Contents
What is scalded skin syndrome
Scalded skin syndrome is commonly called staphylococcal scalded skin syndrome (staph scalded skin syndrome) is the most serious staph skin infection characterized by red blistering skin that looks like a burn or scald, hence its name scalded skin syndrome. Staphylococcal scalded skin syndrome is caused by the release of two exotoxins (epidermolytic toxins A and B) from toxigenic strains of the bacteria Staphylococcus aureus. Desmosomes are the part of the skin cell responsible for adhering to the adjacent skin cell 1. The toxins bind to a molecule within the desmosome in the the superficial epidermis called Desmoglein 1 and break it up so the skin cells become unstuck.
When the toxins are released into the blood stream, the lack of protective antitoxin antibody in neonates allows the toxins to reach the epidermis where they act locally to produce the characteristic skin lesions 2. These human exfoliative toxin antibodies which have neutralizing properties decrease from 0 to 3 months 3. This could explain the severity of staphylococcal scalded skin syndrome in newborns.
Staphylococcal scalded skin syndrome has also been called Ritter disease or Lyell disease when it appears in newborns or young infants. In most cases staphylococcal scalded skin syndrome is cured completely, especially when diagnosed and treated appropriately. Once cured there is no visible difference or lasting effects to the skin. However, if left untreated or treatment is unsuccessful, severe infections such as sepsis, cellulitis, and pneumonia may develop. Death can follow severe infection. The mortality rate is approximately 4% and it is associated with extensive skin involvement 4.
Staphylococcal scalded skin syndrome differs from the more severe, and generally drug-induced, toxic epidermal necrolysis (Stevens-Johnson syndrome), in that the cleavage site in staphylococcal scalded skin syndrome is intraepidermal, as opposed to toxic epidermal necrolysis (Stevens-Johnson syndrome), which involves necrosis of the entire epidermis
- Staphylococcal scalded skin syndrome occurs mostly affects babies and children under the age of 5, especially neonates (newborn babies).
- Lifelong protective antibodies against staphylococcal exotoxins are usually acquired during childhood which makes staphylococcal scalded skin syndrome much less common in older children and adults. Lack of specific immunity to the toxins and an immature renal clearance system (toxins are primarily cleared from the body through the kidneys) make neonates the most at risk.
- Immunocompromised individuals (e.g., those on immune suppressant drugs or undergoing chemotherapy) and individuals with renal failure, regardless of age, may also be at risk of staphylococcal scalded skin syndrome.
Staphylococcal scalded skin syndrome usually starts with fever, irritability and widespread redness of the skin. Within 24-48 hours fluid-filled blisters form. These rupture easily, leaving an area that looks like a burn.
Your child may have staphylococcal scalded skin syndrome if they are feeling unwell with:
- a temperature over 38 °C (100.4 °F)
- skin which is painful to touch
- skin that has a burnt appearance or is peeling off
Characteristics of the staphylococcal scalded skin syndrome rash include:
- Tissue paper-like wrinkling of the skin is followed by the appearance of large fluid-filled blisters (bullae) in the armpits, groin and body orifices such as the nose and ears.
- Rash spreads to other parts of the body including the arms, legs and trunk. In newborns, lesions are often found in the diaper area or around the umbilical cord.
- Top layer of skin begins peeling off in sheets, leaving exposed a moist, red and tender area. Nikolsky sign (separation of the superficial skin from the deeper layers on application of light pressure) is positive.
- The mucous membranes of the mouth and anus were unaffected.
- Skin cultures showed a growth of Staphylococcus aureus, which produces exfoliative endotoxin B 5.
- Unless the primary infection site is observed swabs are often negative as the skin eruption is mediated by toxins.
- Other symptoms may include tender and painful areas around the infection site, weakness, and dehydration.
Staphylococcal scalded skin syndrome treatment
Usually antibiotics will need to be given intravenously, through a drip or cannula (small tube) inserted into a vein for a day or two. Once recovery has started treatment is then changed to an oral antibiotic usually for another 5 or 8 days. If the infection is caught early, it can sometimes be treated with oral antibiotics straightaway and intravenous antibiotics can be avoided. At the same time as having antibiotics, the skin needs to be gently cleansed at least once per day with a soap substitute, which may contain an antiseptic. Greasy moisturizers are recommended in order to soothe the skin and to stop the healing skin from sticking to clothing or bedding. In some cases it may be necessary to treat the area with burns dressings. Pain killers (e.g., acetaminophen) are also useful and can be used regularly until the skin has fully healed.
What are the features of the staphylococcal scalded skin syndrome?
The original infection may be relatively minor, for example an infected graze, nappy rash or a red sticky eye. After a few days a widespread patchy red rash appears with little blisters and then the patches rapidly join up to cover most of the skin surface. Unlike most rashes it is painful and affected children are miserable, feverish and may not want to be held or touched. Soon the skin begins to peel leaving painful raw patches.
