Contents
What is total parenteral nutrition
Total parenteral nutrition (TPN) is a way of supplying all the nutritional needs of the body by bypassing the digestive system and dripping nutrient solution directly into a vein. Total parenteral nutrition is used when individuals cannot or should not get their nutrition through eating. Total parenteral nutrition is used when the intestines are obstructed, when the small intestine is not absorbing nutrients properly or a gastrointestinal fistula (abnormal connection) is present. Total parenteral nutrition (TPN) is also used when the bowels need to rest and not have any food passing through them. Bowel rest may be necessary in Crohn’s disease, pancreatitis, ulcerative colitis, and with prolonged bouts of diarrhea in young children. total parenteral nutrition is also used for individuals with severe burns, multiple fractures, and in malnourished individuals to prepare them for major surgery, chemotherapy, or radiation treatment. Individuals with AIDS or widespread infection (sepsis) may also benefit from total parenteral nutrition. Total parenteral nutrition (TPN) is also used for patients who have gastroparesis and cannot digest food properly.
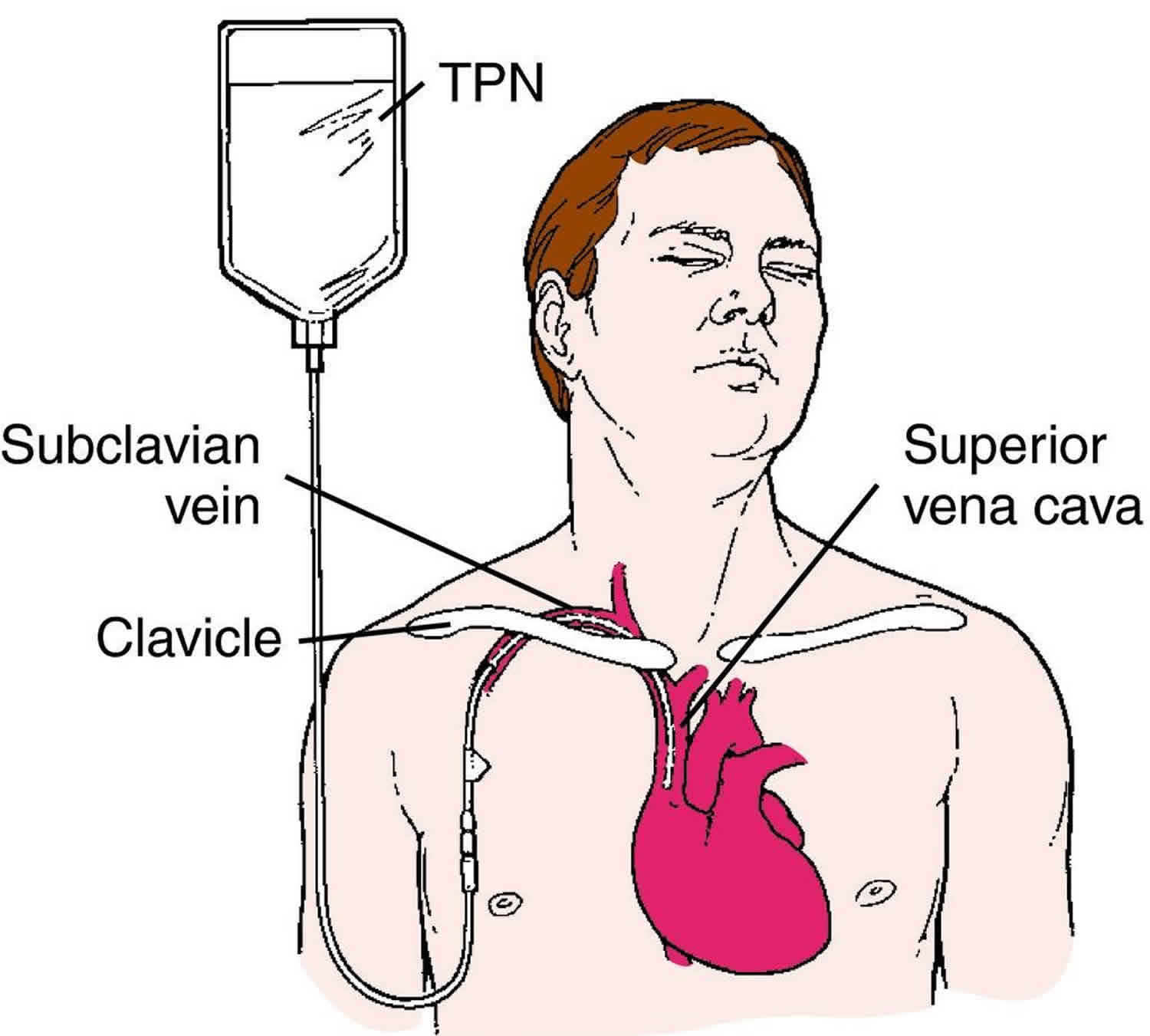
Total parenteral nutrition is normally given through a large central vein, generally through a PICC (peripherally inserted central catheter) line, but can also be administered through a central line or port-a-cath. A catheter is inserted into the vein in the chest area under local anesthesia and sterile conditions. Often the placement is done in an operating room to decrease the chance of infection. Several different types catheters are used based on the reason total parenteral nutrition is needed and the expected length of treatment. Once the catheter is in place, a chest x ray is done to make sure the placement is correct.
