Contents
What is sedimentation rate
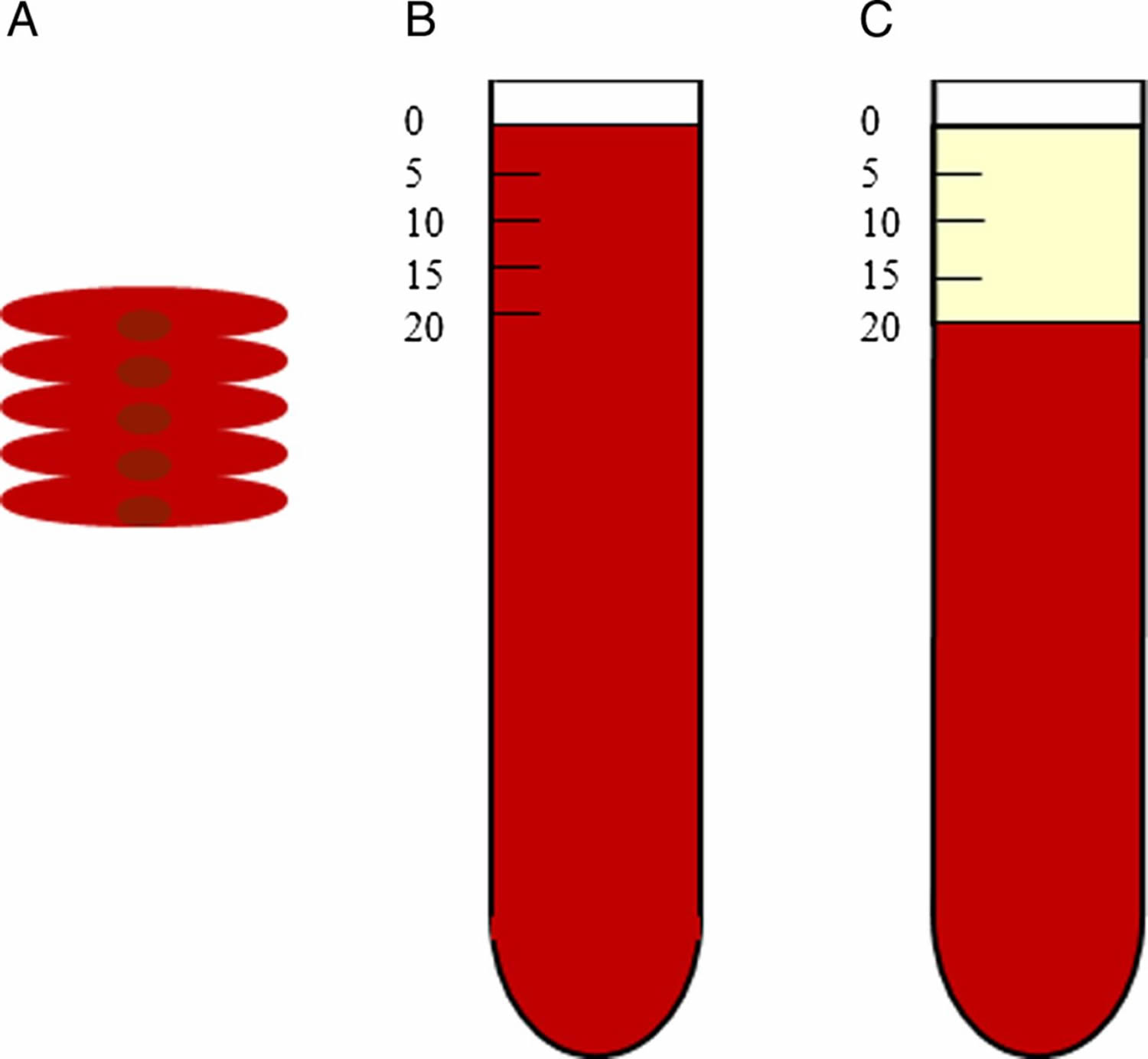
The sedimentation rate also called erythrocyte sedimentation rate, ESR, or sed rate, is a type of blood test that works by measuring the distance red blood cells travel under gravity in one hour in a sample of anticoagulated blood as they settle to the bottom of a test tube. The sedimentation rate is measured as the length, in mm (millimeter), of clear plasma at the top of a vertical tube. Sedimentation rate measures how long it takes for red blood cells to fall to the bottom of a test tube. Normally, red blood cells settle relatively slowly. The quicker the red blood cells fall, the more likely it is there are high levels of inflammation. The sedimentation rate is increased in inflammation, infection, injury, chronic disease, an immune disorder, cancer, rheumatic diseases, and diseases of the blood and bone marrow. The sedimentation rate is a simple and inexpensive test that has been used for almost a century.
