Contents
- Herniated disc
- What are spinal discs?
- Herniated (prolapsed) disc causes
- Prevention of spinal disc problems and back injury
- Herniated disc complications
- Herniated disc in neck
- Herniated disc lower back
- Herniated disc symptoms
- Herniated disc diagnosis
- Herniated disc differential diagnosis
- Herniated disc treatment
- Herniated disc prognosis
Herniated disc
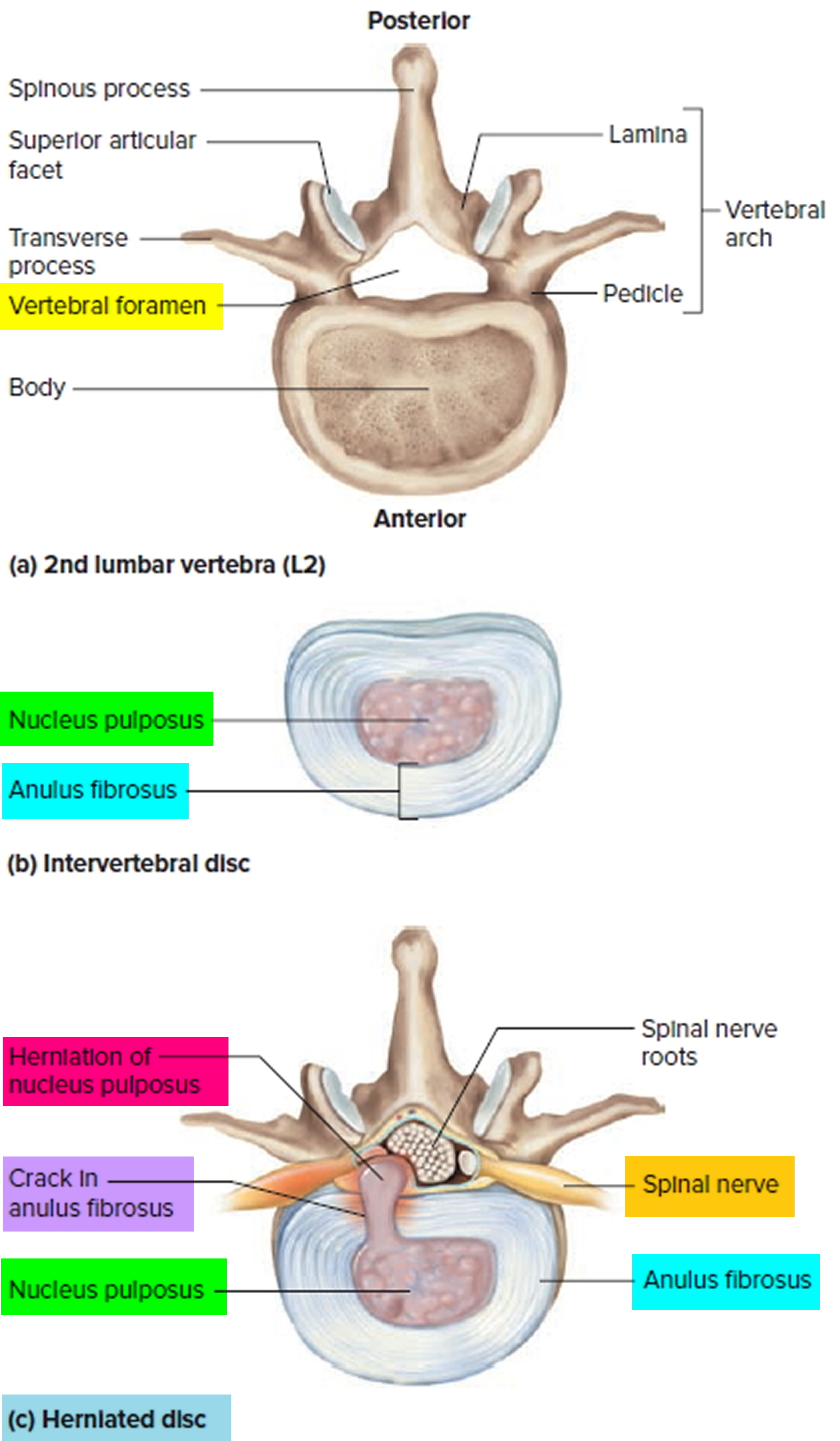
A herniated (ruptured) intervertebral disc occurs when all or part of an intervertebral disc in your spine is forced through a weakened part of the disc (see Figure 1 c). The word “herniate” means to bulge or to stick out. This allows the jelly-like center of the disc to leak, irritating the nearby spinal nerves. This is also called a slipped disc or a bulging disc. These discs become a problem when the center of the disc pushes against a nerve or the spinal cord. Spinal nerves are very sensitive to even slight amounts of pressure, which can result in pain that can vary from mild to severe, numbness, or weakness in one or both legs. This can cause sciatica or back pain and other problems.
- Although a herniated disc can sometimes be very painful, most people feel much better with just a few months of simple, nonsurgical treatments.
- Not all herniated discs cause symptoms. Many people will never know they have slipped a disc.
Herniated discs are most common in the lumbar spine — the lower part of your backbone, between the bottom of your ribs and your hips. They can also happen cervical area (your neck). The discs in your upper-to-mid back (thoracic area) are rarely involved.
A herniated disc (also called a prolapsed or slipped disc) can cause:
- lower back pain – the most common symptom
- numbness or tingling in your shoulders, back, arms, hands, legs or feet
- neck pain
- problems bending or straightening your back
- muscle weakness
- pain in the buttocks, hips or legs if the disc is pressing on the sciatic nerve (sciatica)
Your doctor will diagnose a herniated disc with a physical exam and, sometimes, imaging tests. With treatment, most people recover. Treatments include rest, pain and anti-inflammatory medicines, physical therapy, and sometimes surgery.
Risk Factors for herniated disc
In children and young adults, discs have high water content. As people age, the water content in the discs decreases and the discs become less flexible. The discs begin to shrink and the spaces between the vertebrae get narrower. Conditions that can weaken the disc include:
- Improper lifting
- Smoking
- Excessive body weight that places added stress on the discs (in the lower back)
- Sudden pressure (which may be slight)
- Repetitive strenuous activities
Other types of spinal disc problems include:
- degenerative disc disease, which is the natural change that happen to your discs as you age, and is not really a disease
- injury from falls or accidents
- infection
- cancers that affect the spine.
Other causes of back pain
Sometimes the pain may be a result of an injury such as a sprain or strain but often there’s no obvious reason. Back pain is rarely caused by anything serious.
Nonsurgical treatment is effective in treating the symptoms of herniated discs in the majority of patients. Most neck or back pain will resolve gradually with simple measures.
- Rest and over-the-counter pain relievers may be all that is needed.
- Muscle relaxers, analgesics, and anti-inflammatory medications are also helpful.
- Cold compresses or ice can also be applied several times a day for no more than 20 minutes at a time.
- After any spasms settle, gentle heat applications may be used.
See your doctor right away if you have any of the following symptoms:
- have numbness around your bottom or genitals
