The Skin
The skin (integument) is the body’s largest and heaviest organ. In adults, the skin covers an area of 1.5 to 2.0 m2 and accounts for about 15% of the body weight.
The skin consists of two layers:
- a stratified squamous epithelium called the Epidermis and
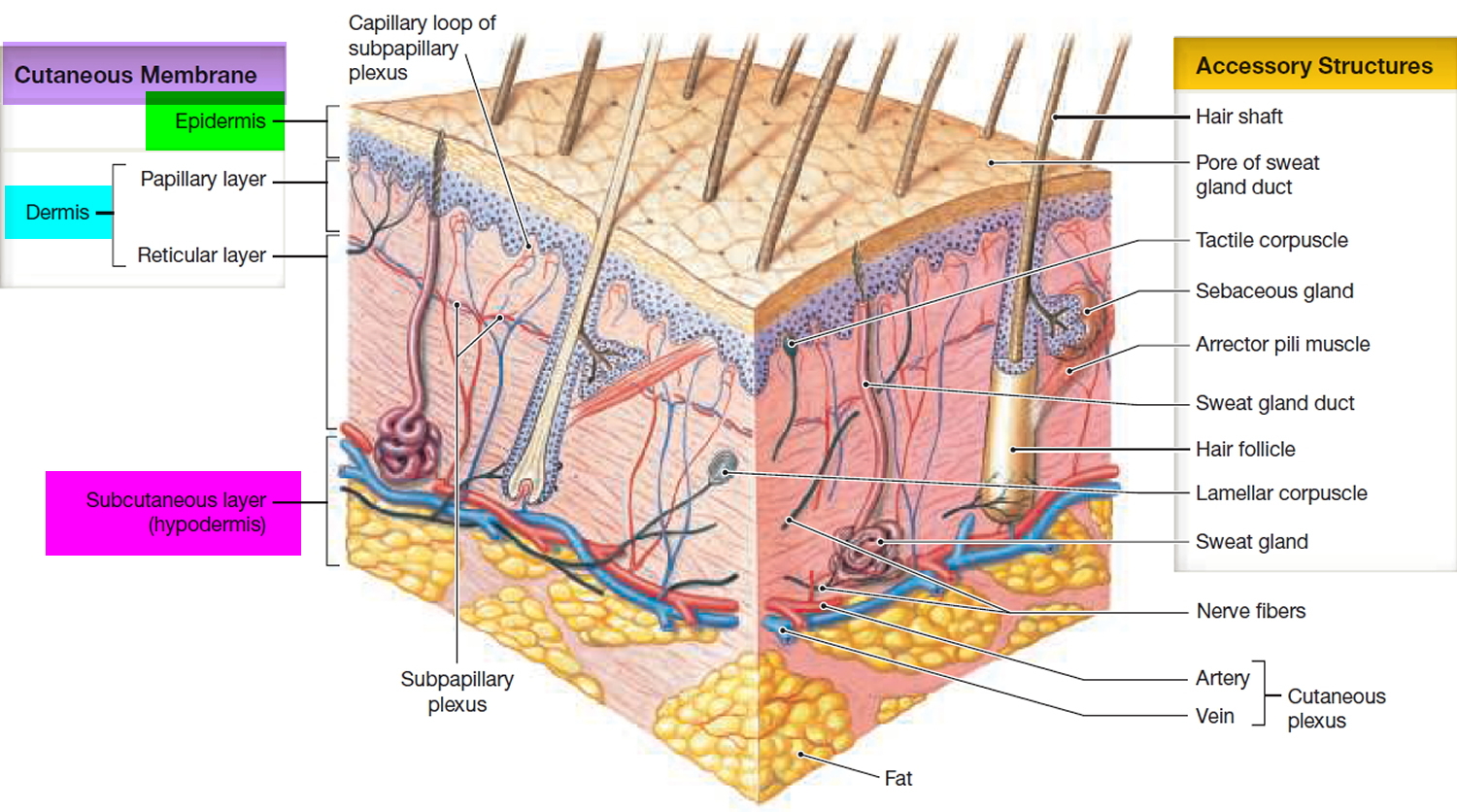
- a deeper connective tissue layer called the Dermis (Figure 1).
Figure 1. Skin structure
Below the dermis is another connective tissue layer, the hypodermis, which is not part of the skin but is customarily studied in conjunction with it. Most of the skin is 1 to 2 mm thick, but it ranges from less than 0.5 mm on the eyelids to 6 mm between the shoulder blades. The difference is due mainly to variation in thickness of the dermis, although skin is classified as thick or thin based on the relative thickness of the epidermis alone.