Erythrocyte sedimentation rate (ESR) is a blood test that indirectly measures the degree of inflammation present in your body. The sedimentation rate blood test actually measures the rate of fall (sedimentation) of erythrocytes (red blood cells) in a sample of blood that has been placed into a tall, thin, vertical tube. Results are reported as the millimeters of clear fluid (plasma) that are present at the top portion of the tube after one hour.
In the laboratory, there are two main methods for measuring ESR: the Westergren and Wintrobe methods. These two methods use different standardized tubes and anticoagulants, and the results are not interchangeable 1.
Traditional ESR tests are read by a technician one hour after the test is started. Newer methods can be read at 20-30 minutes; and there are now commercial rapid tests available that use a centrifugal method and can be read five minutes after setup. This new method is being used more widely to shorten waiting times for patients, particularly in emergency departments.
Figure 1. Sedimentation rate – Note: (A) Rouleaux of red blood cells. (B) Test tube with anticoagulated whole blood at time O hour (C) Erythrocyte sedimentation rate of 20 mm/h at 1 hour later, plasma at top of tube.
Inflammation is part of the body’s immune response. It can be acute, developing rapidly after trauma, injury or infection, for example, or can occur over an extended time (chronic) with conditions such as autoimmune diseases or cancer.
The ESR is not diagnostic; it is a non-specific test that may be elevated in a number of these different conditions. It provides general information about the presence or absence of an inflammatory condition.
When a sample of blood is placed in a test tube, the red blood cells normally settle out relatively slowly, leaving little clear plasma. The red blood cells settle at a faster rate in the presence of an increased level of proteins, particularly proteins called acute phase reactants. The level of acute phase reactants such as C-reactive protein (CRP) and fibrinogen increases in the blood in response to inflammation. The C-reactive protein (CRP) test measures the level of a plasma protein (C-reactive protein) produced by liver cells in response to acute inflammation or infection 2. Unlike C-reactive protein (CRP), which is a direct measure of inflammatory response, ESR (erythrocyte sedimentation rate) is an indirect measure of the level of inflammation in the body. ESR measures the rate at which red blood cells settle in a specially designated tube of anticoagulated blood, an effect that is altered by proteins associated with an inflammatory response.
Both CRP and ESR are usually increased in acute inflammatory conditions. However, patterns of response are different for each test. CRP rises within hours of onset of an infection or inflammatory condition and returns to normal within three to seven days if the acute process is resolved. ESR, on the other hand, increases in a slower manner and remains elevated for a longer period of time 3. In addition, ESR is a non-specific measure that can be affected by factors other than inflammation, such as the size, shape, and number of red blood cells; levels of serum fibrinogen and immunoglobulins; renal function; age and sex; pregnancy; and use of medications 3. Because of these differences, CRP testing is often chosen over ESR in the assessment of early inflammation 4; however, there is no consensus on which single test is preferred 5 and as a result, physicians often request both tests.
The ESR differs from C-reactive protein (CRP) in that it is not a measurement of a single acute-phase protein. Rather, it measures not only several acute-phase proteins, but also a host of other factors. Erythrocyte sedimentation rate is dependent on the ability of red blood cells to aggregate and form rouleaux (stacks or aggregations of red blood cells). This, in turn, is determined by factors such as red blood cell number, size and shape, electrostatic charges and plasma viscosity 6. It is estimated that the acute-phase protein fibrinogen accounts for approximately 60-70% of the increase in ESR during an inflammatory state due to its ability to neutralize sialic acid residues on red blood cells that normally prevent rouleaux formation 7. As with CRP, fibrinogen is produced in the liver and is regulated primarily by IL-6, IL-1 and TNF-alpha.