- can’t urinate
- lose feeling in one or both feet or legs
- loss of bowel or bladder function
- ave a very high temperature or you feel hot and shivery
- have unexplained weight loss
- have a swelling in your back
- notice the pain is worse at night
- got it after a serious accident, such as a car accident
- more pain or weakness than usual in your backbone.
These could be signs of complications or a more serious problem.
What are spinal discs?
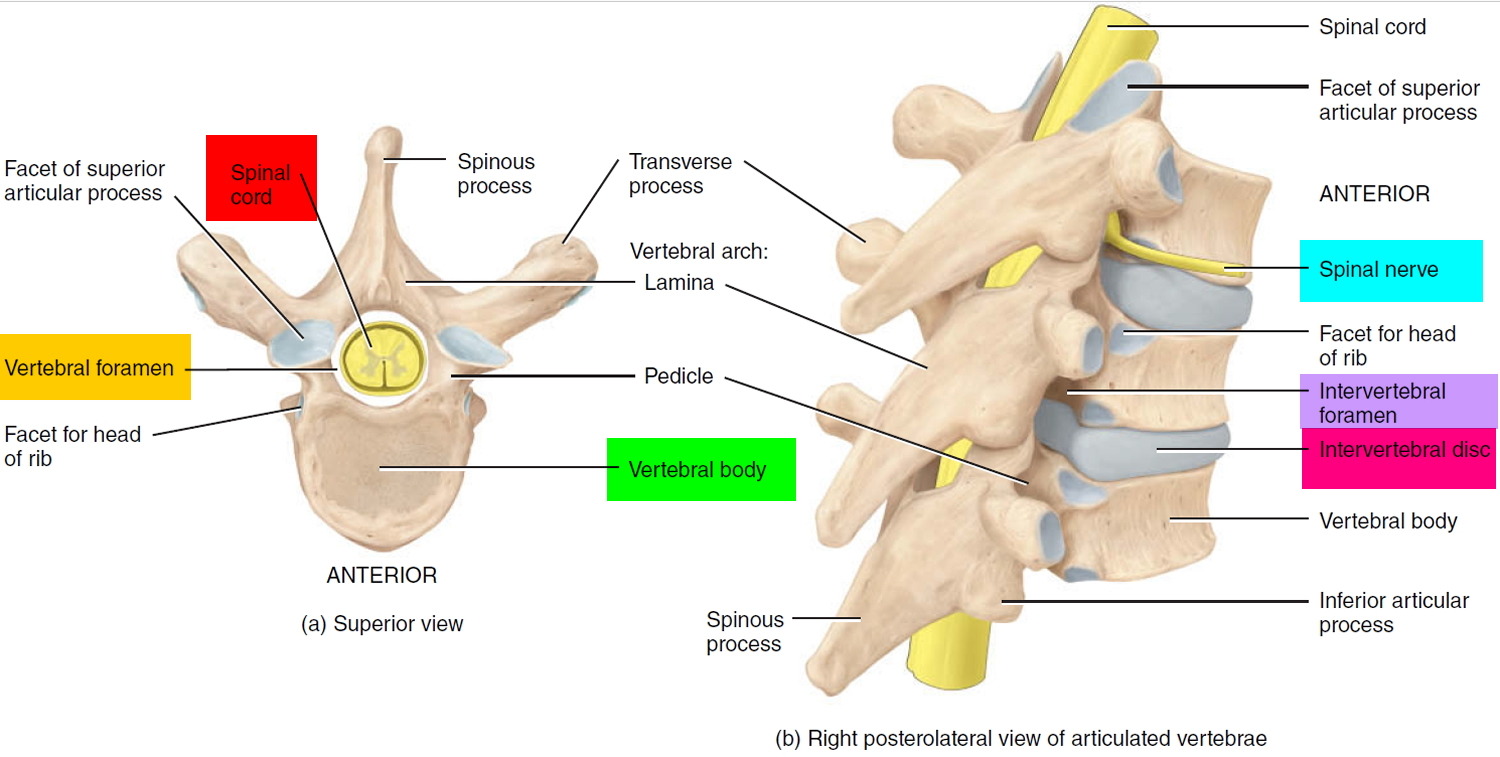
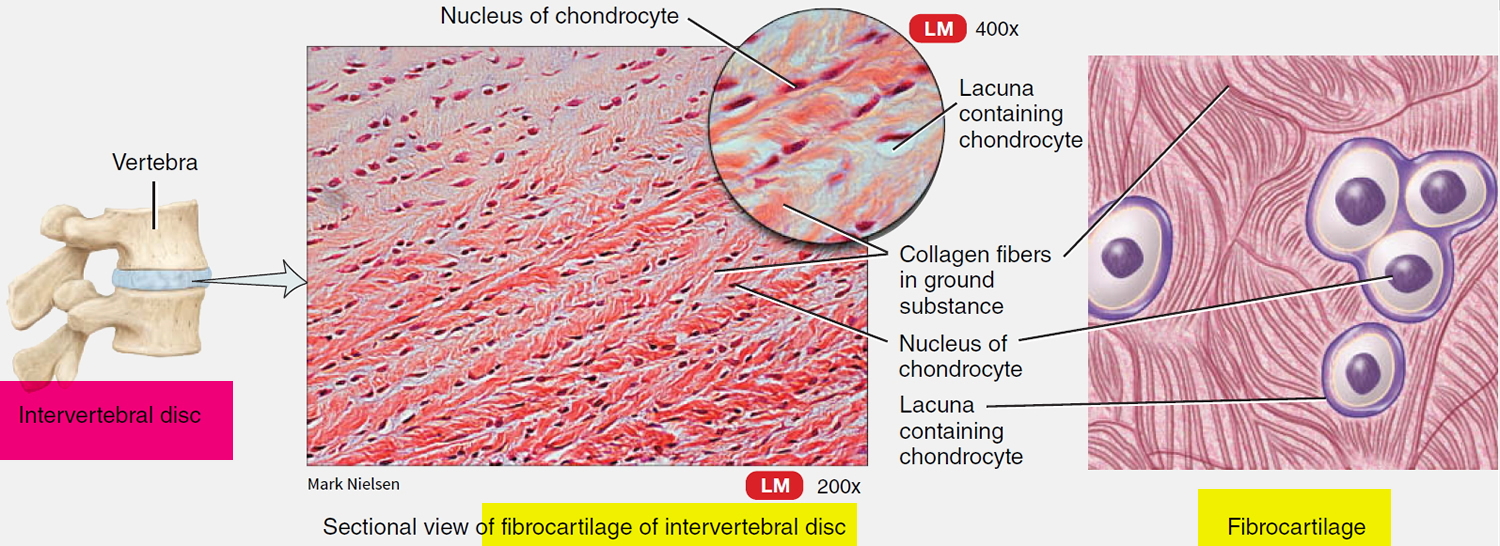
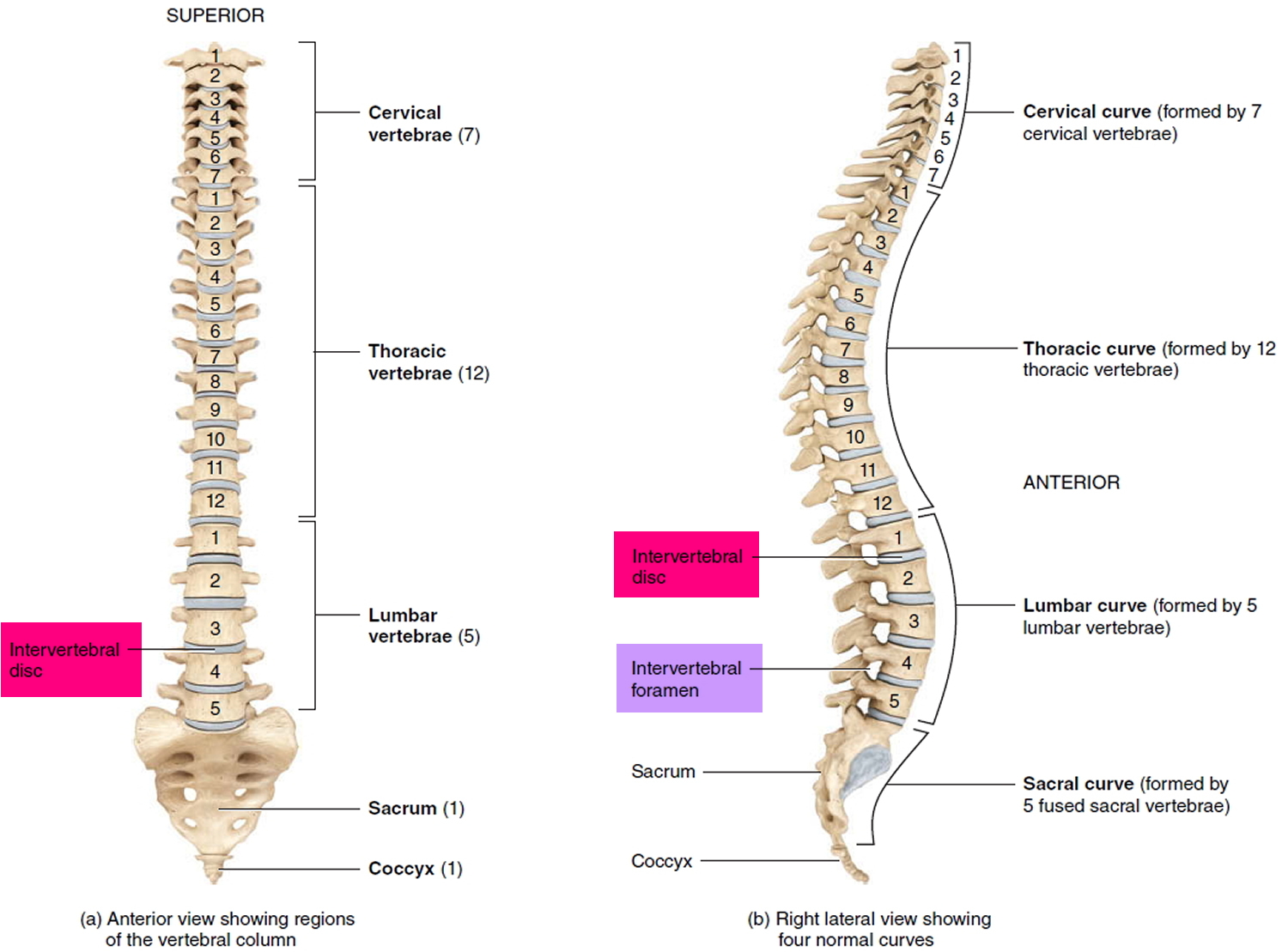
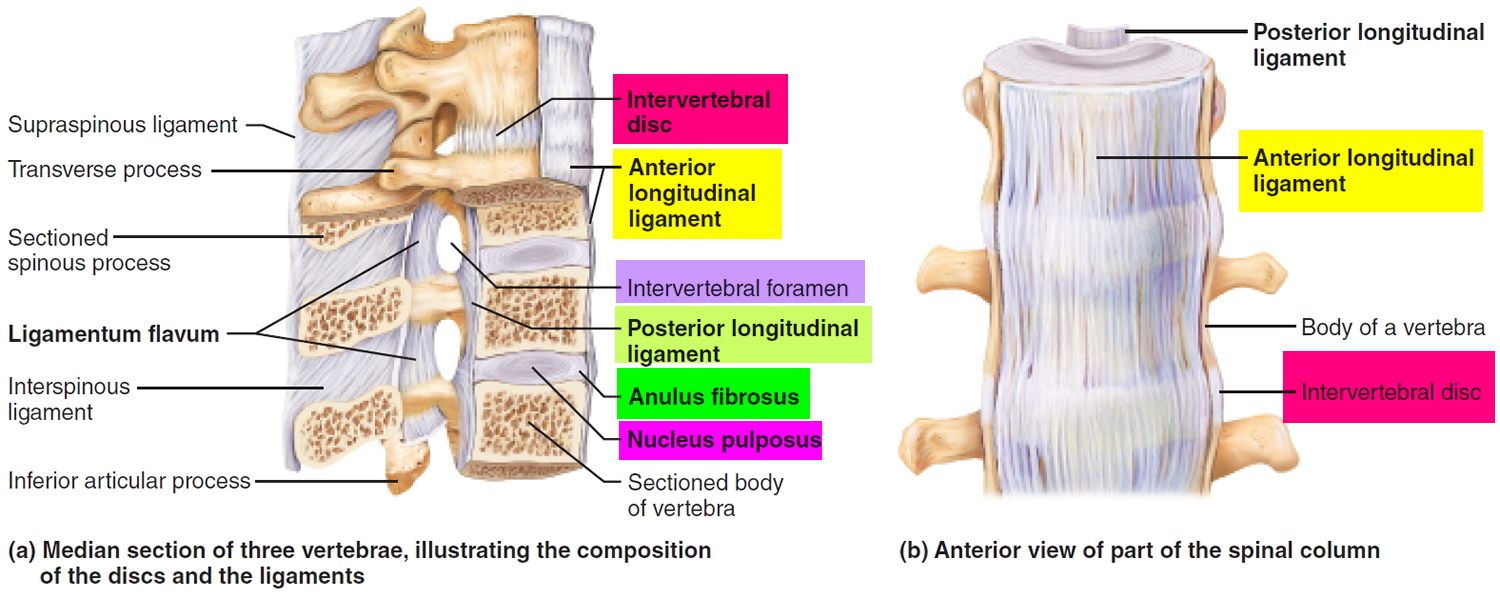
Intervertebral discs (inter- = between) are found between the bodies of adjacent vertebrae from the second cervical (C2) vertebra to the sacrum (see Figures 1 to 4) and collectively, the intervertebral discs account for about 25% to 33% of the height of the vertebral column. There are 25 intervertebral discs (7 cervical, 12 thoracic, 5 lumbar, and 1 sacral). There is no intervertebral disc between C1 and C2, which is unique in the spine 1. Together the vertebrae and the discs surround and protect your spinal cord, the bundle of nerves that connects your brain to the nerves in your body (see Figures 1 and 2). Each intervertebral disc is a cushionlike pad composed of an inner soft, pulpy, highly elastic substance, the nucleus pulposus (pulposus = pulplike) and an outer fibrous ring of about 12 concentric rings consisting of fibrocartilage called the anulus fibrosus (“fibrous ring”) (annulus = ringlike). The main function of these fibrous rings (anulus fibrosus) is to contain the nucleus pulposus (the inner soft, pulpy, highly elastic substance), limiting its expansion when the spine is compressed. However, the fibrocartilage rings (anulus fibrosus) also function like a woven strap, binding the successive vertebrae together, resisting tension on the spine, and absorbing compressive forces.
- The anulus fibrosus is a ring-shaped disc of fibrous connective tissue that surrounds the nucleus pulposus. This structure is highly organized, consisting of 15 to 25 stacked sheets, or “lamellae,” of predominantly collagen, with interspersed proteoglycans, glycoproteins, elastic fibers, and the connective tissue cells that secrete these extracellular matrix products. Each lamella contains collagen uniformly oriented in a plane that differs in orientation to adjacent lamella by about 60 degrees. This alignment leads to the parallel orientation of alternate lamella. This “radial-ply” formation provides exceptional strength compared to an entirely longitudinal setup and has been mimicked in the construction of products such as car tires. The lamellae are interconnected through translamellar bridges. The number of translamellar bridges per unit area is set to achieve a balance between strength and flexibility. A greater number of bridges would provide greater resistance to compressive forces, but would limit flexibility, and vice-versa. The anulus fibrosus contains an inner and an outer portion. They differ primarily in their collagen composition. While both are primarily collagen, the outer annulus contains mostly type I collagen, while the inner has predominantly type II. The inner annulus also contains more proteoglycans than the inner. The ratio of type I to type II changes gradually; as the distance from the nucleus pulposus increases, the amount of type II collagen decreases, while the amount of type I increases. Another major difference between the two segments is the morphology of the connective tissue cells that secrete extracellular matrix. The cells of the inner annulus are described as round, while the outer annulus has a more oblong, fibroblast-like appearance 2.
