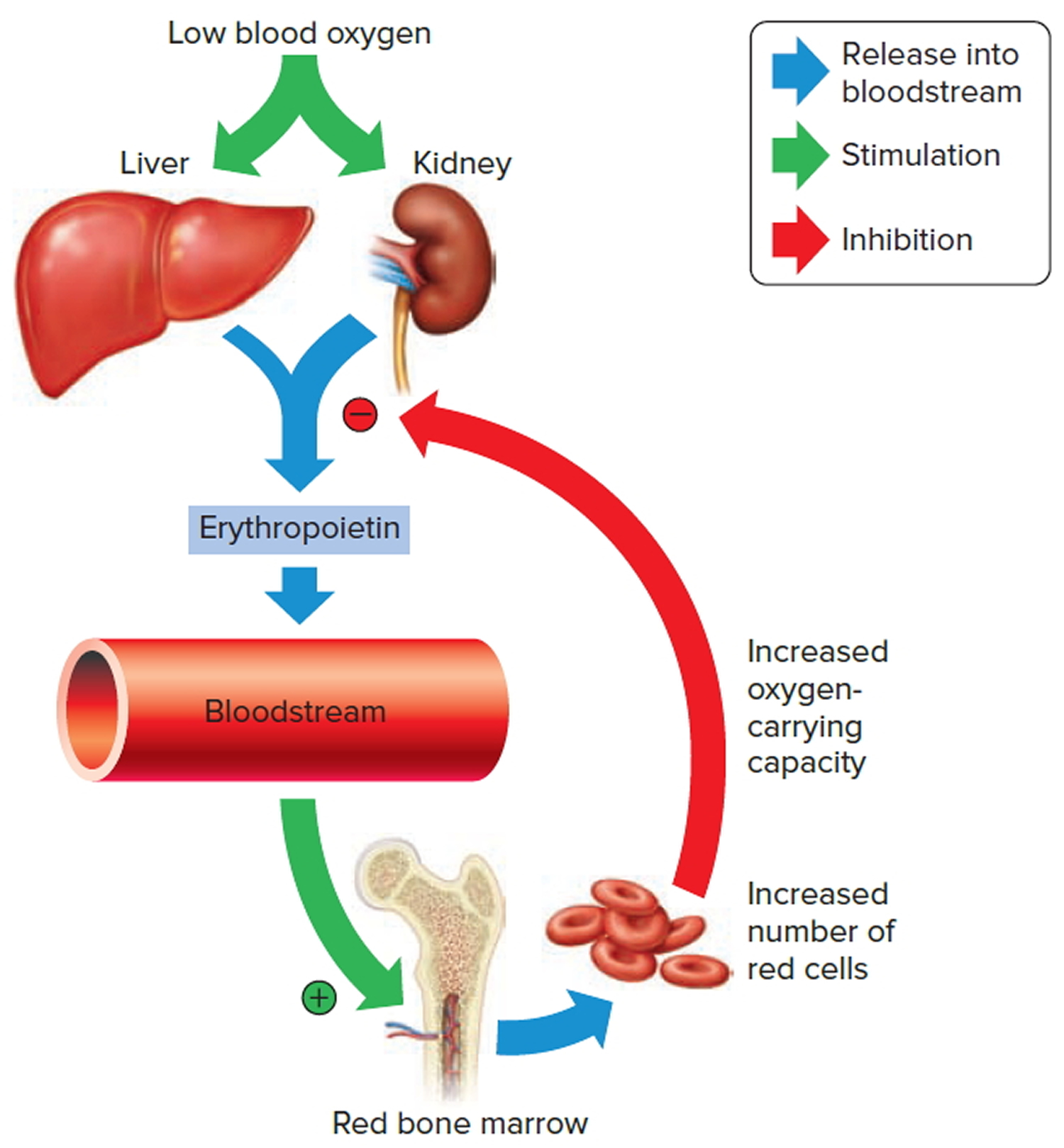
The hormone erythropoietin (EPO) controls the rate of red blood cell formation through negative feedback. The kidneys, and to a lesser extent the liver, release erythropoietin in response to prolonged oxygen deficiency (Figure 6). At high altitudes, for example, where the amount of oxygen in the air is reduced, the blood oxygen level initially decreases. This drop in the blood oxygen level triggers the release of erythropoietin, which travels via the blood to the red bone marrow and stimulates red blood cell production.
After a few days of exposure to high altitudes, many newly formed red blood cells appear in the circulating blood. The increased rate of production continues until the number of erythrocytes in the circulation is sufficient to supply tissues with oxygen. When the availability of oxygen returns to normal, erythropoietin release decreases, and the rate of red blood cell production returns to normal as well. An excessive increase in red blood cells is called polycythemia. This condition increases blood viscosity, slowing blood flow and impairing circulation.
Figure 2. Bone marrow anatomy
Anatomy of the bone. The bone is made up of compact bone, spongy bone, and bone marrow. Compact bone makes up the outer layer of the bone. Spongy bone is found mostly at the ends of bones and contains red marrow. Bone marrow is found in the center of most bones and has many blood vessels. There are two types of bone marrow: red and yellow. Red marrow contains blood stem cells that can become red blood cells, white blood cells, or platelets. Yellow marrow is made mostly of fat.
