Contents
What is volvulus
A volvulus is a twisting of a loop of intestine around itself and the mesentery that supports it, causing impairment of the blood supply or can result in complete or partial bowel obstruction 1. A volvulus causes a blockage that may cut off blood flow. Part of the intestine may be damaged as a result. The term volvulus is Latin for “volvere,” which means “to roll.”
Volvulus symptoms include abdominal bloating, pain, vomiting, constipation, and bloody stools. The onset of symptoms may be gradual or rapid. The mesentery becomes so tightly twisted that blood supply is cut off, resulting in an ischemic bowel. Pain may be significant and fever may develop.
Risk factors for volvulus include a birth defect known as intestinal malrotation, Hirschsprung disease, an enlarged colon, pregnancy, and abdominal adhesions. A high fiber diet and chronic constipation also increase the risk. In adults, the sigmoid colon and cecum are most affected. In children, the small intestine and stomach are more commonly involved. Diagnosis is typically made with medical imaging such as plain X-rays, CT scan, or a GI series.
Initial treatment for sigmoid volvulus may be with sigmoidoscopy or a barium enema. Due to the high risk of recurrence, a bowel resection within two days is generally recommended. If the bowel is severely twisted or the blood supply is cut off, emergent surgery is required. In a cecal volvulus, part of the bowel is usually removed. If the cecum is still healthy, it may be returned and sutured in place.
Sigmoid and cecal volvulus most often occurs between the ages of 30 and 70.
- Volvulus occurs more frequently in middle-aged and elderly men.
- Volvulus arises as a rare complication in patients with a redundant colon, a normal anatomic variation resulting in extra-colonic loops.
- Sigmoid volvulus is a very common form of volvulus and is responsible for 8% of all intestinal obstructions. Sigmoid volvulus is particularly common in constipated and elderly persons. Patients experience pain, distension, and constipation.
- Cecal volvulus is less common than sigmoid volvulus and is associated with pain and small bowel obstruction.
- Midgut volvulus typically occurs in babies that are predisposed because of congenital intestinal malrotation.
- Segmental volvulus occurs in people of any age, usually with a predisposition because of abnormal intestinal contents or adhesions.
- Volvulus of the cecum, transverse colon, or sigmoid colon usually occurs in adults with minor predisposing factors such as redundant intestinal tissue and constipation.
Cases of volvulus occur commonly in Africa, the Middle East, and India, presumably because of a high-fiber diet. Rates of volvulus in the United States are about 2 to 3 per 100,000 people per year. Outcomes are related to whether bowel tissue is ischemic or necrotic.
Colonic volvulus
Volvulus usually affects the colon. Colonic volvulus is a rare occurrence in the United States, attributing to approximately 4% of causes of large bowel obstruction, followed by cancer and diverticulitis 2. Of note, there are certain regions of the world where colonic volvulus happens more frequently. In areas of the Middle East, India, South America, Africa, and Russia, colonic volvulus attributes for approximately 50% of all accounts of colonic obstruction. The regional areas listed above have been coined the “volvulus belt.” Sigmoid volvulus occurs more frequently compared to cecal volvulus 3.
United States
Colonic volvulus ranks below cancer and diverticulitis as a cause of large-bowel obstruction.
- Colonic volvulus causes make up approximately 5% of intestinal obstruction.
- Colonic volvulus causes constitute 10% to 15% of all cases of large-bowel obstruction. The most common location of large-bowel torsion is the sigmoid colon (80%), the cecum (15%), transverse colon (3%), and splenic flexure (2%).
International
In Africa and the Middle East, nearly 50% of large-bowel obstructions are caused by volvulus, usually of the sigmoid colon.
Colonic volvulus causes
Associated risk factors for colonic volvulus are advanced age, chronic constipation, and diets rich in high fiber 2. Cecal volvulus most commonly occurs in the second and third decade of life, compared to sigmoid volvulus that occurs in the seventh and eighth decade of life. Patients that have psychiatric conditions or are institutionalized and taking psychotropic drugs have a higher incidence of colonic volvulus. The use of psychotropic drugs can cause hindered intestinal mobility and predispose patients to volvuluses 1.
Colonic volvulus signs and symptoms
Patients with colonic volvulus may present with an intestinal obstruction. Often, the symptoms are hard to differentiate from blockages caused by colon cancers. Common symptoms are acute onset of severe abdominal pain, constipation, obstipation, nausea, and vomiting. Often, a tympanitic and markedly distended abdomen are seen, and often, the distention is more impressive than other causes of bowel obstruction. When the wall of the distended bowel is placed under increased tension, the cecal volvulus may be associated with ischemia. Another cause of ischemia may be occlusion of the arterial blood supply to the mesentery cause by torsion. Ominous signs include tachycardia, rebound tenderness, and severe abdominal pain not improved with medical management.
Colonic volvulus diagnosis
Work up for a colonic volvulus includes a complete blood count (CBC) with differential, a comprehensive metabolic panel, and a lactic acid. Laboratory findings may be useful; however, they are not diagnostic. A leukocytosis level, a left shift (pandemic), or a metabolic acidosis may indicate systemic sepsis, bowel ischemia, or peritoneal infection. Electrolyte abnormalities may develop in the setting of a bowel obstruction and vomiting.
Abdominal plain x-rays may be confirmatory for a volvulus, especially if a “bent inner tube” or a “coffee bean” sign are seen. These refer to the appearance of the air-filled closed loop of the colon which forms the volvulus. A barium enema is used to demonstrate a “bird’s beak” at the point where the segment of proximal bowel and distal bowel rotate to form the obstructing volvulus. This area will show an acute and sharp tapering that has the appearance of a bird’s beak. If a perforation is suspected, barium should be avoided due to its potentially lethal effects when distributed throughout the free intraperitoneal cavity. Gastrografin, which is safer, can be substituted for barium.
In approximately 80% of colonic obstructions, a carcinoma invading the wall of the intestine is found to be the cause of the obstruction. This is usually easily diagnosed with CT scan and endoscopic biopsies.
Cecal volvulus
In cecal volvulus, the terminal ileum and right colon are involved. Cecal volvulus describes torsion of the cecum around its mesentery which often results in obstruction. If unrecognized, it can result in bowel perforation and fecal peritonitis. When a volvulus involves the cecum alone, it is also called a cecal bascule 2. This occurs when a highly mobile cecum traverses from a caudad to cephalad direction 4. Cecal volvulus is less common than sigmoid volvulus, accounting for 10% to 15% of all cases of volvulus, and it tends to affect women in the sixth decade of life.