If large areas of skin are shed, body fluid and salts can be lost causing dehydration, and further infection may get through into the bloodstream.
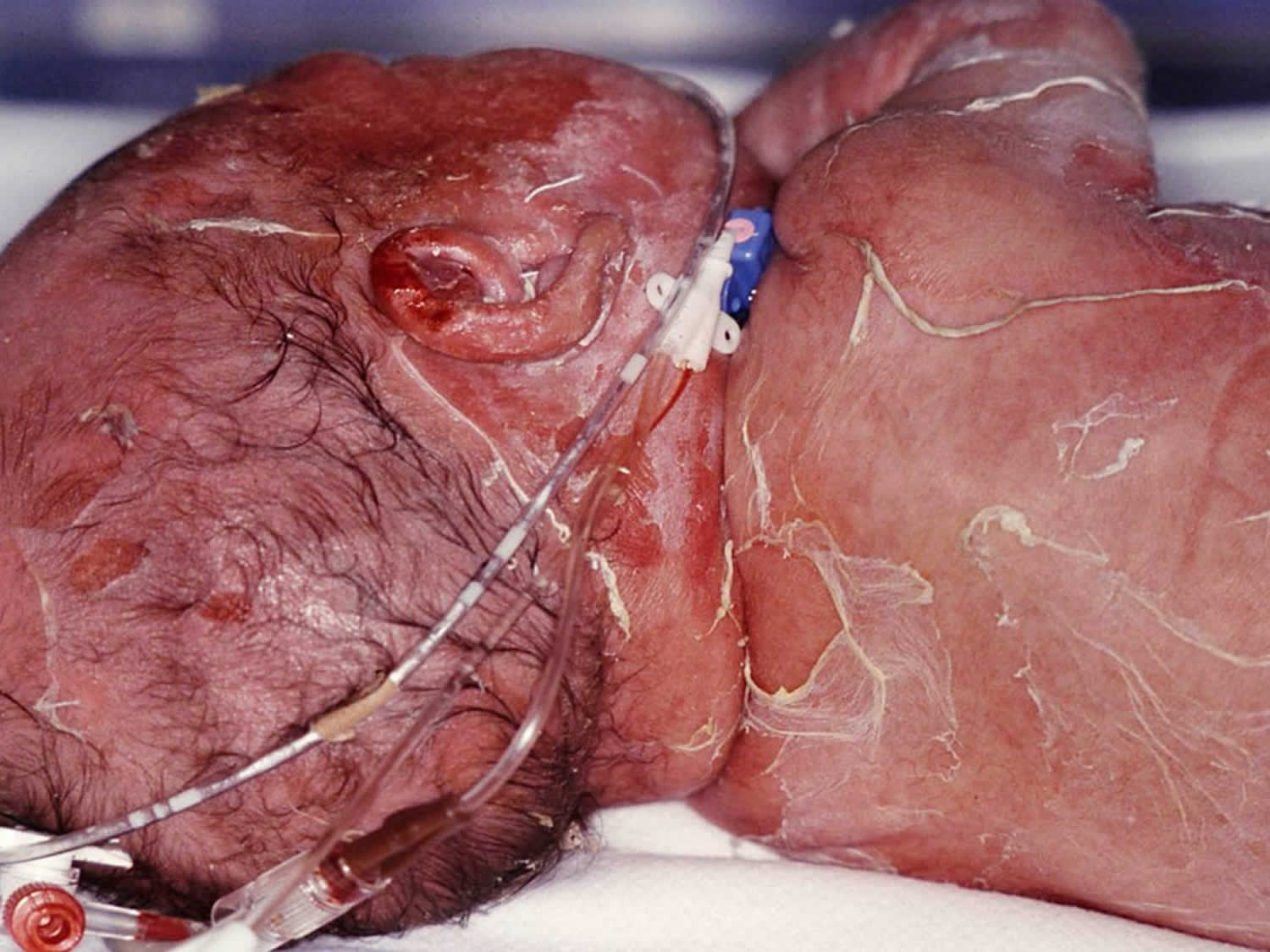
Figure 1. staphylococcal scalded skin syndrome neonate
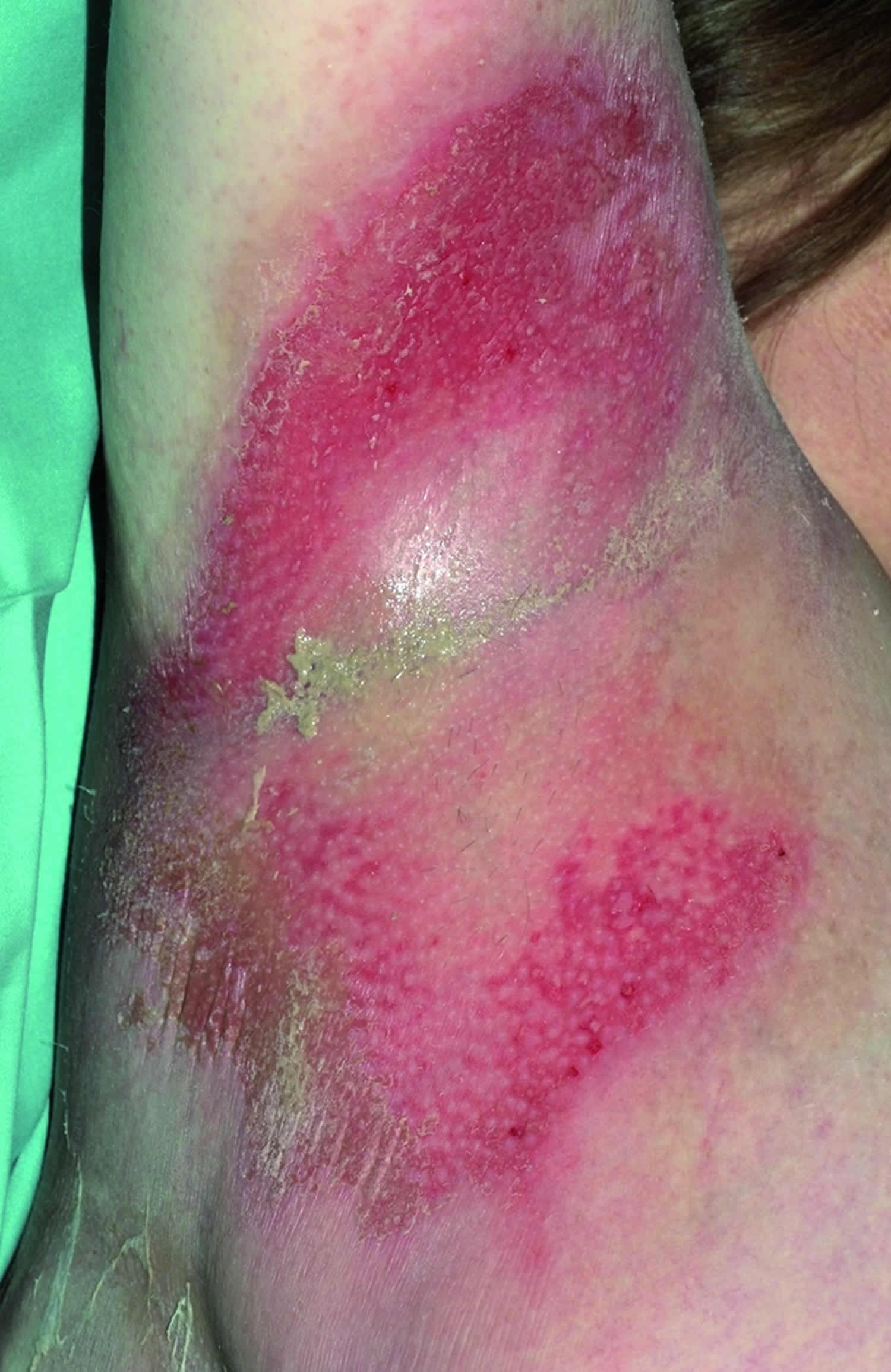
[Source 6]Figure 2. Staphylococcal scalded skin syndrome
Figure 3. Staphylococcal scalded skin syndrome in adults
Footnote: A 50 year old woman presented acutely with a rash and systemic upset. She was taking methotrexate for her arthritis and had type 2 diabetes.
[Source 7]How do you get staphylococcal scalded skin syndrome?
Staphylococcal scalded skin syndrome starts from a localized staphylococcal infection that is a producer of the two causative exotoxins (epidermolytic toxins A and B). Outbreaks of staphylococcal scalded skin syndrome often occur in childcare facilities. An asymptomatic adult carrier of Staphylococcus aureus introduces the bacteria into the nursery. About 15-40% of healthy humans are carriers of Staphylococcus aureus, that is, they have the bacteria on their skin without any sign of infection or disease (colonization). As staphylococcus bacteria can be carried by adults in their nose, throat or mouth without being infected or unwell it is easily passed from person to person from their hands, towels, and droplets from either coughing or sneezing. Staphylococcus aureus is also commonly found in infections of the throat, ears and eyes. Staphylococcal skin infections are seen commonly in infants and younger children, thus an obvious increased risk of staphylococcal scalded skin syndrome.
Is scalded skin syndrome contagious?
About 15-40% of healthy humans are asymptomatic carriers of Staphylococcus aureus and have no symptoms of scalded skin syndrome in adults.
