Contents
What is frozen shoulder
Frozen shoulder, also known as adhesive capsulitis, is a common, yet poorly understood condition causing pain, stiffness and loss of range of motion in the shoulder joint. Signs and symptoms typically begin gradually, worsen over time and then resolve, usually within one to three years. Frozen shoulder can occur in isolation or concomitantly with other shoulder conditions (e.g., rotator cuff tendinopathy, bursitis) or diabetes mellitus. Frozen shoulder is often self-limited, but can persist for years and may never fully resolve.
Frozen shoulder occurs in about 2% of the general population. It most commonly affects people between the ages of 40 and 60, and occurs in women more often than men.
Your risk of developing frozen shoulder increases if you’re recovering from a medical condition or procedure that prevents you from moving your arm — such as a stroke or a mastectomy.
The diagnosis is usually clinical, although imaging can help rule out other conditions. The differential diagnosis includes acromioclavicular arthropathy, autoimmune disease (e.g., systemic lupus erythematosus, rheumatoid arthritis), biceps tendinopathy, glenohumeral osteoarthritis, neoplasm, rotator cuff tendinopathy or tear (with or without impingement), and subacromial and subdeltoid bursitis.
Several treatment options are commonly used, but few have high-level evidence to support them. Because the condition is often self-limited, observation and reassurance may be considered; however, this may not be acceptable to many patients because of the painful and debilitating nature of the condition. Home exercise regimens and physical therapy are often prescribed.
Nonsurgical treatments for frozen shoulder usually involves range-of-motion exercises, analgesics (e.g., acetaminophen, nonsteroidal anti-inflammatory drugs), oral prednisone, intra-articular corticosteroid injections and numbing medications injected into the joint capsule.
In a small percentage of cases, surgical treatments include manipulation of the joint under anesthesia or arthroscopic capsular release surgery may be indicated to loosen the joint capsule so that it can move more freely.
It’s unusual for frozen shoulder to recur in the same shoulder, but some people can develop it in the opposite shoulder.
The shoulder joint
The shoulder joint is a ball-and-socket joint formed by the head of the humerus and the glenoid cavity of the scapula. It is also referred to as the humeroscapular or glenohumeral joint.
Anatomical components of the shoulder joint
- Articular capsule. Thin, loose sac that completely envelops the joint and extends from the glenoid cavity to the anatomical neck of the humerus. The inferior part of the capsule is its weakest area (Figures 2, 3 and 4).
- Coracohumeral ligament. Strong, broad ligament that strengthens the superior part of the articular capsule and extends from the coracoid process of the scapula to the greater tubercle of the humerus. The ligament strengthens the superior part of the articular capsule and reinforces the anterior aspect of the articular capsule.
- Glenohumeral ligaments. Three thickenings of the articular capsule over the anterior surface of the joint that extend from the glenoid cavity to the lesser tubercle and anatomical neck of the humerus. These ligaments are often indistinct or absent and provide only minimal strength. They play a role in joint stabilization when the humerus approaches or exceeds its limits of motion.
- Transverse humeral ligament. Narrow sheet extending from the greater tubercle to the lesser tubercle of the humerus. The ligament functions as a retinaculum (retaining band of connective tissue) to hold the long head of the biceps brachii muscle.
- Glenoid labrum. Narrow rim of fibrocartilage around the edge of the glenoid cavity that slightly deepens and enlarges the glenoid cavity.
- Bursae. Four bursae are associated with the shoulder joint. They are the subscapular bursa, subdeltoid bursa, not labeled in subacromial bursa and subcoracoid bursa.
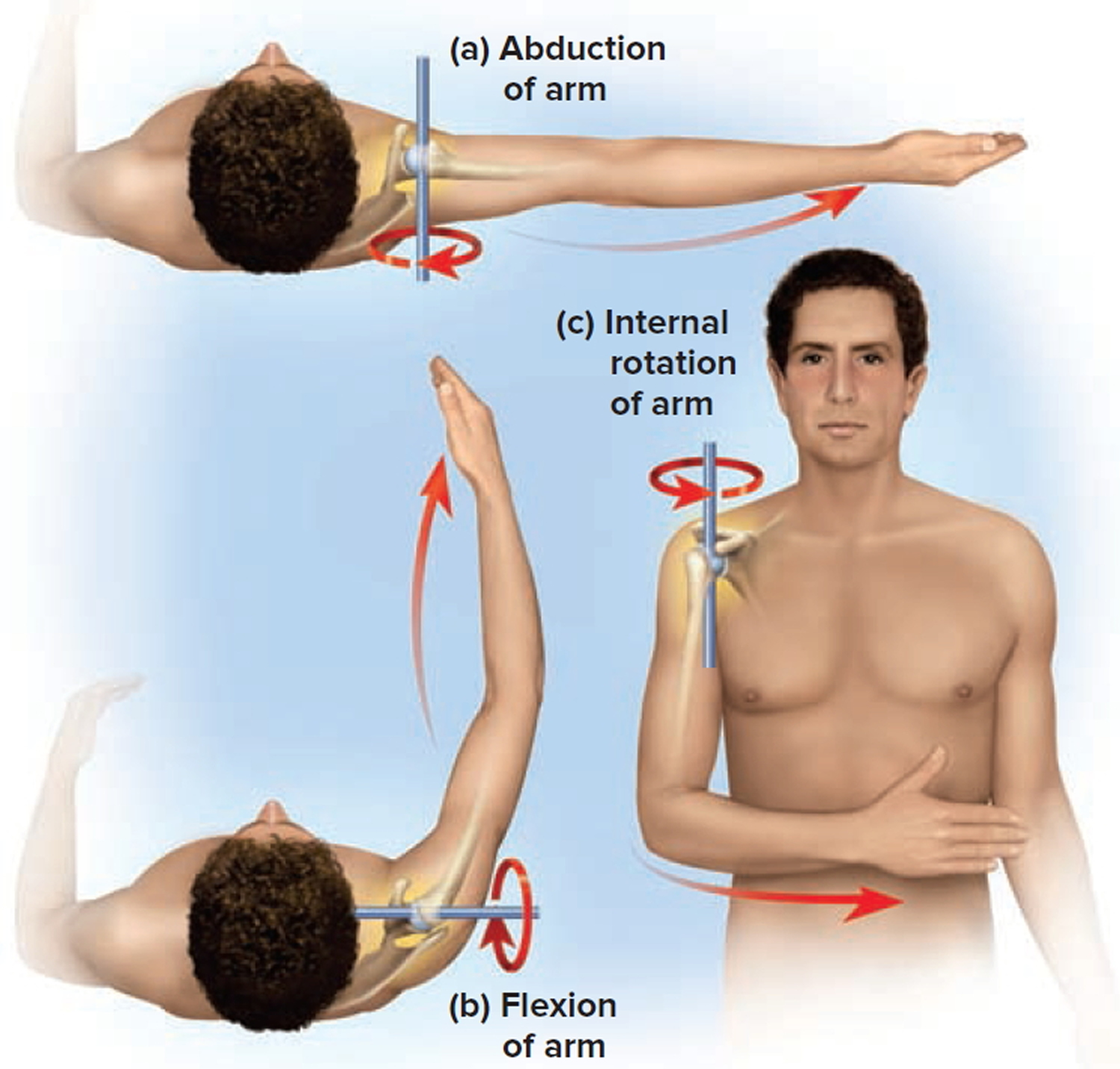
The shoulder joint allows flexion, extension, hyperextension, abduction, adduction, medial rotation, lateral rotation, and circumduction of the arm (see Figure 5). It has more freedom of movement than any other joint of the body. This freedom results from the looseness of the articular capsule and the shallowness of the glenoid cavity in relation to the large size of the head of the humerus.
