Contents
- What is diabetes?
- What is insulin?
- How does insulin work?
- What is glucose?
- What is normal blood glucose levels?
- What is diabetes blood glucose levels?
- What happens when my blood sugar levels are too high?
- What is HbA1c?
- What are the most common symptoms of diabetes?
- What is insulin resistance?
- What are insulin resistance symptoms?
- How is insulin resistance treated?
- What is diabetic ketoacidosis?
- What are low blood sugar symptoms?
- Is there a cure for diabetes?
- Is there a cure for type 1 diabetes?
- Is diabetes a serious disease?
- Do people with diabetes need to eat special foods?
- What is diabetic neuropathy?
- What is diabetic retinopathy?
- What is diabetic nephropathy?
- What is diabetic coma?
- Types of diabetes
- Causes of diabetes
- Diabetes risk factors
- Diabetes prevention
- Symptoms and signs of diabetes
- Diabetes complications
- Diabetes diagnosis
- Diabetes treatment
- Diabetic diet
- Prediabetes
- Type 1 diabetes
- Type 1 diabetes causes
- Risk factors for type 1 diabetes
- Can type 1 diabetes be reversed?
- Type 1 diabetes prevention
- Type 1 diabetes symptoms and signs
- Type 1 diabetes complications
- Type 1 diabetes diagnosis
- Type 1 diabetes treatment
- Potential future treatments
- Situational concerns
- What can I eat with type 1 diabetes?
- Type 2 diabetes
- Can type 2 diabetes be cured?
- How to reverse type 2 diabetes?
- Who is more likely to develop type 2 diabetes?
- What is the difference between type 1 and type 2 diabetes?
- If I’m overweight, will I always develop type 2 diabetes?
- Do sugary drinks cause diabetes?
- Pregnancy and type 2 diabetes
- Type 2 diabetes causes
- Risk factors for developing type 2 diabetes
- Type 2 diabetes symptoms and signs
- Type 2 diabetes complications
- Type 2 diabetes prevention
- Type 2 diabetes diagnosis
- Type 2 diabetes treatment
- What can I eat with type 2 diabetes?
- Type 2 diabetes food list
- Can I snack in between meals?
- Type 3 diabetes
- Gestational diabetes
- What causes gestational diabetes?
- Risk factors for gestational diabetes
- Gestational diabetes symptoms
- What are complications of gestational diabetes?
- Gestational diabetes diagnosis
- Gestational diabetes treatment
- Gestational diabetes diet
- Exercise
- Medication
- How can I help prevent getting diabetes later in life?
What is diabetes?
Diabetes also known as diabetes mellitus, is a disease that occurs when your blood sugar, also called blood glucose, is too high (hyperglycemia) due to an inability to produce enough insulin and/or to respond to insulin. Over time, having too much sugar (glucose) in your blood can cause health problems, such as heart disease, nerve damage, eye problems, and kidney disease. If you’re diagnosed with diabetes, you’ll need to eat healthily, take regular exercise and carry out regular blood tests to ensure your blood glucose levels stay balanced.
An estimated 30.3 million people in the United States or 9.4 percent of the population, have diabetes, but as many as 8 million are not yet aware that diabetes is affecting their health. About one in four people with diabetes don’t know they have the disease. An estimated 84.1 million Americans aged 18 years or older have prediabetes.
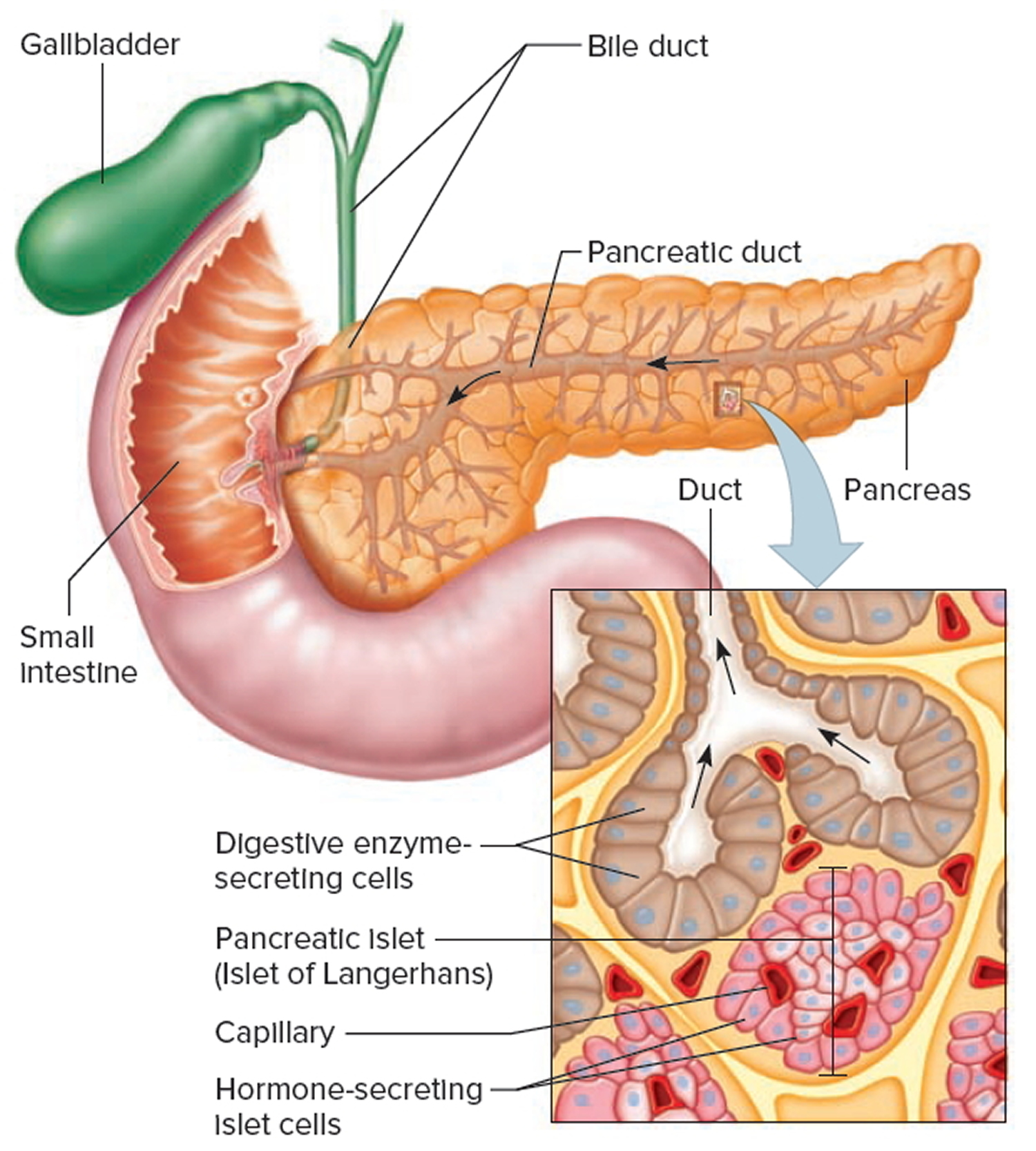
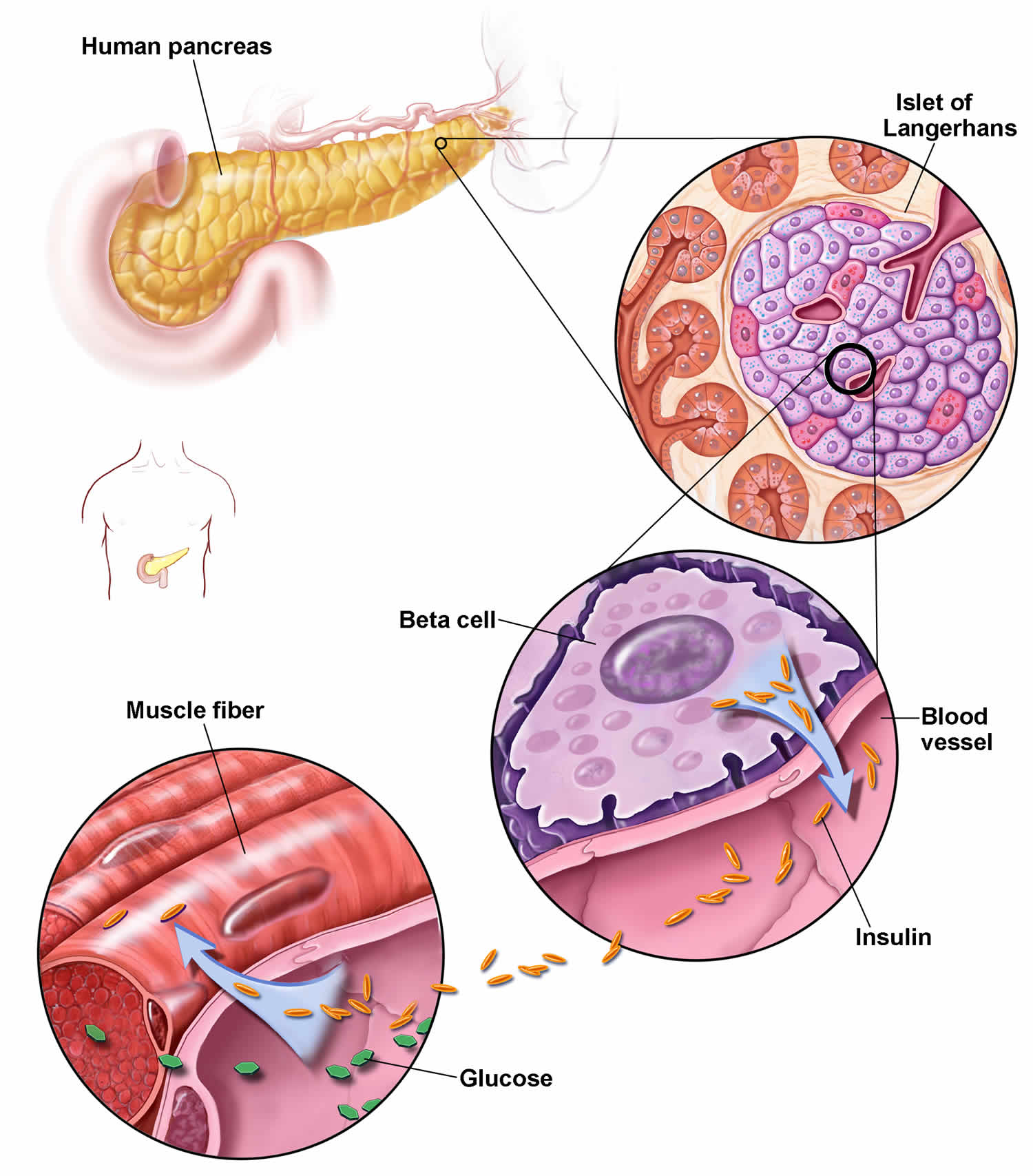
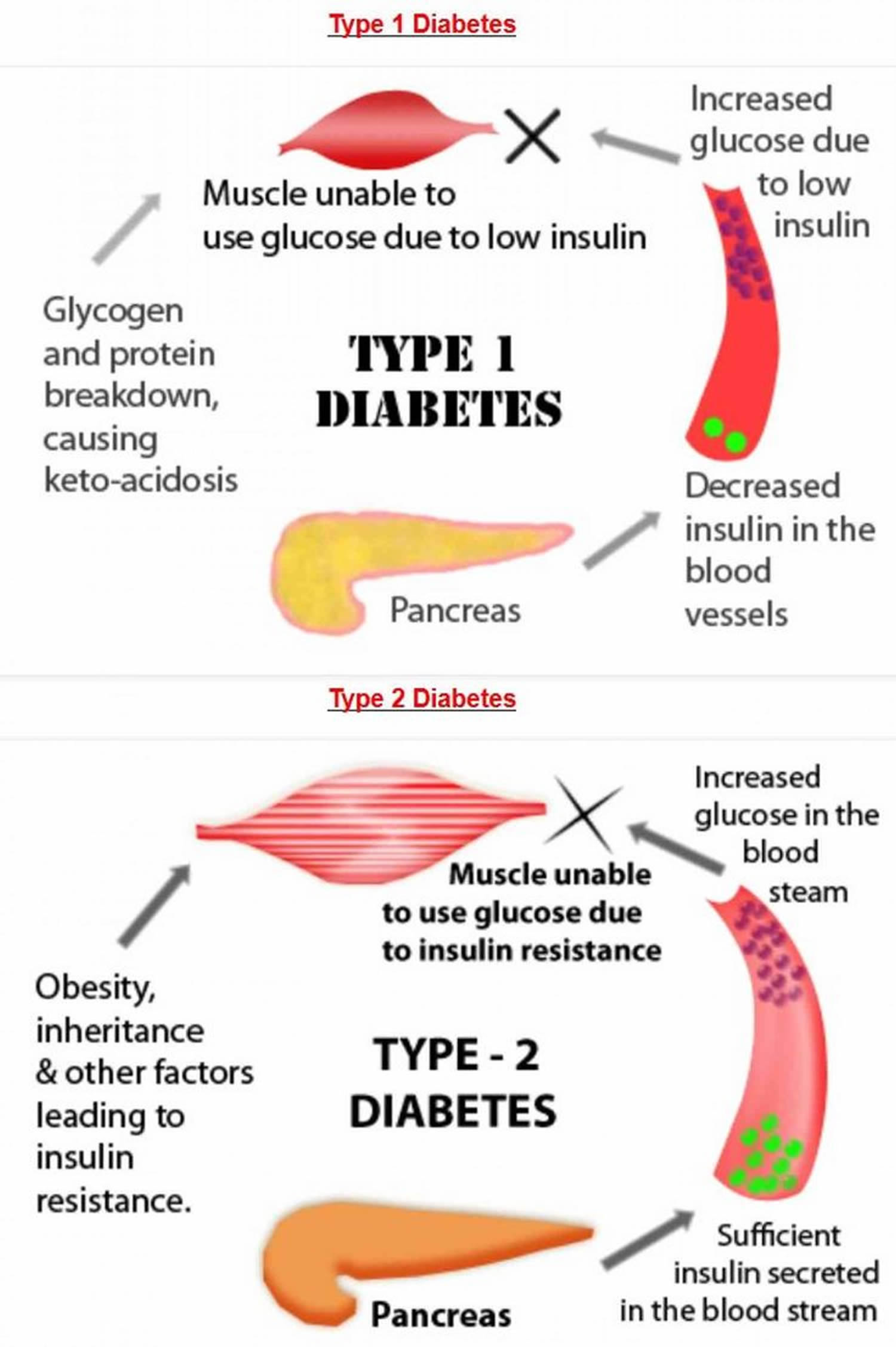
Normally, after a meal, your body breaks down sugar and starches from food into glucose to use for energy. This causes blood glucose levels to rise. Your pancreas (an organ behind your stomach) makes a hormone called insulin that helps your body keep the right amount of glucose in your blood. Insulin is a hormone produced by the beta cells in your pancreas. Insulin regulates the transport of glucose into most of your body’s cells and works with glucagon, another pancreatic hormone, to maintain blood glucose levels within a narrow range. When you have diabetes, your body doesn’t make enough insulin or can’t use insulin well (insulin resistance), so you end up with too much sugar in your blood. This can cause serious health problems, like heart disease, kidney failure and blindness.
If someone is unable to produce enough insulin, or if the body’s cells are resistant to its effects (insulin resistance), then less glucose is transported from the blood into cells. Blood glucose levels remain high but the body’s cells “starve.” This can cause both short-term and long-term health problems, depending on the severity of the insulin deficiency and/or resistance. Diabetics typically have to control their blood glucose levels on a daily basis and over time to avoid health problems and complications.
A very high blood glucose level (acute hyperglycemia) can be a medical emergency. The body tries to rid the blood of excess glucose by flushing it out of the system with increased urination. This process can cause dehydration and upset the body’s electrolyte balance as sodium and potassium are lost in the urine. With severe insulin deficiency, glucose is not available to the cells and the body may attempt to provide an alternate energy source by metabolizing fatty acids. This less efficient process leads to a buildup of ketones and upsets the body’s acid-base balance, producing a state known as ketoacidosis or diabetic ketoacidosis. Left unchecked, acute hyperglycemia can lead to severe dehydration, loss of consciousness, and even death.
A very low blood glucose level (hypoglycemia), often as a result of too much insulin, can also be life-threatening. It can lead to hunger, sweating, irregular and rapid heart beat, confusion, blurred vision, dizziness, fainting, and seizures. Severely low blood glucose can lead fairly quickly to insulin shock and death.
Glucose levels that rise over time and become chronically elevated may not be initially noticed. The body tries to control the amount of glucose in the blood by increasing insulin production and by eliminating glucose in the urine. Signs and symptoms usually begin to arise when the body is no longer able to compensate for the higher levels of blood glucose. Chronic high blood glucose can cause long-term damage to blood vessels, nerves, and organs throughout the body and can lead to other conditions such as kidney disease (diabetic nephropathy), loss of vision (diabetic retinopathy), strokes, cardiovascular disease, and circulatory problems in the legs. Damage from hyperglycemia (high blood glucose level) is cumulative and may begin before a person is aware that he or she has diabetes. The sooner the diabetes is detected and treated, the better the chances are of minimizing long-term complications.
Diabetes treatment may involve healthy diets, exercise and/or medications, including insulin, with aims to ensure that your blood glucose does not get too high or too low.
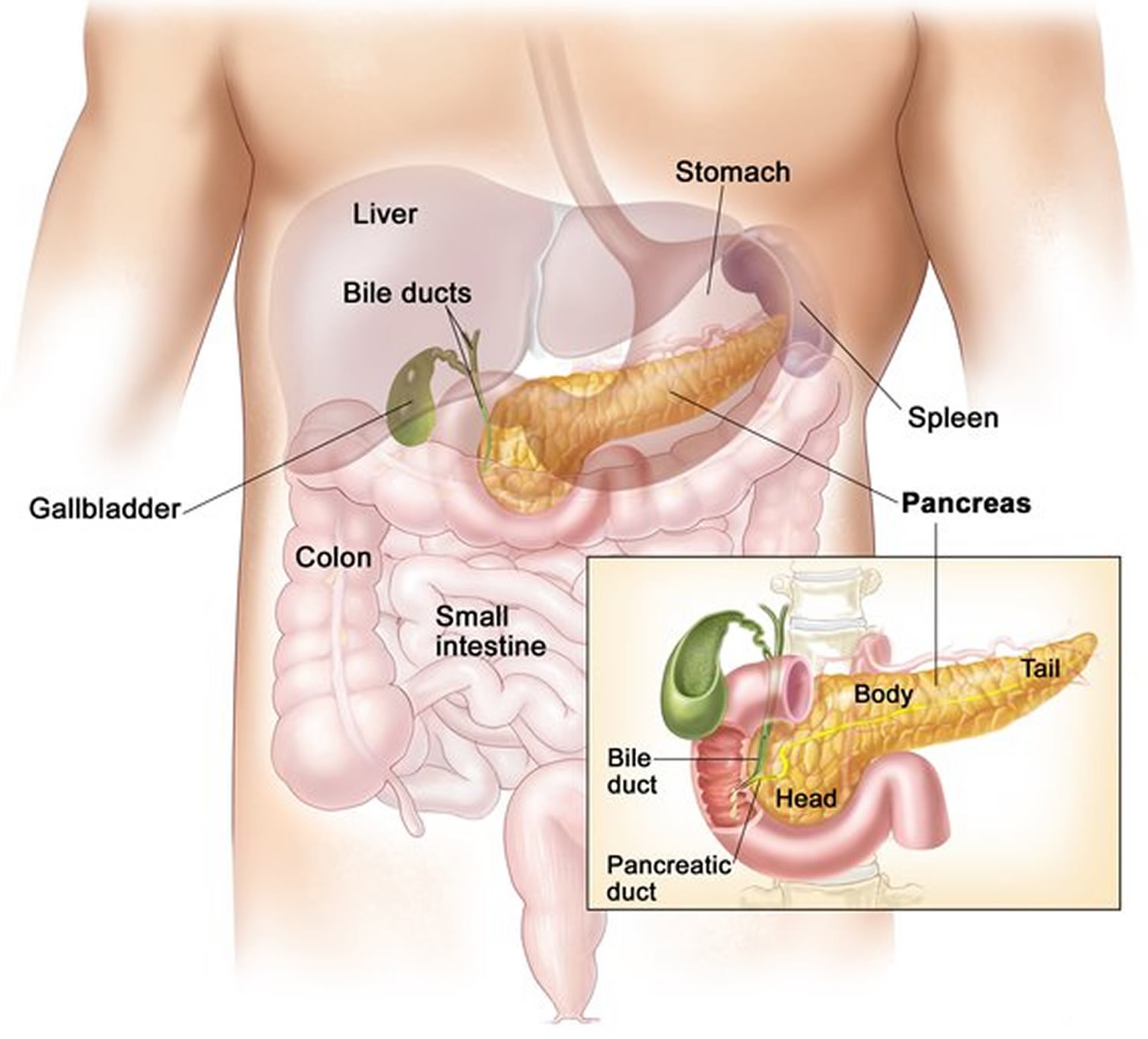
Figure 1. Pancreas location
Figure 2. Pancreas anatomy
What is insulin?
Insulin is a hormone that comes from your pancreas, a gland situated behind and below the stomach. The pancreas secretes insulin into the bloodstream. The insulin circulates, enabling sugar to enter your cells. Insulin lowers the amount of sugar in your bloodstream. As your blood sugar level drops, so does the secretion of insulin from your pancreas.
If your body isn’t able to make enough insulin or if your body’s cells have trouble accepting insulin, your blood glucose level can rise to a dangerous level. This may lead to diabetes, a serious disease that can damage your body’s organs if it is not kept under control.
How does insulin work?
Insulin is a hormone that comes from the gland situated behind and below the stomach (pancreas). Insulin regulates how the body uses sugar in the following ways:
- Sugar in the bloodstream triggers the pancreas to secrete insulin.
- Insulin circulates in the bloodstream, enabling sugar to enter your cells.
- The amount of sugar in your bloodstream drops.
- In response to this drop, the pancreas releases less insulin.
What is glucose?
Glucose is the type of sugar that your body uses as its principal energy source. Glucose comes from two major sources: the food you eat and your liver. Your liver stores glucose as glycogen and makes glucose. The glucose enters your bloodstream and is taken up by your body’s cells with the help of a hormone called insulin.
If your body isn’t able to make enough insulin, or if your body’s cells have trouble accepting insulin, your blood glucose level can rise to a dangerous level. This may lead to diabetes, a serious disease that can damage your body’s organs if it is not kept under control.
When your glucose levels are low, such as when you haven’t eaten in a while, the liver breaks down stored glycogen into glucose to keep your glucose level within a normal range.
What is normal blood glucose levels?
A blood sugar level with blood sample taken at a random time (regardless of when you last ate) less than 140 mg/dL (7.8 mmol/L) is normal.
A fasting blood sugar level (a blood sample taken after an overnight fast) less than 100 mg/dL (5.6 mmol/L) is normal.
What is diabetes blood glucose levels?
A blood sugar level with blood sample taken at a random time (regardless of when you last ate) of 200 milligrams per deciliter (mg/dL) [11.1 millimoles per liter (mmol/L)] or higher suggests diabetes.
A fasting blood sugar level (a blood sample taken after an overnight fast) of 126 mg/dL (7 mmol/L) or higher on two separate tests, you have diabetes.
What happens when my blood sugar levels are too high?
If your blood sugar levels are slightly above your targets, there are usually no symptoms. But if your blood sugar levels become too high, you may experience some symptoms associated with a hyperglycemia (or hyper).
The blood sugar level at which symptoms begin to appear is different for everyone, but the common symptoms include passing more urine than normal, being very thirsty, having headaches and feeling tired and lethargic.
What is HbA1c?
The HbA1c (hemoglobin A1c) also known as glycated hemoglobin (A1C) or glycohemoglobin measures the percentage of hemoglobin A in your blood that has glucose attached. The HbA1c (glycated hemoglobin A1C) test estimates how much glucose or blood sugar, has been in your bloodstream over the last two to three months. HbA1c is a marker for long-term glucose control and the HbA1c test can identify diabetes or keep track of how well diabetes is being controlled. Since red blood cells live about three months, your hemoglobin A1c test result corresponds to your average blood glucose level throughout the three months before your test.
The hemoglobin A1c (HbA1c) test is NOT used to diagnose gestational diabetes, a form of the disease that can develop during pregnancy.
Glucose has the ability to attach to hemoglobin in the blood and form hemoglobin A1c (HbA1c). Hemoglobin is the protein in red blood cells that carries oxygen. A measurement of hemoglobin A1c (HbA1c) reflects the percentage of hemoglobin A that is attached to glucose compared to the total amount of hemoglobin A in the blood.
The more glucose is in the blood, the more glucose can attach to hemoglobin. If your hemoglobin A1c (HbA1c) percentage is too high, this means that your average blood glucose in the previous months has been too high as well.
If you have diabetes, an ideal HbA1c level is 48mmol/mol (6.5%) or below. If you’re at risk of developing type 2 diabetes, your target HbA1c level should be below 42mmol/mol (6%).
The hemoglobin A1c (HbA1c) test may have several purposes:
- Screening for prediabetes and diabetes: Screening means checking for health conditions before a person experiences symptoms. If you are over 40 and are obese or overweight, or if you are otherwise at a high risk for diabetes, your doctor may want to screen you. The hemoglobin A1c test can be used for diabetes screening, but the results may need to be confirmed by repeating the test or using another type of test.
- Diagnosing prediabetes and diabetes: Diagnosis uses tests and procedures to find out the cause of health changes. Your doctor may order a hemoglobin A1c test for you, among other tests, if you have symptoms or show signs of diabetes. Diabetes symptoms can include excessive thirst, frequent urination, blurred vision, tingling or loss of sensation in the feet and hands, and feeling extremely tired.
- Monitoring diabetes: If you have been diagnosed with diabetes, your doctor may order a hemoglobin A1c test for you at least twice a year. This helps give your doctor an idea of how well your blood glucose has been controlled in the months between your appointments. Keeping track of your blood glucose allows your doctor to make adjustments to your treatment plan and lower your chance of health problems.
Table 1. HbA1c (A1c) test results
| A1c (HbA1c) Level | Indication |
|---|---|
| Less than 5.7% (39 mmol/mol) | Normal |
| 5.7% to 6.4% (39-46 mmol/mol) | Prediabetes |
| 6.5% (47 mmol/mol) or higher | Diabetes |
What are the most common symptoms of diabetes?
No individual is the same. The symptoms you experience won’t exactly match those of another person. However, the most common symptoms experienced by many people with diabetes are increased thirst, increased urination , feeling tired and losing weight. These symptoms occur because some or all of the glucose stays in your blood, and isn’t being used as fuel for energy. Your body tries to reduce blood glucose levels by flushing the excess glucose out of your body in your urine, making you more thirsty. High levels of glucose being passed in the urine are a perfect breeding ground for the fungal infection which causes thrush. But not everyone gets symptoms. In fact, 6 out of 10 people have no symptoms when they’re diagnosed with type 2 diabetes.
What is insulin resistance?
Insulin resistance also known as impaired insulin sensitivity, is when the insulin that you produce, or the insulin you inject, doesn’t work properly, making the insulin hormone less effective. Insulin resistance is when cells in your muscles, fat, and liver don’t respond well to insulin and can’t easily take up glucose from your blood. Insulin resistance is identified as an impaired biologic response to insulin stimulation of target tissues, primarily the liver, muscle, and adipose tissue 1. As a result, your pancreas makes more insulin and more insulin is needed to persuade fat and muscle cells to take up glucose and the liver to continue to store it. As long as your pancreas can make enough insulin to overcome your cells’ weak response to insulin, your blood glucose levels will stay in the healthy range.
However, the clinical definition of insulin resistance remains elusive as there is not a generally accepted test for insulin resistance 2. Clinically, insulin resistance is recognized via the metabolic consequences associated with insulin resistance as described in metabolic syndrome and insulin resistance syndrome 1. While insulin resistance is a hallmark of prediabetes and type 2 diabetes it can also affect those with type 1 diabetes.
Scientists are beginning to get a better understanding of how insulin resistance develops. For starters, several genes have been identified that make a person more or less likely to develop insulin resistance. It’s also known that older people are more prone to insulin resistance. Lifestyle can play a role, too. Being sedentary, overweight or obese and having too much fat around your stomach increases your risk for insulin resistance. Why? It’s not clear, but some researchers theorize that extra fat tissue may cause inflammation, physiological stress or other changes in the cells that contribute to insulin resistance. There may even be some undiscovered factor produced by fat tissue, perhaps a hormone, that signals the body to become insulin resistant. Just why a person fails to respond properly to insulin is still a mystery. But there are ways to make the body more receptive to insulin, which can help prevent or delay type 2 diabetes or help someone with type 1 diabetes manage their blood sugar (blood glucose).
In response to the body’s insulin resistance, the pancreas deploys greater amounts of the hormone to keep cells energized and blood glucose levels under control. This is why people with type 2 diabetes tend to have elevated levels of circulating insulin. The ability of the pancreas to increase insulin production means that insulin resistance alone won’t have any symptoms at first. Over time, though, insulin resistance tends to get worse, and the pancreatic beta cells that make insulin can wear out. Eventually, the pancreas no longer produces enough insulin to overcome the cells’ resistance. The result is higher blood sugar levels, and ultimately prediabetes or type 2 diabetes.
Insulin has other roles in the body besides regulating blood sugar levels, and the effects of insulin resistance are thought to go beyond diabetes. For example, some research has shown that insulin resistance, independent of diabetes, is associated with heart disease.
Insulin resistance is more likely to happen as a teenager when hormones are unpredictable and can be completely unrelated to your weight. To reduce your insulin resistance you might need to start oral medications alongside your insulin, making insulin more effective again. Your healthcare team will advise you on the best method to reduce your insulin resistance.
What are insulin resistance symptoms?
The clinical presentation of insulin resistance is variable and is dependent on the subset of insulin resistance present, duration of the condition, level of beta-cell function, and the individual’s propensity for the secondary illnesses due to insulin resistance. Insulin resistance is commonly associated with visceral adiposity, glucose intolerance, hypertension, dyslipidemia, hypercoagulable state, endothelial dysfunction, and/or elevated markers of inflammation. Therefore, the presence of these clinical abnormalities is usually characteristic of an insulin resistant state 3.
Common insulin resistance signs and symptoms include:
- The asymptomatic patients with obesity, hypertension, or hyperlipidemia
- Those with metabolic syndrome
- Prediabetes or type 2 diabetes mellitus
- Those with symptomatic microvascular disease (retinopathy, neuropathy, or nephropathy)
- Those with macrovascular disease (stroke, peripheral artery disease and coronary artery disease)
- Those with polycystic ovary syndrome (PCOS)
- Those with type A or type B insulin resistance
- Elevated blood pressure
- Gender and race-specific increased waist circumference
- Those with xanthelasma or xanthomas
- The signs and symptoms of polycystic ovary syndrome (PCOS) (menstrual irregularities, hirsutism, acne, and alopecia)
- Acanthosis nigricans, a patchy velvety brown pigmentation around the neck axilla and groin regions.
