Contents
- What is uterus
- What is the function of the uterus ?
- What is Inverted uterus ?
- What is Tipped uterus ?
- What is irritable uterus ?
- What are the signs and symptoms of irritable uterus (preterm labor uterus contractions) and what should you do if you have any of them ?
- Causes of irritable uterus (preterm labor)
- Can anything be done to prevent preterm birth if you’re at high risk ?
- Why is irritable uterus (preterm labor uterus contractions) a concern ?
- If you have preterm labor, will you have a preterm birth ?
- How is preterm labor diagnosed ?
- What happens if your preterm labor continues ?
- What are corticosteroids ?
- What is magnesium sulfate ?
- What are tocolytics ?
- What happens if your labor does not stop ?
- What is uterus transplant ?
What is uterus
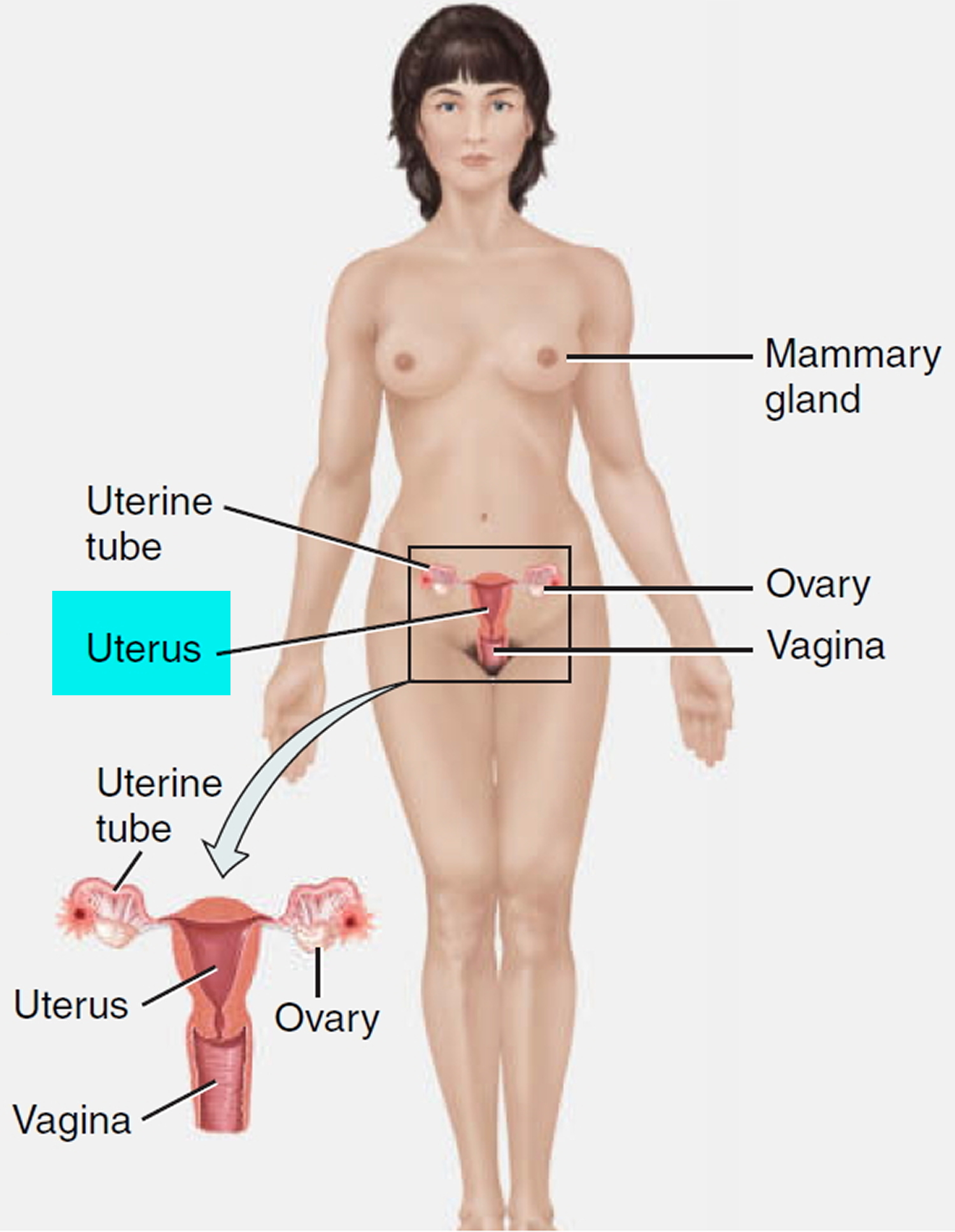
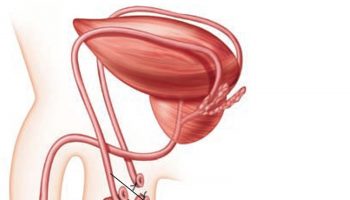
The uterus is a hollow, muscular organ shaped somewhat like an inverted pear. The uterus receives the embryo that develops from an oocyte fertilized in the uterine tube, and sustains its development.