The bacteria that cause staphylococcal scalded skin syndrome, Staphylococcus aureus, live harmlessly on many people’s skin, often in the nose and armpits and on the buttocks.
They usually only cause an infection if they get into the skin – for example, through a bite or cut.
Staphylococcus aureus bacteria can spread to others through:
- close skin contact
- sharing things like towels or toothbrushes
- droplets in coughs and sneezes (less common)
In most cases you can avoid developing a staph skin infection through basic hygiene. Always wash your hands thoroughly with soap and running water and dry them with a clean towel, or disposable paper towel.
If you live with someone who has a staph skin infection you may be able to avoid developing the condition by not sharing any personal items with them such as toothbrushes, towels, clothes and linen, washing their towels and bed linen every day, and washing your hands immediately if you come into contact with them.
You can’t always prevent staph infections
It can be difficult to prevent staph infections because many people have the bacteria on their skin.
But there are things you can do to reduce your chances of getting an infection or spreading the bacteria to others.
DO
- wash your hands with soap and water regularly
- keep your skin clean by having a bath or shower every day
- keep any cuts clean and covered
- use disposable tissues to blow your nose
DON’T
- share towels, washcloths, bed linen, toothbrushes and razors
Staphylococcal scalded skin syndrome fever diagnosis
Diagnosis of staphylococcal scalded skin syndrome depends on:
- History and physical examination
- Tzanck smear. Tzanck smear test is a simple and cheap test that relies on viewing and interpretation of single cells (cytology). The Tzanck smear is mainly used in an acute setting to distinguish Stevens Johnson syndrome / toxic epidermal necrolysis from staphylococcal scalded skin syndrome. However, it can be used to diagnose a variety cutaneous infections and blistering diseases.
- Skin biopsy, which shows intraepidermal cleavage at the granular layer
- Bacterial culture from skin, blood, urine or umblical cord sample (in a newborn baby)
Scalded skin syndrome treatment
Treatment of staphylococcal scalded skin syndrome usually requires hospitalization, as intravenous antibiotics are generally necessary to eradicate the staphylococcal infection. A penicillinase-resistant, anti-staphylococcal antibiotic such as flucloxacillin is used. Other antibiotics include nafcillin, oxacillin, cephalosporin and clindamycin. Vancomycin is used in infections suspected with methicillin resistance (MRSA). Depending on response to treatment, oral antibiotics can be substituted within several days. The patient may be discharged from hospital to continue treatment at home.
Corticosteroids slow down healing and hence are not given to patients with staphylococcal scalded skin syndrome.
Other supportive treatments for staphylococcal scalded skin syndrome include:
- Acetaminophen (paracetamol) when necessary for fever and pain.
- Monitoring and maintaining fluid and electrolyte intake.
- Skin care (the skin is often very fragile). Petroleum jelly should be applied to keep the skin moisturized.
- Newborn babies affected by staphylococcal scalded skin syndrome are usually kept in incubators.
Although the outward signs of staphylococcal scalded skin syndrome look bad, children generally recover well and healing is usually complete within 5–7 days of starting treatment.
- Site of action of exfoliative toxin in the staphylococcal scaled-skin syndrome. Lillibridge CB, Melish ME, Glasgow LA. Pediatrics. 1972 Nov; 50(5):728-38.[↩]
- Understanding the mechanism of action of the exfoliative toxins of Staphylococcus aureus. Ladhani S. FEMS Immunol Med Microbiol. 2003 Nov 28; 39(2):181-9. https://www.ncbi.nlm.nih.gov/pubmed/14625102/[↩]
- Mild staphylococcal scalded skin syndrome: an underdiagnosed clinical disorder. Hubiche T, Bes M, Roudiere L, Langlaude F, Etienne J, Del Giudice P. Br J Dermatol. 2012 Jan; 166(1):213-5.[↩]
- Staphylococcal scalded skin syndrome: diagnosis and management. Patel GK, Finlay AY. Am J Clin Dermatol. 2003; 4(3):165-75. https://www.ncbi.nlm.nih.gov/pubmed/12627992/[↩]
- Ladhani S, Joannou CL, Lochrie DP, et al. Clinical, microbial, and biochemical aspects of the exfoliative toxins causing staphylococcal scalded-skin syndrome. Clin Microbiol Rev1999;12:224–42.[↩]
- Baartmans MGA, Maas MH, Dokter J. Neonate with staphylococcal scalded skin syndrome. Archives of Disease in Childhood Fetal and Neonatal Edition. 2006;91(1):F25. doi:10.1136/adc.2005.082610. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2672643/[↩]
- Hoey S, Chuah SY, Poole H, Allen S. BMJ : British Medical Journal. 2008;337(7660):60. doi:10.1136/bmj.a587. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2443568/[↩]