- The signs and symptoms of one of several genetic syndromes that include insulin resistance
How is insulin resistance treated?
While it may not be possible to defeat insulin resistance entirely, there are ways to make the body’s cells more receptive to insulin.
- Getting active is probably the best way to combat insulin resistance. Exercise can dramatically reduce insulin resistance in both the short and long terms. In addition to making the body more sensitive to insulin and building muscle that can absorb blood glucose, physical activity opens up an alternate gateway for glucose to enter muscle cells without insulin acting as an intermediary, reducing the cells’ dependence on insulin for energy. While this doesn’t reduce insulin resistance itself, it can help people who are insulin resistant improve their blood sugar control.
- Weight loss can also cut down on insulin resistance. No single diet has been proved to be the most effective. Some evidence suggests, though, that eating foods that are low in fat and high in carbohydrates can worsen insulin resistance. Research has also shown that people who undergo weight-loss surgery are likely to become significantly more sensitive to insulin.
- No medications are specifically approved to treat insulin resistance. Yet diabetes medications like metformin and thiazolidinediones, or thiazolidinediones, are insulin sensitizers that lower blood sugar, at least in part, by reducing insulin resistance.
What is diabetic ketoacidosis?
Diabetic ketoacidosis (DKA) is a serious complication of diabetes that occurs when your body produces high levels of blood acids called ketones. Diabetic ketoacidosis is a serious condition that affects people with type 1 diabetes, and occasionally those with type 2 diabetes. Untreated diabetic ketoacidosis can lead to death.
The condition develops when your body can’t produce enough insulin. Insulin normally plays a key role in helping sugar (glucose) — a major source of energy for your muscles and other tissues — enter your cells. Without enough insulin, your body begins to break down fat as fuel. This process produces a buildup of acids in the bloodstream called ketones, eventually leading to diabetic ketoacidosis if untreated.
If you have diabetes or you’re at risk of diabetes, learn the warning signs of diabetic ketoacidosis and when to seek emergency care.
Diabetic ketoacidosis signs and symptoms often develop quickly, sometimes within 24 hours. For some, these signs and symptoms may be the first indication of having diabetes. You may notice:
- Excessive thirst
- Frequent urination
- Nausea and vomiting
- Stomach pain
- Weakness or fatigue
- Shortness of breath
- Fruity-scented breath
- Confusion
More-specific signs of diabetic ketoacidosis — which can be detected through home blood and urine testing kits — include:
- High blood sugar level
- High ketone levels in your urine
If you feel ill or stressed or you’ve had a recent illness or injury, check your blood sugar level often. You might also try an over-the-counter urine ketones testing kit.
See your doctor immediately if:
- You’re vomiting and unable to tolerate food or liquid
- Your blood sugar level is higher than your target range and doesn’t respond to home treatment
- Your urine ketone level is moderate or high
Seek emergency care if:
- Your blood sugar level is consistently higher than 300 milligrams per deciliter (mg/dL), or 16.7 millimoles per liter (mmol/L)
- You have ketones in your urine and can’t reach your doctor for advice
- You have many signs and symptoms of diabetic ketoacidosis — excessive thirst, frequent urination, nausea and vomiting, stomach pain, weakness or fatigue, shortness of breath, fruity-scented breath, and confusion.
What are low blood sugar symptoms?
Temporary low blood sugar level (hypoglycemia) in the diabetic may be caused by the accidental injection of too much insulin, not eating enough or waiting too long to eat, exercising strenuously, or by the swings in glucose levels seen with “brittle” diabetes. Hypoglycemia needs to be addressed as soon as it is noticed as it can rapidly progress to unconsciousness.
Signs and symptoms of a low blood sugar level (hypoglycemia) may include:
- Shakiness or nervousness
- Anxiety
- Fatigue
- Weakness
- Sweating
- Sudden severe hunger
- Nausea
- Dizziness or lightheadedness
- Headache
- Difficulty speaking
- Confusion
- Double vision
- Convulsions
- Coma
Some people, especially those who’ve had diabetes for a long time, develop a condition known as hypoglycemia unawareness and won’t have the warning signs that signal a drop in blood sugar.
Is there a cure for diabetes?
Unfortunately, there’s currently no permanent cure for either type 1 or type 2 diabetes, but scientists are working on a ground-breaking weight management study, to help people put their type 2 diabetes into remission. There’s evidence that some people with type 2 can put their diabetes into remission by losing weight. Following a very low-calorie diet under medical supervision, or having weight loss surgery (bariatric surgery) are some ways you can put your type 2 diabetes into remission. Remission is when blood glucose (or blood sugar) levels are in a normal range again. This doesn’t mean diabetes has gone for good. It’s still really important for people in remission to get regular healthcare checks. But being in remission can be life changing.
Is there a cure for type 1 diabetes?
In type 1 diabetes, insulin-producing beta cells in the pancreas are destroyed by the immune system. This means you can’t make the insulin you need to live. To stop type 1 diabetes scientists need to disrupt the immune system’s attack on beta cells. Currently scientists are working on it. They’re aiming to develop and test treatments – called immunotherapies – that target the immune system to stop it destroying beta cells.
Is diabetes a serious disease?
Yes. Diabetes causes more deaths per year than breast cancer and AIDS combined and having diabetes nearly doubles your chance of having a heart attack. The good news is that managing your diabetes can reduce your risk for diabetes complications.
Common diabetes health complications include heart disease, chronic kidney disease, nerve damage, and other problems with feet, oral health, vision, hearing, and mental health.
- Heart and blood vessel (cardiovascular) disease. Diabetes majorly increases the risk of many heart problems. These can include coronary artery disease with chest pain (angina), heart attack, stroke and narrowing of arteries (atherosclerosis). If you have diabetes, you’re more likely to have heart disease or stroke.
- Nerve damage (diabetic neuropathy). Too much sugar can injure the walls of the tiny blood vessels (capillaries) that nourish the nerves, especially in the legs. This can cause tingling, numbness, burning or pain that usually begins at the tips of the toes or fingers and gradually spreads upward. Damage to the nerves related to digestion can cause problems with nausea, vomiting, diarrhea or constipation. For men, it may lead to erectile dysfunction.
- Kidney damage (diabetic nephropathy). The kidneys hold millions of tiny blood vessel clusters (glomeruli) that filter waste from the blood. Diabetes can damage this delicate filtering system.
- Eye damage (diabetic retinopathy). Diabetes can damage the blood vessels of the eye (diabetic retinopathy). This could lead to blindness.
- Foot damage. Nerve damage in the feet or poor blood flow to the feet increases the risk of many foot complications.
- Skin and mouth conditions. Diabetes may leave you more prone to skin problems, including bacterial and fungal infections.
- Hearing impairment. Hearing problems are more common in people with diabetes.
- Alzheimer’s disease. Type 2 diabetes may increase the risk of dementia, such as Alzheimer’s disease.
- Depression. Depression symptoms are common in people with type 1 and type 2 diabetes.
Do people with diabetes need to eat special foods?
No, you don’t need special food. Packaged foods with special “diabetes-friendly” claims may still raise blood glucose levels, be more expensive, and/or contain sugar alcohols that can have a laxative effect.
A healthy meal plan for people with diabetes is generally the same as healthy eating for anyone. In fact, there are a lot of different eating plans that can help you manage your diabetes. In general, a healthy eating plan for diabetes will include lots of non-starchy vegetables, limit added sugars, swap refined grains for whole grains and prioritize whole foods over highly processed foods when possible.
What is diabetic neuropathy?
Diabetic neuropathy is nerve damage that is caused by diabetes. Excess sugar can injure the walls of the tiny blood vessels (capillaries) that nourish your nerves, especially in your legs. Research suggests that up to one-half of people with diabetes have peripheral neuropathy 4. Different types of nerve damage cause different symptoms. Diabetic neuropathy symptoms can range from pain and numbness in your feet to problems with the functions of your internal organs, such as your heart and bladder.
Diabetic neuropathy can cause tingling, numbness, burning or pain that usually begins at the tips of the toes or fingers and gradually spreads upward. Left untreated, you could lose all sense of feeling in the affected limbs.
Damage to the nerves related to digestion can cause problems with nausea, vomiting, diarrhea or constipation. For men, it may lead to erectile dysfunction.
Types of diabetic neuropathy include the following:
- Peripheral neuropathy: Peripheral neuropathy is nerve damage that typically affects the feet and legs and sometimes affects the hands and arms.
- Autonomic neuropathy: Autonomic neuropathy is damage to nerves that control your internal organs. Autonomic neuropathy can lead to problems with your heart rate and blood pressure, digestive system, bladder, sex organs, sweat glands, eyes, and ability to sense hypoglycemia. More than 30 percent of people with diabetes have autonomic neuropathy 5.
- Focal neuropathies: Focal neuropathies are conditions in which you typically have damage to single nerves, most often in your hand, head, torso, and leg.
- Proximal neuropathy: Proximal neuropathy is a rare and disabling type of nerve damage in your hip, buttock, or thigh. This type of nerve damage typically affects one side of your body and may rarely spread to the other side. Proximal neuropathy often causes severe pain and may lead to significant weight loss.
If you have diabetes, your chance of developing nerve damage caused by diabetes increases the older you get and the longer you have diabetes.
You are also more likely to develop nerve damage if you have diabetes and
- are overweight
- have high blood pressure
- have high cholesterol
- have advanced kidney disease
- drink too many alcoholic drinks
- smoke
Research also suggests that certain genes may make people more likely to develop diabetic neuropathy.
Managing your diabetes is an important part of preventing health problems such as diabetic neuropathy. This means managing your blood glucose, blood pressure, cholesterol levels, and weight to keep nerve damage from getting worse.
Foot care is very important for all people with diabetes, and it’s even more important if you have peripheral neuropathy. Check your feet for problems every day, and take good care of your feet. See your doctor for a neurological exam and a foot exam at least once a year—more often if you have foot problems.
What is diabetic retinopathy?
Diabetic retinopathy is a complication of diabetes. The retina is a layer of light-sensitive layer of cells at the back of your eyes that converts light into electrical signals. The signals are sent to your brain which turns them into the images you see. The retina needs a constant supply of blood, which it receives through a network of tiny blood vessels. Diabetes can cause the tiny blood vessels in the retina to swell and then bleed or leak fluid. This happens in many parts of the body, and can cause problems like kidney disease and poor circulation to the legs. Over time, a persistently high blood sugar level can damage these blood vessels in 3 main stages:
- Background retinopathy – tiny bulges develop in the blood vessels, which may bleed slightly but don’t usually affect your vision
- Pre-proliferative retinopathy – more severe and widespread changes affect the blood vessels, including more significant bleeding into the eye
- Proliferative retinopathy – scar tissue and new blood vessels, which are weak and bleed easily, develop on the retina, this can result in some loss of vision
Anyone with type 1 diabetes or type 2 diabetes is potentially at risk of developing diabetic retinopathy. Both eyes are usually affected. However, if a problem with your eyes is picked up early, lifestyle changes and/or treatment can stop it getting worse.
The longer you have diabetes, the more likely it is that you’ll get diabetic retinopathy. Your risk also increases if your diabetes is not well controlled or if you have high blood pressure or high cholesterol.
You’re at a greater risk of diabetic retinopathy if you:
- have had diabetes for a long time
- have a persistently high blood sugar (blood glucose) level
- have high blood pressure
- have high cholesterol
- are pregnant
- are of Asian or Afro-Caribbean background
By keeping your blood sugar, blood pressure and cholesterol levels under control, you can reduce your chances of developing diabetic retinopathy.
You might not notice diabetic retinopathy in the early stages, as it doesn’t tend to have any obvious symptoms until it’s more advanced. So, if you have diabetes, it is important to get your eyes checked regularly. Early signs of diabetic retinopathy can be picked up by taking photographs of your eyes during diabetic eye screening.
If you have diabetic retinopathy, you might:
- have blurred, distorted or patchy vision that can’t be corrected with prescription glasses
- have eye floaters (moving specks) in your vision
- find it more difficult to read or watch television
- have pain in one or both eyes
- have trouble seeing straight lines
- become sensitive to glare
- have trouble seeing at night
- have problems with your balance
See your doctor or diabetes care team immediately if you experience:
- gradually worsening vision
- sudden vision loss
- shapes floating in your field of vision (floaters)
- blurred or patchy vision
- eye pain or redness
These symptoms don’t necessarily mean you have diabetic retinopathy, but it’s important to get them checked out. Don’t wait until your next screening appointment.
You can reduce your risk of developing diabetic retinopathy or help prevent it getting worse, by:
- Controlling your blood sugar levels, blood pressure and cholesterol
- Having regular eye checks or diabetic eye screening – annual eye screening is offered to all people with diabetes aged 12 and over to pick up and treat any problems early on. The screening test involves examining the back of the eyes and taking photographs.
- Taking your diabetes medication as prescribed
- Getting medical advice quickly if you notice any changes to your vision
- Maintaining a healthy weight, eating a healthy, balanced diet, exercising regularly and stopping smoking
If problems are caught early, treatment can help prevent or reduce vision loss. Treatment for diabetic retinopathy is only necessary if screening detects significant problems that mean your vision is at risk.
Keeping your blood sugar, blood pressure and cholesterol under control can treat diabetic retinopathy. There are injections of medication into your eyes that can reduce swelling in the retina.
Laser treatment can be used to seal leaking blood vessels and stop the growth of abnormal blood vessels. Surgery to remove blood or scar tissue from your eyes may be needed in people with more advanced diabetic retinopathy.
What is diabetic nephropathy?
If you have diabetes, your blood glucose or blood sugar levels are too high. Over time, this can damage your kidneys. Diabetic nephropathy is the name given to kidney damage caused by diabetes. It develops slowly, over many years, and is also referred to as diabetic kidney disease. Having high blood glucose levels due to diabetes can damage the part of the kidneys that filters your blood known as nephrons. Inside the nephrons are tiny blood vessels called capillaries and tiny urine-collecting tubes. One of the major structures in the nephron is a group of blood vessels known as the glomerulus, which acts as a filter. Having high blood glucose levels can interfere with the function of the glomerulus. High blood glucose levels can also cause scarring of the glomerulus (called glomerulosclerosis). As the scarring gets worse, the kidneys stop being able to filter waste products from the blood. The damaged filters becomes ‘leaky’ and lets protein into your urine. When enough glomeruli have been damaged, kidney failure results. Diabetic nephropathy begins long before you have symptoms. People with diabetes should get regular screenings for kidney disease. Tests include a urine test to detect protein in your urine and a blood test to show how well your kidneys are working.
If the damage continues, your kidneys could fail. For some people, diabetic nephropathy can progress to chronic kidney disease (CKD) and kidney failure. In fact, diabetes is the most common cause of kidney failure in the United States. One in 4 women and one in 5 men with type 2 diabetes develops diabetic nephropathy. It is even more common in type 1 diabetes. Almost one in five people with diabetes will need treatment for diabetic nephropathy. People with kidney failure need either dialysis or a kidney transplant.
Diabetic nephropathy usually has no symptoms early on. You can’t tell that there is protein in your urine – it’s something that is detected with a urine test.
It can take many years for the kidney damage to progress. Symptoms usually only appear when kidney damage has deteriorated significantly. Even then, the symptoms tend to be vague.
If the kidney damage becomes severe, you may notice:
- weight loss;
- a poor appetite or feeling sick;
- swollen ankles and feet (due to retaining fluid);
- puffiness around the eyes;
- dry, itchy skin;
- muscle cramps;
- needing to pass urine more often;
- feeling tired; and
- having difficulty concentrating.
People who have diabetic nephropathy also often have high blood pressure. High blood pressure can further contribute to kidney damage.
There are many factors that can increase your risk of developing diabetic nephropathy. These include:
- the length of time that you have had diabetes;
- having high blood glucose levels (because your diabetes is not well managed);
- having high blood pressure;
- being overweight or obese; and
- smoking.
Your risk is also higher if you have other problems related to your diabetes. These include diabetic retinopathy or diabetic neuropathy.
You can slow down kidney damage or keep it from getting worse. Controlling your blood sugar and blood pressure, taking your medicines and not eating too much protein can help.
Blood glucose levels should be kept in the normal range as much as possible to prevent or slow the progression of diabetic nephropathy. Lifestyle measures (including diet and exercise) in combination with oral diabetes medicines (oral hypoglycemics) or insulin can be used to control blood glucose levels.
People with type 2 diabetes who have microalbuminuria or proteinuria (evidence of some degree of diabetic nephropathy) are usually also treated with medicines called angiotensin-converting enzyme inhibitors (ACE inhibitors) or angiotensin receptor blockers (ARBs). These medicines are also used to control blood pressure, but even if your blood pressure is normal, your doctor may prescribe an ACE inhibitor or ARB because they decrease the amount of protein in the urine and can prevent or slow the progression of diabetic kidney disease.
Other medicines may also be prescribed to help control high blood pressure.
What is diabetic coma?
A diabetic coma is a life-threatening diabetes complication that causes unconsciousness. A diabetic coma is a medical emergency that you won’t have time to prepare for. When someone is in a coma, they are unconscious, they do not respond, and they cannot be woken up. A diabetic coma is a medical emergency and the person in diabetic coma will need immediate treatment in hospital. If you feel extreme high or low blood sugar signs or symptoms and think you might pass out, call your local emergency number. If you’re with someone with diabetes who has passed out, call for emergency help, and be sure to let the emergency personnel know that the unconscious person has diabetes.
If you have diabetes, dangerously high blood sugar (hyperglycemia) or dangerously low blood sugar (hypoglycemia) can lead to a diabetic coma.
If you lapse into a diabetic coma, you’re alive — but you can’t awaken or respond purposefully to sights, sounds or other types of stimulation. Left untreated, a diabetic coma can lead to permanent brain damage and death.
Anyone who has diabetes is at risk of a diabetic coma, but the following factors can increase your risk:
- Insulin delivery problems. If you’re on an insulin pump, you have to check your blood sugar frequently. Insulin delivery can stop if the pump fails or the tubing (catheter) is twisted or falls out of place. A lack of insulin can lead to diabetic ketoacidosis.
- An illness, trauma or surgery. When you’re sick or injured, blood sugar levels tend to rise, sometimes dramatically. This may cause diabetic ketoacidosis if you have type 1 diabetes and don’t increase your insulin dosage to compensate.
- Medical conditions, such as congestive heart failure or kidney disease, also may increase your risk of diabetic hyperosmolar syndrome or Hyperosmolar Hyperglycaemic State (HHS). Diabetic hyperosmolar syndrome or Hyperosmolar Hyperglycaemic State (HHS) occurs in people with Type 2 diabetes who experience very high blood glucose levels (often over 40mmol/l). It can develop over a course of weeks through a combination of illness (e.g.infection) and dehydration..
- Poorly managed diabetes. If you don’t monitor your blood sugar properly or take your medications as directed, you’ll have a higher risk of developing long-term complications and a diabetic coma.
- Deliberately skipping meals or insulin. Sometimes, people with diabetes who also have an eating disorder choose not to use their insulin as directed with the hope of losing weight. This is a dangerous, life-threatening practice that increases the risk of a diabetic coma.
- Drinking alcohol. Alcohol can have unpredictable effects on your blood sugar. Alcohol’s sedating effects may make it harder for you to know when you’re having low blood sugar symptoms. This can increase your risk of a diabetic coma caused by hypoglycemia.
- Illegal drug use. Illegal drugs, such as cocaine and ecstasy, can increase your risk of severe high blood sugar levels and conditions linked to diabetic coma.
Before developing a diabetic coma, you’ll usually experience signs and symptoms of high blood sugar (hyperglycemia) or low blood sugar (hypoglycemia).
High blood sugar (hyperglycemia)
If your blood sugar level is too high, you may experience:
- Increased thirst
- Frequent urination
- Fatigue
- Nausea and vomiting
- Shortness of breath
- Stomach pain
- Fruity breath odor
- A very dry mouth
- A rapid heartbeat
Low blood sugar (hypoglycemia)
Signs and symptoms of a low blood sugar level may include:
- Shakiness or nervousness
- Anxiety
- Fatigue
- Weakness
- Sweating
- Hunger
- Nausea
- Dizziness or lightheadedness
- Difficulty speaking
- Confusion
Some people, especially those who’ve had diabetes for a long time, develop a condition known as hypoglycemia unawareness and won’t have the warning signs that signal a drop in blood sugar.
If you experience any symptoms of high or low blood sugar, test your blood sugar and follow your diabetes treatment plan based on the test results. If you don’t start to feel better quickly, or you start to feel worse, call for emergency help.
- If you’re with someone with diabetes who has passed out or is acting strange, possibly as if he or she has had too much alcohol, call for immediate medical help.
- If you have no training in diabetes care, wait for the emergency care team to arrive.
- If you are familiar with diabetes care, test the unconscious person’s blood sugar and follow these steps:
- If the blood sugar level is lower than 70 mg/dL (3.9 mmol/L), give the person an injection of glucagon. Do not try to give fluids to drink and do not give insulin to someone with low blood sugar.
- If the blood sugar level is above 70 mg/dL (3.9 mmol/L) wait for medical help to arrive. Don’t give sugar to someone whose blood sugar isn’t low.
- If you called for medical help, let the emergency care team know about the diabetes and what steps you’ve taken, if any.
Types of diabetes
There are five types of diabetes:
- Type 1 diabetes occurs when a person’s own immune system breaks down the cells in the pancreas that produce insulin.
- Type 2 diabetes occurs when the body’s cells do not respond effectively to insulin or lose the ability to produce enough insulin in the pancreas. This causes glucose to stay in your blood, leading to a higher-than-normal level of glucose in your body. Both type 1 and type 2 diabetes can begin during childhood and adulthood.
- Gestational diabetes occurs when a woman experiences high blood glucose levels during pregnancy. It usually goes away after the baby is born. During pregnancy, the placenta produces hormones to sustain your pregnancy. These hormones make your cells more resistant to insulin. Normally, your pancreas responds by producing enough extra insulin to overcome this resistance. But sometimes your pancreas can’t keep up. When this happens, too little glucose gets into your cells and too much stays in your blood, resulting in gestational diabetes. Women who experience gestational diabetes have a higher risk of developing type 2 diabetes in the future.
- Pre-diabetes is where blood glucose levels are higher than usual, but not high enough for a diagnosis of diabetes. In prediabetes — which can lead to type 2 diabetes — and in type 2 diabetes, your cells become resistant to the action of insulin, and your pancreas is unable to make enough insulin to overcome this resistance. Instead of moving into your cells where it’s needed for energy, sugar builds up in your bloodstream. Exactly why this happens is uncertain, although it’s believed that genetic and environmental factors play a role in the development of prediabetes and type 2 diabetes. Being overweight is strongly linked to the development of type 2 diabetes, but not everyone with type 2 is overweight.
- Type 3 diabetes. This lesser-known diabetes type manifests as insulin resistance within the brain and has major potential to impact neurocognition and contributes to the cause of Alzheimer’s disease 6.
- There are a variety of less common causes of diabetes. Any condition that damages the pancreas and/or affects insulin production or usage can lead to the development of diabetes.
- Latent autoimmune diabetes in adults (LADA or sometimes called diabetes type 1.5) is a slowly progressing type 1 diabetes that is often misdiagnosed as type 2 diabetes. Those who have it tend to produce some of their own insulin when first diagnosed and most have diabetes autoantibodies.
- Monogenic diabetes is a group of causes associated with faulty genes that affect the body’s ability to produce insulin:
- Maturity onset diabetes of the young or MODY, is a type of diabetes that is caused by a gene mutation. Several different genes that affect the production of insulin are grouped under MODY. This is an inherited cause of diabetes that is typically detected in children or adolescents, but some people develop it later and some do not develop diabetes.
- Neonatal diabetes mellitus or NDM, is a rare type found in newborns and young infants.
- Conditions that block or damage the pancreas can lead to the development of diabetes. Examples include:
- Cystic fibrosis produces thick mucus that can block the release of pancreatic enzymes and damage the pancreas.
- Hemochromatosis is an inherited condition associated with increased iron storage. Iron buildup can damage the pancreas and other organs. It is sometimes referred to as “bronze diabetes” because the excess iron can turn a person’s skin a bronze color.
- Pancreatitis, pancreatic cancer, and other pancreatic diseases that damage the pancreas and/or beta cell production
- Pancreas trauma or removal
Table 2 summarizes some types of diabetes. Read the sections below to learn more about the various types.
Table 2. Types of diabetes
| Type of Diabetes | Description |
|---|---|
| Type 1 diabetes | Exact cause unknown; thought to be primarily an autoimmune disease that involves the destruction of the insulin-producing beta cells in the pancreas; can occur at any age but usually diagnosed in children and young adults. |
| Type 2 diabetes | Most common type; associated with insulin resistance and with insulin production that is insufficient to meet the body’s needs and to compensate for resistance. It develops most frequently in overweight middle-aged and elderly people. With increased obesity in children and adolescents, the condition is becoming more common at younger ages. |
| Gestational diabetes | Develops during a woman’s pregnancy and affects both mother and developing baby; typically develops late in the pregnancy. |
| Prediabetes | Higher blood glucose than normal, but not considered diabetes; people with prediabetes are at an increased risk of developing type 2 diabetes. |
| Other diabetes | A group of less common types of diabetes. Any condition that damages the pancreas and/or affects insulin production or usage can cause diabetes. |
Causes of diabetes
What all types of diabetes have in common is that they cause people to have too much glucose (sugar) in their blood. But we all need some glucose. It’s what gives you energy. You get glucose when your body breaks down the carbohydrates that you eat or drink. And that glucose is released into your blood.
You also need a hormone called insulin. It’s made by your pancreas, and it’s insulin that allows the glucose in your blood to enter your cells and fuel your body.
If you don’t have diabetes, your pancreas senses when glucose has entered your bloodstream and releases the right amount of insulin, so the glucose can get into your cells. But if you have diabetes, this system doesn’t work.
Genetic mutations, other diseases, damage to the pancreas, and certain medicines may also cause diabetes.
Genetic mutations
- Monogenic diabetes is caused by mutations, or changes, in a single gene. These changes are usually passed through families, but sometimes the gene mutation happens on its own. Most of these gene mutations cause diabetes by making the pancreas less able to make insulin. The most common types of monogenic diabetes are neonatal diabetes and maturity-onset diabetes of the young (MODY). Neonatal diabetes occurs in the first 6 months of life. Doctors usually diagnose MODY (maturity-onset diabetes of the young) during adolescence or early adulthood, but sometimes the disease is not diagnosed until later in life.
- Cystic fibrosis produces thick mucus that causes scarring in the pancreas. This scarring can prevent the pancreas from making enough insulin.
- Hemochromatosis causes the body to store too much iron. If the disease is not treated, iron can build up in and damage the pancreas and other organs.
Hormonal diseases
Some hormonal diseases cause the body to produce too much of certain hormones, which sometimes cause insulin resistance and diabetes.
- Cushing’s syndrome occurs when the body produces too much cortisol—often called the “stress hormone.”
- Acromegaly occurs when the body produces too much growth hormone.
- Hyperthyroidism occurs when the thyroid gland produces too much thyroid hormone.
Damage to or removal of the pancreas
Pancreatitis, pancreatic cancer, and trauma can all harm the beta cells or make them less able to produce insulin, resulting in diabetes. If the damaged pancreas is removed, diabetes will occur due to the loss of the beta cells.
Medicines
Sometimes certain medicines can harm beta cells or disrupt the way insulin works. These include:
- niacin, a type of vitamin B3
- certain types of diuretics, also called water pills
- anti-seizure drugs
- psychiatric drugs
- drugs to treat human immunodeficiency virus (HIV)
- pentamidine, a drug used to treat a type of pneumonia
- glucocorticoids—medicines used to treat inflammatory illnesses such as rheumatoid arthritis, asthma, lupus and ulcerative colitis
- anti-rejection medicines, used to help stop the body from rejecting a transplanted organ
Statins, which are medicines to reduce LDL (“bad”) cholesterol levels, can slightly increase the chance that you’ll develop diabetes. However, statins help protect you from heart disease and stroke. For this reason, the strong benefits of taking statins outweigh the small chance that you could develop diabetes.
If you take any of these medicines and are concerned about their side effects, talk with your doctor.
Diabetes risk factors
Some people are at a higher risk of developing diabetes than others.
Depending on the type of diabetes, this can be due to their ethnicity, their genetics or even their lifestyle choices. These are known as the risk factors of diabetes. Knowing what the risk factors are, and if they affect you, can help you decide if you need to do something to reduce your risk.
Risk factors for developing type 2 diabetes
Some things can increase your chance of getting type 2 diabetes. Because the symptoms of type 2 diabetes are not always obvious, it’s really important to be aware of these risk factors. Factors that may increase your risk of type 2 diabetes include:
- Weight. Being overweight or obese is a main risk.
- Fat distribution. Storing fat mainly in your abdomen (waist size is too large) — rather than your hips and thighs — indicates a greater risk. Your risk of type 2 diabetes rises if you’re a man with a waist circumference above 40 inches (101.6 centimeters) or a woman with a measurement above 35 inches (88.9 centimeters).
- How to measure your waist: Find the top of your hip bone and the bottom of your ribcage. In the middle of these two points is where you need to measure. For many people, the belly button is a good guide, but this might not be the case for you, so it’s best to find that midpoint between your ribcage and hip. If you’re still not sure, watch the video below.
- What is a healthy waist size? This all depends on your gender and ethnicity. For a healthy measurement you need to aim to be less than:
- 80 cm (31.5 in) for all women
- 94 cm (37 in) for most men
- 90cm (35in) for South Asian men. This is because you have a higher risk of type 2 diabetes if you are of black or South Asian background.
- Inactivity. The less active you are, the greater your risk. Physical activity helps control your weight, uses up glucose as energy and makes your cells more sensitive to insulin.
- Family history. The risk of type 2 diabetes increases if your parent, brother or sister has type 2 diabetes.
- Race and ethnicity. Although it’s unclear why, people of certain races and ethnicities — including African Caribbean, Black African, Hispanic, Native American and Asian people (Indian, Pakistani, Bangladeshi or Chinese), and Pacific Islanders — are more likely to develop type 2 diabetes than white people are.
- Blood lipid levels. An increased risk is associated with low levels of high-density lipoprotein (HDL) cholesterol — the “good” cholesterol — and high levels of triglycerides.
- Age. You’re more at risk if you’re white and over 40, or over 25 if you’re African Caribbean, Black African, or South Asian (Indian, Pakistani or Bangladeshi).
- Medical history. For example if you have a history of high blood pressure, heart attack or strokes, gestational diabetes or severe mental illness.
- Prediabetes. Prediabetes is a condition in which your blood sugar level is higher than normal, but not high enough to be classified as diabetes. Left untreated, prediabetes often progresses to type 2 diabetes.
- Pregnancy-related risks. Your risk of developing type 2 diabetes increases if you developed gestational diabetes when you were pregnant or if you gave birth to a baby weighing more than 9 pounds (4 kilograms).
- Polycystic ovary syndrome (PCOS). Having polycystic ovary syndrome — a common condition characterized by irregular menstrual periods, excess hair growth and obesity — increases the risk of diabetes.