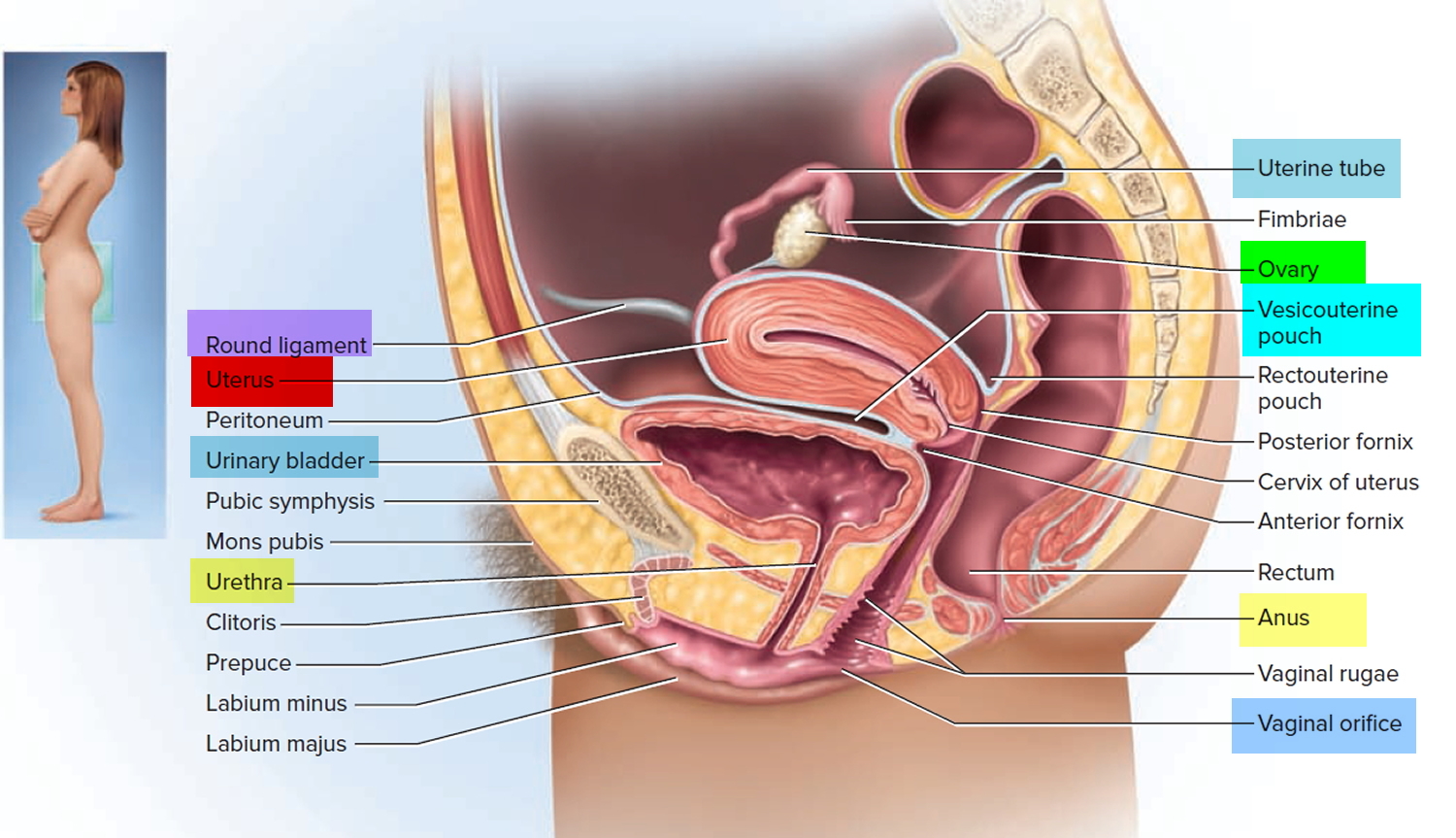
In its nonpregnant, adult state, the uterus is about 7 centimeters long, 5 centimeters wide (at its broadest point), and 2.5 centimeters in diameter. The size of the uterus changes greatly during pregnancy and it is somewhat larger in women who have been pregnant. The uterus is located medially in the anterior part of the pelvic cavity, superior to the vagina, and usually bends forward over the urinary bladder (see Figure 3).
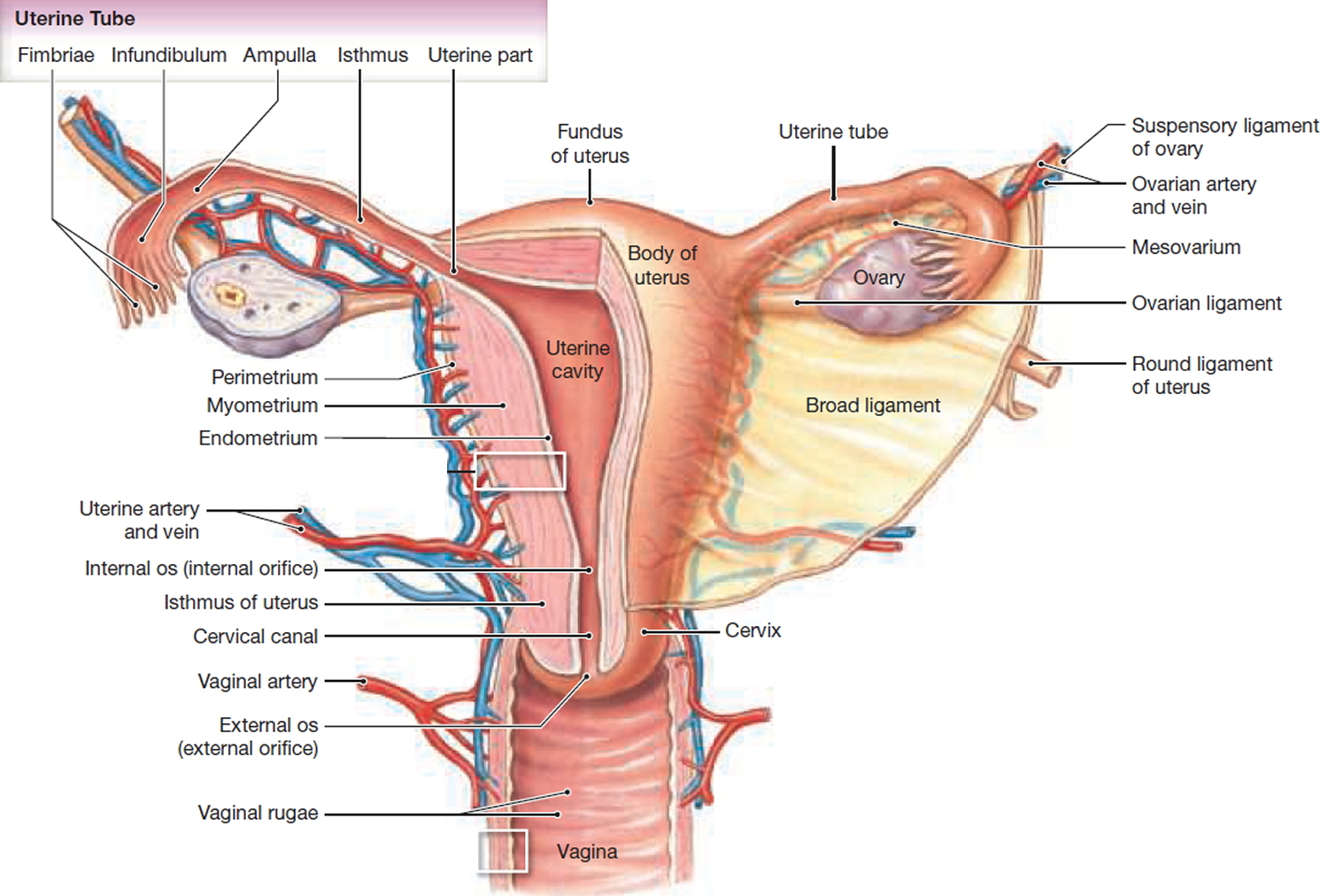
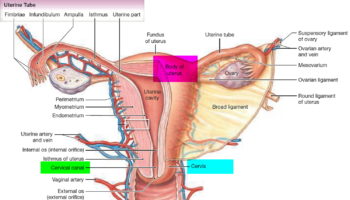
The upper two-thirds or body (corpus), of the uterus has a domeshaped top called the fundus (see Figure 1). The uterine tubes (also called Fallopian tubes) connect at the upper lateral edges of the uterus. The lower third of the uterus is called the cervix. This tubular part extends downward into the upper part of the vagina. The cervix surrounds the opening called the cervical orifice, through which the uterus opens to the vagina.