Thick skin covers the palms, soles, and corresponding surfaces of the fingers and toes. Its epidermis alone is about 0.5 mm thick, due to a very thick surface layer of dead cells called the stratum corneum (see Figure 2). Thick skin has sweat glands but no hair follicles or sebaceous (oil) glands. The rest of the body is covered with thin skin, which has an epidermis about 0.1 mm thick, with a thin stratum corneum. It possesses hair follicles, sebaceous glands, and sweat glands.
The accessory structures include hair, nails, and a variety of multicellular exocrine glands. These structures are located in the dermis and protrude through the epidermis to the surface.
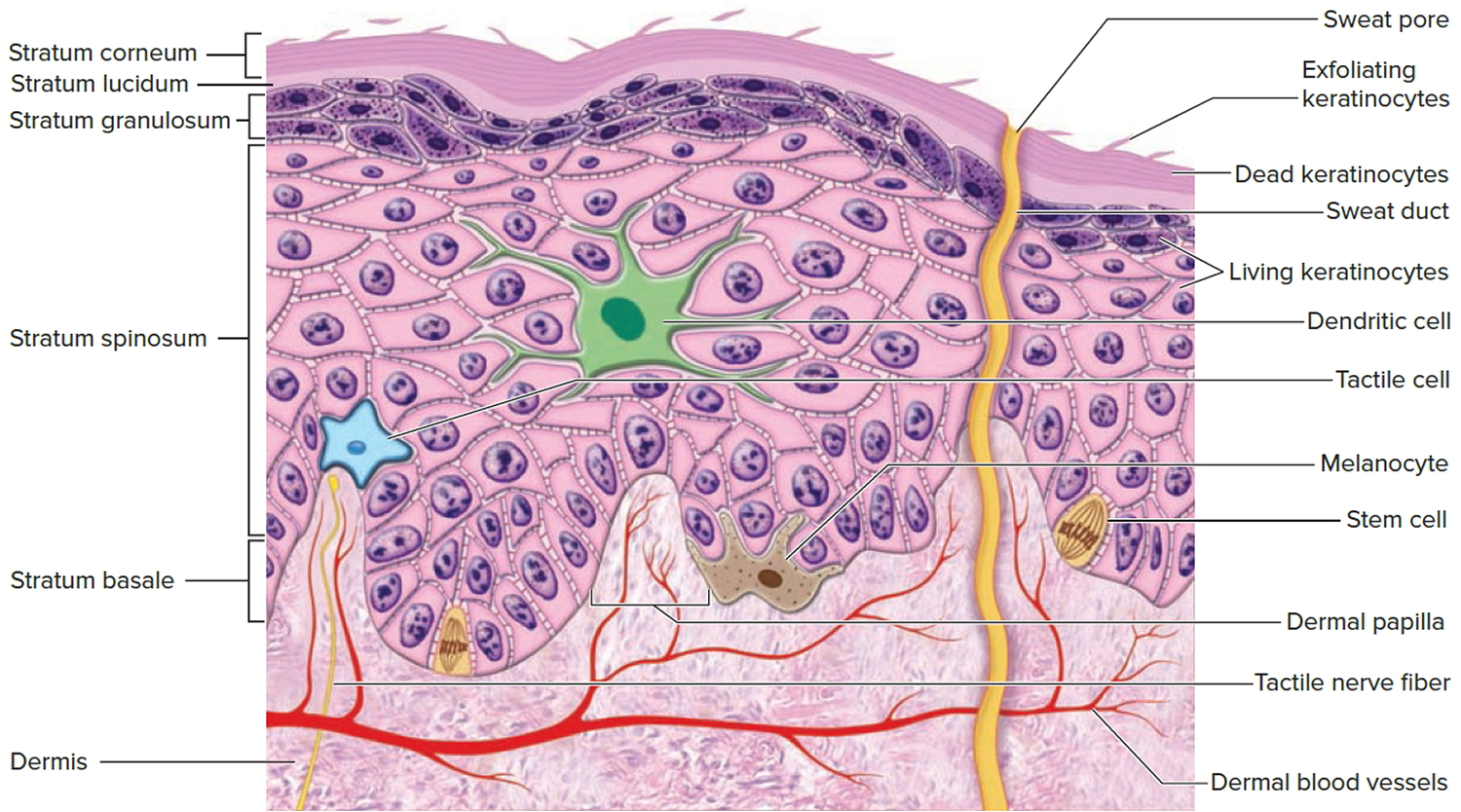
Figure 2. Structure and skin cells of the Epidermis
Functions of the skin
The skin is much more than a container for the body. It has a variety of very important functions that go well beyond appearance, as you shall see here.