- High blood pressure. Having blood pressure over 140/90 millimeters of mercury (mm Hg) is linked to an increased risk of type 2 diabetes.
- Abnormal cholesterol and triglyceride levels. If you have low levels of high-density lipoprotein (HDL), or “good,” cholesterol, your risk of type 2 diabetes is higher. Triglycerides are another type of fat carried in the blood. People with high levels of triglycerides have an increased risk of type 2 diabetes. Your doctor can let you know what your cholesterol and triglyceride levels are.
- Smoking. Smoking is associated with a higher risk of type 2 diabetes, and also increases the risk of other health conditions such as heart disease and cancer.
- Areas of darkened skin, usually in the armpits and neck. This condition, called acanthosis nigricans. This condition often indicates insulin resistance. Acanthosis nigricans is most common in those who are overweight, have darker skin, and have diabetes or pre-diabetic conditions. Acanthosis nigricans is not contagious. It is not harmful. Acanthosis nigricans is a warning sign of a health problem that requires medical attention.
Figure 3. Acanthosis nigricans
Diabetes prevention
Type 1 diabetes can’t be prevented. However, the same healthy lifestyle choices that help treat prediabetes, type 2 diabetes and gestational diabetes can also help prevent them:
- Eat healthy foods. Choose foods lower in fat and calories and higher in fiber. Focus on fruits, vegetables and whole grains. Strive for variety to prevent boredom.
Get more physical activity. Aim for about 30 minutes of moderate aerobic activity on most days of the week, or at least 150 minutes of moderate aerobic activity a week. - Lose excess pounds. If you’re overweight, losing even 7% of your body weight — for example, 14 pounds (6.4 kilograms) if you weigh 200 pounds (90.7 kilograms) — can reduce the risk of diabetes. Don’t try to lose weight during pregnancy, however. Talk to your doctor about how much weight is healthy for you to gain during pregnancy. To keep your weight in a healthy range, focus on permanent changes to your eating and exercise habits. Motivate yourself by remembering the benefits of losing weight, such as a healthier heart, more energy and improved self-esteem.
Sometimes medication is an option as well. Oral diabetes drugs such as metformin (Glumetza, Fortamet, others) may reduce the risk of type 2 diabetes — but healthy lifestyle choices remain essential. Have your blood sugar checked at least once a year to check that you haven’t developed type 2 diabetes.
Symptoms and signs of diabetes
The signs and symptoms of diabetes are related to high glucose levels (hyperglycemia), low glucose levels (hypoglycemia), and complications associated with diabetes.
The following symptoms of diabetes are typical. However, some people with diabetes have symptoms so mild that they go unnoticed.
Common symptoms of diabetes include:
- increased thirst and urination
- feeling very thirsty
- urinating more frequently than usual, particularly at night
- increased hunger
- fatigue or feeling very tired
- blurred vision
- numbness or tingling in the feet or hands (neuropathy)
- sores that do not heal or wounds that heal slowly
- unexplained weight loss and loss of muscle bulk
- itching around the penis or vagina, or frequent episodes of thrush
- erectile dysfunction in men
- absence of menstruation in women
These symptoms can affect anyone – adult or child. Symptoms of type 1 diabetes can start quickly, in a matter of weeks or even days. Symptoms of type 2 diabetes often develop slowly, over the course of several years and can be so mild that you might not even notice them. Many people with type 2 diabetes have no symptoms. Some people do not find out they have the disease until they have diabetes-related health problems, such as blurred vision or heart trouble.
Diabetes complications
Diabetes increases your risk for many serious health problems. Over a long period of time, high glucose levels in your blood can seriously damage your heart, your eyes, your feet and your kidneys. These are known as the complications of diabetes. However, with the correct treatment and recommended lifestyle changes, many people with diabetes are able to prevent or delay the onset of these complications.
There are two types of diabetes complications: serious ones that build up over time called chronic complications and ones that can happen at any time called acute complications.
Acute diabetes complications
These can happen at any time and may lead to chronic complications.
- Hypos or hypoglycemia – when your blood sugars are too low
- Hypers or hyperglycemia – when your blood sugars are too high
- Hyperosmolar Hyperglycemic State (HHS)– a life-threatening emergency that only happens in people with type 2 diabetes. It’s brought on by severe dehydration and very high blood sugars (often over 40mmol/l). It can develop over a course of weeks through a combination of illness (e.g.infection) and dehydration.
- Diabetic ketoacidosis (DKA) – a life-threatening emergency where the lack of insulin and high blood sugars leads to a build-up of ketones. If your muscle cells become starved for energy, your body may respond by breaking down fat stores. This process forms toxic acids known as ketones. If you have ketones (measured in blood or urine) and high blood sugar, the condition is called diabetic ketoacidosis. Left untreated, it can lead to a diabetic coma. Diabetic ketoacidosis is most common in type 1 diabetes but sometimes occurs in type 2 diabetes or gestational diabetes.
Other acute complications may include:
- Skin conditions. Diabetes may leave you more susceptible to skin problems, including bacterial and fungal infections.
- Wound infections, especially on the feet; they can be slow to heal and, if not addressed promptly, may eventually lead to an amputation. Aggressive and specialized measures are often necessary, and the affected person may need to consult with a diabetic wound specialist, a health practitioner trained in working with the altered healing of diabetics.
- Urinary tract infections (UTIs), which can be frequent and resistant to antibiotic treatment; delayed or inadequate treatment can lead to or exacerbate kidney damage.
Chronic diabetes complications
Long-term complications of diabetes develop gradually and can lead to serious damage if they go unchecked and untreated. The longer you have diabetes — and the less controlled your blood sugar — the higher the risk of complications. Eventually, diabetes complications may be disabling or even life-threatening. Possible long-term problems include:
- Eye problems (diabetic retinopathy). Some people with diabetes develop an eye disease called diabetic retinopathy which can affect their eyesight. If retinopathy is picked up – usually from an eye screening test – it can be treated and sight loss prevented.
- Foot problems. Having diabetes means that you’re more at risk of serious foot problems and which can lead to amputation if untreated. Nerve damage can affect the feeling in your feet and raised blood sugar can damage the circulation, making it slower for sores and cuts to heal. That’s why it’s important to tell your doctor if you notice any change in how your feet look or feel.
- Heart attack and stroke. When you have diabetes, high blood sugar for a period of time can damage your blood vessels. This can sometimes lead to heart attacks and strokes.
- Kidney problems (diabetic nephropathy). Diabetes can cause damage to your kidneys over a long period of time making it harder to clear extra fluid and waste from your body. This is caused by high blood sugar levels and high blood pressure. It is known as diabetic nephropathy or kidney disease.
- Nerve damage (diabetic neuropathy). Some people with diabetes may develop nerve damage caused over time by high blood sugar levels. This can make it harder for the nerves to carry messages between the brain and every part of our body so it can affect how we see, hear, feel and move.
- Gum disease and other mouth problems. Too much sugar in your blood can lead to more sugar in your saliva. This brings bacteria which produces acid which attacks your tooth enamel and damages your gums. The blood vessels in your gums can also become damaged, making gums more likely to get infected.
- Related conditions, like cancer. If you have diabetes, you’re more at risk of developing certain cancers. And some cancer treatments can affect your diabetes and make it harder to control your blood sugar.
- Sexual problems in women. Damage to blood vessels and nerves can restrict the amount of blood flowing to your sexual organs so you can lose some sensation. If you have high blood sugar, you are also more likely to get thrush or a urinary tract infection.
- Sexual problems in men. The amount of blood flowing to your sexual organs can be restricted which may cause you to have difficulty getting aroused. It may lead to erectile dysfunction, sometimes called impotence.
- Hearing impairment. Hearing problems are more common in people with diabetes.
- Alzheimer’s disease. Type 2 diabetes may increase the risk of dementia, such as Alzheimer’s disease. The poorer your blood sugar control, the greater the risk appears to be. Although there are theories as to how these disorders might be connected, none has yet been proved.
- Depression. Depression symptoms are common in people with type 1 and type 2 diabetes. Depression can affect diabetes management.
How do I prevent or delay diabetes complications?
High sugar levels in your blood over a long period of time can seriously damage your blood vessels. If your blood vessels aren’t working properly, blood can’t travel to the parts of your body it needs to. This means your nerves won’t work properly either and means you lose feeling in parts of your body. Once you’ve damaged the blood vessels and nerves in one part of your body, you’re more likely to develop similar problems in other parts of your body. So if your feet are damaged, serious heart problems can follow.
Scientists know that the higher your HbA1c level, the more you’re at risk of developing complications. Even a slightly high HbA1c increases your risk.
But it’s not just about blood sugars. High blood pressure, smoking and a lot of fat in your blood (cholesterol) can all damage your blood vessels and put you even more at risk.
Type 2 diabetes prevention
Healthy lifestyle choices can help prevent type 2 diabetes, and that’s true even if you have biological relatives living with diabetes. If you’ve received a diagnosis of prediabetes, lifestyle changes may slow or stop the progression to diabetes.
Prevention of diabetes through healthy lifestyle includes:
- Eating healthy foods. Choose foods lower in fat and calories and higher in fiber. Focus on fruits, vegetables and whole grains.
- Getting active. Aim for 150 or more minutes a week of moderate to vigorous aerobic activity, such as a brisk walk, bicycling, running or swimming.
- Losing weight. Losing a modest amount of weight and keeping it off can delay the progression from prediabetes to type 2 diabetes. If you have prediabetes, losing 7% to 10% of your body weight can reduce the risk of diabetes.
- Avoiding inactivity for long periods. Sitting still for long periods can increase your risk of type 2 diabetes. Try to get up every 30 minutes and move around for at least a few minutes.
For people with prediabetes, metformin (Fortamet, Glumetza, others), an oral diabetes medication, may be prescribed to reduce the risk of type 2 diabetes. This is usually prescribed for older adults who are obese and unable to lower blood sugar levels with lifestyle changes.
How to reduce your waist size
Unfortunately, there are no quick fixes when it comes to reducing your waist size. It comes down to eating well and moving more. Start by setting some realistic, achievable changes to suit your lifestyle. You can become more active by making small changes to your lifestyle. You can fit them around your daily life and in your budget. Here are three top tips to help make your life more active:
- Set clear goals to move more – setting goals can help you break down what you need to do and how to do it. This could be aiming to walk more, taking up a new activity or learning a new skill such as swimming or running.
- Plan ahead – we all have busy lives, so try to plan what you’re going to eat and what activity you’re going to do this week, fitting it around your social life. You can always squeeze in an activity during your lunch hour or go for walk instead of getting another form of transport.
- Start by making small changes – it’s time to put your plan into action. Start small and do something you enjoy. Doing just a little bit more each day will still make a difference. It also means you’re more likely to stick to it. Just remember, small changes to your routine won’t have such a big impact, so start small and grow.
Diabetes diagnosis
Symptoms of type 1 diabetes often appear suddenly and are often the reason for checking blood sugar levels. Because symptoms of other types of diabetes and prediabetes come on more gradually or may not be evident, the American Diabetes Association (ADA) has recommended screening guidelines. The American Diabetes Association recommends that the following people be screened for diabetes:
- Anyone with a body mass index (BMI) higher than 25 (23 for Asian Americans), regardless of age, who has additional risk factors, such as high blood pressure, abnormal cholesterol levels, a sedentary lifestyle, a history of polycystic ovary syndrome or heart disease, and who has a close relative with diabetes.
- Anyone older than age 45 is advised to receive an initial blood sugar screening, and then, if the results are normal, to be screened every three years thereafter.
- Women who have had gestational diabetes are advised to be screened for diabetes every three years.
- Anyone who has been diagnosed with prediabetes is advised to be tested every year.
According to the American Diabetes Association, a few different tests may be used for screening and diagnosis of diabetes or prediabetes and each test has advantages, disadvantages, and limitations.
Tests for type 1 and type 2 diabetes and prediabetes
Glycated hemoglobin (A1C) also known as hemoglobin A1c (HbA1C) test. The A1c blood test, which doesn’t require fasting, indicates your average blood sugar level for the past two to three months. It measures the percentage of blood sugar attached to hemoglobin, the oxygen-carrying protein in red blood cells. But the HbA1c blood test is not recommended for everyone. It should not be used for diabetes diagnosis in pregnant women, people who have had recent severe bleeding or blood transfusions, those with chronic kidney or liver disease, or people with blood disorders such as iron-deficiency anemia, vitamin B12 anemia, and hemoglobin variants. Also, only A1c tests that have been referenced to an accepted laboratory method (standardized) should be used for diagnostic or screening purposes. Currently, point-of-care tests, such as those that may be used at a doctor’s office or a patient’s bedside, are too variable for use in diagnosis but can be used to monitor treatment (lifestyle and drug therapies).
The higher your blood sugar levels, the more hemoglobin you’ll have with sugar attached. A hemoglobin A1c (HbA1C) level of 6.5% or higher on two separate tests indicates that you have diabetes. Hemoglobin A1c (HbA1C) between 5.7 and 6.4 % indicates prediabetes. Below 5.7% is considered normal.
Table 3. A1c (HbA1c) test results
| Result | A1C (HbA1c) |
|---|---|
| Normal | less than 5.7% |
| Prediabetes | 5.7% to 6.4% |
| Diabetes | 6.5% or higher |
If the hemoglobin A1c (HbA1C) test results aren’t consistent, the test isn’t available, or you have certain conditions that can make the A1C test inaccurate — such as if you are pregnant or have an uncommon form of hemoglobin (known as a hemoglobin variant) — your doctor may use the following tests to diagnose diabetes:
- Random blood sugar test also called Casual Plasma Glucose Test. A blood sample will be taken at a random time. Regardless of when you last ate, a blood sugar level of 200 milligrams per deciliter (mg/dL) — 11.1 millimoles per liter (mmol/L) — or higher suggests diabetes.
- Fasting blood sugar test. A blood sample will be taken after an overnight fast. A fasting blood sugar level less than 100 mg/dL (5.6 mmol/L) is normal. A fasting blood sugar level from 100 to 125 mg/dL (5.6 to 6.9 mmol/L) is considered prediabetes. If it’s 126 mg/dL (7 mmol/L) or higher on two separate tests, you have diabetes.
- Oral glucose tolerance test (OGTT). For this test, you fast overnight, and the fasting blood sugar level is measured. Then you drink a sugary liquid, and blood sugar levels are tested periodically for the next two hours. A blood sugar level less than 140 mg/dL (7.8 mmol/L) is normal. A reading of more than 200 mg/dL (11.1 mmol/L) after two hours indicates diabetes. A reading between 140 and 199 mg/dL (7.8 mmol/L and 11.0 mmol/L) indicates prediabetes.
If type 1 diabetes is suspected, your urine will be tested to look for the presence of a byproduct produced when muscle and fat tissue are used for energy because the body doesn’t have enough insulin to use the available glucose (ketones). Your doctor will also likely run a test to see if you have the destructive immune system cells associated with type 1 diabetes called autoantibodies.
In addition to diabetes tests listed above, used for screening, diagnosing and monitoring, a few other tests may be used in the evaluation of other types and causes of diabetes:
- Diabetes autoantibodies – this test may help detect latent autoimmune diabetes in adults (LADA) and distinguish it from type 2 diabetes if the diagnosis is unclear.
- Five of the most common diabetes-related autoantibody tests include:
- Islet Cell Cytoplasmic Autoantibodies (ICA)
- Glutamic Acid Decarboxylase Autoantibodies (GADA)
- Insulinoma-Associated-2 Autoantibodies (IA-2A)
- Insulin Autoantibodies (IAA)
- Zinc Transporter-8 Autoantibodies (ZnT8A)
- Five of the most common diabetes-related autoantibody tests include:
- Genetic testing may be performed to detect the specific gene mutation associated with MODY or NDM. In some cases, family members may also be tested to determine if they have inherited the same altered gene.
- Testing to detect other conditions that may cause diabetes is usually done separately. There is an awareness that these conditions are associated with an increased risk for the development of diabetes.
Several other laboratory tests may be used to evaluate glucose control, organ function, and to detect emerging complications. These may include:
- Fructosamine – evaluates average glucose levels over the past 2 to 3 weeks
- 1,5 Anhydroglucitol – a new test that detects high glucose levels in the past 1 to 2 weeks
- To monitor kidney function: urine albumin (microalbumin), creatinine clearance, eGFR, CMP, BUN, creatinine, cystatin C
- To monitor cholesterol and other lipids: cholesterol, HDL cholesterol, LDL cholesterol, triglycerides, lipid panel
Fasting blood glucose
Fasting glucose (fasting blood glucose, FBG) – this test measures the level of glucose in your blood after an 8-12 hour fast. This test is usually done first thing in the morning, before breakfast.
Table 4. Fasting blood glucose test results
| Fasting Glucose Level | Indication |
|---|---|
| From 70 to 99 mg/dL (3.9 to 5.5 mmol/L) | Normal fasting glucose |
| From 100 to 125 mg/dL (5.6 to 6.9 mmol/L) | Prediabetes (impaired fasting glucose) |
| 126 mg/dL (7.0 mmol/L) and above on more than one testing occasion | Diabetes |
Glucose tolerance test
When you receive a glucose tolerance test, a phlebotomist will draw a sample of your blood through a needle from a vein in your arm after you have fasted for at least eight hours, typically overnight. Then you will drink a sweet drink, and the technician will take more blood samples over the next two to three hours.
Diabetes is diagnosed at 2 hour blood sugar of greater than or equal to 200 mg/dl.
Table 5. Oral Glucose Tolerance Test (OGTT) results
| Result | Oral Glucose Tolerance Test (OGTT) |
|---|---|
| Normal | less than 140 mg/dl |
| Prediabetes | 140 mg/dl to 199 mg/dl |
| Diabetes | 200 mg/dl or higher |
Before the glucose tolerance test
You will be required to fast for at least eight hours before you take the test. This means you will need to go without any food or any drink besides water. Since the test is often scheduled for the morning, most of your fasting can happen while you sleep the night before.
You can generally follow a normal diet up until the time you begin fasting. Your doctor may ask you to make sure you consume at least 150 grams of carbohydrates each day in the three days before your glucose tolerance test.
If you take any prescription medications or over-the-counter drugs, be sure to discuss these with your doctor before you take the test. Your doctor can let you know whether any of these might alter the results of the test. They can also advise you whether you will need to stop taking any medications during the time you are fasting.
To ensure the most reliable results, ask your doctor for any specific pretest preparations and carefully follow those instructions on the days leading up to your glucose tolerance test.
During the glucose tolerance test
Glucose tolerance testing usually takes place in the morning. You may need to stay at the testing site for up to three hours.
The phlebotomist who gives you the test will start by drawing a small amount of your blood from a vein, most often in your arm. The technician may tie a band around your upper arm so the vein is easier to see. After cleaning the skin over your vein with a sterile wipe, a small needle will be inserted through the skin and into the vein. The sample of blood goes into a tube attached to the needle.
When the needle comes out, the phlebotomist will release the band on your arm and cover the injection site with a small bandage. Some people experience minor pain or discomfort when the needle goes in or comes out, but this usually does not last very long.
Once the first blood sample is taken, you will drink a bottle of liquid containing a defined amount of glucose. In adults, the drink usually contains 75 grams of glucose. In children, the amount is calculated based on body weight with a maximum of 75 grams. This drink tastes sweet like a sugary soda.
After you drink the glucose solution, your blood will be drawn several more times at regular intervals over the next two or three hours. You should not eat anything during this time, and you typically will remain in the waiting area.
After the glucose tolerance test
After the series of blood draws is complete, you may experience slight pain where the blood was taken. You can generally resume normal activities after your glucose tolerance test is performed. When the test is completed, you will be able to eat again. You may wish to take a snack with you to the testing site to have on hand after your last blood draw is finished.
Interpreting test results
The National Institute of Diabetes and Digestive and Kidney Disorders and the American Diabetes Association, among other organizations, list the following reference ranges for this two-hour value:
- Normal: Under 140 mg/dL
- Prediabetes: 140 to 199 mg/dL
- Diabetes: At or over 200 mg/dL
While this test can be used to diagnose both type 1 and type 2 diabetes, one test alone does not usually determine if you have diabetes. The doctor normally considers whether you have symptoms of diabetes, the results of other blood tests, or a repeated glucose tolerance test to arrive at a definitive diagnosis.
As a result, the best way to understand what your glucose tolerance test results mean is to discuss them with your doctor. Your doctor can explain how your results compare to the reference ranges, whether you will need a repeat test or other follow-up tests, and what further steps you may need to take for your health.
Diabetes treatment
Depending on what type of diabetes you have, blood sugar monitoring, insulin and oral medications may play a role in your treatment. People who have underlying conditions will need to be treated for these conditions, in addition to diabetes treatment. Eating a healthy diet, maintaining a healthy weight and participating in regular activity also are important factors in managing diabetes.
Treatments for all types of diabetes
An important part of managing diabetes — as well as your overall health — is maintaining a healthy weight through a healthy diet and exercise plan:
- Healthy eating. Contrary to popular perception, there’s no specific diabetes diet. You’ll need to center your diet on more fruits, vegetables, lean proteins and whole grains — foods that are high in nutrition and fiber and low in fat and calories — and cut down on saturated fats, refined carbohydrates and sweets. In fact, it’s the best eating plan for the entire family. Sugary foods are OK once in a while, as long as they’re counted as part of your meal plan. Yet, understanding what and how much to eat can be a challenge. A registered dietitian can help you create a meal plan that fits your health goals, food preferences and lifestyle. This will likely include carbohydrate counting, especially if you have type 1 diabetes or use insulin as part of your treatment.
- Physical activity. Everyone needs regular aerobic exercise, and people who have diabetes are no exception. Exercise lowers your blood sugar level by moving sugar into your cells, where it’s used for energy. Exercise also increases your sensitivity to insulin, which means your body needs less insulin to transport sugar to your cells. Get your doctor’s OK to exercise. Then choose activities you enjoy, such as walking, swimming or biking. What’s most important is making physical activity part of your daily routine. Aim for at least 30 minutes or more of aerobic exercise most days of the week, or at least 150 minutes of moderate physical activity a week. Bouts of activity can be as brief as 10 minutes, three times a day. If you haven’t been active for a while, start slowly and build up gradually. It’s also a good idea to avoid sitting for too long — aim to get up and move if you’ve been sitting for more than 30 minutes.
Diabetic diet
There is no specific diet for diabetes. But the foods you eat not only make a difference to how you manage your diabetes, but also to how well you feel and how much energy you have.
Fruit and vegetables
Fruit and veg are naturally low in calories and packed full of vitamins, minerals and fiber. They also add flavor and variety to every meal. Fruit and vegetables can help protect against stroke, heart disease, high blood pressure and some cancers – and when you have diabetes, you’re more at risk of developing these conditions.
Fruit and vegetables benefits
- Help to keep your digestive system working well
- Help protect the body from heart disease, stroke and some cancers
Examples of what to try:
- sliced melon or grapefruit topped with unsweetened yogurt, or a handful of berries, or fresh dates, apricots or prunes for breakfast
- mix carrots, peas and green beans into your pasta bake
- add an extra handful of peas to rice, spinach to lamb or onions to chicken
- try mushrooms, cucumber, spinach, cabbage, cauliflower, broccoli, celery and lettuce for lower carb vegetable options
- try avocados, blackberries, raspberries, strawberries, plums, peaches and watermelon for lower carb fruit options
Fresh, frozen, dried and canned – they all count. Go for a rainbow of colors to get as wide a range of vitamins and minerals as possible. Try to avoid fruit juices and smoothies as they don’t have as much fiber.
Everyone should aim to eat at least five portions a day. A portion is roughly what fits in the palm of your hand.
Starchy foods
Starchy foods are things like potatoes, rice, pasta, bread, chapattis, naan and plantain. They all contain carbohydrate, which is broken down into glucose and used by our cells as fuel. The problem with some starchy foods is that it can raise blood glucose levels quickly, which can make it harder for you to manage your diabetes. These foods have something called a high glycemic index (GI).
There are some better options for starchy foods – ones that affect blood glucose levels more slowly. These are foods with a low glycemic index (GI), like wholegrain bread, whole-wheat pasta and basmati, brown or wild rice. They also have more fiber, which helps to keep your digestive system working well. So if you’re trying to cut down on carbs, cut down on things like white bread, pasta and rice first.
Starchy foods benefits
- The fiber helps to keep your digestive system healthy
- Some affect your blood sugar levels more slowly
- Wholegrains help protect your heart
Examples of what to try
- two slices of multigrain toast with a bit of spread and Marmite or peanut butter
- brown rice, pasta or noodles in risottos, salads or stir-fries
- baked sweet potato with the skin left on – add toppings like cottage cheese or beans
- boiled cassava, flavored with chilli and lemon
- chapatti made with brown or wholemeal atta.
Proteins
Meat and fish are high in protein, which keeps your muscles healthy. But a healthy diet means less red and processed meat – they’ve been linked to cancer and heart disease. Oily fish like mackerel, salmon and sardines have a lot of omega-3 oil, which can help protect the heart.
Protein foods benefits
- Helps keep your muscles healthy
- Oily fish protects your heart
Aim to have some food from this group every day. Specifically at least 1 or 2 portions of oily fish each week. But you don’t need to eat meat every day.
Examples of what to try
- a small handful of raw nuts and seeds as a snack or chopped with a green salad
- using beans and pulses in a casserole to replace some – or all – of the meat
- eggs scrambled, poached, dry fried or boiled – the choice is yours
- grilled fish with masala, fish pie, or make your own fishcakes
- chicken grilled, roasted or stir-fried
Dairy foods
Milk, cheese and yogurt have lots of calcium and protein in – great for your bones, teeth and muscles. But some dairy foods are high in fat, particularly saturated fat, so choose lower-fat alternatives.
Check for added sugar in lower-fat versions of dairy foods, like yoghurt. It’s better to go for unsweetened yoghurt and add some berries if you want it sweeter. If you prefer a dairy alternative like soya milk, choose one that’s unsweetened and calcium-fortified.
Dairy foods Benefits
- Good for bones and teeth
- Keeps your muscles healthy
Examples of what to try
- a glass of milk straight, flavored with a little cinnamon or added to porridge
- natural or unsweetened yogurt with fruit or on curry
- cottage cheese scooped on carrot sticks
- a bowl of breakfast cereal in the morning, with skimmed or semi-skimmed milk
- a cheese sandwich for lunch, packed with salad
- a refreshing lassi or some plain yogurt with your evening meal
Oils and fats
You need some healthy fat in your diet but you need less saturated fat. This is because some saturated fats can increase cholesterol in your blood, increasing your risk of heart diseases and stroke. These less healthy options are butter, palm nut oil and coconut oil.
Healthier unsaturated fats are foods like olive oil, vegetable oil, rapeseed oil, spreads made from these oils, and nut butters.
Examples of what to try
- A drizzle of olive oil on your salad
- Peanut butter on your wholemeal toast
Avoid foods high in saturated fat, salt and sugar
You don’t need any of these as part of a healthy diet. The less often, the better. But we know you’re bound to eat these foods from time to time, so it’s really important to know how they might affect your body.
These foods include biscuits, crisps, chocolates, cakes, ice cream, butter and sugary drinks. These sugary foods and drinks are high in calories and raise blood sugar levels, so go for diet, light or low-calorie alternatives. And the best drink to choose is water – it’s calorie free.
They’re also high in unhealthy saturated fats, so they aren’t good for cholesterol levels and your heart.
And they can also be full of salt – processed foods especially. Too much salt can make you more at risk of high blood pressure and stroke. You should have no more than 1 tsp (6g) of salt a day.
Experts don’t recommend ‘diabetic’ ice cream or sweets. It’s now against the law to label any food as diabetic and there’s no evidence to suggest that food for diabetics offer any benefits over eating a healthy balanced diet.
Tips for cutting out saturated fat, salt and sugar
- Cook more meals from scratch at home, where you can control the amount of salt you use.
- Check food labels – look for green and orange colors.
- Try unsweetened teas and coffees – they’re better than fruit juices and smoothies as they don’t add any extra calories and carbs.
- Banish the salt shaker from the table – black pepper, herbs and spices are great ways of adding extra flavor to your food.
- Making your own sauces, like tomato ketchup and tandoori marinades.
Prediabetes
Prediabetes, also called borderline diabetes, means your blood sugar levels are higher than normal, but not high enough yet to be diagnosed as type 2 diabetes 7. In people with prediabetes, you can expect to see fasting blood glucose levels elevated between 100 mg/dL to 125 mg/dL (5.5 to 6.9 mmol/L) or 2 hours after eating blood glucose levels between 140 mg/dL to 199 mg/dL (7.8 to 11.0 mmol/L) 8, 9, 10. However, these blood sugar levels do not meet the required criteria for a diagnosis of diabetes mellitus (see below). For this reason, many people with prediabetes are not aware that they are living with prediabetes 11, 12, 13. Doctors sometimes refer to prediabetes as impaired glucose tolerance (IGT) or impaired fasting glucose (IFG), depending on what test was used when it was detected. Prediabetes puts you at a higher risk for developing type 2 diabetes, cardiovascular disease and stroke 10.
NOTE: Fasting means after not having anything to eat or drink (except water) for at least 8 hours before the test. This test is usually done first thing in the morning, before breakfast.
Healthy individuals, normal blood sugar levels are 14, 10:
- Between 70 to 99 mg/dL (4.0 to 5.4 mmol/L) when fasting.
- Up to 140 mg/dL (7.8 mmol/L) 2 hours after eating.
Blood sugar levels in diagnosing diabetes 8, 9:
- 126 mg/dL or higher (7.0 mmol/L or more) when fasting.
- 200 mg/dL or higher (11.1 mmol/L or more) 2 hours after eating.
- Random blood glucose test also called casual plasma glucose test (is a blood sugar check at any time of the day) of greater than or equal to 200 mg/dL (11.1 mmol/L or more).
NOTE: Fasting means after not having anything to eat or drink (except water) for at least 8 hours before the test. This test is usually done first thing in the morning, before breakfast.
Prediabetes usually occurs in people who already have some insulin resistance or whose beta cells in the pancreas aren’t making enough insulin to keep blood glucose in the normal range. Without enough insulin, extra glucose stays in your bloodstream rather than entering your cells. Over time, you could develop type 2 diabetes. Therefore, if you have prediabetes, you should be checked for type 2 diabetes every one to two years. If screening is negative for prediabetes, repeat screening should be carried out every 3 years as per the United States Preventive Services Task Force 10.
People with prediabetes often may show no signs or symptoms of diabetes, but will have blood sugar levels higher than normal, so you may have prediabetes and not know it.
Some people with prediabetes may have some of the symptoms of diabetes or even problems from diabetes already. You usually find out that you have prediabetes when being tested for diabetes.
Approximately 96 million American adults (18 and older), that’s more than 1 in 3, have prediabetes 15. Of those with prediabetes, more than 80% don’t know they have it. Prediabetes puts you at increased risk of developing type 2 diabetes, heart disease, and stroke. Without lifestyle changes, a person with prediabetes is at high risk of going on to develop type 2 diabetes. People with prediabetes have up to a 50 percent chance of developing type 2 diabetes over the next 5 to 10 years. So if you’ve been told you have prediabetes, this is a warning sign that you are at high risk of developing type 2 diabetes. The good news is you don’t have it yet, and by making changes to your diet, increasing physical activity and losing weight, up to 70% of cases of type 2 diabetes can be prevented or delayed in some people 10.
