Contents
What causes testicle pain
Testicle pain is also called testicular pain, is pain that occurs in or around one or both testicles. Sometimes testicle pain actually originates from somewhere else in the groin or abdomen, and is felt in one or both testicles (known as referred pain).
Testicle pain has a number of possible causes. The testicles are very sensitive, and even a minor injury can cause testicle pain or discomfort. Testicle pain might arise from within the testicle itself or from the coiled tube and supporting tissue behind the testicle (epididymis).
Sometimes, what seems to be testicle pain is caused by a problem that starts in the groin, abdomen or somewhere else — for example, kidney stones and some hernias can cause testicle pain. The cause of testicle pain can’t always be identified.
Causes of testicle pain or pain in the testicle area can include:
- Acute appendicitis can cause left- or right-sided testicular and inguinal pain as purulent material spreads to the dependent portions of the inguinal canal 1. Abdominal pain is associated with the testicular pain. The testicle may be drawn up into the scrotum. This more commonly occurs with torsion or epididymo-orchitis.
- Cremasteric spasm is of unknown cause. It can be treated by excision of the cremasteric muscle and interruption of the genital branch of the genitofemoral nerve 1.
- Diabetic neuropathy (nerve damage caused by diabetes)
- Drug side effect, such as certain antibiotics and chemotherapy drugs. The most frequent cause of drug-related testicular pain is mazindol, a drug used to promote weight reduction 1. In some individuals, it can cause sexual dysfunction and testicular pain which resolve on stopping the drug and recur when the patient is challenged again with the drug.
- Epididymitis (testicle inflammation)
- Gangrene (specifically, a type of gangrene called Fournier’s gangrene)
- Genitofemoral neuralgia causes intermittent or constant inguinal, testicular, and upper medial thigh pain. The pain is increased by walking, stooping, or extension of the hips and is decreased by hip flexion and bed rest 1. The inguinal canal may be tender. Neuralgia results from nerve entrapment following appendectomy or a hernia repair. Neurectomy of the genitofemoral nerve within the abdomen brings relief. Bilateral involvement may occur. Some cases are idiopathic.
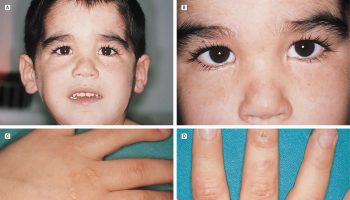
- Henoch-Schonlein purpura (blood vessel inflammation)
- Hydrocele (fluid buildup that causes swelling of the scrotum)
- Idiopathic testicular pain (unknown cause)
- Ilioinguinal neuralgia causes inguinal, testicular, and low back pain. Tenderness occurs medial to the anterosuperior iliac spine. There is limitation of internal rotation of the hips and extension. Hypesthesia may occur in the inguinal area. Nerve blocks may relieve the pain.
- Inguinal hernia. A small incarcerated inguinal hernia can cause inguinal and testicular pain by compression of the genital branch of the genitofemoral nerve 1.
- Kidney stones. Ureterolithiasis may present with hematuria, flank and lower abdominal pain, testicular pain, and a positive intravenous pyelogram 1. Microscopic hematuria is more common than gross hematuria. Such stones usually pass down the ureter and out in the urine, since testicular pain occurs with stones in the lower ureter.
- Iliac artery aneurysm may be associated with inguinal and testicular pain and a pulsatile unilateral lower abdominal mass 1.
- Leukemia. Testicular involvement by leukemia causes bilateral enlargement and sometimes pain and tenderness. Six to 36% of leukemic patients have clinical evidence of testicular disease. Hepatic, splenic, and nodal involvement are frequent associated findings. In one series of acute lymphoblastic leukemia, the clinical incidence of testicular involvement was 9% 1.
- Lyme arthritis follows a tick bite that causes infection with Borrelia burgdorferi, a spirochetal organism 1. Fever, disabling arthritis, and a distinctive skin rash characterize this disorder, which now occurs in many geographic regions in the United States.
- Mumps
- Nodular fibrositis causes low back pain relieved by injection of the subcutaneous mobile nodule with lidocaine and methylprednisolone. Rarely, palpation of such a nodule can reproduce testicular pain.
- Orchitis (inflamed testicle)
- Polyarteritis nodosa very rarely may present with bilateral testicular pain and tenderness as well as testicular induration 1. Biopsy of a tender indurated area may reveal the diagnosis in 80 to 90% of cases. Only 2 to 18% of patients with this disorder have orchialgia, while biopsies in 36 to 86% of testes in patients with polyarteritis nodosa are abnormal.
- Prostatitis (infection or inflammation of the prostate). Prostatitis causes urinary frequency, urgency, penile discomfort, dysuria, and perineal and testicular aching as well as lower abdominal pain 1. The diagnosis can be made by examination of the first ounce of a voided early morning urine or by massage of the prostate to obtain prostatic fluid. The latter procedure should be avoided in acute prostatitis because of the possibility of producing bacteremia.
- Scrotal masses
- Spermatocele (fluid buildup in the testicle)
- Testicular abscess can complicate epididymo-orchitis or torsion and requires surgical drainage 1. It can be suspected from the radionuclide scan and a prolonged course in a patient presenting with the symptoms and signs of epididymo-orchitis.
- Testicle injury or blow to the testicles
- Testicular cancer. Thirty percent of patients with testicular tumors present with testicular pain, tenderness, and swelling 1. This is most common with teratomas, but also occurs with seminomas and embryonal carcinomas. Radionuclide scans may be “hot” or show a halo effect similar to that seen with an abscess or a missed torsion. Surgical removal, radiotherapy, and chemotherapy are required.
- Testicular torsion (twisted testicle)
- Undescended testicle (also called cryptorchidism)
- Urinary tract infection (UTI)
- Varicocele (enlarged veins in the scrotum)
- Vasectomy. A small number of patients develop testicular pain within months or years after vasectomy 1. In some patients, postvasectomy pain is associated with a tender sperm granuloma at the vasectomy site. In others, it is associated with epididymal swelling and tenderness. These pains are increased by ejaculation and can be relieved by vasovasostomy, which restores fertility and reduces the high back-pressure in the vas and epididymis. Excision of painful sperm granulomas at the vasectomy site brings relief without restoring fertility to patients with painful vasectomy site granulomas.
- Viral orchitis may occur with mumps, with salivary gland involvement, and with rubella and coxsackie viral infections 1. Orchids also occurs with chickenpox, some echovirus infections, dengue, and lymphocytic choriomeningitis. Analgesics and scrotal support are required for symptomatic relief until the testicular pain and tenderness resolve in 1 to 8 weeks.
Common causes of testicle pain include:
- Injury. Testicular blunt trauma may cause hematoma and contusion, rupture of the testis, or secondary torsion and infarction. Acute scrotal swelling from blunt trauma should be studied by radionuclide angiography and explored for rupture or torsion.
- Infection or swelling of the sperm ducts (epididymitis) or testicles (orchitis).
- Twisting of the testicles that can cut off the blood supply (testicular torsion). It is most common in young men between 10 and 20 years old. It is a medical emergency that needs to be treated as soon as possible. If surgery is performed within 6 hours, most testicles can be saved.
By far the most common causes of testicular pain are epididymitis/epididymal-orchitis, testicular appendage torsion, spermatic cord torsion (commonly referred to as testicular torsion), varicoceles, and inguinal hernias 2. The incidence and frequency of these causes are highly variable by age groups. Acute testicle pain in children is much more likely to represent torsion of the spermatic cord or testicular appendages whereas patient older than 25 are much more likely to have epididymitis 2.
There is little data which specifically reports the incidence of the acute scrotum as a presenting complaint, but male genitourinary complaints are estimated at between 0.5% and 2.5% of all emergency department visits. The annual incidence of testicular torsion, however, is estimated 1 in 4000. This means however that an estimated 1 in every 160 men will experience spermatic cord torsion within their first 25 years of life. Although it is possible to occur at any age, the incidence drops off dramatically in the adult years. Even among children, however, the most common cause of acute scrotal pain is torsion of the appendix testis rather than that of the spermatic cord.