Normally total parenteral nutrition is administered in a hospital, but under certain conditions and with proper patient and caregiver education, it may also be used at home for long-term therapy. total parenteral nutrition solution is mixed daily under sterile conditions. Maintaining sterility is essential for preventing infection. For this reason, the outside tubing leading from the bag of solution to the catheter is changed daily, and special dressings covering the catheter are changed every other day.
Patients may be on total parenteral nutrition for many weeks or months until their issues resolve. Throughout the course of therapy, patients may or may not be able to ingest anything orally; whatever the case, they will not get any substantive nutrition via the oral route.
Because patients are not getting any other true form of nutrition, the total parenteral nutrition formula needs to contain all of the essential nutrients a body needs to be healthy. This includes proteins, carbohydrates, fats, electrolytes, vitamins, and minerals. There are standard formulations that are available, and these are often what are used by large hospital systems. Infusion Solutions, however, batches each total parenteral nutrition formula to meet the individual dietary needs of the patient. This leads to optimal nutrition and a better chance of restoring health.
The total parenteral nutrition formulation is a complex mixture containing up to 40 different chemical components that may cause problems with stability and compatibility. Serious harm and death have resulted from improperly compounded parenteral feeding formulations.
The contents of the total parenteral nutrition solution are determined based on the age, weight, height, and the medical condition of the individual. All solutions contain sugar (dextrose) for energy and protein (amino acids). Fats (lipids) may also be added to the solution. Electrolytes such as potassium, sodium, calcium, magnesium, chloride, and phosphate are also included, as these are essential to the normal functioning of the body. Trace elements such as zinc, copper, manganese and chromium are also needed. Vitamins can be included in the total parenteral nutrition solution, and insulin, a hormone that helps the body use sugar, may need to be added. Adults need approximately 2 liters of total parenteral nutrition solution daily, although this amount varies with the age, size, and health of the individual. Special solutions have been developed for individuals with reduced liver and kidney function.
The formula can be adjusted as necessary based on lab markers and the progress of the disease state. The rate of total parenteral nutrition administration can also be changed under some circumstances. Generally, patients are initially started on a continuous cycle and are given their total parenteral nutrition over a 24 hour period. As patients progress, it may be possible to move to an 18, 15, or even a 12-hour infusion cycle. This can certainly improve the quality of life for those patients managing this infusion at home.
The total parenteral nutrition itself comes in a 2-3 liter bag, and most patients infuse one bag per day. The bag itself is connected to a portable infusion pump that has been pre-programmed by the pharmacy team to deliver the total parenteral nutrition over a specified amount of time. The whole system fits nicely into a small backpack that can be worn by the patient or hung nearby throughout the infusion. As with all home infusion therapies, the intent is for the patient to be as mobile as he or she would like to accommodate their lifestyle.
Successful total parenteral nutrition requires frequent, often daily monitoring of the individual’s weight, glucose (blood sugar) level, blood count, blood gasses, fluid balance, urine output, waste products in the blood (plasma urea) and electrolytes. Liver and kidney function tests may also be performed. The contents of the solution are individualized based on the results of these tests.
Total parenteral nutrition calculations
This total parenteral nutrition calculator (https://clincalc.com/TPN/Macronutrients.aspx) provides an empiric dose for the macronutrients included in a total parenteral nutrition formulation. In addition to providing an initial recommended dose, you may alter the contents of each macronutrient while maintaining a specified daily caloric requirement.