If you have prediabetes, losing a small amount of weight if you’re overweight and getting regular physical activity can lower your risk for developing type 2 diabetes. A small amount of weight loss means around 5% to 7% of your body weight or just 10 to 14 pounds for a 200-pound person can significantly reduce your risk. There are lots of ways you can lose weight and it’s about finding what works best for you. If you need help with managing your weight, a dietitian can help you.
Regular physical activity means getting at least 150 minutes a week of brisk walking or a similar activity. That’s just 30 minutes a day, five days a week.
Making healthier food choices and being more active are both positive ways to start making positive changes that will benefit your health.
Healthy lifestyle choices can help you prevent prediabetes and its progression to type 2 diabetes, even if diabetes runs in your family. Try to:
- Eat healthy foods. Choose foods lower in fat and calories and higher in fiber. Focus on fruits, vegetables and whole grains. Strive for variety to prevent boredom.
Get more physical activity. Aim for about 30 minutes of moderate aerobic activity on most days of the week, or at least 150 minutes of moderate aerobic activity a week. - Lose excess pounds. If you’re overweight, losing even 7% of your body weight — for example, 14 pounds (6.4 kilograms) if you weigh 200 pounds (90.7 kilograms) — can reduce the risk of diabetes. Don’t try to lose weight during pregnancy, however. Talk to your doctor about how much weight is healthy for you to gain during pregnancy. To keep your weight in a healthy range, focus on permanent changes to your eating and exercise habits. Motivate yourself by remembering the benefits of losing weight, such as a healthier heart, more energy and improved self-esteem.
- Get at least 150 minutes of moderate aerobic physical activity a week, or about 30 minutes on most days of the week.
- Control your blood pressure and cholesterol.
- Don’t smoke.
Prediabetes causes
The exact cause of prediabetes is unknown. But family history and genetics appear to play an important role. A lack of regular physical activity and being overweight with excess fat around your abdomen also seem to be important factors.
What is clear is that people with prediabetes don’t process sugar (glucose) properly anymore. As a result, sugar builds up in the blood instead of doing its normal job of giving energy to the cells that make up muscles and other tissues.
Most of the glucose in your body comes from the food you eat. When food is digested, sugar enters your bloodstream. Moving sugar from your bloodstream to your body’s cells requires a hormone called insulin.
Insulin comes from a gland located behind the stomach called the pancreas. Your pancreas sends insulin to your blood when you eat.
As insulin circulates, it allows sugar to enter your cells — and lowers the amount of sugar in your blood. When your blood sugar level starts to drop, the pancreas slows down the secretion of insulin into the blood.
When you have prediabetes, this process doesn’t work as well. Your pancreas may not make enough insulin or cells become resistant to insulin and don’t allow as much sugar in. So, instead of fueling your cells, sugar builds up in your bloodstream.
Excess weight
Experts believe obesity, especially too much fat in the abdomen and around the organs, called visceral fat, is a main cause of insulin resistance. A waist measurement of 40 inches or more for men and 35 inches or more for women is linked to insulin resistance. This is true even if your body mass index (BMI) falls within the normal range. However, research has shown that Asian Americans may have an increased risk for insulin resistance even without a high BMI.
Researchers used to think that fat tissue was only for energy storage. However, studies have shown that belly fat makes hormones and other substances that can contribute to chronic, or long-lasting, inflammation in the body. Inflammation may play a role in insulin resistance, type 2 diabetes, and cardiovascular disease.
Excess weight may lead to insulin resistance, which in turn may play a part in the development of fatty liver disease.
Physical inactivity
Not getting enough physical activity is linked to insulin resistance and prediabetes. Regular physical activity causes changes in your body that make it better able to keep your blood glucose levels in balance.
Risk factors for developing prediabetes
The same factors that increase the odds of getting type 2 diabetes also increase your risk of prediabetes.
Risk factors for developing prediabetes include:
- Being overweight or obese. Being overweight or obese is a primary risk factor for prediabetes. The more fatty tissue you have — especially inside and between the muscle and skin around your abdomen — the more resistant your cells become to insulin.
- Physically inactive. The less active you are, the greater your risk of prediabetes. Physical activity helps you control your weight, uses up sugar for energy and makes the body use insulin more effectively.
- Poor diet. Eating red meat and processed meat, and drinking sugar-sweetened beverages, is associated with a higher risk of prediabetes. A diet high in fruits, vegetables, nuts, whole grains and olive oil is associated with a lower risk of prediabetes.
- Large waist size. A large waist size can indicate insulin resistance. The risk of insulin resistance goes up for men with waists larger than 40 inches and for women with waists larger than 35 inches.
- Having a close (first degree) relative with diabetes. Your risk of prediabetes increases if you have a parent or sibling with type 2 diabetes.
- Being a woman who delivered a baby weighing more than 9 pounds or with a history of gestational diabetes. If you’ve had gestational diabetes, your doctor will likely check your blood sugar levels at least once every three years.
- Being a woman with polycystic ovary syndrome (PCOS). Women with this common condition — characterized by irregular menstrual periods, excess hair growth and obesity — have a higher risk of prediabetes.
- Being of a high-risk race or ethnicity such as African American, Latino, Native American, Asian American, Pacific Islander
- Having high blood pressure (hypertension) or taking medication for high blood pressure
- Having a low high-density lipoprotein (HDL) (“good”) cholesterol level (less than 35 mg/dL or 0.90 mmol/L and/or a high triglyceride level (more than 250 mg/dL or 2.82 mmol/L). The combination of high blood pressure, low levels of high-density lipoprotein (HDL) cholesterol and high levels of triglycerides is often called metabolic syndrome.
- Having an A1C equal to or above 5.7% or prediabetes identified by previous testing
- Having a history of cardiovascular disease
- Age. Although diabetes can develop at any age, the risk of prediabetes increases after age 45.
- People with obstructive sleep apnea — a condition that disrupts sleep repeatedly — have an increased risk of insulin resistance.
- Tobacco smoke. Smoking may increase insulin resistance. Smokers also seem to carry more weight around the middle.
The American Diabetes Association also recommends that children who are overweight and have two or more risk factors should be considered for diabetes screening. If prediabetes is detected, then yearly follow-up testing is recommended.
How do I prevent getting prediabetes?
Physical activity and losing weight may help your body respond better to insulin. Taking small steps, such as eating healthier foods and moving more to lose weight, can help reverse insulin resistance and prevent or delay type 2 diabetes in people with prediabetes.
The Diabetes Prevention Program research studies 16, 17, showed that for people at high risk of developing diabetes, losing 5 to 7 percent of their starting weight helped reduce their chance of developing the disease 17. That’s 10 to 14 pounds for someone who weighs 200 pounds. People in the study lost weight by changing their diet and being more physically active.
The Diabetes Prevention Program research studies 16, 17 also showed that taking metformin, a medicine used to treat type 2 diabetes, could delay diabetes. Metformin worked best for women with a history of gestational diabetes, younger adults, and people with obesity. Ask your doctor if metformin might be right for you.
Prediabetes symptoms
Prediabetes doesn’t have any signs or symptoms. One possible sign of prediabetes is darkened skin (a patch of velvety brown pigmentation) around your neck, armpits and groin regions called acanthosis nigricans (see Figure 3). A lot of people don’t get any symptoms when it comes to type 2 diabetes, or don’t notice them. If you start to have any of the symptoms of type 2 diabetes it means you have probably already developed it.
Classic signs and symptoms that suggest you’ve moved from prediabetes to type 2 diabetes include:
- Increased thirst
- Going to the toilet to urinate more often, especially at night
- Increased hunger
- Feeling more tired, because your body can’t get enough glucose in to your cells for energy
- Blurred vision
- Numbness or tingling in the feet or hands
- Frequent infections
- Slow-healing sores or cuts and wounds taking longer to heal
- Losing weight without trying
- Genital itching or thrush.
Prediabetes complications
People with prediabetes may already have damage to their eyes, kidneys, blood vessels, and heart. Evidence from numerous studies suggests that the chronic complications of type 2 diabetes start to develop during the prediabetic state. So by the time we have prediabetes, it may already too late to prevent organ damage, so best to prevent prediabetes in the first place, and the earlier the better.
The most serious consequence of prediabetes is progression to type 2 diabetes. That’s because type 2 diabetes can lead to:
- High blood pressure
- High cholesterol
- Heart disease
- Stroke
- Kidney disease
- Blindness
- Amputations
Research indicates that prediabetes is often associated with heart attacks and can damage your kidneys, even if you haven’t progressed to type 2 diabetes.
Prediabetes diagnosis
Screening and diagnostic tests are the same as those used for type 2 diabetes. Monitoring is not generally indicated, but the American Diabetes Association recommends that people with prediabetes be screened for the development of type 2 diabetes on a yearly basis. The American Diabetes Association also recommends that diabetes screening for most adults begin at age 35. And if you’ve had gestational diabetes, your doctor will likely check your blood sugar levels at least once every three years.
Doctors most often use the fasting plasma glucose (FPG) test or the A1C (HbA1C) test to find out if someone has prediabetes. Less often, doctors use the oral glucose tolerance test (OGTT), which is more expensive and not as easy to give.
Doctors don’t usually test for insulin resistance. The most accurate test for insulin resistance is complicated and used mostly for research.
You should be tested for prediabetes if you are overweight or have obesity and have one or more other risk factors for diabetes, or if your parents, siblings, or children have type 2 diabetes. Even if you don’t have risk factors, you should start getting tested once you reach age 45.
The following test results show prediabetes 18:
- A1C (HbA1C): 5.7 to 6.4 percent
- Fasting plasma glucose (FPG): 100 to 125 mg/dL (5.6 to 6.9 mmol/L)
- Oral glucose tolerance test (OGTT): 140 to 199 mg/dL (7.8 to 11.1 mmol/L)
If the results are normal but you have other risk factors for diabetes, you should be retested at least every 3 years (testing might occur more frequently if you have additional risk factors for diabetes) 18.
Glycated hemoglobin (A1C) test
This test shows your average blood sugar level for the past three months. The test measures the percentage of blood sugar attached to the oxygen-carrying protein in red blood cells called hemoglobin. The higher your blood sugar levels, the more hemoglobin you’ll have with sugar attached.
Glycated hemoglobin (A1C) test in general:
- An A1C level below 5.7% is considered normal
- An A1C level between 5.7% and 6.4% is considered prediabetes
- An A1C level of 6.5% or higher on two separate tests indicates type 2 diabetes
Certain conditions can make the A1C test inaccurate — such as if you’re pregnant or have an uncommon form of hemoglobin.
Fasting blood sugar test
A blood sample is taken after you fast for at least eight hours or overnight.
In general:
- A fasting blood sugar level below 100 milligrams per deciliter (mg/dL) — 5.6 millimoles per liter (mmol/L) — is considered normal.
- A fasting blood sugar level from 100 to 125 mg/dL (5.6 to 7.0 mmol/L) is considered prediabetes. This result is sometimes called impaired fasting glucose.
- A fasting blood sugar level of 126 mg/dL (7.0 mmol/L) or higher indicates type 2 diabetes.
Oral glucose tolerance test (OGTT)
This test is usually used to diagnose diabetes only during pregnancy. A blood sample is taken after you fast for at least eight hours or overnight. Then you’ll drink a sugary solution, and your blood sugar level will be measured again after two hours.
In general:
- A blood sugar level less than 140 mg/dL (7.8 mmol/L) is considered normal.
- A blood sugar level from 140 to 199 mg/dL (7.8 to 11.0 mmol/L) is considered prediabetes. This is sometimes referred to as impaired glucose tolerance.
- A blood sugar level of 200 mg/dL (11.1 mmol/L) or higher indicates type 2 diabetes.
If you have prediabetes, your doctor will typically check your blood sugar levels at least once a year.
Children and prediabetes testing
Type 2 diabetes is becoming more common in children and adolescents, likely due to the rise in childhood obesity. The American Diabetes Association recommends prediabetes testing for children who are overweight or obese and who have one or more other risk factors for type 2 diabetes.
These other risk factors include:
- Family history of type 2 diabetes.
- Race. Children who are African American, Hispanic, Native American, Asian American and Pacific Islander are at higher risk.
- Low birth weight.
- Being born to a mother who had gestational diabetes.
The ranges of blood sugar level considered normal, prediabetic and diabetic are the same for children and adults.
Children who have prediabetes should be tested annually for type 2 diabetes — or more often if the child experiences a change in weight or develops signs or symptoms of diabetes, such as increased thirst, increased urination, fatigue or blurred vision.
Prediabetes treatment
The primary focus of treatment for prediabetes and prevention of progression to type 2 diabetes is lifestyle changes. Weight loss, eating a healthy diet, and regular physical activity can help prevent or delay the development of type 2 diabetes and reduce blood glucose levels. In some cases, oral diabetes medications may also be prescribed.
Research shows that you can lower your risk for type 2 diabetes by 58% by:
- Losing 7% of your body weight (or 15 pounds if you weigh 200 pounds)
- Exercising moderately (such as brisk walking) 30 minutes a day, five days a week
Don’t worry if you can’t get to your ideal body weight. Losing even 10 to 15 pounds can make a huge difference.
To prevent prediabetes from progressing to type 2 diabetes, try to:
- Eat healthy foods. Choose foods low in fat and calories and high in fiber. Focus on fruits, vegetables and whole grains. Eat a variety of foods to help you achieve your goals without compromising taste or nutrition.
- Be more active. Aim for at least 150 minutes of moderate or 75 minutes of vigorous aerobic activity a week.
- Lose excess weight. If you’re overweight, losing just 5% to 7% of your body weight — about 14 pounds (6.4 kilograms) if you weigh 200 pounds (91 kilograms) — can reduce the risk of type 2 diabetes. To keep your weight in a healthy range, focus on permanent changes to your eating and exercise habits.
- Stop smoking. Smoking may up your risk of developing type 2 diabetes.
- Take medications as needed. If you’re at high risk of diabetes, your doctor might recommend metformin (Glumetza, others). This is usually prescribed for older adults who are obese and unable to lower blood sugar levels with lifestyle changes. Medications to control cholesterol and high blood pressure might also be prescribed.
Children prediabetes treatment
Children with prediabetes should undertake the lifestyle changes recommended for adults with type 2 diabetes, including:
- Losing weight
- Eating fewer refined carbohydrates and fats, and more fiber
- Reducing portion sizes
- Eating out less often
- Spending at least one hour every day in physical activity
Medication generally isn’t recommended for children with prediabetes unless lifestyle changes aren’t improving blood sugar levels. If medication is needed, metformin (Glumetza, others) is usually the recommended drug.
Type 1 diabetes
Type 1 diabetes which used to be called insulin dependent or juvenile diabetes, is a serious condition where your blood glucose (sugar) level is too high because your body can’t make a hormone called insulin. This happens because your body attacks the cells in your pancreas that make the insulin, meaning you can’t produce any at all. We all need insulin to live. Type 1 diabetics make very little or no insulin. Any insulin-producing beta cells they do have at the time of diagnosis are usually completely destroyed within 5 to 10 years, leaving them entirely reliant on insulin injections to live. Insulin allows the glucose in your blood to enter your cells and fuel your body. In type 1 diabetes, there’s no insulin to let glucose into the cells, so sugar builds up in your bloodstream. This can cause life-threatening complications.
When you have type 1 diabetes, your body still breaks down the carbohydrate from food and drink and turns it into glucose. But when the glucose enters your bloodstream, there’s no insulin to allow it into your body’s cells. More and more glucose then builds up in your bloodstream, leading to high blood sugar levels.
Type 1 diabetes occurs at every age and in people of every race, shape, and size. Type 1 diabetes makes up about 5% of the diabetes cases in the United States. Most cases of type 1 diabetes are diagnosed in those under the age of 30.
The exact cause of type 1 diabetes is unknown, but a family history of diabetes, viruses that injure the pancreas, and autoimmune processes, in which the body’s own immune system destroys the beta cells, are all thought to play a role. Type 1 diabetics may have more severe medical complications sooner than other diabetics. About 40% of those with type 1 diabetes will develop serious kidney problems leading to kidney failure by the age of 50.
Despite active research, type 1 diabetes has no cure. Type 1 diabetics treatment focuses on managing blood sugar levels with insulin, diet and lifestyle to prevent complications.
Type 1 diabetes causes
The exact cause of type 1 diabetes is unknown. What is known about Type 1 diabetes is that your immune system — which normally fights harmful bacteria or viruses — attacks and destroys your insulin-producing beta cells in your pancreas. This leaves you with little or no insulin. Instead of being transported into your cells, sugar builds up in your bloodstream.
Scientists think type 1 diabetes is caused by genes and environmental factors, such as viruses, that might trigger the disease, though exactly what those factors are is still unclear. Weight is not believed to be a factor in type 1 diabetes.
Risk factors for type 1 diabetes
Although the exact cause of type 1 diabetes is unknown, factors that may signal an increased risk include:
- Family history. Your risk increases if a parent or sibling has type 1 diabetes.
- Environmental factors. Circumstances such as exposure to a viral illness likely play some role in type 1 diabetes.
- The presence of damaging immune system cells (autoantibodies). Autoantibodies are antibodies (immune proteins) that mistakenly target and react with a person’s own tissues or organs. One or more autoantibodies may be produced by a person’s immune system when it fails to distinguish between “self” and “non-self.” Their presence in the blood can indicate that an autoimmune process is ongoing. Usually your immune system is able to discriminate between foreign substances (“non-self”) and your body’s own cells (“self”). Your immune system produces antibodies only when it perceives that it has been exposed to a threat (“non-self”), such as bacteria or viruses. However, when your immune system ceases to recognize one or more of your body’s normal constituents as “self,” it may produce autoantibodies that react with its own cells, tissues, and/or organs. This may cause inflammation, damage, and/or dysfunction of organs or systems, leading to signs and symptoms of autoimmune disorders such as Type 1 diabetes. Sometimes family members of people with type 1 diabetes are tested for the presence of diabetes autoantibodies. If you have these autoantibodies, you have an increased risk of developing type 1 diabetes. But not everyone who has these autoantibodies develops diabetes. About 10% of all cases of diabetes are type 1 (autoimmune) and the majority of these cases are diagnosed in people younger than 20.
- Geography. The incidence of type 1 diabetes tends to increase as you travel away from the equator. Certain countries, such as Finland and Sweden, have higher rates of type 1 diabetes.
- Genetics. The presence of certain genes indicates an increased risk of developing type 1 diabetes.
- Age. Although type 1 diabetes can appear at any age, it appears at two noticeable peaks. The first peak occurs in children between 4 and 7 years old, and the second is in children between 10 and 14 years old.
Can type 1 diabetes be reversed?
There’s no known cure for type 1 diabetes right now. But scientists are looking at new treatments called immunotherapies, which could help to prevent, stop and cure type 1 diabetes.
Type 1 diabetes prevention
There’s no known way to prevent type 1 diabetes. But researchers are working on preventing the disease or further destruction of the islet cells in people who are newly diagnosed.
Ask your doctor if you might be eligible for one of these clinical trials, but carefully weigh the risks and benefits of any treatment available in a trial.
Type 1 diabetes symptoms and signs
Signs and symptoms in type 1 diabetes often develop abruptly and the diagnosis is often made in an emergency room setting. The affected person may be seriously ill, even comatose, with very high glucose levels and high levels of ketones (ketoacidosis) and may require hospitalization.
Type 1 diabetes signs and symptoms can appear relatively suddenly and may include:
- Increased thirst
- Frequent urination
- Bed-wetting in children who previously didn’t wet the bed during the night
- Extreme hunger
- Unintended weight loss
- Irritability and other mood changes
- Fatigue and weakness
- Blurred vision.
Type 1 diabetes complications
Over time, type 1 diabetes complications can affect major organs in your body, including heart, blood vessels, nerves, eyes and kidneys. Maintaining a normal blood sugar level can dramatically reduce the risk of many complications.
Eventually, diabetes complications may be disabling or even life-threatening.
- Heart and blood vessel disease. Diabetes dramatically increases your risk of various cardiovascular problems, including coronary artery disease with chest pain (angina), heart attack, stroke, narrowing of the arteries (atherosclerosis) and high blood pressure.
- Nerve damage (diabetic neuropathy). Excess sugar can injure the walls of the tiny blood vessels (capillaries) that nourish your nerves, especially in the legs. This can cause tingling, numbness, burning or pain that usually begins at the tips of the toes or fingers and gradually spreads upward. Poorly controlled blood sugar could cause you to eventually lose all sense of feeling in the affected limbs. Damage to the nerves that affect the gastrointestinal tract can cause problems with nausea, vomiting, diarrhea or constipation. For men, erectile dysfunction may be an issue.
- Kidney damage (diabetic nephropathy). The kidneys contain millions of tiny blood vessel clusters that filter waste from your blood. Diabetes can damage this delicate filtering system. Severe damage can lead to kidney failure or irreversible end-stage kidney disease, which requires dialysis or a kidney transplant.
- Eye damage (diabetic retinopathy). Diabetes can damage the blood vessels of the retina (diabetic retinopathy), potentially causing blindness. Diabetes also increases the risk of other serious vision conditions, such as cataracts and glaucoma.
- Foot damage. Nerve damage in the feet or poor blood flow to the feet increases the risk of various foot complications. Left untreated, cuts and blisters can become serious infections that may ultimately require toe, foot or leg amputation.
- Skin and mouth conditions. Diabetes may leave you more susceptible to infections of the skin and mouth, including bacterial and fungal infections. Gum disease and dry mouth also are more likely.
- Pregnancy complications. High blood sugar levels can be dangerous for both the mother and the baby. The risk of miscarriage, stillbirth and birth defects increases when diabetes isn’t well-controlled. For the mother, diabetes increases the risk of diabetic ketoacidosis, diabetic eye problems (retinopathy), pregnancy-induced high blood pressure and preeclampsia.
Low blood sugar (hypoglycemia)
Despite your best efforts, sometimes problems will arise. Certain short-term complications of type 1 diabetes, such as hypoglycemia, require immediate care. Left untreated, low blood sugar will cause you to lose consciousness. If this occurs, you may need an emergency injection of glucagon — a hormone that stimulates the release of sugar into the blood. Be sure you always have an unexpired glucagon emergency kit available at home, at work and when you’re out. Make sure that co-workers, family and friends know how to use the kit in case you are unable to give yourself the injection.
Low blood sugar (hypoglycemia) occurs when your blood sugar level drops below your target range. Ask your doctor what’s considered a low blood sugar level for you. Blood sugar levels can drop for many reasons, including skipping a meal, eating fewer carbohydrates than called for in your meal plan, getting more physical activity than normal or injecting too much insulin.
Learn the symptoms of hypoglycemia, and test your blood sugar if you think your levels are dropping. When in doubt, always test your blood sugar. Early signs and symptoms of low blood sugar (hypoglycemia) include:
- Sweating
- Shakiness
- Hunger
- Dizziness or lightheadedness
- Rapid or irregular heart rate
- Fatigue
- Headaches
- Blurred vision
- Irritability
Later signs and symptoms of low blood sugar, which can sometimes be mistaken for alcohol intoxication in teens and adults, include:
- Lethargy
- Confusion
- Behavior changes, sometimes dramatic
- Poor coordination
- Convulsions
Nighttime hypoglycemia may cause you to wake with sweat-soaked pajamas or a headache. Due to a natural rebound effect, nighttime hypoglycemia sometimes might cause an unusually high blood sugar reading first thing in the morning, also known as Somogyi effect.
If you have a low blood sugar reading:
- Have 15 to 20 grams of a fast-acting carbohydrate, such as fruit juice, glucose tablets, hard candy, regular (not diet) soda or another source of sugar. Avoid foods with added fat, which don’t raise blood sugar as quickly because fat slows sugar absorption.
- Retest your blood sugar in about 15 minutes to make sure it’s normal.
- If it’s still low, have another 15 to 20 grams of carbohydrate and retest in another 15 minutes.
- Repeat until you get a normal reading.
- Eat a mixed food source, such as peanut butter and crackers, to help stabilize your blood sugar.
If a blood glucose meter isn’t readily available, treat for low blood sugar anyway if you have symptoms of hypoglycemia, and then test as soon as possible.
Hypoglycemia unawareness. Some people may lose the ability to sense that their blood sugar levels are getting low, called hypoglycemia unawareness. The body no longer reacts to a low blood sugar level with symptoms such as lightheadedness or headaches. The more you experience low blood sugar, the more likely you are to develop hypoglycemia unawareness. If you can avoid having a hypoglycemic episode for several weeks, you may start to become more aware of impending lows. Sometimes increasing the blood sugar target (for example, from 80 to 120 mg/dL to 100 to 140 mg/dL) at least temporarily can also help improve hypoglycemia awareness.
High blood sugar (hyperglycemia)
Your blood sugar can rise for many reasons, including eating too much, eating the wrong types of foods, not taking enough insulin or fighting an illness.
Watch for:
- Frequent urination
- Increased thirst
- Blurred vision
- Fatigue
- Irritability
- Hunger
- Difficulty concentrating
If you suspect hyperglycemia, check your blood sugar. If your blood sugar is higher than your target range, you’ll likely need to administer a “correction” — an additional dose of insulin that should bring your blood sugar back to normal. High blood sugar levels don’t come down as quickly as they go up. Ask your doctor how long to wait until you recheck. If you use an insulin pump, random high blood sugar readings may mean you need to change the pump site.
- If you have a blood sugar reading above 240 mg/dL (13.3 mmol/L), test for ketones using a urine test stick. Don’t exercise if your blood sugar level is above 240 mg/dL or if ketones are present. If only a trace or small amounts of ketones are present, drink extra fluids to flush out the ketones.
- If your blood sugar is persistently above 300 mg/dL (16.7 mmol/L), or if your urine ketones remain high despite taking appropriate correction doses of insulin, call your doctor or seek emergency care.
Increased ketones in your urine (diabetic ketoacidosis)
If your cells are starved for energy, your body may begin to break down fat — producing toxic acids known as ketones. Diabetic ketoacidosis is a life-threatening emergency.
Signs and symptoms of diabetic ketoacidosis include:
- Nausea
- Vomiting
- Abdominal pain
- A sweet, fruity smell on your breath
- Weight loss
If you suspect ketoacidosis, check your urine for excess ketones with an over-the-counter ketones test kit. If you have large amounts of ketones in your urine, call your doctor right away or seek emergency care. Also, call your doctor if you have vomited more than once and you have ketones in your urine.
Type 1 diabetes diagnosis
Diagnostic tests include:
- Glycated hemoglobin (A1C) test. This blood test indicates your average blood sugar level for the past two to three months. It measures the percentage of blood sugar attached to the oxygen-carrying protein in red blood cells (hemoglobin). The higher your blood sugar levels, the more hemoglobin you’ll have with sugar attached. An A1C level of 6.5 percent or higher on two separate tests indicates diabetes.
If the A1C test isn’t available, or if you have certain conditions that can make the A1C test inaccurate — such as pregnancy or an uncommon form of hemoglobin (hemoglobin variant) — your doctor may use these tests:
- Random blood sugar test. A blood sample will be taken at a random time and may be confirmed by repeat testing. Blood sugar values are expressed in milligrams per deciliter (mg/dL) or millimoles per liter (mmol/L). Regardless of when you last ate, a random blood sugar level of 200 mg/dL (11.1 mmol/L) or higher suggests diabetes, especially when coupled with any of the signs and symptoms of diabetes, such as frequent urination and extreme thirst.
- Fasting blood sugar test. A blood sample will be taken after an overnight fast. A fasting blood sugar level less than 100 mg/dL (5.6 mmol/L) is normal. A fasting blood sugar level from 100 to 125 mg/dL (5.6 to 6.9 mmol/L) is considered prediabetes. If it’s 126 mg/dL (7 mmol/L) or higher on two separate tests, you have diabetes.
In addition to diabetes tests listed above, a few other tests may be used in the evaluation of type 1 diabetes:
- Diabetes autoantibodies – this test may help distinguish between type 1 and type 2 diabetes if the diagnosis is unclear. The presence of one or more of these antibodies indicates type 1 diabetes.
- Five of the most common diabetes-related autoantibody tests include:
- Islet Cell Cytoplasmic Autoantibodies (ICA)
- Glutamic Acid Decarboxylase Autoantibodies (GADA)
- Insulinoma-Associated-2 Autoantibodies (IA-2A)
- Insulin Autoantibodies (IAA)
- Zinc Transporter-8 Autoantibodies (ZnT8A)
- Five of the most common diabetes-related autoantibody tests include:
- Insulin, C-peptide – to monitor insulin production
- Urine and/or blood ketone tests may be ordered to monitor people who present at the emergency room with symptoms suggesting acute hyperglycemia and to monitor those who are being treated for ketoacidosis. The presence of ketones — byproducts from the breakdown of fat — in your urine also suggests type 1 diabetes, rather than type 2. A build up of ketones can occur whenever there is a decrease in the amount or effectiveness of insulin in the body.
Table 6. Diabetes autoantibodies test results
| Test | Abbreviation | Description | Results Interpretation |
|---|---|---|---|
| Islet Cell Cytoplasmic Autoantibodies | ICA | Measures a group of islet cell autoantibodies targeted against a variety of islet cell proteins (Note: beta cells are one type of islet cell) | The presence of ICA in patients with diabetes indicates the presence of autoimmune, type 1 diabetes. ICA are present in approximately 70-80% of people with new-onset type 1 diabetes. The presence of ICA in asymptomatic individuals indicates they are at increased risk for the development of type 1 diabetes. |
| Glutamic Acid Decarboxylase Autoantibodies | GADA | Tests for autoantibodies directed against beta cell protein (antigen) but is not specific to beta cells; also known as GAD65 autoantibodies | The presence of GADA in patients with diabetes indicates the presence of autoimmune, type 1 diabetes. GADA are present in approximately 70-80% of persons with new-onset type 1 diabetes. GADA in asymptomatic individuals indicates they have increased risk for the development of type 1 diabetes. |
| Insulinoma-Associated-2 Autoantibodies | IA-2A | Tests for autoantibodies directed against beta cell antigens | The presence of IA-2A in patients with diabetes indicates the presence of autoimmune, type 1 diabetes. IA-2A are present in approximately 60% of persons with new-onset type 1 diabetes. IA-2A in asymptomatic individuals means they have increased risk for the development of type 1 diabetes. |
| Insulin Autoantibodies | IAA | Autoantibody targeted to insulin; insulin is the only antigen thought to be highly specific for beta cells. | The presence of IAA in patients with diabetes who are not insulin-treated indicates the presence of autoimmune, type 1 diabetes. It is advised that blood for IAA testing be drawn before insulin therapy is initiated. For the IAA result to be valid, the patient must not be insulin-treated for more than 14 days. IAA are present in approximately 50% of children with new-onset type 1 diabetes. IAA are uncommon in adults with type 1 diabetes. Therefore, IAA testing in adults is not advised. IAA in asymptomatic individuals indicates they have increased risk for the development of type 1 diabetes. IAA test does not distinguish between autoantibodies that target the endogenous insulin and antibodies produced against exogenous insulin. |
| Zinc Transporter-8 Autoantibodies | ZnT8A | Autoantibody targeted against a protein that pumps zinc into insulin-containing granules in beta cells | The presence of ZnT8A in people with diabetes mellitus indicates that they have diabetes that is autoimmune (i.e., type 1 diabetes). ZnT8A are present in approximately 60% of persons with new-onset type 1 diabetes. ZnT8A are also valuable in the diagnosis of latent autoimmune diabetes of adulthood (LADA). ZnT8A in asymptomatic individuals means they have increased risk for developing type 1 diabetes. The presence of ZnT8A in the blood of patients who have undergone a pancreas transplant predicts beta-cell failure. |
After the diagnosis
You’ll regularly visit your doctor to discuss diabetes management. During these visits, the doctor will check your A1C levels. Your target A1C goal may vary depending on your age and various other factors, but the American Diabetes Association generally recommends that A1C levels be below 7 percent, which translates to an estimated average glucose of 154 mg/dL (8.5 mmol/L).