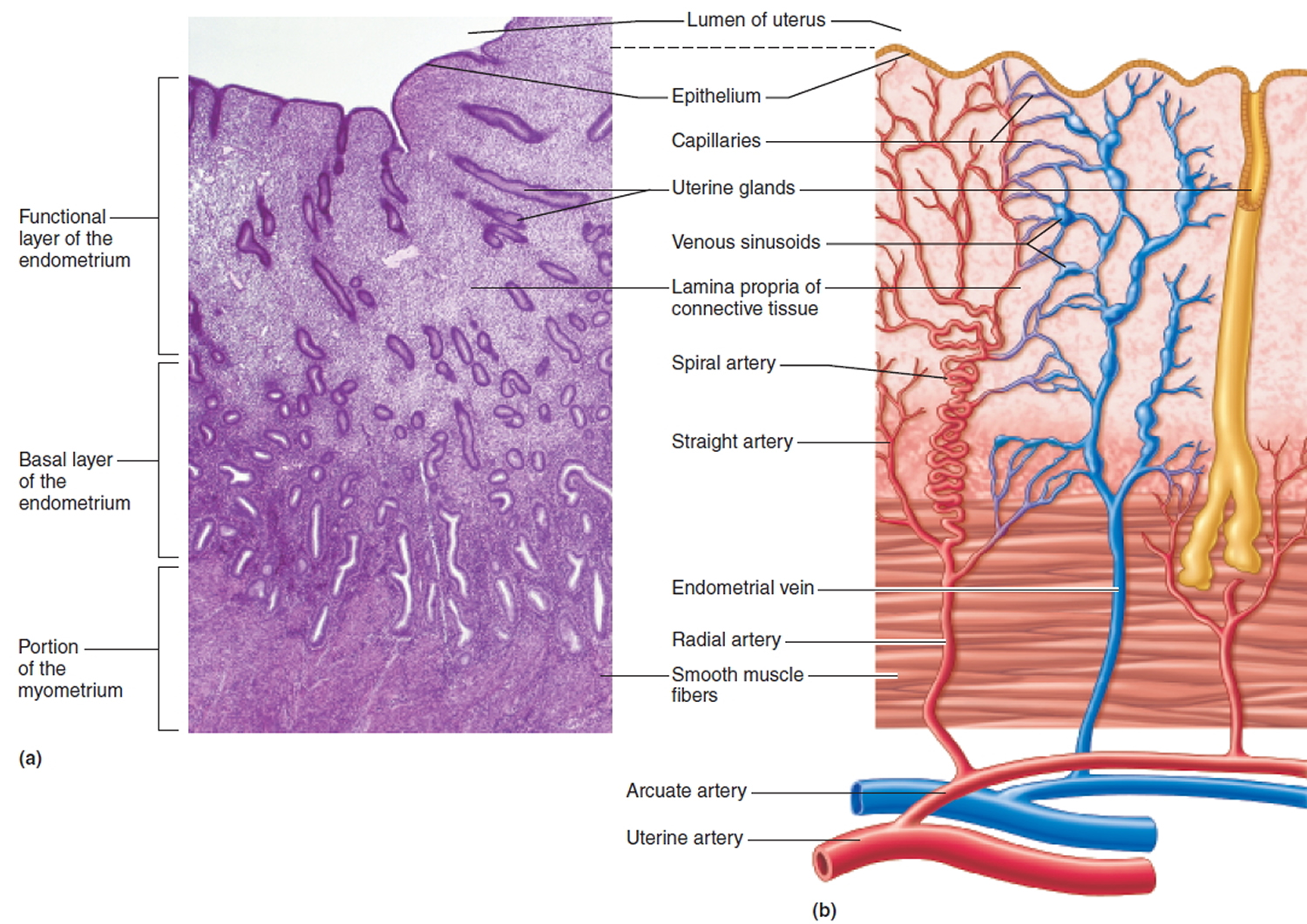
The uterine wall is thick and has three layers (Figure 1). The endometrium, the inner mucosal layer, is covered with columnar epithelium and contains abundant tubular glands. The myometrium, a thick, middle, muscular layer, consists largely of bundles of smooth muscle cells. During the monthly female menstrual cycles and during pregnancy, the endometrium and myometrium change extensively. The perimetrium consists of an outer serosal layer, which covers the body of the uterus and part of the cervix.
Uterus anatomy
The uterus is supported by the muscular floor of the pelvis and folds of peritoneum that form supportive ligaments around the organ, as they do for the ovary and uterine tube. The broad ligament has two parts: the mesosalpinx mentioned earlier and the mesometrium on each side of the uterus. The cervix and superior part of the vagina are supported by cardinal (lateral cervical) ligaments extending to the pelvic wall. A pair of uterosacral ligaments attaches the posterior side of the uterus to the sacrum, and a pair of round ligaments arises from the anterior surface of the uterus, passes through the inguinal canals, and terminates in the labia majora.
As the peritoneum folds around the various pelvic organs, it creates several dead-end recesses and pouches (extensions of the peritoneal cavity). Two major ones are the vesicouterine pouch, which forms the space between the uterus and urinary bladder, and rectouterine pouch between the uterus and rectum (see Figure 3).