There are two predisposing factors that are important for the development of a cecal volvulus:
- a developmental failure of peritoneal fixation allows the proximal colon to be free and mobile: this occurs in 11-25% of the population
- restriction of the bowel at a fixed point within the abdomen, acting as a fulcrum for rotation, e.g. adhesion, abdominal mass, scarring from calcified lymph nodes
Medical history of these patients may include prior abdominal surgery, the presence of a pelvic mass, violent coughing, atonia of the colon, extreme exertion, unpressurised air travel, or third-trimester pregnancy.
In general, there are three different types of cecal volvulus 2:
- Type 1: This cecal volvulus forms by a clockwise axial twisting or torsion of the cecum along the long axis. The location of the cecal volvulus is in the right lower quadrant.
- Type 2: This cecal volvulus develops from a twisting or torsion of a portion of the cecum and a portion of the terminal ileum. The location of the cecum gets displaced to an ectopic location (typically left upper quadrant) and is relocated in an inverted orientation. Traditionally, but not for all cases, a type 2 cecal volvulus will encounter a counterclockwise twist.
- Type 3: This cecal volvulus (also known as cecal bascule) is the upward folding of the cecum. There is no axial twisting like with type 1 and type 2.
Type 1 and type 2 cecal volvulus, which involve axial torsion, account for approximately 80% of all cecal volvuli. Cecal bascules account for the remaining 20% of cecal volvuli 2.
There are no evidence-based studies on the diagnosis or treatment of cecal volvulus 2. Cecal volvulus is not so common in North America but since it carries a very high mortality, it is important that healthcare workers be aware of the disorder.
Colonoscopic decompression may be appropriate if patient unfit for surgery. However, laparotomy is normally required. Where there is colonic ischemia, a right hemicolectomy is performed; in some cases, the primary anastomosis is not possible, and stoma formation at both ends is the safest option.
If the cecum is viable and the volvulus reduces, there are a number of options:
- reduction alone, but this is associated with the highest risk of recurrence
- right hemicolectomy
- cecostomy
- cecopexy
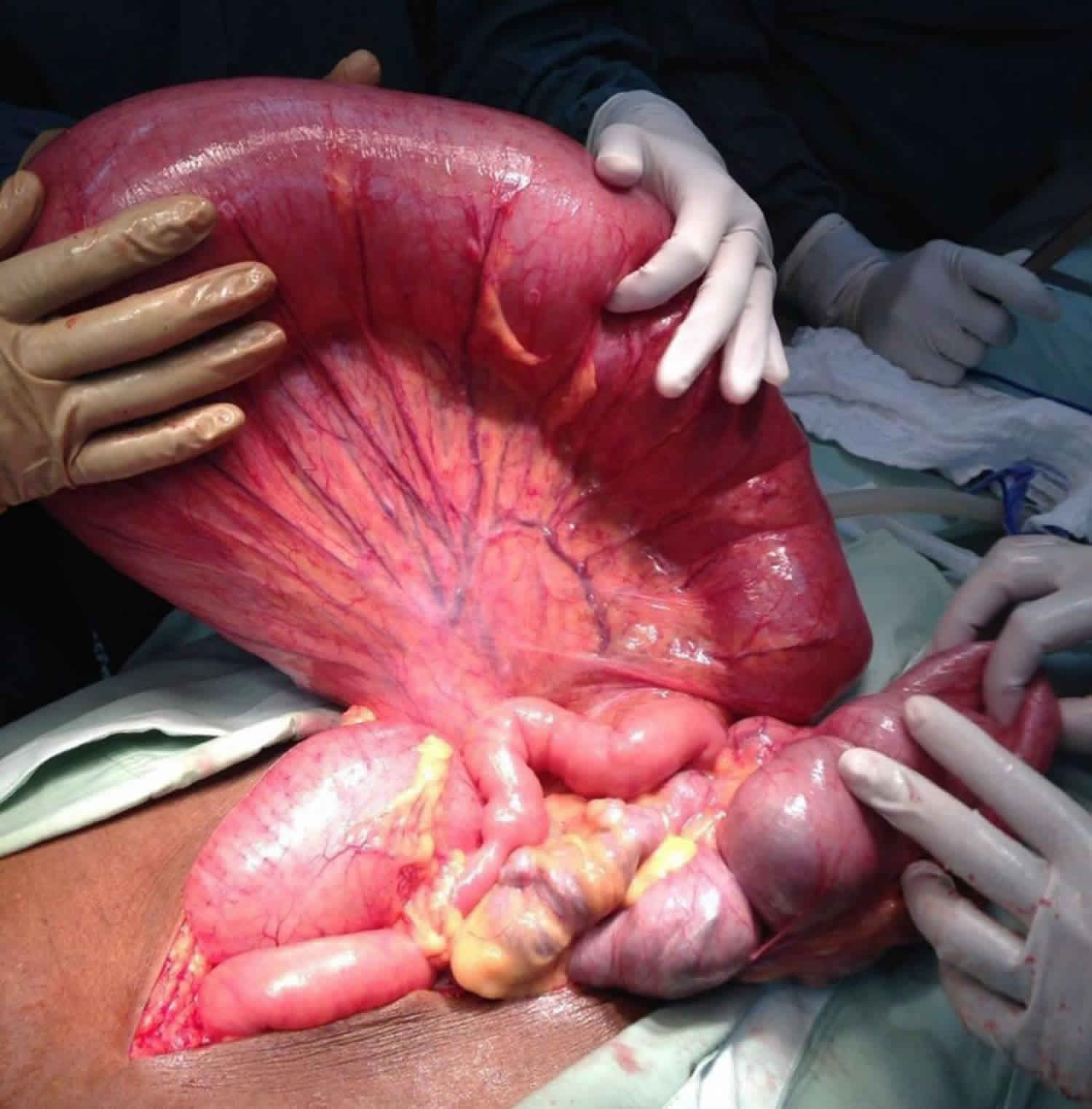
Figure 1. Cecal volvulus
Footnote: Abdominal xray of a cecal volvulus revealing a dramatic dilation of bowel extending from the right lower quadrant moving upwards to the left upper quadrant of the abdomen.
[Source 2 ]Cecal volvulus pathology
In ~50% of the patients, the cecum twists in the axial plane, rotating clockwise or counter-clockwise around its long axis and appearing in the right lower quadrant.
The other half of patients have what is known as the loop type of cecal volvulus, in which the cecum both twists and inverts, occupying the left upper quadrant of the abdomen. The terminal ileum is usually twisted along with the cecum. Visualization of a gas-filled appendix confirms the diagnosis.
There is a variant of cecal volvulus termed a “cecal bascule” that occurs when the cecum folds anteriorly without any torsion. A cecal bascule is often seen as a dilated loop in the mid-abdomen and although there is an association with prior surgery, adhesions and bands they are not essential for a volvulus to occur. In 10% of the population, there is a deficient peritoneal fixation of the cecum and ascending colon allowing abnormal mobility. Depending on the length of the mobile segment of right colon a variety of obstructive bowel patterns may result.
