Contents
- What is saccharomyces cerevisiae
- Saccharomyces cerevisiae life cycle
- Saccharomyces cerevisiae antibody
- When is Saccharomyces cerevisiae antibody ordered?
- What does the Saccharomyces cerevisiae antibody test result mean?
- Is it necessary to perform Saccharomyces cerevisiae antibody testing more than once?
- Should everyone with abdominal pain and diarrhea have Saccharomyces cerevisiae antibody test performed?
- Will Saccharomyces cerevisiae antibody go away once they have developed?
- Can Saccharomyces cerevisiae antibody testing be performed in my doctor’s office?
- Saccharomyces cerevisiae infection
What is saccharomyces cerevisiae
Saccharomyces cerevisiae also known as baker’s yeast or brewer’s yeast, is also used as a probiotic agent to treat gastroenteritis by modulating the endogenous flora and immune system 1. Saccharomyces cerevisiae is normally considered a non-pathogenic yeast, in humans has several well-documented clinical indications, such as inflammatory bowel disease (IBD), malabsorption syndrome, prevention and treatment of diarrhea secondary to enteral or parenteral nutrition, and prophylaxis for infection from Clostridium difficile 2. A genetically very similar subtype, Saccharomyces boulardii, is used in a probioticum (Sacchaflor) to prevent antibiotic-associated diarrhea and in the treatment of recurrent Clostridium difficile associated diarrhea 3.
The countless domesticated strains of Saccharomyces cerevisiae are recognized the world over for their ability to ferment sugars to ethanol and carbon dioxide, producing a variety of beverages enjoyed by all cultures 4. Human use of yeast is thought to have begun >7000 years ago with the discovery that crushed grapes in water would ferment, as yeast is found in high abundance on the fruit 5. Yeast can be purposefully added to other sources of sugars, such as grains, malts, or other plant materials, to produce other alcoholic beverages. Although a relatively “newer” discovery, the carbon dioxide released by yeast has been used for centuries to raise bread dough, resulting in the light texture of leavened bread. For most of history, wine makers relied solely on the yeast present on the harvested grapes, but brewers and bakers would lovingly transfer their starter cultures from batch to batch as Saccharomyces cerevisiae worked unknown and unseen to ferment the various sugars provided by their owners. In the