Epididymitis is the most common cause of acute scrotal pain in adults. It is estimated that over 600,000 cases are diagnosed in United States emergency departments each year, and this condition was responsible for 1 out of every 144 outpatient visits for men between 18 and 50 years of age 2. Epididymitis tends to have a bimodal age incidence due to differing microbiological causes and risk factors 3.
Mild pain may be caused by fluid collection in the scrotum, such as:
- Enlarged veins in the scrotum (varicocele).
- Cyst in the epididymis that often contains dead sperm cells (spermatocele).
- Fluid surrounding the testicle (hydrocele).
- Pain in the testicles may also be caused by a hernia or kidney stone.
- Testicular cancer is almost always painless. But any testicle lump should be checked out by your health care provider, whether or not there is pain.
Sudden, severe testicle pain can be a sign of testicular torsion — a twisted testicle that can quickly lose its blood supply. This condition requires immediate medical treatment to prevent loss of the testicle. Testicular torsion can occur in males of any age, although it is more common in adolescents.
Seek immediate medical attention if you have:
- Sudden, severe testicle pain
- Testicle pain accompanied by nausea, fever, chills or blood in your urine
- You have had an injury or trauma to the scrotum, and you still have pain or swelling after 1 hour.
Also see your provider right away if:
- Mild testicle pain lasting longer than a few days
- You have a fever.
- Your scrotum is warm, tender to the touch, or red.
- You have been in contact with someone who has the mumps.
- A lump or swelling in or around a testicle
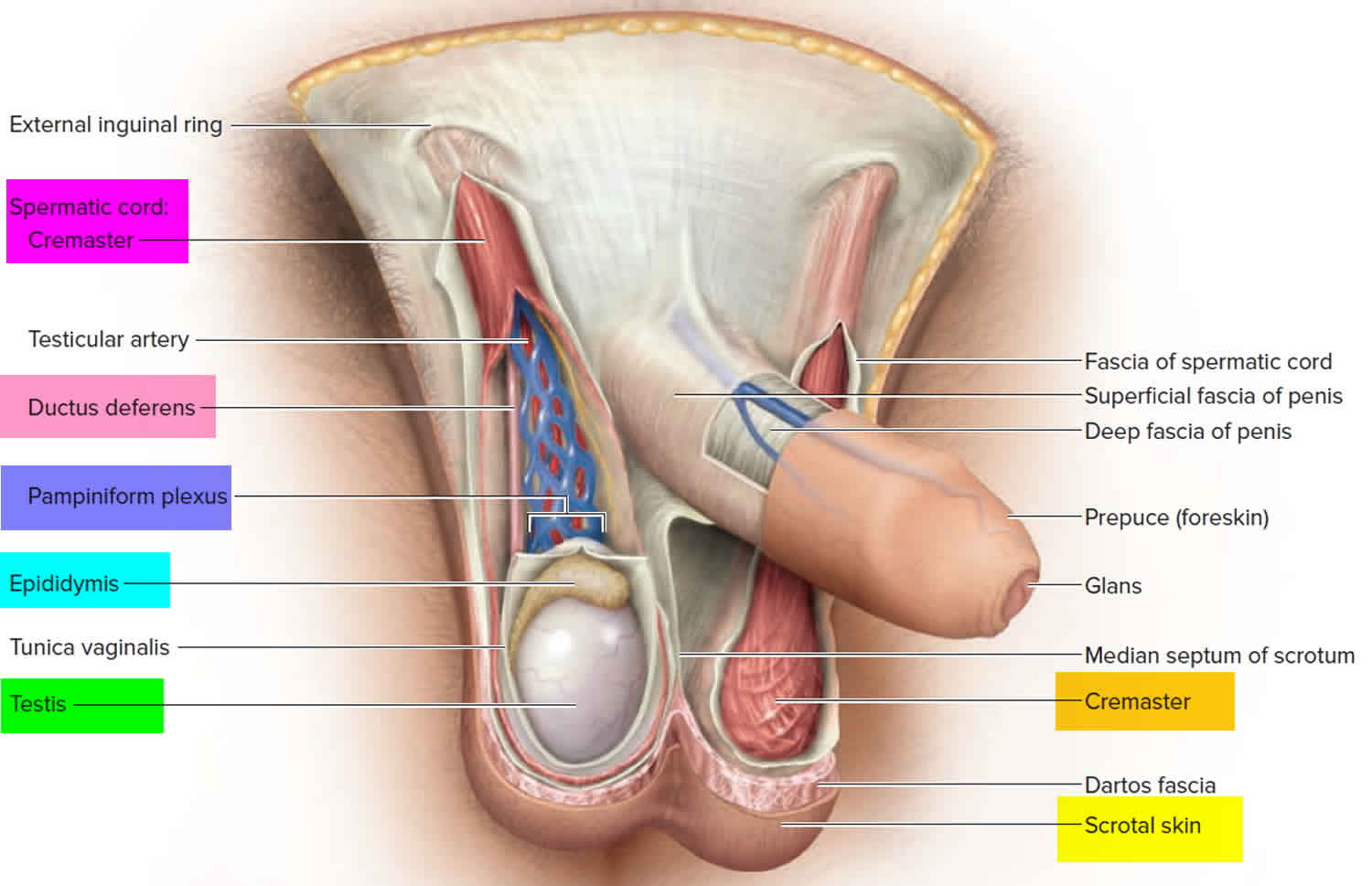
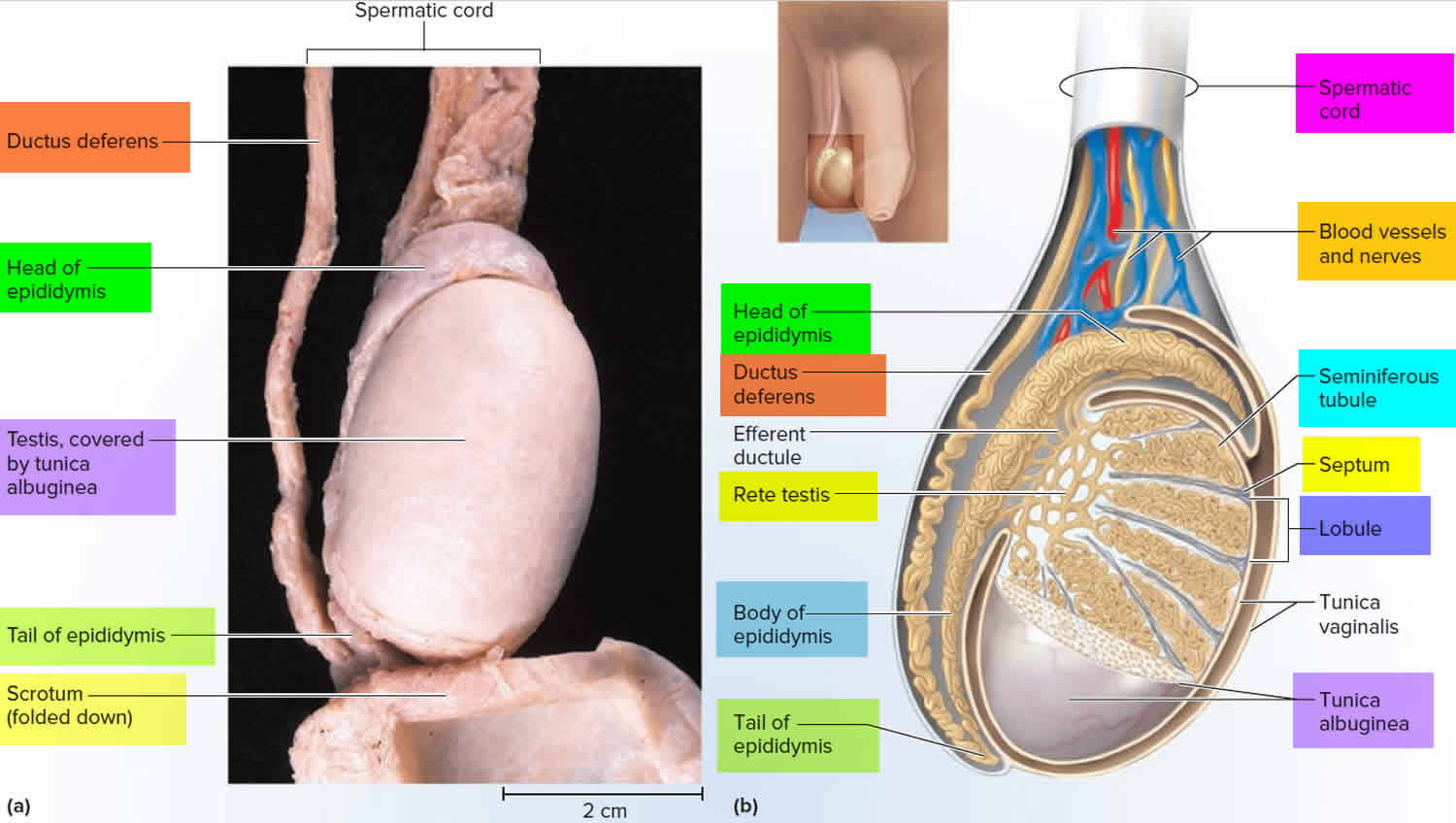
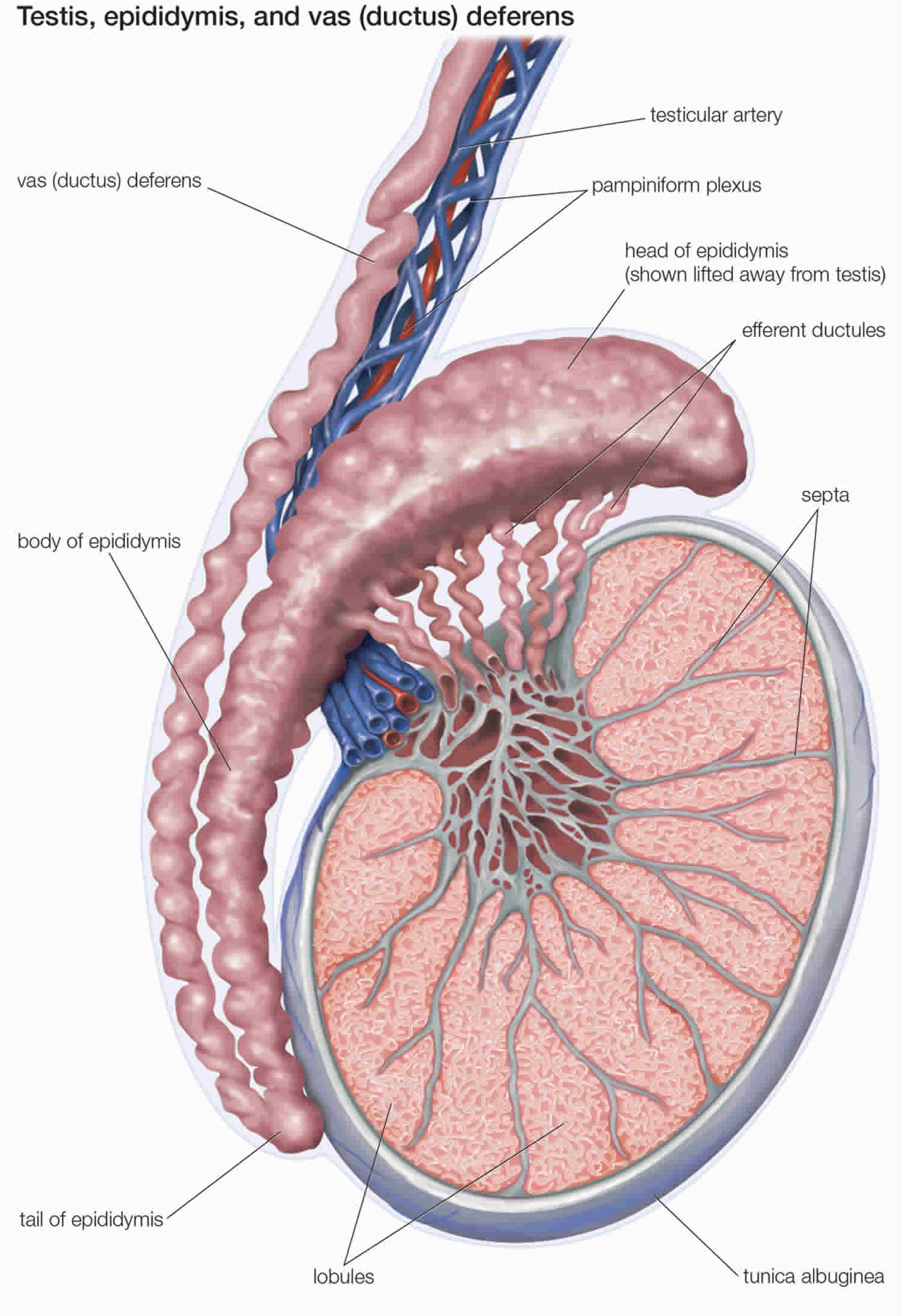
Testicle anatomy
Knowledge of the relevant anatomy is essential to understanding the possible causes and subsequent steps in the evaluation of testicle pain. The testes are ovoid-shaped organs roughly 3 cm to 5 cm by 3 cm by 3 cm and vertically-oriented. The tunica albuginea envelops them with continuous internal septations converging into a mediastinum tests which acts as the structural support for the organ. This, in turn, is enveloped by the tunica vaginalis. Posterolateral to the testis is the epididymis, a curved structure roughly 6 cm to 7 cm in its longest dimension. Its efferent ductules converge to form the ductus epididymis and eventually the vas deferens.