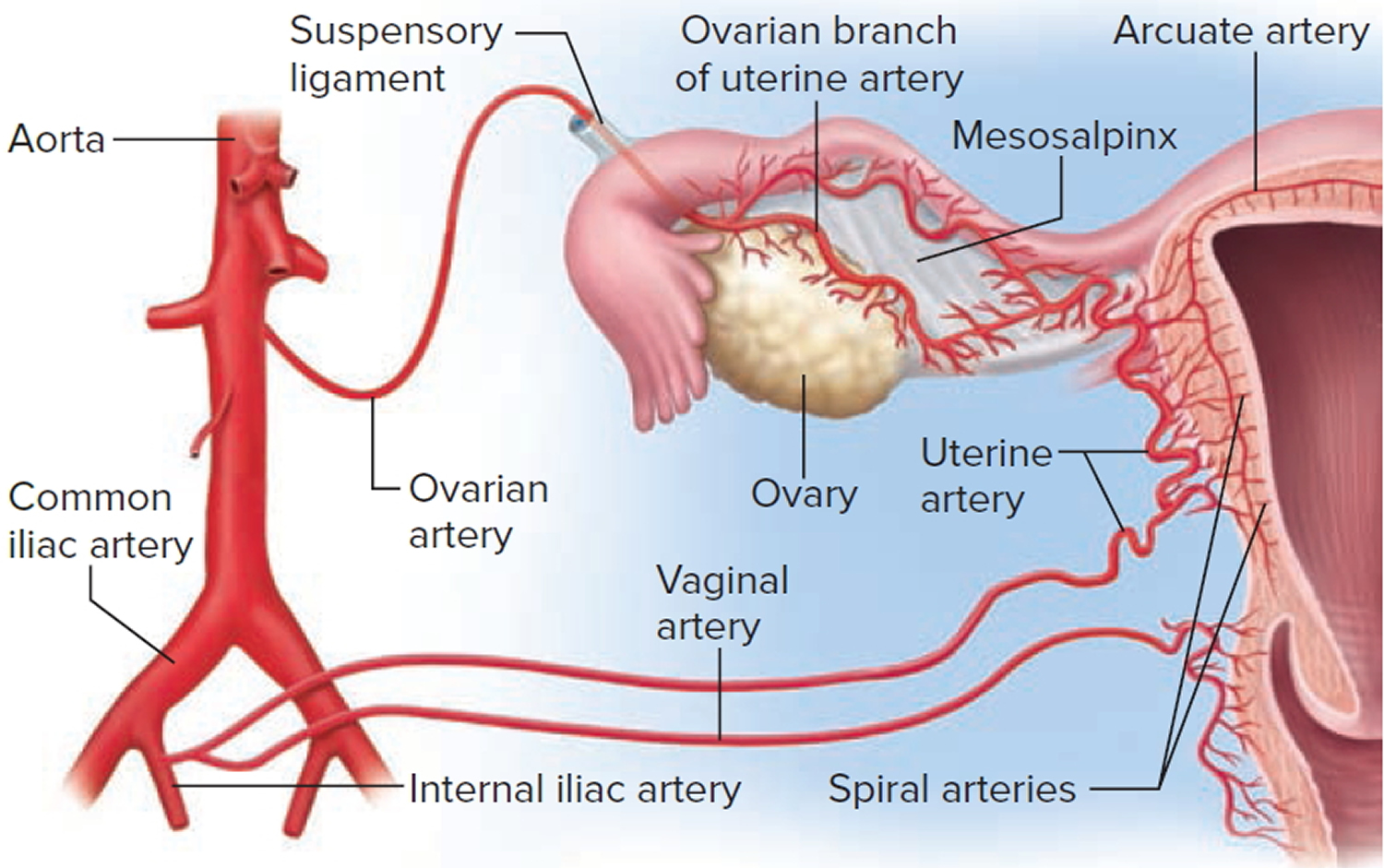
The uterine blood supply to the uterus is particularly important to the menstrual cycle and pregnancy. A uterine artery arises from each internal iliac artery and travels through the broad ligament to the uterus (Figure 2). It gives off several branches that penetrate into the myometrium and lead to arcuate arteries. Each arcuate artery travels in a circle around the uterus and anastomoses with the arcuate artery on the other side. Along its course, it gives rise to smaller arteries that penetrate the rest of the way through the myometrium, into the endometrium, and give off spiral arteries. The spiral arteries wind tortuously between the endometrial glands toward the surface of the mucosa. They rhythmically constrict and dilate, making the mucosa alternately blanch and flush with blood.
Figure 1. Uterus anatomy
Figure 2. Blood supply to the uterus
Figure 3. Uterus location
Figure 4. Uterus location in the female pelvis
What is the function of the uterus ?
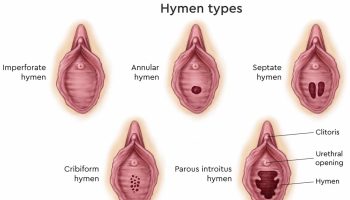
The lumen of the uterus is roughly triangular, with its two upper corners opening into the uterine tubes. In the nonpregnant uterus, the lumen isn’t a hollow cavity but rather a potential space; the mucous membranes of the opposite walls are pressed against each other with little room between them. The lumen communicates with the vagina by way of a narrow passage through the cervix called the cervical canal. The superior opening of this canal into the body of the uterus is the internal os and its opening into the vagina is the external os. The canal contains cervical glands that secrete mucus, thought to prevent the spread of microorganisms from the vagina into the uterus. Near the time of ovulation, the mucus becomes thinner than usual and allows easier passage for sperm.
The uterine wall consists of three layers. The outermost layer, the perimetrium, is a thin serosa of simple squamous epithelium and loose connective tissue. The middle and thickest layer is the myometrium, about 1.25 cm thick in the nonpregnant uterus. It is composed mainly of bundles of smooth muscle that sweep downward from the fundus and spiral around the body of the uterus. The myometrium is less muscular and more fibrous near the cervix; the cervix itself is almost entirely collagenous. The muscle cells of the myometrium are about 40 μm long immediately after menstruation, but they are twice this long at the middle of the menstrual cycle and 10 times as long in pregnancy. The function of the myometrium is to produce the labor contractions that help to expel the fetus.
The innermost layer is a mucosa called the endometrium. It has a simple columnar epithelium, compound (branching) tubular glands, and a lamina propria populated by leukocytes, macrophages, and other cells. The superficial half to two-thirds of it, called the functional layer (stratum functionalis), is shed in each menstrual period. The deeper layer, called the basal layer (stratum basalis), stays behind and regenerates a new functional layer in the next cycle. When pregnancy occurs, the endometrium is the site of attachment of the embryo and forms the maternal part of the placenta from which the fetus is nourished.
Figure 5. Endometrium of the uterus and its blood supply
What is Inverted uterus ?
Inversion of the uterus is a very serious and fortunately relatively rare complication of delivery (at childbirth). A non-puerperal (non-childbirth) uterine inversion is even more uncommon, with only 150 cases published between 1887 and 2006 1, 2. In the vast majority the incidence was observed in women older than 45 years. 85% of uterine inversion was caused by benign pathology, only 15% was associated with cancer 3.