Fibrinogen levels do not always correlate with ESR; other proteins in blood also affect red blood cell sedimentation rate. These proteins include, in order of
decreasing influence: beta-globulins, alpha-globulins, gamma-globulins and albumin. Globulins have roughly half the aggregating power of fibrinogen; albumin makes the least contribution 1. Other factors not necessarily related to inflammation that can influence ESR include anemia (increased sedimentation rate), polycythaemia (low sedimentation rate), and advancing age in women (increased sedimentation rate). These factors are taken into account when determining normal reference ranges. Medications can also affect ESR; for example, both the oral contraceptive
pill and heparin increase sedimentation rate.
There are a small number of conditions for which an elevated ESR is included in the diagnostic criteria. These include giant cell arteritis (GCA) and polymyalgia
rheumatic (PMR). There are no specific serological tests for these conditions. A provisional diagnosis is generally made on the basis of suggestive signs and symptoms in a patient aged more than 50-65 with an ESR of greater than 40-50mm/hour (though it is typically higher than this). Although there is some evidence to suggest that CRP may be more sensitive than ESR, it is the ESR that is included in the majority of published diagnostic criteria 8.
As many of the factors that determine the ESR have long half-lives, it is less valuable in assessing acute changes than CRP. An elevated ESR may be due to events that have occurred weeks to months previously and may have resolved at the time of measurement. In the investigation of a patient with an unclear source of inflammation, a mild to moderate elevation in ESR by itself lacks the specificity to be of great diagnostic value. Marked elevation of ESR (i.e, greater than 100mm/hr), on the other hand, is almost always significant. In patients with an ESR greater than 100mm/hr, a significant diagnosis will be made in over
90% of cases 9.
As a general rule, an ESR of over 100mm/hr should prompt consideration and investigation for these conditions:
- Infection
- Tuberculosis
- Endocarditis
- Abscess
- Malignancy
- Dysproteinemia (i.e, multiple myeloma)
- Metastatic cancer
- Rheumatological conditions
- Vasculitis
- Inflammatory arthritis
- Rheumatoid arthritis
- Crystal arthropathies.
Some clinicians use the term “vasculitic screen” to describe a set of tests ordered when vasculitis is suspected or needs to be excluded. The composition of this panel of tests may vary between clinicians, but generally includes a mix of autoimmune serology including antinuclear antibodies (ANA), antibodies to extractable nuclear antigens (ENA) and ANCA. It will often also include serology for SLE (double-stranded DNA), rheumatoid arthritis (rheumatoid factor and cyclic-citrullinated peptide antibodies), as well as ESR and CRP.
A requirement of a good screening test is a high sensitivity. These tests may detect a proportion of patients with either ANCA-associated or lupus-related vasculitis, but — with the exception of ESR — will likely miss the many forms of vasculitis such as GCA, polyarteritis nodosa (PAN), Behcet’s syndrome and others, which do not have specific serological tests. The ESR is perhaps the closest test to an actual vasculitis screen, as a normal ESR would make active vasculitis very unlikely, with the exception of exceedingly rare forms such as primary vasculitis of the central nervous system.
Sedimentation Rate Key Points
- An ESR does not specifically diagnose any diseases, but it can provide information about whether or not there is inflammation in your body. If your ESR results are abnormal, your health care provider will need more information and will likely order more lab tests before making a diagnosis.
- Since ESR is a non-specific marker of inflammation and is affected by other factors, the results must be used along with other clinical findings, the individual’s health history, and results from other laboratory tests. If the ESR and clinical findings match, the health practitioner may be able to confirm or rule out a suspected diagnosis.
- ESR rate is useful for diagnosing and monitoring of Temporal arteritis and Polymyalgia rheumatica. ESR is also useful for following up of osteomyelitis and prosthetic joint infection.
- The ESR should not be used to screen asymptomatic patients for the presence of disease.
- A normal ESR does not exclude active disease.
- A single elevated ESR, without any symptoms of a specific disease, will usually not give enough information to make a medical decision. Furthermore, a normal result does not rule out inflammation or disease.
- Moderately elevated ESR occurs with inflammation but also with anemia, infection, pregnancy and with aging.
- Women tend to have a higher ESR, and menstruation and pregnancy can cause temporary elevations.
- In a pediatric setting, the ESR test is used for the diagnosis and monitoring of children with rheumatoid arthritis or Kawasaki disease.
