Contents
- Hair loss
- How does your hair grow?
- Types of Hair loss (Alopecia)
- Causes of hair loss
- How is hair loss diagnosed?
- Hair loss in men
- Hair loss in women
- Hair loss treatment
Hair loss
Hair loss (also known as alopecia) is a common problem and can affect just your scalp or your entire body. There are many types of hair loss with different symptoms and causes. Hair loss can occur in different patterns, depending on the cause. Hair loss (alopecia) can affect both men and women and also children.
Hair loss is a common problem that affects up to 50 percent of men and women throughout their lives 1. Hair loss can occur anywhere on the body, but more commonly affects just the scalp when the patient presents with concerns about the cosmetic effect.
Hair loss is not life threatening, but it is distressing and significantly affects a person’s quality of life.
Hair loss can cause significant worry and anxiety, but there are several ways of treating and managing hair loss. Treatment depends on the type of hair loss.
You should seek medical advice for hair loss if:
- you have recently started a new medicine;
- you are a woman and your hair loss is accompanied by excess growth of facial and body hair or you have acne;
- you have been diagnosed with (or think you may have) an autoimmune disorder such as systemic lupus erythematosis (SLE), nutritional deficiency or thyroid disease;
- you have been recently treated with chemotherapy or have used a hormonal medicine;
- the hair loss occurs in discrete patches;
- the hair loss is associated with scaling or inflammation of the scalp;
- you also have loss of body hair; or
- you are aware you have a compulsive hair-pulling habit.
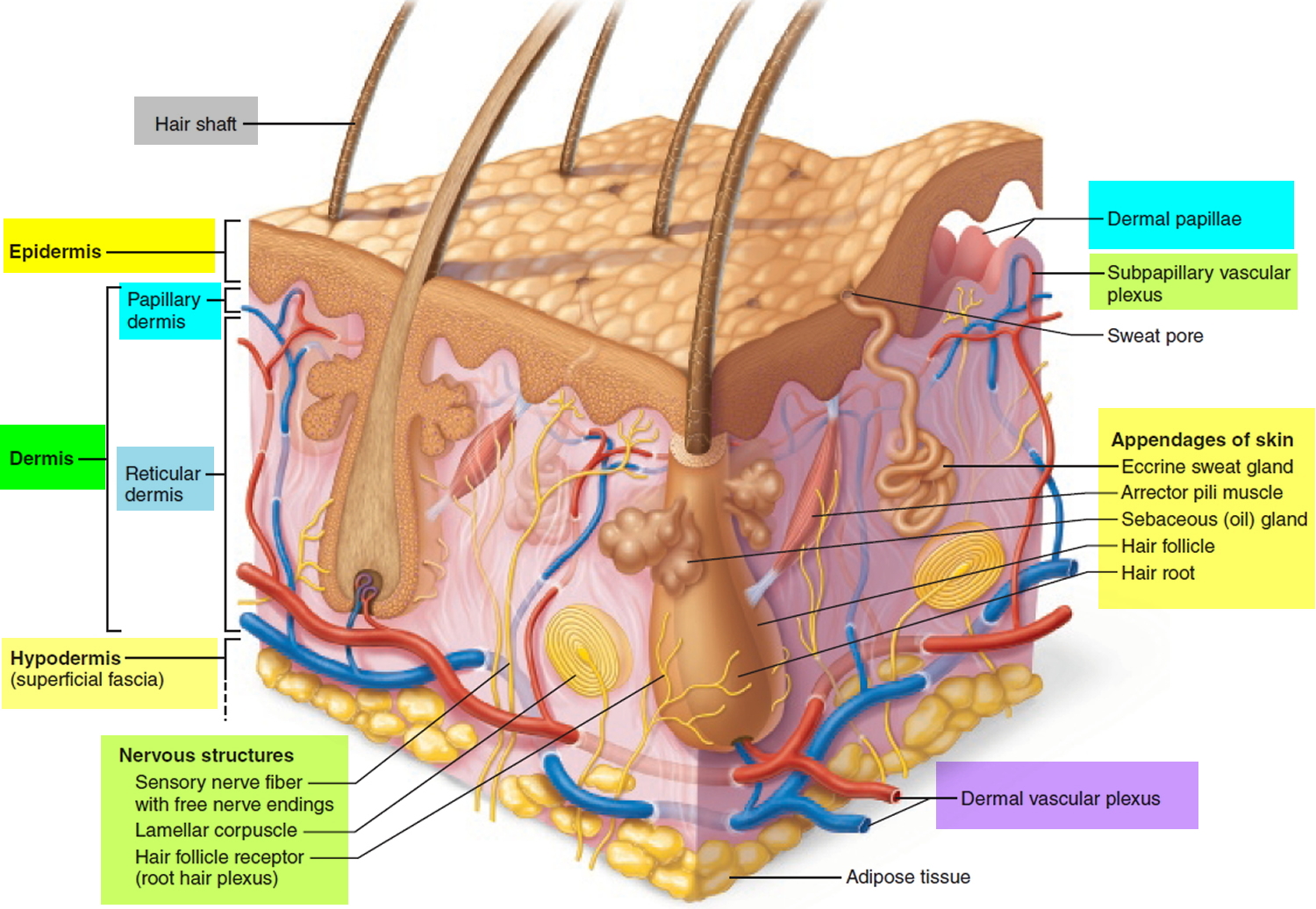
How does your hair grow?
Hair is a slender filament of keratinized cells that grows from an oblique tube in the skin called a hair follicle. Each hair is composed of columns of dead, keratinized epidermal cells bonded together by extracellular proteins. The hair shaft is the superficial portion of the hair, which projects above the surface of the skin. The hair root is the portion of the hair deep to the shaft that penetrates into the dermis, and sometimes into the subcutaneous layer.
Hairs project beyond the surface of the skin almost everywhere except the sides and soles of the feet, the palms of the hands, the sides of the fingers and toes, the lips, and portions of the external genitalia. There are about 5 million hairs on the human body, and 98 percent of them are on the general body surface, not the head. Hairs are nonliving structures that form in organs called hair follicles.
The density of hair does not differ much from one person to another or even between the sexes; indeed, it is virtually the same in humans, chimpanzees, and gorillas. Differences in apparent hairiness are due mainly to differences in texture and pigmentation.
Types of Hairs
Hairs first appear after about three months of embryonic development. These hairs, collectively known as lanugo, are extremely fine and unpigmented. Most lanugo hairs are shed before birth.
The two types of hairs in the adult skin are vellus hairs and terminal hairs:
- Vellus hairs are the fine “peach fuzz” hairs found over much of the body surface.
- Terminal hairs are heavy, more deeply pigmented, and sometimes curly. The hairs on your head, including your eyebrows and eyelashes, are terminal hairs. After puberty, it also forms the armpit and pubic hair, male facial hair, and some of the hair on the trunk and limbs.
Hair follicles may alter the structure of the hairs they produce in response to circulating hormones.
Figure 1. Hair structure
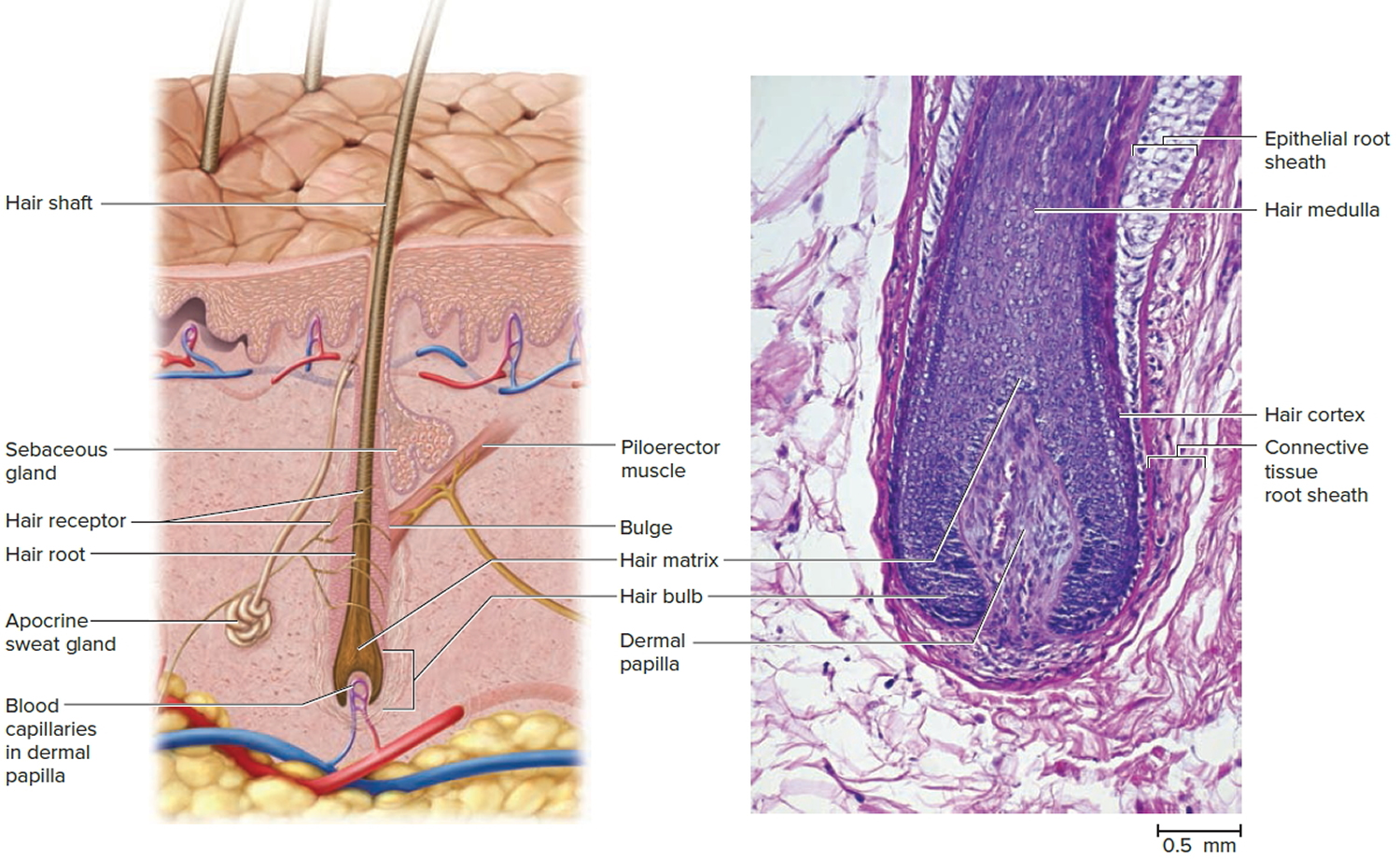
Figure 2. Hair follicle
Structure of Hair Follicle
The portion of a hair above the skin is called the shaft, and all that beneath the surface is the root. The root penetrates deeply into the dermis or hypodermis and ends with a dilation called the hair bulb. The only living cells of a hair are in and near the hair bulb. The hair bulb grows around a bud of vascular connective tissue called the dermal papilla, which provides the hair with its sole source of nutrition. Immediately above the papilla is a region of mitotically active cells, the hair matrix, which is the hair’s growth center. All cells higher up are dead.