Dietary Factors Affecting Red Blood Cell Production
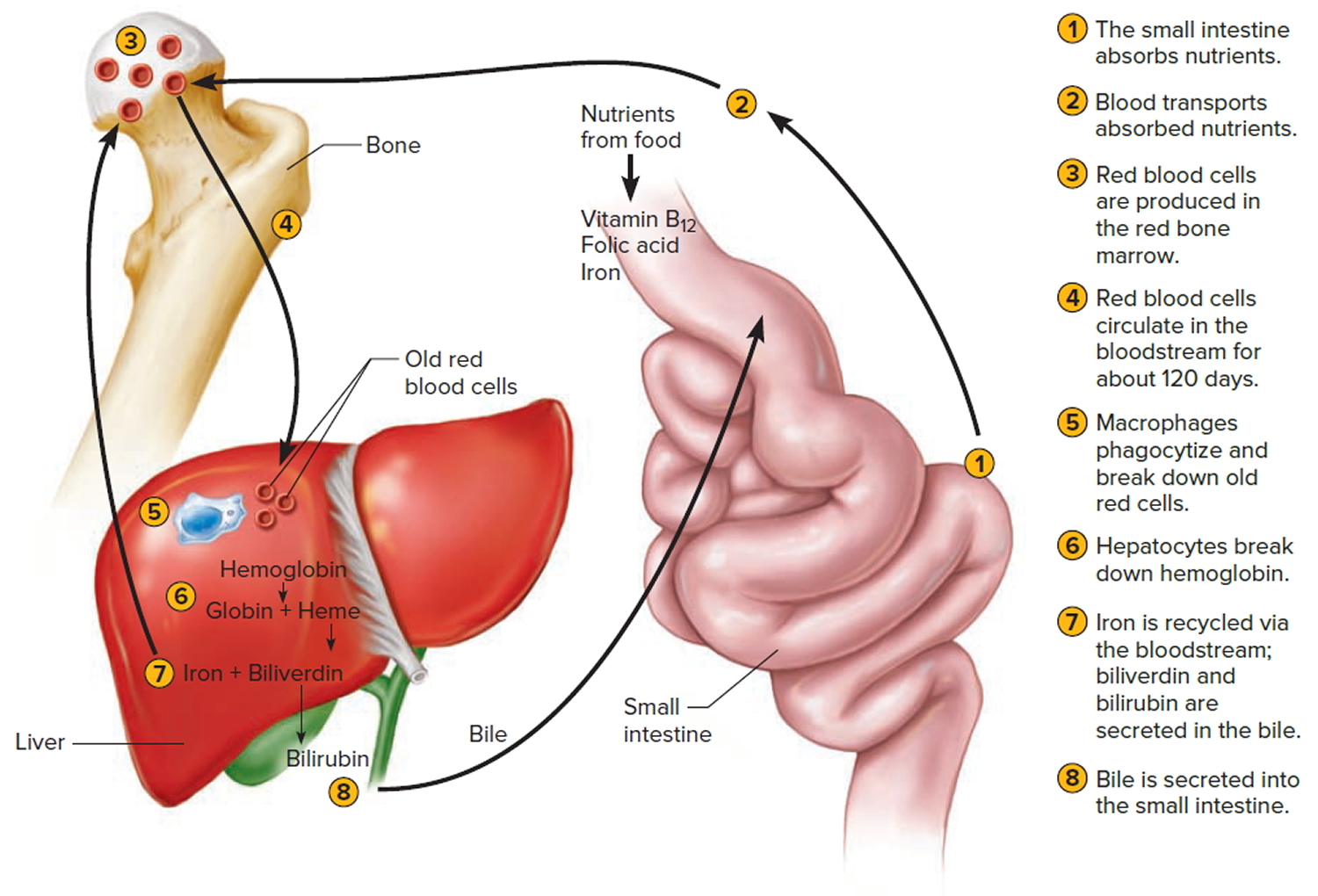
Availability of B-complex vitamins—vitamin B12 and folic acid—significantly influences red blood cell production. Because these vitamins are required for DNA synthesis, they are necessary for the growth and division of cells. Cell division is frequent in blood-forming (hematopoietic) tissue, so this tissue is especially vulnerable to a deficiency of either of these vitamins.
Hemoglobin synthesis and normal red blood cell production also require iron. The small intestine absorbs iron slowly from food. The body reuses much of the iron released by the decomposition of hemoglobin from damaged red blood cells. Nonetheless, insufficient dietary iron can reduce hemoglobin synthesis.
A deficiency of red blood cells or a reduction in the amount of hemoglobin they contain results in a condition called anemia. This reduces the oxygen-carrying capacity of the blood, and the affected person may appear pale and lack energy. A pregnant woman may have a normal number of red blood cells, but she develops a relative anemia because her plasma volume increases due to fluid retention. This shows up as a decreased hematocrit.
In contrast to anemia, the inherited disorder called hemochromatosis results in the absorption of iron in the small intestine at ten times the normal rate. Iron builds up in organs, to toxic levels. Treatment is periodic blood removal, as often as every week.
Figure 3. Blood cell development. A blood stem cell goes through several steps to become a red blood cell, platelet, or white blood cell
Figure 4. Blood cells
Note: Blood tissue consists of red blood cells, white blood cells, and platelets suspended in plasma. (a) Idealized representation of a sample of blood. (b) Micrograph of a sample of blood (1,000x).