- Resistance to trauma and infection. The skin suffers the most physical injuries to the body, but it resists and recovers from trauma better than other organs do. The epidermal cells are packed with the tough protein keratin and linked by strong desmosomes that give this epithelium its durability. Few infectious organisms can penetrate the intact skin. Bacteria and fungi colonize the surface, but their numbers are kept in check by its relative dryness, its slight acidity (pH 4–6), and defensive antimicrobial peptides called dermcidin and defensins. The protective acidic film is called the acid mantle.
- Other barrier functions. The skin is important as a barrier to water. It prevents the body from absorbing excess water when you are swimming or bathing, but even more importantly, it prevents the body from losing excess water. The epidermis is also a barrier to ultraviolet (UV) rays, blocking much of this cancer causing radiation from reaching deeper tissue layers; and it is a barrier to many potentially harmful chemicals. It is, however, permeable to several drugs and poisons.
- Vitamin D synthesis. The skin carries out the first step in the synthesis of vitamin D, which is needed for bone development and maintenance. The liver and kidneys complete the process.
- Sensation. The skin is our most extensive sense organ. It is equipped with a variety of nerve endings that react to heat, cold, touch, texture, pressure, vibration, and tissue injury. These sensory receptors are especially abundant on the face, palms, fingers, soles, nipples, and genitals. There are relatively few on the back and in skin overlying joints such as the knees and elbows.
- Thermoregulation. The skin receives 10 times as much blood flow as it needs for its own maintenance, and is richly supplied with nerve endings called thermoreceptors, which monitor the body surface temperature. All of this relates to its great importance in regulating body temperature. In response to chilling, the body retains heat by constricting blood vessels of the dermis (cutaneous vasoconstriction), keeping warm blood deeper in the body. In response to overheating, it loses excess heat by dilating those vessels (cutaneous vasodilation), allowing more blood to flow close to the surface and lose heat through the skin. If this is insufficient to restore normal temperature, sweat glands secrete perspiration. The evaporation of sweat can have a powerful cooling effect. Thus, the skin plays roles in both warming and cooling the body.
- Nonverbal communication. The skin is an important means of nonverbal communication. Humans, like most other primates, have much more expressive faces than other mammals. Complex skeletal muscles insert in the dermis and pull on the skin to create subtle and varied facial expressions. The general appearance of the skin, hair, and nails is also important to social acceptance and to a person’s self-image and emotional state—whether the ravages of adolescent acne, the presence of a birthmark or scar, or just a “bad hair day.”
The Epidermis
The epidermis is a keratinized stratified squamous epithelium. That is, its surface consists of dead cells packed with the tough protein keratin. Like other epithelia, the epidermis lacks blood vessels and depends on the diffusion of nutrients from the underlying connective tissue. It has sparse nerve endings for touch and pain, but most sensations of the skin are due to nerve endings in the dermis.
There are 5 cell types in the epidermis: stem cells, keratinocytes, melanocytes, Merkel cells (Tactile cells) and Dendritic cells (Langerhans cells).
Cells of the Epidermis
The epidermis is composed of five types of cells (Figure 2):
- Stem cells are undifferentiated cells that divide and give rise to the keratinocytes described next. They are found only in the deepest layer of the epidermis, called the stratum basale.
- Keratinocytes are the great majority of epidermal cells. They are named for their role in synthesizing keratin. In ordinary histological specimens, nearly all visible epidermal cells are keratinocytes.
- Melanocytes also occur only in the stratum basale, amid the stem cells and deepest keratinocytes. They synthesize the brown to black pigment melanin. They have branching processes that spread among the keratinocytes and continually shed melanin-containing fragments (melanosomes) from their tips. The keratinocytes phagocytize these and gather the melanin granules on the “sunny side” of their nucleus. Like a parasol, the dark granules shield the DNA from ultraviolet rays.
- Merkel cells (Tactile cells), relatively few in number, are receptors for touch. They, too, are found in the basal layer of the epidermis and are associated with an underlying dermal nerve fiber. The tactile cell and its nerve fiber are collectively called a tactile disc.