Cecal volvulus signs and symptoms
Cecal volvulus presents with clinical features of proximal large bowel obstruction. This is usually with colicky abdominal pain, vomiting, and abdominal distension.
Cecal volvulus diagnosis
Radiographic imaging can help differentiate between a sigmoid and cecal volvulus from other abdominal pathologies. For a cecal volvulus, an abdominal x-ray will reveal a dramatic dilation of bowel extending from the right lower quadrant moving upwards to the left upper quadrant of the abdomen. Usually, a patient with a cecal volvulus will present with small and large bowel obstructions, with the collapse of the distal large bowel, and with extensive dilation of the proximal small bowel. A definitive sign of a cecal volvulus is the upward displacement of the appendix with obstruction of the large bowel. Comparatively, a sigmoid volvulus will show findings of a bent inner tube sign with the apex of the volvulus located in the left upper quadrant.
Abdominal plain films are sufficient to make the diagnosis of a sigmoid volvulus; however, abdominal x-rays are less diagnostic for a cecal volvulus. Thus, the additional imaging of a CT scan can help differentiate the approximate location of torsion. An abdominopelvic CT scan is diagnostic for a cecal volvulus in approximately 90% of the patients. About 10% of the time, patients are diagnosed with a cecal volvulus intraoperatively 5.
A mesentery torsion around the ileocolic vessels as seen on a CT scan is described as a “whirl sign” and is considered pathognomonic for diagnosis of a cecal volvulus.
Cecal volvulus treatment
Treatment for cecal volvuli usually entails a surgical intervention. Other inventions such as a barium enema or a colonoscopy, can offer a non-operative reduction of a cecal volvulus. However, these modalities are rarely successful. For these non-operative treatments, there is a high risk of perforations and should not be attempted. Colonic necrosis can be miss up to approximately 20% to 25% of the time when non-operative modalities are used. Surgical treatment and will vary based on patient stability and findings seen intraoperatively. Intraoperatively, the surgeon will ascertain if there is bowel compromise or if the bowel is viable. These findings will help dictate appropriate surgical intervention 6.
For patients who are stable with no bowel compromise, an ileocolic resection or a right hemicolectomy should be performed. In patients that receive an ileocolic resection, an additional colopexy to tack the right remnant colon to the posterior peritoneum to minimize the recurrence of another volvulus.
For patients who are hemodynamically unstable without bowel compromise, a cecopexy should be performed in conjunction with a cecostomy tube placement or cecopexy can be done alone.
For patients who are stable with bowel, the surgeon should proceed with a right hemicolectomy or ileocolic resection followed by an ileocolic anastomosis.
For patients who are unstable with bowel, the surgeon should proceed with a right hemicolectomy or ileocolic resection with an ileostomy creation. Later, once the patient is stabilized, the ileostomy may be reversed.
Common complications after cecal volvulus treatment include:
- Wound infection
- Sepsis
- Anastomotic leak
- Colocutaneous fistula
- Pelvic or abdominal abscess
Postoperative and rehabilitation care
Patients often require a prolonged stay in the hospital. Most patients are elderly and frail. If the ileus is prolonged, they often require IV fluids for a few days. DVT prophylaxis and physical therapy are recommended.
Cecal volvulus prognosis
Cecal volvulus is not a benign disorder. If the treatment is delayed, it carries a mortality in excess of 30%. Most studies indicate that the time to treat should be within 24-72 hours after diagnosis. This much time is required for hydration and any investigations. Even after cecal volvulus is treated, patients have high morbidity due to a prolonged ileus, wound infection, respiratory failure, and bowel obstruction 7.
There are only small case series and isolated reports on outcomes of patients managed with cecal volvulus. For those who have delayed diagnosis, the outcomes are poor. Even those who undergo timely surgery have high morbidity as a consequence of their age. Laparoscopic surgery is preferred to open surgery but sometimes the urgency of the situation may not allow it. No matter how one approaches the patient, the family must be fully informed of the potential complications, including recurrence and a stoma 8.
Sigmoid volvulus
Sigmoid volvulus is an abnormal twisting of the sigmoid colon along its mesenteric axis that causes closed-loop obstruction and can lead to ischemia, perforation, and death. Sigmoid volvulus is the most common type of volvulus of the colon 9. Large bowel volvulus accounts for ~5% of all large bowel obstructions, with ~60% of intestinal volvulus involving the sigmoid colon 10. Sigmoid volvulus is more common in the elderly 11. Less common are caecal volvulus and volvulus of the transverse colon. Sigmoid volvulus presents most commonly in patients who are less mobile, bed bound and institutionalized, usually with a background of chronic constipation.
Sigmoid volvulus is more common in Africa, as the food intake is of high fiber and the base of the sigmoid mesentery in the African population is narrow compared with other ethnic groups, leading to an anatomical situation that makes the population more susceptible to developing a sigmoid volvulus.
In order for a volvulus to occur, the bowel needs to be able to twist around a narrow-based mesentery. This occurs mostly in less mobile patients with a history of chronic constipation, where the sigmoid colon becomes chronically distended and redundant 9.