Compared with repeated daily blood sugar tests, A1C testing better indicates how well your diabetes treatment plan is working. An elevated A1C level may signal the need for a change in your insulin regimen, meal plan or both.
In addition to the A1C test, the doctor will also take blood and urine samples periodically to check your cholesterol levels, thyroid function, liver function and kidney function. The doctor will also examine you to assess your blood pressure and will check the sites where you test your blood sugar and deliver insulin.
Type 1 diabetes treatment
Anyone who has type 1 diabetes needs lifelong insulin therapy. There is currently no cure for type 1 diabetes, although there has been some limited success with islet (beta) cell transplantations as a way to potentially restore insulin production.
Diabetic treatment at the time of diagnosis is somewhat different than ongoing treatment. Type 1 diabetics are sometimes diagnosed when symptoms are acute, with very high blood glucose levels, electrolytes out of balance, and in a state of diabetic ketoacidosis with some degree of dehydration affecting the function of the kidneys. In a worst case scenario, a person may have become unconscious and comatose. This is a life-threatening condition requiring immediate hospitalization and expert care to get the person’s body back to its normal balance.
Ongoing treatment of type 1 diabetes includes:
- Taking insulin
- Carbohydrate, fat and protein counting
- Frequent blood sugar monitoring
- Eating healthy foods
- Exercising regularly and maintaining a healthy weight
Ongoing treatment of type 1 diabetes revolves around daily glucose monitoring and control, eating a healthy planned diet, and exercising regularly. Regular exercise lowers blood glucose, increases the body’s sensitivity to insulin, and increases circulation.
Type 1 diabetics must self-check their glucose levels and inject themselves with insulin several times a day. The goal is to keep your blood sugar level as close to normal as possible to delay or prevent complications. Generally, the goal is to keep your daytime blood sugar levels before meals between 80 and 130 mg/dL (4.44 to 7.2 mmol/L) and your after-meal numbers no higher than 180 mg/dL (10 mmol/L) two hours after eating.
As an alternative, a number of type 1 diabetics have turned to wearing insulin pumps, programmable devices that are carried at the waist and provide small amounts of insulin (through a needle under the skin) throughout the day to more closely match normal insulin secretion The amount and type of insulin administered must be adjusted to take into account what you’re eating, the size of your meals, and the amount of activity you are getting. There are several types of insulin available; some are fast-acting and short-lived while others take longer to act but have a longer duration.
Most type 1 diabetics use a combination of insulins to meet their needs, and maintaining control can sometimes be a challenge. Stress, illnesses, and infections can alter the amount of insulin necessary, and some type 1 diabetics have “brittle” control: their glucose levels make rapid swings during the day. As another complicating factor, type 1 diabetics may develop antibodies to insulin over time; their body begins to identify the injections as an “intruder” and works to destroy the insulin, resulting in the necessity of higher doses of insulin or of switching to a different kind.
Type 1 diabetics may also “overshoot,” running into trouble with low glucose levels if they inject too much insulin, go extended periods of time without eating, or if their needs change unexpectedly. They must carry glucose with them, in the form of tablets or candy, and be ready to take some at the first signs of low blood sugar (hypoglycemia). Carrying glucagon injections (which stimulate the liver to release glucose) is also recommended for times when a person’s hypoglycemia is not responding to oral glucose or for someone else to give them if the person has become unconscious. Acute conditions, such as diabetic ketoacidosis or kidney failure, may require hospitalization to resolve.
Blood sugar monitoring
Depending on what type of insulin therapy you select or require, you may need to check and record your blood sugar level at least four times a day. The American Diabetes Association recommends testing blood sugar levels before meals and snacks, before bed, before exercising or driving, and if you suspect you have low blood sugar. Careful monitoring is the only way to make sure that your blood sugar level remains within your target range — and more frequent monitoring can lower A1C levels.
Even if you take insulin and eat on a rigid schedule, blood sugar levels can change unpredictably. You’ll learn how your blood sugar level changes in response to food, activity, illness, medications, stress, hormonal changes and alcohol.
Continuous glucose monitoring (CGM) is the newest way to monitor blood sugar levels, and may be especially helpful for preventing hypoglycemia. The devices have been shown to lower A1C.
Continuous glucose monitors attach to the body using a fine needle just under the skin that checks blood glucose level every few minutes. CGM isn’t yet considered as accurate as standard blood sugar monitoring, so at this time it’s still important to check your blood sugar levels manually.
Insulin and other medications
Types of insulin are many and include:
- Short-acting (regular) insulin
- Rapid-acting insulin
- Intermediate-acting (NPH) insulin
- Long-acting insulin
Examples of short-acting (regular) insulin include Humulin R and Novolin R. Rapid-acting insulin examples are insulin glulisine (Apidra), insulin lispro (Humalog) and insulin aspart (Novolog). Long-acting insulins include insulin glargine (Lantus, Toujeo Solostar), insulin detemir (Levemir) and insulin degludec (Tresiba). Intermediate-acting insulins include insulin NPH (Novolin N, Humulin N).
Insulin administration
Insulin can’t be taken orally to lower blood sugar because stomach enzymes will break down the insulin, preventing its action. You’ll need to receive it either through injections or an insulin pump.
- Injections. You can use a fine needle and syringe or an insulin pen to inject insulin under your skin. Insulin pens look similar to ink pens and are available in disposable or refillable varieties. If you choose injections, you’ll likely need a mixture of insulin types to use throughout the day and night. Multiple daily injections that include a combination of a long-acting insulin combined with a rapid-acting insulin more closely mimic the body’s normal use of insulin than do older insulin regimens that only required one or two shots a day. A regimen of three or more insulin injections a day has been shown to improve blood sugar levels.
- An insulin pump. You wear this device, which is about the size of a cellphone, on the outside of your body. A tube connects a reservoir of insulin to a catheter that’s inserted under the skin of your abdomen. This type of pump can be worn in a variety of ways, such as on your waistband, in your pocket or with specially designed pump belts. There’s also a wireless pump option. You wear a pod that houses the insulin reservoir on your body that has a tiny catheter that’s inserted under your skin. The insulin pod can be worn on your abdomen, lower back, or on a leg or an arm. The programming is done with a wireless device that communicates with the pod. Pumps are programmed to dispense specific amounts of rapid-acting insulin automatically. This steady dose of insulin is known as your basal rate, and it replaces whatever long-acting insulin you were using. When you eat, you program the pump with the amount of carbohydrates you’re eating and your current blood sugar, and it will give you what’s called a bolus dose of insulin to cover your meal and to correct your blood sugar if it’s elevated. Some research has found that in some people an insulin pump can be more effective at controlling blood sugar levels than injections. But many people achieve good blood sugar levels with injections, too. An insulin pump combined with a continuous glucose monitoring (CGM) device may provide even tighter blood sugar control.
Other medications
Additional medications also may be prescribed for people with type 1 diabetes, such as:
- High blood pressure medications. Your doctor may prescribe angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) to help keep your kidneys healthy. These medications are recommended for people with diabetes who have blood pressures above 140/90 millimeters of mercury (mm Hg).
- Aspirin. Your doctor may recommend you take baby or regular aspirin daily to protect your heart if your doctor feels you have an increased risk for a cardiovascular event, after discussing with you the potential risk of bleeding.
- Cholesterol-lowering drugs. Cholesterol guidelines tend to be more aggressive for people with diabetes because of the elevated risk of heart disease. The American Diabetes Association recommends that low-density lipoprotein (LDL, or “bad”) cholesterol be below 100 mg/dL (2.6 mmol/L). Your high-density lipoprotein (HDL, or “good”) cholesterol is recommended to be over 50 mg/dL (1.3 mmol/L) in women and over 40 mg/dL (1 mmol/L) in men. Triglycerides, another type of blood fat, are ideal when they’re less than 150 mg/dL (1.7 mmol/L).
Physical activity
Everyone needs regular aerobic exercise, and people who have type 1 diabetes are no exception. First, get your doctor’s OK to exercise. Then choose activities you enjoy, such as walking or swimming, and make them part of your daily routine. Aim for at least 150 minutes of aerobic exercise a week, with no more than two days without any exercise. The goal for children is at least an hour of activity a day.
Remember that physical activity lowers blood sugar. If you begin a new activity, check your blood sugar level more often than usual until you know how that activity affects your blood sugar levels. You might need to adjust your meal plan or insulin doses to compensate for the increased activity.
Potential future treatments
- Pancreas transplant. With a successful pancreas transplant, you would no longer need insulin. But pancreas transplants aren’t always successful and the procedure poses serious risks. Because these risks can be more dangerous than the diabetes itself, pancreas transplants are generally reserved for those with very difficult-to-manage diabetes, or for people who also need a kidney transplant.
- Islet cell transplantation. Researchers are experimenting with islet cell transplantation, which provides new insulin-producing cells from a donor pancreas. Although this experimental procedure had some problems in the past, new techniques and better drugs to prevent islet cell rejection may improve its future chances of becoming a successful treatment.
Artificial pancreas
In September 2016, the Food and Drug Administration (FDA) approved the first artificial pancreas for people with type 1 diabetes who are age 14 and older. A second artificial pancreas was approved in December 2019.
It’s also called closed-loop insulin delivery. The implanted device links a continuous glucose monitor, which checks blood sugar levels every five minutes, to an insulin pump. The device automatically delivers the correct amount of insulin when the monitor indicates it’s needed.
There are more artificial pancreas (closed loop) systems currently in clinical trials.
Situational concerns
Certain life circumstances call for different considerations.
- Driving. Hypoglycemia can occur at any time. It’s a good idea to check your blood sugar anytime you’re getting behind the wheel. If it’s below 70 mg/dL (3.9 mmol/L), have a snack with 15 grams of carbohydrates. Retest again in 15 minutes to make sure it has risen to a safe level.
- Working. Type 1 diabetes can pose some challenges in the workplace. For example, if you work in a job that involves driving or operating heavy machinery, hypoglycemia could pose a serious risk to you and those around you. You may need to work with your doctor and your employer to ensure that certain accommodations are made, such as additional breaks for blood sugar testing and fast access to food and drink. There are federal and state laws in place that require employers to make reasonable accommodations for people with diabetes.
- Being pregnant. Because the risk of pregnancy complications is higher for women with type 1 diabetes, experts recommend that women have a preconception evaluation and that A1C readings ideally should be less than 6.5% before they attempt to get pregnant. The risk of birth defects is increased for women with type 1 diabetes, particularly when diabetes is poorly controlled during the first six to eight weeks of pregnancy. Careful management of your diabetes during pregnancy can decrease your risk of complications.
- Being older. For those who are frail or sick or have cognitive deficits, tight control of blood sugar may not be practical and could increase the risk of hypoglycemia. For many people with type 1 diabetes, a less stringent A1C goal of less than 8% may be appropriate.
What can I eat with type 1 diabetes?
Anything, because there’s no such thing as a ‘diabetic diet’ for type 1 diabetes. It may come as a surprise, but all kinds of food are fine for people with type 1 diabetes to eat. Don’t bother with foods labelled ‘diabetic’ or ‘suitable for diabetics’. These foods contain similar amounts of calories and fat, and they can affect your blood glucose levels. They are usually more expensive and can have a laxative effect. Stick to your usual foods. If you want to have an occasional treat, go for your normal treats and watch your portion sizes. However, it’s important to center your diet on nutritious, low-fat, high-fiber foods such as:
- Fruits
- Vegetables
- Whole grains
Your dietitian will recommend that you eat fewer animal products and refined carbohydrates, such as white bread and sweets. This healthy-eating plan is recommended even for people without diabetes.
You’ll need to learn how to count the amount of carbohydrates in the foods you eat so that you can give yourself enough insulin to properly metabolize those carbohydrates. A registered dietitian can help you create a meal plan that fits your needs.
With more flexible insulin regimens and the use of insulin pumps, the days of “do’s and don’ts” are long gone. The way to go nowadays is to try and fit your diabetes treatment around your current lifestyle. But the same healthy, balanced diet is recommended for everyone, which includes food from all the main food groups.
It is a good idea to include some carbs with your meals as, without carbohydrate, your insulin may cause blood glucose levels to drop too low. Choose healthier carbs such as wholegrains, starchy foods, fruit and veg, pulses, unsweetened yogurt and milk, nut and seeds.
There is no strong evidence that a low carb diet is safe or beneficial for people with type 1 diabetes.
If you are stuck for ideas, choose one of these:
Breakfast
- a bowl of wholegrain cereal such as porridge or bran flakes, with semi-skimmed or skimmed milk. If you prefer a dairy alternative like soya or almond milk, choose one that’s unsweetened and calcium-fortified.
- egg and wholegrain toast with unsaturated spread (sunflower or olive oil)
- unsweetened yogurt and fruit
- fruity French toast
Lunch
- a sandwich made with wholegrain bread or a wrap with chicken, turkey or fish, filled with plenty of salad
- a bean or chickpea and tuna salad
- a healthy soup such as our cauliflower and leek soup, paired with wholegrain/rye crispbreads
- sesame salmon and broccoli microwave mug with a piece of fruit and an unsweetened yogurt.
Dinner
- lasagne and salad
- roast chicken with potatoes and vegetables
- Thai chicken stir fry
- fish, chips and peas
- mixed vegetable and bean curry
- chicken tortillas and salad
Healthy snacks
Sometimes, you might need to eat a small snack between meals, to help keep blood glucose levels up. Regular snacks can make it difficult to maintain a healthy weight so check with the diabetes team for specific advice that is tailored for your diabetes management.
The healthiest snack choices are unsweetened yogurts, unsalted nuts, seeds, fruits and vegetables instead of crisps, chips, biscuits and chocolates. But watch your portions still, it’ll help you keep an eye on your weight.
Your diet and insulin
If you are using a basal bolus insulin regime, injecting several times a day, or you’re on an insulin pump then it’s possible to be much more flexible in how many carbs you can eat and when.
Most people who follow this regime will count the carbohydrates that they eat and drink, and then calculate how much insulin they need to take. The amount of insulin will be adjusted depending on how much carbohydrate they are eating and other factors, such as physical activity, blood sugar levels or illness.
This can let you be more flexible with your food choices and meal times, without compromising your blood glucose control.
If you are on a twice-daily fixed insulin regimen you need to have regular meal times and eat roughly the same carbohydrate portion at these meals from day to day.
More carbohydrate than usual can cause blood glucose levels to go too high. In contrast, eating less carbs than usual can cause a hypo.
Type 2 diabetes
Type 2 diabetes also known as type 2 diabetes mellitus and used to be known as “adult-onset” diabetes or or noninsulin-dependent diabetes mellitus (NIDDM), develops when your body does not use insulin efficiently and gradually loses the ability to make enough insulin. Type 2 diabetes develops when the body does not make enough insulin or does not use insulin efficiently, so you end up with too much sugar in your blood. This long-term (chronic) condition results in too much sugar circulating in the bloodstream (also known as hyperglycemia, usually above 7 mmol/L [126 mg/dL] before a meal and above 8.5 mmol/L [153 mg/dL] two hours after a meal). The normal blood sugar level is between 4.0 mmol/L (72 mg/dL) and 5.5 mmol/L (99 mg/dL) when fasting (before meals), and less than 7.0 mmol/L [126 mg/dL] 2 hours after a meal. Eventually, high blood sugar levels can lead to serious health problems, like heart disease, kidney failure, blindness and disorders of the immune systems. People who have type 2 diabetes are also at greater risk of developing cardiovascular diseases such as heart attack, stroke or problems with circulation in their legs and feet (peripheral artery disease). These are the “macrovascular” complications of diabetes. “Macrovascular” means that these complications affect the larger blood vessels. This risk is especially high in people who also have high blood pressure. But with the right treatment and care, you can live well with type 2 diabetes and reduce your risk of developing them.
In type 2 diabetes, there are primarily two interrelated problems at work. Your pancreas does not produce enough insulin — a hormone that regulates the movement of sugar into your cells — and cells respond poorly to insulin and take in less sugar (also known as insulin resistance).
When you have type 2 diabetes, your body still breaks down carbohydrate from your food and drink and turns it into glucose. The pancreas then responds to this by releasing insulin. But because this insulin can’t work properly, your blood sugar levels keep rising. This means more insulin is released. For some people with type 2 diabetes this can eventually tire the pancreas out, meaning their body makes less and less insulin. This can lead to even higher blood sugar levels and mean you are at risk of hyperglycemia (high blood sugar level).
Type 2 diabetes is the most common type of diabetes. More than 37 million Americans have diabetes (about 1 in 10), and approximately 90-95% of them have type 2 diabetes 19. Type 2 diabetes most often develops in people over age 45, but more and more children, teens, and young adults are also developing it. More common in adults, type 2 diabetes increasingly affects children as childhood obesity increases.
When you have type 2 diabetes your body can’t get enough glucose into your cells, so a common symptom is feeling very tired. There are also other symptoms to look out for. These include feeling thirsty, going to the toilet a lot and losing weight without trying to.
There’s no cure for type 2 diabetes, but losing weight and maintaining a healthy weight, eating well and exercising can help you manage the disease. If diet and exercise aren’t enough to manage your blood sugar well, you also may need diabetes medications or insulin therapy.
The severity of diabetes can vary quite a bit. Some people only have to make minor changes to their lifestyle after they are diagnosed. Just losing a little weight and getting some more exercise may be enough for them to manage their diabetes.
It also important to note that not everyone with type 2 diabetes is overweight, but weight gain and obesity are the most important risk factors for type 2 diabetes and the reason why type 2 has become a global epidemic that affects overweight people of all ages 20.
Other people who have type 2 diabetes need more permanent therapy that involves taking tablets or insulin. It is then especially important to have a good understanding of the disease and know what they can do to stay healthy 21.
Type 2 diabetes screening. The American Diabetes Association recommends routine screening with diagnostic tests for type 2 diabetes in all adults age 45 or older and in the following groups:
- People younger than 45 who are overweight or obese and have one or more risk factors associated with diabetes
- Women who have had gestational diabetes
- People who have been diagnosed with prediabetes
- Children who are overweight or obese and who have a family history of type 2 diabetes or other risk factors
Healthy lifestyle choices can help prevent type 2 diabetes. If you’ve received a diagnosis of prediabetes, lifestyle changes may slow or stop the progression to diabetes.
A healthy lifestyle includes:
- Eating healthy foods. Choose foods lower in fat and calories and higher in fiber. Focus on fruits, vegetables and whole grains.
- Getting active. Aim for 150 or more minutes a week of moderate to vigorous aerobic activity, such as a brisk walk, bicycling, running or swimming.
- Losing weight. Losing a modest amount of weight and keeping it off can delay the progression from prediabetes to type 2 diabetes. If you have prediabetes, losing 7% to 10% of your body weight can reduce the risk of diabetes.
- Avoiding inactivity for long periods. Sitting still for long periods can increase your risk of type 2 diabetes. Try to get up every 30 minutes and move around for at least a few minutes.
If diet and exercise aren’t enough to manage your blood sugar, you may also need diabetes medications or insulin therapy.
Can type 2 diabetes be cured?
There is no cure for type 2 diabetes, but some people are able to put their diabetes into remission. This means that your blood sugar levels are healthy and you don’t need to take diabetes medication any more. Remission can be life-changing, but it’s not possible for everyone.
How to reverse type 2 diabetes?
The strongest evidence we have at the moment suggests that type 2 diabetes can be reversed or put into remission is by weight loss 22. If you have obesity or overweight, your diabetes is more likely to go into remission if you lose a substantial amount of weight – 15kg (or 2 stone 5lbs) – as quickly and safely as possible following diagnosis. Type 2 diabetes remission is when your blood sugar levels are below the diabetes range and you don’t need to take diabetes medication anymore. Remission is when your HbA1c — a measure of long-term blood glucose levels — remains below 48mmol/mol or 6.5% for at least three months, without diabetes medication 23. This definition has been agreed by a team of international experts at Diabetes UK, the American Diabetes Association and the European Association for the Study of Diabetes. Some people call this ‘reversing type 2 diabetes’, but experts use the term remission because your blood sugar levels can rise again and there’s no guarantee that your diabetes has gone forever. If your regular blood tests show your HbA1c remaining below 48 mmol/mol or 6.5%, talk to your healthcare team to discuss diabetes remission and how this applies to you. Remission is more likely if you lose weight as soon as possible after your diabetes diagnosis. However, scientists do know of people who have put their diabetes into remission 25 years after diagnosis.
There is no such thing as a special diet for people with diabetes or those aiming for diabetes reversal. There are a lot of different ways to lose weight – but there’s no one-size-fits-all diet. Some people have lost a substantial amount of weight and put their diabetes into remission through lifestyle and diet changes or by having weight loss surgery (called bariatric surgery). Scientists do know that some people have put their diabetes into remission by losing weight through following the Mediterranean diet or a low-carb diet 24, 25, 26.
It’s important to know that not everyone who loses this much weight will be able to put their diabetes into remission. But losing 15kg comes with a lot of health benefits, even if you don’t lead to remission. Research shows that getting support to lose just 5% of your body weight can have huge benefits for your health. People with obesity have an increased risk of serious health conditions, including heart attack, stroke and certain cancers. Research has shown that losing just 5% of your body weight can lead to:
- fewer medications
- better blood sugar levels
- lowering your blood pressure and cholesterol levels
- a lower risk of complications.
Scientists believe that just as storing fat around the liver and pancreas affects how type 2 diabetes develops, losing fat affects remission.
To understand how losing weight can help someone go into remission, you need to understand why obesity or overweight can lead to type 2 diabetes. If someone’s carrying extra weight around their waist, fat can build up around important organs like the liver and pancreas. This makes it more difficult for those organs to work properly, leading to type 2 diabetes.
But not everyone who develops type 2 diabetes lives with obesity or overweight. There are other factors, like age, ethnicity and family history that play a role in our risk of type 2 too. These factors influence how well the liver and pancreas work, and also where you store your fat. You can’t change those things, but you can usually change your weight.
Diabetes remission is quite a new idea. A lot of research is needed before we fully understand it. Diabetes experts don’t have enough evidence that remission is permanent. It needs to be maintained and in many cases, blood sugar levels can rise again, which is why it is so important to continue your diabetes appointments while in remission, because there’s always a chance that your diabetes might return. So, you’ll need ongoing support to keep an eye on your weight, and if it starts to creep up again, ask for extra support to adjust your eating pattern and activity levels.
You’ll also want to ensure that your HbA1c levels stay below 48 mmol/L or 6.5%.
Be sure to have regular health checks with your healthcare team at least once a year, including retinal screening. That way, your healthcare team can follow up on existing complications, pick up on new complications and give you support as soon as possible if your HbA1c levels go up again.
Who is more likely to develop type 2 diabetes?
You can develop type 2 diabetes at any age, even during childhood. However, type 2 diabetes occurs most often in middle-aged and older people. You are more likely to develop type 2 diabetes if you are age 45 or older, have a family history of diabetes, or are overweight or have obesity. Diabetes is more common in people who are African American, Hispanic/Latino, American Indian, Asian American, or Pacific Islander.
Physical inactivity and certain health problems such as high blood pressure affect your chances of developing type 2 diabetes. You are also more likely to develop type 2 diabetes if you have prediabetes or had gestational diabetes when you were pregnant.
The American Diabetes Association recommends routine screening with diagnostic tests for type 2 diabetes in all adults age 35 or older and in the following groups:
- People younger than 35 who are overweight or obese and have one or more risk factors associated with diabetes
- Women who have had gestational diabetes
- People who have been diagnosed with prediabetes
- Children who are overweight or obese and who have a family history of type 2 diabetes or other risk factors
What is the difference between type 1 and type 2 diabetes?
The main difference between the type 1 and type 2 diabetes is that type 1 diabetes is a genetic condition that often shows up early in life, and type 2 is mainly lifestyle-related and develops over time. Type 1 diabetes is an auto-immune disease where your immune system is attacking and destroying the insulin-producing cells in your pancreas. In type 1 diabetes, people produce little or no insulin, as the insulin-producing cells have been destroyed by the body’s immune system. Approximately 5-10% of the people who have diabetes have type 1 diabetes. Currently, no one knows how to prevent type 1 diabetes.
In type 2 diabetes, the body may make enough insulin early in the disease, but doesn’t respond to it effectively. As type 2 diabetes progresses, the pancreas gradually loses the ability to produce enough insulin. Type 2 diabetes is associated with inherited factors and lifestyle risk factors such as being overweight or obese, poor diet, and insufficient physical activity. Type 2 diabetes most often develops in people over age 45, but more and more children, teens, and young adults are also developing it because the increase in the number of children with obesity.
Type 1 diabetes affects 8% of everyone with diabetes. While type 2 diabetes affects about 90% of people with diabetes.
Although type 1 and type 2 diabetes both have things in common, there are lots of differences. Like what causes them, who they affect, and how you should manage them.
A big difference between the two is that type 1 diabetes isn’t affected by your lifestyle. Or your weight. That means you can’t affect your risk of developing type 1 diabetes by lifestyle changes.
It’s different for type 2 diabetes. Scientists know some things put you at more risk:
- If you’re overweight or obese. Being overweight or obese is a main risk.
- Fat distribution. Storing fat mainly in your abdomen (waist size is too large) — rather than your hips and thighs — indicates a greater risk. Your risk of type 2 diabetes rises if you’re a man with a waist circumference above 40 inches (101.6 centimeters) or a woman with a measurement above 35 inches (88.9 centimeters).
- How to measure your waist: Find the top of your hip bone and the bottom of your ribcage. In the middle of these two points is where you need to measure. For many people, the belly button is a good guide, but this might not be the case for you, so it’s best to find that midpoint between your ribcage and hip. If you’re still not sure, watch the video below.
- What is a healthy waist size? This all depends on your gender and ethnicity. For a healthy measurement you need to aim to be less than:
- 80 cm (31.5 in) for all women
- 94 cm (37 in) for most men
- 90cm (35in) for South Asian men. This is because you have a higher risk of type 2 diabetes if you are of black or South Asian background.
- Inactivity. The less active you are, the greater your risk. Physical activity helps control your weight, uses up glucose as energy and makes your cells more sensitive to insulin.
- Family history. The risk of type 2 diabetes increases if your parent, brother or sister has type 2 diabetes.
- Race and ethnicity. Although it’s unclear why, people of certain races and ethnicities — including African Caribbean, Black African, Hispanic, Native American and Asian people (Indian, Pakistani, Bangladeshi or Chinese), and Pacific Islanders — are more likely to develop type 2 diabetes than white people are.
- Blood lipid levels. An increased risk is associated with low levels of high-density lipoprotein (HDL) cholesterol — the “good” cholesterol — and high levels of triglycerides.
- Age. You’re more at risk if you’re white and over 40, or over 25 if you’re African Caribbean, Black African, or South Asian (Indian, Pakistani or Bangladeshi).
- Medical history. For example if you have a history of high blood pressure, heart attack or strokes, gestational diabetes or severe mental illness.
- Prediabetes. Prediabetes is a condition in which your blood sugar level is higher than normal, but not high enough to be classified as diabetes. Left untreated, prediabetes often progresses to type 2 diabetes.
- Pregnancy-related risks. Your risk of developing type 2 diabetes increases if you developed gestational diabetes when you were pregnant or if you gave birth to a baby weighing more than 9 pounds (4 kilograms).
- Polycystic ovary syndrome (PCOS). Having polycystic ovary syndrome — a common condition characterized by irregular menstrual periods, excess hair growth and obesity — increases the risk of diabetes.
- High blood pressure. Having blood pressure over 140/90 millimeters of mercury (mm Hg) is linked to an increased risk of type 2 diabetes.
- Abnormal cholesterol and triglyceride levels. If you have low levels of high-density lipoprotein (HDL), or “good,” cholesterol, your risk of type 2 diabetes is higher. Triglycerides are another type of fat carried in the blood. People with high levels of triglycerides have an increased risk of type 2 diabetes. Your doctor can let you know what your cholesterol and triglyceride levels are.
- Smoking. Smoking is associated with a higher risk of type 2 diabetes, and also increases the risk of other health conditions such as heart disease and cancer.
- Areas of darkened skin, usually in the armpits and neck. This condition, called acanthosis nigricans. This condition often indicates insulin resistance. Acanthosis nigricans is most common in those who are overweight, have darker skin, and have diabetes or pre-diabetic conditions. Acanthosis nigricans is not contagious. It is not harmful. Acanthosis nigricans is a warning sign of a health problem that requires medical attention.
Scientists also know that there are things you can do to reduce your risk of developing type 2 diabetes. Things like eating healthily, being active and maintaining a healthy weight can help you to prevent type 2 diabetes.
Some people still get confused between type 1 and type 2 diabetes. Below is a guide to some of the main differences between type 1 and type 2 diabetes. The main thing to remember is that both are as serious as each other. Having high blood glucose (or sugar) levels can lead to serious health complications, no matter whether you have type 1 or type 2 diabetes. So if you have either condition, you need to take the right steps to manage it.
Table 7. Type 1 and type 2 diabetes differences
| Type 1 diabetes | Type 2 diabetes | |
|---|---|---|
| What is happening? | Your body attacks the cells in your pancreas which means it cannot make any insulin. | Your body is unable to make enough insulin or the insulin you do make doesn’t work properly. |
| Risk factors | Scientists don’t currently know what causes type 1 diabetes. | Scientists know some things can put you at risk of having type 2 like weight and ethnicity. |
| Symptoms | The symptoms for type 1 appear more quickly. | Type 2 symptoms can be easier to miss because they appear more slowly. |
| Management | Type 1 is managed by taking insulin to control your blood sugar. | You can manage type 2 diabetes in more ways than type 1. These include through medication, exercise and diet. People with type 2 can also be prescribed insulin. |
| Cure and Prevention | Currently there is no cure for type 1 but research continues. | Type 2 cannot be cured but there is evidence to say in many cases it can be prevented and put into remission. If you have obesity or overweight, your type 2 diabetes is more likely to go into remission if you lose a substantial amount of weight – 15kg (or 2 stone 5lbs) – as quickly and safely as possible following diagnosis. Type 2 diabetes remission is when your blood sugar levels are below the diabetes range and you don’t need to take diabetes medication anymore. Remission is when your HbA1c — a measure of long-term blood glucose levels — remains below 48mmol/mol or 6.5% for at least three months, without diabetes medication 23. |
If I’m overweight, will I always develop type 2 diabetes?