- Osmolarity = measure of solute concentration, defined as the number of osmoles (Osm) of solute per liter (L) of solution (Osm/L)
- Osmolality = measure of osmoles of solute per kilogram of solvent (Osm/kg)
Osmolarity of total parenteral nutrition calculations
- Dextrose% X 50
- Amino Acid% X 100
- All electrolytes combined in mEq/L X 2
- Total = TPN Osmolarity
Total parenteral nutrition Osmolarity Calculator (http://www.rxkinetics.com/tpnosmolcalc.html).
Energy requirement
Harris-Benedict equation + activity +infection/fever factor = Energy (Kcal)
The Harris–Benedict equation (also called the Harris-Benedict principle) is a method used to estimate an individual’s basal metabolic rate (BMR). The estimated BMR value may be multiplied by a number that corresponds to the individual’s activity level; the resulting number is the approximate daily kilocalorie intake to maintain current body weight.
Men BMR = (10 × weight in kg) + (6.25 × height in cm) – (5 × age in years) + 5
Women BMR = (10 × weight in kg) + (6.25 × height in cm) – (5 × age in years) – 161
- Scale:
- Normal need: 25-30 kcal/kg/day
- Elective surgery: 28-30 kcal/kg/day
- Severe injury: 30-40 kcal/kg/day
- Extensive trauma/burn: 45-55 kcal/kg/day
Dextrose
- Primary energy source
- 70% => 70 g/100 ml
- 3.4 kcal/g
- 45 -60% total kcal
Glucose Infusion Rate
Dextrose Infusion Rate (DIR) or Glucose Infusion Rate (GIR)
- Glucose Infusion Rate (GIR) = _____ mg / kg / min
- Steps to calculate Glucose Infusion Rate (GIR):
- Convert grams to milligrams
- Divide by patient’s weight in kilogram (kg)
- Divide by minutes per day
Amino Acid
- Crystalline L-amino acid solution – 100% utilizable
- 10% => 10 g / 100 mL
- 15% => 15 g / 100 mL
- 10-20% total kcal
- Hypertonic
- 4 kcal /gram
Fat
- 20-40% of total kcal
- Most common is 20% soybean oil emulsion
- 10% fat emulsion = 1.1 kcal/mL
- 20% fat emulsion = 2 kcal/mL
- 30% fat emulsion = 3 kcal/mL (only used as ingredient of 3 in 1)
Fat Requirements
- To prevent essential fatty acid deficiency, 2 2-4% of kcal should come from linoleic acid (~10% of total kcal from lipid)
- Fat should generally provide 20 20-40% of total kcal
- Maximal fat dosage should not exceed 60% of total kcal
Lipid dose = ____ g/kg/day
- Convert milliliters to grams lipid
- Divide by weight
Hourly Lipid Infusion Rate = ___ g/kg/hour