Uterine inversions are classified into two groups, including (a) puerperal (childbirth) that is due to obstetric problem and (b) non-puerperal (non-childbirth) inversions that is due to gynecological problem 4. The diagnosis can be difficult even on physical examination. Most non-puerperal (non-childbirth) uterine inversions are caused by benign submucous myomas, while other causes are leiomyosarcoma, rhabdomyosarcoma, malignant mixed müllerian tumour and endometrial polyp. Women of reproductive age who present with the rare finding of non-puerperal uterine inversion are likely to have a malignancy. Most cases have reported puerperal uterine inversion as a rare condition 5. Leiomyomas (uterine fibroids – benign tumor of the uterus) are considered as the most frequent gynecologic problems. A report has been shown that submucosal leiomyoma dilated cervix and prolapsed into the vagina 6. Furthermore, some cases of prolapsed cervical myoma may show some malignancy features that lead to differential diagnoses, and frozen section analysis during surgery is considered as a logical action 7.
The cause of uterine inversion is not clearly defined. Possible explanations could be a thin uterine wall, rapid growth of the tumour, tumour size, fundic localisation of the tumour, tumour attachment to the uterine wall with a thin pedicle, dilatation of the cervix by distension of the uterine cavity, and sudden expulsion of the tumour 2, 8.
Non-puerperal uterine inversion caused by submucousal leiomyoma has been more frequently reported in African women 9. The clinical diagnosis of non-puerperal uterine inversion is divided into (a) chronic signs including irregular vaginal bleeding, anemia, and a feeling of mass coming down in vagina and (b) acute signs including pelvic pain and heavy vaginal bleeding 10. Some literatures have also pointed to vaginal discharge, urethrovaginal fistula and intermittent acute urinary retention 11.
Imaging procedures such as ultrasound and magnetic resonance imaging will contribute to the diagnosis 12. Unfortunately, because of the rare nature of the disorder, uterine inversion frequently goes undetected until surgery unless a high index of suspicion is maintained.
Types of treatment vary greatly from case to case. Abdominal and vaginal hysterectomies are recommended for women who have completed their family size. Vaginal myomectomy is suggested for the cases showing no malignancy. Finally, for uterine inversion caused by malignancy, advanced surgery such as radical abdominal hysterectomy is indicated.
What is Tipped uterus ?
Tipped uterus, also called tilted uterus or retroverted uterus is a condition where the woman’s uterus (womb) tilts backward rather than forward 13.
Causes of tipped uterus
Tipped uterus or retroversion of the uterus is common. One in 5 women has this condition. The problem may also occur due to weakening of the pelvic ligaments at the time of menopause. An enlarged uterus can also be caused by pregnancy or a tumor.
Scar tissue in the pelvis (pelvic adhesions) can also hold the uterus in a retroverted position. Scarring may come from:
- Endometriosis
- Infection in uterus or tubes
- Pelvic surgery
Symptoms of tipped uterus
Tipped uterus almost never causes any symptoms.
Rarely, it may cause pain or discomfort.
How is tipped uterus diagnosed ?
A pelvic exam will show the position of the uterus. However, a tipped uterus can sometimes be mistaken for a pelvic mass or a growing fibroid. A rectovaginal exam may be used to distinguish between a mass and a tipped uterus.
An ultrasound test can be used to see the exact position of the uterus.
Treatment for tipped uterus
Treatment is not needed most of the time. Underlying disorders, such as endometriosis or adhesions, should be treated as needed.
Outlook (Prognosis) for tipped uterus
In most cases, the condition does not cause problems.
Possible Complications of Tipped uterus
Atypical positioning of the uterus may be caused by endometriosis, salpingitis, or pressure from a growing tumor.
When to Contact a Medical Professional
Call your health care provider if you have ongoing pelvic pain or discomfort.
Prevention of tipped uterus
There is no way to prevent the problem. Early treatment of uterine infections or endometriosis may reduce the chances of a change in the position of the uterus.
What is irritable uterus ?
In general, a normal human pregnancy lasts about 40 weeks, or just more than 9 months, from the start of the last menstrual period to childbirth 14. Labor that begins before 37 weeks is called preterm labor (or premature labor). When birth occurs between 20 weeks of pregnancy and 37 weeks of pregnancy, it is called preterm birth 14.
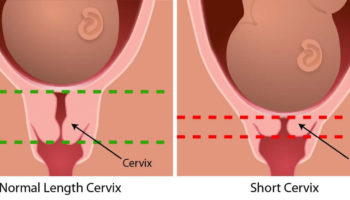
Irritable uterus (preterm labor uterus contractions) is the regular contractions of the uterus, every 10-15 minutes or more often, that start before 37 weeks of pregnancy resulting in changes in the cervix 15. Changes in the cervix include effacement (the cervix thins out) and dilation (the cervix opens so that the fetus can enter the birth canal) 16.
What are the signs and symptoms of irritable uterus (preterm labor uterus contractions) and what should you do if you have any of them ?
See your obstetrician or other health care professional right away if you notice any of these signs or symptoms:
- Leaking fluid or bleeding from the vagina (watery, mucus, or bloody)
- Increase in amount of discharge
- Feeling of pressure in the pelvis or or lower abdomen
- Constant low, dull backache
- Cramps that feel like menstrual cramps
- Abdominal cramps with or without diarrhea
- Ruptured membranes (your water breaks with a gush or a trickle of fluid)
Causes of irritable uterus (preterm labor)
Factors associated with irritable uterus (preterm labor uterus contractions) 17:
- Maternal factors
- Low socioeconomic status
- Nonwhite race
- Maternal age ≤18 or ≥40 years
- Low pre-pregnancy weight
- Smoking during pregnancy
- Substance abuse during pregnancy
- Certain pregnancy complications, such as multiple pregnancy and vaginal bleeding.
Maternal history
- Previous history of preterm delivery
- Previous history of a second-trimester abortion
- Short interval between pregnancies
Uterine factors
- Having a short cervix: Cervical incompetence from trauma or exposure to diethylstilbestrol can lead to painless cervical dilation and preterm labor. Both of these conditions may respond to the placement of a cerclage (this is a stitch that your provider puts in your cervix); however, no controlled trials have been conducted to support this approach.
- Uterine volume increased
- History of certain types of surgery on the uterus or cervix
- Uterine anomalies: Uterine malformations that predispose a patient to preterm labor include a bicornate or unicorn uterus, and uterine fibroids, particularly submucosal and subplacental fibroids. Women who are diagnosed with uterine malformations before conception may be given the option of birth control or surgery, if applicable.