- A very high ESR usually has an obvious cause, such as a severe infection, marked by an increase in globulins, polymyalgia rheumatica or temporal arteritis. A health practitioner will typically use other follow-up tests, such as blood cultures, depending on the person’s symptoms. People with multiple myeloma or Waldenstrom’s macroglobulinemia (tumors that make large amounts of immunoglobulins) typically have very high ESRs even if they don’t have inflammation.
- The ESR may be very high (> 100 mm in 1 hour) in Plasma cell myeloma and autoimmune disease, especially Temporal arteritis (giant cell arteritis), Polymyalgia rheumatica and Systemic lupus erythematosus.
- A low ESR (< 1 mm in 1 hour) may be seen in Polycythemia vera and Sickle cell disorders.
- When monitoring a condition over time, rising ESRs may indicate increasing inflammation or a poor response to a therapy; normal or decreasing ESRs may indicate an appropriate response to treatment.
There have been questions about the usefulness of the ESR in light of newer tests that have come into use that are more specific. However, ESR test is typically indicated for the diagnosis and monitoring of temporal arteritis, systemic vasculitis and polymyalgia rheumatica. Extremely elevated ESR is useful in developing a rheumatic disease differential diagnosis. In addition, ESR may still be a good option in some situations, when, for example, the newer tests are not available in areas with limited resources or when monitoring the course of a disease.
An ESR is often used to help diagnose conditions associated with inflammation, such as:
- Arthritis
- Endocarditis
- Crohn’s disease
- Giant cell arteritis
- Polymyalgia rheumatica
Along with other tests, an ESR can also be useful in confirming whether you have an infection.
How the sedimentation rate test is performed
A blood sample is needed. Most of the time, blood is drawn from a vein located on the inside of the elbow or the back of the hand. The blood sample is sent to a lab.
The test measures how fast red blood cells (called erythrocytes) fall to the bottom of a tall, thin tube.
How to prepare for the sedimentation rate test
There are no special steps needed to prepare for ESR test.
Why get tested for ESR?
To detect the presence of inflammation caused by one or more conditions such as infections, tumors or autoimmune diseases; to help diagnose and monitor specific conditions such as temporal arteritis, systemic vasculitis, polymyalgia rheumatica, or rheumatoid arthritis.
Reasons why a sedimentation rate may be done include:
- Unexplained fevers
- Certain types of arthritis
- Muscle symptoms
- Other vague symptoms that cannot be explained
ESR test may also be used to monitor whether an illness is responding to treatment.
Erythrocyte sedimentation rate test can be used to monitor inflammatory diseases or cancer. It is not used to diagnose a specific disorder.
However, the ESR test is useful for detecting and monitoring:
- Autoimmune disorders
- Bone infections
- Certain forms of arthritis
- Inflammatory diseases that cause vague symptoms
- Tissue death
When to get ESR test done?
When your health practitioner thinks that you might have a condition causing inflammation; when you have signs and symptoms associated with temporal arteritis, systemic vasculitis, polymyalgia rheumatica, or rheumatoid arthritis such as headaches, neck or shoulder pain, pelvic pain, anemia, poor appetite, unexplained weight loss, and joint stiffness. The ESR may also be ordered at regular intervals to assist in monitoring the course of these diseases.
Before doing an extensive workup looking for disease, a health practitioner may want to repeat the ESR.
An ESR may be ordered when a condition or disease is suspected of causing inflammation somewhere in the body. There are numerous inflammatory conditions that may be detected using this test. For example, it may be ordered when arthritis is suspected of causing inflammation and pain in the joints or when digestive symptoms are suspected to be caused by inflammatory bowel disease.
What other tests might my doctor order besides ESR?
Your health practitioner may order the C-reactive protein (CRP) test as well as other general tests, such as a comprehensive metabolic panel (CMP) or a complete blood count (CBC), at the same time as the ESR. ESR and C-reactive protein (CRP) are both markers of inflammation. Generally, ESR does not change as rapidly as does CRP, either at the start of inflammation or as it resolves. CRP is not affected by as many other factors as is ESR, making it a better marker of inflammation. However, because ESR is an easily performed test, many health practitioners still use ESR as an initial test when they think a patient has inflammation.