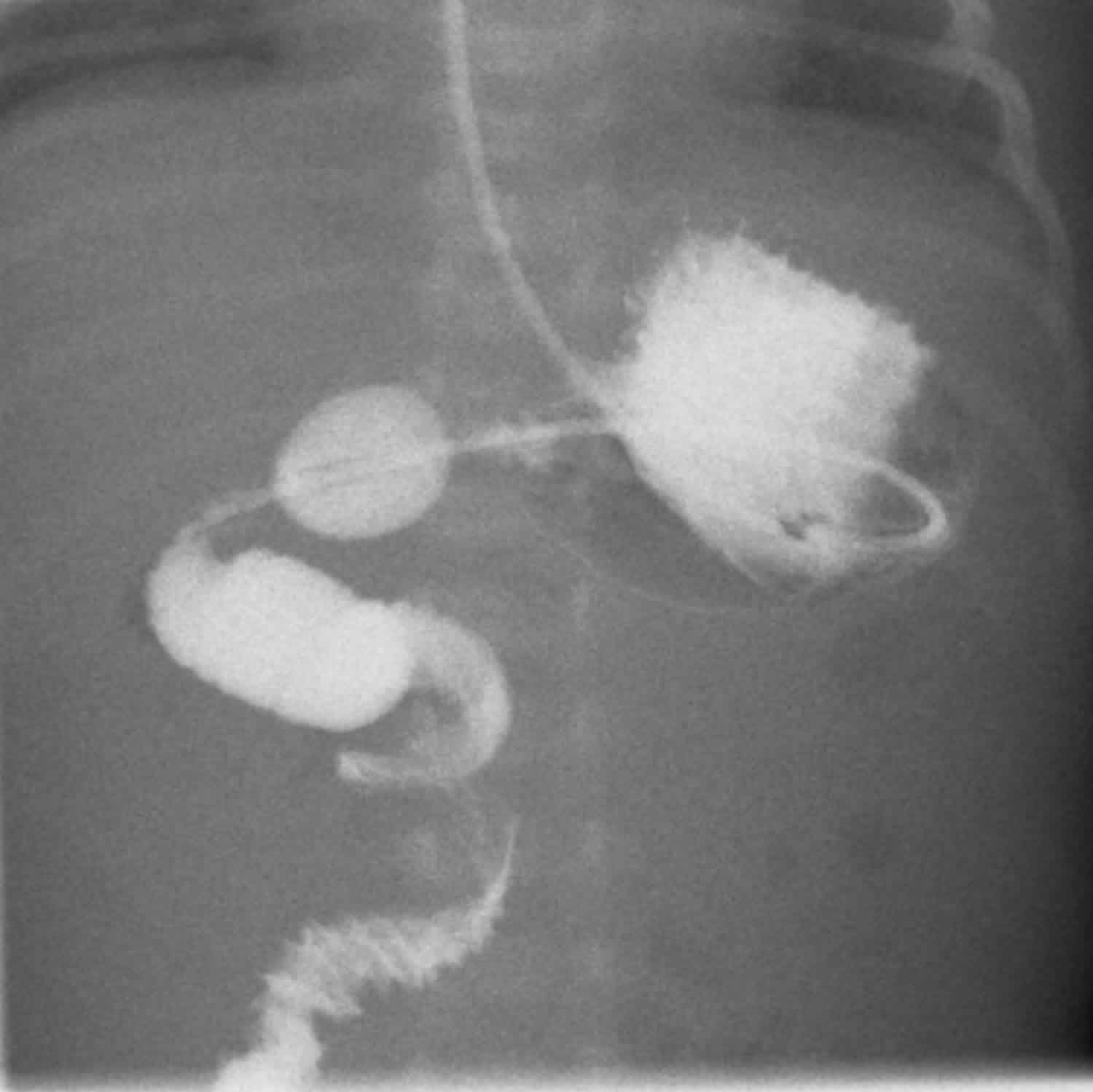
Figure 2. Sigmoid volvulus
Footnote: 85 year old male with one day of distension and progressive diffuse abdominal pain. Constipation but no fever or vomiting.
[Source 12 ]Sigmoid volvulus causes
There is a wide range of sigmoid volvulus causes; some are geographically-specific 13:
- Chronic constipation and/or laxative abuse
- Fiber-rich diet (especially in Africa)
- Chagas disease (especially in South America)
Associations
- chronic neurological conditions (e.g. Parkinson disease, multiple sclerosis, pseudobulbar palsy)
- medications from chronic psychiatric conditions (e.g. chronic schizophrenia)
Pathophysiology
Volvulus is a classical example of a large bowel closed loop obstruction. If inflow and outflow of the colon are both obstructed, the obstructed bowel will continue to distend, due to a large amount of gas forming bacteria trapped inside. This will eventually lead to a perforation of the obstructed segment.
While the colon is obstructed and distending, there is impaired blood supply, leading to ischemia, as well as bacterial translocation of the gut flora. Usually, the venous outflow is compromised first, increasing congestion even further, until arterial supply stops. The colonic mucosa is most susceptible to ischaemic insult, leading to an impaired barrier and translocation of bacteria, until the ischemia affects muscular and serosa, leading to necrosis and perforation.
Sigmoid volvulus can become a recurrent situation, and in those patients treated conservatively, the base of mesentery will eventually become fibrotic and the bowel chronically distended.
Sigmoid volvulus signs and symptoms
Patients presenting with volvulus are usually of an older age group with potential other comorbidities, often have reduced mobility or are bed bound and commonly get referred from residential and nursing homes. A history of chronic constipation is common. The symptoms usually leading to acute hospital admission are a loss of appetite and reduced oral intake, increasing abdominal distension, and cessation of bowel output. Patients complain of discomfort due to the significant distension, but are rarely in pain, unless ischemia and/or a perforation have occurred. They can, however, have respiratory compromise due to the splinting of the diaphragm that is a result of the colonic distension.
Patients may present with sigmoid volvulus as a recurrent problem if they have been treated with conservative measures in the past. A recurrent episode of volvulus needs to be taken a seriously as a first presentation and requires the same attention to history and physical examination as a patient presenting with volvulus for the first time.
Examination of the abdomen reveals significant distension, a generalized tympanitic percussion note and potentially guarding and rebound over areas of ischemia or impending perforation. If a perforation has already occurred, the patient will be grossly peritonitic. Digital rectal examination reveals an empty and often capacious rectum.
Sigmoid volvulus diagnosis
The patient should have the standard blood work (full blood count and renal function tests), to aid in resuscitation and assess the kidney function for a potential CT scan with contrast. Plain abdominal radiographs will show the classical coffee bean or kidney bean sign, and often dilatation of the proximal colon. Depending on the duration of symptoms, the proximal colon can decompress into the distal small bowel, as long as the ileocaecal valve is incompetent. CT scan shows the characteristic “whirl” appearance of the twisted mesentery, as well as the distended loop of sigmoid colon with an air-fluid level. Free air on either the abdominal radiograph or the CT scan indicates a more serious bowel perforation and requires immediate action.
A CT scan is recommended to establish the diagnosis and distinguish the etiology from other causes of large bowel obstruction, such as a malignant tumor. This is especially the case if the patients present with symptoms for the first time and have not had any previous colonic investigations such as a colonoscopy.
Sigmoid volvulus treatment
Rectal tube insertion is successful in treating 90% of cases 13. The mortality rate is 20-25% 11. The most serious complication is bowel ischemia.
Before any surgical intervention, the patient needs to be adequately resuscitated with intravenous fluids, and electrolyte imbalances should be corrected. A nasogastric tube can aid proximal decompression. Decompression of the sigmoid volvulus should be attempted with a soft rectal flatus tube by the bedside, ideally feeding the tube under direct vision through a rigid sigmoidoscope. Flexible Sigmoidoscopy with gentle insufflation is indicated if the bedside decompression fails or if there are concerns about the viability of the bowel wall, as the mucosa can be inspected during the sigmoidoscopy and areas of mucosal ischemia will become obvious.