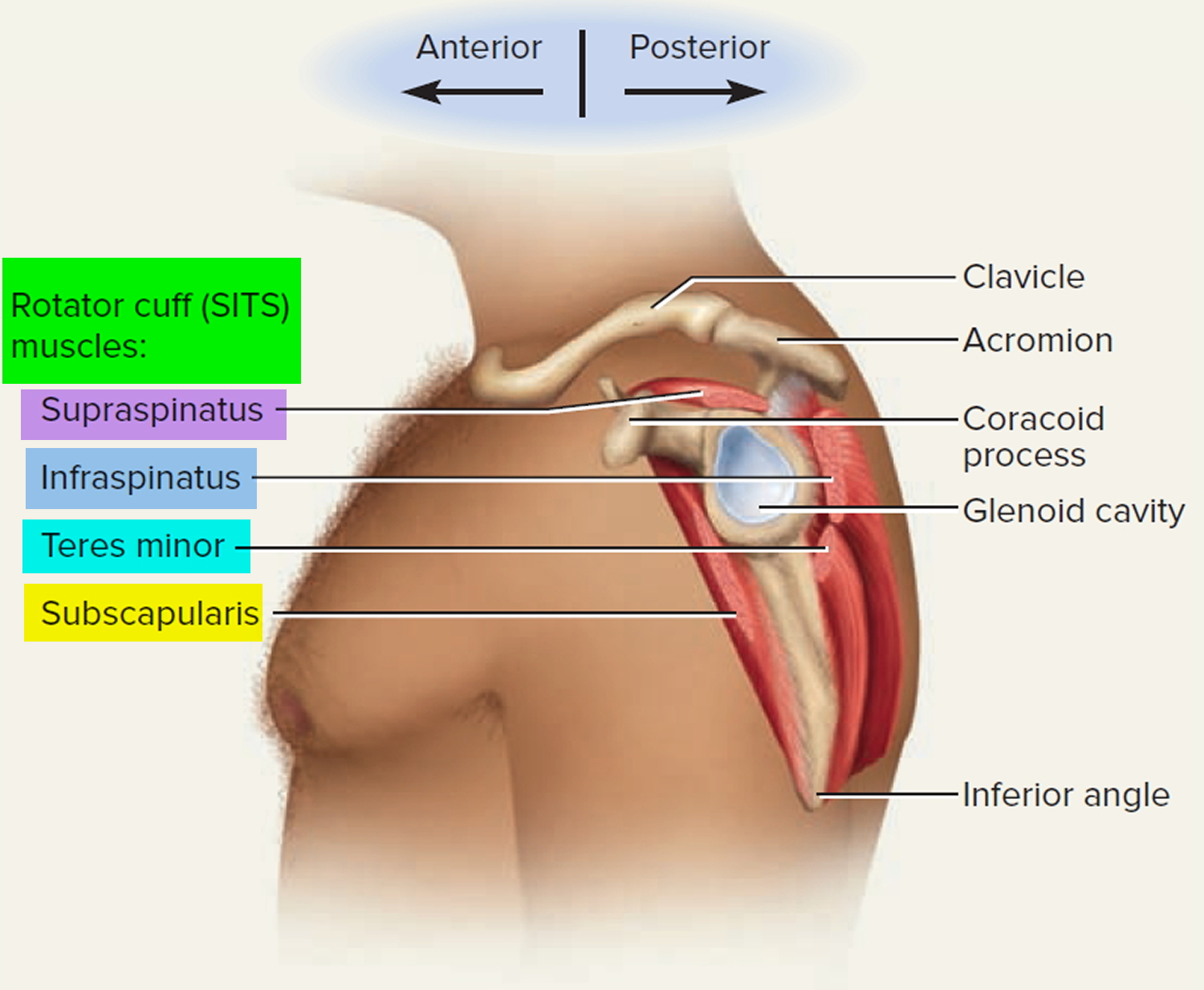
Although the ligaments of the shoulder joint strengthen it to some extent, most of the strength results from the muscles that surround the joint, especially the rotator cuff muscles. These muscles (supraspinatus, infraspinatus, teres minor, and subscapularis) anchor the humerus to the scapula (see Figure 6). The tendons of the rotator
cuff muscles encircle the joint (except for the inferior portion) and intimately surround the articular capsule. The rotator cuff muscles work as a group to hold the head of the humerus in the glenoid cavity.
The Pectoral Girdle (shoulder girdle)
The pectoral girdle (shoulder girdle) supports the arm and links it to the axial skeleton. It consists of two bones on each side of the body: the clavicle (collarbone) and scapula (shoulder blade). The medial end of the clavicle articulates with the sternum at the sternoclavicular joint, and its lateral end articulates with the scapula at the acromioclavicular joint (see Figure 1). The scapula also articulates with the humerus at the glenohumeral joint. These are loose attachments that result in a shoulder far more flexible, but they also make the shoulder joint easy to dislocate.