Figure 5. Red blood cells
What is the function of red blood cells
Red blood cells function is to transports oxygen and carbon dioxide. to body tissues by blood flow via circulatory system. Red blood cells take oxygen from the lungs and release it into the cells or tissues. Lipids and proteins make up the cell membrane of red blood cells. Hemoglobin, an iron containing biomolecule, is the rich component of the cytoplasm of red blood cells mainly responsible for the oxygen binding and red color of the erythrocytes (see Figure 6).
Figure 6. Red blood cell formation
Note: Low blood oxygen causes the kidneys and to a lesser degree, the liver to release erythropoietin. Erythropoietin stimulates target cells in the red bone marrow to increase the production of red blood cells, which carry oxygen to tissues.
Destruction of Red Blood Cells
The average life span of red blood cells is about four months (120 days) after which it breaks down. Red blood cells are elastic and flexible, and they readily bend as they pass through small blood vessels. As the cells near the end of their four-month life span, however, they become more fragile. The cells may sustain damage simply passing through capillaries, particularly those in active muscles that must withstand strong forces. Macrophages phagocytize and destroy damaged red blood cells, primarily in the liver and spleen. Macrophages are large, phagocytic, wandering cells. During phagocytosis, the iron from the hemoglobin is retained in the liver and spleen cells and is again used in the formation of red blood cells in the body. About 2-10 million red blood cells are formed and destroyed each second in a normal person.
Hemoglobin molecules liberated from red blood cells break down into their four component polypeptide “globin” chains, each surrounding a heme group. The heme further decomposes into iron and a greenish pigment called biliverdin. The blood may transport the iron, combined with a protein, to the hematopoietic tissue in red bone marrow to be reused in synthesizing new hemoglobin. About 80% of the iron is stored in the liver in the form of an iron-protein complex. Biliverdin eventually is converted to an orange-yellow pigment called bilirubin. Biliverdin and bilirubin are secreted in the bile as bile pigments. Figure 7 summarizes the life cycle of a red blood cell.
In jaundice (yellow discoloration of the skin and the whites of the eyes), accumulation of bilirubin turns the skin and eyes yellowish. Newborns can develop physiologic jaundice a few days after birth. This condition may be the result of immature liver cells that ineffectively secrete bilirubin into the bile. Treatment includes exposure to fluorescent light, which breaks down bilirubin in the tissues, and feedings that promote bowel movements. In hospital nurseries, babies being treated for physiological jaundice lie under “bili lights,” clad only in diapers and protective goggles.
Figure 7. Red blood cell hemoglobin
Figure 8. Lifecycle of a red blood cell
High red blood cell count
Polycythemia, or erythrocytosis, means having a high concentration of red blood cells in your blood. This makes the blood thicker and less able to travel through blood vessels and organs. Many of the symptoms of polycythaemia are caused by this sluggish flow of blood.
The definition of a high red blood cell count varies from one medical practice to another. A normal range in adults is generally considered to be 700,000 to 5.2 million red blood cells per microliter (mcL) of blood for men and 500,000 to 4.6 million red blood cells per mcL of blood for women. In children, the threshold for high red blood cell count varies with age and sex.
A high red blood cell count is usually found when your doctor has ordered tests to help diagnose a condition you have. Talk to your doctor about what your test results mean. A high red blood cell count and results from other tests may indicate the cause of your illness. Or your doctor may suggest additional tests to monitor your condition.
High red blood cell count causes
High red blood cell count (polycythemia) can be divided into several different types, depending on the underlying cause of the condition. In some cases, an underlying cause can’t be identified.
Apparent polycythemia
“Apparent polycythemia” is where your red cell count is normal, but you have a reduced amount of a fluid called plasma in your blood, making it thicker.
The condition is often caused by being overweight, smoking, drinking excessive amounts of alcohol or taking certain medications – such as diuretics. A similar condition that’s sometimes called “relative polycythemia” can also occur as a result of dehydration.
Apparent polycythemia may improve if the underlying cause is identified and managed. Stopping smoking or reducing your alcohol intake, for example, may help.
Absolute polycythemia
“Absolute polycythemia” is where your body produces too many red blood cells. There are two main types:
- Primary polycythemia – there’s a problem in the cells produced by the bone marrow that become red blood cells; the most common type is known as polycythemia vera (PV)
- Secondary polycythemia – too many red blood cells are produced as the result of an underlying condition
Both polycythemia vera and secondary polycythemia are described in more detail below.
Polycythemia vera (PV)
Polycythemia vera is a rare condition usually caused by a fault in the JAK2 gene, which causes the bone marrow cells to produce too many red blood cells.
The affected bone marrow cells can also develop into other cells found in the blood, which means that people with polycythemia vera may also have abnormally high numbers of both platelets (thrombocytosis) and white bloods cells (leukocytosis).
Although caused by a genetic fault, polycythemia vera isn’t usually inherited. Most cases develop later in life, with 60 the average age of diagnosis.
Secondary polycythemia
Secondary polycythemia is where an underlying condition causes more erythropoietin to be produced. This is a hormone produced by the kidneys that stimulates the bone marrow cells to produce red blood cells.
Conditions that can cause secondary polycythaemia include:
- chronic obstructive pulmonary disease (COPD) and sleep apnea – these can cause an increase in erythropoietin, due to not enough oxygen reaching the body’s tissues
- a problem with the kidneys – such as a kidney tumor or narrowing of the arteries supplying blood to the kidneys
High red blood cell count may also be caused by low oxygen levels, kidney disease or other problems.