Examples of other tests that may be ordered based on your symptoms include antinuclear antibody (ANA), rheumatoid factor (RF), fibrinogen or serum protein electrophoresis. An elevated ESR is typically a result of two types of proteins, globulins or fibrinogen. Depending on your medical history, signs, symptoms and what your health practitioner suspects is the cause, he or she may order a fibrinogen level (a clotting protein that is another marker of inflammation) and a serum protein electrophoresis to determine which of these (or both) is causing the elevated ESR. If severe infection is suspected, a blood culture may be done.
What is inflammation?
Inflammation is described as having four major features:
- Redness
- Heat
- Pain
- Loss of Function
Inflammation is a completely natural process that is part of your body’s response to any injury that it undergoes. Inflammation can result from a variety of tissue insults including infections, trauma, autoimmunity, toxins, chemicals and malignancy. These stimuli lead to the production of cytokines (small molecules that communicate between cells), which trigger the up- or down-regulation of acute-phase proteins 10. Acute-phase proteins are primarily produced in the liver by hepatocytes. These proteins can be separated into groups with different functional properties. There is marked variation in the timing and magnitude of response among different acute-phase proteins. As an example, ceruloplasmin and complement proteins increase by around 50% while C-reactive protein (CRP) and serum amyloid A can be induced by 1000-fold 11. CRP begins to rise within 4-6 hours after an inflammatory stimulus and reaches its peak level in blood within 48-72 hours 12.
Inflammation is designed to wall off the area so that damage cannot spread very far. It then tries to destroy the cause of the damage. Finally, inflammation is involved in healing the body and hopefully returning it to the exact state that it was in before the injury. There are two types of inflammation, acute inflammation which starts suddenly but goes away relatively quickly, and chronic inflammation that can remain active for months, years or decades. Inflammation is an integral part of the immune system, and for more information about some of the terms used below, see information about the acquired and innate immune systems.
Inflammation can occur over the short term (acute) or over a long period of time (chronic) and can be caused by a variety of conditions and disease. Some examples include:
- Infections
- Arthritis
- Autoimmune diseases, such as lupus or Systemic Lupus Erythematosus (SLE)
- Inflammatory bowel disease
The most common cause of a relatively short period of inflammation is an infection, and almost all infections wither with bacteria, fungus or virus will cause inflammation. The red, sore throat of a cold is an example of inflammation secondary to a virus. As mentioned previously though, things such as physical trauma, toxins, heat, cold and allergic reactions also cause inflammation.
Below are some of the more common causes of chronic inflammation.
Persistent infections:
- Syphilis;
- Certain fungi.
Prolonged exposure to potentially toxic agents:
- Silicosis;
- Breathing in a lot of carbon (e.g., coal miners);
- Atherosclerosis (plaque build-up on blood vessel walls).
Autoimmunity:
- Rheumatoid arthritis;
- Systemic lupus erythematosus (SLE);
- Most other auto-immune conditions.
What do changes in my ESR mean?
Changes in the ESR may indicate the presence or abatement of infection or inflammation. If you have a chronic inflammatory disease, the ESR may fluctuate with the degree of severity or clinical course of your condition.
Normal Sedimentation Rate
The result of an ESR is reported as the millimeters of clear fluid (plasma) that are present at the top portion of the tube after one hour (mm/hr = millimeters per hour).
For adults (Sedimentation rate Westergren method):
- Men under 50 years old: less than 15 mm/hr
- Men over 50 years old: less than 20 mm/hr
- Women under 50 years old: less than 20 mm/hr
- Women over 50 years old: less than 30 mm/hr
For children (Sedimentation rate Westergren method):
- Newborn: 0 to 2 mm/hr
- Newborn to puberty: 3 to 13 mm/hr
Note: mm/hr = millimeters per hour
Normal value ranges may vary slightly among different laboratories. Talk to your health care provider about the meaning of your specific test results.
If your sedimentation rate results are not in the normal range, it doesn’t necessarily mean you have a medical condition that requires treatment. A moderate ESR may indicate pregnancy, menstruation, or anemia, rather than an inflammatory disease. Certain medicines and supplements can also affect your results. These include oral contraceptives, aspirin, cortisone, and vitamin A. Be sure to tell your health care provider about any drugs or supplements you are taking.