Being overweight is a risk factor for developing diabetes, but other risk factors such as how much physical activity you get, family history, ethnicity, and age also play a role. Unfortunately, many people think that weight is the only risk factor for type 2 diabetes, but many people with type 2 diabetes are at a normal weight or only moderately overweight.
Do sugary drinks cause diabetes?
Research has also shown that drinking sugary drinks is linked to type 2 diabetes. The American Diabetes Association recommends that people avoid drinking sugar-sweetened beverages and switch to water whenever possible to help prevent type 2 diabetes.
Sugary drinks also raise blood sugar and can provide several hundred calories in just one serving. Just one 12-ounce can of regular soda has about 150 calories and 40 grams of sugar, a type of carbohydrate (carb). This is the same as 10 teaspoons of sugar.
Sugar-sweetened beverages include beverages like:
- Regular soda
- Fruit punch
- Fruit drinks
- Energy drinks
- Sports drinks
- Sweet tea
- Sweetened coffee drinks
- Other sugary drinks
Pregnancy and type 2 diabetes
Preexisting diabetes also called pregestational diabetes means you have diabetes before you get pregnant. This is different from gestational diabetes, which is a kind of diabetes that some women get during pregnancy. In the United States, about 1 to 2 percent of pregnant women have preexisting diabetes. The number of women with diabetes during pregnancy has increased in recent years. High blood sugar can be harmful to your baby during the first few weeks of pregnancy when his brain, heart, kidneys and lungs begin to form. There is a chance that some of the potential complications of diabetes, like eye disease (diabetic retinopathy) and kidney disease (diabetic nephropathy), may develop while you are pregnant. Your doctors will keep an eye on this. If you are pregnant or planning a pregnancy, visit an ophthalmologist during each trimester of your pregnancy, one year postpartum or as advised. There is also a risk of developing pre-eclampsia, a condition involving high blood pressure during pregnancy, which can cause problems for the baby.
If you have type 1 or type 2 diabetes and are planning a family, you should plan your pregnancy as much as possible. Controlling your blood sugars before conception and throughout pregnancy gives you the best chance of having a trouble-free pregnancy and birth and a healthy baby. Most women with diabetes have a healthy baby.
Having diabetes means that you and your baby are more at risk of serious health complications during pregnancy and childbirth. The good news is that by planning ahead and getting support from your doctor and diabetes team, you can really reduce the risks involved. So you’re more likely to enjoy a healthy pregnancy and give birth to a healthy baby.
If you have diabetes and your pregnancy is unplanned, there’s still plenty you can do to give your baby the best start in life.
Women with type 2 diabetes will likely need to change their treatment plans and adhere to diets that carefully controls carbohydrate intake. Many women will need insulin therapy during pregnancy and may need to discontinue other treatments, such as blood pressure medications.
Signs of trouble
Regularly monitoring your blood sugar levels is important to avoid severe complications. Also, be aware of signs and symptoms that may suggest irregular blood sugar levels and the need for immediate care:
High blood sugar (hyperglycemia). Eating certain foods or too much food, being sick, or not taking medications at the right time can cause high blood sugar. Signs and symptoms include:
- Frequent urination
- Increased thirst
- Dry mouth
- Blurred vision
- Fatigue
- Headache
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS). This life-threatening condition includes a blood sugar reading higher than 600 mg/dL (33.3 mmol/L). Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) may be more likely if you have an infection, are not taking medicines as prescribed, or take certain steroids or drugs that cause frequent urination. Signs and symptoms of hyperglycemic hyperosmolar nonketotic syndrome (HHNS) include:
- Dry mouth
- Extreme thirst
- Drowsiness
- Confusion
- Dark urine
- Seizures
Diabetic ketoacidosis. Diabetic ketoacidosis occurs when a lack of insulin results in the body breaking down fat for fuel rather than sugar. This results in a buildup of acids called ketones in the bloodstream. Triggers of diabetic ketoacidosis include certain illnesses, pregnancy, trauma and medications — including the diabetes medications called SGLT2 inhibitors.
Although diabetic ketoacidosis is usually less severe in type 2 diabetes, the toxicity of the acids can be life-threatening. In addition to the signs and symptoms of low blood sugar (hypoglycemia), such as frequent urination and increased thirst, ketoacidosis may result in:
- Nausea
- Vomiting
- Abdominal pain
- Shortness of breath
- Fruity-smelling breath
Low blood sugar (hypoglycemia). If your blood sugar level drops below your target range, it’s known as low blood sugar (hypoglycemia). Your blood sugar level can drop for many reasons, including skipping a meal, unintentionally taking more medication than usual or being more physical activity than usual. Signs and symptoms include:
- Sweating
- Shakiness
- Weakness
- Hunger
- Irritability
- Dizziness
- Headache
- Blurred vision
- Heart palpitations
- Slurred speech
- Drowsiness
- Confusion
If you have signs or symptoms of low blood sugar, drink or eat something that will quickly raise your blood sugar level — fruit juice, glucose tablets, hard candy or another source of sugar. Retest your blood in 15 minutes. If levels are not at your target, repeat the sugar intake. Eat a meal after levels return to normal.
If you lose consciousness, you will need to be given an emergency injection of glucagon, a hormone that stimulates the release of sugar into the blood.
Type 2 diabetes causes
Type 2 diabetes is primarily the result of two interrelated problems:
- Cells in muscle, fat and the liver become resistant to insulin. Because these cells don’t interact in a normal way with insulin, they don’t take in enough sugar.
- The pancreas is unable to produce enough insulin to manage blood sugar levels.
Exactly why this happens is unknown, but being overweight and inactive are key contributing factors.
Glucose (a sugar) is a main source of energy for the cells that make up muscles and other tissues. The use and regulation of glucose includes the following:
- Glucose comes from two major sources: food and your liver.
- Glucose is absorbed into the bloodstream, where it enters cells with the help of insulin.
- Your liver stores and makes glucose.
- When your glucose levels are low, such as when you haven’t eaten in a while, the liver breaks down stored glycogen into glucose to keep your glucose level within a normal range.
In type 2 diabetes, this process doesn’t work well. Instead of moving into your cells, sugar builds up in your bloodstream. As blood sugar levels increase, the insulin-producing beta cells in the pancreas release more insulin. Eventually these cells become impaired and can’t make enough insulin to meet the body’s demands.
Risk factors for developing type 2 diabetes
Some things can increase your chance of getting type 2 diabetes. Because the symptoms of type 2 diabetes are not always obvious, it’s really important to be aware of these risk factors. Factors that may increase your risk of type 2 diabetes include:
- Weight. Being overweight or obese is a main risk.
- Fat distribution. Storing fat mainly in your abdomen (waist size is too large) — rather than your hips and thighs — indicates a greater risk. Your risk of type 2 diabetes rises if you’re a man with a waist circumference above 40 inches (101.6 centimeters) or a woman with a measurement above 35 inches (88.9 centimeters).
- How to measure your waist: Find the top of your hip bone and the bottom of your ribcage. In the middle of these two points is where you need to measure. For many people, the belly button is a good guide, but this might not be the case for you, so it’s best to find that midpoint between your ribcage and hip. If you’re still not sure, watch the video below.
- What is a healthy waist size? This all depends on your gender and ethnicity. For a healthy measurement you need to aim to be less than:
- 80 cm (31.5 in) for all women
- 94 cm (37 in) for most men
- 90cm (35in) for South Asian men. This is because you have a higher risk of type 2 diabetes if you are of black or South Asian background.
- Inactivity. The less active you are, the greater your risk. Physical activity helps control your weight, uses up glucose as energy and makes your cells more sensitive to insulin.
- Family history. The risk of type 2 diabetes increases if your parent, brother or sister has type 2 diabetes.
- Race and ethnicity. Although it’s unclear why, people of certain races and ethnicities — including African Caribbean, Black African, Hispanic, Native American and Asian people (Indian, Pakistani, Bangladeshi or Chinese), and Pacific Islanders — are more likely to develop type 2 diabetes than white people are.
- Blood lipid levels. An increased risk is associated with low levels of high-density lipoprotein (HDL) cholesterol — the “good” cholesterol — and high levels of triglycerides.
- Age. You’re more at risk if you’re white and over 40, or over 25 if you’re African Caribbean, Black African, or South Asian (Indian, Pakistani or Bangladeshi).
- Medical history. For example if you have a history of high blood pressure, heart attack or strokes, gestational diabetes or severe mental illness.
- Prediabetes. Prediabetes is a condition in which your blood sugar level is higher than normal, but not high enough to be classified as diabetes. Left untreated, prediabetes often progresses to type 2 diabetes.
- Pregnancy-related risks. Your risk of developing type 2 diabetes increases if you developed gestational diabetes when you were pregnant or if you gave birth to a baby weighing more than 9 pounds (4 kilograms).
- Polycystic ovary syndrome (PCOS). Having polycystic ovary syndrome — a common condition characterized by irregular menstrual periods, excess hair growth and obesity — increases the risk of diabetes.
- Smoking. Smoking is associated with a higher risk of type 2 diabetes, and also increases the risk of other health conditions such as heart disease and cancer.
- High blood pressure. Having blood pressure over 140/90 millimeters of mercury (mm Hg) is linked to an increased risk of type 2 diabetes.
- Abnormal cholesterol and triglyceride levels. If you have low levels of high-density lipoprotein (HDL), or “good,” cholesterol, your risk of type 2 diabetes is higher. Triglycerides are another type of fat carried in the blood. People with high levels of triglycerides have an increased risk of type 2 diabetes. Your doctor can let you know what your cholesterol and triglyceride levels are.
- Areas of darkened skin, usually in the armpits and neck. This condition, called acanthosis nigricans. This condition often indicates insulin resistance. Acanthosis nigricans is most common in those who are overweight, have darker skin, and have diabetes or pre-diabetic conditions. Acanthosis nigricans is not contagious. It is not harmful. Acanthosis nigricans is a warning sign of a health problem that requires medical attention.
Type 2 diabetes symptoms and signs
Many people with type 2 diabetes do not experience any symptoms at first and it may go undiagnosed for years. In fact, you can be living with type 2 diabetes for years and not know it.
Signs and symptoms of type 2 diabetes often develop slowly. When signs and symptoms are present, they may include:
- Increased thirst or being very thirsty
- Frequent urination (passing more urine). Excess sugar building up in your bloodstream causes fluid to be pulled from the tissues. This may leave you thirsty. As a result, you may drink and urinate more than usual.
- Increased hunger. Without enough insulin to move sugar into your cells, your muscles and organs become depleted of energy. This triggers intense hunger.
- Unintended weight loss. Despite eating more than usual to relieve hunger, you may lose weight. Without the ability to metabolize glucose, the body uses alternative fuels stored in muscle and fat. Calories are lost as excess glucose is released in the urine.
- Fatigue (feeling tired). If your cells are deprived of sugar, you may become tired and irritable.
- Blurred vision. If your blood sugar is too high, fluid may be pulled from the lenses of your eyes. This may affect your ability to focus.
- Slow-healing sores or having cuts that heal slowly.
- Frequent infections. Type 2 diabetes affects your ability to heal and resist infections.
- Numbness or tingling in the hands or feet (diabetic neuropathy). Diabetic neuropathy is when diabetes causes damage to your nerves. It can affect different types of nerves in your body, including in your feet, organs and muscles.
- Areas of darkened skin, usually in the armpits and neck. Some people with type 2 diabetes have patches of dark, velvety skin in the folds and creases of their bodies — usually in the armpits and neck. This condition, called acanthosis nigricans, may be a sign of insulin resistance.
Over time, diabetes can lead to complications, which can then cause other symptoms.
Blood glucose testing is important for detecting pre-diabetes and type 2 diabetes before complications arise.
Type 2 diabetes complications
Type 2 diabetes affects many major organs, including your heart, blood vessels, nerves, eyes and kidneys. Also, factors that increase the risk of diabetes are risk factors for other serious chronic diseases. Managing diabetes and controlling your blood sugar can lower your risk for these complications or coexisting conditions (comorbidities).
Potential complications of type 2 diabetes and frequent comorbidities include:
- Heart and blood vessel disease. Diabetes is associated with an increased risk of heart disease, stroke, high blood pressure and narrowing of blood vessels (atherosclerosis).
- Nerve damage (neuropathy) in limbs. High blood sugar over time can damage or destroy nerves, resulting in tingling, numbness, burning, pain or eventual loss of feeling that usually begins at the tips of the toes or fingers and gradually spreads upward.
- Other nerve damage. Damage to nerves of the heart can contribute to irregular heart rhythms. Nerve damage in the digestive system can cause problems with nausea, vomiting, diarrhea or constipation. For men, nerve damage may cause erectile dysfunction.
- Kidney disease (diabetic nephropathy). Diabetes may lead to chronic kidney disease or irreversible end-stage kidney disease, which may require dialysis or a kidney transplant.
- Eye damage. Diabetes increases the risk of serious eye diseases, such as cataracts and glaucoma, and may damage the blood vessels of the retina, potentially leading to blindness.
- Skin conditions. Diabetes may leave you more susceptible to skin problems, including bacterial and fungal infections.
- Slow healing. Left untreated, cuts and blisters can become serious infections, which may heal poorly. Severe damage might require toe, foot or leg amputation.
- Hearing impairment. Hearing problems are more common in people with diabetes.
- Sleep apnea. Obstructive sleep apnea is common in people living with type 2 diabetes. Obesity may be the main contributing factor to both conditions. It’s not clear whether treating sleep apnea improves blood sugar control.
- Dementia. Type 2 diabetes seems to increase the risk of Alzheimer’s disease and other disorders that cause dementia. Poor control of blood sugar levels is linked to more-rapid decline in memory and other thinking skills.
Type 2 diabetes prevention
Healthy lifestyle choices can help prevent type 2 diabetes, and that’s true even if you have biological relatives living with diabetes. If you’ve received a diagnosis of prediabetes, lifestyle changes may slow or stop the progression to diabetes.
Prevention of diabetes through healthy lifestyle includes:
- Eating healthy foods. Choose foods lower in fat and calories and higher in fiber. Focus on fruits, vegetables and whole grains.
- Getting active. Aim for 150 or more minutes a week of moderate to vigorous aerobic activity, such as a brisk walk, bicycling, running or swimming.
- Losing weight. Losing a modest amount of weight and keeping it off can delay the progression from prediabetes to type 2 diabetes. If you have prediabetes, losing 7% to 10% of your body weight can reduce the risk of diabetes.
- Avoiding inactivity for long periods. Sitting still for long periods can increase your risk of type 2 diabetes. Try to get up every 30 minutes and move around for at least a few minutes.
For people with prediabetes, metformin (Fortamet, Glumetza, others), an oral diabetes medication, may be prescribed to reduce the risk of type 2 diabetes. This is usually prescribed for older adults who are obese and unable to lower blood sugar levels with lifestyle changes.
How to reduce your waist size
Unfortunately, there are no quick fixes when it comes to reducing your waist size. It comes down to eating well and moving more. Start by setting some realistic, achievable changes to suit your lifestyle. You can become more active by making small changes to your lifestyle. You can fit them around your daily life and in your budget. Here are three top tips to help make your life more active:
- Set clear goals to move more – setting goals can help you break down what you need to do and how to do it. This could be aiming to walk more, taking up a new activity or learning a new skill such as swimming or running.
- Plan ahead – we all have busy lives, so try to plan what you’re going to eat and what activity you’re going to do this week, fitting it around your social life. You can always squeeze in an activity during your lunch hour or go for walk instead of getting another form of transport.
- Start by making small changes – it’s time to put your plan into action. Start small and do something you enjoy. Doing just a little bit more each day will still make a difference. It also means you’re more likely to stick to it. Just remember, small changes to your routine won’t have such a big impact, so start small and grow.
Manage your weight
If you are living with overweight or obesity and are at high risk of type 2 diabetes, losing just 5% of your body weight can significantly reduce your risk. There are lots of ways you can lose weight and it’s about finding what works best for you.
Making healthier food choices and being more active are both positive ways to start making these changes. If you need help with managing your weight, a dietitian can help you. Your family physician may also be able to help you find weight management services in your local area.
Eat a healthy and balanced diet
There’s no one special diet for all people at high risk of developing type 2 diabetes. Everyone is individual, so there isn’t a one size fits all way of eating for everyone. But, the food and drink you have in your overall diet is linked to your risk of developing type 2 diabetes. For example, if your overall diet is made up of food and drinks that are in high fat, have a high GI (glycemic index) and low fiber content, this is linked to an increased risk of type 2 diabetes. But the good news is that by changing some of your food and drink choices, you can reduce your risk of type 2 diabetes.
All of these ways of eating have been linked with a decreased risk of type 2 diabetes:
- Mediterranean diet.
- Dietary Approaches to Stop Hypertension (DASH) diet
- Vegetarian and vegan diets
- Nordic diet
- Moderately cutting down on carbohydrates.
This is because they are made up of healthy foods like fruits, vegetables, wholegrains and lean proteins and it’s the overall balance of your diet that is important in keeping you healthy.
Additionally, there are some foods experts recommend reducing your intake of, as these have been associated with an increased risk. These foods include:
- sugar sweetened drinks
- red and processed meats
- refined carbohydrates (like sugary snacks, white bread, sugary cereals)
- potatoes (particularly French fries)
So, to reduce your risk, aim to eat more of the foods linked with a decreased risk.
Research has shown that the following foods and drinks can be associated with a decreased risk:
- total fruit and veg intake (including specifically green leafy veg, blueberries, grapes and apples)
- wholegrains
- yogurt and cheese
- unsweetened tea and coffee
Be more active
If you spend a lot of time sitting down, this is known as a sedentary lifestyle. Being sedentary is linked with an increased risk of type 2 diabetes. So being active in your daily life can help to reduce your risk of type 2 diabetes. This doesn’t mean you need to take up a new sport or join the gym. You could make small changes so that you are being more active every day. Think about taking phone calls standing up, using stairs instead of the lift, and going for a walk on your lunch break.
Type 2 diabetes diagnosis
Type 2 diabetes is usually diagnosed using the glycated hemoglobin (A1C or HbA1C) test. This blood test indicates your average blood sugar level for the past two to three months. Results are interpreted as follows:
- Below 5.7% is normal.
- 5.7% to 6.4% is diagnosed as prediabetes.
- 6.5% or higher on two separate tests indicates diabetes.
If the A1C test isn’t available, or if you have certain conditions that interfere with an A1C test, your doctor may use the following tests to diagnose diabetes:
- Random blood sugar test. Blood sugar values are expressed in milligrams of sugar per deciliter (mg/dL) or millimoles of sugar per liter (mmol/L) of blood. Regardless of when you last ate, a level of 200 mg/dL (11.1 mmol/L) or higher suggests diabetes, especially if you also have signs and symptoms of diabetes, such as frequent urination and extreme thirst.
- Fasting blood sugar test. A blood sample is taken after an overnight fast. Results are interpreted as follows:
- Less than 100 mg/dL (5.6 mmol/L) is normal.
- 100 to 125 mg/dL (5.6 to 6.9 mmol/L) is diagnosed as prediabetes.
- 126 mg/dL (7 mmol/L) or higher on two separate tests is diagnosed as diabetes.
- Oral glucose tolerance test (OGTT). This test is less commonly used than the others, except during pregnancy. You’ll need to fast overnight and then drink a sugary liquid at the doctor’s office. Blood sugar levels are tested periodically for the next two hours. Results are interpreted as follows:
- Less than 140 mg/dL (7.8 mmol/L) is normal.
- 140 to 199 mg/dL (7.8 mmol/L and 11.0 mmol/L) is diagnosed as prediabetes.
- 200 mg/dL (11.1 mmol/L) or higher after two hours suggests diabetes.
After a diagnosis
If you’re diagnosed with diabetes, your doctor or health care provider may do other tests to distinguish between type 1 and type 2 diabetes — since the two conditions often require different treatments.
Your health care provider will repeat the test A1C levels at least two times a year and when there are any changes in treatment. Target A1C goals vary depending on your age and other factors. For most people, the American Diabetes Association recommends an A1C level below 7%.
You will also receive regular diagnostic tests to screen for complications of diabetes or comorbid conditions.
Type 2 diabetes treatment
Management of type 2 diabetes includes:
- Healthy eating
- Regular exercise
- Weight loss
- Possibly, diabetes medication or insulin therapy
- Blood sugar monitoring
These steps will help keep your blood sugar level closer to normal, which can delay or prevent complications.
Healthy eating
Contrary to popular perception, there’s no specific diabetes diet. However, it’s important to center your diet around:
- A regular schedule for meals and healthy snacks
- Smaller portion sizes
- More high-fiber foods, such as fruits, nonstarchy vegetables and whole grains
- Fewer refined grains, starchy vegetables and sweets
- Modest servings of low-fat dairy, low-fat meats and fish
- Healthy cooking oils, such as olive oil or canola oil
- Fewer calories
Your health care provider may recommend seeing a registered dietitian, who can help you:
- Identify healthy choices among your food preferences
- Plan well-balanced, nutritional meals
- Develop new habits and address barriers to changing habits
- Monitor carbohydrate intake to keep your blood sugar levels more stable
Physical activity
Exercise is important for losing weight or maintaining a healthy weight. It also helps with regulating blood sugar levels. Talk to your primary health care provider before starting or changing your exercise program to ensure that activities are safe for you.
- Aerobic exercise. Choose an aerobic exercise that you enjoy, such as walking, swimming, biking or running. Adults should aim for 30 minutes or more of moderate aerobic exercise on most days of the week, or at least 150 minutes a week. Children should have 60 minutes of moderate to vigorous aerobic exercise daily.
- Resistance exercise. Resistance exercise increases your strength, balance and ability to perform activities of daily living more easily. Resistance training includes weightlifting, yoga and calisthenics. Adults living with type 2 diabetes should aim for two to three sessions of resistance exercise each week. Children should engage in activities that build strength and flexibility at least three days a week. This can include resistance exercises, sports and climbing on playground equipment.
- Limit inactivity. Breaking up long bouts of inactivity, such as sitting at the computer, can help control blood sugar levels. Take a few minutes to stand, walk around or do some light activity every 30 minutes.
Weight loss
Weight loss results in better control of blood sugar levels, cholesterol, triglycerides and blood pressure. If you’re overweight, you may begin to see improvements in these factors after losing as little as 5% of your body weight. However, the more weight you lose, the greater the benefit to your health and disease management. Your health care provider or dietitian can help you set appropriate weight-loss goals and encourage lifestyle changes to help you achieve them.
Monitoring your blood sugar
Your health care provider will advise you on how often to check your blood sugar level to make sure you remain within your target range. You may, for example, need to check it once a day and before or after exercise. If you take insulin, you may need to do this multiple times a day.
Monitoring is usually done with a small, at-home device called a blood glucose meter, which measures the amount of sugar in a drop of your blood. You should keep a record of your measurements to share with your health care team.
Continuous glucose monitoring is an electronic system that records glucose levels every few minutes from a sensor placed under your skin. Information can be transmitted to a mobile device such as your phone, and the system can send alerts when levels are too high or too low.
Dietary supplements
Research has shown the following results about popular supplements for type 2 diabetes:
- Chromium supplements have been shown to have few or no benefits. Large doses can result in kidney damage, muscular problems and skin reactions.
- Magnesium supplements have shown benefits for blood sugar control in some but not all studies. Side effects include diarrhea and cramping. Very large doses — more than 5,000 mg a day — can be fatal.
- Cinnamon, in some studies, has lowered fasting glucose levels but not A1C levels. Therefore, there’s no evidence of overall improved glucose management. Most cinnamon contains a substance called coumarin that may cause or worsen liver disease.
Talk to your doctor before starting a dietary supplement or natural remedy. Do not replace your prescribed diabetes medication with alternative medicines.
Diabetes medications
If you can’t maintain your target blood sugar level with diet and exercise, your doctor may prescribe diabetes medications that help lower insulin levels or insulin therapy. Drug treatments for type 2 diabetes include the following.
Metformin (Fortamet, Glumetza, others) is generally the first medication prescribed for type 2 diabetes. It works primarily by lowering glucose production in the liver and improving your body’s sensitivity to insulin so that your body uses insulin more effectively. Some people experience vitamin B-12 deficiency and may need to take supplements. Other possible side effects, which may improve over time, include:
- Nausea
- Abdominal pain
- Bloating
- Diarrhea
Sulfonylureas help your body secrete more insulin. Examples include glyburide (DiaBeta, Glynase), glipizide (Glucotrol) and glimepiride (Amaryl). Possible side effects include:
- Low blood sugar
- Weight gain
Glinides stimulate your pancreas to secrete more insulin. Glinides are faster acting than sulfonylureas, and the duration of their effect in the body is shorter. Examples include repaglinide and nateglinide. Possible side effects include:
- Low blood sugar
- Weight gain
Thiazolidinediones make the body’s tissues more sensitive to insulin. Examples include rosiglitazone (Avandia) and pioglitazone (Actos). Possible side effects include:
- Risk of congestive heart failure
- Risk of bladder cancer (pioglitazone)
- Risk of bone fractures
- High cholesterol (rosiglitazone)
- Weight gain
DPP-4 inhibitors help reduce blood sugar levels but tend to have a very modest effect. Examples include sitagliptin (Januvia), saxagliptin (Onglyza) and linagliptin (Tradjenta). Possible side effects include:
- Risk of pancreatitis
- Joint pain
GLP-1 receptor agonists are injectable medications that slow digestion and help lower blood sugar levels. Their use is often associated with weight loss, and some may reduce the risk of heart attack and stroke. Examples include exenatide (Byetta, Bydureon), liraglutide (Saxenda, Victoza) and semaglutide (Rybelsus, Ozempic). Possible side effects include:
- Risk of pancreatitis
- Nausea
- Vomiting
- Diarrhea
SGLT2 inhibitors affect the blood-filtering functions in your kidneys by inhibiting the return of glucose to the bloodstream. As a result, glucose is excreted in the urine. These drugs may reduce the risk of heart attack and stroke in people with a high risk of those conditions. Examples include canagliflozin (Invokana), dapagliflozin (Farxiga) and empagliflozin (Jardiance). Possible side effects include:
- Risk of amputation (canagliflozin)
- Risk of bone fractures (canagliflozin)
- Risk of gangrene
- Vaginal yeast infections
- Urinary tract infections
- Low blood pressure
- High cholesterol
Other medications your doctor might prescribe in addition to diabetes medications include blood pressure and cholesterol-lowering medications, as well as low-dose aspirin, to help prevent heart and blood vessel disease.
Insulin therapy
Some people who have type 2 diabetes need insulin therapy. You may not need to use insulin straight away but many people with type 2 diabetes need to use insulin as treatment at some point. In the past, insulin therapy was used as a last resort, but today it may be prescribed sooner if blood sugar targets aren’t met with lifestyle changes and other medications.
Some people have very high blood sugar levels when they are first diagnosed. Insulin can be used as a short-term treatment to help quickly bring down your blood sugar levels.
Some people may need to take insulin for a particular reason, like during pregnancy, a severe illness, or after surgery. But you may also need to start insulin as a treatment if other medications haven’t helped managed your blood sugar levels or aren’t appropriate for you.
Different types of insulin vary on how quickly they begin to work and how long they have an effect. Long-acting insulin, for example, is designed to work overnight or throughout the day to keep blood sugar levels stable. Short-acting insulin might be used at mealtime.
Your doctor will determine what type of insulin is appropriate for you and when you should take it. Your insulin type, dosage and schedule may change depending on how stable your blood sugar levels are. Most types of insulin are taken by injection.
Side effects of insulin include the risk of low blood sugar (hypoglycemia), diabetic ketoacidosis and high triglycerides.
When you start taking insulin, you may notice that you start to put on weight. There are lots of reasons for this, like how much insulin you take, your diet and the type of insulin you’re taking.
It’s still important to keep going to manage your diabetes with healthy lifestyle choices. Staying active and eating a healthy diet will reduce the risk of complications from your diabetes.
Weight-loss surgery (bariatric surgery)
Weight-loss surgery changes the shape and function of your digestive system. This surgery may help you lose weight and manage type 2 diabetes and other conditions related to obesity. There are various surgical procedures, but all of them help you lose weight by limiting how much food you can eat. Some procedures also limit the amount of nutrients you can absorb.
Weight-loss surgery is only one part of an overall treatment plan. Your treatment will also include diet and nutritional supplement guidelines, exercise and mental health care.
Generally, weight-loss surgery (bariatric surgery) may be an option for adults living with type 2 diabetes who have a body mass index (BMI) of 35 or higher. BMI is a formula that uses weight and height to estimate body fat. Depending on the severity of diabetes or comorbid conditions, surgery may be an option for someone with a BMI lower than 35.
Weight-loss surgery requires a lifelong commitment to lifestyle changes. Long-term side effects include nutritional deficiencies and osteoporosis.
What can I eat with type 2 diabetes?
There is no such thing as a ‘diabetic diet’ or a special diet exclusively for people with type 2 diabetes 22, 27. No two people with diabetes are the same. So there isn’t a one-size-fits-all way of eating for everyone with diabetes. In the past, people with type 2 diabetes were sent away after their diagnosis with a list of foods they weren’t allowed to eat, or often told to cut out sugar. But the best advice is to make healthier choices more often, and only have treats occasionally and in small portions. Because experts know that making healthier food choices is important to managing your diabetes and to reducing your risk of diabetes complications, like heart problems and strokes, and other health conditions including certain types of cancers.
Healthy eating centers around:
- A regular schedule for meals and healthy snacks
- Smaller portion sizes
- More high-fiber foods, such as fruits, nonstarchy vegetables and whole grains
- Fewer refined grains, starchy vegetables and sweets
- Modest servings of low-fat dairy, low-fat meats and fish
- Healthy cooking oils, such as olive oil or canola oil
- Fewer calories
Your health care provider may recommend seeing a registered dietitian, who can help you:
- Identify healthy choices among your food preferences
- Plan well-balanced, nutritional meals
- Develop new habits and address barriers to changing habits
- Monitor carbohydrate intake to keep your blood sugar levels more stable
Try and make changes to your food choices that are realistic and achievable so you’ll stick with them. This will be different for everyone, depending on what you eat now and the goals you want to achieve.
Breakfast. Here are some healthy breakfast ideas to choose from:
- a bowl of wholegrain cereal with milk
- two slices of wholegrain toast with olive oil-based spread
- a pot of natural unsweetened yogurt and fruit
- two slices of avocado with a hardboiled egg.
Lunch. Here are some healthy lunch ideas to choose from:
- a chicken or tuna salad sandwich
- a small pasta salad
- soup with or without a wholegrain roll
- a piece of salmon or tuna steak and salad.
Think about having a piece of fruit or a pot of natural unsweetened yogurt afterwards too.