Bedside decompression with a flatus tube should only be carried out by experienced physicians, and under no circumstance against resistance, as there is a risk of inadvertent iatrogenic perforation. The safest method to decompress the sigmoid colon is under direct vision with rigid or flexible sigmoidoscopy.
A successful decompression will immediately result in the evacuation of liquid and gas per rectum with subsequent resolution of the abdominal distension, resulting in a soft abdomen.
This resolution can be documented on a repeat abdominal radiograph.
It is important to assess the patient for sustained resolution once the flatus tube has been removed and the patient is started on oral intake, to avoid the volvulus recur before the patient is even discharged.
Those patients who cannot be decompressed or who have progressed to compromised viability of the colon will need surgical intervention. The surgery of choice is a sigmoid colectomy with either a primary anastomosis or an end colostomy, depending on findings during the surgery and the individual patients’ physiological reserves.
A patient presenting with bowel perforation will require aggressive resuscitation and an immediate laparotomy to control the fecal contamination and remove the perforated segment of bowel.
Patients presenting with recurrent episodes of sigmoid volvulus that can be decompressed should have an informed discussion about the benefits and risks of an elective resection of the sigmoid to prevent further episodes of volvulus leading to emergency admission to hospital. In the elective situation, a sigmoid colectomy can usually be performed with a primary anastomosis instead of an end colostomy, unless the patient has significant comorbidities.
Gastric volvulus
Gastric volvulus is a rare, clinical event that occurs in both adults and pediatric patients. A gastric volvulus occurs when the stomach rotates on itself at least 180 degrees along its transverse or longitudinal axis 14. It should be at least 180° and cause bowel obstruction to be called gastric volvulus. Merely gastric rotation on its root is not considered gastric volvulus.
Gastric volvulus occurs in children usually less than 1 year of age and occurs in older adults, those who are older than 50 years. There does not seem to a predilection for gastric volvulus for either gender or race. The most common cause of a gastric volvulus in both children and adults is a paraesophageal hernia.
Organo-axial volvulus is more common in adults, responsible for 60% of presentations. Mesentero-axial volvulus is more common in children.
Gastric strangulation is a complication that can occur after the development of acute gastric volvulus. Gastric volvulus causes a foregut obstruction in the patients. Gastric volvulus may present either acutely, or it may present with intermittent, recurrent, and chronic symptoms. When the stomach twist on itself there is always a risk for stomach strangulation with necrosis, perforation, and shock. The mortality for an acute volvulus can range from 30% to 50%, thus highlighting the importance of early diagnosis and treatment of gastric volvulus.
Timely diagnosis and treatment of acute gastric volvulus can potentially decrease morbidity and mortality. Patients can simply present with mild abdominal pain associated with nausea and vomiting, without emesis. Other patients can present with sepsis from necrosis of their volvulus and similar chief complaints.
Surgical repair, including stomach detorsion and gastropexy, is the main treatment modality for gastric volvulus. Detorsion may be performed open or laparoscopically. If the stomach is strangulated or necrotic, gastric resection may be required.
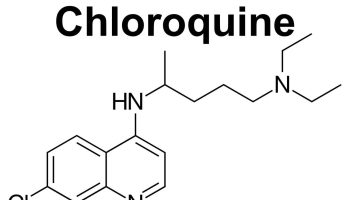
Figure 3. Gastric volvulus (organoaxial volvulus)
Footnote: 4 year old boy presented with acute abdominal pain, tenderness and dyspnea. The stomach twists along its own longitudinal axis giving rise to organoaxial volvulus. Organoaxial volvulus is the most common gastric volvulus and occurs secondary to diaphragmatic trauma or paraesophageal hernia. When the stomach twists along its longitudinal axis the esophago-gastric junction lies below the pyloro-duodenal junction.
[Source 15 ]Gastric volvulus subtypes
Both subtypes are surgical emergencies.
Organo-axial volvulus
- more common of the two types in adults (2/3 of cases)
- commonly occurs in the setting of trauma or para-esophageal hernia
- stomach is rotated along its long axis (along the cardiopyloric line, which is drawn between the cardia and the pylorus)
- mirror image of normal anatomy can occur with reversal of the greater and lesser curves
- antrum rotates anterosuperiorly
- fundus rotates posteroinferiorly
- complete (>180º) present with obstruction or ischemia
- incomplete rotation (<180º) also called organo-axial position of the stomach, usually asymptomatic
Mesentero-axial volvulus
- less common in adults, but is more common than organo-axial volvulus in the pediatric population (59% of gastric volvulus)
- rotation around short axis from the lesser to greater curvature (i.e. perpendicular to the cardiopyloric line)
- usually incomplete, <180°
- displacement of antrum above gastro-esophageal junction; stomach appears upside-down with the antrum and pylorus superior to the fundus and proximal body
- coincides with the axis of mesenteric attachment and is associated with severe obstruction and strangulation
- less associated with diaphragmatic defect
- plain films may show an intrathoracic stomach with two air fluid levels 16
Gastric volvulus causes
In 10% to 30% of cases, gastric volvulus is considered primary and results from laxity and disruption of the stomach’s ligamentous attachments (gastrohepatic, gastrocolic, gastrolienal, and gastrophrenic). For the majority of cases, gastric volvulus is caused by a gastric, splenic, or diaphragmatic anatomic disorder, the most common being a diaphragmatic hernia or an abnormality in gastric function. The organoaxial rotation of the stomach as described by Singleton is the most common gastric volvulus (two-thirds of cases) and occurs when the stomach rotates around the pylorus and the gastroesophageal (GE) junction. Mesenteroaxial rotation is less common (one-third of cases), and occurs when the stomach rotates longitudinal line parallel to the gastrohepatic omentum.
Associations
- wandering spleen 17
- congenital diaphragmatic hernia
- diaphragmatic eventration
- laparoscopic adjustable gastric banding 18
Gastric volvulus signs and symptoms
Patients may present with the classic triad of Borchardt:
- severe sudden epigastric pain
- intractable retching without vomiting
- inability to pass a nasogastric tube
Chronic symptoms are more common in patients with mesentero-axial volvulus.
A patient’s clinical presentation depends on the speed of onset, the type of stomach rotation (volvulus), and the completeness of the foregut obstruction. The presentation of an acute gastric volvulus can be quite severe with acute epigastric abdominal pain associated with severe retching. In 1904, Borchardt described the triad of acute epigastric pain, retching with the inability to vomit, and the difficulty or inability to pass a nasogastric tube. This triad occurs in up to 70% of patients who present with an acute organoaxial volvulus. The nasogastric tube passes easily in patients who present with an acute mesenteroaxial volvulus, as the lower esophageal sphincter remains open. The opposite is appreciated with organoaxial volvulus, as the nasogastric tube is more difficult to pass, due to the involvement of more proximal structures including the lower esophageal sphincter, the fundus, or the cardia. Patients who present with chronic, intermittent, and vague signs and symptoms of upper abdominal pain, nausea, dysphagia, early satiety vomiting, and hiccups may have a chronic partial or intermittent gastric volvulus.