The vascular anatomy of the scrotal contents is also important to review. The testes receive a joint supply of blood from the testicular artery, deferential artery, and the cremasteric artery. While the deferential artery and the cremasteric artery are branches of the inferior vesical and inferior epigastric artery, respectively, the testicular artery branches directly from the abdominal aorta. The testes are drained via small branching veins forming the pampiniform plexus and ultimately the testicular vein. Notably, the testicular vein drains directly into the inferior vena cava on the right while it drains into the left renal vein contralaterally.
The vascular structures, vas deferens, and nerves are all bound within the spermatic cord, a conduit allowing passage from the peritoneum to the scrotum via the inguinal canal. The cremaster muscle is also found within the spermatic cord. The tunica vaginalis usually surrounds only part of the testis and epididymis and then attaches posteriorly to the scrotal wall. However, when the tunica vaginally surrounds the testis and part of the spermatic cord, the testicle is no longer fixed to the scrotal wall and able to twist freely. This is known as the Bell-Clapper deformity and has an incidence of up to 12% 4.
Figure 1. Testicles and scrotum anatomy
Figure 2. Testicle anatomy
 Testicular torsion
Testicular torsion
Testicular torsion is a medical emergency, requiring prompt treatment or risking the loss of the testicle. The incidence is 1 in 4,000 males under the age of 25 years 5.
Testicular torsion may be intravaginal or extravaginal 6. Intravaginal torsion occurs when the testicle can freely rotate within the tunica vaginalis; this can be due to a congenital anomaly called the Bell-Clapper deformity. This deformity is due to failure of posterior anchorage of the gubernaculum, epididymis, and testis, thus allowing the testis to freely rotate within the tunica vaginalis, ultimately pinching off arterial blood supply to the testicle leading to ischemia and infarction. Extravaginal torsion is seen almost exclusively in neonates, occurs when the testis rotates within the scrotum owing to inadequate fusion of the testicle to the scrotal wall via the tunica vaginalis or increased mobility of the testicle before the descent into the scrotum 7. The torsion follows rotation of the spermatic cord and results in ischemia. The degree of testicular torsion is directly correlated with the possibility of salvage after torsion and time to necrosis. The degree of torsion may be variable, usually causing venous occlusion and congestion first. Most cases of spermatic cord torsion leading to infarction are twisted at least 720 degrees. Torsion of the testicular appendages, often presenting in 7- to 13-year-old children, presents similarly to testicular torsion and accounts for 24% to 46% of acute scrotal presentations 8.