- Trauma
- Infection: Infections of the genitourinary tract are an important and treatable factor associated with preterm labor. Women with Neisseria gonorrhoeae, Chlamydia trachomatis, Treponema pallidum, Trichomonas vaginalis, Gardnerella vaginalis or group B streptococci infections have higher rates of preterm births. Although cause and effect have not yet been conclusively defined, diagnosis and treatment of these infections are necessary to prevent perinatal transmission 18. Therefore, women with sexually transmitted diseases, urinary tract infections, severe respiratory infections and vaginitis should be treated appropriately. Patients with intact amniotic membranes and a history of positive group B streptococcal culture are usually treated with intravenous penicillin. This approach is based on the rationale that treatment will prevent perinatal transmission, although this approach is not substantiated in the prevention of preterm labor. Pregnancy and delivery may be prolonged in women treated with erythromycin, ampicillin and clindamycin (Cleocin) 19.
In most cases, the cause of preterm labor is not diagnosed, and the etiology is likely to be multifactorial.
Can anything be done to prevent preterm birth if you’re at high risk ?
If you have had a prior preterm birth and you are planning another pregnancy, a preconception care checkup can help you get in the best possible health before you become pregnant. When you become pregnant, be sure to start prenatal care early. You may be referred to a health care professional who has expertise in managing high-risk pregnancies. In addition, you may be given certain medications or other treatment to help prevent preterm birth if you have risk factors. Treatment is given based on your individual situation and your risk factors for preterm birth.
Why is irritable uterus (preterm labor uterus contractions) a concern ?
Irritable uterus (preterm labor uterus contractions) can lead to preterm birth, which is a concern for the babies because babies who are born too early may not be fully developed. They may be born with serious health problems. Some health problems, like cerebral palsy, can last a lifetime. Other problems, such as learning disabilities, may appear later in childhood or even in adulthood.
The risk of health problems is greatest for babies born before 34 weeks of pregnancy. But babies born between 34 weeks of pregnancy and 37 weeks of pregnancy also are at risk 16.
If you have preterm labor, will you have a preterm birth ?
It is difficult for health care professionals to predict which women with preterm labor will go on to have preterm birth. Only about 10% of women with preterm labor will give birth within the next 7 days. For about 30% of women, preterm labor stops on its own.
How is preterm labor diagnosed ?
Preterm labor can be diagnosed only when changes in the cervix are found. Your obstetrician or other health care professional may perform a pelvic exam to see if your cervix has started to change. You may need to be examined several times over a period of a few hours. Your contractions also may be monitored.
Your obstetrician or other health care professional may do certain tests to determine whether you need to be hospitalized or if you need immediate specialized care. A transvaginal ultrasound exam may be done to measure the length of your cervix. The level of a protein called fetal fibronectin in the vaginal discharge may be measured. The presence of this protein is linked to preterm birth.
What happens if your preterm labor continues ?
If your preterm labor continues, how it is managed is based on what is thought to be best for your health and your baby’s health. When there is a chance that the baby would benefit from a delay in delivery, certain medications may be given. These medications include corticosteroids, magnesium sulfate, and tocolytics.
What are corticosteroids ?
Corticosteroids are drugs that cross the placenta and help speed up development of the baby’s lungs, brain, and digestive organs. Corticosteroids are most likely to help your baby when they are given between 24 weeks of pregnancy and 34 weeks of pregnancy, but consideration can also be given to providing corticosteroids between 23 and 24 weeks of pregnancy.
Corticosteroid therapy is presently the only treatment shown to improve fetal survival when given to a woman in preterm labor between 24 and 34 weeks of gestation 20. Studies have shown a decrease in intraventricular hemorrhage, respiratory distress syndrome and mortality even when treatment lasts for less than 24 hours, although optimal benefits begin 24 hours after therapy and last for seven days 20. Corticosteroid therapy is also beneficial in pregnant women of less than 30 to 32 weeks of gestation with preterm premature rupture of membranes and no evidence of chorioamnionitis. Treatment regimens include betamethasone, in a dosage of 12 mg given intramuscularly every 24 hours for two days, or dexamethasone, in a dosage of 6 mg given intramuscularly every 12 hours for two days..
What is magnesium sulfate ?
Magnesium sulfate is a medication that may be given if you are less than 32 weeks pregnant, are in preterm labor, and are at risk of delivery within the next 24 hours. This medication may help reduce the risk of cerebral palsy that is associated with early preterm birth.
Magnesium sulfate acts centrally to decrease seizures and blocks neuromuscular transmission. The mechanism for preventing uterine contraction is unknown but may be related to calcium antagonist activity 21.
Complications associated with the use of magnesium sulfate are 22:
- Maternal side effects include nausea, vomiting, hypotension, headache and the more severe effects of respiratory depression and pulmonary edema.
- Because magnesium sulfate crosses the placenta, fetal side effects include decreased muscle tone and lethargy. An immediate antidote to magnesium toxicity is an infusion of calcium gluconate.
What are tocolytics ?
Tocolytics are drugs used to delay delivery for a short time (up to 48 hours). They may allow time for corticosteroids or magnesium sulfate to be given or for you to be transferred to a hospital that offers specialized care for preterm infants. In addition to its role in protecting against cerebral palsy, magnesium sulfate also can be used as a tocolytic drug.
Drugs used for tocolysis include magnesium sulfate, ritodrine (Yutopar), terbutaline, nifedipine (Adalat, Procardia) and indomethacin (Indocin) 23. Recent studies have shown that antocin (Atosiban), an oxytocin receptor inhibitor (not labeled by the FDA for this purpose) may also be effective 24.
It is difficult to evaluate the efficacy of these drugs because of the inability to establish a definitive diagnosis of labor and the lack of consensus regarding the definition of successful treatment of preterm labor. However, it should be emphasized that tocolytic therapy has not been definitively shown to improve fetal outcome.
Oxytocin inhibitors offer a potential new therapeutic agent for the treatment of preterm labor. Although the exact mechanism of action is not known, uterine oxytocin receptors and/or oxytocin may have etiologic roles in uterine hyperactivity in women with preterm labor. Studies of the two oxytocin antagonists, antocin 24 and an orally active nonpeptidyl oxytocin antagonist 25, have suggested a high level of efficacy and few side effects (primarily nausea and vomiting). Phase III trials are currently being conducted to examine the effect of antocin on preterm uterine activity.
What happens if your labor does not stop ?
If your labor does not stop and it looks like you will give birth to your baby early, you and the baby usually will be cared for by a team of health care professionals. The team may include a neonatologist, a doctor who specializes in treating problems in newborns. The care your baby needs depends on how early he or she is born. High-level neonatal intensive care units provide this specialized care for preterm infants.
What is uterus transplant ?