Low oxygen levels
Your body may increase red blood cell production to compensate for any condition that results in low oxygen levels, including:
- Heart disease (such as congenital heart disease in adults)
- Heart failure
- A condition present at birth that reduces the oxygen-carrying capacity of red blood cells (hemoglobinopathy)
- High altitudes
- COPD (chronic obstructive pulmonary disease)
- Pulmonary fibrosis (scarred and damaged lungs)
- Other lung diseases
- Sleep apnea
- Nicotine dependence (smoking)
Performance-enhancing drugs
Certain drugs stimulate the production of red blood cells, including:
- Anabolic steroids
- Blood doping (transfusion)
- Injections of a protein (erythropoietin) that enhances red blood cell production
Increased red blood cell concentration
Dehydration (If the liquid component of the blood (plasma) is decreased, as in dehydration, the red blood cell count increases. This is due to the red blood cells becoming more concentrated. The actual number of red blood cells stays the same.)
Kidney disease
Rarely, in some kidney cancers and sometimes after kidney transplants, the kidneys might produce too much erythropoietin. This enhances red blood cell production.
Bone marrow overproduction
- Polycythemia vera
- Other myeloproliferative disorders
High red blood cell count symptoms
Mild cases of high red blood cell count (polycythemia) may not cause any problems, but some people with high red blood cell count can experience:
- headaches
- blurred vision
- red skin – particularly in the face, hands and feet
- tiredness
- high blood pressure
- dizziness
- discomfort in the tummy (abdomen)
- periods of confusion
- bleeding problems – such as nosebleeds and bruising
- gout – which can cause joint pain, stiffness and swelling
- itchy skin – especially after a bath or shower; this is the result of white blood cells (levels of which can also be high) releasing the chemical histamine
You should make an appointment to see your doctor if you have persistent symptoms of high red blood cell count.
The slow blood flow associated with high red blood cell count (polycythemia) can also cause blood clots. These can be serious because they may put you at risk of life-threatening problems such as:
- heart attacks
- pulmonary embolisms – a blockage in the blood vessel that carries blood from the heart to the lungs
- strokes
In some cases, a blood clot – known as deep vein thrombosis (DVT) – may form in your leg, before moving elsewhere in your body. Signs of DVT or a pulmonary embolism can include:
- pain, swelling, redness and tenderness in one of your legs
- a heavy ache in the affected area
- warm skin in the area of the clot
- breathlessness
- chest or upper back pain
- coughing up blood
- feeling lightheaded or dizzy
- fainting
If you experience any of the above symptoms, seek medical help immediately. You should also seek emergency medical help if you think that you or someone you’re with is having a heart attack or stroke.
Possible complications of polycythemia vera
Complications of polycythemia vera may include:
- Acute myelogenous leukemia (AML)
- Bleeding from the stomach or other parts of the intestinal tract
- Gout (painful swelling of a joint)
- Heart failure
- Myelofibrosis (disorder of the bone marrow in which the marrow is replaced by fibrous scar tissue)
- Thrombosis (blood clotting, which can cause a stroke, heart attack, or other body damage)
High red blood cell count diagnosis
High red blood cell count (polycythemia) can be diagnosed by carrying out a blood test to check:
- the number of red blood cells in your blood (red blood cell count)
- the amount of space the red blood cells take up in the blood (hematocrit level)
A high concentration of red blood cells suggests you have polycythemia.
Your doctor may have ordered a blood test because you reported some of the above symptoms or complications, but high red blood cell count is sometimes only discovered during a routine blood test for another reason.
Your doctor may refer you to a hematologist (a specialist in conditions affecting the blood) for more tests, to confirm the diagnosis and to determine the underlying cause.
These may include a blood test to look for the faulty JAK2 gene and an ultrasound scan of your abdomen to look for problems in your kidneys.
High red blood cell count treatment
Treatment for high red blood cell count aims to prevent symptoms and complications (such as blood clots), and treat any underlying causes.
Venesection (phlebotomy)
Phlebotomy is the simplest and quickest way of reducing the number of red cells in your blood. It may be recommended if you have polycythemia vera, a history of blood clots, or symptoms suggesting your blood is too thick.
Venesection involves removing about one pint (half a liter) of blood at a time, in a similar way to the procedure used for blood donation. Initially one unit of blood (about 1 pint, or 1/2 liter) is removed each week until the number of red blood cells drops. The treatment is continued as needed.
How often this is needed will be different for each person. At first, you may need the treatment every week, but once your condition is under control you may only need it every 6-12 weeks or less.
Medication to reduce the production of red blood cells
In cases of polycythemia vera, medication may be prescribed to slow down the production of red blood cells.
Many different medications are available and your specialist will take into account your age and health, response to phlebotomy and red blood cell count when choosing the most appropriate one for you. Examples include:
- Hydroxycarbamide – generally tolerated well, but shouldn’t be taken by pregnant women or women trying to conceive
- Hydroxyurea to reduce the number of red blood cells made by the bone marrow. This drug may be used when the numbers of other blood cell types are also high.
- Interferon – can be taken in pregnancy, but may cause unpleasant side effects, such as hair loss and flu-like symptoms
- Anagrelide to lower platelet counts.
- Ruxolitinib (Jakafi) to reduce the number of red blood cells and reduce an enlarged spleen. This drug is prescribed when hydroxyurea and other treatments have failed.
Taking aspirin to reduce the risk of blood clots may be an option for some people. But, aspirin increases the risk of stomach bleeding.
Ultraviolet-B light therapy can reduce the severe itching some people experience.
