Contents
What is the soft palate
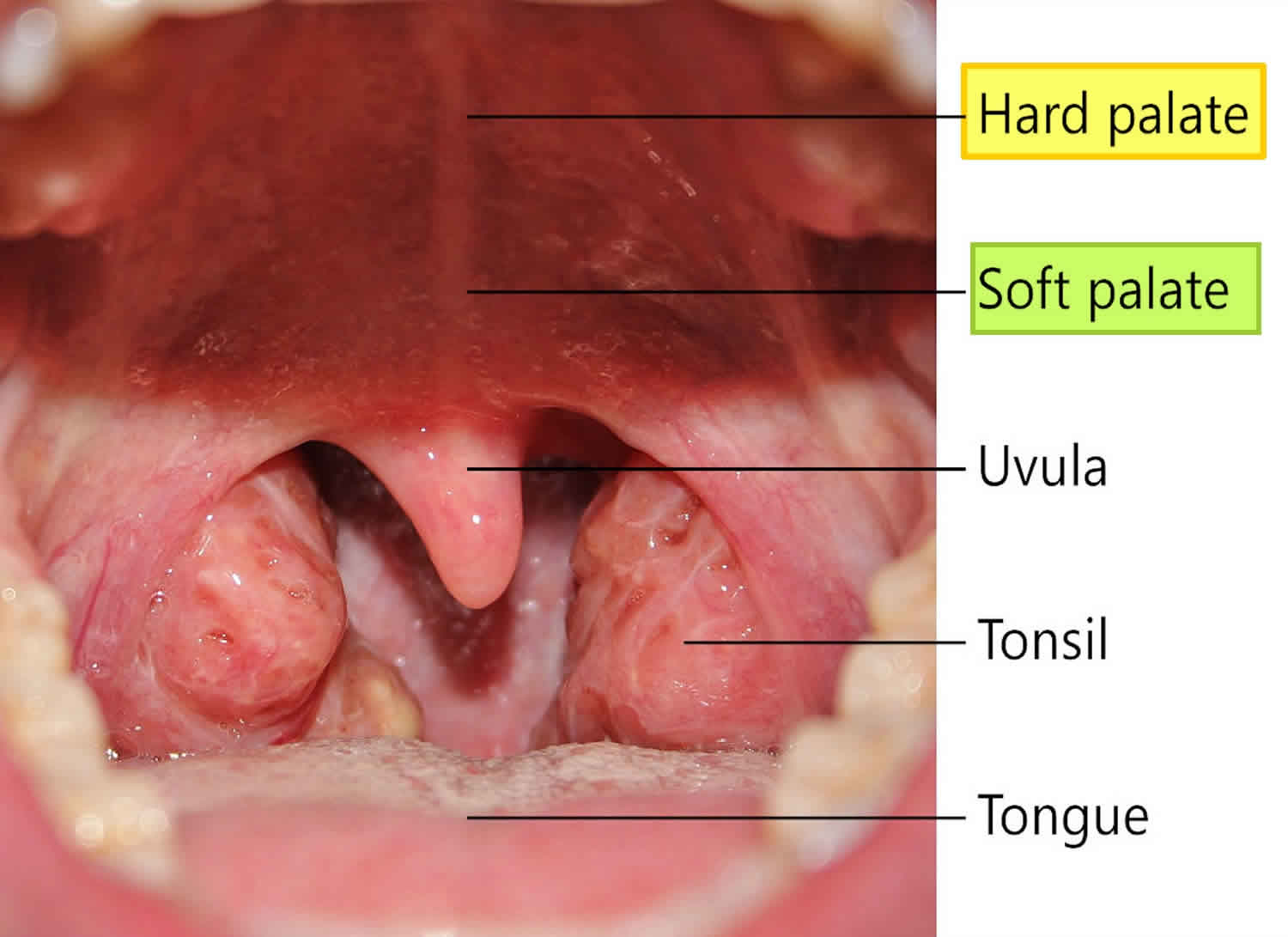
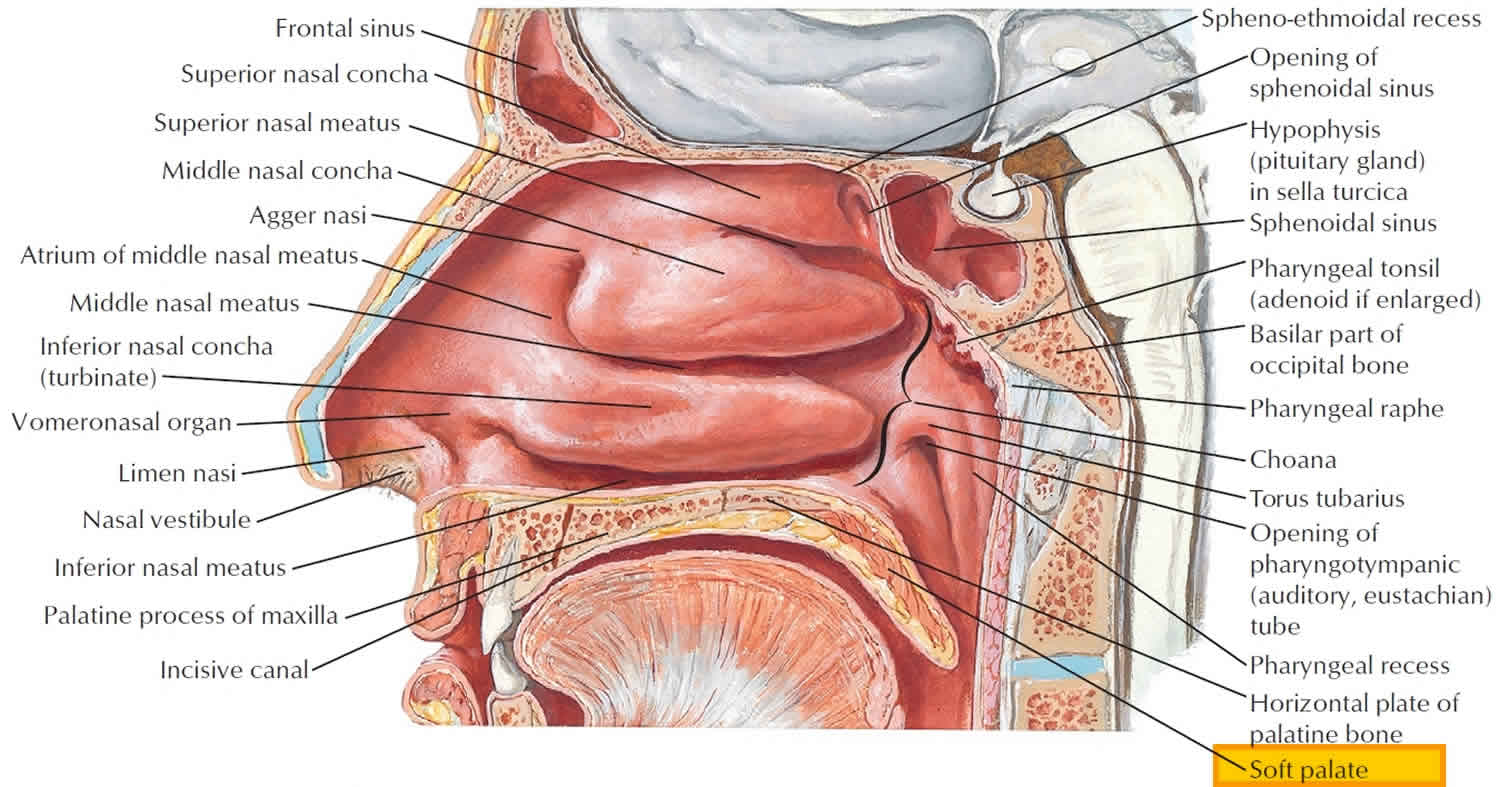
The palate forms the roof of the mouth and floor of the nasal cavity. The palate is divided anatomically into the bony hard palate anteriorly (part of the oral cavity) and the fleshy soft palate posteriorly (part of the oropharynx). The soft palate projects into the cavity of the pharynx from its attachment to the posterior edge of the hard palate. When elevated, it separates the oropharynx from the nasopharynx. Five paired muscles attach to the soft palate and contribute to its structure. In the midline the uvula projects downwards from its posterior free border.