Figure 1. Shoulder girdle (pectoral girdle)
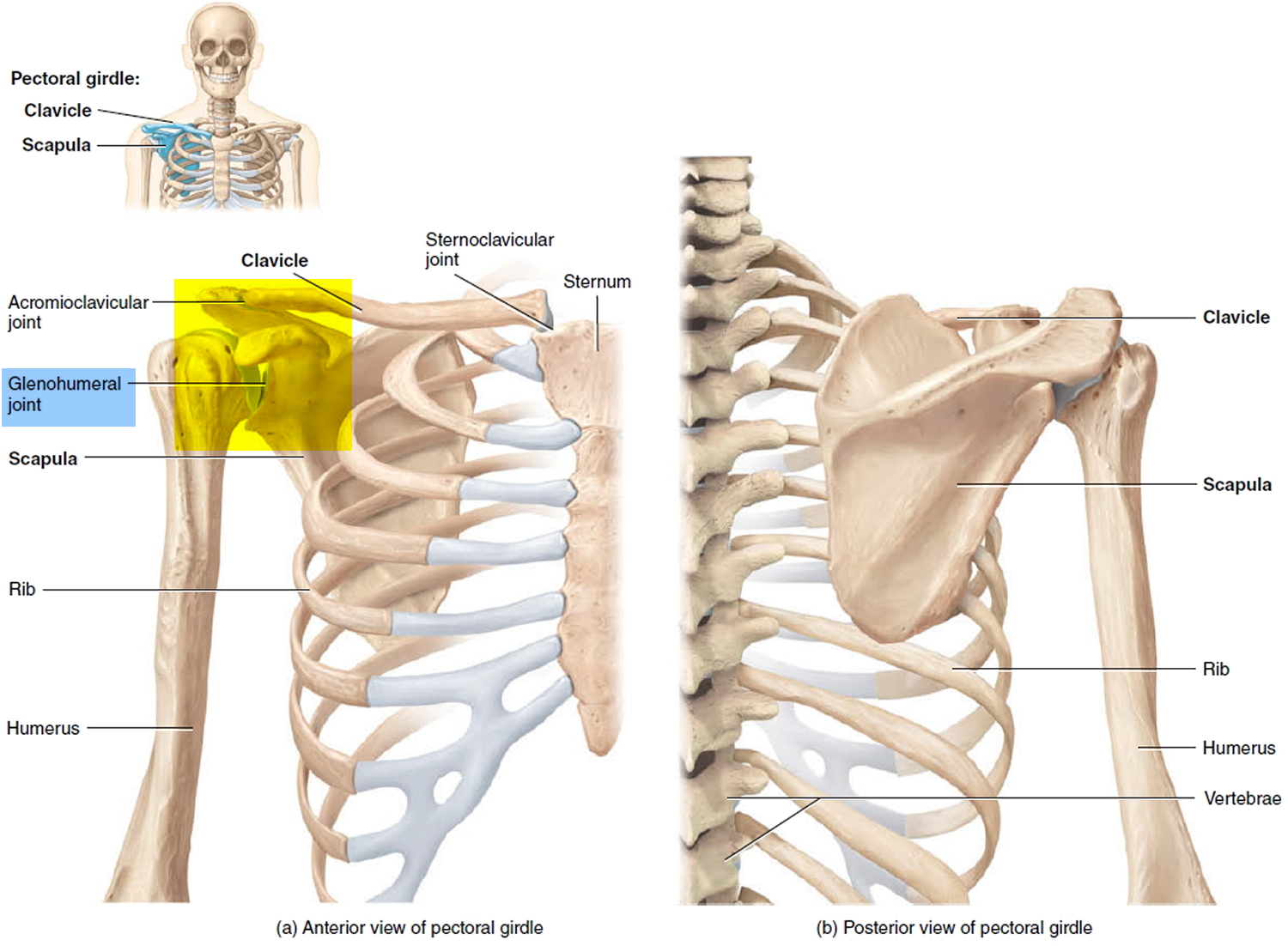 Figure 2. Shoulder joint
Figure 2. Shoulder joint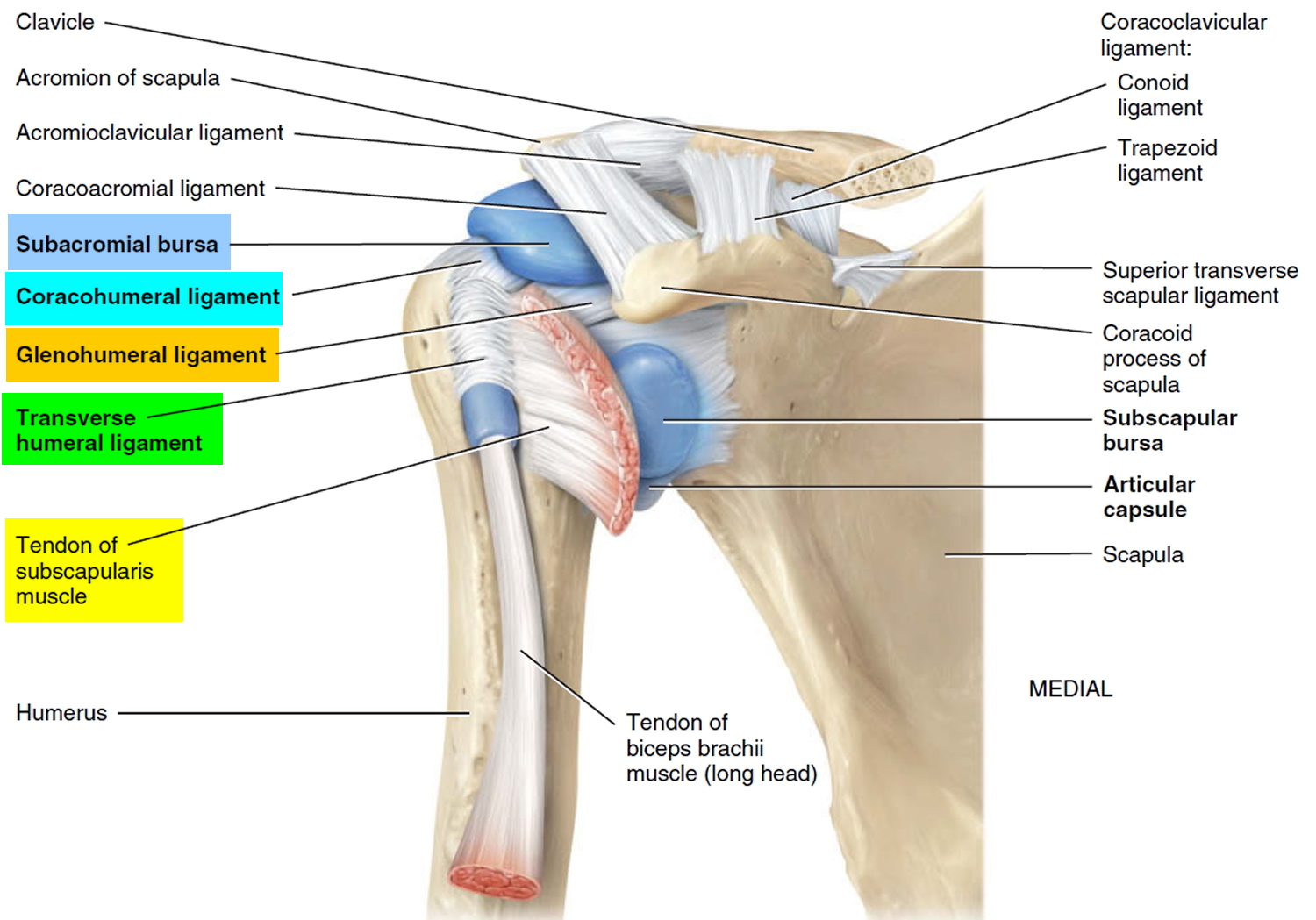 Figure 3. Shoulder joint (frontal view)
Figure 3. Shoulder joint (frontal view)
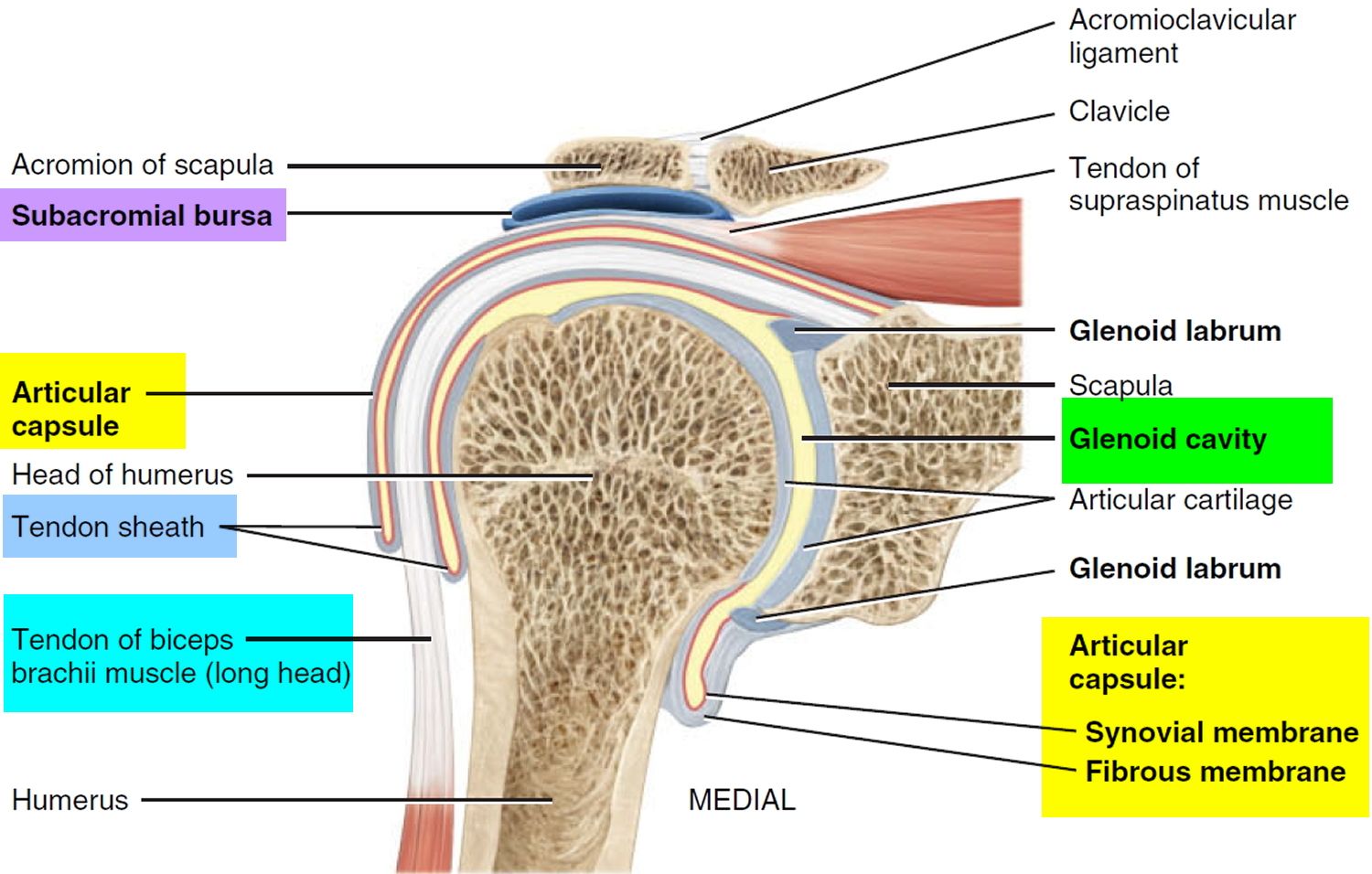 Figure 4. Shoulder joint (lateral view)
Figure 4. Shoulder joint (lateral view)
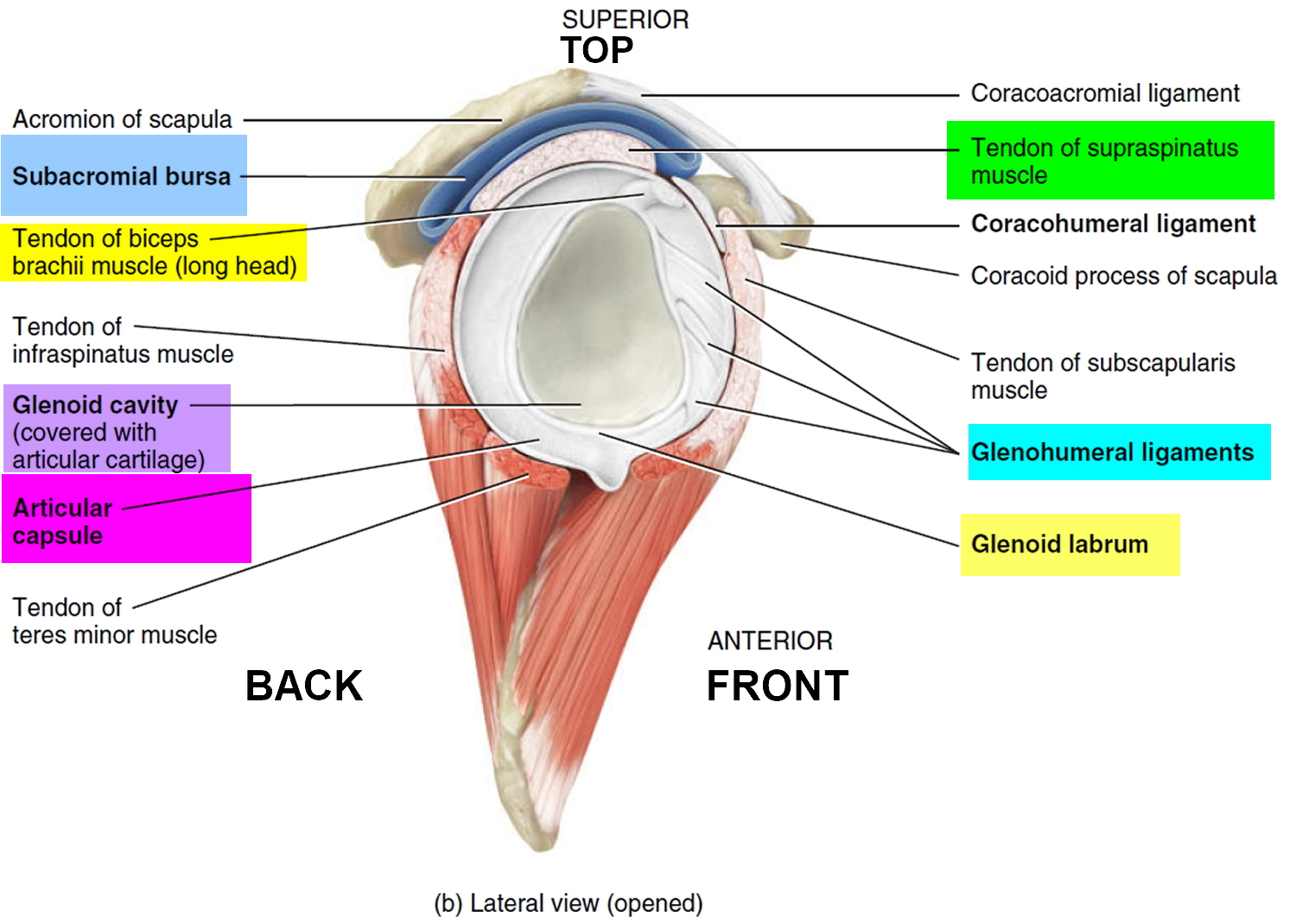 Figure 5. Shoulder joint movement
Figure 5. Shoulder joint movement
Frozen shoulder stages
In frozen shoulder, the shoulder capsule thickens and becomes tight. Stiff bands of tissue — called adhesions — develop. In many cases, there is less synovial fluid in the joint.
The hallmark sign of this condition is being unable to move your shoulder – either on your own or with the help of someone else. It develops in three stages.
There is, however, no evidence to validate this classification, and its clinical utility is questionable. Pain and limited range of motion can occur in all phases of adhesive capsulitis, which often does not follow a stepwise course. Pain and decreased range of motion can persist for one to two years 1 and up to 10 percent of patients never recover full range of motion. However, this loss of motion is seldom functionally limiting 2.
Freezing