- Convert milliliters to grams lipid
- Divide by weight
- Divide by infusion time in hours
- Max 0.11 g/kg/hour
Calculating Parenteral Fluids Volume
- Methods of Calculating Fluids Volume:
- mL per kcal: 1-1.5 mL/kcal
- mL per kg:
- >65 years old, 25mL/kg fluid
- 55 -65 years old, 30mL/kg fluid
- 30 -55 years old, 35mL/kg fluid
- 30 years old, 40mL/kg fluid
- Holliday-Segar
- <10 kg, 100 mL/kg
- 10-20 kg, 1000 mL + 50 mL/kg for every kg between between 10 -20 kg
- >20 kg, 1500 mL + 20 mL/kg for every kg >20 kg
- 4-2-1 rule
- <10 kg, 4 mL/kg/hr
- 10-20 kg, 40 mL/hr + 2 mL/kg/hr for every kg between 10-20kg
- >20 kg, 60 mL/hr + 1 mL/kg/hr for every kg >20 kg
Cycling
Initial administration 24 hours (continuous)
- Especially for critically ill patients
- Minimizes glucose, fluid, and electrolyte abnormalities
Eventually may be able to “cycle” total parenteral nutrition
- 8-22 hour infusion time
- Decrease infusion time gradually over several days to weeks depending on patient age/status
- Titrate total parenteral nutrition infusion rate over 1-2 hours (i.e., ramp up and down over 1 1-2 hours to cycle up and cycle down total parenteral nutrition)
- Helps prevent hyper hyper-and hypoglycemia
- Improves quality of life
- May reduce intestinal failure associated liver disease
- Cycling Example:
- Cycle 2000 mL total parenteral nutrition over 20 hours: 1 h – 1 h – 16 h – 1 h – 1 h
Total parenteral nutrition procedure
Vascular Access
- Individualize access device selection
- Risk / benefit
- Clinical factors
- Psychosocial considerations
- Fewest lumens possible
- Dedicate 1 lumen to total parenteral nutrition when able
- Position tip in lower third of the superior vena cava near the junction with the right atrium
- Confirm optimal position before initiating total parenteral nutrition
Central-Line
- Distal catheter tip in vena cava or right atrium
- Access sites: subclavian, jugular, femoral, cephalic, and basilic veins
- Provides access for infusion and blood aspiration
- Placement is verified by chest X-ray or fluoroscopy
- Ideal for hyperosmolar solutions
Mid-Line
- 3 to 8 inches in length
- Inserted into main veins of arm
- Tip rests in proximal limb
- Decreased phlebitis
- Increased dwell time
Peripheral-Line
- Access is easy to establish
- Intended for short term use