Figure 1. Soft palate anatomy
Soft palate anatomy
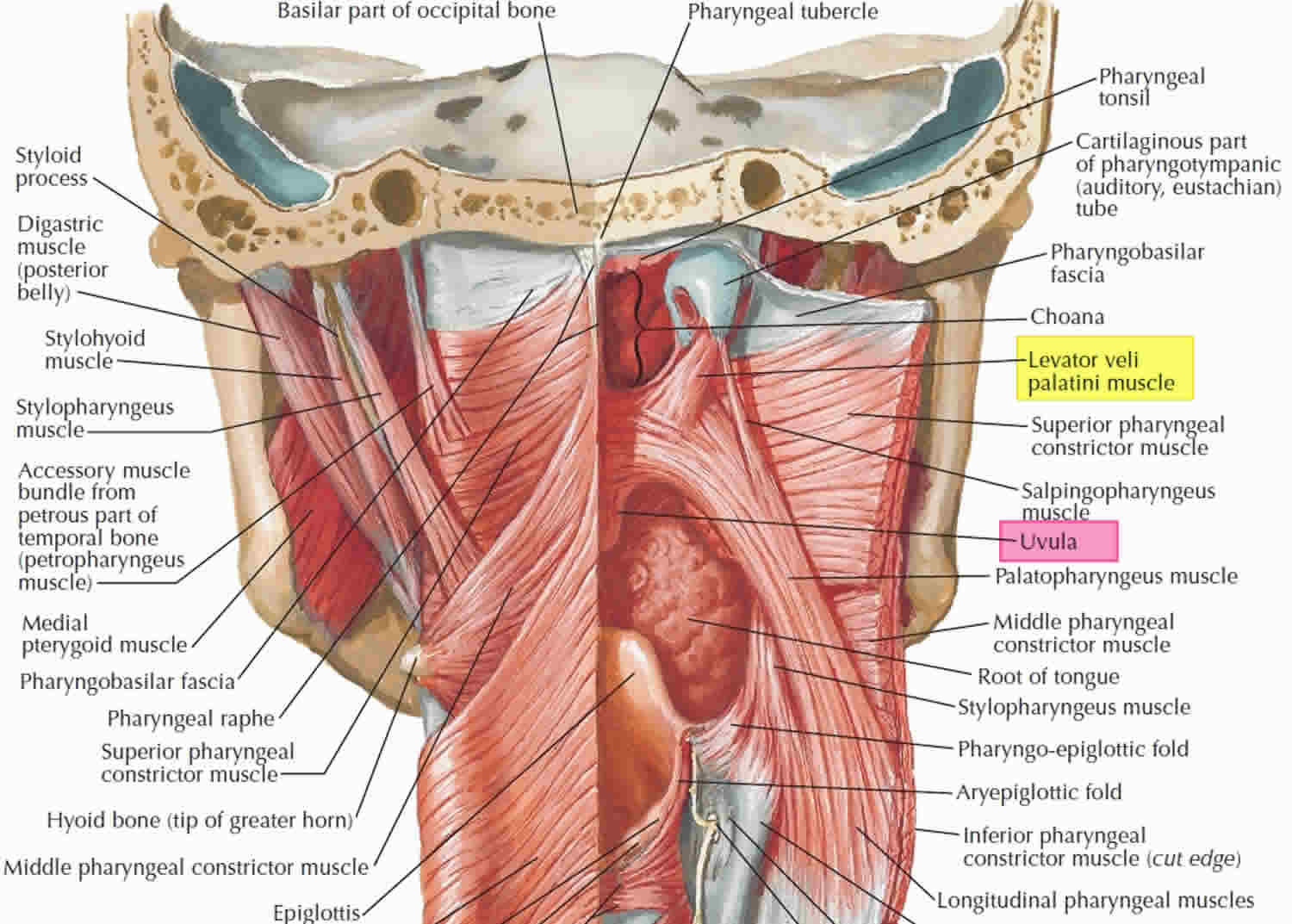
Muscles of the soft palate – the tensor veli palatini (Figure 2) attaches to the scaphoid fossa and spine of the sphenoid and to the lateral surface of the cartilaginous portion of the auditory (Eustachian) tube. Its fibers descend between the lateral and medial pterygoid plates on the lateral aspect of the pharyngeal wall and give way to a tendon just above the pterygoid hamulus. The tendon hooks under the hamulus and turns medially to enter the soft palate, where it forms the palatine aponeurosis by fanning out and attaching to the posterior border of the hard palate. The palatine aponeurosis forms the basic structure of the soft palate to which other muscles gain attachment. Tensor veli palatini is supplied by the mandibular (V3) division of the trigeminal nerve and tenses the soft palate.