Testicular torsion diagnosis
The classic presentation of testicular torsion is acute-onset, intense, unilateral scrotal pain. Patients may also complain of nausea and vomiting, likely secondary to pain 8. Intensity increases owing to edema and resultant capsular stretching 9. Patients may also have a history of scrotal pain that may be related to prior ischemic episodes that resolved spontaneously. On examination, the hallmark of testicular torsion is a ‘high riding’ testis due to shortening of the cord. Additionally, the testis may have an abnormal (e.g., transverse) position in the scrotum 8. Absence of the cremasteric reflex is a characteristic of torsion in the pediatric population 10. A normal cremasteric reflex would result in elevation of the ipsilateral testis after an extra gentle stroke of the inner thigh. The cremasteric reflex is rarely seen in patients with testicular torsion. Labs and studies should include urinalysis and scrotal ultrasound to confirm the diagnosis. Urinalysis showing hematuria or leukocytosis is more typical of epididymo-orchitis than torsion. Doppler ultrasonography can be used to assess testicular blood flow, which is reduced or absent in testicular torsion. This technique, however, is highly operator dependent and may have significantly high false interpretations in young children or neonates with small vessels 11. Although torsion usually occurs around puberty and epididymitis typically affects sexually active men after the age of 20 years, age distribution may be clinically misleading and should not be relied upon for a diagnosis.
In contrast to testicular torsion, patients with torsion of a testicular appendage (appendix testis or appendix epididymis) rarely have systemic complaints and typically present with a gradual-onset, less intense, unilateral scrotal pain that is localized to the superior pole of the testis 12. Careful examination of the scrotal skin early in the course may reveal the ‘blue dot sign’ owing to the nonviable appendage 13.
Testicular torsion treatment
Testicular torsion requires immediate surgical intervention with scrotal exploration, detorsion, and orchidopexy. In a review of 543 surgical explorations for acute scrotal pain in boys, Van Glabeke et al. 14 found a 16.6% incidence of testicular torsion and a 46% incidence of appendage torsion. The authors recommended surgical intervention in all male children complaining of acute scrotal pain. If immediate operative intervention is not possible, manual detorsion may be attempted.
It is helpful to recall the anatomy of testicular torsion. Specifically, torsion typically occurs in a medial direction, and detorsion should therefore be initially tried in a clockwise direction on the left and counterclockwise on the patient’s right side 8. In contrast to testicular torsion, appendicular torsion does not necessarily require surgical intervention. However, the distinction between appendicular torsion and testicular torsion remains difficult. As a general rule, surgical intervention is required in all cases where Doppler sonography demonstrates decreased or absent testicular blood flow. Failure to treat promptly will result in loss of the affected testicle.
Epididymitis
Epididymitis is a genitourinary tract infection which is usually due to continuous spread from pathogens affecting the bladder of the urethra. In men less than 35 years old this is most commonly associated with sexually transmitted organisms such as Chlamydia trachomatis and, less commonly, Neisseria gonorrhea. Men older than 35 years or those without sexual partners usually present with gram-negative urinary pathogens which are also responsible for cystitis and prostatitis, predominantly Escherichia coli. Other urinary pathogens such as Klebsiella pneumoniae, Proteus mirabilis, and Ureaplasma urealyticum may be seen. Rare organisms can occur such as cytomegalovirus, Mycobacterium, and other fungal causes may be seen in immunocompromised hosts such as those with HIV 15.
According to the Centers for Disease Control and Prevention’s ambulatory health care data, epididymitis accounted for 1 in 144 outpatient visits in 2002 in the United States in men aged 18 to 50 years 16. The pathophysiology involves the spread of microorganisms from the urethra, prostate, or seminal vesicles, as well as hematogenous spread as in tuberculosis, causing a painful, parenchymal inflammatory process resulting in epididymal swelling. The swelling may affect the testicles, which is known as epididymo-orchitis. The common causative agents are dependent on age and sexual activity.
Sexually active men younger than 35 years are usually infected with Chlamydia trachomatis and Neisseria gonorrhea, whereas older patients, patients who have undergone recent genitourinary surgery, and patients with anatomical abnormalities often have infection with gram-negative enterococci associated with urinary tract infections 8. Fungal agents such as Candida species, very rarely, can also cause epididymitis 17.
Epididymitis in the pediatric population has a peak incidence during puberty. The pathophysiology of infantile epididymitis is, in contrast to adult cases, rarely due to bacterial pathogens and remains largely unknown. Bacterial causes have been implicated in 6.2% to 9.9% of pediatric cases. Other etiologies may include anatomical abnormalities causing reflux of sterile or infected urine into the ejaculatory ducts or sequelae of a viral illness 18. It has been suggested that the association of infantile epididymitis with other urogenital abnormalities mandates further diagnostic evaluation 19. However, this recommendation remains controversial. One study assessed 49 boys for acute epididymis and found only 1 to have a relevant structural urinary tract malformation 20.
Finally, there has been an association of sterile epididymitis with the antiarrhythmic agent amiodarone in up to 11% of adult patients and rarely in children. The mechanism behind this is unknown but may be related to the accumulation of amiodarone in high concentrations in the testicular tissue 21.
Epididymitis diagnosis
Epididymitis, unlike testicular torsion, presents with gradually increasing dull, unilateral scrotal pain. Involvement of the vasa may result in exquisite pain that affects the entire hemiscrotum as well as the spermatic cord. Discerning epididymitis from torsion may be difficult; however, a history of prior genitourinary tract procedures and sexual activity are more suggestive of epididymitis 13. On physical examination, a tender and swollen epididymis and normal cremasteric reflex is observed. Urinalysis, urine cultures, and urethral cultures must be performed to identify possible causative agents. A positive urinalysis and urine cultures, along with elevated white blood cell count, favor a diagnosis of epididymitis but do not exclude torsion. Color Doppler ultrasound or nuclear scintigraphy to assess blood flow to the scrotum and its contents will help to differentiate between the two entities. Doppler ultrasound would show increased blood flow, because this is an inflammatory condition 13.
Although the incidence of tuberculous epididymitis has gradually declined in the Western hemisphere, it is important to be familiar with the typical presentation. Genital-urinary tuberculosis is the most common form of extrapulmonary tuberculosis, with tuberculous epididymitis commonly being the first manifestation 22. The frequency of genital-urinary tuberculosis among those diagnosed with tuberculosis is reported to range from 2.3% to 40.9%, with tuberculous epididymitis having an incidence of 7.4% to 34.1% within this population. Tuberculous epididymitis is most common in the 35- to 55-year-old age group and can present as acute epididymitis refractory to conventional antibiotic treatment. On exam, a painful, hard, bulky mass can be appreciated. Rapid diagnosis is essential and can be made with direct examination by using auramine staining as well as genomic amplif ication polymerase chain reaction. Cultures can be concurrently taken and can be used to confirm the diagnosis and determine sensitivities for treatment 22.
Epididymitis treatment
Empiric antibiotic treatment should be started if the clinical suspicion is high. Once cultures and sensitivities are back from the lab, antibiotics should be adjusted accordingly. In the pediatric population, epididymitis should be treated with antibiotics if the urine analysis or urine culture suggests bacterial etiology; if there is no evidence of bacteria, supportive measures are suggested 23. Surgery is an option for patients with genitourinary abnormalities 18. In sexually active males younger than 35 years, empiric treatment includes ceftriaxone and doxycycline or ofloxacin. Sexual partners should also be evaluated and treated. Older patients (age greater than 35 years old) should be treated with oral levofloxacin or ofloxacin 8. Treatment also includes symptomatic relief with bed rest, scrotal elevation, analgesics, and nonsteroidal anti-inflammatory drugs (NSAIDs). In severe cases, a cord block may be used to alleviate pain. It is also important to discontinue or reduce the dosage of offending agents such as amiodarone for rapid resolution and avoidance of unnecessary surgical interventions in high-risk groups 24. The patient should be advised that the pain and edema usually subside in 7 to 10 days, but the epididymal induration may persist for a few weeks. If symptoms do not improve within 3 days, early follow-up is advised. Cases that persist for 6 to 8 weeks after completion of antimicrobial therapy should be reevaluated with a higher index of suspicion for unusual organisms (i.e., tuberculous or fungal etiology) 8.