- Langerhans cells (Dendritic cells) are found in two layers of the epidermis called the stratum spinosum and stratum granulosum (described in the next section). They are immune cells that originate in the bone marrow but migrate to the epidermis and epithelia of the oral cavity, esophagus, and vagina. The epidermis has as many as 800 dendritic cells per square millimeter. They stand guard against toxins, microbes, and other pathogens that penetrate into the skin. When they detect such invaders, they alert the immune system so the body can defend itself.
Layers of the Epidermis
The epidermis of thick skin has five layers. Beginning at the basal lamina and traveling superficially toward the epithelial surface, we find the stratum basale, stratum spinosum, stratum granulosum, stratum lucidum, and stratum corneum. Refer to Figure 2 as we describe the layers in a section of thick skin.
Stratum Basale
The deepest epidermal layer is the stratum basale or stratum germinativum. This single layer of cells is firmly attached to the basal lamina, which separates the epidermis from the loose connective tissue of the adjacent dermis. Large stem cells, termed basal cells, dominate the stratum basale. As basal cells undergo mitosis, new keratinocytes are formed and move into the more superficial layers of the epidermis. This upward migration of cells replaces more superficial keratinocytes that are shed at the epithelial surface.
The brown tones of the skin result from the pigment-producing cells called melanocytes. Melanocytes are scattered among the basal cells of the stratum basale. They have numerous cytoplasmic processes that inject melanin—a black, yellow-brown, or brown pigment—into the basal cells in this layer and into the keratinocytes of more superficial layers. The ratio of melanocytes to stem cells ranges between 1:4 and 1:20 depending on the region examined. Melanocytes are most abundant in the cheeks, forehead, nipples, and genital region.
Differences in skin color result from varying levels of melanocyte activity, not varying numbers of melanocytes. Albinism is an inherited disorder characterized by deficient melanin production; individuals with this condition have a normal distribution of melanocytes, but the cells cannot produce melanin. It affects approximately one person in 10,000.
Skin surfaces that lack hair contain specialized epithelial cells known as Merkel cells (tactile cells). These cells are found among the cells of the stratum basale and are most abundant in skin where sensory perception is most acute, such as fingertips and lips. Merkel cells are sensitive to touch and, when compressed, release chemicals that stimulate sensory nerve endings, providing information about objects touching the skin. There are many other kinds of touch receptors,
but they are located in the dermis and will be introduced in later sections.
Stratum Spinosum
Each time a basal cell divides, one of the daughter cells is pushed into the next, more superficial layer, the stratum spinosum. The stratum spinosum is several cells thick. Each keratinocyte in the stratum spinosum contains bundles of protein filaments that extend from one side of the cell to the other. These bundles, called tonofibrils, begin and end at a desmosome (macula adherens) that connects the keratinocyte to its neighbors. The tonofibrils act as cross braces, strengthening and supporting the cell junctions. This interlocking network of desmosomes and tonofibrils ties all the cells in the stratum spinosum together.
The deepest cells within the stratum spinosum are mitotically active and continue to divide, making the epithelium thicker. Melanocytes are common in this layer, as are Langerhans cells (also termed dendritic cells). Langerhans cells, which account for 3–8 percent of the cells in the epidermis, are most common in the superficial portion of the stratum spinosum. These cells play an important role in triggering an immune response against epidermal cancer cells and pathogens that have penetrated the superficial layers of the epidermis.
Stratum Granulosum
Superficial to the stratum spinosum is the stratum granulosum (granular layer). This is the most superficial layer of the epidermis in which all the cells still possess a nucleus. The stratum granulosum consists of keratinocytes that have moved out of the stratum spinosum. By the time cells reach this layer, they have begun to manufacture large quantities of the proteins keratohyalin and keratin. Keratohyalin accumulates in electron dense keratohyalin granules. These granules form an intracellular matrix that surrounds the keratin filaments. Cells of this layer also contain membrane-bound granules that release their contents by exocytosis, which forms sheets of a lipid-rich substance that begins to coat the cells of the stratum granulosum. In more superficial layers, this substance forms a complete water resistant layer around the cells that protects the epidermis, but also prevents the diffusion of nutrients and wastes into and out of the cells. As a result, cells in the more superficial layers of the epidermis die.