- The nucleus pulposus fills the center of the intervertebral disc, is gelatinous, and absorbs compression forces between vertebrae. The nucleus pulposus is a gel-like structure that sits at the center of the intervertebral disc and accounts for much of the strength and flexibility of the spine. It is made of 66% to 86% water with the remainder consisting of primarily type II collagen (it may also contain type VI, IX, and XI) and proteoglycans. The proteoglycans include the larger aggrecan and versican that bind to hyaluronic acid, as well as several small leucine-rich proteoglycans. Aggrecan is largely responsible for retaining water within the nucleus pulposus. This structure also contains a low density of cells. While sparse, these cells produce the extracellular matrix (ECM) products (aggrecan, type II collagen, etc.) and maintain the integrity of the nucleus pulposus.
The superior (top) and inferior (bottom) surfaces of the intervertebral disc consist of a thin plate of hyaline cartilage endplates that anchor the discs to adjacent vertebrae 3. Collagen fibers in adjacent rings in the anulus cross like an X, allowing the spine to withstand twisting. This arrangement creates the same antitwisting design provided by bone lamellae in osteons (see Figure 3). Each nucleus pulposus is gelatinous and acts like a rubber ball, enabling the spine to absorb compressive stress.
The intervertebral discs form strong joints, permit various movements of the vertebral column, and absorb vertical shock. Under compression, they flatten and broaden. Degenerative changes in the anulus fibrosus can lead to herniation of the nucleus pulposus. Posterolateral herniation can impinge on the roots of a spinal nerve in the intervertebral foramen.
The intervertebral discs act as shock absorbers during walking, jumping, and running. At points of compression, the discs flatten and bulge out a bit between the vertebrae. The discs are thickest in the lumbar (lower back) and cervical (neck) regions of the vertebral column. As a result of compression and loss of fluid from the gelatinous nucleus pulposus, they flatten somewhat by the end of each day. So, you are probably 1 to 2 centimeters shorter at night than when you awake in the morning.
During the course of a day the discs compress and lose water from their cartilage so that we are a bit shorter at night. While you are sleeping there is less compression and rehydration occurs, so that you are taller when you awaken in the morning. With age, the nucleus pulposus hardens and becomes less elastic. Decrease in vertebral height with age results from bone loss in the vertebral bodies and not a decrease in thickness of the intervertebral discs.
Since intervertebral discs are avascular, the annulus fibrosus and nucleus pulposus rely on blood vessels from the bodies of vertebrae to obtain oxygen and nutrients and remove wastes. Certain stretching exercises, such as yoga, decompress discs and increase general blood circulation, both of which speed up the uptake of oxygen and nutrients by discs and the removal of wastes.
The vertebral column, or spine (see Figure 4), physically supports the skull and trunk, allows for their movement, protects the spinal cord and absorbs stresses produced by walking, running, and lifting. It also provides attachment for the limbs, thoracic cage, and postural muscles. Although commonly called the backbone, it consists of not a single bone but a flexible chain of 33 vertebrae with intervertebral discs of fibrocartilage between most of them. The adult vertebral column averages about 71 cm (28 in.) long, with the intervertebral discs accounting for about one-quarter of the length.
During the course of a day the discs compress and lose water from their cartilage so that we are a bit shorter at night. While you are sleeping there is less compression and rehydration occurs, so that you are taller when you awaken in the morning. With age, the nucleus pulposus hardens and becomes less elastic. Decrease in vertebral height with age results from bone loss in the vertebral bodies and not a decrease in thickness of the intervertebral discs.
Intervertebral disc thickness generally increases from rostral to caudal, except for a nadir at T3-T4. The thickness of the intervertebral discs relative to the size of the vertebral bodies is highest in the cervical and lumbar regions. This reflects the increased range of motion found in those regions.
In the cervical and lumbar regions, the intervertebral discs are thicker anteriorly. This creates the secondary curvature of the spine – the cervical and lumbar lordoses.
Since intervertebral discs are avascular, the annulus fibrosus and nucleus pulposus rely on blood vessels from the bodies of vertebrae to obtain oxygen and nutrients and remove wastes. Certain stretching exercises, such as yoga, decompress discs and increase general blood circulation, both of which speed up the uptake of oxygen and nutrients by discs and the removal of wastes.
While only the outer third of the anulus fibrosus is vascular and innervated in a non-pathologic state, in aging and states of inflammation, nerve growth and granulation tissue growth are stimulated. Additionally, the granulation tissue secretes inflammatory cytokines, which further increases sensitivity to pain sensations.
Two major ligaments support the intervertebral discs. The anterior longitudinal ligament is a broadband that covers the anterolateral surface of the spine from the foramen magnum in the skull to the sacrum. This ligament assists the spine in preventing hyperextension and prevents intervertebral disc herniation in the anterolateral direction. The posterior longitudinal ligament covers the posterior aspect of the vertebral bodies, within the vertebral canal, and serves mainly to prevent a posterior herniation of the intervertebral discs, and is therefore responsible for the most herniations being in the postero-lateral direction.
Figure 1. Intervertebral disc
Figure 2. Structure of typical intervertebral disc
Figure 3. Fibrocartilage of a typical intervertebral disc
Figure 4. Structure of typical vertebral column
Ligaments of the Spine
Like a tremulous telecommunication transmitting tower, the vertebral column cannot stand upright by itself. It must be held in place by an elaborate system of supports. Serving this role are the straplike ligaments of the back and the muscles of the trunk.
The major supporting ligaments are the anterior and posterior longitudinal ligaments (Figure 5) that run vertically along the anterior and posterior surfaces of the bodies of the vertebrae, from the neck to the sacrum. The anterior longitudinal ligament is wide and attaches strongly to both the bony vertebrae and the intervertebral discs. Along with its supporting role, this thick anterior ligament prevents hyperextension of the back (bending too far backward). The posterior longitudinal ligament, which is narrow and relatively weak, attaches only to the intervertebral discs. This ligament helps to prevent hyperflexion (bending the vertebral column too sharply forward).
Several other posterior ligaments connect each vertebra to those immediately superior and inferior (Figure 5 a). Among these is the ligamentum flavum (fla vum; “yellow”), which connects the lamina of adjacent vertebrae. It contains elastic connective tissue and is especially strong: It stretches as you bend forward, then recoils as you straighten to an erect position.
Figure 5. Ligaments of the spine
Herniated (prolapsed) disc causes
The cause will depend on your type of spinal disc problem, such as prolapsed disc or degenerative disc disease.
Disc herniation is most often the result of a gradual, aging-related wear and tear called disc degeneration. As you age, your spinal discs lose some of their water content. That makes them less flexible and more prone to tearing or rupturing with even a minor strain or twist.
Most people can’t pinpoint the exact cause of their herniated disc. Sometimes, using your back muscles instead of your leg and thigh muscles to lift large, heavy objects can lead to a herniated disc, as can twisting and turning while lifting. Rarely, a traumatic event such as a fall or a blow to the back can cause a herniated disc.
The true cause is usually not known, but it is more common in people who:
- are middle-aged or older
- are male
- lift heavy objects
- are overweight or obese. Excess body weight causes extra stress on the discs in your lower back.
- do repetitive actions involving bending or twisting
- Occupation. People with physically demanding jobs have a greater risk of back problems. Repetitive lifting, pulling, pushing, bending sideways and twisting also may increase your risk of a herniated disc.
- sit in the same position for a long time regularly
- live an inactive lifestyle
- smoke
- Genetics. Some people inherit a predisposition to developing a herniated disc.
Causes of degenerative disc disease
This condition is more common as you age. People who have had spinal injuries or infections are also more likely to get degenerative disc disease.
Prevention of spinal disc problems and back injury
There’s not much you can do to prevent a herniated disc. It is often caused by natural aging and deterioration. To keep your discs and back in good working order, work on living a healthy lifestyle:
- Keeping your body in the correct posture
- Avoiding heavy lifting
- Maintain a healthy weight.
- Exercise regularly.
- Regularly doing exercises to strengthen your core stomach and back muscles.
- void repetitive movements.
- If you sit all day make sure you have correct sitting position and get up and walk around every hour.
- Practice safe lifting and bending techniques.
If you have undiagnosed back problems, see your doctor.
Herniated disc complications
Your spinal cord doesn’t extend into the lower portion of your spinal canal. Just below your waist, the spinal cord separates into a group of long nerve roots (cauda equina) that resemble a horse’s tail. Rarely, disc herniation can compress the entire cauda equina. Emergency surgery may be required to avoid permanent weakness or paralysis.
Seek emergency medical attention if you have:
- Worsening symptoms. Pain, numbness or weakness may increase to the point that you can’t perform your usual daily activities.
- Bladder or bowel dysfunction. People who have cauda equina syndrome may become incontinent or have difficulty urinating even with a full bladder.
- Saddle anesthesia. This progressive loss of sensation affects the areas that would touch a saddle — the inner thighs, back of legs and the area around the rectum.
Herniated disc in neck
Herniated disc in neck is also known as cervical radiculopathy, commonly called a “pinched nerve”, occurs when a nerve in your neck is compressed or irritated where it branches away from the spinal cord. This may cause pain that radiates into your shoulder, as well as muscle weakness and numbness that travels down your arm and into your hand.
Herniated disc in neck (cervical radiculopathy) is often caused by “wear and tear” changes that occur in the spine as you age, such as arthritis. In younger people, it is most often caused by a sudden injury that results in a herniated disc.
In most cases, herniated disc in neck or cervical radiculopathy responds well to conservative treatment that includes medication and physical therapy.
Herniated disc in neck cause
Herniated disc in neck (cervical radiculopathy) most often arises from degenerative changes that occur in your spine as you age or from an injury that causes a herniated, or bulging, intervertebral disc.
- Degenerative changes. As the discs in the spine age, they lose height and begin to bulge. They also lose water content, begin to dry out, and become stiffer. This problem causes settling, or collapse, of the disc spaces and loss of disc space height. As the discs lose height, the vertebrae move closer together. The body responds to the collapsed disc by forming more bone —called bone spurs—around the disc to strengthen it. These bone spurs contribute to the stiffening of the spine. They may also narrow the foramen—the small openings on each side of the spinal column where the nerve roots exit—and pinch the nerve root. Degenerative changes in the discs are often called arthritis or spondylosis. These changes are normal and they occur in everyone. In fact, nearly half of all people middle-aged and older have worn discs and pinched nerves that do not cause painful symptoms. It is not known why some patients develop symptoms and others do not.
- Herniated disc. A disc herniates when its jelly-like center (nucleus) pushes against its outer ring (annulus). If the disc is very worn or injured, the nucleus may squeeze all the way through. When the herniated disc bulges out toward the spinal canal, it puts pressure on the sensitive nerve root, causing pain and weakness in the area the nerve supplies. A herniated disc often occurs with lifting, pulling, bending, or twisting movements.