In the”freezing” stage, you slowly have more and more pain. As the pain worsens, your shoulder loses range of motion. Freezing typically lasts from 6 weeks to 9 months.
Frozen
Painful symptoms may actually improve during this stage, but the stiffness remains. During the 4 to 6 months of the “frozen” stage, daily activities may be very difficult.
Thawing
Shoulder motion slowly improves during the “thawing” stage. Complete return to normal or close to normal strength and motion typically takes from 6 months to 2 years.
What causes frozen shoulder
The bones, ligaments and tendons that make up your shoulder joint are encased in a capsule of connective tissue. Frozen shoulder occurs when this capsule thickens and tightens around the shoulder joint, restricting its movement.
Doctors aren’t sure why this happens to some people, although it’s more likely to occur in people who have diabetes or those who recently had to immobilize their shoulder for a long period, such as after surgery or an arm fracture.
Analysis of surgical specimens suggests that capsular hyperplasia and fibrosis have a role. The presence of cytokines suggests a possible autoimmune process, but the relationship is not well established 3.
Risk factors for frozen shoulder
Certain factors may increase your risk of developing frozen shoulder.
Age and sex
People 40 and older, particularly women, are more likely to have frozen shoulder.
Immobility or reduced mobility
People who’ve had prolonged immobility or reduced mobility of the shoulder are at higher risk of developing frozen shoulder. Immobility may be the result of many factors, including:
- Rotator cuff injury
- Broken arm
- Stroke
- Recovery from surgery
Systemic diseases
People who have certain diseases appear more likely to develop frozen shoulder. Diseases that might increase risk include:
- Diabetes
- Overactive thyroid (hyperthyroidism)
- Underactive thyroid (hypothyroidism)
- Cardiovascular disease
- Tuberculosis
- Parkinson’s disease
Frozen shoulder prevention
One of the most common causes of frozen shoulder is the immobility that may result during recovery from a shoulder injury, broken arm or a stroke. If you’ve had an injury that makes it difficult to move your shoulder, talk to your doctor about exercises you can do to maintain the range of motion in your shoulder joint.
Frozen shoulder symptoms
Pain from frozen shoulder is usually dull or aching. It is typically worse early in the course of the disease and when you move your arm. The pain is usually located over the outer shoulder area and sometimes the upper arm.