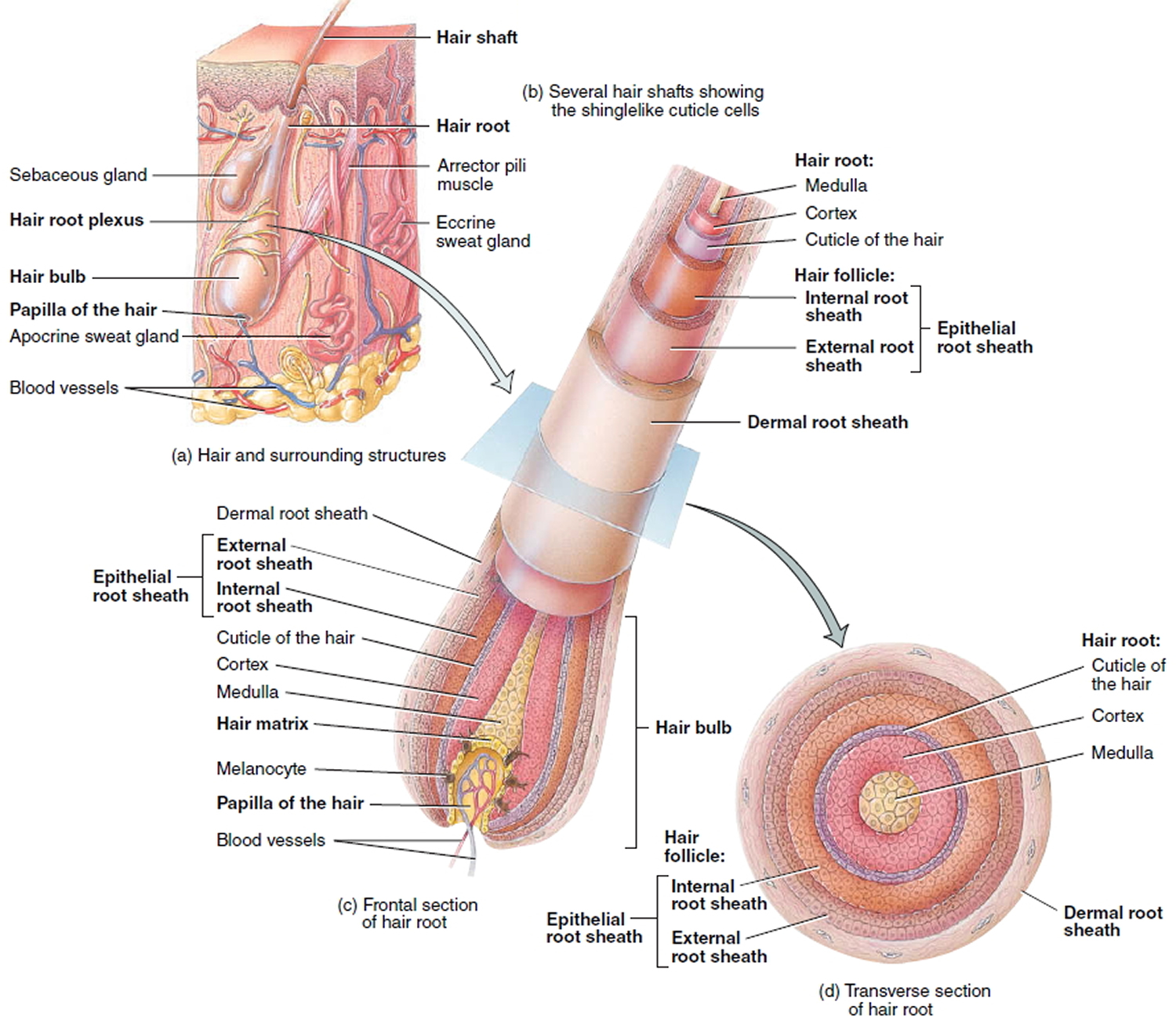
Figure 3. Hair follicle and hair structure
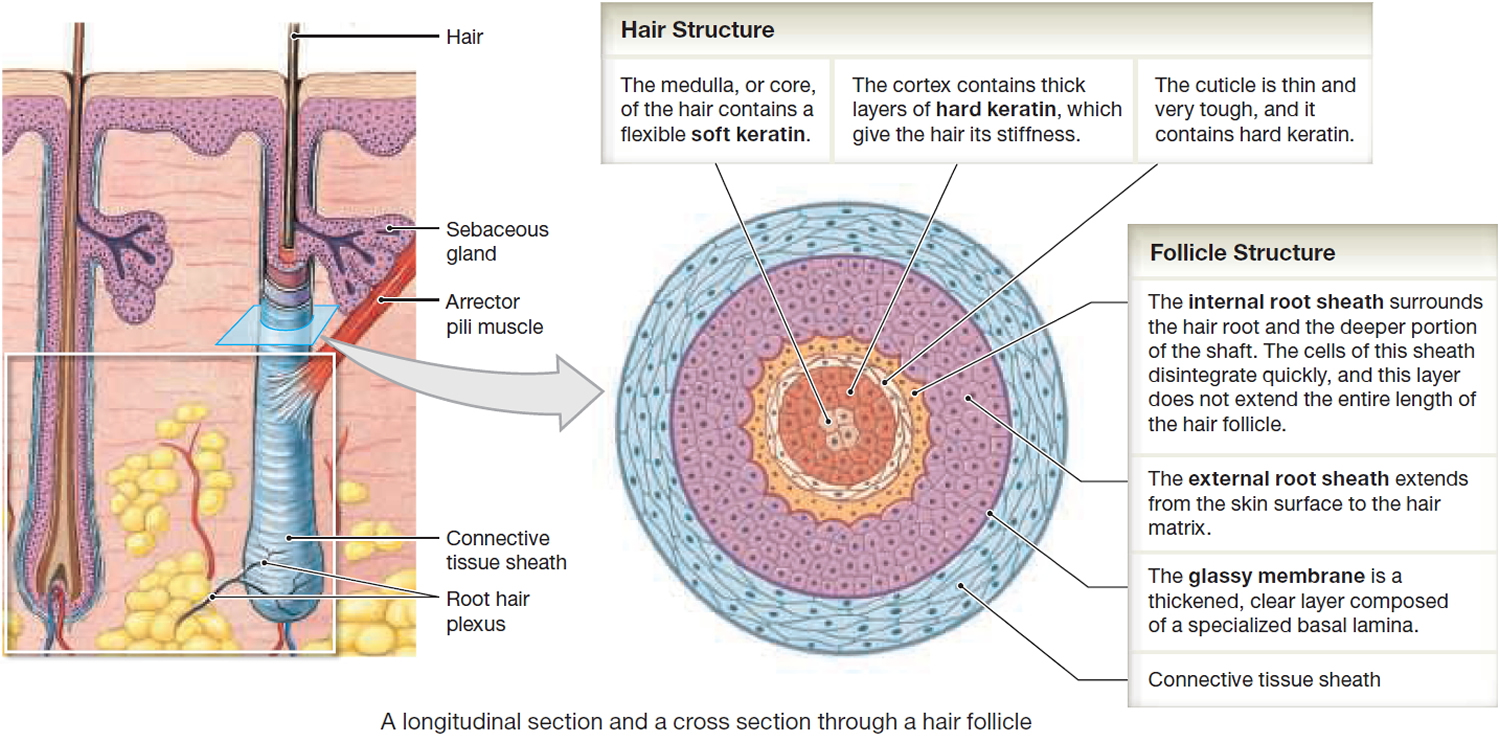
Hair Structure
In cross section, a hair reveals up to three layers. From the inside out, these are the medulla, cortex, and cuticle.
The medulla is a core of loosely arranged cells and air spaces. It is most prominent in thick hairs such as those of the eyebrows, but narrower in hairs of medium thickness and absent from the thinnest hairs of the scalp and elsewhere.
The cortex constitutes most of the bulk of a hair. It consists of several layers of elongated keratinized cells that appear cuboidal to flattened in cross sections.
The cuticle is composed of multiple layers of very thin, scaly cells that overlap each other like roof shingles with their free edges directed upward.
Hair Follicle
Cells lining the hair follicle are like shingles facing in the opposite direction. They interlock with the scales of the hair cuticle and resist pulling on the hair. When a hair is pulled out, this layer of follicle cells comes with it.
The hair follicle is a diagonal tube that contains the hair root. It has two principal layers: an epithelial root sheath and a connective tissue root sheath. The epithelial root sheath is an extension of the epidermis; it consists of stratified squamous epithelium and lies immediately adjacent to the hair root. Toward the deep end of the follicle, it widens to form a bulge, a source of stem cells for follicle growth. The connective tissue root sheath, which is derived from the dermis and composed of collagenous connective tissue, surrounds the epithelial sheath and is somewhat denser than the adjacent dermis.
Associated with the hair follicle are nerve and muscle fibers. Nerve fibers called hair receptors entwine each hair follicle and respond to hair movements. You can feel their effect by carefully moving a single hair with a pin or by lightly running your finger over the hairs of your forearm without touching the skin.
Each hair has a piloerector muscle—also known as a pilomotor muscle or arrector pili—a bundle of smooth muscle cells extending from dermal collagen fibers to the connective tissue root sheath of the follicle. In response to cold, fear, touch, or other stimuli, the sympathetic nervous system stimulates the piloerector to contract, making the hair stand on end and wrinkling the skin in such areas as the scrotum and areola. In humans, it pulls the follicles into a vertical position and causes “goose bumps,” but serves no useful purpose.
Figure 4. Hair structure
Hair Production
Hair follicles extend deep into the dermis, often projecting into the underlying subcutaneous layer. The epithelium at the follicle base surrounds a small hair papilla, a peg of connective tissue containing capillaries and nerves. The hair bulb consists of epithelial cells that surround the papilla.
Hair production involves a specialized keratinization process. The hair matrix is the epithelial layer involved in hair production. When the superficial basal cells divide, they produce daughter cells that are pushed toward the surface as part of the developing hair. Most hairs have an inner medulla and an outer cortex. The medulla contains relatively soft and flexible soft keratin. Matrix cells closer to the edge of the developing hair form the relatively hard cortex. The cortex contains
hard keratin, which gives hair its stiffness. A single layer of dead, keratinized cells at the outer surface of the hair overlap and form the cuticle that coats the hair.
The hair root anchors the hair into the skin. The root begins at the hair bulb and extends distally to the point where the internal organization of the hair is complete, about halfway to the skin surface. The hair shaft extends from this halfway point to the skin surface, where we see the exposed hair tip.
The size, shape, and color of the hair shaft are highly variable.
Growth and Replacement of Hair
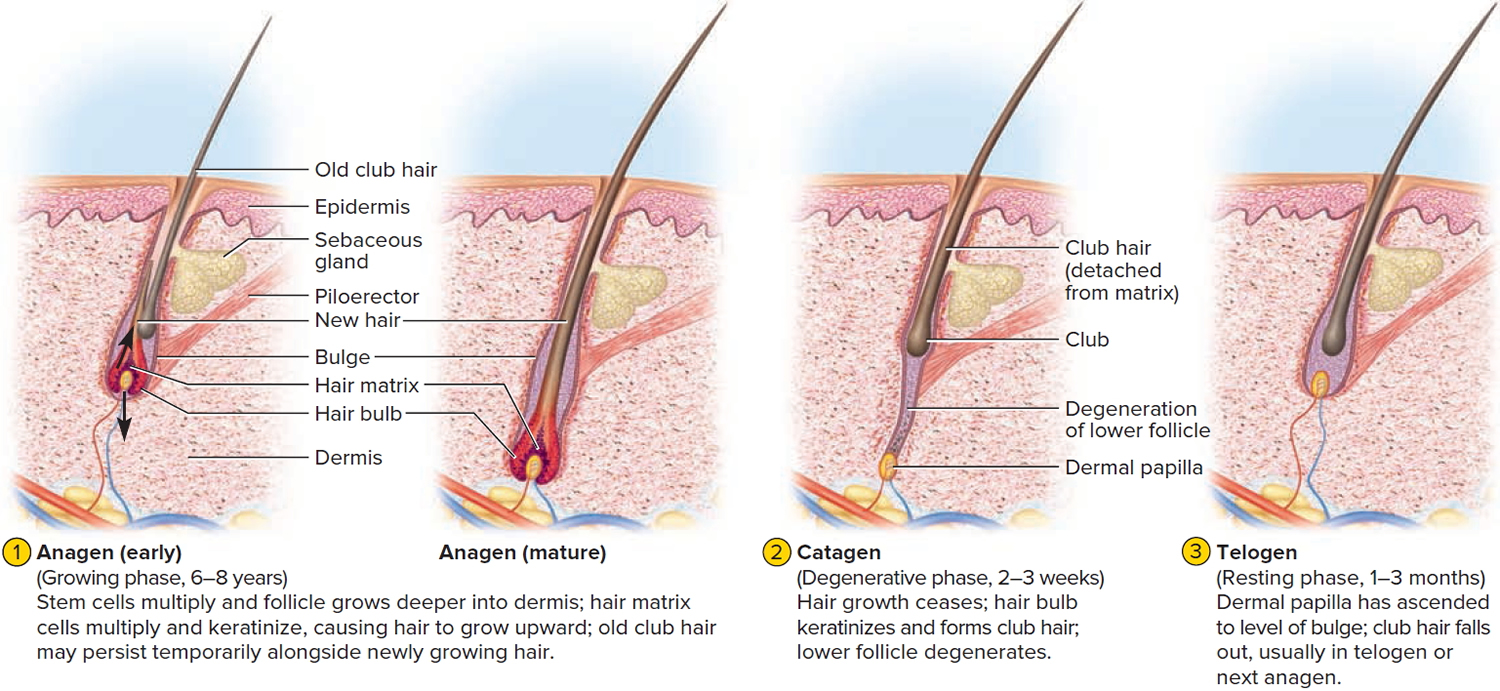
The human scalp contains about 100,000 hair follicles. These anchor the hair to the skin and contain the cells that produce new hairs. A hair in the scalp grows for two to five years, at a rate of around 0.33 mm/day (about 1/64 inch). Variations in hair growth rate and the duration of the hair growth cycle account for individual differences in uncut hair length. Hair grows in 3 developmental stages (see Figure 5):
- Anagen. The anagen or follicle growing phase starts growing the new hair. This phase is genetically determined and can vary from 2 to 6 years (the average is just under 3 years). Most hair follicles on the scalp are in the anagen phase.