Medication to prevent blood clots
If you have polycythemia vera, daily low-dose aspirin tablets may be prescribed to help prevent blood clots and reduce the risk of serious complications.
You may also be offered treatment with low-dose aspirin if you have apparent or secondary polycythemia and another condition affecting your blood vessels, such as coronary heart disease or cerebrovascular disease.
Treating and preventing other conditions
Some people may also need treatment for any other symptoms or complications of high red blood cell count they have, or for any underlying cause of the condition.
For example, you may be given medication to help relieve itching, manage COPD or treat gout.
Lifestyle changes
As well as improving some cases of apparent polycythemia, making healthy lifestyle changes can also reduce your risk of potentially serious blood clots for people with all types of polycythemia.
Having high red blood cell count means you’re already at high risk of a blood clot, and being overweight or smoking only increases this risk.
You may find the following advice and information helpful:
- losing weight
- preventing cardiovascular disease
- managing high blood pressure
- stopping smoking
High red blood cell count prognosis
The outlook for high red blood cell count largely depends on the underlying cause.
Many cases are mild and may not lead to any further complications. However, some cases – particularly cases of polycythemia vera – can be more serious and require long-term treatment.
If well controlled, high red blood cell count shouldn’t affect your life expectancy, and you should be able to live a normal life. However, people with polycythemia vera can have a slightly lower life expectancy than normal due to the increased risk of problems, such as heart attacks and strokes.
Polycythemia vera can also sometimes cause scarring of the bone marrow (myelofibrosis), which can eventually lead to you having too few blood cells. In some rare cases, the condition can develop into a type of cancer called acute myeloid leukemia (AML).
If you have high red blood cell count, it’s important to take any medication you’re prescribed and keep an eye out for signs of possible blood clots to help reduce your risk of serious complications.
Low red blood cell count
Anemia is a condition in which your blood has a lower than normal number of red blood cells 1. Anemia also can occur if your red blood cells don’t contain enough hemoglobin. Hemoglobin is an iron-rich protein that gives blood its red color. This protein helps red blood cells carry oxygen from the lungs to the rest of the body. Anemia is the most common blood disorder in the United States. It affects your red blood cells and hemoglobin. This is the protein in red blood cells that carries oxygen from your lungs to the rest of your body. You need iron in order to make hemoglobin. Most people who have anemia have a shortage of iron. This condition is called iron deficiency anemia.
There are a few other types of anemia, including:
- Aplastic anemia. This occurs when your bone marrow has damaged stem cells. Your body fails to produce enough new blood cells. The condition affects your red blood cells, white blood cells, and platelets. Sometimes it is called bone marrow failure.
- Hemolytic anemia. This occurs when your body destroys red blood cells before they should. The normal lifespan of red blood cells is 120 days.
- Normocytic anemia. This occurs when your red blood cells are normal in size, but low in count.
- Pernicious anemia. This occurs when your body lacks vitamin B12. It causes a shortage of healthy red blood cells.
- Sickle cell anemia (a form of sickle cell disease). This is a genetic disease that affects your red blood cells. It occurs when you are born with 2 abnormal hemoglobin genes.
Low red blood cell count causes
Anemia has three main causes 1:
- Blood loss,
- Lack of red blood cell production, or
- High rates of red blood cell destruction.
These causes might be the result of diseases, conditions, or other factors.
If you have anemia, your body doesn’t get enough oxygen-rich blood. As a result, you may appear pale, feel tired or weak. You also may have other symptoms, such as shortness of breath, dizziness, or headaches.
Severe or long-lasting anemia can damage your heart, brain, and other organs in your body. Very severe anemia may even cause death 1.
Many types of anemia can be mild, short term, and easily treated. You can even prevent some types with a healthy diet. Other types can be treated with dietary supplements.
However, certain types of anemia can be severe, long lasting, and even life threatening if not diagnosed and treated.
If you have signs or symptoms of anemia, see your doctor to find out whether you have the condition. Treatment will depend on the cause of the anemia and how severe it is.
There are many types of anemia with specific causes and traits.
Some of these include:
- Aplastic anemia
- Blood loss anemia
- Cooley’s anemia
- Diamond-Blackfan anemia
- Fanconi anemia
- Folate- or folic acid-deficiency anemia
- Hemolytic anemia
- Iron-deficiency anemia
- Pernicious anemia
- Sickle cell anemia
- Thalassemias; Cooley’s anemia is another name for beta thalassemia major
Blood loss that creates a shortage of red blood cells
Blood loss is the most common cause of anemia, especially iron-deficiency anemia. Blood loss can be short term or persist over time.
Heavy menstrual periods or bleeding in the digestive or urinary tract can cause blood loss. Surgery, trauma, or cancer also can cause blood loss.
If a lot of blood is lost, the body may lose enough red blood cells to cause anemia.
Heavy periods may cause low iron levels in women. Internal bleeding, such as in your digestive or urinary tract, can cause blood loss. This can be caused by conditions such as a stomach ulcer or ulcerative colitis. Other reasons for blood loss include:
- cancer
- surgery
- trauma
- taking aspirin or a similar medicine for a long time.
Lack of Red Blood Cell Production
Both acquired and inherited conditions and factors can prevent your body from making enough red blood cells. “Acquired” means you aren’t born with the condition, but you develop it. “Inherited” means your parents passed the gene for the condition on to you.