Levator veli palatini attaches to the inferior surface of the petrous temporal bone just medial to the opening of the auditory tube and to the adjacent part of the tube. Its fibers descend medial to the medial pterygoid plate within the pharynx and attach to the upper surface of the palatine aponeurosis. The muscle is innervated by the pharyngeal plexus. Levator veli palatini elevates the soft palate during swallowing, preventing regurgitation of food into the nasal cavities.
Palatoglossus descends from the inferior surface of the palatine aponeurosis and inclines slightly forwards to enter the posterolateral part of the tongue. The position of palatoglossus is evident on the inner surface of the oral cavity as a mucosal elevation, the palatoglossal ridge (anterior pillar of the fauces). The two palatoglossal ridges form the oropharyngeal isthmus, which marks the posterior boundary of the oral cavity. Innervated by fibers from the pharyngeal plexus, palatoglossus lowers the soft palate, raises the posterior part of the tongue and moves the palatoglossal ridge towards the midline, thus narrowing the isthmus.
Palatopharyngeus attaches to the undersurface of the soft palate. Most of its fibres run posteroinferiorly as part of the longitudinal layer of muscle inside the pharynx and form the palatopharyngeal ridge (posterior pillar of the fauces). On contraction, these fibres depress the soft palate. Other fibres pass horizontally backwards, raising the mucosa into a ridge, against which the soft palate is elevated. Palatopharyngeus receives its motor supply from the pharyngeal plexus.
The uvular muscle, also supplied by the pharyngeal plexus, lies entirely within the soft palate and elevates the uvula. In cases of unilateral paralysis of the soft palate, the uvula rises asymmetrically, being pulled away from the paralyzed side.
Sensory and secretomotor innervation to the soft palate is from the lesser palatine nerves of the maxillary (V2) division of the trigeminal nerve, supplemented laterally on the undersurface of the palate by the glossopharyngeal (IX or 9th cranial nerve) nerve.
Figure 2. Muscles of the soft palate
Soft palate function
The hard and soft palates separate the oral cavity from the nasal cavity. The combination of the two palates also helps humans breathe and chew simultaneously. That’s because the passage remains open when a person is not swallowing food, thus allowing him to breathe through the mouth and nose. However, the soft palate moves upward and blocks off the entrance to the back nasal passage when a person is swallowing food, preventing regurgitation of food into the nasal cavities.
Swallowing mechanism
Swallowing has three stages. In the first stage, which is voluntary, food is chewed and mixed with saliva. Then the tongue rolls this mixture into a mass, or bolus, and forces it into the oropharynx.
The second stage of swallowing begins as food reaches the oropharynx and stimulates sensory receptors around the pharyngeal opening. This triggers the swallowing reflex, which includes the following actions:
- The soft palate (including the uvula) rises, preventing food from entering the nasal cavity.
- The hyoid bone and the larynx are elevated. A flaplike structure attached to the larynx, called the epiglottis, closes off the top of the larynx so that food is less likely to enter the trachea.
- The tongue is pressed against the soft palate, sealing off the oral cavity from the nasopharynx.
- The longitudinal muscles in the pharyngeal wall contract, pulling the pharynx upward toward the food.
- Muscles in the laryngopharynx relax, opening the esophagus.
- A peristaltic wave begins in the pharyngeal muscles and forces food into the esophagus.
The swallowing reflex momentarily inhibits breathing. Then, during the third stage of swallowing, peristalsis transports the food in the esophagus to the stomach.
Soft palate problems
Snoring and Obstructive Sleep Apnea
Nearly half of adults snore, and over 25 percent are habitual snorers. Problem snoring and sleeping disorders are more frequent in males and people who are overweight, and usually worsens with age.
The noisy sounds of snoring occur when there is a partial obstruction to the flow of air through the passages at the back of the mouth and nose. This area is the collapsible part of the airway where the tongue and upper throat meet the soft palate and uvula. Snoring occurs when these structures strike each other and vibrate during breathing. Apnea occurs when the obstruction of air flow is more severe, leading to reduced, compromised, or completely blocked air flow while trying to breathe.