Herniated disc in neck symptoms
In most cases, the pain of herniated disc in neck or cervical radiculopathy starts at the neck and travels down the arm in the area served by the damaged nerve. This pain is usually described as burning or sharp. Certain neck movements—like extending or straining the neck or turning the head—may increase the pain. Other symptoms include:
- Tingling or the feeling of “pins and needles” in the fingers or hand
- Weakness in the muscles of the arm, shoulder, or hand
- Loss of sensation
Some patients report that pain decreases when they place their hands on top of their head. This movement may temporarily relieve pressure on the nerve root.
Herniated disc in neck diagnosis
Your doctor will ask you questions about your symptoms and give you an exam. He or she will check you for numbness, weakness, reflexes changes, and pain. They will probably order X-rays or other pictures to see if you have a herniated disc. These could include a CT scan or an MRI. There are also nerve tests your doctor can order. These can determine what nerves are involved, if there is nerve damage, and how well your nerves are conducting feelings.
- Physical Examination
After discussing your medical history and general health, your doctor will ask you about your symptoms. He or she will then examine your neck, shoulder, arms and hands—looking for muscle weakness, loss of sensation, or any change in your reflexes.
Your doctor may also ask you to perform certain neck and arm movements to try to recreate and/or relieve your symptoms.
- Tests
X-rays. These provide images of dense structures, such as bone. An x-ray will show the alignment of bones along your neck. It can also reveal whether there is any narrowing of the foramen and damage to the discs.
Computed tomography (CT) scans. More detailed than a plain x-ray, a CT scan can help your doctor determine whether you have developed bone spurs near the foramen in your cervical spine.
Magnetic resonance imaging (MRI) scans. These studies create better images of the body’s soft tissues. An MRI of the neck can show if your nerve compression is caused by damage to soft tissues—such as a bulging or herniated disc. It can also help your doctor determine whether there is any damage to your spinal cord or nerve roots.
Electromyography (EMG). Electromyography measures the electrical impulses of the muscles at rest and during contractions. Nerve conduction studies are often done along with EMG to determine if a nerve is functioning normally. Together, these tests can help your doctor determine whether your symptoms are caused by pressure on spinal nerve roots and nerve damage or by another condition that causes damage to nerves, such as diabetes.
Herniated disc in neck treatment
It is important to note that the majority of patients with herniated disc in neck or cervical radiculopathy get better over time and do not need treatment. For some patients, the pain goes away relatively quickly—in days or weeks. For others, it may take longer.
It is also common for herniated disc in neck or cervical radiculopathy that has improved to return at some point in the future. Even when this occurs, it usually gets better without any specific treatment.
In some cases, herniated disc in neck or cervical radiculopathy does not improve, however. These patients require evaluation and treatment.
Nonsurgical Treatment
Initial treatment for cervical radiculopathy is nonsurgical. Nonsurgical treatment options include:
Soft cervical collar. This is a padded ring that wraps around the neck and is held in place with Velcro. Your doctor may advise you to wear a soft cervical collar to allow the muscles in your neck to rest and to limit neck motion. This can help decrease the pinching of the nerve roots that accompany movement of the neck. A soft collar should only be worn for a short period of time since long-term wear may decrease the strength of the muscles in your neck.
Physical therapy. Specific exercises can help relieve pain, strengthen neck muscles, and improve range of motion. In some cases, traction can be used to gently stretch the joints and muscles of the neck.
Medications. In some cases, medications can help improve your symptoms.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs, including aspirin, ibuprofen, and naproxen, may provide relief if your pain is caused by nerve irritation or inflammation.
- Oral corticosteroids. A short course of oral corticosteroids may help relieve pain by reducing swelling and inflammation around the nerve.
- Steroid injection. In this procedure, steroids are injected near the affected nerve to reduce local inflammation. The injection may be placed between the laminae (epidural injection), in the foramen (selective nerve injection), or into the facet joint. Although steroid injections do not relieve the pressure on the nerve caused by a narrow foramen or by a bulging or herniated disc, they may lessen the swelling and relieve the pain long enough to allow the nerve to recover.
- Narcotics. These medications are reserved for patients with severe pain that is not relieved by other options. Narcotics are usually prescribed for a limited time only.
Surgical Treatment
If after a period of time nonsurgical treatment does not relieve your symptoms, your doctor may recommend surgery. There are several surgical procedures to treat cervical radiculopathy. The procedure your doctor recommends will depend on many factors, including what symptoms you are experiencing and the location of the involved nerve root.
Herniated disc in neck or cervical radiculopathy Surgical Treatment Options
When symptoms of cervical radiculopathy persist or worsen despite nonsurgical treatment, your doctor may recommend surgery.
The primary goal of surgery is to relieve your symptoms by decompressing, or relieving pressure on, the compressed nerves in your neck. Other goals of surgery include:
- Improving neck pain
- Maintaining stability of the spine
- Improving alignment of the spine
- Preserving range of motion in the neck
In most cases, surgery for cervical radiculopathy involves removing pieces of bone or soft tissue (such as a herniated disc)—or both. This relieves pressure by creating more space for the nerves to exit the spinal canal.
Complications
As with any surgical procedure, there are risks associated with cervical spine surgery. Possible complications can be related to the approach used, the bone graft, healing, and long-term changes. Before your surgery, your doctor will discuss each of the risks with you and will take specific measures to help avoid potential complications.
General Risks
The possible risks and complications for any cervical spine surgery include:
- Infection
- Bleeding
- Nerve injury
- Spinal cord injury
- Reaction to anesthesia
- The need for additional surgery in the future
- Failure to relieve symptoms
- Tear of the sac covering the nerves (dural tear)
- Life-threatening medical problems, such as heart attack, lung complications, or stroke
Anterior Cervical Diskectomy and Fusion and Artificial Disk Replacement Risks
There are additional potential risks and complications when an anterior approach is used in spine surgery. They include:
- Misplaced, broken, or loosened plates, screws, or implants
- Soreness or difficulty with swallowing
- Voice changes
- Breathing difficulty
- Injury to the esophagus
- Pain at the site the bone was taken from—if an autograft is used
- Nonunion of the spinal fusion (in Anterior Cervical Diskectomy and Fusion)
Herniated disc in neck surgical procedures
There are three surgical procedures commonly performed to treat cervical radiculopathy. They are:
- Anterior Cervical Diskectomy and Fusion
- Artificial Disk Replacement
- Posterior Cervical Laminoforaminotomy
The procedure your doctor recommends will depend on a number of factors–most importantly, the type and location of your problem. Other factors include:
- Your preference for a procedure
- Your doctor’s preference and experience
- Your overall health and medical history (including whether you have had prior neck surgery)
Anterior Cervical Diskectomy and Fusion
Anterior Cervical Diskectomy and Fusion is the most commonly performed procedure to treat cervical radiculopathy. The procedure involves removing the problematic disc or bone spurs and then stabilizing the spine through spinal fusion.
The goals of anterior cervical diskectomy and fusion are to:
- Restore alignment of the spine
- Maintain the space available for the nerve roots to leave the spine
- Limit motion across the degenerated segment of the spine
Procedure. An “anterior” approach means that the doctor will approach your neck from the front. He or she will operate through a 1- to 2-inch incision along the neck crease. The exact location and length of your incision may vary depending on your specific condition.
During the procedure, your doctor will remove the problematic disc and any additional bone spurs, if necessary. The disc space is restored to the height it was prior to the disc wearing out. This makes more room for the nerves to leave the spine and aids in decompression.
Spinal fusion. After the disc space has been cleared out, your doctor will use spinal fusion to stabilize your spine. Spinal fusion is essentially a “welding” process. The basic idea is to fuse together the vertebrae so that they heal into a single, solid bone. Fusion eliminates motion between the degenerated vertebrae and takes away some spinal flexibility. The theory is that if the painful spine segments do not move, they should not hurt.
All spinal fusions use some type of bone material, called a bone graft, to help promote the fusion. The small pieces of bone are placed into the space left where the disc has been removed. Sometimes larger, solid pieces are used to provide immediate structural support to the vertebrae.
In some cases, the doctor may implant a metal, plastic, or bone spacer between the two adjoining vertebrae. This spacer, or “cage,” usually contains bone graft material to allow a spinal fusion to occur between the two vertebrae.
After the bone graft is placed or the cage is inserted, your doctor will use metal screws, plates and rods to increase the rate of fusion and further stabilize the spine.
Bone graft sources. The bone graft will come from either your own bone (autograft) or from a donor (allograft). If an autograft is used, the bone is usually taken from your hip area. Harvesting the bone graft requires an additional incision during your surgery. It lengthens surgical time and may cause increased pain after the operation. Your doctor will talk to you about the advantages and disadvantages of using an autograft versus an allograft, as well as a traditional bone graft versus a cage.
Artificial Disc Replacement
This procedure involves removing the degenerated disc and replacing it with artificial parts, as is done in hip or knee replacement. The goal of disc replacement is to allow the spinal segment to keep some flexibility and maintain more normal motion.
Similar to anterior cervical diskectomy and fusion, your doctor will use an “anterior” approach for the surgery—making a 1- to 2-inch incision along the neck crease. The exact location and length of your incision may vary depending on your specific condition.
During the surgery, your doctor will remove your problematic disc and then insert an artificial disc implant into the disc space. The implant is made of all metal or metal and plastic. It is designed to maintain the motion between the vertebrae after the degenerated disc has been removed. The implant may help restore the height between the vertebrae and widen the passageway for the nerve roots to exit the spinal canal.
Although no longer considered a new technology, the development of Artificial Disk Replacement is more recent than that of Anterior Cervical Diskectomy and Fusion. To date, the outcomes of Artificial Disk Replacement surgery are promising and are comparable to that of Anterior Cervical Diskectomy and Fusion surgery. The long-term outcomes are still being researched.
Artificial Disk Replacement may be an option for you—depending on the type and location of your problem. Your doctor will talk with you about your options.
Posterior Cervical Laminoforaminotomy
“Posterior” refers to the back part of your body. In this procedure, the doctor will make a 1- to 2-inch incision along the midline of the back of the neck. The exact location and size of your scar may vary depending on your condition.
During a posterior cervical laminoforaminotomy, the doctor uses a burr and other specialized tools to thin down the lamina—the bony arch that forms the backside of the spinal canal. Removing this allows the doctor better access to the damaged nerve.
He or she then removes the bone, bone spurs, and tissues that are compressing the nerve root. If your compression is due to a herniated disc, your doctor will remove the portion of the disc that is compressing the nerve, as well.
Unlike anterior cervical diskectomy and fusion, posterior cervical laminoforaminotomy does not require spinal fusion to stabilize the spine. Because of this, you will maintain better range of motion in your neck and your recovery will be quicker.
The procedure can be performed as open surgery, in which your doctor uses a single, larger incision to access your spine. It can also be done using a minimally invasive method, where several smaller incisions are made. Your doctor will discuss with you whether posterior cervical laminoforaminotomy is an option for you and, if so, how the surgery will be performed.
Recovery
After surgery, you will typically stay in the hospital for 1 or 2 days. This will vary, however, depending on the type of surgery you have had and how many disc levels were involved.
Most patients are able to walk and eat on the first day after surgery. It is normal to have difficulty swallowing solid foods for a few weeks or have some hoarseness following anterior cervical spine surgery.
You may need to wear a soft or a rigid cervical collar at first. How long you should wear it will depend on the type of surgery you have had.
After spinal fusion, it may take from 6 to 12 months for the bone to become solid. Because of this, your doctor will give you specific restrictions for some time period after your surgery. Right after your operation, your doctor may recommend only light activity, like walking. As you regain strength, you will be able to slowly increase your activity level.