In the year 2000, in Jeddah, Saudi Arabia, the first uterus transplant was attempted using a living donor in a woman submitted to emergency peripartum hysterectomy. Although the transplant did not result in pregnancy, it is credited with having achieved living-donor and recipient surgeries without major complications 26. However, the uterus in the recipient only remained viable for 100 days 27; the donor had a perioperative ureteral lesion, and it is questionable whether the uterus was correctly perfused. A necrotic uterus was removed after three months 28.
In 2011, a second human uterus transplant was attempted. In Antalya, Turkey, a 21-year-old patient with MRKH – Mayer-Rokitansky-Küster-Hauser syndrome, a rare congenital condition that significantly impacts the lives of affected women, received a uterus from a deceased 22-year-old donor 29. The donor’s multi-organ retrieval surgery lasted two hours, and the uterus was the first organ to be procured. The transplant procedure lasted six hours and included bilateral end-to-side anastomosis of the graft common iliac vessels to the external iliac vessels. The immunosuppression protocol included thymoglobulin for ten days and maintenance suppressive therapy with a triple-drug regimen with prednisolone, mycophenolate mofetil, and tacrolimus. Eighteen months after uterine transplant, the embryo-transfer attempts began. The patient attempted IVF multiple times, but only two very early miscarriages were observed 30. The reasons for the failed pregnancies are unknown in this case; however, it is important to bear in mind that a nulliparous uterus was transplanted and that its capacity to carry a pregnancy to term had not been demonstrated.
Mayer–Rokitansky–Küster–Hauser Syndrome is characterized by the presence of only a rudimentary solid bipartite uterus in combination with absence of the upper third of the vagina. The syndrome accounts for <3% of Müllerian malformations 31, and it is seen in 1:4500 females 32. Three Mayer–Rokitansky–Küster–Hauser Syndrome subtypes exist: (i) the typical form, with no extra genital malformation (50% of patients); (ii) the atypical form, with associated malformations in the renal system (20% of patients) and (iii) the severe form, with associated renal and skeletal malformations. This type is also known as MURCS (Müllerian duct aplasia, Renal aplasia and Cervicothoracic Somite dysplasia) and is found in around 30% of these patients 33. So far, Mayer–Rokitansky–Küster–Hauser Syndrome has been the main indication for uterus transplantation with nine patients being transplanted 34.
Uterus transplantation is now a new type of quality of life enhancing as well as a life-giving transplantation, which is the first potential treatment for absolute uterine factor infertility 35. This affects around 1 in every 500 women of fertile age,1 which on a worldwide base would be around 1.5 million women.
A unique feature of modern uterus transplantation is that it is temporary, since the allograft (the donated uterus) would be kept for a restricted time, until the recipient has delivered the desired number of children. The uterus would then be removed by hysterectomy or by discontinuing immunosuppression. This restricted time on immunosuppressive medications would minimize the long-term side effects of these potent pharmaceuticals 36.
There were several mild rejection episodes, although subclinical, which were diagnosed on protocol cervical biopsies (1, 2, 4 weeks after surgery and thereafter monthly) in five out of the seven patients 34. All the rejection events were effectively reversed by 2 weeks treatment of corticosteroid or tacrolimus dose increments. During the first post transplantation year, the uterine artery blood flow was within normal ranges 34.
Single embryo transfers to achieve pregnancies were initiated 12 months after uterus transplantation, and the first live birth from our human clinical trial took place in September 2014 37. This is the first successful human uterus transplantation procedure, since the goal of the uterus transplantation is a healthy baby. The recipient had an uneventful pregnancy until she was admitted at 31 full weeks and 5 days due to headache, high blood pressure and pre-eclampsia was diagnosed. An abnormal fetal cardiotocography showing fetal distress was registered the following night, and a cesarean section was performed and a healthy and normal-sized (1.8 kg) male baby was delivered. The cause of pre-eclampsia may be related to her unilateral renal ageneneis 38. Subsequently, three more uterus recipients have given birth (unpublished observations). All these, in total, four boys are developing in good health and thriving. Interestingly, in another one of these pregnancies, pre-eclampsia was developed and that patient had also a single kidney. The other two patients had double kidneys and did not develop pre-eclampsia. Additionally, there is presently, as of October 2015, one more ongoing pregnancy and doctors estimate that more live births will follow.
- Nonpuerperal uterine inversion associated with an immature teratoma of the uterus in an adolescent. Gomez-Lobo V, Burch W, Khanna PC. Obstet Gynecol. 2007 Aug; 110(2 Pt 2):491-3. https://www.ncbi.nlm.nih.gov/pubmed/17666639/[↩]
- Non-puerperal uterine inversion in association with uterine sarcoma: case report in a 26-year-old and review of the literature. Lupovitch A, England ER, Chen R. Gynecol Oncol. 2005 Jun; 97(3):938-41. https://www.ncbi.nlm.nih.gov/pubmed/15885762/[↩][↩]
- UTERINE INVERSION http://www.prolekare.cz/pdf?id=61064[↩]
- Non-puerperal uterine inversion due to submucous myoma in a young woman: a case report. de Vries M, Perquin DA. J Med Case Rep. 2010 Jan 24; 4():21. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2822794/[↩]
- Uterine inversion caused by uterine sarcoma: a case report. Takano K, Ichikawa Y, Tsunoda H, Nishida M. Jpn J Clin Oncol. 2001 Jan; 31(1):39-42. https://www.ncbi.nlm.nih.gov/pubmed/11256840/[↩]
