Contents
- What is tuberculin skin test
- What is Latent Tuberculosis Infection and Tuberculosis Disease?
- What does the tuberculin skin test measure?
- Who should be tested for tuberculosis infection?
- When should I get a tuberculin skin test?
- Who can receive a tuberculin skin test?
- Are tuberculin skin test results accurate?
- Do I need follow-up tests?
- Testing for tuberculosis in BCG-vaccinated people
- Can tuberculin skin tests be given to persons receiving vaccinations?
- How often can tuberculin skin tests be repeated?
- What is a boosted reaction?
- Why is two-step testing conducted?
- Tuberculin skin test results
- Tuberculin vaccine
What is tuberculin skin test
Tuberculin is also called tuberculin PPD (purified protein derivative), which is a solution Mycobacterium tuberculosis complex antigens 1. Tuberculin skin test is also known as the Mantoux test or Mantoux tuberculin skin test, is a skin test to detect if you have been infected with tuberculosis bacteria (Mycobacterium tuberculosis). A tuberculin skin test is used to screen for tuberculosis infection when someone has potentially been exposed to tuberculosis. Tuberculin skin test is also used as a diagnostic tool when someone is showing symptoms of tuberculosis disease. This test is conducted by injecting a small amount of testing fluid called tuberculin into the inside of your forearm and measuring the resulting swelling several days later.
A tuberculin skin test is used to detect exposure to tuberculosis bacteria by measuring your immune response to an inactivated or killed version of Mycobacterium tuberculosis.
If you have had prior exposure to the tuberculosis bacteria (Mycobacterium tuberculosis), antibodies are formed and remain in your body. During the tuberculin purified protein derivative (PPD) skin test, the tuberculosis antigen (inactivated or killed version of Mycobacterium tuberculosis) is injected under your skin and if antibodies are present, your body will have an immune response. There will be an area of inflammation at the site of the injection. Reliable administration and reading of the tuberculin skin test requires standardization of procedures, training, supervision, and practice.
A tuberculin skin test detects if a patient has ever been infected with tuberculosis bacteria (Mycobacterium tuberculosis) but does not determine if a patient currently has tuberculosis infection or tuberculosis disease. Further testing is required to confirm or rule-out a diagnosis of tuberculosis disease.
There are two tuberculosis-related conditions.
- The first is called tuberculosis infection or latent tuberculosis infection. Tuberculosis infection describes a stage of tuberculosis in which a person’s immune system is able to control the infection. Patients with tuberculosis infection or latent tuberculosis infection don’t become ill or spread tuberculosis to others, but may develop tuberculosis disease if left untreated.
- The second is referred to as tuberculosis disease, active tuberculosis, or reactivation tuberculosis. Tuberculosis disease occurs in 5 to 10% of people with tuberculosis infection. Patients with tuberculosis disease usually develop symptoms of tuberculosis and can spread tuberculosis to others.
A tuberculin skin test may be performed to screen for tuberculosis infections or to assist in diagnosing tuberculosis disease:
- Screening for tuberculosis infection: Screening for tuberculosis infection means testing for TB in a patient without symptoms. Screening is often conducted when someone has a high risk of having tuberculosis and would benefit from treatment if a tuberculosis infection is diagnosed.
- Diagnosing tuberculosis disease: Diagnostic tests are used when a patient has symptoms of tuberculosis. A positive tuberculin skin test supports a diagnosis of tuberculosis disease. In addition to the results of a tuberculin skin test, doctors consider a patient’s medical history and the results of a physical exam, imaging, and other lab tests to diagnose tuberculosis disease.
A tuberculin skin test requires two visits with a health care provider. On the first visit the tuberculin purified protein derivative (PPD) skin test is placed; on the second visit the health care provider reads the test result. A person given the tuberculin skin test must return within 48 to 72 hours to have a trained health care worker look for a reaction on the arm.