- Catagen. The catagen phase is a transition stage between the growing and resting phases and lasts 1-2 weeks.
- Telogen. The telogen or resting phase is a mature hair with a root, which is held very loosely in the follicle. The telogen phase generally lasts about 4-5 months. About 100 telogen hairs are lost from the human scalp each day.
Figure 5. Hair growth cycle
At any given time, about 90% of the scalp follicles are in the Anagen stage. In this stage, stem cells from the bulge in the hair follicle multiply and travel downward, pushing the dermal papilla deeper into the skin and forming the epithelial root sheath. Root sheath cells directly above the papilla form the hair matrix. Here, sheath cells transform into hair cells, which synthesize keratin and then die as they are pushed upward away from the papilla. The new hair grows up the follicle, often alongside an old club hair left from the previous cycle.
In the Catagen stage, mitosis in the hair matrix ceases and sheath cells below the bulge die. The follicle shrinks and the dermal papilla draws up toward the bulge. The base of the hair keratinizes into a hard club and the hair, now known as a club hair, loses its anchorage. Club hairs are easily pulled out by brushing the hair, and the hard club can be felt at the hair’s end. When the papilla reaches the bulge, the hair goes into a resting period called the Telogen stage. Eventually, anagen begins anew and the cycle repeats itself. A club hair may fall out during catagen or telogen, or as it is pushed out by the new hair in the next anagen phase.
You lose about 50 to 100 scalp hairs daily. In a young adult, scalp follicles typically spend 6 to 8 years in anagen, 2 to 3 weeks in catagen, and 1 to 3 months in telogen. Scalp hairs grow at a rate of about 1 mm per 3 days (10–18 cm/yr) in the anagen phase.
Hair grows fastest from adolescence until the 40s. After that, an increasing percentage of follicles are in the catagen and telogen phases rather than the growing anagen phase. Hair follicles also shrink and begin producing wispy vellus hairs instead of thicker terminal hairs. Thinning of the hair or baldness, is called alopecia. It occurs to some degree in both sexes and may be worsened by disease, poor nutrition, fever, emotional stress, radiation, or chemotherapy. In the great majority of cases, however, it is simply a matter of aging.
Pattern baldness is the condition in which hair is lost unevenly across the scalp rather than thinning uniformly. It results from a combination of genetic and hormonal influences. The relevant gene has two alleles: one for uniform hair growth and a baldness allele for patchy hair growth. The baldness allele is dominant in males and is expressed only in the presence of the high level of testosterone characteristic of men. In men who are either heterozygous or homozygous for the baldness allele, testosterone causes terminal hair to be replaced by vellus hair, beginning on top of the head and later the sides. In women, the baldness allele is recessive. Homozygous dominant and heterozygous women show normal hair distribution; only homozygous recessive women are at risk of pattern baldness. Even then, they exhibit the trait only if their testosterone levels are abnormally high for a woman (for example, because of a tumor of the adrenal gland, a woman’s principal source of testosterone). Such characteristics in which an allele is dominant in one sex and recessive in the other are called sex-influenced traits.
Excessive or undesirable hairiness in areas that are not usually hairy, especially in women and children, is called hirsutism. It tends to run in families and usually results from either masculinizing ovarian tumors or hypersecretion of testosterone by the adrenal cortex. It is often associated with menopause.
Contrary to popular misconceptions, hair and nails do not continue to grow after a person dies, cutting hair does not make it grow faster or thicker, and emotional stress cannot make the hair turn white overnight.
Different causes of hair loss affect the hair follicles in different phases of growth. See below for the different types of hair loss.
Types of Hair loss (Alopecia)
There are different types of alopecia. Listed below are the main types of hair loss:
Androgenetic Alopecia
Also known as “male pattern baldness” or “female pattern baldness.” It is a thinning of the hair to an almost transparent state, in both men or women. It is thought to be a hereditary form of hair loss and is the most common type of progressive hair loss.
It is the most common type of hair loss affecting approximately 50% of men over the age of 50 and around 50% of women over the age of 65. Androgenetic Alopecia can also affect younger men and women. It is caused by a number of genetic and hormonal factors. Dihydrotestosterone (DHT) is the main hormone responsible for Androgenetic Alopecia in genetically susceptible individuals. Dihydrotestosterone (DHT) causes hair loss by inducing a change in the hair follicles. The hairs produced by the follicles affected by dihydrotestosterone (DHT) become progressively smaller until eventually the follicles shrink completely and stop producing hair entirely.
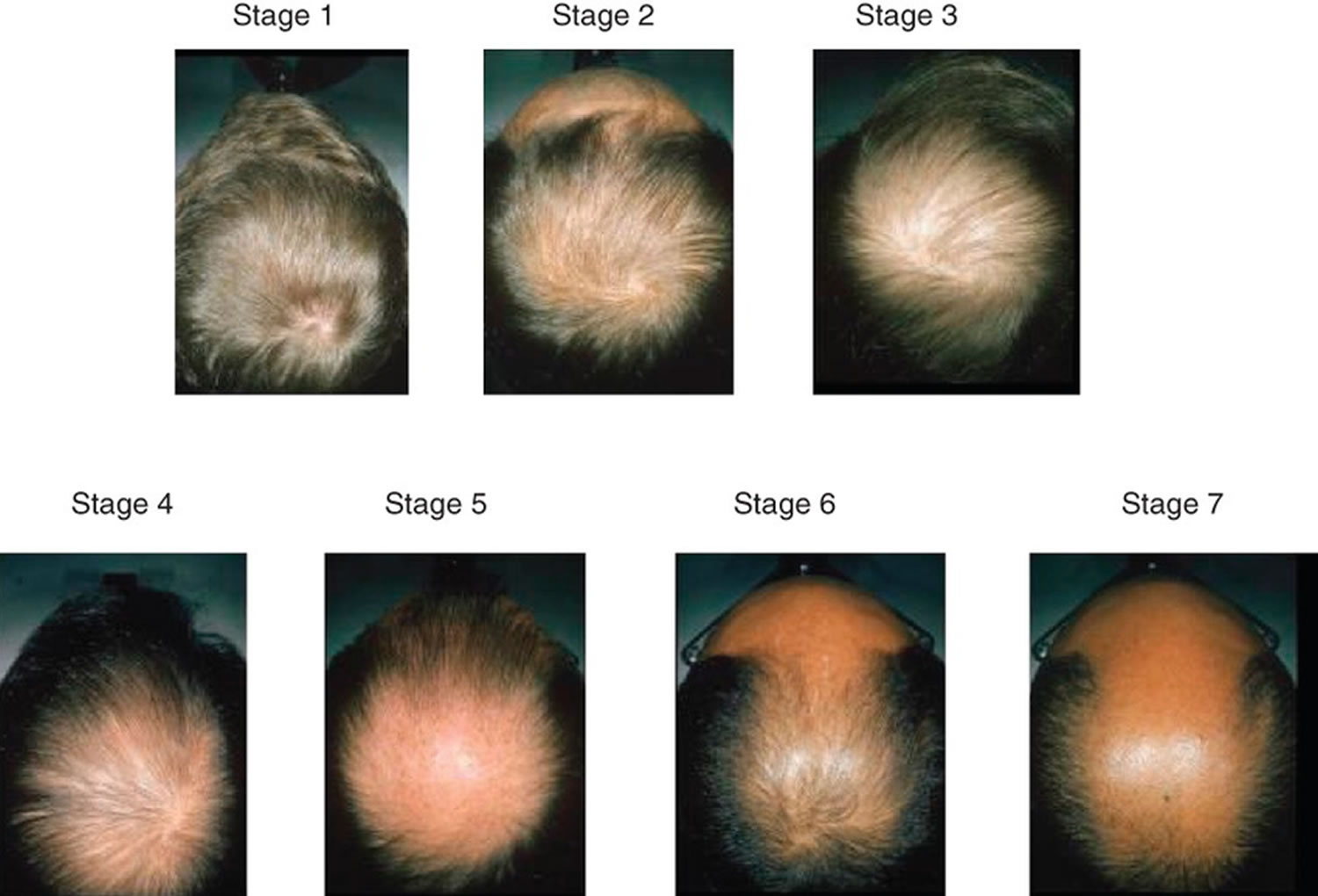
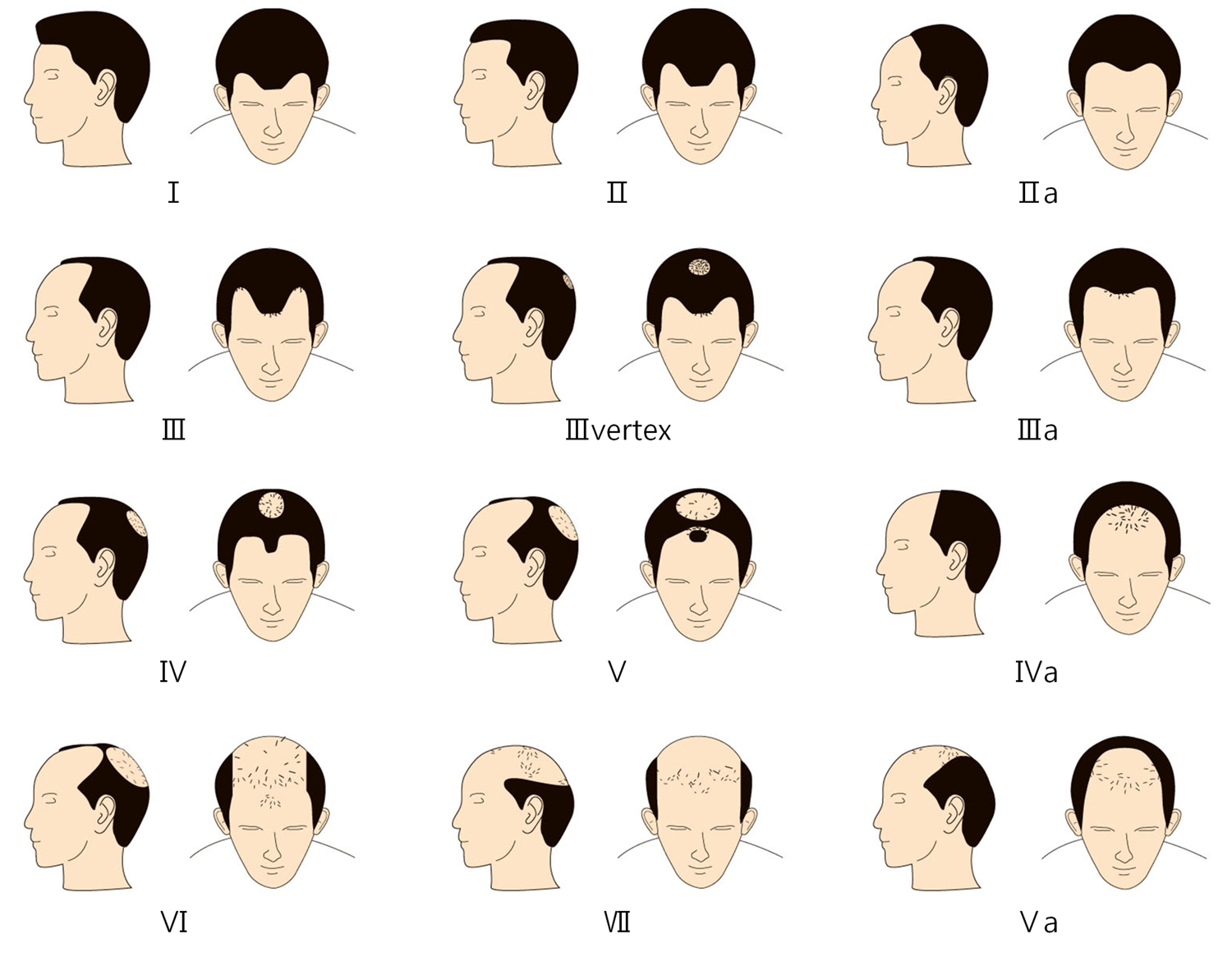
What does Androgenetic Alopecia look like?