- Bezircioglu I, Sakarya DK, Yetimalar MH, Kayhan E, Yildiz A, Baser E, et al. A Huge Vaginal Prolapsed Pedunculated Uterine Leiomyoma: A Case Report. J Clin Stud Med Case Rep. 2015;2:005.[↩]
- Babah O, Afolabi B, Ayanbode O, Atoki A, Okafor O. Prolapsed submucous uterine fibroid with associated uterovaginal prolapsed, a case report. IOSR J Dent Med Sci. 2014;13:64–67[↩]
- Non-puerperal uterine inversion. Case report. Krenning RA, Dörr PJ, de Groot WH, de Goey WB. Br J Obstet Gynaecol. 1982 Mar; 89(3):247-9. https://www.ncbi.nlm.nih.gov/pubmed/7066262/[↩]
- Ymele FF, Nana P, Fouedjio J, Bechem E, Mbu R. Non-puerperal uterine inversion following a prolapsed leiomyoma in a Cameroonian woman. Clin Mother Child Health. 2011;8:C110602.[↩]
- Muhammad Z, Ibrahim S, Yakasai I. Chronic Non-Puerperal Uterine Inversion: A report of two cases. Borno Med J. 2012;9:18–21.[↩]
- Babah O, Afolabi B, Ayanbode O, Atoki A, Okafor O. Prolapsed submucous uterine fibroid with associated uterovaginal prolapsed, a case report. IOSR J Dent Med Sci. 2014;13:64–67.[↩]
- MR imaging of uterine inversion. Lewin JS, Bryan PJ. J Comput Assist Tomogr. 1989 Mar-Apr; 13(2):357-9. https://www.ncbi.nlm.nih.gov/pubmed/2647797/[↩]
- Retroversion of the uterus. Medline Plus. https://medlineplus.gov/ency/article/001506.htm[↩]
- Preterm Labor and Birth: Overview. National Institute of Child Health and Human Development. https://www.nichd.nih.gov/health/topics/preterm/Pages/default.aspx[↩][↩]
- Preterm Labor. Medline Plus. https://medlineplus.gov/pretermlabor.html[↩]
- Preterm (Premature) Labor and Birth. American Congress of Obstetricians and Gynecologists. https://www.acog.org/Patients/FAQs/Preterm-Premature-Labor-and-Birth[↩][↩]
- Preterm Labor: Diagnosis and Treatment. American Academy of Family Physicians. http://www.aafp.org/afp/1998/0515/p2457.html[↩]
- Romero R, Mazor M, Munoz H, Gomez R, Galasso M, Sherer DM. The preterm labor syndrome. Ann N Y Acad Sci. 1994;734:414–29.[↩]
- McGregor JA, French JI, Reller LB, Todd JK, Makowski EL. Adjunctive erythromycin treatment for idiopathic preterm labor: results of a randomized, double blind, placebo-controlled trial. Am J Obstet Gynecol. 1986;154:98–103.[↩]
- Effect of corticosteroids for fetal maturation on perinatal outcomes NIH Consens Statement. 1994Feb 28 – Mar 2;12(2):1–18.[↩][↩]
- Beall MH, Edgar BW, Paul RH, Smith-Wallace T. A comparison of ritodrine, terbutaline, and magnesium sulfate for the suppression of preterm labor. Am J Obstet Gynecol. 1985;153:854–9.[↩]
- American College of Obstetricians and Gynecologists. Preterm labor. Technical bulletin no. 206. Washington, D.C.: ACOG, 1995. [↩]
- McCombs J. Update on tocolytic therapy. Ann Pharmacother. 1995;29:515–22.[↩]
- Goodwin TM, Paul R, Silver H, Spellacy W, Parsons M, Chez R, et al. The effect of the oxytocin antagonist atosiban on preterm uterine activity in the human. Am J Obstet Gynecol. 1994;170:474–8.[↩][↩]
- Pettibone DJ, Clineschmidt BV, Kishel MT, Lis EV, Reiss DR, Woyden CJ, et al. Identification of an orally active, nonpeptidyl oxytocin antagonist. J Pharmacol Exp Ther. 1993;264:308–14.[↩]
- Castellón LAR, Amador MIG, González RED, et al. The history behind successful uterine transplantation in humans. JBRA Assisted Reproduction. 2017;21(2):126-134. doi:10.5935/1518-0557.20170028. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5473706/[↩]
- Transplantation of the human uterus. Fageeh W, Raffa H, Jabbad H, Marzouki A. Int J Gynaecol Obstet. 2002 Mar; 76(3):245-51. https://www.ncbi.nlm.nih.gov/pubmed/11880127/[↩]
- Uterine transplantation research: laboratory protocols for clinical application. Díaz-García C, Johannesson L, Enskog A, Tzakis A, Olausson M, Brännström M. Mol Hum Reprod. 2012 Feb; 18(2):68-78. https://www.ncbi.nlm.nih.gov/pubmed/21900333/[↩]
- Preliminary results of the first human uterus transplantation from a multiorgan donor. Ozkan O, Akar ME, Ozkan O, Erdogan O, Hadimioglu N, Yilmaz M, Gunseren F, Cincik M, Pestereli E, Kocak H, Mutlu D, Dinckan A, Gecici O, Bektas G, Suleymanlar G. Fertil Steril. 2013 Feb; 99(2):470-6. https://www.ncbi.nlm.nih.gov/pubmed/23084266/[↩]
- Clinical pregnancy after uterus transplantation. Erman Akar M, Ozkan O, Aydinuraz B, Dirican K, Cincik M, Mendilcioglu I, Simsek M, Gunseren F, Kocak H, Ciftcioglu A, Gecici O, Ozkan O. Fertil Steril. 2013 Nov; 100(5):1358-63. https://www.ncbi.nlm.nih.gov/pubmed/23830110/[↩]
- Clinical implications of uterine malformations and hysteroscopic treatment results. Hum Reprod Update. 2001 Mar-Apr;7(2):161-74. https://www.ncbi.nlm.nih.gov/pubmed/11284660[↩]
- Müllerian agenesis: etiology, diagnosis, and management. Obstet Gynecol Surv. 2000 Oct;55(10):644-9. https://www.ncbi.nlm.nih.gov/pubmed/11023205[↩]
- Clinical aspects of Mayer-Rokitansky-Kuester-Hauser syndrome: recommendations for clinical diagnosis and staging. Hum Reprod. 2006 Mar;21(3):792-7. Epub 2005 Nov 10. https://www.ncbi.nlm.nih.gov/pubmed/16284062[↩]
- Uterus transplantation trial: 1-year outcome. Fertil Steril. 2015 Jan;103(1):199-204. doi: 10.1016/j.fertnstert.2014.09.024. Epub 2014 Oct 22. https://www.ncbi.nlm.nih.gov/pubmed/25439846[↩][↩][↩]
- Pernilla Dahm-Kähler, Cesar Diaz-Garcia, Mats Brännström; Human uterus transplantation in focus, British Medical Bulletin, Volume 117, Issue 1, 1 March 2016, Pages 69–78, https://doi.org/10.1093/bmb/ldw002 [↩]
- Pernilla Dahm-Kähler, Cesar Diaz-Garcia, Mats Brännström; Human uterus transplantation in focus, British Medical Bulletin, Volume 117, Issue 1, 1 March 2016, Pages 69–78, https://doi.org/10.1093/bmb/ldw002[↩]
- Livebirth after uterus transplantation. Lancet. 2015 Feb 14;385(9968):607-616. doi: 10.1016/S0140-6736(14)61728-1. Epub 2014 Oct 6. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(14)61728-1/fulltext[↩]
- Livebirth after uterus transplantation – Authors’ reply. Lancet. 2015 Jun 13;385(9985):2352-3. doi: 10.1016/S0140-6736(15)61098-4. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(15)61098-4/fulltext[↩]