The hallmark of adhesive capsulitis is decreased range of motion and shoulder pain. There often is no identifiable cause or trigger. The pain is often described as a poorly localized, deep ache. If the pain is localized, it is usually in the area of the anterior or posterior capsule. The pain may radiate to the biceps area. Patients may have progressive pain and stiffness when reaching overhead, away, and behind the back. Weakness is often related to pain or concomitant tendinopathy. Crepitus may be present on the involved side. As with many shoulder conditions, pain may impair sleep. Unlike more serious causes of shoulder pain, adhesive capsulitis does not cause red flag symptoms such as fever, night sweats, and unexplained weight loss. Neuropathic symptoms in the forearm and hand suggest another diagnosis, such as cervical radiculopathy.
Frozen shoulder typically develops slowly, and in three stages. Each stage can last a number of months.
- Freezing stage. Any movement of your shoulder causes pain, and your shoulder’s range of motion starts to become limited.
- Frozen stage. Pain may begin to diminish during this stage. However, your shoulder becomes stiffer, and using it becomes more difficult.
- Thawing stage. The range of motion in your shoulder begins to improve.
For some people, the pain worsens at night, sometimes disrupting sleep.
Frozen shoulder diagnosis
During the physical exam, your doctor may ask you to move in certain ways to check for pain and evaluate your range of motion (active range of motion). Your doctor might then ask you to relax your muscles while he or she moves your arm (passive range of motion). Frozen shoulder affects both active and passive range of motion.
Hawkin’s Test
Neer test
Yergason test
Speed test
In some cases, your doctor might inject your shoulder with a numbing medicine (anesthetic) to determine your passive and active range of motion.
Frozen shoulder can usually be diagnosed from signs and symptoms alone. But your doctor may suggest blood tests and imaging tests — such as X-rays or an MRI — to rule out other problems.
Because of the high prevalence of diabetes and prediabetes in patients with adhesive capsulitis, docotors should consider fasting glucose testing in patients who have not been diagnosed with diabetes. Additional serologies are usually not indicated, but may be performed if autoimmune or infectious conditions are suspected. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels may be elevated in patients with primary adhesive capsulitis, but these tests are not sensitive or specific 4.
X-rays. Dense structures, such as bone, show up clearly on x-rays. X-rays may show other problems in your shoulder, such as arthritis.
Magnetic resonance imaging (MRI) and ultrasound. Magnetic resonance imaging is not diagnostic for adhesive capsulitis, but can be helpful in identifying other conditions, such as rotator cuff tendinopathy, torn rotator cuff and subacromial bursitis. Capsular thickening can sometimes be observed on magnetic resonance imaging in patients with adhesive capsulitis 5.
Differential Diagnosis
The diagnosis of adhesive capsulitis is usually clinical. Other conditions that should be considered in a patient who presents with a stiff, painful shoulder include acromioclavicular arthropathy, autoimmune disease (e.g., systemic lupus erythematosus, rheumatoid arthritis), biceps tendinopathy, glenohumeral osteoarthritis, neoplasm, rotator cuff tendinopathy or tear (with or without impingement), cervical disk degeneration, and subacromial and subdeltoid bursitis. Table 1 includes conditions that can mimic adhesive capsulitis, but may also occur concomitantly. Adhesive capsulitis in the presence of associated conditions is most appropriately described as painful shoulder syndrome.
Table 1. Adhesive Capsulitis: Alternative Diagnoses
| Condition | Distinguishing physical examination findings | Distinguishing historical findings | Diagnostic tests |
|---|---|---|---|
Acromioclavicular arthropathy | Positive cross-arm adduction and compression testing; glenohumeral range of motion is preserved | Localizes over acromioclavicular joint (superiorly); history of repetitive overuse (e.g., weight lifting) | Plain radiography |
Autoimmune disease (e.g., systemic lupus erythematosus, rheumatoid arthritis) | Malar rash; synovitis (tenderness and effusions) in other joints | Multisystem involvement; multiple joints involved | Antinuclear antibody testing; rheumatoid factor test |
Biceps tendinopathy | Tenderness over long head of the biceps tendon; positive Speed or Yergason test | Localizes anteriorly | MRI (radiography may determine whether calcifications are present) |
Cervical disk degeneration | Limited range of motion in neck and pain with active movement; intrinsic hand weakness; impaired light touch | Localizes posteriorly; hand numbness and weakness in radiculopathy | Cervical spine radiography |
Glenohumeral osteoarthritis | Similar to adhesive capsulitis; shoulder girdle atrophy may be present | History of shoulder trauma or surgery; older age | Plain radiography |
Neoplasm | Similar to adhesive capsulitis | Fevers, night sweats, unexplained weight loss (if advanced); dyspnea or cough (if Pancoast tumor present) | Plain radiography, MRI |
Rotator cuff tendinopathy or tear, with or without impingement | Passive range of motion is preserved; painful arc, focal tenderness, positive Hawkins and Neer tests | Possible history of repetitive overuse; often localizes anteriorly or laterally | MRI (radiography may determine whether calcifications are present) |
Subacromial and subdeltoid bursitis | Passive range of motion is preserved | Possible history of repetitive overuse | Diagnostic subacromial lidocaine (Xylocaine) injection, MRI |
Footnote: Secondary adhesive capsulitis can also result from these conditions.
MRI = magnetic resonance imaging
[Source 6]Frozen shoulder treatment
Frozen shoulder generally gets better over time, although it may take up to 3 years.
Most frozen shoulder treatment involves controlling shoulder pain and preserving as much range of motion in the shoulder as possible.
Nonsurgical Treatment
More than 90% of patients improve with relatively simple treatments to control pain and restore motion.
Medications
Over-the-counter pain relievers, such as acetaminophen and non-steroidal anti-inflammatory medicines like aspirin and ibuprofen (Advil, Motrin IB, others), can help reduce pain and inflammation associated with frozen shoulder. In some cases, your doctor may prescribe stronger pain-relieving and anti-inflammatory drugs.
For more severe cases, a tapering course of oral prednisone is often prescribed, usually over two to three weeks. Starting dosages typically range from 40 to 60 mg per day, and are tapered by 10 mg every four to seven days. Oral corticosteroids provide short-term benefit in pain relief and improved range of motion (up to six weeks) in patients with adhesive capsulitis, but they have not been proven to shorten the duration of the condition 7.