Androgenetic Alopecia tends to look different between males and females. In men, the typical pattern of hair loss is a receding hair line with loss of hair from the top and front of the head. In women, the usual pattern of hair loss is thinning at the crown of the head. Often in women the frontal hairline remains. There are of course exceptions to these patterns but these are typically how Androgenetic Alopecia presents itself in men and women. It is less likely that a woman will experience total baldness as a result of Androgenetic Alopecia.
Figure 6. Androgenetic Alopecia
Figure 7. Androgenetic Alopecia Norwood Classification
Is Androgenetic Alopecia permanent?
The hair follicles affected by Androgenetic Alopecia are permanently damaged and any hair loss as a result is irreversible.
Can Androgenetic Alopecia be treated?
As with other types of alopecia, there is no cure for Androgenetic Alopecia. However, the effects of Androgenetic Alopecia may be slowed down with treatments. Minoxidil is licensed to treat both male and female pattern baldness.
Is Androgenetic Alopecia hereditary?
Yes, it is understood that genetic susceptibility is inherited from either or both parents.
Alopecia Areata
Alopecia areata causes patches of baldness about the size of a large coin. It can result in a single bald patch or extensive patchy hair loss. They usually appear on the scalp but can occur anywhere on the body.
It is not unusual for people with alopecia areata to notice some scalp discomfort. Symptoms may include soreness, itching and tingling sensations, with many describing a sensation similar to that of a very tight ponytail. In cases of alopecia areata, hair loss is caused by inflammation around the hair roots. There are a lot of nerves around the hair follicles so it is not surprising that the inflammation can cause discomfort.
Men and women are equally affected, and, although it can occur at any age, the most common presentation is in children and young adults, with 30 to 48 percent of patients affected before 20 years of age 2. It affects 1 or 2 people in every 1,000 in the US.
The lifetime risk of developing alopecia areata is 1.7 percent, with a prevalence of 0.1 percent 2. There is a genetic predisposition to alopecia areata with a polygenic pattern of inheritance. It’s also believed some people’s genes make them more susceptible to alopecia areata, as 1 in 5 people with the condition have a family history of the condition.
In most studies, 20 to 42 percent of those affected have a family history of the disease 3. Skin biopsy from areas of alopecia may show multiple lymphocytes, which supports the theory for an autoimmune cause.
Alopecia areata is understood to be an autoimmune condition. The immune system which normally protects your body from foreign invaders, such as viruses and bacteria, mistakenly attacks your hair follicles. This is what leads to hair loss. Alopecia Areata typically starts as one or more small, smooth bald patches on the scalp. The hair loss can remain as patchy hair loss or can continue until all hair on the scalp is lost (Alopecia Totalis) or complete loss of hair from the body (Alopecia Universalis). In case series, alopecia totalis and universalis are less common than alopecia areata and account for 4.5 to 30 percent of all alopecia cases. Note that most cases of Alopecia Areata do not develop to the ‘totalis’ or ‘universalis’ stage. Alopecia Barbae is a type of Alopecia Areata which affects facial hair only.
Alopecia areata is more common among people with autoimmune conditions, such as vitiligo, diabetes, an overactive thyroid (hyperthyroidism), rheumatoid arthritis, discoid lupus erythematosus or Down’s syndrome. Patients with a history of atopy are also at an increased risk of developing alopecia.
In most cases of alopecia areata, hair will grow back in a few months. At first, hair may grow back fine and white, but over time it should thicken and regain its normal color.
Figure 8. Alopecia areata
The patient with alopecia areata (Figure 8) typically presents with bald patches on the scalp that often have developed rapidly with sudden loss of hair. In diffuse alopecia, there is more widespread hair loss, often associated with graying of the hair. The classic finding is a smooth, hairless patch surrounded by so-called exclamation point hairs. These are 2- to 3-mm broken hairs that have a club-shaped root with a thinner proximal shaft and a normal caliber distal shaft on microscopic examination.
Some people go on to develop a more severe form of hair loss, such as:
- Alopecia totalis (no scalp hair)
- Alopecia universalis (no hair on the scalp and body).
Is Alopecia Areata permanent?
Alopecia Areata does not cause permanent hair loss. The hair follicles are not destroyed and hair does have the possibility to re-grow. This means that hair can regrow anywhere, even after several years. It doesn’t mean it will happen but the possibility is there. It’s not possible to predict if people will experience full regrowth. Many people with Alopecia Areata do experience full regrowth. However once the condition has developed to Alopecia Totalis or Alopecia Universalis, the chances of full regrowth become smaller. It is quite common for people with Alopecia Areata to experience hair loss on and off throughout their life.
In most cases of regrowth in alopecia areata, the hair regrows the same color as it was before. In some people the regrowing hair is initially lighter in color but then recovers its normal pigmentation. Occasionally, however, the regrowing hair remains white permanently. Some scientists have suggested that alopecia areata specifically affects pigment cells (melanocytes) in the hair root and this may be true in some cases. More commonly it affects the ability of hair cells to take up pigment from melanocytes. Very occasionally the regrowing hair is darker than normal. Regardless, a change in color of any regrowth is nothing to be concerned about.
Can Alopecia Areata be treated?
Treatments may be offered by a Dermatologist but unfortunately none are guaranteed to work. Many people experience spontaneous regrowth without treatment.
Treatments are more likely to be effective in milder cases of alopecia areata with small patches of hair loss. No treatments are universally effective.
Treatment may induce hair growth, but usually does not change the course of the disease. When treatment is stopped, hair loss recurs. Many patients with one or two small patches can be managed without treatment and with reassurance of the benign nature of the condition. A systematic review of 17 randomized controlled trials of topical and oral steroids, topical minoxidil (Rogaine), topical cyclosporine, and photo-dynamic therapy found no long-term benefit of these interventions 4. In patients with persistent hair loss and less than 50 percent scalp involvement, intralesional corticosteroid therapy is the first-line treatment.6 Patients with more than 50 percent hair loss can be treated with topical immunotherapy using diphenyl-cyclopropenone or squaric acid 4. Overall, 34 to 50 percent of patients with alopecia areata will recover within one year; this number is as high as 80 percent in patients with one or two patches 5. The more severe the disease at onset, the worse the prognosis, with fewer than 10 percent of patients recovering from alopecia totalis and alopecia universalis 6.
Is there a cure for Alopecia Areata?
No, currently there is no cure for alopecia areata.
Is Alopecia Areata hereditiary?
It is understood that genetics plays a role in alopecia areata. Around 20% of people with alopecia areata will have a family member with the condition.
Those with alopecia areata are more likely to have family members with other autoimmune or atopic conditions, such as asthma, eczema, hay fever, rheumatoid arthritis, lupus, psoriasis, thyroid disease and vitiligo.
Alopecia Totalis
Alopecia totalis is a more advanced form of alopecia areata which results in total loss of all hair on the scalp.
Alopecia Universalis
Alopecia universalis is the most advanced form of alopecia areata which results in total loss of all hair on the body, including eyelashes and eyebrows.
Alopecia Barbae
Alopecia barbae is alopecia areata that is localized to the beard area. It can be a single bald patch or more extensive hair loss across the whole of the beard area.
Scarring Alopecias (Cicatricial Alopecias)
Scarring alopecias, also known as cicatricial alopecias, refers to a group of rare disorders that destroy hair follicles, which cause permanent hair loss.
In this type of alopecia, the hair follicle (the small hole in your skin that an individual hair grows out of) is completely destroyed. This means your hair won’t grow back.
The hair follicles are replaced with scar tissue (hence the name). In some cases the hair loss is without symptoms and can go unnoticed for long periods. In other cases the hair loss is accompanied by burning, itching and pain and is more progressive. It occurs in men and women of all ages but it less common in children. Frontal Fibrosing Alopecia and Lichen Planopilaris are two of the more well known Scarring Alopecias.
Depending on the condition, the skin where the hair has fallen out is likely to be affected in some way.
Conditions that can cause scarring alopecia include:
- scleroderma – a condition affecting the body’s connective (supporting) tissues, resulting in hard, puffy and itchy skin
- lichen planus – an itchy rash affecting many areas of the body
- discoid lupus – a mild form of lupus affecting the skin, causing scaly marks and hair loss
- folliculitis decalvans – a rare form of alopecia that most commonly affects men, causing baldness and scarring of the affected areas
- frontal fibrosing alopecia – a type of alopecia that affects post-menopausal women where the hair follicles are damaged, and the hair falls out and is unable to grow back
Scarring alopecia occurs in both males and females, but is less common in children than adults. It accounts for about 7% of hair loss cases.
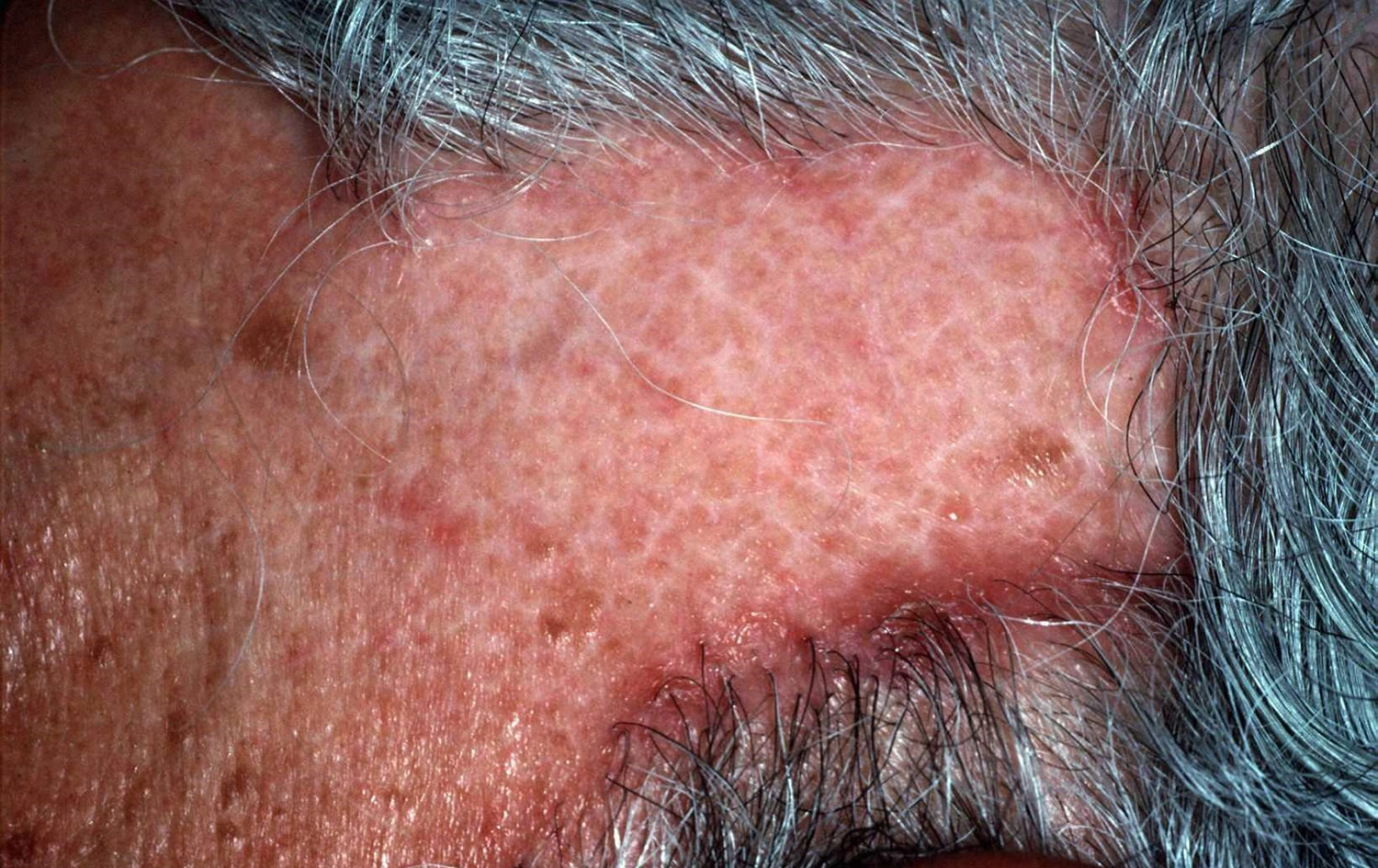
What do Scarring Alopecias look like?
Despite the name, there is usually no scar on the scalp as the inflammation that destroys the hair follicle occurs below the skin surface.
Figure 8. Scarring Alopecia
Are Scarring Alopecias permanent?