Gastric volvulus diagnosis
The diagnosis of a gastric volvulus can be suspected with a good history and physical exam; however, diagnosis can be difficult. The diagnosis of a gastric volvulus may be confirmed radiologically when patients are symptomatic. Plain chest x-ray films that are suspicious for a gastric volvulus are those that demonstrate a spherical stomach or a double air-fluid level on upright chest films and the retrocardiac air-fluid level above the diaphragm on lateral chest film. Albas et al. described 4 radiologic findings predictive for a gastric volvulus on an upper gastrointestinal (GI) contrast study by showing gastric air-fluid level above the diaphragm, a paucity of distal bowel gas, reversal of the relative position of the greater curvature of the stomach, and a downward pointing pylorus. A barium swallow may be helpful as an adjunct to chest x-ray. Computed tomography (CT) scans of the chest, abdomen, and pelvis can also be diagnostic. CT scan of the chest, abdomen, and pelvis can provide information about the nature of volvulus, and other intraabdominal organs that may be involved, thus assisting pre-operative planning.
Gastric volvulus treatment
The traditional treatment for a patient presenting with an acute gastric volvulus has been an immediate operation reducing and untwisting the volvulus. This remains the gold standard; however, attempted medical management may be useful in patients that are a very high risk for surgery. Immediate surgical resection is required for necrosis or perforation of the stomach. Simultaneously, the diaphragmatic hernia should be reduced and closed. The stomach is then fixed to the anterior abdominal wall with suture, or by the placement of a gastrostomy tube. Open surgery, or the combination of laparoscopic and endoscopic surgical techniques, have good results. Laparoscopy, when used to repair chronic and intermittent gastric volvulus, is often be less morbid than an open operation. Patients who are fit enough to undergo a surgical procedure should proceed to have their chronic gastric volvulus repaired because of the high morbidity and mortality (30% to 50%) associated with strangulated gastric volvulus.
Good results have also been reported with conservative treatment of an acute gastric volvulus in elderly patients if they are not presenting in extremis. Conservative treatment has also been used to help patients with intermittent and chronic volvulus. The patient should be kept sitting upright, and a nasogastric tube should be gently inserted to decompress the stomach. The patient should be adequately resuscitated and re-evaluated often. Some high-risk, elderly patients can be treated endoscopically with decompression and reduction of the stomach, and placement of a percutaneous gastrostomy tube to gastropexy the stomach to the abdominal wall. Percutaneous gastrostomy placement can be done as an adjunct in ill patients with chronic or intermittent volvulus, or that may have other critical issues that need to be handled before definitive surgery, for example, sepsis from another source.
Midgut volvulus
A midgut volvulus of malrotated bowel can potentially occur at any age but in approximately 75% of cases occur within a month of birth 19. Most of these are within the first week 20, with 90% occuring within 1 year 21. Typically the infant is entirely normal for a period before suddenly presenting with bilious vomiting. If the midgut volvulus does not spontaneously reduce, then the venous obstruction created by the superior mesenteric vein wrapped around the superior mesenteric artery results in venous obstruction and gradual onset of ischemia and eventual necrosis. As this occurs, the abdomen becomes swollen as fluid accumulates in the lumen of the bowel, and becomes tender. Eventually, peritonitis and shock become established.
Midgut volvulus occurs as a complication of intestinal malrotation. A midgut volvulus is usually part of a vascular compromise in the intestinal mesentery in intestinal malrotation. Anomalies of rotation and fixation are twice as common in males as in females 22. They are classified as non-rotation, incomplete rotation, reverse rotation, and anomalous fixation of the mesentery.
A small portion patients that present with malrotation will demonstrate chronic obstructive symptoms. These symptoms may result from Ladd bands across the duodenum or, occasionally, from intermittent volvulus. Symptoms include intermittent abdominal pain and intermittent vomiting, which may occasionally be bilious. Infants with malrotation may demonstrate a failure to thrive, and they may be diagnosed initially as having gastroesophageal reflux disease (GERD).
Urgent surgical repair (Ladd procedure) is required to prevent ischemia or to resect infarcted bowel loops. If resection is performed stomas are usually created. Additionally, the Ladd bands are divided and the mesenteric pedicle widened. In some instances, pexy (surgical fixation) of the duodenum and cecum may be performed although it is unclear if this is of benefit in preventing recurrence 23. It should be noted that normal anatomical positioning is not achieved; the duodenum and small bowel remain on the right, and the cecum and colon are on the left side of the abdomen 23.
Figure 4. Midgut volvulus
Footnote: 6 weeks old infant with bilious vomiting and abdominal pain. Contrast has been administered via a nasogastric tube to a child. It passes from the stomach into the duodenum. Contrast demonstrates a malplaced duodenojejunal flexure and a corkscrew appearance of the jejunum. This confirms both malrotation and volvulus. The duodenojejunal flexure should usually be located to the left of midline at the level of the duodenal cap. Here it is not, indicating that there is malrotation. The lumen is narrowed and passes directly inferiorly in a corkscrew pattern. Findings are of midgut volvulus secondary to intestinal malrotation.
[Source 24 ]Midgut volvulus causes
During fetal development, the intestines develop as three portions. These are foregut, midgut, and hindgut. The midgut portion of the intestines undergoes normal rotation during the four weeks and six weeks of gestation. The fetal midgut intestines develop so rapidly that the abdominal cavity cannot house the all the intestines. Therefore, a portion of intestines herniates into the umbilical cord. The intestines herniate back into the abdominal cavity with a 270-degree counter-clockwise rotation around the bloody supply to midgut, the superior mesenteric artery. The fourth portion of the duodenum and proximal jejunum of the intestines acquires a C-loop, with the development of the ligament of Treitz, and is superior to the superior mesenteric artery. The cecal portion of the intestine becomes fixed to the retroperitoneum, superior to the superior mesenteric artery, in a diagonal axis at approximately the level of the T12 vertebra to the level of the right of the L5 vertebra.
Genetic mutations likely disrupt the signaling critical for normal intestinal rotation. For instance, mutations in the gene BCL6 leading to the absence of left-sided expression of its transcript result in malrotation. In an incomplete rotation, the cecum remains in the epigastrium, and the fibrotic band forms from the duodenum to the retroperitoneum as the cecum continues to form. The band, also knowns as Ladd’s bands, crosses over the duodenum, connecting the cecum to the lateral abdominal wall. The Ladd’s band creates a potential point of obstruction.