Orchitis
Orchitis is swelling (inflammation) of one or both of the testicles. Bacterial or viral infections can cause orchitis, or the cause can be unknown. Orchitis is most often the result of a bacterial infection, such as a sexually transmitted infection (STI). In some cases, the mumps virus can cause orchitis.
Bacterial orchitis might be associated with epididymitis — an inflammation of the coiled tube (epididymis) at the back of the testicle that stores and carries sperm. In that case, it’s called epididymo-orchitis.
Orchitis causes pain and can affect fertility. Medication can treat the causes of bacterial orchitis and can ease some signs and symptoms of viral orchitis. But it can take several weeks for scrotal tenderness to disappear.
If you have pain or swelling in your scrotum, especially if the pain occurs suddenly, see your doctor right away.
A number of conditions can cause testicle pain, and some require immediate treatment. One such condition involves twisting of the spermatic cord (testicular torsion), which might cause pain similar to that caused by orchitis. Your doctor can perform tests to determine which condition is causing your pain.
Orchitis causes
Orchitis may be caused by an infection. Many types of bacteria and viruses can cause this condition. Sometimes a cause of orchitis can’t be determined.
The most common virus that causes orchitis is mumps. It most often occurs in boys after puberty. Orchitis most often develops 4 to 6 days after the mumps begins.
Orchitis may also occur along with infections of the prostate or epididymis.
Orchitis may be caused by an sexually transmitted infection (STI), such as gonorrhea or chlamydia. The rate of sexually transmitted orchitis or epididymitis is higher in men ages 19 to 35.
Bacterial orchitis
Most often, bacterial orchitis is associated with or the result of epididymitis. Epididymitis usually is caused by an infection of the urethra or bladder that spreads to the epididymis.
Often, the cause of the infection is an sexually transmitted infection (STI). Other causes of infection can be related to having been born with abnormalities in your urinary tract or having had a catheter or medical instruments inserted into your penis.
Viral orchitis
The mumps virus usually causes viral orchitis. Nearly one-third of males who contract the mumps after puberty develop orchitis, usually four to seven days after onset of the mumps.
Risk factors for orchitis
Risk factors for sexually transmitted orchitis include:
- High-risk sexual behaviors
- Multiple sexual partners
- Personal history of gonorrhea or another sexually transmitted infection (STI)
- Sexual partner with a diagnosed sexually transmitted infection (STI)
- Sex without a condom
- A personal history of an STI
Risk factors for orchitis not due to an STI include:
- Being older than age 45
- Long-term use of a Foley catheter
- Not being vaccinated against the mumps
- Problems of the urinary tract that were present at birth (congenital)
- Repeated urinary tract infections
- Surgery of the urinary tract (genitourinary surgery)
Orchitis prevention
To prevent orchitis:
- Get immunized against mumps, the most common cause of viral orchitis
- Practice safe sex, to help protect against STIs that can cause bacterial orchitis
Orchitis symptoms
Orchitis signs and symptoms usually develop suddenly and can include:
- Swelling in one or both testicles
- Pain in the testicle. Pain ranging from mild to severe
- Fever
- Nausea and vomiting
- General feeling of unwellness (malaise)
- Blood in the semen
- Discharge from penis
- Groin pain
- Pain with intercourse or ejaculation
- Pain with urination (dysuria)
- Scrotal swelling
- Tender, swollen groin area on affected side
- Tender, swollen, heavy feeling in the testicle
The terms “testicle pain” and “groin pain” are sometimes used interchangeably. But groin pain occurs in the fold of skin between the thigh and abdomen — not in the testicle. The causes of groin pain are different from the causes of testicle pain.
Orchitis complications
Complications of orchitis may include:
- Testicular atrophy. Orchitis can eventually cause the affected testicle to shrink. Some boys who get orchitis caused by mumps will have shrinking of the testicles (testicular atrophy).
- Scrotal abscess. The infected tissue fills with pus.
- Infertility. Occasionally, orchitis can cause infertility or inadequate testosterone production (hypogonadism). But these are less likely if orchitis affects only one testicle.
- Chronic epididymitis
- Death of testicle tissue (testicular infarction)
- Fistula on the skin of the scrotum (cutaneous scrotal fistula)
Acute pain in the scrotum or testicles can be caused by twisting of the testicular blood vessels (torsion). This is a medical emergency that requires immediate surgery.
A swollen testicle with little or no pain may be a sign of testicular cancer. If this is the case, you should have a testicular ultrasound.
Orchitis diagnosis
Your doctor is likely to start with your medical history and a physical exam to check for enlarged lymph nodes in your groin and an enlarged testicle on the affected side. Your doctor might also do a rectal examination to check for prostate enlargement or tenderness.
A physical exam may show:
- Enlarged or tender prostate gland
- Tender and enlarged lymph nodes in the groin (inguinal) area on the affected side
- Tender and enlarged testicle on the affected side
- Redness or tenderness of scrotum
Your doctor might recommend:
- Sexually transmitted infection (STI) screen. If you have discharge from your urethra, a narrow swab is inserted into the end of your penis to obtain a sample of the discharge. The sample is checked in the laboratory for gonorrhea and chlamydia. Some sexually transmitted infection (STI) screens are done with a urine test.
- Urinalysis. A sample of your urine is analyzed to see if anything’s abnormal.
- Urine culture (clean catch) — may need several samples, including initial stream, midstream, and after prostate massage
- Complete blood count (CBC).
- Ultrasound. This imaging test is the one most commonly used to assess testicular pain. Ultrasound with color Doppler can determine if the blood flow to your testicles is lower than normal — indicating torsion — or higher than normal, which helps confirm the diagnosis of orchitis.
Orchitis treatment
Treatment depends on the cause of orchitis.
Treating bacterial orchitis
Antibiotics are needed to treat bacterial orchitis and epididymo-orchitis. If the cause of the bacterial infection is an STI, your sexual partner also needs treatment.
Take the entire course of antibiotics prescribed by your doctor, even if your symptoms ease sooner, to ensure that the infection is gone.
It may take several weeks for the tenderness to disappear. Resting, supporting the scrotum with an athletic strap, applying ice packs and taking pain medication can help relieve discomfort.
Treating viral orchitis
Treatment is aimed at relieving symptoms. Your doctor might recommend:
- Nonsteroidal anti-inflammatory drugs, such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve)
- Bed rest and elevating your scrotum
- Cold packs
Most people with viral orchitis start to feel better in three to 10 days, although it can take several weeks for the scrotal tenderness to disappear.
Orchitis prognosis
Getting the right diagnosis and treatment for orchitis caused by bacteria can most often allow the testicle to recover normally.
You will need further testing to rule out testicular cancer if the testicle does not completely return to normal after treatment.
Mumps orchitis cannot be treated, and the outcome can vary. Men who have had mumps orchitis can become sterile.
Varicocele
A varicocele is an abnormal dilation of the spermatic veins commonly due to an anatomical abnormality with an incidence of 10% to 20% in the general male population and 2% to 15% in adolescent males 25. The mechanism is thought to involve absent or malfunctioning vein valves, thus resulting in retrograde flow into the pampiniform plexus located in the spermatic cord and scrotum from the internal spermatic and cremasteric veins. Some investigators have also demonstrated lack of valves as proximal as the renal veins and absent or incomplete valves along the internal spermatic vein 26. Furthermore, it has been postulated that the longer length of the left gonadal vein, as well as insertion into the left renal vein, results in greater hydrostatic pressures and thus more common expression of varicocele on the left side 27. Varicoceles have been associated with male infertility, although the exact cause-and-effect relationships have not been established. Leading theories suggest that elevated scrotal temperature, hypoxia secondary to stasis, and reflux of renal and adrenal metabolites result in impaired spermatogenesis and infertility 28.