Physical Therapy
Usually by 4 to 6 weeks, you can gradually begin to do range-of-motion and strengthening exercises. Your doctor may prescribe physical therapy during the recovery period to help you regain full function.
Return to Work
Most people are able to return to a desk job within a few days to a few weeks after surgery. They may be able to return to full activities by 3 to 4 months, depending on the procedure. For some people, healing may take longer.
Outcomes
Most patients experience favorable outcomes after surgery for cervical radiculopathy. In most cases, they experience relief from their pain and other symptoms and are able to successfully return to the activities of daily life after a period of recovery.
Herniated disc lower back
Sometimes called a slipped or ruptured disc, a herniated disc most often occurs in your lower back. It is one of the most common causes of low back pain, as well as leg pain (sciatica).
Between 60% and 80% of people will experience low back pain at some point in their lives 4. A high percentage of people will have low back and leg pain caused by a herniated disc. Approximately 95% of disc herniations in the lumbar area occur at L4-L5 or L5-S1 5, 6. Herniated disc lower back or lumbar disc herniation is relatively common, with 5 to 20 cases per 1000 adults annually. Herniated disc lower back is most prevalent in the 3rd to the 5th decade of life, with a male to female ratio of 2 to 1 7.
In many cases, a herniated disc in the lower back is related to the natural aging of your spine.
A recent meta-analysis concluded that a clinical diagnosis of lumbar disc herniation with radiculopathy, could be made with a straight leg raise screening test, if also Hancock rule requirement is met (having three positives out of the four following findings: dermatomal pain in the nerve root distribution, and associated sensory deficit, reflex abnormality, and motor weakness) 7, 8. Muscle weakness is present in up to 37%, absent ankle reflexes in up to 40%, and absent knee reflexes in 18% of patients 9, 10, 11.
Although a herniated disc can sometimes be very painful, most people feel much better with just a few weeks or months of nonsurgical treatment. Patients who do not respond to conservative therapies will likely need an magnetic resonance imaging (MRI) for further evaluation and characterization of nerve root involvement. Referral to a specialist for interventional therapies such as an epidural steroid injection or surgical decompression may be considered, depending on the severity of symptoms 12.
Herniated disc lower back cause
Disc degeneration is usually associated with herniated disc lower back . With aging, the disc fibrochondrocytes undergo senescence and a reduction in proteoglycans production 13. This reduction in proteoglycans leads to dehydration and disc collapse, increasing the strain on the annulus fibrosus, resulting in tears and fissures, and consequentially facilitating the nucleus pulposus herniation 13. Therefore, when repetitive mechanical stressors are applied on the disc, it results in a gradual onset of symptoms that tend to be chronic.
On the other hand, axial overloading applies a large biomechanical force on the healthy disc, which may result in extrusion of disc material through a failing annulus fibrosus. Those injuries usually result in more severe acute symptoms 14. Other less common causes are connective tissue disorders and congenital disorders like short pedicles 15.
Herniated disc lower back risk factors
In addition to the gradual wear and tear that comes with aging, other factors can increase the likelihood of a herniated disc. Knowing what puts you at risk for a herniated disc can help you prevent further problems.
- Gender. Men between the ages of 30 and 50 are most likely to have a herniated disc.
- Improper lifting. Using your back muscles to lift heavy objects, instead of your legs, can cause a herniated disc. Twisting while you lift can also make your back vulnerable. Lifting with your legs, not your back, may protect your spine.
- Weight. Being overweight puts added stress on the discs in your lower back.
- Repetitive activities that strain your spine. Many jobs are physically demanding. Some require constant lifting, pulling, bending, or twisting. Using safe lifting and movement techniques can help protect your back.
- Frequent driving. Staying seated for long periods, plus the vibration from the car engine, can put pressure on your spine and discs.
- Sedentary lifestyle. Regular exercise is important in preventing many medical conditions, including a herniated disc.
- Smoking. It is believed that smoking lessens oxygen supply to the disc and causes more rapid degeneration.
Herniated disc lower back symptoms
For most people with a herniated disc, low back pain is the initial symptom. This pain may last for a few days, then improve. It is often followed by the eventual onset of leg pain, numbness, or weakness. This leg pain typically extends below the knee, and often into the foot and ankle. It is described as moving from the back or buttock down the leg into the foot.
Symptoms may be one or all of the following:
- Back pain
- Leg and/or foot pain (sciatica)
- Numbness or a tingling sensation in the leg and/or foot
- Weakness in the leg and /or foot
- Loss of bladder or bowel control (extremely rare) This may indicate a more serious problem called cauda equina syndrome. This condition is caused by the spinal nerve roots being compressed. It requires immediate medical attention.
Not all patients will experience pain as a disc degenerates. It remains a great challenge for the doctor to determine whether a disc that is wearing out is the source of a patient’s pain.
Herniated disc lower back diagnosis
Your doctor will ask you questions about your symptoms and give you an exam. He or she will check you for numbness, weakness, reflexes changes, and pain. They will probably order X-rays or other pictures to see if you have a herniated disc. These could include a CT scan or an MRI. There are also nerve tests your doctor can order. These can determine what nerves are involved, if there is nerve damage, and how well your nerves are conducting feelings.
Herniated disc lower back treatment
In the majority of cases, a herniated lumbar disc will slowly improve over a period of several days to weeks. Typically, most patients are free of symptoms by 3 to 4 months. However, some patients do experience episodes of pain during their recovery.
Considerations
Regardless of the kind of treatment prescribed, there is a 5% chance of the disc herniating again.
The risk of nonsurgical treatment is that your symptoms may take a long time to resolve. If after about 6 months, you elect to have surgery, the final outcome may not be as good as if you had elected surgery earlier.
Nonsurgical Treatment
Unless there are neurological deficits — muscle weakness, difficulty walking — or cauda equina syndrome, conservative care is the first course of treatment. Because it is not clear that nonsurgical care is any better than letting the condition resolve on its own, the focus is on providing pain relief.
Common nonsurgical measures include:
- Rest. Usually 1-2 days of bed rest will calm severe back pain. Do not stay off your feet for longer, though. Take rest breaks throughout the day, but avoid sitting for long periods of time. Make all your movements slow and controlled. Change your daily activities so that you avoid movements that can cause further pain, especially bending forward and lifting.
- Anti-inflammatory medications. Medicines like ibuprofen or naproxen may relieve pain.
- Physical therapy. Specific exercises can strengthen your lower back and abdominal muscles.
- Epidural steroid injection. In this procedure, steroids are injected into your back to reduce local inflammation.
Of the above measures, only epidural injections have been proven effective at reducing symptoms. There is good evidence that epidural injections can be successful in 42-56% of patients who have not been helped by 6 weeks or more of other nonsurgical care.
Overall, the most effective nonsurgical care for lumbar herniated disc includes observation and an epidural steroid injection for short-term pain relief.
Surgical Treatment
Only a small percentage of patients with lumbar disc herniations require surgery. Spine surgery is typically recommended only after a period of nonsurgical treatment has not relieved painful symptoms.
- Microdiskectomy. The most common surgical procedure for a herniated disc in the lower back is a lumbar microdiskectomy. Microdisketomy involves removing the herniated part of the disc and any fragments that are putting pressure on the spinal nerve.
- Rehabilitation. Most patients do not require formal physical therapy after surgery. After your surgeon evaluates you and confirms that your incision is healed, you may begin a rehabilitation exercise program. A simple walking program 30 minutes each day, along with flexibility exercises for the back and legs, can be done as a home program. If needed, your surgeon will refer you to a physical therapist.
The risk of surgical complications may include:
- Infection
- Nerve damage
- Dural leak — An opening of the thin lining of the nerve root canal may cause loss of the watery liquid (cerebrospinal fluid) that bathes the nerves roots. When seen during surgery, the lining may be repaired. Sometimes headaches occur afterward, but typically improve with time.
- Hematoma causing nerve compression — This is caused by blood collecting around the nerve roots after the surgery.
- Recurrent disc herniation — another piece of disc material may break off at the same site and cause the leg pain to return. This may be managed with conservative treatment, but another surgery may be necessary.
Outcomes
The results of microdiskectomy surgery are generally very good. The outcome of leg pain improvement is much more reliable than back pain and therefore this surgery is rarey performed for back pain only.
Most patients notice improvement over the first several weeks following surgery, but may also experience continued improvement over several months. Pain is typically the first symptom to improve, followed by improvement in overall strength of the leg, and then sensation. It is common for some patients to state that although pain symptoms are better, they still have a numb spot on their leg or foot.
Most patients will slowly resume normal daily activities over the first several weeks following surgery.
Over the last several years, there has been extensive research on lumbar disc surgery and patient improvement. One of the most publicized research projects in this area is the Spinal Patient Outcomes Research Trial (SPORT). The study followed patients with herniated disc from across the country. Half were treated with conservative measures, and half with surgery.
The initial outcomes for patients treated with surgery were much better than those who followed conservative treatment, including improvement in pain relief and function. At the 2-year follow-up, patients treated with surgery again showed improvements over those treated conservatively. However, over the course of the study, numerous patients did change their treatments. Your surgeon will be best able to explain what the actual study results are with any recommended approach for you.
Herniated disc symptoms
When part of a disc presses on a nerve, it can cause pain. Often the pain occurs on one side of your body. Where the pain is located depends on where the herniated disc is located.
You also can have a herniated disc without knowing it — herniated discs sometimes show up on spinal images of people who have no symptoms of a disc problem.
A slipped disc in the cervical section of your spine can cause pain in your neck and arms. You could experience:
- Pain when moving your neck.
- Pain near the shoulder blade.
- Shooting pain down the arm and into the fingers.
- Numbness in the shoulder, elbow, forearm, or fingers.
Nerve pain can happen if the affected disc is pressing on a nerve. A slipped disc in the lumbar part of your spine can cause pain in the back and legs. It is often referred to as sciatica. This is because the disc pushes on the sciatic nerve. The sciatic nerve travels from your hip and buttock down your legs. The pain can be sudden and sharp, and move down the nerve to your leg, calf and even foot, causing numbness and tingling. Symptoms include:
- Pain in the leg, hip, or buttocks.
- Numbness or tingling in these areas.
- Pain or numbness in the back of the calf or sole of the foot.
- Weakness in one leg.
How bad the symptoms are depends on how much of the disc is pressing on the nerve.
The pain from a herniated disc is usually worse when you’re active and gets better when you’re resting. Coughing, sneezing, sitting, driving, and bending forward may make the pain worse. The pain gets worse because these movements put more pressure on the nerve. People who have painful herniated discs often try to change positions to reduce the pain.
Herniated disc diagnosis
Your doctor will ask you questions about your symptoms and give you an exam.
After discussing your symptoms and medical history, your doctor will examine your spine, check you for numbness, weakness, reflexes, and pain. During the physical examination, your doctor may conduct the following tests to help determine the cause of your low back pain.
Neurological examination. A physical examination should include a neurological examination to detect weakness or sensory loss. To test muscle weakness, your doctor will assess how you walk on your heels and toes. Your thigh, ankle, and toe strength may also be tested. Your doctor can detect any loss of sensation by checking whether you are numb to light touch in the leg and foot. In addition, your reflexes at the knee and ankle will be tested, and sometimes may be absent.
Straight leg raise (SLR) test. This test is a very accurate predictor of a disc herniation in patients under the age of 35. In this test, you lie on your back and your doctor lifts your affected leg. Your knee stays straight. If you feel pain down your leg and below the knee, you test positive for a herniated disc.