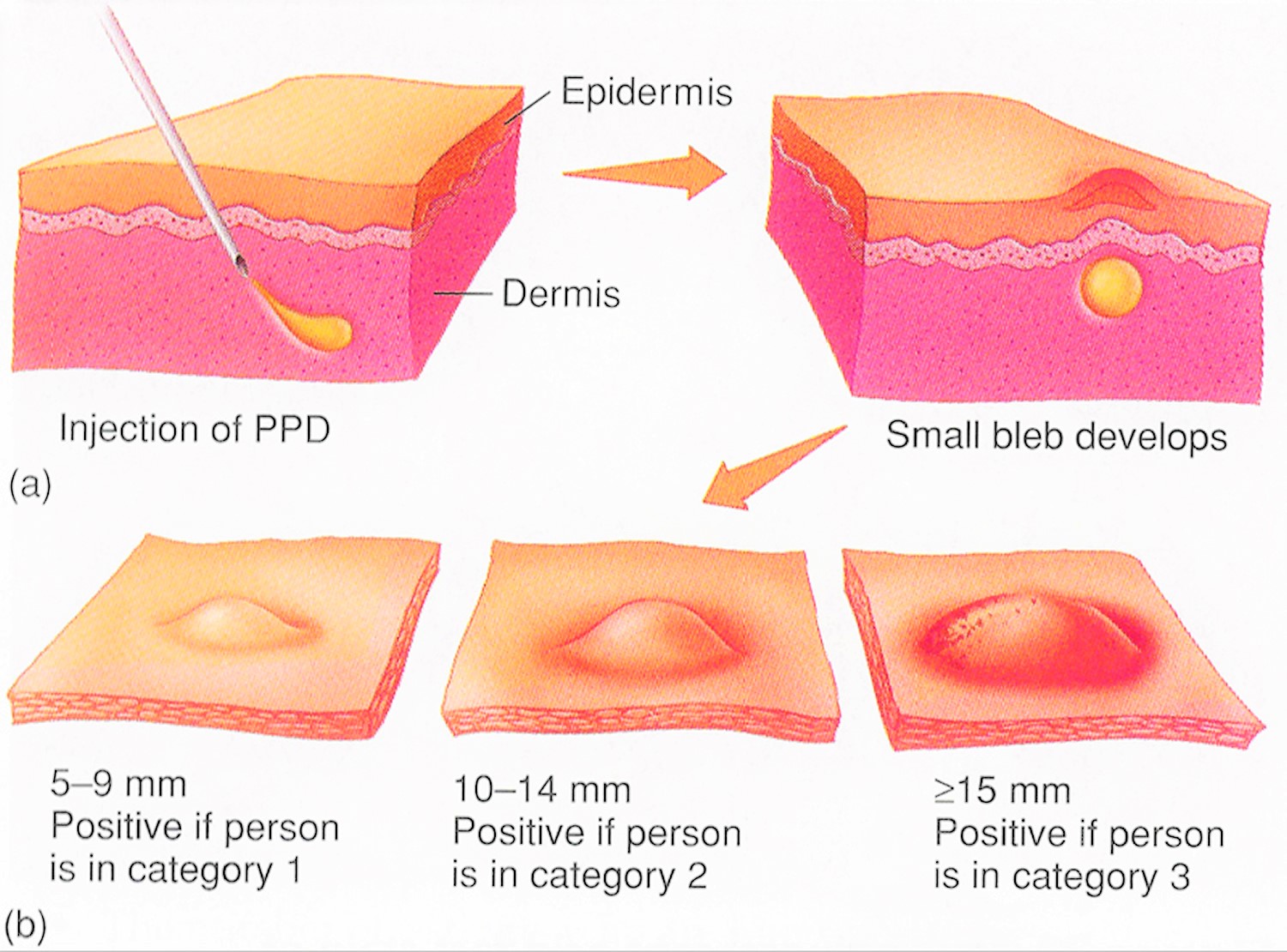
The tuberculin skin test is performed by injecting 0.1 ml of tuberculin purified protein derivative (PPD) into the inner surface of the forearm. The injection should be made with a tuberculin syringe, with the needle bevel facing upward. The tuberculin skin test is an intradermal injection. When placed correctly, the injection should produce a pale elevation of the skin (a wheal) 6 to 10 mm in diameter.