Environmental factors often influence the rate at which keratinocytes synthesize keratohyalin and keratin. Increased friction against the skin, for example, stimulates increased synthesis, thickening the skin and forming a callus (also termed a clavus).
In humans, keratin forms the basic structural component of hair and nails. It is a very versatile material, however, and it also forms the claws of dogs and cats, the horns of cattle and rhinos, the feathers of birds, the scales of snakes, the baleen of whales, and a variety of other interesting epidermal structures.
Stratum Lucidum
The stratum lucidum is a thin zone superficial to the stratum granulosum, seen only in thick skin. Here, the keratinocytes are densely packed with a clear protein named eleidin. The cells have no nuclei or other organelles. This zone has a pale, featureless appearance with indistinct cell boundaries.
Stratum Corneum
The stratum corneum is the most superficial layer of both thick and thin skin. It consists of numerous layers of flattened, dead cells that possess a thickened plasma membrane. These dehydrated cells lack organelles and a nucleus, but still contain many keratin filaments. Because the interconnections established in the stratum spinosum remain intact, the cells of this layer are usually shed in large groups or sheets, rather than individually.
An epithelium containing large amounts of keratin is termed a keratinized or cornified epithelium.
Normally, the stratum corneum is relatively dry, which makes the surface unsuitable for the growth of many microorganisms. Maintenance of this barrier involves coating the surface with the secretions of sebaceous and sweat glands (discussed in a later section). The process of keratinization occurs everywhere on exposed skin surfaces except over the anterior surface of the eyes. Although the stratum corneum is water resistant, it is not waterproof. Water from the interstitial fluids slowly penetrates the surface and evaporates into the surrounding air. This process, called insensible perspiration, accounts for a loss of roughly 500 ml (about 1 pint) of water per day.
It takes 15–30 days for a cell to move superficially from the stratum basale to the stratum corneum. The dead cells in the exposed stratum corneum layer usually remain for two weeks before they are shed or washed away. Thus, the deeper portions of the epithelium—and all underlying tissues—are always protected by a barrier composed of dead, durable, and expendable cells.
The Life History of a Keratinocyte
Dead cells constantly flake off the skin surface. Because you constantly lose these epidermal cells, they must be continually replaced. Keratinocytes are produced deep in the epidermis by the mitosis of stem cells in the stratum basale. Some of the deepest keratinocytes in the stratum spinosum also continue dividing. Mitosis requires an abundant supply of oxygen and nutrients, which these deep cells acquire from the blood vessels in the nearby dermis.
Once the epidermal cells migrate more than two or three cells away from the dermis, their mitosis ceases. As new keratinocytes form, they push the older ones toward the surface. In 30 to 40 days, a keratinocyte makes its way to the surface and flakes off. This migration is slower in old age and faster in skin that has been injured or stressed. Injured epidermis regenerates more rapidly than any other tissue in the body. Mechanical stress from manual labor or tight shoes accelerates keratinocyte multiplication and results in calluses or corns, thick accumulations of dead keratinocytes on the hands or feet.
As keratinocytes are shoved upward by the dividing cells below, they flatten and produce more keratin filaments and lipid-filled membrane-coating vesicles. In the stratum granulosum, four important developments occur: (1) Keratohyalin granules release a protein called filaggrin that binds the cytoskeletal keratin filaments together into coarse, tough bundles. (2) The cells produce a tough layer of envelope proteins just beneath the plasma membrane, resulting in a nearly indestructible protein sac around the keratin bundles. (3) Membrane-coating vesicles release a lipid mixture that spreads out over the cell surface and waterproofs it. (4) Finally, as these barriers cut the keratinocytes off from the supply of nutrients from below, their organelles degenerate and the cells die, leaving just the tough waterproof sac enclosing coarse bundles of keratin. These processes, along with the tight junctions between keratinocytes, result in an epidermal water barrier that is crucial to the retention of body water.
Thin and Thick Skin
Most of the body is covered by thin skin, which has only four layers because the stratum lucidum is typically absent. In thin skin, the epidermis is a mere 0.08 mm thick and the stratum corneum is only a few cell layers deep. Thick skin, found only on the palms of the hands and soles of the feet, contains all five layers and may be covered by 30 or more layers of keratinized cells. As a result, the epidermis in these locations is up to six times thicker than the epidermis covering the general body surface.
Dermal Ridges
The stratum basale of the epidermis forms dermal ridges (also known as friction ridges) that extend into the dermis, increasing the area of contact between the two regions. Projections from the dermis toward the epidermis, called dermal papillae (singular, papilla), extend between adjacent ridges (Figure 1 and 2).