Unfortunately once hair loss has occurred in cases of Scarring Alopecias, the damage is permanent. The cause of Scarring Alopecias is not well understood. What is known is that the inflammation occurs in the upper part of the hair follicle. This is where the stem cells and sebaceous glands are located. If the stem cells and sebaceous glands are destroyed, the hair follicle cannot regrow and hair loss is permanent.
Can Scarring Alopecias be treated?
Yes, treatments are available for the different kinds of Scarring Alopecias. Some Scarring Alopecias are more treatable than others and an early diagnosis from a Dermatologist will provide the best chance of success.
Infections
Fungal infections (e.g. ringworm, also known as tinea capitis when it affects the scalp) can cause patchy hair loss. This is more common in young children and rarely affects adults.
The scalp is also usually scaly or crusty as a result of the fungal infection.
Hair usually grows back once the fungal infection has been treated with antifungal medicines.
Traction Alopecia
Traction alopecia is usually due to excessive pulling or tension on hair shafts as a result of certain hair styles. Traction alopecia is a form of unintentional hair loss associated with specific social, cultural, and cosmetic practices. It is seen more often in women, particularly those of East Indian and Afro-Caribbean origin. Hair loss depends on the way the hair is being pulled. Prolonged traction alopecia can stop new hair follicles developing and lead to permanent hair loss.
Patients (primarily women) wearing wigs, tight braids, or using curling rollers are at risk. Hair processing including bleaching, coloring, and waving also puts patients at risk. Hair loss usually occurs in the frontotemporal area, although it can vary. Eliminating the stressor or source of traction on the hair commonly cures the problem and returns hair growth to normal. Several small case reports have shown topical minoxidil 2% to be beneficial for treatment 7. In rare circumstances, chronic traction can set in motion a process of folliculitis and subsequent scarring that can result in permanent hair loss to the affected area.
Trichotillomania
Trichotillomania is a condition of compulsive hair picking or pulling that can lead to patches of near complete hair loss. The areas most often affected are the front and side of the scalp.
In children, trichotillomania is usually just a habit and parents can help stop their child from hair pulling and plucking. In adults (and some children) the condition may be related to other psychological issues, and seeing a psychologist or psychiatrist may be recommended.
Telogen Effluvium
A form of hair loss where more than normal amounts of hair fall out. There is a widespread ‘thinning’ of the hair, rather than specific bald patches. Your hair may feel thinner, but you’re unlikely to lose it all and your other body hair isn’t usually affected. Unlike some other hair and scalp conditions, telogen effluvium is temporary and the hair growth usually recovers.
Normally 10% of a person’s hair is in the telogen phase (see 3 hair developmental stages in Figure 5 above). Telogen effluvium occurs when there is a higher than average amount of hair shedding, 30% of more. Common triggers for this change in the usual telogen stage include psychological stress, childbirth, trauma, severe illness, injury, infection, surgery, crash diets, bereavement, sudden weight loss, new medication, hormonal changes, thyroid disorders, iron deficiency or anemia. In around a third of those affected, no cause can be found.
Hyperthyroidism and hypothyroidism can cause telogen effluvium, which is usually reversible when the thyroid status is corrected (except in long-standing hypothyroidism). Severe iron deficiency anemia may be associated with it, but this remains controversial. Drugs that cause telogen effluvium include antithyroid agents, hormones, anticonvulsants, anticoagulants, beta blockers, angiotensin-converting enzyme inhibitors, and lithium. No cause is found in approximately one third of cases 8.
Telogen effluvium can be caused by your body reacting to:
- hormonal changes, such as those that take place when a woman is pregnant
- intense emotional stress
- intense physical stress, such as childbirth
- a short-term illness, such as a severe infection or an operation
- a long-term illness, such as cancer or liver disease
- changes in your diet, such as crash dieting
- some medications, such as anticoagulants (medicines that reduce the ability of your blood to clot) or beta-blockers (used to treat a number of conditions, such as high blood pressure)
In most cases, your hair will stop falling out and start to grow back within 6 months.
What does Telogen Effluvium look like?
Hair loss occurs all over the scalp, resulting in a reduced volume of hair.
People with telogen effluvium usually present with an increased number of hairs in their hairbrush or shower, and sometimes thinning of the hair in the scalp, axillary, and pubic areas. A detailed history may indicate the cause of the hair loss, which usually has occurred two or three months before the hair falls out. On examination, there is generalized hair loss with a positive hair pull test, indicating active hair shedding, particularly at the vertex and scalp margin. The hair pull test is done by grasping approximately 40 to 60 hairs between the thumb and fore-finger and applying steady traction (slightly stretching the scalp) as you slide your fingers along the length of the hair. Generally, only a few hairs in the telogen phase can be plucked in this fashion. Less than 10 percent is considered normal, whereas greater than this is considered indicative of a pathologic process 9. Treatment of telogen effluvium primarily involves removal of the underlying stressors or correction of any precipitating medical conditions.
Figure 9. Telogen Effluvium
Is Telogen Effluvium permanent?
Telogen Effluvium usually resolves itself completely, as the normal length of the telogen phase is around 3 to 6 months after which period the hair begins to grow again (anagen phase). How long it takes for hair volume to return to normal will vary according to the length of hair.
Can Telogen Effluvium be treated?
There is normally no treatment required for Telogen Effluvium as the hair will start growing once the trigger is removed. Medication is not required. Telogen Efflvium can return if the underlying cause is not treated or if it recurs.
Anagen Effluvium
Anagen Effluvium refers to widespread hair loss that can affect your scalp, face and body, that arises during the anagen (growth) stage of the hair cycle. One of the most common causes of this type of hair loss is the cancer treatment chemotherapy. In some cases, other cancer treatments – including immunotherapy and radiotherapy – may also cause hair loss. But not all chemotherapy drugs cause hair loss, and sometimes the hair loss is so small it’s hardly noticeable. It may be possible to reduce hair loss from chemotherapy by wearing a special cap that keeps the scalp cool, but this isn’t always effective or widely available.
The hair loss is usually noticeable within a few weeks of starting treatment. Initially it causes patchy hair loss, which often then becomes total hair loss. The good news is that in most cases, hair loss in anagen effluvium is temporary. Your hair should start to grow back a few months (usually about 6 months later) after chemotherapy has stopped.
Other drugs also can cause hair loss. Many medicines used to treat even common diseases can cause hair loss. Anagen Effluvium can also be due to infection and toxins.
What does Anagen Effluvium look like?
Sudden shedding of much of or all of the hair on the scalp and often from the entire body, including eyebrows, eyelashes and body hair.
Figure 10. Anagen Effluvium
Is Anagen Effluvium permanent?
In most cases the hair will eventually return once the underlying cause is treated/removed. Anagen Effluvium as a result of chemotherapy treatment will normally recover within 3-6 months of the treatment being stopped.
Causes of hair loss
The causes of hair loss can be broadly divided into focal or diffuse hair loss (Table 1). Focal hair loss is secondary to an underlying disorder that may cause nonscarring or scarring alopecia. Nonscarring focal alopecia is usually caused by tinea capitis or alopecia areata, although patchy hair loss may also be caused by traction alopecia or trichotillomania. Scarring alopecia is rare and has a number of causes, usually discoid lupus erythematosus. Diffuse hair loss can be further categorized into conditions that cause hair shedding, of which the most common is telogen effluvium, and predominant hair thinning caused by male or female pattern hair loss (previously called androgenetic alopecia).
Table 1. Causes of Hair loss (Alopecia)
| Type of alopecia | Distinguishing characteristics | |
|---|---|---|
Diffuse | ||
Female pattern hair loss | Presents with hair thinning; frontal hairline intact; negative pull test away from hair loss | |
Male pattern hair loss | Presents with hair thinning; M pattern; negative pull test away from hair loss | |
Diffuse alopecia areata | Distribution more patchy; positive pull test | |
Alopecia totalis or universalis | Total hair loss on the scalp and/or body | |
Telogen effluvium | 30 to 50 percent of hair loss three months after precipitating event; positive pull test | |
Anagen effluvium | Sudden hair loss of up to 90 percent two weeks following chemotherapy | |
Focal | ||
Nonscarring | ||
Alopecia areata | Normal scalp with surrounding exclamation point hairs | |
Tinea capitis | Scaly scalp with fungus visible on potassium hydroxide examination | |
Traction alopecia | Patchy; related to hair practices; may have some scarring | |
Trichotillomania | Patchy; may be some scarring and associated psychological disturbance | |
Scarring (cicatricial) | Scarring and atrophy of scalp (e.g., discoid lupus erythematosus) | |
Note: Listed in order of clinical importance.
Hair shaft abnormalities
Hair shaft defects can be inherited and congenital, or acquired due to disease or injury (eg excessive brushing, hair pulling [trichotillomania], hair dryer heat, relaxing chemicals, bleach). African hair practices.
Hair shaft abnormalities are diagnosed by dermatoscopy or microscopic examination of the hair, and sometimes by scanning electron microscopy. They include:
- Fractures: trichorrhexis nodosa, trichoschisis, trichoclasis (trichothiodystrophy)
- Irregularities: trichorrhexis invaginata (seen with ichthyosis in Netherton syndrome), Marie-Unna hypotrichosis (uncombable hair), pili bifurcati, pili annulati, pseudopili annulati, monilethrix (beaded hair), pseudomonilethrix
- Coiling and twisting: pili torti (twisted hair), woolly hair, trichonodosis (knotted hair)
Dermatological disease
Conditions resulting in reversible patchy hair thinning, poor hair quality and bald patches include:
- Localised alopecia areata
- Localised infection, such as tinea capitis
- Severe local skin disease, such as psoriasis, seborrhoeic dermatitis, atopic dermatitis, pityriasis rubra pilaris, cutaneous lupus erythematosus, cutaneous T-cell lymphoma
- Generalised skin disease (erythroderma)
Systemic disease
Systemic diseases resulting in reversible patchy hair thinning, poor hair quality and bald patches include:
- Iron deficiency
- Thyroid hormone deficiency
- Systemic lupus erythematosus
- Syphilis
- Severe acute or chronic illness
Destructive inflammatory skin diseases
Inflammation in the dermis or subcutaneous tissue may injure the hair follicle resulting in localised bald patches in which there are no visible follicles; this is called scarring alopecia or cicatricial alopecia.
Traumatic causes of scarring alopecia may be due to:
- Injury
- Surgery
- Radiation
- Traction (tight curls)
- Central centrifugal cicatricial alopecia
Infections causing scarring alopecia include:
- Bacterial infection: boils and abscesses (Staphylococcus aureus)
- Fungal infection: kerion (inflammatory tinea capitis)
- Viral infection: shingles (herpes zoster)
Inflammatory skin diseases causing scarring alopecia include:
- Folliculitis decalvans
- Dissecting cellulitis
- Lichen planopilaris
- Frontal fibrosing alopecia
- Alopecia mucinosa
- Discoid lupus erythematosus
- Localised scleroderma
Pseudopelade of Brocq is a condition in which there are localised areas of the scalp in which hair follicles have disappeared without visible inflammation.
Zinc and copper
Even though zinc and copper are theoretically considered to play certain roles in the pathogenesis of hair loss, clinical research has shown opposing views on the relationship. Oral zinc compounds have been used for decades for treating disorders such as telogen effluvium 11 and alopecia areata 12. Reports have also been published on oral zinc sulfate therapy with encouraging results for some cases of alopecia areata. In 1976 Wolowa and Jablonska 13 reported that two patients with alopecia areata regrew their hair after treatment with oral zinc sulfate. It has been reported that some alopecia areata patients have zinc deficiency 14. Zinc is an essential cofactor for multiple enzymes and it is involved with important functional activities in the hair follicle. Furthermore, zinc is a potent inhibitor of hair follicle regression and it accelerates hair follicle recovery 14. More specifically, transient zinc deficiency is a major pathogenesis in acrodermatitis enteropathica, resulting in hair loss 15. Arguments that zinc deficiency can be a disturbing factor for the growth of hair have been emerging since the 1990s 16. There is also a contradicting argument that there exists no relationship between zinc and hair loss 17. Even though a few studies have reported that zinc deficiency has correlations with alopecia areata and telogen effluvium, no studies have mentioned the relation between zinc and androgenic alopecia so far 11. In a recent study 18, alopecia areata patients whose serum zinc was lower than 70 µg/dl were administered zinc gluconate 50 mg every day for 12 weeks. The findings showed that the serum zinc concentration was elevated by 27.6 µg/dl on average, and 60% of the patients administered zinc showed a clinically therapeutic effect, suggest that zinc supplementation could become an adjuvant therapy for the alopecia areata patients with a low serum zinc level and for whom the traditional therapeutic methods have been unsuccessful. Another study examined the blood and urine samples of children with alopecia, and found that the zinc concentrations in blood and urine were lower than in the normal group12. However, another study found that even though there was a difference in serum zinc and copper concentrations between hair loss patients and normal individuals, there was no statistical significance. A similar study also found that there was no difference in zinc and copper, but the concentration of serum magnesium was quite higher 19. Although it is likely that there is a close theoretical relationship between serum copper and hair loss, as with zinc, more studies have shown contradictory results. In a study conducted on Koreans consisting of a control group of 10 normal people and a group of 30 alopecia areata patients, the serum zinc concentration was significantly low in the patients group, but the serum copper concentration was a little higher in the patients group without any statistical significance 20. In a study conducted in Indonesia that measured serum zinc, copper, and magnesium for 50 alopecia areata patients and 50 people in a normal control group, copper and magnesium levels did not show any significant differences, in contrast to the zinc levels 16. However, there was a study that indicated the serum copper concentration in alopecia universalis was lower in the patient group 19.