Frozen shoulder exercises
A physical therapist can teach you range-of-motion exercises to help recover as much mobility in your shoulder as possible. Your commitment to doing these exercises is important to optimize recovery of your mobility.
Specific exercises will help restore motion. These may be under the supervision of a physical therapist or via a home program. Therapy includes stretching or range of motion exercises for the shoulder. Sometimes heat is used to help loosen the shoulder up before the stretching exercises.. Below are examples of some of the exercises that might be recommended.
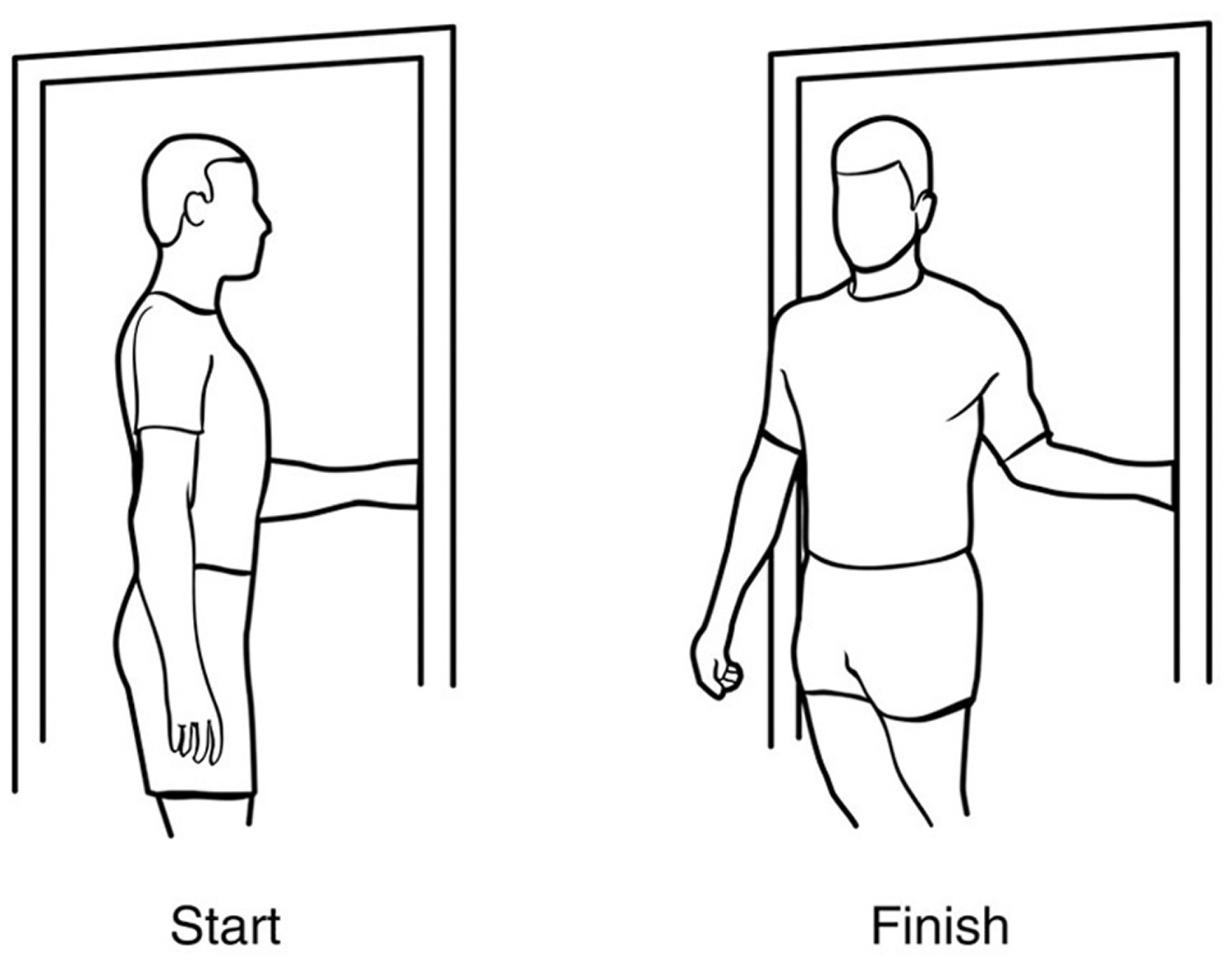
External rotation — passive stretch
Stand in a doorway and bend your affected arm 90 degrees to reach the doorjamb. Keep your hand in place and rotate your body as shown in the illustration (Figure 7). Hold for 30 seconds. Relax and repeat.