Acquired conditions and factors that can lead to anemia include poor diet, abnormal hormone levels, some chronic (ongoing) diseases, and pregnancy.
Aplastic anemia also can prevent your body from making enough red blood cells. This condition can be acquired or inherited.
Diet
Your body may not produce enough red blood cells if you lack certain nutrients. Low iron is a common problem. People who don’t eat meat or follow “fad” diets are more at risk of low iron. Infants and toddlers are at risk of getting anemia from a low-iron diet. Low vitamin B12 and folic acid can cause anemia as well.
Unable to absorb
Certain diseases affect your small intestine’s ability to absorb nutrients. For example, Crohn’s disease and celiac disease can cause low iron levels in your body. Some foods, like milk, can prevent your body from absorbing iron. Taking vitamin C can help this. Medicines, such as antacids or prescriptions to reduce acid in your stomach, can affect it as well.
Pregnancy
Women who are pregnant or breastfeeding can get anemia. When you’re pregnant, you need more blood (up to 30%) to share with the baby. If your body lacks iron or vitamin B12, your body can’t produce enough red blood cells.
The following factors may increase your risk of anemia during pregnancy.
- Vomiting a lot from morning sickness.
- Having a diet low in nutrients.
- Having heavy periods before pregnancy.
- Having 2 pregnancies close together.
- Being pregnant with multiple babies at once.
- Becoming pregnant as a teenager.
- Losing a lot of blood from an injury or surgery.
Growth spurts
Children younger than 3 years of age are prone to anemia. Their bodies grow so fast that they can have a hard time getting or keeping enough iron.
Normocytic anemia
Normocytic anemia can be congenital (from birth) or acquired (from a disease or infection). The most common cause of the acquired form is a chronic (long-term) disease. Examples include kidney disease, cancer, rheumatoid arthritis, and thyroiditis. Some medicines can cause normocytic anemia, but this is rare.
Hormones
Your body needs the hormone erythropoietin to make red blood cells. This hormone stimulates the bone marrow to make these cells. A low level of this hormone can lead to anemia.
Diseases and Disease Treatments
Chronic diseases, like kidney disease and cancer, can make it hard for your body to make enough red blood cells.
Some cancer treatments may damage the bone marrow or damage the red blood cells’ ability to carry oxygen. If the bone marrow is damaged, it can’t make red blood cells fast enough to replace the ones that die or are destroyed.
People who have HIV/AIDS may develop anemia due to infections or medicines used to treat their diseases.
Aplastic Anemia
Some infants are born without the ability to make enough red blood cells. This condition is called aplastic anemia. Infants and children who have aplastic anemia often need blood transfusions to increase the number of red blood cells in their blood.
Acquired conditions or factors, such as certain medicines, toxins, and infectious diseases, also can cause aplastic anemia.
High Rates of Red Blood Cell Destruction
Both acquired and inherited conditions and factors can cause your body to destroy too many red blood cells. One example of an acquired condition is an enlarged or diseased spleen.
The spleen is an organ that removes wornout red blood cells from the body. If the spleen is enlarged or diseased, it may remove more red blood cells than normal, causing anemia.
Examples of inherited conditions that can cause your body to destroy too many red blood cells include sickle cell anemia, thalassemias, and lack of certain enzymes. These conditions create defects in the red blood cells that cause them to die faster than healthy red blood cells.
Hemolytic anemia is another example of a condition in which your body destroys too many red blood cells. Inherited or acquired conditions or factors can cause hemolytic anemia. Examples include immune disorders, infections, certain medicines, or reactions to blood transfusions.
Treatments, such as chemotherapy, can damage your red blood cells and/or bone marrow. Infection caused by a weakened immune system can lead to anemia. Having an enlarged or diseased spleen can cause anemia, too.
Who is at risk for low red blood cell count?
Anemia is a common condition. It occurs in all age, racial, and ethnic groups. Both men and women can have anemia. However, women of childbearing age are at higher risk for the condition because of blood loss from menstruation.
Anemia can develop during pregnancy due to low levels of iron and folic acid (folate) and changes in the blood. During the first 6 months of pregnancy, the fluid portion of a woman’s blood (the plasma) increases faster than the number of red blood cells. This dilutes the blood and can lead to anemia.
During the first year of life, some babies are at risk for anemia because of iron deficiency. At-risk infants include those who are born too early and infants who are fed breast milk only or formula that isn’t fortified with iron. These infants can develop iron deficiency by 6 months of age.
Infants between 1 and 2 years of age also are at risk for anemia. They may not get enough iron in their diets, especially if they drink a lot of cow’s milk. Cow’s milk is low in the iron needed for growth.
Drinking too much cow’s milk may keep an infant or toddler from eating enough iron-rich foods or absorbing enough iron from foods.
Older adults also are at increased risk for anemia. Researchers continue to study how the condition affects older adults. Many of these people have other medical conditions as well.
Major Risk Factors
Factors that raise your risk for anemia include:
- A diet that is low in iron, vitamins, or minerals
- Blood loss from surgery or an injury
- Long-term or serious illnesses, such as kidney disease, cancer, diabetes, rheumatoid arthritis, HIV/AIDS, inflammatory bowel disease (including Crohn’s disease), liver disease, heart failure, and thyroid disease
- Long-term infections
- A family history of inherited anemia, such as sickle cell anemia or thalassemia
Can low red blood cell count be prevented or avoided?