Varicocele pain typically presents as a dull, aching, and throbbing sensation in the scrotum without sharp or radiating components 29. Varicocele can be exacerbated by long periods of standing owing to the resultant increased hydrostatic pressure in the valveless veins of the pampiniform plexus. Careful physical examination of the scrotum and spermatic cord is required and the classic finding is a ‘bag of worms’ on palpation 27. Cremasteric relaxation should be facilitated by allowing the patient to stand in a warm room for a few minutes. Varicoceles are classified in grades: grade 0, no palpable varicocele; grade 1, palpable during a Valsalva maneuver; grade 2, visible in the standing position during a Valsalva maneuver; and grade 3, visible in the standing position through scrotal skin without Valsalva maneuver. Although varicocele is considered a clinical diagnosis, color Doppler imaging can be used as an adjunctive diagnostic tool in equivocal cases. Evidence of venous dilation and reflux during a Valsalva maneuver are sonographic criteria for the diagnosis of varicocele 27. Pilatz et al. 30 demonstrated that grades 1 to 3 varicoceles can be predicted with a greater than 80% sensitivity and specificity by using cutoff vein diameters of 2.45 mm at rest and 2.95 mm during Valsalva maneuvers. Reflux is determined by calculating the retrograde flow of contrast material via an internal spermatic vein. A study conducted by Chiou et al. 31 used a scoring system with the following parameters: maximal venous diameter, presence of a venous plexus, sum of the diameters of veins in the plexus, and change of flow during a Valsalva maneuver to diagnose varicoceles with a sensitivity of 93% and a specificity of 85%. Each parameter is given a score from 0 to 3 and a total score of greater than 4 is considered positive for varicocele 27.
Varicocele treatment
Varicoceles can affect various seminal parameters including sperm production. Most authors agree that surgical therapy of varicoceles is an accepted intervention in the treatment of male factor infertility; microsurgical varicocelectomy is regarded as the gold standard 32. When compared to androgen replacement therapy, a study by Cho and Seo 32 found varicocele repair to be more cost-effective in treating infertility. Pain secondary to varicoceles is estimated to affect 2% to 10% of men, but surgical intervention for relief of pain is controversial 29.
Several recent studies, including a large study from Turkey evaluating 119 men, have evaluated the results of varicocelectomy performed for relief of pain. In the study from Turkey, microsurgical varicocele ligation was performed in patients diagnosed on the basis of findings from the physical examination and Doppler ultrasound 33. At the end of the study, 82 patients were evaluated. A total of 72 patients (88%) reported complete resolution of pain, 4 (5%) reported partial resolution, 5 (6%) reported no change, and 1 (1%) reported epididymal discomfort that resolved with conservative measures. Another study reviewed 58 patients who underwent varicocele ligation for pain relief and obtained follow-up on 35 of the 58 patients in whom initial conservative measures had failed. The study showed resolution of pain postoperatively in 86% and partial resolution in 1 patient, whereas 4 patients (11%) had persistent or worsened symptoms 29. A more recent study conducted by Kim et al. 34 reported that 91.2% had complete or marked resolution of pain at a 1-year follow-up. The authors used microsurgical inguinal varicocelectomy, with 8.8% of patients having recurrent pain and 0.8% having recurrence. None were found to have hydroceles or evidence of testicular loss or atrophy.
Chronic testicle pain
Chronic testicle pain (chronic orchialgia) is a common and frustrating problem. Chronic testicle pain prevalence, frequently idiopathic cause, psychosocial impact, and treatment dilemma often lead to patient distress, physician frustration, and incomplete care 6. It is defined as intermittent or constant testicular pain for a period of 3 or more months that interferes with daily activities 35. The pain may involve any of the scrotal contents including the testicle, epididymis, paratesticular structures, and spermatic cord 36. The etiology of chronic orchialgia remains largely unknown with up to 50% of patients presenting with an idiopathic etiology, but has been found to be associated with nerve damage to the spermatic cord after vasectomy, trauma, inguinal herniorrhaphy, and epididymitis 37. Similarly, the pathophysiology is not well understood, but involves nerve sensitization following repeated stimulation leading to modulation of these pathways, ultimately resulting in spontaneous firing. These chronically up-regulated pathways are thought to be responsible for chronic testicle pain 38.
Chronic testicle pain diagnosis
Chronic testicle pain is a diagnosis of exclusion, thus requiring a great emphasis on the history and physical examination 24. The history should be focused on identifying other causes of pain including tumor, torsion, infection, postvasectomy pain, and varicocele. The character of the pain, onset, duration, severity (using a standardized pain scale), location, referral of pain, and psychosocial impact should be investigated. Activities that exacerbate or alleviate the pain, including urinary habits, bowel movements, as well as sexual and physical activities, should be carefully documented. Previous surgeries, history of trauma, or infections localized to the back, inguinal, scrotal, and retroperitoneal areas should also be elicited. As with all sexual pain, it is important to ask questions about sexual health and abuse 36. A focused and detailed examination of the genitalia followed by a rectal exam should be performed to identify other causes of the chronic pain. Laboratory tests, including urinalysis and urine and semen cultures, should be obtained when indicated (i.e., suspicion of malignancy or infection). Initial imaging should be limited to duplex scrotal ultrasound to exclude structural abnormalities; more advanced imaging may be obtained if indicated. If history and physical examination do not identify a cause, a spermatic cord block using 20 mL of 0.25% bupivacaine without epinephrine should be performed. Temporary pain relief is highly suggestive of chronic testicle pain 35.
Chronic testicle pain treatment
The first-line treatment is nonsurgical therapy including nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics (if indicated), antidepressants, anticonvulsants, nerve block, and pulsed radiofrequency 6. Antibiotics of choice include doxycycline and quinolones, as they have the highest penetration into the affected structures 37. Antidepressants used are amitriptyline (10-25 mg per oral at bed time) or nortriptyline (10-150 mg per oral daily), which inhibits norepinephrine release, thereby attenuating the neuronal pain pathways. The anticonvulsant gabapentin (300 mg per oral titrated up to 3,600 mg daily) is used for neuropathic pain and works by modulating calcium channels in the central nervous system 39. Therapeutic nerve blocks with or without steroids can be done to provide relief from pain. Psychological counseling may be offered to the patient to better deal with the pain 37. Lastly, a novel technique using pulsed radiofrequency to denervate the spermatic cord has been attempted. The efficacy of the procedure has yet to be determined 40.
Patients who fail nonsurgical therapy may consider surgical therapy. Unfortunately, there is no standard of care f or the surgical intervention of chronic orchialgia. Current treatment includes epididymectomy, vasovasostomy and vasectomy reversal for postvasectomy cases, orchiectomy, laparoscopic testicular denervation, and microsurgical denervation of the spermatic cord (MDSC). Epididymectomy has success rates ranging from 10% to 80% and is reserved for patients whose pain is localized to the epididymis 41. A report on vasovasostomy for chronic pain found that 75% had complete relief, 10% had partial relief (improved by 30%), and 10% had no improvement 42. Other studies have shown that vasectomy reversals have success rates ranging from 69% to 84% 43. The major drawback for vasovasostomy and vasectomy reversal is loss of desired sterility. Orchiectomy success rates range from 20% to 80%. However, it is important to take into consideration the physiological and psychological damage that is frequently associated with this procedure 44.
Laparoscopic testicular denervation has been shown to result in 78% achieving partial relief and 28% with no relief of pain. However, the efficacy of this treatment has not been fully studied 44. Microsurgical denervation of the spermatic cord treats chronic orchialgia by denervating the chronically up-regulated pathways theorized to cause the pain. With the use of this technique, 71% had complete resolution of pain, 17% had greater than 50% reduction, and 12% had no resolution of pain. The advantage to this technique is preservation of organs and scrotal contents 44. Temporary relief from a spermatic cord block may be a positive predictor for success 45. The aforementioned surgical procedures all come with similar risks, including infection, bleeding (hematoma), hydrocele formation, testicular atrophy, possibility of no relief or worsened pain, and hypogonadism 37.