The straight leg raise (SLR) is positive when it reproduces the patient’s symptoms (pain and paresthesia) at an angle lower than 45 degrees with radiation below the knee (Lasegue sign). It is most helpful in diagnosing L4, L5, and S1 radiculopathies. The patient is asked to dorsiflex the foot while the examiner is raising the leg (Bragaad’s sign) to increase the sensitivity of the test.
L1 nerve root exits at the L1-L2 foramina, assessed with a cremasteric reflex (male). When compressed by a herniated disc, it causes pain, and sensory loss in the inguinal region rarely causes weakness in the hip flexion.
The L2 and L3 nerve roots exit at the L2-L3 and L3-L4 foramina, respectively. Symptoms worsen with sneezing, coughing, or leg straightening.
L4 nerve root exits at the L4-L5 foramina. L4 has a reflex assessed with a patellar reflex. When compressed by a herniated disc, it causes back pain that radiates into the anterior thigh and the medial aspect of the leg, accompanied with sensory loss in the same distribution, weakness in the hip flexion and adduction, weakness in knee extension, and a decreased patellar reflex.
L5 nerve root exits at the L5-S1 foramina. When compressed by a herniated disc, it causes back pain that radiates into the buttock, lateral thigh, lateral calf, the dorsum of the foot, and the great toe. Sensory loss is present on the web space between the big toe and second toe, the dorsum of the foot, and lateral calf. There is a weakness in hip abduction, knee flexion, foot dorsiflexion, big toe dorsiflexion, foot inversion, and eversion. Patients present with decreased semitendinosus/semimembranosus reflex. Weakness in foot dorsiflexion makes it challenging to walk on the heels. Chronic L5 radiculopathy may cause atrophy of the extensor digitorum brevis and the tibialis anterior of the anterior leg.
S1 nerve root exits at the S1-S2 foramina, assessed with the Achilles reflex. When compressed with a herniated disc, it presents with sacral or buttock pain that radiates into the posterolateral thigh, the calf, plantar or lateral foot or the perineum. Sensory loss is present on the calf, lateral, or plantar aspect of the foot. There is weakness on foot plantar flexion, hip extension, and flexion of the knee. Weakness in foot plantar flexion causes an inability to tiptoe walk. It could also cause urinary and fecal incontinence and sexual dysfunction 15, 16, 17.
Your doctor will probably order X-rays or imaging tests to see whether you have a herniated disc. These could include a CT scan, an MRI scan or a myelogram. A myelogram is where a dye is injected into the spinal fluid, and then X-rays are taken. This test can show pressure on your spinal cord or nerves due to multiple herniated discs or other conditions. This is to rule out any potential rare causes, including spinal cancer, bone growths (spurs), fracture or narrowing of spinal canal (stenosis). There are also nerve tests your doctor can order. These can determine what nerves are involved, if there is nerve damage, and how well your nerves are conducting feelings.
Herniated disc differential diagnosis
The differential diagnoses for a herniated disc include 15:
- Discal cyst
- Mechanical back pain
- Degenerative spinal stenosis
- Epidural abscess
- Epidural hematoma
- Metastasis
- Diabetic amyotrophy
- Neurinoma
- Osteophytes
- Cauda equina syndrome
- Synovial cyst
Herniated disc treatment
There are a number of steps that can be taken to treat a herniated disc.
Conservative treatment — mainly avoiding painful positions and following a planned exercise and pain-medication regimen — relieves symptoms in most people within a few days or weeks.
Medications
Your doctor may recommend over-the-counter pain medicine like acetaminophen (Tylenol, others) ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve). He or she may prescribe you pain medicine, such as a narcotic, to help with severe pain. They may also give you muscle relaxants to help relieve muscle spasms that can increase pain.
Narcotics (Opioids). If your pain doesn’t improve with over-the-counter medications, your doctor might prescribe opioids (narcotics), such as codeine or an oxycodone-acetaminophen combination (Percocet, OxyContin, others), for a short time. Sedation, nausea, confusion and constipation are possible side effects from these drugs. However, because of the side effects of opioids (narcotics) and the potential for addiction, many health care professionals hesitate to prescribe them for disc herniation.
Neuropathic drugs. These drugs affect nerve impulses to decrease pain. The drugs originally designed to control seizures also may be helpful in the treatment of the radiating nerve pain often associated with a herniated disc. They include gabapentin (Horizant, Neurontin), pregabalin (Lyrica), duloxetine (Cymbalta), or venlafaxine (Effexor XR).
Muscle relaxers. You might be prescribed these if you have muscle spasms. Sedation and dizziness are common side effects.
Cortisone injections (steroid injections). If your pain doesn’t improve with oral medicines, your doctor might recommend a corticosteroid injection or steroid injection. These are shots of steroids that are injected directly into the area around the spinal nerves. Spinal imaging can help guide the needle. The steroids reduce the swelling around the disc and can lessen the pain. Sometimes 1 injection is enough. Often, they are given in a series of shots over a few weeks. These injections can bring relief for weeks or months at a time.
Physical therapy
Certain exercises can be helpful for a herniated disc. The goal of exercise is to make your back and stomach muscles stronger. This will ease the pressure on your disc and make you hurt less. Ask your doctor or physical therapist about exercises for your back. Your doctor may want you to see a physical therapist to learn about safe back exercises.
Physiotherapists usually recommend movement and exercise to help improve your mobility and function. This may include:
- exercises designed to improve movement and strength in a specific part of the body – these usually need to be repeated regularly for a set length of time
- activities that involve moving your whole body, such as walking or swimming – these can help if you’re recovering from an operation or injury that affects your mobility
- exercises carried out in warm, shallow water (hydrotherapy or aquatic therapy) – the water can help relax and support the muscles and joints, while providing resistance to help you gradually strengthen
- advice and exercises to help you increase or maintain your physical activity – advice will be given on the importance of keeping active, and how to do this in a safe, effective way
- providing mobility aids – such as crutches or a walking stick to help you move around
Your physiotherapist may also recommend exercises that you can continue doing to help you manage pain in the long term or reduce your risk of injuring yourself again.
Herniated disc exercises
Exercise is the most important way that you can:
- Ease stiffness and pain build up muscle strength and stamina
- Improve your flexibility and general fitness.
If your back pain lasts a while, lack of movement can cause the muscles to become weak. This makes it more likely that you’ll strain them in future. It’s important that you don’t rest for too long and keep moving.
Your pain should ease within 2 weeks and you should recover over approximately a 4–6 week period. You should carry on with the exercises for at least 6–8 weeks to help prevent another injury. If the pain is severe or not improving after a week or so, see your doctor.
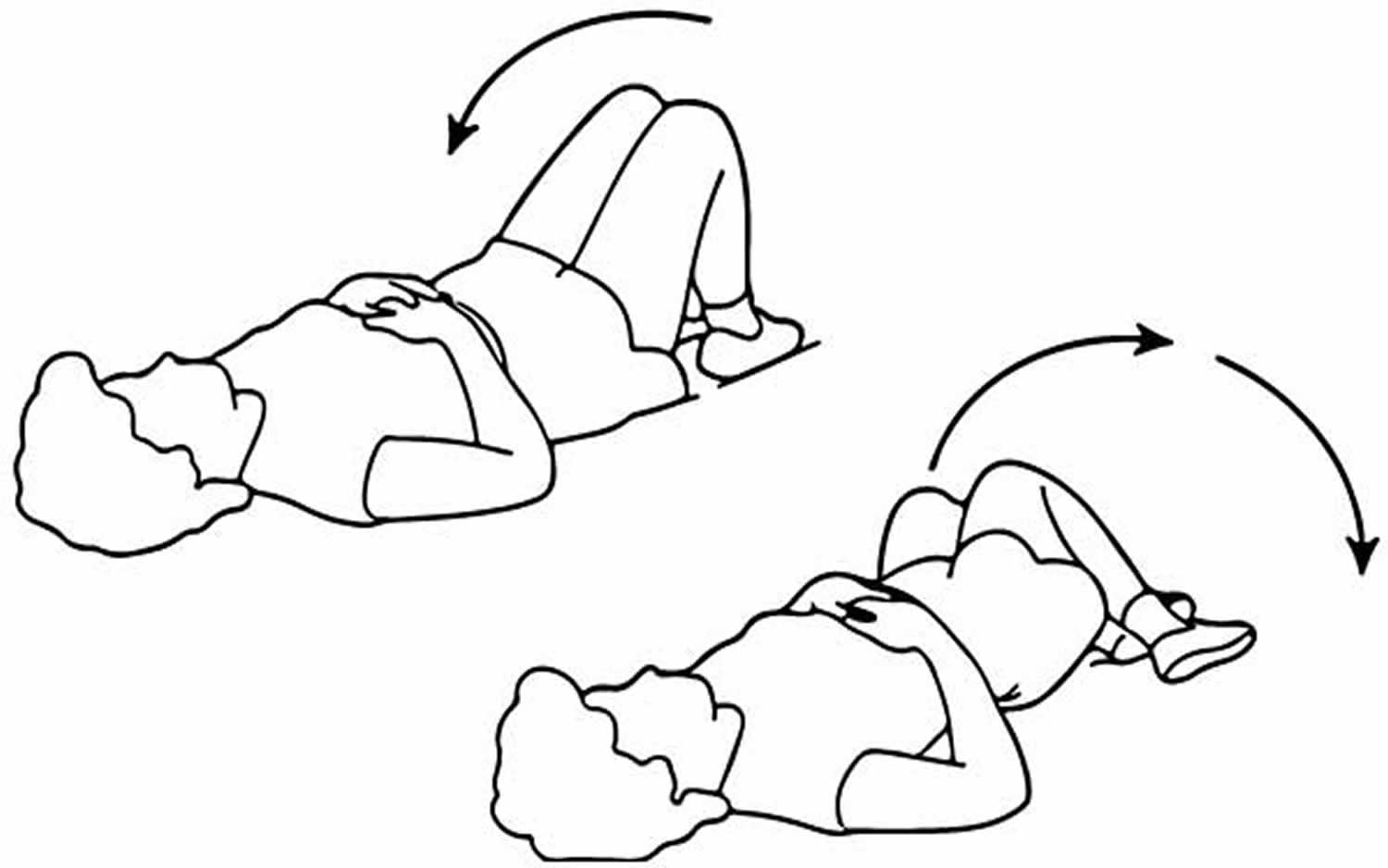
- Back stretch
Lie on your back, hands above your head. Bend your knees and roll them slowly to one side, keeping your feet on the floor. Hold for 10 seconds. Repeat 3 times on each side. Note your upper knee should be directly above lower knee.