- Central access is not feasible
- Limited osmolarity (900mOsm/kg)
- Complication – phlebitis
- Extend < 3 inches into vein
Know your total parenteral nutrition fluids
- Read the medicine sheet that comes with the total parenteral nutrition. Be aware of any warnings and side effects.
- Check the label on the total parenteral nutrition bag before starting an IV. Make sure the patient name, total parenteral nutrition fluids, and dose are correct.
- Don’t use total parenteral nutrition with an expired date.
- Don’t use total parenteral nutrition if the bag is leaking.
- Don’t use total parenteral nutrition if it looks lumpy or oily.
- Don’t use total parenteral nutrition if anything is floating in it.
Handle supplies as directed
- Store total parenteral nutrition in the refrigerator. If it’s not kept cold, total parenteral nutrition lasts only 24 hours. Don’t freeze.
- Before using total parenteral nutrition, let it get close to room temperature. Don’t heat.
- If vitamins need to be added to the total parenteral nutrition, do so as directed.
- Put all used needles and syringes in a special container (sharps container).
- When the IV is done, put the used supplies in a plastic bag. Seal the bag and throw it in the trash.
Track your health
- Weigh yourself daily. If you lose or gain weight, your total parenteral nutrition dose may need adjusting.
- Keep track of your urine output as directed. Tell the nurse if the amount increases or decreases a lot.
- Check your blood sugar if directed. A nurse may take a blood sample from you each week. This is to make sure your total parenteral nutrition dose is right for you.
Know these IV basics
- Keep the dressing over the catheter exit site clean and dry. Change the dressing if it comes loose or gets soiled or wet.
- Flush the catheter with saline or heparin as directed.
- Wipe all injection sites with alcohol.
- Be sure all IV supplies are in sealed packets. If sterile packets are open, throw away those supplies.
- Do not stop the pump during an IV infusion unless a nurse tells you to.
Call your healthcare provider right away if you have any of the following:
- Trouble breathing – call your local emergency services number
- Redness near the catheter exit site or at any spot along the catheter line
- Fever or chills
- Swelling in the arm, neck, or chest