Microsurgical denervation of the spermatic cord, which was popularized by Levine 37, is performed under general anesthesia with the use of an operating microscope powered at 8× to 14×. A low inguinal incision is made and carried down to the level of the external inguinal ring. The spermatic cord is isolated and the ilioinguinal nerve and branches are identified and divided. To reduce neuroma formation, the proximal end of the ilioinguinal nerve should be buried under external oblique fascia. Next, all fascia and cremasteric fibers in the cord should be divided with electrocautery while taking care to isolate and spare arterial structures (testicular, cremasteric, and deferential). Internal spermatic veins should be ligated and divided. In addition to arterial structures, one or two lymphatic vessels should be identified and spared to maintain proper drainage postoperatively and to reduce the chance of a hydrocele formation. Next, the vas deferens is identified and the nerve-rich perivasal fascia is stripped away because it contains afferent nerve pathways that can carry noxious stimuli and propagate scrotal pain. If the patient underwent a vasectomy, the vas and fascia should be stripped again. At the end of the operation, the remaining structures include the spermatic arteries, one to two lymphatic vessels, and the vas deferens (unless there is a prior history of vasectomy) 37. At the risk of oversimplification, the procedure may be described as a more extensive or ‘radical’ varicocelectomy. Since 2012, we have performed this operation at our center on several patients refractory to other therapies and have found success rates similar to the rates reported by Levine 37. A more recent study found that success rates with microsurgical denervation of the spermatic cord were not statistically significantly different between men who had undergone surgical treatment in the past and surgery-naive men 45.
What to expect at your doctor’s office visit
Your doctor will do an exam of your groin, testicles, and abdomen.
Your doctor will ask you questions about the pain in testicle such as:
- How long have you had testicular pain? Did it start suddenly or slowly?
- Is one side higher than usual?
- Where do you feel the pain? Is it on one or both sides?
- How bad is the pain? Is it constant or does it come and go?
- Does the pain reach into your abdomen or back?
- Have you had any injuries?
- Have you ever had an infection spread by sexual contact?
- Do you have any other symptoms like swelling, redness, change in the color of your urine, fever, or unexpected weight loss?
A “high-riding” asymmetrical testicle with an abnormal lay and loss of ipsilateral cremasteric reflex is historically described as the classic presentation of acute testicular torsion. However, this dogmatic description of the classic presentation is not universally observed in all cases and may lead to misdiagnosis or delay in definitive treatment. The cremasteric reflex is fickle and may be absent in up to 30% of normal males without any pathology. Conversely, several case series report patients with surgically confirmed testicular torsion may still have preserved cremasteric reflexes anywhere from 8% to 30% of the time. Other scrotal pathology such as epididymo-orchitis may also result in loss of a normal reflex.
If the diagnosis of spermatic cord torsion is strongly suspected, then an emergency surgical consultation is warranted without further delay. The “classic” cutoff for salvage of testicular torsion is surgical exploration and detorsion within six hours of symptoms onset. This does not mean however that prompt evaluation and definitive surgical exploration be delayed for patients in whom symptoms have been present for greater than 6 hours. The salvage rates do drop to between 80% to 88%% at 12 hours, 31% at 24 hours, and only 2.6% at 48 hours. This may be due to variable degrees or torsion (incomplete torsion) or torsion-detorsion phenomena.
The following tests may be performed:
- Ultrasound of the testicles
- Urinalysis and urine cultures
- Testing of prostate secretions
- CT scan or other imaging tests
Doppler ultrasound is the most appropriate imaging modality for evaluation of the acute testicular pain when it does not delay definitive surgical consultation in cases of presumed testicular torsion. The sensitivity of color Doppler ultrasound is reported to range between 96% to 100% with a specificity of between 84% to 95%. A body of literature exists which also supports the role of point-of-care ultrasound by the treatment provider for the evaluation of the acute scrotum. A detailed review of this technique is beyond the scope of this article, but findings on ultrasound suggestive of testicular torsion include an enlarged, homogenous, hypoechoic testicle with absent color flow or spectral Doppler waveforms suggesting increased vascular resistive index. The spermatic cord torsion may also be directly observed with ultrasound; a finding described as the “whirlpool” or “snail” sign.
Conversely, infectious etiologies of the acute scrotum cause an increase in blood flow to the testicle or epididymis, which is apparent of Doppler imaging. Resistive indices of the testicle may be abnormally low, and the testicle or epididymis will again be larger than the asymmetry side. Abscesses may also be identified, as well as the presence of subcutaneous gas within the scrotal wall.
Other imaging modalities are also available. Radionuclide scrotal imaging was at one point the primary modality since its implementation in the 1970s. In the differentiation of testicular torsion and epididymo-orchitis, there is a reported sensitivity range of 89% to 98% and specificity of 90% to 100%. However, this modality is prone to false positives particularly in cases of spermatocele, hydrocele, and inguinal hernias and may lead to unnecessary surgical exploration when compared to modern ultrasonography. MRI had 93% sensitivity and 100% specificity for diagnosing torsion; however, availability and length of time required to complete may limit its appropriateness. CT imaging is useful when there is a concern for necrotizing skin and soft tissue infections and Fournier’s gangrene 46.
Testicular pain home treatment
Non-urgent causes of testicle pain, such as minor injuries and fluid collection, can often be treated with home care. The following steps may reduce discomfort and swelling:
- Provide support to the scrotum by wearing an athletic supporter.
- Apply ice to the scrotum.
- Take warm baths if there are signs of swelling.
- While lying down, place a rolled towel under your scrotum for support and elevation when you’re lying down.
- Take an over-the-counter pain reliever such as aspirin, ibuprofen (Advil, Motrin IB, others) or acetaminophen (Tylenol, others), unless your doctor has given you other instructions. Do NOT give aspirin to children. Though aspirin is approved for use in children older than age 3, children and teenagers recovering from chickenpox or flu-like symptoms should never take aspirin. This is because aspirin has been linked to Reye’s syndrome, a rare but potentially life-threatening condition, in such children.
Take the antibiotics your health care provider gives you if the pain is caused by infection.
Preventive measures to take:
- Prevent injury by wearing an athletic supporter during contact sports.
- Follow safe sex practices. If you are diagnosed with chlamydia or another STD, all of your sexual partners need to be checked to see if they are infected.
- Make sure that children have received the MMR (mumps, measles, and rubella) vaccine.
Testicular pain prognosis
The prognosis of testicular pain depends on the cause. In patients with epididymitis, pain improves within several days of treatment, but the induration may last weeks or months. Some diabetics may develop an abscess and sepsis is a potential consequence. In patients who developed epididymitis secondary to sexual activity, the partner needs to be referred and treated, to stop the cycle of transmission. For patients with a diagnosis of testicular torsion, the diagnosis depends on early diagnosis and treatment. If the treatment is delayed by 12-24 hours, the risk of losing testis and infertility is high 47.