The tuberculin skin test reaction should be read between 48 and 72 hours after administration. A patient who does not return within 72 hours will need to be rescheduled for another tuberculin skin test as soon as possible.
The reaction should be measured in millimeters of the induration (palpable, raised, hardened area or swelling). The reader should not measure erythema (redness). The diameter of the indurated area should be measured across the forearm (perpendicular to the long axis).
The result of the tuberculin skin test depends on the size of the raised, hard area or swelling.
- Positive tuberculin skin test: This means the person’s body was infected with tuberculosis bacteria. Additional tests are needed to determine if the person has latent tuberculosis infection or tuberculosis disease. Other tests, such as a chest x-ray and a sample of sputum, are needed to see whether the person has tuberculosis disease.
- Negative tuberculin skin test: This means the person’s body did not react to the test, and that latent tuberculosis infection or tuberculosis disease is not likely.
There is no problem in repeating a tuberculosis skin test. If repeated, the additional test should be placed in a different location on the body (e.g., other arm).
The tuberculosis skin test is the preferred tuberculosis test for children under the age of five.
Figure 1. Tuberculin PPD skin test
Figure 2. Tuberculosis test pictures
Figure 3. Positive tuberculin skin test
What is Latent Tuberculosis Infection and Tuberculosis Disease?
Not everyone infected with tuberculosis bacteria (Mycobacterium tuberculosis) becomes sick. As a result, two TB-related conditions exist: latent tuberculosis infection (LTBI) and tuberculosis disease 2.
- Latent Tuberculosis Infection (LTBI). Tuberculosis bacteria (Mycobacterium tuberculosis) can live in the body without making you sick. This is called latent tuberculosis infection (LTBI). In most people who breathe in TB bacteria and become infected, the body is able to fight the bacteria to stop them from growing. People with latent tuberculosis infection (LTBI):
- Have no symptoms
- Don’t feel sick
- Can’t spread TB bacteria to others
- Usually have a positive tuberculin skin test reaction or positive TB blood test
- May develop tuberculosis disease if they do not receive treatment for latent tuberculosis infection (LTBI)
- Many people who have latent tuberculosis infection (LTBI) never develop tuberculosis disease. In these people, the tuberculosis bacteria (Mycobacterium tuberculosis) remain inactive for a lifetime without causing disease. But in other people, especially people who have a weak immune system, the bacteria become active, multiply, and cause tuberculosis disease.
- Tuberculosis Disease (active tuberculosis). Tuberculosis bacteria (Mycobacterium tuberculosis) become active if your immune system can’t stop them from growing. When TB bacteria are active (multiplying in your body), this is called tuberculosis disease. People with tuberculosis disease are sick. They may also be able to spread the bacteria to people they spend time with every day.
Many people who have latent tuberculosis infection (LTBI) never develop tuberculosis disease. Some people develop tuberculosis disease soon after becoming infected (within weeks) before their immune system can fight the tuberculosis bacteria (Mycobacterium tuberculosis). Other people may get sick years later when their immune system becomes weak for another reason.
For people whose immune systems are weak, especially those with HIV infection, the risk of developing tuberculosis disease is much higher than for people with normal immune systems.
Table 1. Difference between Latent Tuberculosis Infection (LTBI) and Tuberculosis Disease
| A Person with Latent Tuberculosis Infection (LTBI) | A Person with Tuberculosis Disease |
|---|---|
| Has NO symptoms | Has symptoms that may include:
|
| Does not feel sick | Usually feels sick |
| Cannot spread TB bacteria to others | May spread TB bacteria to others |
| Usually has a skin test or blood test result indicating TB infection | Usually has a skin test or blood test result indicating TB infection |
| Has a normal chest x-ray and a negative sputum smear | May have an abnormal chest x-ray, or positive sputum smear or culture |
| Needs treatment for latent TB infection to prevent TB disease | Needs treatment to treat TB disease |
What does the tuberculin skin test measure?
A tuberculin skin test measures a person’s immune response to a testing solution that is made from Mycobacterium tuberculosis antigens. Antigens are protein markers that exist on the surface of the bacteria and trigger an immune response.