How is hair loss diagnosed?
A careful history and full skin examination can generally result in the correct diagnosis. Additional tests may include:
- Hair pull test to determine relative proportion of anagen and telogen hairs
- Wood lamp examination
- Swabs of pustules for bacterial and/or viral culture
- Skin scrapings and hair clippings for mycology
- Blood tests for haematology, thyroid function, serology
Hair loss in men
Male-pattern hair loss or baldness (sometimes referred to as male androgenetic alopecia) is the most common type of hair loss, affecting around half of all men by the age of 50 1.
It usually starts around the late 20s or early 30s and most men have some degree of hair loss by their late 30s.
It generally follows a pattern of a receding hairline, followed by thinning of the hair on the crown and temples, leaving a horseshoe shape around the back and sides of the head.
Sometimes it can progress to complete baldness, although this is uncommon.
Male-pattern baldness is hereditary, which means it runs in families. It’s thought to be caused by oversensitive hair follicles, linked to having too much of a certain male hormone.
Although it is not life threatening, it is associated with negative psychological effects, including low self-esteem, depression, and a general dissatisfaction with body appearance 21. Hair loss affects the androgen-sensitive follicles, starting with bitemporal recession, and then spreads to thinning of the vertex and frontal regions in a classic M pattern. Dihydrotestosterone (DHT), the androgen derived from testosterone, plays a key role in male pattern hair loss, and men with lower levels of dihydrotestosterone (DHT) have less hair loss 22.
Hair loss treatment for men
Topical minoxidil (2% and 5%) and oral finasteride are the only treatments approved by the FDA for treatment of male pattern hair loss in men older than 18 years. Treatment with finasteride can cause decreased libido, impotence, and ejaculation disorders 23. These adverse effects often abate with continued treatment and happen in less than 2 percent of men younger than 40 years 24. Finasteride may also induce depression 25. Minoxidil is available over-the-counter, and it should be applied to the scalp and not the hair. Its mechanism of action is unclear. Some shedding during the first few months of treatment is common. The minoxidil 5% solution has not been shown to be consistently more effective than the 2% solution, and patients using the higher concentration had more adverse effects, including allergic contact dermatitis, dryness, and itching 26. These typically resolve after treatment is discontinued 27.
Several small studies have shown some increased effectiveness with combined minoxidil and finasteride treatment 28, 29. Starting treatment early can help maximize success, and patients can expect to see results after three to six months, although dense regrowth is not likely. Discontinuation of finasteride or minoxidil results in loss of any positive effects on hair growth within 12 and six months, respectively 30. When switching between treatment with finasteride and minoxidil, it is best to overlap treatments for three months to minimize hair loss 31. Additional treatment options are listed in Table 2: Treatment of Hair Loss (Summary & Evidence) below.
Hair loss in women
As well as affecting men, hair loss can sometimes affect women (female-pattern baldness). It’s estimated, for instance, that around 50% of women over the age of 65 experience female-pattern baldness – the most common type of hair loss, which is thought to be inherited. However, it’s not clear if female-pattern baldness is hereditary and the causes are less well understood. Because there is a genetic basis to female pattern baldness, different racial populations are affected at different rates. Almost half of men, and perhaps as many women who are postmenopausal, are affected by hair loss to some degree. Onset of hair loss seems most common at either 20–30 or 40–50 years of age. The incidence is highest in Caucasians followed by Asians and African Americans, and the lowest incidence of hair loss is in Native Americans.
In female-pattern baldness, hair usually only thins on top of the head. It tends to be more noticeable in women who have been through the menopause (when a woman’s periods stop at around age 50-52), perhaps because they have fewer female hormones.
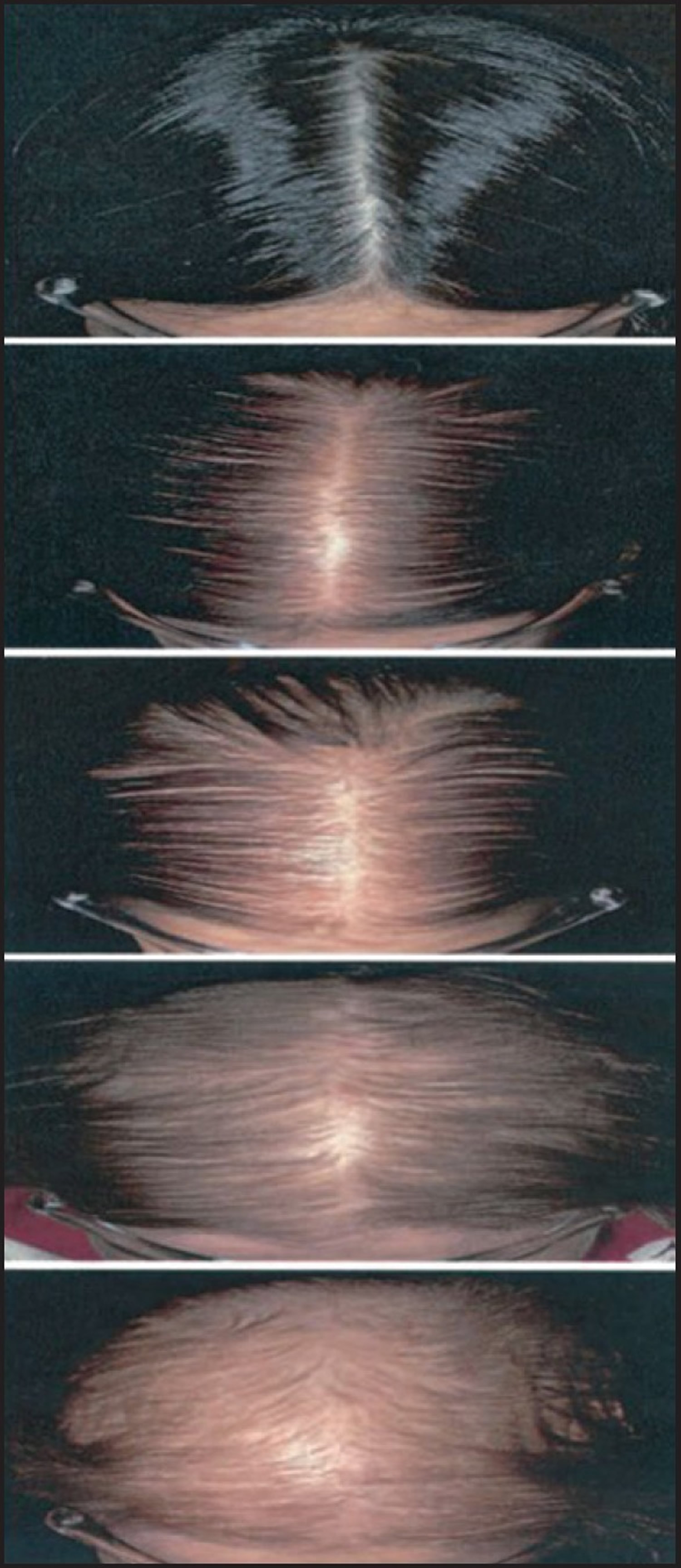
Up to 50 percent of women will experience female pattern hair loss during their lifetime 1. Women usually present with hair thinning over the central area of the scalp and widening of the midline part, but with reservation of the frontal hairline (Figure 11). Women who also have abnormal menses, history of infertility, hirsutism, unresponsive cystic acne, virilization, or galactorrhea should have a targeted endocrine work-up for hyperandrogenism (i.e., testosterone, dehydroepiandrosterone sulfate, and prolactin), although most will have normal androgen levels 32. Evaluation for iron deficiency, thyroid disease, and syphilis (a rare cause) should be considered because they can contribute to hair thinning or generalized hair loss.
Figure 11. Female pattern hair loss
Note: The pattern of hair loss is different in women than men; the hairline is preserved while there is diffuse thinning of the hair of the crown and frontal scalp. Total hair loss is very rare.
Figure 12. Sinclair’s self-reporting photographic measure of female pattern of hair loss
Hair loss treatment for women
Minoxidil 2% is the only treatment approved by the U.S. Food and Drug Administration (FDA) for treating female pattern hair loss in women older than 18 years. Topical minoxidil; the 2% preparation recommended for women is available over the counter. This may help hair to grow in a quarter of the women using it, and it will stop or slow hair loss in the majority of users. A hyperandrogenic state may limit the success of treatment with minoxidil 33 and, in these women, spironolactone (Aldactone) 100 to 200 mg daily may slow the rate of hair loss 34. Women with evidence of a hyperandrogenic state requesting combined oral contraceptives would benefit from using antiandrogenic progesterones, such as drospirenone 35. Finasteride (Propecia) is ineffective in postmenopausal women with female pattern hair loss 36. Finasteride, spironolactone, and cyproterone should not be used in women of childbearing potential.
Over-the-counter topical preparations, hair extensions, and hairpieces are available for women with poor response to treatment.
There is no known prevention for hair loss; shampooing and other hair products have no adverse effects other than harsh products or practices that may damage the hair shaft, causing breakage.
Surgical therapy to improve the appearance includes scalp reduction, flaps, and hair transplants (micrografting). Not everyone is a good candidate for these procedures.
Hair loss treatment
There is no cure for hair loss (alopecia) and no universally proven therapy to induce hair re-growth and sustain remission, however, there are treatments. The effectiveness of treatments tends to vary and something that works well for one person may not work well for another. If you find one treatment doesn’t work don’t assume others won’t either. However, bear in mind for some people none of the treatments are effective. Treatments for hair loss are generally divided into two groups:
- People with less than 50% hair loss
- People with over 50% hair loss
All of the therapies have documented side effects, some of which can be unpleasant. Treatments such as topical immunotherapy can be very time consuming. Individuals may decide that some of the adverse effects of treatment and the unpredictable outcome are unacceptable.
Table 2. Treatment of Hair Loss (Summary & Evidence)
| Treatment | Dosing | Strength of evidence | Comments |
|---|---|---|---|
Alopecia areata | |||
Topical steroids | Applied twice daily to scalp | B | Evidence for short-term growth, but none for long-term growth5 |
Topical minoxidil (Rogaine) | Applied twice daily | B | Evidence for short-term growth; one study showed more hair regrowth with 5% than 1% formulation 4, 4 |
Topical immunotherapy with diphenylcyclopropenone (DPCP) or squaric acid | Treatment applied by dermatologist every few weeks | B | Unlicensed treatment; may cause severe dermatitis 37 |
Oral steroids | Six-week tapering course of prednisone starting at 40 mg per day | B | Continued treatment is needed to maintain hair growth; risks of prolonged steroid use outweighs the benefits 5 |
Intralesional corticosteroids | Triamcinolone acetonide (Kenalog) 5 to 10 mg per mL; 0.1 mL injected with a 30-gauge needle into the dermis 1 cm apart to a maximum of 3 mL; can be repeated every four to six weeks | C | Hair regrowth lasts a few months; effect on long-term outcome is unknown 5 |
Anthralin cream (Dritho-Creme HP) | 0.5% to 1% cream once daily for 20 to 30 minutes, increasing by 10 to 15 minutes every two weeks | C | Hair staining prevents use in fair-haired patients 5 |
Female pattern hair loss | |||
Minoxidil 2% | Apply twice daily to dry scalp | B | 20 percent of women using the drug versus 7 percent of women taking a placebo reported moderate new hair growth after 32 weeks; number needed to treat = 8 38; 7 percent of women using minoxidil experience undesirable hypertrichosis 27 |
Spironolactone (Aldactone) | 100 to 200 mg orally daily | C | 88 percent of women had a modest decrease in hair loss with treatment 27 |
Flutamide (formerly Eulexin) | 250 mg orally daily | C | Treatment for one year resulted in a modest improvement in alopecia; 32 percent of participants experienced elevated liver function tests while taking the medication, resulting in some safety concerns 39 |
Male pattern hair loss | |||
Finasteride (Propecia) | 1 mg orally daily | A | Promotes hair growth for more than two years, with the effect waning by year three 23, 24 ; does not significantly affect sperm production and poses no risk to a female sex partner; when screening men on finasteride for prostate cancer, the upper limit of normal prostate specific antigen levels should be doubled to ensure appropriate interpretation 40, 41 |
Minoxidil (2%) | 1 mL to scalp twice daily | A | Consistent evidence showing moderate to dense regrowth of hair 26 |
Minoxidil (5%) | 1 mL to scalp twice daily | A | Consistent evidence showing moderate to dense regrowth of hair 26 |
Ketoconazole (2%) shampoo (Nizoral) | Daily | C | Increased hair density, size, and proportion of anagen follicles after shampooing two to four times per week for 21 weeks 42 |
Pyrithione zinc (1%) shampoo (Head and Shoulders) | Daily | C | Increased total visible hair count, but 5 percent less than treatment with minoxidil 5% 43 |
A = consistent, good-quality patient-oriented evidence; B = inconsistent or limited-quality patient-oriented evidence; C = consensus, disease-oriented evidence, usual practice, expert opinion, or case series.