The mesenteric takeoff is then confined to the epigastrium leading to a narrow pedicle, constricting all the branches of the superior mesenteric artery that supplies the midgut. A volvulus can occur around the mesentery which then obstructs the proximal jejunum and causes ischemia to the midgut. Obstruction and bowel ischemia can then ensue if the problem is not promptly corrected surgically.
Associations
These include 25:
- gastroschisis
- omphalocele
- diaphragmatic hernia
- duodenal or jejunal atresia
Midgut volvulus signs and symptoms
Midgut volvulus can happen at any age, but most commonly occurs during the first few weeks of life. Bilious emesis is usually the first sign of volvulus. Infants that present with bilious vomiting, acute duodenal obstruction, or abdominal tenderness associated with hemodynamic deterioration must be rapidly evaluated to ensure that they do not have intestinal malrotation along with volvulus, as this should raise particular suspicions for this diagnosis. If left untreated, vascular compromise of the midgut initially causes bloody stools but eventually results in circulatory collapse. Physical exam findings for the advanced disease will show signs of peritonitis suggestive of intestinal ischemia with erythema and edema of the abdominal wall which will lead to shock and death if left untreated. An index of suspicion for this condition must be high, as the abdominal signs are minimal early in the disease process. Plain abdominal x-rays show a paucity of gas throughout the intestine with a few scattered air-fluid levels. When these findings are present, the patient should undergo immediate fluid resuscitation to ensure adequate perfusion and urine output followed by prompt exploratory laparotomy. In cases where the child is stable, consider laparoscopy.
In older children and adults, abdominal pain is the most common symptom and may present with abrupt onset over hours or days or as chronic intermittent pain over weeks, months, or years. Intermittent vomiting, chronic diarrhea, malabsorption, or failure to thrive comprises other potential presenting symptoms.
Midgut volvulus diagnosis
The patient may not always appear ill, and the plain films may suggest partial duodenal obstruction. Upper gastrointestinal series that shows incomplete rotation with the duodenojejunal junction displaced to the right is the best indication of obstruction. The duodenum may show a corkscrew effect diagnosing volvulus or complete duodenal obstruction, with the small bowel looping entirely on the right side of the abdomen. A barium enema may show a displaced cecum, but this sign is unreliable, especially in a small infant in whom the cecum is normally in a somewhat higher position than in an older child.
Midgut volvulus treatment
When volvulus is suspected, early surgical intervention is mandatory if the ischemic process is to be prevented or reversed. Volvulus occurs clockwise and is therefore untwisted counterclockwise; which one can remember with the phrase “turning back the hands of time.”
Follow by a Ladd procedure, named after William Edward Ladd, the pediatrician who first performed the procedure in 1936. This operation does not correct the malrotation but instead helps to open the narrow mesenteric pedicle to prevent volvulus from recurring. The Ladd procedure is performed by lysing the band formed between the cecum and the lateral abdominal wall as well as duodenum and terminal ileum, which allows the superior mesenteric artery to relax. This maneuver allows the duodenum to relax into the right lower quadrant and the cecum into the left lower quadrant; these structures do not need to be secured with a suture. An appendectomy (removal of the appendix) is also done to circumvent errors in the event patient has diagnostic imaging.
When a patient presents with advanced ischemia, a simple reduction of the volvulus without the Ladd procedure should be performed followed by a “second-look” laparotomy which is performed 24 to 36 hours later to evaluate the vascular integrity of the small intestines.
A transparent plastic silo may be placed to facilitate constant evaluation of the intestine and to plan for the timing of re-exploration. If a necrotic bowel is present, then the surgeon can conservatively resect it to ensure adequate length for feeding and prevention of short-gut syndrome. With early diagnosis and correction, the prognosis is excellent. Delay can lead to mortality or short-gut syndrome requiring intestinal transplantation.
Midgut volvulus prognosis
Prognosis is dependent on the state of the small bowel and presence of systemic shock. In cases where no ischemia of the bowel is present, and the child is otherwise well, the prognosis is extremely good. Overall a mortality of 3-9% is reported 23.
Small bowel obstruction for adhesions is seen a distant complication in 5-10% of cases.
Volvulus causes
Volvulus occurs when redundant and loose mesentery twist around an axis. Volvulus is associated with intestinal malrotation, an enlarged colon, a long mesentery, Hirschsprung disease, pregnancy, abdominal adhesions, and chronic constipation. In adults, the sigmoid colon is most affected, with the cecum being second most affected. In children, the small intestine is more commonly involved.
Volvulus is typically caused by two mechanisms:
- chronic constipation and
- a high-fiber diet
In both the instances, the sigmoid colon becomes dilated and heavy making it susceptible to torsion. With repeated attacks of torsion, the mesentery shortens. The chronic inflammation leads to the formation of adhesions which then entrap the sigmoid colon into fixed twisted position.
In cecal volvulus, the predominant symptom is small bowel obstruction (nausea, vomiting, and lack of flatus), because the obstructing point is close to the ileocecal valve and small intestine.
In sigmoid volvulus, although pain may be present, constipation may be more prominent.
Volvulus causes severe pain with an accumulation of gas and fluid in the portion of the bowel obstructed resulting in necrosis of the affected intestinal wall, acidosis, and death. This is known as a closed loop obstruction. Acute volvulus requires immediate surgical intervention to untwist the affected segment of bowel.
Volvulus may occur in patients with Duchenne muscular dystrophy due to the smooth muscle dysfunction.
Volvulus symptoms
Patients with volvulus are usually debilitated and bedridden. Many of these individuals have a history of neuropsychiatry dysfunction, and thus, a medical history is usually unavailable.
Signs and symptoms of volvulus include pain, bloating, vomiting, constipation, bloody stool, fever, and significant pain when the abdomen is palpated. Depending on the duration of the condition, there may be signs of peritonitis and bleeding per rectum. The severe abdominal distension can also compromise respiration in some patients.
Volvulus complications
Complications of volvulus include gangrene, strangulation, perforation fecal peritonitis, and recurrent volvulus.
Volvulus diagnosis
Diagnosis usually is made by taking a thorough history and performing a physical examination; it is confirmed by radiographic studies. The diagnosis of colonic volvulus usually is included in the differential diagnosis which also includes bowel obstruction, mesenteric ischemia, and malignancy.
Abdominal plain x-rays may be confirmatory for a volvulus, especially if a “bent inner tube” or a “coffee bean” sign are seen. These refer to the appearance of the air-filled closed loop of the colon which forms the volvulus. A barium enema is used to demonstrate a “bird’s beak” at the point where the segment of proximal bowel and distal bowel rotate to form the obstructing volvulus. This area will show an acute and sharp tapering that has the appearance of a bird’s beak. If a perforation is suspected, barium should be avoided due to its potentially lethal effects when distributed throughout the free intraperitoneal cavity. Gastrografin, which is safer, can be substituted for barium.