Figure 7. Frozen shoulder exercise – external rotation passive stretch
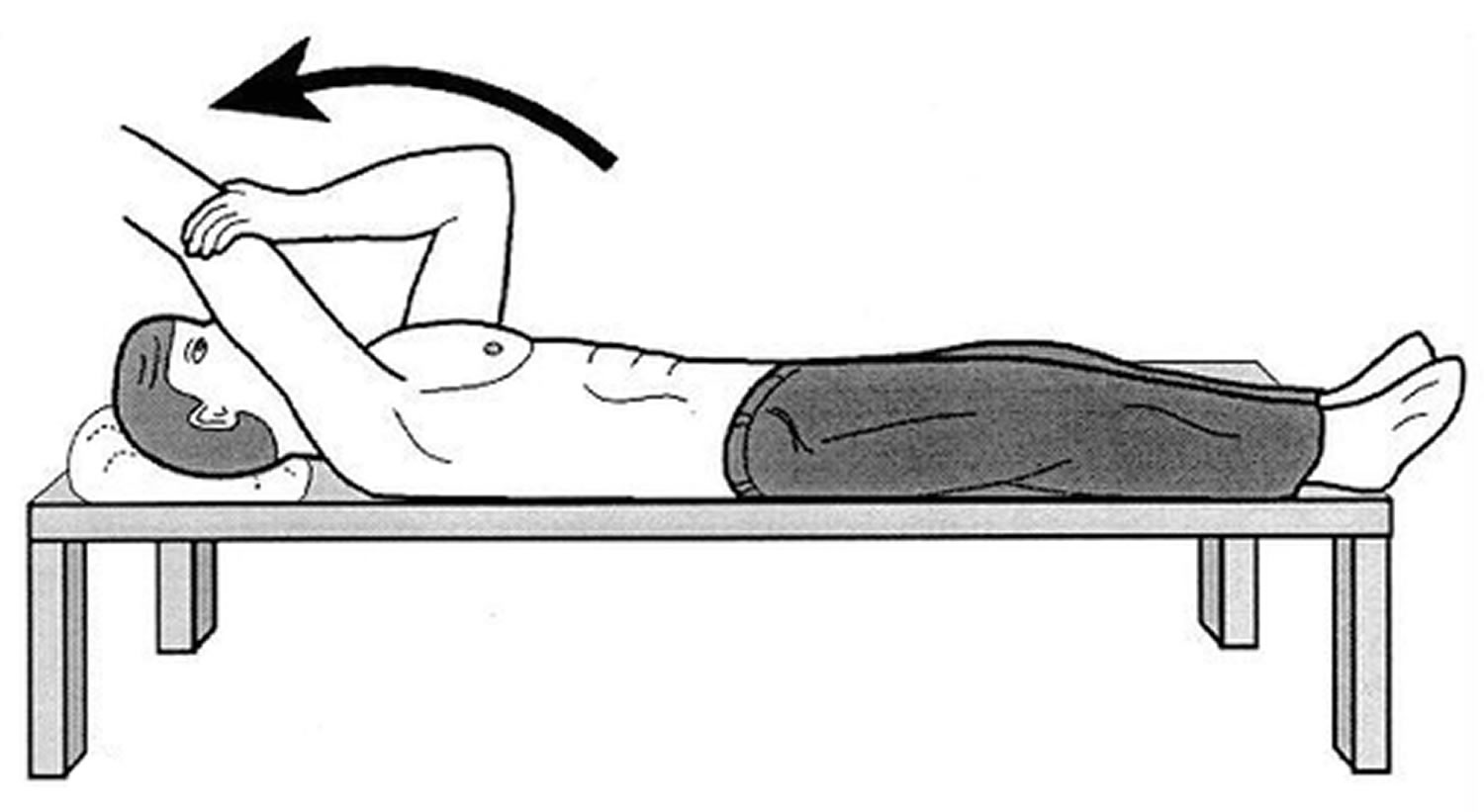
Forward flexion — supine position
Lie on your back with your legs straight. Use your unaffected arm to lift your affected arm overhead until you feel a gentle stretch. Hold for 15 seconds and slowly lower to start position. Relax and repeat.
Figure 8. Frozen shoulder exercise – forward flexion in supine position
 Crossover arm stretch
Crossover arm stretch
Gently pull one arm across your chest just below your chin as far as possible without causing pain. Hold for 30 seconds. Relax and repeat.
Figure 9. Frozen shoulder exercise – crossover arm stretch
Surgical and other procedures
Most frozen shoulders get better on their own within 12 to 18 months. For persistent symptoms, your doctor may suggest:
- Steroid injections. Injecting corticosteroids into your shoulder joint may help decrease pain and improve shoulder mobility, especially in the early stages of the process.
- Joint distension. Injecting sterile water into the joint capsule can help stretch the tissue and make it easier to move the joint.
- Shoulder manipulation. In this procedure, you receive a general anesthetic, so you’ll be unconscious and feel no pain. Then the doctor moves your shoulder joint in different directions, to help loosen the tightened tissue.
- Surgery. Surgery for frozen shoulder is rare, but if nothing else has helped, your doctor may recommend surgery to remove scar tissue and adhesions from inside your shoulder joint. Doctors usually perform this surgery with lighted, tubular instruments inserted through small incisions around your joint (arthroscopically).
In many cases, manipulation and arthroscopy are used in combination to obtain maximum results. Most patients have very good outcomes with these procedures.
Another treatment option for patients with adhesive capsulitis is radiographically guided capsular distension with saline, with or without corticosteroid injection. This treatment is as effective or better than manipulation under anesthesia, and carries less risk. However, the benefit may not last beyond six to 12 weeks 8.
There is limited evidence that acupuncture can improve pain and function for two to four weeks in patients with shoulder pain, but there is no definitive evidence of benefit in patients with adhesive capsulitis 9.
Recovery. After surgery, physical therapy is necessary to maintain the motion that was achieved with surgery. Recovery times vary, from 6 weeks to three months. Although it is a slow process, your commitment to therapy is the most important factor in returning to all the activities you enjoy.
Long-term outcomes after surgery are generally good, with most patients having reduced or no pain and greatly improved range of motion. In some cases, however, even after several years, the motion does not return completely and a small amount of stiffness remains.
Although uncommon, frozen shoulder can recur, especially if a contributing factor like diabetes is still present.
- Tveitå EK, Sandvik L, Ekeberg OM, Juel NG, Bautz-Holter E. Factor structure of the Shoulder Pain and Disability Index in patients with adhesive capsulitis. BMC Musculoskelet Disord. 2008;9103.[↩]
- McLaughlin HL. On the frozen shoulder. Bull Hosp Joint Dis. 1951;12(2):383–393.[↩]
- Rodeo SA, Hannafin JA, Tom J, Warren RF, Wickiewicz TL. Immunolocalization of cytokines and their receptors in adhesive capsulitis of the shoulder. J Orthop Res. 1997;15(3):427–436.[↩]
- Bulgen DY, Binder A, Hazleman BL, Park JR. Immunological studies in frozen shoulder. J Rheumatol. 1982;9(6):893–898.[↩]
- Yoo JC, Ahn JH, Lee YS, Koh KH. Magnetic resonance arthrographic findings of presumed stage-2 adhesive capsulitis: focus on combined rotator cuff pathology. Orthopedics. 2009;32(1):22.[↩]
- Adhesive Capsulitis: A Review. Am Fam Physician. 2011 Feb 15;83(4):417-422. https://www.aafp.org/afp/2011/0215/p417.html[↩]
- Buchbinder R, Green S, Youd JM, Johnston RV. Oral steroids for adhesive capsulitis. Cochrane Database Syst Rev. 2006;(4):CD006189.[↩]
- Buchbinder R, Green S, Youd JM, Johnston RV, Cumpston M. Arthrographic distension for adhesive capsulitis (frozen shoulder). Cochrane Database Syst Rev. 2008;(1):CD007005.[↩]
- Green S, Buchbinder R, Hetrick S. Acupuncture for shoulder pain. Cochrane Database Syst Rev. 2005;(2):CD005319.[↩]