You cannot avoid anemia caused by a genetic disease. You often cannot avoid it due to blood loss. If your blood loss is from heavy periods, receiving treatment can help prevent anemia. If your body can’t absorb certain nutrients, such as iron or vitamin B12, talk to your doctor about taking a supplement. This can help manage your levels and prevent anemia.
A balanced diet can help prevent some types of anemia.
Low red blood cell count signs and symptoms
The most common symptom of anemia is fatigue (feeling tired or weak). If you have anemia, you may find it hard to find the energy to do normal activities.
Other signs and symptoms of anemia include:
- Shortness of breath
- Dizziness
- Headache
- Coldness in the hands and feet
- Pale skin
- Chest pain
These signs and symptoms can occur because your heart has to work harder to pump oxygen-rich blood through your body.
Mild to moderate anemia may cause very mild symptoms or none at all.
Complications of low red blood cell count
Some people who have anemia may have arrhythmias. Arrhythmias are problems with the rate or rhythm of the heartbeat. Over time, arrhythmias can damage your heart and possibly lead to heart failure.
Anemia also can damage other organs in your body because your blood can’t get enough oxygen to them.
Anemia can weaken people who have cancer or HIV/AIDS. This can make their treatments not work as well.
Anemia also can cause many other health problems. People who have kidney disease and anemia are more likely to have heart problems. With some types of anemia, too little fluid intake or too much loss of fluid in the blood and body can occur. Severe loss of fluid can be life threatening.
Low red blood cell count diagnosis
Your doctor will diagnose anemia based on your medical and family histories, a physical exam, and results from tests and procedures.
Because anemia doesn’t always cause symptoms, your doctor may find out you have it while checking for another condition.
Medical and Family Histories
Your doctor may ask whether you have any of the common signs or symptoms of anemia. He or she also may ask whether you’ve had an illness or condition that could cause anemia.
Let your doctor know about any medicines you take, what you typically eat (your diet), and whether you have family members who have anemia or a history of it.
Physical Exam
Your doctor will do a physical exam to find out how severe your anemia is and to check for possible causes. He or she may:
- Listen to your heart for a rapid or irregular heartbeat
- Listen to your lungs for rapid or uneven breathing
- Feel your abdomen to check the size of your liver and spleen
Your doctor also may do a pelvic or rectal exam to check for common sources of blood loss.
Diagnostic Tests and Procedures
You may have various blood tests and other tests or procedures to find out what type of anemia you have and how severe it is.
Complete Blood Count
Often, the first test used to diagnose anemia is a complete blood count (CBC). The CBC measures many parts of your blood.
The test checks your hemoglobin and hematocrit levels. Hemoglobin is the iron-rich protein in red blood cells that carries oxygen to the body. Hematocrit is a measure of how much space red blood cells take up in your blood. A low level of hemoglobin or hematocrit is a sign of anemia.
The normal range of these levels might be lower in certain racial and ethnic populations. Your doctor can explain your test results to you.
The CBC also checks the number of red blood cells, white blood cells, and platelets in your blood. Abnormal results might be a sign of anemia, another blood disorder, an infection, or another condition.
Finally, the CBC looks at mean corpuscular volume (MCV). MCV is a measure of the average size of your red blood cells and a clue as to the cause of your anemia. In iron-deficiency anemia, for example, red blood cells usually are smaller than normal.
Other Tests and Procedures
If the CBC results show that you have anemia, you may need other tests, such as:
- Hemoglobin electrophoresis. This test looks at the different types of hemoglobin in your blood. The test can help diagnose the type of anemia you have.
- A reticulocyte count. This test measures the number of young red blood cells in your blood. The test shows whether your bone marrow is making red blood cells at the correct rate.
- Tests for the level of iron in your blood and body. These tests include serum iron and serum ferritin tests. Transferrin level and total iron-binding capacity tests also measure iron levels.
Because anemia has many causes, you also might be tested for conditions such as kidney failure, lead poisoning (in children), and vitamin deficiencies (lack of vitamins, such as B12 and folic acid).
If your doctor thinks that you have anemia due to internal bleeding, he or she may suggest several tests to look for the source of the bleeding. A test to check the stool for blood might be done in your doctor’s office or at home. Your doctor can give you a kit to help you get a sample at home. He or she will tell you to bring the sample back to the office or send it to a laboratory.
If blood is found in the stool, you may have other tests to find the source of the bleeding. One such test is endoscopy. For this test, a tube with a tiny camera is used to view the lining of the digestive tract.
Your doctor also may want to do bone marrow tests. These tests show whether your bone marrow is healthy and making enough blood cells.
Low red blood cell count treatment
Treatment for anemia depends on the type, cause, and severity of the condition. Treatments may include dietary changes or supplements, medicines, procedures, or surgery to treat blood loss.
Goals of Treatment
The goal of treatment is to increase the amount of oxygen that your blood can carry. This is done by raising the red blood cell count and/or hemoglobin level. (Hemoglobin is the iron-rich protein in red blood cells that carries oxygen to the body.)
Another goal is to treat the underlying cause of the anemia.
Dietary Changes and Supplements
Low levels of vitamins or iron in the body can cause some types of anemia. These low levels might be the result of a poor diet or certain diseases or conditions.
To raise your vitamin or iron level, your doctor may ask you to change your diet or take vitamin or iron supplements. Common vitamin supplements are vitamin B12 and folic acid (folate). Vitamin C sometimes is given to help the body absorb iron.