late 1800s, the Carlsberg Laboratory introduced the brewing industry to the process of science, and Emil Christian Hansen discovered how to purify yeast from mixed starter cultures 6. In the past 60 years, a rather short time evolutionarily speaking, the strains of Saccharomyces cerevisiae used in modern baking, brewing, fermenting, and wine-making have been carefully cultured, selected, and purified by these respective industries; each strain has its own particular characteristics and they are not interchangeable 5. However, a few wineries continue the practice of indigenous yeast fermentation, relying on the naturally provided yeasts of the grapes.
Saccharomyces cerevisiae life cycle
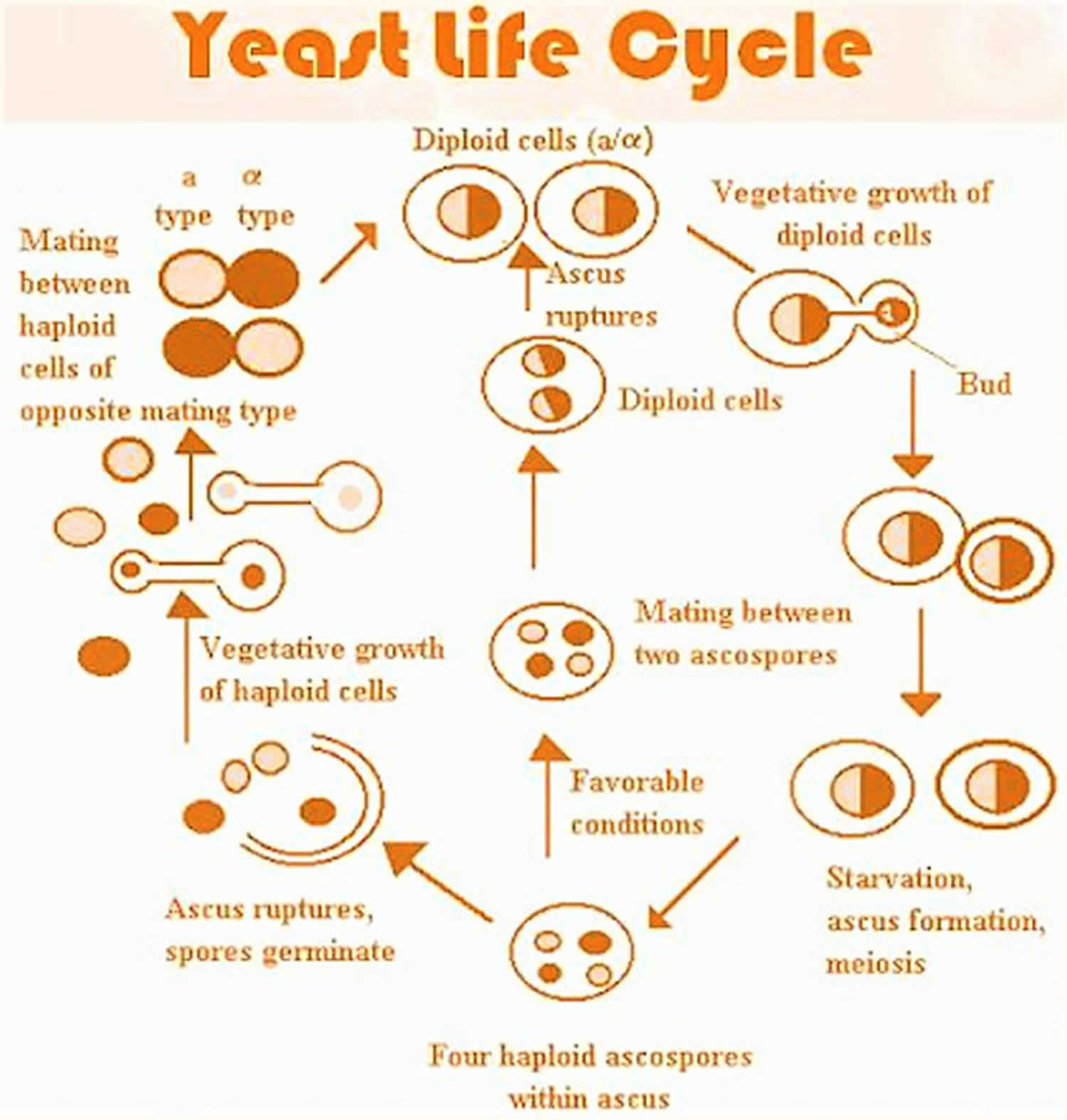
Like many other fungal organisms, Saccharomyces cerevisiae cells can reproduce both asexually and sexually. In fact, environmental conditions often determine the method of reproduction of these cells. Asexual reproduction of Saccharomyces cerevisiae cells is called budding, while sexual reproduction of the cells is called sporulation. Saccharomyces cerevisiae exists as either a diploid or a haploid cell. Both haploid and diploid Saccharomyces cerevisiae cells can reproduce by mitosis under favorable environmental conditions, where daughter cells bud off from their mother cells. During the budding process, the nucleus of the parent cell splits and locate itself towards the daughter cell. The bud continually grows and when it is fully matured, it can separate from the parent cell and function as an independent cell. Interestingly, diploid cells can undergo meiosis to produce four haploid spores that is composed of two a spores and two α (alpha) spores upon facing stressful conditions, such as nutrient depletion. Haploid cells are capable of mating with other haploid cells, but of the opposite mating type (an a cell can only mate with an α (alpha) cell, and vice versa) to produce a diploid cell. This process begins with the fusion of the cytoplasm, and then the haploid cells become fertilized and become a diploid zygote. After this, the zygote can undergo meiosis and form an ascus which will split into four ascospores. Finally, these haploids can then undergo germination and become haploid cells again. With sufficient and appropriate nutrition, Saccharomyces cerevisiae cells can reproduce every 100 minutes. Their average replicative lifespan lasts about 26 cell divisions.