Dinner. Here are some healthy dinner ideas to choose from:
- lasagne and salad
- roast chicken and vegetables, with or without potatoes
- beef stir-fry and vegetables, with or without brown rice
- chicken tortillas and salad
- salmon and vegetables, with or without noodles
- curry with chickpeas and brown rice
Mediterranean diet
The Mediterranean Diet is a way of eating rather than a formal diet plan. The Mediterranean Diet features foods eaten in more than 20 countries bordering the Mediterranean Sea including Greece, Spain, southern Italy, Portugal, Morocco, Cyprus, Croatia and France and each has their own unique culture and cuisine. In reality there is no “one” Mediterranean Diet 28, which in 2010 was recognized by UNESCO as an intangible cultural heritage of humanity. The “Mediterranean diet” encompasses all of them—it’s not one size fits all 29. Despite regional variations, common components and cultural aspects can be identified, namely olive oil as the main source of lipids, the consumption of large amounts of seasonal vegetables, fruits and aromatic herbs (some of them gathered from the wild), as well as small intakes of meat and fish, often replaced or complemented with pulses, as sources of protein.
A Mediterranean-style diet typically includes:
- plenty of fruits, vegetables, bread and other grains, potatoes, beans, nuts and seeds are eaten daily and make up the majority of food consumed;
- olive oil as a primary fat source, may account for up to 40% of daily calories; and
- small portions of cheese or yogurt are usually eaten each day, along with a serving of fish, poultry, or eggs.
Fish and poultry are more common than red meat in the Mediterranean diet. The Mediterranean diet also centers on minimally processed, plant-based foods. Wine may be consumed in low to moderate amounts, usually with meals. Fruit is a common dessert instead of sweets.
Main meals consumed daily should be a combination of three elements: cereals, vegetables and fruits, and a small quantity of legumes, beans or other (though not in every meal). Cereals in the form of bread, pasta, rice, couscous or bulgur (cracked wheat) should be consumed as one–two servings per meal, preferably using whole or partly refined grains. Vegetable consumption should amount to two or more servings per day, in raw form for at least one of the two main meals (lunch and dinner). Fruit should be considered as the primary form of dessert, with one–two servings per meal. Consuming a variety of colors of both vegetables and fruit is strongly recommended to help ensure intake of a broad range of micronutrients and phytochemicals. The less these foods are cooked, the higher the retention of vitamins and the lower use of fuel, thus minimizing environmental impact.
The Mediterranean Diet is characterized by 30:
- An abundance of plant food (fruit, vegetables, breads, cereals, potatoes, beans, nuts, and seeds);
- Minimally processed, seasonally fresh, locally grown foods;
- Desserts comprised typically of fresh fruit daily and occasional sweets containing refined sugars or honey;
- Olive oil (high in polyunsaturated fat) as the principal source of fat;
- Daily dairy products (mainly cheese and yogurt) in low to moderate amounts;
- Fish and poultry in low to moderate amounts;
- Up to four eggs weekly;
- Red meat rarely; and
- Wine in low to moderate amounts with meals.
Here are some things you can do to switch from a traditional Western-style diet to a more Mediterranean way of eating.
- Dip bread in a mix of olive oil and fresh herbs instead of using butter.
- Add avocado slices to your sandwich instead of bacon.
- Have fish for lunch or dinner instead of red meat. Brush it with olive oil, and broil or grill it.
- Sprinkle your salad with seeds or nuts instead of cheese.
- Cook with olive or canola oil instead of butter or oils that are high in saturated fat.
- Choose whole-grain bread, pasta, rice, and flour instead of foods made with white flour.
- Add ground flaxseed to cereal, low-fat yogurt, and soups.
- Cut back on meat in meals. Instead of having pasta with meat sauce, try pasta tossed with olive oil and topped with pine nuts and a sprinkle of Parmesan cheese.
- Dip raw vegetables in a vinaigrette dressing or hummus instead of dips made from mayonnaise or sour cream.
- Have a piece of fruit for dessert instead of a piece of cake.
- Use herbs and spices instead of salt to add flavor to foods.
A Mediterranean-style diet can help you achieve the American Heart Association’s recommendations for a healthy dietary pattern that:
- emphasizes vegetables, fruits, whole grains, beans and legumes;
- includes low-fat or fat-free dairy products, fish, poultry, non-tropical vegetable oils and nuts; and
- limits added sugars, sugary beverages, sodium, highly processed foods, refined carbohydrates, saturated fats, and fatty or processed meats.
This style of eating can play a big role in preventing heart disease and stroke and reducing risk factors such as obesity, diabetes, high cholesterol and high blood pressure. There is some evidence that a Mediterranean diet rich in virgin olive oil may help the body remove excess cholesterol from arteries and keep blood vessels open.
The traditional Mediterranean dietary pattern is of particular interest to healthcare providers and dietary scientists, because of observations from the 1960s that populations in countries of the Mediterranean region, such as Greece and Italy, had lower mortality from cardiovascular disease compared with northern European populations or the US, probably as a result of different eating habits.
However, adherence to the Mediterranean diet dietary pattern has been rapidly decreasing in the region since 2000, particularly in Greece, Portugal and Spain – due to the wide dissemination of the fast-food culture. These observations point to a nutrition transition period that encompasses considerable changes in diet and physical activity patterns, which may be leading to an increase in the incidence of chronic and degenerative diseases in the Mediterranean region.
Traditionally characterized by vegetables, legumes, beans, fruits, nuts, seeds, olives, lots of extra virgin olive oil, high-fiber breads and whole grains and fish, this way of eating not only involves a low consumption of processed food, processed carbohydrates, sweets, chocolate and red meat. The recommended foods are rich with monounsaturated fats, fiber, and omega-3 fatty acids.
The Mediterranean Diet is associated with a lower incidence of mortality from all-causes 31 and is also related to lower incidence of cardiovascular diseases 32, type 2 diabetes 33, certain types of cancer 34, and neurodegenerative diseases 35. The Mediterranean diet is now recognized as one of the most healthy food patterns in the world.
The Mediterranean diet is like other heart-healthy diets in that it recommends eating plenty of fruits, vegetables, and high-fiber grains. But in the Mediterranean diet, an average of 35% to 40% of calories can come from fat. Most other heart-healthy guidelines recommend getting less than 35% of your calories from fat. The fats allowed in the Mediterranean diet are mainly from unsaturated oils such as fish oils, olive oil, and certain nut or seed oils (such as canola, soybean, or flaxseed oil) and from nuts (walnuts, hazelnuts, and almonds). These types of oils may have a protective effect on the heart.
Mediterranean Diet Food List
There’s no one “Mediterranean diet food list” because there are more than 20 countries bordering the Mediterranean Sea. Diets vary between these countries and also between regions within a country. Many differences in culture, ethnic background, religion, economy and agricultural production result in different diets. But the common Mediterranean dietary meal plan (source 36) has these characteristics:
- High consumption of fruits, vegetables, bread and other cereals, potatoes, beans, nuts and seeds
- Olive oil is an important monounsaturated fat source
- Dairy products, fish and poultry are consumed in low to moderate amounts, and little red meat is eaten
- Eggs are consumed zero to four times a week
- Wine is consumed in low to moderate amounts
Mediterranean Diet Meal Plan:
- Eating a variety of fruits and vegetables each day, such as grapes, blueberries, tomatoes, broccoli, peppers, figs, olives, spinach, eggplant, beans, lentils, and chickpeas.
- Eating a variety of whole-grain foods each day, such as oats, brown rice, and whole wheat bread, pasta, and couscous.
- Choosing healthy (unsaturated) fats, such as nuts, olive oil, and certain nut or seed oils like canola, soybean, and flaxseed. About 35% to 40% of daily calories can come from fat, mainly from unsaturated fats. More than half the fat calories in a Mediterranean diet come from monounsaturated fats (mainly from olive oil). Monounsaturated fat doesn’t raise blood cholesterol levels the way saturated fat does. (source 36).
- Limiting unhealthy (saturated) fats, such as butter, palm oil, and coconut oil. And limit fats found in animal products, such as meat and dairy products made with whole milk.
- Eating mostly vegetarian meals that include whole grains, beans, lentils, and vegetables.
- Eating fish at least 2 times a week, such as tuna, salmon, mackerel, lake trout, herring, or sardines.
- Eating moderate amounts of low-fat dairy products each day or weekly, such as milk, cheese, or yogurt.
- Eating moderate amounts of poultry and eggs every 2 days or weekly.
- Limiting red meat to only a few times a month in very small amounts. For example, a serving of meat is 3 ounces. This is about the size of a deck of cards.
- Limiting sweets and desserts to only a few times a week. This includes sugar-sweetened drinks like soda.
Low-carb diet
There are many different types of low-carb diets. Eating a low-carb diet means cutting down on the amount of carbohydrates (carbs) you eat to less than 130 grams a day 37, 38. A low-carb diet focuses on foods high in protein and fat. But low-carb eating shouldn’t be no-carb eating. Some carbohydrate foods contain essential vitamins, minerals and fiber, which form an important part of a healthy diet 39.
A low-carb diet is generally used for weight loss. Some low-carb diets may have health benefits beyond weight loss, such as lowering your risk of type 2 diabetes and metabolic syndrome.
There are three macronutrients, carbohydrates (4 kcal/g), fat (9 kcal/g), and protein (4 kcal/g) found in food. Therefore, studies have defined low carbohydrate as a percent of daily macronutrient intake or total daily carbohydrate load. This article will define it as 40:
- Very low-carbohydrate (less than 10% carbohydrates) or 20 to 50 g/day
- Low-carbohydrate (less than 26% carbohydrates) or less than 130 g/day
- Moderate-carbohydrate (26% to 44%)
- High-carbohydrate (45% or greater)
For reference, the institute of medicine proposes Americans obtain 45% to 65% of calories from carbohydrates 41.
To put this into context, a medium-sized slice of bread is about 15 to 20g of carbs, which is about the same as a regular apple. On the other hand, a large jacket potato could have as much as 90g of carbs, as does one liter of orange juice.
A low-carb diet limits the amount of carbohydrates you eat. Carbs are grouped as:
- Simple natural, such as lactose in milk and fructose in fruit.
- Simple refined, such as table sugar.
- Complex natural, such as whole grains or beans.
- Complex refined, such as white flour.
Common sources of natural carbohydrates include:
- Grains.
- Fruits.
- Vegetables.
- Milk.
- Nuts.
- Seeds.
- Legumes, such as beans, lentils and peas.
In general, you digest complex carbs more slowly. Complex carbs also have less effect on blood sugar than refined carbs do. They also offer fiber.
Refined carbs such as sugar or white flour are often added to processed foods. Examples of foods with refined carbs are white breads and pasta, cookies, cake, candy, and sugar-sweetened sodas and drinks.
The body uses carbs as its main energy source. During digestion, complex carbs are broken down into simple sugars, also called glucose, and released into your blood. This is called blood glucose.
Insulin is released to help glucose enter the body’s cells, where it can be used for energy. Extra glucose is stored in the liver and in muscles. Some is changed to body fat.
A low-carb diet is meant to cause the body to burn stored fat for energy, which leads to weight loss 42, 43.
A low-carb diet isn’t for everyone. The evidence shows they can be safe and effective in helping people with type 2 diabetes manage their weight, blood glucose (sugar) levels and risk of heart disease in the short term 44. But the evidence also shows they can affect growth in children, and so should not be recommended for them. And there is little evidence to show the benefits of this type of diet in people with type 1 diabetes.
If you do decide to follow a low-carb diet, it’s important to know all the potential benefits and how to manage any potential risks.
One hypothesis of why low-carb diet produces rapid weight loss compared to other diets is that fats and protein increase the feeling of fullness (satiety) and produce less concomitant hypoglycemia. This increase in satiety and less rebound hypoglycemia reduces hunger and overall food intake and produces a caloric deficit 40. Another hypothesis contends that low-carb diets can produce a higher metabolic burn than high-carb diets. In recent studies, there appears to be a metabolic advantage of approximately 200 to 300 more calories burned compared to an iso-caloric high-carb diet 42, 45. However, these theories remain controversial 46.
Typical foods for a low-carb diet
In broad terms, a low-carb diet focuses on proteins and some nonstarchy vegetables 47. A low-carb diet generally limits grains, legumes, fruits, breads, sweets, pastas and starchy vegetables, and sometimes nuts and seeds. But some low-carb diet plans allow small amounts of fruits, vegetables and whole grains.
A daily limit of 0.7 to 2 ounces (20 to 57 grams) of carbohydrates is typical with a low-carb diet. These amounts of carbohydrates provide 80 to 240 calories. Some low-carb diets greatly limit carbs during the early phase of the diet. Then those diets allow more carbs over time.
In contrast, the Dietary Guidelines for Americans recommend that carbohydrates make up 45% to 65% of your total daily calorie intake 48. So if you eat or drink 2,000 calories a day, carbs would account for between 900 and 1,300 calories a day.
Side effects of low-carb diet
A sudden and large drop in carbs can cause short term side effects, such as:
- Constipation.
- Headache.
- Muscle cramps.
Severe carb limits can cause your body to break down fat into ketones for energy. This is called ketosis. Ketosis can cause side effects such as bad breath, headache, fatigue and weakness.
It’s not clear what kind of possible long-term health risks a low-carb diet may pose. If you limit carbs in the long term, it may cause you to have too little of some vitamins or minerals and to have digestive issues.
Some health experts think that if you eat large amounts of fat and protein from animal sources, your risk of heart disease or certain cancers may go up.
If you opt to follow a low-carb diet, think about the fats and proteins you choose. Limit foods with saturated and trans fats, such as meat and high-fat dairy products. These foods may make your risk for heart disease go up.
Type 2 diabetes food list
You may worry that having diabetes means going without foods you enjoy. The good news is that you can still eat your favorite foods, but you might need to eat smaller portions or enjoy them less often. Your health care team will help create a diabetes meal plan for you that meets your needs and likes.
The key to eating with diabetes is to eat a variety of healthy foods from all food groups, in the amounts your meal plan outlines.
The food groups are:
- Vegetables
- nonstarchy: includes broccoli, carrots, greens, peppers, and tomatoes
- starchy: includes potatoes, corn, and green peas
- Fruits—includes oranges, melon, berries, apples, bananas, and grapes
- Grains—at least half of your grains for the day should be whole grains
- includes wheat, rice, oats, cornmeal, barley, and quinoa
- examples: bread, pasta, cereal, and tortillas
- Protein
- lean meat
- chicken or turkey without the skin
- fish
- eggs
- nuts and peanuts
- dried beans and certain peas, such as chickpeas and split peas
- meat substitutes, such as tofu
- Dairy—nonfat or low fat
- milk or lactose-free milk if you have lactose intolerance
- yogurt
- cheese
- Heart-healthy fats. Eat foods with heart-healthy fats, which mainly come from these foods:
- oils that are liquid at room temperature, such as canola and olive oil
- nuts and seeds
- heart-healthy fish such as salmon, tuna, and mackerel
- avocado
Use oils when cooking food instead of butter, cream, shortening, lard, or stick margarine.
Foods and drinks to limit include:
- fried foods and other foods high in saturated fat and trans fat
- foods high in salt, also called sodium
- sweets, such as baked goods, candy, and ice cream
- beverages with added sugars, such as juice, regular soda, and regular sports or energy drinks
Drink water instead of sweetened beverages. Consider using a sugar substitute in your coffee or tea.
If you drink alcohol, drink moderately—no more than one drink a day if you’re a woman or two drinks a day if you’re a man. If you use insulin or diabetes medicines that increase the amount of insulin your body makes, alcohol can make your blood glucose level drop too low. This is especially true if you haven’t eaten in a while. It’s best to eat some food when you drink alcohol.
Can I snack in between meals?
Some people with type 2 diabetes hear about hypos (when your blood sugar gets too low) and think they need to eat snacks to avoid them. But this isn’t the case for everyone. You don’t need to eat snacks if you’re not taking any medication for your type 2 diabetes. If you treat your type 2 diabetes with medication that puts you at risk of hypos, like insulin, you may need a snack to prevent a hypo. But if you find you’re having to snack a lot to prevent hypos, talk to your healthcare team so they can give you more advice.
Snacking in general can make it harder to manage a healthy weight though, which is really important for managing your diabetes. So if you do feel like a snack, go for a healthier option like carrot sticks and hummus or some dark chocolate rice cakes.
Type 3 diabetes
Type 3 diabetes is a proposed term to describe the interlinked association between type 1 diabetes and type 2 diabetes and Alzheimer’s disease 49, 50. In 2008, researchers from Brown University, Dr Suzanne de la Monte and Dr Jack Wands 6, put forward a proposal that Alzheimer’s disease could be termed type 3 diabetes. The reasoning is based on the fact that insulin resistance within the brain was shown to be a feature of Alzheimer’s disease. While this has been proposed, major health organizations do not recognise Alzheimer’s disease as a type of diabetes within their classifications. While type 3 diabetes is not yet a medical term or a recognised condition, it is a term now used in research looking into the causes of Alzheimer’s disease.
Diabetics have up to 73% increased risk of dementia and a 100% higher risk of developing vascular dementia than non-diabetics 51, 52. The association between diabetes and dementia risk is even stronger in people with the APOE4 gene 51. Diabetes can lead to subtle cognitive decline and, in patients with mild cognitive impairment, it increases the odds of progressing to dementia 53. The side effects of diabetes can worsen confusion and cognitive impairment in people with dementia.
Type 2 diabetes and Alzheimer’s disease share certain characteristics, including impaired insulin signaling and oxidative stress 54. Because of this, research is underway to evaluate whether some specific diabetes drugs including metformin 55, liraglutide 56, exenatide 57 and pioglitazone 58 can prevent or treat dementia even in patients without diabetes 53.
Gestational diabetes
Gestational diabetes also called gestational diabetes mellitus (GDM) is a type of diabetes that some women get during pregnancy who don’t already have diabetes. Diabetes is a condition in which your body has too much sugar (also called glucose) in your blood. As gestational diabetes is a condition that occurs during pregnancy, it is not the same as having pre-existing diabetes during your pregnancy. Gestational diabetes occurs when your body can’t make enough insulin during your pregnancy. Insulin is a hormone made by your pancreas that acts like a key to let blood sugar into the cells in your body for use as energy. This leads to higher than normal levels of sugar in the blood, which can be unhealthy for both you and the baby. Typically, women with gestational diabetes have no symptoms. Your medical history and whether you have any risk factors may suggest to your doctor that you could have gestational diabetes, but you’ll need to be tested to know for sure. Most women are diagnosed after routine tests during pregnancy. Most pregnant women get tested for gestational diabetes at 24 to 28 weeks of pregnancy.
During pregnancy, your body makes more hormones and goes through other changes, such as weight gain. These changes cause your body’s cells to use insulin less effectively, a condition called insulin resistance. Insulin resistance increases your body’s need for insulin.
All pregnant women have some insulin resistance during late pregnancy. However, some women have insulin resistance even before they get pregnant. They start pregnancy with an increased need for insulin and are more likely to have gestational diabetes.
Every year, 7 out of every 100 pregnancies in the United States are affected by gestational diabetes. You’re more likely than other women to have gestational diabetes (GDM) if you’re Asian, South Asian, African-American or African Caribbean, Middle Eastern, Native American, Hispanic or Pacific Islander.
Most of the time it can be controlled and treated during pregnancy. If it’s not treated, gestational diabetes can cause problems for you and your baby.
Having gestational diabetes increases your risk of developing it again in future pregnancies. It also increases your risk of developing type 2 diabetes after giving birth or later in life.
Babies born to women with diabetes are at risk of being born larger than average, or with a birth defect. They may also be born prematurely or even stillborn. They are also at risk of becoming overweight and going on to develop type 2 diabetes as an adult.
These risks are greatly reduced if you keep your blood sugars under good control.
Managing gestational diabetes will help make sure you have a healthy pregnancy and a healthy baby. This will include eating well and keeping active.
Gestational diabetes usually goes away after you have your baby.
If not treated, gestational diabetes can cause pregnancy complications, including:
- Cesarean birth also called C-section, is a surgery in which your baby is born through a cut that your doctor makes in your belly and uterus (womb). You may need to have a c-section if you have complications during pregnancy, like your baby being very large (macrosomia). Most women with gestational diabetes can have a vaginal birth. But they’re more likely to have a c-section than women without gestational diabetes.
- High blood pressure and preeclampsia. High blood pressure (hypertension) is when the force of blood against the walls of the blood vessels is too high. It can stress your heart and cause problems during pregnancy. Preeclampsia is when a pregnant woman has high blood pressure and signs that some of her organs, like her kidneys and liver, may not be working properly. Signs of preeclampsia include having protein in the urine, changes in vision and severe headaches. High blood pressure and preeclampsia can increase your risk for premature birth.
- Macrosomia (baby being very large). This means your baby weighs more than 8 pounds, 13 ounces (4,000 grams) at birth. Weighing this much makes your baby more likely to get hurt during labor and birth. And you may need to have a c-section to keep you and your baby safe.
- Perinatal depression also called postpartum depression. This is depression that happens during pregnancy or in the first year after having a baby. Depression is a medical condition that causes feelings of sadness and a loss of interest in things you like to do. It can affect how you feel, think and act and can interfere with your daily life. It needs treatment to get better.
- Premature birth. This is birth before 37 weeks of pregnancy. Most women with gestational diabetes have a full-term pregnancy that lasts between 39 and 40 weeks. But if there are complications with your pregnancy, you may need to have your labor induced before your due date. Inducing labor means your provider gives you medicine or breaks your water (amniotic sac) to make your labor begin.
- Shoulder dystocia or other birth injuries (also called birth trauma). Shoulder dystocia happens when a baby’s shoulders get stuck inside the mother’s pelvis during labor and birth. It often happens when a baby is very large. It can cause serious injury to both mom and baby. Complications for moms caused by shoulder dystocia include postpartum hemorrhage (heavy bleeding). For babies, the most common injuries are fractures to the collarbone and arm and damage to the brachial plexus nerves. These nerves go from the spinal cord in the neck down the arm. They provide feeling and movement in the shoulder, arm and hand.
- Death. Untreated gestational diabetes can result in a baby’s death either before or shortly after birth.
- Stillbirth. This is the death of a baby in the womb after 20 weeks of pregnancy.
Gestational diabetes also can cause health complications for your baby after birth, including:
- Breathing problems, including respiratory distress syndrome (also called RDS). This is a breathing problem caused when babies don’t have enough surfactant in their lungs. Surfactant is a protein that keeps the small air sacs in the lungs from collapsing.
- Jaundice. This is a medical condition in which a baby’s eyes and skin look yellow. A baby has jaundice when his liver isn’t fully developed or isn’t working well.
- Low blood sugar (also called hypoglycemia). Sometimes babies of mothers with gestational diabetes develop low blood sugar (hypoglycemia) shortly after birth because their own insulin production is high. Prompt feedings and sometimes an intravenous glucose solution can return the baby’s blood sugar level to normal.
- Obesity later in life
- Diabetes later in life
Gestational diabetes key points:
- If untreated, gestational diabetes can cause problems for your baby, like premature birth and stillbirth.
- Women with gestational diabetes can and do have healthy pregnancies and healthy babies.
- Most pregnant women get a test for gestational diabetes at 24 to 28 weeks of pregnancy.
- Gestational diabetes usually goes away after you have your baby; but if you have it, you’re more likely to develop diabetes later in life.
- Talk to your health care provider about what you can do to reduce your risk for gestational diabetes and help prevent diabetes in the future.
If I have gestational diabetes, how can I prevent getting diabetes later in life?
For most people, gestational diabetes goes away after giving birth. But having it makes you more likely to develop type 2 diabetes later in life. Type 2 diabetes is the most common kind of diabetes.
Here’s what you can do to help reduce your risk of developing type 2 diabetes after pregnancy:
- Get tested for diabetes 4 to 12 weeks after your baby is born. If the test is normal, get tested again every 1 to 3 years.
- Get to and stay at a healthy weight.
- Talk to your provider about medicine that may help prevent type 2 diabetes.
Can gestational diabetes increase my risk for problems during pregnancy?
Yes. If not treated, gestational diabetes can increase your risk for pregnancy complications and procedures, including:
- Macrosomia. This means your baby weighs more than 8 pounds, 13 ounces (4,000 grams) at birth. Babies who weigh this much are more likely to be hurt during labor and birth, and can cause damage to his or her mother during delivery.
- Shoulder dystocia or other birth injuries (also called birth trauma). Complications for birthing parents caused by shoulder dystocia include postpartum hemorrhage (heavy bleeding). For babies, the most common injuries are fractures to the collarbone and arm and damage to the brachial plexus nerves. These nerves go from the spinal cord in the neck down the arm. They provide feeling and movement in the shoulder, arm and hand.
- High blood pressure and preeclampsia. High blood pressure (also called hypertension) is when the force of blood against the walls of the blood vessels is too high. It can stress your heart and cause problems during pregnancy. Preeclampsia is when a pregnant person has high blood pressure and signs that some of their organs, such as the kidneys and liver, may not be working properly.
- Perinatal depression. This is depression that happens during pregnancy or in the first year after having a baby (also called postpartum depression). Depression is a medical condition that causes feelings of sadness and a loss of interest in things you like to do. It can affect how you think, feel, and act and can interfere with your daily life.
- Preterm birth. This is birth before 37 weeks of pregnancy. Most women who have gestational diabetes have a full-term pregnancy that lasts between 39 and 40 weeks. However, if there are complications, your health care provider may need to induce labor before your due date. This means your provider will give you medicine or break your water (amniotic sac) to make your labor begin.
- Stillbirth. This is the death of a baby after 20 weeks of pregnancy.
- Cesarean birth also called C-section. This is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus. You may need to have a c-section if you have complications during pregnancy, or if your baby is very large (also known as macrosomia). Most people who have gestational diabetes can have a vaginal birth. But they’re more likely to have a c-section than people who don’t have gestational diabetes.
Gestational diabetes also can cause health complications for your baby after birth, including:
- Breathing problems, including respiratory distress syndrome. This can happen when babies don’t have enough surfactant in their lungs. Surfactant is a protein that keeps the small air sacs in the lungs from collapsing.
- Jaundice. This is a medical condition in which the baby’s liver isn’t fully developed or isn’t working well. A jaundiced baby’s eyes and skin look yellow.
- Low blood sugar (hypoglycemia)
- Obesity later in life
- Diabetes later in life
What causes gestational diabetes?
Scientists believe gestational diabetes, a type of diabetes that develops during pregnancy, is caused by the hormonal changes of pregnancy along with genetic and lifestyle factors.
When you are pregnant, your placenta produces hormones to help the baby grow. Pregnancy hormones you produce block the action of insulin in your body (called insulin resistance). This puts you at an increased risk of insulin resistance, and some women can’t produce enough insulin to overcome it. This makes it difficult to use glucose (sugar) properly for energy, so it stays in your blood and the sugar levels rise. This then leads to gestational diabetes.
- Insulin resistance: Hormones produced by the placenta contribute to insulin resistance, which occurs in all women during late pregnancy. Most pregnant women can produce enough insulin to overcome insulin resistance, but some cannot. Gestational diabetes occurs when the pancreas can’t make enough insulin.
- Extra weight is linked to gestational diabetes. Women who are overweight or obese may already have insulin resistance when they become pregnant. Gaining too much weight during pregnancy may also be a factor.
- Genes and family history: Having a family history of diabetes makes it more likely that a woman will develop gestational diabetes, which suggests that genes play a role. Genes may also explain why the disorder occurs more often in African Americans, American Indians, Asians, and Hispanics/Latinas.
You are at higher risk of developing gestational diabetes if you:
- are overweight or obese and not physically active or gaining too much weight in the first half of pregnancy
- are over the age of 35 years
- have a family history (parent, brother or sister) of type 2 diabetes
- come from a racial or ethnic group that has a higher prevalence of diabetes that isn’t entirely explained by race or ethnicity, such as Black, American Indian, Alaska Native, Asian, Hispanic/Latino or Pacific Islander
- have had gestational diabetes before
- have prediabetes. This means your blood glucose levels are higher than normal but not high enough to be diagnosed with diabetes.
- have had polycystic ovary syndrome (PCOS). This is a hormone problem that can affect reproductive and overall health.
- have had a large baby (macrosomia) in a past pregnancy
- are taking some types of anti-psychotic or steroid medications
- have high blood pressure or you’ve had heart disease
Risk factors for gestational diabetes
You may be more likely than other women to develop gestational diabetes if:
- You’re older than 25.
- You’re overweight or obese and not physically active.
- You had gestational diabetes or a very large baby (~ 4.5kg/10lb or more) in a previous pregnancy (baby with macrosomia in a past pregnancy).
- You have high blood pressure or you’ve had heart disease.
- You have polycystic ovarian syndrome (also called polycystic ovary syndrome or PCOS). This is a hormone imbalance that can affect a women’s reproductive and overall health.
- You have prediabetes. This means your blood glucose levels are higher than normal but not high enough to be diabetes.
- You have a family history of diabetes – a parent, brother or sister who has diabetes.
- You have a Asian, South Asian, African-American or African Caribbean, Middle Eastern, Native American, Hispanic or Pacific Islander background.
However, even women without any of these risk factors can develop gestational diabetes. This is why your health care provider tests you for gestational diabetes during pregnancy.
Gestational diabetes symptoms
Many women with gestational diabetes have no noticeable symptoms.
As some of the signs of diabetes are like symptoms experienced in pregnancy anyway – like feeling more tired or going to the toilet more – most gestational diabetes cases are diagnosed during screening for gestational diabetes. This is called a Glucose Tolerance Test, also known as an Oral Glucose Tolerance Test (OGTT).
What are complications of gestational diabetes?
Most women who have gestational diabetes deliver healthy babies. However, untreated or uncontrolled blood sugar levels can cause problems for you and your baby.
Complications in your baby can be caused by gestational diabetes, including:
- Excess growth (also known as macrosomia). Extra glucose can cross the placenta. Extra glucose triggers the baby’s pancreas to make extra insulin. This can cause your baby to grow too large. It can lead to a difficult birth and sometimes the need for a C-section.
- Low blood sugar (hypoglycemia). Sometimes babies of mothers with gestational diabetes develop low blood sugar (hypoglycemia) shortly after birth. This is because their own insulin production is high.
- Type 2 diabetes later in life. Babies of mothers who have gestational diabetes have a higher risk of developing obesity and type 2 diabetes later in life.
- Death. Untreated gestational diabetes can lead to a baby’s death either before or shortly after birth.
Complications in the mother also can be caused by gestational diabetes, including:
- Preeclampsia. Symptoms of this condition include high blood pressure, too much protein in the urine, and swelling in the legs and feet.
- Gestational diabetes. If you had gestational diabetes in one pregnancy, you’re more likely to have it again with the next pregnancy.
Gestational diabetes diagnosis
Your health care provider tests you for gestational diabetes with a prenatal test called a glucose tolerance test or an Oral Glucose Tolerance Test (OGTT). The OGTT is done when you’re between 24-28 weeks pregnant. If you’ve had gestational diabetes before, you’ll be offered the OGTT or self monitoring of your blood sugar levels at home early in your pregnancy. You’ll be shown how to do this and given a blood monitoring kit.