- Drainage at the exit site
- The catheter slips or comes out
- The total parenteral nutrition doesn’t flow well through the tubing
- The alarm on the pump comes on
Total parenteral nutrition guidelines
Total parenteral nutrition indications
Adults
- “Initiate total parenteral nutrition after 7 days for well well-nourished, stable adult patients who have been unable to receive significant (50% or more of estimated requirements) oral or enteral nutrients”
- “Initiate total parenteral nutrition within 3-5 days in those who are nutritionally nutritionally-at -risk and unlikely to achieve desired oral intake or enteral nutrition”
- “Initiate total parenteral nutrition as soon as is feasible for patients with baseline moderate or severe malnutrition in whom oral intake or enteral nutrition is not possible or sufficient”
Children
- “Consider total parenteral nutrition for neonates in the critical care setting, regardless of diagnosis, when enteral nutrition is unable to meet energy requirements for energy expenditure and growth”
- “Use total parenteral nutrition for children when the intestinal tract is not functional or cannot be accessed or when nutrient needs to provide for growth are greater than that which can be provided through oral intake or enteral nutrition support alone”
- “Initiate total parenteral nutrition within 1 1-3 days in infants and within 4 4-5 days in older children and adolescents when it is evident that they will not tolerate full oral intake or enteral nutrition for an extended period”
- “Begin total parenteral nutrition promptly after birth in the very low birth weight infant (<1500g)”
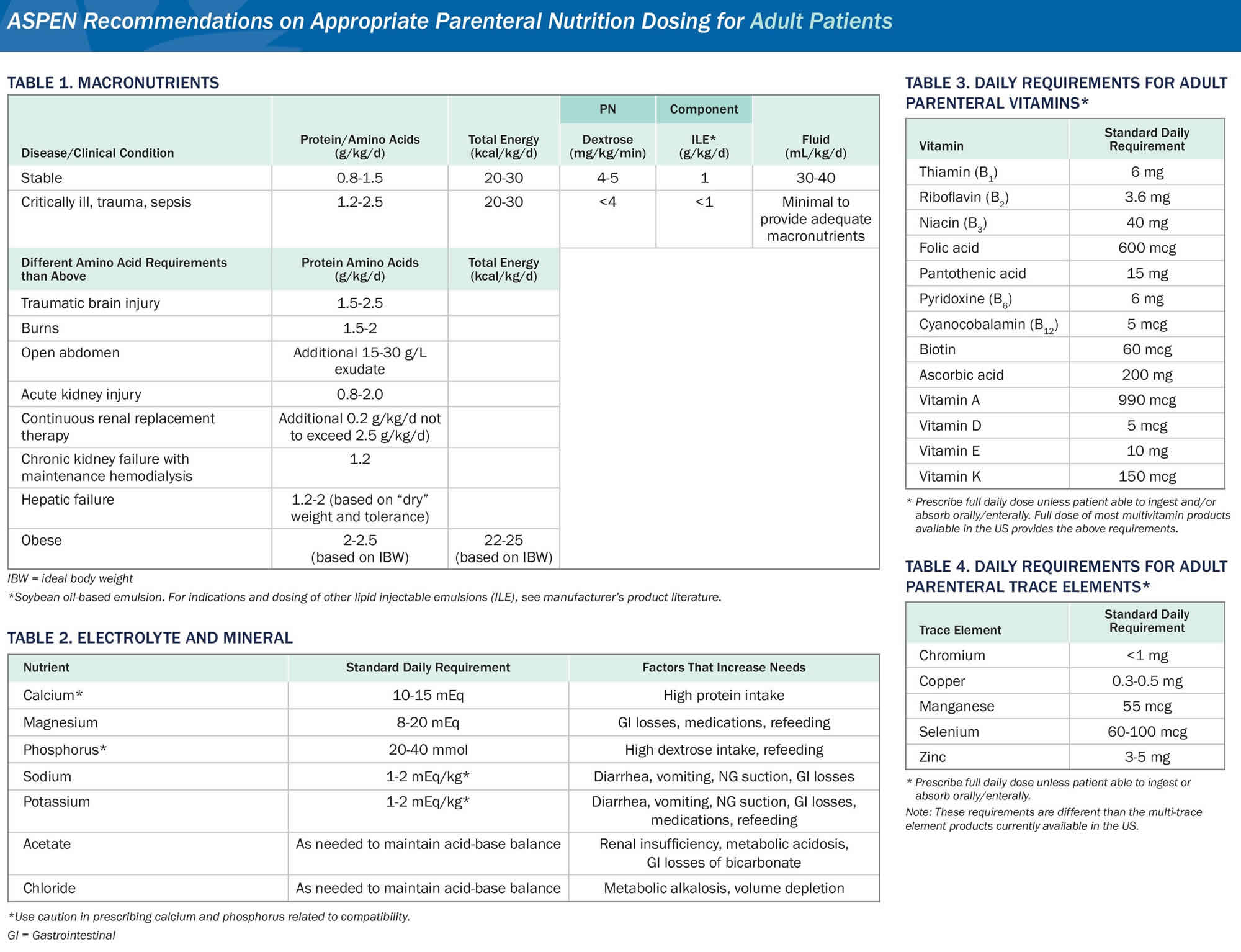
Figure 1. Total parenteral nutrition guidelines adults
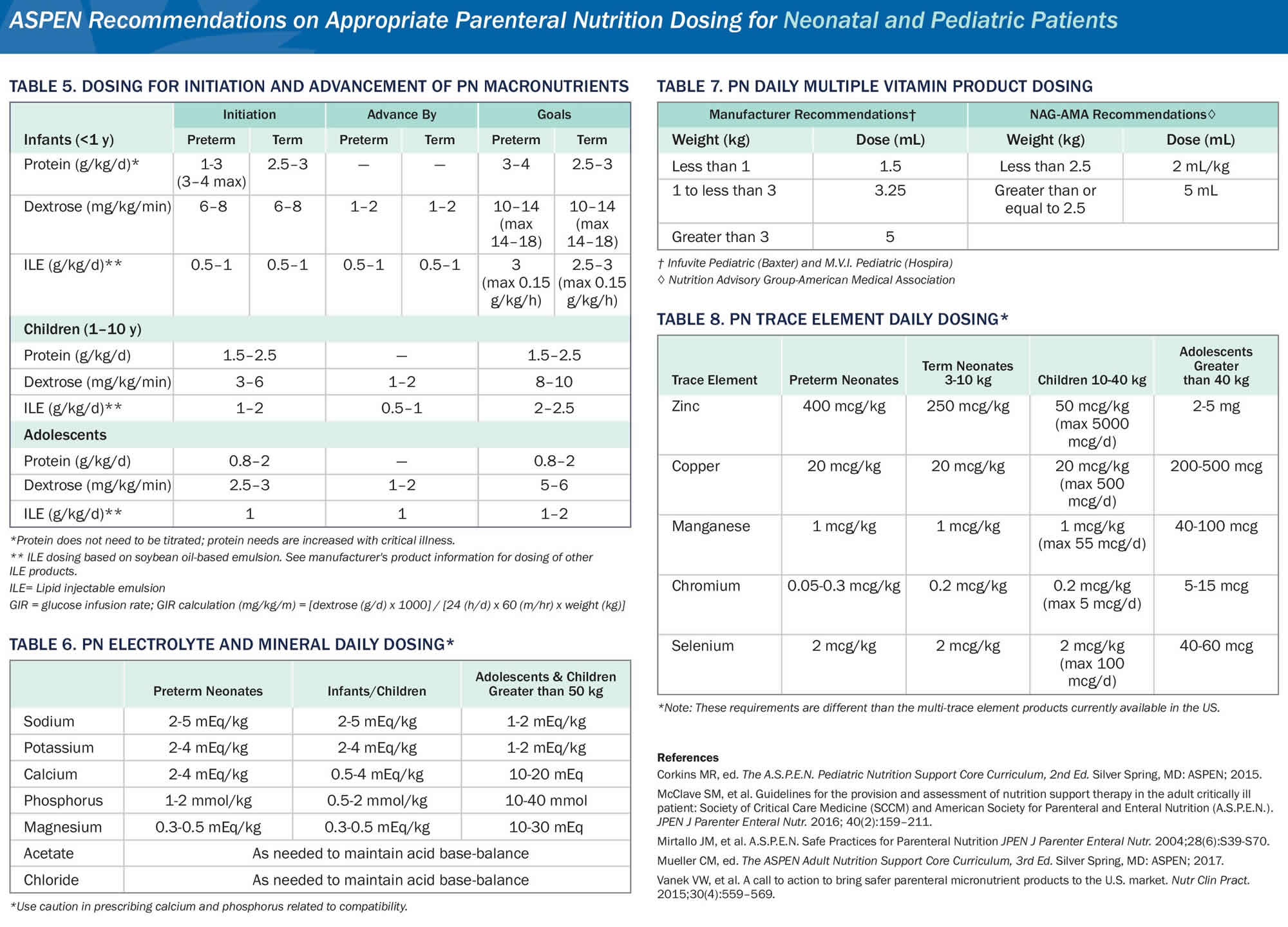
[Source American Society for Parenteral and Enteral Nutrition (ASPEN) 1 ]Figure 2. Total parenteral nutrition guidelines for children
[Source American Society for Parenteral and Enteral Nutrition (ASPEN) 1 ]Total parenteral nutrition complications
Total parenteral nutrition complications include:
Mechanical complications
Mechanical complications are primarily related to the initial placement of a central venous catheter. Improper placement may cause pneumothorax, vascular injury with hemothorax, brachial plexus injury or cardiac arrhythmia.