Lower than normal ESR
A low ESR can be seen with conditions that inhibit the normal sedimentation of red blood cells, such as a high red blood cell count (polycythemia), significantly high white blood cell count (leukocytosis), and some protein abnormalities. Some changes in red cell shape (such as sickle cells in sickle cell anemia) also lower the ESR.
Lower-than-normal sedimentation rate levels occur with:
- Congestive heart failure
- Hyperviscosity
- Hypofibrinogenemia (decreased fibrinogen levels)
- Leukemia
- Leukocytosis, an abnormal increase in white blood cells
- Low plasma protein (due to liver or kidney disease)
- Polycythemia
- Sickle cell anemia
What happens if erythrocyte sedimentation rate is high?
An abnormal ESR may help with a diagnosis, but it does not prove that you have a certain condition. Other tests are almost always needed.
A high ESR is an indicator in your body that can indicate inflammation somewhere in the body, but it does not say where or indicate the specific cause. Like pain, it is giving you a warning that something is wrong. In most cases, the ESR will decrease over time once the underlying inflammation is addressed. If you have a chronic (longstanding) inflammatory disease, the ESR may fluctuate with the degree of activity your condition.
The ESR also increases with age, pregnancy and in those with anemia.
It is important to speak with your doctor about your results.
An increased ESR rate may be due to:
- Anemia
- Cancers such as lymphoma or multiple myeloma
- Kidney disease
- Pregnancy
- Thyroid disease
The immune system helps protect the body against harmful substances. An autoimmune disorder is when the immune system mistakenly attacks and destroys healthy body tissue. ESR is often higher than normal in people with an autoimmune disorder.
However, a moderate ESR may also indicate pregnancy, menstruation, or anemia, rather than an inflammatory disease. Certain medicines and supplements can also affect your results. These include oral contraceptives, aspirin, cortisone, and vitamin A. Be sure to tell your health care provider about any drugs or supplements you are taking.
Common autoimmune disorders include:
- Lupus or or Systemic Lupus Erythematosus (SLE)
- Rheumatoid arthritis in adults or children
Very high ESR levels occur with less common autoimmune disorders, including:
- Allergic vasculitis
- Giant cell arteritis
- Hyperfibrinogenemia (increased fibrinogen levels in the blood)
- Macroglobulinemia – primary
- Necrotizing vasculitis
- Polymyalgia rheumatica
An increased ESR rate may be due to some infections, including:
- Body-wide (systemic) infection
- Bone infections
- Infection of the heart or heart valves
- Rheumatic fever
- Severe skin infections, such as erysipelas
- Tuberculosis
Elevated sedimentation rate symptoms
Elevated sedimentation rate usually means inflammation. Symptoms of an inflammatory disorder includes:
- Headaches
- Fever
- Weight loss
- Joint stiffness
- Neck or shoulder pain
- Loss of appetite
- Anemia
- Plant MJ, et al. Arthritis & Rheumatism 2000; 43(7):1473-77.[↩][↩]
- Pagana KD, Pagana TJ, MacDonald S. Mosby’s Canadian manual of diagnostic and laboratory tests. Toronto: Mosby Canada; 2013.[↩]
- CRP vs ESR assessing & measuring the inflammatory response. Dunedin (New Zealand): bpacnz; 2005 https://bpac.org.nz/resources/other/audits/bpac_crp_audit_wv.pdf[↩][↩]
- Morris SA. C-Reactive Protein (CRP): the best lab test for inflammation/infection. Alberta Health Serv Lab Rep. 2013 Apr 1 https://www.albertahealthservices.ca/default.aspx[↩]
- Watson J, Round A, Hamilton W. Raised inflammatory markers. BMJ. 2012;344:e454.[↩]
- Bedell SE, Bush BT. American Journal of Medicine 1985; 76:1001-09.[↩]
- Paulus HE, Brahn E. Journal of Rheumatology 2004; 31:838-40.[↩]
- Laria A, et al. Clinical Rheumatology 2012; 31:1389-93.[↩]
- Fincher RME, Page MI. Archives of Internal Medicine 1986; 146:1581-83.[↩]
- Pepys MB, Hirschfield GM. Journal of Clinical Investigation 2003; 111:1805-12[↩]
- Gabay C, Kushner I. New England Journal of Medicine 1999; 340(6):449-54.[↩]
- Volanakis JE. Molecular Immunology 2001; 38:189-97.[↩]