During a tuberculin skin test, the testing solution is injected under the skin of the forearm, which creates an elevated, swollen spot on the surface of the skin. After 48 to 72 hours, a health professional reads the results of a tuberculin skin test by measuring the size of the elevated spot. To interpret this test, a doctor considers a person’s risk of tuberculosis infection and the diameter of the swelling, measured in millimeters.
The tuberculin skin test is one of two types of tests used to detect TB. The other type of test is a TB blood test called an IGRA TB Test (interferon-gamma release assays). The decision of which type of TB test to use for an individual patient depends on several factors including where the test is conducted, availability, and the cost of each test.
An IGRA (interferon gamma release assay) TB test may be used instead of a tuberculin skin test for a number of reasons, including the test setting, the cost of testing, and test availability. Doctors may also recommend an IGRA TB test because this test only requires one visit. However, both tests are acceptable for detecting TB infections.
Who should be tested for tuberculosis infection?
Certain people should be tested for tuberculosis infection because they are at higher risk for being infected with tuberculosis bacteria, including:
- People who have spent time with someone who has tuberculosis disease
- People from a country where tuberculosis disease is common (most countries in Latin America, the Caribbean, Africa, Asia, Eastern Europe, and Russia)
- People who live or work in high-risk settings (for example: correctional facilities, long-term care facilities or nursing homes, and homeless shelters)
- Health-care workers who care for patients at increased risk for tuberculosis disease
- Infants, children and adolescents exposed to adults who are at increased risk for latent tuberculosis infection or tuberculosis disease
Many people who have latent tuberculosis infection never develop tuberculosis disease. But some people who have latent tuberculosis infection are more likely to develop tuberculosis disease than others. Those at high risk for developing tuberculosis disease include:
- People with HIV infection
- People who became infected with tuberculosis bacteria in the last 2 years
- Babies and young children
- People who inject illegal drugs
- People who are sick with other diseases that weaken the immune system
- Elderly people
- People who were not treated correctly for tuberculosis in the past
Tuberculosis tests are generally not needed for people with a low risk of infection with tuberculosis bacteria.
When should I get a tuberculin skin test?
A tuberculin skin test may be recommended to screen a person who is at an increased risk of TB infection. People whose job or living condition puts them at an increased risk of TB infection include those who live or work in group settings where tuberculosis is more common, such as:
- Health care settings
- Correctional facilities
- Homeless shelters
- Nursing homes
- Countries where TB infection is common, including Mexico, India, and China
If a patient is showing symptoms of TB disease, a tuberculin skin test may be ordered to assist in making a diagnosis. Symptoms of TB disease include:
- A bad cough that lasts longer than 3 weeks
- Coughing up blood and mucus
- Chest pain
- Fatigue
- Lack of appetite or weight loss
- Fever, chills, or night sweats
Who can receive a tuberculin skin test?
Most persons can receive a tuberculin skin test. Tuberculin skin test is contraindicated only for persons who have had a severe reaction (e.g., necrosis, blistering, anaphylactic shock, or ulcerations) to a previous tuberculin skin test. It is not contraindicated for any other persons, including infants, children, pregnant women, persons who are HIV-infected, or persons who have been vaccinated with Bacille Calmette-Guérin (BCG) vaccine.
BCG (Bacillus Calmette-Guérin) vaccine is a vaccine for tuberculosis (TB) disease. Bacillus Calmette-Guérin (BCG) vaccine contains a live attenuated strain of Mycobacterium bovis. BCG vaccine is not widely used in the United States, but it is often given to infants and small children in other countries where tuberculosis (TB) is common. BCG vaccine does not always protect people from getting tuberculosis (TB).
Are tuberculin skin test results accurate?
The tuberculin skin test is a widely used test. There are known circumstances that can lead to false negative and false positive test results.
There are several factors that can contribute to false positive test results, in which a person has a positive test result despite not having an infection.