[Source 10]Treatment for Less than 50% hair loss
Corticosteroids
Today, corticosteroids are the most common treatment for hair loss. In mild cases of hair loss the first choice of treatment would be a corticosteroid cream or lotion which is applied directly to the area(s) of hair loss. Alternatively an injection of corticosteroid can be given directly onto and around the bald area(s).
Side Effects: Side effects are generally rare when corticosteroids are used for a short time. However, when they are taken by mouth and when used ovr a longer period, they may lower the body’s ability to fight off infections or may make infections harder to treat. Other common side effects include changes in appetite (increase or decrease), nervousness, restlessness, sleep problems, and indigestion. These problems usually go away as the body adjusts to the drug and do not require medical treatment. Less common side effects may occur with some forms of corticosteroids. Gels or creams may irritate the skin. Again, these side effects do not need medical attention unless they don’t go away or they interfere with normal activities. More serious side effects are very unlikely, but they may occur.
Effectiveness: This type of treatment can sometimes result in a recovery or can cause hair to grow only for the period during which the treatment occurs, so when the treatment is stopped the hair may fall out again. In the case of corticosteroid injections an average of 4 to 6 monthly injections are usually required for significant improvement. However although some re-growth is common it does not always occur.
Finasteride
Finasteride is marketed under the brand name of Propecia along with other generic names. It is a licensed synthetic type II 5α-reductase inhibitor. The enzyme converts testosterone to dihydrotestosterone. Systemic Finasteride (1mg Propecia) can be used for the treatment of male pattern baldness. It is still in the experimental stages of use for female pattern baldness.
Side Effects: Side effects of finasteride can include impotence and reduced libido, abnormal ejaculation, decreased ejaculatory volume, abnormal sexual function, swelling and tenderness of the breast tissue and testicular pain.
Effectiveness: It has shown a significant improvement for men (80% of men presenting with male pattern baldness, with 60% of those showing some regrowth). The effects do not continue if the treatment is stopped. For women the results have been less successful (if not disappointing) and it must not be used for women likely to become pregnant.
Retin A / Tretinoin
Retin-A was originally used for the treatment of acne and other skin problems. However studies have shown that Retin-A, when used alone in the form of a gel, which is rubbed onto the area of hair loss, or in combination with topical Minoxidil can result in moderate to good hair growth in individuals with hair loss. It is recommended that Minoxidil is used in the morning and Retin-A in the evening as Retin-A increases the skin’s sensitivity to sunlight.
Side Effects: Immediately after applying, the skin may feel warm or mild stinging or redness may occur. Some peeling of the skin may occur. These effects should subside as your skin adjusts to the medication.
Effectiveness: Studies have shown that Retin-A, when used alone in the form of a gel, which is rubbed onto the area of hair loss, or in combination with topical Minoxidil can result in moderate to good hair growth in individuals with alopecia.
Diphenylcyclopropenone (DPCP)
Immunotherapy may be an effective form of treatment for extensive or total hair loss, but less than half of those treated will see worthwhile hair regrowth. Diphenylcyclopropenone (DPCP) is a chemical agent used to treat severe alopecia areata. It is said to be safe although there is no information about the long term side effects when used over many years. Diphenylcyclopropenone (DPCP) comes as a fluid and is applied to the bald areas once a week. Sensitizing is achieved with the application of a 2% solution and is applied to a 4x4cm area on the scalp. One week later the area is examined. If there is a severe response with blisters , intense redness , scaling and itching, treatment is postponed till the following week. If there is only mild redness , scaling and itching, a lower concentrate of diphenylcyclopropenone (DPCP) can be applied on the hairloss areas. After every administration of diphenylcyclopropenone (DPCP), the painted area should not be washed for 48 hours and kept covered because sunlight inhibits the action of diphenylcyclopropenone (DPCP). After DPCP has been applied, you’ll need to wear a hat or scarf over the treated area for 24 hours because light can interact with the chemical.
Side Effects: Eczema, Lymph node enlargement and skin discoloration (vitiligo) are all possible side effects. This can be avoided by increasing the DPCP concentration gradually.
Effectiveness: First evidence of hair growth is expected to occur after 3 months, full growth after 6 months. Once full regrowth occurs, the frequency of application is decreased. Even after full growth of hair, some patients may stop responding to further application of diphenylcyclopropenone (DPCP) and may lose all their hair again. If after 5 months of using diphenylcyclopropenone (DPCP) no hair regrowth is noticed DPCP is discontinued.
Dithranol (also known as Anthralin)
Similar to immunotherapy (DPCP), dithranol cream is applied regularly to the scalp before being washed off. It causes a skin reaction, followed by hair regrowth in some cases. Dithranol is a tar-like ointment that is applied to the scalp and is especially good in the treatment of psoriasis (a skin condition causing red scaly patches). The pharmacist can compound it in various different pastes, ointments, and creams, and the strength may vary from 0.1 to 4%.
Side Effects: It can irritate the skin when applied and can cause burning and redness. It can also stain.
Effectiveness: Dithranol can be effective even if only left on the skin for 10 minutes. This ‘short contact’ method allows stronger concentrations of Dithranol to be used with much less burning and staining. But it hasn’t been proven that dithranol cream is significantly effective in the long term. It can also cause itchiness and scaling of the skin and can stain the scalp and hair. For these reasons, dithranol isn’t widely used.
Topical Minoxidil (Regaine, Rogaine or Headway)
Topical Minoxidil can be successful in hair loss, slowing down hair loss, and bridging the gap until hair starts growing again on its own.
Minoxidil is not available on prescription. Minoxidil comes in a 2% and 5% solution. However the 2% and 5% solutions can be ordered online. A bottle will normally last for about a month. The solution should not be used by women during pregnancy.
A Minoxidil 5% foam is also available, and is shown to be just as effective as the 5% solution. The foam will last about a month.
Side Effects: Side effects may include irritation of the scalp, itching, scaling, a rash, and on the odd occasion excessive hair growth.
Effectiveness: Topical Minoxidil can be effective on patchy alopecia. Unfortunately topical Minoxidil is not normally effective in individuals with extensive, total or universal alopecia.
Zinc
Oral zinc has been shown to be of occasional benefit in alopecia.
Zinc can be bought in any chemist or health food shop. A variety of tablets are sold with different amounts of zinc.
Side Effects: Very high doses are needed for it to be effective and this can result in side effects such as vomiting and diarrhea.
Effectiveness: Prolonged treatment with zinc sulphate is helpful. There is no zinc deficiency noticeable in the body, and short term treatment with zinc is not helpful.
Treatment for Over 50% hair loss
Immunosuppressive drugs
It is thought that Immunosuppressive drugs should be able to suppress the immune system giving the hair a chance to re-grow. The main problem with taking immunosuppressive drugs is that it can lead to a lowered resistance to infection.
Side Effects: Increased chance of infection as the immune system is suppressed and may affect bone marrow, liver or kidneys.
PUVA
PUVA or photochemotherapy is a type of ultraviolet radiation treatment (phototherapy) that involves taking or applying a light sensitive drug and then undergoing a short exposure to UVA (long wave ultraviolet radiation).
PUVA is a combination treatment which consists of Psoralens (P) and then exposing the skin to UVA. It has been available in its present form since 1976.
Psoralens are compounds found in many plants which make the skin temporarily sensitive to UVA. The ancient Egyptians were the first to use psoralens for the treatment of skin diseases thousands of years ago. Medicine psoralens include methoxsalen (8-methoxypsoralen), 5-methoxypsoralen and trisoralen.
Treatment takes place over a three to six week period with sessions two to three times a week. The more recent the hair loss, the more likely it is that there will be a response to treatment.
Side Effects: The likelihood is your skin will burn, as if over tanned, but it’s hoped the body’s immune system gets so busy repairing skin tissue that it lets your hair begin to grow.
PUVA but can be very time consuming involving two or three treatments per week.
Effectiveness: It has not been shown to have a very high success rate (around 6-12%) – and it can be very painful. It is not considered to be an effective long-term treatment.
Systemic Corticosteroids
Oral corticosteroids (Prednisone) are used to try to partially suppress the immune system and allow hair to grow. Corticosteroids taken orally are sometimes prescribed for extensive hair loss or when the condition is rapidly spreading. Corticosteroids taken internally are much more powerful than local injections into the skin. May be used in conjunction with Minoxidil as the dose is being reduced.
Side Effects: The most common side effects reported with the short-term (days to weeks) use of oral corticosteroids include a bigger appetite, weight gain, upset stomach, headache, mood changes, and trouble sleeping. Some people may also have an increase in blood sugar and blood pressure. In general, all of these side effects go away after you stop taking corticosteroids. Side effects associated with long-term (months to years) oral corticosteroid include weakening of the immune system, elevations in cholesterol levels, and weight gain. These side effects also usually improve when you stop taking corticosteroids. Long-term use of corticosteroids may also cause brittle bones (osteoporosis), fat deposits on the face and back, thinning of the skin, and cataracts in the eyes. These side effects may improve but usually don’t go away completely after stopping the drug. In children, long-term use of oral corticosteroids may cause stunted growth.
Effectiveness: When taking oral corticosteroids you are likely to experience some re-growth. However unless your immune system kicks into `normal’ action and allows you to produce hair yourself, the re-growth you have experienced will cease and the hair will unfortunately fall out again after you cease the treatment.
PUVB
This treatment is similar to PUVA but using a different wavelength of light. It is generally used to treat skin conditions but is also used for people with severe hair loss (e.g. more than 90%). It involves standing in a cubicle of ultraviolet lights two to three times a week for an increasing amount of time.
PUVB is the combination of Psoralens and UVB (short wavelength ultraviolet radiation). This is rarely used, as the wavelength that activates the psoralens most effectively is in the UVA range.
Side Effects: Like PUVA you may have redness and burning of the skin, similar to spending too long in the sun.
Effectiveness: Although there is some documented evidence of success, in most cases this treatment does not appear to help with hair growth and the redness and burning can be quite painful. It may also increase your chance of getting skin cancer.
Hair loss surgery
Most men and women considering hair loss surgery have male-pattern or female-pattern baldness. But surgery is also sometimes suitable for a range of alopecia conditions.
Surgery for hair loss should only be considered after trying less invasive treatments.
The success of hair loss surgery depends on the skill of the surgeon, as complications can arise. It’s best to speak to your doctor for advice before seeking out a surgeon in the private sector.
The main types of hair loss surgery are explained below.
Hair transplantation
Modern hair transplant techniques involve follicular unit grafting. A follicular unit is the natural grouping of hairs with most hairs grouped as 2, 3, or 4 hairs in a close bunch. There will also be a small number of single hairs that grow on their own. When doctors do surgery they try to keep these natural groupings together and move them surgically by two main techniques. One method involves the removal of a strip of hair (about 1cm wide and 30 to 35cm long) bearing scalp from the back of the head where there’s plenty of hair, then stitching the area. The hair above the surgery site will disguise the stitches until they heal at which point you are left with a scar averaging 1mm in width. The strip of skin and hair is then dissected under microscopes to isolate the follicular units. The other method is called follicular unit extraction (FUE) and is a process of meticulously coring out each grouping with a tiny punch. Usually with this technique the back of the head needs to be shaved. When the scalp heals there are small dot scars that are left behind. Once the follicular unit grafts are prepared these are then inserted into a small incision made in the bald area. Doctors normally place 20-40 of these grafts in each square centimeter of bald scalp. The procedure is done as a day case under local anesthetic.