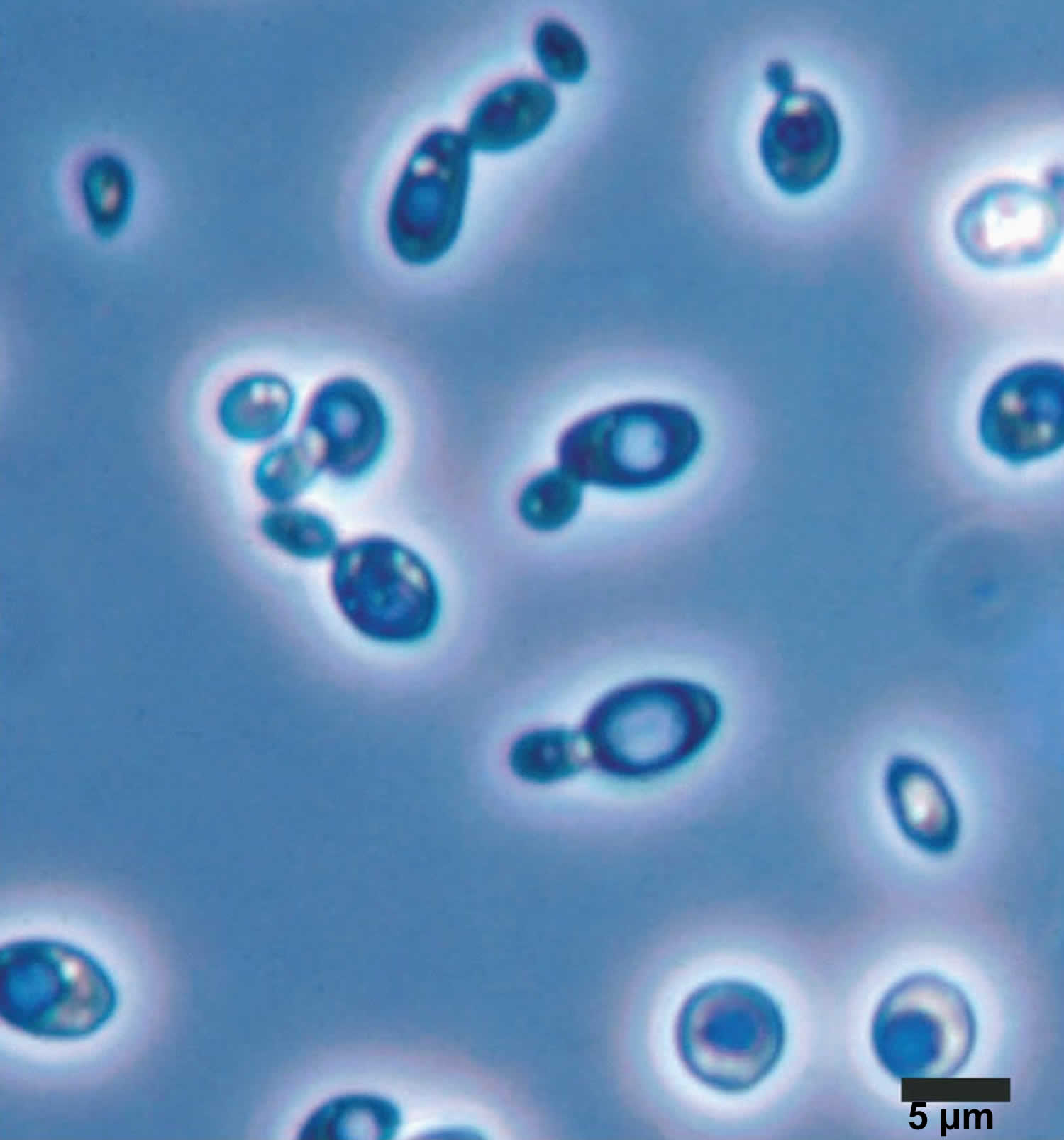
Saccharomyces cerevisiae size is generally larger than most bacteria: (1-5) μm (micrometer) wide and (5-30) μm (micrometer) length.
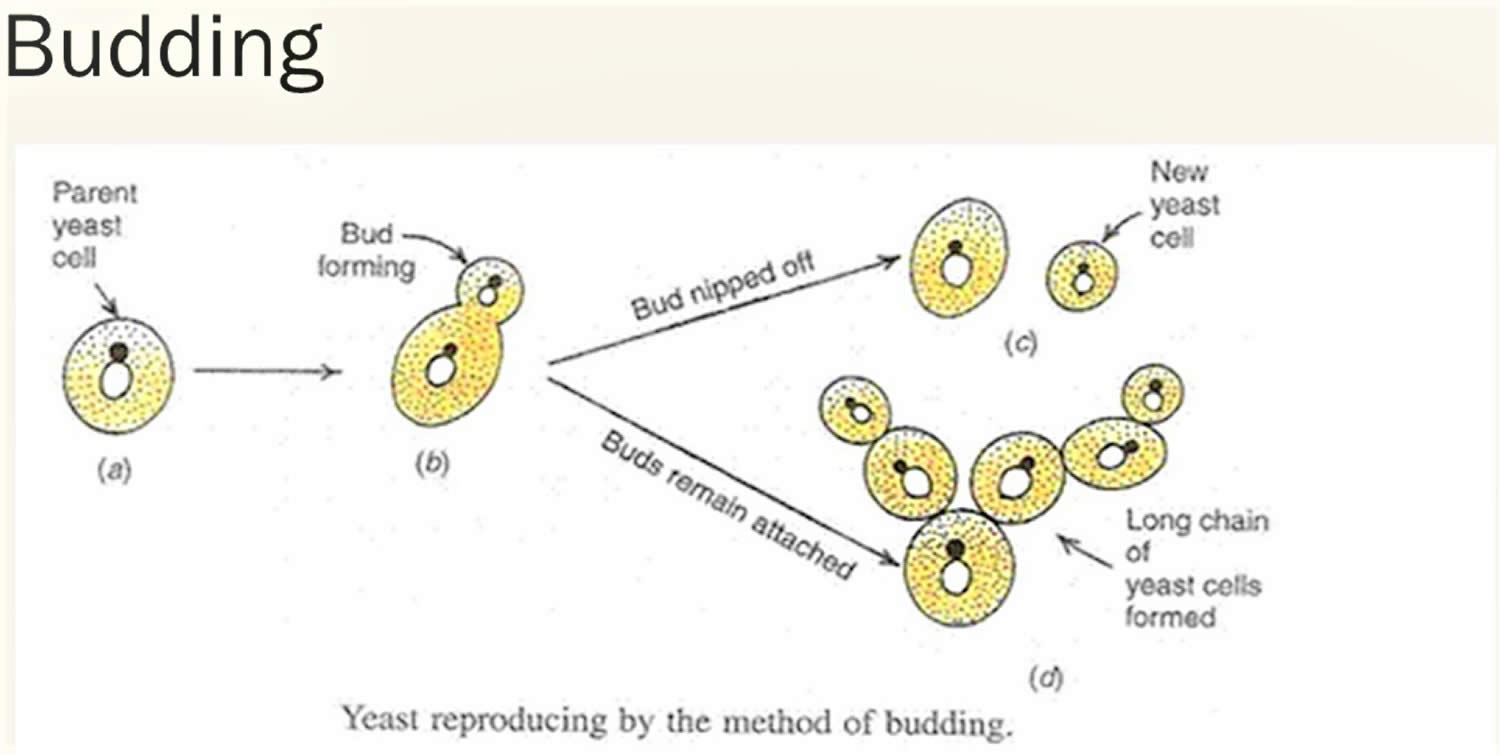
Asexual cycle (budding):
- Occurs during abundant supply of nutrition
- Parent nucleus divides and moves toward daughter cell
- Enzymatic activities increases,
- Increased turger pressure acts on weaker part of cell wall and bud erupts
- Septum formation and bud separates into individual cell
The rate of growth of Saccharomyces cerevisiae cells is synchronized with the growth rate of the bud, which separates from its parent cell when it reaches the size of the mature cell. In rapidly proliferating Saccharomyces cerevisiae populations, every cell can be seen with buds on the surface of the cell. This bud formation occupies the entire cell cycle. In slowly growing populations, cells lacking buds can be found easily, and bud formation only occupies a part of its entire cell cycle. This cell cycle normally consists of the following stages: G1, S, G2, and M.
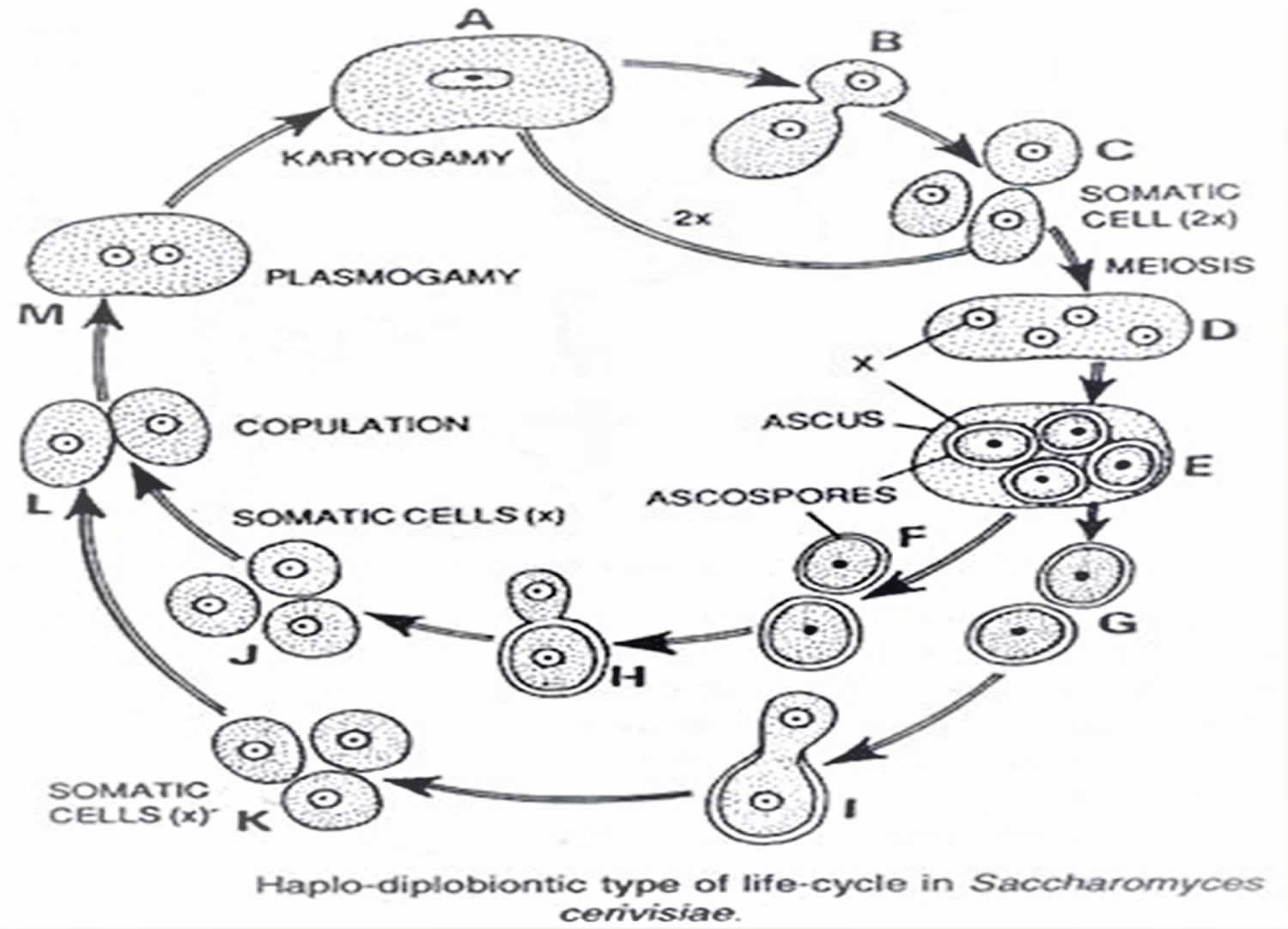
Sexual reproduction (Haplodiplobiontic life cycle):
- In this life cycle somatic cell of Saccharomyces cerevisiae yeast exists in two form (Haploid dwarf cell and Diploid large cell)
- Haploid cell contains two mating types “a” and “α” (alpha)