Figure 6. Lower back stretch
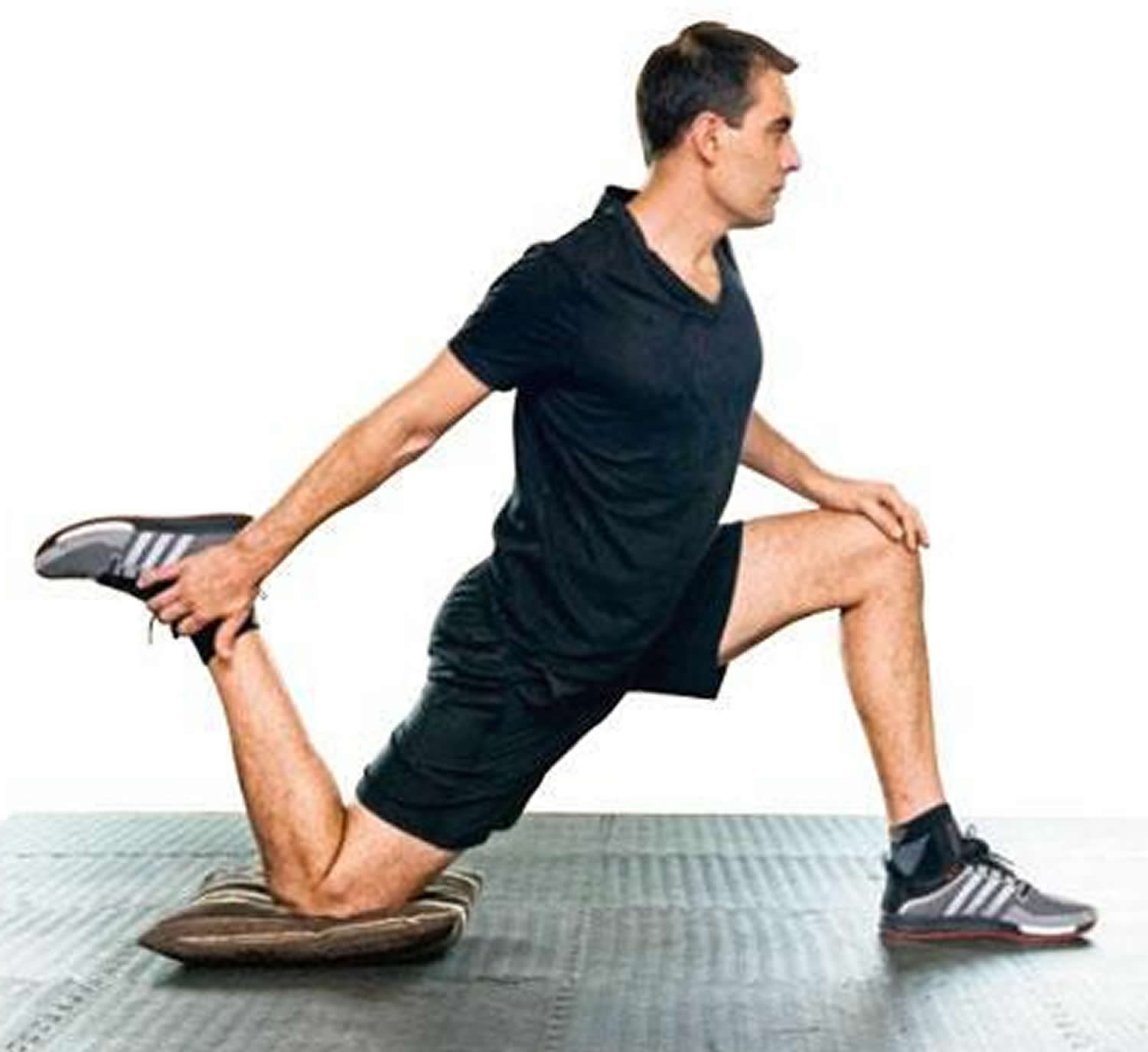
- Deep Lunge
Kneel on one knee, the other foot in front. Facing forwards, lift the back knee up. Hold for 5 seconds. Repeat 3 times on each side.
Figure 7. Deep Lunge
One-leg stand (front)
Holding onto something for support if needed, bend one leg up behind you. Hold for 5 seconds. Repeat 3 times on each side.
Figure 8. One-leg stand (front)
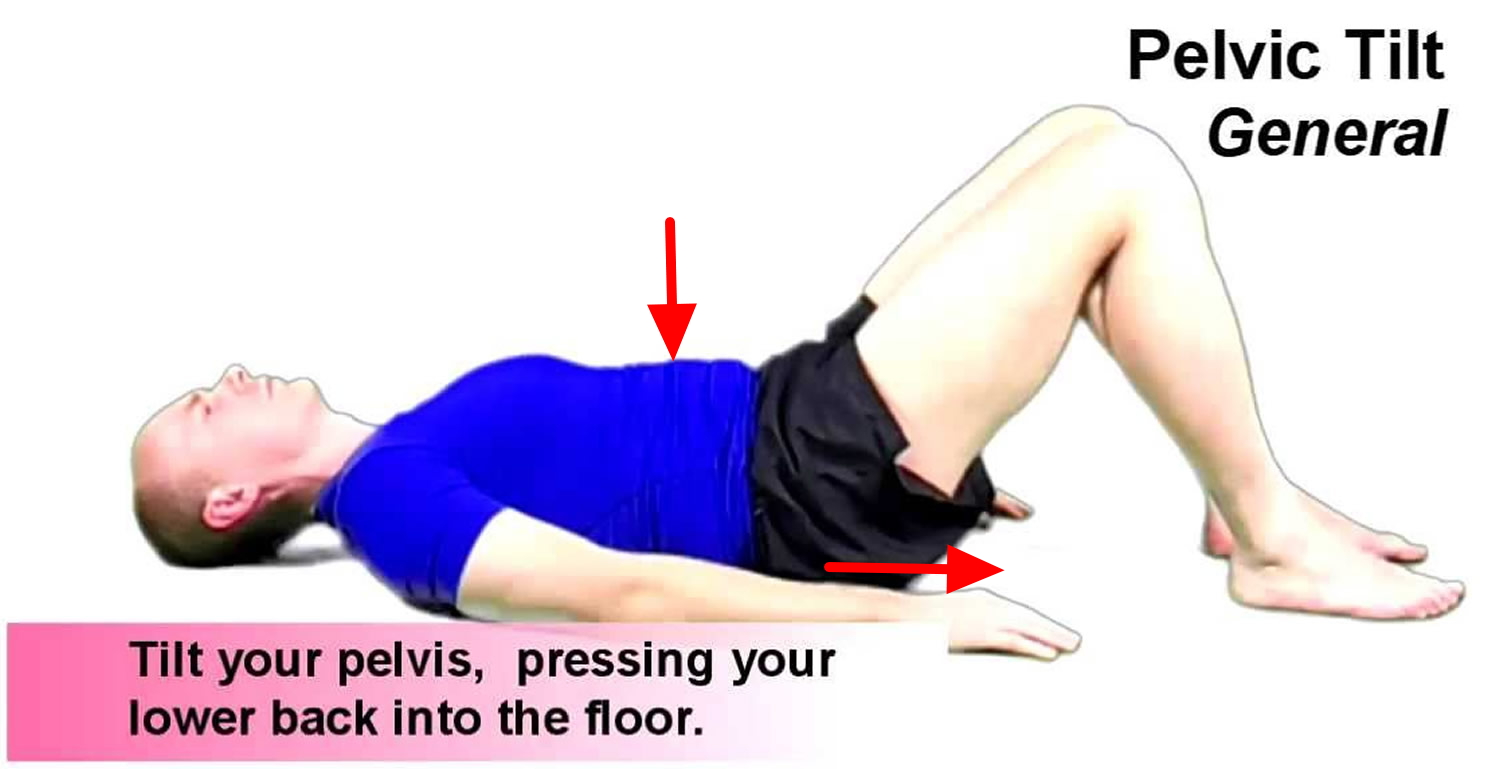
Pelvic tilt
Lie down with your knees bent. Tighten your stomach muscles, flattening your back against the floor. Hold for 5 seconds. Repeat 5 times.
Figure 9. Pelvic tilt
Knees to chest
Lie on your back, knees bent. Bring one knee up and pull it gently into your chest for 5 seconds. Repeat up to 5 times on each side.
Figure 10. Knees to chest
Manual therapy
Manual therapy is a technique where a physiotherapist uses their hands to manipulate, mobilize and massage the body tissues.
This can help:
- relieve pain and stiffness
- improve blood circulation
- help fluid drain more efficiently from parts of the body
- improve the movement of different parts of the body
- promote relaxation
Manual therapy can be used to treat specific problems, such as back pain, but may also be useful for a range of conditions that don’t affect the bones, joints or muscles.
For example, massage may improve quality of life for some people with serious or long-term conditions by reducing levels of anxiety and improving sleep quality.
Manual techniques are also used to help certain lung conditions.
Alternative medicine
Some alternative and complementary medicine treatments might help ease chronic back pain. Examples include:
- Chiropractic – spinal manipulation has been found to be moderately effective for low back pain that has lasted for at least a month.
- Yoga. A combination of physical activity, breathing exercises and meditation, yoga can improve function and relieve chronic back pain in some people.
- Acupuncture – where fine needles are inserted into specific points of the body, with the aim of reducing pain and promoting recovery.
- Transcutaneous Electrical Nerve Stimulation (TENS) – a small, battery-operated device is used to deliver an electric current to the affected area, with the aim of relieving pain.
- Ultrasound – where high-frequency sound waves are used to treat deep tissue injuries by stimulating blood circulation and cell activity, with the aim of reducing pain and spasms, as well as speeding up healing.
- Massage. This hands-on therapy can provide short-term relief to people dealing with chronic low back pain.
Steroid injections
If medicine and physical therapy aren’t helping, your doctor may suggest steroid injections. Inflammation-suppressing corticosteroids may be given by injection directly into the area around the spinal nerves. Transforaminal epidural steroid injection is recommended to provide short-term (2–4 week) help provide pain relief in patients with lumbar disc herniations with radiculopathy. Spinal imaging can help guide the needle more safely. Occasionally a course of oral steroids may be tried to reduce swelling and inflammation. The steroids reduce the swelling around the disc and can lessen the pain. Sometimes 1 injection is enough. Often they are given in a series of shots over a few weeks. These injections can bring relief for weeks or months at a time.
Herniated disc surgery
If nothing else is helping your pain, your doctor may want to do surgery. He or she will remove all or part of the damaged disc so it no longer presses on the nerve.
Only a small percentage of patients with disc herniations eventually need surgery. Your doctor may suggest surgery if conservative treatments fail to improve your symptoms after six weeks, especially if you continue to experience:
- Numbness or weakness
- Difficulty standing or walking
- Loss of bladder or bowel control
In many cases, surgeons can remove just the protruding portion of the disc. Rarely, however, the entire disc must be removed. In these cases, the vertebrae may need to be fused together with metal hardware to provide spinal stability to allow the process of bone fusion, which takes months. Rarely, your surgeon might suggest the implantation of an artificial disc.
- Lumbar microdiskectomy. This is the most common procedure for a herniated disk in the lower back. Microdiskectomy involves removing the herniated part of the disc and any fragments that are putting pressure on the spinal nerve.
- Cervical diskectomy and fusion. Cervical diskectomy is a procedure for the herniated disc in the neck. To relieve pressure, the entire herniated disc is removed. Bone is placed in the disc space and a metal plate may be used to help support the spine.