Taking a Glucose Tolerance Test
Your test preparation depends on whether a one-step or two-step glucose tolerance test is done. American College of Obstetricians and Gynecologists (ACOG) and the National Institutes of Health (NIH) consensus conference currently recommend the two-step approach, while the Endocrine Society recommends the one-step approach, and the American Diabetes Association (ADA) says either the one-step or two-step approach is appropriate.
- One-step 2-hour oral glucose tolerance test: you will need to fast (usually overnight) before an initial blood sample is drawn. You will then be given a 75-gram dose of glucose to drink and your blood will be drawn at 1 hour and 2 hours after the dose. Only one of the values (including the fasting glucose level) needs to be above a cutoff value for diagnosis of diabetes to be made.
- Two-step oral glucose tolerance test:
- Glucose challenge test: you do not need to fast. You will be given a 50-gram glucose dose to drink and your blood is drawn after 1 hour.
- If the challenge test is abnormal, a 3-hour oral glucose tolerance test will be performed. You will need to fast before an initial blood sample is drawn. Then you will be given a 100-gram glucose dose and your blood drawn at 1 hour, 2 hours, and 3 hours after the dose. If at least 2 of the glucose levels at fasting, 1 hour, 2 hours, or 3 hours are above a certain level, then a diagnosis of gestational diabetes is made.
What does the Glucose Tolerance Test result mean?
The following tables summarize the meaning of gestational diabetes glucose tolerance testing results.
Table 8. Gestational Diabetes One-Step Approach test results
| Time of sample collection | Glucose level |
|---|---|
| Fasting | Equal to or greater than 92 mg/dL (5.1 mmol/L) |
| 1 hour | Equal to or greater than 180 mg/dL (10.0 mmol/L) |
| 2 hour | Equal to or greater than 153 mg/dL (8.5 mmol/L) |
Footnote: Samples drawn fasting and then 1 hour and 2 hours after a 75-gram glucose drink. Diagnosis of gestational diabetes is made when any of the values meet or exceed the limit.
Table 9. Gestational Diabetes Two-Step Approach: Step One (Glucose Challenge Screen) test results
| Glucose Level | Interpretation |
|---|---|
| Less than 140* mg/dL (7.8 mmol/L) | Normal screen |
| 140* mg/dL (7.8 mmol/L) or greater | Abnormal, needs OGTT (see Step Two below) |
Footnote: Sample drawn 1 hour after a 50-gram glucose drink. *Some experts recommend a cutoff of 130 mg/dL (7.2 mmol/L) because that identifies 90% of women with gestational diabetes, compared to 80% identified using the threshold of 140 mg/dL (7.8 mmol/L). The American College of Obstetricians and Gynecologists (ACOG) recommends a lower threshold of 135 mg/dL (7.5 mmol/L) in high-risk ethnic groups with higher prevalence of gestational diabetes.
Table 10. Gestational Diabetes Two-Step Approach: Step Two (Diagnostic OGTT) test results
| Time of sample collection | Target levels** |
|---|---|
| Fasting (prior to glucose load) | 95 mg/dL (5.3 mmol/L) |
| 1 hour after glucose load | 180 mg/dL (10.0 mmol/L) |
| 2 hours after glucose load | 155 mg/dL (8.6 mmol/L) |
| 3 hours after glucose load | 140 mg/dL (7.8 mmol/L) |
Footnote: **Some labs may use different numbers. Samples drawn at fasting and then 1, 2 and 3 hours after a 100-gram glucose drink. If two or more values meet or exceed the target level, gestational diabetes is diagnosed.
Gestational diabetes treatment
If you have gestational diabetes, your prenatal care provider wants to see you more often at prenatal care checkups so she can monitor you and your baby closely to help prevent problems. At each checkup, you get tests to make sure you and your baby are doing well. Tests include a nonstress test and a biophysical profile. The nonstress test checks your baby’s heart rate. The biophysical profile is a nonstress test with an ultrasound. An ultrasound uses sound waves and a computer screen to show a picture of your baby in the womb.
Your prenatal care provider also may ask you to do kick counts (also called fetal movement counts). This is way for you to keep track of how often your baby moves in the womb. Here are two ways to do kick counts:
- Every day, time how long it takes for your baby to move ten times. If it takes longer than 2 hours, tell your prenatal care provider.
- See how many movements you feel in 1 hour. Do this three times each week. If the number changes, tell your prenatal care provider.
If you have gestational diabetes, your prenatal care provider tells you how often to check your blood sugar, what your levels should be and how to manage them during pregnancy. Blood sugar is affected by pregnancy, what you eat and drink, how much physical activity you get. You may need to eat differently and be more active.
For many women with gestational diabetes, eating a healthy diet that is high in fiber and low in carbohydrates and getting regular exercise may be enough to lower blood glucose levels. However, some women may need to take insulin shots and/or a diabetes medication called metformin.
Treatment for gestational diabetes can help reduce your risk for pregnancy complications. Your prenatal care provider begins treatment with monitoring your blood sugar levels, healthy eating and physical activity. If this doesn’t do enough to control your blood sugar, you may need medicine. Insulin is the most common medicine for gestational diabetes. It’s safe to take during pregnancy.
Here’s what you can do to help manage gestational diabetes:
- Go to all your prenatal care checkups, even if you’re feeling fine.
- Follow your prenatal care provider’s directions about how often to check your blood sugar. Your prenatal care provider shows you how to check your blood sugar on your own. She tells you how often to check it and what to do if it’s too high. Keep a log that includes your blood sugar level every time you check it. Share the log with your prenatal care provider at each checkup. Most women can check their blood sugar four times each day: once after fasting (first thing in the morning before you’ve eaten) and again after each meal.
- Eat healthy foods. Eat three regular meals and two to three snacks each day. Have one of the snacks at night. Talk to your prenatal care provider about the right kinds of foods to eat to help control your blood sugar.
- Do something active every day. Try to get 30 minutes of moderate-intensity activity at least 5 days each week. Talk to your prenatal care provider about activities that are safe during pregnancy, like walking. Walk for 10 to 15 minutes after each meal to help control your blood sugar.
- If you take medicine for diabetes, take it exactly as your prenatal care provider tells you to. If you take insulin, your prenatal care provider teaches you how to give yourself insulin shots. Tell your prenatal care provider about any medicine you take, even medicine that’s not related to gestational diabetes. Some medicines can be harmful during pregnancy, so your prenatal care provider may need to change them to ones that are safer for you and your baby. Don’t start or stop taking any medicine during pregnancy without talking to your prenatal care provider first.
- Check your weight gain during pregnancy. Gaining too much weight or gaining weight too fast can make it harder to manage your blood sugar. Talk to your prenatal care provider about the right amount of weight to gain during pregnancy.
Gestational diabetes diet
If you are diagnosed with gestational diabetes you should be referred to a dietitian for individual advice. If this has not happened ask your maternity care team to refer you.
Understanding your diet and eating healthily is an important part of your treatment for gestational diabetes. It will help you keep your blood sugar levels in the safe range so you’re more likely to enjoy a healthy pregnancy and give birth to a healthy baby.
These healthy eating tips for women with gestational diabetes are general. Your care team should talk to you about making changes to your diet and refer you to a dietitian for individual advice that’s right for you.
1. Choose healthier carbohydrates (carbs)
All carbs or carbohydrates affect your blood sugar levels, so you need to know which foods contain carbs. The type and amount of carbs you eat or drink makes a difference to your blood sugar levels. The amount makes the biggest difference. And your dietitian may talk to you about reducing your carb portion sizes. It’s important too, to choose healthier carbs.
Easy swaps for healthier carbs:
- Swap white bread for multigrain, wholegrain, wholemeal, rye, linseed or pumpernickel.
- Swap chapatti and roti made with white flour to those made with wholemeal flour.
- Swap white pittas for brown pittas.
- Swap chips and mash for wholemeal pasta, baked plantain or sweet potato.
- Swap white rice for brown rice.
- Swap cereals like Cornflakes and Rice Krispies for Weetabix, Branflakes, Shredded Wheat (or supermarket brand ones) or porridge
You can check food labels when you’re looking for foods high in fiber if you’re unsure.
2. Cut down on sugar
Cutting down sugar can be really hard at the beginning, so small practical swaps are a good starting point.
Easy ways to cut down on excess sugar:
- Swap sugary drinks, energy drinks and fruit juices with water, plain skimmed or semi-skimmed milk, or decaffeinated tea and coffee.
- Try low or zero-calorie sweeteners, also known as artificial sweeteners, instead of using sugar.
- Have fewer foods like cakes, chocolates, ice cream and biscuits.
- Know the other names for sugar on the food label. These are sucrose, glucose, dextrose, fructose, lactose, maltose, honey, invert sugar, syrup, corn sweetener and molasses.
3. Perfect your portion sizes
It isn’t always easy to get portion sizes right, and it can make managing your weight and blood glucose levels more difficult. Using everyday items and household utensils to get your portion sizes right can be really useful. It’s an easy way to visualize what a portion should look like.
However, everybody’s needs are different so the number of portion sizes you need is individual – and your weight, pregnancy, body composition and activity levels all make a difference. Your dietitian will be able to advise you on the amount of portions that are right for you.
Top tips for managing portion sizes:
- Use smaller plates and bowls to help make your portion sizes look bigger.
- Weigh food if you find it hard to gauge portion sizes. Foods like muesli, pasta and rice can be difficult to get right at first, so try using the same container to measure out certain foods.
- Be mindful of what you’re eating. It takes about 20 minutes before your brain registers that you’re full, so eat slowly, putting your knife and fork down in between mouthfuls.
Starchy food
Starchy food includes rice, pasta, bread and chapattis for energy. Choose wholegrain where possible.
One portion is:
- Cooked rice = 2 heaped tablespoons
- Half a jacket potato = 1 computer mouse
- Breakfast cereal = 3 tablespoons
- Boiled pasta or cooked noodles = 3 heaped tablespoons
Dairy food
Includes milk, cheese and yogurt for calcium, which is essential for strong bones and teeth.
One portion is:
- Semi or skimmed milk = one medium glass (200ml or 1/3 pint)
- Hard cheese = small matchbox (30g)
- Reduced or low-fat cream cheese = two small matchboxes (60g)
- Low-sugar, low-fat fromage frais/yogurt = 125g pot
Meat, fish, eggs, pulses, beans and nuts
These foods are high in protein, essential to build and replace muscle.
One portion is:
- Cooked lean meat (e.g., chicken, beef or pork) = deck of playing cards (60–90g)
- Beans and pulses (e.g., red kidney beans, butter beans, chickpeas or lentils) = 4 tablespoons
- Nuts or peanut butter (unsalted) = golf ball (2 level tablespoons)
- Quorn, tofu or soya = snooker ball (120g)
Fruits
Fruits provide you with important vitamins, minerals and fiber that help protect you against stroke, high blood pressure, heart disease and certain cancers.
One portion is:
- One handful of grapes
- One small glass (150ml) of fruit juice (limit to one portion a day)
- Two small satsumas, clementines or tangerines
- Two medium plums
- Two tinned pineapple rings or 12 chunks in natural juice
- One heaped tbsp raisins, sultanas, currants or dried cranberries
- Seven strawberries
Vegetables
An important source of fiber, minerals and vitamins, and an important part of any five-a-day plan.
One portion is:
- Three heaped tablespoons cooked veg (e.g., carrots, peas, sweetcorn, mixed veg)
- One medium onion
- One large sweet potato
- Two broccoli spears
- One heaped tablespoon tomato purée
- One piece of cucumber (5cm)
- Four large mushrooms or 14 button mushrooms
- Three heaped tablespoons beans or pulses (e.g., kidney beans, chickpeas or lentils)
Foods high in fat and sugar
You can enjoy foods from this group as an occasional treat, but they will add extra calories so it’s best to keep them to a minimum, especially if you are trying to lose weight. However, evidence suggests that pregnancy isn’t the time to be on a really strict diet and you shouldn’t aim to lose weight. But it’s important that your weight is monitored by your care team and you don’t gain too much weight, which could cause problems for you and your baby.
One portion is:
- Butter/margarine = one dice (5g)
- Low fat spread = two dice (10g)
- Unsaturated oil (e.g., sunflower, rapeseed, olive oil) = 1 teaspoon
- Chocolate = one fun size bar
4. Plan for snack attacks
If you do need to snack when you have gestational diabetes, swap cake, biscuits, crisps and chocolate for:
- plain or low sugar yogurt
- unsalted nuts
- seeds, fruit and veg
But watch your portion sizes still – it’ll help you keep an eye on your weight.
5. Avoid diabetic foods
The law has changed and manufacturers are no longer allowed to label food as diabetic or suitable for diabetics. They don’t have any special health benefits, they’re expensive, could still affect your blood sugar and may cause an upset stomach.
6. Understand the glycemic index
The gylcemic index (GI) is a measure of how quickly foods containing carbs affect your blood sugar levels after you eat them. Some foods affect sugars levels quickly and so have a high gylcemic index and others take longer to affect blood sugar levels and so have a low gylcemic index. To help you manage your blood sugar levels, go for carbs with a lower GI. You’ll still need to think about your portion sizes. It’s the amount of carbs in the meal that will affect your blood sugar levels the most. And not all low gylcemic index foods are healthy, so make sure you read food labels and make a healthy choice.
7. Manage your weight
If you gain too much weight in pregnancy it can affect your health and increase your blood pressure. However, evidence suggests that pregnancy isn’t the time to be on a really strict diet and you shouldn’t aim to lose weight. But it’s important that your weight is monitored by your care team and you don’t gain too much weight, which could cause problems for you and your baby.
Making changes to your diet and physical activity levels can help you avoid gaining too much weight. It’ll also help you to keep your blood sugar within a safe range.
It’s important to keep going with your healthier lifestyle after you’ve had your baby and keep to a healthy weight. This will reduce your risk of developing gestational diabetes in future pregnancies. And, it will also help to reduce your future risk of developing type 2 diabetes too.
8. Eat more fish
Try to eat fish regularly, as it’s good for you and the development of your baby. The advice is to eat at least two portions a week, including at least one portion of oily fish – like mackerel, sardines, salmon, herrings, trout or pilchards. Oily fish is really good for heart health, but don’t have more than two portions a week because it contains low levels of pollutants (toxins). A portion is about 140g.
Avoid fish which tend to have higher levels of mercury, like swordfish, shark and marlin. And, don’t have more than four medium-sized cans of tuna, or two tuna steaks a week, as it can have relatively high amounts of mercury compared to other fish.
Exercise
Moderate intensity physical activity — physical activity that raises your breathing or heart rate — can help you manage your blood glucose levels and reduces insulin resistance.
The best form of exercise if you have gestational diabetes is to build walking into your daily routine. Always check with your doctor first before you start exercising while you are pregnant.
Medication
If your blood sugar levels remain high despite changes to your diet and an exercise regime, you may need medication to lower your blood sugar levels.
Both insulin injections and metformin pills have been shown to be safe for the unborn baby. If you already have diabetes when you become pregnant, discuss with your doctor whether you will need to change any of your medicines.
If you are worried about taking medicines while you are pregnant, discuss the risks with your doctor. Remember, the risks of not treating your gestational diabetes could be much higher for both you and your baby.
How can I help prevent getting diabetes later in life?
For most women, gestational diabetes goes away after giving birth. But having gestational diabetes makes you more likely to develop type 2 diabetes later in life. Type 2 diabetes is the most common kind of diabetes. If you have type 2 diabetes, your pancreas makes too little insulin or your body becomes resistant to it (can’t use it normally).
Here’s what you can do to help reduce your risk of developing type 2 diabetes after pregnancy:
- Breastfeed. Breastfeeding is one of the ways you can help reduce your risk of developing type 2 diabetes after giving birth. Breastfeeding can help you lose weight after pregnancy. Being overweight makes you more likely to develop type 2 diabetes.
- Get tested for diabetes 4 to 12 weeks after your baby is born. If the test is normal, get tested again every 1 to 3 years.
- Get to and stay at a healthy weight.
- Talk to your family physician about medicine that may help prevent type 2 diabetes.
- Freeman AM, Pennings N. Insulin Resistance. [Updated 2021 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507839[↩][↩]
- Bothou C, Beuschlein F, Spyroglou A. Links between aldosterone excess and metabolic complications: A comprehensive review. Diabetes Metab. 2020 Feb;46(1):1-7. doi: 10.1016/j.diabet.2019.02.003[↩]
- Muniyappa R, Madan R, Varghese RT. Assessing Insulin Sensitivity and Resistance in Humans. [Updated 2021 Aug 9]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK278954[↩]
- Pop-Busui R, Boulton AJ, Feldman EL, et al. Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care. 2017;40(1):136–154.[↩]
- Izenberg A, Perkins BA, Bril V. Diabetic neuropathies. Seminars in Neurology. 2015;35(4):424–430.[↩]
- de la Monte, S. M., & Wands, J. R. (2008). Alzheimer’s disease is type 3 diabetes-evidence reviewed. Journal of diabetes science and technology, 2(6), 1101–1113. https://doi.org/10.1177/193229680800200619[↩][↩]
- What is prediabetes? https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance#prediabetes[↩]
- Blood Sugar Level Ranges. https://www.diabetes.co.uk/diabetes_care/blood-sugar-level-ranges.html[↩][↩]
- Diabetes Diagnosis. https://diabetes.org/diabetes/a1c/diagnosis[↩][↩]
- Alvarez S, Coffey R, Algotar AM. Prediabetes. [Updated 2022 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459332[↩][↩][↩][↩][↩]
- Horstman C, Aronne L, Wing R, Ryan DH, Johnson WD. Implementing an Online Weight-Management Intervention to an Employee Population: Initial Experience with Real Appeal. Obesity (Silver Spring). 2018 Nov;26(11):1704-1708. doi: 10.1002/oby.22309[↩]
- Moin T, Damschroder LJ, AuYoung M, Maciejewski ML, Havens K, Ertl K, Vasti E, Weinreb JE, Steinle NI, Billington CJ, Hughes M, Makki F, Youles B, Holleman RG, Kim HM, Kinsinger LS, Richardson CR. Results From a Trial of an Online Diabetes Prevention Program Intervention. Am J Prev Med. 2018 Nov;55(5):583-591. doi: 10.1016/j.amepre.2018.06.028[↩]
- Stepanek L, Horakova D, Nakladalova M, Cibickova L, Karasek D, Zadrazil J. Significance of prediabetes as a nosological entity. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2018 Sep 24. doi: 10.5507/bp.2018.057[↩]
- Type 2 diabetes: prevention in people at high risk. National Institute for Health and Care Excellence. Public health guideline 12 July 2012. https://www.nice.org.uk/guidance/ph38/resources/type-2-diabetes-prevention-in-people-at-high-risk-pdf-1996304192197[↩]
- National Diabetes Statistics Report. https://www.cdc.gov/diabetes/data/statistics-report/index.html[↩]
- Diabetes Prevention Program Outcomes Study Research Group; Orchard TJ, Temprosa M, Barrett-Connor E, Fowler SE, Goldberg RB, Mather KJ, Marcovina SM, Montez M, Ratner RE, Saudek CD, Sherif H, Watson KE. Long-term effects of the Diabetes Prevention Program interventions on cardiovascular risk factors: a report from the DPP Outcomes Study. Diabet Med. 2013 Jan;30(1):46-55. doi: 10.1111/j.1464-5491.2012.03750.x[↩][↩]
- Diabetes Prevention Program Research Group. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the Diabetes Prevention Program Outcomes Study. Lancet Diabetes Endocrinol. 2015 Nov;3(11):866-75. doi: 10.1016/S2213-8587(15)00291-0[↩][↩][↩]
- American Diabetes Association. Standards of Medical Care in Diabetes-2017 Abridged for Primary Care Providers. Clin Diabetes. 2017 Jan;35(1):5-26. doi: 10.2337/cd16-0067[↩][↩]
- Type 2 Diabetes. https://www.cdc.gov/diabetes/basics/type2.html[↩]
- Diabetes UK. Research spotlight – low-calorie diet for Type 2 diabetes. https://www.diabetes.org.uk/Research/Research-round-up/Research-spotlight/Research-spotlight-low-calorie-liquid-diet/[↩]
- National Center for Biotechnology Information. PubMed Health. Type 2 Diabetes. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0024703/[↩]
- Evert AB, Dennison M, Gardner CD, Garvey WT, Lau KHK, MacLeod J, Mitri J, Pereira RF, Rawlings K, Robinson S, Saslow L, Uelmen S, Urbanski PB, Yancy WS Jr. Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report. Diabetes Care. 2019 May;42(5):731-754. doi: 10.2337/dci19-0014[↩][↩]
- Diabetes remission. https://www.diabetes.org.uk/guide-to-diabetes/managing-your-diabetes/treating-your-diabetes/type2-diabetes-remission[↩][↩]
- Westman EC, Yancy WS Jr. Using a low-carbohydrate diet to treat obesity and type 2 diabetes mellitus. Curr Opin Endocrinol Diabetes Obes. 2020 Oct;27(5):255-260. doi: 10.1097/MED.0000000000000565[↩]
- Gepner Y, Shelef I, Komy O, Cohen N, Schwarzfuchs D, Bril N, Rein M, Serfaty D, Kenigsbuch S, Zelicha H, Yaskolka Meir A, Tene L, Bilitzky A, Tsaban G, Chassidim Y, Sarusy B, Ceglarek U, Thiery J, Stumvoll M, Blüher M, Stampfer MJ, Rudich A, Shai I. The beneficial effects of Mediterranean diet over low-fat diet may be mediated by decreasing hepatic fat content. J Hepatol. 2019 Aug;71(2):379-388. doi: 10.1016/j.jhep.2019.04.013[↩]
- Kirkpatrick CF, Bolick JP, Kris-Etherton PM, Sikand G, Aspry KE, Soffer DE, Willard KE, Maki KC. Review of current evidence and clinical recommendations on the effects of low-carbohydrate and very-low-carbohydrate (including ketogenic) diets for the management of body weight and other cardiometabolic risk factors: A scientific statement from the National Lipid Association Nutrition and Lifestyle Task Force. J Clin Lipidol. 2019 Sep-Oct;13(5):689-711.e1. doi: 10.1016/j.jacl.2019.08.003[↩]
- Food for Thought. Key Takeaways from ADA’s Nutrition Consensus Report. https://diabetes.org/sites/default/files/2019-10/ADV_2019_Consumer_Nutrition_One%20Pager.pdf[↩]
- Altomare, R., Cacciabaudo, F., Damiano, G., Palumbo, V. D., Gioviale, M. C., Bellavia, M., Tomasello, G., & Lo Monte, A. I. (2013). The mediterranean diet: a history of health. Iranian journal of public health, 42(5), 449–457. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3684452[↩]
- Castro-Quezada, I., Román-Viñas, B., & Serra-Majem, L. (2014). The Mediterranean diet and nutritional adequacy: a review. Nutrients, 6(1), 231–248. https://doi.org/10.3390/nu6010231[↩]
- F.B. Hu. The Mediterranean Diet and mortality—olive oil and beyond. N Engl J Med, 348 (2003), pp. 2595-2596[↩]
- Sofi F., Macchi C., Abbate R., Gensini G.F., Casini A. Mediterranean diet and health. Biofactors. 2013;39:335–342. doi: 10.1002/biof.1096[↩]
- Estruch R., Ros E., Salas-Salvadó J., Covas M.I., Corella D., Arós F., Gómez-Gracia E., Ruiz-Gutiérrez V., Fiol M., Lapetra J., et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013;368:1279–1290. doi: 10.1056/NEJMoa1200303[↩]
- Mitrou P.N., Kipnis V., Thiébaut A.C., Reedy J., Subar A.F., Wirfält E., Flood A., Mouw T., Hollenbeck A.R., Leitzmann M.F., et al. Mediterranean dietary pattern and prediction of all-cause mortality in a US population: Results from the NIH-AARP Diet and Health Study. Arch. Intern. Med. 2007;167:2461–2468. doi: 10.1001/archinte.167.22.2461[↩]
- Couto E., Boffetta P., Lagiou P., Ferrari P., Buckland G., Overvad K., Dahm C.C., Tjønneland A., Olsen A., Clavel-Chapelon F., et al. Mediterranean dietary pattern and cancer risk in the EPIC cohort. Br. J. Cancer. 2011;104:1493–1499. doi: 10.1038/bjc.2011.106[↩]
- Sofi F., Abbate R., Gensini G.F., Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: An updated systematic review and meta-analysis. Am. J. Clin. Nutr. 2010;92:1189–1196. doi: 10.3945/ajcn.2010.29673[↩]
- American Heart Association – Mediterranean Diet – http://www.heart.org/HEARTORG/HealthyLiving/HealthyEating/Nutrition/Mediterranean-Diet_UCM_306004_Article.jsp[↩][↩]
- Hite, A.H., Berkowitz, V.G. and Berkowitz, K. (2011), Low-Carbohydrate Diet Review. Nutrition in Clinical Practice, 26: 300-308. https://doi.org/10.1177/0884533611405791[↩]
- Adam-Perrot, A., Clifton, P. and Brouns, F. (2006), Low-carbohydrate diets: nutritional and physiological aspects. Obesity Reviews, 7: 49-58. https://doi.org/10.1111/j.1467-789X.2006.00222.x[↩]
- Freire R. Scientific evidence of diets for weight loss: Different macronutrient composition, intermittent fasting, and popular diets. Nutrition. 2020 Jan;69:110549. doi: 10.1016/j.nut.2019.07.001[↩]
- Oh R, Gilani B, Uppaluri KR. Low Carbohydrate Diet. [Updated 2022 Jul 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537084[↩][↩]
- Trumbo P, Schlicker S, Yates AA, Poos M; Food and Nutrition Board of the Institute of Medicine, The National Academies. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J Am Diet Assoc. 2002 Nov;102(11):1621-30. doi: 10.1016/s0002-8223(02)90346-9. Erratum in: J Am Diet Assoc. 2003 May;103(5):563.[↩]
- Ebbeling CB, Feldman HA, Klein GL, Wong JMW, Bielak L, Steltz SK, Luoto PK, Wolfe RR, Wong WW, Ludwig DS. Effects of a low carbohydrate diet on energy expenditure during weight loss maintenance: randomized trial. BMJ. 2018 Nov 14;363:k4583. doi: 10.1136/bmj.k4583. Erratum in: BMJ. 2020 Nov 3;371:m4264[↩][↩]
- Raynor HA, Champagne CM. Position of the Academy of Nutrition and Dietetics: Interventions for the Treatment of Overweight and Obesity in Adults. J Acad Nutr Diet. 2016 Jan;116(1):129-147. doi: 10.1016/j.jand.2015.10.031[↩]
- Shan Z, Guo Y, Hu FB, Liu L, Qi Q. Association of Low-Carbohydrate and Low-Fat Diets With Mortality Among US Adults. JAMA Intern Med. 2020 Apr 1;180(4):513-523. doi: 10.1001/jamainternmed.2019.6980[↩]
- Ebbeling CB, Swain JF, Feldman HA, Wong WW, Hachey DL, Garcia-Lago E, Ludwig DS. Effects of dietary composition on energy expenditure during weight-loss maintenance. JAMA. 2012 Jun 27;307(24):2627-34. doi: 10.1001/jama.2012.6607[↩]
- Hall KD, Bemis T, Brychta R, Chen KY, Courville A, Crayner EJ, Goodwin S, Guo J, Howard L, Knuth ND, Miller BV 3rd, Prado CM, Siervo M, Skarulis MC, Walter M, Walter PJ, Yannai L. Calorie for Calorie, Dietary Fat Restriction Results in More Body Fat Loss than Carbohydrate Restriction in People with Obesity. Cell Metab. 2015 Sep 1;22(3):427-36. doi: 10.1016/j.cmet.2015.07.021[↩]
- Duyff RL. Carbs: Sugars, starches, and fiber. In: Academy of Nutrition and Dietetics Complete Food and Nutrition Guide. 5th ed. Houghton Mifflin Harcourt; 2017.[↩]
- 2015-2020 Dietary Guidelines for Americans. U.S. Department of Health and Human Services and U.S. Department of Agriculture. https://health.gov/our-work/nutrition-physical-activity/dietary-guidelines[↩]
- Deckers K, van Boxtel MP, Schiepers OJ, de Vugt M, Muñoz Sánchez JL, Anstey KJ, Brayne C, Dartigues JF, Engedal K, Kivipelto M, Ritchie K, Starr JM, Yaffe K, Irving K, Verhey FR, Köhler S. Target risk factors for dementia prevention: a systematic review and Delphi consensus study on the evidence from observational studies. Int J Geriatr Psychiatry. 2015 Mar;30(3):234-46. doi: 10.1002/gps.4245[↩]
- Chatterjee, S., Peters, S. A., Woodward, M., Mejia Arango, S., Batty, G. D., Beckett, N., Beiser, A., Borenstein, A. R., Crane, P. K., Haan, M., Hassing, L. B., Hayden, K. M., Kiyohara, Y., Larson, E. B., Li, C. Y., Ninomiya, T., Ohara, T., Peters, R., Russ, T. C., Seshadri, S., … Huxley, R. R. (2016). Type 2 Diabetes as a Risk Factor for Dementia in Women Compared With Men: A Pooled Analysis of 2.3 Million People Comprising More Than 100,000 Cases of Dementia. Diabetes care, 39(2), 300–307. https://doi.org/10.2337/dc15-1588[↩]
- Vagelatos NT, Eslick GD. Type 2 diabetes as a risk factor for Alzheimer’s disease: the confounders, interactions, and neuropathology associated with this relationship. Epidemiol Rev. 2013;35:152-60. doi: 10.1093/epirev/mxs012[↩][↩]
- Gudala, K., Bansal, D., Schifano, F., & Bhansali, A. (2013). Diabetes mellitus and risk of dementia: A meta-analysis of prospective observational studies. Journal of diabetes investigation, 4(6), 640–650. https://doi.org/10.1111/jdi.12087[↩]
- Cooper C, Sommerlad A, Lyketsos CG, Livingston G. Modifiable predictors of dementia in mild cognitive impairment: a systematic review and meta-analysis. Am J Psychiatry. 2015 Apr;172(4):323-34. doi: 10.1176/appi.ajp.2014.14070878[↩][↩]
- Sebastião I, Candeias E, Santos MS, de Oliveira CR, Moreira PI, Duarte AI. Insulin as a Bridge between Type 2 Diabetes and Alzheimer Disease – How Anti-Diabetics Could be a Solution for Dementia. Front Endocrinol (Lausanne). 2014 Jul 8;5:110. doi: 10.3389/fendo.2014.00110[↩]
- Effect of Insulin Sensitizer Metformin on AD Biomarkers. https://clinicaltrials.gov/ct2/show/NCT01965756[↩]
- Evaluating Liraglutide in Alzheimer’s Disease (ELAD). https://clinicaltrials.gov/ct2/show/NCT01843075[↩]
- A Pilot Clinical Trial of Exendin-4 in Alzheimer’s Disease. https://clinicaltrials.gov/ct2/show/NCT01255163[↩]
- Biomarker Qualification for Risk of Mild Cognitive Impairment (MCI) Due to Alzheimer’s Disease (AD) and Safety and Efficacy Evaluation of Pioglitazone in Delaying Its Onset (TOMMORROW). https://clinicaltrials.gov/ct2/show/NCT01931566[↩]