- During favorable condition each of the haploid cell multiply by budding only
- If these mating types comes in contact with each other, they form gametangia and starts sexual reproduction
- Fusion of these two haploid cell form large fusion cell called Plasmogamy
- Nucleus also fused by karyogamy to form zygote
- Zygote multiply by budding and forms several diploid cells
- these diploid cells are larger than haploid cells
- Like haploid cell, these large diploid cells also live independent life and reproduce by budding
- Under unfavorable condition, diploid large cell become spherical and directly behaves as ascus mother cell
- Nucleus of ascus mother cell divides by meiosis to form 4- haploid nuclei
- Out of 4-nuclei, 2 belongs to mating type “a” and t2 belongs to “α” (alpha)
- Each nuclei gather some cytoplasm and becomes ascospore
- Each ascospore is globular and thick walled structure and relased by rapture of ascus wall.
- Ascospore germinates to give haploid dwarf cell.
Figure 1. Saccharomyces cerevisiae life cycle
Figure 2. Saccharomyces cerevisiae life cycle (Budding)
Figure 3. Saccharomyces cerevisiae life cycle (Haplodiplobiontic life cycle)
Saccharomyces cerevisiae antibody
Anti-Saccharomyces cerevisiae antibodies (ASCA) are immune proteins that are frequently present in people who have inflammatory bowel disease (IBD). Saccharomyces cerevisiae antibody and perinuclear antineutrophil cytoplasmic antibodies (pANCA) testing are specific but not sensitive for Crohn’s disease and ulcerative colitis. It may be particularly useful for differentiating between Crohn’s disease and ulcerative colitis. Testing usually includes detecting two different classes of Saccharomyces cerevisiae antibody in the blood, IgG and IgA.
Saccharomyces cerevisiae are common yeast found in various foods. However, the correlation between the presence of antibodies to Saccharomyces cerevisiae and their involvement in the inflammatory bowel disease process is not understood at this time.
Inflammatory bowel disease (IBD) is a group of chronic disorders, thought to be an autoimmune process, characterized by swollen and damaged tissues in the lining of the intestinal tract. The symptoms and severity of inflammatory bowel disease vary from person to person and may fluctuate over time. Many of those affected experience flare-ups followed by periods of lessened symptoms or even remission.
Testing for Saccharomyces cerevisiae antibody can be useful in helping to distinguish between the two most common types of inflammatory bowel disease, Crohn disease and ulcerative colitis. Crohn’s disease can affect any part of the intestinal tract, from mouth to anus, but is primarily found in the small intestine and/or in the colon, while ulcerative colitis occurs in the colon.