In children, snoring may be a sign of problems with the tonsils and adenoids. In adults, the site of obstruction may not be as simple to identify. Obstruction in an adult may be due to a combination of factors in different areas, making it more challenging to identify and treat.
Snoring is bothersome to others, but it can also be a sign of a more serious condition known as obstructive sleep apnea (OSA), which is present in one out of five Americansin the general population. Obstructive sleep apnea (OSA) is a serious health condition characterized by multiple stopping in breathing greater than 10 seconds at a time or slowing of breathing due to upper airway narrowing or collapse. This lowers the amount of oxygen in the blood, and causes the heart to work harder. This can occur hundreds of times while you sleep, reducing your quality of sleep and making you feel tired during the day, which decreases your performance. Untreated obstructive sleep apnea (OSA) can contribute to high blood pressure, stroke, heart disease, workplace or motor vehicle accidents, and significant loss of productivity.
Medical and surgical options are available for the management of snoring and obstructive sleep apnea. Medical options include continuous positive airway pressure (CPAP) treatment, oral appliance therapy, positional therapy, and weight loss. Treatment effectiveness depends on how long and how consistently you follow your doctor’s plan. When medical management is inadequate, well-selected surgical procedures can help reduce the severity of the disorder, support medical therapy, or even lead to a cure.
Other factors that contribute to snoring and sleep apnea
Poor muscle tone in the tongue and throat—When muscles are too relaxed, the tongue falls backward into the airway, or the throat muscles draw in from the sides into the airway. Alcohol or drugs that cause sleepiness may worsen muscle relaxation and obstruction.
Excessive bulkiness of throat tissue
Children with large tonsils and adenoids often snore. Overweight people may have excess soft tissue in the neck that can lead to airway narrowing. Those with very large tongues are especially susceptible to snoring and obstructive sleep apnea (OSA). Cysts or tumors are rare causes of airway narrowing.
Long soft palate and/or uvula
A long palate narrows the opening from the nose into the throat. The excessive length of the soft palate and/or uvula acts as a noisy flutter valve during relaxed breathing.
Obstructed nasal airways
A stuffy nose requires extra effort to pull air through it. This creates an exaggerated vacuum in the throat that pulls together the floppy tissues of the throat. Sometimes, snoring only occurs during allergy season or with a cold or sinus infection. Deformities of the nose or nasal septum, such as a deviated septum (a deformity of the wall that separates one nostril from the other) can also cause snoring and obstructive sleep apnea (OSA).
Symptoms of obstructive sleep apnea
Symptoms associated with obstructive sleep apnea can include:
- Loud snoring
- Pauses in breathing during sleep
- Waking up gasping or choking
- Waking up with a dry mouth or sore throat
- Daytime sleepiness or fatigue
- Frequent nighttime urination
- Morning headache
- Irritability, mood changes, depression, difficulty concentrating
- High blood pressure, heart disease, stroke, or other cardiac issues
Obstructive sleep apnea treatment options
Heavy snorers—people who snore constantly in any position or who negatively impact a bed partner’s sleep—should seek medical advice to ensure that sleep apnea is not a problem. An ENT (ear, nose, and throat) specialist, or otolaryngologist, will provide a thorough examination of the nose, mouth, throat, palate, and neck, often using a fiberoptic scope. An examination can reveal if the snoring is caused by nasal allergy, infection, nasal obstruction, or enlargement of tonsils and adenoids. A sleep study in a laboratory or at home may be necessary to determine if snoring is due to obstructive sleep apnea.
Obstructive sleep apnea is most often treated with a device that opens the airway with a small amount of positive pressure. This pressure is delivered by an appliance through either the nose and/or mouth that is worn during sleep. This treatment is called continuous positive airway pressure, or CPAP, and it is currently the initial treatment of choice for patients with obstructive sleep apnea. The challenge of treating obstructive sleep apnea is that obstruction can occur at multiple levels of the airway. CPAP (continuous positive airway pressure) stabilizes pressure at all parts of the upper airway and can be very effective, but some wearers cannot tolerate CPAP (continuous positive airway pressure) and must seek other options.
A custom-fit oral appliance, which repositions the lower jaw forward, may also be considered for certain patients with snoring/obstructive sleep apnea. This should be fitted by an ENT specialist, dentist, or oral surgeon with expertise in sleep dentistry. In some patients, significant weight loss can also improve snoring and obstructive sleep apnea.