Known causes for False Positive test results include:
- Previous vaccination with the bacille Calmette-Guérin (BCG) TB vaccine
- An infection from another type of bacteria from the same family as Mycobacterium tuberculosis
False Negative results, in which a person has a negative test result despite having a TB infection, can occur for several reasons, including:
- Recent vaccination using the live-virus measles or smallpox vaccine
- A recent TB infection acquired within 8 to 10 weeks before a TB skin test
- Testing on infants
- A phenomenon known as anergy, which describes a lack of normal immune response to the test fluid.
Do I need follow-up tests?
In the event of a positive tuberculin skin test result, follow-up tests are used to rule out TB disease. Tests used to rule out TB disease include a physical exam, chest x-rays and sputum culture. In some cases, doctors may suggest an IGRA TB test to confirm a positive tuberculin skin test result.
If the result of a tuberculin skin test is negative, follow-up testing depends on the patient’s circumstances. For example, if a patient with a compromised immune system is exposed to someone with TB disease, they may be treated for TB even after a negative tuberculin skin test. TB testing is then repeated eight weeks after the patient begins treatment. In older adults who were previously infected with TB bacteria, a second tuberculin skin test may be administered after an initial negative test result, known as two-step testing.
If tuberculin skin test results are not read by a trained provider within the 48 to 72 hour window, another tuberculin skin test may be ordered.
Testing for tuberculosis in BCG-vaccinated people
Many people born outside of the United States have been BCG-vaccinated.
People who were previously vaccinated with BCG may receive a tuberculosis skin test to test for tuberculosis infection. Vaccination with BCG may cause a positive reaction to a tuberculosis skin test. A positive reaction to a tuberculosis skin test may be due to the BCG vaccine itself or due to infection with tuberculosis bacteria.
Tuberculosis blood tests (IGRAs or interferon-gamma release assays), unlike the tuberculosis skin test, are not affected by prior BCG vaccination and are not expected to give a false-positive result in people who have received BCG. Two tuberculosis blood tests are approved by the U.S. Food and Drug Administration (FDA) and are available in the United States: the QuantiFERON®–tuberculosis Gold In-Tube test (QFT-GIT) and the T-SPOT®.tuberculosis test (T-Spot). A health care provider will draw a patient’s blood and send it to a laboratory for analysis and results.
Tuberculosis blood tests are the preferred tuberculosis test for:
- People who have received the tuberculosis vaccine bacille Calmette–Guérin (BCG).
- People who have a difficult time returning for a second appointment to look for a reaction to the tuberculin skin test.
For children under the age of five, the tuberculosis skin test is preferred over tuberculosis blood tests.
A positive tuberculosis skin test or tuberculosis blood test only tells that a person has been infected with tuberculosis bacteria. It does not tell whether the person has latent tuberculosis infection or has progressed to tuberculosis disease. Other tests, such as a chest x-ray and a sample of sputum, are needed to see whether the person has tuberculosis disease.
Can tuberculin skin tests be given to persons receiving vaccinations?
Vaccination with live viruses may interfere with tuberculin skin test reactions. For persons scheduled to receive a tuberculin skin test, testing should be done as follows:
- Either on the same day as vaccination with live-virus vaccine or 4-6 weeks after the administration of the live-virus vaccine
- At least one month after smallpox vaccination
How often can tuberculin skin tests be repeated?
In general, there is no risk associated with repeated tuberculin skin test placements. If a person does not return within 48-72 hours for a tuberculin skin test reading, a second test can be placed as soon as possible. There is no contraindication to repeating the tuberculin skin test, unless a previous tuberculin skin test was associated with a severe reaction.
What is a boosted reaction?
In some persons who are infected with Mycobacterium tuberculosis, the ability to react to tuberculin may wane over time. When given a tuberculin skin test years after TB infection, these persons may have a false-negative reaction. However, the tuberculin skin test may stimulate the immune system, causing a positive, or boosted reaction to subsequent tests. Giving a second tuberculin skin test after an initial negative tuberculin skin test reaction is called two-step testing.
Why is two-step testing conducted?
Two-step testing is useful for the initial skin testing of adults who are going to be retested periodically, such as health care workers or nursing home residents. This two-step approach can reduce the likelihood that a boosted reaction to a subsequent tuberculin skin test will be misinterpreted as a recent TB infection.