The diagnosis of Crohn’s disease or ulcerative colitis is usually made through non-laboratory evaluations on the basis of endoscopic testing and the examination of biopsy samples from the intestines. Because both Crohn’s disease and ulcerative colitis can be found in the colon, it can sometimes be difficult to distinguish between the two. When this occurs, Saccharomyces cerevisiae antibody testing may be helpful as Saccharomyces cerevisiae antibody is much more frequently found in people with Crohn’s disease than in those with ulcerative colitis.
There are two classes of Saccharomyces cerevisiae antibodies produced by the body, Saccharomyces cerevisiae antibody IgG and Saccharomyces cerevisiae antibody IgA. Testing usually includes both classes.
Sometimes several antibodies, including Saccharomyces cerevisiae antibody, perinuclear anti-neutrophil cytoplasmic antibody (pANCA), anti-CBir1 (anti-flagellin antibody), and anti-Omp C (anti-outer membrane protein antibody), may be ordered together as a panel and the overall findings evaluated to either help distinguish between Crohn’s disease and ulcerative colitis or to try to help determine a prognosis for a person’s Crohn’s disease. The presence of multiple antibodies may indicate the likelihood of a more aggressive disease, but negative results do not rule out aggressive disease.
When is Saccharomyces cerevisiae antibody ordered?
Saccharomyces cerevisiae antibody testing is primarily ordered when a person has signs and symptoms that suggest inflammatory bowel disease and a healthcare practitioner is attempting to distinguish between Crohn’s disease and ulcerative colitis. It may be ordered along with perinuclear antineutrophil cytoplasmic antibodies (pANCA) and other antibody testing.
Signs and symptoms of an inflammatory bowel disease may include:
- Abdominal pain and cramps
- Diarrhea
- Rectal bleeding
- Fever
- Fatigue
- In some people, joint, skin, bone and organ-related symptoms
- Children may also have delayed development and growth retardation.
What does the Saccharomyces cerevisiae antibody test result mean?
A positive Saccharomyces cerevisiae antibody result is not diagnostic of Crohn’s disease, ulcerative colitis, or of an inflammatory bowel disease, but it does make it more likely that a person with symptoms has an inflammatory bowel disease 7.
Results of Saccharomyces cerevisiae antibody testing are often interpreted in conjunction with the results of perinuclear anti-neutrophil cytoplasmic antibody (pANCA) testing 7:
- If Saccharomyces cerevisiae antibody is positive and pANCA is negative, then it is likely that the person has Crohn’s disease.
- If Saccharomyces cerevisiae antibody is negative and pANCA is positive, then it is likely that the person has ulcerative colitis.
A negative result for Saccharomyces cerevisiae antibody and pANCA does necessarily rule out inflammatory bowel disease. A person who is negative may still have Crohn’s disease, ulcerative colitis, or another inflammatory bowel disease.
The presence of multiple antibodies (Saccharomyces cerevisiae antibody, anti-CBir1, anti-Omp C) may indicate the likelihood of a more aggressive disease, but negative results do not rule out aggressive disease.
The amount of Saccharomyces cerevisiae antibody and/or perinuclear anti-neutrophil cytoplasmic antibody (pANCA) present does not correlate with the severity of a person’s symptoms or condition and it cannot be used to monitor response to treatment.
Is it necessary to perform Saccharomyces cerevisiae antibody testing more than once?
Testing is usually only performed once, to help distinguish between Crohn’s disease and ulcerative colitis. It is typical to order tests for the two classes of antibody, Saccharomyces cerevisiae antibody IgG and Saccharomyces cerevisiae antibody IgA, at the same time. However, if only one of the types was initially ordered, then the other type (or more likely both) may be ordered at a later date.
Should everyone with abdominal pain and diarrhea have Saccharomyces cerevisiae antibody test performed?
No, it is not necessary in most cases as these symptoms are common and are most frequently due to something other than inflammatory bowel disease. Most people will never need to have Saccharomyces cerevisiae antibody testing performed.
Will Saccharomyces cerevisiae antibody go away once they have developed?
The level of antibody may vary over time, but once a person’s body has produced Saccharomyces cerevisiae antibody, it will continue to be present.
Can Saccharomyces cerevisiae antibody testing be performed in my doctor’s office?
In general, no. It is not offered by every hospital laboratory. It may be necessary to send your blood sample to a reference laboratory for testing.
Saccharomyces cerevisiae infection
Saccharomyces cerevisiae can be pathogenic and cause systemic infection from the microorganism itself and its subspecies Saccharomyces boulardii, in debilitated or immunosuppressed patients, especially when used as probiotic for treatment of diarrhea caused by antibiotics 8. Cases of the use of probiotics (e.g., Saccharomyces boulardii) immediately preceding or concomitant to the occurrence of fungemia by Saccharomyces cerevisiae are reported in literature 9. One of the main factors associated with this fungemia is the presence of a central venous catheter 10.