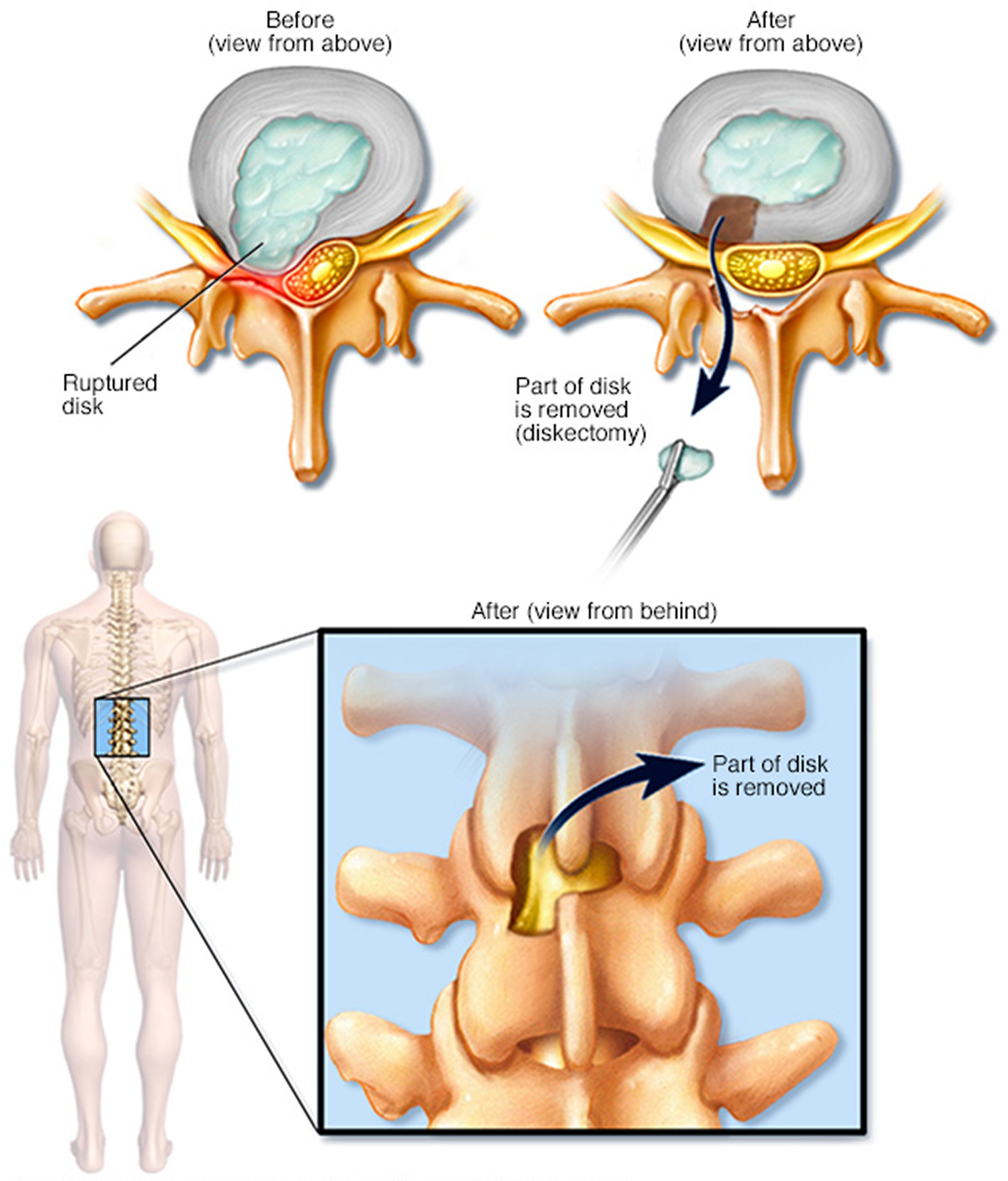
Figure 11. Diskectomy
Note: Diskectomy is the surgical removal of the damaged portion of a herniated disc in your spine. A herniated disc occurs when some of the softer material inside the disc pushes out through a crack in the tougher exterior. This can irritate or compress nearby nerves and cause pain, numbness or weakness.
Home treatment
You can practice good home care to treat your disc, as well. Good posture can help your back by reducing the pressure on your disc. Focus on standing up straight, sitting straight, and lifting with your back straight. Follow these tips to do what you can on your own to ease your symptoms.
- Heat or cold treatment, such as placing a heat or cold pack on the affected area. Initially, cold packs can be used to relieve pain and inflammation. After a few days, you may switch to gentle heat to give relief and comfort.
- Bend your knees and hips when you lift something, and keep your back straight.
- Hold an object close to your body when you carry it.
- If you stand for a long time, put one foot on a small stool or box for a while.
- If you sit for a long time, put your feet on a small stool so your knees are higher than your hips.
- Don’t wear high-heeled shoes.
- Don’t sleep on your stomach.
- Avoid too much bed rest. Too much bed rest can lead to stiff joints and weak muscles — which can complicate your recovery. Instead, rest in a position of comfort for 30 minutes, and then go for a short walk or do some work. Try to avoid activities that worsen your pain during the healing process.
- Take pain relievers. Over-the-counter medications — such as ibuprofen (Advil, Motrin IB, others) or naproxen (Aleve, others) — may help reduce the pain associated with a herniated disc.
Most people with acute back pain improve rapidly within a month, often without treatment. Some continue to have pain for longer. Some might have a repeat of the pain at another time, while others won’t.
Living with a herniated disc
Your chances of getting better are good. Most people who have a herniated disc are better in about 4 weeks. Sometimes it takes longer. If you still have pain or numbness after 4 to 6 weeks, or if you feel worse, talk with your doctor. Sometimes it takes surgery to relieve pain.
Herniated disc prognosis
Studies vary on outcomes of herniated disc prognosis, but the majority of cases respond to conservative management 15. One study did show that 30% of patients complain of back pain at one year 18. Many cases of disc herniation are asymptomatic and are found by accident on advanced imaging. Of symptomatic disc herniation cases, 90% of them resolve at six weeks following injury. Surgery may lead to more rapid recovery of the symptomatic herniated disc, but results are also similar to conservative management at one year post-operatively 19, 20, 14, 21. A review of over 600 patients concluded that non-contained disc herniations may respond more successfully to nonsurgical treatment 22. Epidural steroid injections can be used at almost any time; however, the use of steroid injection has been questioned 23.
- Waxenbaum JA, Futterman B. Anatomy, Back, Intervertebral Discs. [Updated 2018 Dec 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470583[↩]
- van Uden S, Silva-Correia J, Oliveira JM, Reis RL. Current strategies for treatment of intervertebral disc degeneration: substitution and regeneration possibilities. Biomater Res. 2017;21:22[↩]
- Huang YC, Hu Y, Li Z, Luk KDK. Biomaterials for intervertebral disc regeneration: Current status and looming challenges. J Tissue Eng Regen Med. 2018 Nov;12(11):2188-2202[↩]
- BROWN HA, PONT ME. DISEASE OF LUMBAR DISCS. TEN YEARS OF SURGICAL TREATMENT. J Neurosurg. 1963 May;20:410-7. doi: 10.3171/jns.1963.20.5.0410[↩]
- Amin RM, Andrade NS, Neuman BJ. Lumbar Disc Herniation. Curr Rev Musculoskelet Med. 2017 Dec;10(4):507-516. doi: 10.1007/s12178-017-9441-4[↩]
- Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001 Feb 1;344(5):363-70. doi: 10.1056/NEJM200102013440508[↩]
- Fjeld OR, Grøvle L, Helgeland J, Småstuen MC, Solberg TK, Zwart JA, Grotle M. Complications, reoperations, readmissions, and length of hospital stay in 34 639 surgical cases of lumbar disc herniation. Bone Joint J. 2019 Apr;101-B(4):470-477. doi: 10.1302/0301-620X.101B4.BJJ-2018-1184.R1[↩][↩]
- Petersen T, Laslett M, Juhl C. Clinical classification in low back pain: best-evidence diagnostic rules based on systematic reviews. BMC Musculoskelet Disord. 2017 May 12;18(1):188. doi: 10.1186/s12891-017-1549-6[↩]
- Acute low back problems in adults: assessment and treatment. Acute Low Back Problems Guideline Panel. Agency for Health Care Policy and Research. Am Fam Physician. 1995 Feb 1;51(2):469-84.[↩]
- Katz JN, Dalgas M, Stucki G, Katz NP, Bayley J, Fossel AH, Chang LC, Lipson SJ. Degenerative lumbar spinal stenosis. Diagnostic value of the history and physical examination. Arthritis Rheum. 1995 Sep;38(9):1236-41. doi: 10.1002/art.1780380910[↩]
- Hall S, Bartleson JD, Onofrio BM, Baker HL Jr, Okazaki H, O’Duffy JD. Lumbar spinal stenosis. Clinical features, diagnostic procedures, and results of surgical treatment in 68 patients. Ann Intern Med. 1985 Aug;103(2):271-5. doi: 10.7326/0003-4819-103-2-271[↩]
- Chou R, Qaseem A, Owens DK, Shekelle P; Clinical Guidelines Committee of the American College of Physicians. Diagnostic imaging for low back pain: advice for high-value health care from the American College of Physicians. Ann Intern Med. 2011 Feb 1;154(3):181-9. doi: 10.7326/0003-4819-154-3-201102010-00008. Erratum in: Ann Intern Med. 2012 Jan 3;156(1 Pt 1):71.[↩]
- Al Qaraghli MI, De Jesus O. Lumbar Disc Herniation. [Updated 2023 Aug 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560878[↩][↩]
- Schoenfeld AJ, Weiner BK. Treatment of lumbar disc herniation: Evidence-based practice. Int J Gen Med. 2010 Jul 21;3:209-14. doi: 10.2147/ijgm.s12270[↩][↩]
- Dydyk AM, Ngnitewe Massa R, Mesfin FB. Disc Herniation. [Updated 2023 Jan 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441822[↩][↩][↩][↩]
- De Cicco FL, Camino Willhuber GO. Nucleus Pulposus Herniation. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542307[↩]
- Dydyk AM, Khan MZ, Singh P. Radicular Back Pain. [Updated 2022 Oct 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546593[↩]
- Amlie E, Weber H, Holme I. Treatment of acute low-back pain with piroxicam: results of a double-blind placebo-controlled trial. Spine (Phila Pa 1976). 1987 Jun;12(5):473-6. doi: 10.1097/00007632-198706000-00010[↩]
- Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Hanscom B, Skinner JS, Abdu WA, Hilibrand AS, Boden SD, Deyo RA. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006 Nov 22;296(20):2441-50. doi: 10.1001/jama.296.20.2441[↩]
- Weinstein JN, Lurie JD, Tosteson TD, Skinner JS, Hanscom B, Tosteson AN, Herkowitz H, Fischgrund J, Cammisa FP, Albert T, Deyo RA. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA. 2006 Nov 22;296(20):2451-9. doi: 10.1001/jama.296.20.2451[↩]
- Buttermann GR. Treatment of lumbar disc herniation: epidural steroid injection compared with discectomy. A prospective, randomized study. J Bone Joint Surg Am. 2004 Apr;86(4):670-9. https://journals.lww.com/jbjsjournal/abstract/2004/04000/treatment_of_lumbar_disc_herniation__epidural.2.aspx[↩]
- Nakagawa H, Kamimura M, Takahara K, Hashidate H, Kawaguchi A, Uchiyama S, Miyasaka T. Optimal duration of conservative treatment for lumbar disc herniation depending on the type of herniation. J Clin Neurosci. 2007 Feb;14(2):104-9. doi: 10.1016/j.jocn.2006.08.001[↩]
- Iversen T, Solberg TK, Romner B, Wilsgaard T, Twisk J, Anke A, Nygaard O, Hasvold T, Ingebrigtsen T. Effect of caudal epidural steroid or saline injection in chronic lumbar radiculopathy: multicentre, blinded, randomised controlled trial. BMJ. 2011 Sep 13;343:d5278. doi: 10.1136/bmj.d5278[↩]