Tuberculin skin test results
Tuberculin skin test interpretation depends on two factors:
- The measurement of the diameter of the swelling in millimeters.
- Person’s risk of being infected with TB (tuberculosis) and of progression to disease if infected.
These criteria mean that the size of an induration required for a positive test result depends on other aspects of a patient’s risk profile. For example, an induration of 5 or more millimeters is considered positive in people living with HIV or who have imaging test results suggestive of TB disease. An induration of 15 or more millimeters is required for a positive diagnosis in patients with no known risk factors for TB.
Tuberculin skin test positive
An induration of 5 or more millimeters is considered positive in:
- HIV-infected persons
- A recent contact of a person with tuberculosis disease
- Persons with fibrotic changes on chest radiograph consistent with prior tuberculosis
- Patients with organ transplants
- Persons who are immunosuppressed for other reasons (e.g., taking the equivalent of >15 mg/day of prednisone for 1 month or longer, taking TNF-a antagonists)
An induration of 10 or more millimeters is considered positive in:
- Recent immigrants (< 5 years) from high-prevalence countries
- Injection drug users
- Residents and employees of high-risk congregate settings
- Mycobacteriology laboratory personnel
- Persons with clinical conditions that place them at high risk
- Children < 4 years of age
- Infants, children, and adolescents exposed to adults in high-risk categories
An induration of 15 or more millimeters is considered positive in any person, including persons with no known risk factors for tuberculosis (TB). However, targeted skin testing programs should only be conducted among high-risk groups.
False-Positive reactions
Some persons may react to the tuberculin skin test even though they are not infected with Mycobacterium tuberculosis (TB). The causes of these false-positive reactions may include, but are not limited to, the following:
- Infection with nontuberculosis mycobacteria
- Previous BCG (Bacille Calmette-Guérin) vaccination
- Incorrect method of tuberculin skin test administration
- Incorrect interpretation of reaction
- Incorrect bottle of antigen used
False-Negative reactions
Some persons may not react to the tuberculin skin test even though they are infected with Mycobacterium tuberculosis. The reasons for these false-negative reactions may include, but are not limited to, the following:
- Cutaneous anergy (anergy is the inability to react to skin tests because of a weakened immune system)
- Recent TB infection (within 8-10 weeks of exposure)
- Very old TB infection (many years)
- Very young age (less than 6 months old)
- Recent live-virus vaccination (e.g., measles and smallpox)
- Overwhelming TB disease
- Some viral illnesses (e.g., measles and chicken pox)
- Incorrect method of tuberculin skin test administration
- Incorrect interpretation of reaction
Tuberculin vaccine
BCG (Bacillus Calmette-Guérin) vaccine is a vaccine for tuberculosis (TB) disease. Bacillus Calmette-Guérin (BCG) vaccine a live attenuated strain of Mycobacterium bovis. BCG vaccine is not widely used in the United States, but it is often given to infants and small children in other countries where tuberculosis (TB) is common. BCG vaccine does not always protect people from getting tuberculosis (TB).
BCG vaccine recommendations
In the United States, BCG should be considered for only very select people who meet specific criteria and in consultation with a tuberculosis expert. Health care providers who are considering BCG vaccination for their patients are encouraged to discuss this intervention with the tuberculosis control program in their area.
Children
BCG vaccination should only be considered for children who have a negative tuberculosis test and who are continually exposed, and cannot be separated from adults who
- Are untreated or ineffectively treated for tuberculosis disease, and the child cannot be given long-term primary preventive treatment for tuberculosis infection; or
- Have tuberculosis disease caused by strains resistant to isoniazid and rifampin.
Health Care Workers
BCG vaccination of health care workers should be considered on an individual basis in settings in which
- A high percentage of tuberculosis patients are infected with tuberculosis strains resistant to both isoniazid and rifampin;
- There is ongoing transmission of drug-resistant tuberculosis strains to health care workers and subsequent infection is likely; or
- Comprehensive tuberculosis infection-control precautions have been implemented, but have not been successful.
Health care workers considered for BCG vaccination should be counseled regarding the risks and benefits associated with both BCG vaccination and treatment of latent tuberculosis infection.