In approximately 80% of colonic obstructions, a carcinoma invading the wall of the intestine is found to be the cause of the obstruction. This is usually easily diagnosed with CT scan and endoscopic biopsies.
Volvulus treatment
Initial treatment for sigmoid volvulus is sigmoidoscopy or a barium enema. Due to a high recurrence rate, a bowel resection within two days is recommended. In a cecal volvulus, part of the bowel often needs to be removed.
Treatment for sigmoid volvulus includes sigmoidoscopy. If the mucosa of the sigmoid looks normal, place a rectal tube for decompression, correct electrolytes, ensure adequate fluids, and optimize cardiac, renal and pulmonary abnormalities. The patient should then be taken for surgical repair. If surgery is not performed, there is a high rate of recurrence of volvulus and obstruction. For patients with signs of sepsis or an acute abdominal catastrophe, immediate surgery and resection are advised. In a cecal volvulus, the cecum may be returned to a normal position and then sutured in place via a procedure known as cecopexy. If the bowel is obviously necrotic, then resection with an ileostomy or a colostomy is necessary.
Volvulus surgery
Over the years many surgical techniques have been developed to treat cecal and sigmoid volvulus. In general, conservative procedures where the bowel is adhered with sutures are often associated with higher recurrence rates compared to procedures that involve resection of the bowel. Whether to do the surgery via an open or laparoscopic method depends on surgeon preference and experience. Elderly patients may benefit from minimally invasive procedures.
Volvulus prognosis
Delay in diagnosis and treatment of volvulus is associated with a high morbidity and mortality. The mortality is 30% to 40% in patients in whom treatment of cecal volvulus is delayed.
The recommended interval between endoscopic decompression and surgical intervention is 48 to 72 hours. This allows time for investigation, resuscitation, and intervention to reduce surgical risk 1.
- Even when volvulus is successfully treated with endoscopic decompression and surgical resection, mortality is still 12% to 15%.
- 50% of patients who undergo endoscopic decompression alone experience recurrence.
- Endoscopic decompression alone for sigmoid volvulus carries a recurrence rate of 40% to 50% and a mortality of 25% to 30% after surgical treatment of the recurrence.
- Bhimji SS, Cooper W. Volvulus. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441836[↩][↩][↩]
- Le CK, Qaja E. Cecal Volvulus. [Updated 2018 Nov 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470305[↩][↩][↩][↩][↩][↩][↩]
- Kaushal-Deep SM, Anees A, Khan S, Khan MA, Lodhi M. Primary cecal pathologies presenting as acute abdomen and critical appraisal of their current management strategies in emergency settings with review of literature. Int J Crit Illn Inj Sci. 2018 Apr-Jun;8(2):90-99.[↩]
- Lung BE, Yelika SB, Murthy AS, Gachabayov M, Denoya P. Cecal bascule: a systematic review of the literature. Tech Coloproctol. 2018 Feb;22(2):75-80.[↩]
- Dane B, Hindman N, Johnson E, Rosenkrantz AB. Utility of CT Findings in the Diagnosis of Cecal Volvulus. AJR Am J Roentgenol. 2017 Oct;209(4):762-766.[↩]
- Miura da Costa K, Saxena AK. A systematic review of the management and outcomes of cecal and appendiceal volvulus in children. Acta Paediatr. 2018 Dec;107(12):2054-2058.[↩]
- Gomes CA, Soares C, Catena F, Di Saverio S, Sartelli M, Gomes CC, Gomes FC. Laparoscopic Management of Mobile Cecum. JSLS. 2016 Oct-Dec;20, 4.[↩]
- Ramírez-Ramírez MM, Villanueva-Sáenz E, Ramírez-Wiella-Schwuchow G. [Elective laparoscopic right colectomy for caecal volvulus: case report and literature review]. Cir Cir. 2017 Jan – Feb;85(1):87-92.[↩]
- Lieske B, Antunes C. Sigmoid Volvulus. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441925[↩][↩]
- Vandendries C, Jullès MC, Boulay-Coletta I et-al. Diagnosis of colonic volvulus: findings on multidetector CT with three-dimensional reconstructions. Br J Radiol. 2010;83 (995): 983-90. doi:10.1259/bjr/35714052[↩]
- Brant WE, Helms CA. Fundamentals of Diagnostic Radiology. Lippincott Williams & Wilkins. (2007) ISBN:0781761352.[↩][↩]
- Sigmoid volvulus. https://radiopaedia.org/cases/sigmoid-volvulus-6?lang=us[↩]
- Salati U, Mcneill G, Torreggiani WC. The coffee bean sign in sigmoid volvulus. Radiology. 2011;258 (2): 651-2. doi:10.1148/radiol.101882[↩][↩]
- Lopez PP, Megha R. Gastric Volvulus. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507886[↩]
- Gastric volvulus. https://radiopaedia.org/cases/gastric-volvulus-3?lang=us[↩]
- Menuck L. Plain film findings of gastric volvulus herniating into the chest. AJR Am J Roentgenol. 1976;126 (6): 1169-74.[↩]
- Liu HT, Lau KK. Wandering spleen: an unusual association with gastric volvulus. AJR Am J Roentgenol. 2007;188 (4): W328-30. doi:10.2214/AJR.05.0672[↩]
- Kicska G, Levine MS, Raper SE et-al. Gastric volvulus after laparoscopic adjustable gastric banding for morbid obesity. AJR Am J Roentgenol. 2007;189 (6): 1469-72. doi:10.2214/AJR.05.1547[↩]
- Peterson CM, Anderson JS, Hara AK et-al. Volvulus of the gastrointestinal tract: appearances at multimodality imaging. Radiographics. 29 (5): 1281-93. doi:10.1148/rg.295095011[↩]
- Devos AS, Blickman JG, Blickman JG. Radiological Imaging of the Digestive Tract in Infants and Children. Springer Verlag. (2007) ISBN:3540407332.[↩]
- Fischer JE, Bland KI. Mastery of surgery. Lippincott Williams & Wilkins. (2007) ISBN:078177165X[↩]
- Coste AH, Bhimji SS. Midgut Volvulus. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441962[↩]
- Fischer JE, Bland KI. Mastery of surgery. Lippincott Williams & Wilkins. (2007) ISBN:078177165X.[↩][↩][↩]
- Midgut volvulus. https://radiopaedia.org/cases/midgut-volvulus?lang=us[↩]
- Weissleder R, Wittenberg J, Harisinghani MG et-al. Primer of diagnostic imaging. Mosby Inc. (2007) ISBN:0323040683.[↩]