The contours of the skin surface follow the ridge patterns, which vary from small conical pegs (in thin skin) to the complex whorls seen on the thick skin of the palms and soles. Ridges on the palms and soles increase the surface area of the skin and promote friction, ensuring a secure grip. Ridge shapes are genetically determined: Those of each person are unique and do not change during a lifetime. Ridge patterns on the fingertips can therefore identify individuals.
The Dermis
Beneath the epidermis is a connective tissue layer, the dermis. It ranges from 0.2 mm thick in the eyelids to about 4 mm thick in the palms and soles. It is composed mainly of collagen, but also contains elastic and reticular fibers, fibroblasts, and the other cells typical of fibrous connective tissue. It is well supplied with blood vessels, cutaneous glands, and nerve endings. The hair follicles and nail roots are embedded in the dermis. In the face, skeletal muscles attach to dermal collagen fibers and produce such expressions as a smile, a wrinkle of the forehead, or the lifting of an eyebrow.
The boundary between the epidermis and dermis is histologically conspicuous and usually wavy. The upward waves are fingerlike extensions of the dermis called dermal papillae and the downward epidermal waves between the papillae are called epidermal ridges. The dermal and epidermal boundaries thus interlock like corrugated cardboard, an arrangement that resists slippage of the epidermis across the dermis. If you look closely at your hand and wrist, you will see delicate furrows that divide the skin into tiny rectangular to rhomboidal areas. The dermal papillae produce the raised areas between the furrows. On the fingertips, this wavy boundary forms the friction ridges that produce fingerprints. In highly sensitive areas such as the lips and genitals, exceptionally tall dermal papillae allow blood capillaries and nerve fibers to reach close to the surface. This imparts a redder color and more sensitivity to touch in such areas.
There are two zones of dermis called the papillary and reticular layers:
- The papillary layer is a thin zone of areolar tissue in and near the dermal papillae. This loosely organized tissue allows for mobility of leukocytes and other defenses against organisms introduced through breaks in the epidermis. This layer is especially rich in small blood vessels. The reticular layer of the dermis is deeper and much thicker. It consists of dense irregular connective tissue. The boundary between the papillary and reticular layers is often vague.
- In the reticular layer, the collagen forms thicker bundles with less room for ground substance, and there are often small clusters of adipocytes. Stretching of the skin in obesity and pregnancy can tear the collagen fibers and produce striae or stretch marks. These occur especially in areas most stretched by weight gain: the thighs, buttocks, abdomen, and breasts.
There are extensive plexuses of blood vessels at the dermal–epidermal boundary, in mid-dermis, and between the dermis and hypodermis. When dermal blood vessels are damaged by such causes as burns and friction from tight shoes, serous fluid can seep out of the vessels and accumulate as a blister, separating the epidermis from the dermis until the fluid is either reabsorbed or expelled by rupture of the blister.
The Hypodermis
Beneath the skin is a layer called the hypodermis9 or subcutaneous tissue. The boundary between the dermis and hypodermis is indistinct, but the hypodermis generally has more areolar and adipose tissue. It pads the body and binds the skin to the underlying tissues. Drugs are introduced into the hypodermis by injection because the subcutaneous tissue is highly vascular and absorbs them quickly.
Subcutaneous fat is hypodermis composed predominantly of adipose tissue. It serves as an energy reservoir and thermal insulation. It is not uniformly distributed; for example, it is virtually absent from the scalp but relatively abundant in the abdomen, hips, thighs, and female breasts. The subcutaneous fat averages about 8% thicker in women than in men, and varies with age. Infants and elderly people have less subcutaneous fat than other people and are therefore more sensitive to cold.
Skin Color
The color of the epidermis is due to a combination of factors: circulation in the dermis and variable quantities of two epidermal pigments, carotene and melanin.
Dermal Blood Supply
Blood contains red blood cells that carry the protein hemoglobin. When hemoglobin is bound to oxygen, it has a bright red color, giving blood vessels in the dermis a reddish tint that is most visible in fair-skinned people. When those vessels dilate, as during inflammation, the red tones become much more pronounced.