Venous thrombosis is one of the two most common problems that occur after central venous access is established. The other is infection. Venous thrombosis is associated with significant morbidity rates. Signs include distended neck veins and swelling of the face and ipsilateral arm. The risk of venous thrombosis is greater if patients are dehydrated, have certain malignancies, have had prolonged bed rest, have venous stasis, have sepsis, or have hypercoagulation. Additional risk factors include morbid obesity, smoking, or ongoing estrogen therapy.
Mechanical complications:
- Hemothorax
- Pneumothorax
- Arterial puncture
- Air embolism
- Nerve damage
- Thoracic duct damage
- Hematoma
- Misplaced catheter
Infections
Total parenteral nutrition imposes a chronic breech in the body’s barrier system. The infusion apparatus from container to catheter tip may prove a source for the introduction of bacterial or fungal organisms.
Infection is one of the two most common problems that arise after central venous access is established. The other is venous thrombosis, discussed earlier. The mortality rate from catheter sepsis may be as high as 15%.
The primary preventive measures include adhering to strict aseptic procedure while establishing access and providing care of the dressing and line, and prohibiting the use of the total parenteral nutrition line for other purposes. Other preventive measures include:
- Changing the dressing routinely (every 48-72 hours) or when it becomes soiled, wet or loose. The care-giver should wear a mask and gloves while changing the dressing.
- Extending the application of antimicrobial solution at least 1 inch beyond the final dressing.
- Placing a sterile sponge over the catheter, then placing an occlusive dressing.
- Inspecting the site for tenderness, erythema, edema, loose sutures, or drainage.
- Changing the total parenteral nutrition intravenous tubing every 48 hours. A 0.22 μm in-line filter should be used whenever fat is not being infused.
- Avoiding violation of total parenteral nutrition catheters for central venous pressure monitoring or the administration of intravenous medications or blood products.
Metabolic complications
Metabolic complications fall into two broad categories: early and late complications. Those in the first category occur early in the process of feeding and may be anticipated. They are avoided by careful monitoring and appropriate adjustment of intake. Late metabolic complications are less predictable. They may be caused by an exacerbation of preexisting abnormalities, unpredictable long-term requirements, inadequate solution composition, or failure to monitor adequately.
Metabolic complications of total parenteral nutrition:
Early complications
- Volume overload
- Hyerglycemia
- Refeeding syndrome
- Hypokalemia
- Hypophosphatemia
- Hypomagnesemia
- Hyperchloremic acidosis
Late complications
- Essential fatty acid deficiency
- Trace mineral deficiency
- Vitamin deficiency
- Metabolic bone disease
- Hepatic steatosis
- Hepatic cholestasis
Fluid and electrolyte imbalance
Electrolyte management is one of the most difficult aspects of total parenteral nutrition therapy. Often electrolytes are outside of the normal range based on an underlying cause rather than directly related to the total parenteral nutrition solution. For this reason, no specific guidance can be given to adjust individual electrolytes based on laboratory serum concentration. Instead, incremental dose adjustments are made concurrent with treatment of the underlying cause of electrolyte abnormality. In general, supplemental electrolyte doses in response to an acute underlying condition are best managed outside of total parenteral nutrition therapy.
Table 1. Sodium – Normal = 135 – 145 mEq/L
| Excess (Hypernatremia) | Deficiency (Hyponatremia) | |
|---|---|---|
| Contributing Factors |
|
|
| Signs & symptoms |
|
|
| Intervention |
|
|
Table 2. Potassium – Normal = 3.5 – 5.0 mEq/L
| Excess (Hyperkalemia) | Deficiency (Hypokalemia) | |
|---|---|---|
| Contributing Factors |
|
|
| Signs & Symptoms |
|
|
| Intervention |
|
|
Table 3. Magnesium – Normal = 1.5 – 2.0 mEq/L
| Excess (Hypermagnesemia) | Deficiency (Hypomagnesemia) | |
|---|---|---|
| Contributing Factors |
|
|
| Signs & Symptoms |
|
|
| Intervention |
|
|
Table 4. Calcium – Normal = 8.5 – 10.5 mg/dl
| Excess (Hypercalcemia) | Deficiency (Hypocalcemia) | |
|---|---|---|
| Contributing Factors |
|
|
| Signs & Symptoms |
|
|
| Intervention |
|
|
Table 5. Phosphorus – Normal = 3.0 – 4.5 mg/dl
| Excess (Hyperphosphatemia) | Deficiency (Hypophosphatemia) | |
|---|---|---|
| Contributing Factors |
|
|
| Signs & Symptoms |
|
|
| Intervention |
|
|
Refeeding syndrome
Refeeding of severely malnourished patients may result in “refeeding syndrome” in which there are acute decreases in circulating levels of potassium, magnesium, and phosphate. The consequences of refeeding syndrome adversely affect nearly every organ system and include cardiac dysrhythmias, heart failure, acute respiratory failure, coma, paralysis, nephropathy, and liver dysfunction.