- Wiener SL. Testicular Pain. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 186. Available from: https://www.ncbi.nlm.nih.gov/books/NBK296[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Boniface MP, Mohseni M. Acute Scrotum Pain. [Updated 2018 Dec 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470335[↩][↩][↩]
- Kim JS, Shin YS, Park JK. Clinical features of acute scrotum in childhood and adolescence: Based on 17years experiences in primary care clinic. Am J Emerg Med. 2018 Jul;36(7):1302-1303.[↩]
- Mellick LB, Al-Dhahir MA. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Oct 27, 2018. Cremasteric Reflex.[↩]
- Ringdahl E, Teague L. Testicular torsion. Am Fam Physician. 2006;74:1739–1743.[↩]
- Gordhan CG, Sadeghi-Nejad H. Scrotal pain: evaluation and management. Korean J Urol. 2015;56(1):3-11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4294852/[↩][↩][↩]
- Dogra V, Bhatt S. Acute painful scrotum. Radiol Clin North Am. 2004;42:349–363.[↩]
- Marcozzi D, Suner S. The nontraumatic, acute scrotum. Emerg Med Clin North Am. 2001;19:547–568.[↩][↩][↩][↩][↩][↩][↩]
- Gerber GS, Brendler CB. Evaluation of the urologic patient: history, physical examination, and urinalysis. In: Walsh PC, Retik AB, Vaughan ED Jr, Wein AJ, Kavoussi LR, Novick AC, et al., editors. Campbell’s urology. 8th ed. Philadelphia: Saunders; 2002. pp. 83–110.[↩]
- Rabinowitz R. The importance of the cremasteric reflex in acute scrotal swelling in children. J Urol. 1984;132:89–90.[↩]
- Herbener TE. Ultrasound in the assessment of the acute scrotum. J Clin Ultrasound. 1996;24:405–421.[↩]
- Burgher SW. Acute scrotal pain. Emerg Med Clin North Am. 1998;16:781–809.[↩]
- Boettcher M, Bergholz R, Krebs TF, Wenke K, Treszl A, Aronson DC, et al. Differentiation of epididymitis and appendix testis torsion by clinical and ultrasound signs in children. Urology. 2013;82:899–904.[↩][↩][↩]
- Van Glabeke E, Khairouni A, Larroquet M, Audry G, Gruner M. Acute scrotal pain in children: results of 543 surgical explorations. Pediatr Surg Int. 1999;15:353–357.[↩]
- Santi M, Lava SAG, Simonetti GD, Bianchetti MG, Milani GP. Acute Idiopathic Scrotal Edema: Systematic Literature Review. Eur J Pediatr Surg. 2018 Jun;28(3):222-226.[↩]
- Trojian TH, Lishnak TS, Heiman D. Epididymitis and orchitis: an overview. Am Fam Physician. 2009;79:583–587.[↩]
- Hori S, Tsutsumi Y. Histological differentiation between chlamydial and bacterial epididymitis: nondestructive and proliferative versus destructive and abscess forming: immunohistochemical and clinicopathological findings. Hum Pathol. 1995;26:402–407.[↩]
- Redshaw JD, Tran TL, Wallis MC, deVries CR. Epididymitis: a 21-year retrospective review of presentations to an outpatient urology clinic. J Urol. 2014;192:1203–1207.[↩][↩]
- Hamdan M, Cerabona V. Epididymitis in infants. Apropos of a case and review of the literature. J Urol (Paris) 1991;97:228–229.[↩]
- Haecker FM, Hauri-Hohl A, von Schweinitz D. Acute epididymitis in children: a 4-year retrospective study. Eur J Pediatr Surg. 2005;15:180–186.[↩]
- Cicek T, Cicek Demir C, Coban G, Coner A. Amiodarone induced epididymitis: a case report. Iran Red Crescent Med J. 2014;16:e13929.[↩]
- Gomez Garcia I, Gomez Mampaso E, Burgos Revilla J, Molina MR, Sampietro Crespo A, Buitrago LA, et al. Tuberculous orchiepididymitis during 1978-2003 period: review of 34 cases and role of 16S rRNA amplification. Urology. 2010;76:776–781.[↩][↩]
- Joo JM, Yang SH, Kang TW, Jung JH, Kim SJ, Kim KJ. Acute epididymitis in children: the role of the urine test. Korean J Urol. 2013;54:135–138.[↩]
- Kavoussi PK, Costabile RA. Orchialgia and the chronic pelvic pain syndrome. World J Urol. 2013;31:773–778.[↩][↩]
- Lee HJ, Cheon SH, Ji YH, Moon KH, Kim KS, Park S, et al. Clinical characteristics and surgical outcomes in adolescents and adults with varicocele. Korean J Urol. 2011;52:489–493.[↩]
- Comhaire F, Kunnen M, Nahoum C. Radiological anatomy of the internal spermatic vein(s) in 200 retrograde venograms. Int J Androl. 1981;4:379–387.[↩]
- Kwak N, Siegel D. Imaging and interventional therapy for varicoceles. Curr Urol Rep. 2014;15:399.[↩][↩][↩][↩]
- Agarwal A, Sharma RK, Desai NR, Prabakaran S, Tavares A, Sabanegh E. Role of oxidative stress in pathogenesis of varicocele and infertility. Urology. 2009;73:461–469.[↩]
- Peterson AC, Lance RS, Ruiz HE. Outcomes of varicocele ligation done for pain. J Urol. 1998;159:1565–1567.[↩][↩][↩]
- Pilatz A, Altinkilic B, Kohler E, Marconi M, Weidner W. Color Doppler ultrasound imaging in varicoceles: is the venous diameter sufficient for predicting clinical and subclinical varicocele? World J Urol. 2011;29:645–650.[↩]
- Chiou RK, Anderson JC, Wobig RK, Rosinsky DE, Matamoros A, Jr, Chen WS, et al. Color Doppler ultrasound criteria to diagnose varicoceles: correlation of a new scoring system with physical examination. Urology. 1997;50:953–956.[↩]
- Cho KS, Seo JT. Effect of varicocelectomy on male infertility. Korean J Urol. 2014;55:703–709.[↩][↩]
- Yaman O, Ozdiler E, Anafarta K, Gogus O. Effect of microsurgical subinguinal varicocele ligation to treat pain. Urology. 2000;55:107–108.[↩]
- Kim HT, Song PH, Moon KH. Microsurgical ligation for painful varicocele: effectiveness and predictors of pain resolution. Yonsei Med J. 2012;53:145–150.[↩]
- Davis BE, Noble MJ, Weigel JW, Foret JD, Mebust WK. Analysis and management of chronic testicular pain. J Urol. 1990;143:936–939.[↩][↩]
- Levine L. Chronic orchialgia: evaluation and discussion of treatment options. Ther Adv Urol. 2010;2:209–214.[↩][↩]
- Levine LA, Matkov TG. Microsurgical denervation of the spermatic cord as primary surgical treatment of chronic orchialgia. J Urol. 2001;165(6 Pt 1):1927–1929.[↩][↩][↩][↩][↩][↩][↩]
- Woolf CJ, Salter MW. Neuronal plasticity: increasing the gain in pain. Science. 2000;288:1765–1769.[↩]
- Sinclair AM, Miller B, Lee LK. Chronic orchialgia: consider gabapentin or nortriptyline before considering surgery. Int J Urol. 2007;14:622–625.[↩]
- Basal S, Ergin A, Yildirim I, Goktas S, Atim A, Sizlan A, et al. A novel treatment of chronic orchialgia. J Androl. 2012;33:22–26.[↩]
- Siu W, Ohl DA, Schuster TG. Long-term follow-up after epididymectomy for chronic epididymal pain. Urology. 2007;70:333–335.[↩]
- Werthman P. Vasectomy reversal for post-vasectomy pain syndrome: a ten-year experience. J Urol. 2010;183(Suppl):e752.[↩]
- Myers SA, Mershon CE, Fuchs EF. Vasectomy reversal for treatment of the post-vasectomy pain syndrome. J Urol. 1997;157:518–520.[↩]
- Strom KH, Levine LA. Microsurgical denervation of the spermatic cord for chronic orchialgia: long-term results from a single center. J Urol. 2008;180:949–953.[↩][↩][↩]
- Larsen SM, Benson JS, Levine LA. Microdenervation of the spermatic cord for chronic scrotal content pain: single institution review analyzing success rate after prior attempts at surgical correction. J Urol. 2013;189:554–558.[↩][↩]
- Pogorelić Z, Mustapić K, Jukić M, Todorić J, Mrklić I, Mešštrović J, Jurić I, Furlan D. Management of acute scrotum in children: a 25-year single center experience on 558 pediatric patients. Can J Urol. 2016 Dec;23(6):8594-8601.[↩]
- Rottenstreich M, Glick Y, Gofrit ON. The clinical findings in young adults with acute scrotal pain. Am J Emerg Med. 2016 Oct;34(10):1931-1933.[↩]