There are reports in the literature of systemic Saccharomyces cerevisiae infection, especially in adults; however, there are few cases among children 11. The infection can occur via two routes: intestinal translocation and venous catheter contamination, both from health care workers handling the medication with their hands, or the aerial drift of the strains after the capsules are opened. There are reports of infected individuals not only among those who received treatment with probiotics, but also in patients who shared the room with another patient undergoing treatment. Some studies showed that viable strains could be detected up to one meter away from the site of manipulation and persisted on the surface after two hours. Thus, it is therefore more prudent to handle them away from patients 12. Moreover, the Saccharomyces cerevisiae strains remain on the hands of professionals who handled them without gloves, even after appropriate cleaning 13.
Population-based studies suggest that Saccharomyces cerevisiae is responsible for 0.1%–3.6% of all episodes of fungemia 14. Since 1991 a few cases of fungemia with Saccharomyces species have been reported 15. This coincides with the time when the probioticum containing Saccharomyces boulardii was introduced at the market for treatment or prophylaxis of Clostridium difficile associated diarrhea 15. Fungemia by Saccharomyces species is mostly reported in patients treated with a probioticum, and who are critically ill or immunocompromised 16. However, it has also been reported in patients not receiving treatment with the probioticum themselves, but who share room with probioticum treated patients 17. Saccharomyces boulardii fungemia was reported in patients receiving high doses of probioticum, 1–3 g/day 15. In another case, a 79-year-old woman with rheumatoid arthritis was transferred from the surgical department after a bowel resection of one-meter ischemic distal ileum patient was treated with a low dose of 280 mg/day 3.
A review of the literature concerning 60 cases of fungemia with Saccharomyces cerevisiae found, that the most consistent risk factor for Saccharomyces cerevisiae fungemia was the use of probiotics containing Saccharomyces boulardii 3. In order to differentiate Saccharomyces cerevisiae from Saccharomyces boulardii a PCR fingerprinting procedure was used. Moreover, in the studies included in the review a high mortality, up to 29, 5%, was reported for patients with fungemia caused by Saccharomyces species 18.
According to previous studies, fungemia is seen in median 10 days after treatment initiation 18.
Different theories concerning the main mechanisms of developing fungemia with Saccharomyces cerevisiae or Saccharomyces boulardii have been propounded 16. One theory is that central venous catheter (CVC) may be contaminated from the hands of healthcare workers, when the probiotic capsules are opened and administered as a powder though nasogastric tubes. Accordingly, it has been demonstrated that when the probiotic capsules are opened, the powder with the yeast may persist on room surfaces after 2 hours at a 1 meter distance and can be detected on the bare hands of the healthcare workers even after washing hands. Hence, the central venous catheter of patients treated with probioticum as well as central venous catheter of non-treated patients may be contaminated. Another route of transmission is by enteral translocation through the intestine of ingested microorganisms from probiotic capsules. This way of transmission has also been described to be in evidence for bacteria. Colonic ulceration may predispose to the translocation of the yeast through the intestine. Finally, debilitated patient are more susceptible to develop infections due to almost non-pathogenic microorganisms.
Most of the patients reported, who have developed a fungemia with Saccharomyces cerevisiae or Saccharomyces boulardii, were critically ill, were intubated, had a central venous catheter in place, received intravenous alimentation and/or broad-spectrum antimicrobial therapy 16.
Saccharomyces cerevisiae or Saccharomyces boulardii are unusual causes of fungemia, but should never be dismissed as non-pathogenic when detected in blood cultures and especially not, when recovered from critically ill and immunocompromised patients. Due to the high mortality, immediate treatment is important. The suggested treatment is interruption of probioticum therapy, removal of central venous catheter and initiation of treatment with an antifungal agent as amphotericin B or according to sensitivity test.
The treatment indicated for bloodstream infection associated with the use of probiotics is the removal of the contaminated central venous catheter and the use of Amphotericin B 1 mg/kg/day or Fluconazole 10 mg/kg/day, although some articles describe strains resistant to Fluconazole and even to Amphotericin B 12. An article concerning the fungi colonization in hematologic patients revealed Saccharomyces cerevisiae with reduced sensitivity to fluconazole, although none of these patients have developed an invasive disease. In Spain, three cases of concomitant fungaemia caused by Saccharomyces cerevisiae were reported in an Intensive Care Unit (ICU) and isolated strains also showed reduced sensitivity to Fluconazole (MIC 8 mcg/dL). Some authors attribute this sensitivity spectrum to the frequent use of Fluconazole in the ICU and in patients with multiple comorbidities, and to the transmission of this agent through the hands of professionals. There are also reports of patients who developed fungemia caused by Saccharomyces cerevisiae during the use of Fluconazole (or prophylactic treatment of candidemia). Nevertheless, the outcome is usually favorable and similar to the outcome found from the use of the two antifungals 11.