When circulation in the dermis is temporarily reduced, the skin becomes relatively pale. A frightened Caucasian may “turn white” because of a sudden drop in blood flow to the skin. During a sustained reduction in oxygen content in the blood, hemoglobin becomes a darker red. Seen from the surface, the skin takes on a bluish coloration called cyanosis. In people of any skin color, cyanosis is most apparent in areas of thin skin, such as the lips or beneath the nails. It can be a response to extreme cold or the result of circulatory or respiratory disorders, such as heart failure or severe asthma.
Epidermal Pigments
Two pigments determine skin color: carotene and melanin.
Carotene is an orange-yellow pigment also found in various orange- or yellow-colored vegetables, such as carrots, corn, and squashes. It can be converted to vitamin A, which is required for epithelial maintenance and the synthesis of photoreceptor pigments in the eye. Carotene normally accumulates in the subcutaneous fat as well as inside keratinocytes, becoming especially evident in the dehydrated cells of the stratum corneum.
Melanin is produced and stored in melanocytes of thin skin, and the amount produced is genetically determined. The black, yellow-brown, or brown melanin forms in intracellular vesicles called melanosomes. These vesicles, which are transferred to keratinocytes, color the keratinocytes temporarily, until lysosomes destroy the melanosomes. As a result, the cells in more superficial layers of the epidermis have less melanin, and therefore are lighter in color, than cells within the deeper layers of the epithelium. In light-skinned individuals, melanosome transfer occurs in the stratum basale and stratum spinosum, and the cells of more superficial layers lose their pigmentation. In dark-skinned individuals, the melanosomes are larger and the transfer may occur in the stratum granulosum as well, making the pigmentation darker and more persistent.
Little or no melanin is produced in the thick skin of the palms of the hands and soles of the feet. Melanin produced in thick skin is difficult to see because of the thickness of the stratum corneum.
Melanin pigments help protect the underlying dermis and also prevent skin damage by absorbing ultraviolet (UV) radiation in sunlight. A little ultraviolet radiation is necessary because the skin requires it to form vitamin D. The small intestine needs vitamin D to absorb calcium and phosphorus; inadequate vitamin D impairs bone maintenance and growth. However, too much UV radiation may damage chromosomes and cause widespread tissue damage similar to that caused by mild to moderate burns.
Within each keratinocyte, the melanosomes are most abundant around the cell’s nucleus, helping absorb the UV radiation before it can damage the nuclear DNA. Melanocytes respond to UV exposure by synthesizing and transferring more melanin. The skin “tans,” but this response is not quick enough to prevent a sunburn on the first day at the beach; it takes about 10 days. Anyone can get a sunburn, but dark-skinned individuals have greater initial protection against the effects of UV radiation. Repeated UV exposure sufficient to stimulate tanning will result in long-term skin damage in the dermis and epidermis. In the dermis, damage to fibrocytes causes abnormal connective tissue structure and premature wrinkling. In the epidermis, chromosomal damage in basal cells or melanocytes can lead to skin cancer.
Blood Supply to the Skin
Arteries and veins supplying the skin form an interconnected network at the junction between the reticular layer of the dermis and the subcutaneous layer. This network is called the cutaneous plexus. Branches of the arteries supply the adipose tissue of the subcutaneous layer as well as more superficial tissues of the skin. As small arteries travel toward the epidermis, branches supply the hair follicles, sweat glands, and other structures in the dermis.
Upon reaching the papillary layer, these small arteries enter another branching network, the subpapillary plexus. From there, capillary loops follow the contours of the epidermal–dermal boundary. These capillaries empty into a network of delicate veins that rejoin the papillary plexus. From there, larger veins drain into a network of veins in the deeper cutaneous plexus. Circulation to the skin must be tightly regulated. Skin plays a key role in thermoregulation, the control of body temperature. When body temperature increases, increased circulation to the skin permits the loss of excess heat. When body temperature decreases, reduced circulation to the skin promotes retention of body heat.
Total blood volume in the body is relatively constant. Thus, increased blood flow to the skin means a decreased blood flow to some other organ(s). The nervous, cardiovascular, and endocrine systems interact to regulate blood flow to the skin while maintaining adequate blood flow to other organs and systems.
Nerve Supply to the Skin
Nerve fibers in the skin control blood flow, adjust gland secretion rates, and monitor sensory receptors in the dermis and the deeper layers of the epidermis – the presence of Merkel cells in the deeper layers of the epidermis. These cells are touch receptors monitored by sensory nerve endings known as tactile discs. The epidermis also contains sensory nerves that are believed to respond to pain and temperature. The dermis contains similar receptors as well as other, more specialized receptors.