There are numerous surgical treatments for snoring/obstructive sleep apnea, including:
- Uvulopalatopharyngoplasty is a common surgery for treating snoring and obstructive sleep apnea. It removes the uvula along with excess soft palate tissue and opens the airway. In addition, the remaining tissue stiffens as it heals, helping to minimize tissue vibration. In children and some adults who have obstructive sleep apnea (OSA) with enlarged tonsils and/or adenoids, a tonsillectomy and/or adenoidectomy can resolve snoring, sleep apnea, and associated symptoms.
- Thermal ablation procedures reduce tissue bulk in the nasal turbinates (structures on the side wall of the inside of the nose), tongue base, and/or soft palate. These procedures are used for both snoring and obstructive sleep apnea, and several treatments may be required.
- The soft palate may be stiffened by inserting stiffening rods into the soft palate, or by injecting an irritating substance that causes stiffness in the injected area near the uvula.
- “Hypoglossal nerve stimulator” technology implants a tongue pacemaker, which stiffens and projects the tongue forward during sleep. Other procedures may be used to surgically target tongue muscles or the boney configuration of the midface. As with palate surgery, these procedures are patient-specific depending on the nature of your airway, and can be assessed during an airway endoscopy.
- Maxillomandibular advancement – Since airway muscles are supported by the jaw, the orientation or position of the jaw bones affect the opening and stability of the airway during sleep. Patients with complete upper airway collapse during sleep, or a retracted jaw position, may benefit from a “maxillomandibular advancement” surgical procedure. If the problem is limited to the upper jaw, where it is too narrow for the tongue and soft palate, the upper jaw can be widened in both children and adults. When maxillomandibular advancement is performed properly, it provides a reliable and high surgical success rate. Current techniques allow patients to quickly return to regular chewing function. Patients may also benefit from improved bite—how their teeth come together—and facial balance. It is highly recommended that these procedures be performed by an experienced surgeon for optimal results, so patients can return to their normal function usually within two to three weeks.
Soft palate cancer
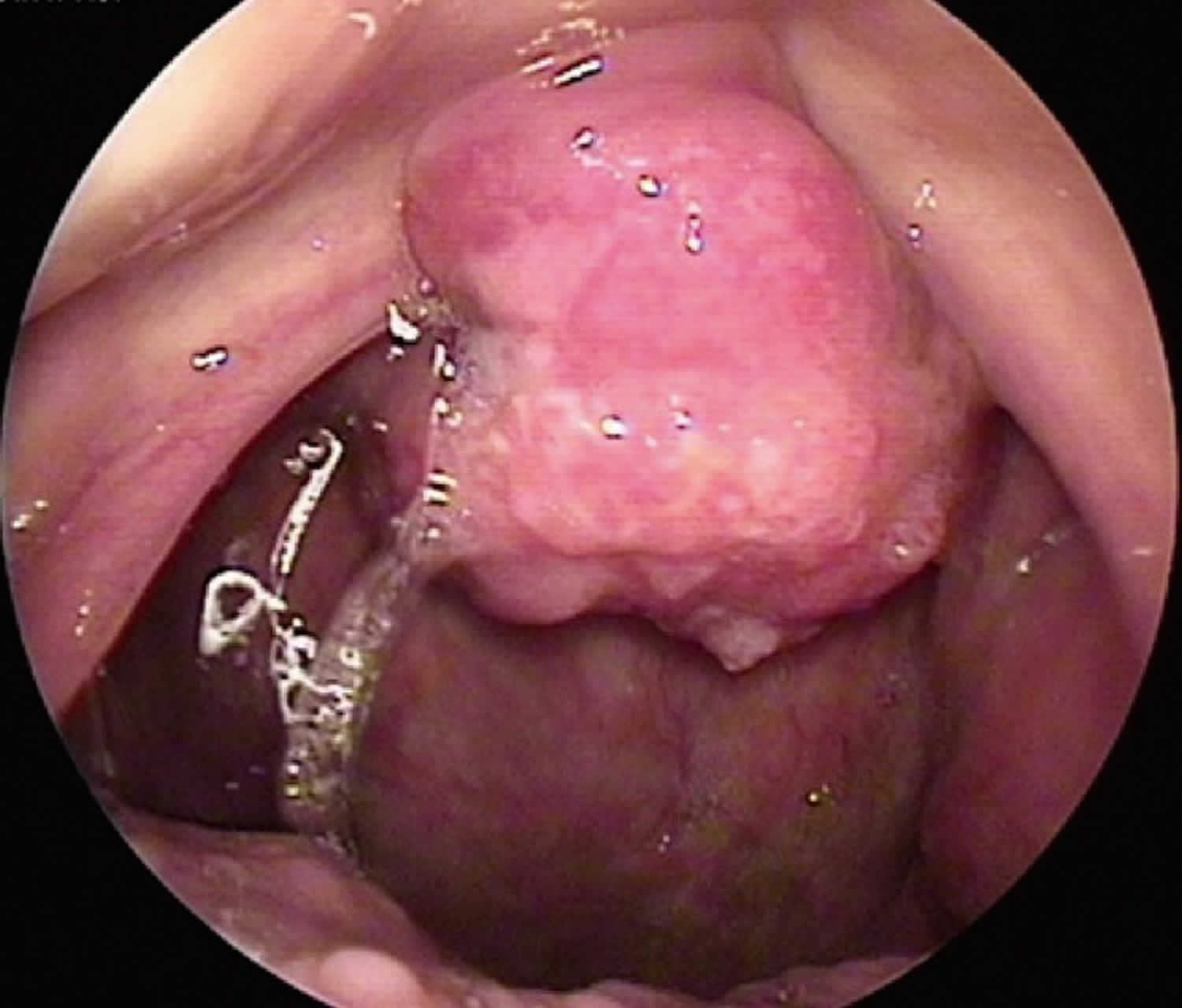