Stitches are not needed to attach the grafts because they are held in place by the clotting (thickening) action of the blood when the hairs are inserted.
Fine hairs are placed at the front of the scalp and thicker hairs towards the back in a process called grading. This helps achieve a more natural result.
The hair should settle and start to regrow within 6 months.
Hair transplants are carried out over a number of sessions. There should be a break of 9 to 12 months between procedures.
As with any type of surgery, there’s a risk of infection and bleeding, which can lead to hair loss and noticeable scarring.
In a completely bald area with one operation doctors can achieve about 30% of the original density so some patients may require 2 operations to achieve a thicker look. If hair loss is due to genetics then the result should be long lasting. In other situations, if hair is lost due to a medical condition such as Alopecia Areata, then transplantation cannot be guaranteed as the disease process can recur at any time. But for some patients even a temporary return to ‘normal’ hair is acceptable.
Scalp reduction
Scalp reduction involves removing pieces of bald scalp from the crown and the top of the head to move hairy parts of the scalp closer together.
This can be done by cutting out loose skin and stitching the scalp back together, or by tissue expansion.
Tissue expansion is where a balloon is placed underneath the scalp and inflated over several weeks to expand the skin in stages. The balloon is then removed and the excess skin is cut out.
Scalp reductions aren’t suitable for hair loss at the front of the scalp because it can cause scarring. There’s also the risk of infection in the area.
Scalp reduction isn’t usually used for male-pattern baldness, but it’s available to people with scarring alopecia. Surgery should only be carried out after any underlying conditions have cleared up.
Artificial hair
Artificial hair implantation is marketed as a treatment for male-pattern baldness. It involves implanting synthetic fibres into the scalp under local anaesthetic.
Artificial hair implantation carries serious risks of infection and scarring, but clinics may be reluctant to inform people of the possible complications to avoid losing potential clients.
Artificial hair implantation isn’t recommended by dermatologists because of the risk of complications, such as:
- infection
- scarring
- synthetic fibres falling out
People considering hair loss surgery should explore more established treatments, such as hair transplantation and scalp reduction, because the advantages and disadvantages of these techniques are better understood.
Cloning
The latest research into hair loss treatments is studying hair cell cloning.
The technique involves taking small amounts of a person’s remaining hair cells, multiplying them, and injecting them into bald areas.
Cloning is intended to treat both male- and female-pattern baldness. But the science behind the technique is new and more trials are needed before it can be fully assessed.
Tattooing
For many people, it’s possible to replicate hair with a tattoo. This is known as dermatography and generally produces good long-term results, although it’s usually expensive and can only be used to replicate very short hair.
This is usually carried out for eyebrows over a few hourly sessions, and can even be used as a treatment for scalp hair loss caused by male-pattern baldness.
Unproven treatments
There are many treatments suggested for hair loss which have not been shown to be effective. These include jojoba oil, lanolin, wheatgerm oil, nutritional supplements, scalp massage, laser and acupuncture. Again, speak to your doctor before opting for these or any other hair loss treatment options to avoid unwanted effects and spending time or money on a treatment that is unlikely to help.
- Price VH. Treatment of hair loss. N Engl J Med. 1999;341(13):964–973.[↩][↩][↩]
- Shellow WV, Edwards JE, Koo JY. Profile of alopecia areata: a questionnaire analysis of patient and family. Int J Dermatol. 1992;31(3):186–189.[↩][↩]
- McDonagh AJ, Messenger AG. The pathogenesis of alopecia areata. Dermatol Clin. 1996;14(4):661–670.[↩]
- Delamere FM, Sladden MM, Dobbins HM, Leonardi-Bee J. Interventions for alopecia areata. Cochrane Database Syst Rev. 2008;(2):CD004413.[↩][↩][↩][↩]
- MacDonald Hull SP, Wood ML, Hutchinson PE, Sladden M, Messenger AG, for the British Association of Dermatologists. Guidelines for the management of alopecia areata. Br J Dermatol. 2003;149(4):692–699.[↩][↩][↩][↩]
- Tosti A, Bellavista S, Iorizzo M. Alopecia areata: a long term follow-up study of 191 patients. J Am Acad Dermatol. 2006;55(3):438–441.[↩]
- Khumalo NP, Ngwanya RM. Traction alopecia: 2% topical minoxidil shows promise. Report of two cases. J Eur Acad Dermatol Venereol. 2007;21(3):433–434.[↩]
- Harrison S, Sinclair R. Telogen effluvium. Clin Exp Dermatol. 2002;27(5):389–395.[↩]
- Piérard GE, Piérard-Franchimont C, Marks R, Elsner P, for the EEMCO group (European Expert Group on Efficacy Measurement of Cosmetics and Other Topical Products). EEMCO guidance for the assessment of hair shedding and alopecia. Skin Pharmacol Physiol. 2004;17(2):98–110.[↩]
- Diagnosing and Treating Hair Loss. Am Fam Physician. 2009 Aug 15;80(4):356-362. https://www.aafp.org/afp/2009/0815/p356.html[↩][↩]
- Arnaud J, Beani JC, Favier AE, Amblard P. Zinc status in patients with telogen defluvium. Acta Derm Venereol. 1995;75:248–249. https://www.ncbi.nlm.nih.gov/pubmed/7653193[↩][↩]
- Camacho FM, Garcia-Hernandez MJ. Zinc aspartate, biotin, and clobetasol propionate in the treatment of alopecia areata in childhood. Pediatr Dermatol. 1999;16:336–338. https://www.ncbi.nlm.nih.gov/pubmed/10515774[↩]
- Wolowa F, Jablonska S. Zinc in the treatment of alopecia areata. In: Kobori T, Montagna W, Toda K, editors. Biology and disease of the hair. 2nd ed. Tokyo: University of Tokyo Press; 1976. pp. 305–308.[↩]
- Plonka PM, Handjiski B, Popik M, Michalczyk D, Paus R. Zinc as an ambivalent but potent modulator of murine hair growth in vivo-preliminary observations. Exp Dermatol. 2005;14:844–853. https://www.ncbi.nlm.nih.gov/pubmed/16232307[↩][↩]
- Cheshire H, Stather P, Vorster J. Acquired acrodermatitis enteropathica due to zinc deficiency in a patient with pre-existing Darier’s disease. J Dermatol Case Rep. 2009;3:41–43. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3157796/[↩]
- Bhat YJ, Manzoor S, Khan AR, Qayoom S. Trace element levels in alopecia areata. Indian J Dermatol Venereol Leprol. 2009;75:29–31. https://www.ncbi.nlm.nih.gov/pubmed/19172027[↩][↩]
- Rushton DH. Nutritional factors and hair loss. Clin Exp Dermatol. 2002;27:396–404. https://www.ncbi.nlm.nih.gov/pubmed/12190640[↩]
- Park H, Kim CW, Kim SS, Park CW. The Therapeutic Effect and the Changed Serum Zinc Level after Zinc Supplementation in Alopecia Areata Patients Who Had a Low Serum Zinc Level. Annals of Dermatology. 2009;21(2):142-146. doi:10.5021/ad.2009.21.2.142. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2861201/[↩]
- Mussalo-Rauhamaa H, Lakomaa EL, Kianto U, Lehto J. Element concentrations in serum, erythrocytes, hair and urine of alopecia patients. Acta Derm Venereol. 1986;66:103–109. https://www.ncbi.nlm.nih.gov/pubmed/2424231[↩][↩]
- Lee SY, Nam KS, Seo YW, Lee JS, Chung H. Analysis of serum zinc and copper levels in alopecia areata. Ann Dermatol. 1997;9:239–241.[↩]
- Wells PA, Willmoth T, Russell RJ. Does fortune favour the bald? Psychological correlates of hair loss in males. Br J Psychol. 1995;86(pt 3):337–344.[↩]
- Bergfeld WF. Androgenetic alopecia: an autosomal dominant disorder. Am J Med. 1995;98(1A):95S–98S.[↩]
- Leyden J, Dunlap F, Miller B, et al. Finasteride in the treatment of men with frontal male pattern hair loss. J Am Acad Dermatol. 1999;40(6 pt 1):930–937.[↩][↩]
- Kaufman KD, Olsen EA, Whiting D, et al. Finasteride in the treatment of men with androgenetic alopecia. Finasteride Male Pattern Hair Loss Study Group. J Am Acad Dermatol. 1998;39(4 pt 1):578–589.[↩][↩]
- Rahimi-Ardabili B, Pourandarjani R, Habibollahi P, Mualeki A. Finasteride induced depression: a prospective study. BMC Clin Pharmacol. 2006;6:7.[↩]
- Olsen EA, Dunlap FE, Funicella T, et al. A randomized clinical trial of 5% topical minoxidil versus 2% topical minoxidil and placebo in the treatment of androgenetic alopecia in men. J Am Acad Dermatol. 2002;47(3):377–385.[↩][↩][↩]
- Dawber RP, Rundegren J. Hypertrichosis in females applying minoxidil topical solution and in normal controls. J Eur Acad Dermatol Venereol. 2003;17(3):271–275.[↩][↩][↩]
- Diani AR, Mulholland MJ, Shull KL, et al. Hair growth effects of oral administration of finasteride, a steroid 5 alpha-reductase inhibitor, alone and in combination with topical minoxidil in the balding stumptail macaque. J Clin Endocrinol Metab. 1992;74(2):345–350.[↩]
- Khandpur S, Suman M, Reddy BS. Comparative efficacy of various treatment regimens for androgenetic alopecia in men. J Dermatol. 2002;29(8):489–498.[↩]
- Olsen EA, Weiner MS. Topical minoxidil in male pattern baldness: effects of discontinuation of treatment. J Am Acad Dermatol. 1987;17(1):97–101.[↩]
- Olsen EA. Female pattern hair loss and its relationship to permanent/cicatricial alopecia: a new perspective. J Investig Dermatol Symp Proc. 2005;10(3):217–221.[↩]
- Drake LA, Dinehart SM, Farmer ER, et al. Guidelines of care for andro-genetic alopecia. American Academy of Dermatology. J Am Acad Dermatol. 1996;35(3 pt 1):465–469.[↩]
- Vexiau P, Chaspoux C, Boudou P, et al. Effects of minoxidil 2% vs. cyproterone acetate treatment on female androgenetic alopecia: a controlled, 12-month randomized trial. Br J Dermatol. 2002;146(6):992–999[↩]
- Burke BM, Cunliffe WJ. Oral spironolactone therapy for female patients with acne, hirsutism or androgenic alopecia. Br J Dermatol. 1985;112(1):124–125.[↩]
- Raudrant D, Rabe T. Progestogens with antiandrogenic properties. Drugs. 2003;63(5):463–492.[↩]
- Price VH, Roberts JL, Hordinsky M, et al. Lack of efficacy of finasteride in postmenopausal women with androgenetic alopecia. J Am Acad Dermatol. 2000;43(5 pt 1):768–776.[↩]
- Rokhsar CK, Shupack JL, Vafai JJ, Washenik K. Efficacy of topical sensitizers in the treatment of alopecia areata. J Am Acad Dermatol. 1998;39(5 pt 1):751–761.[↩]
- DeVillez RL, Jacobs JP, Szpunar CA, Warner ML. Androgenetic alopecia in the female. Treatment with 2% topical minoxidil solution. Arch Dermatol. 1994;130(3):303–307.[↩]
- Carmina E, Lobo RA. Treatment of hyperandrogenic alopecia in women. Fertil Steril. 2003;79(1):91–95.[↩]
- Overstreet JW, Fuh VL, Gould J, et al. Chronic treatment with finasteride daily does not affect spermatogenesis or semen production in young men. J Urol. 1999;162(4):1295–1300.[↩]
- Oesterling JE, Roy J, Agha A, et al. Biologic variability of prostate-specific antigen and its usefulness as a marker for prostate cancer: effects of finasteride. The Finasteride PSA Study Group. Urology. 1997;50(1):13–18.[↩]
- Piérard-Franchimont C, De Doncker P, Cauwenbergh G, Piérard GE. Ketoconazole shampoo: effect of long-term use in androgenic alopecia. Dermatology. 1998;196(4):474–477.[↩]
- Berger RS, Fu JL, Smiles KA, et al. The effects of minoxidil, 1% pyrithione zinc and a combination of both on hair density: a randomized controlled trial. Br J Dermatol. 2003;149(2):354–362.[↩]