Iron
Your body needs iron to make hemoglobin. Your body can more easily absorb iron from meats than from vegetables or other foods. To treat your anemia, your doctor may suggest eating more meat—especially red meat (such as beef or liver), as well as chicken, turkey, pork, fish, and shellfish.
Foods high in iron include:
- red meat
- seafood
- organ meats, such as liver
- whole grains
- dried fruits
- nuts
- beans, especially lima beans
- dark green leafy vegetables, such as spinach and broccoli
- iron-fortified foods, such as breads and cereals (check the label).
Vitamin C can help your body absorb iron. Try eating foods, such as citrus fruits or juice. Some foods can make it harder for your body to absorb iron. These include coffee, tea, milk, egg whites, fiber, and soy protein. Try to avoid these foods if you have iron deficiency anemia.
Nonmeat foods that are good sources of iron include:
- Spinach and other dark green leafy vegetables
- Tofu
- Peas; lentils; white, red, and baked beans; soybeans; and chickpeas
- Dried fruits, such as prunes, raisins, and apricots
- Prune juice
- Iron-fortified cereals and breads
You can look at the Nutrition Facts label on packaged foods to find out how much iron the items contain. The amount is given as a percentage of the total amount of iron you need every day.
Iron also is available as a supplement. It’s usually combined with multivitamins and other minerals that help your body absorb iron.
Doctors may recommend iron supplements for premature infants, infants and young children who drink a lot of cow’s milk, and infants who are fed breast milk only or formula that isn’t fortified with iron.
To help prevent your child from getting iron deficiency anemia, you can:
- use iron-fortified formula
- use iron-fortified cereal starting around 4 months of age
- limit your child to less than 24 oz. (3 cups) of cow’s milk per day (after 12 months of age)
- introduce foods high in iron starting around 12 months of age.
Large amounts of iron can be harmful, so take iron supplements only as your doctor prescribes. Keep all products with iron stored out of reach of your child. Iron can be toxic if taken in large amounts.
Vitamin B12
Low levels of vitamin B12 can lead to pernicious anemia. This type of anemia often is treated with vitamin B12 supplements.
Foods high in vitamin B12 include:
- Breakfast cereals with added vitamin B12
- Meats such as beef, liver, poultry, and fish and shellfish
- Eggs and dairy products (such as milk, yogurt, and cheese)
- Foods fortified with vitamin B12, such as soy-based beverages and vegetarian burgers
Folic Acid
Folic acid (folate) is a vitamin B-9 that’s found in foods. Your body needs folic acid to make and maintain new cells. Folic acid also is very important for pregnant women. It helps them avoid anemia and promotes healthy growth of the fetus.
Foods high in folic acid (folate) include:
- Bread, pasta, and rice with added folic acid
- Spinach and other dark green leafy vegetables, such as spinach and broccoli
- Black-eyed peas, lentils and dried beans
- Beef liver
- Eggs
- Bananas, oranges, orange juice, and some other fruits and juices
Vitamin C
Vitamin C helps the body absorb iron. Good sources of vitamin C are vegetables and fruits, especially citrus fruits. Citrus fruits include oranges, grapefruits, tangerines, and similar fruits. Fresh and frozen fruits, vegetables, and juices usually have more vitamin C than canned ones.
If you’re taking medicines, ask your doctor or pharmacist whether you can eat grapefruit or drink grapefruit juice. This fruit can affect the strength of a few medicines and how well they work.
Other fruits rich in vitamin C include kiwi fruit, strawberries, and cantaloupes.
Vegetables rich in vitamin C include broccoli, peppers, Brussels sprouts, tomatoes, cabbage, potatoes, and leafy green vegetables like turnip greens and spinach.
Medicines
Your doctor may prescribe medicines to help your body make more red blood cells or to treat an underlying cause of anemia. Some of these medicines include:
- Antibiotics to treat infections.
- Hormones to treat heavy menstrual bleeding in teenaged and adult women.
- A man-made version of erythropoietin to stimulate your body to make more red blood cells. This hormone has some risks. You and your doctor will decide whether the benefits of this treatment outweigh the risks.
- Medicines to prevent the body’s immune system from destroying its own red blood cells.
- Chelation therapy for lead poisoning. Chelation therapy is used mainly in children. This is because children who have iron-deficiency anemia are at increased risk of lead poisoning.
Procedures
If your anemia is severe, your doctor may recommend a medical procedure. Procedures include blood transfusions and blood and marrow stem cell transplants.
Blood Transfusion
A blood transfusion is a safe, common procedure in which blood is given to you through an intravenous (IV) line in one of your blood vessels. Transfusions require careful matching of donated blood with the recipient’s blood.
For more information, see Blood Transfusion topic below.
Blood and Marrow Stem Cell Transplant
A blood and marrow stem cell transplant replaces your faulty stem cells with healthy ones from another person (a donor). Stem cells are made in the bone marrow. They develop into red and white blood cells and platelets.
During the transplant, which is like a blood transfusion, you get donated stem cells through a tube placed in a vein in your chest. Once the stem cells are in your body, they travel to your bone marrow and begin making new blood cells.
Surgery
If you have serious or life-threatening bleeding that’s causing anemia, you may need surgery. For example, you may need surgery to control ongoing bleeding due to a stomach ulcer or colon cancer.
If your body is destroying red blood cells at a high rate, you may need to have your spleen removed. The spleen is an organ that removes wornout red blood cells from the body. An enlarged or diseased spleen may remove more red blood cells than normal, causing anemia.