Squamous cell carcinoma very rarely occurs at the soft palate 1, 2. Squamous cell carcinoma (SCC) of the soft palate has clinical symptoms such as dysphagia, pain, awareness of a neck mass, and intraoral bleeding. Squamous cell carcinoma (SCC) of the soft palate can be easily found because it is mainly positioned at the anterior part of the oropharynx. A histologic examination can be conducted in the clinic. In cases of early soft palate cancer, it can be cured using surgical treatment and radiotherapy. At the same time, in advanced cases, surgical resection, supportive radiotherapy, and additional chemotherapy can be applied.
Oropharyngeal cancer accounts for approximately 12% of all head and neck cancers, and that squamous cell carcinoma accounts for more than 90% of cancers that occur in the oropharynx 1. Squamous cell carcinoma (SCC) occurs most frequently at the peritonsillar area, followed by the tongue base, soft palate, and oropharyngeal wall in that order 3. Squamous cell carcinoma rarely occurs at the soft palate and uvula, but in most cases of soft palate cancer, if it is diagnosed early, it can be cured using surgical resection and radiotherapy 4. In the case of a surgical treatment of a lesion that invades the muscle of the soft palate, metastasis may increase and serious functional complications may occur after resection. Thus, radiotherapy is the preferred treatment 3. However, considering the possible long-term side defects caused by radiation therapy and good reconstructive options with a positive functional outcome, surgery might be preferred. In principle, a combined treatment of surgical resection and postoperative radiotherapy is another treatment option for soft palate cancer in the advanced stage 4.
The soft palatal area is a dynamic muscular structure, which effectively separates the pathway of the oral and nasal cavities. Soft palate defects that occur after resection may cause hypernasal speech and food reflux into the nose upon swallowing. Thus, functional mucomuscular soft palate structure and oronasal obstruction are the goals of reconstruction of the palate 4.
To overcome language impairment and dysphagia that occurs after surgical resection of a soft palate, which has various functions, surgical reconstruction with various prostheses has been conducted. Reconstruction with a prosthesis is relatively easy, but results in decreased functional recovery and patient compliance 3. For surgical reconstruction, various reconstruction methods are used such as uvulopalatal flap 5, buccal mucosal flap 6, and radial forearm free flap 7, but they all result in donor site complications and unsatisfactory functional outcomes.
Prostheses and surgical reconstruction are used for the functional reconstruction of the soft palate. Although reconstruction with a prosthesis is relatively easy to perform, it decreases function and patient compliance, and the procedure is difficult to perform in patients with a large defect or without teeth 3.