The primary cause of the metabolic response to refeeding is the shift from stored body fat to carbohydrate as the primary fuel source. Serum insulin levels rise, causing intracellular movement of electrolytes for use in metabolism.
The best advice when initiating nutritional support is to “start low and go slow”.
Recommendations to reduce the risk of refeeding syndrome include:
- Recognize patients at risk
- Anorexia nervosa
- Classic kwashiorkor or marasmus
- Chronic malnutrition
- Chronic alcoholism
- Prolonged fasting
- Prolonged IV hydration
- Significant stress and depletion
- Correct electrolyte abnormalities before starting nutritional support
- Administer volume and energy slowly
- Monitor pulse, input and output, electrolytes closely
- Provide appropriate vitamin supplementation
- Avoid overfeeding
Total parenteral nutrition side effects
Central-vein total parenteral nutrition is associated with mechanical, metabolic, and infectious complications 2. Such complications are much more common when parenteral nutrition is not properly administered and when current standards of practice are not applied 3. Complications such as pneumothorax, bleeding, and thrombus formation can occur owing to the insertion of the central venous catheter, which is typically performed as a component of usual critical care. Catheter-related and non–catheter-related infections are not uncommon and are associated with hyperglycemia 4, the use of internal jugular-vein or femoral-vein central venous catheters, and the use of nondedicated infusion ports for parenteral nutrition 5.
Overfeeding (the administration of excess dextrose, fat, or calories) and the refeeding syndrome (rapid feeding of patients with preexisting malnutrition) can induce a variety of metabolic complications during parenteral nutrition 6. Accelerated carbohydrate metabolism increases the body’s use of thiamine and can precipitate symptoms and signs of thiamine deficiency 7. Insulin has an antinatriuretic effect 8, which, when coupled with increased sodium and fluid intake during refeeding, can cause a rapid expansion of the volume of extracellular fluid in some patients 7. Decreased levels of blood electrolytes can induce cardiac arrhythmias. In cases, these result in heart failure, particularly in patients with preexisting cardiac dysfunction 7. Other metabolic effects can include hypercapnia, hepatic steatosis, neuromuscular dysfunction, and immunologic defects.
- http://www.nutritioncare.org/uploadedFiles/Documents/Guidelines_and_Clinical_Resources/PN%20Dosing%201-Sheet-FINAL.pdf[↩][↩]
- ASPEN Board of Directors, Clinical Guidelines Task Force Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. JPEN J Parenter Enteral Nutr. 2002;26(Suppl):1SA–138SA. [Erratum, JPEN J Parenter Enteral Nutr 2002;26:144.][↩]
- Ziegler TR. Parenteral nutrition in the critically ill patient. N Engl J Med. 2009;361(11):1088–1097. doi:10.1056/NEJMct0806956 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3064749[↩]
- Elke G, Schädler D, Engel C, et al. Current practice in nutritional support and its association with mortality in septic patients — results from a national, prospective, multicenter study. Crit Care Med. 2008;36:1762–7.[↩]
- Mirtallo J, Canada T, Johnson D, et al. Safe practices for parenteral nutrition. JPEN J Parenter Enteral Nutr. 2004;28:S39–S70. [Erratum, JPEN J Parenter Enteral Nutr 2006;30:177.][↩]
- Stanga Z, Brunner A, Leuenberger M, et al. Nutrition in clinical practice — the refeeding syndrome: illustrative cases and guidelines for prevention and treatment. Eur J Clin Nutr. 2008;62:687–94 [↩]
- Stanga Z, Brunner A, Leuenberger M, et al. Nutrition in clinical practice — the refeeding syndrome: illustrative cases and guidelines for prevention and treatment. Eur J Clin Nutr. 2008;62:687–94[↩][↩][↩]
- Quiñones-Galvan A, Ferrannini E. Renal effects of insulin in man. J Nephrol. 1997;10:188–91[↩]