- [Saccharomyces cerevisiae fungemia in an elderly patient following probiotic treatment]. Mikrobiyol Bul. 2014 Apr;48(2):351-5. https://www.ncbi.nlm.nih.gov/pubmed/24819274[↩]
- Vandenplas Y, Salvatore S, Vieira M, Devreker T, Hauser B. Probiotics in infectious diarrhoea in children: are they indicated?Eur. J Pediatr. 2007;166:1211–1218[↩]
- Thygesen JB, Glerup H, Tarp B. Saccharomyces boulardii fungemia caused by treatment with a probioticum. BMJ Case Reports. 2012;2012:bcr0620114412. doi:10.1136/bcr.06.2011.4412. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3316799/[↩][↩][↩]
- Duina AA, Miller ME, Keeney JB. Budding Yeast for Budding Geneticists: A Primer on the Saccharomyces cerevisiae Model System. Genetics. 2014;197(1):33-48. doi:10.1534/genetics.114.163188. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4012490/[↩]
- Mortimer R. K., 2000. Evolution and variation of the yeast (Saccharomyces) genome. Genome Res. 10: 403–409[↩][↩]
- Greig D., Leu J. Y., 2009. Natural history of budding yeast. Curr. Biol. 19: R886–R890.[↩]
- Diagnostic precision of anti-Saccharomyces cerevisiae antibodies and perinuclear antineutrophil cytoplasmic antibodies in inflammatory bowel disease. Am J Gastroenterol. 2006 Oct;101(10):2410-22. Epub 2006 Sep 4. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0022907[↩][↩]
- Food and probiotic strains from the Saccharomyces cerevisiae species as a possible origin of human systemic infections. de Llanos R, Querol A, Pemán J, Gobernado M, Fernández-Espinar MT. Int J Food Microbiol. 2006 Aug 1; 110(3):286-90. https://www.ncbi.nlm.nih.gov/pubmed/16782223/[↩]
- Romanio MR, Coraine LA, Maielo VP, Abramczyc ML, de Souza RL, Oliveira NF. SACCHAROMYCES CEREVISIAE FUNGEMIA IN A PEDIATRIC PATIENT AFTER TREATMENT WITH PROBIOTICS. Revista Paulista de Pediatria. 2017;35(3):361-364. doi:10.1590/1984-0462/;2017;35;3;00014. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5606182/[↩]
- Herbrecht R, Nivoix Y. Saccharomyces cerevisiae fungemia: an adverse effect of Saccharomyces boulardii probiotic administration. Clin Infect Dis. 2005;40:1635–1637[↩]
- Thygesen JB, Glerup H, Tarp B. Saccharomyces boulardii fungemia caused by treatment with a probioticum. BMJ Case Rep. Epub. 2012 Mar 27 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3316799/[↩][↩]
- Muñoz P, Bouza E, Cuenca-Estrella M, Eiros JM, Pérez MJ, Sánchez-Somolinos M. Saccharomyces cerevisae fungemia: an emerging infectious disease. Clin Infec Dis. 2005;40:1625–1634[↩][↩]
- Lherm T, Monet C, Nougière B, Soulier M, Larbi D, Le Gall C. Seven cases of fungemia with Saccharomyces boulardii in critically ill patients. Intensive Care Med. 2002;28:797–801[↩]
- Muñoz P, Bouza E, Cuenca-Estrella M, et al. Saccharomyces cerevisiae fungemia: an emerging infectious disease. Clin Infect Dis 2005;40:1625–34 https://www.ncbi.nlm.nih.gov/pubmed/15889360[↩]
- Lherm T, Monet C, Nougière B, et al. Seven cases of fungemia with Saccharomyces boulardii in critically ill patients. Intensive Care Med 2002;28:797–801[↩][↩][↩]
- Cherifi S, Robberecht J, Miendje Y. Saccharomyces cerevisiae fungemia in an elderly patient with Clostridium difficile colitis. Acta Clin Belg 2004;59:223–4[↩][↩][↩]
- Cassone M, Serra P, Mondello F, et al. Outbreak of Saccharomyces cerevisiae subtype boulardii fungemia in patients neighboring those treated with a probiotic preparation of the organism. J Clin Microbiol 2003;41:5340–3[↩]
- Muñoz P, Bouza E, Cuenca-Estrella M, et al. Saccharomyces cerevisiae fungemia: an emerging infectious disease. Clin Infect Dis 2005;40:1625–34[↩][↩]