Among the surgical reconstructions available, superior constrictor advancement-rotation flap reconstructs the valvular sphincteric function by incising the opposite tonsillar pillar and rotating the velopharyngeal area for the circumferential closure. The procedure can be used in 35% to 65% of soft palate defect cases, but it is restricted for large defects of the soft palate, tonsil, and marginal pharyngeal wall 8.
Radial forearm free flap is most frequently used among soft palate reconstructions using free flap. It can be applied without the limitation of defect size, but has disadvantages of requiring a longer operation time, the addition of skin transplantation to the donor site, and sacrificing the radial artery 9.
Gangloff et al. 10 reported that hypo-hyoid myocutaneous flap was performed in order to reconstruct small or intermediate soft palate defects, and that its use was limited if patients had previously undergone thyroid surgery or radical neck dissection.
Pharyngeal flap is commonly used for velopharyngeal insufficiency. Satisfactory speech and swallowing results can be obtained after surgery. Superiorly based posterior pharyngeal flap can be designed as a pharyngeal flap with a sufficient length and can be used in all age groups 11. However, it may be difficult to apply a pharyngeal flap if the lateral wall movement of the pharynx is weak. Pharyngeal flap was applied in this study because the lateral wall movement of the pharynx was normal in the two patients. The defect of the oral cavity was reconstructed by posteriorly extending the soft palatal area that remained after resection using mucomuscular flap, and the defect of the nasal cavity was reconstructed using superiorly based pharyngeal flap. The adjacent tissue using the remaining soft palatal area and posterior wall of the pharynx was used in this study, and this method had the advantages of decreased impairment of the donor site, only requiring a single operation, and short hospitalization. Furthermore, a satisfactory result was obtained for swallowing. Therefore, this method is a good reconstructive option for soft palate defects of small to moderate size.
A limitation of this method is that it is difficult to perform in a large soft palate defect. Thus, in the cases of large soft palate defects or defects requiring resection of other areas, a free flap or the additional use of other flaps would be required 1.
Figure 3. Soft palate cancer
[Source 1 ]- Kim JS, Jo HJ, Kim NG, Lee KS. Soft palate reconstruction using bilateral palatal mucomuscular flap and pharyngeal flap after resection of squamous cell carcinoma. Arch Plast Surg. 2012;39(6):655-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3518011/[↩][↩][↩][↩]
- Kim CL, Cho KS, Kim KY, et al. Squamous cell carcinoma of the soft palate and uvula. J Korean Assoc Maxillofac Plast Reconstr Surg. 1996;18:673–678.[↩]
- Kim YM. Malignant neoplasms of the oropharynx. In: Na KS, editor. Otolaryngology-head and neck surgery. 2nd ed. Seoul: Iljogak; 2009. pp. 1624–1644.[↩][↩][↩][↩]
- Harreus U. Malignant neoplasms of the oropharynx. In: Flint PW, Haughey BH, Lund VJ, et al., editors. Cummings otolaryngology-head and neck surgery. 5th ed. Philadelphia: Mosby; 2010. pp. 1365–1368.[↩][↩][↩]
- Gillespie MB, Eisele DW. The uvulopalatal flap for reconstruction of the soft palate. Laryngoscope. 2000;110:612–615[↩]
- Tezel E. Buccal mucosal flaps: a review. Plast Reconstr Surg. 2002;109:735–741.[↩]
- Lacombe V, Blackwell KE. Radial forearm free flap for soft palate reconstruction. Arch Facial Plast Surg. 1999;1:130–132.[↩]
- Zeitels SM, Kim J. Soft-palate reconstruction with a “SCARF” superior-constrictor advancement-rotation flap. Laryngoscope. 1998;108:1136–1140.[↩]
- Kim UK, Lee SH, Hwang DS, et al. Clinical review of soft tissue reconstructive methods on intraoral defects. J Korean Assoc Maxillofac Plast Reconstr Surg. 2007;29:527–537.[↩]
- Gangloff P, Deganello A, Lacave ML, et al. Use of the infra hyoid musculo-cutaneous flap in soft palate reconstruction. Eur J Surg Oncol. 2006;32:1165–1169[↩]
- Seyfer AE, Prohazka D, Leahy E. The effectiveness of the superiorly based pharyngeal flap in relation to the type of palatal defect and timing of the operation. Plast Reconstr Surg. 1988;82:760–764.[↩]